TRICARE Overseas Program Provider Manual
TRICARE Overseas Program Provider Manual
TRICARE Overseas Program Provider Manual
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
R<br />
<strong>TRICARE</strong> <strong>Overseas</strong> <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong>
An Important Note About <strong>TRICARE</strong> <strong>Program</strong> Information:<br />
At the time of printing, the information in this <strong>TRICARE</strong> <strong>Overseas</strong> <strong>Program</strong> (TOP) <strong>Provider</strong> <strong>Manual</strong> is current.<br />
It is important to remember that <strong>TRICARE</strong> policies and benefits are governed by United States public law and federal regulations.<br />
Changes to <strong>TRICARE</strong> programs are continually made as public law and/or federal regulations are amended.<br />
For the most recent information, contact International SOS or visit www.tricare.mil.<br />
More information regarding <strong>TRICARE</strong>, including the Health Insurance Portability<br />
and Accountability Act (HIPAA) Notice of Privacy Practices, can be<br />
found online at www.tricare.mil.<br />
2
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Table of Contents<br />
SECTIoN 1: About International SoS and <strong>TRICARE</strong> overseas <strong>Program</strong> . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .5<br />
Introduction Letter . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .5<br />
About International SOS . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .6<br />
About Defense Health Agency and the Military Health System . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .6<br />
What is the <strong>TRICARE</strong> <strong>Overseas</strong> <strong>Program</strong>? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .6<br />
<strong>TRICARE</strong> <strong>Overseas</strong> <strong>Program</strong> <strong>Provider</strong> <strong>Manual</strong> Overview . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .7<br />
International SOS <strong>TRICARE</strong> Contact Information . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .7<br />
Reporting Fraud and Abuse . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .8<br />
SECTIoN 2: <strong>TRICARE</strong> overseas <strong>Program</strong> Benefits . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .9<br />
Identifying <strong>TRICARE</strong> Patients and Validating Coverage . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .9<br />
Sample TOP Prime and TOP Prime Remote Enrollment Cards . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .9<br />
TOP Prime and TOP Prime Remote Eligibility . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .10<br />
— TOP Prime . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .11<br />
— TOP Prime Remote . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .11<br />
Other Covered Beneficiaries . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .12<br />
— Beneficiaries on Active Duty for More Than 30 Days . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .12<br />
— Beneficiaries on Active Duty for 30 Days or Less . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .12<br />
— Beneficiaries Enrolled in the Continental U.S. (CONUS) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .12<br />
Other Health Insurance . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .12<br />
<strong>TRICARE</strong> Pharmacy <strong>Program</strong> . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .12<br />
<strong>TRICARE</strong> Dental <strong>Program</strong> . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .13<br />
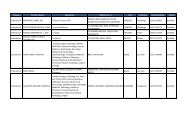
TOP Prime and TOP Prime Remote Beneficiary Covered Services . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .13<br />
TOP Prime and TOP Prime Remote Beneficiary Coverage Limitations . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .20<br />
TOP Prime and TOP Prime Remote Beneficiary Coverage Exclusions . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .22<br />
SECTIoN 3: International SoS Network <strong>Provider</strong>s and <strong>Provider</strong> Credentialing . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .24<br />
What is a Network <strong>Provider</strong>? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .24<br />
Becoming an International SOS Network <strong>Provider</strong> . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .24<br />
How to Become an International SOS Network <strong>Provider</strong> . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .24<br />
Network <strong>Provider</strong> Responsibilities . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .24<br />
Keeping Your <strong>Provider</strong> File Current . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .25<br />
Network <strong>Provider</strong> Quality Mission . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .25<br />
TOP <strong>Provider</strong> Support Services . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .25<br />
Access to Care . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .26<br />
<strong>Provider</strong> Credentialing Process . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .26<br />
Beneficiary Access to TOP Network <strong>Provider</strong>s . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .27<br />
SECTIoN 4: Authorizations and Seeing <strong>TRICARE</strong> Patients . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .28<br />
How Are Patients Referred to You? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .28<br />
— TOP Prime and TOP Prime Remote Beneficiaries . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .28<br />
— TOP Standard Beneficiaries . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .28<br />
Determining Patient Eligibility for Authorized Care . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .28<br />
Authorization Forms . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .30<br />
— Authorization for Cases of Pregnancy . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .32<br />
— Emergency Assistance Treatment and Authorizations and Payment . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .32<br />
— Clear and Legible Reporting: Issuing a Medical Report Following Patient Care . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .32<br />
Patient Records and Privacy . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .32<br />
Cultural Differences and Host Nation Patient Liaisons . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .32<br />
3
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Table of Contents (continued)<br />
SECTIoN 5: <strong>Provider</strong> Claims Information . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .33<br />
Process for Submitting Claims . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .33<br />
Web-based Claims Submission Options . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .34<br />
— Secure Message Transmission . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .34<br />
— Online Claim Submission . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .41<br />
Claims for Services Rendered Before September 1, 2010 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .49<br />
Claim Tracking and Monitoring . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .49<br />
Timely Filing of Claims . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .49<br />
Claim Reimbursement and Payment . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .49<br />
Required Criteria for Ensuring Payment of Claims . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .50<br />
Explanation of Benefits and Applicable Exchange Rate Information . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .50<br />
Transaction Fees Associated with Claim Reimbursement and Payments . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .56<br />
What if Both Non-Institutional & Institutional <strong>Provider</strong>s Are Used for the Same ‘Episode of Care’ and Billed Independently? . . . . . . . . . .56<br />
What if a Beneficiary Does Not Show for an Appointment? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .56<br />
Step-By-Step Instructions for Accurately Completing Claim Forms . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .56<br />
— The Claims Process . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .57<br />
SECTIoN 6: The <strong>Provider</strong> Portal . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .69<br />
Registering to the <strong>Provider</strong> Portal . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .69<br />
Using the <strong>Provider</strong> Portal . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .77<br />
— The <strong>Provider</strong> Dashboard . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .77<br />
— Claim Status . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .86<br />
— Patient Eligibility . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .95<br />
— Manage Locations . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .96<br />
— My Profile . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .97<br />
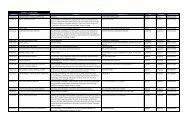
<strong>TRICARE</strong> Covered Benefits . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .98<br />
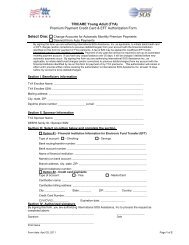
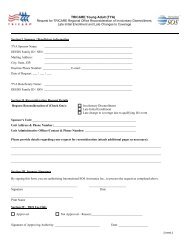
SECTIoN 7: <strong>TRICARE</strong> overseas <strong>Program</strong> <strong>Provider</strong> Forms . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .100<br />
Sample: CMS 1500 Claim Form . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .100<br />
Sample: UB-04 Claim Form . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .102<br />
Sample: International SOS Authorization Form . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .104<br />
Sample: EDI Agreement Form . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .105<br />
Sample: EFT Form for <strong>Provider</strong>s . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .106<br />
Sample: EFT Form for <strong>Provider</strong>s Who Use a Billing Agency . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .107<br />
SECTIoN 8: List of Acronyms . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .108<br />
Appendix . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .109<br />
TOP: Explanation of Benefits Denial Codes and Remarks . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .109<br />
4
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
SECTIoN 1<br />
About International SoS and<br />
the <strong>TRICARE</strong> overseas <strong>Program</strong><br />
SECTIoN 1:<br />
About International SoS and the <strong>TRICARE</strong> overseas <strong>Program</strong><br />
April 2011<br />
Dear <strong>TRICARE</strong> <strong>Provider</strong>,<br />
International SOS Assistance, Inc. (International SOS) is proud to serve as the Department of Defense <strong>TRICARE</strong> <strong>Overseas</strong> <strong>Program</strong> (TOP)<br />
contractor, effective September 1, 2010. We are fully committed to delivering high-quality, readily available, and comprehensive health<br />
care services for the nearly half a million <strong>TRICARE</strong> beneficiaries, including deployed personnel, travelers, and retirees outside the 50<br />
United States and the District of Columbia.<br />
International SOS remains focused on processing all claims and inquiries in a timely and accurate manner. Working together with you, our<br />
network of health care <strong>Provider</strong>s who will be supporting us, we have created an efficient and timely cashless, claimless process for<br />
beneficiaries. International SOS has been serving a large population of this customer base since 1998.<br />
This manual describes the <strong>TRICARE</strong> program and requirements. It also provides important TOP Regional Call Center numbers and<br />
website information. International SOS is always here for you in case you need further assistance. We encourage you to visit<br />
www.tricare-overseas.com for various <strong>Provider</strong> services, including covered services, how to submit claims for timely reimbursement,<br />
referrals and authorizations, credentialing and the benefits of becoming part of the <strong>TRICARE</strong> <strong>Provider</strong> Network.<br />
International SOS understands the value of services you provide to our Department of Defense military members and their families.<br />
We look forward to our continued successful relationships bringing the very best care to beneficiaries worldwide. Thank you for the very<br />
important role you play in helping us to achieve this goal.<br />
Kind regards,<br />
Kelley Harar<br />
Chief Operating Officer, <strong>TRICARE</strong> <strong>Overseas</strong> <strong>Program</strong><br />
International SOS<br />
5
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Since 1998,<br />
International SOS has<br />
supported <strong>TRICARE</strong> in<br />
ensuring that Active Duty<br />
Service Members and their<br />
families receive the highest<br />
quality care, no matter<br />
where their work or<br />
travels take them.<br />
About International SoS<br />
International SOS (http://www.internationalsos.com) is<br />
the world's leading medical and travel security risk services<br />
company. We care for clients across the globe, from more<br />
than 700 locations in 89 countries. Our expertise is unique:<br />
approximately 11,000 employees are led by 1,200 doctors<br />
and 200 security specialists. Teams work night and day to<br />
protect our members.<br />
Since 1998, International SOS has supported <strong>TRICARE</strong> in<br />
ensuring that Active Duty Service Members (ADSM) and their<br />
families receive the highest quality care, no matter where<br />
their work or travels take them.<br />
About Defense Health Agency and<br />
the Military Health System<br />
Defense Health Agency (DHA), the Defense Department activity<br />
that administers the health care plan for the uniformed services,<br />
retirees and their families, serves more than 9.5 million eligible<br />
beneficiaries worldwide in the Military Health System (MHS). The<br />
mission of the MHS is to enhance Department of Defense and<br />
national security by providing health support for the full range of<br />
military operations. The MHS provides quality medical care<br />
through a network of <strong>Provider</strong>s, Military Treatment Facilities<br />
(MTF), medical clinics and dental clinics worldwide.<br />
What is the <strong>TRICARE</strong> overseas<br />
<strong>Program</strong>?<br />
<strong>TRICARE</strong> is a comprehensive health care program provided to<br />
active and retired members of the United States uniformed<br />
services, their spouses and children, survivors and certain other<br />
beneficiaries.<br />
On October 21, 2009, International SOS was selected by DHA as<br />
the contractor for the <strong>TRICARE</strong> <strong>Overseas</strong> <strong>Program</strong> (TOP) in<br />
locations outside the 50 United States and the District of<br />
Columbia. International SOS began delivering health care<br />
services on September 1, 2010.<br />
TOP is designed to enhance existing operations, improve<br />
<strong>Provider</strong> satisfaction and deliver high-quality, patient-centered<br />
care for nearly half a million beneficiaries overseas.<br />
For <strong>TRICARE</strong> beneficiaries living overseas, TOP will offer options<br />
including TOP Prime, TOP Prime Remote and TOP Standard as<br />
6
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
SECTIoN 1<br />
About International SoS and<br />
the <strong>TRICARE</strong> overseas <strong>Program</strong><br />
well as <strong>TRICARE</strong> for Life, <strong>TRICARE</strong> Reserve Select, <strong>TRICARE</strong><br />
Retired Reserve, and <strong>TRICARE</strong> Young Adult.<br />
International SOS is developing a network of <strong>Provider</strong>s primarily<br />
to support TOP Prime and TOP Prime Remote beneficiaries. We<br />
recognize that TOP Standard beneficiaries may also choose to<br />
seek care from some Network <strong>Provider</strong>s.<br />
The TOP Prime program delivers the prime benefit to ADSM and<br />
their families in the three overseas areas: Eurasia-Africa, the<br />
Pacific, and Latin America and Canada. The TOP Prime Remote<br />
program delivers the prime benefit to ADSM and their families<br />
stationed in designated remote locations overseas.<br />
International SoS <strong>TRICARE</strong><br />
Contact Information<br />
If you have any questions about claims, payments, how to<br />
become a Network <strong>Provider</strong> or credentialing and certification<br />
requirements, please contact your TOP Regional Call Center.<br />
Customer Service Phone Numbers<br />
Europe, Middle East & Africa +44-20-8762-8384<br />
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong> overview<br />
Latin America and Canada +1-215-942-8393<br />
Puerto Rico +1-877-867-1091<br />
This TOP <strong>Provider</strong> <strong>Manual</strong> has been developed to provide you<br />
and your staff with basic, important information about the<br />
<strong>TRICARE</strong> <strong>Overseas</strong> <strong>Program</strong> (TOP). The manual will assist you in<br />
coordinating care for TOP beneficiaries. It contains detailed<br />
information about TOP programs, policies and procedures.<br />
Additional TOP program information can be found online by<br />
visiting www.tricare-overseas.com. <strong>Provider</strong>s can also visit the<br />
<strong>TRICARE</strong> website at www.tricare.mil. <strong>TRICARE</strong> program<br />
manuals are available in their entirety at the DHA <strong>Manual</strong>s<br />
website.<br />
Thank you for your commitment to the Department of Defense<br />
overseas military community.<br />
Asia-Pacific +65-6339-2676<br />
Australasia +61-2-9273-2710<br />
If a patient attends an appointment and you require assistance<br />
with determining eligibility, covered benefits, or receiving prior<br />
authorization for care, please contact the Medical Assistance<br />
lines below:<br />
Medical Assistance Phone Numbers<br />
Europe, Middle East & Africa +44-20-8762-8133<br />
Latin America and Canada +1-215-942-8320<br />
Puerto Rico +1-215-942-8320<br />
Asia-Pacific +65-6338-9277<br />
Australasia +61-2-9273-2760<br />
Visit www.tricare-overseas.com for a full listing of toll free phone<br />
numbers by country. This website will be updated regularly, as<br />
additional information becomes available.<br />
7
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
The following email addresses are also available, for contacting<br />
your TOP <strong>Provider</strong> Support Services staff:<br />
Europe, Middle East & Africa<br />
providerseurasiaafrica@internationalsos.com<br />
Latin America and Canada<br />
providerslatinamerica@internationalsos.com<br />
Puerto Rico<br />
provider.inquiries.PR@internationalsos.com<br />
Asia-Pacific<br />
providersasiapacific@internationalsos.com<br />
Additionally, <strong>Provider</strong>s can inquire about specific claims issues<br />
by sending their questions to the International SOS TOP Claims<br />
Processing Department via the Web-based Secure Message<br />
Transmission function on the <strong>Provider</strong> Portal. Please see Section<br />
6: The <strong>Provider</strong> Portal for additional information about accessing<br />
the Secure Message Inbox.<br />
Reporting Fraud and Abuse<br />
International SOS as part of the <strong>TRICARE</strong> <strong>Overseas</strong> <strong>Program</strong> is<br />
committed to detecting, correcting, and preventing health care<br />
fraud and abuse.<br />
Fraud happens when a person or organization takes action to<br />
deliberately deceive others to gain an unauthorized benefit.<br />
Health care abuse occurs when <strong>Provider</strong>s supply services or<br />
products that are medically unnecessary or that do not meet<br />
professional standards.<br />
Write to the customer service department for TOP to report<br />
suspected fraud and abuse:<br />
ATTN: <strong>TRICARE</strong> <strong>Program</strong> Integrity<br />
1717 W. Broadway<br />
PO Box 7635<br />
Madison, Wisconsin 53707<br />
USA<br />
You can also send an email to reportit@wpsic.com<br />
or submit an electronic form posted on<br />
http://www.tricare-overseas.com/fraud.htm.<br />
Be sure to provide as much information as possible.<br />
Fraud or abuse issues can also be reported directly to<br />
<strong>TRICARE</strong> by emailing fraudline@dha.osd.mil.<br />
If you would like to obtain additional information about<br />
International SOS’ <strong>Program</strong> Integrity mission, please email<br />
ToP<strong>Program</strong>Integrity@internationalsos.com.<br />
<strong>Program</strong> Integrity information is also available online at<br />
www.tricare-overseas.com/fraud.htm.<br />
8
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
SECTIoN 2:<br />
<strong>TRICARE</strong> overseas <strong>Program</strong> Benefits<br />
Identifying <strong>TRICARE</strong> Patients and<br />
Validating Coverage<br />
Sample ToP Prime and ToP Prime<br />
Remote Enrollment Cards<br />
SECTIoN 2<br />
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
Benefits<br />
<strong>TRICARE</strong> is available to a range of members serving under the<br />
U.S. Department of Defense.<br />
It is important to remember that not all U.S. patients are <strong>TRICARE</strong><br />
patients.<br />
Sample ToP Prime Enrollment Card<br />
■ Front of Card<br />
Because there are so many types of U.S. military patients who<br />
may seek care from you, it is critical to properly identify both the<br />
patient and their <strong>TRICARE</strong> status.<br />
<strong>TRICARE</strong> patients who seek care from you will have some<br />
way to prove that they are <strong>TRICARE</strong> eligible – this can be a U.S.<br />
Military Identification Card, a written confirmation from the<br />
Military Treatment Facility (MTF), or an Authorization Form from<br />
International SOS.<br />
■ Generally, children under 10 will not have their own Military<br />
Identification Card. The parent’s valid identification card is<br />
considered sufficient.<br />
■ <strong>TRICARE</strong> Prime Enrollment Cards are only valid when<br />
presented with a valid Military ID Card or Common Access<br />
Card (CAC). Please ensure that the names on both cards<br />
match, that the expiration date on the Military ID Card or CAC<br />
has not lapsed, and that the photo on this card accurately<br />
represents the patient.<br />
■ Back of Card<br />
■ If you have a concern about an individual patient, you may<br />
contact your TOP Regional Call Center for assistance 24/7.<br />
■ <strong>Provider</strong>s are authorized and encouraged to photocopy both<br />
sides of a patient’s Military ID Card or <strong>TRICARE</strong> Enrollment<br />
Card.<br />
■ Once the <strong>Provider</strong> is registered to the online <strong>Provider</strong> Portal<br />
available at www.tricare-overseas.com they will also be able<br />
to check a patient’s eligibility through the portal.<br />
Sample TOP Prime and TOP Prime Remote Enrollment Cards are<br />
included here for your reference.<br />
9
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Sample ToP Prime Remote Enrollment Card<br />
■ Front of Card<br />
ToP Prime and ToP Prime Remote<br />
Eligibility<br />
This section introduces several terms you may come across while<br />
treating <strong>TRICARE</strong> beneficiaries.<br />
<strong>TRICARE</strong> provides payment for covered services as long as the<br />
beneficiary is eligible and the care is properly authorized.<br />
Once a <strong>Provider</strong> agrees to participate, and they have agreed to<br />
provide cashless, claimless services to TOP Prime and TOP<br />
Prime Remote beneficiaries, they will submit the appropriate<br />
Standard U.S. Claim Forms on behalf of the beneficiaries and will<br />
provide medical services in line with <strong>TRICARE</strong> policy.<br />
■ Back of Card<br />
With the exception of emergency care and the first eight<br />
outpatient visits for behavioral health care, and one annual<br />
optometry screening (3 years and older), TOP Prime and TOP<br />
Prime Remote beneficiaries are eligible to receive cashless,<br />
claimless service from a Host Nation <strong>Provider</strong>. 1<br />
It is important to remember that in most cases International SOS<br />
will provide you with an Authorization Form for TOP Prime and<br />
TOP Prime Remote beneficiaries.<br />
All other beneficiaries who are not TOP Prime or TOP Prime<br />
Remote are required to pay for service upfront and then file a<br />
<strong>TRICARE</strong> claim directly. As an International SOS Network<br />
<strong>Provider</strong>, you may choose to file claims on behalf of beneficiaries<br />
who are not TOP Prime or TOP Prime Remote, but are not<br />
required to do so.<br />
Active Duty Service Members (ADSM) are required to enroll in<br />
TOP Prime. Depending on where they are stationed overseas,<br />
they must enroll in one of the following two TOP Prime options:<br />
TOP Prime and TOP Prime Remote Active Duty Service Members<br />
(ADSM) will receive an enrollment card similar to the sample card<br />
graphic above. When presented with the beneficiary’s Military ID<br />
Card or CAC, this is one method <strong>Provider</strong>s can use to validate<br />
<strong>TRICARE</strong> eligibility.<br />
Note: Only TOP Prime and TOP Prime Remote beneficiaries will<br />
receive an enrollment card. Other <strong>TRICARE</strong> beneficiaries, such<br />
as TOP Standard, will not be issued an enrollment card. However,<br />
they will be given a Military ID Card or CAC. Therefore, the<br />
enrollment card is key for identifying those beneficiaries who are<br />
eligible for TOP Prime or TOP Prime Remote care.<br />
■ TOP Prime<br />
■ TOP Prime Remote<br />
Note: If you have any questions about how to determine<br />
beneficiary eligibility or the TOP option under which the<br />
beneficiary is covered, please contact your TOP Regional<br />
Call Center and select option #5 to speak with a member of<br />
your TOP <strong>Provider</strong> Support Services staff.<br />
10<br />
1 The <strong>TRICARE</strong> <strong>Overseas</strong> <strong>Program</strong> also operates in Puerto Rico, Guam,<br />
American Samoa, U.S. Virgin Islands and Northern Marianas.
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
ToP Prime<br />
TOP Prime beneficiaries live within a 40-mile radius of a U.S. MTF.<br />
These beneficiaries are required to seek care through their local<br />
MTF.<br />
If an MTF does not have the capability to provide treatment to the<br />
beneficiary, the assigned Primary Care Manager (or treating<br />
practitioner within the MTF) may refer the beneficiary to<br />
International SOS to find a Network <strong>Provider</strong>. International SOS<br />
will issue an Authorization Form to the Network <strong>Provider</strong> before<br />
care can be delivered.<br />
The medical oversight of the beneficiary’s care still resides with<br />
the MTF Primary Care Manager or assigned host nation Primary<br />
Care Manager. All medical notes and consult findings should be<br />
sent back to the MTF or assigned host nation Primary Care<br />
Manager within 10 working days for routine consultation reports<br />
and within 24 hours for urgent consultation reports.<br />
ToP Prime Remote<br />
TOP Prime Remote beneficiaries live more than 40 miles away<br />
from an overseas U.S. MTF. TOP Prime Remote beneficiaries will<br />
receive their primary care from a Host Nation <strong>Provider</strong> who will<br />
serve as their Primary Care Physician.<br />
International SOS acts as the Primary Care Manager for all TOP<br />
Prime Remote Beneficiaries.<br />
International SOS manages all referrals and medical oversight of<br />
TOP Prime Remote beneficiaries living overseas. All medical<br />
notes and consult findings, including authorizations for referrals<br />
to secondary care or inpatient admissions should be discussed<br />
with International SOS.<br />
11<br />
The following table shows the various TOP options available by<br />
beneficiary type:<br />
Beneficiary Type<br />
Active Duty Service<br />
Members (ADSM)<br />
Active Duty Family<br />
Members 2<br />
(ADFM) and transitional<br />
survivors<br />
Retired service members 4<br />
and family members,<br />
survivors, Medal of Honor<br />
recipients, certain unremarried<br />
former spouse,<br />
and others who are<br />
registered in the Defense<br />
Enrollment Eligibility<br />
Reporting System (DEERS). 6<br />
ToP <strong>Program</strong> options<br />
■ TOP Prime<br />
■ TOP Prime Remote<br />
■ <strong>TRICARE</strong> Active Duty<br />
Dental <strong>Program</strong> (ADDP) 1<br />
■ TOP Prime<br />
■ TOP Prime Remote<br />
■ TOP Standard 3<br />
■ <strong>TRICARE</strong> For Life (TFL)<br />
(if you have both Medicare<br />
Part A and Part B) 4<br />
■ <strong>TRICARE</strong> Dental <strong>Program</strong><br />
■ <strong>TRICARE</strong> Young Adult<br />
<strong>Program</strong> (TYA) 7<br />
■ TOP Standard<br />
■ TFL (if you have both<br />
Medicare Part A and Part B) 4<br />
■ <strong>TRICARE</strong> Retired Reserve 5<br />
■ TYA 7<br />
■ <strong>TRICARE</strong> Reserve Select<br />
■ Enhanced-<strong>Overseas</strong>e<br />
<strong>TRICARE</strong> Retiree Dental<br />
<strong>Program</strong><br />
■ <strong>TRICARE</strong> PLUS (depending<br />
on military hospital or<br />
clinical availability)<br />
SECTIoN 2<br />
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
Benefits<br />
1 The ADDP is only available in the United States and in U.S. territories (American Samoa, Guam,<br />
the Northern Mariana Islands, Puerto Rico, and the U.S. Virgin Islands). See page 13 for<br />
additional details about the <strong>TRICARE</strong> Dental <strong>Program</strong>.<br />
2 Active Duty Family Members (ADFM) include the sponsor’s <strong>TRICARE</strong>-eligible spouse and<br />
children. Unmarried children may remain <strong>TRICARE</strong>-eligible until age 21 (or age 23 if enrolled<br />
in a full-time course of study at an approved institution of higher learning, and if the sponsor<br />
provides 50 percent or more of the financial support, (but have not yet reached age 26). A<br />
disabled child may remain <strong>TRICARE</strong>-eligible beyond normal age limits.<br />
3 ADFM who are not eligible for, or choose not to enroll in TOP Prime options may use TOP<br />
Standard.<br />
4 Most beneficiaries who are entitled to Medicare Part A must have Medicare Part B to remain<br />
<strong>TRICARE</strong>-eligible. ADFMs who have Medicare Part A are not required to have Medicare Part B<br />
to remain eligible for <strong>TRICARE</strong>. However, once the sponsor reaches age 65, Medicare Part B<br />
must be in effect no later than the sponsor’s retirement date to avoid a break in <strong>TRICARE</strong><br />
coverage.<br />
5 Retired service members and their family members are not eligible to enroll in TOP Prime<br />
options. They may be eligible to use TOP Standard or <strong>TRICARE</strong> for Life. Certain retired National<br />
Guard and Reserve members and their families may qualify to purchase <strong>TRICARE</strong> Retired<br />
Reserve coverage.<br />
6 Individual eligibility is determined by DEERS. Beneficiaries are responsible for ensuring their<br />
information is current in this system. <strong>TRICARE</strong> claims for patients who are not listed as eligible in<br />
DEERS cannot be paid by International SOS.<br />
7 The premium-based <strong>TRICARE</strong> Young Adult (TYA) program extends <strong>TRICARE</strong> coverage to<br />
certain qualified dependents until reaching age 26, and may be an option for adult children who<br />
‘age out’ of other <strong>TRICARE</strong> benefits. For more information, please visit www.tricare.mil/tya.
