Effect of weight on indwelling catheter use among long-term ... - SUNA
Effect of weight on indwelling catheter use among long-term ... - SUNA
Effect of weight on indwelling catheter use among long-term ... - SUNA
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Research<br />
<str<strong>on</strong>g>Effect</str<strong>on</strong>g> <str<strong>on</strong>g>of</str<strong>on</strong>g> Weight <strong>on</strong> Indwelling<br />
Catheter Use am<strong>on</strong>g L<strong>on</strong>g-Term<br />
Care Facility Residents<br />
Holly C. Felix, Jeffrey D. Thostens<strong>on</strong>, Zoran Bursac, and Christine Bradway<br />
L<strong>on</strong>g-<strong>term</strong> <strong>use</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> indwell -<br />
ing urinary <strong>catheter</strong>s for<br />
urinary inc<strong>on</strong>tinence (UI)<br />
is not recommended (Cen-<br />
ters for Disease C<strong>on</strong>trol and Pre -<br />
venti<strong>on</strong> [CDC]/Nati<strong>on</strong>al Health -<br />
care Safety Network, 2009; Cen -<br />
ters for Medicare & Medicaid<br />
Services [CMS], 2005) beca<strong>use</strong><br />
<strong>indwelling</strong> urinary <strong>catheter</strong>s can<br />
increase the risk for urinary tract<br />
infecti<strong>on</strong>s, urethral complicati<strong>on</strong>s,<br />
bladder st<strong>on</strong>es, and bladder<br />
cancer (Igawa, Wyndaele, &<br />
Nishizawa, 2008), as well as mortality<br />
(Landi et al., 2004). Never -<br />
theless, their <strong>use</strong> can be c<strong>on</strong>sidered<br />
for management <str<strong>on</strong>g>of</str<strong>on</strong>g> UI in<br />
very specific circumstances (see<br />
Table 1). However, over<strong>use</strong> or<br />
inappropriate <strong>use</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> <strong>indwelling</strong><br />
urinary <strong>catheter</strong>s may occur<br />
(Doughty & Kisanga, 2010).<br />
Holly C. Felix, PhD, MPA, is an Assistant<br />
Pr<str<strong>on</strong>g>of</str<strong>on</strong>g>essor, University <str<strong>on</strong>g>of</str<strong>on</strong>g> Arkansas for Med -<br />
ical Sciences, Little Rock, AR.<br />
Jeffrey D. Thostens<strong>on</strong>, MS, is a Research<br />
Associate, University <str<strong>on</strong>g>of</str<strong>on</strong>g> Arkansas for Med -<br />
ical Sciences, Little Rock, AR.<br />
Zoran Bursac, PhD, is an Associate Pro -<br />
fessor, University <str<strong>on</strong>g>of</str<strong>on</strong>g> Arkansas for Medical<br />
Sciences, Little Rock, AR.<br />
Christine Bradway, PhD, RN, FAAN, is an<br />
Associate Pr<str<strong>on</strong>g>of</str<strong>on</strong>g>essor <str<strong>on</strong>g>of</str<strong>on</strong>g> Ger<strong>on</strong>tological<br />
Nursing, University <str<strong>on</strong>g>of</str<strong>on</strong>g> Pennsylvania School<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> Nursing, Philadelphia, PA; and a member<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> the Urologic Nursing Editorial Board.<br />
Acknowledgements: The authors acknow -<br />
ledge support from the Arkansas Center for<br />
Minority Health Disparities, funded by the<br />
Nati<strong>on</strong>al Institute for Minority Health Dis -<br />
parities under award 5PO20MD002329.<br />
© 2013 Society <str<strong>on</strong>g>of</str<strong>on</strong>g> Urologic Nurses and Associates<br />
Felix, H.S., Thostens<strong>on</strong>, J.D., Bursac, Z., & Bradway, C. (2013). <str<strong>on</strong>g>Effect</str<strong>on</strong>g> <str<strong>on</strong>g>of</str<strong>on</strong>g> <str<strong>on</strong>g>weight</str<strong>on</strong>g> <strong>on</strong><br />
<strong>indwelling</strong> <strong>catheter</strong> <strong>use</strong> am<strong>on</strong>g l<strong>on</strong>g-<strong>term</strong> care facility residents. Urologic<br />
Nursing, 33(3). doi:10.7257/1053-816X.2013.33.3.<br />
This study examined the effect <str<strong>on</strong>g>of</str<strong>on</strong>g> obesity <strong>on</strong> the <strong>use</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> <strong>indwelling</strong> urinary<br />
<strong>catheter</strong>s am<strong>on</strong>g l<strong>on</strong>g-<strong>term</strong> care facility residents and found initial increases in<br />
usage by <str<strong>on</strong>g>weight</str<strong>on</strong>g> category, which declined during the next 12 m<strong>on</strong>ths.<br />
Key Words:<br />
Obesity, older adults, l<strong>on</strong>g-<strong>term</strong> care facilities, <strong>indwelling</strong><br />
urinary <strong>catheter</strong>s.<br />
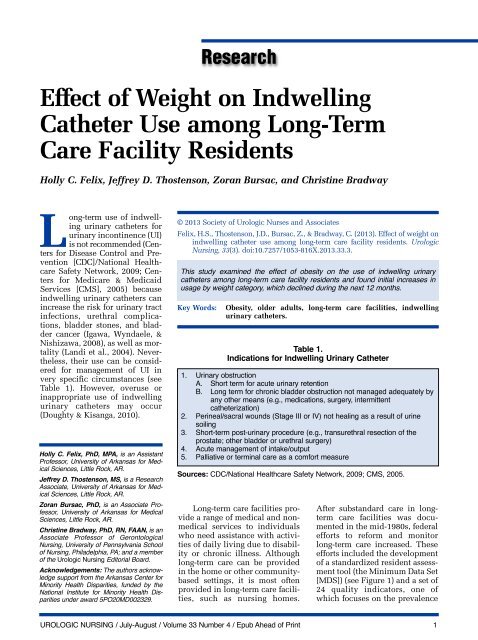
Table 1.<br />
Indicati<strong>on</strong>s for Indwelling Urinary Catheter<br />
1. Urinary obstructi<strong>on</strong><br />
A. Short <strong>term</strong> for acute urinary retenti<strong>on</strong><br />
B. L<strong>on</strong>g <strong>term</strong> for chr<strong>on</strong>ic bladder obstructi<strong>on</strong> not managed adequately by<br />
any other means (e.g., medicati<strong>on</strong>s, surgery, in<strong>term</strong>ittent<br />
<strong>catheter</strong>izati<strong>on</strong>)<br />
2. Perineal/sacral wounds (Stage III or IV) not healing as a result <str<strong>on</strong>g>of</str<strong>on</strong>g> urine<br />
soiling<br />
3. Short-<strong>term</strong> post-urinary procedure (e.g., transurethral resecti<strong>on</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> the<br />
prostate; other bladder or urethral surgery)<br />
4. Acute management <str<strong>on</strong>g>of</str<strong>on</strong>g> intake/output<br />
5. Palliative or <strong>term</strong>inal care as a comfort measure<br />
Sources: CDC/Nati<strong>on</strong>al Healthcare Safety Network, 2009; CMS, 2005.<br />
L<strong>on</strong>g-<strong>term</strong> care facilities provide<br />
a range <str<strong>on</strong>g>of</str<strong>on</strong>g> medical and n<strong>on</strong>medical<br />
services to individuals<br />
who need assistance with activities<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> daily living due to disability<br />
or chr<strong>on</strong>ic illness. Although<br />
l<strong>on</strong>g-<strong>term</strong> care can be provided<br />
in the home or other communitybased<br />
settings, it is most <str<strong>on</strong>g>of</str<strong>on</strong>g>ten<br />
provided in l<strong>on</strong>g-<strong>term</strong> care facilities,<br />
such as nursing homes.<br />
After substandard care in l<strong>on</strong>g<strong>term</strong><br />
care facilities was documented<br />
in the mid-1980s, federal<br />
efforts to reform and m<strong>on</strong>itor<br />
l<strong>on</strong>g-<strong>term</strong> care increased. These<br />
efforts included the development<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> a standardized resident assessment<br />
tool (the Minimum Data Set<br />
