Nurse Reporter Spring 2011 - Wyoming State Board of Nursing
Nurse Reporter Spring 2011 - Wyoming State Board of Nursing
Nurse Reporter Spring 2011 - Wyoming State Board of Nursing
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Vol. 7<br />
<strong>Nurse</strong><br />
Number 1 <strong>Spring</strong> <strong>2011</strong><br />
R E P O R T E R<br />
<strong>Wyoming</strong><br />
In Celebration <strong>of</strong><br />
<strong>Wyoming</strong> <strong>Nurse</strong>s and<br />
<strong>Nurse</strong>s Week <strong>2011</strong><br />
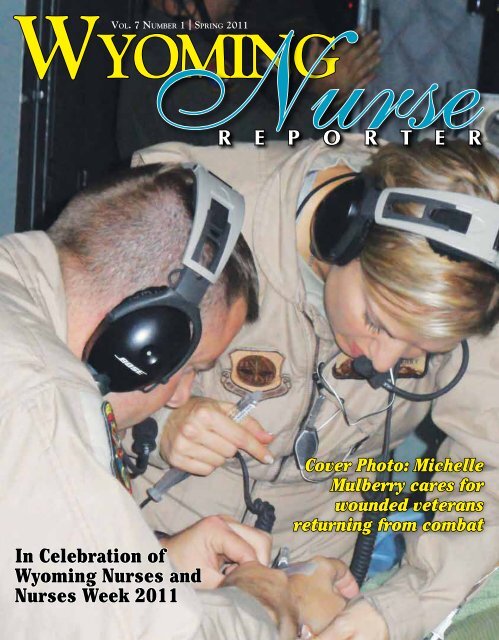
Cover Photo: Michelle<br />
Mulberry cares for<br />
wounded veterans<br />
returning from combat
CHOOSE<br />
EXCELLENCE<br />
A Rare Opportunity to Become a Part <strong>of</strong> <strong>Nursing</strong> Excellence<br />
Our nurses enjoy a low nurse-to-patient ratio, a warm, family-oriented environment,<br />
state-<strong>of</strong>-the-art facilities, and an emphasis on balancing work and life.<br />
Maybe that’s why our hospital receives near-perfect patient satisfaction<br />
survey scores every month!<br />
We are currently accepting applications for RNs trained in the following specialties:<br />
Surgical • ICU/Critical Care • ER • CNAs • Full-Time and PRN Positions Available<br />
307.995.8100 • 6550 E. 2ND STREET • CASPER, WYOMING<br />
WWW.MOUNTAINVIEWREGIONALHOSPITAL.COM
<strong>Wyoming</strong><br />
<strong>Spring</strong> <strong>2011</strong> Vol. 7 Number 1<br />
Editor<br />
Mary Kay Goetter<br />
Assistant Editor<br />
Patti Gardner<br />
<strong>Nurse</strong> R<br />
T a b l e o f C o n t e n t s<br />
“Serving and safeguarding the<br />
people <strong>of</strong> <strong>Wyoming</strong> through the<br />
regulation <strong>of</strong> nursing education and<br />
practice”<br />
E P O R T E R<br />
Published by the<br />
<strong>Wyoming</strong> <strong>State</strong> <strong>Board</strong> <strong>of</strong> <strong>Nursing</strong><br />
1810 Pioneer Ave.<br />
Cheyenne, <strong>Wyoming</strong> 82002<br />
Phone: 307-777-7601<br />
Fax: 307-777-3519<br />
Web Address: http://nursing.state.wy.us<br />
Mission: To serve and safeguard the people <strong>of</strong><br />
<strong>Wyoming</strong> through the regulation <strong>of</strong> nursing education<br />
and practice.<br />
Vision <strong>State</strong>ment: Acknowledging the dynamic<br />
nature <strong>of</strong> healthcare, provides the climate, collaboration<br />
and regulatory framework for nurses to practice to the<br />
fullest extent <strong>of</strong> their scope.<br />
Values: Excellence, Ethics, Education, Safety and<br />
Competence.<br />
Executive Director<br />
Mary Kay Goetter, PhD, RNC, NEA-BC<br />
Assistant Executive Director,<br />
Practice and Education Consultant<br />
Todd Berger, MSN, ACNP-BC, ACNS-BC<br />
Compliance Consultant<br />
Patti Hefflin, BSN, RN<br />
Financial and Human Resources Officer<br />
Cindy Stillahn<br />
Executive Assistant<br />
Amanda Roberts<br />
Licensing Coordinators<br />
Maxine Hernandez<br />
LaVelle Ojeda<br />
Disciplinary Assistant<br />
Debra Ball<br />
Legal Assistant<br />
Jan Ross<br />
3 Editorial<br />
5 President’s Message<br />
6 Life are You Ready?<br />
7 The <strong>Wyoming</strong> Center for <strong>Nursing</strong> and Health Care Partnerships Corner<br />
9 Getting to Know <strong>Wyoming</strong> <strong>Nurse</strong>s: Meet Michelle Mulberry<br />
10 Returning to School: Is It Right for You?<br />
12 First CNA II Training Class Held in Gillette<br />
13 Inside Scoop<br />
14 Getting to Know <strong>Wyoming</strong> <strong>Nurse</strong>s: Meet Mariusz Pieczalski<br />
16 Practice Questions Requiring Substantial Thought<br />
20 Faith Community <strong>Nursing</strong><br />
21 Customer Service Corner<br />
21 Getting to Know <strong>Wyoming</strong> <strong>Nursing</strong> Students: Meet Lilian Ogana<br />
22 Getting to Know <strong>Wyoming</strong> <strong>Nursing</strong> Students: Meet Mallory Davis<br />
22 Legislative Review<br />
23 Delegation <strong>State</strong>ment<br />
24 Disciplinary Actions<br />
30 Pearls <strong>of</strong> Practice<br />
Greetings<br />
From Mary Kay Goetter<br />
Executive Director<br />
<strong>Board</strong> <strong>of</strong> <strong>Nursing</strong> Members<br />
Kellie Clausen, FNP, WHCNP, RN President<br />
Tracy Wasserburger, RN-C, APRN, NNP-BC<br />
Vice President<br />
Marguerite Herman Consumer Secretary<br />
Lee Carruthers, RN--RN<br />
Representative<br />
Kim Williamson, LPN Expires February 2, <strong>2011</strong><br />
Marcie Burr, RN, HSA, CCHP Member<br />
Carrie Deselms, APRN, FNP-BC Member<br />
<strong>Wyoming</strong> <strong>Nurse</strong> <strong>Reporter</strong> does not necessarily<br />
endorse advertisements contained herein. The<br />
publisher reserves the right to accept or reject<br />
advertisements for <strong>Wyoming</strong> <strong>Nurse</strong> <strong>Reporter</strong>.<br />
For Advertising Information:<br />
Victor Horne<br />
vhorne@pcipublishing.com<br />
501.221.9986 or 800.561.4686 ext. 114<br />
Created By:<br />
Publishing Concepts, Inc.<br />
Virginia Robertson, Publisher<br />
vrobertson@pcipublishing.com<br />
Think<strong>Nurse</strong>.com<br />
Publishing Concepts, Inc.<br />
14109 Taylor Loop Road<br />
Little Rock, AR 72223<br />
EDITION 24<br />
<strong>Spring</strong> is really coming!<br />
It seems impossible to<br />
believe, but in fact, the sun<br />
is particularly warm today,<br />
reminding me that spring<br />
truly is just around the<br />
corner! With the spring<br />
seasonal change always<br />
comes <strong>Nurse</strong>s’ Week and<br />
all the celebrations that<br />
accompany it. We decided<br />
here at WSBN to herald<br />
<strong>Spring</strong> <strong>2011</strong> and <strong>Nurse</strong>s’<br />
Week with an issue<br />
focusing on celebrating<br />
nurses, both the people and<br />
the pr<strong>of</strong>ession as a whole.<br />
There are so many<br />
things to be grateful for in<br />
nursing today, not the least<br />
<strong>of</strong> which is a President<br />
who is outspoken in his<br />
support <strong>of</strong> nurses and their<br />
role in healthcare reform.<br />
But rather than discuss<br />
politics in this forum, I<br />
am going to share a story<br />
that I believe captures the<br />
essence <strong>of</strong> why being a<br />
nurse today is a reason to<br />
Continued on next page<br />
pause and express gratitude<br />
and humility. This is the<br />
story <strong>of</strong> how one nurse<br />
made all the difference to<br />
one family.<br />
My mother, Virginia,<br />
lives in a suburb <strong>of</strong><br />
Milwaukee and despite<br />
being 85 years <strong>of</strong> age<br />
she works about 10-14<br />
hours a week in church<br />
volunteer activities. No<br />
visit or phone call with her<br />
is complete without her<br />
regaling me with the latest<br />
stories about her volunteer<br />
work serving on the<br />
parish council or making<br />
regular rounds <strong>of</strong> hospital<br />
<strong>Wyoming</strong> <strong>Nurse</strong> <strong>Reporter</strong> 3
visits to bring communion or just pray with<br />
people. One family in particular has figured<br />
prominently in her stories in the past several<br />
years.<br />
Tom and Erica, a married couple in their<br />
40s, had two daughters and both <strong>of</strong> them were<br />
affected by MELAS Syndrome: an incredibly<br />
rare genetic disease that causes debilitation,<br />
dementia and death, with symptoms usually<br />
apparent in the teen years. It was especially<br />
grievous to Erica that, although she herself<br />
was not afflicted by the condition, she was<br />
the carrier. The older <strong>of</strong> the two, Ashley,<br />
was far more ill and had been confined to<br />
a wheelchair since her mid-teens. She had<br />
also become progressively blind, but retained<br />
her mind’s ability to think and enjoy some<br />
cognitive activities. Although diagnosed<br />
with the same disease, the younger daughter,<br />
Brittany, remained seemingly healthy. Tom<br />
and Erica tried their best to care for Ashley<br />
while allowing Brittany to have as normal <strong>of</strong><br />
a life as possible. My mother was part <strong>of</strong> a<br />
parish ministry that went to their home to<br />
help out and her task was to read aloud to<br />
Ashley. Though in her 20s and completely<br />
bedridden, Ashley still loved Nancy Drew<br />
Mystery stories and my mother spent many<br />
hours in the last year <strong>of</strong> Ashley’s life reading<br />
Nancy’s adventures aloud to the young<br />
woman. Ultimately, Ashley died at home at<br />
age 24, in hospice care, surrounded by her<br />
family.<br />
For the next few years, Brittany continued<br />
to do well. She had graduated from high<br />
school, attended some college classes and was<br />
employed in a job that she loved. She had<br />
some symptoms, was painfully thin and <strong>of</strong>ten<br />
fatigued, but her ability to finish school and<br />
be employed encouraged Tom and Erica that<br />
maybe this time, it would be different. Maybe<br />
Brittany could defy the odds and survive with<br />
a mild case <strong>of</strong> the disease. Everyone tried to<br />
remain optimistic, despite the physicians’<br />
sympathetic, though realistic prognosis <strong>of</strong><br />
premature debilitation and death.<br />
Last October, Brittany reported to her<br />
doctor’s <strong>of</strong>fice for a routine check-up and flu<br />
shot. A few hours later, she felt terribly ill.<br />
Thinking it was only a reaction to the flu<br />
shot, she crawled into bed. By morning, she<br />
was barely responsive and Tom and Erica<br />
called an ambulance. She usually received<br />
all her care at a regional medical center in<br />
Milwaukee, but her condition was so grave,<br />
she was taken to the Emergency Department<br />
<strong>of</strong> the nearest community hospital, where she<br />
was admitted to the Intensive Care Unit.<br />
Brittany was already in respiratory failure<br />
and soon needed to be intubated and placed<br />
on mechanical ventilation. Less than 24 hours<br />
after admission, despite vigilant medical and<br />
nursing care, Brittany had a cardiac arrest. Tom<br />
and Erica stood by, numb and helpless, while<br />
they watched the resuscitation procedures<br />
being done on their daughter. The physicians<br />
had confirmed that her rapid deterioration was<br />
related to MYLAS Syndrome and not the flu<br />
shot or some other more treatable condition.<br />
It seemed inconceivable that she could have<br />
had such a reprieve from this disease, only to<br />
be facing the dreaded outcome right now.<br />
The resuscitation efforts were successful,<br />
in that the healthcare providers were able<br />
to stabilize Brittany’s heart rate and blood<br />
pressure. However, as the next few days<br />
unfolded, it was evident that Brittany would<br />
not leave the hospital. She was mostly<br />
unconscious, but now and then a glimmer <strong>of</strong><br />
responsiveness would shine through, sparking<br />
hope in Tom and Erica. However, their fervent<br />
wishes were denied when Brittany once again<br />
showed signs <strong>of</strong> imminent decline. Brittany’s<br />
caregivers gently broached the topic <strong>of</strong> end<strong>of</strong>-life<br />
care with her distraught parents.<br />
Her body was failing rapidly, they said.<br />
But she was doing so well up until less than 2<br />
weeks ago! The disease process is taking over,<br />
they said. But, surely if we can buy her some<br />
time she can recover enough to come home, at<br />
least for a little while! The doctors and nurses<br />
found themselves in the position <strong>of</strong> helping<br />
this family hear and understand the most<br />
heartbreaking information imaginable—Your<br />
child will not recover. This position is not<br />
unfamiliar to many <strong>of</strong> WNR’s readers.<br />
After all <strong>of</strong> their questions were answered,<br />
every “What if?” was brought out in the open,<br />
after all the tears and prayers, the answer was<br />
affirmative; Tom and Erica agreed to a “Do<br />
not resuscitate” order for their 24-year old<br />
daughter. Brittany would not after all, outlive<br />
Ashley.<br />
As so <strong>of</strong>ten happens after such a decision is<br />
made, Brittany seemed to rally a bit. She still<br />
responded to her mother’s voice and touch.<br />
But it was short-lived. Brittany was near death<br />
and the accoutrements <strong>of</strong> intensive care were<br />
only prolonging her suffering. Their suffering.<br />
The physician suggested that perhaps it would<br />
be best for Brittany if they discontinued life<br />
support.<br />
Members <strong>of</strong> my mother’s church were<br />
contacted to renew their prayers and support<br />
for this family during these last difficult days<br />
and hours. Erica agreed that it was futile to<br />
allow Brittany to continue to suffer, but this<br />
decision proved even more difficult than the<br />
“Do not resuscitate” decision. It is one thing<br />
to agree to a DNR order, but another matter<br />
to say, go ahead and turn <strong>of</strong>f the ventilator, go<br />
ahead and extubate her. Erica did say OK, but<br />
on one condition; I want to hold her in my<br />
arms. I want her to leave this world the same<br />
way she came into it—in my arms. I want to<br />
hold my baby as she dies so she knows she is<br />
not alone.<br />
Afterwards, my mother went to visit Erica<br />
and Tom at their home and just be with them.<br />
Erica had been so distraught after Ashley’s<br />
death, she could barely speak to anyone, but<br />
it had seemed to help when church members<br />
came and just sat with her and prayed with<br />
her. But when my mother came after Brittnay<br />
died, Erica wanted to talk. She wanted to<br />
share the story <strong>of</strong> her daughter’s death much<br />
like a new mother wants to share her birth<br />
story to everyone who comes to see the new<br />
baby.<br />
“I told them I would only let them turn <strong>of</strong>f<br />
the machines if I could get in bed with her<br />
and hold her. I thought they might argue with<br />
me but they didn’t! Not at all! The nurses<br />
were so wonderful to me, Virginia! They<br />
lifted my baby so gently to the edge <strong>of</strong> the<br />
bed, they arranged all the tubes and lines, and<br />
moved everything aside. They made a spot for<br />
me and helped me to hold her just so. And<br />
then they turned <strong>of</strong>f the machines and made<br />
sure Brittany and I were as comfortable and<br />
supported as could be. And Virginia, her nurse<br />
stayed! She just stayed there long after her<br />
shift was over. She just sat there and stayed<br />
with us. I could not believe it. They weren’t<br />
used to this kind <strong>of</strong> thing, not in an intensive<br />
care unit. But she did everything she could to<br />
make sure we could just be together and that<br />
Brittany’s death could be peaceful. And she<br />
cried! I could not believe it, Virginia, but the<br />
nurse held me and cried with me afterwards. I<br />
didn’t know a nurse would do that.”<br />
I do know that a nurse would do that. I<br />
think that, as nurses, we all know that most<br />
<strong>of</strong> us would do just about anything possible<br />
to relieve suffering, express compassion,<br />
embrace new life, and when necessary, ease<br />
the transition from life to death. I don’t know<br />
any <strong>of</strong> the nurses in that intensive care unit<br />
in Wisconsin, but I don’t believe they are<br />
much different than nurses in <strong>Wyoming</strong>, or<br />
anywhere else for that matter.<br />
To all the nurses I do know, as well as the<br />
ones I do not, I express my gratitude for being<br />
in this pr<strong>of</strong>ession. We are all honored to be<br />
part <strong>of</strong> people’s lives on the journey from birth<br />
to death and I am most honored to stand with<br />
you as colleagues.<br />
4 <strong>Wyoming</strong> <strong>Nurse</strong> <strong>Reporter</strong>
According to the Chinese Zodiac, the Year<br />
<strong>of</strong> <strong>2011</strong> is the Year <strong>of</strong> the Golden Rabbit, which<br />
begins on February<br />
3, <strong>2011</strong> and ends on<br />
January 22, 2012.<br />
The Rabbit is the<br />
fourth sign <strong>of</strong> the<br />
Chinese Zodiac,<br />
which consists <strong>of</strong><br />
12 animal signs.<br />
The Rabbit is a<br />
lucky sign. I readily<br />
recognize that this<br />
astrology is felt to relate to those who are born<br />
this year, but my readings have also led me to<br />
appreciate that this can also be applied to the<br />
business world as well. I feel the Year <strong>of</strong> the<br />
Rabbit is going to be lucky for me and in part it<br />
is because I feel honored to be a member <strong>of</strong> the<br />
<strong>Board</strong> <strong>of</strong> <strong>Nursing</strong>, serving you, the licensees, in<br />
our fabulous state.<br />
Last year, the <strong>Board</strong> put great effort in<br />
establishing and implementing a strategic plan<br />
for our organization. We have focused on some<br />
key areas which include: Public relations-<br />
A Message from Tracy Wasserburger<br />
President <strong>of</strong> <strong>Wyoming</strong> <strong>State</strong> <strong>Board</strong> <strong>of</strong> <strong>Nursing</strong><br />
establish and authenticate the board’s mission<br />
to the public; Policy Making - Establish wellorganized,<br />
efficient and effective processes<br />
and procedures; Service - Deliver a reliable<br />
and consistent service to public and licensees;<br />
Safety - Ensure public safety through all WSBN<br />
processes; and Education - Sustain progressive<br />
and dynamic standards <strong>of</strong> quality nursing<br />
education. We know that we have a lot <strong>of</strong> work<br />
to do in each <strong>of</strong> these areas, but we also know<br />
that we have many opportunities as well. We<br />
will work diligently to take these key areas <strong>of</strong><br />
focus and deliver the kind <strong>of</strong> support, assistance,<br />
direction and service that you need from us. For<br />
<strong>Board</strong> members and <strong>Board</strong> staff, it will serve as<br />
a tool that will not be looked at just once a year,<br />
but on a consistent basis so that we keep these<br />
four key areas at the heart <strong>of</strong> what we do for you<br />
and the public.<br />
The forecast for those who are born this year<br />
is said to be balanced in outlook and cautious<br />
in approach. I feel that the <strong>Board</strong> <strong>of</strong> <strong>Nursing</strong> is<br />
required to practice with these same attributes<br />
to ensure safety <strong>of</strong> the public. Not unlike those<br />
born this year who are said to be prone to having<br />
the trait <strong>of</strong> being informed <strong>of</strong> all the facts before<br />
making a judgment, we as a <strong>Board</strong> also have<br />
made the same commitment in gaining as much<br />
knowledge and education as feasible as we move<br />
forward in decision or policy making. Chinese<br />
astrology goes on to say that those who are<br />
born in <strong>2011</strong> are likely to identify opportunity.<br />
I feel that we have very strong and intelligent<br />
members and staff who too are gifted with<br />
identifying opportunity. We will work hard to<br />
turn these opportunities in to advantages for<br />
those we interact with.<br />
According to Chinese tradition, the Rabbit<br />
brings a year in which you can catch your breath<br />
and calm your nerves. It is a time for negotiation.<br />
It is a time not to force issues. One is suppose to<br />
make it a goal to create a safe, peaceful lifestyle,<br />
so you will be able to calmly deal with any<br />
problem that may arise. Although I was born<br />
in the Year <strong>of</strong> the Tiger, as <strong>Board</strong> President I will<br />
try to adopt the attributes <strong>of</strong> the Rabbit so that<br />
we at the WSBN, may do our greatest service<br />
for those who rely on us most.<br />
Tracy Wasserburger, RNC, MSN, NNP-BC<br />
WYOMING HEALTH<br />
MINISTRY SUMMIT<br />
INVITES<br />
Faith Community & Parish <strong>Nurse</strong>s, Health Pr<strong>of</strong>essionals,<br />
Clergy & Faith Pr<strong>of</strong>essionals and Laypersons to:<br />
“INTEGRATING BODY, MIND, SPIRIT:<br />
BUILDING THE FOUNDATION”<br />
Friday, April 29, <strong>2011</strong><br />
Faith Community & Parish <strong>Nurse</strong> Reception<br />
Saturday, April 30, <strong>2011</strong><br />
General Session & Presentations<br />
Cheyenne, WY ~ Little America Hotel<br />
Sponsored by:<br />
<strong>Wyoming</strong> Health Council<br />
Cheyenne Regional Medical Center<br />
Visit: www.wyhc.org for<br />
registration information<br />
Month<br />
January 10-14, <strong>2011</strong><br />
February 1, <strong>2011</strong><br />
April 4-8, <strong>2011</strong><br />
April 26, <strong>2011</strong><br />
July 4-8, <strong>2011</strong><br />