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
other Covered Beneficiaries<br />
Beneficiaries on Active Duty for More Than 30 Days<br />
If a beneficiary is activated for more than 30 consecutive days,<br />
they receive <strong>TRICARE</strong> benefits as an ADSM.<br />
The <strong>TRICARE</strong>-eligible family members who reside overseas with<br />
the ADSM sponsor receive coverage as Active Duty Family<br />
Members (ADFM) while the sponsor is activated. These ADFM<br />
are eligible to enroll in TOP Prime options if they are Command<br />
Sponsored (authorized by the U.S. Government to accompany<br />
their sponsor to the overseas location). If ADFM do not enroll in<br />
TOP Prime or TOP Prime Remote, they may choose to use TOP<br />
Standard, which does not require enrollment.<br />
Beneficiaries on Active Duty for 30 Days or Less<br />
National Guard and Reserve members serving overseas on<br />
orders for 30 days or less are not eligible for <strong>TRICARE</strong> active duty<br />
benefits. However, if the beneficiary is injured or becomes ill while<br />
traveling to or from annual training while on active duty, he/she is<br />
eligible for line-of-duty care. Beneficiaries may also seek<br />
emergency and urgent care while serving on their orders.<br />
Beneficiaries Enrolled in the Continental U.S. (CoNUS)<br />
For beneficiaries who are enrolled in a Continental U.S. (CONUS)<br />
<strong>TRICARE</strong> program and are traveling overseas, authorizations are<br />
needed for urgent care. Emergency care services can be<br />
delivered on a cashless, claimless basis without authorization.<br />
However, <strong>Provider</strong>s are encouraged to call International SOS to<br />
coordinate care upfront.<br />
other Health Insurance<br />
As required by law, <strong>TRICARE</strong> can only pay after all other active<br />
insurance policies have paid their share. This includes National<br />
Health Insurance. As outlined below, proof of submitting the claim<br />
to the other health insurer (including any payment information) must<br />
be submitted with the Claim Form.<br />
If the patient has Other Health Insurance (OHI), you must claim<br />
payment from the OHI first.<br />
Once the OHI has processed and paid the claim, you can then<br />
seek reimbursement for any outstanding payments from <strong>TRICARE</strong><br />
directly. If the OHI covers all costs associated with treating the<br />
beneficiary, then you will not need to submit a claim to <strong>TRICARE</strong>.<br />
Once the OHI has issued your payment, you must enter the amount<br />
paid in the relevant field on the corresponding Claim Form (field 29<br />
on the CMS 1500 or field 54 on the UB-04 Claim Form). You may<br />
also submit a copy of the Explanation of Benefits (EOB) from the<br />
OHI, when submitting your Claim Form and Itemized Invoice.<br />
If the OHI has not made any payment, you must submit the EOB<br />
from the OHI to International SOS when submitting the claim.<br />
<strong>TRICARE</strong> Pharmacy <strong>Program</strong><br />
<strong>TRICARE</strong> offers comprehensive prescription drug coverage and<br />
several options for filling prescriptions. The beneficiary is<br />
responsible for paying and claiming for their medications, unless<br />
the Pharmacy agrees to file claims on behalf of the beneficiary.<br />
Some Pharmacies may decide to offer cashless medical services to<br />
<strong>TRICARE</strong> beneficiaries. This means that the <strong>Provider</strong> will be<br />
responsible for submitting a completed Claim Form and Itemized<br />
Invoice to International SOS for reimbursement. Pharmacists will not<br />
require an Authorization Form to deliver this service. A TOP<br />
Pharmacy Pack is available for Pharmacies who decide to provide<br />
cashless medical services to <strong>TRICARE</strong> beneficiaries. The TOP<br />
Pharmacy Pack includes step-by-step instructions for the<br />
Pharmacist on how to complete the correct Claim Form as well as<br />
an information guide about formulary drug coverage. To request<br />
a TOP Pharmacy Pack, please contact your TOP Regional Call<br />
Center and press option #5 to speak with a member of your<br />
TOP <strong>Provider</strong> Support Services staff.<br />
To fill a prescription, <strong>TRICARE</strong> beneficiaries will need a written<br />
prescription and a <strong>TRICARE</strong> Prime Enrollment Card as well as a<br />
valid Military ID Card or CAC.<br />
When <strong>Provider</strong>s write a prescription they are asked to include all of<br />
the information shown on Figure 2.1:<br />
12
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Figure 2.1<br />
Name of the clinic<br />
Patient’s name and<br />
date of birth<br />
Clinic<br />
Name<br />
Name of <strong>Provider</strong><br />
<strong>Provider</strong> Street<br />
<strong>Provider</strong> Town<br />
<strong>Provider</strong> Telephone<br />
Date of Prescription<br />
<strong>Provider</strong>’s name<br />
<strong>Provider</strong>’s full<br />
address/phone number<br />
Date prescription is issued<br />
SECTIoN 2<br />
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
Benefits<br />
Generic (chemical)<br />
name of the medication<br />
being prescribed. NOTE:<br />
Do not use the brand name<br />
Please include dosage<br />
instructions (e.g. “Take<br />
2 tablets 2x a day”)<br />
Attending physician’s<br />
signature and name<br />
Name of Patient<br />
Patient DOB<br />
Generic (chemical) name of drug xxmg<br />
capsules, 30<br />
Dosage instructions<br />
Refill: not to exceed 12 months<br />
Dr. <strong>Provider</strong><br />
Dr. <strong>Provider</strong><br />
Strength of the medication<br />
(e.g. 50mg tablets)<br />
Number of tablets required<br />
Please include the number of<br />
refills the patient may receive.<br />
This cannot cover more than<br />
a year.<br />
<strong>Provider</strong>’s stamp<br />
Additional information about the <strong>TRICARE</strong> Pharmacy <strong>Program</strong><br />
can be found online at www.tricare.mil/pharmacy or<br />
www.express-scripts.com/<strong>TRICARE</strong>.<br />
<strong>TRICARE</strong> Dental <strong>Program</strong><br />
Active Duty Family Members<br />
ADFM enrolled in TOP Prime and TOP Prime Remote may receive<br />
their dental care under the <strong>TRICARE</strong> Dental <strong>Program</strong>. This is an<br />
optional program that requires enrollment. International SOS does<br />
not manage this care and cannot authorize these treatments.<br />
For additional information about the <strong>TRICARE</strong> Dental <strong>Program</strong>,<br />
please visit http://www.tricare.mil/Dental/TDP.aspx.<br />
Active Duty Service Members<br />
International SOS coordinates dental care for ADSM enrolled in<br />
TOP Prime Remote only. Care will be referred to an International<br />
SOS Network <strong>Provider</strong> Dentist.<br />
13<br />
Note: The Network <strong>Provider</strong> Dentist will need to receive an<br />
Authorization Form from International SOS first, and will then need<br />
to file a claim for reimbursement, accordingly.<br />
TOP Prime ASDM dental care is covered by United Concordia<br />
(UCCI). TOP Prime ADSM will receive their dental care at the<br />
Dental Treatment Facility at the MTF. For more information, please<br />
visit http://www/tricare.mil.<br />
ToP Prime and ToP Prime Remote<br />
Beneficiary Covered Services<br />
<strong>TRICARE</strong> covers most care that is medically necessary and<br />
considered proven. Some types of care are not covered at all,<br />
and there are special rules and limits for certain types of care.<br />
This section is not intended to be all-inclusive.<br />
<strong>TRICARE</strong> policies are very specific about which services are covered<br />
and which are not. It is in your best interest to take an active role in<br />
verifying coverage. If you have any questions about whether or not<br />
services are covered for the TOP Prime or TOP Prime Remote<br />
beneficiary you are seeing, please contact International SOS.<br />
Note: The following lists of services are subject to change.<br />
Please visit www.tricare.mil for a full list of covered services,<br />
limitations and exclusions.
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
outpatient Services: Coverage Details<br />
Figure 2.2<br />
Service<br />
Ambulance Services<br />
Description<br />
The following ambulance services are covered:<br />
■ Emergency transfers from a beneficiary’s home, accident scene, or other location to a hospital<br />
■ Transfers between hospitals<br />
■ Ambulance transfers from a hospital-based emergency room to a hospital more capable of providing<br />
the required care<br />
■ Transfers between a hospital or skilled nursing facility 1 and another hospital-based or freestanding<br />
outpatient therapeutic or diagnostic department/facility<br />
The following are excluded:<br />
■ Use of an ambulance service instead of taxi service when the patient’s condition would have permitted<br />
use of regular private transportation<br />
■ Transport or transfer of a patient primarily for the purpose of having the patient nearer to home, family,<br />
friends, or personal physician<br />
■ Medicabs or ambicabs that function primarily as public–passenger conveyances transporting patients to<br />
and from their medical appointments<br />
Note: Air or boat ambulance is only covered when the pickup point is inaccessible by a land<br />
vehicle, or when great distance or other obstacles are involved in transporting the beneficiary to<br />
the nearest hospital with appropriate facilities, and the patient’s medical condition warrants<br />
speedy admission or is such that transfer by other means is not advisable.<br />
Durable Medical Equipment,<br />
Prosthetics, orthotics, and<br />
Supplies (DMEPoS)<br />
Emergency Services<br />
Generally covered if prescribed by a physician and if directly related to a medical condition. Covered<br />
DMEPOS generally includes:<br />
■ DMEPOS that are medically necessary and appropriate and prescribed by a physician for a beneficiary’s<br />
specific use<br />
■ Duplicate DMEPOS items that are necessary to provide a fail-safe, in-home life-support system (In this<br />
case, “duplicate” means an item that meets the definition of DMEPOS and serves the same purpose but may<br />
not be an exact duplicate of the original DMEPOS item. For example, a portable oxygen concentrator may be<br />
covered as a backup for a stationary oxygen generator.)<br />
Note: Prosthetic devices must be U.S. Food and Drug Administration–approved.<br />
<strong>TRICARE</strong> defines an emergency as a serious medical condition that the average person would consider to<br />
be a threat to life, limb, sight, or safety. However, most dental emergencies, such as going to the emergency<br />
room for a severe toothache, are not a covered medical benefit under <strong>TRICARE</strong>.<br />
Home Health Care 1<br />
Covers part-time or intermittent skilled nursing services and home health care services for those confined to<br />
the home. (All care must be provided by a participating home health care agency and be authorized in advance<br />
by the regional contractor.)<br />
Individual <strong>Provider</strong> Services<br />
Covers office visits; outpatient, office-based medical and surgical care; consultation, diagnosis, and treatment<br />
by a specialist; allergy tests and treatment; osteopathic manipulation; rehabilitation services (e.g., physical<br />
and occupational therapy and speech pathology services); and medical supplies used within the office.<br />
1<br />
Skilled nursing facility care and home health care services are only available in the United States and U.S. territories (American Samoa, Guam, the Northern Mariana<br />
Islands, Puerto Rico, and the U.S. Virgin Islands).<br />
14
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
outpatient Services: Coverage Details (continued)<br />
Service<br />
Laboratory and X-ray Services<br />
Active Duty Service Member<br />
(ADSM) Respite Care<br />
Generally covered if prescribed by a physician.<br />
Description<br />
Covers respite care for ADSMs who are homebound as a result of a serious injury or illness incurred<br />
while serving on active duty; available if the ADSM’s plan of care includes frequent interventions by<br />
the primary caregiver. 1<br />
SECTIoN 2<br />
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
Benefits<br />
The following respite care limits apply:<br />
■ Five days per calendar week<br />
■ Eight hours per calendar day<br />
Note: Respite care must be provided by a <strong>TRICARE</strong>-authorized home health care agency and<br />
requires prior authorization from your regional contractor and the ADSM’s approving authority<br />
(i.e., referring military hospital or clinic). The ADSM is not required to be enrolled in the <strong>TRICARE</strong><br />
Extended Care Health Option program to receive the respite benefit.<br />
1<br />
More than two interventions are required during the eight-hour period per day that the primary caregiver would normally be sleeping.<br />
Inpatient Services: Coverage Details<br />
Figure 2.3<br />
Service<br />
Hospitalization<br />
(semi-private room/special care<br />
units when medically necessary)<br />
Skilled Nursing Facility Care 1<br />
(semiprivate room)<br />
Description<br />
Covers general nursing; hospital, physician, and surgical services; meals (including special diets);<br />
drugs and medications; operating and recovery room care; anesthesia; laboratory tests; X-rays and<br />
other radiology services; medical supplies and appliances; and blood and blood products.<br />
Note: Surgical procedures designated “inpatient only” may only be covered when performed in an<br />
inpatient setting.<br />
Covers skilled nursing services; meals (including special diets); physical, occupational, and speech<br />
therapy; drugs furnished by the facility; and necessary medical supplies and appliances. (<strong>TRICARE</strong><br />
covers an unlimited number of days as medically necessary.)<br />
1<br />
Skilled nursing facility care is only available in the United States and U.S. territories (American Samoa, Guam, the Northern Mariana Islands, Puerto Rico, and the U.S. Virgin<br />
Islands).<br />
15
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Clinical Preventive Service: Coverage Details Figure 2.4<br />
Service<br />
Comprehensive Health<br />
Promotion and Disease<br />
Prevention<br />
Examinations<br />
Targeted Health<br />
Promotion and Disease<br />
Prevention Services<br />
Cancer Screenings<br />
Description<br />
A comprehensive clinical preventive exam is covered if it includes an immunization, Pap test, mammogram, colon<br />
cancer screening, or prostate cancer screening. School enrollment physicals for children ages 5–11 are also covered.<br />
Beneficiaries in each of the following age groups may receive one comprehensive clinical preventive exam without<br />
receiving an immunization, Pap test, mammogram, colon cancer screening, or prostate cancer screening (one exam<br />
per age group): 2–4, 5–11, 12–17, 18–39, and 40–64.<br />
The screening examinations listed below may be covered if provided in conjunction with a comprehensive clinical<br />
preventive exam. The intent is to maximize preventive care.<br />
■ Colonoscopy:<br />
— Average Risk: Individuals at average risk for colon cancer are covered once every 10 years beginning at age 50.<br />
— Increased Risk: Once every five years for individuals with a first-degree relative diagnosed with a colorectal cancer or an<br />
adenomatous polyp before age 60, or in two or more first-degree relatives at any age. Optical colonoscopy should be performed<br />
beginning at age 40 or 10 years younger than the earliest affected relative, whichever is earlier. Once every 10 years, beginning at<br />
age 40, for individuals with a first-degree relative diagnosed with colorectal cancer or an adenomatous polyp at age 60 or older, or<br />
colorectal cancer diagnosed in two second-degree relatives.<br />
— High Risk: Once every one to two years for individuals with a genetic or clinical diagnosis of hereditary non-polyposis colorectal<br />
cancer (HNPCC) or individuals at increased risk for HNPCC. Optical colonoscopy should be performed beginning at age 20-25 or<br />
10 years younger than the earliest age of diagnosis, whichever is earlier. For individuals diagnosed with inflammatory bowel disease,<br />
chronic ulcerative colitis, or Crohn’s disease, cancer risk begins to be significant eight years after the onset of pancolitis or 10-12<br />
years after the onset of left-sided colitis. For individuals meeting these risk parameters, optical colonoscopy should be performed<br />
every one to two years with biopsies for dysplasia.<br />
■ Fecal occult blood testing: Conduct testing annually starting at age 50.<br />
■ Breast Cancer:<br />
— Clinical breast examination: For women under age 40, a clinical breast examination may be performed during a<br />
preventive health visit. For women age 40 and older, a clinical breast examination should be performed annually.<br />
— Mammograms: Covered annually for all women beginning at age 40. Covered annually beginning at age 30 for women who<br />
have a 15 percent or greater lifetime risk of breast cancer (according to risk-assessment tools based on family history such<br />
as the Gail model, the Claus model, and the Tyrer-Cuzick model), or who have any of the following risk factors:<br />
• History of breast cancer, ductal carcinoma in situ, lobular carcinoma in situ, atypical ductal hyperplasia, or atypical<br />
lobular hyperplasia<br />
• Extremely dense breasts when viewed by mammogram<br />
• Known BRCA1 or BRCA2 gene mutation<br />
• First-degree relative (parent, child, sibling) with a BRCA1 or BRCA2 gene mutation, and have not had genetic testing themselves<br />
• Radiation therapy to the chest between ages 10 and 30<br />
• History of Li-Fraumeni, Cowden, or hereditary diffuse gastric cancer syndrome, or a first-degree relative with a<br />
history of one of these syndromes<br />
• Breast screening magnetic resonance imaging (MRI): Covered annually, in addition to the annual screening mammogram,<br />
beginning at age 30 for women who have a 20 percent or greater lifetime risk of breast cancer (according to risk assessment<br />
tools based on family history such as the Gail model, the Claus model, and the Tyrer-Cuzick model), or who have any of the<br />
following risk factors:<br />
– Known BRCA1 or BRCA2 gene mutation<br />
– First-degree relative (parent, child, sibling) with a BRCA1 or BRCA2 gene mutation, and have not had genetic<br />
testing themselves<br />
– Radiation to the chest between ages 10 and 30<br />
– History of Li-Fraumeni, Cowden, or hereditary diffuse gastric cancer syndrome, or a first-degree relative with a<br />
history of one of these syndromes<br />
■<br />
Proctosigmoidoscopy or sigmoidoscopy:<br />
— Average Risk: Once every three to five years beginning at age 50.<br />
— Increased Risk: Once every five years beginning at age 40 for individuals with a first-degree relative diagnosed with a colorectal<br />
cancer or an adenomatous polyp at age 60 or older, or two second-degree relatives diagnosed with colorectal cancer.<br />
— High Risk: Annual flexible sigmoidoscopy, beginning at age 10–12, for individuals with known or suspected familial<br />
adenomatous polyposis.<br />
■ Prostate cancer: Perform a digital rectal exam and prostate-specific antigen screening annually for certain high-risk<br />
men ages 40–49 and all men over age 50.<br />
16
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Clinical Preventive Service: Coverage Details (continued)<br />
Service<br />
Cancer Screenings<br />
(continued)<br />
Description<br />
■ Routine Pap tests: Perform a Pap test annually for women starting at age 18 (younger if sexually active) or less often at<br />
patient and provider discretion (though not less than every three years). Human papillomavirus (HPV) DNA testing is covered<br />
as a cervical cancer screening only when performed in conjunction with a Pap test, and only for women age 30 and older.<br />
■ Skin cancer: Exams are covered at any age for a beneficiary who is at high risk due to family history or increased sun<br />
exposure.<br />
SECTIoN 2<br />
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
Benefits<br />
Cardiovascular<br />
Diseases<br />
■ Cholesterol test (non-fasting): Testing is covered for a lipid panel at least once every five years,<br />
beginning at age 18.<br />
■ Blood pressure screening: Screening is covered annually for children (ages 3–6) and a minimum of every<br />
two years after age 6 (children and adults).<br />
Eye Examinations ■ Well-child care coverage (infants and children up to age 6):<br />
— Infants (until reaching age 3): Conduct one eye and vision screening at birth and at 6 months.<br />
— Children (from age 3 until reaching age 6): Conduct a routine eye exam every two years. Active<br />
Duty Family Member (ADFM) children are covered for one routine eye exam annually.<br />
■ Adults and children (over age 6): Conduct a routine eye exam every two years. Active Duty Service<br />
Members (ADSM) and ADFMs receive one eye exam each year.<br />
■ Diabetic patients (any age): Eye exams are not limited. One eye exam per year is recommended.<br />
Note: ADSMs enrolled in <strong>TRICARE</strong> Prime must receive all vision care at military hospitals or clinics unless<br />
specifically referred by their primary care managers to civilian network providers, or to non-network providers if a<br />
network provider is not available. ADSMs enrolled in <strong>TRICARE</strong> <strong>Overseas</strong> <strong>Program</strong> Prime Remote may obtain periodic<br />
eye examinations from network providers without prior authorizations as needed to maintain fitness-for-duty status.<br />
Hearing<br />
Preventive hearing examinations are only allowed under the well-child care benefit. A newborn audiology<br />
screening should be performed on newborns before hospital discharge or within the first month after birth.<br />
Evaluative hearing tests may be performed at other ages during routine exams.<br />
Immunizations<br />
Infectious Disease<br />
Screening<br />
Patient and Parent<br />
Education<br />
Counseling<br />
School Physicals<br />
Well-Child Care<br />
(birth until reaching<br />
age 6)<br />
Age-appropriate doses of vaccines, including annual influenza vaccines, are covered as recommended by the<br />
Centers for Disease Control and Prevention (CDC).<br />
The HPV vaccine is a limited benefit and may be covered when the beneficiary has not been previously<br />
vaccinated or completed the vaccine series.<br />
—Females: The HPV vaccine Gardasil (HPV4) or Cervarix (HPV2) is covered for females ages 11–26. The<br />
series of injections must be completed prior to age 27 for coverage under <strong>TRICARE</strong>.<br />
— Males: The HPV vaccine Gardasil (HPV4) is covered for all males ages 11–21 and is covered for males<br />
ages 22–26 who meet certain criteria.<br />
A single dose of the shingles vaccine Zostavax ® is covered for beneficiaries age 60 and older.<br />
Coverage is effective the date the recommendations are published in the CDC’s Morbidity and Mortality Weekly<br />
Report. Refer to the CDC’s Web site at www.cdc.gov for a current schedule of recommended vaccines.<br />
Note: Immunizations for ADFMs whose sponsors have permanent change-of-station orders to overseas locations<br />
are also covered. Immunizations for personal overseas travel are not covered.<br />
<strong>TRICARE</strong> covers screening for infectious diseases, including hepatitis B, rubella antibodies and HIV, and<br />
screening and/or prophylaxis for tetanus, rabies, hepatitis A and B, meningococcal meningitis, and tuberculosis.<br />
Counseling services expected of good clinical practice that are included with the appropriate office visit are<br />
covered at no additional charge for dietary assessment and nutrition; physical activity and exercise; cancer<br />
surveillance; safe sexual practices; tobacco, alcohol, and substance abuse; dental health promotion; accident<br />
and injury prevention; stress; bereavement; and suicide risk assessment.<br />
Covered for children ages 5–11 if required in connection with school enrollment.<br />
Note: Annual sports physicals are not covered.<br />
Covers routine newborn care; comprehensive health promotion and disease prevention exams; vision and<br />
hearing screenings; height, weight, and head circumference measurement; routine immunizations; and<br />
developmental and behavioral appraisal. <strong>TRICARE</strong> covers well-child care in accordance with American<br />
Academy of Pediatrics (AAP) and CDC guidelines. Your child can receive preventive care well-child visits as<br />
frequently as the AAP recommends, but no more than nine visits in two years. Visits for diagnosis or treatment of<br />
an illness or injury are covered separately under outpatient care.<br />
17
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Behavioral Health Care Services: outpatient Coverage Details Figure 2.5<br />
Service<br />
outpatient Psychotherapy*<br />
(physician referral and supervision<br />
required when seeing licensed or<br />
certified mental health counselors<br />
and pastoral counselors)<br />
Description<br />
The following outpatient psychotherapy limits apply:<br />
■ Psychotherapy: Two sessions per week, in any combination of the following types:<br />
— Individual (adult or child): 60 minutes per session; may extend to 120 minutes for<br />
crisis intervention<br />
— Family or conjoint: 90 minutes per session; may extend to 180 minutes for crisis intervention<br />
— Group: 90 minutes per session<br />
■ Collateral visits Up to 60 minutes per visit (Collateral visits are counted as individual<br />
psychotherapy sessions. Beneficiaries have the option of combining collateral visits with<br />
other individual or group psychotherapy visits.)<br />
Psychoanalysis<br />
Psychological Testing and<br />
Assessment<br />
Psychoanalysis differs from psychotherapy and requires prior authorization. After prior authorization<br />
is obtained, treatment must be given by approved providers who are specifically trained in<br />
psychoanalysis.<br />
Testing and assessment is generally covered when medically or psychologically necessary and<br />
provided in conjunction with otherwise-covered psychotherapy. Psychological tests are considered<br />
to be diagnostic services and are not counted toward the limit of two psychotherapy visits per week.<br />
■ Limitations:<br />
— Testing and assessment is generally limited to six hours per fiscal year (FY 1 ). Any testing<br />
beyond six hours requires a review for medical necessity. Psychological testing must be<br />
medically necessary and not for educational purposes.<br />
■ Exclusions:<br />
Psychological testing is not covered for the following circumstances:<br />
• Academic placement<br />
• Job placement<br />
• Child-custody disputes<br />
• General screening in the absence of specific symptoms<br />
• Teacher or parental referrals<br />
• Testing to determine whether a beneficiary has a learning disability<br />
• Diagnosed, specific learning disorders or learning disabilities<br />
Medication Management<br />
If you are taking prescription medications for a behavioral health condition, you must be under the<br />
care of a provider who is authorized to prescribe those medications. Your provider will manage the<br />
dosage and duration of your prescription to ensure you are receiving the best care possible.<br />
Medication-management appointments are medical appointments and do not count against the first<br />
eight outpatient behavioral health care visits per FY. 1<br />
1<br />
For ADFM, the first 8 outpatient visits per FY 1 do not require authorization. For ADSM, authorization is required for all behavioral health care. Also, certain clinical<br />
preventive services do not require authorization when received from a Network <strong>Provider</strong>. If you are unsure about covered services, please contact International SOS and<br />
press option #5 to speak with a member of the TOP <strong>Provider</strong> Support Services staff.<br />
2<br />
October 1- September 30.<br />
18
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Behavioral Health Care Services: Inpatient Coverage Details<br />
Prior authorization is required for all nonemergency inpatient behavioral health care services. Psychiatric emergencies do not require<br />
prior authorization for inpatient admissions, but authorization is required for continued stay. Admissions resulting from psychiatric<br />
emergencies should be reported to the TOP contractor within 24 hours of admission or on the next business day, and must be reported<br />
within 72 hours of an admission. Authorization for continued stay is coordinated between the inpatient unit and the TOP contractor.<br />
Note: Active duty service members who receive care at military hospitals or clinics do not require prior authorization.<br />
Note: This figure is not all-inclusive and additional limitations on behavioral health care services may apply overseas.<br />
Figure 2.6<br />
SECTIoN 2<br />
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
Benefits<br />
Service<br />
Acute Inpatient Psychiatric Care<br />
Description<br />
May be covered on an emergency or nonemergency basis. Prior authorization from your regional<br />
contractor is required for all nonemergency inpatient admissions. In emergency situations,<br />
authorization is required for continued stay.<br />
■ Limitations:<br />
— Patients age 19 and older: 30 days per fiscal year (FY 1 ) or in any single admission<br />
— Patients age 18 and under: 45 days per FY 1 or in any single admission<br />
— Inpatient admissions for substance use disorder detoxification and rehabilitation<br />
count toward the 30- or 45-day limit for acute inpatient psychiatric care.<br />
(Limitations may be waived if determined to be medically or psychologically necessary.)<br />
Psychiatric Partial<br />
Hospitalization <strong>Program</strong> (PHP)<br />
Psychiatric PHPs are treatment settings capable of providing interdisciplinary therapeutic services at<br />
least three hours a day, five days a week, in any combination of day, evening, night, and weekend<br />
treatment programs. The following rules apply:<br />
— Prior authorization is required. PHP admissions are not considered emergencies.<br />
— Facilities must be <strong>TRICARE</strong>-authorized.<br />
— PHPs must have participation agreements with <strong>TRICARE</strong>.<br />
■ Limitations:<br />
— PHP care is limited to 60 treatment days (whether full- or partial-day treatment) per FY 1 .<br />