[MDS]) (see Figure 1) and a set <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
24 quality indicators, <strong>on</strong>e <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
which foc<strong>use</strong>s <strong>on</strong> the prevalence<br />
UROLOGIC NURSING / July-August / Volume 33 Number 4 / Epub Ahead <str<strong>on</strong>g>of</str<strong>on</strong>g> Print 1
Research Summary<br />
Background/Objectives<br />
Use <str<strong>on</strong>g>of</str<strong>on</strong>g> <strong>indwelling</strong> urinary <strong>catheter</strong>s am<strong>on</strong>g residents <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
l<strong>on</strong>g-<strong>term</strong> care facilities is low and within recommended<br />
thresholds. Utilizati<strong>on</strong> rates may be different by individual<br />
characteristics, including obesity status. We hypothesized<br />
that the challenges <str<strong>on</strong>g>of</str<strong>on</strong>g> providing c<strong>on</strong>tinence care for obese<br />
(body mass index ≥ 30) l<strong>on</strong>g-<strong>term</strong> care facility residents<br />
might increase the <strong>use</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> <strong>indwelling</strong> urinary <strong>catheter</strong>s<br />
am<strong>on</strong>g these residents.<br />
Design<br />
L<strong>on</strong>gitudinal cohort design.<br />
Setting<br />
All federally certified l<strong>on</strong>g-<strong>term</strong> care facilities in<br />
Arkansas.<br />
Participants<br />
All older adults (N = 3,879) admitted to federally certified<br />
l<strong>on</strong>g-<strong>term</strong> care facilities in Arkansas in quarter <strong>on</strong>e <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
2008.<br />
Measurements<br />
Minimum Data Set assessments at admissi<strong>on</strong> and at<br />
each quarter were <strong>use</strong>d to de<strong>term</strong>ine <strong>indwelling</strong> urinary<br />
<strong>catheter</strong> <strong>use</strong> and to obtain height and <str<strong>on</strong>g>weight</str<strong>on</strong>g> to calculate<br />
body mass index.<br />
Results<br />
There were significantly higher rates <str<strong>on</strong>g>of</str<strong>on</strong>g> <strong>indwelling</strong> urinary<br />
<strong>catheter</strong> <strong>use</strong> am<strong>on</strong>g obese residents at admissi<strong>on</strong> and<br />
in the sec<strong>on</strong>d quarter <str<strong>on</strong>g>of</str<strong>on</strong>g> the year. However, no differences<br />
between obese and n<strong>on</strong>-obese residents were detected in<br />
the third and fourth quarter when usage rates were nearly<br />
the same.<br />
C<strong>on</strong>clusi<strong>on</strong>s<br />
This research found initial differences in the usage <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
<strong>indwelling</strong> urinary <strong>catheter</strong>s am<strong>on</strong>g l<strong>on</strong>g-<strong>term</strong> care facility<br />
residents by <str<strong>on</strong>g>weight</str<strong>on</strong>g> status, with a higher percentage <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
obese residents having <strong>indwelling</strong> urinary <strong>catheter</strong>s than<br />
n<strong>on</strong>-obese residents over the six m<strong>on</strong>ths post-admissi<strong>on</strong>.<br />
Although lower usage rates <str<strong>on</strong>g>of</str<strong>on</strong>g> <strong>indwelling</strong> urinary <strong>catheter</strong>s<br />
are preferred for clinical reas<strong>on</strong>s, obese l<strong>on</strong>g-<strong>term</strong> care facility<br />
residents may prefer them to other inc<strong>on</strong>tinence strategies,<br />
which should be explored in future research.<br />
Level – II<br />
(Polit & Beck, 2012)<br />
Figure 1.<br />
Minimum Data Set (MDS)<br />
Federal regulati<strong>on</strong>s require c<strong>on</strong>tinuous and standardized clinical assessments <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
all residents <str<strong>on</strong>g>of</str<strong>on</strong>g> federally certified nursing homes in the United States. The MDS<br />
is a tool <strong>use</strong>d to c<strong>on</strong>duct the assessment, which covers 15 health status and<br />
physical functi<strong>on</strong>ing categories (listed below) and is designed to help nursing<br />
home staff identify and m<strong>on</strong>itor changes (particularly declines) in health status or<br />
functi<strong>on</strong>ing. Assessments are c<strong>on</strong>ducted up<strong>on</strong> admissi<strong>on</strong> to a facility quarterly,<br />
annually, and at the point <str<strong>on</strong>g>of</str<strong>on</strong>g> a significant event (e.g. admissi<strong>on</strong> to a hospital).<br />
Data extracted from the MDS are also <strong>use</strong>d to calculate the quality indicators<br />
<strong>use</strong>d by the Centers for Medicare & Medicaid Services to m<strong>on</strong>itor the quality <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
nursing home care.<br />
1. Cognitive patterns<br />
2. Communicati<strong>on</strong> and hearing<br />
patterns<br />
3. Visi<strong>on</strong> patterns<br />
4. Physical functi<strong>on</strong>ing and structural<br />
problems<br />
5. C<strong>on</strong>tinence<br />
6. Psychosocial well-being<br />
7. Mood and behavior patterns<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> <strong>indwelling</strong> urinary <strong>catheter</strong>s<br />
(Capitman, Leutz, Bishop, &<br />
Casler, 2005). Additi<strong>on</strong>ally, federal<br />
tags (F-tags) have been developed<br />
to provide care protocols for<br />
certain c<strong>on</strong>diti<strong>on</strong>s. F-tag 315 provides<br />
detailed guidance to l<strong>on</strong>g<strong>term</strong><br />
care facilities for the management<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> UI, including appropriate<br />
<strong>use</strong> and management <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
8. Activity pursuit patterns<br />
9. Disease diagnosis<br />
10. Other health c<strong>on</strong>diti<strong>on</strong>s<br />
11. Oral/nutriti<strong>on</strong>al status<br />
12. Oral/dental status<br />
13. Skin c<strong>on</strong>diti<strong>on</strong><br />
14. Medicati<strong>on</strong> <strong>use</strong><br />
15. Treatments and procedures<br />
<strong>indwelling</strong> urinary <strong>catheter</strong>s<br />
(Doughty & Kisanga, 2010).<br />
The current nati<strong>on</strong>al in -<br />
dwelling urinary <strong>catheter</strong> prevalence<br />
rate <str<strong>on</strong>g>of</str<strong>on</strong>g> 5% <str<strong>on</strong>g>of</str<strong>on</strong>g> l<strong>on</strong>g-<strong>term</strong> care<br />
facility residents (CMS, 2011) is<br />
within recommended thresholds,<br />
which range from 2.1% to 6.5%<br />
(Rantz et al., 2000). Certain l<strong>on</strong>g<strong>term</strong><br />