July 25, <strong>2011</strong><br />
October 3-7, <strong>2011</strong><br />
October 25, <strong>2011</strong><br />
January 9-13, 2012<br />
<strong>Nurse</strong>s are welcome!<br />
WSBN <strong>Board</strong> Meeting<br />
Schedule <strong>2011</strong>-2012<br />
Location<br />
WSBN Office, 1810 Pioneer Ave, Cheyenne,<br />
WY<br />
Teleconference (Dial In 877-278-8686 Pin<br />
517378)<br />
<strong>Board</strong> <strong>of</strong> Medicine Office, 320 W. 25th St. 2nd<br />
Floor Cheyenne, WY<br />
Teleconference (Dial In 877-278-8686 Pin<br />
517378)<br />
TA Ranch Buffalo, WY<br />
Teleconference (Dial In 877-278-8686 Pin<br />
517378)<br />
TBD<br />
Teleconference (Dial In 877-278-8686 Pin<br />
517378)<br />
TBD<br />
<strong>Wyoming</strong> <strong>Nurse</strong> <strong>Reporter</strong> 5
Life R U Ready? originated in Tucson,<br />
Arizona and was originally called “Sex<br />
R U Ready?” The name was changed to<br />
“Life R U Ready?” when it was <strong>of</strong>fered to<br />
Campbell County students in Gillette,<br />
<strong>Wyoming</strong>. Washakie County <strong>of</strong>fers this real<br />
life simulation to middle school students in<br />
Worland and Ten Sleep, <strong>Wyoming</strong>.<br />
The goals <strong>of</strong> “Life R U Ready?” are to<br />
increase awareness <strong>of</strong> the consequences<br />
<strong>of</strong> alcohol, tobacco, and other drug use;<br />
to decrease the motivation to participate<br />
in risk-taking behavior and provide<br />
LIFE are YOU READY?<br />
new opportunities for parent-teen<br />
communication. This program is a real life<br />
simulation where students find themselves<br />
at a party with a variety <strong>of</strong> opportunity<br />
to participate in risky behaviors. Each<br />
behavior results in consequences, such as<br />
jail, court trial, hospital emergency room,<br />
morgue, pregnancy, disabilities, etc. The<br />
event provides 6th, 7th, and 8th graders<br />
with the opportunity to use the skills and<br />
knowledge they have learned in simulated<br />
situations where they can safely experience<br />
the outcomes <strong>of</strong> their decisions.<br />
Lori Schaal<br />
Numerous agencies and community<br />
volunteers are needed for this annual<br />
event. As students attend this scenario and<br />
experience its consequences, they interact<br />
with law enforcement <strong>of</strong>ficials, judges,<br />
nurses, doctors, EMTs, morticians and<br />
counselors. <strong>Nurse</strong>s participate from the<br />
hospital, the clinic, the ambulance, Public<br />
Health and Family Planning.<br />
Lori L. Schaal RN, is the Washakie<br />
County Public Health <strong>Nursing</strong> Manager.<br />
VA Montana Health Care System<br />
Offers Great Career Opportunities<br />
Helena:<br />
- Deputy Chief <strong>Nurse</strong> Executive<br />
- Operating Room <strong>Nurse</strong> Manager<br />
- Chief, Out-Patient Behavioral Health,<br />
RN/NP<br />
<strong>Nurse</strong> Practitioners – Various opportunities<br />
state<br />
LPNs – Various locations around the state<br />
Visit www.usajobs.gov or contact<br />
Human Resources at<br />
(406)447-7933 EOE<br />
Competitive Salaries!<br />
Generous Benefit Packages!<br />
Excellent Career Paths!<br />
Weston County<br />
Health Services<br />
Seeks<br />
<strong>Nurse</strong> Program Manager<br />
Newcastle, WY<br />
Great opportunity for a <strong>Nurse</strong><br />
Program Manager. Key<br />
responsibilities include infection<br />
control, employee health, disaster<br />
planning, nurse in-service<br />
education, worker’s compensation,<br />
case management and physician<br />
credentialing. <strong>Wyoming</strong> RN license<br />
req with BSN preferred; 5 years<br />
nursing management experience.<br />
Competitive salary and benefits.<br />
Send resume to<br />
hgilliland@wchs-wy.org<br />
or call 307-746-3707<br />
6 <strong>Wyoming</strong> <strong>Nurse</strong> <strong>Reporter</strong>
Mary E. Burman and Matt Sholty<br />
<strong>Nursing</strong> Accomplishments in Recruitment and Retention<br />
The <strong>Wyoming</strong> Center for <strong>Nursing</strong> and<br />
Health Care Partnerships Corner<br />
In this issue <strong>of</strong> the <strong>Wyoming</strong> <strong>Nurse</strong> <strong>Reporter</strong>, the accomplishments <strong>of</strong><br />
<strong>Wyoming</strong> nurses are applauded and celebrated. In keeping with this theme,<br />
the <strong>Wyoming</strong> Center for <strong>Nursing</strong> and Health Care Partnerships (WCNHCP)<br />
would like to feature five pilot projects from around the state that highlight<br />
the kind <strong>of</strong> accomplishments nurses can have when they address significant<br />
issues, such as recruitment and retention <strong>of</strong> nurses.<br />
In Fall <strong>of</strong> 2008, the WCNHCP put out a<br />
call for proposals to address nurse recruitment,<br />
training, and retention, especially in long-term<br />
care. The Center received a number <strong>of</strong> proposals<br />
and funded five projects that began in March<br />
2009 and continued through <strong>Spring</strong>/Summer<br />
<strong>of</strong> 2010. In this column, we’ll describe each<br />
<strong>of</strong> the projects and <strong>of</strong>fer recommendations for<br />
successful recruitment and retention projects.<br />
More information about the projects and their<br />
evaluation is available on the WCNHCP’s<br />
website.<br />
Powell Valley Healthcare (PVHC) was<br />
awarded funds to implement a CNA mentorship<br />
project to enhance retention <strong>of</strong> CNAs. The<br />
project was based on a successful program for<br />
nurse mentoring, in which the implementation<br />
<strong>of</strong> a mentoring program for nurses at PVHC<br />
decreased the turnover rate from 66.7% to 0%<br />
during the one year study (Blough, 2006). The<br />
project is based on development <strong>of</strong> a mentoring<br />
process in which an experienced expert CNA<br />
acquaints a novice CNA to the customs, resources,<br />
and values <strong>of</strong> the organization, while at the same<br />
time serves as a role model. The desired outcomes<br />
include turnover reduction, financial savings,<br />
increased job satisfaction, enhanced quality <strong>of</strong><br />
care, and provide veteran CNA’s advancement<br />
opportunities and recognition. The mentoring<br />
program did decrease recruitment and turnover<br />
costs and generated positive feedback from those<br />
involved.<br />
The <strong>Wyoming</strong> <strong>Nurse</strong>s Association received<br />
funding to develop a leadership institute, called<br />
the <strong>Wyoming</strong> <strong>Nurse</strong> Leadership Institute<br />
(WNLI). Leadership style and behaviors are<br />
associated with staff nurse job satisfaction and<br />
intent to stay and organizational commitment in<br />
both the US and in other countries. In a study<br />
by the <strong>Wyoming</strong> Department <strong>of</strong> Employment,<br />
satisfaction with salary, interpersonal relations<br />
Continued on page 8<br />
<strong>Nursing</strong><br />
Excellence<br />
Sign-on Bonus and<br />
Relocation Assistance<br />
- Director <strong>of</strong> Emergency Services<br />
- ER/ICU RNs<br />
Riverton Memorial Hospital is committed<br />
to nursing excellence. Join our team and<br />
make a difference in an environment where<br />
you will be appreciated. We provide<br />
medical, dental, vision, Life, AD&D, STD,<br />
LTD, EAP, 401(k), PTO, EIB, and<br />
competitive wages. EEO<br />
Call 307-857-3465 or<br />
email norma.atwood@lpnt.net<br />
Visit www.Riverton-Hospital.com<br />
Great People. Great Benefits. Great Pay.<br />
GREAT NURSING OPPORTUNITIES<br />
Relocation Assistance is Available!<br />
<strong>Wyoming</strong> Medical Center has openings for<br />
Registered <strong>Nurse</strong>s in the following departments:<br />
• OR <strong>Nurse</strong> Manager • Progressive Care Unit<br />
• Surgical Unit • Medical Unit • Neuro Unit<br />
Contact: Sammie Stephens RN <strong>Nurse</strong> Recruiter<br />
307.577.2669 • sstephens@wmcnet.org<br />
1233 E. 2nd St., Casper, WY 82601<br />
Equal Opportunity Employer<br />
Visit us online to apply: www.wyomingmedicalcenter.com<br />
<strong>Wyoming</strong> <strong>Nurse</strong> <strong>Reporter</strong> 7
and pr<strong>of</strong>essional development opportunities are<br />
strongly correlated to intent to stay/leave current<br />
nursing positions for <strong>Wyoming</strong> nurses. WNLI<br />
was developed to strengthen nursing leadership<br />
in the state <strong>of</strong> <strong>Wyoming</strong>. The Institute involved<br />
four face-to-face sessions addressing a variety <strong>of</strong><br />
topics including leadership competencies, nursing<br />
and health care policy, quality and patient safety,<br />
work with a mentor to provide support and<br />
guidance during the program, and completion <strong>of</strong><br />
a leadership project. Six participants completed<br />
the first institute, which has been continued for<br />
another year.<br />
Public Health <strong>Nursing</strong> in the <strong>Wyoming</strong><br />
Department <strong>of</strong> Health developed a statewide<br />
recruitment, retention and succession plan for<br />
<strong>Wyoming</strong> public health nursing. The projected<br />
nursing shortage and the upcoming retirement<br />
<strong>of</strong> PHNs was the major impetus for this project.<br />
This plan is imperative for a competent PHN<br />
workforce to promote and protect the health<br />
<strong>of</strong> <strong>Wyoming</strong> citizens (Robert Woods Johnson<br />
Foundation [RWJF], 2008). As part <strong>of</strong> the<br />
project, two preceptor manuals were developed<br />
to ensure that students had a meaningful and<br />
structured experience in public health nursing<br />
as a mechanism to recruit more graduates into<br />
public health. In addition, a consultant was<br />
hired to facilitate a retreat and the development<br />
<strong>of</strong> a succession plan. PHNs from all levels<br />
participated in the process used to development<br />
the plan. The preceptor manuals lead to more<br />
understanding <strong>of</strong> PHN by nursing faculty and<br />
helped PHNs develop their skills as preceptors.<br />
<strong>Wyoming</strong> Medical Center was funded to<br />
lengthen their traditional nursing orientation<br />
from three months to a yearlong graduate nurse<br />
residency program. <strong>Nurse</strong> residency programs<br />
are one <strong>of</strong> the “best practices” for recruitment<br />
and retention <strong>of</strong> graduate nurses (Altier & Krsek,<br />
2006). Graduate nurses participated in monthly<br />
didactic courses, unit specific orientation, a<br />
preceptor/mentor program, and interdisciplinary<br />
rotations through the hospital. As part <strong>of</strong> the<br />
project, preceptor education was enhanced<br />
through basic and advanced preceptor classes in<br />
order to enhance preceptor ability to stimulate<br />
critical thinking, evaluation <strong>of</strong> graduate nurse<br />
development and management <strong>of</strong> conflict. The<br />
12 month residency was more appealing to<br />
nurses applying to WMC and a majority <strong>of</strong> the<br />
new graduates successfully made the transition<br />
into their nursing roles at the hospital.<br />
Finally, Campbell County Memorial Hospital<br />
focused on improving preceptor education for<br />
nurses in acute and long-term care settings in<br />
northeastern <strong>Wyoming</strong>. The overall goal was<br />
to increase satisfaction by nurses who serve as<br />
preceptors and the pool <strong>of</strong> nurse preceptors<br />
available for nursing students and/or graduate<br />
nurses. The project staff worked with current<br />
preceptors, nurse managers and nurse educators<br />
to outline the knowledge and skills needed<br />
for nurses to be effective preceptors. Based on<br />
those competencies, a curriculum for preceptor<br />
education was developed with the goal that the<br />
education modules be available on-line. As a<br />
result <strong>of</strong> the project, a network for preceptors in<br />
northeastern <strong>Wyoming</strong> has been developed and<br />
managers remain passionate and committed to<br />
the project.<br />
Each <strong>of</strong> the project directors submitted a<br />
final evaluation report to the WCNHCP. In<br />
addition, Laran Despain and Laura Feldman,<br />
from the <strong>Wyoming</strong> Statistical & Analysis<br />
Center (WYSAC), conducted a systematic<br />
overall evaluation <strong>of</strong> the projects (available on<br />
the WCNHCPs website). This is a rich analysis<br />
and addresses outcomes related to recruitment,<br />
training, retention and sustainability, as well as<br />
describing the challenges faced by these nurses<br />
in implementing their projects. Despain and<br />
Feldman provide a number <strong>of</strong> recommendations<br />
to enhance the success <strong>of</strong> recruitment and<br />
retention projects. Overall, they conclude<br />
that projects, such as these described in<br />
this column, can improve recruitment and<br />
decrease recruitment costs. In relation to<br />
retention, job satisfaction can be increased<br />
through pr<strong>of</strong>essional development efforts,<br />
such as through preceptor training, although<br />
examining retention is challenging because not<br />
all facilities had mechanisms to collect this kind<br />
<strong>of</strong> data. To optimize training efforts, gathering<br />
regular participant feedback, using consultants,<br />
matching mentors and mentees, and facilitating<br />
regular contact between mentors and mentees<br />
are critical. To ensure sustainability <strong>of</strong> the<br />
projects, it is important to garner administrative<br />
support through ongoing participant feedback<br />
and find other funding and resources.<br />
Our congratulations to the nurses who<br />
directed these projects! They are strong<br />
examples <strong>of</strong> what nurses can do in this state to<br />
enhance the nursing workforce and meet the<br />
health needs <strong>of</strong> people in <strong>Wyoming</strong>.<br />
The WCNHCP is the nursing workforce<br />
center for the <strong>State</strong> <strong>of</strong> <strong>Wyoming</strong>. The mission<br />
<strong>of</strong> the center is to strengthen the nursing<br />
workforce through on-going collaboration,<br />
communication, and consensus building<br />
to meet the health needs <strong>of</strong> the people <strong>of</strong><br />
<strong>Wyoming</strong>. For further information, please visit<br />
the WCNHCP’s webpage at<br />
wynursing.org.<br />
Join one <strong>of</strong> state’s top<br />
healthcare teams in delivering<br />
outstanding patient care<br />
throughout south central<br />
<strong>Wyoming</strong>. Our facilities<br />
are state-<strong>of</strong>-the-art and our<br />
commitment to nursing<br />
excellence and positive patient<br />
outcomes is unmatched!<br />
Current opportunities:<br />
- Med/Surg<br />
- PRN/Per Diem<br />
- Case Manager<br />
- House Supervisor<br />
- Women’s Health<br />
- OutPatient Surgery<br />
We deliver world class<br />
care close to home.<br />
Discover for yourself why<br />
people fall in love with beautiful<br />
Lander Valley – Nestled against<br />
the foothills <strong>of</strong> the Wind River<br />
Mountains on the banks <strong>of</strong> the<br />
Popo Agie River, it is home to<br />
blue skies, breath taking scenery<br />
and adventure filled days.<br />
To apply, visit our website at<br />
www.landerhospital.com<br />
Lander Regional Hospital<br />
1320 Bishop Randall Drive<br />
Lander, WY 82520<br />
307-335-6580<br />
Fax 307-332-3548<br />
EOE<br />
8 <strong>Wyoming</strong> <strong>Nurse</strong> <strong>Reporter</strong>
Getting to Know <strong>Wyoming</strong> <strong>Nurse</strong>s<br />
Meet Michelle Mulberry<br />
Patti Gardner<br />
My name is Michelle Mulberry, RN, BSN.<br />
I have been a nurse in <strong>Wyoming</strong> since 1999.<br />
I decided to attend LCCC School <strong>of</strong> <strong>Nursing</strong><br />
after working as a paramedic for 5 years.<br />
While going to nursing school, I worked<br />
full time in the Emergency Department at<br />
CRMC as an ER tech. I completed my LPN<br />
in 1999. I continued to work full time as<br />
an LPN in the ER while I finished school<br />
and eventually graduated with my RN in<br />
2000. I later went on to complete my BSN<br />
through the University <strong>of</strong> <strong>Wyoming</strong>. I<br />
worked in the Emergency Department at<br />
CRMC in various nursing positions for<br />
a total <strong>of</strong> 10 years prior to moving to the<br />
Cheyenne VA Medical Center, where I<br />
am currently the Mobile Telehealth Clinic<br />
Coordinator. My role at the VA is to<br />
facilitate providing primary care and mental<br />
health to veterans in rural and highly rural<br />
areas <strong>of</strong> <strong>Wyoming</strong> and Colorado. The clinic<br />
travels to Sterling, Colorado, Wheatland,<br />
Torrington, and Laramie, <strong>Wyoming</strong> and<br />
conducts primary care and mental health<br />
visits via Telehealth.<br />
Working with our veterans is very near<br />
and dear to my heart. I come from a very<br />
military family. My father a retired Army<br />
Colonel, my older sister, currently serving a<br />
second tour in Iraq, is a Lieutenant Colonel,<br />
and my younger sister is a Staff Sergeant<br />
who, after completing a tour in Afghanistan,<br />
completed her Law Degree in North Dakota,<br />
and continues to serve in the North Dakota<br />
Army National Guard. I am currently<br />
a member <strong>of</strong> the <strong>Wyoming</strong> Air National<br />
Guard and have been in the military for 21<br />
years. I spent 10 years in the Army National<br />
Guard both in North Dakota and <strong>Wyoming</strong>,<br />
where I flew as a medic on Blackhawk<br />
helicopters. Upon completion <strong>of</strong> my nursing<br />
degree, I wanted to stay in the military and<br />
stay flying, so I transferred to the <strong>Wyoming</strong><br />
Air National Guard in Sept <strong>of</strong> 2000, where<br />
I began flying as a flight nurse on C-130s.<br />
In 2004 I deployed to Al Udeid Air Base,<br />
Qatar, where I flew Aeromedical Evacuation<br />
(AE) missions in and around Iraq and<br />
Kuwait. In 2007, I deployed to Bagram Air<br />
Field, Afghanistan, where I again flew AE<br />
missions in and around Afghanistan and on<br />
occasion to Ramstein, Germany. In 2009 I<br />
deployed to Andrews Air Force Base, MD,<br />
flying AE missions up and down the coast,<br />
returning the wounded to military bases as<br />
close to their home station as possible. This<br />
last year, I did my fourth deployment to<br />
Ramstein Air Base, Germany, where I flew<br />
into and out <strong>of</strong> Iraq, Kuwait, Afghanistan<br />
and back to the United <strong>State</strong>s. Between the<br />
C-130, C-17 and KC-135, I have flown over<br />
1000 hours, 468 <strong>of</strong> those are combat hours.<br />
I am currently in an on-line Master’s<br />
program for the military. I began the program<br />
last year, and plan to have it completed by<br />
April <strong>of</strong> 2012.<br />
I am blessed with the most amazing family.<br />
My husband Ron and I have been married<br />
for almost 12 years. He is a Lieutenant<br />
working for Cheyenne Fire and Rescue in<br />
Cheyenne. I also have two wonderful step<br />
children, Jessica, 19 and David, 16. They<br />
have all been so supportive during all <strong>of</strong> my<br />
deployments , school, etc. Ron and I live<br />
on 11 acres NE <strong>of</strong> Cheyenne with our two<br />
lab dogs, Libby and Oprah. A typical day at<br />
the Mulberry’s starts at 0415, when Ron and<br />
I get up and do an hour <strong>of</strong> P90X before we go<br />
to work, and then we meet at the gym after<br />
work for an hour <strong>of</strong> cardio. Fitness is very<br />
important to both <strong>of</strong> us. With the jobs we<br />
have we must be at the top <strong>of</strong> our fitness at<br />
all times, so this is pretty much our routine<br />
6 days a week. We are a very active family,<br />
to say the least.<br />
Being a nurse has <strong>of</strong>fered me so many<br />
opportunities in life I would not have<br />
otherwise had. I always say being a flight<br />
nurse in the military is the most rewarding<br />
job I have ever had, and I truly mean that.<br />
I have had the privilege <strong>of</strong> traveling all over<br />
the world and meeting so many wonderful<br />
people. Most importantly I have been<br />
blessed and have had the honor <strong>of</strong> meeting<br />
and transporting some true American hero’s,<br />
our military men and women.<br />
<strong>Wyoming</strong> <strong>Nurse</strong> <strong>Reporter</strong> 9
Returning to School: Is It Right for You?<br />
Pamala D. Larsen<br />
The kids need picked up from soccer<br />
practice and ballet and you’re late, again. You<br />