These 60 days are not offset by or counted toward the 30- or 45-day limit for acute inpatient<br />
psychiatric care.<br />
(Limitations may be waived if determined to be medically or psychologically necessary.)<br />
Residential Treatment Center<br />
(RTC) Care<br />
RTC care provides extended psychiatric care for children and adolescents with psychological<br />
disorders that require continued treatment in a therapeutic environment. The following rules apply:<br />
— Facilities must be <strong>TRICARE</strong>-authorized.<br />
— Unless therapeutically contraindicated, the family and/or guardian should actively participate<br />
in the continuing care of the patient through either direct involvement at the facility or<br />
geographically distant family therapy.<br />
— Prior authorization is always required. RTC admissions are not considered emergencies.<br />
— RTC care is considered elective and will not be covered for emergencies.<br />
— Admission primarily for substance use rehabilitation is not authorized for psychiatric RTC<br />
care. In an emergency, psychiatric inpatient hospitalization must be sought first.<br />
— Care must be recommended and directed by a psychiatrist or clinical psychologist.<br />
■ Limitations:<br />
— Care is limited to 150 days per FY 1 or for a single admission. (Limitations may be waived if<br />
determined to be medically or psychologically necessary.)<br />
— RTC care is only covered for patients until reaching age 21.<br />
— RTC care does not count toward the 30- or 45-day inpatient limit.<br />
1<br />
October 1- September 30.<br />
19
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Behavioral Health Care Services: Substance Use Disorder Services<br />
Figure 2.7 provides coverage details for covered substance use disorder services (up to three benefit periods per beneficiary, per lifetime).<br />
NoTE: This figure is not all-inclusive and additional limitations on substance use disorder services may apply overseas.<br />
Figure 2.7<br />
Service<br />
Inpatient Detoxification<br />
Description<br />
<strong>TRICARE</strong> covers emergency and inpatient hospital services for the treatment of the acute phases of<br />
substance use withdrawal (detoxification) when the patient’s condition requires the personnel and<br />
facilities of a hospital or substance use disorder rehabilitation facility (SUDRF).<br />
■ Limitations:<br />
— Diagnosis-related group-exempt facility, services are limited to seven days per episode.<br />
— Inpatient detoxification in a free-standing SUDRF counts toward the 30- or 45-day inpatient<br />
psychiatric care limit.<br />
SUDRF Rehabilitation<br />
Rehabilitation of a substance use disorder may occur in an inpatient (residential) or partial<br />
hospitalization setting. <strong>TRICARE</strong> covers 21 days of rehabilitation per benefit period in a <strong>TRICARE</strong>authorized<br />
facility, whether in an inpatient or partial hospitalization facility or a combination of both. 1<br />
■ Limitations:<br />
— 21-day rehabilitation limit per episode<br />
— Three episodes per lifetime<br />
— Days for inpatient rehabilitation count toward the 30- or 45-day limit for acute inpatient<br />
psychiatric care<br />
(Limitations may be waived if determined to be medically or psychologically necessary.)<br />
SUDRF outpatient Care Outpatient substance use care must be provided by an approved SUDRF.<br />
■ Limitations:<br />
— Individual or group therapy: Up to 60 visits per benefit period 1<br />
— Family therapy: Up to 15 visits per benefit period 1<br />
— Partial hospitalization program care: 21 treatment days per fiscal year 2<br />
(Limitations may be waived if determined to be medically or psychologically necessary.)<br />
1<br />
A benefit period begins with the first day of covered treatments and ends 365 days later. Stay limitations for inpatient services may be waived if determined<br />
to be medically or psychologically necessary.<br />
2<br />
October 1- September 30.<br />
ToP Prime and ToP Prime Remote<br />
Beneficiary Coverage Limitations<br />
The following is a list of medical, surgical and behavioral health<br />
care services that may not be covered unless exceptional<br />
circumstances exist. This list is not intended to be all-inclusive.<br />
Please visit www.tricare.mil for a full list of covered services,<br />
limitations and exclusions.<br />
20
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Services or Procedures with Significant Limitations Figure 2.8<br />
Service<br />
Botulinum Toxin Type A<br />
Injections<br />
Description<br />
Botulinum toxin type A injections for cosmetic procedures, myofascial pain, and fibromyalgia are not<br />
covered. Cost-sharing may apply for injections to treat severe primary axillary hyperhidrosis,<br />
dystonia-related blepharospasm or strabismus, cervical dystonia, cerebral palsy-related spasticity,<br />
or for the treatment of sialorrhea associated with Parkinson’s disease. Botulinum toxin type A<br />
injections may also be cost-shared for prophylaxis of headaches in adult patients with chronic<br />
migraines, which is defined as 15 days or more per month with headache lasting four hours a day or<br />
longer. <strong>TRICARE</strong> may also consider off-label cost-sharing for Botox ® injections used to treat chronic<br />
anal fissure (if unresponsive to conservative therapeutic measures).<br />
SECTIoN 2<br />
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
Benefits<br />
Breast Pumps<br />
Cardiac and Pulmonary<br />
Rehabilitation<br />
Cosmetic, Plastic or<br />
Reconstructive Surgery<br />
Cranial orthotic Device or<br />
Molding Helmet<br />
Dental Care and Dental X-rays<br />
Education and Training<br />
Eyeglasses or Contact Lenses<br />
Facility Charges for Non-<br />
Adjunctive Dental Services<br />
Food, Food Substitutes and<br />
Supplements, or Vitamins<br />
Heavy-duty, hospital-grade electric breast pumps (including services and supplies related to the use of<br />
the pump) for mothers of premature infants are covered. An electric breast pump is covered while<br />
the premature infant remains hospitalized during the immediate postpartum period. Hospital-grade<br />
electric breast pumps may also be covered after the premature infant is discharged from the<br />
hospital with a physician-documented medical reason. This documentation is also required for<br />
premature infants delivered in non-hospital settings. Breast pumps of any type, when used for<br />
reasons of personal convenience, are excluded even if prescribed by a physician.<br />
Both are covered only for certain indications. Phase III cardiac rehabilitation for lifetime maintenance<br />
performed at home or in medically unsupervised settings is excluded.<br />
Surgery is only covered when used to restore function, correct a serious birth defect, restore body<br />
form after a serious injury, improve appearance of a severe disfigurement after cancer surgery, or<br />
reconstruct the breast after cancer surgery.<br />
Cranial orthotic devices are excluded for treatment of nonsynostic positional plagiocephaly.<br />
Both are covered only for adjunctive dental care (i.e., dental care that is medically necessary in the<br />
treatment of an otherwise covered medical – not dental – condition). Prior authorization is required for<br />
adjunctive dental care.<br />
Education and training are covered under the <strong>TRICARE</strong> Extended Care Health Option (ECHO)<br />
and diabetic outpatient self-management training programs. Diabetic outpatient self-management<br />
training programs must be accredited by the American Diabetes Association ® . The provider’s<br />
accreditation must accompany the claim for reimbursement.<br />
Active duty service members may receive eyeglasses at a militray hospital or clinic at no cost. For all<br />
other beneficiaries, the following are covered:<br />
— Contact lenses and/or eyeglasses for treatment of infantile glaucoma<br />
— Corneal or scleral lenses for treatment of keratoconus<br />
— Scleral lenses to retain moisture when normal tearing is not present or is inadequate<br />
— Corneal or scleral lenses to reduce corneal irregularities other than astigmatism<br />
— Intraocular lenses, contact lenses, or eyeglasses for loss of human lens function resulting from<br />
intraocular surgery, ocular injury, or congenital absence<br />
Note: Adjustments, cleaning, and repairs for eyeglasses are not covered.<br />
Hospital and anesthesia charges related to routine dental care for children under age 5, or those<br />
with disabilities, may be covered in addition to dental care related to some medical conditions.<br />
Medically necessary nutrition formulas are covered when used as the primary source of nutrition for<br />
enteral, parenteral, or oral nutritional therapy. Intraperitoneal nutrition therapy is covered for<br />
malnutrition as a result of end-stage renal disease. Vitamins may be reimbursed when used as a<br />
specific treatment of a medical condition. Additionally, prenatal vitamins that require a prescription<br />
may be reimbursed for prenatal care only.<br />
21
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Services or Procedures with Significant Limitations (continued)<br />
Gastric Bypass<br />
Genetic Testing<br />
Hearing Aids<br />
Service<br />
Laser/LASIK/Refractive<br />
Corneal Surgery<br />
Private Hospital Rooms<br />
Shoes, Shoe Inserts, Shoe<br />
Modifications, and Arch<br />
Supports<br />
Description<br />
This procedure is covered for the treatment of morbid obesity under certain limited circumstances.<br />
Testing is covered when medically proven and appropriate, and when the results of the test will<br />
influence the medical management of the patient. Routine genetic testing is not covered.<br />
Hearing aids are covered only for active duty family members who meet specific hearing-loss<br />
requirements.<br />
Surgery is covered only to relieve astigmatism following a corneal transplant.<br />
Private rooms are not covered unless ordered for medical reasons or because a semi-private room is<br />
not available. Hospitals that are subject to the <strong>TRICARE</strong> diagnosis-related group (DRG) payment<br />
system may provide the patient with a private room but will receive only the standard DRG amount.<br />
The hospital may bill the patient for the extra charges if the patient requests a private room.<br />
Shoe and shoe inserts are covered only in very limited circumstances. Orthopedic shoes may be<br />
covered if they are a permanent part of a brace. For beneficiaries with diabetes, extra-depth shoes<br />
with inserts or custom-molded shoes with inserts may be covered.<br />
ToP Prime and ToP Prime Remote<br />
Beneficiary Coverage Exclusions<br />
In general, <strong>TRICARE</strong> excludes services and supplies that are not<br />
medically or psychologically necessary for the diagnosis or<br />
treatment of a covered illness (including behavorial health<br />
disorders), injury, or for the diagnosis and treatment of pregnancy<br />
or well-child care. All services and supplies (including inpatient<br />
institutional costs) related to a non-covered condition or<br />
treatment, or provided by an unauthorized <strong>Provider</strong>, are excluded.<br />
The following specific services are excluded under all<br />
circumstances. This list is not intended to be all-inclusive. Please<br />
visit www.tricare.mil for a full list of covered services, limitations<br />
and exclusions.<br />
■ Abortion (except in cases where the life of the mother would<br />
be endangered if the pregnancy were carried to term or when<br />
the pregnancy is the result of rape or incest)<br />
■ Acupuncture (may be offered at some military hospitals or<br />
clinics and approved for certain active duty service members,<br />
but is not covered for care received by civilian providers)<br />
■ Alterations to living spaces<br />
■ Artificial insemination, including in vitro fertilization, gamete<br />
intrafallopian transfer, and all other such reproductive<br />
technologies (except in very limited circumstances for some<br />
wounded, ill, or injured service members)<br />
■ Autopsy services or post-mortem examinations<br />
■ Birth control/contraceptives (non-prescription)<br />
■ Camps (e.g., for weight loss)<br />
■ Charges that providers may apply to missed or rescheduled<br />
appointments<br />
■ Counseling services that are not medically necessary in the<br />
treatment of a diagnosed medical condition (e.g., educational,<br />
vocational, and socioeconomic counseling; stress management;<br />
or lifestyle modification)<br />
■ Custodial care<br />
■ Diagnostic admissions<br />
■ Domiciliary care<br />
■ Dyslexia treatment<br />
■ Electrolysis<br />
■ Elevators or chair lifts<br />
■ Exercise equipment, spas, whirlpools, hot tubs, swimming<br />
pools, health club memberships, or other such charges or<br />
items<br />
■ Experimental or unproven procedures (unless authorized<br />
under specific exceptions in the <strong>TRICARE</strong> regulations)<br />
22
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
■ Foot care (routine), except if required as a result of a<br />
diagnosed, systemic medical disease affecting the lower limbs,<br />
such as severe diabetes<br />
■ General exercise programs, even if recommended by a<br />
physician and regardless of whether rendered by an authorized<br />
<strong>Provider</strong><br />
■ Inpatient stays:<br />
— For rest or rest cures<br />
— To control or detain a runaway child, whether or not<br />
admission is to an authorized institution<br />
— To perform diagnostic tests, examinations, and procedures<br />
that could have been and are performed routinely on an<br />
outpatient basis<br />
— In hospitals or other authorized institutions above the<br />
appropriate level required to provide necessary medical<br />
care<br />
■ Learning disability services<br />
■ Medications:<br />
— Drugs prescribed for cosmetic purposes<br />
— Fluoride preparations<br />
— Food supplements<br />
— Homeopathic and herbal preparations<br />
— Multivitamins<br />
— Over-the-counter products (except insulin and diabetic<br />
supplies)<br />
— Weight reduction products<br />
■ Megavitamins and orthomolecular psychiatric therapy<br />
■ Mind expansion and elective psychotherapy<br />
■ Naturopaths<br />
■ Non-surgical treatment of obesity or morbid obesity<br />
■ Personal, comfort, or convenience items, such as beauty and<br />
barber services, radio, television, and telephone<br />
■ Postpartum inpatient stay for a mother to stay with a newborn<br />
infant (usually primarily for the purpose of breast-feeding the<br />
infant) when the infant (but not the mother) requires the<br />
extended stay, or continued inpatient stay of a newborn infant<br />
primarily for purposes of remaining with the mother when the<br />
mother (but not the newborn infant) requires extended<br />
postpartum inpatient stay<br />
■ Preventive care, such as routine, annual, or employmentrequested<br />
physical examinations; routine screening<br />
procedures; or immunizations (except as provided under the<br />
clinical preventive services benefit. See “Clinical Preventive<br />
Services” earlier in this section.)<br />
■ Psychiatric treatment for sexual dysfunction<br />
■ Services and supplies:<br />
— Provided under a scientific or medical study, grant, or<br />
research program<br />
— Furnished or prescribed by an immediate family member<br />
— For which the beneficiary has no legal obligation to pay or<br />
for which no charge would be made if the beneficiary or<br />
sponsor were not <strong>TRICARE</strong>-eligible<br />
— Furnished without charge (i.e., cannot file claims for<br />
services provided free-of-charge)<br />
— For the treatment of obesity, such as diets, weight-loss<br />
counseling, weight-loss medications, wiring of the jaw, or<br />
similar procedures (See “Services or Procedures with<br />
Significant Limitations” earlier in this section.)<br />
■ Inpatient stays directed or agreed to by a court or other<br />
governmental agency (unless medically necessary)<br />
■ Required as a result of occupational disease or injury for which<br />
any benefits are payable under a worker’s compensation or<br />
similar law, whether such benefits have been applied for or paid<br />
(except if benefits provided under these laws have run out)<br />
■ That are (or are eligible to be) fully payable under another medical<br />
insurance or program, either private or governmental, such as<br />
coverage through employment or Medicare (in such instances,<br />
<strong>TRICARE</strong> is the last payer for any remaining charges)<br />
■ Sex changes or sexual inadequacy treatment (except for the<br />
treatment of ambiguous genitalia that has been documented<br />
to be present at birth)<br />
■ Sterilization reversal surgery<br />
■ Surgery performed primarily for psychological reasons (such as<br />
psychogenic surgery)<br />
■ Therapeutic absences from an inpatient facility (except when<br />
such absences are specifically included in a treatment plan<br />
approved by <strong>TRICARE</strong>)<br />
■ Transportation (except by ambulance)<br />
■ X-ray, laboratory, and pathological services and machine<br />
diagnostic tests not related to a specific illness or injury or a<br />
definitive set of symptoms (except for cancer-screening<br />
mammography, cancer screening, Pap tests, and other tests<br />
allowed under the clinical preventive services benefit)<br />
SECTIoN 2<br />
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
Benefits<br />
23
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
SECTIoN 3:<br />
International SoS Network <strong>Provider</strong>s and <strong>Provider</strong> Credentialing<br />
What is a Network <strong>Provider</strong>?<br />
Network <strong>Provider</strong>s are <strong>Provider</strong>s who have entered into a formal<br />
agreement with International SOS, have signed a Mutual<br />
Cooperation Protocol Agreement and supplied International SOS<br />
with their full credentials. Network <strong>Provider</strong>s have agreed to<br />
provide cashless, claimless services to TOP Prime and TOP<br />
Prime Remote beneficiaries, submit the appropriate Standard<br />
U.S. Claim Forms on behalf of the <strong>TRICARE</strong> beneficiaries they<br />
treat, and provide medical services in line with <strong>TRICARE</strong> policy.<br />
Network <strong>Provider</strong>s are added to International SOS’ database of<br />
<strong>Provider</strong>s and will always be our first choice when referring<br />
patients to the host nation network. Network <strong>Provider</strong>s will also be<br />
continually published on www.tricare-overseas.com, which can<br />
be accessed by all <strong>TRICARE</strong> beneficiaries.<br />
If a <strong>Provider</strong> wishes to participate in TOP, but does not wish to<br />
sign a Mutual Protocol Agreement with International SOS, they<br />
may agree to participate without the contract. These <strong>Provider</strong>s<br />
will still be required to provide cashless, claimless services to<br />
TOP Prime and TOP Prime Remote beneficiaries, submit the<br />
appropriate Standard U.S. Claim Forms on behalf of the<br />
beneficiaries they treat, and provide medical services in line with<br />
<strong>TRICARE</strong> policy. They will also be required to provide<br />
International SOS with their license. These <strong>Provider</strong>s will not be<br />
published on www.tricare-overseas.com.<br />
Becoming an International SoS<br />
Network <strong>Provider</strong><br />
Becoming an International SOS Network <strong>Provider</strong> benefits both<br />
Host Nation <strong>Provider</strong>s and TOP beneficiaries. When TOP Prime<br />
and TOP Prime Remote beneficiaries are referred for host nation<br />
care, they are referred to one of International SOS’ Network<br />
<strong>Provider</strong>s. Network <strong>Provider</strong>s are always International SOS’ first<br />
choice of <strong>Provider</strong>s.<br />
International SOS’ TOP <strong>Provider</strong> Support Services staff is<br />
available 24 hours a day, 365 days a year to assist Network<br />
<strong>Provider</strong>s.<br />
In turn, Network <strong>Provider</strong>s offer a number of benefits to <strong>TRICARE</strong><br />
patients:<br />
■ Patients feel confident that they are receiving quality care,<br />
because Network <strong>Provider</strong>s’ credentials have been reviewed.<br />
■ Beneficiaries are more comfortable, because their <strong>Provider</strong><br />
can directly or indirectly communicate with them in English.<br />
■ TOP Prime and TOP Prime Remote beneficiaries can receive<br />
cashless, claimless health care.<br />
How to Become an<br />
International SoS Network <strong>Provider</strong><br />
We encourage you to contact your International SOS TOP<br />
Regional Call Center and press option #5 to speak with a TOP<br />
<strong>Provider</strong> Support Services staff member on how to become a<br />
Network <strong>Provider</strong>. For a full list of phone numbers, see page 7<br />
of this TOP <strong>Provider</strong> <strong>Manual</strong> or visit www.tricare-overseas.com.<br />
Your Network Coordinator will provide you with all the information<br />
you need, along with a Mutual Cooperation Protocol Agreement<br />
between you and International SOS. Once you have reviewed the<br />
document, provided the required information (including your<br />
credentials), and both parties have signed the Mutual<br />
Cooperation Protocol Agreement, you may become an<br />
International SOS Network <strong>Provider</strong>.<br />
Examples of credentials include a copy of professional license,<br />
proof of malpractice insurance (where applicable), fee schedules<br />
and other information.<br />
Network <strong>Provider</strong> Responsibilities<br />
A detailed list of Network <strong>Provider</strong> responsibilities can be found in<br />
the International SOS Mutual Cooperation Protocol Agreement.<br />
Network <strong>Provider</strong>s are expected to follow the guidelines below:<br />
■ Do not discriminate based on sex, race, color, creed or<br />
religion.<br />
■ Communicate directly or indirectly with patients in English.<br />
■ Identify and assist <strong>TRICARE</strong> patients who seek emergency<br />
care and properly authorized routine and specialty care.<br />
24
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
■ Maintain health records for <strong>TRICARE</strong> beneficiaries and,<br />
whenever possible, make English-language summaries of<br />
these records available for inclusion in the beneficiaries’ U.S.<br />
military medical records.<br />
■ Promptly return consultation results to the referring Military<br />
Treatment Facility (MTF).<br />
Note: Routine consultation reports should be returned within 10<br />
working days, emergency consultation reports should be<br />
returned within 24 hours.<br />
Keeping Your <strong>Provider</strong> File Current<br />
International SOS’ TOP <strong>Provider</strong> Support Services staff is<br />
committed to keeping Network <strong>Provider</strong> files current and<br />
accurate. Reviewing this information on an annual basis helps<br />
prevent confusion and avoid problems.<br />
Listed below are events that will require a yearly update to your<br />
Network <strong>Provider</strong> file:<br />
■ The address from which you provide care changes.<br />
■ Your billing address or other billing information changes.<br />
■ Your phone, fax, email or other contact information changes.<br />
■ Your office hours change.<br />
■ Your credentials change or are renewed.<br />
In the case of these events, please contact your TOP Network<br />
Executive using the email addresses below, or you can refer to<br />
page 7 of this TOP <strong>Provider</strong> <strong>Manual</strong> for your TOP Regional Call<br />
Center numbers and select option #5.<br />
Europe, Middle East & Africa<br />
providerseurasiaafrica@internationalsos.com<br />
Network <strong>Provider</strong> Quality Mission<br />
International SOS is committed to delivering quality medical care<br />
to all beneficiaries living overseas. By becoming a Network<br />
<strong>Provider</strong>, you can be proud to know that you are part of this<br />
mission.<br />
International SOS works with you to understand how problems<br />
can be corrected or improved. We also work with you to develop<br />
a plan for avoiding quality- or service-related problems in the<br />
future.<br />
The Mutual Cooperation Protocol Agreement, together with our<br />
ongoing development and maintenance of the Network <strong>Provider</strong>s,<br />
helps International SOS ensure our quality performance.<br />
From time to time, you may be contacted by International SOS or<br />
<strong>TRICARE</strong> directly, to assess and monitor your overall satisfaction<br />
with TOP, including service, accessibility, <strong>Provider</strong> education and<br />
other topics.<br />
ToP <strong>Provider</strong> Support Services<br />
A dedicated team of administrators, nurses and quality staff<br />
dedicated to the <strong>TRICARE</strong> <strong>Overseas</strong> <strong>Program</strong> are available to<br />
assist you. The team is responsible for working with <strong>Provider</strong>s in<br />
their respective countries, building and maintaining relationships<br />
and answering questions in local languages about TOP covered<br />
services, authorizations and submitting claims for payment.<br />
SECTIoN 3<br />
International SoS Network<br />
<strong>Provider</strong>s & <strong>Provider</strong> Credentialing<br />
Latin America and Canada<br />
providerslatinamerica@internationalsos.com<br />
Puerto Rico<br />
provider.inquiries.PR@internationalsos.com<br />
Asia-Pacific<br />
providersasiapacific@internationalsos.com<br />
25
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Access to Care<br />
International SOS is committed to ensuring that TOP beneficiaries<br />
have access to quality care with suitable wait times and other<br />
standards of service delivery. Below is an overview of these<br />
standards and guidelines, as established by <strong>TRICARE</strong> policy.<br />
Element<br />
Wait Time for an<br />
Appointment<br />
office Waiting<br />
Times<br />
ToP Access to Care Standards<br />
Definition<br />
When a <strong>TRICARE</strong><br />
beneficiary contacts you<br />
to make an appointment,<br />
you are expected to follow<br />
the guidelines below for<br />
seeing the patient:<br />
— Well-patient Visit or<br />
Specialty Care Referral:<br />
4 weeks<br />
— Routine Visit: 1 week<br />
— Urgent Care: 24 hours<br />
When a <strong>TRICARE</strong><br />
beneficiary comes in for<br />
their appointment, the<br />
office waiting time to see<br />
their clinician can be no<br />
more than 30 minutes –<br />
unless the clinician’s<br />
schedule is disrupted<br />
because of a medical<br />
emergency.<br />
Service<br />
Standard<br />
Well-patient:<br />
4 weeks<br />
Routine:<br />
1 week<br />
Urgent:<br />
24 hours<br />
No more than<br />
30 minutes<br />
<strong>Provider</strong> Credentialing Process<br />
With 25 years of experience in international health care and<br />
medical assistance services, and operations in 70+ countries,<br />
International SOS understands that health care delivery differs<br />
significantly from country to country.<br />
Factors such as local country legislation and regulations are<br />
considered, as well as existing health care infrastructure and any<br />
unique challenges that may impact the delivery of care in a<br />
specific region.<br />
International SOS takes these differences into account, when<br />
reviewing <strong>Provider</strong> capabilities and determining eligibility to<br />
participate in TOP. Country-specific credentialing guidelines are<br />
used and we work with host nation licensing agencies, to<br />
maintain accurate and up-to-date information about local<br />
standards.<br />
<strong>Provider</strong> performance is monitored on an ongoing basis so that<br />
potential problems can be addressed before they impact<br />
beneficiary satisfaction and quality of care. <strong>Provider</strong> satisfaction<br />
surveys are also used to monitor your overall satisfaction with<br />
International SOS, including how accessible or helpful our call<br />
center and TOP <strong>Provider</strong> Support Services staff is in assisting<br />
with claims processing, <strong>Provider</strong> education, and other topics.<br />
The following credentialing items are required to become an<br />
International SOS Network <strong>Provider</strong>:<br />
Availability of<br />
Emergency<br />
Services<br />
<strong>Provider</strong>s of emergency<br />
care services are<br />
expected to be available<br />
24 hours a day, 7 days a<br />
week. Emergency care<br />
<strong>Provider</strong>s are selected<br />
based on their abililty to<br />
meet this requirment. If<br />
your availability changes,<br />
you must notify us<br />
immediately.<br />
24 hours a<br />
day /<br />
7 days a week<br />
Note: If you have any questions or concerns about your ability to<br />
meet these standards and guidelines, please contact<br />
International SOS.<br />
26
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Criteria<br />
Signed <strong>Provider</strong> Agreement<br />
Meet the Standards for<br />
Authorization<br />
Standards<br />
An International SOS <strong>Provider</strong> Agreement (Mutual Cooperation Protocol) must be signed, in order to<br />
become a Network <strong>Provider</strong>.<br />
All health care services for TOP Prime and TOP Prime Remote beneficiaries are provided on an<br />
authorized basis. You will be expected to accept International SOS’ authorization for services, and<br />
agree to submit claims and invoices for payment to International SOS, through our subcontractor<br />
Wisconsin Physicians Service (WPS). You agree not to balance bill a TOP Prime or TOP Prime<br />
Remote beneficiary for uncovered services.<br />
Valid Malpractice Insurance<br />
(If Applicable)<br />
Licensure/Registration<br />
Evidence of Professional<br />
Qualifications and Experience<br />
You must have professional liability insurance, if this is required by the laws of your respective host<br />
nation. If you are a country, state, province, etc., entity <strong>Provider</strong>, and you are self-insured, then you<br />
are not required to have malpractice insurance.<br />
You must meet the requirements for licensure/registration as specified by your local governmental<br />
authority or licensing board. This includes having a valid license or registration in the host nation<br />
where you practice.<br />
You must be a graduate of an accredited program in health care sciences. This includes completing<br />
