the cultural formulation: a method for assessing cultural factors
the cultural formulation: a method for assessing cultural factors
the cultural formulation: a method for assessing cultural factors
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Psychiatric Quarterly, Vol. 73, No. 4, Winter 2002 ( C○ 2002)<br />
THE CULTURAL FORMULATION: A METHOD<br />
FOR ASSESSING CULTURAL FACTORS<br />
AFFECTING THE CLINICAL ENCOUNTER<br />
Roberto Lewis-Fernández, M.D.<br />
and Naelys Díaz, M.S.W.<br />
The growing <strong>cultural</strong> pluralism of US society requires clinicians to examine <strong>the</strong><br />
impact of <strong>cultural</strong> <strong>factors</strong> on psychiatric illness, including on symptom presentation<br />
and help-seeking behavior. In order to render an accurate diagnosis across<br />
<strong>cultural</strong> boundaries and <strong>for</strong>mulate treatment plans acceptable to <strong>the</strong> patient,<br />
clinicians need a systematic <strong>method</strong> <strong>for</strong> eliciting and evaluating <strong>cultural</strong> in<strong>for</strong>mation<br />
in <strong>the</strong> clinical encounter. This article describes one such <strong>method</strong>, <strong>the</strong><br />
Cultural Formulation model, expanding on <strong>the</strong> guidelines published in DSM-IV.<br />
It consists of five components, <strong>assessing</strong> <strong>cultural</strong> identity, <strong>cultural</strong> explanations<br />
of <strong>the</strong> illness, <strong>cultural</strong> <strong>factors</strong> related to <strong>the</strong> psychosocial environment and levels<br />
of functioning, <strong>cultural</strong> elements of <strong>the</strong> clinician–patient relationship, and<br />
<strong>the</strong> overall impact of culture on diagnosis and care. We present a brief historical<br />
overview of <strong>the</strong> model and use a case scenario to illustrate each of its<br />
Roberto Lewis-Fernández, M.D., is an Assistant Professor of Clinical Psychiatry at<br />
Columbia University, a Lecturer on Social Medicine at Harvard University, and is <strong>the</strong><br />
Director of <strong>the</strong> Hispanic Treatment Program at NY State Psychiatric Institute, New<br />
York, NY.<br />
Naelys Díaz, M.S.W., is a Doctoral Candidate in Social Work at Fordham University.<br />
Address correspondence to Roberto Lewis-Fernández, M.D., New York State Psychiatric<br />
Institute, Unit 69, 1051 Riverside Drive, New York, NY 10032; e-mail: rlewis@<br />
nyspi.cpmc.columbia.edu.<br />
271<br />
0033-2720/02/1200-0271/0 C○ 2002 Human Sciences Press, Inc.
272 PSYCHIATRIC QUARTERLY<br />
components and <strong>the</strong> substantial effect on illness course and treatment outcome<br />
of implementing <strong>the</strong> model in clinical practice.<br />
KEY WORDS: <strong>cultural</strong> <strong><strong>for</strong>mulation</strong>; diagnostic assessment; <strong>cultural</strong> psychiatry; popular<br />
syndromes; Latinos.<br />
As rising immigration causes industrialized societies to become even<br />
more <strong>cultural</strong>ly pluralistic and organized mental health services in developing<br />
nations face <strong>the</strong> challenge of distributing care more broadly,<br />
psychiatrists will increasingly come in contact with a larger diversity<br />
of social groups (1). The evaluation of patients from disparate ethno<strong>cultural</strong><br />
backgrounds requires clinicians to assess <strong>the</strong> impact of <strong>cultural</strong><br />
<strong>factors</strong> on all aspects of psychiatric illness, including symptom<br />
presentation and help-seeking behavior. In order to render an accurate<br />
diagnosis across <strong>cultural</strong> boundaries and <strong>for</strong>mulate treatment plans<br />
acceptable to <strong>the</strong> patient and oftentimes <strong>the</strong> family, clinicians need a<br />
<strong>method</strong> <strong>for</strong> eliciting and evaluating <strong>cultural</strong> in<strong>for</strong>mation during <strong>the</strong><br />
clinical encounter.<br />
Standardizing <strong>the</strong> assessment <strong>method</strong> is particularly important in order<br />
to avoid systematic misjudgments of which <strong>the</strong> clinician is often unaware.<br />
An example of this is <strong>the</strong> apparent clinician bias that results in<br />
a higher rate of misdiagnosis of paranoid schizophrenia among African<br />
American and Latino patients suffering from bipolar disorder or depression<br />
with psychotic features, compared to non-Latino Whites (2,3).<br />
In one key study, misdiagnosis by race was found to be related to<br />
“in<strong>for</strong>mation variance,” differences in <strong>the</strong> amount of in<strong>for</strong>mation <strong>the</strong><br />
predominantly White clinicians obtained from African American as opposed<br />
to White patients, ra<strong>the</strong>r than race-specific discrepancies in <strong>the</strong><br />
way diagnostic criteria were applied (“criterion variance”) (4). This suggests<br />
that standardizing <strong>the</strong> process of clinical in<strong>for</strong>mation-ga<strong>the</strong>ring<br />
would reduce misdiagnosis.<br />
Using a systematic <strong>method</strong> <strong>for</strong> <strong>assessing</strong> <strong>cultural</strong> contributions to<br />
illness presentation would also help <strong>the</strong> clinician diagnose <strong>cultural</strong>ly<br />
patterned experiences of illness that are distinct from mainstream psychiatric<br />
diagnostic criteria. Many societies around <strong>the</strong> world have developed<br />
folk mental health classification systems that are distinct from<br />
US psychiatric nosology (5,6). Patients from <strong>the</strong>se societies and <strong>cultural</strong><br />
backgrounds often express distress and psychopathology less in accord<br />
with US diagnostic categories than with <strong>the</strong>ir popular syndromes.<br />
The translation between popular and professional nosologies is often<br />
complicated. Neuras<strong>the</strong>nia, <strong>for</strong> example, originally a US professional
ROBERTO LEWIS-FERNÁNDEZ AND NAELYS DÍAZ 273<br />
diagnosis that is no longer included in <strong>the</strong> DSM system but is retained<br />
in ICD-10, is <strong>the</strong> most prevalent current (12-month) disorder among<br />
Chinese Americans in Los Angeles County (7). For US psychiatrists,<br />
however, it presents a diagnostic challenge, due to its partial overlap<br />
with multiple diagnostic categories, including mood, anxiety, and somato<strong>for</strong>m<br />
disorders (7,8).<br />
Ataque de nervios (attacks of nerves), on which we will focus later<br />
in this article, is ano<strong>the</strong>r example of a popular category that presents<br />
diagnostic challenges <strong>for</strong> US psychiatrists. This Latino syndrome is<br />
characterized by paroxysms of intense emotionality, acute anxiety<br />
symptoms, and loss of control, often associated with dissociative experiences<br />
and occasionally with o<strong>the</strong>r- or self-directed aggressive behaviors<br />
(9). It constitutes <strong>the</strong> second most prevalent psychopathological<br />
syndrome in Puerto Rico and has a complex relationship with psychiatric<br />
diagnoses (10). Mainly associated with mood and anxiety disorders,<br />
it also can occur in conjunction with dissociative disorders (11)<br />
and in individuals with impulse control, somato<strong>for</strong>m, or psychotic disorders.<br />
The existence of <strong>the</strong>se popular syndromes and <strong>the</strong> need <strong>for</strong> a<br />
case-by-case translation into DSM-IV categories underscores <strong>the</strong> risks<br />
of not obtaining sufficient <strong>cultural</strong> in<strong>for</strong>mation as part of <strong>the</strong> diagnostic<br />
assessment.<br />
In order to deliver care that is <strong>cultural</strong>ly valid, <strong>the</strong>re<strong>for</strong>e, clinicians<br />
need a <strong>method</strong> that systematically allows <strong>the</strong>m to take culture into<br />
account when conducting a clinical evaluation. One such <strong>method</strong> that<br />
has been operationalized in recent years is <strong>the</strong> Cultural Formulation<br />
(CF) model. The CF model supplements <strong>the</strong> biopsychosocial approach<br />
by highlighting <strong>the</strong> effect of culture on <strong>the</strong> patient’s symptomatology,<br />
explanatory models of illness, help-seeking preferences, and outcome<br />
expectations (12–15). It is described in Appendix I of DSM-IV (16) and<br />
is recommended <strong>for</strong> implementation during <strong>the</strong> assessment phase of<br />
every clinical relationship.<br />
The CF model is especially necessary when <strong>the</strong> clinician and <strong>the</strong> patient<br />
do not share <strong>the</strong> same <strong>cultural</strong> background, since it is <strong>the</strong>n that<br />
particular attention to <strong>cultural</strong> features can be most helpful in orienting<br />
<strong>the</strong> clinical intervention. It is important to remember, however, that<br />
even persons sharing <strong>the</strong> same race or ethnicity can differ in <strong>the</strong>ir <strong>cultural</strong><br />
backgrounds, as race and ethnic groups are <strong>cultural</strong>ly heterogenous<br />
(12,17). Implementation of <strong>the</strong> CF model when <strong>the</strong>re is no ethnic<br />
difference between patients and clinicians can still elicit very useful in<strong>for</strong>mation<br />
about <strong>cultural</strong>ly based values, norms, and behaviors—such<br />
as about alternative health practices, physiological interpretations, or<br />
religious beliefs—that may o<strong>the</strong>rwise go unnoticed because <strong>the</strong> clinician
274 PSYCHIATRIC QUARTERLY<br />
assumes that <strong>the</strong> patient is “just like me.” In addition, <strong>the</strong> CF model<br />
should not be construed <strong>for</strong> use mainly between majority clinicians and<br />
minority patients. Given <strong>the</strong> growing ethno-<strong>cultural</strong> pluralism of psychiatric<br />
residency programs in <strong>the</strong> US (including a high proportion of<br />
International Medical Graduates), <strong>the</strong> existence of <strong>cultural</strong> differences<br />
is becoming perhaps just as likely between majority patients and <strong>the</strong>ir<br />
clinicians.<br />
This article will present <strong>the</strong> Cultural Formulation model. The first<br />
part of <strong>the</strong> discussion will give a brief historical overview of <strong>the</strong> model<br />
and its components. The second part will consist of a case scenario that<br />
will illustrate <strong>the</strong> purpose of each section of <strong>the</strong> model and its usefulness<br />
in psychiatry and mental health in general.<br />
HISTORICAL OVERVIEW AND COMPONENTS OF THE<br />
CULTURAL FORMULATION MODEL<br />
The contemporary version of <strong>the</strong> CF model dates from <strong>the</strong> process of<br />
