TRICARE Overseas Program Provider Manual
TRICARE Overseas Program Provider Manual
TRICARE Overseas Program Provider Manual
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Behavioral Health Care Services: Substance Use Disorder Services<br />
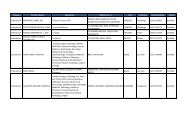
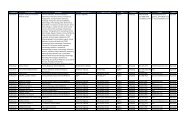
Figure 2.7 provides coverage details for covered substance use disorder services (up to three benefit periods per beneficiary, per lifetime).<br />
NoTE: This figure is not all-inclusive and additional limitations on substance use disorder services may apply overseas.<br />
Figure 2.7<br />
Service<br />
Inpatient Detoxification<br />
Description<br />
<strong>TRICARE</strong> covers emergency and inpatient hospital services for the treatment of the acute phases of<br />
substance use withdrawal (detoxification) when the patient’s condition requires the personnel and<br />
facilities of a hospital or substance use disorder rehabilitation facility (SUDRF).<br />
■ Limitations:<br />
— Diagnosis-related group-exempt facility, services are limited to seven days per episode.<br />
— Inpatient detoxification in a free-standing SUDRF counts toward the 30- or 45-day inpatient<br />
psychiatric care limit.<br />
SUDRF Rehabilitation<br />
Rehabilitation of a substance use disorder may occur in an inpatient (residential) or partial<br />
hospitalization setting. <strong>TRICARE</strong> covers 21 days of rehabilitation per benefit period in a <strong>TRICARE</strong>authorized<br />
facility, whether in an inpatient or partial hospitalization facility or a combination of both. 1<br />
■ Limitations:<br />
— 21-day rehabilitation limit per episode<br />
— Three episodes per lifetime<br />
— Days for inpatient rehabilitation count toward the 30- or 45-day limit for acute inpatient<br />
psychiatric care<br />
(Limitations may be waived if determined to be medically or psychologically necessary.)<br />
SUDRF outpatient Care Outpatient substance use care must be provided by an approved SUDRF.<br />
■ Limitations:<br />
— Individual or group therapy: Up to 60 visits per benefit period 1<br />
— Family therapy: Up to 15 visits per benefit period 1<br />
— Partial hospitalization program care: 21 treatment days per fiscal year 2<br />
(Limitations may be waived if determined to be medically or psychologically necessary.)<br />
1<br />
A benefit period begins with the first day of covered treatments and ends 365 days later. Stay limitations for inpatient services may be waived if determined<br />
to be medically or psychologically necessary.<br />
2<br />
October 1- September 30.<br />
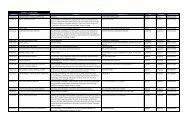
ToP Prime and ToP Prime Remote<br />
Beneficiary Coverage Limitations<br />
The following is a list of medical, surgical and behavioral health<br />
care services that may not be covered unless exceptional<br />
circumstances exist. This list is not intended to be all-inclusive.<br />
Please visit www.tricare.mil for a full list of covered services,<br />
limitations and exclusions.<br />
20