TRICARE Overseas Program Provider Manual
TRICARE Overseas Program Provider Manual
TRICARE Overseas Program Provider Manual
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
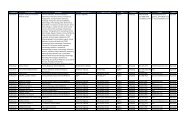
To confirm a <strong>TRICARE</strong> beneficiary’s eligibility, <strong>Provider</strong>s should<br />
ask to see both of the following:<br />
■ TOP Prime Enrollment Card and<br />
■ U.S. Military ID or CAC<br />
It is important to verify that the name on both cards matches<br />
exactly, and that the photo on the U.S. Military ID Card or CAC<br />
accurately represents the patient.<br />
<strong>Provider</strong>s should also check:<br />
■ The expiration date on the U.S. Military ID Card or CAC<br />
(to ensure that coverage is still valid)<br />
■ The sponsor’s Social Security Number (this will always be<br />
in the same format: XXX-XX-XXXX) or the Department of<br />
Defense (DOD) Benefits Number (this can be found above the<br />
bar code on the back of the beneficiary’s ID card and will be<br />
in the following format: XXXXXXXXX-XX). Only the first 9 digits<br />
of the DOD Benefits Number will be needed for the <strong>Provider</strong> to<br />
verify eligibility.<br />
You can also call your International SOS TOP Regional Call<br />
Center for assistance, if you are unsure.<br />
Note: International SOS will only issue a <strong>TRICARE</strong> Authorization<br />
Form for TOP Standard beneficiaries for the following types of<br />
medical care, which do require prior authorization:<br />
■ Adjunctive Dental Services<br />
■ Home Health Services<br />
■ Hospice Care<br />
■ Non-emergency Inpatient Admissions for Substance Use<br />
Disorders or Behavioral Health Care<br />
■ Outpatient Behavioral Health Care Visits Beyond 8th Visit per<br />
Fiscal Year (10/1-9/30)<br />
■ Transplants (all solid organ and stem cell)<br />
The <strong>TRICARE</strong> Standard Authorization Form will be issued to the<br />
MTF and the TOP Standard beneficiary. The TOP Standard<br />
beneficiary may give this to the <strong>Provider</strong> when they seek medical<br />
care.<br />
TOP Standard coverage is available to the family members of<br />
Active Duty Service Members (ADSM) living and working<br />
overseas. TOP Standard enrolled beneficiaries manage their own<br />
health care and also have the freedom to choose any Host Nation<br />
<strong>Provider</strong> they wish to see.<br />
TOP Standard beneficiaries receive reimbursable health care,<br />
after meeting their annual deductible payment and cost-sharing<br />
obligations. This means that the beneficiary will pay the first<br />
portion of costs toward health care services received each year<br />
(the annual deductible). After this portion is paid, the beneficiary<br />
is responsible to pay a certain percentage of each medical bill<br />
they receive – TOP Standard beneficiaries who are Active Duty<br />
Family Members (ADFM) pay 20% of the total cost and Retirees<br />
29<br />
pay 25% of the total cost. Once the beneficiary has contributed<br />
over a determined limit (i.e., they reach their catastrophic cap),<br />
<strong>TRICARE</strong> will pay all medical costs for the remainder of the<br />
financial year.<br />
TOP Standard beneficiaries will not be issued a <strong>TRICARE</strong><br />
Enrollment Card. They will only have a Military ID Card. As a Host<br />
Nation <strong>Provider</strong> under TOP, your commitment is to provide<br />
cashless, claimless services to TOP Prime and TOP Prime<br />
Remote beneficiaries only. You are not obligated to provide<br />
similar services to TOP Standard beneficiaries.<br />
Depending on your location, you may experience a large number<br />
of TOP Standard beneficiaries living and working in your region.<br />
If you decide to provide services to these beneficiaries, you may<br />
do so in one of the following two ways:<br />
■ Request TOP Standard beneficiaries to pay the cost of<br />
treatment upfront. This means the TOP Standard beneficiary<br />
will be personally responsible for claiming reimbursement from<br />
<strong>TRICARE</strong>.<br />
■ File the claim on behalf of the TOP Standard beneficiary (using<br />
the CMS 1500 for Non-Institutional <strong>Provider</strong>s or UB-04 Claim<br />
Form for Institutional <strong>Provider</strong>s) and bill the patient directly for<br />
the patient responsibility amount.<br />
Note: <strong>Provider</strong>s should be prepared to collect required<br />
beneficiary cost shares at the time of service delivery. The<br />
most up-to-date beneficiary cost-share information can be<br />
found online at www.tricare.mil. <strong>Provider</strong>s registered to the<br />
<strong>Provider</strong> Portal can also check patient eligibility on<br />
www.tricare-overseas.com by entering the sponsor’s Social<br />
Security Number or DOD Benefits Number, and date of<br />
service. Additional information on understanding the <strong>Provider</strong><br />
Portal can be found in Section 6 of this TOP <strong>Provider</strong> <strong>Manual</strong>.<br />
Based on your location, you may see TOP Prime, TOP Prime<br />
Remote and TOP Standard beneficiaries. TOP Standard<br />
beneficiaries are required to pay upfront and submit their<br />
claims for reimbursement. As a <strong>TRICARE</strong> <strong>Overseas</strong> <strong>Provider</strong>,<br />
you are not required to file claims on behalf of TOP Standard<br />
beneficiaries. If you would like to offer this service, you are<br />
responsible for ensuring that any cost shares or deductibles<br />
are collected from the TOP Standard beneficiary by your<br />
facility.<br />
Note: When submitting claims on behalf of TOP Standard<br />
beneficiaries, <strong>Provider</strong>s must invoice for the full amount<br />
charged. If the <strong>Provider</strong> submits an invoice for only the<br />
balance (after the TOP Standard beneficiary has paid their<br />
deductible and cost share), International SOS will apply the<br />
deductible and cost share to the balance, as required by<br />
<strong>TRICARE</strong> policy. Therefore, International SOS will need the<br />
Itemized Invoice to reflect the full cost of medical care<br />
(i.e., the total invoiced amount).<br />
Please visit www.tricare-overseas.com for additional information<br />
about how to handle TOP Standard claims for reimbursement.<br />
SECTIoN 4<br />
Authorizations and Seeing<br />
<strong>TRICARE</strong> Patients