preparing DSM-IV. Due in part to criticisms of insensitivity to <strong>cultural</strong><br />
issues in DSM-III and DSM-III-R, <strong>the</strong> National Institute of Mental<br />
Health supported <strong>the</strong> creation in 1991 of a Group on Culture and Diagnosis.<br />
The main goal of this Group was to advise <strong>the</strong> DSM-IV Task<br />
Force on how to make culture more central to <strong>the</strong> Manual. One of <strong>the</strong><br />
ways proposed by <strong>the</strong> Group was <strong>the</strong> development of a standard <strong>method</strong><br />
<strong>for</strong> applying a <strong>cultural</strong> perspective to <strong>the</strong> clinical evaluation (15,18).<br />
Early ef<strong>for</strong>ts focused on supplementing <strong>the</strong> five existing axes with a<br />
sixth or “Cultural Axis.” However, this approach was soon abandoned as<br />
too limiting, since at best it would only permit <strong>the</strong> use of a restricted list<br />
of socio-<strong>cultural</strong> labels which would be of little clinical significance (14).<br />
The Group aimed <strong>for</strong> a more thorough re-thinking by <strong>the</strong> clinician of<br />
<strong>the</strong> patient’s <strong>cultural</strong> picture and how it affects all five axes, as well as<br />
clinical elements not contemplated by <strong>the</strong> multi-axial structure, such<br />
as help-seeking expectations, family and community views of <strong>the</strong> illness<br />
and its outcome, and institutional pressures on <strong>the</strong> clinical encounter.<br />
A key aim of <strong>the</strong> Group was to operationalize a <strong>method</strong> that,<br />
while standardized, still allowed <strong>for</strong> an individualized assessment of<br />
<strong>cultural</strong> <strong>factors</strong> (15). This was based on <strong>the</strong> perspective that a person’s<br />
<strong>cultural</strong> background is affected by <strong>the</strong> intersection of multiple social<br />
influences—including those due to gender, class, race, sexual orientation,<br />
etc.—and <strong>the</strong>re<strong>for</strong>e would need to be described in individual ra<strong>the</strong>r<br />
than solely collective terms in order to avoid stereotyping (12).<br />
The Group settled on a narrative <strong>for</strong>mat that follows a standard set<br />
of components. These are listed in Table 1. Every patient would have
ROBERTO LEWIS-FERNÁNDEZ AND NAELYS DÍAZ 275<br />
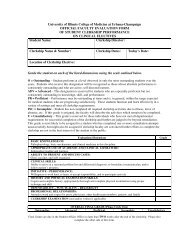
TABLE 1<br />
Components of <strong>the</strong> Cultural Formulation<br />
Cultural <strong><strong>for</strong>mulation</strong><br />
section<br />
Cultural identity of <strong>the</strong><br />
individual<br />
Cultural explanations<br />
of <strong>the</strong> individual’s<br />
illness<br />
Cultural <strong>factors</strong><br />
related to psychosocial<br />
environment and<br />
levels of functioning<br />
Cultural elements of <strong>the</strong><br />
relationship between<br />
<strong>the</strong> individual and<br />
<strong>the</strong> clinician<br />
Overall <strong>cultural</strong><br />
assessment <strong>for</strong><br />
diagnosis and care<br />
Subheading<br />
• Individual’s ethnic or <strong>cultural</strong> reference<br />
group(s)<br />
• Degree of involvement with both <strong>the</strong> culture<br />
of origin and <strong>the</strong> host culture (<strong>for</strong> immigrants<br />
and ethnic minorities)<br />
• Language abilities, use, and preference<br />
(including multilingualism)<br />
• Predominant idioms of distress through<br />
which symptoms or <strong>the</strong> need <strong>for</strong> social<br />
support are communicated<br />
• Meaning and perceived severity of <strong>the</strong><br />
individual’s symptoms in relation to norms of<br />
<strong>the</strong> <strong>cultural</strong> reference group(s)<br />
• Local illness categories used by <strong>the</strong><br />
individual’s family and community to identify<br />
<strong>the</strong> condition<br />
• Perceived causes and explanatory models that<br />
<strong>the</strong> individual and <strong>the</strong> reference group(s) use<br />
to explain <strong>the</strong> illness<br />
• Current preferences <strong>for</strong> and past experiences<br />
with professional and popular sources of care<br />
• Culturally relevant interpretations of social<br />
stressors, available social supports, and levels<br />
of functioning and disability<br />
• Stresses in <strong>the</strong> local social environment<br />
• Role of religion and kin networks in providing<br />
emotional, instrumental, and in<strong>for</strong>mational<br />
support<br />
• Individual differences in culture and social<br />
status between <strong>the</strong> individual and <strong>the</strong><br />
clinician<br />
• Problems that <strong>the</strong>se differences may cause in<br />
diagnosis and treatment (e.g. difficulties in<br />
eliciting symptoms and understanding <strong>the</strong>ir<br />
<strong>cultural</strong> significance, in determining whe<strong>the</strong>r<br />
a behavior is normal or pathological, etc.)<br />
• Discussion of how <strong>cultural</strong> considerations<br />
specifically influence comprehensive<br />
diagnosis and care<br />
Note. Summarized from DSM-IV, pp. 843–844.
276 PSYCHIATRIC QUARTERLY<br />
his/her <strong>cultural</strong> background described in a brief text that incorporates<br />
each of <strong>the</strong> listed elements. This Cultural Formulation is based on prior<br />
work on <strong>the</strong> “mini clinical ethnography,” which sets out a brief anthropological<br />
assessment of <strong>the</strong> <strong>cultural</strong> <strong>factors</strong> that are immediately relevant<br />
to <strong>the</strong> clinical situation (19,20).<br />
In selecting a narrative model, <strong>the</strong> Group was consciously endorsing<br />
<strong>the</strong> growing importance of <strong>the</strong> study of narrative in anthropology<br />
and o<strong>the</strong>r social sciences, as well as echoing a tradition within mental<br />
health assessment: <strong>the</strong> psychodynamic <strong><strong>for</strong>mulation</strong> (14). In medicine<br />
in general, <strong>the</strong> use of narrative accounts of illness goes beyond diagnostic<br />
typologies to claim a different “truth” in <strong>the</strong> creation of a humanized<br />
account of suffering from <strong>the</strong> patient’s perspective that encompasses<br />
a greater view of <strong>the</strong> social world than <strong>the</strong> purely diagnostic<br />
evaluation (19). The use of this technique can also account <strong>for</strong> <strong>the</strong> role<br />
that health institutions and practitioners have on <strong>the</strong> evolution of <strong>the</strong><br />
person’s illness and his/her perception and interpretation of it (21,22).<br />
This allows a reflexive stance on <strong>the</strong> clinician-patient interaction, in<br />
which <strong>the</strong> role of <strong>the</strong> practitioner in shaping <strong>the</strong> process of evaluation,<br />
including what is reported by <strong>the</strong> patient and what is perceived by <strong>the</strong><br />
clinician, can be “painted back in.”<br />
An outline of <strong>the</strong> Cultural Formulation was prepared and submitted<br />
to <strong>the</strong> DSM-IV Task Force. In addition, a field test was per<strong>for</strong>med on<br />
patients from four US ethnic minorities: African American, American<br />
Indian, Asian American, and Latino. The results revealed that <strong>the</strong> CF<br />
model could be successfully applied to patients from different <strong>cultural</strong><br />
backgrounds. An edited version of <strong>the</strong> proposed text was published in<br />
Appendix I of DSM-IV (15).<br />
As a result of its publication in DSM-IV, <strong>the</strong> Cultural Formulation<br />
has begun to <strong>for</strong>m part of <strong>the</strong> curricula of US psychiatry residency<br />
programs. Since 1996, <strong>the</strong> CF model has been <strong>the</strong> subject of a regular<br />
section on clinical case studies in Culture, Medicine and Psychiatry (14),<br />
of whom <strong>the</strong> senior author is <strong>the</strong> section editor, and of a yearly course at<br />
<strong>the</strong> Annual Meeting of <strong>the</strong> American Psychiatric Association. In 2001,<br />
<strong>the</strong> Cultural Psychiatry Committee of <strong>the</strong> Group <strong>for</strong> <strong>the</strong> Advancement<br />
of Psychiatry published a book on <strong>the</strong> CF model that includes a number<br />
of case examples (12).<br />
CULTURAL FORMULATION OF A CLINICAL CASE<br />
The second part of this article summarizes a case study of an actual<br />
patient (23) that illustrates <strong>the</strong> purpose of each of <strong>the</strong> components<br />
of <strong>the</strong> Cultural Formulation and <strong>the</strong> impact on treatment outcome of
ROBERTO LEWIS-FERNÁNDEZ AND NAELYS DÍAZ 277<br />
implementing this model in clinical practice. In particular, <strong>the</strong> case<br />
highlights some of <strong>the</strong> diagnostic complexities involved in <strong>assessing</strong><br />
patients reporting nervios (nerves) and ataques de nervios (attacks of<br />
nerves), prevalent popular syndromes among Latinos. A brief summary<br />
of <strong>the</strong> clinical history is followed by <strong>the</strong> <strong>cultural</strong> <strong><strong>for</strong>mulation</strong> of <strong>the</strong> case.<br />
In<strong>for</strong>med consent was obtained from <strong>the</strong> patient <strong>for</strong> description of this<br />
clinical material.<br />
Clinical History<br />
A 49 year-old widowed Puerto Rican woman presented to an outpatient<br />
Latino Mental Health Clinic in New England after a 3-year history of<br />
prolonged hospitalizations due to recurrent major depressive disorder<br />
with diagnosed psychotic features and chronic impulsive suicidality.<br />
Except <strong>for</strong> brief periods of partial recovery lasting less <strong>the</strong>n 2 weeks,<br />
<strong>the</strong> patient reported several years of chronic sadness, anhedonia, tearfulness,<br />
psychomotor retardation, suicidality, guilty ruminations, decreased<br />
sleep and appetite, interest, energy, and concentration. She<br />
also suffered from restlessness, “nervousness,” trembling, increased<br />
startle, anguish, and severe headaches. Patient’s “psychotic” diagnosis<br />
was due to <strong>the</strong> following during her affective decompensations: hearing<br />
her name called when alone, glimpsing a darting shadow, and “feeling”<br />
someone behind her. Despite past traumas (physical abuse, husband’s<br />
murder) she denied many of <strong>the</strong> symptoms of posttraumatic stress disorder.<br />
There was no history of substance abuse. Her first episode of<br />
major depression dated from age 32 and had recurred at least once<br />
be<strong>for</strong>e <strong>the</strong> current episode.<br />
Patient was born in rural Puerto Rico and had a 5th grade education.<br />
