Dr Nicola Pritchard.pdf
Dr Nicola Pritchard.pdf
Dr Nicola Pritchard.pdf
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Dr</strong> <strong>Nicola</strong> <strong>Pritchard</strong><br />
May 2011
Why Breast feed?<br />
Immediate Benefits<br />
Nutritionally complete<br />
Hormones<br />
Growth factors<br />
Nucleotides<br />
Enzymes<br />
LC PUFA<br />
Live cells
Breast feeding -Longterm<br />
Long term Benefits<br />
Small effect BP (2mmHg)<br />
22% reduction in adult obesity<br />
Reduced cholesterol<br />
19-27% reduction IDDM<br />
39% reduction NIDDM<br />
36% reduction SIDS<br />
4.9 points IQ
Exclusive Breast Feeding UK<br />
Infant Feeding Survey 2005<br />
78% Initiation rates<br />
35% exclusively breastfed at one week<br />
21 % at six weeks<br />
7% at four months<br />
3% at five months<br />
Reduction<br />
Second baby<br />
Socioeconomic<br />
Education<br />
Age of mother<br />
ONS 2005 (2010 results due 2013)
UNICEF Baby Friendly<br />
Breast feeding Policy<br />
Education and Advice<br />
Early first feed<br />
Skin-to-skin<br />
Privacy<br />
Adequate rest, food and drink<br />
Support for expressing<br />
Formula milk should not be given to breastfed<br />
babies unless medically indicated.<br />
Avoid dummies
RBH<br />
Breast Feeding Clinic<br />
Contact<br />
Rose Tilbury, Lead Midwife for Breast Feeding<br />
Breastfeeding clinic hours<br />
Weekday 10.00am - 13.00pm<br />
Appointments 322 8964.<br />
Breastfeeding classes<br />
Maternity unit Tuesday 2-4pm<br />
To book Tel: 322 8964 between 9-5pm.
Breastfeeding<br />
How to know if it is successful?<br />
Indicators of good attachment and positioning<br />
mouth wide open<br />
less areola visible underneath the chin than above nipple<br />
chin touching breast, lower lip rolled down, and nose free<br />
no pain<br />
Indicators of successful feeding in babies<br />
audible and visible swallowing<br />
sustained rhythmic suck<br />
relaxed arms and hands<br />
moist mouth<br />
regular soaked/heavy nappies<br />
Indicators of successful breastfeeding in women<br />
breast softening<br />
no compression of the nipple at the end of the feed<br />
woman feels relaxed and sleepy.
When should a new mother<br />
be advised against breastfeeding?<br />
Diagnosis of galactosaemia<br />
Pregestamil or soya formula<br />
+/- HIV<br />
+/- Hepatitis B<br />
IMPORTANT WHO Advice<br />
<br />
All infants must be managed individually; insufficient<br />
growth or other adverse outcomes not to be ignored
Mastitis<br />
Women should be offered assistance & advice<br />
Positioning and attachment<br />
Continue breastfeeding and/or hand<br />
expression<br />
Analgesia compatible with breastfeeding<br />
Increase fluid intake.
Advantages of<br />
Pre-term Maternal Milk<br />
Higher macrophages and Ig A<br />
More energy, lipid, LC PUFA, Protein, iron and<br />
vitamins<br />
Skin to skin – Maternal Ig A transfer<br />
Need to express at least 4 x day<br />
Aim for 100mins a day
Milk Banks<br />
Collection of donor “drip milk” from term mothers<br />
Positive<br />
79% reduction in NEC<br />
But<br />
NOT preterm milk<br />
Fore rather than hind milk<br />
Lower protein, sodium zinc and copper<br />
Loss of “live” immune protection<br />
Viral infection risk
What should I do?<br />
Breast fed pre-term infant not gaining weight<br />
Options<br />
Increase volume<br />
Check for other reasons<br />
Fortify?<br />
Evidence for fortifying milk<br />
Short term improved weight gain<br />
No evidence for increase in NEC<br />
? Osmolality
General Advice<br />
Breast Milk Fortifiers<br />
Max volumes of EBM tolerated first<br />
Only use after first 2 weeks<br />
Fortify milk as close as possible to the feed<br />
time.<br />
Assess closely for feed intolerance<br />
Change only one thing at a time<br />
Do not use if strong FHx of atopy<br />
Don’t add to preterm or term formula
Formula milks<br />
Whey based<br />
More similar to breast milk<br />
Caesin based<br />
Claimed to be better for hungry babies<br />
Strict guidelines<br />
More calcium and phosphate than cows milk<br />
More iron<br />
LC PUFA<br />
Component of cell membrane of CNS and retina
Follow on milks<br />
UK recommendations for term infants<br />
Not prior to 6 months<br />
Why<br />
More iron (cover low iron weaning)<br />
More vitamin D<br />
Less saturated fatty acids<br />
Not required if thriving
What the Mum’s want to know
Nucleotides<br />
Evidence available to support<br />
Growth enhancement of babies born light for<br />
gestational age<br />
Decreased episodes of diarrhoea<br />
Greater antibody responses to primary<br />
immunisations<br />
Theoretical<br />
Changes in lipid metabolism - ? Effect<br />
Br J Nutr. 2007 Immune response to nucleotide-supplemented infant formulae: systematic review &<br />
meta-analysis.