didn’t sleep that well during the morning and<br />
then fell asleep hard around 1 p.m., making<br />
you late for the soccer and ballet car pools.<br />
Plus you need to be back at the hospital by<br />
6:45 p.m. for your shift. Although you’d been<br />
thinking about going back to school for your<br />
BSN, on days like this, how in the world<br />
could you ever fit it into your life? There<br />
just isn’t enough time. It’s the start <strong>of</strong> a new<br />
semester and a number <strong>of</strong> your colleagues<br />
are taking classes. But you hesitate because<br />
<strong>of</strong> the time commitment, family obligations,<br />
work obligations, and for you, a primary issue<br />
is….will my brain cells still work? Your brain<br />
works fine at work, but writing a paper for<br />
school, doing the readings, participating in<br />
threaded discussions (whatever the heck<br />
those are)?<br />
The decision to go back to school is always<br />
a tough one. You worry about the timing <strong>of</strong><br />
doing it now versus later. Will things just<br />
fall into place and make sense? How much<br />
financial support, if any, will I get from my<br />
employer? And what could they possibly<br />
teach me that I haven’t already learned from<br />
my previous education and my experience?<br />
Cullen and Asselin (2009) <strong>of</strong>fer several<br />
questions for prospective students to<br />
consider. In addition, I’ve added my own<br />
comments from various students I’ve talked<br />
with over the years.<br />
• Do you want to prepare for another<br />
position in nursing? In your facility or<br />
another one?<br />
o Think hard…..what do you really want<br />
to be when you ‘grow up’? Allow time to<br />
think and daydream about ‘what if’?<br />
• Do you need the degree for advancement<br />
in your facility?<br />
o Perhaps you need this degree for<br />
certification in your area, or your facility is<br />
on the Magnet journey and administration<br />
is pushing everyone towards school?<br />
• Do you like to study?<br />
o Ok, perhaps that’s not a fair question, but<br />
think about experiences on your unit. Do<br />
you seek out learning opportunities? Are<br />
you a staff member that is always looking<br />
for the latest evidence on a clinical issue?<br />
• How will you balance school, work and<br />
your personal life?<br />
o This is definitely the tricky part. Balance<br />
is the key word. However, I think you<br />
will find that you are more efficient with<br />
your ‘time to study’ when you don’t have<br />
much time. Many <strong>of</strong> your colleagues<br />
have worked part-time or full-time while<br />
pursuing a higher degree. Find that magic<br />
time that is ‘all yours’ to study.<br />
• Is the timing right for you to return to<br />
school? Do you have support from family<br />
and friends to return to school?<br />
o This is a toughie that only you can answer.<br />
Don’t expect the stars to be in alignment<br />
and everything goes perfectly. That just<br />
doesn’t happen. Most RN-BSN programs<br />
encourage part-time study, and students<br />
may take just 1 course/semester or even sit<br />
out a semester when things are tough at<br />
work and home.<br />
• Will your peers at work be supportive?<br />
o There are many working RNs that are<br />
returning to school so I’m guessing that<br />
finding a support group at work will<br />
be relatively easy to do. However, be<br />
prepared to field questions from some<br />
peers such as…….who do you think you<br />
are going back to school? They could be<br />
jealous and want to do it as well. Do you<br />
have the support <strong>of</strong> your unit’s manager/<br />
head nurse//patient care coordinator, etc?<br />
Are they willing to work with you and<br />
your schedule? Are they willing to provide<br />
some financial assistance?<br />
(Cullen & Asselin, 2009, p. 33)<br />
After making the decision to return to<br />
school, determine the type <strong>of</strong> program that<br />
is best for you. Obviously, I think UW’s<br />
program is top-notch (if you’ve not been in<br />
touch with the program within the last 3-4<br />
years, give us a call. You will find that many<br />
things have changed), but there are lots <strong>of</strong><br />
things to consider as you return to being a<br />
student. The majority <strong>of</strong> RN-BSN programs<br />
available across the country are on-line<br />
programs. These programs are <strong>of</strong>fered strictly<br />
on the internet, and you don’t go to a campus<br />
or classroom. On-line programs are great<br />
for that reason, but the real issue is staying<br />
focused to complete your work on-line and<br />
making the time for it. On-line programs<br />
aren’t any easier than face to face programs.<br />
UW counsels students to plan on spending 3<br />
hours a week for a 1 credit course, translating<br />
into 9 hours a week for a standard 3 credit<br />
hour course. However, the advantages <strong>of</strong><br />
working on the class when you have time<br />
<strong>of</strong>ten outweighs the standard class times.<br />
Students <strong>of</strong>ten ask the School <strong>of</strong> <strong>Nursing</strong><br />
to send information about our program. We<br />
do not have standard written materials on<br />
the program (or any <strong>of</strong> our programs). The<br />
most up-to-date information is always on the<br />
webpage (http://www.uwyo.edu/NURSING/<br />
programs/RN-BSN%20Completion/index.<br />
html) The School <strong>of</strong> <strong>Nursing</strong> has two fulltime<br />
administrative staff that are always<br />
available to answer questions for you as well<br />
as any <strong>of</strong> our RN-BSN faculty (307-766-<br />
3907 or email RN.BSN@uwyo.edu)<br />
Finally, one <strong>of</strong> our current MS nurse<br />
practitioner students, Corrie Carver, recently<br />
posted a comment in one <strong>of</strong> her classes, and I<br />
asked her permission to use it in this article.<br />
Although she did not graduate from the<br />
RN-BSN program at UW, she is a staunch<br />
supporter <strong>of</strong> RN-BSN education. Corrie<br />
writes, “Little did I know, that while in<br />
the RN to BS program, I would learn how<br />
to REALLY be a nurse. I was amazed at the<br />
level <strong>of</strong> understanding I gained during that<br />
extra year <strong>of</strong> instruction. I learned how to<br />
better relate to and communicate with my<br />
patients. Looking back I now realize that as<br />
an ADN I understood the ‘physical’ aspect <strong>of</strong><br />
the pr<strong>of</strong>ession, but it wasn’t until I became a<br />
BSN that I started to understand the art and<br />
‘mental’ side <strong>of</strong> the pr<strong>of</strong>ession”.<br />
If RN-BSN education is in your future,<br />
please give us a call or email us at the Fay W.<br />
Whitney School <strong>of</strong> <strong>Nursing</strong> at the University<br />
<strong>of</strong> <strong>Wyoming</strong>. Good luck as you continue<br />
your education!<br />
Pamala D. Larsen, PhD, CRRN,<br />
FNGNA<br />
Associate Dean for Academic Affairs<br />
Fay W. Whitney School <strong>of</strong> <strong>Nursing</strong><br />
University <strong>of</strong> <strong>Wyoming</strong><br />
Laramie, <strong>Wyoming</strong><br />
Source: Cullen, H.A., & Asselin, M.E.<br />
(2009). Why go back for a baccalaureate<br />
degree? American <strong>Nurse</strong> Today, 4(5),<br />
33-34.<br />
10 <strong>Wyoming</strong> <strong>Nurse</strong> <strong>Reporter</strong>
Fay W. Whitney<br />
SCHOOL OF NURSING<br />
On the Peak <strong>of</strong> Excellence!<br />
Fay W. Whitney School oF nurSing<br />
The Fay W. Whitney School <strong>of</strong> <strong>Nursing</strong> has an atmosphere<br />
that is friendly, scholarly, pr<strong>of</strong>essional and forwardminded.<br />
Join an exciting and dynamic community where<br />
active learning and teacher-student partnerships, scholarly<br />
practice, interpr<strong>of</strong>essional education and practice, and rural<br />
health care are valued.<br />
Fay W. Whitney School oF nurSing<br />
www.uwyo.edu/nursing • (307) 766-4312<br />
~ Dr. Mary E. Burman, Dean and Pr<strong>of</strong>essor<br />
· <strong>State</strong>-<strong>of</strong>-the-Art nursing school with Simulation<br />
Center for hands on experience<br />
· Offering three ways to obtain a baccalaureate<br />
degree in nursing<br />
· Offering two graduate degrees: <strong>Nurse</strong> Educator and<br />
<strong>Nurse</strong> Practitioner (FNP or PMHNP)<br />
· UW graduates are highly valued throughout <strong>Wyoming</strong><br />
and the region<br />
Accredited by the Commission on Collegiate<br />
<strong>Nursing</strong> Education (CCNE)<br />
You Dreamed<br />
<strong>of</strong> Being a<br />
<strong>Nurse</strong>.<br />
Now Become the<br />
<strong>Nurse</strong> You Dreamed<br />
<strong>of</strong> Being.<br />
One <strong>of</strong> “America’s Best Colleges”<br />
U.S. News & World Report<br />
Earn Your RN<br />
to BSN Online!<br />
RNs: Get 30<br />
Credits Free!<br />
Call 800-571-4934<br />
JacksonvilleU.com/PC<br />
© 2009 All Rights Reserved.<br />
Made Available by University Alliance ® –<br />
The Nation’s Leading Universities Online.<br />
SC: 191734zj1 | MCID: 2742<br />
EOE<br />
Behavioral Health<br />
<strong>Nursing</strong> Supervisor<br />
Rapid City Regional Hospital, a 417-bed Regional<br />
Referral Center located in the beautiful and historic<br />
Black Hills <strong>of</strong> South Dakota, has a full-time opening<br />
for a <strong>Nursing</strong> Supervisor in Behavioral Health.<br />
This position exists within the Behavioral Health<br />
Child / Adolescent inpatient unit, and will manage<br />
the clinical program through staff supervision, quality<br />
I<br />
leadership, continuity <strong>of</strong> work flow, patient care and n the Black Hills, you’ll discover a great place<br />
safety. Position requires a current SD RN license with<br />
to live<br />
a<br />
and a great place to work. We’ve invested<br />
our resources to create a career environment<br />
Bachelors Degree in nursing or related field and at least<br />
built upon a commitment to excellence. You’ll find<br />
three years’ clinical experience.<br />
yourself putting compassion into practice while<br />
RCRH <strong>of</strong>fers a competitive salary and an you work with leading-edge technology.<br />
excellent benefit Call package, Today including relocation Regional Health, a system <strong>of</strong> hospitals, clinics,<br />
1-800-865-2638<br />
assistance.<br />
and senior care facilities, <strong>of</strong>fers the best <strong>of</strong> both<br />
or visit<br />
worlds to nurses: competitive pay and benefits<br />
Apply on-line at www.regionalhealth.com for<br />
www.regionalhealth.com<br />
for current IRC5134 openings<br />
job and descriptions, upload or and fax a benefits resume.<br />
13790-0710<br />
presented with valuable opportunities for career<br />
development in an atmosphere <strong>of</strong> respect where<br />
the sky is the limit— inside and out.<br />
It’s no wonder our nurses<br />
find it hard to leave.<br />
Rapid City Regional Hospital • CusteR Regional Hospital • lead-deadwood Regional Hospital<br />
speaRfisH Attn: Regional Judy McCarthy, Hospital • stuRgis Recruiter Regional Hospital<br />
Equal Opportunity Employer<br />
Rapid City, SD 57701<br />
Email: jmccarthy@regionalhealth.com<br />
(800) 865-2638<br />
Fax: (605) 719-5500<br />
<strong>Wyoming</strong> <strong>Nurse</strong> <strong>Reporter</strong> 11
Improving Patient Care<br />
First CNA II Training Class Held in Gillette<br />
The state’s first CNA II training class was<br />
held January 17-21, <strong>2011</strong> at Campbell County<br />
Memorial Hospital. Todd Berger, Practice and<br />
Education Consultant, traveled to Gillette to<br />
personally talk with the students and answer<br />
questions about the program. Six CNAs<br />
completed the one week training and then had<br />
to verify competency in the hospital under the<br />
supervision <strong>of</strong> other nursing staff.<br />
This is the first CNA II program organized<br />
after the approval <strong>of</strong> the changes to Chapter 7 <strong>of</strong><br />
the Certified <strong>Nursing</strong> Assistant Administrative<br />
Rules and Regulations in July 2010. The CNA<br />
II program allows CNAs who meet certain<br />
requirements to take advanced training in specific<br />
skills. These skills may include oxygen therapy,<br />
sterile technique, wound care, oropharyngeal<br />
suctioning, tracheostomy care for patients<br />
with well established tracheostomies, urinary<br />
catheter, PEG tubes, elimination procedures,<br />
and responding to mental health needs. The<br />
CNA II role was designed to improve patient<br />
care by augmenting licensed nurses in providing<br />
skilled care for STABLE patients. The goal <strong>of</strong><br />
Powell Valley Healthcare is a<br />
facility<br />
Powell<br />
dedicated<br />
Valley Healthcare<br />
to improving<br />
is a<br />
facility<br />
quality<br />
dedicated<br />
<strong>of</strong> life through<br />
to improving<br />
excellent<br />
quality <strong>of</strong><br />
healthcare.<br />
life through<br />
We are<br />
excellent<br />
looking for<br />
healthcare.<br />
outstanding<br />
team<br />
We are<br />
members<br />
looking for<br />
that<br />
outstanding<br />
want to<br />
grow within our organization.<br />
Powell Valley Healthcare is a<br />
facility team dedicated members that to improving want to<br />
quality <strong>of</strong> life through<br />
Located<br />
grow within<br />
excellent<br />
near<br />
our<br />
healthcare.<br />
Yellowstone<br />
organization.<br />
Located near Yellowstone<br />
We are looking for outstanding<br />
team members that want to<br />
grow by within our organization.<br />
opportunity<br />
mountains,<br />
Located near<br />
for<br />
there<br />
Yellowstone<br />
outdoor<br />
is ample<br />
National recreation<br />
opportunity<br />
Park year<br />
for<br />
and around.<br />
outdoor<br />
surrounded<br />
by recreation mountains, year there around. is ample<br />
opportunity for outdoor<br />
recreation year around.<br />
National Park and surrounded<br />
by<br />
National<br />
mountains,<br />
Park<br />
there<br />
and surrounded<br />
is ample<br />
this new rule is to improve patient outcomes by<br />
allowing designated CNAs to perform certain<br />
routine nursing procedures, thereby freeing<br />
the licensed nurse to focus on other aspects <strong>of</strong><br />
pr<strong>of</strong>essional nursing care.<br />
WSBN expects that with the success <strong>of</strong><br />
this training program we will be able to <strong>of</strong>fer a<br />
template to other facilities looking to provide<br />
the training for CNA II advancement. Special<br />
recognition goes to Susan Howard MSN, RN,<br />
Clinical Education Supervisor at Campbell<br />
County Memorial Hospital for her work<br />
initiating the course and developing course<br />
materials.<br />
For more information on the CNA II<br />
requirements and standards read Chapter 7,<br />
sections 10-12 <strong>of</strong> the Rules and Regulations<br />
found on WSBN website under information.<br />
As information becomes available regarding<br />
the pilot program <strong>of</strong> the CNA II course it will<br />
be posted on the WSBN website. If you or<br />
your facility are considering <strong>of</strong>fering a CNA II<br />
program, please contact Todd Berger at tberge@<br />
wyo.gov for details.<br />
Instructors and students <strong>of</strong> the first <strong>Wyoming</strong><br />
CNAII Class<br />
Checking tube feeding<br />
Practicing sterile technique<br />
An experience with us includes:<br />
•<br />
An<br />
Generous<br />
experience<br />
compensation<br />
with<br />
based<br />
us<br />
on<br />
includes:<br />
years <strong>of</strong><br />
•<br />
experience<br />
Generous compensation based on years <strong>of</strong><br />
• Career<br />
experience<br />
Ladder that recognizes achievements in<br />
•<br />
education,<br />
Career Ladder<br />
certification,<br />
that recognizes<br />
cross-training,<br />
achievements<br />
quality,<br />
in<br />
and<br />
education,<br />
mentorship<br />
certification, cross-training, quality,<br />
• Differential for evenings & nights<br />
• Tuition Reimbursement<br />
• Paid time <strong>of</strong>f starting at 18 days<br />
• Health insurance, including dental & vision<br />
• Retirement plan<br />
• Life & Disability insurance<br />
• Extended Illness Plan<br />
An experience with us includes:<br />
• Generous<br />
and mentorship<br />
compensation based on years <strong>of</strong><br />
• experience Differential for evenings & nights<br />
•<br />
•<br />
Career<br />
Tuition<br />
Ladder<br />
Reimbursement<br />
that recognizes achievements in<br />
education, certification, cross-training, quality,<br />
•<br />
and<br />
Paid<br />
mentorship<br />
time <strong>of</strong>f starting at 18 days<br />
• • Differential Health insurance, for evenings including & nights dental & vision<br />
•<br />
•<br />
Tuition<br />
Retirement<br />
Reimbursement<br />
plan<br />
• Paid time <strong>of</strong>f starting at 18 days<br />
•<br />
•<br />
Health<br />
Life &<br />
insurance,<br />
Disability insurance<br />
including dental & vision<br />
• • Retirement Extended plan Illness Plan<br />
• Life & Disability insurance<br />
• Extended Illness Plan<br />
12 <strong>Wyoming</strong> <strong>Nurse</strong> <strong>Reporter</strong>
Inside Scoop<br />
News, Requests, Updates<br />
<strong>Board</strong> Staff Position<br />
WSBN currently has a job opening for<br />
the position <strong>of</strong> Compliance Consultant.<br />
This full time position handles complaints<br />
and investigations into disciplinary matters<br />
for the board. Must have a minimum <strong>of</strong><br />
a Bachelor’s degree in nursing or closely<br />
related field PLUS five years <strong>of</strong> pr<strong>of</strong>essional<br />
work experience as Registered <strong>Nurse</strong> (RN).<br />
Must be licensed or eligible for licensure<br />
as a Registered <strong>Nurse</strong> (RN) in the <strong>State</strong> <strong>of</strong><br />
<strong>Wyoming</strong>. For a full job description and<br />
online application go to:http://statejobs.<br />
state.wy.us/JobSearchDetail.aspx?ID=17886<br />
Become a <strong>Nursing</strong> Leader<br />
Interested in being involved in <strong>Board</strong><br />
Activities? Would you like to make your<br />
thoughts known on a certain issue? Is there<br />
a topic you want the board to consider? It is<br />
easy to be involved with WSBN.<br />
Are you aware <strong>of</strong> WSBN website listing<br />
all board meetings?<br />
Are you aware that all board meetings are<br />
open to the public?<br />
Would you attend a board meeting if it<br />
was held near your home?<br />
If you would be interested in more<br />
information regarding these or any other<br />
board matters please contact us at wynursing@<br />
state.wy.us .<br />
NCSBN Institute <strong>of</strong> Regulatory<br />
Excellence<br />
to developing administrative regulations and<br />
supporting research that helps formulate<br />
regulatory policy. WSBN has been involved<br />
with the IRE for many years and Mary Beth<br />
Stepans, the previous Education and Practice<br />
Consultant, was a member <strong>of</strong> the IRE research<br />
proposal review committee.<br />
The <strong>Wyoming</strong> <strong>Nurse</strong> <strong>Reporter</strong><br />
wants you!<br />
Are you doing something unique,<br />
challenging, cutting-edge or newsworthy<br />
in some way? Are you volunteering, did<br />
you change your life, have you overcome<br />
obstacles to get where you are? We want your<br />
story! The <strong>Wyoming</strong> <strong>Nurse</strong> <strong>Reporter</strong> would<br />
love to introduce you to nurses all over the<br />
state! Email us about yourself or a colleague<br />
@ WNREditor@aol.com. We want to hear<br />
from you!<br />
Getting to Know <strong>Wyoming</strong> <strong>Nursing</strong><br />
Students!<br />
<strong>Wyoming</strong> <strong>State</strong> <strong>Board</strong> <strong>of</strong><br />
<strong>Nursing</strong> Updates<br />
As we exit the renewal cycle, the licensing<br />
department will be looking closely at all<br />
processes. We are mapping out the tasks we<br />
do on a daily basis to create efficiencies and<br />
eliminate redundancies. We hope to improve<br />
licensing time as we find ways to make the<br />
licensing process more efficient.<br />
Staff Member Spotlight<br />
Maxine Hernandez has been with the<br />
WSBN since May 2008. She works in the<br />
licensing department and works primarily<br />
with processing applications and issuing<br />
new licenses. She has a great amount<br />
<strong>of</strong> knowledge about the WSBN nursing<br />
database and continues to streamline the<br />
application process. Her expertise has<br />
helped thousands <strong>of</strong> nurses and CNAs start<br />
their careers.<br />
Roseanne Colosimo, Nevada BON, Nancy<br />