Her fa<strong>the</strong>r developed alcoholism while working as a seasonal agri<strong>cultural</strong><br />
migrant in <strong>the</strong> United States and was verbally abusive and physically<br />
threatening to <strong>the</strong> patient’s mo<strong>the</strong>r when intoxicated. The patient<br />
denied witnessing overt physical or sexual abuse or being <strong>the</strong> object<br />
of childhood trauma, but did complain of her mo<strong>the</strong>r’s cold distance.<br />
Patient married at 16 and had 6 children, one of whom died of pneumonia<br />
at 3 months of age. Husband also developed alcohol problems<br />
and became physically and emotionally abusive towards her. After an<br />
escalation of his abuse, patient ended <strong>the</strong> marriage by migrating to <strong>the</strong><br />
Eastern United States at age 31 with <strong>the</strong> man who became her second<br />
husband. She left four of her children behind with relatives, a decision<br />
that resulted in her parents’ rejection. Five years later she returned to<br />
Puerto Rico after <strong>the</strong> murder of her second husband in a street fight.<br />
The son who had migrated with her to <strong>the</strong> US entered a residential
278 PSYCHIATRIC QUARTERLY<br />
drug abuse program 11 years later, at which point she migrated to a<br />
different East Coast city at age 47 to be near her oldest son from whom<br />
she felt estranged. Her conflicts with this son and her o<strong>the</strong>r children<br />
precipitated her inpatient admissions.<br />
Inpatient psycho<strong>the</strong>rapy, antidepressants, and antipsychotics only<br />
produced minor improvement of her depression and suicidality and no<br />
change in her psychotic symptoms. After discharge to <strong>the</strong> outpatient<br />
Latino Clinic, her psychotic symptoms were reassessed as normative<br />
Puerto Rican spiritual expressions of demoralization and her molindone<br />
was discontinued. While still on phenelzine during evaluation <strong>for</strong> family<br />
<strong>the</strong>rapy, <strong>the</strong> patient suffered an ataque de nervios in <strong>the</strong> midst of an<br />
argument with her son. During <strong>the</strong> ataque, which was characterized by<br />
dissociative symptoms (depersonalization, “numbness”), she attempted<br />
an impulsive overdose with phenelzine. She required ICU treatment<br />
and a brief in-patient stay, and was taken off all psychiatric medications.<br />
Intensive psycho<strong>the</strong>rapeutic management was instituted, initially including<br />
individual, family, and group modalities. Improved family relations<br />
resulted in marked decrease in symptoms. Outpatient assessment<br />
and psycho<strong>the</strong>rapy revealed patient’s longstanding characterological<br />
symptoms and she received a diagnosis of Borderline Personality Disorder.<br />
She reduced her participation in treatment after a few months,<br />
preferring weekly supportive psycho<strong>the</strong>rapy and monthly psychiatric<br />
visits. These latter acted as a kind of supervision of her clinical picture,<br />
since medications were not prescribed. Patient was followed off<br />
medications <strong>for</strong> 8 years without recurrence of major depression or suicidality.<br />
She did develop periodic exacerbations of depressive, anxiety,<br />
dissociative, and somatization symptoms that did not meet specified diagnostic<br />
criteria. Though she continued to perceive “shadows” and hear<br />
her name called when alone, <strong>the</strong>se experiences produced only temporary<br />
concern. There was never any evidence of <strong>for</strong>mal thought disorder<br />
nor loss of generalized reality orientation [Summarized from (23)].<br />
Cultural Formulation<br />
Cultural Identity<br />
The section on Cultural Identity serves as an introduction to <strong>the</strong> rest of<br />
<strong>the</strong> Cultural Formulation. Its purpose is to identify <strong>for</strong> each patient <strong>the</strong><br />
particular mix of socio-<strong>cultural</strong> influences that has patterned his/her<br />
individual <strong>cultural</strong> world. As stated earlier, cultures are experienced<br />
differently by different members according to subgroup characteristics<br />
such as gender, class, religion, race, and sexual orientation, among
ROBERTO LEWIS-FERNÁNDEZ AND NAELYS DÍAZ 279<br />
o<strong>the</strong>r <strong>factors</strong>. This section of <strong>the</strong> <strong><strong>for</strong>mulation</strong> collects in<strong>for</strong>mation on<br />
how <strong>the</strong>se various social <strong>factors</strong> impact <strong>the</strong> person’s <strong>cultural</strong> environment<br />
in order to prevent overly general or stereotypical interpretations<br />
of <strong>cultural</strong> influence (13). This section also permits assessment of <strong>the</strong><br />
person’s own sense of his/her ethno-<strong>cultural</strong> identity, particularly in<br />
respect to o<strong>the</strong>r alternative identities; this takes on particular significance<br />
in settings of rapid <strong>cultural</strong> change or ethnic conflict, or among<br />
migrants or persons of multi<strong>cultural</strong> heritage. At <strong>the</strong> conclusion of this<br />
section, <strong>the</strong> <strong><strong>for</strong>mulation</strong> writer should have a sense of how <strong>the</strong> person<br />
fits against a specific <strong>cultural</strong> background. This serves as a prelude to<br />
understanding how his/her individual experience of <strong>the</strong> illness and its<br />
meanings and outcomes fit within that <strong>cultural</strong> context, which is <strong>the</strong><br />
topic of <strong>the</strong> rest of <strong>the</strong> CF model (12).<br />
The following subsections are included within <strong>the</strong> general section on<br />
Cultural Identity. For <strong>the</strong> purpose of illustrating its content, each subsection<br />
begins with one key question regarding <strong>the</strong> case under discussion<br />
that summarizes <strong>the</strong> subsection topic. We will follow this <strong>for</strong>mat<br />
<strong>for</strong> every subsection throughout <strong>the</strong> article.<br />
Reference Group. Within her overall group (Puerto Rican culture),<br />
which particular <strong>cultural</strong> subgroups <strong>for</strong>m <strong>the</strong> relevant context <strong>for</strong> <strong>assessing</strong><br />
this person?<br />
A key influence on this patient’s <strong>cultural</strong> background is her status<br />
as a rural person with limited <strong>for</strong>mal education who migrated twice<br />
to <strong>the</strong> US <strong>for</strong> a total of 13 years’ residence as part of <strong>the</strong> “circular”<br />
pattern of Puerto Rican migration that intensified in <strong>the</strong> 1960’s and<br />
70’s. The “circularity” of this migratory stream consists of recurrent<br />
“back and <strong>for</strong>th” moves between Puerto Rico and usually <strong>the</strong> East Coast<br />
of <strong>the</strong> United States in search of better economic and health care opportunities<br />
and in order to reestablish family and <strong>cultural</strong> links (24).<br />
Like many of <strong>the</strong>se migrants, she was only mildly acculturated despite<br />
this extended stay, given her periodic returns to her culture of origin<br />
and <strong>the</strong> barriers to integration into <strong>the</strong> US mainstream <strong>for</strong> persons<br />
of her ethnic, class, and educational background caused by chronic<br />
unemployment and limited housing options outside of encapsulated<br />
Latino neighborhoods (25). Her self-identity remained that of an Island<br />
Puerto Rican, despite her migratory experience. In effect, this<br />
patient had retained most of <strong>the</strong> traditional views of illness from her<br />
rural background despite several years of residence in US urban<br />
settings.<br />
In this subsection it is also important to understand <strong>the</strong> patient’s migratory<br />
process in <strong>the</strong> context of her <strong>for</strong>mer experience in Puerto Rico
280 PSYCHIATRIC QUARTERLY<br />
and <strong>the</strong> reasons <strong>for</strong> her migration (13). Because her initial migration occurred<br />
in order to escape her husband’s physical abuse, and involved a<br />
prolonged separation from her children, this person’s migratory process<br />
is akin in some respects to that of a refugee, an unusual status among<br />
low-income Puerto Rican migrants, who are usually motivated by economic<br />
reasons. Some of her subsequent psychiatric symptoms, such as<br />
her acute alienation, guilt, and suicidality, can be better understood<br />
against this unusual migratory context.<br />
Language. Does <strong>the</strong> patient have access to more than one language<br />
<strong>for</strong> expressing her illness-related experiences and obtaining care, and if<br />
so, which language predominates?<br />
Language assessment is an important element of <strong>the</strong> CF model because<br />
language identifies and codifies a person’s experience, which can<br />
be distorted in <strong>the</strong> process of translation. In <strong>the</strong> case of multilingual<br />
individuals, <strong>the</strong> use of a secondary language may limit <strong>the</strong> ability to obtain<br />
an accurate history and reach a valid diagnosis, since emotionality<br />
and cognition may be expressed differently in different languages. For<br />
example, an individual may appear more or less pathological depending<br />
on <strong>the</strong> language of <strong>the</strong> evaluation (26).<br />
This patient used Spanish predominantly in all her daily interactions.<br />
Her use of English was very rare and her fluency poor. This constitutes<br />
ano<strong>the</strong>r sign of her limited participation in non-Latino US society.<br />
Although <strong>the</strong> in-patient unit employed interpreters regularly in <strong>the</strong><br />
care of <strong>the</strong> patient, it is likely that some of <strong>the</strong> limitations in <strong>the</strong>ir clinical<br />
assessment were related to difficulties in bridging <strong>the</strong> language gap,<br />
resulting in relatively shallow interpretations of her experience. For example,<br />
<strong>the</strong> <strong>cultural</strong> connotations <strong>for</strong> <strong>the</strong> Spanish terms that <strong>the</strong> patient<br />
used to express her distress, such as nervios (nerves), ataques (attacks),<br />
and celajes (glimpses or shadows, understood by <strong>the</strong> staff as visual hallucinations),<br />
appear to have been lost or distorted during <strong>the</strong> translation<br />
process.<br />
Cultural Factors in Development. Are <strong>the</strong>re features of <strong>the</strong> patient’s<br />
childhood development that should be placed in a specific <strong>cultural</strong> context<br />
in order to be properly understood?<br />