care facility residents, how-<br />
ever, may be at risk for over<strong>use</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
<strong>indwelling</strong> urinary <strong>catheter</strong>s.<br />
Research has shown that obesity<br />
(body mass index [BMI] greater<br />
than or equal to 30) is associated<br />
with UI (Hunskaar, 2008). Obese<br />
l<strong>on</strong>g-<strong>term</strong> care facility residents<br />
require significantly more assistance<br />
from staff for the performance<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> activities <str<strong>on</strong>g>of</str<strong>on</strong>g> daily living,<br />
including using the toilet (Felix,<br />
2008). One l<strong>on</strong>g-<strong>term</strong> care facility<br />
staff member reported in a qualitative<br />
study <strong>on</strong> the provisi<strong>on</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
c<strong>on</strong>tinence care for obese l<strong>on</strong>g<strong>term</strong><br />
care facility residents that<br />
“it’s more difficult for us [caregivers]<br />
… it always takes two<br />
[nursing aides] to clean [the resident]<br />
up after every inc<strong>on</strong>tinent<br />
episode…” (Bradway, Miller,<br />
Heivly, & Fleshner, 2010, p. 125).<br />
Beca<strong>use</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> staff burden to<br />
address UI am<strong>on</strong>g obese residents,<br />
we hypothesized these<br />
residents may be more likely to<br />
have an <strong>indwelling</strong> urinary<br />
<strong>catheter</strong>. At least <strong>on</strong>e study that<br />
examined <strong>indwelling</strong> urinary<br />
<strong>catheter</strong>s in l<strong>on</strong>g-<strong>term</strong> care facilities<br />
in five states found that those<br />
weighing 250 or more pounds<br />
were more likely to have an<br />
<strong>indwelling</strong> urinary <strong>catheter</strong> at<br />
2 UROLOGIC NURSING / July-August / Volume 33 Number 4 / Epub Ahead <str<strong>on</strong>g>of</str<strong>on</strong>g> Print
admissi<strong>on</strong>, at quarterly assessments,<br />
and at <strong>on</strong>e year (Rogers et<br />
al., 2008). How ever, this disparity<br />
in <strong>use</strong> is not regularly m<strong>on</strong>itored,<br />
nor has it been recently<br />
examined. Given the rising rates<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> obesity am<strong>on</strong>g older<br />
Americans (Flegal, Carroll,<br />
Ogden, & Curtin, 2010), and the<br />
associati<strong>on</strong> between obesity and<br />
l<strong>on</strong>g-<strong>term</strong> care facility admissi<strong>on</strong><br />
(Elkins et al., 2006; Valiyeva,<br />
Russell, Miller, & Safford, 2006),<br />
further examinati<strong>on</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> this issue<br />
is warranted, and it prompted the<br />
current analysis to assess differences<br />
in the utilizati<strong>on</strong> rates <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
<strong>indwelling</strong> urinary <strong>catheter</strong>s<br />
am<strong>on</strong>g obese and n<strong>on</strong>-obese<br />
l<strong>on</strong>g-<strong>term</strong> care facility residents.<br />
Methods<br />
This study utilized a l<strong>on</strong>gitudinal<br />
cohort design that followed<br />
all older adults (65 years <str<strong>on</strong>g>of</str<strong>on</strong>g> age or<br />
older) admitted to any federally<br />
certified l<strong>on</strong>g-<strong>term</strong> care facility in<br />
Arkansas and resided there for at<br />
least <strong>on</strong>e year.<br />
Data Source<br />
Data were obtained from the<br />
Arkansas MDS. The MDS c<strong>on</strong>tains<br />
federally required assessment<br />
data <strong>on</strong> physical and mental<br />
health c<strong>on</strong>diti<strong>on</strong>s, quality <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
life, and well-being (am<strong>on</strong>g other<br />
domains) <str<strong>on</strong>g>of</str<strong>on</strong>g> all residents in federally<br />
certified l<strong>on</strong>g-<strong>term</strong> care<br />
facilities in the United States (see<br />
Figure 1) (Wunderlich & Kohler,<br />
2001).<br />
Table 2.<br />
Characteristics <str<strong>on</strong>g>of</str<strong>on</strong>g> Older Arkansas L<strong>on</strong>g-Term Care Facility<br />
Residents (N = 3,879) at Admissi<strong>on</strong> and Associati<strong>on</strong>s with<br />
Indwelling Urinary Catheter Use over One Year from GEE Model<br />
Characteristics at Admissi<strong>on</strong><br />
C<strong>on</strong>tinuous Variables<br />
Variables<br />
The dependent variables <strong>on</strong><br />
<strong>indwelling</strong> urinary <strong>catheter</strong> <strong>use</strong><br />
for quarters two, three, and four<br />
were created using the Quality<br />
Measures User’s Manual formula<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> l<strong>on</strong>g-<strong>term</strong> care facility residents<br />
with an <strong>indwelling</strong> urinary<br />
<strong>catheter</strong> in the numerator and all<br />
residents in denominator (Abt<br />
Associates, Inc., 2004). The<br />
<strong>indwelling</strong> urinary <strong>catheter</strong> quality<br />
measure formula excludes the<br />
admissi<strong>on</strong> assessment. There -<br />
fore, the <strong>indwelling</strong> urinary<br />
<strong>catheter</strong>-dependent variable at<br />
admissi<strong>on</strong> in quarter <strong>on</strong>e <strong>use</strong>d<br />
the resp<strong>on</strong>se from the MDS questi<strong>on</strong><br />
<strong>on</strong> c<strong>on</strong>tinence applicati<strong>on</strong>s<br />
and programs (questi<strong>on</strong> H3) <strong>on</strong><br />
the admissi<strong>on</strong> assessment. Sec -<br />
ti<strong>on</strong> H <str<strong>on</strong>g>of</str<strong>on</strong>g> the MDS assesses bladder<br />
and bowel c<strong>on</strong>tinence <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
l<strong>on</strong>g-<strong>term</strong> care facility residents<br />
in the 14 days prior to the date <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
the assessment. C<strong>on</strong>tinence selfc<strong>on</strong>trol<br />
is assessed <strong>on</strong> a fivepoint<br />
scale ranging from complete<br />
c<strong>on</strong>trol (c<strong>on</strong>tinent) to inadequate<br />
c<strong>on</strong>trol (inc<strong>on</strong>tinent).<br />
Questi<strong>on</strong>s also assess <strong>use</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> c<strong>on</strong>tinent<br />
appliances and programs<br />
(e.g. toileting plan, pads, or<br />
<strong>catheter</strong>s) and whether c<strong>on</strong>tinence<br />
c<strong>on</strong>trol is achieved with<br />
the assistance <str<strong>on</strong>g>of</str<strong>on</strong>g> appliances.<br />
The primary independent<br />