a certificate (residency) program, leading to certification in general medicine, family practice,<br />
gynecology, pediatrics, dentistry or other disciplines/specialties recognized by the applicable<br />
certifying agency in your country.<br />
SECTIoN 3<br />
International SoS Network<br />
<strong>Provider</strong>s & <strong>Provider</strong> Credentialing<br />
English Language Proficiency<br />
You must be able to proficiently communicate in English (both verbally and in writing), or to provide<br />
English translation and interpretation services at the time of service.<br />
Beneficiary Access to ToP<br />
Network <strong>Provider</strong>s<br />
All Host Nation <strong>Provider</strong>s with a signed Mutual Cooperation<br />
Protocol Agreement and approved credentials on file with<br />
International SOS will be published on www.tricareoverseas.com<br />
and displayed for beneficiaries.<br />
The published list of Network <strong>Provider</strong>s is matched with<br />
International SOS’ internal database, so it is important that you<br />
keep all of your information up-to-date.<br />
<strong>TRICARE</strong> beneficiaries using the www.tricare-overseas.com<br />
website have the comfort of knowing that listed <strong>Provider</strong>s are<br />
“quality assured” and recommended for care locally. Detailed<br />
information about referrals and authorizations is also included on<br />
this website, making <strong>Provider</strong> selection easier and more<br />
convenient for beneficiaries.<br />
Note: If you would not like your <strong>Provider</strong> information published,<br />
please contact your TOP Regional Call Center and select option<br />
#5 to speak with a member of the TOP <strong>Provider</strong> Support Services<br />
staff.<br />
27
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
SECTIoN 4:<br />
Authorizations and Seeing <strong>TRICARE</strong> Patients<br />
Effective September 1, 2010, <strong>Provider</strong>s will receive authorization<br />
from International SOS before providing care to TOP Prime and<br />
TOP Prime Remote beneficiaries.<br />
Prior authorization is required for certain procedures and inpatient<br />
hospital admissions, including patient rehabilitation and skilled<br />
nursing facilities. Authorizations are based on medical necessity and<br />
are not a guarantee of payment.<br />
This section explains the authorization process and what you can<br />
expect when seeing <strong>TRICARE</strong> patients.<br />
How Are Patients Referred to You?<br />
ToP Prime and ToP Prime Remote<br />
Beneficiaries<br />
TOP Prime and TOP Prime Remote beneficiaries should first visit<br />
their Primary Care Manager when seeking medical care.<br />
ToP Prime Beneficiaries:<br />
For TOP Prime beneficiaries, the Primary Care Manager is<br />
typically based at a Military Treatment Facility (MTF). If the MTF<br />
does not have the capability to provide the necessary care, they<br />
will refer the beneficiary to a Host Nation <strong>Provider</strong>.<br />
ToP Prime Remote Beneficiaries:<br />
International SOS acts as the Primary Care Manager for TOP<br />
Prime Remote beneficiaries and can authorize and refer these<br />
beneficiaries to Host Nation <strong>Provider</strong>s for primary and secondary<br />
care. Host Nation <strong>Provider</strong>s receive authorization directly from<br />
International SOS, to ensure that the services are covered. The<br />
authorization will be sent to the Network <strong>Provider</strong> via fax or secure<br />
email. The beneficiary will also be informed when the<br />
authorization has been sent.<br />
TOP Prime and TOP Prime Remote beneficiaries may only receive<br />
care from a Network <strong>Provider</strong>. After the authorization has been<br />
issued, the beneficiary may contact the Network <strong>Provider</strong> directly<br />
to schedule an appointment.<br />
ToP Standard Beneficiaries<br />
TOP Standard beneficiaries may seek care from any <strong>Provider</strong><br />
they prefer. They are required to pay and claim for any medical<br />
care they receive from a Host Nation <strong>Provider</strong>.<br />
Standard beneficiaries often prefer to seek care from a TOP<br />
Network <strong>Provider</strong>, because of the guaranteed quality of care they<br />
will receive. Host Nation <strong>Provider</strong>s may offer to file a claim on<br />
behalf of the TOP Standard beneficiary and bill them for the<br />
balance owed. However, you are not required/obligated to do<br />
this.<br />
Additional information about submitting claims can be found in<br />
Section 5 of this TOP <strong>Provider</strong> <strong>Manual</strong> as well as online at<br />
www.tricare-overseas.com.<br />
Note: TOP Prime and TOP Prime Remote beneficiaries may<br />
come to your office without an Authorization Form. If a <strong>TRICARE</strong><br />
beneficiary requests non-emergent health care at your facility<br />
without prior <strong>TRICARE</strong> authorization, the claims submitted for<br />
these services may be denied.<br />
Determining Patient Eligibility for<br />
Authorized Care<br />
You will receive an Authorization Form for TOP Prime and TOP<br />
Prime Remote beneficiaries that are eligible for cashless,<br />
claimless care under TOP. The authorization will state ‘<strong>TRICARE</strong><br />
Authorization Form’ in the title and specify whether the<br />
authorization is for a TOP Prime or TOP Prime Remote<br />
beneficiary. It will also specify what type of care is being<br />
authorized.<br />
Before an Authorization Form is issued, International SOS will<br />
verify the patient’s eligibility to receive care from your facility.<br />
The Authorization Form will have a unique identification number<br />
(Authorization Number), which will be located on the top right<br />
section of the form.<br />
The Authorization Form will indicate the name and address of<br />
your facility, and will also contain the first name, surname and<br />
date of birth of the patient eligible for care.<br />
28
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
To confirm a <strong>TRICARE</strong> beneficiary’s eligibility, <strong>Provider</strong>s should<br />
ask to see both of the following:<br />
■ TOP Prime Enrollment Card and<br />
■ U.S. Military ID or CAC<br />
It is important to verify that the name on both cards matches<br />
exactly, and that the photo on the U.S. Military ID Card or CAC<br />
accurately represents the patient.<br />
<strong>Provider</strong>s should also check:<br />
■ The expiration date on the U.S. Military ID Card or CAC<br />
(to ensure that coverage is still valid)<br />
■ The sponsor’s Social Security Number (this will always be<br />
in the same format: XXX-XX-XXXX) or the Department of<br />
Defense (DOD) Benefits Number (this can be found above the<br />
bar code on the back of the beneficiary’s ID card and will be<br />
in the following format: XXXXXXXXX-XX). Only the first 9 digits<br />
of the DOD Benefits Number will be needed for the <strong>Provider</strong> to<br />
verify eligibility.<br />
You can also call your International SOS TOP Regional Call<br />
Center for assistance, if you are unsure.<br />
Note: International SOS will only issue a <strong>TRICARE</strong> Authorization<br />
Form for TOP Standard beneficiaries for the following types of<br />
medical care, which do require prior authorization:<br />
■ Adjunctive Dental Services<br />
■ Home Health Services<br />
■ Hospice Care<br />
■ Non-emergency Inpatient Admissions for Substance Use<br />
Disorders or Behavioral Health Care<br />
■ Outpatient Behavioral Health Care Visits Beyond 8th Visit per<br />
Fiscal Year (10/1-9/30)<br />
■ Transplants (all solid organ and stem cell)<br />
The <strong>TRICARE</strong> Standard Authorization Form will be issued to the<br />
MTF and the TOP Standard beneficiary. The TOP Standard<br />
beneficiary may give this to the <strong>Provider</strong> when they seek medical<br />
care.<br />
TOP Standard coverage is available to the family members of<br />
Active Duty Service Members (ADSM) living and working<br />
overseas. TOP Standard enrolled beneficiaries manage their own<br />
health care and also have the freedom to choose any Host Nation<br />
<strong>Provider</strong> they wish to see.<br />
TOP Standard beneficiaries receive reimbursable health care,<br />
after meeting their annual deductible payment and cost-sharing<br />
obligations. This means that the beneficiary will pay the first<br />
portion of costs toward health care services received each year<br />
(the annual deductible). After this portion is paid, the beneficiary<br />
is responsible to pay a certain percentage of each medical bill<br />
they receive – TOP Standard beneficiaries who are Active Duty<br />
Family Members (ADFM) pay 20% of the total cost and Retirees<br />
29<br />
pay 25% of the total cost. Once the beneficiary has contributed<br />
over a determined limit (i.e., they reach their catastrophic cap),<br />
<strong>TRICARE</strong> will pay all medical costs for the remainder of the<br />
financial year.<br />
TOP Standard beneficiaries will not be issued a <strong>TRICARE</strong><br />
Enrollment Card. They will only have a Military ID Card. As a Host<br />
Nation <strong>Provider</strong> under TOP, your commitment is to provide<br />
cashless, claimless services to TOP Prime and TOP Prime<br />
Remote beneficiaries only. You are not obligated to provide<br />
similar services to TOP Standard beneficiaries.<br />
Depending on your location, you may experience a large number<br />
of TOP Standard beneficiaries living and working in your region.<br />
If you decide to provide services to these beneficiaries, you may<br />
do so in one of the following two ways:<br />
■ Request TOP Standard beneficiaries to pay the cost of<br />
treatment upfront. This means the TOP Standard beneficiary<br />
will be personally responsible for claiming reimbursement from<br />
<strong>TRICARE</strong>.<br />
■ File the claim on behalf of the TOP Standard beneficiary (using<br />
the CMS 1500 for Non-Institutional <strong>Provider</strong>s or UB-04 Claim<br />
Form for Institutional <strong>Provider</strong>s) and bill the patient directly for<br />
the patient responsibility amount.<br />
Note: <strong>Provider</strong>s should be prepared to collect required<br />
beneficiary cost shares at the time of service delivery. The<br />
most up-to-date beneficiary cost-share information can be<br />
found online at www.tricare.mil. <strong>Provider</strong>s registered to the<br />
<strong>Provider</strong> Portal can also check patient eligibility on<br />
www.tricare-overseas.com by entering the sponsor’s Social<br />
Security Number or DOD Benefits Number, and date of<br />
service. Additional information on understanding the <strong>Provider</strong><br />
Portal can be found in Section 6 of this TOP <strong>Provider</strong> <strong>Manual</strong>.<br />
Based on your location, you may see TOP Prime, TOP Prime<br />
Remote and TOP Standard beneficiaries. TOP Standard<br />
beneficiaries are required to pay upfront and submit their<br />
claims for reimbursement. As a <strong>TRICARE</strong> <strong>Overseas</strong> <strong>Provider</strong>,<br />
you are not required to file claims on behalf of TOP Standard<br />
beneficiaries. If you would like to offer this service, you are<br />
responsible for ensuring that any cost shares or deductibles<br />
are collected from the TOP Standard beneficiary by your<br />
facility.<br />
Note: When submitting claims on behalf of TOP Standard<br />
beneficiaries, <strong>Provider</strong>s must invoice for the full amount<br />
charged. If the <strong>Provider</strong> submits an invoice for only the<br />
balance (after the TOP Standard beneficiary has paid their<br />
deductible and cost share), International SOS will apply the<br />
deductible and cost share to the balance, as required by<br />
<strong>TRICARE</strong> policy. Therefore, International SOS will need the<br />
Itemized Invoice to reflect the full cost of medical care<br />
(i.e., the total invoiced amount).<br />
Please visit www.tricare-overseas.com for additional information<br />
about how to handle TOP Standard claims for reimbursement.<br />
SECTIoN 4<br />
Authorizations and Seeing<br />
<strong>TRICARE</strong> Patients
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Authorization Forms<br />
International SOS will send an Authorization Form to you and the<br />
referring MTF along with a pre-populated Claim Form (see<br />
Section 5).<br />
The Authorization Form will include your contact information (as<br />
the Network <strong>Provider</strong>), the patient’s name, date of birth, and<br />
instructions regarding the scope and validity of the authorization.<br />
The Authorization Form will also include the name of the MTF<br />
referring the care.<br />
A sample <strong>TRICARE</strong> Authorization Form is included on the<br />
following page, as well as in Section 7 of this TOP <strong>Provider</strong><br />
<strong>Manual</strong>.<br />
A specific Authorization Form will be issued depending on<br />
whether a beneficiary is a TOP Prime or TOP Prime Remote<br />
patient. Authorization Forms will also vary depending on whether<br />
the beneficiary is receiving inpatient or outpatient care.<br />
A separate Authorization Form will be needed for TOP Prime<br />
Remote ADSM before receiving dental care.<br />
Below is a brief description about the fields you will find on an<br />
International SOS Authorization Form. You will need this<br />
information before delivering health care services.<br />
■ Priority Care — this will either state ‘Urgent’ or ‘Routine’<br />
— Urgent: An appointment must be provided within 24 hours<br />
of the beneficiary’s request for care.<br />
Note: For urgent care, medical results and any consult notes<br />
must be sent to the referring party, either the MTF or<br />
International SOS, within 24 hours.<br />
The referring party’s contact details are indicated on the<br />
Authorization Form.<br />
— Routine: An appointment must be provided within 1 week<br />
of the beneficiary’s request for routine care and within<br />
4 weeks of the beneficiary’s request for specialty care.<br />
Note: For routine care, medical results and any consult<br />
notes must be sent to the referring party, either the MTF,<br />
the assigned Primary Care Manager (in Puerto Rico) or<br />
International SOS, within 10 days.<br />
■ Specialty required<br />
■ Preliminary diagnosis from referring physician<br />
■ Scope of care – this will either state ‘Evaluate’ or<br />
‘Evaluate and Treat’<br />
— Evaluate: You are authorized to evaluate only, using<br />
diagnostic tools such as laboratory tests, consultation,<br />
X-rays (to determine appropriate treatment).<br />
— Evaluate and Treat: You are authorized to both evaluate<br />
and treat the patient. A separate Authorization Form will be<br />
provided for surgical procedures and inpatient care, if<br />
admission is required as part of the treatment. Please notify<br />
the MTF or International SOS if this is the case.<br />
■ Detailed Instructions<br />
■ Inclusions<br />
Note: If you have any questions about the medical care that is<br />
being authorized, please call International SOS before delivering<br />
service.<br />
Note: The authorization will indicate how long it is valid.<br />
Authorizations are typically valid for 90 days. If your treatment<br />
dates exceed the time the Authorization Form is valid, please<br />
contact International SOS or your local MTF to obtain a new<br />
Authorization Form.<br />
Note: To access the full terms and conditions of the Authorization<br />
Form, please visit www.tricare-overseas.com. You may also<br />
contact your International SOS TOP Regional Call Center and<br />
press option #5 to request a copy of the terms and conditions.<br />
30
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
<strong>TRICARE</strong> AUTHORIZATION FORM<br />
FOR OUTPATIENT CARE<br />
<strong>TRICARE</strong> PRIME BENEFICIARY<br />
To:<br />
<br />
<br />
<br />
<br />
Tel: <br />
Fax: <br />
Authorization Number: <br />
Date: 14 April 2010<br />
Pages: 1<br />
SERVICE(S) REQUEST IN RESPECT OF:<br />
<br />
This is to confirm the Authorization for the above patient at for outpatient care. This Authorization is only valid<br />
between and .<br />
Priority<br />
Specialty<br />
Preliminary Diagnosis<br />
Number of Visits<br />
Scope<br />
Instructions:<br />
<br />
<br />
As per referral<br />
<br />
<br />
<br />
<br />
Inclusions:<br />
Further to medical information received, International SOS authorizes all reasonable, customary and necessary medical expenses<br />
within the scope of the approved authorization.<br />
Medical Reports:<br />
Please send a written medical report and discharge summary to the below addressee after this patient’s episode of care /<br />
procedure. Please follow any special arrangements you may have between you and the Military Treatment Facility (MTF).<br />
, Fax: <br />
<br />
SECTIoN 4<br />
Authorizations and Seeing<br />
<strong>TRICARE</strong> Patients<br />
Priority:<br />
For urgent medical appointments please return a copy of medical results within 24 hours.<br />
For routine appointments please return a copy of medical results within 10 calendar days.<br />
Important:<br />
An authorization is issued for requested services, procedures, or admissions that require medical necessity review prior to services<br />
being rendered. The terms of this Authorization are only applicable to the specific service provider indicated above and to this<br />
instance of service requested.<br />
Billing Instructions:<br />
If the Beneficiary has "other" healthcare coverage in addition to <strong>TRICARE</strong>, the "other" healthcare coverage is the Primary Insurer.<br />
All invoices must reach us within 12 calendar months from date of service to avoid denial of settlement. An itemized invoice<br />
accompanied with a duly completed Claim Form and a copy of this Authorization Form is to be sent to the following address. :<br />
<br />
<br />
For full terms and conditions of this Authorization Form, please refer to www.tricare-overseas.com . Alternatively, you may contact<br />
our office for a copy of the terms and conditions.<br />
Yours sincerely<br />
<br />
<strong>TRICARE</strong> Department<br />
31
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Authorization Forms (continued)<br />
Authorizations for Cases of Pregnancy<br />
All care related to pregnancy and childbirth is covered by one<br />
referral from the MTF. Authorization Forms will be issued to for<br />
365 days to the OB/GYN or Medical Practitioner covering care. If<br />
any pregnancy and childbirth care (e.g., ultrasound scans) is to<br />
be conducted by other <strong>Provider</strong>s, additonal Authorization Forms<br />
may be requested. The beneficiary or <strong>Provider</strong> should contact<br />
International SOS directly to request additional Authorization<br />
Forms.<br />
Patient Records and Privacy<br />
International SOS Network <strong>Provider</strong>s must maintain medical<br />
health records for all <strong>TRICARE</strong> beneficiaries they treat. These<br />
records should be protected as stipulated by an addendum to<br />
the Mutual Cooperation Protocol.<br />
When possible, Network <strong>Provider</strong>s should provide English<br />
language summaries of their records for inclusion in the patient’s<br />
U.S. military medical records. If you have any questions or need<br />
assistance in maintaining these records, please contact your TOP<br />
Regional Call Center or International SOS.<br />
Emergency Assistance Treatment and Authorizations and<br />
Payment<br />
If a TOP Prime or TOP Prime Remote beneficiary is unable to<br />
contact International SOS before receiving emergency care, then<br />
no Authorization Form or Authorization Number will be issued.<br />
The medical services rendered will be authorized retrospectively.<br />
Authorization Forms are not required to treat beneficiaries for<br />
Emergency Care. However, the words ‘Emergency Care’ or<br />
‘Emergency Room’ must be written on the Claim Form or Itemized<br />
Invoice so that these claims are processed without an<br />
Authorization Number. Please refer to the TOP <strong>Provider</strong><br />
Emergency Care brief available at www.tricare-overseas.com<br />
for more information on how to receive retrospective authorization<br />
and submit your Emergency Care claims on behalf of TOP Prime<br />
or TOP Prime Remote beneficiaries.<br />
Clear and Legible Reporting: Issuing a Medical Report<br />
Following Patient Care<br />
After providing care to a <strong>TRICARE</strong> beneficiary, please send a<br />
medical report of your findings and/or treatment to the referring<br />
party. The Authorization Form will clearly indicate whether this<br />
should be returned to your local MTF (for TOP Prime<br />
beneficiaries) or International SOS (for TOP Prime Remote<br />
beneficiaries).<br />
Cultural Differences and Host<br />
Nation Patient Liaisons<br />
Health care delivery in the United States may vary from local<br />
overseas practices. Language is the most obvious and<br />
challenging difference. Even if your English language skills are<br />
considered strong, it is important that any care instructions are<br />
clear and fully understood by the patient. You should be aware,<br />
language differences may discourage some patients from asking<br />
questions when they don’t understand.<br />
U.S. patients may have a high degree of modesty and find<br />
cultural differences in personal privacy to be uncomfortable,<br />
particularly in the hospital setting. Curtains or privacy screens are<br />
expected in hospital rooms and examination rooms in the U.S.,<br />
and U.S. patients may find it very difficult to undress (to any<br />
degree) without them.<br />
To help make care more comfortable for <strong>TRICARE</strong> beneficiaries,<br />
most MTFs use one or more host nation patient liaisons. These<br />
liaisons are fluent in English as well as the local language, and<br />
are familiar with how the host nation health care system works.<br />
Their primary role is to assist U.S. patients in a hospital setting.<br />
They may also be used to assist with particularly difficult<br />
outpatient situations.<br />
You may already have an existing relationship with your local host<br />
nation patient liaison. You can be assured that this relationship<br />
will not be interrupted or changed in any way with TOP.<br />
32
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
SECTIoN 5:<br />
<strong>Provider</strong> Claims Information<br />
As a TOP Host Nation <strong>Provider</strong>, you will be able to choose one of<br />
four methods for submitting your claims. A Standard U.S. Claim<br />
Form is required when submitting <strong>TRICARE</strong> claims for<br />
reimbursement.<br />
International SOS has designed its systems to support you with<br />
this process, by generating a partially completed Claim Form.<br />
You will receive this partially completed Claim Form with each<br />
authorization issued. This Claim Form must be submitted with an<br />
Itemized Invoice for services rendered.<br />
All Host Nation <strong>Provider</strong>s will be required to submit a Standard<br />
U.S. Claim Form along with the invoice for reimbursement:<br />
■ Non-Institutional <strong>Provider</strong>s will be required to submit a CMS<br />
1500 Claim Form (see Section 7)<br />
■ Institutional <strong>Provider</strong>s (e.g., hospitals) will be required to<br />
submit a UB-04 Claim Form (see Section 7)<br />
International SOS’ TOP <strong>Provider</strong> Support Services staff will work<br />
with you to show you how to complete the Claim Form properly.<br />
Detailed step-by-step instructions and tools are available, to<br />
help simplify the process of filling out and submitting<br />
Claim Forms.<br />
Process for Submitting Claims<br />
You can submit your claim using any of the following four<br />
methods:<br />
1.) online Claim Submission: This is the preferred method for<br />
claims submission, as it significantly reduces the amount of<br />
time it takes for a claim to be received by our TOP Claims<br />
Processing Department and therefore can result in faster<br />
payments. <strong>Provider</strong>s do not need to complete a paper Claim<br />
Form or produce an Itemized Invoice when using the Online<br />
Claim Submission method. After submitting your claim<br />
electronically, it can be tracked within 12 business hours.<br />
Note: A signed Electronic Data Interchange (EDI) Form must<br />
be submitted to International SOS before your claims can be<br />
submitted using the Online Claim Submission method.<br />
2.) Secure Message Transmission: This claims submission<br />
method allows <strong>Provider</strong>s to upload and send their claims and<br />
invoices via a Secure Messaging System. Claim Forms<br />
submitted using Secure Message Transmission can be<br />
tracked within 15 days of receipt. <strong>Provider</strong>s must still complete<br />
the appropriate paper Claim Form and produce an Itemized<br />
Invoice when using this method of submission.<br />
3.) Fax: This method should be used if the <strong>Provider</strong> does not<br />
have an Internet connection. This method will only work if the<br />
fax transmission is legible. Quality can be impacted by fax<br />
transmission and phone line connection. This method is also<br />
subject to overseas toll charges.<br />
Note: Fax submission is still faster than overseas mail.<br />
4.) overseas Mail: This method should be used only when the<br />
other three claims submission methods (above) are not<br />
available. Depending on where the <strong>Provider</strong> is located, using<br />
overseas mail can significantly increase the amount of time it<br />
takes for claims to be received by our TOP Claims Processor<br />
and therefore can result in delayed payment.<br />
The following table details the benefits of each claims submission<br />
method:<br />
Benefits of Each Claims Submission Method<br />
Preference Submission<br />
Method<br />
#1<br />
#2<br />
Online<br />
Claim<br />
Submission<br />
Secure<br />
Message<br />
Transmission<br />
#3 Fax<br />
#4<br />
<strong>Overseas</strong><br />
Mail<br />
Internet<br />
Connection Cost Speed Tracking<br />
Claims<br />
Required<br />
Required<br />
Not<br />
Required<br />
Not<br />
Required<br />
None<br />
None<br />
$$<br />
$<br />
Received<br />
immediately<br />
Received<br />
immediately<br />
Received<br />
immediately<br />
Time it takes<br />
for claims to<br />
arrive depends<br />
on <strong>Provider</strong>’s<br />
location<br />
Within<br />
12<br />
business<br />
hours<br />
of<br />
receipt<br />
Within<br />
15 days<br />
of<br />
receipt<br />
Within<br />
15 days<br />
of<br />
receipt<br />
Within<br />
15 days<br />
of<br />
receipt<br />
SECTIoN 5<br />
<strong>Provider</strong> Claims Information<br />
33
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Mail<br />
You can submit a Claim Form, along with the Itemized Invoice,<br />
by mail. Claim Forms and invoices can be sent in any language,<br />
in any currency. If you receive an Authorization Form from<br />
International SOS, the proper mailing address will be included<br />
on this form.<br />
For Active Duty Service Members (ADSM), all completed paper<br />
Claim Forms and Itemized Invoices can be mailed to:<br />
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
P.O. BOX 7968<br />
Madison, Wisconsin 53707-7968<br />
USA<br />
For all other beneficiaries in the Eurasia-Africa Region, all<br />
completed paper Claim Forms and Itemized Invoices can be<br />
mailed to:<br />
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
P.O. BOX 8976<br />
Madison, Wisconsin 53708-8976<br />
USA<br />
For all other beneficiaries in the Pacific Region and Latin America<br />
Region, all completed paper Claim Forms and Itemized Invoices<br />
can be mailed to:<br />
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
P.O. BOX 7985<br />
Madison, Wisconsin 53707-7985<br />
USA<br />
Web-based Claims Submission<br />
options<br />
There are two Web-based claims submission options available –<br />
Online Claim Submission and Secure Message Transmission.<br />
To use either of these options, you will need to register on the<br />
<strong>Provider</strong> Portal online at www.tricare-overseas.com to obtain a<br />
username and password. Additional information about how to<br />
register and use the <strong>Provider</strong> Portal can be found in Section 6<br />
(page 69) of this TOP <strong>Provider</strong> <strong>Manual</strong>.<br />
Note: <strong>Provider</strong>s who do not have Internet access will need to<br />
submit their claims via overseas fax or overseas mail.<br />
Secure Message Transmission<br />
The first web-based option is Secure Message Transmission.<br />
Once you become a registered <strong>Provider</strong> on the<br />
www.tricare-overseas.com portal, you can upload a scanned<br />
copy of the completed paper Claim Form and Itemized Invoice.<br />
Below is the screen that will appear when you log onto<br />
www.tricare-overseas.com.<br />
Click here to submit<br />
claims using Secure<br />
Message Transmission.<br />
Note: Due to the lead time involved with overseas mail,<br />
submitting your claims via overseas mail may result in delayed<br />
payment.<br />
Fax<br />
Claim Forms and invoices can be faxed in any language, in any<br />
currency.<br />
You can submit a Claim Form, along with the Itemized Invoice, to<br />
the following fax number: +1-608-301-2251<br />
Note: All claims must be sent to this fax number, which is<br />
equipped to handle large volumes of faxes.<br />
Additionally, any claims-related correspondence can be faxed to:<br />
+1-608-301-2250<br />
Note: Claims sent to this correspondence fax number will not be<br />
processed for reimbursement.<br />
34
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Secure Message Transmission: Compose a Message<br />
To send a message to the TOP Claims Customer Service<br />
Department, you can click the ‘Compose Message’ button.<br />
Selecting the ‘Compose Message’ button allows you to see<br />
a subset of message subjects to select: New Claim, Claim<br />
Status, General, Eligibility, or Appeals. Each message type<br />
has a set of input fields where you will supply information<br />
that will help the TOP Claims Customer Service Department<br />
assist in the resolution of your inquiry.<br />
{<br />
Here you can see a record of other<br />
claims which have been previously<br />
sent and processed.<br />
SECTIoN 5<br />
<strong>Provider</strong> Claims Information<br />
Note: There is also the quick button option ‘Send New Claim’ to<br />