Spector NCSBN Director <strong>of</strong> Regulatory<br />
Innovations, and Todd Berger, WSBN<br />
Assistant Executive Director at the <strong>2011</strong><br />
NCSBN Annual Institute <strong>of</strong> Regulatory<br />
Excellence Conference in February. The IRE<br />
focuses on evidence based practice as it applies<br />
Know an up and coming <strong>Nursing</strong> Student<br />
in <strong>Wyoming</strong> who deserves to be recognized?<br />
Contact us at WNReditor@aol.com with<br />
their name and contact information and<br />
we’ll pr<strong>of</strong>ile them in an upcoming issue <strong>of</strong> the<br />
<strong>Wyoming</strong> <strong>Nurse</strong> <strong>Reporter</strong>. An easy way to<br />
recognize excellence!<br />
Debra Ball started working with the<br />
WSBN in 2006. She previously served as<br />
a Licensing Coordinator and has been the<br />
WSBN Discipline Assistant since April,<br />
2008. She assists the Compliance Consultants<br />
with complaint investigations; investigating<br />
applications with “yes” answers to the history<br />
questions and she forwards applications<br />
needing further review to the Application<br />
Review Committee.<br />
<strong>Wyoming</strong> <strong>Nurse</strong> <strong>Reporter</strong> 13
Getting to Know <strong>Wyoming</strong> <strong>Nurse</strong>s<br />
Meet Mariusz Pieczalski<br />
Patti Gardner<br />
My name is Mariusz<br />
Pieczalski, I was born in<br />
Poland and lived there for<br />
the first 27 years <strong>of</strong> my life.<br />
As many young people in<br />
a communist country do, I<br />
dreamed <strong>of</strong> living in a free<br />
and democratic country,<br />
with a lot <strong>of</strong> opportunities. I<br />
graduated from nursing school<br />
with a diploma in <strong>Nursing</strong> in<br />
1982 and my destiny brought<br />
me initially to Italy, where I<br />
spent 3 years. I learned a new<br />
language and began to pursue<br />
my career in nursing. This<br />
was my first time taking care<br />
<strong>of</strong> elderly patients in various<br />
While working with the elderly population I have<br />
grown a lot pr<strong>of</strong>essionally and personally. Their<br />
gratitude and appreciation fueled my desire to work<br />
and help patients and their families to heal and/or<br />
deal with end <strong>of</strong> life issues.<br />
settings; from hospitals to private homes. I surprised myself as I<br />
found a lot <strong>of</strong> satisfaction working with this patient population in<br />
a completely different culture from my own. Dealing with chronic<br />
diseases and end <strong>of</strong> life issues helped me to gain a new prospective<br />
on nursing and to develop a more multicultural approach to the<br />
patient’s I cared for.<br />
I had an opportunity to immigrate to South Africa, Canada or<br />
Australia and eventually I decided to travel to Canada, to look at<br />
nursing in a new way and maybe to even look at a different nursing<br />
practice. I had to learn English and complete a Total Upgrading<br />
<strong>Nursing</strong> Program to update my credentials and to be eligible to take<br />
a Canadian Licensing <strong>Board</strong> Examination. I learned the language<br />
and passed the exam with no difficulties and started my career in<br />
the Canadian health care system. I worked in a <strong>Nursing</strong> home<br />
mostly with an elderly Asian population. I gained another view<br />
on practicing nursing and another exposure to yet another culture,<br />
their approach to illness, healing and the rehabilitation process.<br />
My wife was a physician and wanted to go to the United <strong>State</strong>s<br />
to pursue her pr<strong>of</strong>essional career and I have followed her. It had<br />
been a tough time for both <strong>of</strong> us; for me trying to prepare for the<br />
CGFNS (Commission on Graduate <strong>of</strong> Foreign <strong>Nursing</strong> School--an<br />
exam foreign nurses have to take in order to practice in the US)<br />
exam with a 6month old son and for my wife who had to spend the<br />
majority <strong>of</strong> her time in the hospital during residency. I have to<br />
admit that was a most difficult exam to pass, however, I overcame<br />
that obstacle as well.<br />
With many opportunities in front <strong>of</strong> me, I decided to pursue my<br />
pr<strong>of</strong>essional career as a nurse at Acute Care for Elderly at University<br />
<strong>of</strong> Texas in Galveston. This was a highly specialized unit with a team<br />
<strong>of</strong> Geriatricians and board certified Geriatric <strong>Nurse</strong>s with a widely<br />
recognized Geriatric residency program that had a model approach<br />
on Holistic Elderly Care. I joined the team and gained a lot <strong>of</strong> new<br />
knowledge and experience and after some time there, I decided to<br />
take the board certification exam in geriatric nursing..<br />
While working with the elderly population I have grown a lot<br />
pr<strong>of</strong>essionally and personally. Their gratitude and appreciation<br />
fueled my desire to work and help patients and their families to heal<br />
and/or deal with end <strong>of</strong> life issues. Understanding health issues in the<br />
geriatric population is a key issue in prevention as well as treatment<br />
<strong>of</strong> many medical conditions . Polypharmacy and multiple chronic<br />
illnesses <strong>of</strong>ten make diagnosis and treatment a very challenging<br />
task. I am happy I can share my knowledge and experience with my<br />
colleagues, patients and families to improve their health and lives.<br />
Mariusz currently works as a charge nurse on the Transitional<br />
Care Unit at Cheyenne Regional Medical Center at TCU Unit. He<br />
is board certified in Geriatric <strong>Nursing</strong>.<br />
14 <strong>Wyoming</strong> <strong>Nurse</strong> <strong>Reporter</strong>
LICENSE<br />
TROUBLE?<br />
SUSPENSION?<br />
SEEKING<br />
REINSTATEMENT?<br />
Have you received a letter for<br />
suspension or discipline? You worked<br />
hard for your license so don’t make an<br />
uninformed decision about the future<br />
<strong>of</strong> your career. Remember you have<br />
options and we can help.<br />
PROFESSIONALS<br />
HELPING<br />
PROFESSIONALS<br />
NOW WE KNOW<br />
… WHAT TO SAY WHEN ASKED ABOUT ADOPTION.<br />
Learn best adoption practices allowing you to better serve those<br />
experiencing an unintended pregnancy. The Infant Adoption Training<br />
Initiative enhances understanding and knowledge about current<br />
adoption practice, laws, birth fathers and referral strategies.<br />
For training dates and locations, and for quick and easy online registration, simply visit<br />
our Web site at www.infantadoptiontraining.org or contact us at 1.888.201.5061.<br />
“All <strong>of</strong> the information was very beneficial.<br />
Thank you for the program.”<br />
To us,<br />
exploration<br />
is a way <strong>of</strong><br />
life.<br />
–Director <strong>of</strong> <strong>Nursing</strong><br />
This project is funded through the Children’s Bureau<br />
<strong>of</strong> the U.S. Department <strong>of</strong> Health and Human Services.<br />
WOODHOUSE RODEN, LLC<br />
Attorneys at Law<br />
We seek it, we find it. Groundbreaking accomplishments,<br />
medical innovations that improve<br />
the way we care for our patients and dynamic,<br />
passionate leaders like you. At Cheyenne<br />
Regional Medical Center, where growth is<br />
ongoing, we <strong>of</strong>fer stimulating careers and a<br />
warm, friendly environment with opportunities<br />
to achieve more.<br />
1912 Capitol Avenue, Suite 500<br />
Cheyenne, WY 82033<br />
307/432-9399<br />
Partner: Gay Woodhouse<br />
gaywoodhouselaw@aol.com<br />
Partner: Deborah Roden<br />
debb@woodhouseroden.com<br />
Associate: Tara Nethercott<br />
tara@woodhouseroden.com<br />
Careers that blend heart<br />
science.<br />
• Certified <strong>Nursing</strong> Assistants<br />
• Registered <strong>Nurse</strong>s<br />
• Charge <strong>Nurse</strong>s<br />
• Advanced Practice <strong>Nurse</strong>s<br />
• Clinical Managers<br />
• Clinical Documentation Specialists<br />
Life is good here. We <strong>of</strong>fer a generous benefi ts<br />
and compensation package.<br />
Contact:<br />
Teresa McCarrel, Talent Consultant<br />
214 East 23rd Street • Cheyenne, WY 82001<br />
Phone: 888-967-5862 or 307-633-7639<br />
Email: teresa.mccarrel@crmcwy.org<br />
www.crmcwy.org/career<br />
EOE<br />
© <strong>2011</strong> NAS<br />
(Media: delete copyright notice)<br />
<strong>Wyoming</strong> <strong>State</strong> <strong>Board</strong> <strong>of</strong> <strong>Nursing</strong><br />
<strong>Wyoming</strong> <strong>Nurse</strong> <strong>Reporter</strong> 15
P Q R S T<br />
(Practice Questions Requiring Substantial Thought)<br />
Q & a<br />
Q I am a new nurse working in <strong>Wyoming</strong> and<br />
am wondering what the NPA (nurse practice<br />
act) states regarding RNs and abnormal result<br />
notifications (labs, rads, pathology).<br />
A Your facility would have their own policy<br />
regarding reporting <strong>of</strong> critical results. It is a<br />
JCAHO requirement to address this issue.<br />
WSBN regulates nursing practice, not facility<br />
policy. As an RN you would be held accountable<br />
for recognizing abnormal lab values, the effect<br />
they would have on your patient, and taking<br />
appropriate action for the patient’s care.<br />
Q I am taking courses to get into the nursing<br />
program in Casper. I am taking Medical<br />
Terminology and Microbiology this fall. I was<br />
wondering if they count as hours for CNA<br />
continuing education?<br />
A The prerequisite courses you list are not<br />
integral to CNA practice and would not count<br />
(also they would be in 2010 and the next 2<br />
year renewal period starts in Jan <strong>2011</strong>). If you<br />
start a nursing program in the next 2 years one<br />
<strong>of</strong> the first semester courses will be devoted to<br />
basic patient care. That is generally accepted<br />
as qualifying for education hours toward CNA<br />
renewal. Academic semester credit hours equal<br />
15 contact hours each and most <strong>of</strong> these courses<br />
are 2-3 credit hours so you would be covered if<br />
you get into a nursing program.<br />
Q I am wondering if there has already been a<br />
position statement written regarding trained<br />
RN’s providing conservative sharp debridement<br />
in the state <strong>of</strong> <strong>Wyoming</strong>.<br />
If not, would the next step be to complete a<br />
decision tree outline and submit it to <strong>Wyoming</strong><br />
<strong>State</strong> board <strong>of</strong> <strong>Nursing</strong>? I am developing a<br />
policy for the facility that I work at to cover<br />
me in doing SD.<br />
A <strong>Nurse</strong>s can become certified in wound care<br />
and have greater authority to accept delegation <strong>of</strong><br />
certain tasks. Certification courses <strong>of</strong>ten include<br />
debridement as part <strong>of</strong> their overall curricula.<br />
<strong>Nurse</strong>s should look for courses accredited by<br />
the Wound Ostomy and Continence <strong>Nursing</strong><br />
Certification <strong>Board</strong>. My question for you is<br />
did your Wound certification prepare you to do<br />
debridement and are you competent to provide<br />
this service? Does your facility allow you to<br />
provide this service? Will you be providing this<br />
service under a Doctor’s order or are you making<br />
the wound management decisions as part <strong>of</strong><br />
your job? Although many previous opinions<br />
have been eliminated in favor <strong>of</strong> utilizing the<br />
Decision tree model to determine scope issues,<br />
there is a WSBN opinion from 1997 (97-77)<br />
that said in effect “that sharps debridement may<br />
be considered a delegated function from the<br />
surgeon to the registered nurse. Any registered<br />
nurse accepting such delegation will need to be<br />
appropriately educationally and experientially<br />
prepared for this procedure and any such<br />
delegation should be case specific, client specific,<br />
and nurse specific.”<br />
To determine your personal scope <strong>of</strong> practice<br />
I refer you to the Decision Tree Model found<br />
on our website under opinions. Work through<br />
it and if you have questions you may submit it<br />
to the board for an opinion. You might also<br />
consider the acronym LACEE in your policy<br />
statement; licensure / accreditation / certification<br />
/ education / experience. This is a concept under<br />
consideration in conjunction to the Decision<br />
Tree Model. Each <strong>of</strong> these can provide weight<br />
to the decision and ability to shape practice in a<br />
specific area.<br />
Q If someone suffering from a chronic pain<br />
condition is taking a long term narcotic<br />
prescription, will she be able to still receive a<br />
CNA license through the state <strong>of</strong> <strong>Wyoming</strong>?<br />
A Thanks for contacting the WSBN. First <strong>of</strong>f,<br />
let me correct one thing. The term narcotic<br />
is <strong>of</strong>ten misused. Narcotic is not a class <strong>of</strong><br />
medication. It is a legal and law enforcement<br />
term referring to many illegal substances and<br />
has tremendous negative connotations. You<br />
don’t get prescriptions for illegal medication.<br />
The preferred term is opioids which are legal<br />
controlled substances.<br />
Now to answer your question: Does it impair<br />
her ability to do her job or does it allow her to<br />
function at the best <strong>of</strong> her ability? Opioids,<br />
diabetic medications, seizure medications, antianxiety<br />
medications, muscle relaxants, etc. and<br />
the chronic medical conditions that require their<br />
use all have the capability to impact a person’s<br />
job performance. Their misuse or abuse can<br />
have serious consequences related to licensure<br />
or certification. A CNA applicant is asked to<br />
reveal if they are taking any controlled substances<br />
either by prescription or not. Each application<br />
is reviewed individually. Simply taking a<br />
controlled substance for a chronic condition is<br />
not an automatic barrier to certification.<br />
Q I need to know if a LPN who has an<br />
“Advanced IV Certification” can change<br />
dressings, access, and administer pre mixed/<br />
labeled IV Medications for a central line.....a<br />
groshong cath.<br />
A While an IV certified LPN may administer<br />
certain medications via a peripheral line Chapter<br />
3,Section 3 (c)(iv) states:<br />
(C) Assist the registered pr<strong>of</strong>essional nurse in<br />
16 <strong>Wyoming</strong> <strong>Nurse</strong> <strong>Reporter</strong>
the administration <strong>of</strong> midline or central venous<br />
infusion <strong>of</strong> approved IV fluids by:<br />
(I) Checking the flow rate;<br />
(II) Maintaining patency by use <strong>of</strong> saline/heparin<br />
flush;<br />
(III) Changing the tubing(s) and site<br />
dressing(s);<br />
(IV) Administering TPN; and<br />
(V) Obtaining a blood sample.<br />
This would indicate that the central line IV<br />
medication is not started by an LPN but may<br />
be monitored by the LPN to assist the RN in<br />
delivering the medication. If it were otherwise<br />
it would state that an LPN may administer IV<br />
medications via a central line. It does not say<br />
that and allows an LPN to access Central lines<br />
only to flush or obtain blood. They may change<br />
central line dressings but administering premixed<br />
IV medications is reserved for peripheral<br />
lines. TPN is the only fluid identified for Central<br />
line administration. I hope that helps with your<br />
interpretation.<br />
Q I am an RN working in LTC. I am looking<br />
for information on caring for persons with<br />
MRSA. Specifically, I want to know if once a<br />
person has been treated for an active infection<br />
what are the guidelines for safe contact. I<br />
am concerned about keeping other residents<br />
protected as well as the issue <strong>of</strong> continued<br />
isolation for the resident with MRSA. The<br />
information presented to our staff was that<br />
once treated there is no longer an issue. Can<br />
you answer this question or direct me to the<br />
most current literature on the subject? Thank<br />
you in advance,<br />
A As a nurse, you need to be aware <strong>of</strong> evidence<br />
based practice and the means to obtain such<br />
evidence. You are responsible for seeking<br />
knowledge to expand your practice and the<br />
information base you provide your patients. A<br />
one minute google search <strong>of</strong> “MRSA carrier<br />
contagious” turned up a wealth <strong>of</strong> information.<br />
This brief search found a PDF brochure prepared<br />
by the Washington <strong>Board</strong> <strong>of</strong> Health called<br />
Living with MRSA which provides answers to<br />
your questions and many others you might have.<br />
Your own search may turn up more information<br />
you could share with everyone at your facility.<br />
Your risk management or infection control<br />
departments should have policies in place to<br />
address this issue as well. I don’t agree that once<br />
treated there is no longer an issue because many<br />
people remain carriers for life although personally<br />
exhibiting no symptoms. Some hospitals have<br />
initiated standard nares swabbing on admission<br />
to identify such carriers and initiate appropriate<br />
transmission precautions. Find your evidence<br />
based research and initiate a best practice<br />
program. Let me know how it works out.<br />
Q I have a question about a CNA splitting<br />
her time at a clinic between a CNA and a<br />
phlebotomist. I also would like some guidance<br />
on what requirements a phlebotomist has for<br />
<strong>Wyoming</strong>. A local phlebotomist stated that<br />
there is no requirement for <strong>Wyoming</strong> but<br />
I would rather be correct than to create a<br />
problem<br />
A Phlebotomy technicians are not licensed or<br />
certified by any board authority that I am aware<br />
<strong>of</strong>. They pass a skills training and are allowed<br />
to practice under the policies determined by the<br />
facility. A CNA may have phlebotomy training<br />
but it would be outside their scope to perform such<br />
acts when representing themselves as a CNA. It<br />
can become very complicated to work with two<br />
job titles and if the person were working as a<br />
CNA could they refuse a request to draw blood<br />
during that shift (or would they refuse). There is<br />
a distinction to be drawn between being a CNA<br />
and being a medical assistant or technician. A<br />
CNA must work under the direction <strong>of</strong> an RN<br />
and an RN would not delegate that to a CNA.<br />
I hope that clarifies the issue.<br />
Q I have had several questions from our<br />
staff who are enrolled at UW in the nurse<br />
practitioner program about whether an APRN<br />
can practice as RN? Are they held to the<br />
higher license? They’ve been getting conflict<br />
messages from their pr<strong>of</strong>essors.<br />
A I am glad to try to provide some insight into<br />
your question. As you may know, in <strong>Wyoming</strong>,<br />
APRNs have an RN license with APRN<br />
recognition. Therefore, an APRN is an RN<br />
and will always have an RN license. The only<br />
confusion that may arise from an APRN being<br />
employed as an RN is one <strong>of</strong> accountability. An<br />
APRN, despite their job title, may be held to a<br />
greater expectation than an RN because <strong>of</strong> their<br />
advanced training.<br />
Hypothetically, consider a Certified <strong>Nurse</strong><br />
Midwife working as an RN on a labor & delivery<br />
floor. A mother goes into labor. The doctor is<br />
called but can’t be reached. The mother begins<br />
progressing rapidly and the baby begins showing<br />
signs <strong>of</strong> distress but there is still no doctor. The<br />
CNM cannot claim to be only working as an<br />
RN and not utilize her advanced knowledge and<br />
training in protecting the safety <strong>of</strong> mother and<br />
child.<br />
Secondly is the issue <strong>of</strong> insurance. It may be<br />
questionable whether a carrier would allow an<br />
APRN to work below their scope or whether<br />
they would be covered in the event <strong>of</strong> a claim<br />
if they did not act to the full extent <strong>of</strong> their<br />
license.<br />
And third is the legal aspect. Many a jury<br />
would look at the CNM and fully expect that<br />
person to step in and perform because <strong>of</strong> their<br />
training no matter what the regulation, facility<br />
policy, or job title may say. Legal Eagle Eye (a<br />
newsletter) <strong>of</strong>ten has examples <strong>of</strong> juries finding<br />
that a nurse was expected to know something or<br />