variable <str<strong>on</strong>g>of</str<strong>on</strong>g> interest was BMI,<br />
which was calculated using the<br />
standard formula <str<strong>on</strong>g>of</str<strong>on</strong>g> <str<strong>on</strong>g>weight</str<strong>on</strong>g> (in<br />
kilograms) divided by height (in<br />
meters) squared (Nati<strong>on</strong>al Heart,<br />
Lung & Blood Institute [NHLBI]<br />
Mean (SD)<br />
at Admissi<strong>on</strong><br />
GEE Model Results<br />
OR<br />
(95% CI) p-Value<br />
Age, years 84.1 (8.4) 0.985<br />
(0.96, 1.01)<br />
Categorical Variables<br />
% (n)<br />
0.27<br />
OR<br />
(95% CI) p-Value<br />
Under<str<strong>on</strong>g>weight</str<strong>on</strong>g> (BMI < 18.5) 9.0 (346) 1.00 0.99<br />
(0.50, 2.00)<br />
Normal <str<strong>on</strong>g>weight</str<strong>on</strong>g> (BMI = 18.5 to 24.9) 43.5 (1673) Referent –<br />
Over<str<strong>on</strong>g>weight</str<strong>on</strong>g> (BMI = 25 to 29.9) 27.8 (1067) 0.982<br />
(0.67, 1.43)<br />
Obesity (30 to 34.9) 11.89 (456) 0.770<br />
(0.42, 1.41)<br />
Severe obesity (≥ 35) 7.9 (302) 1.686<br />
(0.91, 3.12)<br />
Time (quarter intervals) – 0.998<br />
(1.00, 1.00)<br />
Female 66.9 (2593) 0.673<br />
(0.43, 1.06)<br />
African American 10.2 (393) 1.586<br />
(0.94, 1.67)<br />
0.93<br />
0.40<br />
0.10<br />
0.04<br />
0.09<br />
0.08<br />
Notes: BMI = body mass index, CI = c<strong>on</strong>fidence interval, n = number, OR = odds<br />
ratio, SD = standard deviati<strong>on</strong>; ORs generated using generalized estimating equati<strong>on</strong><br />
(GEE) model.<br />
Obesity Educati<strong>on</strong> Initiative<br />
Expert Panel, 1998), and resident<br />
height and <str<strong>on</strong>g>weight</str<strong>on</strong>g> as recorded <strong>on</strong><br />
the MDS admissi<strong>on</strong> assessment.<br />
BMI was categorized into five<br />
levels (see Table 2), with normal<br />
<str<strong>on</strong>g>weight</str<strong>on</strong>g> serving as the reference<br />
category in multivariate analyses.<br />
Age, gender, race/ethnicity, and<br />
assessment time were included<br />
as additi<strong>on</strong>al covariates. Other<br />
clinical characteristics (e.g. ADL<br />
score, cognitive status) obtained<br />
from the MDS and facility characteristics<br />
(e.g. number <str<strong>on</strong>g>of</str<strong>on</strong>g> beds,<br />
staff) obtained from the Nursing<br />
Home Compare database, as well<br />
as a race-<str<strong>on</strong>g>weight</str<strong>on</strong>g> status interacti<strong>on</strong><br />
<strong>term</strong>, were included in initial<br />
models but were not retained<br />
in the final model for parsim<strong>on</strong>y<br />
sake beca<strong>use</strong> they were not significant<br />
and did not c<strong>on</strong>tribute to<br />
the model.<br />
UROLOGIC NURSING / July-August / Volume 33 Number 4 / Epub Ahead <str<strong>on</strong>g>of</str<strong>on</strong>g> Print 3
Analytic Methods<br />
Descriptive statistics were<br />
<strong>use</strong>d to characterize l<strong>on</strong>g-<strong>term</strong><br />
care facility residents in the analytic<br />
file. Two-sample t-tests and<br />
Chi-square tests were <strong>use</strong>d to<br />
assess the equality <str<strong>on</strong>g>of</str<strong>on</strong>g> demographic<br />
characteristics <str<strong>on</strong>g>of</str<strong>on</strong>g> l<strong>on</strong>g<strong>term</strong><br />
care facility residents based<br />
<strong>on</strong> BMI category. To account for<br />
repeated measures <strong>on</strong> residents<br />
and the clustering <str<strong>on</strong>g>of</str<strong>on</strong>g> residents<br />
within l<strong>on</strong>g-<strong>term</strong> care facilities, a<br />
generalized estimating equati<strong>on</strong><br />
(GEE) model was <strong>use</strong>d to examine<br />
the effect <str<strong>on</strong>g>of</str<strong>on</strong>g> obesity <strong>on</strong> the<br />
<strong>indwelling</strong> urinary <strong>catheter</strong> indicator<br />
over time.<br />
The University <str<strong>on</strong>g>of</str<strong>on</strong>g> Arkansas<br />
for Medical Sciences Institu ti<strong>on</strong> -<br />
al Review Board approved the<br />
study under expedited procedures.<br />
Results<br />
Table 2 lists characteristics <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
the 3,879 Arkansas l<strong>on</strong>g-<strong>term</strong><br />
care facility residents included in<br />
the analysis. These residents<br />
were mostly female (66.9%) and<br />
were <strong>on</strong> average 84.1 years <str<strong>on</strong>g>of</str<strong>on</strong>g> age<br />
(8.4 SD). The average BMI was<br />
25.8 (6.5 SD), with 19.5% <str<strong>on</strong>g>of</str<strong>on</strong>g> residents<br />
at admissi<strong>on</strong> being classified<br />
as obese (BMI ≥ 30). At<br />
admissi<strong>on</strong>, 24.2% <str<strong>on</strong>g>of</str<strong>on</strong>g> African<br />
Americans were obese, compared<br />
to 19.2% <str<strong>on</strong>g>of</str<strong>on</strong>g> Caucasians (p<br />
= 0.02), and 22.7% <str<strong>on</strong>g>of</str<strong>on</strong>g> females<br />
were obese compared to 15.7%<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> males (p < 0.0001). Table 3<br />
shows the percentage <str<strong>on</strong>g>of</str<strong>on</strong>g> all residents<br />
with <strong>indwelling</strong> urinary<br />
<strong>catheter</strong>s at admissi<strong>on</strong> and at<br />
quarter points over the observati<strong>on</strong><br />
year, as well as by residents<br />
by obesity status. At admissi<strong>on</strong>,<br />
the prevalence rate <str<strong>on</strong>g>of</str<strong>on</strong>g> <strong>indwelling</strong><br />
urinary <strong>catheter</strong>s am<strong>on</strong>g all residents<br />
was 16.8%, which de -<br />
clined to 4.1% by the fourth<br />
quarter. Obese residents had a<br />
significantly higher prevalence<br />
rate <str<strong>on</strong>g>of</str<strong>on</strong>g> <strong>indwelling</strong> urinary cath -<br />
eters than n<strong>on</strong>-obese residents at<br />
admissi<strong>on</strong> (19. 4% vs. 16.2%, p =<br />
0.034) and a borderline significantly<br />
higher prevalence rate (p =<br />
0.09, suggesting a trend toward<br />
statistical significance) at the sec<strong>on</strong>d<br />
quarter than n<strong>on</strong>-obese resi-<br />
Table 3.<br />
Percent <str<strong>on</strong>g>of</str<strong>on</strong>g> Older L<strong>on</strong>g-Term Care Facility Residents in Arkansas<br />
with Indwelling Urinary Catheters over Four Quarters (2008) by<br />
Obesity Status, and by Race and Gender<br />
All (%) O (%) NO (%) p-Value<br />
All Residents<br />
Admissi<strong>on</strong> (Quarter 1) 16.8 19.4 16.2 0.03<br />
Quarter 2 5.1 7.3 4.6 0.09<br />
Quarter 3 4.6 5.3 4.4 0.55<br />
Quarter 4 4.1 4.7 3.9 0.64<br />