Locating childhood development within a <strong>cultural</strong> context can help<br />
clarify <strong>the</strong> contribution of environmental <strong>factors</strong> to personality characteristics<br />
(12). Experience is made meaningful and incorporated as enduring<br />
personal attributes partly in response to its perceived normality<br />
and collective interpretation. Factors that influence personality development<br />
and that vary across cultures include, among o<strong>the</strong>rs: gender
ROBERTO LEWIS-FERNÁNDEZ AND NAELYS DÍAZ 281<br />
roles, relational characteristics within <strong>the</strong> family and roles within <strong>the</strong><br />
family constellation, socialization experiences, and social valuation of<br />
emotional expression (27,28).<br />
In this case, <strong>the</strong> patient’s childhood contacts were limited to her extended<br />
kin group, given <strong>the</strong> rural isolation of her family compound and<br />
her early school termination. This may have intensified <strong>the</strong> negative<br />
impact on her personality development of her fa<strong>the</strong>r’s disruptive and<br />
abusive behavior and her mo<strong>the</strong>r’s affective distance despite <strong>the</strong> stated<br />
absence of witnessed or experienced physical or sexual abuse during<br />
childhood. These personality patterns were probably also rein<strong>for</strong>ced<br />
by later adult episodes of physical abuse and traumatic loss. Ano<strong>the</strong>r<br />
socio<strong>cultural</strong> feature of <strong>the</strong> patient’s early socialization that appears<br />
to have influenced her later symptomatology relates to her role as a<br />
parentified child who was removed from elementary school in order to<br />
help raise her younger siblings. Though not an uncommon practice in<br />
<strong>the</strong> patient’s <strong>cultural</strong> reference group, this seems to have determined a<br />
particularly important element in her self-perception, as evidenced by<br />
her lifelong nickname within <strong>the</strong> family which refers to this maternal<br />
function. The loss of this <strong>cultural</strong>ly established role, through separation<br />
and subsequent estrangement from her children, was <strong>the</strong> main<br />
cause of <strong>the</strong> patient’s affective decompensation. The partial resumption<br />
of this role through family <strong>the</strong>rapy marked <strong>the</strong> beginning of her<br />
improvement.<br />
Involvement with Culture of Origin and Host Culture. How does understanding<br />
a migrant like this patient in <strong>the</strong> context of her culture of<br />
origin separately from <strong>the</strong> host culture reveal something about her as a<br />
person and about her migration experience?<br />
This subsection is primarily relevant to migrants. Its purpose is to<br />
compare <strong>the</strong> individual’s involvement with <strong>the</strong> culture of origin, on <strong>the</strong><br />
one hand, to his/her involvement with <strong>the</strong> host culture, on <strong>the</strong> o<strong>the</strong>r.<br />
By evaluating each attachment independently, <strong>the</strong> clinician can avoid<br />
a zero-sum model of acculturation, which mistakenly assumes that as<br />
a person becomes more fluent in <strong>the</strong> new culture, he/she necessarily<br />
becomes disconnected from his/her culture of origin (29). Instead, contemporary<br />
acculturation models understand that, in a world where multi<strong>cultural</strong>ity<br />
and geographical displacement are becoming increasingly<br />
prevalent, multiple combinations of involvement are possible, such as<br />
<strong>the</strong> alternative of developing a deep connection to both <strong>cultural</strong> environments<br />
(30). Finally, by establishing <strong>the</strong> migrant’s relative <strong>cultural</strong><br />
attachments, <strong>the</strong> person’s <strong>cultural</strong> identity is rounded out, setting <strong>the</strong><br />
stage <strong>for</strong> <strong>the</strong> o<strong>the</strong>r topics of <strong>the</strong> CF model.
282 PSYCHIATRIC QUARTERLY<br />
This patient was predominantly connected to her culture of origin<br />
and had limited contact with <strong>the</strong> host culture. She lived in a mainly<br />
Latino neighborhood and traveled frequently to Puerto Rico, where<br />
she kept in close contact with several siblings; she had few friends,<br />
mostly Latinas, apart from her family. She was, however, able to maneuver<br />
some aspects of United States urban life well, such as obtaining<br />
elderly subsidized housing (though only in her 50’s) and disability<br />
benefits.<br />
Cultural Explanations of <strong>the</strong> Illness<br />
The heart of <strong>the</strong> Cultural Formulation is this second section, which<br />
examines <strong>the</strong> <strong>cultural</strong> <strong>factors</strong> that affect <strong>the</strong> experience and interpretation<br />
of illness, as understood by <strong>the</strong> patient, <strong>the</strong> family, and <strong>the</strong> social<br />
network. These <strong>cultural</strong> <strong>factors</strong> exert a deeper influence than just covering<br />
over an unchanging reality with curious <strong>cultural</strong> explanations.<br />
They instead help to create <strong>the</strong> illness experience by affecting cognitive,<br />
bodily, and interpersonal aspects of disease, including by helping<br />
to shape symptom presentations, perceived etiologies, severity attributions,<br />
treatment choices, and outcome expectations (6,31). In particular,<br />
explicit <strong>cultural</strong> analysis is required <strong>for</strong> accurate assessment of<br />
<strong>the</strong> severity of <strong>the</strong> presenting problems, since patients’ attributions of<br />
severity are acutely impacted by <strong>cultural</strong> interpretations. Finally, adherence<br />
to clinicians’ recommendations may be compromised without<br />
careful attention to patients’ <strong>cultural</strong> views of treatment. In this respect,<br />
it may also be necessary to account <strong>for</strong> <strong>the</strong> views of key relatives<br />
or members of <strong>the</strong> larger social network (32).<br />
Idioms of Distress and Local Illness Categories. How do <strong>cultural</strong> <strong>factors</strong><br />
affect <strong>the</strong> way this person experiences and understands her distress,<br />
including <strong>the</strong> specific shape of <strong>the</strong> presenting symptoms and <strong>the</strong> way<br />
<strong>the</strong>y are clustered?<br />
Cross-<strong>cultural</strong> research reveals <strong>the</strong> existence of multiple overall perspectives<br />
on distress—ways in which to experience, understand, and<br />
describe it—that are so comprehensive that <strong>the</strong>y seem akin to different<br />
languages of suffering ra<strong>the</strong>r than specific syndromes. The term<br />
“idioms of distress” is used to denote <strong>the</strong>se different languages of experience<br />
(33). Examples of idioms are: <strong>the</strong> tendency to somatize suffering,<br />
or to psychologize it; experiencing interpersonal problems or physical<br />
illness as <strong>for</strong>ms of possession; attributing illness to <strong>the</strong> impact of suffering<br />
on <strong>the</strong> anatomical “nerves”; or describing distress in terms of “fate,”<br />
or as a kind of “spiritual test” (16).
ROBERTO LEWIS-FERNÁNDEZ AND NAELYS DÍAZ 283<br />
In addition to <strong>the</strong>se general <strong>for</strong>ms, cultures have also evolved more<br />
specific illness categories or syndromes, assembled according to alternative<br />
systems of causation. The organizing principle can be a relatively<br />
invariant collections of symptoms, a perceived common etiology,<br />
or a shared response to treatment (5). One of <strong>the</strong> essential tasks of a<br />
Cultural Formulation is to discover <strong>the</strong> idioms of distress and <strong>the</strong> illness<br />
categories that are evoked by <strong>the</strong> patient’s presentation. Often<br />
<strong>the</strong> patient is not fully conscious of <strong>the</strong> categories he/she is referencing,<br />
and yet may be acutely aware of <strong>the</strong> dissonance between his/her<br />
understandings and those of <strong>the</strong> clinician.<br />
In this case, <strong>the</strong> patient’s illness was described by herself and her community<br />
as nervios (nerves) and ataques de nervios (attacks of nerves).<br />
Patient’s view of her nervios was typical of many traditional Puerto<br />
Ricans, <strong>for</strong> whom it is an idiom of distress describing a vulnerability to<br />
experiencing symptoms of depression, anxiety, dissociation, somatization<br />
and rarely psychosis or poor impulse control given interpersonal<br />
frustrations (34). The idiom is held toge<strong>the</strong>r conceptually by <strong>the</strong> <strong>cultural</strong><br />
understanding that all its presentations reflect an “alteration,”<br />
acquired or inherited, of <strong>the</strong> nervous system, and specifically of <strong>the</strong><br />
anatomical nerves. The patient had suffered from all <strong>the</strong> symptoms<br />
of nervios except psychosis. Her acute fit-like exacerbations of nervios<br />
are known as ataques de nervios, and were characterized by paroxysms<br />
of anxiety, rage, dissociation, and impulsive suicidality followed<br />
by depression and exhaustion in response to acute interpersonal conflicts<br />
(9,11). In this patient’s case, nervios and ataques were associated<br />
with her character pathology, but many Puerto Ricans suffer from similar<br />
folk syndromes without showing characterological deficits, though<br />
<strong>the</strong> exact relationship between <strong>the</strong>se clinical conditions has not been<br />
ascertained.<br />
Ano<strong>the</strong>r critical aspect of her nervios was <strong>the</strong> high frequency and<br />
distressing nature of <strong>the</strong> <strong>cultural</strong>ly specific perceptual distortions she<br />
reported (hearing voices, feeling presences, seeing shadows [known as<br />
celajes; glimpses]). These experiences are very prevalent among Puerto<br />
Ricans with and without nervios, but sufferers of ataques are markedly<br />
more distressed by <strong>the</strong>m (35). They probably represent <strong>cultural</strong>ly patterned<br />
signs of anxiety or emotional distress determined by a person’s<br />
dissociative capacity. In <strong>the</strong> patient’s case, <strong>the</strong>se experiences were mistaken<br />
<strong>for</strong> psychotic symptoms by her inpatient clinicians. As such, discussion<br />
of <strong>the</strong>se symptoms in <strong>the</strong> Cultural Formulation straddles this<br />
subsection and <strong>the</strong> next, as <strong>the</strong>y constitute <strong>cultural</strong>ly specific idioms of<br />
distress whose interpretation can affect <strong>the</strong> perceived severity of <strong>the</strong><br />
presenting complaints.
