TRICARE Overseas Program Provider Manual
TRICARE Overseas Program Provider Manual
TRICARE Overseas Program Provider Manual
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
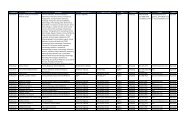
ToP: Explanation of Benefits Denial Codes and Remarks (continued)<br />
Code Description Additional Information<br />
044 Duplicate of services previously claimed (system).<br />
045 Applied to deductible – see Item Six on Reverse.<br />
049 Authorization not on file. Contact your HBA.<br />
050 Insufficient Diagnosis – see Item Four on Reverse.<br />
056 Chiropractic services not covered.<br />
059 Obesity not a covered diagnosis – see Item Four on Reverse.<br />
067 Medical need not documented.<br />
070 Patient not eligible. Per DEERS, patient is not eligible.<br />
072<br />
Claim requires drug name, strength and quantity. See Item Two on Reverse for<br />
time limit to send requested information.<br />
074 Sponsor not on DEERS.<br />
075 Patient not on DEERS.<br />
077 Dependent patient not on DEERS.<br />
080 ID card or eligibility expired on DEERS.<br />
083 Insufficient information received.<br />
126 Level of care billed not substantiated.<br />
Information requested (such as<br />
medical records) were insufficient<br />
to support the care/request.<br />
Upon review, it was determined<br />
that the charges billed were for<br />
more services than what was<br />
actually provided. For example,<br />
<strong>Provider</strong> is billing for a new patient<br />
office visit when we have already<br />
paid a new patient office visit for<br />
the same <strong>Provider</strong>. So, the <strong>Provider</strong><br />
should have been billing as an<br />
established patient office visit.<br />
110