Caucasian Residents<br />
Admissi<strong>on</strong> (Quarter 1) 16.7 19.7 16.0 0.02<br />
Quarter 2 4.8 6.7 4.3 0.15<br />
Quarter 3 4.0 4.1 4.0 0.94<br />
Quarter 4 4.0 5.4 3.6 0.28<br />
African-American Residents<br />
Admissi<strong>on</strong> (Quarter 1) 17.9 18.3 17.8 0.92<br />
Quarter 2 7.3 8.6 7.0 0.75<br />
Quarter 3 8.1 9.7 7.6 0.71<br />
Quarter 4 5.2 0.0 7.0 0.16<br />
Female Residents<br />
Admissi<strong>on</strong> (Quarter 1) 16.9 19.2 16.2 0.09<br />
Quarter 2 4.5 7.6 3.7 0.02<br />
Quarter 3 4.2 4.7 4.0 0.69<br />
Quarter 4 3.3 4.1 3.1 0.55<br />
Male Residents<br />
Admissi<strong>on</strong> (Quarter 1) 16.7 19.9 16.1 0.19<br />
Quarter 2 6.6 6.4 6.6 0.94<br />
Quarter 3 5.6 7.1 5.3 0.58<br />
Quarter 4 6.0 6.3 5.9 0.93<br />
Notes: O = obese, NO = n<strong>on</strong>-obese; p values generated using Chi-square.<br />
dents (7.3% vs. 4.6%). However,<br />
rates were not statistically different<br />
at quarters three and four.<br />
Results <str<strong>on</strong>g>of</str<strong>on</strong>g> the GEE model (see<br />
Table 2) indicate that residents<br />
with severe obesity had an<br />
increased odds (odds ratio [OR] =<br />
1.69) <str<strong>on</strong>g>of</str<strong>on</strong>g> having an <strong>indwelling</strong> urinary<br />
<strong>catheter</strong>; however, the odds<br />
were not statistically significant.<br />
The <strong>on</strong>ly variable for which a significant<br />
associati<strong>on</strong> was detected<br />
was time; as time (by quarter <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
the year) progressed, the likelihood<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> an <strong>indwelling</strong> urinary<br />
<strong>catheter</strong> was significantly lower<br />
(p = 0.04). In additi<strong>on</strong> to severe<br />
obesity (BMI > 35), two other<br />
variables trended toward a statistically<br />
significant associati<strong>on</strong><br />
with <strong>indwelling</strong> urinary <strong>catheter</strong><br />
<strong>use</strong>: gender and race. There was a<br />
trend toward females being less<br />
likely (OR = 0.67, p = 0.09) to<br />
have an <strong>indwelling</strong> urinary cath -<br />
eter than males. There was also a<br />
trend toward African Americans<br />
being more likely (OR = 1.6, p =<br />
0.08) to have an <strong>indwelling</strong> urinary<br />
<strong>catheter</strong> than Caucasians.<br />
Discussi<strong>on</strong><br />
The <strong>use</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> <strong>indwelling</strong> urinary<br />
<strong>catheter</strong>s am<strong>on</strong>g older residents<br />
in federally certified l<strong>on</strong>g-<strong>term</strong><br />
4 UROLOGIC NURSING / July-August / Volume 33 Number 4 / Epub Ahead <str<strong>on</strong>g>of</str<strong>on</strong>g> Print
care facilities in Arkansas in<br />
2008 at admissi<strong>on</strong> was 16.8%<br />
am<strong>on</strong>g all new residents, and<br />
was significantly higher am<strong>on</strong>g<br />
newly admitted obese, older<br />
l<strong>on</strong>g-<strong>term</strong> care facility residents<br />
(19.4%). These rates were c<strong>on</strong>siderably<br />
higher than the nati<strong>on</strong>al<br />
quality benchmark for in -<br />
dwelling urinary <strong>catheter</strong> (Rantz<br />
et al., 2000). However, over <strong>on</strong>e<br />
year, the <strong>use</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> <strong>indwelling</strong> urinary<br />
<strong>catheter</strong>s am<strong>on</strong>g older l<strong>on</strong>g<strong>term</strong><br />
care facility residents, both<br />
obese and n<strong>on</strong>-obese, decreased<br />
substantially, with no statistical<br />
difference persisting am<strong>on</strong>g residents<br />
based <strong>on</strong> obesity status.<br />
Federal guidelines call for minimal<br />
<strong>use</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> <strong>indwelling</strong> urinary<br />
<strong>catheter</strong>s with l<strong>on</strong>g-<strong>term</strong> care<br />
facility residents. High in dwell -<br />
ing urinary <strong>catheter</strong> rates at ad -<br />
missi<strong>on</strong>, with sharp declines in<br />
the following three m<strong>on</strong>ths, suggest<br />
nursing staff, in collaborati<strong>on</strong><br />
with other health care pro -<br />
viders and the l<strong>on</strong>g-<strong>term</strong> care<br />
facility resident, are able to either<br />
achieve c<strong>on</strong>tinence or implement<br />
strategies (other than <strong>use</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> an<br />
<strong>indwelling</strong> urinary <strong>catheter</strong>) to<br />
successfully manage the resident’s<br />
UI.<br />
Indwelling urinary <strong>catheter</strong><br />
<strong>use</strong> can increase risk for infecti<strong>on</strong>s,<br />
other medical complicati<strong>on</strong>s<br />
(Igawa et al., 2008), and<br />
even death (Landi et al., 2004),<br />
and are therefore not recommended<br />
for the l<strong>on</strong>g-<strong>term</strong>. Find -<br />
ings from the study reported here<br />
are c<strong>on</strong>gruent with nati<strong>on</strong>al<br />
guidelines and best-practice<br />
models that require l<strong>on</strong>g-<strong>term</strong><br />
care facility staff to carefully<br />
assess the resident’s need for an<br />
<strong>indwelling</strong> urinary <strong>catheter</strong>,<br />
develop individualized plans <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
care for <strong>catheter</strong> removal, and<br />
manage UI with a variety <str<strong>on</strong>g>of</str<strong>on</strong>g> evidence-based<br />
interventi<strong>on</strong>s that<br />
do not include a l<strong>on</strong>g-<strong>term</strong> in -<br />
dwelling urinary <strong>catheter</strong> (e.g.,<br />
scheduled or prompted voiding,<br />
judicious medicati<strong>on</strong> <strong>use</strong> for<br />
overactive bladder or urgency UI,<br />
behavioral strategies) (CDC/<br />
Nati<strong>on</strong>al Healthcare Safety Net -<br />
work, 2009; CMS, 2005; Newman<br />
& Wein, 2009), as indicated by<br />
the sharp decrease in <strong>indwelling</strong><br />
urinary <strong>catheter</strong> <strong>use</strong> found from<br />
admissi<strong>on</strong> to quarter four. These<br />
findings indicate that quality<br />
improvement efforts – c<strong>on</strong>sistent<br />
c<strong>on</strong>tinence care m<strong>on</strong>itoring and<br />
treatment by nursing staff – can<br />
improve l<strong>on</strong>g-<strong>term</strong> care and resident<br />
outcomes. Counter to our<br />
hypothesis and previous re -<br />
search (Rogers et al., 2008), we<br />
did not detect a high likelihood<br />
for the <strong>use</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> <strong>indwelling</strong> urinary<br />