284 PSYCHIATRIC QUARTERLY<br />
Meaning and Severity of Symptoms in Relation to Cultural Norms.<br />
How does taking her <strong>cultural</strong> background into account affect <strong>the</strong> level<br />
of pathology suggested by her presenting symptoms and <strong>the</strong>ir meaning<br />
as a <strong>for</strong>m of communication in her interpersonal context?<br />
This subsection is devoted to a careful assessment of <strong>the</strong> level of<br />
severity implied by <strong>the</strong> person’s symptoms, as well as to discussion of<br />
<strong>the</strong> role of <strong>the</strong> illness as a <strong>for</strong>m of interpersonal communication that is<br />
interpreted by o<strong>the</strong>rs in <strong>the</strong> social network. It is essential that <strong>cultural</strong><br />
norms be considered when <strong>assessing</strong> <strong>the</strong> clinical severity of specific behaviors,<br />
so as to avoid two erroneous extremes: overpathologizing what<br />
is normative in a <strong>cultural</strong> group, or ascribing to normal behavior what is<br />
considered pathological in that culture (13,36). Whe<strong>the</strong>r what is at issue<br />
is <strong>the</strong> normal degree of individuation of an 18 year-old in relation to<br />
his/her parents, or <strong>the</strong> potential delusionality of a person who ascribes<br />
his/her symptoms to a supernatural etiology, some knowledge of local<br />
behavioral norms is essential to <strong>the</strong> process of diagnosis. The fact that<br />
different subgroups within a larger <strong>cultural</strong> setting may interpret <strong>the</strong>se<br />
behaviors differently complicates <strong>the</strong> process of assessment and <strong>for</strong>ces<br />
an individualized evaluation of <strong>cultural</strong> <strong>factors</strong> in each case.<br />
In addition, illness expressions convey a range of meanings to o<strong>the</strong>rs<br />
in <strong>the</strong> social network. Which set of meanings is imputed by <strong>the</strong> community<br />
actually has an impact on <strong>the</strong> patient’s course, both through interpersonal<br />
interactions that promote improvement or pathology and<br />
through concrete levels of assistance or rejection. The cross-<strong>cultural</strong><br />
literature on <strong>the</strong> contribution of expressed emotion to <strong>the</strong> course of<br />
schizophrenia represents a well-developed example of this issue (37).<br />
In this patient’s case, her symptoms at <strong>the</strong> time of presentation were<br />
seen by her community to reflect a severe <strong>for</strong>m of nervios because <strong>the</strong>y<br />
could precipitate rage and dissociation ataques with impulsive suicidality<br />
and because <strong>the</strong>y had “penetrated deeply,” causing her character<br />
pathology. As opposed to her outpatient clinicians, who saw her character<br />
problems as preceding and partly determining her Axis I disorders,<br />
<strong>the</strong> patient’s social network understood her characterological symptoms<br />
as a consequence of her nervios, ra<strong>the</strong>r than as a cause (i.e., a <strong>for</strong>m of<br />
bitterness due to her continued suffering), and thus as a sign of nervios<br />
severity. In ano<strong>the</strong>r discrepancy between <strong>the</strong> social network and <strong>the</strong><br />
clinical team, <strong>the</strong> patient’s inpatient clinicians judged her perceptual<br />
distortions to be much more severe than her community, understanding<br />
<strong>the</strong>m as signs of psychosis ra<strong>the</strong>r than minor elements of her overall<br />
condition.<br />
Fur<strong>the</strong>r, <strong>the</strong> expectation of her interpersonal network was that <strong>the</strong><br />
patient actively ward against any worsening of her character pathology
ROBERTO LEWIS-FERNÁNDEZ AND NAELYS DÍAZ 285<br />
by “controlling” her needs and desires and focusing on <strong>the</strong> needs of<br />
o<strong>the</strong>rs, such as her children. The community thus validated <strong>the</strong> patient’s<br />
understanding that reestablishing positive affective links with<br />
her family would improve <strong>the</strong> outcome of her nervios. Her achievement<br />
of this goal, as well as her coming off psychiatric medications and preventing<br />
fur<strong>the</strong>r ataques, were considered signs of improvement. The<br />
patient’s children, however, initially rejected <strong>the</strong> patient’s and <strong>the</strong> community’s<br />
understanding that her character pathology stemmed from<br />
her nervios and ataques, attributing it instead to manipulative ploys<br />
aimed at deflecting <strong>the</strong>ir justified anger due to what <strong>the</strong>y perceived as<br />
her neglectful parenting. Therapy helped to bridge <strong>the</strong>se conflicting interpretations,<br />
but several of her children always retained <strong>the</strong> sense that<br />
<strong>the</strong> patient’s personality conflicts exceeded <strong>the</strong> norm even <strong>for</strong> nervios.<br />
Perceived Causes and Explanatory Models. How is her clinical management<br />
affected by knowing about her <strong>cultural</strong>ly based etiological<br />
attributions, her understandings of pathophysiology, and her hopes and<br />
concerns about <strong>the</strong> course of <strong>the</strong> illness?<br />
This subsection focuses on <strong>the</strong> patient’s views on how <strong>the</strong> illness<br />
“works”: what caused it; why did it present now and in this way; how is it<br />
affecting <strong>the</strong> person; what would happen if it was not treated; and what<br />
are <strong>the</strong> possible outcomes even with treatment? (12,38). This subsection,<br />
like <strong>the</strong> next one on help-seeking to which it is closely linked, is especially<br />
important during <strong>the</strong> process of enlisting <strong>the</strong> patient’s and <strong>the</strong><br />
family’s adherence to <strong>the</strong> clinician’s recommendations. Patients rarely<br />
pursue treatments <strong>for</strong> long that run counter to <strong>the</strong>ir primary etiological<br />
understandings. Cultural attributions of causation actually vary widely<br />
across societies, from biological to spiritual etiologies, and from drastically<br />
individual, internal views to social and even cosmological interpretations<br />
(39). Often, <strong>the</strong>re are a mix of attributions, at times partly<br />
or wholly contradictory within one person or across <strong>the</strong> patient’s social<br />
network. Treatment may thus involve negotiating <strong>the</strong> appearance<br />
of <strong>the</strong>se various perspectives and bringing <strong>the</strong>m into some coherent<br />
strategy (19).<br />
At first, <strong>the</strong> patient saw her condition fundamentally as a medical<br />
problem caused by an “alteration” of her nervous system due to <strong>the</strong><br />
suffering produced by chronically unresolved family conflicts. Primary<br />
among <strong>the</strong>se were <strong>the</strong> physical abuse by her husband, <strong>the</strong> parental<br />
rejection, and her separation from several of her children during most<br />
of <strong>the</strong>ir childhood, which led to <strong>the</strong>ir ongoing anger toward her. This is a<br />
typical traditional Puerto Rican interpretation of <strong>the</strong> impact of chronic<br />
suffering on <strong>the</strong> “nerves.” If untreated, <strong>the</strong> patient feared that she would
286 PSYCHIATRIC QUARTERLY<br />
become chronically psychotic (“loca”; crazy), given her limited ability, by<br />
herself, to “control” her symptoms, particularly her anger and grief (40).<br />
Over time, however, medical treatment without family reconciliation<br />
was likewise experienced as insufficient. The traditional link between<br />
nervous ailments and past stressors served <strong>the</strong> outpatient clinicians as<br />
an entry point <strong>for</strong> discussing her interpersonal history, including <strong>the</strong><br />
conflict with her children. One important function of her caregivers became<br />
that of contributing medical authority to <strong>the</strong> patient’s claims <strong>for</strong><br />
filial support. In that sense, <strong>the</strong> interpersonal element in her system<br />
of etiological attributions grew to supersede <strong>the</strong> more physiological aspects<br />
of her explanatory model. Her ongoing participation in treatment<br />
was attained in large measure by <strong>the</strong> growing confluence of this model<br />
with that of her providers, who also saw her problematic family relationships<br />
as a main cause of her illness. In fact, clinicians’ success in enlisting<br />
family support <strong>for</strong> <strong>the</strong> patient became proof of <strong>the</strong>ir <strong>the</strong>rapeutic<br />
value.<br />
A secondary element of her explanatory model was <strong>the</strong> notion that<br />
her nervios illness produced a kind of spiritual “weakness,” which led to<br />
<strong>the</strong> irruption of distressing spiritual visitations, perhaps by deceased<br />
relatives, which were experienced as perceptual distortions. This aspect<br />
of her model was never primary nor fully worked out, yet it initially<br />
disrupted her care, as it led to a diagnosis of psychosis by <strong>the</strong> inpatient<br />
team. Even when improved, however, <strong>the</strong> patient remained leery of<br />
<strong>the</strong>se experiences, preferring to pay <strong>the</strong>m minimal attention.<br />
Help-Seeking Experiences and Plans. How does <strong>the</strong> patient’s <strong>cultural</strong><br />
identity help explain her past help-seeking choices and expectations<br />
about current and future <strong>for</strong>ms of assistance and treatment?<br />
This subsection is closely linked to <strong>the</strong> previous one, as individuals<br />
usually seek out caregivers who offer assistance in ways that match<br />
<strong>the</strong>ir explanatory models (13,19). Patients’ help-seeking choices actually<br />
tend to follow “pathways” of care which are partly determined<br />
by psychosocial and <strong>cultural</strong> <strong>for</strong>ces. One expression of this is <strong>the</strong> way<br />
<strong>cultural</strong> perceptions and interpretations of illness affect not only <strong>the</strong><br />
decision whe<strong>the</strong>r and when to seek <strong>for</strong>mal care (as opposed to being<br />
self-reliant or asking <strong>for</strong> help from <strong>the</strong> immediate social network), but<br />
also <strong>the</strong> type of treatment that is considered to be adequate and effective<br />
(41). As with etiological attributions, help-seeking pathways can<br />