submit your claim via Secure Message Transmission directly.<br />
Full instructions on how to submit claims via Secure Message<br />
Transmission are included in this section, see page 37.<br />
35
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
The Secure Message Transmission method available through<br />
your secure account on www.tricare-overseas.com allows you<br />
to submit messages directly to the <strong>TRICARE</strong> <strong>Overseas</strong> <strong>Program</strong><br />
(TOP) Customer Service department.<br />
To access your secure messages, select the ‘Secure Message’<br />
button in the top navigation bar to be taken to your secure<br />
message inbox. Your Inbox is a record of inquiries you have<br />
made to the <strong>TRICARE</strong> <strong>Overseas</strong> <strong>Program</strong> via the secure<br />
messaging service and replies received from our Customer<br />
Service department.<br />
The Secure Message Inbox tab will display all messages<br />
currently in your secure message account.<br />
The Inbox view uses the following display format:<br />
■ Check Box: This box is used to mark messages for deletion.<br />
Only use this box when you want to delete a message from<br />
your Inbox. You can select an individual message or multiple<br />
messages for deletion. Deletion of messages is permanent.<br />
■ Date: Date of last action on the email message. Date format is<br />
MM/DD/YYYY. By default, messages will display in your Inbox<br />
in the order of most recent date to oldest date.<br />
■ Subject: This field displays the message subject. The<br />
message subject is set to the inquiry type you select when<br />
composing the original message. Subject options include only<br />
the following:<br />
— New Claim<br />
— Claim Status<br />
— General<br />
— Eligibility<br />
— Appeal<br />
■ Status: The Status field will display one of the following two<br />
options:<br />
— Sent: These are messages you have composed and sent<br />
to the <strong>TRICARE</strong> <strong>Overseas</strong> <strong>Program</strong> that have not yet been<br />
viewed by our Customer Service department.<br />
— Received: The received status appears when your sent<br />
message has been reviewed by the Customer Service<br />
department.<br />
Note that the column heading can be clicked to sort the view of<br />
your Inbox by Date, Subject, or Status.<br />
The New Messages tab of the mailbox uses the same format as<br />
the Message Inbox tab, but will only display messages with a<br />
status of Sent, allowing you to see only those messages to which<br />
the Customer Service department has not yet replied.<br />
Your Inbox will store up to a maximum of 2,500 messages. To<br />
avoid potential issues with your secured mail account, be sure to<br />
manage your mail to not exceed this limit.<br />
36
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Secure Message Transmission: New Claim<br />
The ‘Send New Claim’ button is used when you want to submit a claim (as an attachment)<br />
to the TOP Claims Processor using the Secure Message Transmission method.<br />
Note: A ‘New Claim’ message can be initiated by selecting the<br />
‘Send New Claim’ button OR by selecting the ‘Compose Message’ button<br />
and then choosing ‘New Claim’ as the message subject.<br />
When sending a new claim, you will see there is a notice<br />
informing you of what information you will need in order to<br />
successfully send a ‘New Claim’ via the Secure Message<br />
Transmission method.<br />
This includes:<br />
• Claim information: Such as provider location (e.g.,<br />
country of origin, billed charges and currency).<br />
• Electronic Copy of a Signed Claim Form or Signed<br />
Claim Development Worksheet: You will need this to<br />
upload during the Secure Message Transmission process.<br />
• Patient Information: Including patient name, sponsor’s<br />
SSN, and beginning and ending dates of service.<br />
SECTIoN 5<br />
<strong>Provider</strong> Claims Information<br />
Once you have the information available, click the<br />
‘Get Started Sending a Secure Online Claim’ button<br />
at the bottom of the screen to begin the Secure<br />
Message Transmission process.<br />
37
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Secure Message Transmission: New Claim/Claim Information<br />
Upload Attachments:<br />
You must upload at least one of the following:<br />
• UB-04 Claim Form<br />
• CMS 1500 Claim Form<br />
• Claim Development Worksheet<br />
*Attachments uploaded through the site,<br />
including the claim form or worksheet, must<br />
be in one of the file formats listed under the<br />
‘Attachments’ field. There are additional<br />
attachment fields available for uploading other<br />
documents to accompany your claim. These<br />
additional attachment fields are optional.<br />
The screen will update to display the data fields you need to fill in<br />
along with the basic claim summary data fields for uploading the<br />
claim form and any additional attachments you wish to provide.<br />
Note: All fields are required unless otherwise noted:<br />
■ Location: Select the physical location address where the<br />
service took place.<br />
■ Total Billed Charges: Enter the sum of all charges on the<br />
claim form or worksheet.<br />
■ Currency Type: Enter the name or code of the currency in<br />
which the claim charges are listed. Note: If the beneficiary has<br />
other health insurance, the claim will be paid in $USD (United<br />
States Dollars) regardless of the currency type listed here.<br />
■ Invoice Number: This is an optional field to enter your office’s<br />
internal tracking number for the claim or bill.<br />
When all necessary fields are entered and your attachments have<br />
been uploaded, click ‘Next’.<br />
38
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Secure Message Transmission: Patient Information<br />
On the ‘Patient Information’ screen, you will be asked to provide the following patient<br />
information:<br />
• Sponsor Social Security Number (SSN): Select the patient’s benefit type from the drop<br />
down menu and then enter the corresponding benefit number in the text field to the right.<br />
• Patient First Name and Patient Last Name: Enter the patient’s first and last names in the<br />
corresponding fields.<br />
• Beginning Date of Service: Enter the earliest date of health care service as it is listed for<br />
the procedures being submitted on this claim. The date must be entered in MM/DD/YYYY<br />
format or you can click the calendar icon to select the date.<br />
• Ending Date of Service: Enter the last date of health care service as it is listed for the<br />
procedures being submitted on this claim. This date must be entered in the MM/DD/YYYY<br />
format or you can click the calendar icon to select the date.<br />
Click ‘Next.’<br />
SECTIoN 5<br />
<strong>Provider</strong> Claims Information<br />
39
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Secure Message Transmission: New Claim/Confirmation<br />
If you need to make changes to either the<br />
Claim Information section or the Patient<br />
Information section, click the ‘Edit’ button<br />
next to the section that requires changes.<br />
A Confirmation screen summarizing the data you entered will appear.<br />
Verify the information you provided.<br />
If all of the information is correct, click ‘Submit’ to send your claim to the TOP<br />
Claims Processor.<br />
When you click ‘Submit’ the screen will update to confirm that your TOP Claim has<br />
been successfully submitted via the Secure Message Transmission method. You<br />
will also receive an automated email response confirming your Secure Message<br />
Transmission. The automated email response will summarize the claim data you<br />
entered and will also provide you with the TOP claim number for your claim. The<br />
TOP claim number can be used to track the progress of your claim through the<br />
‘Claim Status and Claims Report’ functions available in your secured account area.<br />
Note: The ‘Secure Message Transmission’ function should only be used to submit<br />
ONE claim per each secure message.<br />
40
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Claim Forms can be submitted in any language and invoices in<br />
any currency. Only one claim can be submitted per Secure<br />
Message Transmission transaction (the secure <strong>Provider</strong> portal<br />
will allow a maximum of 15MB total).<br />
The following formats are accepted: .doc, .xls, .jpg, .jpeg, .tf, .tiff<br />
or .pdf.<br />
The claim will be entered into the TOP Claims Processor’s system<br />
and can be tracked on the Secure Claims Portal using the<br />
patient’s name, the sponsor’s Social Security Number, DOD<br />
Benefits Number, DEERS Family ID, and DOB or Dates of<br />
Service.<br />
Claims will be available for you to review within 15 days of<br />
receipt. Secure Message Transmission through the Secure<br />
Claims Portal can be used to submit claims for TOP Prime and<br />
TOP Prime Remote beneficiaries.<br />
This transmission method can also be used if the <strong>Provider</strong><br />
chooses to submit claims on behalf of TOP Standard<br />
beneficiaries.<br />
Note: Claims may not be emailed to International SOS directly. If<br />
Claim Forms and Itemized Invoices are emailed to International<br />
SOS directly, they will not be processed.<br />
online Claim Submission<br />
Note: Standard Web-based submission software packages such<br />
as PC-Ace require that all claims are submitted in U.S. Dollars.<br />
These packages are most suitable for <strong>Provider</strong>s located in U.S.<br />
Territories familiar with Standard U.S. Claim Form procedures.<br />
For this reason, International SOS has developed a customized<br />
claims submission program, which is available on the un-secure<br />
<strong>Provider</strong> portal. User-friendly field descriptions and built-in<br />
prompts are used on this site to assist <strong>Provider</strong>s in submitting<br />
claims. When using the ‘Online Claim’ submission option,<br />
claims can be tracked within 12 business hours of receipt.<br />
This portal also allows <strong>Provider</strong>s to submit claims in certain<br />
foreign currencies. Using the <strong>Provider</strong> Portal to submit claims<br />
electronically is the recommended option for overseas <strong>Provider</strong>s.<br />
This option significantly reduces the amount of time it takes to<br />
process payments.<br />
To use ‘Online Claim’ submission, you must first sign an<br />
Electronic Data Interchange (EDI) Agreement. The EDI Form is<br />
effectively a record of your signature on file for each claim that<br />
you submit through the portal. This form can be obtained from<br />
your International SOS TOP <strong>Provider</strong> Support Services staff,<br />
or it can be downloaded from www.tricare-overseas.com.<br />
A sample EDI Agreement Form can be found on page 105 of<br />
this TOP <strong>Provider</strong> <strong>Manual</strong>.<br />
All EDI Agreements are subject to acceptance by International<br />
SOS and Wisconsin Physicians Service (WPS).<br />
The second Web-based claims submission method is also<br />
available via the Secure Claims Portal on www.tricareoverseas.com.<br />
This portal has a custom-built ‘Online Claim’ submission option,<br />
which can be used to submit TOP Claims.<br />
Alternatively, <strong>Provider</strong>s may download and submit claims using<br />
other Web-based submission software, such as PC-Ace. PC-Ace<br />
is available free of charge from International SOS. Please contact<br />
your TOP Regional Call Center and press option #5 to speak with<br />
a TOP <strong>Provider</strong> Support Services staff member to request this<br />
software.<br />
Claim Forms and Itemized Invoices are not required when<br />
submitting claims electronically through the Secure Claims Portal.<br />
Instead, <strong>Provider</strong>s will be prompted to enter the claim data using<br />
ICD diagnosis codes and CPT procedure codes. These<br />
requirements vary slightly, depending on whether the claim is for<br />
an Institutional or Non-Institutional <strong>Provider</strong>.<br />
Finally, a clearing house or billing agency can be used for claims<br />
submission. In this case, it is the <strong>Provider</strong>’s responsibility to<br />
supply all required paperwork for accurate, complete processing<br />
of claims. If a clearing house or billing agency is used, a CMS<br />
1500 Form or a UB-04 Form is still required.<br />
Note: Please visit www.tricare-overseas.com/provider.htm to<br />
download a Computer Based Training Module on Web-based<br />
‘Online Claim’ submission of TOP claims.<br />
SECTIoN 5<br />
<strong>Provider</strong> Claims Information<br />
41
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
online Claim Submission: Select a Location<br />
The www.tricare-overseas.com Secure Claims Portal has field<br />
descriptions and built-in prompts that will assist you while entering<br />
the claim electronically. If you choose to submit claims using this<br />
website, you will see the following page after you log-in and click<br />
‘Online Claim.’<br />
Your screen will update to display the ‘Online Claim’ submission<br />
page.<br />
The Select Location section of the page displays a ‘Submit Claim’<br />
tab which lists all current locations for which you have an<br />
agreement for electronic claim submission.<br />
Click the radio button in the ‘Submit Online’ column that<br />
corresponds to the location where the medical services were<br />
rendered.<br />
Note: If you have a location on file with the TOP Claims Processor<br />
but do not have an electronic claims submission agreement for<br />
that location, you can see that location by clicking on the ‘Need<br />
Web Claim Submission Agreement’ tab. On that tab you can also<br />
request electronic claims submission by clicking on the ‘Sign Up’<br />
link for those locations.<br />
If the location where the services were rendered does not<br />
appear on either the ‘Submit Online’ tab or the ‘Need Web<br />
Claim Submission Agreement’ tab, you can add the location<br />
by clicking the ‘Request a New Location’ link.<br />
42
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
online Claim Submission: Select a Patient<br />
Scroll down the page to the ‘Select Patient’ section. In this section, you can search for<br />
patients by using their <strong>TRICARE</strong> Sponsor Social Security Number (SSN) or DEERS Family<br />
ID as indicated on the patient’s Military ID card, which the patient should always carry<br />
with them.<br />
This search function will return a list of beneficiaries, their date of birth, and gender<br />
indicator based on the ID number. You can select the correct patient for your claim by<br />
clicking the ‘Radio’ button in front of their name.<br />
You have the alternative of selecting from a list of recent patients<br />
from claims you have submitted to the TOP Claims Processor.<br />
Click the ‘Choose from Recent Patients’ tab, select the letter that<br />
corresponds with the first letter of the patient's last name, and<br />
view a list of your recent <strong>TRICARE</strong> patients on screen.<br />
Note: If your search does not return any results, you will not be able to use the ‘Online<br />
Claim’ submission feature through www.tricare-overseas.com unless your patient is<br />
under 1 year of age. If your patient is a <strong>TRICARE</strong> beneficiary under 1 year of age and their<br />
name does not come up in a search result, select the ‘I am unable to find an eligible child<br />
under 1 year of age’ button and complete the First Name, Last Name and Date of Birth<br />
fields for this patient.<br />
Select the patient from this list by clicking the ‘Radio’ button in<br />
front of the patient's name.<br />
After selecting the patient for your claim, click ‘Next’.<br />
SECTIoN 5<br />
<strong>Provider</strong> Claims Information<br />
43
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
online Claim Submission: Verify a Patient<br />
Please verify that this is the patient’s<br />
current and correct address. If you<br />
have a more current address for the<br />
patient, select the ‘Edit’ button next<br />
to the address and input the up-todate<br />
correct address you have on<br />
file. This will help expedite the claims<br />
process.<br />
The selected patient's name, date of birth, gender indicator and<br />
address will appear on the screen.<br />
Please verify that this is the patient that corresponds with your<br />
TOP Claim before proceeding.<br />
Note: If the TOP Claims Processor has information that indicates<br />
the patient may have Other Health Insurance (OHI) that should<br />
pay on the claim before <strong>TRICARE</strong> makes payment, you will<br />
receive a notice. If your patient does have OHI that should be<br />
paying, you will be responsible for entering the OHI payment<br />
information when completing the ‘Claim Information’ section.<br />
You have the option to attach an invoice number or code used by<br />
your office to identify this claim. To use this feature, enter your<br />
invoice or tracking number in the open field provided. A<br />
maximum of 20 characters are allowed for the invoice number.<br />
Note: Adding an invoice number or code will allow you to easily<br />
track this claim on the Secure Claims Portal as you will be able to<br />
use the invoice number or code to search for the claim and view<br />
its processing status.<br />
Once you’ve verified the patient data, click ‘Next.’<br />
44
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
online Claim Submission: Enter Claim Information<br />
If you do not know the ICD diagnosis codes for the<br />
patient's diagnosis, you can use the ‘Code Lookup’<br />
feature and search for the code by its description.<br />
To use the Code Lookup:<br />
• Click on ‘Code Lookup’<br />
• The ‘Diagnosis Lookup’ pop-up box will appear<br />
• Type the description of the diagnosis in the box<br />
• Click the ‘Search’ button<br />
A list of descriptions containing your search word will<br />
appear. The ICD code corresponding to each<br />
description appears in the column to the left of the<br />
description. Find the diagnosis description for your<br />
claim and then click the code to the left to enter it into<br />
the Diagnosis field of the online claim form.<br />
The Claim Information page is where you begin entering the data<br />
about the health care encounter. Required fields are indicated<br />
with an asterisk.<br />
In the Diagnosis section, enter the ICD diagnosis codes that<br />
correspond to the reason the patient needed medical care. If you<br />
know the ICD code that represents the patient's diagnosis, it can<br />
be keyed directly into this field.<br />
Note: The Principal DX, or diagnosis, field is required for claims<br />
processing. There are seven additional fields for entering other<br />
diagnoses describing the patient's condition. These additional<br />
fields are optional.<br />
Select the ‘Assignment of Benefits’ indicator. Select ‘Yes’ if you<br />
want to receive reimbursement directly from <strong>TRICARE</strong>.<br />
If the patient made a payment to you for services on this claim<br />
prior to this claim being submitted, you must indicate their<br />
payment amount in the ‘Patient Paid’ field. The amount entered<br />
here should be given in the currency you will select below.<br />
However, if the patient has OHI, the ‘Patient Paid’ field must be<br />
completed in $USD (United States dollars).<br />
Note: This is a required field and must be completed, so if there<br />
is no patient payment prior to claim submission, enter zeroes<br />
(0000000) in these fields.<br />
In the field ‘Patient has Other Health Insurance (OHI)’, if the<br />
patient does not have another health insurance paying you for<br />
this claim (i.e., before <strong>TRICARE</strong> will pay), select ‘No’ and continue<br />
to the next section of the form.<br />
SECTIoN 5<br />
<strong>Provider</strong> Claims Information<br />
45
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
If the patient does have another health insurance paying before<br />
<strong>TRICARE</strong> select ‘Yes.’ When you select ‘Yes’ the screen will<br />
update to display 3 additional fields to provide the payment<br />
information from the OHI:<br />
■ other Health Insurance Allowed – Enter the amount the OHI<br />
indicated as its ‘Allowed’ amount for the entire claim. Enter<br />
this amount in $USD (United States Dollars).<br />
■ other Health Insurance Paid – Enter the amount the OHI<br />
paid for the entire claim. Enter this amount in $USD (United<br />
States Dollars).<br />
■ other Health Insurance Payment Reason – The OHI will<br />
typically provide a code or comment explaining how they<br />
processed the claim. Click the ‘Look Up’ and from the pop-up<br />
box, select the reason that matches the OHI explanation.<br />
— Either Deductible, Copay/Cost Share, Non-Covered<br />
Service or Other.<br />
— Note: This is a required field when there is OHI, so if there<br />
is no payment reason from the OHI or if there isn’t one that<br />
matches these choices, select ‘Other.’<br />
Be aware that claims transactions involving OHI must be<br />
conducted in $USD (United States Dollars). The currency type<br />
for the claim will default to $USD and cannot be changed. If you<br />
previously entered a patient payment amount in a currency other<br />
than $USD, please return to that field and enter the correct<br />
amount for $USD currency.<br />
You can select a currency type for the claims transaction from a<br />
drop down menu.<br />
However, if the claim transaction does include OHI, this option<br />
will not be available as the claim transaction with OHI must be<br />
in $USD.<br />
online Claim Submission: Claim Line Item Form<br />
To use the ‘Lookup’ feature:<br />
• Click on ‘Code Lookup’<br />
• The CPT/HCPCS Lookup pop-up box will appear<br />
• Type the description of the procedure in the box<br />
• Click the ‘Search’ button<br />
A list of descriptions containing your search word will<br />
appear. The code corresponding to each description<br />
appears in the column to the left of the description. Find<br />
the diagnosis description for your claim and then click<br />
the code to the left to enter it into the CPT/ HCPCS field<br />
of the online claim form.<br />
46
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
The ‘Claim Line Item Form’ section is for entering the details about the<br />
medical services and/or supplies provided during the health care<br />
encounter. The ‘Claim Line Item Form’ section is not a summary<br />
section: you can enter multiple procedures per claim. Each procedure<br />
will have its own claim line.<br />
Note: Required fields are indicated with an asterisk.<br />
Begin by entering the dates of service for the procedure. Dates of<br />
service can be typed directly into the ‘From’ and ‘To’ fields or you can<br />
use the calendar icon to select the dates of service.<br />
Note: The required format for the ‘Dates of Service’ fields is Month,<br />
Day and Year.<br />
Enter the Current Procedural Terminology (CPT) code or the Health<br />
Care Procedure Coding System (HCPCS) code that represents the<br />
medical procedure or service that was performed. If you know the<br />
code representing the procedure or supply, you can type it directly<br />
into this field.<br />
The ‘Modifier’ field is used to enter 2 character codes that represent<br />
additional descriptors or clarifiers to the procedure performed. The<br />
modifier is not a required field and can be left blank.<br />
The ‘National Drug Code’ field is for listing the code the United States<br />
Food and Drug Administration assigns to any marketed prescription<br />
drug or insulin. This field is not required and should be left blank<br />
unless the medical procedure code entered in the CPT/HCPCS field<br />
represents a prescription drug or insulin.<br />
The ‘Anesthesia’ field should be checked ‘Yes’ only if the code<br />
entered in the CPT/HCPCS field represents anesthesia. If you<br />
selected ‘Yes’ here, the ‘Units’ field should be entered with the number<br />
of minutes anesthesia was administered.<br />
The ‘Units’ field is for entering the number of times the procedure in<br />
the CPT/HCPCS field was performed during the dates of service OR it<br />
should represent the number of units of the supply provided.<br />
Note: If the procedure or supply is a prescription or injection and the<br />
National Drug Code was also provided, enter the National Drug Code<br />
quantity in this field and not the HCPCS quantity. If you selected ‘Yes’<br />
in the Anesthesia field, the number of units should be the number of<br />
minutes billed for anesthesia.<br />
The ‘Charges’ field is used to enter the amount you are billing for the<br />
procedure or service. Type the amount directly into these fields.<br />
Note: The amount entered in this field must be in the currency type<br />
selected in the ‘Claim Information’ section of the form. If the ‘Currency<br />
Type’ field displays $USD (United States dollars), the amount entered<br />
here must also be in $USD.<br />
The ‘Place of Service’ field is for entering the 2-digit code that<br />
describes the type of facility where the procedure was performed. If<br />
you know the correct code, it can be typed directly into this field. If<br />
you do not know the code, click the ‘Lookup’ button. A pop-up box<br />
with a list of descriptions will appear. The ‘Place of Service’ code<br />
corresponding to each description displays in a column to the left of<br />
the description. Select the code for the description that matched the<br />
location description to enter it into the ‘Online Claim Form.’<br />
The ‘Service Location Zip Code’ field is an optional field, but if<br />
applicable enter the Zip Code of the location where the services were<br />
rendered in this field. This field only accepts Zip Codes in a 5-digit, allnumeric<br />
format. If your service location Zip Code does not meet the<br />
required format, leave this field blank.<br />
The ‘<strong>Provider</strong>’ field is a drop down menu of names of individuals on<br />
file for the ‘<strong>Provider</strong> Location’ you selected at the start of the ‘Online<br />
Claim’ submission process. Choose the name of the individual that<br />
performed the procedure or service given in the CPT/HCPCS field. If<br />
the name of the individual is not listed here, you can add them to the<br />
provider list for the location through the ‘Administration’ console OR if<br />
you cannot add them, you will not be able to include the procedures<br />
or services that person performed in your online claim submission.<br />
You have the option to provide comments or additional information to<br />
the line item you are currently entering. Click the ‘Insert Comment’ link<br />
to open a box that will allow you to enter up to 80 characters of text to<br />
accompany this procedure or service item.<br />
Once you have entered all required information for the procedure or<br />
service in the ‘Claim Line Item Form’ fields, click the ‘Add Line Item’<br />
button to include the item in your claim.<br />
When you click the ‘Add Line Item’ button, the information for the<br />
procedure or service item in the ‘Line Item Form’ will move to the ‘Line<br />
Item List’ section, displaying all details you entered for the item. The<br />
‘Claim Line Item Form’ fields will reset to blank so that additional<br />
procedures or services can be entered on your claim.<br />
online Claim Submission: Line Item List<br />
The ‘Line Item List’ section will display all procedure or service items<br />
you have added to the claim, along with all details you entered for<br />
each item. If you need to correct or modify a line item, select the ‘Edit’<br />
button for that item. If the line item should not be submitted with the<br />
claim, select the ‘Delete’ button for that item to completely remove it<br />
from the claim before submission.<br />
At the end of the ‘Line Item List’ section, the Total Charges are given<br />
for the claim. The total charges will be the sum of the charges in the<br />
currency type you selected for all line items you have added to the<br />
claim.<br />
Once you have completed entering line items to your claim, click the<br />
‘Next’ button<br />
SECTIoN 5<br />
<strong>Provider</strong> Claims Information<br />
47
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
online Claim Submission: Review and Submit<br />
To end the ‘Online Claim’ submission transaction<br />
without submitting the form, click ‘Cancel.’<br />
Note: Data will NOT be saved if you select ‘Cancel’.<br />
To make revisions, click the ‘Edit Claim Information’<br />
button to return to the claim form and update your<br />
patient or claim information.<br />
To submit your claim for processing, click the ‘Submit<br />
Claim’ button.<br />
The ‘Review and Submit’ page gives you one additional chance<br />
to confirm all the data you have entered into the ‘Online Claim’<br />
form (i.e., patient information, diagnosis and OHI data and all<br />
procedural information you’ve entered into the claim form).<br />
Note: When you click ‘Submit Claim’ the data will transmit to the<br />
TOP Claims Processor and you will not be able to make further<br />
changes.<br />
online Claim Submission: Claim Received<br />
If the ‘Online Claim’ submission is successful, you will see the<br />
‘Claim Received’ page.<br />
This page will summarize the currency selection and the total<br />
billed amount submitted on the TOP Claim. It will also provide you<br />
with a claim number.<br />
The claim number can be used to track the status of the TOP<br />
Claim using the ‘Claim Status’ feature.<br />
Note: It may take up to 12 business hours from submission for<br />
the claim to appear using the ‘Claim Status’ feature. Claims can<br />
be searched using the patient’s name, the sponsor’s Social<br />
Security Number of DOD Benefits Number, or by the Date of<br />
Service.<br />
48
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Claims for Services Rendered<br />
Before September 1, 2010<br />
Effective September 1, 2010, all claims must be submitted using<br />
one of the International SOS submission methods outlined. This<br />
applies, even if treatment was provided for dates of service<br />
before September 1, 2010.<br />
For services delivered before September 1, 2010, a Claim Form<br />
and Itemized Invoice must be submitted. The correct Claim Form<br />
must be used, to ensure payment.<br />
CMS 1500 (Non-Institutional <strong>Provider</strong>s) and UB-04 (Institutional<br />