<strong>catheter</strong>s am<strong>on</strong>g severely obese,<br />
older l<strong>on</strong>g-<strong>term</strong> care facility residents<br />
compared to those <str<strong>on</strong>g>of</str<strong>on</strong>g> normal<br />
<str<strong>on</strong>g>weight</str<strong>on</strong>g>, except at admissi<strong>on</strong>.<br />
Our study did not identify the<br />
locati<strong>on</strong> from which new residents<br />
were admitted (e.g. hospital<br />
or home). Admissi<strong>on</strong> from<br />
<strong>on</strong>e locati<strong>on</strong> versus another may<br />
explain differences in <strong>indwelling</strong><br />
urinary <strong>catheter</strong> rates at admissi<strong>on</strong><br />
and warrants further investigati<strong>on</strong>.<br />
Despite negative c<strong>on</strong>sequences<br />
and nati<strong>on</strong>al guidelines, little<br />
evidence exists regarding the<br />
c<strong>on</strong>sequences or any potential<br />
benefits <str<strong>on</strong>g>of</str<strong>on</strong>g> <strong>indwelling</strong> urinary<br />
<strong>catheter</strong> <strong>use</strong> in an obese l<strong>on</strong>g<strong>term</strong><br />
care facility populati<strong>on</strong>.<br />
Bradway et al. (2010) ob served<br />
that some obese l<strong>on</strong>g-<strong>term</strong> care<br />
facility residents and their caregivers<br />
may prefer <strong>indwelling</strong> urinary<br />
<strong>catheter</strong>s over other in -<br />
c<strong>on</strong>tinence c<strong>on</strong>trol strategies to<br />
minimize the day-to-day bathing<br />
and skin care challenges associated<br />
with using absorbent pads<br />
and reduce barriers to engaging<br />
with others residents. This observati<strong>on</strong><br />
may account for the higher<br />
odds (albeit not significantly<br />
different) for <strong>indwelling</strong> urinary<br />
<strong>catheter</strong> usage am<strong>on</strong>g obese l<strong>on</strong>g<strong>term</strong><br />
care facility residents found<br />
in the current study. However,<br />
the current study did not examine<br />
individual patient or caregiver<br />
preferences for UI management.<br />
Future research should<br />
examine this issue further with<br />
obese l<strong>on</strong>g-<strong>term</strong> care facility residents<br />
taking into account this<br />
limitati<strong>on</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> the current study by<br />
assessing <strong>indwelling</strong> urinary<br />
cath eter usage rates, positive and<br />
negative outcomes <str<strong>on</strong>g>of</str<strong>on</strong>g> <strong>catheter</strong>izati<strong>on</strong>,<br />
and patient and caregiver<br />
preferences in choosing UI management<br />
strategies. Further, fu -<br />
ture research should also support<br />
development and testing <str<strong>on</strong>g>of</str<strong>on</strong>g> protocols<br />
for c<strong>on</strong>tinence care and<br />
best practices associated with<br />
<strong>indwelling</strong> urinary <strong>catheter</strong> <strong>use</strong><br />
in obese l<strong>on</strong>g-<strong>term</strong> care facility<br />
residents.<br />
Finally, male l<strong>on</strong>g-<strong>term</strong> care<br />
facility residents were more likely<br />
than female l<strong>on</strong>g-<strong>term</strong> care<br />
facility residents to have an<br />
<strong>indwelling</strong> urinary <strong>catheter</strong>, and<br />
African-American l<strong>on</strong>g-<strong>term</strong> care<br />
facility residents were more likely<br />
than Caucasian l<strong>on</strong>g-<strong>term</strong> care<br />
facility residents to have an<br />
<strong>indwelling</strong> urinary <strong>catheter</strong>. The<br />
increased likelihoods were not<br />
statistically significant but could<br />
have implicati<strong>on</strong>s for future<br />
research. Older men are at high<br />
risk for urinary retenti<strong>on</strong> due to<br />
prostate disease (Meigs et al.,<br />
1999), which could explain the<br />
higher <strong>use</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> <strong>indwelling</strong> urinary<br />
<strong>catheter</strong>s am<strong>on</strong>g this group.<br />
However, in numerous studies <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
both community-dwelling and<br />
l<strong>on</strong>g-<strong>term</strong> care facility older<br />
adults, women are disproporti<strong>on</strong>ately<br />
affected by UI (Aslan,<br />
Beji, Erkan, Yalcin, & Gungor,<br />
2009; Boyingt<strong>on</strong> et al., 2007;<br />
Goode et al., 2008; Landefeld et<br />
al., 2008; Moore & Gray, 2004).<br />
How or if this relates to gender<br />
differences in <strong>indwelling</strong> urinary<br />
<strong>catheter</strong> <strong>use</strong> in l<strong>on</strong>g-<strong>term</strong> care<br />
facility residents requires further<br />
explorati<strong>on</strong>. In additi<strong>on</strong>, relatively<br />
little is known about racial differences<br />
in UI, particularly in the<br />
l<strong>on</strong>g-<strong>term</strong> care facility setting. In<br />
<strong>on</strong>e study (Boyingt<strong>on</strong> et al.,<br />
2007), African-American l<strong>on</strong>g<strong>term</strong><br />
care facility residents were<br />
more likely to have UI than their<br />
Caucasian counterparts (OR =<br />
1.07, 95% CI: 1.01-1.14) with a<br />
significantly higher prevalence<br />
in specific regi<strong>on</strong>s <str<strong>on</strong>g>of</str<strong>on</strong>g> the United<br />
States; <strong>indwelling</strong> urinary cath -<br />
eter <strong>use</strong> was not described in that<br />
study. To our knowledge, racial<br />
differences in UI and <strong>indwelling</strong><br />
urinary <strong>catheter</strong> <strong>use</strong> between<br />
obese and n<strong>on</strong>-obese l<strong>on</strong>g-<strong>term</strong><br />
care facility residents have not<br />
been described. This is str<strong>on</strong>gly<br />
recommended as an area for<br />
future research.<br />
UROLOGIC NURSING / July-August / Volume 33 Number 4 / Epub Ahead <str<strong>on</strong>g>of</str<strong>on</strong>g> Print 5
Limitati<strong>on</strong>s<br />
There are several limitati<strong>on</strong>s<br />
to this work that should be noted.<br />
First, this study was unable to<br />
identify why a <strong>catheter</strong> was in<br />
place and for how l<strong>on</strong>g it had<br />
been in place at the time <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
admissi<strong>on</strong>. It is possible that the<br />
<strong>catheter</strong> was in place for a medical<br />
reas<strong>on</strong>, such as to prevent<br />
urine c<strong>on</strong>taminati<strong>on</strong> while treating<br />
a n<strong>on</strong>-healing wound. Being<br />
able to differentiate the reas<strong>on</strong>(s)<br />