do something simply because <strong>of</strong> their education.<br />
So, can an APRN work as an RN... absolutely,<br />
they are licensed as an RN. Should they accept<br />
employment as an RN is really the question and<br />
the answer to that is full <strong>of</strong> variables. Personally,<br />
after achieving my APRN I wouldn’t want to<br />
accept anything less.<br />
Q Can an RN place an external jugular vein<br />
IV catheter with the proper training? Can an<br />
RN place a chest decompression needle in the<br />
case <strong>of</strong> pneumothorax?<br />
A Every nurse has skills and abilities that range<br />
from novice to expert on a variety <strong>of</strong> tasks. A<br />
veteran nurse may be a novice in an area outside<br />
their expertise. Please direct each nurse to the<br />
Decision Tree model as found on our website<br />
under opinions. WSBN does not issue scope<br />
<strong>of</strong> practice decisions individually and prefers for<br />
each nurse to study the algorithm to determine if<br />
they are capable, competent and willing to take<br />
responsibility for their actions. The answers to<br />
your questions may also be found in your facility<br />
policy which may be more restrictive than what<br />
would be allowed by scope.<br />
Questions you could ask yourself: Generally,<br />
needle decompression would be a procedure<br />
only initiated in an emergency where failure to<br />
perform it could be fatal. In the ER there should<br />
be someone trained in this procedure. With<br />
proper training and continued competency<br />
nurses do many invasive procedures. What<br />
is the alternative to the RN not doing NDC?<br />
Why do your RNs want to access an External<br />
Jugular? Although it is considered peripheral<br />
IV access, there are specific risks involved and<br />
they are difficult to secure. Intraosseous infusion<br />
is one <strong>of</strong> the quickest ways to establish access<br />
for the rapid infusion <strong>of</strong> fluids, drugs and blood<br />
products in emergency situations. Training in<br />
these techniques may be more beneficial. If time<br />
is not critical, a central line or PICC might be<br />
an alternative providing more access ports and<br />
greater infusion capacity than an EJ.<br />
Q I am an RN in <strong>Wyoming</strong>. Because I work<br />
in a rural area and in an industrial setting with<br />
Continued on page 18<br />
<strong>Wyoming</strong> <strong>Nurse</strong> <strong>Reporter</strong> 17
an ambulance transportation time <strong>of</strong> at least 45<br />
minutes to the nearest hospital, I am looking<br />
into improving my pre-hospital knowledge<br />
and skills by taking a RN to Paramedic Bridge<br />
Program. Are there any programs that are<br />
recognized by the <strong>State</strong> <strong>of</strong> <strong>Wyoming</strong>? I am<br />
specifically looking for programs that can be<br />
mainly done on line with in class clinical, as I<br />
work full time.<br />
A It is a very intelligent decision to evaluate<br />
your setting and look for ways to enhance your<br />
training to fit the needs <strong>of</strong> your area. WSBN does<br />
not evaluate RN to Paramedic programs because<br />
they are not nursing based. Although they<br />
have additional training and skills, paramedics<br />
are considered unlicensed medical personnel<br />
and certifying as such can create nightmares for<br />
your scope <strong>of</strong> practice. Have you considered the<br />
FCCS (Fundamental Critical Care Support)<br />
classes or studying for and obtaining your CCRN<br />
certification? FCCS classes are 2 day programs<br />
designed for the stabilization and transport <strong>of</strong><br />
Critical patients in the first 24 hours and the<br />
CCRN can be self studied and then test for<br />
certification. These both give you advanced<br />
insight and skills related to critical care treatment<br />
and are designed for nurses. You probably want<br />
to complement your RN license rather than<br />
train for an unlicensed position. Talk to your<br />
employer about supporting you in expanding<br />
your skills. Perhaps they will send you to a<br />
conference where you can obtain skills and take<br />
preparation classes. Good Luck,<br />
Q I work in an <strong>of</strong>fice where we do surgeries.<br />
The Doctor would like the RN and LPN to do<br />
the Pre-ops for Surgeries. Should we be doing<br />
this? Also he would like us to numb areas<br />
with 1% Xylocaine with Epi, prior to excision<br />
<strong>of</strong> moles or lesions. Should we be doing this<br />
as well?<br />
A I am not sure what specifically you mean by<br />
pre-ops. If your doctor is asking you to fill out<br />
a form prior to surgery, you probably have the<br />
skill to do so. However, if you are referring to<br />
obtaining a History and Physical (H&P) and a<br />
pre-op physical, that is a process taught in graduate<br />
school to advanced practice nurses. Performing<br />
a full H&P assessment requires graduate training<br />
and is one <strong>of</strong> the defining features <strong>of</strong> an APRN<br />
education. A nursing assessment is not designed<br />
to take into consideration the factors required<br />
to evaluate a patient for surgery. The H&P is<br />
an evaluative process and therefore completely<br />
outside the scope <strong>of</strong> an LPN whose scope is<br />
defined by the collection <strong>of</strong> data. It could be<br />
asked <strong>of</strong> you to do it, but as an RN you would<br />
not want to take responsibility for missing<br />
a medication incompatibility, an allergy, a<br />
comorbid condition, or a physical inconsistency<br />
that would put a person at risk in surgery. In the<br />
end I do not believe the H&P is delegatable to<br />
an RN.<br />
Regarding giving sub-q injections, if you<br />
have been given the training to competently<br />
perform these tasks in the <strong>of</strong>fice setting it would<br />
be in both your scopes to do this with a doctor’s<br />
order. Providing injectable medication is taught<br />
as a basic nursing skill and prepping an area for<br />
excision would be a skill set you could acquire.<br />
Please check the Decision tree model for advice<br />
on how to evaluate your individual scope <strong>of</strong><br />
practice.<br />
Q I’m a CNA and I work for two companies<br />
in Rock <strong>Spring</strong>s. I had a Med training class for<br />
Nowcap and I read the state regulations for<br />
CNA’s when assisting with meds. I was told by<br />
a student nurse that CNA’s cannot assist with<br />
meds. Is this true?<br />
A Thank you for contacting the board <strong>of</strong><br />
nursing. What you were told is partially correct.<br />
A CNA cannot administer medications but<br />
Chapt.7, Section 7 (ii)(K) allows for “assisting<br />
with the self-administration <strong>of</strong> medication” and<br />
then defines the very limited scope <strong>of</strong> what that<br />
includes. What you may have read is the inclusion<br />
in Chapter 7 (Certified <strong>Nursing</strong> Assistants) <strong>of</strong> an<br />
advanced level <strong>of</strong> nursing assistant, CNA II, who<br />
is given additional training to provide a select set<br />
<strong>of</strong> nursing skills primarily in a long term care or<br />
nursing home environment. This was approved<br />
in July <strong>of</strong> 2010. In addition to the CNA II is the<br />
Medication Assistant certified (MA-C) which<br />
requires 100 hours <strong>of</strong> instruction beyond the<br />
CNA II. Although these levels <strong>of</strong> CNA are in<br />
the regulations there currently are no programs<br />
developed to train them at the present time and<br />
no one is registered in the state in that capacity..<br />
WSBN is working with several facilities to<br />
approve these new courses and we hope to have<br />
them more available later in the year.<br />
Regarding your Med training with NOWCAP,<br />
as a CNA you must verify that you are following<br />
the scope <strong>of</strong> practice as defined in the Rules &<br />
Regulations, Chapter 7. If you have questions,<br />
your NOWCAP director should be able to<br />
clarify the rules as they apply to this assistance<br />
program.<br />
Q I want to know if with the trouble I go<br />
through for my CNA recertification every two<br />
years if it would be worth my time and money<br />
to go to college to be a LPN or RN? PLEASE<br />
RESPOND<br />
A If you feel that submitting a log <strong>of</strong> 24 in-services<br />
every 2 years to renew a CNA certification is a<br />
lot <strong>of</strong> trouble then perhaps going on to become a<br />
nurse would not be worth it for you. Becoming a<br />
nurse means a lifelong commitment to continuing<br />
education and keeping your skills sharp. It means<br />
a commitment to evidence based practice which<br />
can only be developed by staying current with<br />
latest knowledge and trends. It means hundreds<br />
<strong>of</strong> hours <strong>of</strong> studying and classroom lectures. It<br />
means accepting responsibility not only for<br />
your actions, but for the actions <strong>of</strong> others. It<br />
means long and stressful hours. And it means<br />
developing the ability to reflect on your practice<br />
and see where you need to improve and take<br />
steps to achieve improvement.<br />
Of course becoming a nurse also means having a<br />
pr<strong>of</strong>ession, not just a job. It means having a career<br />
that is open ended with possibilities. It means<br />
being able to travel and work almost anywhere<br />
in the world. It means being a member <strong>of</strong> one <strong>of</strong><br />
the most respected groups in the nation. It means<br />
helping others and having the opportunity to see<br />
miracles happen. And it means that you have<br />
made a wise choice. Money and time spent on<br />
education is never wasted. Good luck on your<br />
decision,<br />
Q I am working with some <strong>of</strong> our physicians<br />
trying to determine what would be the best rate<br />
to run the IV solution with PCA infusions.<br />
Currently, we use a TKO (to keep open) rate.<br />
However, there has been much discussion<br />
regarding if this rate allows the medication to be<br />
effectively administered to the patient. We are<br />
trying to decide if there should be a set rate for<br />
all patients, or if the prescriber should choose<br />
a rate based on the patient’s comorbidities.<br />
How do you decide what the TKO rate is?<br />
What rate do you run the IV solution in the<br />
line infusing the PCA?<br />
A Keep in mind that the Y-PCA tubing is<br />
designed with an anti-backflow valve to have<br />
a carrier solution. These safety devices prevent<br />
opioid solutions from backing up into the<br />
tubing if the patient access is blocked and then<br />
inadvertently delivering a large bolus dose if the<br />
obstruction clears. The carrier solution prevents<br />
single doses from sitting in the line undelivered to<br />
the patient. A direct line to the patient without<br />
a carrier solution, if clotted, would prevent any<br />
medication from reaching the patient. Also, the<br />
carrier solution should be on pump, rather than<br />
gravity feed, to alarm when the flow is obstructed<br />
and prevent the accumulation <strong>of</strong> a bolus dose.<br />
The rate should be consistent with the<br />
volume <strong>of</strong> the extension set or tubing volume<br />
between the PCA and the patient. If there is a<br />
18 <strong>Wyoming</strong> <strong>Nurse</strong> <strong>Reporter</strong>
10ml tubing volume between the PCA and the<br />
patient and the TKO (to keep open) is 20ml/<br />
hr it would take 30 minutes for a PCA dose to<br />
reach the patient. (These numbers are just for<br />
example but do point out why it is discouraged<br />
to use extension sets with PCA tubing).<br />
TKO rates can also be based on the fluid<br />
needs <strong>of</strong> the patient or the provider’s orders.<br />
Q2 I agree with your analysis for the valve<br />
and the TKO; could you provide me with the<br />
evidence? Is the evidence from the company?<br />
A2 Evidence generally flows from research<br />
involving experimentation and testing.<br />
What was stated is critical thinking. It is an<br />
examination <strong>of</strong> the physical principles involved<br />
and how they will impact the patient. You could<br />
say the evidence is physics. There generally is no<br />
argument in how to set up a PCA line.....connect<br />
as close to the patient as possible, carrier solution<br />
piggybacked above the backflow valve into the<br />
y port <strong>of</strong> the PCA tubing. The only pushback I<br />
have seen is when the patient is fluid overloaded<br />
and the physician does not want any extra fluid<br />
administered. At that point it becomes a safety<br />
issue to maintain KVO (keep vein open) carrier<br />
solution (maybe as little as 10cc ... but still on a<br />
pump) vs. the danger <strong>of</strong> a opioid bolus impacting<br />
respirations. It doesn’t need to be a clot to<br />
obstruct the line. A positional IV or simply<br />
laying or twisting the tubing can store up extra<br />
doses in the line. That is why I always advocate<br />
for an infusion pump with the carrier solution.<br />
Sometimes it takes a sentinel event for some to<br />
see the danger <strong>of</strong> not running a carrier line. A<br />
bag <strong>of</strong> normal saline is much cheaper.<br />
Q Just wondering if LPNs can triage in the<br />
emergency department.<br />
A Before answering I need to know what you<br />
mean by triage. If you mean assessing and<br />
evaluating a patient’s condition and need for<br />
treatment then the answer is no.<br />
Rules and Regulations Chapter 3, Section 3.<br />
Standards <strong>of</strong> <strong>Nursing</strong> Practice for the Licensed<br />
Practical <strong>Nurse</strong> says “The licensed practical<br />
nurse shall:<br />
(A) Contribute to the nursing assessment by:<br />
(I) Collecting, reporting, and recording<br />
objective and subjective data in an accurate<br />
and timely manner. Data collection includes<br />
observations about the condition or change in<br />
condition <strong>of</strong> the client.<br />
The LPN scope does not allow for assessment<br />
and evaluation but does allow the LPN to gather<br />
information to assist the RN in making the<br />
evaluation and assessment.<br />
If you can find a role for the LPN in ED triage<br />
that meets that scope, then all right. Otherwise<br />
the LPN should recognize the limitations <strong>of</strong> their<br />
practice and inform you if the job requirements<br />
exceed their scope.<br />
For further information on determining<br />
scope <strong>of</strong> practice please refer to the Decision<br />
Tree located on our website under opinions.<br />
The Decision Tree algorithm is designed to help<br />
nurses determine scope <strong>of</strong> practice issues.<br />
Q I am a psychiatric CNS, certified in adult<br />
psychiatry. My question is at what age does the<br />
WSBN consider it within my scope <strong>of</strong> practice<br />
to begin treating. I get different answers from<br />
the UW School <strong>of</strong> <strong>Nursing</strong> and what I had<br />
been told verbally by a person at WSBN. Also<br />
if a child or adolescent has been evaluated by a<br />
physician or a Pediatric Psychiatric APN can<br />
I then follow them. I would like something<br />
in writing from the state board so that I am<br />
clear. In the center <strong>of</strong> WY there is a paucity<br />
<strong>of</strong> accessible psychiatric care for children and<br />
adolescents. There is one psychiatrist in the<br />
area who sees children and it takes at least 2<br />
months for people to get in to see her. The<br />
other two will not see children one until 13<br />
and the other until 16. When UW graduates<br />
this class in 2012 it will help, but until then<br />
it is a problem. Thanks for considering this<br />
issue.<br />
A I have been presented with this question<br />
before and I am glad to provide you an in-depth<br />
answer.<br />
First <strong>of</strong>f -ANCC adult psychiatric mental<br />
health nurse practitioner (PMHNP) certification<br />
starts at 13 years <strong>of</strong> age on up through geriatrics.<br />
I consulted with someone who has done both<br />
programs and they do not believe that an adult<br />
trained PMHNP is educated on how to manage<br />
child psychiatric disorders. After the adult<br />
program, this person completed an additional<br />
500 hours to certify Family/Child Psych NP.<br />
A child psych practitioner must consider the<br />
presenting symptoms and then put the symptoms<br />
into the context <strong>of</strong> child development normals<br />
versus abnormals. This is not part <strong>of</strong> an adult<br />
PMHNP program. Consider a 4 year old with<br />
multiple foster care, fetal alcohol syndrome,<br />
mental retardation, sexual acting out issues --<br />
see how this does not fit into the scope <strong>of</strong> an<br />
adult PMHNP? Childhood onset disorders in<br />
the DSM would rarely be studied by and adult<br />
PMHNP.<br />
The way a child versus teen versus adult<br />
presents with bipolar disorder differs. Many<br />
many <strong>of</strong> the meds used for pediatric populations<br />
are technically <strong>of</strong>f label and that is not the case<br />
for adult patients for the most part. There is a<br />
learning curve to prescribing this way especially<br />
since the lawsuit risk is greater with children<br />
because <strong>of</strong> the lifelong responsibility for the<br />
damages caused at an early age.<br />
Family therapy and family systems therapy<br />
are not part <strong>of</strong> an adult program. School<br />
special education systems to include school<br />
IEP (individual educational plans) are not in<br />
adult programs. Adult programs do not cover<br />
the national EBP and national guidelines on<br />
pediatric psychiatry that a family PMHNP<br />
program teaches.<br />
The idea that an adult PMHNP could<br />
take on a child that has been seen by a child<br />
psych person does not take into account the<br />
fact that children need much more titration<br />
<strong>of</strong> medications than adult patients do so one<br />
visit with a child psychiatrist would hardly be<br />
adequate for effective care. Plus once you get it<br />
just right, the child grows and you have to then<br />
readjust once again.<br />
There are Child/Pediatric PMHNPs available<br />
and parents will drive considerable distances to<br />
get the right care. A shortage <strong>of</strong> surgeons does<br />
not indicate that internists need to take on liver<br />
transplants. Just because there’s a shortage <strong>of</strong><br />
child psych practitioners doesn’t mean people<br />
who aren’t qualified can start seeing populations<br />
they haven’t been educationally prepared for.<br />
In the end, the WSBN takes the stance<br />
that <strong>Nurse</strong>s determine their own scope by the<br />
licensure, accreditation, certification, education,<br />
and experience they possess. That is why we<br />
adopted the decision tree model for determining<br />
scope <strong>of</strong> practice. Located on our website under<br />
information/opinions, it is an algorithm that will<br />
help determine if you feel you have the training,<br />
skill, ability, and are ready to accept responsibility<br />
for your actions.<br />
I hope that helps you in your deliberations.<br />
Q I am a hospice RN and I am wondering if it<br />
is standard practice to teach competent family<br />
members to administer class II medications to<br />
their terminally ill family member in the home<br />
setting. This would include both PO and SC<br />
morphine.<br />
A Thank you so much for bringing this question<br />
to the WSBN. Family members are exempt<br />
from the requirements <strong>of</strong> nursing licensure. The<br />
<strong>Nurse</strong> Practice Act specifies:<br />
33-21-154. Exemptions.<br />
(a) No provisions in this act ...prohibit:<br />
(iii) The incidental health care by members <strong>of</strong><br />
the family and friends;<br />
Consider, what would be the alternative?<br />
Continued on page 20<br />
<strong>Wyoming</strong> <strong>Nurse</strong> <strong>Reporter</strong> 19
That the family member endure the pain <strong>of</strong> a<br />
terminal illness? Patients have a right to have<br />
their pain managed in an appropriate manner. If<br />
you determine that family assistance is necessary<br />
for proper management then they should be<br />
educated and utilized. I also believe you use<br />
the correct terminology by saying “competent<br />
family member” as this is an important aspect <strong>of</strong><br />
proper delegation. I wouldn’t turn the task over<br />
to someone I felt might be a diversion or abuse<br />
risk because, not only would you enable their<br />
problem, but your patient might not receive the<br />
necessary medication and suffer needlessly.<br />
The real elephant in the room for this question<br />