<strong>Provider</strong>s) Claim Forms can be downloaded at www.tricareoverseas.com.<br />
Detailed instructions for completing these forms<br />
can be found in Section 5 of this TOP <strong>Provider</strong> <strong>Manual</strong>. An online<br />
eLearning Module on how to properly fill out your Claim Forms is<br />
also available. Please contact your TOP Regional Call Center and<br />
select option #5 to request access details on the eLearning<br />
Module.<br />
Claim Tracking and Monitoring<br />
Once you become a registered user on the <strong>Provider</strong> Portal, you<br />
can track your claims online at www.tricare-overseas.com.<br />
After claims are submitted on this portal, they are entered into<br />
International SOS’ system.<br />
If you submitted your claims by overseas mail, overseas fax or<br />
Secure Message, you can view them online within 15 days of<br />
receipt. If you submitted your claims via Online Claim Submission<br />
using the <strong>Provider</strong> Portal, you can view them online within<br />
12 business hours.<br />
<strong>Provider</strong>s can search for claims using the patient’s name, the<br />
sponsor’s Social Security Number or DOD Benefits Number, and<br />
DOB, or Dates of Service, or Claim Number.<br />
The claim status will indicate whether the claim is being<br />
processed and if it has been paid. If the claim has been paid, the<br />
claim status update will indicate how much has been paid or if<br />
the claim has been denied. Once the claim has been processed,<br />
the <strong>Provider</strong> will be able to view the Explanation of Benefits (EOB)<br />
for that claim online.<br />
Full instructions on using the <strong>Provider</strong> Portal ‘Dashboard’ features<br />
are included in Section 6 of this TOP <strong>Provider</strong> <strong>Manual</strong>, see pages<br />
77-85.<br />
Timely Filing of Claims<br />
All claims must be submitted within 1 year of the Date of Service.<br />
Claims must be date stamped/received by International SOS<br />
within 12 months of the last date of treatment in order to be<br />
reimbursed. Any claims exceeding this 12 month timely filing<br />
deadline will be declined.<br />
Claim Reimbursement and<br />
Payment<br />
<strong>Provider</strong> payments can be made in the following ways:<br />
■ By Check (Local Currency)<br />
■ Bank Draft (Local Currency)<br />
■ Electronic Fund Transfer (EFT) (Local Currency)<br />
Payments will be made in the currency in which the invoice is<br />
submitted, wherever possible. If the <strong>Provider</strong> submits an invoice in<br />
U.S. Dollars, payment will be made in U.S. Dollar check. If invoices<br />
are submitted in local currency, payment will be made by local<br />
currency bank draft, whenever possible. International SOS can<br />
make payments in over 100 currencies. If your currency is not<br />
available, payment will be made by U.S. Dollar check. Checks and<br />
bank drafts will be sent to the <strong>Provider</strong> by overseas mail.<br />
If <strong>Provider</strong>s would like to receive payment via Electronic Funds<br />
Transfer (EFT), they must submit a request by completing and<br />
submitting an EFT Form. EFT Forms can be downloaded at<br />
www.tricare-overseas.com or you can contact your TOP<br />
Regional Call Center and select option #5 to speak to a TOP<br />
<strong>Provider</strong> Support Services staff member to obtain a form.<br />
When completing the EFT Form, please be sure to include the<br />
following information:<br />
■ <strong>Provider</strong> ID number<br />
■ The name of your bank and the name on the account<br />
■ Account number or IBAN number<br />
■ SWIFT code<br />
Please also include the currency in which you would like to<br />
receive payment. This must be the same as the currency in which<br />
you submit your claims. If any of these details is incomplete or<br />
missing, International SOS will not be able to process your EFT<br />
request. Once your EFT is set up, this will be your default method<br />
of payment.<br />
EFT is our recommended method of payment, as it reduces the<br />
amount of time it takes to receive payments.<br />
Remittance advice will be sent to the <strong>Provider</strong> in the form of an<br />
Explanation of Benefits (EOB). If the <strong>Provider</strong> receives payment<br />
by U.S. Dollar check or bank draft, the EOB will be sent to you by<br />
mail with the check or bank draft. If the <strong>Provider</strong> has an EFT set<br />
up, EOBs will be sent separately by mail. EOBs are also available<br />
to view online, on the <strong>Provider</strong> Portal available on www.tricareoverseas.com.<br />
Please see Section 6: The <strong>Provider</strong> Portal for<br />
additional information about viewing your EOB online.<br />
SECTIoN 5<br />
<strong>Provider</strong> Claims Information<br />
49
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Required Criteria for Ensuring<br />
Payment of Claims<br />
<strong>Provider</strong>s can help to ensure that claims are processed (and<br />
payments made) in a timely manner, by making sure that the<br />
following minimum required fields are completed on their Claim<br />
Form, before it is submitted:<br />
CMS 1500:<br />
1. <strong>TRICARE</strong> Ticked<br />
2. Patient Name<br />
3. Patient Address<br />
4. Sponsor Name<br />
5. Sponsor’s Social Security Number or DOD Benefits Number<br />
6. Other Health Insurance (OHI) Details (if applicable)<br />
7. Patient Signature x2 and the date<br />
8. Diagnosis (if this cannot be written on the invoice)<br />
9. Authorization Number<br />
10. Federal Tax ID (<strong>Provider</strong> ID or TEPRV)<br />
11. Accept Assignment? YES<br />
12. Amount Paid by OHI or Beneficiary (if applicable)<br />
13. <strong>Provider</strong> Signature<br />
14. <strong>Provider</strong> Name and Billing Address<br />
UB-04:<br />
1. <strong>Provider</strong> Name and Billing Address<br />
2. Federal Tax ID (<strong>Provider</strong> ID or TEPRV)<br />
3. Patient Name<br />
4. Patient Address<br />
5. Other Health Insurance (OHI) Details (if applicable)<br />
6. Assignment of Benefits – YES<br />
7. Amount Paid by OHI or Beneficiary (if applicable)<br />
8. Sponsor Name<br />
9. Sponsor’s Social Security Number or DOD Benefits Number<br />
10. Authorization Number<br />
11. Diagnosis (if this cannot be written on the invoice)<br />
12. <strong>Provider</strong> Signature<br />
<strong>Provider</strong>s must also ensure that the Itemized Invoice they submit<br />
contains all of the following information:<br />
■ Date of Service<br />
■ Letterhead Containing the <strong>Provider</strong>’s Name, Physical Address<br />
and Billing Address<br />
■ Invoice Number or Patient Account Number<br />
■ Corresponding Authorization Number (when required) prior to<br />
Treatment (this can be found on the Authorization Form)<br />
■ Patient Name<br />
■ Description of Diagnosis (if the diagnosis cannot be written on<br />
the invoice, please include this on the Claim Form)<br />
■ Breakdown of Services Rendered, Listing Corresponding<br />
Costs (and Taxes) and Overall Total Owed<br />
■ Invoice Currency<br />
Important: Claim Forms that are received without an invoice, or<br />
invoices that are received without a Claim Form will not be<br />
processed. The received document will be returned to the<br />
<strong>Provider</strong>.<br />
Note: If <strong>Provider</strong>s would like to receive payment for claims in the<br />
fastest possible time, International SOS recommends using the<br />
Online Claim Submission option via the <strong>Provider</strong> Portal AND<br />
registering to receive EFT payments. This helps avoid the delays<br />
associated with overseas mailing times.<br />
Explanation of Benefits and<br />
Applicable Exchange Rate<br />
Information<br />
Remittance Advice is sent to the <strong>Provider</strong> in the form of an EOB.<br />
EOBs are sent to the <strong>Provider</strong> by mail however this information is<br />
also available to be viewed online via the <strong>Provider</strong> Portal. The<br />
electronic EOB is available on the same date the payment is<br />
issued.<br />
The EOB includes detailed information regarding any items that<br />
may have been denied for payment. It also includes important<br />
exchange rate data, which was used for issuing payment.<br />
Deductibles and co-payments that TOP Standard beneficiaries<br />
are responsible for paying will also be included on the EOB.<br />
According to TOP policy, the exchange rate applied will be the<br />
exchange rate valid on the last day of the ‘episode of care’ or last<br />
date of invoiced services. Citigroup is the standard exchange<br />
rate used by International SOS.<br />
If a claim is denied or not paid in full, a denial code will be<br />
assigned to that charge. An explanation of the denial codes<br />
is included on the last page of the EOB. A list of denial<br />
codes and their explanations is available online at<br />
www.tricare-overseas.com as well as in the Appendix of this<br />
TOP <strong>Provider</strong> <strong>Manual</strong>.<br />
You can also contact your TOP Regional Call Centre or submit a<br />
request via the Secure Message Transmission option on the<br />
<strong>Provider</strong> Portal.<br />
Note: Responses to Secure Messages transmitted via the<br />
<strong>Provider</strong> Portal will be sent to the Secure Message Inbox on the<br />
<strong>Provider</strong> Portal. Please see Section 6: The <strong>Provider</strong> Portal for<br />
additional information about accessing Secure Messages.<br />
50
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Below are sample EOB statements for TOP Prime and TOP Prime Remote beneficiaries:<br />
Here are the <strong>Provider</strong>’s details. This<br />
is to whom the payment is made.<br />
The number in this corner will be a local<br />
toll free number which the <strong>Provider</strong> can<br />
call if they need assistance.<br />
®<br />
This is the Claim Number, also known as the<br />
Internal Control Number (ICN).<br />
The Check Number helps <strong>Provider</strong>s match the payments that have been made to the Claims they have submitted. If the <strong>Provider</strong> has<br />
been paid by check, this number will correspond with the check number on the payment check. If the <strong>Provider</strong> has been paid by<br />
bank draft, this number will correspond with the number on the perforated record attached to the bank draft. If the <strong>Provider</strong> has been<br />
paid by Electronic Fund Transfer (EFT) up to six check numbers will appear in the payment line on the bank statement.<br />
®<br />
SECTIoN 5<br />
<strong>Provider</strong> Claims Information<br />
This is the<br />
Check Number.<br />
51
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
®<br />
‘PT Resp’ means Patient’s Responsibility.<br />
TOP Prime beneficiaries receive a cashless<br />
service. Therefore, the deductibles and<br />
cost-shares are listed as $0.00.<br />
If any charges are denied,<br />
the denial code will be<br />
listed here.<br />
This is the total amount<br />
International SOS will<br />
reimburse.<br />
These are the dates of<br />
the ‘Episodes of Care’ as<br />
indicated on the invoice.<br />
These are the costs for<br />
the treatments the<br />
patient received.<br />
This is the total amount<br />
International SOS will<br />
reimburse.<br />
These are the CPT<br />
procedure codes.<br />
International SOS will<br />
translate the treatment<br />
details from the invoice<br />
into CPT codes.<br />
These are the costs that are allowed<br />
under the beneficiary’s <strong>TRICARE</strong><br />
policy. If any payments are denied, a<br />
denial code will be indicated. An<br />
explanation of the code is given on the<br />
last page of the EOB.<br />
52
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
On the bottom half of the EOB, you will find the payment summary showing the amount International SOS will reimburse and the<br />
amount that is still outstanding.<br />
A brief explanation of the Denial Codes (if any) will appear here. A full list of Denial Codes is available in Host Nation<br />
Languages on www.tricare-overseas.com. No charges have been denied, therefore there are no denial codes listed here.<br />
Here, you will find the exchange rate that was used. Exchange rates will be in effect on the last date of service. International<br />
SOS uses Citigroup’s exchange rates.<br />
This is a sample TOP Standard beneficiary EOB<br />
If more than one invoice is submitted, or if a single invoice for multiple procedures is submitted with a single Claim Form, the EOB will<br />
appear as follows:<br />
SECTIoN 5<br />
<strong>Provider</strong> Claims Information<br />
These are the dates for<br />
the ‘Episodes of Care’<br />
indicated on the Itemized<br />
Invoice.<br />
These are the CPT<br />
procedure codes.<br />
International SOS will<br />
translate the treatment<br />
details from the invoice<br />
into CPT codes.<br />
This EOB is for a Standard beneficiary and some of the services<br />
are not covered. Therefore, there is the total which is allowed<br />
under the policy; the amount the beneficiary must pay and the<br />
amount International SOS will reimburse.<br />
53
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
On the reverse side of the EOB will be additional information regarding <strong>Provider</strong> and beneficiary rights, as well as beneficiary<br />
co-payments, appeals process details and other information.<br />
54
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
The Bank Draft<br />
If the <strong>Provider</strong> is being paid by bank draft, it will be attached to the bottom of a letter, which will be sent to the <strong>Provider</strong> along with<br />
their EOB via overseas mail.<br />
This is the<br />
Check Number.<br />
123456<br />
SECTIoN 5<br />
<strong>Provider</strong> Claims Information<br />
The bottom part of the bank draft letter is the bank draft itself.<br />
The beneficiary and <strong>Provider</strong> details are located at the top of the letter, along with the issue date, the amount being paid, a payment<br />
reference number and the Check Number. The Check Number corresponds with the Check Number on the bank draft, as well as the number<br />
on the EOB.<br />
55
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Transaction Fees Associated with<br />
Claim Reimbursement and<br />
Payments<br />
International SOS is responsible for any costs associated with<br />
issuing payments, such as issuing checks and bank drafts,<br />
sending EFT payments (and related transaction fees), and<br />
sending the EOBs. <strong>Provider</strong>s are responsible for all of the costs<br />
associated with receiving payments, such as depositing checks<br />
and bank drafts, collecting EFT payments, and exchanging<br />
payments into local currency.<br />
What if Both Non-Institutional and<br />
Institutional <strong>Provider</strong>s Are Used for<br />
the Same ‘Episode of Care’ and<br />
Billed Independently?<br />
Two separate Claim Forms will be needed: one from the Non-<br />
Institutional <strong>Provider</strong> (CMS 1500) and one from the Institutional<br />
<strong>Provider</strong> (UB-04).<br />
Each entity that requests to receive payment independently must<br />
submit a separate Claim Form (CMS 1500 for Non-Institutional<br />
<strong>Provider</strong>s or UB-04 for Institutional <strong>Provider</strong>s) and an Itemized<br />
Invoice.<br />
Step-by-Step Instructions for<br />
Accurately Completing Claim<br />
Forms<br />
TOP <strong>Provider</strong> Support Services staff will work with you to show<br />
you how to complete each of the following Claim Forms properly.<br />
When you receive an International SOS Authorization Form, a<br />
pre-populated Claim Form will be sent to you simultaneously. If<br />
you do not receive an Authorization Form or if you need<br />
additional Claim Forms, these are available to be downloaded on<br />
www.tricare-overseas.com.<br />
Note: These Claim Forms will not be pre-populated.<br />
Full instructions on how to complete Claim Forms that have not<br />
been pre-populated are included in this TOP <strong>Provider</strong> <strong>Manual</strong><br />
and are also available at www.tricare-overseas.com.<br />
Instructions on how to complete a pre-populated Claim Form are<br />
available at www.tricare-overseas.com.<br />
International SOS has also developed an eLearning Module to<br />
help you complete Claim Forms. Please contact your TOP<br />
Regional Call Center and press option #5 to request access to<br />
the eLearning Module.<br />
If needed, additional Claim Forms can be downloaded at<br />
www.tricare-overseas.com.<br />
What if a Beneficiary Does Not<br />
Show for an Appointment?<br />
<strong>TRICARE</strong> beneficiaries are directly responsible for paying noshow<br />
fees. You should invoice the patient directly for failing to<br />
cancel an appointment (without sufficient advance notice) or<br />
failing to show up for a scheduled appointment.<br />
56
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
The Claims Process<br />
Completing the CMS 1500<br />
PART 1<br />
Patient’s and<br />
Sponsor’s<br />
Details<br />
PART 2<br />
Patient’s Signature<br />
PART 3<br />
Diagnosis and<br />
Authorization<br />
Number<br />
PART 4<br />
<strong>Provider</strong>’s Details<br />
{{<br />
{{<br />
SECTIoN 5<br />
<strong>Provider</strong> Claims Information<br />
57
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
The Pre-Populated Claim Form CMS 1500<br />
When you receive an<br />
Authorization Form from<br />
International SOS, you<br />
will also receive a<br />
pre-populated Claim Form.<br />
All the fields highlighted<br />
in purple will be<br />
pre-populated. All the<br />
fields highlighted in green<br />
can be left blank.<br />
You will only have to<br />
complete these few<br />
fields shown here in white.<br />
58
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Part 1: Patient’s and Sponsor’s Details<br />
Always choose the<br />
<strong>TRICARE</strong> option.<br />
Please enter the patient’s<br />
DOB using the format<br />
MM DD YY and tick M or F to<br />
indicate the patient’s gender.<br />
Enter the sponsor’s ID number (10-digit DOD<br />
Benefit or 9-digit Social Security Number (SSN))<br />
and name using the format Last Name, First<br />
Name, Middle Initial. This information will appear<br />
on the patient’s Military ID Card.<br />
Enter the patient’s name,<br />
using the format Last Name,<br />
First Name, Middle Initial and<br />
the patient’s full physical<br />
address including post code.<br />
Enter the patient’s relationship<br />
to the sponsor.<br />
Fields highlighted in green<br />
can be left blank<br />
Enter the sponsor’s<br />
full address if different than<br />
the patient’s.<br />
If the patient has OHI enter<br />
the name of the insured party<br />
using the format Last Name,<br />
First Name, Middle Initial, the<br />
policy number and in field 9d<br />
enter the name of the<br />
insurance plan.<br />
<strong>TRICARE</strong> is always the secondary<br />
payer. If the patient has OHI policy,<br />
tick ‘YES’ here and then<br />
complete 9, 9a and 9d.<br />
If the patient does not have OHI<br />
policy, section 9 can be left blank.<br />
Enter the sponsor’s DOB,<br />
using the format MM DD YY<br />
and indicate the sponsor’s<br />
gender marking either M for<br />
Male or F for Female.<br />
SECTIoN 5<br />
<strong>Provider</strong> Claims Information<br />
Fields highlighted in green<br />
can be left blank<br />
59
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Part 2: Patient’s Signature<br />
These two fields require the signature of the patient.<br />
• The patient and the insured party can be the same person. Even if the patient is not the Active Duty Service Member, the Active Duty Family<br />
Member is an eligible <strong>TRICARE</strong> beneficiary and considered the insured party.<br />
• The requirement for signature can be met by obtaining a ‘Signature on File’. This means the <strong>Provider</strong> will have the patient’s signature on file<br />
(collected at ‘registration’ at the <strong>Provider</strong> facility or at first appointment).<br />
• If the patient is incapable of signing or under 18 years of age, the parent or legal guardian’s signature will be kept on file.<br />
• Signature on File: International SOS will assist <strong>Provider</strong>s with education on how to obtain this in the correct manner and which wording to<br />
include in collecting the signature. <strong>Provider</strong>s will then simply write ‘Signature on File’ in BOTH fields and will not be required to obtain the<br />
beneficiary’s or insured’s signature when completing the Claim Form.<br />
• Laboratories: if the patient is not present, the laboratory should enter ‘Patient not Present’ on the line in both signature fields.<br />
• Ambulance Companies: Enter 'Patient Unable to Sign' on the line in both signature fields.<br />
IMPoRTANT NoTE: Both boxes must be signed and completed!<br />
An example ‘Signature on File’ letter:<br />
60
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Part 3: Authorization Number<br />
If you are not able to include the diagnosis on the<br />
invoice, you can write it here. If the diagnosis is on<br />
the invoice, leave this field blank. The diagnosis can<br />
be a written description or an ICD or CPT Code.<br />
Please enter the appropriate<br />
Authorization Number. This can be<br />
found on the top right corner of the<br />
Authorization Form.<br />
The rest of this information should be on the Itemized Invoice which must be submitted with the Claim Form.<br />
Fields highlighted in green<br />
can be left blank<br />
SECTIoN 5<br />
<strong>Provider</strong> Claims Information<br />
61
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Emergency Care<br />
If the <strong>Provider</strong> is providing Emergency Care, they will not necessarily have an<br />
Authorization Number. In this case, the <strong>Provider</strong> should write the words<br />
‘Emergency Care’ in this section.<br />
EMERGENCY CARE<br />
62
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Part 4: <strong>Provider</strong>’s Details<br />
The ‘Federal Tax ID Number’ is the<br />
<strong>Provider</strong>’s <strong>TRICARE</strong> ID Number<br />
(or TEPRV). Please enter this here.<br />
Always indicate ‘Yes’ here. This<br />
ensures that payment goes to the<br />
<strong>Provider</strong>.<br />
If the patient has OHI, it will be the primary payer<br />
for the claim. After the OHI has processed the<br />
claim, indicate here how much they have paid.<br />
Also include any payments the patient has made<br />
towards the claim. If <strong>TRICARE</strong> is the patient’s only<br />
health insurance plan, leave this field blank.<br />
This must be signed and<br />
dated by the <strong>Provider</strong>.<br />
This does not<br />
necessarily have to be<br />
the attending physician,<br />
but can be signed by an<br />
authorized person.<br />
Note: The <strong>Provider</strong><br />
‘Signature on File’<br />
procedure can be<br />
used here.<br />
Please enter the<br />
patient’s account<br />
number. This is<br />
generated by the<br />
<strong>Provider</strong> and<br />
should not be<br />
longer than 18<br />
digits long.<br />
Please enter<br />
the <strong>Provider</strong>’s<br />
name and full<br />
physical<br />
address.<br />
Fields highlighted in green<br />
can be left blank<br />
Please enter the<br />
<strong>Provider</strong>’s full billing<br />
address if different to<br />
the physical address.<br />
SECTIoN 5<br />
<strong>Provider</strong> Claims Information<br />
63
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Completing the UB-04<br />
PART 1<br />
<strong>Provider</strong>’s Details<br />
{<br />
{<br />
{ { {<br />
PART 2<br />
Patient’s Details<br />
and Address<br />
PART 3<br />
This can be left<br />
blank as long as<br />
an Itemized<br />
Invoice is<br />
submitted<br />
PART 4<br />
Sponsor’s Details<br />
and Authorization<br />
Number<br />
PART 5<br />
Diagnosis and<br />
<strong>Provider</strong> Signature<br />
64
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
The Pre-Populated Claim Form UB-04<br />
When you receive<br />
an Authorization<br />
Form from<br />
International SOS,<br />
you will also<br />
receive a<br />
pre-populated<br />
Claim Form.<br />
All the fields<br />
highlighted in<br />
purple will be<br />
pre-populated.<br />
All the fields<br />
highlighted in<br />
green can be<br />
left blank.<br />
You will only have<br />
to complete these<br />
few fields shown<br />
here in white.<br />
SECTIoN 5<br />
<strong>Provider</strong> Claims Information<br />
65
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Part 1: <strong>Provider</strong>’s Details<br />
Please enter the Patient’s account number.<br />
This is generated by the <strong>Provider</strong> and<br />
should not be longer than 18 digits long.<br />
Please enter the<br />
<strong>Provider</strong>’s name<br />
and full physical<br />
address.<br />
Please enter the<br />
<strong>Provider</strong>’s full billing<br />
address if different<br />
to the physical<br />
address.<br />
The ‘Federal Tax<br />
Number’ is the<br />
<strong>Provider</strong>’s <strong>TRICARE</strong> ID<br />
Number (or TEPRV).<br />
Please enter this here.<br />
Part 2: Patient’s Details and Address<br />
Enter the patient’s name, using the format Last<br />
Name, First Name, Middle Initial and the patient’s<br />
full physical address including post code.<br />
Please enter the<br />
patient’s DOB<br />
using the format<br />
MM DD YY and<br />
write M or F to<br />
indicate the<br />
patient’s gender.<br />
Enter the<br />
sponsor’s name<br />
and full address<br />
if different than<br />
the patient’s.<br />
66
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Part 3: This section can be left blank, as long as an Itemized Invoice is submitted<br />
This information should be on the Itemized Invoice which must be submitted with the Claim Form.<br />
Part 4: Sponsor’s Details and Authorization Number<br />
If the patient has OHI, enter the name<br />
of the insured party using the format<br />
Last Name, First Name, Middle Initial<br />
and the policy number.<br />
Always indicate ‘Y’ for ‘Yes’<br />
here. This ensures that<br />
payment goes to the <strong>Provider</strong>.<br />
If the patient has OHI, it will be the primary payer for the claim.<br />
After the OHI has processed the claim, indicate here how<br />
much they have paid. Also include any payments the patient<br />
has made towards the claim. If <strong>TRICARE</strong> is the patient’s only<br />
health insurance plan, leave this field blank.<br />
SECTIoN 5<br />
<strong>Provider</strong> Claims Information<br />
Please enter the appropriate<br />
Authorization Number. This can<br />
be found on the top right corner<br />
of the Authorization Form.<br />
Enter the sponsor’s name using the format Last Name, First<br />
Name, Middle Initial and the sponsor’s ID number (SSN or the<br />
first 9 digits of the DOD Benefits Number). This information will<br />
appear on the patient’s Military ID Card.<br />
67
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Emergency Care<br />
If the <strong>Provider</strong> is providing Emergency Care, they will not necessarily have an<br />
Authorization Number. In this case, the <strong>Provider</strong> should write the words<br />
‘Emergency Room’ in this section.<br />
EMERGENCY ROOM<br />
Part 5: Diagnosis and <strong>Provider</strong> Signature<br />
If you are not able to include the diagnosis on the invoice, you can<br />
write it here. If the diagnosis is on the invoice, leave this field blank.<br />
This must be signed and dated by the <strong>Provider</strong>. This does not necessarily have<br />
to be the attending physician, but can be signed by an authorized person.<br />
Note: The <strong>Provider</strong> ‘Signature on File’ procedure can be used here.<br />
68
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
SECTIoN 6:<br />
The <strong>Provider</strong> Portal<br />
Registering to the <strong>Provider</strong> Portal<br />
In order to access the <strong>Provider</strong> Portal on www.tricare-overseas.com the <strong>Provider</strong> will need to become a registered user first and set up a<br />
unique username and password.<br />
Note: Please visit www.tricare-overseas.com/provider.htm to download a Computer Based Training Module on Web-based Claim<br />
Submission options.<br />
To begin the registration process, go to the <strong>Provider</strong>s section of www.tricare-overseas.com<br />
and click on ‘Register’.<br />
Your <strong>TRICARE</strong> overseas <strong>Program</strong> (ToP) <strong>Provider</strong> Number<br />
You will advance to the TOP<br />
<strong>Provider</strong> Number page. Enter<br />
your TOP <strong>Provider</strong> Number in the<br />
open field (this is a required<br />
field). If you do not know your<br />
TOP <strong>Provider</strong> Number, it can be<br />
found in your <strong>TRICARE</strong> <strong>Overseas</strong><br />
Explanation of Benefits (EOB)<br />
(see example above).<br />
The <strong>Provider</strong> must enter their <strong>Provider</strong> ID Number (or TEPRV) –<br />
this is a number assigned to the <strong>Provider</strong> by International SOS<br />
and appears in the following format: DEU123456DEU A000.<br />
The <strong>Provider</strong> ID Number is indicated at the top of the Explanation<br />
of Benefits (EOB), which you may have received from<br />
International SOS.<br />
If you have not yet received an EOB for a <strong>TRICARE</strong> beneficiary,<br />
please contact your TOP Regional Call Center and press option<br />
#5 to speak with a member of the TOP <strong>Provider</strong> Support Services<br />
team, who can provide you with your TOP <strong>Provider</strong> ID Number.<br />
After entering your TOP <strong>Provider</strong> ID Number, click ‘Next.’<br />
SECTIoN 6<br />
The <strong>Provider</strong> Portal<br />
69
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
<strong>Provider</strong> Information<br />
The <strong>Provider</strong> must enter their<br />
contact information, including full<br />
name, and contact telephone<br />
number (optional). <strong>Provider</strong>s will<br />
also be required to enter a valid<br />
email address where they can be<br />
contacted. Updates such as<br />
password information will be sent<br />
to this address.<br />
On the ‘<strong>Provider</strong> Information’ page you will enter the name and<br />
contact information of the <strong>TRICARE</strong> <strong>Overseas</strong> <strong>Program</strong> (TOP)<br />
<strong>Provider</strong>. All fields on this page are required for registration.<br />