for <strong>catheter</strong>izati<strong>on</strong> in the analysis<br />
would have been helpful in identifying<br />
the characteristics <str<strong>on</strong>g>of</str<strong>on</strong>g> residents<br />
who were inappropriately<br />
<strong>catheter</strong>ized and de<strong>term</strong>ining the<br />
durati<strong>on</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> <strong>indwelling</strong> urinary<br />
<strong>catheter</strong> <strong>use</strong> in our study subjects.<br />
Finer detail <strong>on</strong> factors associated<br />
with <strong>indwelling</strong> urinary<br />
<strong>catheter</strong>s, such as durati<strong>on</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> <strong>use</strong>,<br />
would add important informati<strong>on</strong><br />
<strong>use</strong>ful to caregivers in volved in<br />
developing interventi<strong>on</strong>s for<br />
<strong>catheter</strong> removal and targeting<br />
other residents at highest risk for<br />
<strong>indwelling</strong> urinary <strong>catheter</strong>s.<br />
Sec<strong>on</strong>d, this study was limited<br />
to data from l<strong>on</strong>g-<strong>term</strong> care<br />
facilities in <strong>on</strong>e state and from<br />
<strong>on</strong>e year. Additi<strong>on</strong>al data from<br />
more states and from multiple<br />
years would allow trends in<br />
<strong>catheter</strong>izati<strong>on</strong> to be m<strong>on</strong>itored.<br />
C<strong>on</strong>clusi<strong>on</strong>/Recommendati<strong>on</strong>s<br />
This study examined the<br />
associati<strong>on</strong> between <strong>indwelling</strong><br />
urinary <strong>catheter</strong> usage and obesity<br />
am<strong>on</strong>g l<strong>on</strong>g-<strong>term</strong> care facility<br />
residents. The results <str<strong>on</strong>g>of</str<strong>on</strong>g> this<br />
study de<strong>term</strong>ined that there are<br />
higher rates <str<strong>on</strong>g>of</str<strong>on</strong>g> <strong>indwelling</strong> urinary<br />
<strong>catheter</strong> usage at admissi<strong>on</strong><br />
overall and significantly higher<br />
rates <str<strong>on</strong>g>of</str<strong>on</strong>g> <strong>indwelling</strong> urinary cath -<br />
eter usage if obesity is present at<br />
the time <str<strong>on</strong>g>of</str<strong>on</strong>g> admissi<strong>on</strong> to a l<strong>on</strong>g<strong>term</strong><br />
care facility. However, in -<br />
dwelling urinary <strong>catheter</strong> usage<br />
rates declined within 12 m<strong>on</strong>ths<br />
after admissi<strong>on</strong>, and statistical<br />
differences associated with obesity<br />
disappeared. These results<br />
suggest that l<strong>on</strong>g-<strong>term</strong> care facility<br />
staff are able to assist residents<br />
to achieve c<strong>on</strong>tinence or employ<br />
alternate strategies to address<br />
persistent inc<strong>on</strong>tinence.<br />
Despite these positive findings,<br />
additi<strong>on</strong>al research for this<br />
study populati<strong>on</strong> should be performed.<br />
Obesity has been correlated<br />
to other health c<strong>on</strong>diti<strong>on</strong>s,<br />
and the effect obesity has with or<br />
without other co-morbidities <strong>on</strong><br />
inc<strong>on</strong>tinence is unknown. The<br />
type <str<strong>on</strong>g>of</str<strong>on</strong>g> admissi<strong>on</strong> to the l<strong>on</strong>g<strong>term</strong><br />
care facility may have an<br />
impact <strong>on</strong> the presence <str<strong>on</strong>g>of</str<strong>on</strong>g> an<br />
<strong>indwelling</strong> urinary <strong>catheter</strong>; data<br />
from residents admitted from<br />
acute care facilities may have a<br />
higher prevalence <str<strong>on</strong>g>of</str<strong>on</strong>g> <strong>indwelling</strong><br />
urinary <strong>catheter</strong> than those<br />
admitted from home. The interventi<strong>on</strong>(s)<br />
employed by the staff<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> the l<strong>on</strong>g-<strong>term</strong> care facility<br />
should be evaluated, as this will<br />
de<strong>term</strong>ine which interventi<strong>on</strong> is<br />
most successful. Comparis<strong>on</strong><br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> any interventi<strong>on</strong> to the standard<br />
practice will identify the<br />
strength, cost savings, and timing<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> the interventi<strong>on</strong>. While the<br />
most appropriate evidence-based<br />
care has yet to be de<strong>term</strong>ined,<br />
results <str<strong>on</strong>g>of</str<strong>on</strong>g> this study indicate that<br />
the <strong>use</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> <strong>indwelling</strong> urinary<br />
<strong>catheter</strong>s am<strong>on</strong>g l<strong>on</strong>g-<strong>term</strong> care<br />
facility residents can be de -<br />
creased.<br />
References<br />
Abt Associates, Inc. (2004). Nati<strong>on</strong>al<br />
nursing home quality measures<br />
<strong>use</strong>r’s manual. Cambridge, MA:<br />
Author.<br />
Aslan, E., Beji, N.K., Erkan, H.A., Yalcin,<br />
O., & Gungor, F. (2009). The prevalence<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> and the related factors for<br />
urinary and fecal inc<strong>on</strong>tinence<br />
am<strong>on</strong>g older residing in nursing<br />
homes. Journal <str<strong>on</strong>g>of</str<strong>on</strong>g> Clinical Nursing,<br />
18, 3290-3298.<br />
Boyingt<strong>on</strong>, J., Howard, D., Carter-<br />
Edwards, L., Gooden, K., Erdem, N.,<br />
Jallah, Y., … Busby-Whitehead, J.<br />
(2007). Differences in resident characteristics<br />
and prevalence <str<strong>on</strong>g>of</str<strong>on</strong>g> urinary<br />
inc<strong>on</strong>tinence in nursing homes in<br />
the southeastern United States.<br />
Nursing Research, 56(2), 97-107.<br />
Bradway, C., Miller, E., Heivly, A., &<br />
Fleshner, I. (2010). C<strong>on</strong>tinence care<br />
for obese nursing home residents.<br />
Urologic Nursing, 30(2), 121-129.<br />
Capitman, J., Leutz, W., Bishop, C., &<br />
Casler, R. (2005). L<strong>on</strong>g-<strong>term</strong> care<br />
quality: Historical overview and current<br />
initiatives. Waltham, MA:<br />
Schneider Institute for Health<br />
Policy, Heller School for Social<br />
Policy and Management, Brandeis<br />
University.<br />
Centers for Disease C<strong>on</strong>trol and Pre ven ti<strong>on</strong><br />
(CDC)/Nati<strong>on</strong>al Healthcare Safety<br />
Network. (2009). Catheter-associated<br />
urinary tract infecti<strong>on</strong>s (CAUTI)<br />
event. Atlanta: CDC.<br />
Centers for Medicare & Medicaid Services<br />
(CMS). (2005). CMS manual system:<br />
Pub 100-07 state operati<strong>on</strong>s provider<br />