Pre and Probiotics<br />
Breast fed infants colonised within 12-24 hrs<br />
Bifidobacteria and Lactobacilli<br />
Fermentation of carbohydrates<br />
Causes fall in colonic pH<br />
Favours growth of non-pathogenic species<br />
Improved mucosal barrier
Pre and Probiotics<br />
Prebiotics<br />
Currently Added<br />
Non-digestable<br />
oligosaccharides<br />
Mimics breast milk<br />
Promotes bowel flora<br />
similar to breast fed<br />
infants<br />
Studies underway for<br />
preterm formula<br />
<br />
The Preterm Prebiotic Study Imperial College<br />
Neena Modi, ?Improved feed intolerance<br />
Probiotic<br />
Not recommended<br />
Live microbial food<br />
supplement<br />
Colonise GI tract<br />
Synthesise<br />
Short chain fatty acids<br />
Amino acids<br />
?Infection risk<br />
?How much<br />
?Regulation<br />
?Which organism
Prebiotics in Formula<br />
Stool flora similar to breast fed infants<br />
?Reduction in diarrhoeal episodes<br />
Prebiotics for prevention of allergic disease or<br />
food reactions<br />
Insufficient evidence COCHRANE 2008
Probiotics & Preterm Infants<br />
Reduces the occurrence of NEC (stage 2) and death
Long Chain<br />
Poly Unsaturated Fatty Acids<br />
Docosahexanoeic Acid (DHA Omega 3)<br />
Arachidonic Acid (AA Omega 6)<br />
Variable amounts in breast milk<br />
Constituent of cell membranes and retina<br />
Small studies support improved visual and<br />
cognitive development<br />
Recent RCT Jan 2010 J Ped Gast & Nut<br />
No difference in Baileys at 18 months
Preterm Formula<br />
Standard preterm formula<br />
Usually until 2-2.5kg<br />
More calories and protein than breast milk<br />
Amino acids similar to breast milk<br />
LC PUFA<br />
Vit D
NEC Risk<br />
Formula vs EBM<br />
Exclusively formula fed<br />
6 x rate of NEC<br />
Mixed BF and formula<br />
3 x rate of NEC<br />
Breast Milk<br />
Matures GI tract<br />
Alters bowel flora<br />
Source of growth factors<br />
Matures and provides immune factors
How to feed<br />
Minimal enteral feeds<br />
Orogastric vs Nasogastric<br />
?Transpyloric<br />
Continuous vs Bolus (Cochrane 2008 Insuff evidence)<br />
Demand vs Timed (Cochrane 2008 Insuff evidence)<br />
Non-nutritive sucking
ADEPT Abnormal Doppler Enteral Prescription Trial<br />
Entry Criteria<br />
Antenatal ultrasound<br />
<br />
Absent or reversed EDF or Cerebral redistribution<br />
Pre-term:<br />
Post Discharge Formula<br />
Most pre term infants discharged small for<br />
gestation<br />
Rapid growth – high calorific requirement<br />
Can consume 300mls/kg/day normal formula<br />
<br />
Not an issue if tolerated<br />
Increased risk of long-term growth failure<br />
Better catch up<br />
<br />
Theoretically better brain growth – but not proven
Post discharge Formula<br />
ESPHGAN position statement May 2006<br />
If appropriate wt for gestn: Breast or term<br />
formula<br />
Post discharge formula if not<br />
How long?<br />
At least until CGA 40 weeks<br />
Possibly until CGA 52 weeks<br />
EG Nutriprem 2<br />
RBH Guideline being developed<br />
Halway between preterm and term formula
Is it Milk Allergy Doctor?<br />
Diarrhoea<br />
Pain<br />
Flatus and abdominal distention<br />