is what happens if the family gives a large dose<br />
<strong>of</strong> medication and the patient expires? For<br />
additional thoughts on the subject <strong>of</strong> providing<br />
high dose opioids to terminally ill patients search<br />
for articles on the Rule <strong>of</strong> Double Effect. It poses<br />
interesting ethical questions that all Hospice and<br />
Palliative Care nurses should be aware <strong>of</strong>.<br />
Faith Community <strong>Nursing</strong><br />
Laura Mallett<br />
What is Faith Community <strong>Nursing</strong> (FCN) (Parish <strong>Nursing</strong>)? Until<br />
recently I was not sure either. At present I am learning about FCN through<br />
the <strong>Wyoming</strong> Health Council and Cheyenne Regional Medical Center,<br />
and the FCN’s in <strong>Wyoming</strong>. I started the basic training in January and<br />
will attend classes or be online until April. I’m excited about starting this<br />
aspect <strong>of</strong> nursing in my congregation after I have completed the course.<br />
Laura Mallett, MSN, RN<br />
A little background on FCN; it was<br />
founded by Dr. Westberg, a Lutheran<br />
minister, who had the idea <strong>of</strong> locating<br />
clinics in church with physicians, nurses<br />
and clergy, all working together to provide<br />
holistic care to the members <strong>of</strong> the church.<br />
This project connected nurses with hospitals<br />
and churches in providing preventative care<br />
to the congregation and the community<br />
over the years. Research that has been done<br />
revealed that preventative care reduced<br />
hospital admissions, leaving hospital beds for<br />
the very ill people that needed them.<br />
As nurses we were taught in school to<br />
address the mind, body and spirit <strong>of</strong> the<br />
client and their families. With time restraints<br />
over the years and the illnesses being more<br />
complicated than in years past, we do not<br />
always met the spiritual needs <strong>of</strong> the client<br />
or their families in the institutional setting.<br />
There is a need to make sure that we are<br />
addressing the spiritual needs <strong>of</strong> clients and<br />
their families to begin the healing process.<br />
The FCN is that link for nursing practice;<br />
the link to providing both spiritual and<br />
preventative care at the community level.<br />
In preparation <strong>of</strong> developing a practice in<br />
FCN, I have started putting a bulletin insert<br />
in the church bulletin on Sundays that deals<br />
with preventative health care. I’m a member<br />
<strong>of</strong> the Community <strong>of</strong> Christ Health Ministries<br />
Association through the church that I<br />
attend. After I finish the basic training, I will<br />
develop a program with my Pastor to move<br />
forward in the congregation and surrounding<br />
community over time. I don’t know exactly<br />
what my practice will look like within the<br />
congregation yet, or what their needs are, but<br />
working with them and the Pastor, I hope<br />
to develop a relationship so that I can be a<br />
resource person and educator for the church.<br />
I can also use what I learn in my job at the<br />
University <strong>of</strong> <strong>Wyoming</strong> to better prepare<br />
nurses in assessing their clients spiritual<br />
needs while they are students, emphasizing<br />
the importance <strong>of</strong> mind, body, and spirit in<br />
healing.<br />
FCN is another way nursing can make a<br />
positive impact on the health <strong>of</strong> <strong>Wyoming</strong><br />
citizens. It consists <strong>of</strong> working with resources<br />
we have and developing a team approach<br />
to make the citizens <strong>of</strong> <strong>Wyoming</strong> healthy<br />
and make an impact in lowering the overall<br />
health care cost without compromising<br />
quality <strong>of</strong> care.<br />
I would like to close this and address<br />
the many nurses who feel their career in<br />
nursing is a calling from God. I was called<br />
to the pr<strong>of</strong>ession <strong>of</strong> nursing several years<br />
back. I really didn’t figure I would be called<br />
to other aspects <strong>of</strong> nursing. I was also called<br />
to teaching future nurses and treat every<br />
aspect <strong>of</strong> my career as a blessing from God.<br />
I have always felt that it is privilege to have<br />
the ability and knowledge to care for God’s<br />
children. I think this writing from James N.<br />
Spurgeon says so much about the FCN:<br />
Job or Ministry?<br />
A job is at your choice.<br />
A ministry is at Christ’s call.<br />
In a job you are expected to receive<br />
In a ministry you are expected to give.<br />
In a job you give something for a return.<br />
In a ministry you return something that<br />
has already been received.<br />
A job depends on your abilities;<br />
A ministry depends on your availability<br />
to God.<br />
A job done well brings you praise,<br />
A ministry done well brings honor to<br />
Christ.<br />
Laura Mallett, MSN, RN is Assistant<br />
Lecturer at the Fay W. Whitney School <strong>of</strong><br />
<strong>Nursing</strong> at the University <strong>of</strong> <strong>Wyoming</strong>.<br />
For more information about Faith Community<br />
<strong>Nursing</strong>, please contact<br />
Amanda Hubbard<br />
Project Assistant<br />
Faith Community & Parish <strong>Nursing</strong> Program<br />
<strong>Wyoming</strong> Health Council<br />
307.632.3640 Tel<br />
www.wyhc.org<br />
20 <strong>Wyoming</strong> <strong>Nurse</strong> <strong>Reporter</strong>
Customer Service Corner<br />
With our first on-line renewal season over, we are getting back into<br />
the swing <strong>of</strong> everyday work at the WSBN. Our licensing department<br />
took over 3500 phone calls and assisted over 300 walk in customers<br />
from the period <strong>of</strong> October 1, 2010 through December 31, 2010.<br />
We are very pleased to say that over 90% <strong>of</strong> all license renewals<br />
were processed on-line allowing for instantaneous licensure for many.<br />
We look forward to using your input to improve the process for<br />
2012.<br />
Thank you to you and your employers for assisting us in our success<br />
with paperless licensing! We continue to improve our processes in<br />
order to ensure that all receive the information they need to be<br />
successful.<br />
Please feel free to contact Amanda Roberts at arober@wyo.gov for<br />
your suggestions and feedback on customer service from WSBN.<br />
“Completely unexpected” was the response to the flowers and<br />
card received a few days before this issue went to print. Amanda<br />
had taken a request from a VA Hospital to specify our website license<br />
verification as primary source. After <strong>Board</strong> approval Amanda worked<br />
with our programmer to get it online. “We always try to keep the web<br />
Amanda Roberts, WSBN Executive Assistant<br />
current, so it was quite a surprise when the flowers and heartfelt note<br />
arrived. It really is nice to know people appreciate what you do. “<br />
Patti Gardner<br />
Getting to Know <strong>Wyoming</strong> <strong>Nursing</strong> Students<br />
Meet Lilian Ogana<br />
My name is Lilian Ogana and I am originally<br />
from Kenya. I am currently enrolled as a full<br />
time senior student in the nursing program<br />
at the Fay W. Whitney School <strong>of</strong> <strong>Nursing</strong><br />
at the University <strong>of</strong> <strong>Wyoming</strong>. My husband<br />
and I came to the United <strong>State</strong>s in the fall<br />
<strong>of</strong> 2003 after living in the United Kingdom<br />
for a year. While my husband was pursuing<br />
his education, I stayed home and <strong>of</strong>fered<br />
voluntary services from 2004 at the <strong>Nursing</strong><br />
and <strong>Spring</strong> Wind Assisted Living Homes<br />
in Laramie. I perfected my communication<br />
skills at these residences using my singing<br />
talent to comfort and inspire the residents.<br />
In addition, these services made me connect<br />
not only with the residents but also with the<br />
greater Laramie community.<br />
In 2007, I started taking classes at Laramie<br />
County Community College (LCCC), Albany<br />
Campus, to pursue a nursing degree. It was<br />
my hope that I could positively contribute<br />
to humanity and society by helping and<br />
supporting people who have health concerns<br />
or different disabilities. Having been born<br />
and raised in Kenya, I have seen fatalities<br />
that would have otherwise been prevented<br />
with proper health provision and care. This<br />
has motivated and inspired me to pursue a<br />
nursing career instead <strong>of</strong> other careers so that<br />
I can get the expertise and experience that is<br />
needed to promote better health services in<br />
my country and the rest <strong>of</strong> the world.<br />
While at LCCC, I was involved with<br />
the international students’ body and did<br />
advertisements for the college on television,<br />
radio, newspaper, and school catalogs. After<br />
finishing my prerequisites from LCCC, I<br />
transferred to the University <strong>of</strong> <strong>Wyoming</strong><br />
and got accepted into the BSN nursing<br />
program. My school journey has been rough<br />
but through thick and thin I have persisted<br />
despite the financial and health problems I<br />
have incurred. I am grateful to my husband,<br />
family, and friends for the support they have<br />
given me. In addition, I thank the faculty,<br />
staff, and all the donors for continued<br />
support.<br />
I am currently doing my senior residency<br />
at McKee Hospital in Loveland, Colorado<br />
and will finish the second half <strong>of</strong> residency<br />
in Florida. I plan to graduate in the spring<br />
<strong>of</strong> <strong>2011</strong>. After completion <strong>of</strong> my education,<br />
I will seek for employment in Florida where<br />
my husband and I are planning to relocate to<br />
gain experience and strengthen my career.<br />
My ultimate goal is to use my degree to<br />
help prevent and eradicate the spread <strong>of</strong><br />
diseases such as AIDS, tuberculosis, malaria,<br />
and cholera that are currently annihilating<br />
countries in the sub-Saharan region including<br />
Kenya.<br />
<strong>Wyoming</strong> <strong>Nurse</strong> <strong>Reporter</strong> 21
Patti Gardner<br />
Getting to Know <strong>Wyoming</strong> <strong>Nursing</strong> Students<br />
Meet Mallory Davis<br />
Mallory Davis (left) and Friend<br />
During the last four years, while I have<br />
been in nursing school, I have found that I<br />
had a great deal <strong>of</strong> time to think; not only<br />
about which textbook would I over-highlight<br />
next or what organizational meeting I might<br />
attempt to make, but also about what career<br />
plan I would choose to pursue once I earned<br />
my degree. Of course many options have<br />
come to my mind; public health in <strong>Wyoming</strong><br />
working with HIV/AIDS patients, an ICU<br />
position on a Burn Unit in Colorado or Utah,<br />
or specializing in the geriatrics field.<br />
In order narrow down these possible<br />
pr<strong>of</strong>essional choices, I had to examine my past<br />
and present interests within the academic<br />
Legislative Review<br />
WSBN is involved in all aspects <strong>of</strong><br />
nursing and nursing regulation. That<br />
includes taking an active role in formulating<br />
state policy and the legislative process that<br />
relates to nursing practice or activities that<br />
impact our licensees. This year, WSBN has<br />
been working with two <strong>of</strong> our legislators,<br />
Senator Leslie Nutting from Laramie County<br />
and Representative Noreen Kasperik from<br />
Campbell County, to advance bills favorable<br />
to nursing regulation. Both Registered <strong>Nurse</strong>s<br />
in their own regard, Representative Kasperik<br />
was the Interim Director <strong>of</strong> Gillette College<br />
<strong>Nursing</strong> Program while Senator Nutting is<br />
an Advanced Practice <strong>Nurse</strong> retired from<br />
the Veterans Administration. WSBN is<br />
fortunate to have such knowledgeable and<br />
supportive legislators to advance our issues.<br />
This year saw numerous bills submitted to<br />
the legislature dealing with terminology used<br />
to describe a Doctor <strong>of</strong> <strong>Nursing</strong> Practice,<br />
field and to take under consideration my<br />
extracurricular interests as well. During my<br />
freshman and Sophomore years, I developed<br />
a passion for public health nursing while<br />
participating in an organization called<br />
Face AIDS. As student members, we<br />
raised awareness AND money for smaller<br />
communities in Africa that were victims <strong>of</strong><br />
the growing HIV/AIDS epidemic. During<br />
my experience with this group <strong>of</strong> people, I<br />
became acquainted with pr<strong>of</strong>essionals who<br />
worked specifically with people in <strong>Wyoming</strong><br />
who suffered from AIDS.<br />
Shortly thereafter, I began working<br />
as a CNA during summer and winter breaks<br />
on the Burn ICU at the University <strong>of</strong><br />
Colorado Hospital and my drive to work in<br />
a critical care area grew. The intensity <strong>of</strong> the<br />
unit as well as the overwhelming knowledge<br />
the ICU nurses possessed was impressive and I<br />
felt myself drawn to it. I wanted to be familiar<br />
and comfortable in this critical care area so<br />
that I could have input with residents and<br />
surgeons about what I felt was the patient’s<br />
best plan <strong>of</strong> care. In particular, I found that<br />
I loved taking care <strong>of</strong> burn patients, and as<br />
only two accredited burn centers were in my<br />
granting APRNs admitting authority to<br />
hospitals, recovery <strong>of</strong> fees by WSBN for<br />
disciplinary costs, making it an <strong>of</strong>fense<br />
to violate a board order, and a change to<br />
the student exemption allowing clinical<br />
privileges for someone pursuing post licensure<br />
education. Of special interest to WSBN are<br />
surrounding vicinity, I would either have to<br />
move to Colorado or Utah to chase such an<br />
ambition. My interest in becoming a critical<br />
care nurse has not completely evaporated,<br />
but has been momentarily replaced by a<br />
third, and final career interest: geriatrics.<br />
During my first year <strong>of</strong> nursing school, we<br />
were required to complete a geriatrics course<br />
as well as help at local assisted living facilities.<br />
The class census overall was not in favor <strong>of</strong><br />
this particular course as most students were<br />
more drawn toward pediatrics or obstetrics. I<br />
found that I enjoyed this course after growing<br />
up with a mother who was a nurse that<br />
cherished the older community and became a<br />
hospice nurse. I found that as that particular<br />
semester passed, I had found my niche within<br />
the senior citizen community, always looking<br />
forward to working with older clients.<br />
In the end, despite my changing interests<br />
and involvement in a wide array <strong>of</strong> nursing<br />
specialties, I feel most drawn to care for the<br />
Baby Boomers <strong>of</strong> the generations before<br />
myself. The beautiful thing about the finality<br />
<strong>of</strong> my decision for me, is that I can care for<br />
these men and women anywhere in the<br />
country, and especially in <strong>Wyoming</strong>!<br />
SF90 and HB253 which at the time <strong>of</strong> this<br />
publication deadline had both passed out<br />
<strong>of</strong> their chamber <strong>of</strong> origin and were being<br />
considered by the other chamber. Go to the<br />
legislative website for details on the outcome<br />
<strong>of</strong> these bills. http://legisweb.state.wy.us/<br />
<strong>Board</strong> Consumer Member Marguerite<br />
Herman has been busy meeting with legislators<br />
as an advocate for the board’s mission <strong>of</strong><br />
public protection and following the progress<br />
<strong>of</strong> many <strong>of</strong> these bills that could directly or<br />
indirectly affect nurses in this state. <strong>Board</strong><br />
staff have testified in committee for several <strong>of</strong><br />
the bills up for consideration. The <strong>Wyoming</strong><br />
<strong>Nurse</strong>s Association sponsored a legislative<br />
day in January, bringing student nurse leaders<br />
to Cheyenne to learn about the legislative<br />
process and even mingle with legislators at a<br />
reception. Political involvement is just one<br />
more aspect <strong>of</strong> how WSBN serves the public<br />
and all licensees.<br />
22 <strong>Wyoming</strong> <strong>Nurse</strong> <strong>Reporter</strong>
WYOMING STATE BOARD OF NURSING<br />
Delegation <strong>State</strong>ment<br />
In the <strong>Spring</strong> 2010 issue <strong>of</strong> the <strong>Wyoming</strong> <strong>Nurse</strong> <strong>Reporter</strong> there<br />
was an answer to a practice question regarding a registered nurse’s<br />
authority to delegate to a medical assistant (MA). It stated that<br />
it is not within the scope <strong>of</strong> practice <strong>of</strong> a nurse to delegate tasks<br />
to medical assistants. It cited Rules & Regulations, Chapter 9<br />
and stated, “nurses delegate to other nurses or CNAs.”<br />
That is a common understanding and<br />
statements like this reinforce that belief. <strong>Nurse</strong>s<br />
are taught to value evidence based practice,<br />
proven methods and ideas backed by research.<br />
There is a famous anonymous quote: “Evidence<br />
is not the plural <strong>of</strong> Anecdote”. However, as<br />
much as that delegation statement may seem<br />
to be common practice, the evidence does not<br />
back up the claim.<br />
Careful reading <strong>of</strong> Chapter 9; Delegation and<br />
Assignment finds the following specific wording.<br />
First, Section 1 defines delegation as: “...the<br />
transferring to a competent individual (italics for<br />
emphasis) the authority to perform a specific<br />
nursing task in a selected situation. The nurse<br />
retains responsibility for the delegated tasks.”<br />
It does not say ‘to another nurse or CNA’, but<br />
merely identifies a “competent individual”.<br />
Chapter 9, Section 3 utilizes a number <strong>of</strong><br />
terms to describe who a nurse may delegate<br />
to and is not consistent in specifically naming<br />
other nurses. Instead, it identifies “any nursing<br />
assistant”, “members <strong>of</strong> the nursing team”, “other<br />
health care worker”, “delegatee”, “staff to whom<br />
the task is delegated”. Even when it names a<br />
nursing assistant it is not clear that it is referring<br />
to a Certified <strong>Nursing</strong> Assistant (CNA) or<br />
simply to the person assisting the nurse.<br />
Finally, Chapter 9, Section 8 outlines the<br />
decision tree for delegation based on the joint<br />
statement <strong>of</strong> the American <strong>Nurse</strong>s Association<br />
(ANA) and the National Council <strong>of</strong> <strong>State</strong><br />
<strong>Board</strong>s <strong>of</strong> <strong>Nursing</strong> (NCSBN). In wording<br />
selected by these national agencies, the<br />
delegation tree mentions CNAs specifically and<br />
then reverts to using the term ‘nursing assistive<br />
personnel’.<br />
It should be clear that if the intent was to<br />
limit RN delegation only to other nurses or<br />
CNAs it could have used more consistent<br />
language. The goal is always to provide for<br />
the safety and care <strong>of</strong> the patient. A nurse can<br />
imagine many instances where an RN might<br />
be in a position to delegate specific tasks to a<br />
‘competent individual’. A CNA, MA, PA,<br />
RN, LPN, EMT, Surgical Tech, RT, Speech<br />
therapist, PT, (to name a few) are all medical<br />
staff and healthcare workers who are competent<br />
to perform any number <strong>of</strong> tasks. Just as a family<br />
member <strong>of</strong> a patient with specific training could<br />
be given any number <strong>of</strong> nursing tasks, many <strong>of</strong><br />
these assistive personnel can possess skills that<br />
Today’s nurses must combine expertise in<br />
their field with an ability to lead. A degree<br />
from the University <strong>of</strong> Mary will prepare<br />
you to assume leadership positions in direct<br />
patient care, management and education.<br />
Programs focus on the application <strong>of</strong> knowledge<br />
– you will understand not only what is needed,<br />
but how that service is best provided.<br />
make them competent to perform nursing tasks.<br />
(Think <strong>of</strong> parents <strong>of</strong> Cystic Fibrosis<br />
children who percuss, suction, and administer<br />
tube feedings....all nursing functions.)<br />