certificati<strong>on</strong>. Washingt<strong>on</strong>, DC: U.S.<br />
Department <str<strong>on</strong>g>of</str<strong>on</strong>g> Health and Human<br />
Services.<br />
Centers for Medicare & Medicaid Services<br />
(CMS). (2011). Nursing home compare.<br />
Retrieved from http:// www.<br />
medicare. gov/ NH Compare/ Include/<br />
Data Secti<strong>on</strong>/ Questi<strong>on</strong>s/ Search<br />
Criteria NEW. asp ? versi<strong>on</strong> = default &<br />
browser = IE % 7 C 8 % 7 C Win XP & lan<br />
guage = English & default status = 0 &<br />
page list = Home & Cookies Enabled<br />
Status = True<br />
Doughty, D., & Kisanga, J. (2010).<br />
Regulatory guidelines for bladder<br />
management in l<strong>on</strong>g-<strong>term</strong> care.<br />
Journal <str<strong>on</strong>g>of</str<strong>on</strong>g> Wound, Ostomy C<strong>on</strong>ti -<br />
nence Nursing, 37, 399-411.<br />
Elkins, J., Whitmer, R., Sidney, S., Sorel,<br />
M., Yaffe, K., & Johnst<strong>on</strong>, S. (2006).<br />
Midlife obesity and l<strong>on</strong>g-<strong>term</strong> risk <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
nursing home admissi<strong>on</strong>. Obesity,<br />
14(8), 1472-1478.<br />
Felix, H. (2008). Pers<strong>on</strong>al care assistance<br />
needs <str<strong>on</strong>g>of</str<strong>on</strong>g> obese elders entering nursing<br />
homes. Journal <str<strong>on</strong>g>of</str<strong>on</strong>g> the American<br />
Medical Directors Associati<strong>on</strong>, 9(5),<br />
319-326.<br />
Flegal, K., Carroll, M., Ogden, C., &<br />
Curtin, L. (2010). Prevalence and<br />
trends in obesity am<strong>on</strong>g U.S. adults,<br />
1999-2008. Journal <str<strong>on</strong>g>of</str<strong>on</strong>g> the American<br />
Medical Associati<strong>on</strong>, 303, 235-241.<br />
Goode, P.S., Burgio, K.L., Redden, D.T.,<br />
Markland, A., Richter, H.E., Sawyer,<br />
P., … Allman, R.M. (2008). Pop u la -<br />
ti<strong>on</strong> based study <str<strong>on</strong>g>of</str<strong>on</strong>g> incidence and<br />
predictors <str<strong>on</strong>g>of</str<strong>on</strong>g> urinary inc<strong>on</strong>tinence<br />
in black and white older adults. The<br />
Journal <str<strong>on</strong>g>of</str<strong>on</strong>g> Urology, 179, 1449-1454.<br />
Hunskaar, S. (2008). A systematic review<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> over<str<strong>on</strong>g>weight</str<strong>on</strong>g> and obesity as risk factors<br />
and targets for clinical interventi<strong>on</strong><br />
for urinary inc<strong>on</strong>tinence in<br />
women. Neurourology and Uro dy -<br />
nam ics, 27(8), 749-757.<br />
Igawa, Y., Wyndaele, J.J., & Nishizawa, O.<br />
(2008). Catheterizati<strong>on</strong>: Possible<br />
complicati<strong>on</strong>s and their preventi<strong>on</strong><br />
and treatment. Internati<strong>on</strong>al Journal<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> Urology, 15, 481-485.<br />
Landefeld, C., Bowers, B., Feld, A.,<br />
Hartmann, K., H<str<strong>on</strong>g>of</str<strong>on</strong>g>fman, E., Ingber,<br />
M., … Trock, B.J. (2008). Nati<strong>on</strong>al<br />
Institutes <str<strong>on</strong>g>of</str<strong>on</strong>g> Health state <str<strong>on</strong>g>of</str<strong>on</strong>g> the science<br />
c<strong>on</strong>ference statement: Pre ven -<br />
ti<strong>on</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> fecal and urinary inc<strong>on</strong>tinence<br />
in adults. Annals <str<strong>on</strong>g>of</str<strong>on</strong>g> Internal<br />
Medicine, 148, 449-458.<br />
Landi, F., Cesari, M., Onder, G., Zamb<strong>on</strong>i,<br />
V., Barillaro, C., Lattanzio, F., &<br />
Bernabel, R. (2004). Indwelling urethral<br />
<strong>catheter</strong> and mortality in frail<br />
elderly women living in community.<br />
Neurourology and Urodynamics,<br />
23(7), 697-701.<br />
Meigs, J.B., Barry, M.J., Giovannucci, E.,<br />
Rimm, E.B., Stampfer, M.J., &<br />
Kawachi, I. (1999). Incidence rates<br />
and risk factors for acute urinary<br />
retenti<strong>on</strong>: The Health Pr<str<strong>on</strong>g>of</str<strong>on</strong>g>essi<strong>on</strong>als<br />
6 UROLOGIC NURSING / July-August / Volume 33 Number 4 / Epub Ahead <str<strong>on</strong>g>of</str<strong>on</strong>g> Print
Follow-Up Study. Journal <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
Urology, 162, 376-382.<br />
Moore, K.N., & Gray, M. (2004). Urinary<br />
inc<strong>on</strong>tinence in men: Current status<br />
and future directi<strong>on</strong>s. Nursing Re -<br />
search, 53(Suppl.), S36-S41.<br />
Newman, D.K., & Wein, A.J. (2009).<br />
Managing and treating urinary in -<br />
c<strong>on</strong>tinence (2nd ed.). Baltimore:<br />
Health Pr<str<strong>on</strong>g>of</str<strong>on</strong>g>essi<strong>on</strong>s Press.<br />
Nati<strong>on</strong>al Heart, Lung and Blood Institute<br />
(NHLBI) Obesity Educati<strong>on</strong> Initia -<br />
tive Expert Panel. (1998). Clinical<br />
guidelines <strong>on</strong> the identificati<strong>on</strong>,<br />
evaluati<strong>on</strong> and treatment <str<strong>on</strong>g>of</str<strong>on</strong>g> over<str<strong>on</strong>g>weight</str<strong>on</strong>g><br />
and obesity in adults: The<br />
evidence report. Washingt<strong>on</strong> DC:<br />
Nati<strong>on</strong>al Institutes <str<strong>on</strong>g>of</str<strong>on</strong>g> Health.<br />
Rantz, M., Petroski, G., Madsen, R., Mehr,<br />
D., Popejoy, L., Hicks, L., … Grando,<br />
V. (2000). Setting thresholds for<br />
quality indicators derived from MDS<br />
data for nursing home quality<br />
improvement reports: An update.<br />
Journal <str<strong>on</strong>g>of</str<strong>on</strong>g> Quality Improvement,<br />
20(2), 101-110.<br />
Rogers, M., Mody, L., Kaufman, S., Fries,<br />
B., McMah<strong>on</strong>, L., & Saint, S. (2008).<br />
Use <str<strong>on</strong>g>of</str<strong>on</strong>g> urinary collecti<strong>on</strong> devices in<br />
skilled nursing facilities in five<br />
states. Journal <str<strong>on</strong>g>of</str<strong>on</strong>g> the American<br />
Geriatrics Society, 56, 854-861.<br />
Valiyeva, E., Russell, L., Miller, J., &<br />
Safford, M. (2006). Lifestyle-related<br />
risk factors and risk <str<strong>on</strong>g>of</str<strong>on</strong>g> future nursing<br />
home admissi<strong>on</strong>. Archives <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
Internal Medicine, 166, 985-990.<br />
Wunderlich, G., & Kohler, P. (2001).<br />
Improving the quality <str<strong>on</strong>g>of</str<strong>on</strong>g> l<strong>on</strong>g-<strong>term</strong><br />
care. Washingt<strong>on</strong>, DC: NAP.<br />
UROLOGIC NURSING / July-August / Volume 33 Number 4 / Epub Ahead <str<strong>on</strong>g>of</str<strong>on</strong>g> Print 7