■ Language Preference: The language preference field<br />
determines the site language when you have logged into your<br />
Secure <strong>Provider</strong> Claims Portal account.<br />
– Note: This preference can be changed at a later date<br />
in your personal profile.<br />
■ First Name: Enter the first name of the <strong>Provider</strong>.<br />
– Note: This field has a 25 character limit.<br />
■ Last Name: Enter the last name of the <strong>Provider</strong>.<br />
– Note: This field has a 35 character limit.<br />
■ Telephone Number: Enter the 3-digit international country<br />
code in the first field and the remaining digits of the contact<br />
telephone number in the second field.<br />
■ Email Address and Confirm Email Address: Enter the<br />
contact email address in the first field. Then validate the<br />
contact email address by entering it again in the ‘Confirm<br />
Email Address’ field.<br />
<strong>Provider</strong>s located in the United States and U.S. territories will<br />
additionally be required to provide one of the following:<br />
■ License Number<br />
■ Medicare Certification Number<br />
■ National <strong>Provider</strong> Identifier<br />
Click ‘Next’ to continue the registration process.<br />
70
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
<strong>Provider</strong> Registration Type<br />
Choose the ‘Registration Type.’<br />
Registration options are included on the drop down menu, and<br />
include the following:<br />
1.) Complete a secure instant registration on the site<br />
2.) Complete the registration process by mail<br />
To complete a secure instant registration on the site, <strong>Provider</strong>s<br />
must have had a claim processed within the last 365 days with<br />
the <strong>TRICARE</strong> <strong>Overseas</strong> <strong>Program</strong> (TOP) Claims Processor.<br />
If this is your preferred method of registration, verify the<br />
registration drop down field displays the 'I would like to complete<br />
a secure instant registration' option.<br />
For ‘Secure Instant Registration’ <strong>Provider</strong>s are required to enter a<br />
claim number (also known as the Internal Control Number (ICN))<br />
from their TOP Explanation of Benefits (EOB) and the date of birth<br />
(DOB) of the patient on that claim. See diagram below.<br />
Note: <strong>Provider</strong>s can use any claim number from within the last 365 days.<br />
Once you complete the required ‘Instant Registration’ fields, click ‘Next.’<br />
If you have not submitted a claim to the <strong>TRICARE</strong> <strong>Overseas</strong> <strong>Program</strong> in the last 365 days, or if you prefer to complete registration by mail,<br />
choose the 'I would like to complete registration by mail' option from the drop down menu and click ‘Next.’<br />
SECTIoN 6<br />
The <strong>Provider</strong> Portal<br />
71
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Instant Registration: Account Username and Password<br />
Your password cannot contain spaces and cannot<br />
be the same as your first name, last name or the<br />
Username you have selected for your account.<br />
You can click on the ‘Password Rules’ button for the<br />
full list of requirements and regulations connected<br />
to passwords on www.tricare-overseas.com<br />
After choosing ‘Secure Instant Registration’, you will be taken to<br />
the ‘Username and Password’ page.<br />
The ‘Username’ page is where you will choose your account<br />
name and set up your account security. All fields on this page<br />
are required.<br />
Username: Enter the Username of your choice for your account.<br />
The Username must be a minimum of 5 characters long and<br />
cannot be more than 32 characters long.<br />
The site will validate your Username, displaying confirmation in<br />
green text if the Username you’ve selected is available for your<br />
account. The validation text will turn red if the Username you are<br />
trying to enter is already in use.<br />
72
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Password: Enter the security password for your account. Your<br />
password must be a minimum of 9 characters long and must<br />
contain the following:<br />
■ 2 numbers<br />
■ Any 2 of the following special characters<br />
— ! exclamation point<br />
— @ at sign<br />
— # hashtag, pound sign, or number symbol<br />
— $ dollar sign<br />
— % percent sign<br />
— & ampersand<br />
— * asterisk<br />
— _ underscore<br />
— + plus sign<br />
— , comma<br />
— ? question mark<br />
■ 2 lower case characters<br />
■ 2 capital or upper case characters<br />
Confirm Password: Validate your chosen password by entering<br />
it a second time.<br />
Security Question: Select a security question from the options<br />
available in the drop down menu.<br />
Security Answer: Provide the answer to the security question<br />
you have just chosen.<br />
Note: Your security answer cannot be more than 32 characters<br />
in length.<br />
You must read the ‘Terms and Conditions’<br />
and then click on the box next to this<br />
section, stating that you have read and<br />
accept the ‘Terms and Conditions’ before<br />
proceeding to the next step.<br />
Click ‘Next’ to continue.<br />
SECTIoN 6<br />
The <strong>Provider</strong> Portal<br />
73
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Instant Registration: Confirmation<br />
If you wish to change<br />
any information prior to<br />
submission, click the<br />
‘Edit’ buttons here.<br />
If all the information is<br />
valid and correct, click<br />
the ‘Complete<br />
Registration’ button and<br />
you will be logged in to<br />
your new account on<br />
www.tricareoverseas.com<br />
Next, you will come to the Instant Registration ‘Confirmation’<br />
page. This page displays the <strong>Provider</strong> information and Username<br />
and security question and answer you entered for your account.<br />
Note: <strong>Provider</strong>s in the United States and U.S. territories will see<br />
an additional ‘Confirmation’ field with the License Number,<br />
Medicare <strong>Provider</strong> Number, or National <strong>Provider</strong> Identifier you<br />
entered on the ‘<strong>Provider</strong> Information’ page.<br />
74
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Registration By Mail: Account Username and Password<br />
After choosing ‘Registration by Mail’, you will be taken to the<br />
‘Username’ page where you will set up some of the features for<br />
your account and account security. All fields on this page are<br />
required.<br />
Start by choosing the ‘Username’ for your account.<br />
The Username must be between 5 and 32 characters in length.<br />
The site will validate your Username, displaying confirmation in<br />
green text if the Username you want is available for your account.<br />
The validation text will turn red if the Username you are trying to<br />
enter is already in use.<br />
You will then choose a security question from the drop down<br />
menu.<br />
In the ‘Security Answer’ field, enter the answer to the question<br />
you selected.<br />
Note: Your security answer cannot be more than 32 characters<br />
in length.<br />
Click ‘Next.’<br />
SECTIoN 6<br />
The <strong>Provider</strong> Portal<br />
75
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Registration By Mail: Confirmation<br />
The website will display ‘Confirmation’ of the registration by<br />
displaying the name and address we have on file for the<br />
<strong>Provider</strong> number you’ve entered.<br />
By mail, the TOP Claims Customer Service Department will<br />
send to you (using the address displayed on screen) a<br />
password and instructions for logging in to your account on<br />
www.tricare-overseas.com<br />
The password and instructions should arrive within 7–10<br />
business days.<br />
You can then use these instructions and password to access<br />
your new account.<br />
76
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Using the <strong>Provider</strong> Portal<br />
Using the <strong>Provider</strong> Portal: The <strong>Provider</strong> Dashboard<br />
The ‘<strong>Provider</strong> Dashboard’ is your landing page. It is the first page<br />
you will see after logging in to your secure account. The ‘<strong>Provider</strong><br />
Dashboard’ provides you with a quick view of important Alerts<br />
and Announcements and also contains all your recent claims<br />
activity, including recent payment, returned claims, and pending<br />
claims. You can also check <strong>TRICARE</strong> beneficiary eligibility and<br />
Other Health Insurance from the ‘<strong>Provider</strong> Dashboard.’<br />
Note: There is a ‘What is My Dashboard?’ link available at the top<br />
of the dashboard page. You can click this link to view a quick<br />
explanation of the content and features available on the ‘<strong>Provider</strong><br />
Dashboard.’<br />
SECTIoN 6<br />
The <strong>Provider</strong> Portal<br />
77
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Using the <strong>Provider</strong> Portal: The <strong>Provider</strong> Dashboard: Alerts and Announcements<br />
Check the ‘Alerts and Announcements’ box to see<br />
when your current password is scheduled to expire.<br />
You can click on the day-remaining link, which will<br />
take you to the ‘Password Update’ function in the<br />
Secure <strong>Provider</strong> Claims Portal.<br />
The first section of your ‘<strong>Provider</strong> Dashboard’ is a quick view of<br />
Alerts and Announcements.<br />
If you are an account administrator, in addition to password<br />
notifications you will see alerts for pending location approval<br />
requests and pending user requests. The location approval<br />
request and user request alerts are static – they will always<br />
display in your Alerts section.<br />
Each alert will be accompanied by a number indicating how<br />
many pending requests of each type there are. If there are no<br />
pending requests, the number field will display 0 (zero). The<br />
number field is a link you can click to take you to the<br />
administration page for each function.<br />
78
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Using the <strong>Provider</strong> Portal: The <strong>Provider</strong> Dashboard: Notifications<br />
An Important Notifications page may appear as a splash screen when you first log in.<br />
These are important site-wide messages from the TOP Claims Customer Service Department. Topics range from changes in<br />
requirements in <strong>TRICARE</strong> <strong>Overseas</strong> <strong>Program</strong> policies and procedures to notices about www.tricare-overseas.com secure claims<br />
portal features and functionality.<br />
Be sure to review the notifications before closing the splash page.<br />
To close the notifications splash page, click OK or click the ‘X’ in the upper right-hand corner of the notification window.<br />
SECTIoN 6<br />
The <strong>Provider</strong> Portal<br />
79
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Using the <strong>Provider</strong> Portal: The <strong>Provider</strong> Dashboard: Check Patient Eligibility<br />
The ‘Check Patient Eligibility’ button can be found on the ‘<strong>Provider</strong> Dashboard’ and can be used as a quick link to begin a Beneficiary eligibility<br />
check. You can conduct a Beneficiary eligibility check using either the Sponsor Social Security Number (SSN) or DEERS Family ID.<br />
Once you make a selection, complete the remaining fields in this section and then click the ‘Submit’ button.<br />
The Beneficiary eligibility search will begin and then take you to the ‘Patient Eligibility’ page to view the results.<br />
80
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Using the <strong>Provider</strong> Portal: The <strong>Provider</strong> Dashboard: Recent Payments View<br />
The ‘<strong>Provider</strong> Dashboard’ gives you immediate access to your<br />
most recent claims activity data in three convenient tabs:<br />
1. Recent Payments<br />
2. In-Process Claims<br />
3. Returned Claims<br />
The ‘<strong>Provider</strong> Dashboard’ defaults to the ‘Recent Payments’ tab,<br />
showing you data for your first registered location for the previous<br />
calendar week. You can use the ‘Location’ filter to choose another<br />
location if you have more than one registered location with<br />
www.tricare-overseas.com.<br />
You can also use the ‘View’ filter to choose an alternate time<br />
period of 30 days, 60 days, or 90 days. Each tab defaults to 50<br />
records per page. If you have more than 50 records, there will be<br />
a page selection and arrow navigation to allow you to move<br />
through multiple pages.<br />
Note: In each view the data can be sorted by clicking on the<br />
column heading. Displayed data cannot be sorted by the<br />
currency type.<br />
SECTIoN 6<br />
The <strong>Provider</strong> Portal<br />
81
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Recent Payments: The Recent Payment view provides the following information:<br />
■ CHECK/EFT/ACH Number: Displays the number assigned to the check or electronic payment transaction made via either Electronic<br />
Fund Transfer (EFT) or Automated Clearing House (ACH). Electronic payment transaction numbers are preceded by an asterisk.<br />
■ Approval Date: This is the date the check was issued or the date the electronic payment was made. This appears in MM/DD/YYYY<br />
format.<br />
■ Payment Amount: This displays the full reimbursement amount made in the check or electronic payment transaction.<br />
■ Currency: Displays the code representing the currency in which the payment was made.<br />
■ View Claims: This field provides a link to a detailed view of all your claims that were part of that reimbursement.<br />
When you click on the ‘View Claims’ link, the screen will<br />
automatically update to display the ‘Claim View.’<br />
The ‘Claim View’ provides the following details:<br />
■ EoB: This is a link to an image of your <strong>TRICARE</strong> <strong>Overseas</strong><br />
<strong>Program</strong> (TOP) Explanation of Benefits (EOB) for the claim on<br />
this line. You will be able to view the EOB in either a summary<br />
payment format (.pdf document) or a detailed individual claim<br />
format (.html).<br />
■ Letters: If there was any correspondence or documentation<br />
attached to this claim transaction, the documentation can be<br />
viewed by clicking on the ‘Letters’ link.<br />
■ Invoice Number: If you added an office invoice or record<br />
number to your claim during the online claims submission<br />
process or when you submitted a claim via postal mail, this<br />
number will be displayed here.<br />
■ Date of Service: This field will display the earliest date of<br />
service on the claim. The date format is MM/DD/YYYY.<br />
■ Claim Number: This is the TOP control number assigned to<br />
your claim for processing and tracking on the Secure Claims<br />
<strong>Provider</strong> Portal.<br />
■ Patient Name: Displays the full name of the patient on the<br />
claim.<br />
■ Billed Amount: This field displays the sum of all charges that<br />
were submitted on this claim.<br />
■ Currency: This field displays the code representing the<br />
currency in which the claim transaction was processed.<br />
■ <strong>Provider</strong> Name: Displays the name of the individual provider<br />
or the facility name.<br />
■ Tax ID: Displays the 9-digit tax identification number of the<br />
<strong>Provider</strong>. For <strong>Provider</strong>s outside the 50 United States and the<br />
U.S. territories, this is an identification number assigned to the<br />
<strong>Provider</strong> by the <strong>TRICARE</strong> <strong>Overseas</strong> <strong>Program</strong>.<br />
82
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
■ Paid by Government: This field displays the amount of<br />
payment the <strong>TRICARE</strong> benefit program covers and<br />
reimbursed or paid on the claim.<br />
■ Process Date: This field displays the date the claim<br />
processing was finalized in our system (i.e., by the TOP<br />
Claims Processor).<br />
You can also click the ‘Plus’ (+) symbol at the start of each line to expand additional details about the claim.<br />
Information about these additional claim details is available in the ‘Claim Status’ demonstration, also available on the Secure <strong>Provider</strong><br />
Claims Portal.<br />
Clicking the ‘Back’ button will return you to the ‘Recent Payments’ dashboard summary view.<br />
SECTIoN 6<br />
The <strong>Provider</strong> Portal<br />
83
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Using the <strong>Provider</strong> Portal: The <strong>Provider</strong> Dashboard: In-Process Claims View<br />
In-Process Claims: In-Process Claims shows you the claims you<br />
have submitted and are currently being processed by the TOP<br />
Claims Customer Service Department.<br />
The ‘In-Process View’ provides the following information:<br />
■ Invoice Number: If you added an invoice or record number to<br />
your claim during the ‘Online Claims Submission’ process or<br />
when you submitted a claim via postal mail, this number will<br />
be displayed here.<br />
■ Date of Service: This field displays the earliest date of service<br />
on the claim. The date format is MM/DD/YYYY.<br />
■ Claim Number: This is the <strong>TRICARE</strong> <strong>Overseas</strong> <strong>Program</strong><br />
control number assigned to your claim for processing and<br />
tracking on the Secure Claims <strong>Provider</strong> Portal.<br />
■ Patient Name: Displays the full name of the patient on the<br />
claim.<br />
■ Billed Amount: This field displays the sum of all charges that<br />
were submitted on this claim.<br />
■ Currency: This field displays the code representing the<br />
currency in which the claim transaction was processed.<br />
■ <strong>Provider</strong> Name: Displays the name of the individual provider<br />
or the facility name.<br />
■ Tax ID: Displays the 9-digit tax identification number of the<br />
<strong>Provider</strong>. For <strong>Provider</strong>s outside the 50 United States and the<br />
U.S. territories, this is an identification number assigned to the<br />
<strong>Provider</strong> by the <strong>TRICARE</strong> <strong>Overseas</strong> <strong>Program</strong>.<br />
Note: There is no expanded view for In-Process Claims. These<br />
claims are still being worked on by the TOP Claims Customer<br />
Service Department, so processing details are not yet available.<br />
84
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Using the <strong>Provider</strong> Portal: The <strong>Provider</strong> Dashboard: Returned Claims View<br />
Returned Claims: The Returned Claims tab shows claims that<br />
you have submitted but were returned to you by the TOP Claims<br />
Customer Service Department because information was missing,<br />
which was needed for accurate claims processing and payment.<br />
The Returned Claims view provides the following information:<br />
■ Claim Number: This is the <strong>TRICARE</strong> <strong>Overseas</strong> <strong>Program</strong><br />
control number assigned to your claim for processing and<br />
tracking on the Secure Claims <strong>Provider</strong> Portal.<br />
■ Patient Name: Displays the last name and first name of the<br />
patient on the claim.<br />
■ Billed Amount: This field displays the sum of all charges that<br />
were submitted on this claim.<br />
■ Currency: This field displays the code representing the<br />
currency in which the claim transaction was processed.<br />
■ <strong>Provider</strong> Name: Displays the name of the individual provider<br />
or the facility name.<br />
■ Tax ID: Displays the 9-digit tax identification number of the<br />
<strong>Provider</strong>. For <strong>Provider</strong>s outside the 50 United States and the<br />
U.S. territories, this is an identification number assigned to the<br />
<strong>Provider</strong> by the <strong>TRICARE</strong> <strong>Overseas</strong> <strong>Program</strong>.<br />
■ Date of Service: This field displays the earliest date of<br />
service on the claim.<br />
■ Invoice Number: If you added an invoice or record number to<br />
your claim during the ‘Online Claims Submission’ process or<br />
when you submitted a claim via postal mail, this number will<br />
be displayed here.<br />
■ Claim Status: This will display ‘Returned.’<br />
You can also click the ‘Plus’ (+) symbol at the start of each line to<br />
expand additional details about the claim. Some additional<br />
information you will find in the expanded view includes the<br />
‘Reason Returned’ field, which is a brief summary explaining why<br />
the claim was returned to you, and a link to a .pdf version of the<br />
letter sent to you (along with the returned claim) explaining in<br />
detail why the claim was returned.<br />
SECTIoN 6<br />
The <strong>Provider</strong> Portal<br />
85
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Claim Status<br />
Using the <strong>Provider</strong> Portal: Claim Status: Basic Search<br />
The ‘Basic Search’ allows you to<br />
search for your claim information<br />
by your registered locations,<br />
including an option for all<br />
locations.<br />
The default selection is 'All<br />
Locations' but you can select a<br />
specific location from the drop<br />
down menu.<br />
If the location you want to look up<br />
is not on the drop down menu,<br />
you can register this new location<br />
by selecting the 'Request a New<br />
Location' link.<br />
The ‘Claim Status’ function allows you to search for claim<br />
information and data for claims you have submitted to the TOP<br />
Claims Customer Service Department.<br />
Note: The ‘Claim Status’ function has a 500-claim limit for search<br />
returns and can only return claim data for the last 18 months<br />
(based on when the claim is processed). Please select the<br />
appropriate criteria to filter your search to improve search return<br />
and portal performance.<br />
Next, select the cross-reference search type you would like to<br />
perform.<br />
The choices here include:<br />
■ Patient Information: Selecting Patient Information allows you<br />
to input the data to find claims you submitted for a specific<br />
patient. Complete the following fields:<br />
— Sponsor Social Security Number (SSN): Enter the patient’s<br />
benefit eligibility number.<br />
— Patient First Name: Provide the patient’s first name.<br />
— Date of Birth: Enter the patient’s date of birth. The date<br />
format is MM/DD/YYYY.<br />
— Service Start/End Date: The system will default the service<br />
date fields to the last 30 days. If necessary, you can<br />
change this by typing new dates directly into these fields<br />
or by using the calendar icons to select new dates.<br />
— Claim Number: Selecting the Claim Number allows you to<br />
enter the full 14-digit number assigned to your claim and<br />
search for its status. Claim numbers are assigned<br />
immediately to your claims when you submit them using<br />
the Online Claims submission method on www.tricareoverseas.com<br />
■ Check Number: Selecting the Check Number allows you to<br />
enter the full 11-character check number and search for<br />
claims processed under that check. Check numbers will<br />
appear on your Electronic Funds Transfer (EFT) or Automated<br />
Clearing House (ACH) credit advice, your weekly claim<br />
summary reports, and your dashboard. You can also find the<br />
86
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
check number in the claim detail financial summary section.<br />
Note: When searching with an EFT or ACH check number, you must include the asterisk as the first character.<br />
■ Invoice Number: Selecting the Invoice Number allows you to search for a claim with the identification code you have assigned to the<br />
claim. The Invoice Number search works for claims you have submitted, for which you have also entered an invoice identification code.<br />
Note: The Invoice Number search is limited to 20 characters maximum.<br />
Note: There is a ‘Reset Search’ button which will clear the entire page of any inputs or selected options, if needed.<br />
Once you are satisfied with the search criteria entered, click the ‘Search’ button to perform the location and patient search.<br />
Using the <strong>Provider</strong> Portal: Claim Status: Advanced Search<br />
Selecting the ‘Advanced Search’ tab gives you several additional<br />
search options, which include:<br />
■ Individual Patient DEERS Family ID: Selecting this option<br />
allows you to search for a patient’s claim data by their 9-digit<br />
DEERS Family Identification Number. This option also requires<br />
that you enter the patient’s name, date of birth, and a selected<br />
date span for the claim search.<br />
■ Individual Patient DoD Benefits Number (DBN): Selecting<br />
this option allows you to search for a patient’s claim data by<br />
87<br />
their 10-digit DOD Benefits Number. This option also requires<br />
that you enter the patient’s name, date of birth, and a selected<br />
date span for the claim search.<br />
■ Process Date: Selecting this option allows you to enter a<br />
specific date and view all claims processed on that date. The<br />
date can be typed directly into the field in the MM/DD/YYYY<br />
format or it can be selected using the calendar icon.<br />
■ All Patients: Selecting this option allows you to search for<br />
and view claim data for all patients as cross-referenced with<br />
the selected provider location(s).<br />
SECTIoN 6<br />
The <strong>Provider</strong> Portal
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Using the <strong>Provider</strong> Portal: Claim Status: Claim Search Results<br />
Near the top of the ‘Claim Search Results’ page is a notice<br />
asking if you would like to view any linked documentation<br />
in your ‘Search Results’ claim details.<br />
Note: You will need Adobe Reader. If you do not have<br />
Adobe Reader on your computer, you can download the<br />
program by clicking on the ‘Adobe Reader’ link.<br />
Immediately following the notice are buttons<br />
labeled ‘Edit Search’ or ‘New Search’. If the<br />
search you performed does not show the results<br />
you wanted, you can click ‘Edit Search’, which<br />
will take you back to the Claim Search screen<br />
where you previously entered your search<br />
criteria. Or you can click on ‘New Search’ which<br />
will take you to the blank Claim Search screen<br />
where you can enter your search criteria.<br />
The screen will update to display your search results. The number of results you receive for any search will depend on the type of claim<br />
search performed and the number of claims you have submitted to the TOP Claims Customer Service Department in the last 30 months<br />
(based on when the claim is processed).<br />
The criteria for the search you just performed will appear immediately above your ‘Claim Search Results’ so that you can verify if the<br />
search was performed with the criteria you intended. If the criteria shown are not correct, you can click the ‘Edit Search’ button to modify<br />
the criteria and perform a new search.<br />
The ‘Location’ filter gives you the option to sort your ‘Claim Search Results’ by Tax ID and Zip Code.<br />
Note: There is a paging index that allows you to advance through multiple pages of ‘Claim Search Results.’ Click a page number to<br />
advance to that page or use the arrows to navigate through the ‘Claim Search Results’ one page at a time.<br />
88
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
The ‘Claim Search Results’ box will list all claims that fit the<br />
criteria you selected for the search. The immediate search results<br />
display the following fields for each claim returned in the search:<br />
■ Expand/Contract: This button allows you to display and hide<br />
additional details and functions for the claim specific to that<br />
‘Claim Search Result’ line.<br />
■ Explanation of Benefits (EoB): If an EOB has been<br />
generated for the claim, an icon linking to an Adobe .pdf<br />
version of the EOB will appear in this field.<br />
■ Letters: If additional documentation has been generated by<br />
the TOP Claims Customer Service Department while<br />
processing your claim, an icon linking to an Adobe .pdf<br />
version of this documentation will appear in this field.<br />
■ Invoice Number: This field will display your office Invoice<br />
Number for the claim if you provided one during the Online<br />
Claims submission process or for a claim that you have<br />
submitted via postal mail.<br />
■ Date of Service: This field displays the end date for services<br />
listed on the claim. This field displays in the MM/DD/YYYY<br />
format.<br />
■ Claim Number: This field displays the 14-digit claim control<br />
number assigned to your claim when it was received by the<br />
TOP Claims Customer Service Department.<br />
■ Patient Name: This field displays the last name and first name<br />
of the patient on the claim.<br />
■ Claim Status: This field displays the current status of your<br />
claim (i.e., where the claim is in the process of being handled<br />
by the TOP Claims Customer Service Department). Possible<br />
‘Claim Status’ values include:<br />
■ Currency: This field displays the currency code in which the<br />
claim the claim transaction was processed.<br />
Note: A currency code does not indicate there was a payment<br />
on the claim.<br />
■ Process Date: This field will display the date on which the<br />
TOP Claims Customer Service Department took final action on<br />
the claim. If the claim status is In-Process, this field will be left<br />
blank. The date displays in the MM/DD/YYYY format.<br />
Note: You can expand a claim's record to see more details about<br />
how the claim was processed. Click the ‘Plus’ (+) symbol at the<br />
start of the record line to view the summary payment details.<br />
The expanded record's payment details are presented in 4<br />
columns:<br />
■ The first two columns detail the financial information for the<br />
claim:<br />
— The billed amount, the ‘Paid by Government’ amount, to<br />
whom the payment was directed (if a payment was made),<br />
and any beneficiary liability.<br />
— The third column gives the information for the <strong>Provider</strong> of<br />
services on record for the claim, including the individual or<br />
facility name and address.<br />
— The fourth column lists the check details, including the<br />
check or EFT transaction number, the issue date, and the<br />
payee (i.e., individual or facility recipient) of the payment.<br />
Clicking the ‘Full Claim Detail’ button gives you access to patient<br />
detail information and claim line item detail information.<br />