also be quite complex, with multiple <strong>for</strong>ms of care being accessed at<br />
once, or in apparently contradictory ways.<br />
During her early bouts of depression, which were acute but brief and<br />
occurred years be<strong>for</strong>e <strong>the</strong> current presentation, <strong>the</strong> patient did not seek
ROBERTO LEWIS-FERNÁNDEZ AND NAELYS DÍAZ 287<br />
ongoing medical care, relying only on rare emergency room visits. At<br />
<strong>the</strong> time, she felt her life traumas had not yet permanently “altered” her<br />
nervous system, and she relied mostly on her limited social network and<br />
on home remedies, such as herbal teas. Early on during her current presentation,<br />
however, having come to see her condition as a physiological<br />
reaction to her interpersonal problems, she sought help first from primary<br />
care internists. They in turn referred her to inpatient psychiatric<br />
care, which <strong>the</strong> patient always understood as being sent to <strong>the</strong> medical<br />
specialists of <strong>the</strong> nervous system (“<strong>the</strong> doctors <strong>for</strong> nervios”). This was<br />
a <strong>for</strong>tunate reframing of her treatment, since an alternative and fairly<br />
common interpretation in her <strong>cultural</strong> group could have been to reject<br />
<strong>the</strong> psychiatric referral as a sign that <strong>the</strong> clinicians mistakenly thought<br />
that she was losing her mind. Over time, she accepted some <strong>for</strong>ms of<br />
mental health treatment but refused o<strong>the</strong>rs, due to a mixture of <strong>cultural</strong><br />
and personality characteristics. Family <strong>the</strong>rapy, <strong>for</strong> example, met<br />
her view that an improved relationship with her son would help her recover<br />
from her illness, and was enthusiastically accepted. O<strong>the</strong>r <strong>for</strong>ms<br />
of psycho<strong>the</strong>rapy directed more at intrapsychic change, such as group<br />
<strong>the</strong>rapy, met intense resistance. Day hospital care came to be experienced<br />
as relatively unfocused and off-<strong>the</strong>-mark; instead, patient sought<br />
daily visits with her daughter-in-law, where she could re-establish socialization<br />
skills with family members. Her view of nervios as a medical<br />
condition never fully disappeared. She felt best protected from relapse<br />
by periodic check-ups with a psychiatrist, even when no medications<br />
were prescribed; <strong>the</strong> ongoing decision not to medicate reassured her<br />
that her condition remained stable. Interestingly, despite <strong>the</strong> view that<br />
her perceptual distortions were due to spiritual “weakness,” she never<br />
sought <strong>the</strong> help of folk healers, saying “I don’t believe in any of that.”<br />
This highlights <strong>the</strong> intra-ethnic variation in help-seeking pathways,<br />
since many Puerto Ricans seek <strong>the</strong> assistance of espiritistas and o<strong>the</strong>r<br />
spiritual healers at some point during <strong>the</strong> course of <strong>the</strong>ir illness (42).<br />
Cultural Factors Related to Psychosocial Environment<br />
and Levels of Functioning<br />
This section of <strong>the</strong> CF model allows <strong>the</strong> clinician to examine how culture<br />
patterns some of <strong>the</strong> stressors patients are exposed to and <strong>the</strong>ir reactions<br />
to <strong>the</strong>se situations; <strong>the</strong> social supports available to <strong>the</strong>m; and <strong>the</strong><br />
contexts against which <strong>the</strong>ir levels of functioning should be measured.<br />
Among o<strong>the</strong>r stressors, this part of <strong>the</strong> assessment can be used to elicit<br />
patients’ experiences of trauma and how <strong>the</strong>y incorporate <strong>the</strong>se events<br />
into <strong>the</strong>ir ongoing interpersonal relationships.
288 PSYCHIATRIC QUARTERLY<br />
Social Stressors. How does <strong>the</strong> patient’s <strong>cultural</strong> background clarify<br />
<strong>the</strong> origin and impact of <strong>the</strong> stressors she experienced?<br />
The main stressor affecting <strong>the</strong> patient at <strong>the</strong> time of her presentation<br />
was her estrangement from all of her children, which contradicts traditional<br />
values regarding an extended and close family centered around<br />
a matriarch. The patient alternated between feeling that this situation<br />
was unfair and that it was a deserved punishment <strong>for</strong> abandoning four<br />
of her children in childhood. That decision, which she described as <strong>the</strong><br />
hardest of her life, was influenced by several social and <strong>cultural</strong> <strong>factors</strong>.<br />
These include: <strong>the</strong> existence at that time of very few nonfamily<br />
supports <strong>for</strong> abused women in rural Puerto Rico; <strong>the</strong> emergence of migration<br />
as a government-sponsored escape valve <strong>for</strong> a labor <strong>for</strong>ce made<br />
redundant by rapid industrialization; her parents’ lack of support <strong>for</strong><br />
marital separation, even in <strong>the</strong> case of physical abuse; a tradition in<br />
rural Puerto Rico of placing “extra” children in in<strong>for</strong>mal foster arrangements<br />
with close relatives; and <strong>the</strong> expectation by some new male sexual<br />
partners (<strong>the</strong> man who became <strong>the</strong> patient’s second husband) that<br />
<strong>the</strong>y not be expected to maintain non-infant children from a previous<br />
marriage.<br />
Seen over <strong>the</strong> course of her lifetime, <strong>the</strong> patient’s stressors were severe,<br />
and included <strong>the</strong> family disruption caused by her fa<strong>the</strong>r’s alcoholism,<br />
her husband’s physical abuse, <strong>the</strong> death of a child in infancy,<br />
<strong>the</strong> dispersion of her nuclear family and <strong>the</strong> consequent discord with<br />
her parents and children, difficulties in acculturation to <strong>the</strong> US, ethnic<br />
discrimination, chronic poverty and unemployment, <strong>the</strong> murder of<br />
her second husband, and her children’s substance abuse and subsequent<br />
loss of child custody. These stressors were considered by <strong>the</strong> patient<br />
and her community to be adequate explanation of her nervios<br />
illness.<br />
Social Supports. How does her <strong>cultural</strong> identity contribute to <strong>the</strong><br />
amount, nature, and quality of her social supports?<br />
As a “circular” migrant who engaged in several migratory cycles and<br />
frequent trips to Puerto Rico, <strong>the</strong> patient’s supports beyond her son,<br />
daughter-in-law, and caregivers consisted only of community drop-in<br />
centers and a few elderly Latinas. Her lack of supports probably contributed<br />
to <strong>the</strong> length of her hospitalizations, as her fear of going home<br />
seemed to worsen her suicidality whenever discharge was discussed.<br />
Clinicians’ ef<strong>for</strong>ts to expand her support system through group <strong>the</strong>rapy<br />
membership and psychiatric social clubs were hindered by her<br />
character pathology. Most of <strong>the</strong> patient’s symptoms, including her suicidal<br />
ataques, may be understood as attempts to expand her social
ROBERTO LEWIS-FERNÁNDEZ AND NAELYS DÍAZ 289<br />
support network by engaging <strong>the</strong> attention of family members as well<br />
as professional caregivers. The patient always retained <strong>the</strong> belief that<br />
in <strong>the</strong> face of her overwhelming social limitations and <strong>the</strong> original recalcitrance<br />
of her children, only <strong>the</strong> full expression of her symptomatology<br />
could have produced a positive outcome.<br />
Levels of Functioning and Disability. How does <strong>the</strong> patient’s <strong>cultural</strong><br />
environment affect her level of functioning and degree of impairment?<br />
Prior to her improvement, <strong>the</strong> patient saw her illness as progressive<br />
and without cure, and feared degeneration into permanent insanity,<br />
consistent with widespread <strong>cultural</strong> concerns about severe nervios. As<br />
a result of treatment, she came to feel that her nervios had not progressed<br />
as far as she had feared, but that she would always remain<br />
permanently vulnerable to relapse if confronted with more stress than<br />
she could handle, especially in her family interactions. She interpreted<br />
<strong>the</strong> intermittent appearance of anxiety and depressive symptoms as<br />
signs of ongoing nervios illness which entitled her to lifelong subsidized<br />
housing and financial support from <strong>the</strong> government. Her age and<br />
limited <strong>for</strong>mal education, job skills, and English fluency in any case<br />
narrowed her employment opportunities considerably and contributed<br />
to her expectation of government support. Un<strong>for</strong>tunately, <strong>the</strong> absence<br />
of organized activities such as work also hindered <strong>the</strong> development<br />
of a social network beyond her family, which may have helped to decompress<br />
<strong>the</strong> patient’s dependence on a limited number of supportive<br />
contacts.<br />
Cultural Elements of <strong>the</strong> Clinician–Patient Relationship<br />
This section allows <strong>the</strong> clinician to consider how his/her own role or<br />
institutional setting has affected <strong>the</strong> patient’s illness experience, including<br />
symptom expression and treatment response. The scientific<br />
emphases on objectivity and material reality sometimes cause psychiatrists<br />
to mistake <strong>the</strong>ir activity <strong>for</strong> that of invisible observers, who exert<br />
little effect on <strong>the</strong> situation observed. On <strong>the</strong> contrary, much clinical<br />
and ethnographic research has described how patients’ symptom descriptions<br />
and etiological attributions are shaped across health care<br />
settings in response to clinicians’ verbal and nonverbal elicitations and<br />
to individual and collective expectations of what <strong>the</strong> purpose and <strong>the</strong><br />
norms are <strong>for</strong> each kind of setting (38,43). What counts as good and<br />
bad outcomes also varies across <strong>the</strong>rapeutic interactions, depending<br />
on whe<strong>the</strong>r <strong>the</strong> patient and caregiver are focusing on symptoms, longterm<br />
morbidity and mortality, psychosocial functioning, interpersonal
290 PSYCHIATRIC QUARTERLY<br />
relationships, existential adjustment, ecological integration, or spiritual<br />