It is better for a nurse in a Physician’s <strong>of</strong>fice<br />
to oversee and perhaps sharpen the skills <strong>of</strong> an<br />
Medical Assistant (MA) than to refuse to interact<br />
simply because “they are under a Physician’s<br />
supervision and are not a nurse”. True, the MA<br />
is by definition under the supervision <strong>of</strong> the MD<br />
but that does not mean they will not interact<br />
with nursing staff and could require direction<br />
performing their duties. Does it not make more<br />
sense for an APRN in an emergency room to<br />
coordinate the care <strong>of</strong> a number <strong>of</strong> assistive<br />
personnel during a crisis than wait to find an<br />
available nurse for delegation? <strong>Nurse</strong>s are not<br />
part <strong>of</strong> a medical caste system. They function<br />
in the best interests <strong>of</strong> the patient and as long<br />
as nurses do not delegate the nursing process,<br />
there are many interactions that can flow to<br />
competent individuals.<br />
Earn Your Bachelor’s or Master’s Degree Online from the<br />
University <strong>of</strong> Mary<br />
Classes start in May, September and January.<br />
Financial aid is available. Learn more today!<br />
Programs available:<br />
n LPN/RN to Bachelor <strong>of</strong> Science,<br />
Major: <strong>Nursing</strong><br />
n MSN: <strong>Nurse</strong> Administrator<br />
n MSN: <strong>Nurse</strong> Educator<br />
n MSN: Family <strong>Nurse</strong> Practitioner<br />
blended online/on-site format<br />
n Diploma or ADN to MSN: <strong>Nurse</strong> Administrator<br />
n MBA in Health Care<br />
Classes held<br />
in Casper,<br />
Gillette &<br />
Sheridan,<br />
or online!<br />
Casper 232-8402; Gillette 682-2650; toll free 800-408-6279,<br />
ext. 8353 • cade@umary.edu • www.umary.edu/cade<br />
The University <strong>of</strong> Mary has held continuous accreditation by The Higher Learning<br />
Commission, a Commission <strong>of</strong> the North Central Association <strong>of</strong> Colleges and Schools,<br />
since 1969 and is accredited by the Commission on Collegiate <strong>Nursing</strong> Education.<br />
<strong>Wyoming</strong> <strong>Nurse</strong> <strong>Reporter</strong> 23
Disciplinary Actions<br />
(C) Misappropriation or misuse <strong>of</strong> property; (D)<br />
Abandonment; (E) Abuse, including emotional,<br />
physical or sexual abuse; (F) Neglect, including<br />
substandard care; (G) Violation <strong>of</strong> privacy or<br />
confidentiality in any form, written, verbal or<br />
technological; (H) Drug diversion-self/others;<br />
(I) Sale, unauthorized use, or manufacturing <strong>of</strong><br />
controlled/illicit drugs; (J) Criminal conviction;<br />
(K) Unpr<strong>of</strong>essional conduct; (L) Boundary<br />
violations, including sexual boundaries; (M)<br />
Failure to comply with reasonable requests from<br />
the board including, but not limited to: (I)<br />
Responses to complaints; (II) Responses to formal<br />
Grounds for discipline for Licensed Practical<br />
<strong>Nurse</strong>s and Registered Pr<strong>of</strong>essional <strong>Nurse</strong>s<br />
are located in the Administrative Rules and<br />
Regulations Chapter 3, pages 3-13 through 3-15<br />
and Certified <strong>Nursing</strong> Assistants Chapter 7, pages<br />
7-16 and 7-17 (July 2010).<br />
Grounds for Discipline are: (i) engaging in<br />
any act inconsistent with uniform and reasonable<br />
standards <strong>of</strong> practice, including but not limited<br />
to: (A) Fraud and deceit including, but not<br />
limited to, omission <strong>of</strong> required information<br />
or submission <strong>of</strong> false information written or<br />
verbal; (B) Performance <strong>of</strong> unsafe client care;<br />
pleadings such as notice <strong>of</strong> hearing and/or petition<br />
and complaint; (III) Responses to requests<br />
regarding application and/or renewal information;<br />
(IV) Written response to request for explanation<br />
for failure to disclose required information; (V)<br />
Failure to appear at properly noticed hearings;<br />
(N) Impairment. (I) Lack <strong>of</strong> nursing competence;<br />
(II) Mental illness; (III) Physical illness including,<br />
but not limited to, deterioration through the aging<br />
process or loss <strong>of</strong> motor skills; or (IV) Chemical or<br />
alcohol impairment/abuse. (ii) Failure to conform<br />
to the standards <strong>of</strong> prevailing nursing practice, in<br />
which case actual injury need not be established.<br />
WENDY KING<br />
RN 18437<br />
LICENSE REINSTATED<br />
JANUARY 11, <strong>2011</strong><br />
<strong>Wyoming</strong> <strong>State</strong> <strong>Board</strong> <strong>of</strong> <strong>Nursing</strong> ordered full reinstatement<br />
<strong>of</strong> license because <strong>of</strong> satisfactory compliance with the <strong>Board</strong>’s<br />
previous order <strong>of</strong> conditional licensure dated 7/30/2010.<br />
GWEN ANDREWS<br />
LPN 3242<br />
VOLUNTARY SURRENDER<br />
Gwen Andrews, LPN, agreed to voluntarily surrender her<br />
license on November 17, 2010. Ms. Andrews had been<br />
issued a Conditional License on September 23, 2010, arising<br />
from investigation <strong>of</strong> disciplinary complaint <strong>of</strong> alcohol and/<br />
or chemical dependency. WSBN was informed in October<br />
2010 that Ms. Andrews had been recently arrested for DUI,<br />
which Ms. Andrews subsequently confirmed and explained<br />
was due to her consumption <strong>of</strong> alcohol in combination<br />
with a prescription sleep medication. Such conduct was<br />
alleged to have failed to conform to nursing standards and<br />
to constitute unpr<strong>of</strong>essional conduct in nursing practice.<br />
As a result, Ms. Andrews voluntarily surrendered her LPN<br />
license.<br />
ALFRED BALDES<br />
CNA 20940<br />
VOLUNTARY SURRENDER<br />
Alfred Baldes, CNA, entered into a Settlement Agreement,<br />
Stipulation and Order for Voluntary Surrender on January<br />
11, <strong>2011</strong>. A complaint was filed in February 2010 by<br />
Mr. Baldes’ employer, Amedisys Home Care (“AHC”),<br />
alleging sexual abuse violations and client abuse. Such<br />
complaint alleged that while employed as a CNA at AHC,<br />
complaints were filed on behalf <strong>of</strong> two male patients alleging<br />
sexual abuse by Mr. Baldes. Mr. Baldes’ employment was<br />
consequently terminated. On November 18, 2010, .<br />
Baldes was found “Guilty” by jury verdict in the case<br />
entitled The <strong>State</strong> <strong>of</strong> <strong>Wyoming</strong> vs. Alfred Lee Baldes, <strong>of</strong><br />
two counts <strong>of</strong> Sexual Assault in the Third Degree. Mr.<br />
Baldes subsequently agreed to voluntarily surrender his<br />
CNA certificate.<br />
WENDY BEIGHLEy<br />
LPN 7223<br />
REVOCATION<br />
On or about November 16, 2010, WSBN entered an Order<br />
<strong>of</strong> Default Judgment and an Order <strong>of</strong> Revocation against<br />
Wendy Beighley, LPN. Pursuant to WSBN Rules and<br />
Regulations, Chapter 8, Section 7(a), WSBN may enter an<br />
order <strong>of</strong> default based on the allegations in a petition and<br />
complaint against a respondent/licensee who fails to appear<br />
for a properly noticed hearing. Ms. Beighley was in prison at<br />
the time <strong>of</strong> the scheduled hearing for criminal convictions<br />
related to sexually abuse <strong>of</strong> a minor child. Accordingly,<br />
WSBN revoked Ms. Beighley’s LPN license.<br />
MARY ANNE BERGAN<br />
RN 9649<br />
CONDITIONAL LICENSE<br />
Mary Anne Bergan, RN, entered into a Settlement<br />
Agreement, Stipulation and Order for Conditional License<br />
on December 6, 2010. In June 2009, a complaint was initiated<br />
on grounds <strong>of</strong> substance abuse/chemical dependency. Such<br />
complaint was based upon correspondence from <strong>Wyoming</strong><br />
Pr<strong>of</strong>essional Assistance Program (“WPAP”) Executive<br />
Director, George A. Vandel, NCAC II, CAP, dated June<br />
1, 2009, that Ms. Bergan had self-reported a relapse on May<br />
29, 2009. Ms. Bergan had previously executed a monitoring<br />
agreement with WPAP on July 1, 2008. Mr. Vandel further<br />
indicated that Ms. Bergan would be required to enter<br />
residential treatment before returning to nurse practice.<br />
On June 12, 2009, Ms. Bergan acknowledged her relapse to<br />
alcohol on May 29, 2009, and stated that she had entered<br />
a residential treatment program at <strong>Wyoming</strong> Recovery in<br />
Casper, WY. Correspondence from the <strong>Wyoming</strong> Recovery<br />
Program Director dated June 29, 2009, stated Ms. Bergan<br />
had satisfactorily completed her treatment goals and would<br />
be in a period <strong>of</strong> stabilization for approximately two months<br />
while she became involved in her continuing care program.<br />
On September 1, 2009, Ms. Bergan executed a modified<br />
monitoring agreement with WPAP to add one more year<br />
to the monitoring period. In January 2010 WSBN received<br />
another report from WPAP advising that Ms. Bergan again<br />
self-reported relapse on or about January 18, 2010. WPAP<br />
anticipated further recommendations for evaluation and<br />
treatment. The terms <strong>of</strong> the Conditional License include a<br />
stayed suspension <strong>of</strong> six (6) months and require Ms. Bergan<br />
to: (1) enroll in the <strong>Nurse</strong> Monitoring Program (“NMP”)<br />
for not less than sixty (60) months; (2) submit to random<br />
drug screens; (3) regularly attend AA or NA meetings, and<br />
submit documentation <strong>of</strong> such attendance to the NMP; (4)<br />
not sign out, dispense or administer controlled substances<br />
without direct supervision for at least twenty-four (24)<br />
months; (5) obtain a worksite monitor; (6) provide an<br />
annual report <strong>of</strong> her progression and education in recovery;<br />
(7) provide annual clinical substance abuse evaluations/<br />
assessments; (8) complete courses in ethics, critical thinking<br />
and pr<strong>of</strong>essional accountability; and (9) provide the terms<br />
<strong>of</strong> the Conditional License to present/future employers.<br />
ERIC CANTRELL<br />
RN 18706<br />
CONDITIONAL LICENSE<br />
Eric Cantrell, RN, entered into a Settlement Agreement,<br />
Stipulation and Order for Conditional License on<br />
November 18, 2010, following a positive drug test for Ethyl<br />
Glucoronide on October 4, 2010. In October <strong>of</strong> 2007,<br />
Mr. Cantrell was issued a Conditional License by WSBN<br />
arising from incidents <strong>of</strong> chemical dependency and relapses<br />
during monitoring by the <strong>Wyoming</strong> Pr<strong>of</strong>essional Assistance<br />
Program (“WPAP”) and which was a reinstatement <strong>of</strong> his<br />
previously voluntarily surrendered license due to chemical<br />
dependency issues. Mr. Cantrell also received a Notice<br />
<strong>of</strong> Warning, issued on July 9, 2010, based upon violations<br />
related to his (1) failure to notify WSBN <strong>of</strong> an application<br />
for nursing license in the <strong>State</strong> <strong>of</strong> Utah following his<br />
relocation to Utah; (2) misrepresentation <strong>of</strong> the status <strong>of</strong><br />
Utah application; and (3) failure to comply with WPAP<br />
monitoring. The terms <strong>of</strong> the Conditional License include<br />
a stayed suspension for six (6) months and require Mr.<br />
Cantrell to: (1) enroll in the <strong>Nurse</strong> Monitoring Program<br />
(“NMP”) for not less than thirty-six (36) months; (2) submit<br />
to random drug screens; (3) regularly attend AA or NA<br />
meetings, and submit documentation <strong>of</strong> such attendance<br />
to the NMP; (4) not sign out, dispense or administer<br />
controlled substances without direct supervision for at least<br />
twelve (12) months; (5) obtain a worksite monitor; (6)<br />
provide an annual report <strong>of</strong> his progression and education<br />
in recovery; (7) provide annual clinical substance abuse<br />
evaluation/assessment; (8) complete courses in ethics and<br />
pr<strong>of</strong>essional accountability; and (9) provide the terms <strong>of</strong><br />
the Conditional License to present/future employers.<br />
VICTORIA COLE<br />
CNA 3564<br />
REVOCATION<br />
On or about February 1, <strong>2011</strong>, WSBN entered an Order<br />
<strong>of</strong> Default Judgment and an Order <strong>of</strong> Revocation against<br />
Victoria Cole, CNA. Pursuant to WSBN Rules and<br />
Regulations, Chapter 8, Section 7(a), WSBN may enter an<br />
order <strong>of</strong> default based on the allegations in a petition and<br />
complaint against a respondent/licensee who fails to appear<br />
for a properly noticed hearing. Ms. Cole failed to appear at<br />
a properly noticed disciplinary hearing. Accordingly, based<br />
on the petition and complaint which alleged violations <strong>of</strong><br />
the <strong>Nurse</strong> Practice Act through Ms. Cole’s actions related<br />
to practice beyond the scope <strong>of</strong> her licensure, fraud and<br />
deceit, and unpr<strong>of</strong>essional conduct while employed at<br />
Mountain Towers Healthcare and Rehabilitation Center,<br />
in Cheyenne, <strong>Wyoming</strong>, WSBN revoked Ms. Cole’s CNA<br />
certificate.<br />
RACHEL CRUMP<br />
CNA 18692<br />
LETTER OF REPRIMAND<br />
On or about February 1, <strong>2011</strong>, WSBN entered an Order<br />
<strong>of</strong> Default Judgment and an Order <strong>of</strong> Reprimand against<br />
Rachel Crump, CNA. Pursuant to WSBN Rules and<br />
Regulations, Chapter 8, Section 7(a), WSBN may enter<br />
an order <strong>of</strong> default based on the allegations in a petition<br />
and complaint against a respondent/licensee who fails<br />
to appear for a properly noticed hearing. Ms. Crump<br />
failed to appear at a properly noticed disciplinary hearing.<br />
Accordingly, based on the petition and complaint which<br />
alleged violations <strong>of</strong> the <strong>Nurse</strong> Practice Act through Ms.<br />
Crump’s actions related to criminal conviction, chemical<br />
dependency, unpr<strong>of</strong>essional conduct and failure to comply<br />
with reasonable requests by the <strong>Board</strong>, WSBN reprimanded<br />
Ms. Crump’s CNA certificate.<br />
24 <strong>Wyoming</strong> <strong>Nurse</strong> <strong>Reporter</strong>
JULIANA CULP<br />
LPN 6981<br />
LETTER OF REPRIMAND<br />
Juliana Culp, CNA, entered into a Settlement Agreement,<br />
Stipulation and Order for Letter <strong>of</strong> Reprimand on November<br />
17, 2010. A complaint was filed with WSBN by Ms. Culp’s<br />
employer, Pioneer Manor (“PM”) in Gillette, <strong>Wyoming</strong>,<br />
alleging unpr<strong>of</strong>essional conduct and unsafe practice arising<br />
from a February 2010 event, in which a PM resident<br />
contacted 911 requesting assistance because she was being<br />
ignored by medical personnel. The resident indicated that<br />
she did not feel safe and was not receiving requested medical<br />
treatment. During the internal investigation at PM, it was<br />
determined that Ms. Culp had not properly assessed the<br />
resident for medical treatment, administered medications<br />
without appropriate authorizations and/or insufficiently<br />
documented her activities and response to instructions<br />
from the hospitalist. Investigation by WSBN revealed that<br />
Ms. Culp had been disciplined previously on September<br />
17, 2009, for failure to comply with PM policies and<br />
procedures, including possible endangerment <strong>of</strong> different<br />
resident due to incomplete assessment and documentation.<br />
Ms. Culp also was terminated from employment at PM<br />
for failing to follow policies and procedures. In light <strong>of</strong><br />
Ms. Culp’s cooperation with the investigation, and other<br />
mitigating circumstances, WSBN agreed to issue a Letter<br />
<strong>of</strong> Reprimand for her conduct. Additionally, Ms. Culp was<br />
required to complete courses in ethics, critical thinking, and<br />
pr<strong>of</strong>essional accountability.<br />
ERICA CURRY<br />
RN 21954<br />
SUMMARY SUSPENSION<br />
Erica Curry, RN, stipulated to an Order for Summary<br />
Suspension on December 7, 2010. On or about December<br />
3, 2010, WSBN received a complaint from Ambulatory<br />
Surgery Center (“ASC”) in Laramie, <strong>Wyoming</strong>, which was<br />
based upon allegations <strong>of</strong> Ms. Curry’s admission to diversion<br />
<strong>of</strong> controlled substances for her personal use following<br />
determination <strong>of</strong> discrepancies in the controlled substance<br />
log. This selfadmitted diversion led to a stipulation between<br />
Ms. Curry and WSBN to summarily suspend her registered<br />
nursing license pending further proceedings by WSBN.<br />
ERICA CURRY<br />
RN 21954<br />
CONDITIONAL LICENSE<br />
Erica Curry, RN, entered into a Settlement Agreement,<br />
Stipulation and Order for Conditional License on January<br />
13, <strong>2011</strong>. The issuance <strong>of</strong> a Conditional Licensed followed<br />
Ms. Curry’s previous self-admitted diversion <strong>of</strong> controlled<br />
substances for personal use as a result <strong>of</strong> determination <strong>of</strong><br />
discrepancies in controlled substances log at Ambulatory<br />
Surgery Center in Laramie, <strong>Wyoming</strong>, which resulted in a<br />
Summary Suspension on December 7, 2010. The terms <strong>of</strong><br />
the Conditional License include a stayed suspension for six<br />
(6) months and require Ms. Curry to: (1) enroll in the <strong>Nurse</strong><br />
Monitoring Program (“NMP”) for not less than sixty (60)<br />
months; (2) submit to random drug screens; (3) regularly<br />
attend AA or NA meetings, and submit documentation <strong>of</strong><br />
such attendance to the NMP; (4) not sign out, dispense or<br />
administer controlled substances without direct supervision<br />
for at least twelve (12) months; (5) obtain a worksite<br />
monitor; (6) provide an annual report <strong>of</strong> her progression and<br />
education in recovery; (7) provide annual clinical substance<br />
abuse evaluations/assessments; (8) complete courses in<br />
ethics, critical thinking and pr<strong>of</strong>essional accountability;<br />
and (9) provide the terms <strong>of</strong> the Conditional License to<br />
present/future employers.<br />
CHRISTY DOWNES<br />
CNA 16318<br />
REVOCATION<br />
On or about February 4, <strong>2011</strong>, WSBN entered an Order<br />
<strong>of</strong> Default Judgment and an Order <strong>of</strong> Revocation against<br />
Christy Downes, CNA. Pursuant to WSBN Rules and<br />
Regulations, Chapter 8, Section 7(a), WSBN may enter<br />
an order <strong>of</strong> default based on the allegations in a petition<br />
and complaint against a respondent/licensee who fails<br />
to appear for a properly noticed hearing. Ms. Downes<br />
failed to appear at a properly noticed disciplinary hearing.<br />
Accordingly, based on the petition and complaint which<br />
alleged violations <strong>of</strong> the <strong>Nurse</strong> Practice Act through Ms.<br />
Towns’ actions related to abandonment and unpr<strong>of</strong>essional<br />
conduct while employed at Shepherd <strong>of</strong> the Valley Care<br />
Center, in Casper, <strong>Wyoming</strong>, WSBN revoked Ms. Downes’<br />
CNA certificate.<br />
AMY ELM<br />
RN 21676<br />
SUMMARY SUSPENSION<br />
Amy Elm, RN, stipulated to an Order for Summary<br />
Suspension on January 11, <strong>2011</strong>. On or about December<br />
15, 2010, WSBN received a complaint from Johnson<br />
County Healthcare (“JCHC”) in Buffalo, <strong>Wyoming</strong>, which<br />
was based upon allegations <strong>of</strong> Ms. Elm’s admission on<br />
October 8, 2010, to diversion <strong>of</strong> controlled substances for<br />
her personal use following determination <strong>of</strong> discrepancies<br />
in controlled substances log and/or discovery <strong>of</strong> forgeries.<br />
Ms. Elm subsequently entered residential treatment for<br />
approximately three (3) weeks and was permitted to return<br />
to work on November 1, subject to employer-imposed<br />
restrictions and conditions. Ms. Elm also submitted to a<br />
drug screen by blood but subsequently did not consent to<br />
the test being confirmed or completed and also voluntarily<br />
resigned from her nurse position at JCHC. This selfadmitted<br />
diversion led to a stipulation between Ms. Elm and<br />
WSBN to summarily suspend her registered nursing license<br />
pending further proceedings by WSBN.<br />
BARBARA EMERSON<br />
LPN 6600<br />
REVOCATION<br />
On or about November 16, 2010, WSBN entered an Order<br />
<strong>of</strong> Default Judgment and an Order <strong>of</strong> Revocation against<br />
Barbara Emerson, LPN. Pursuant to WSBN Rules and<br />