Note: Claim line item detail information is not available for claims<br />
that are labeled ‘In-Process.’<br />
— In-Process<br />
— Payment<br />
— No Payment<br />
— Adjustment<br />
— Reissue<br />
— Credit<br />
■ Billed Amount: This field displays the sum of all charges that<br />
were submitted on this claim.<br />
■ Paid by Government: This field displays the amount of<br />
payment the <strong>TRICARE</strong> benefit program covers and<br />
reimbursed or paid on the claim to the <strong>Provider</strong> and/or patient.<br />
This field will display all zeroes (00000) if the claim is In-<br />
Process or No Payment could be made on the claim.<br />
SECTIoN 6<br />
The <strong>Provider</strong> Portal<br />
89
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Using the <strong>Provider</strong> Portal: Claim Status: Claim Search Details<br />
Historical details for each of these<br />
items include:<br />
- Eligibility<br />
- Other Health Insurance<br />
- Out-of-Pocket Expenses<br />
- Primary Care Manager<br />
Clicking the ‘Plus’ (+) symbol to expand the ‘Patient Eligibility’ section will allow you to see the patient's eligibility and benefit information<br />
corresponding to the dates of service of the claim.<br />
The eligibility record will display any records of any insurance program the beneficiary may have in addition to <strong>TRICARE</strong> and the dates<br />
that insurance program is effective. Out-of-Pocket expenses are also detailed here.<br />
Note: Financial values here will be up-to-date with the most recent claim processed for the beneficiary, but ‘In-Process’ claim values will<br />
not have been calculated against these benefits. Also, please note that all values appearing here are given in $USD (United States<br />
Dollars).<br />
Current Primary Care Manager information will be given in the third column.<br />
90
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Using the <strong>Provider</strong> Portal: Claim Status: Claim Search Details<br />
Clicking the ‘Plus’ (+) symbol to expand the ‘Claim Line Items’<br />
section allows you to see details for each service, procedure or<br />
supply you billed for on the claim.<br />
Details will be listed using the following fields:<br />
■ Service Description: Displays the code and partial<br />
description for the service, procedure, or supply.<br />
■ Reason Code: This is a 3-character code indicating<br />
message from the TOP Claims Customer Service Department<br />
explaining claim processing actions take for that service,<br />
procedure or supply. You can select the code to view its<br />
explanation.<br />
■ Start Date, Date of Service, and End Date of Service: The<br />
dates you provided to indicate the beginning and end of the<br />
procedure.<br />
■ Billed Amount: The amount you charged for the service,<br />
procedure or supply.<br />
■ Allowed Amount: The amount <strong>TRICARE</strong> deems the<br />
maximum amount for the service, procedure or supply.<br />
■ Units: The number of times the procedure was performed or<br />
the supply provided during the dates of service.<br />
■ Invoice Number: This field will display your office Invoice<br />
Number for the claim if you provided one during the Online<br />
Claims submission process or for a claim that you have<br />
submitted via postal mail.<br />
■ <strong>Provider</strong> of Service: This field will list the name of the<br />
assigned individual <strong>Provider</strong> or facility that delivered the<br />
medical care on behalf of the beneficiary.<br />
Note: ‘Claim Line Item Details’ will not be available on claims that<br />
are labeled ‘In-Process.’<br />
Full instructions on how to submit claims via ‘Online Claim<br />
Submission’ are included in Section 5 of this TOP <strong>Provider</strong><br />
<strong>Manual</strong> (see pages 33-48).<br />
SECTIoN 6<br />
The <strong>Provider</strong> Portal<br />
91
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Using the <strong>Provider</strong> Portal: Claims Report<br />
To access the ‘Claims Report’ select<br />
the ‘Claims Report’ button in the<br />
navigation bar. This button will take<br />
you to the ‘Claims Report’ menu<br />
page (shown left).<br />
The ‘Claims Report’ page<br />
displays the selection criteria<br />
for building your report.<br />
The ‘Claims Report’ function available through the Secure Claims<br />
<strong>Provider</strong> Portal on www.tricare-overseas.com allows you to<br />
create a report of claims associated with your account up to 9<br />
weeks in the past.<br />
Criterion #1:<br />
The first criterion on the ‘Claims Report’ page is ‘Select Claim<br />
Status.’ Click the ‘Radio’ icon that corresponds with the status<br />
type you would like to view on your report. You can select one of<br />
the following:<br />
— Processed<br />
— In-Process<br />
— Returned<br />
— All<br />
You have the additional option to display individual charges in<br />
your report by clicking the check box marked ‘Display Individual<br />
Charges,’ but please note this will only apply to Processed claims<br />
(i.e., not to claims labeled ‘In-Process’ or ‘Returned.’).<br />
Criterion #2:<br />
The second criterion is the ‘Report Date Range.’<br />
Note: If you have selected ‘In-Process’ as the status type, all<br />
‘In-Process’ claims will display regardless of the date and the<br />
‘Report Date Range’ option will not be available to select.<br />
From the drop down menu, choose one of the following:<br />
■ This Week: This option is defined as being from the previous<br />
Sunday to the current day of the week. When selecting this<br />
92
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
option, the ‘From’ and ‘To’ date range fields will automatically<br />
fill with the corresponding dates and will not be available to<br />
change.<br />
■ Yesterday: This option is defined as the date prior to the<br />
current date you are running the ‘Claims Report’. When<br />
selecting this option, the ‘From’ and ‘To’ date range fields will<br />
automatically fill with the corresponding dates and will not be<br />
available to change.<br />
■ Last Week: This option is defined as being from Sunday to<br />
Saturday of the week prior to the current week. When<br />
selecting this option the ‘From’ and ‘To’ date range fields will<br />
automatically fill with the corresponding dates and will not be<br />
available to change.<br />
■ Select Date Range: This option allows you to enter the ‘From’<br />
and ‘To’ date fields. You can select a span of 7 days within the<br />
last 9 weeks to view a ‘Claims Report.<br />
Criterion #3:<br />
The third criterion is to select the <strong>Provider</strong>. You have the option to<br />
select either a single/specific Individual <strong>Provider</strong> or Institutional<br />
Facility for reporting claims data. Or, you can select all <strong>Provider</strong>s<br />
added to the account for reporting claims data.<br />
Next, select a ‘View Option’ for your report. The ‘View Option’ sets<br />
a sort order for how your claims data will display in the report.<br />
From the drop down menu, choose one of the following:<br />
— Check Number<br />
— Account or Invoice Number<br />
— Patient Name<br />
— Sponsor Number<br />
Note: Sorting the view by ‘Check Number’ is not an option when<br />
the report's claim status is either ‘In-Process’ or ‘Returned’, as<br />
there is no check generated for these statuses. Account or<br />
Invoice Number will only display if you have entered an invoice<br />
number through the Online Claim submission process.<br />
Once you have selected the criteria for your ‘Claims Report,’ click<br />
‘View Report’ to see your claim data in .html format (i.e.,<br />
displayed as a web page).<br />
Or, you can click ‘Export to Excel’ to have your ‘Claims Report’<br />
data display in Microsoft Excel. To use this option, you must have<br />
Microsoft Excel installed on your computer.<br />
The ‘Reset All’ button will set all criteria fields to their default<br />
values, thereby removing any selections you may have made<br />
prior to clicking the button.<br />
SECTIoN 6<br />
The <strong>Provider</strong> Portal<br />
93
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Using the <strong>Provider</strong> Portal: Claims Report: View Report<br />
■ Removed claims will display the following claim-specific<br />
information:<br />
(Note: Actual field order will depend on the view<br />
option selected)<br />
— Account or Invoice Number<br />
— Patient Name<br />
— Sponsor Number<br />
— Claim Number<br />
— Dates of Service<br />
— Reason for Return<br />
■ Processed claims display the following summary<br />
information:<br />
(Note: Actual field order will depend on the view<br />
option selected)<br />
The reports are formatted as follows:<br />
■ Claim dates of service are displayed in the month/day/year<br />
format. The month will be the first 3 characters of the<br />
alphabetic spelling and the year will be in a 4-digit format.<br />
■ All currency values are displayed in the <strong>Provider</strong>'s local<br />
currency and are displayed without a currency symbol or<br />
indicator. The 3-byte currency code will appear in the report<br />
header.<br />
■ In .html or web page format, claims data will be separated by<br />
the <strong>Provider</strong> attributed to the claim. In Excel format, each<br />
<strong>Provider</strong> and their corresponding claim data will display on a<br />
separate tab.<br />
■ In-Process claims will display the following claim-specific<br />
information:<br />
(Note: Actual field order will depend on the<br />
view option selected)<br />
— Account or Invoice Number<br />
— Patient Name<br />
— Sponsor Number<br />
— TOP Claim Number<br />
— Dates of Service<br />
— Amount Billed<br />
— Check Number<br />
— Processed Date<br />
— Check Amount<br />
— Account or Invoice Number<br />
— Patient Name<br />
— Sponsor Number<br />
— Claim Number<br />
— Dates of Service<br />
— Amount Billed<br />
— Amount Allowed<br />
— Patient Owes<br />
— Paid to Patient<br />
— Paid to <strong>Provider</strong><br />
— Denial Flag (Y or N)<br />
■ If the ‘Display Individual Charges’ option was selected for<br />
processed claims, the following fields will display as<br />
applicable to the claim and line:<br />
— Line Item<br />
— Procedure Code<br />
— Revenue Code<br />
— Number of Services<br />
— Dates of Service<br />
— Amount Billed<br />
— Amount Allowed<br />
— Patient Offset<br />
— <strong>Provider</strong> Offset<br />
— Paid by Patient<br />
— OHI Paid<br />
— OHI Patient Owes<br />
— Reject<br />
94
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Patient Eligibility<br />
Using the <strong>Provider</strong> Portal: Patient Eligibility<br />
The ‘Check Patient Eligibility’ button can be found on the<br />
navigation bar (see above).<br />
You can conduct a Beneficiary eligibility check using either the<br />
Sponsor Social Security Number (SSN) or DEERS Family ID.<br />
Once you make a selection, complete the remaining fields in this<br />
section and then click the ‘Submit’ button. The Beneficiary<br />
eligibility search will begin and then take you to the ‘Patient<br />
Eligibility’ page to view the results.<br />
Full instructions on how to submit claims via ‘Secure Message<br />
Transmission’ are included in Section 5 of this TOP <strong>Provider</strong><br />
<strong>Manual</strong> (see pages 35-41).<br />
SECTIoN 6<br />
The <strong>Provider</strong> Portal<br />
95
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Manage Locations<br />
Using the <strong>Provider</strong> Portal: Manage My Locations<br />
You can add one or more locations in order to view payments,<br />
claims, send secure messages and submit Online Claims.<br />
In order to add one or more locations, you will need to have one<br />
claim number along with the corresponding patient ‘Date of Birth’<br />
for that claim number, for the location you wish to add.<br />
After the location is successfully added, you will be able to view<br />
recent payments, claims, send secure messages and submit<br />
Online Claims.<br />
To add a location, click ‘Request Location Access’ which will then<br />
ask you to enter the 9-digit tax identification number (first 9 digits<br />
of the TEPRV) and zip code.<br />
Then click ‘Search’.<br />
A list will display of locations that are available to add.<br />
You will then need to click the ‘Self Authorize For Instant Access’<br />
button, which will prompt you to enter the claim number and<br />
‘Date of Birth’ for the patient on that claim number (for the<br />
location being requested). After the information has been entered<br />
and is verified, you will receive a message stating that the<br />
location was successfully added.<br />
96
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Using the <strong>Provider</strong> Portal: My Profile<br />
You can make any changes to your<br />
<strong>Provider</strong> Profile by clicking on<br />
‘Personal Information’. Update the<br />
information in this section and then<br />
click ‘Save’ to make the updates.<br />
You can change your language<br />
preference by clicking on the<br />
‘Language Preference’ button.<br />
Once you’re finished making your<br />
selection, click ‘Save’ to make the<br />
update.<br />
You can change your password and/or<br />
update your security question and<br />
answer. Click the ‘Password Security<br />
Question’ button and when completed,<br />
click ‘Save’ to make the updates.<br />
SECTIoN 6<br />
The <strong>Provider</strong> Portal<br />
97
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
<strong>TRICARE</strong> Covered Benefits<br />
<strong>Provider</strong>s can check to see which medical care services are covered for each type of <strong>TRICARE</strong> Beneficiary by visiting<br />
www.tricare.mil/coveredservices<br />
You can fill in the fields in the ‘Answer Three Questions’ section at the top of this page to customize the search results and change the<br />
profile of the <strong>TRICARE</strong> Beneficiary.<br />
For Question #2, you can select the country in which the Beneficiary is located. This will assist in determining which <strong>TRICARE</strong> Plan he or<br />
she is using.<br />
Once you have selected the customized profile, you can then click on ‘See What’s Covered’ to bring up a list of <strong>TRICARE</strong> Covered<br />
Services, in alphabetical order.<br />
98
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
<strong>TRICARE</strong> Covered Benefits: See What’s Covered<br />
Once the ‘See What’s Covered’ page opens, you can use the drop down menu to search for the particular treatment or medical service<br />
you are looking for. In the example below, ‘Birth Control’ was selected from the drop down menu. Details regarding covered services and<br />
the relevant exclusions (if any) will appear.<br />
You can also click any of the links in the ‘Most Viewed Topics’ section (top right) to obtain more information regarding related topics.<br />
SECTIoN 6<br />
The <strong>Provider</strong> Portal<br />
99
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
SECTIoN 7:<br />
<strong>TRICARE</strong> overseas <strong>Program</strong> <strong>Provider</strong> Forms<br />
Sample: CMS 1500 Claim Form<br />
100
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
SECTIoN 7<br />
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> Forms<br />
Sample: CMS 1500 Claim Form (continued)<br />
101
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Sample: UB-04 Claim Form<br />
102
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
SECTIoN 7<br />
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> Forms<br />
Sample: UB-04 Claim Form (continued)<br />
103
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Sample: International SoS Authorization Form<br />
<strong>TRICARE</strong> AUTHORIZATION FORM<br />
FOR OUTPATIENT CARE<br />
<strong>TRICARE</strong> PRIME BENEFICIARY<br />
To:<br />
<br />
<br />
<br />
<br />
Tel: <br />
Fax: <br />
Authorization Number: <br />
Date: 14 April 2010<br />
Pages: 1<br />
SERVICE(S) REQUEST IN RESPECT OF:<br />
<br />
This is to confirm the Authorization for the above patient at for outpatient care. This Authorization is only valid<br />
between and .<br />
Priority<br />
Specialty<br />
Preliminary Diagnosis<br />
Number of Visits<br />
Scope<br />
Instructions:<br />
<br />
<br />
As per referral<br />
<br />
<br />
<br />
<br />
Inclusions:<br />
Further to medical information received, International SOS authorizes all reasonable, customary and necessary medical expenses<br />
within the scope of the approved authorization.<br />
Medical Reports:<br />
Please send a written medical report and discharge summary to the below addressee after this patient’s episode of care /<br />
procedure. Please follow any special arrangements you may have between you and the Military Treatment Facility (MTF).<br />
, Fax: <br />
<br />
Priority:<br />
For urgent medical appointments please return a copy of medical results within 24 hours.<br />
For routine appointments please return a copy of medical results within 10 calendar days.<br />
Important:<br />
An authorization is issued for requested services, procedures, or admissions that require medical necessity review prior to services<br />
being rendered. The terms of this Authorization are only applicable to the specific service provider indicated above and to this<br />
instance of service requested.<br />
Billing Instructions:<br />
If the Beneficiary has "other" healthcare coverage in addition to <strong>TRICARE</strong>, the "other" healthcare coverage is the Primary Insurer.<br />
All invoices must reach us within 12 calendar months from date of service to avoid denial of settlement. An itemized invoice<br />
accompanied with a duly completed Claim Form and a copy of this Authorization Form is to be sent to the following address. :<br />
<br />
<br />
For full terms and conditions of this Authorization Form, please refer to www.tricare-overseas.com . Alternatively, you may contact<br />
our office for a copy of the terms and conditions.<br />
Yours sincerely<br />
<br />
<strong>TRICARE</strong> Department<br />
104
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
SECTIoN 7<br />
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> Forms<br />
Sample: EDI (Electronic Data Interchange) Agreement Form<br />
105
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Sample: EFT (Electronic Funds Transfer) Form for <strong>Provider</strong>s<br />
Electronic Funds Transfer (EFT) Claim Payment Request<br />
If you are expecting to receive all your payments directly, please complete your bank details.<br />
If you are processing all of your invoices through a billing agency or a corporate entity, please send them form to provide us with<br />
their bank details and a list of providers billing through them.<br />
PROVIDER INFORMATION:<br />
Do you use a billing agency? Yes / No (If Yes, please request your Billing Agency to complete the EFT Form for Billing Agency)<br />
<strong>TRICARE</strong> ID Number<br />
City<br />
Country<br />
<strong>Provider</strong> Name<br />
State<br />
Zip / Postal Code<br />
BANK DETAILS:<br />
Please provide details of the Account Holder – including Account Holder’s Street Address<br />
Account Holder Name<br />
Street Address<br />
Country<br />
Bank Name<br />
Bank ID Code (Swift, FED,<br />
ABA, etc.)<br />
Bank Street Address<br />
Bank State/ Country<br />
Tel Number<br />
Zip / Postal Code<br />
Full Bank Account<br />
Number (IBAN)<br />
Bank City<br />
Bank Zip / Postal<br />
Code<br />
INTERMEDIARY BANK DETAILS:<br />
Please provide details of the Account Holder – including Account Holder’s Street Address<br />
Intermediary Bank Name<br />
Street Address<br />
State / Country<br />
Bank Swift Code<br />
Tel Number<br />
City<br />
Zip / Postal Code<br />
PAYMENT INFORMATION:<br />
Wire_____________________ (specify currency)<br />
Authorization (Signature and Date Required)<br />
_________________________ (Bank Accountholder) hereby authorizes International SOS and/or its dedicated Agents to make<br />
payments of any benefits payable to us by crediting the payments to my account at the bank or financial institution named above. I<br />
agree to notify in writing of any change relating to the information provided on this form or of a withdrawal of this authorization.<br />
I agree that if, for any reason unearned payments are deposited into my account, I will immediately repay the full amount of any<br />
such payments. I further agree that if I do not immediately repay such unearned payments, I will be liable for all costs of collection.<br />
These costs include reasonable attorney’s fees, incurred by International SOS and/or its dedicated Agents in the collection of such<br />
payments.<br />
In the case of any overpayment of benefits to my account, I agree that International SOS may debit my account for such<br />
overpayment, without further authorization from me.<br />
All bank charges incurred by our organization are our responsibility.<br />
Signature Title Date<br />
Organization Name<br />
Please email this form back to: Europe, Middle East & Africa providerseurasiaafrica@internationalsos.com<br />
Asia Pacific<br />
providersasiapacific@internationalsos.com<br />
Latin America and Canada<br />
providerslatinamerica@internationalsos.com<br />
Puerto Rico<br />
provider.inquiries.PR@internationalsos.com<br />
106
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
SECTIoN 7<br />
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> Forms<br />
Sample: EFT Form for <strong>Provider</strong>s Who Use a Billing Agency<br />
Billing Agency - Electronic Funds Transfer (EFT) Claim Payment Request<br />
If you use the services of a billing agency to submit claims on your behalf for TOP beneficiary claims, please request that your billing<br />
agency completes and returns this form along with your Mutual Cooperation Protocol.<br />
BILLING AGENCY INFORMATION:<br />
<strong>TRICARE</strong> ID Number<br />
City<br />
Country<br />
Billing Agency Name<br />
State<br />
Zip / Postal Code<br />
BANK DETAILS:<br />
Please provide details of the Account Holder – including Account Holder’s Street Address<br />
Account Holder Name<br />
Street Address<br />
Country<br />
Bank Name<br />
Bank ID Code (Swift, FED,<br />
ABA, etc.)<br />
Bank Street Address<br />
Bank State/ Country<br />
Tel Number<br />
Zip / Postal Code<br />
Full Bank Account<br />
Number (IBAN)<br />
Bank City<br />
Bank Zip / Postal<br />
Code<br />
INTERMEDIARY BANK DETAILS:<br />
Please provide details of the Account Holder – including Account Holder’s Street Address<br />
Intermediary Bank Name<br />
Street Address<br />
State / Country<br />
Bank Swift Code<br />
Tel Number<br />
City<br />
Zip / Postal Code<br />
PAYMENT INFORMATION:<br />
Wire_____________________ (specify currency)<br />
Authorization (Signature and Date Required)<br />
_________________________ (Bank Accountholder) hereby authorizes International SOS and/or its dedicated Agents to make<br />
payments of any benefits payable to us by crediting the payments to my account at the bank or financial institution named above. I<br />
agree to notify in writing of any change relating to the information provided on this form or of a withdrawal of this authorization.<br />
I agree that if, for any reason unearned payments are deposited into my account, I will immediately repay the full amount of any<br />
such payments. I further agree that if I do not immediately repay such unearned payments, I will be liable for all costs of collection.<br />
These costs include reasonable attorney’s fees, incurred by International SOS and/or its dedicated Agents in the collection of such<br />
payments.<br />
In the case of any overpayment of benefits to my account, I agree that International SOS may debit my account for such<br />
overpayment, without further authorization from me.<br />
All bank charges incurred by our organization are our responsibility.<br />
Signature Title Date<br />
Organization Name<br />
Please email this form back to: Europe, Middle East & Africa providerseurasiaafrica@internationalsos.com<br />
Asia Pacific<br />
providersasiapacific@internationalsos.com<br />
Latin America and Canada<br />
providerslatinamerica@internationalsos.com<br />
Puerto Rico<br />
provider.inquiries.PR@internationalsos.com<br />
107
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
SECTIoN 8:<br />
List of Acronyms<br />
AAP<br />
ADFM<br />
ADSM<br />
CAC<br />
CDC<br />
CoNUS<br />
CPT<br />
DHA<br />
DMEPoS<br />
DoB<br />
DoD<br />
DRG<br />
ECHo<br />
EDI<br />
EFT<br />
EoB<br />
FY<br />
HPV<br />
ICD<br />
ICN<br />
MHS<br />
MRI<br />
oHI<br />
SSN<br />
TFL<br />
ToP<br />
TRR<br />
TRS<br />
TYA<br />
UCCI<br />
WPS<br />
American Academy of Pediatrics<br />
Active Duty Family Member<br />
Active Duty Service Member<br />
Common Access Card<br />
Centers for Disease Control<br />
Continental United States<br />
Current Procedural Terminology<br />
Defense Health Agency<br />
Durable Medical Equipment, Prosthetics, Orthontics and Supplies<br />
Date of Birth<br />
Department of Defense<br />
Diagnosis-related Group<br />
<strong>TRICARE</strong> Extended Health Care Option<br />
Electronic Data Interchange<br />
Electronic Fund Transfer<br />
Explanation of Benefits<br />
Fiscal Year<br />
Human Papillomavirus<br />
International Classification of Diseases<br />
Internal Control Number<br />
Military Health System<br />
Magnetic Resonance Imaging<br />
Other Health Insurance<br />
Social Security Number<br />
<strong>TRICARE</strong> for Life<br />
<strong>TRICARE</strong> <strong>Overseas</strong> <strong>Program</strong><br />
<strong>TRICARE</strong> Retired Reserve<br />
<strong>TRICARE</strong> Reserve Select<br />
<strong>TRICARE</strong> Young Adult <strong>Program</strong><br />
United Concordia Companies, Inc.<br />
Wisconsin Physicians Service<br />
108
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
Appendix<br />
ToP: Explanation of Benefits Denial Codes and Remarks<br />
Code Description Additional Information<br />
003<br />
See Item Five on Reverse. If you are not satisfied with our determination, you have<br />
the right to request a review within 90 days of the date of this notice.<br />
SECTIoN 8 / APPENDIX<br />
Acronyms<br />
004 Non-prescription drug – see Item Four on Reverse.<br />
008 Routine X-ray not covered – see Item Four on Reverse.<br />
009 Non-covered routine eye examination – see Item Four on Reverse.<br />
010 Routine lab not covered – see Item Four on Reverse.<br />
013 Eyeglasses/lenses not covered – see Item Four on Reverse.<br />
014 Routine foot care not covered – see Item Four on Reverse.<br />
018 <strong>Provider</strong> not <strong>TRICARE</strong>-authorized for this service.<br />
019 Personal comfort item not covered – see Item Four on Reverse.<br />
020 This charge included in a paid service.<br />
This is used when the <strong>Provider</strong> is<br />
billing for a procedure that is<br />
already accounted for in another<br />
procedure. For example, removal<br />
of cerumen (ear wax) is included in<br />
the office visit charge.<br />
027 Authorized service limits exceeded – see Item Four on Reverse.<br />
028 Requested Information Not Received.<br />
030 Service Filed After Time Limit.<br />
032 Non-covered Services.<br />
033 Duplicate of Services Previously Claimed (<strong>Manual</strong>).<br />
Services billed are not a covered<br />
service according to <strong>TRICARE</strong><br />
Policy.<br />
Upon manual review, it was<br />
determined this charge is a<br />
duplicate and has been paid<br />
previously on another line/claim.<br />
109
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
ToP: Explanation of Benefits Denial Codes and Remarks (continued)<br />
Code Description Additional Information<br />
044 Duplicate of services previously claimed (system).<br />
045 Applied to deductible – see Item Six on Reverse.<br />
049 Authorization not on file. Contact your HBA.<br />
050 Insufficient Diagnosis – see Item Four on Reverse.<br />
056 Chiropractic services not covered.<br />
059 Obesity not a covered diagnosis – see Item Four on Reverse.<br />
067 Medical need not documented.<br />
070 Patient not eligible. Per DEERS, patient is not eligible.<br />
072<br />
Claim requires drug name, strength and quantity. See Item Two on Reverse for<br />
time limit to send requested information.<br />
074 Sponsor not on DEERS.<br />
075 Patient not on DEERS.<br />
077 Dependent patient not on DEERS.<br />
080 ID card or eligibility expired on DEERS.<br />
083 Insufficient information received.<br />
126 Level of care billed not substantiated.<br />
Information requested (such as<br />
medical records) were insufficient<br />
to support the care/request.<br />
Upon review, it was determined<br />
that the charges billed were for<br />
more services than what was<br />
actually provided. For example,<br />
<strong>Provider</strong> is billing for a new patient<br />
office visit when we have already<br />
paid a new patient office visit for<br />
the same <strong>Provider</strong>. So, the <strong>Provider</strong><br />
should have been billing as an<br />
established patient office visit.<br />
110
<strong>TRICARE</strong> overseas <strong>Program</strong><br />
<strong>Provider</strong> <strong>Manual</strong><br />
ToP: Explanation of Benefits Denial Codes and Remarks (continued)<br />
Code Description Additional Information<br />
132 Services must be billed by <strong>Provider</strong> of care.<br />
Claim is being submitted by<br />
another <strong>Provider</strong> on behalf of the<br />
<strong>Provider</strong> that rendered care. For<br />
example, St. Mary’s submits the<br />
claim for Meriter.<br />
135 <strong>Provider</strong> is not <strong>TRICARE</strong>-authorized.<br />
136 Services denied because we cannot determine primary insurance payment.<br />
Need Explanation of Benefits from<br />
Other Health Insurance.<br />
APPENDIX<br />
160 Procedure code submitted not payable for this service/beneficiary.<br />
173 Documentation does not support the frequency of visits billed.<br />
219<br />
236<br />
Diagnosis code is missing or invalid. Your claim will be reconsidered upon timely<br />
receipt of information.<br />
Your claim was denied because we did not receive the EOBs from all your primary<br />
insurances.<br />
There is more than one active<br />
health insurance on file. Need<br />
EOBs from ALL active Other Health<br />
Insurances.<br />
308 Authorization not attached. Contact local command personnel or nearest MTF.<br />
Services required an authorization<br />
and there is not one on file.<br />
327 Missing/incomplete/invalid/deactivated/withdrawn National Drug Code (NDC).<br />
111
R<br />
International SOS Assistance, Inc.<br />
www.tricare-overseas.com<br />
Worldwide reach Human touch