Perianal excoriation<br />
Other – older children<br />
<br />
Non specific symptoms such as headache or fatigue<br />
Investigations – not necessary<br />
<br />
Positive stool reducing substances supportive
Lactose Intolerance<br />
Congenital form rare - from birth<br />
Secondary<br />
Onset in infants/children<br />
Secondary to GI infection<br />
<br />
Self limiting in majority in 6=8 weeks<br />
Non resolving consider coeliac disease<br />
Primary Inherited Lactase deficiency<br />
Usually adolescent onset in UK population<br />
Non specific symptoms: thought secondary to effects of<br />
bacterial short chain fatty acid uptake<br />
Can usually tolerate 240mls milk/day<br />
Lactase capsules can be helpful
Infant Management<br />
Infant Treatment<br />
Avoid lactase and maintain nutrition<br />
At least 6 weeks if post gastroenteritis<br />
Lactose free formula<br />
Commercial lactose free or prescribable formula<br />
SMA LF<br />
Cow and Gate Comfort<br />
Enfamil LF<br />
Pregestamil<br />
Nutramigen<br />
Soya milks (consider if >6 months)<br />
Lactose free cows milk if > 12 months
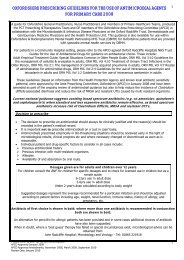
Soya formulae<br />
BDA 2004<br />
<br />
<br />
<br />
<br />
ONLY INDICATIONS<br />
Galactosaemia<br />
Second line for other<br />
NOT FOR<br />
CMPI<br />
Anaphylaxis<br />
Not < 6 months<br />
No evidence<br />
Reduction in: colic/crying/allergy<br />
CONCERNS<br />
Poorer nitrogen source<br />
Phytate may affect absorption of minerals/iodine<br />
<br />
<br />
10x aluminium content<br />
Phyto-oestrogens<br />
Male infertility and menstrual disturbance
Is it Milk Allergy Doctor?<br />
Reaction within hours of ingestion<br />
Blotchy facial rash<br />
Vomiting<br />
Atopic FHx<br />
Investigations?<br />
+/- Positive RAST/skin<br />
+/- Elevated total Ig E<br />
NB Can occur with NEGATIVE tests
Type 1 Hypersensitivity<br />
Cows Milk Allergy<br />
Differentiate from intolerance<br />
Eliminate all cows milk, mammalian milk and<br />
soya<br />
Advise re life threatening features<br />
Refer to paediatrician<br />
Treatment: Avoid ALL animal and soya milk<br />
products until 18 months
Anaphylaxis<br />
Type 1 Hypersensitivity<br />
Milk options<br />
Fully hydrolysed Nutramigen 1 and 2<br />
Elemental<br />
Over 1 year<br />
Aptamil Pepti<br />
Pepti Junior<br />
Neocate/Neocate Active<br />
Nutramigen AA<br />
<br />
Calcium enriched vegetable milks
Is it Milk Allergy Doctor?<br />
Age 1 week – 3 months<br />
Bloody diarrhoea<br />
Malabsorption<br />
GOR Sx
Cows Milk Protein<br />
Intolerance<br />
Non Ig E Mediated<br />
Delayed and cumulative effect<br />
Gastro-oesophageal reflux/Vomiting<br />
Diarrhoea<br />
Constipation<br />
Colic<br />
Blood in stool (commoner infants)<br />
Iron deficiency anaemia<br />
Dermatitis/Eczema<br />
Rhinitis<br />
NB No evidence milk free diet improves wheeze
Management<br />
No specific supportive test<br />
Can occur in breast fed infants<br />
Diagnosis due to resolution of symptoms on<br />
exclusion diet<br />
Maternal dairy free diet<br />
Dairy and soya free diet<br />
Refer if under 1 year
Cows Milk Protein Intolerance<br />
Milk options<br />
Partially hydrolysed<br />
Pregestamil<br />