well-being. The clinical encounter is always a negotiated experience<br />
(44) that in addition echoes a wider system of institutional relationships,<br />
such as <strong>the</strong> organization of health care services, <strong>the</strong> influence of<br />
third-party review, and pressures brought to bear by employers (22).<br />
The clinical relationship is also impacted by ethno-<strong>cultural</strong> clashes in<br />
<strong>the</strong> society at large, requiring clinicians to examine <strong>the</strong>ir attitudes toward<br />
a patient’s ethnicity and culture and how <strong>the</strong>se impact <strong>the</strong> <strong>the</strong>rapeutic<br />
encounter. This understanding can be helpful not only in terms<br />
of evaluating <strong>the</strong> role of <strong>cultural</strong> differences in <strong>the</strong> interpretation of<br />
patients’ presentations, but also in avoiding biases based on ethnic<br />
stereotypes or o<strong>the</strong>r aspects of <strong>cultural</strong> identity (13). The current section<br />
encourages a systematic reflection on <strong>the</strong>se interactions.<br />
In <strong>the</strong> case of this patient, her psychiatric care prior to her referral<br />
to <strong>the</strong> outpatient Latino Clinic was hindered by <strong>the</strong> inpatient unit’s<br />
lack of <strong>cultural</strong> in<strong>for</strong>mation on various aspects of her presentation that<br />
have been outlined in this Formulation. In particular, <strong>the</strong> diagnostic<br />
process was limited by <strong>the</strong> absence of a <strong>cultural</strong>ly normative assessment<br />
of <strong>the</strong> patient’s character structure, which resulted in <strong>the</strong> overemphasis<br />
of her Axis I symptoms and a missed diagnosis of Borderline<br />
Personality Disorder. Likewise, lack of in<strong>for</strong>mation about <strong>the</strong> <strong>cultural</strong><br />
characteristics of nervios and ataques led to <strong>the</strong> misinterpretation of<br />
her perceptual distortions as psychotic symptoms, with consequences<br />
<strong>for</strong> <strong>the</strong> patient’s psychopharmacological treatment. Finally, <strong>the</strong> inpatient<br />
unit’s reliance on pharmacological ra<strong>the</strong>r than psycho<strong>the</strong>rapeutic<br />
interventions was not fully consonant with <strong>the</strong> patient’s treatment<br />
expectations.<br />
The lack of relevant <strong>cultural</strong> in<strong>for</strong>mation contrasts with <strong>the</strong> unit’s<br />
attention to more purely ethnic issues, such as <strong>the</strong> frequent use of<br />
Spanish interpreters to ensure <strong>the</strong> patient’s participation in <strong>the</strong><br />
milieu, and <strong>the</strong> focus on “ethnic matching” (45), achieved by assigning<br />
a Latino psychiatry resident to her care. The emphasis on ethnicity<br />
alone ra<strong>the</strong>r than culture is a problematic characteristic of contemporary<br />
US psychiatry that can lead, as in this case, to <strong>the</strong>rapeutic practices<br />
that only go partway toward eliciting <strong>the</strong> relevant points of difference<br />
in <strong>the</strong> patient’s presentation and treatment response (46). The use of<br />
Spanish, <strong>for</strong> example, is absolutely necessary <strong>for</strong> <strong>assessing</strong> a non-<br />
English speaking Latina such as this patient, but is not sufficient as<br />
a <strong>cultural</strong>ly valid intervention; <strong>for</strong> that, <strong>the</strong>rapeutic approaches based<br />
on <strong>cultural</strong> in<strong>for</strong>mation are also required. Ethnic matching does not<br />
guarantee access to this material, since persons from <strong>the</strong> same ethnic<br />
background can differ in terms of <strong>cultural</strong> experience and clinicians may
ROBERTO LEWIS-FERNÁNDEZ AND NAELYS DÍAZ 291<br />
be influenced less by <strong>the</strong>ir culture of origin than by <strong>the</strong>ir professional<br />
context.<br />
Referral to an outpatient clinic with an explicitly <strong>cultural</strong> focus resulted<br />
in a more comprehensive evaluation <strong>for</strong> <strong>the</strong> patient, leading to a<br />
process of rediagnosis and to <strong>the</strong> implementation of psycho<strong>the</strong>rapeutic<br />
interventions more in accord with her expectations, with more successful<br />
clinical results.<br />
Overall Cultural Assessment<br />
The final section of <strong>the</strong> Cultural Formulation summarizes <strong>the</strong> in<strong>for</strong>mation<br />
in <strong>the</strong> previous sections, focusing on <strong>cultural</strong> material that contributes<br />
to diagnosis and treatment. The role that <strong>cultural</strong> features<br />
have played in determining overall illness outcome are particularly<br />
emphasized.<br />
In this case, <strong>the</strong> overall assessment would mention that <strong>the</strong> patient’s<br />
<strong>cultural</strong> identity is that of a rural Puerto Rican migrant with limited<br />
<strong>for</strong>mal education, who speaks Spanish exclusively and has only lived<br />
<strong>for</strong> limited periods in <strong>the</strong> US, resulting in minimal acculturation. Her<br />
psychopathology is expressed in <strong>the</strong> traditional Puerto Rican idioms of<br />
nervios and ataques de nervios. She attributed <strong>the</strong> origin of <strong>the</strong>se problems<br />
and her relapsing course to multiple past stressors and traumas,<br />
and especially to unresolved conflicts with her children resulting from<br />
her prolonged separation from <strong>the</strong>m during childhood. In fact, her clinical<br />
condition did not improve until <strong>the</strong>ir affective breach was addressed<br />
in family <strong>the</strong>rapy.<br />
The patient’s initial inpatient treatment proved ineffective partly<br />
because of <strong>the</strong> misattribution of a psychotic label to her perceptual<br />
distortions, which are normative idioms of distress <strong>for</strong> this <strong>cultural</strong><br />
group. Misdiagnosis exposed patient to <strong>the</strong> potentially toxic effects of<br />
antipsychotic medication and interfered with referral to family <strong>the</strong>rapy.<br />
In addition, lack of <strong>cultural</strong> in<strong>for</strong>mation also hindered <strong>the</strong> identification<br />
of patient’s underlying Axis II pathology and obscured <strong>the</strong><br />
relationship between her character disorder and her persistent Axis I<br />
symptoms, including her chronic suicidality and its exacerbations in<br />
<strong>the</strong> <strong>for</strong>m of ataques. Pharmacologic treatment of <strong>the</strong> patient’s refractory<br />
depression—dangerous anyway due to her impulsive suicidality—<br />
proved unnecessary once intensive family intervention was underway.<br />
Her remaining intermittent Axis I symptoms led to periodic distress,<br />
warranting NOS diagnoses. But <strong>the</strong> patient’s primary psychopathology<br />
proved to be characterological, fulfilling criteria <strong>for</strong> Borderline<br />
Personality Disorder. Like many patients with this disorder, she
292 PSYCHIATRIC QUARTERLY<br />
displayed recurrent dysphoria, though in her case she did not meet<br />
strict criteria <strong>for</strong> Dysthymia. Unlike many Borderline patients, however,<br />
her course over <strong>the</strong> subsequent 8 years was remarkably uneventful<br />
after her initial response to psycho<strong>the</strong>rapy, perhaps reflecting <strong>cultural</strong><br />
variation in <strong>the</strong> treatment outcome of Borderline Personality Disorder.<br />
CONCLUSION<br />
In this article we have presented <strong>the</strong> Cultural Formulation (CF) model<br />
<strong>for</strong> clinical assessment, discussing its historical development and its<br />
components as outlined in Appendix I of DSM-IV. We also illustrated<br />
<strong>the</strong> application of <strong>the</strong> model with a case scenario of a Puerto Rican<br />
woman suffering from <strong>the</strong> Latino popular syndromes of nervios and<br />
ataques whose care was markedly improved by <strong>the</strong> implementation of<br />
a <strong>cultural</strong> evaluation such as <strong>the</strong> one outlined.<br />
At a time in which <strong>the</strong> value of delivering <strong>cultural</strong>ly congruent care<br />
is increasingly being recognized and requirements <strong>for</strong> <strong>cultural</strong> assessment<br />
are being incorporated into treatment guidelines and professional<br />
training curricula, <strong>the</strong> Cultural Formulation model represents one of<br />
<strong>the</strong> main existing <strong>method</strong>s <strong>for</strong> attaining and implementing a <strong>cultural</strong>ly<br />
valid approach to care (12). Regular use of <strong>the</strong> model teaches clinicians<br />
not only how to elicit <strong>cultural</strong>ly relevant clinical material, but also exposes<br />
<strong>the</strong>m over time to <strong>the</strong> content of many <strong>cultural</strong> perspectives from<br />
diverse patients and <strong>the</strong>ir families, thus increasing caregivers’ fund of<br />
<strong>cultural</strong> knowledge.<br />
The growing <strong>cultural</strong> pluralism of US society requires that <strong>the</strong> CF<br />
model become an essential aspect of every clinical training program.<br />
The “long version” of <strong>the</strong> model, such as <strong>the</strong> one described in this article,<br />
can be taught during clinical supervision as part of comprehensive<br />
patient assessments. This is <strong>the</strong> <strong>for</strong>mat we are using during <strong>the</strong> outpatient<br />
year (PGY-III) at <strong>the</strong> Adult Psychiatry Residency Program of<br />
Columbia University and NY State Psychiatric Institute. The “short<br />
version” of <strong>the</strong> model, similar to <strong>the</strong> Overall Cultural Assessment section<br />
of <strong>the</strong> full Formulation, could <strong>the</strong>n be used <strong>for</strong> all new evaluations<br />
or comprehensive reassessments of refractory patients once proficiency<br />
in <strong>the</strong> full CF model is established.<br />
It is also imperative that research be conducted on <strong>the</strong> effectiveness<br />
of <strong>the</strong> Cultural Formulation as a <strong>method</strong> <strong>for</strong> improving treatment outcomes,<br />
including assessment of its cost-benefit ratio. Findings from this<br />
research will help clarify <strong>the</strong> contribution of <strong>the</strong> CF model to clinical<br />
care, and prepare <strong>the</strong> way <strong>for</strong> its role in DSM-V.
