TRICARE Overseas Program Provider Manual
TRICARE Overseas Program Provider Manual
TRICARE Overseas Program Provider Manual
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
other Covered Beneficiaries<br />
Beneficiaries on Active Duty for More Than 30 Days<br />
If a beneficiary is activated for more than 30 consecutive days,<br />
they receive <strong>TRICARE</strong> benefits as an ADSM.<br />
The <strong>TRICARE</strong>-eligible family members who reside overseas with<br />
the ADSM sponsor receive coverage as Active Duty Family<br />
Members (ADFM) while the sponsor is activated. These ADFM<br />
are eligible to enroll in TOP Prime options if they are Command<br />
Sponsored (authorized by the U.S. Government to accompany<br />
their sponsor to the overseas location). If ADFM do not enroll in<br />
TOP Prime or TOP Prime Remote, they may choose to use TOP<br />
Standard, which does not require enrollment.<br />
Beneficiaries on Active Duty for 30 Days or Less<br />
National Guard and Reserve members serving overseas on<br />
orders for 30 days or less are not eligible for <strong>TRICARE</strong> active duty<br />
benefits. However, if the beneficiary is injured or becomes ill while<br />
traveling to or from annual training while on active duty, he/she is<br />
eligible for line-of-duty care. Beneficiaries may also seek<br />
emergency and urgent care while serving on their orders.<br />
Beneficiaries Enrolled in the Continental U.S. (CoNUS)<br />
For beneficiaries who are enrolled in a Continental U.S. (CONUS)<br />
<strong>TRICARE</strong> program and are traveling overseas, authorizations are<br />
needed for urgent care. Emergency care services can be<br />
delivered on a cashless, claimless basis without authorization.<br />
However, <strong>Provider</strong>s are encouraged to call International SOS to<br />
coordinate care upfront.<br />
other Health Insurance<br />
As required by law, <strong>TRICARE</strong> can only pay after all other active<br />
insurance policies have paid their share. This includes National<br />
Health Insurance. As outlined below, proof of submitting the claim<br />
to the other health insurer (including any payment information) must<br />
be submitted with the Claim Form.<br />
If the patient has Other Health Insurance (OHI), you must claim<br />
payment from the OHI first.<br />
Once the OHI has processed and paid the claim, you can then<br />
seek reimbursement for any outstanding payments from <strong>TRICARE</strong><br />
directly. If the OHI covers all costs associated with treating the<br />
beneficiary, then you will not need to submit a claim to <strong>TRICARE</strong>.<br />
Once the OHI has issued your payment, you must enter the amount<br />
paid in the relevant field on the corresponding Claim Form (field 29<br />
on the CMS 1500 or field 54 on the UB-04 Claim Form). You may<br />
also submit a copy of the Explanation of Benefits (EOB) from the<br />
OHI, when submitting your Claim Form and Itemized Invoice.<br />
If the OHI has not made any payment, you must submit the EOB<br />
from the OHI to International SOS when submitting the claim.<br />
<strong>TRICARE</strong> Pharmacy <strong>Program</strong><br />
<strong>TRICARE</strong> offers comprehensive prescription drug coverage and<br />
several options for filling prescriptions. The beneficiary is<br />
responsible for paying and claiming for their medications, unless<br />
the Pharmacy agrees to file claims on behalf of the beneficiary.<br />
Some Pharmacies may decide to offer cashless medical services to<br />
<strong>TRICARE</strong> beneficiaries. This means that the <strong>Provider</strong> will be<br />
responsible for submitting a completed Claim Form and Itemized<br />
Invoice to International SOS for reimbursement. Pharmacists will not<br />
require an Authorization Form to deliver this service. A TOP<br />
Pharmacy Pack is available for Pharmacies who decide to provide<br />
cashless medical services to <strong>TRICARE</strong> beneficiaries. The TOP<br />
Pharmacy Pack includes step-by-step instructions for the<br />
Pharmacist on how to complete the correct Claim Form as well as<br />
an information guide about formulary drug coverage. To request<br />
a TOP Pharmacy Pack, please contact your TOP Regional Call<br />
Center and press option #5 to speak with a member of your<br />
TOP <strong>Provider</strong> Support Services staff.<br />
To fill a prescription, <strong>TRICARE</strong> beneficiaries will need a written<br />
prescription and a <strong>TRICARE</strong> Prime Enrollment Card as well as a<br />
valid Military ID Card or CAC.<br />
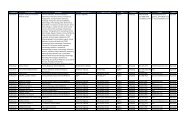
When <strong>Provider</strong>s write a prescription they are asked to include all of<br />
the information shown on Figure 2.1:<br />
12