TRICARE Overseas Program Provider Manual
TRICARE Overseas Program Provider Manual
TRICARE Overseas Program Provider Manual
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
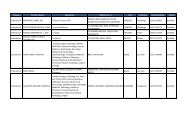
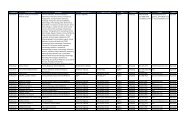
Behavioral Health Care Services: Inpatient Coverage Details<br />
Prior authorization is required for all nonemergency inpatient behavioral health care services. Psychiatric emergencies do not require<br />
prior authorization for inpatient admissions, but authorization is required for continued stay. Admissions resulting from psychiatric<br />
emergencies should be reported to the TOP contractor within 24 hours of admission or on the next business day, and must be reported<br />
within 72 hours of an admission. Authorization for continued stay is coordinated between the inpatient unit and the TOP contractor.<br />
Note: Active duty service members who receive care at military hospitals or clinics do not require prior authorization.<br />
Note: This figure is not all-inclusive and additional limitations on behavioral health care services may apply overseas.<br />
Figure 2.6<br />
SECTIoN 2<br />
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
Benefits<br />
Service<br />
Acute Inpatient Psychiatric Care<br />
Description<br />
May be covered on an emergency or nonemergency basis. Prior authorization from your regional<br />
contractor is required for all nonemergency inpatient admissions. In emergency situations,<br />
authorization is required for continued stay.<br />
■ Limitations:<br />
— Patients age 19 and older: 30 days per fiscal year (FY 1 ) or in any single admission<br />
— Patients age 18 and under: 45 days per FY 1 or in any single admission<br />
— Inpatient admissions for substance use disorder detoxification and rehabilitation<br />
count toward the 30- or 45-day limit for acute inpatient psychiatric care.<br />
(Limitations may be waived if determined to be medically or psychologically necessary.)<br />
Psychiatric Partial<br />
Hospitalization <strong>Program</strong> (PHP)<br />
Psychiatric PHPs are treatment settings capable of providing interdisciplinary therapeutic services at<br />
least three hours a day, five days a week, in any combination of day, evening, night, and weekend<br />
treatment programs. The following rules apply:<br />
— Prior authorization is required. PHP admissions are not considered emergencies.<br />
— Facilities must be <strong>TRICARE</strong>-authorized.<br />
— PHPs must have participation agreements with <strong>TRICARE</strong>.<br />
■ Limitations:<br />
— PHP care is limited to 60 treatment days (whether full- or partial-day treatment) per FY 1 .<br />
These 60 days are not offset by or counted toward the 30- or 45-day limit for acute inpatient<br />
psychiatric care.<br />
(Limitations may be waived if determined to be medically or psychologically necessary.)<br />
Residential Treatment Center<br />
(RTC) Care<br />
RTC care provides extended psychiatric care for children and adolescents with psychological<br />
disorders that require continued treatment in a therapeutic environment. The following rules apply:<br />
— Facilities must be <strong>TRICARE</strong>-authorized.<br />
— Unless therapeutically contraindicated, the family and/or guardian should actively participate<br />
in the continuing care of the patient through either direct involvement at the facility or<br />
geographically distant family therapy.<br />
— Prior authorization is always required. RTC admissions are not considered emergencies.<br />
— RTC care is considered elective and will not be covered for emergencies.<br />
— Admission primarily for substance use rehabilitation is not authorized for psychiatric RTC<br />
care. In an emergency, psychiatric inpatient hospitalization must be sought first.<br />
— Care must be recommended and directed by a psychiatrist or clinical psychologist.<br />
■ Limitations:<br />
— Care is limited to 150 days per FY 1 or for a single admission. (Limitations may be waived if<br />
determined to be medically or psychologically necessary.)<br />
— RTC care is only covered for patients until reaching age 21.<br />
— RTC care does not count toward the 30- or 45-day inpatient limit.<br />
1<br />
October 1- September 30.<br />
19