ROBERTO LEWIS-FERNÁNDEZ AND NAELYS DÍAZ 293<br />
ACKNOWLEDGMENTS<br />
Dr. Lewis-Fernández was supported by a National Institute of Mental<br />
Health (NIMH) Under-represented Minority Research Supplement<br />
(5 R10 MH55165). Ms. Díaz was supported by NIMH grant T32<br />
MH20074 to <strong>the</strong> Center <strong>for</strong> Hispanic Mental Health Research at<br />
Fordham University.<br />
REFERENCES<br />
1. Desjarlais R, Eisenberg L, Good B, Kleinman A: World Mental Health: Problems and<br />
Priorities in Low-Income Countries, New York, Ox<strong>for</strong>d University Press, 1995.<br />
2. Mukherjee S, Shukla S, Woodle J, Rosen AM, Olante S: Misdiagnosis of schizophrenia<br />
in bipolar patients: A multiethnic comparison. American Journal of Psychiatry<br />
140:1571–1574, 1983.<br />
3. Strakowski SM, Flaum M, Amador X, Bracha HS, Pandurangi AK, Robinson D, Tohen<br />
M: Racial differences in <strong>the</strong> diagnosis of psychosis. Schizophrenia Research 21:117–<br />
124, 1996.<br />
4. Strakowski SM, Hawkins JM, Keck PE, McElroy SL, West SA, Bourne ML, Sax KW,<br />
Tugrul MC: The effects of race and in<strong>for</strong>mation variance on disagreement between<br />
psychiatric emergency service and research diagnoses in first-episode psychosis. Journal<br />
of Clinical Psychiatry 58:457–463, 1997.<br />
5. Good BJ, Delvecchio-Good M-J: Toward a meaning-centered analysis of popular<br />
illness categories: “Fright-illness” and “heart distress” in Iran. In: Marsella AJ, White<br />
GM, eds., Cultural Conceptions of Mental Health and Therapy, Dordrecht, D. Reidel,<br />
1982, pp. 141–166.<br />
6. Kleinman A: Rethinking Psychiatry: From Cultural Category to Personal Experience,<br />
New York, The Free Press, 1988.<br />
7. Zheng YP, Lin KM, Takeuchi D, Kuralski KS, Wang YX, Cheung F: An epidemiological<br />
study of neuras<strong>the</strong>nia in Chinese-Americans in Los Angeles. Comprehensive<br />
Psychiatry 38:249–259, 1997.<br />
8. Lee S, Wing Y, Chan C, Lee AM, Lee DTS, Chen CN, Lin KM, Weiss MG: Psychiatric<br />
morbidity and illness experience of primary care patients with chronic fatigue in<br />
Hong Kong. American Journal of Psychiatry 157:380–384, 2000.<br />
9. Guarnaccia PJ, Rivera M, Franco F, Neighbors C: The experiences of ataques de<br />
nervios: Towards an anthropology of emotions in Puerto Rico. Culture, Medicine and<br />
Psychiatry 20:343–367, 1996.<br />
10. Guarnaccia PJ, Canino G, Rubio-Stipec M, Bravo M: The prevalence of ataques de<br />
nervios in <strong>the</strong> Puerto Rico Disaster Study. Journal of Nervous and Mental Disease<br />
181:157–165, 1993.<br />
11. Lewis-Fernández R, Garrido P, Bennasar M, Parrilla E, Laria AJ, Ma G,<br />
Petkova E: Dissociation, childhood trauma, and ataque de nervios among Puerto<br />
Rican psychiatric outpatients. American Journal of Psychiatry, 159:1603–1605,<br />
2002.<br />
12. Group <strong>for</strong> <strong>the</strong> Advancement of Psychiatry Committee on Cultural Psychiatry: Cultural<br />
Assessment in Clinical Psychiatry, Washington, D.C., American Psychiatric<br />
Publishing, 2001.
294 PSYCHIATRIC QUARTERLY<br />
13. Lu FG, Lim RF, Mezzich JE: Issues in <strong>the</strong> assessment and diagnosis of <strong>cultural</strong>ly<br />
diverse individuals. In: Oldham JM, Riba MB, eds., Review of Psychiatry, Vol. 14,<br />
Washington, D.C., APA Press, 1995, pp. 477–510.<br />
14. Lewis-Fernández R: Cultural <strong><strong>for</strong>mulation</strong> of psychiatric diagnosis. Culture, Medicine<br />
and Psychiatry 20:133–144, 1996.<br />
15. Mezzich JE: Cultural <strong><strong>for</strong>mulation</strong> and comprehensive diagnosis: Clinical and research<br />
perspectives. Psychiatric Clinics of North America 18:649–657, 1995.<br />
16. American Psychiatric Association: Diagnostic and Statistical Manual of Mental<br />
Disorders, Fourth Edition (DSM-IV), Washington, D.C., 1994.<br />
17. Smedley A: “Race” and <strong>the</strong> construction of human identity. American Anthropologist<br />
100:690–702, 1999.<br />
18. Alarcón RD: Culture and psychiatric diagnosis: Impact on DSM-IV and ICD-10.<br />
Psychiatric Clinics of North America 18:449–465, 1995.<br />
19. Kleinman A: The Illness Narratives: Suffering, Healing, and <strong>the</strong> Human Condition,<br />
New York, Basic Books, 1988.<br />
20. Weiss M: Explanatory Model Interview Catalogue (EMIC): Framework <strong>for</strong> comparative<br />
study of illness. Trans<strong>cultural</strong> Psychiatry 34:235–263, 1997.<br />
21. Saris JA: Telling stories: Life histories, illness narratives, and institutional landscapes.<br />
Culture, Medicine and Psychiatry 19:39–72, 1995.<br />
22. Mechanic D: The experience and expression of distress: The study of illness behavior<br />
and medical utilization. In Mechanic D, ed., Handbook of Health, Health<br />
Care, and <strong>the</strong> Health Professions, New York, The Free Press, 1983, pp. 591–<br />
607.<br />
23. Lewis-Fernández R: Diagnosis and treatment of nervios and ataques in a female<br />
Puerto Rican migrant. Culture, Medicine and Psychiatry 20:155–163, 1996.<br />
24. Hernández-Cruz J: Migración de retorno o circulación de obreros boricuas? Revista<br />
de Ciencias Sociales 24:81–102, 1985.<br />
25. Rodríguez CE: Puerto Ricans: Born in <strong>the</strong> U.S.A., Boulder, Westview Press, 1991.<br />
26. Oquendo MA: Psychiatric evaluation and psycho<strong>the</strong>rapy in <strong>the</strong> patient’s second language.<br />
Psychiatric Services 47:614–618, 1996.<br />
27. Alarcón RD, Foulks EF, Vakkur M: Personality Disorders and Culture: Clinical and<br />
Conceptual Interactions, New York, Wiley, 1998.<br />
28. Lewis-Fernández R, Kleinman A: Culture, personality, and psychopathology. Journal<br />
of Abnormal Psychology 103:67–71, 1994.<br />
29. Rogler LH, Cortés DE, Malgady RG: Acculturation and mental health status among<br />
Hispanics. American Psychologist 46:585–597, 1991.<br />
30. Marín G, Gamba RJ: A new measurement of acculturation <strong>for</strong> Hispanics: The<br />
Bidimensional Acculturation Scale <strong>for</strong> Hispanics (BAS). Hispanic Journal of Behavioral<br />
Sciences 18:297–316, 1996.<br />
31. Good BJ: Medicine, Rationality, and Experience: An Anthropological Perspective,<br />
Cambridge, Cambridge University Press, 1994.<br />
32. McKinlay JB: Social network influences on morbid episodes and <strong>the</strong> career of helpseeking.<br />
In: Eisenberg L, Kleinman A, eds., The Relevance of Social Science <strong>for</strong><br />
Medicine, Dordrecht, D. Reidel, 1981, pp. 77–107.<br />
33. Nichter M: Idioms of distress: Alternatives in <strong>the</strong> expression of psychosocial<br />
distress: A case study from South India. Culture, Medicine and Psychiatry 5:379–408,<br />
1981.<br />
34. Guarnaccia PJ, Lewis-Fernández R, Rivera M: Towards a Puerto Rican popular<br />
nosology: Nervios and ataques de nervios. Culture, Medicine and Psychiatry,<br />
in press.
ROBERTO LEWIS-FERNÁNDEZ AND NAELYS DÍAZ 295<br />
35. Lewis-Fernández R, Canino G, Ramírez R, Febo V, Bravo M: Latino perspectives on<br />
mental health in primary care. In: Proceedings of <strong>the</strong> 49th Institute on Psychiatric<br />
Services, American Psychiatric Association, 1997, p. 142.<br />
36. López SR: Patient variable biases in clinical judgment: Conceptual overview and<br />
<strong>method</strong>ological considerations. Psychological Bulletin 106:184–203, 1989.<br />
37. Jenkins JH, Karno M: The meaning of expressed emotion: Theoretical issues raised<br />
by cross-<strong>cultural</strong> research. American Journal of Psychiatry 149:9–21, 1992.<br />
38. Kleinman A: Patients and Healers in <strong>the</strong> Context of Culture, Berkeley, University of<br />
Cali<strong>for</strong>nia Press, 1980.<br />
39. Marsella AJ, White GM: Cultural Conceptions of Mental Health and Therapy,<br />
Dordrecht, D. Reidel, 1982.<br />
40. Lewis-Fernández R: “That was not in me ...I couldn’t control myself”: Control, identity,<br />
and emotion in Puerto Rican communities [Spanish]. Revista de Ciencias Sociales<br />
4:268–299, 1998.<br />
41. Rogler LH, Cortés DE: Help-seeking pathways: A unifying concept in mental health<br />
care. American Journal of Psychiatry 150:554–561, 1993.<br />
42. Garrison V: Doctor, espiritista or psychiatrist?: Health-seeking behavior in a Puerto<br />
Rican neighborhood of New York City. Medical Anthropology 1:65–191, 1977.<br />
43. Good BJ, Delvecchio-Good M-J: The meaning of symptoms: A <strong>cultural</strong> hermeneutic<br />
model <strong>for</strong> clinical practice. In: Eisenberg L, Kleinman A, eds., The Relevance of Social<br />
Science <strong>for</strong> Medicine, Dordrecht, D. Reidel, 1980, pp. 165–196.<br />
44. Lazare A, Eisenthal S, Wasserman L: The customer approach to patienthood.<br />
Archives of General Psychiatry 32:553–558, 1975.<br />
45. Sue S, Fujino DC, Hu LT, Takeuchi DT, Zane NWS: Community mental health services<br />
<strong>for</strong> ethnic minority groups: A test of <strong>the</strong> <strong>cultural</strong> responsiveness hypo<strong>the</strong>sis. Journal<br />
of Consulting and Clinical Psychology 59:533–540, 1991.<br />
46. Whaley AL: Cultural mistrust: An important psychological construct <strong>for</strong> diagnosis<br />
and treatment of African Americans. Professional Psychology: Research and Practice<br />
32:555–562, 2001.