Nan HC<br />
Fully hydrolysed Nutramigen 1 and 2<br />
Aptamil Pepti<br />
Pepti Junior<br />
Elemental<br />
Neocate/Neocate Active<br />
Nutramigen AA<br />
NB Advise parents NOT same as lactose intolerance or<br />
anaphylaxis
On going Management<br />
Tolerance improves with age<br />
May tolerate some soya and/or dairy desserts<br />
or cheese towards age of 1 year<br />
Usually tolerate cows milk by 18 months - 2<br />
years<br />
Can rechallenge in community if > 1year and<br />
no history suggestive of type 1 reaction
Is it Milk Allergy Doctor?<br />
< 9 months<br />
Delayed reaction (hours not immediate) after milk<br />
ingestion<br />
Severe diarrhoea and dehydration<br />
Vomiting<br />
Collapse<br />
May appear like sepsis<br />
Also may occur with rice, cereals or meats
Food Protein Induced Enterocolitis<br />
Non Ig E mediated<br />
Older age of onset than Cow milk protein<br />
Enterocolitis<br />
Profuse D&V, dehydration and shock<br />
Elevated blood leucocytes<br />
Due to release of TNF alpha<br />
Referral to Tertiary Allergy Specialist for<br />
careful exclusion diet of milk, animal and<br />
cereal proteins
Is it Milk Allergy Doctor<br />
Older child<br />
GORD symptoms unresponsive to medical<br />
therapy<br />
+/- Atopy<br />
Normal or elevated blood Eosinophils
Eosinophilic Oesophagitis<br />
Biopsy diagnosis<br />
Increasingly common diagnosis (10:100,000)<br />
Treatment Options<br />
Refer to paediatric gastroenterology<br />
Exclusion diet - Neocate
Goats Milk Formula<br />
Goat infant formula not really available in UK<br />
Commonest mammalian milk in UK Goat milk<br />
Not nutritionally complete<br />
Low folic acid<br />
Higher saturated fats<br />
Often unpasteurised –risk of TB<br />
Not for
Other Mammalian milks<br />
Type 1 Reactions and CMPI<br />
High cross-reactivity to cows milk DO NOT USE<br />
Lactose Intolerance<br />
Lactose content very similar in all<br />
Cow 4.7%, Goat 4.7%, Buffalo 4.86%<br />
Yak 4.93%, Sheep 4.6%<br />
Apparently bear and kangaroo milk are low<br />
lactose
Rice Milk<br />
No lactose<br />
Low calcium<br />
Low cholesterol<br />
RESTRICTIONS<br />
“High” levels of inorganic arsenic<br />
FSA - Not for under 5 years (May 2009)<br />
Always recommend calcium enriched
Oat Milk<br />
Suitable for vegans<br />
No lactose<br />
No cholesterol<br />
Lower protein<br />
Low vitamins and calcium<br />
Commercial brands of milks<br />
Fortified with calcium equivalent to cows milk
Prescribable Formula<br />
Hydrolysed Formula<br />
Elemental Formula<br />
Hydrolysed milk<br />
protein<br />
Hypoallergenic<br />
Examples<br />
Pregestamil<br />
Nutramigen<br />
Nan HC<br />
Aptamil Pepti<br />
Synthetic amino<br />
acids<br />
For severe<br />
malabsorption or<br />
allergy<br />
Examples<br />
Neocate<br />
Nutramigen AA
Other Formulas<br />
Thickened formula<br />
Enfamil AR<br />
SMA Staydown<br />
Cow and Gate Comfort<br />
Anti-colic ?Evidence<br />
Low Lactose
High Energy options<br />
SMA High Energy (0.9kcal/ml)<br />
Infatrini (1kcal/ml)<br />
Similac (1kcal/ml)<br />
Duocal – carbohydrate and fat<br />
Maxijul- carbohydrate<br />
Concentrating formula?<br />
Powder first water second
Thank<br />
you