Regulations, Chapter 8, Section 7(a), WSBN may enter<br />
an order <strong>of</strong> default based on the allegations in a petition<br />
and complaint against a respondent/licensee who fails<br />
to appear for a properly noticed hearing. Ms. Emerson<br />
failed to appear at a properly noticed disciplinary hearing.<br />
Accordingly, based on the petition and complaint which<br />
alleged violations <strong>of</strong> the <strong>Nurse</strong> Practice Act through Ms.<br />
Emerson’s actions related to substance abuse/chemical<br />
dependency while employed at the <strong>Wyoming</strong> Retirement<br />
Center in Basin, <strong>Wyoming</strong>, WSBN revoked Ms. Emerson’s<br />
LPN license.<br />
VIOLET FREOUF<br />
CNA 16255<br />
VOLUNTARY SURRENDER<br />
Violet Freouf, CNA, entered into a Settlement Agreement,<br />
Stipulation and Order for Voluntary Surrender on<br />
November 18, 2010. It was alleged that Ms. Freouf failed to<br />
comply with reasonable requests <strong>of</strong> the <strong>Board</strong>. Specifically,<br />
Ms. Freouf provided an affirmative answer on her renewal<br />
application for the 2009-2010 biennium to the question<br />
whether in the past two years (2007-2008) “any disciplinary<br />
action has been taken or is any pending against [her] by a<br />
licensing authority,” without providing the documentation<br />
<strong>of</strong> the same as required in the application. Subsequently,<br />
<strong>Board</strong> compliance staff corresponded with Ms. Freouf<br />
requesting that she respond to requests for a personal<br />
statement or explanation regarding such disciplinary action<br />
or actions and documentation <strong>of</strong> the same, as well as<br />
confirmation <strong>of</strong> compliance with any orders. Ms. Freouf<br />
never responded to such requests, and subsequently agreed<br />
to voluntarily surrender her CNA certificate.<br />
ANNA GALLARDo<br />
CNA 19995<br />
LETTER OF REPRIMAND<br />
Anna Gallardo, CNA, entered into a Settlement<br />
Agreement, Stipulation and Order for Letter <strong>of</strong> Reprimand<br />
on November 17, 2010. On July 31, 2008, Ms. Gallardo<br />
executed an application for certified nursing assistant and<br />
answered in the negative the question whether she had been<br />
“charged, arrested, cited or convicted for any criminal <strong>of</strong>fense<br />
(including DUI).” Ms. Gallardo was issued an unrestricted<br />
certificate for certified nursing assistant on October 1,<br />
2008. A subsequent investigation revealed a conviction<br />
for DUI in 2003 in Scottsbluff, Nebraska. Such conduct is<br />
alleged to have failed to conform to nursing standards and<br />
to constitute unpr<strong>of</strong>essional conduct as well as fraud and<br />
deceit. WSBN agreed to issue a Letter <strong>of</strong> Reprimand to Ms.<br />
Gallardo’s conduct, as well as require completion <strong>of</strong> courses<br />
in ethics and pr<strong>of</strong>essional accountability.<br />
NANCY GILBERT<br />
RN 14495<br />
REVOCATION<br />
On or about November 16, 2010, WSBN entered an<br />
Order <strong>of</strong> Default Judgment and an Order <strong>of</strong> Revocation<br />
against Nancy Gilbert, RN. Pursuant to WSBN Rules<br />
and Regulations, Chapter 8, Section 7(a), WSBN may<br />
enter an order <strong>of</strong> default based on the allegations in a<br />
petition and complaint against a respondent/licensee who<br />
fails to appear for a properly noticed hearing. Ms. Gilbert<br />
failed to appear at a properly noticed disciplinary hearing.<br />
Accordingly, based on the petition and complaint which<br />
alleged violations <strong>of</strong> the <strong>Nurse</strong> Practice Act through Ms.<br />
Gilbert’s actions related to substance abuse, neglect, unsafe<br />
care, and physical/mental disability while employed at<br />
the Indian Health Services in Fort Washakie, <strong>Wyoming</strong>,<br />
WSBN revoked Ms. Gilbert’s license.<br />
CARRIE GILLARD<br />
CNA 11288<br />
LETTER OF REPRIMAND<br />
Carrie Gillard, CNA, entered into a Settlement Agreement,<br />
Stipulation and Order for Letter <strong>of</strong> Reprimand on January<br />
11, <strong>2011</strong>. On or about December 28, 2009, the <strong>Board</strong><br />
<strong>of</strong>fice received a complaint filed by Ms. Gillard’s employer,<br />
<strong>Wyoming</strong> <strong>State</strong> Hospital (“WSH”), alleging sexual<br />
boundary violations and client abuse by Ms. Gillard.<br />
Specifically, WSH had determined as the result <strong>of</strong> an<br />
internal investigation or personnel action that Ms. Gillard<br />
had taken provocative pictures <strong>of</strong> women from a magazine<br />
and posted them on the headboard <strong>of</strong> a patient <strong>of</strong> WSH<br />
as a joke when she was on duty in her employment with<br />
WSH. Ms. Gillard admitted her actions when confronted<br />
and also acknowledged that such actions prompted a<br />
response by the patient, even though the patient is stated<br />
to have cognitive limitations. In addition, Ms. Gillard<br />
expressed remorse for her conduct. In light <strong>of</strong> the isolated<br />
instance <strong>of</strong> the complaint and Ms. Gillard’s willingness to<br />
remediate, WSBN agreed to issue a Letter <strong>of</strong> Reprimand<br />
to her conduct. Additionally, Ms. Gillard was required to<br />
complete courses in ethics and pr<strong>of</strong>essional boundaries.<br />
KRISTINA GOSSMAN<br />
RN 25421<br />
CONDITIONAL LICENSE<br />
Kristina Gossman, RN, entered into a Settlement<br />
Agreement, Stipulation and Order for Conditional License<br />
on January 10, <strong>2011</strong>. In April 2009 a complaint was<br />
initiated with respect to Ms. Gossman, based upon a March<br />
12, 2009, incident in which Ms. Gossman appeared to<br />
be impaired while working by several other co-workers<br />
at the West Park Hospital (“WPH”) in Cody, <strong>Wyoming</strong>.<br />
Ms. Gossman was requested to submit to an alcohol<br />
screen by urinalysis, which she refused. Ms. Gossman<br />
also admitted the use <strong>of</strong> alcohol the previous evening<br />
but denied being under the influence when she reported<br />
to work. Ms. Gossman subsequently was terminated<br />
from employment for violating WPH policy. Further<br />
investigation by WSBN staff revealed: (a) Ms. Gossman<br />
was the subject <strong>of</strong> a prior informal disciplinary action in the<br />
December 2008 time frame, in which a patient at WPH had<br />
reported suspicions <strong>of</strong> Ms. Gossman having alcohol on her<br />
breath. No urinalysis was obtained at such time; and (b)<br />
Witness letters provided to the <strong>Board</strong> with respect to the<br />
events on March 12, 2009, confirmed, without exception,<br />
observations that Ms. Gossman appeared impaired and/or<br />
had the smell <strong>of</strong> alcohol on her breath. The terms <strong>of</strong> the<br />
Conditional License include a stayed suspension <strong>of</strong> six (6)<br />
months and require Ms. Gossman to: (1) enroll in the <strong>Nurse</strong><br />
Monitoring Program (“NMP”) for not less than sixty (60)<br />
Continued on page 26<br />
<strong>Wyoming</strong> <strong>Nurse</strong> <strong>Reporter</strong> 25
months; (2) submit to random drug screens; (3) regularly<br />
attend AA or NA meetings, and submit documentation <strong>of</strong><br />
such attendance to the NMP; (4) not sign out, dispense or<br />
administer controlled substances without direct supervision<br />
for at least twenty-four (24) months; (5) obtain a worksite<br />
monitor; (6) provide an annual report <strong>of</strong> her progression and<br />
education in recovery; (7) provide annual clinical substance<br />
abuse evaluations/assessments; (8) complete courses in<br />
ethics, critical thinking and pr<strong>of</strong>essional accountability;<br />
and (9) provide the terms <strong>of</strong> the Conditional License to<br />
present/future employers.<br />
DIANA GUMM<br />
RN 22394<br />
CONDITIONAL LICENSE<br />
Diana Gumm, RN, entered into a Settlement Agreement,<br />
Stipulation and Order for Conditional License on November<br />
18, 2010. Ms. Gumm was reported to have suffered a Level<br />
III relapse in 2007 while in the <strong>Wyoming</strong> Pr<strong>of</strong>essional<br />
Assistance Program (“WPAP”), with subsequent admission<br />
to residential treatment for opiod detox. Following<br />
discharge from residential treatment, Ms. Gumm returned<br />
to WPAP. The terms <strong>of</strong> the Conditional License include<br />
a stayed suspension for six (6) months and require Ms.<br />
Gumm to: (1) enroll in the <strong>Nurse</strong> Monitoring Program<br />
(“NMP”) for not less than sixty (60) months; (2) submit<br />
to random drug screens; (3) regularly attend AA or NA<br />
meetings, and submit documentation <strong>of</strong> such attendance<br />
to the NMP; (4) not sign out, dispense or administer<br />
controlled substances without direct supervision for at least<br />
twenty-four (24) months; (5) obtain a worksite monitor; (6)<br />
provide an annual report <strong>of</strong> her progression and education<br />
in recovery; (7) provide semi-annual clinical substance<br />
abuse evaluations/assessments; (8) complete courses in<br />
ethics, critical thinking and pr<strong>of</strong>essional accountability; (9)<br />
participate in regular mental health counseling; and (10)<br />
provide the terms <strong>of</strong> the Conditional License to present/<br />
future employers.<br />
KATHERINE HALVORSEN<br />
RN 17718<br />
VOLUNTARY SURRENDER<br />
Katherine Halvorsen, RN, entered into a Settlement<br />
Agreement, Stipulation and Order for Voluntary Surrender<br />
on November 17, 2010. Initially, Ms. Halvorsen was the<br />
subject <strong>of</strong> a disciplinary complaint as the result <strong>of</strong> a WPAP<br />
report <strong>of</strong> three (3) previous Level III relapses while she<br />
was participating in the voluntary impaired nurse program<br />
with WPAP. Respondent acknowledged her chemical<br />
dependency and was issued a Conditional License for sixty<br />
(60) months, subject to monitoring, 36-month restrictions<br />
regarding dispensing <strong>of</strong> medication and other terms and<br />
conditions that was approved by the <strong>Board</strong> on or about<br />
January 12, 2005. Respondent was the subject <strong>of</strong> a further<br />
disciplinary complaint prompted by the September 12, 2005<br />
WPAP notification that Respondent had tested positive<br />
for morphine on August 15, 2005. This relapse was noted<br />
to have occurred only eight (8) months following the<br />
approval <strong>of</strong> the 2005 Conditional License. Ms. Halvorsen<br />
was issued a Conditional License on October 9, 2007,<br />
arising from incidents <strong>of</strong> chemical dependency and relapses<br />
during monitoring by <strong>Wyoming</strong> Pr<strong>of</strong>essional Assistance<br />
Program (“WPAP”). This Conditional License modified<br />
the 2006 Conditional License, which also incorporated<br />
the 2005 Conditional License terms and conditions. On<br />
December 28, 2009, WPAP notified WSBN <strong>of</strong> a Level<br />
III relapse by Ms. Halvorsen, in which she had tested<br />
positive for alcohol and acknowledged the positive test<br />
to WPAP representatives and, subsequently, to WSBN.<br />
Subsequently, on March 12, 2010, WPAP notified WSBN<br />
<strong>of</strong> another Level III relapse by Ms. Halvorsen. Since January<br />
there were several drug screens indicated to be diluted, but<br />
testing negative for drugs or alcohol. A hair specimen was<br />
subsequently collected for testing and returned positive for<br />
morphine and hydromorphone. Such conduct was alleged<br />
to have failed to conform to nursing standards, constitute<br />
unpr<strong>of</strong>essional conduct, and to constitute unauthorized use<br />
<strong>of</strong> a controlled substance. Ms. Halvorsen did not dispute<br />
the findings <strong>of</strong> WSBN and, accordingly, Ms. Halvorsen<br />
agreed to voluntarily surrender her RN license.<br />
TRINA HEIDE<br />
CNA 14087<br />
REVOCATION<br />
On or about November 16, 2010, WSBN entered an<br />
Order <strong>of</strong> Default Judgment and an Order <strong>of</strong> Revocation<br />
against Trina Heide, CNA. Pursuant to WSBN Rules and<br />
Regulations, Chapter 8, Section 7(a), WSBN may enter an<br />
order <strong>of</strong> default based on the allegations in a petition and<br />
complaint against a respondent/licensee who fails to appear<br />
for a properly noticed hearing. Ms. Heide failed to appear at<br />
a properly noticed disciplinary hearing. Accordingly, based<br />
on the petition and complaint which alleged violations<br />
<strong>of</strong> the <strong>Nurse</strong> Practice Act through Ms. Heide’s actions<br />
related to alcohol abuse and unpr<strong>of</strong>essional conduct while<br />
employed at West Park Long Term Care Center and<br />
voluntary admission to an inpatient treatment program for<br />
an addiction to opiate pain medication noted in her 2009-<br />
2010 certification renewal application, WSBN revoked Ms.<br />
Heide’s CNA certificate.<br />
TANIE HEITZ<br />
CNA 11941<br />
CONDITIONAL CERTIFICATE<br />
Tanie Heitz, CNA, entered into a Settlement Agreement,<br />
Stipulation and Order for Conditional Certificate on<br />
January 13, <strong>2011</strong>. In May 2010, Ms. Heitz’s employer,<br />
Laramie Hospice (“LH”), submitted a complaint alleging<br />
Ms. Heitz tested positive at work for alcohol on April 27,<br />
2010. Specifically, the complaint alleged that Ms. Heitz’s<br />
breath alcohol test was .020, and because she was in a<br />
monitored treatment program, was required to test negative<br />
on random tests. Ms. Heitz subsequently submitted a letter<br />
<strong>of</strong> resignation to LH. Ms. Heitz acknowledged the substance<br />
<strong>of</strong> the complaint and denied consumption <strong>of</strong> alcohol, but<br />
instead taking Theraflu, which contained alcohol, as well<br />
as summarizing her subsequent efforts toward treatment and<br />
recovery to prior residential treatment and aftercare. Ms.<br />
Heitz was admitted for residential treatment to Harmony<br />
Foundation in Estes Park, Colorado (“Harmony”) on May<br />
26, 2009 and was discharged on June 23, 2009. Further<br />
communications from LH indicated that since residential<br />
treatment, Ms. Heitz tested positive two <strong>of</strong> three times<br />
for alcohol, which included the incident related to her<br />
resignation, and her supervisor suspected alcohol odor<br />
from Ms. Heitz at work, for which she had been previously<br />
confronted. The terms <strong>of</strong> the Conditional Certificate shall<br />
remain in place for not less than sixty (60) months and<br />
require Ms. Heitz to: (1) abstain from all mind-altering<br />
drugs or medications; (2) notify her designated worksite<br />
monitor(s) within seventy-two hours <strong>of</strong> any prescriptions<br />
or mood-altering substances; (3) obtain a worksite monitor;<br />
(4) submit to random drug screens; (5) regularly attend<br />
AA or NA meetings, and submit documentation <strong>of</strong> such<br />
attendance to WSBN; (6) provide an annual report <strong>of</strong><br />
her progression and education in recovery; (7) provide<br />
annual clinical substance abuse evaluations/assessments; (8)<br />
complete a courses in ethics; and (9) provide the terms <strong>of</strong><br />
the Conditional Certificate to present/future employers.<br />
KATHERINE HENDRICKS<br />
RN 24794<br />
VOLUNTARY SURRENDER<br />
Katherine Hendricks, RN, entered into a Settlement<br />
Agreement, Stipulation and Order for Voluntary Surrender<br />
on November 16, 2010. It was alleged that Ms. Hendricks<br />
was abusing medications, both nonprescription and<br />
prescriptions for mental health conditions (bipolar disorder<br />
and depression), as well as alcohol. WSBN investigation<br />
subsequently confirmed that: (1) Ms. Hendricks had<br />
entered into residential substance abuse treatment at<br />
Transformations Wellness Center, <strong>of</strong> Klamath Falls, Oregon,<br />
following which she participated in aftercare; and (2) On or<br />
about February 11, 2009, according to National Practitioner<br />
Data Bank/Healthcare Integrity Protection Data Bank<br />
records regarding Ms. Hendricks, the Oregon <strong>State</strong> <strong>Board</strong><br />
<strong>of</strong> <strong>Nursing</strong> denied license renewal based upon, among other<br />
things, misrepresentations <strong>of</strong> credentials, practicing without<br />
a valid license and fraud, deceit or material omission in<br />
obtaining license. Such conduct was alleged to have<br />
failed to conform to nursing standards and to constitute<br />
unpr<strong>of</strong>essional conduct in nursing practice. Ms. Hendricks<br />
subsequently advised she would not be continuing to<br />
practice nursing due to medical issues and agreed to<br />
voluntarily surrender her registered nursing license.<br />
MICHELLE JACOBSEN<br />
CNA 17499<br />
LETTER OF REPRIMAND<br />
Michelle Jacobsen, CNA, entered into a Settlement<br />
Agreement, Stipulation and Order for Letter <strong>of</strong> Reprimand<br />
on November 17, 2010. In April 2010, WSBN received<br />
a complaint from Ms. Jacobsen’s employer, Shepherd <strong>of</strong><br />
the Valley Care Center in Casper, <strong>Wyoming</strong> (“SVCC”),<br />
alleging patient abandonment, which also was reported to<br />
the <strong>Wyoming</strong> Department <strong>of</strong> Health, Office <strong>of</strong> Healthcare<br />
Licensing and Surveys (“OHLS”). Specifically, after<br />
reporting for work, Ms. Jacobsen was seen to have left<br />
the premises at SVCC, without returning or making<br />
arrangements for continuing care <strong>of</strong> residents to whom<br />
Ms. Jacobsen had been assigned. Ms. Jacobsen also did<br />
not have prior knowledge or approval for her departure<br />
from her superiors, and her actions resulted in employment<br />
termination. Such conduct is alleged to have failed to<br />
conform to nursing standards, as well as to constitute<br />
abandonment and unpr<strong>of</strong>essional conduct. WSBN agreed<br />
to issue a Letter <strong>of</strong> Reprimand to Ms. Jacobsen’s conduct<br />
and, additionally, require completion <strong>of</strong> courses in ethics<br />
and pr<strong>of</strong>essional accountability.<br />
JAMES JUDD<br />
LPN 6137<br />
VOLUNTARY SURRENDER<br />
James Judd, LPN, entered into a Settlement Agreement,<br />
Stipulation and Order for Voluntary Surrender <strong>of</strong> License<br />
on November 18, 2010. As <strong>of</strong> the date <strong>of</strong> this Agreement,<br />
Mr. Judd’s license was a Conditional License per Settlement<br />
Agreement, Stipulation and Order approved by the <strong>Board</strong><br />
on April 9, 2009, arising from an incident resulting in<br />
criminal conviction for diversion <strong>of</strong> controlled substances.<br />
In September 2010, Mr. Judd returned his nurse license card<br />
for personal reasons and requested that the <strong>Board</strong> accept<br />
his voluntary surrender <strong>of</strong> his LPN license. Although Mr.<br />
Judd’s request did not constitute new violations <strong>of</strong> the NPA<br />
or <strong>Board</strong>’s Rules, the underlying grounds and basis for the<br />
2009 Conditional License have not been excused, and<br />
the <strong>Board</strong> retains continuing jurisdiction over Mr. Judd.<br />
Consequently, Mr. Judd’s voluntary surrender <strong>of</strong> his LPN<br />
license was accepted by WSBN.<br />
DEBORAH KETCHAM<br />
RN 21161<br />
CONDITIONAL LICENSE<br />
Deborah Ketcham, RN, entered into a Settlement Agreement,<br />
Stipulation and Order for Conditional License on November<br />
18, 2010. Ms. Ketcham was alleged to have ordered an<br />
excessive amount <strong>of</strong> Vicodin for a resident under her care,<br />
raising suspicions <strong>of</strong> drug diversion. A patient prescription<br />
pr<strong>of</strong>ile relating to Ms. Ketcham obtained from the <strong>Wyoming</strong><br />
<strong>State</strong> <strong>Board</strong> <strong>of</strong> Pharmacy (“BOP”) covering the period July<br />
2008 through May 2009 revealed numerous prescriptions<br />
for opiod pain relief medication from multiple health care<br />
providers, in addition to prescriptions for Suboxone beginning<br />
in January 2009. In July 2009 it was reported by the WPAP<br />
that Ms. Ketcham had suffered a Level III relapse, following<br />
two positive tests for methadone in May 2009 accompanied by<br />
two additional positive tests for methadone in June 2009. The<br />
terms <strong>of</strong> the Conditional License include a stayed suspension<br />
for six (6) months and require Ms. Ketcham to: (1) enroll in<br />
the <strong>Nurse</strong> Monitoring Program (“NMP”) for not less than sixty<br />
(60) months; (2) submit to random drug screens; (3) regularly<br />
attend AA or NA meetings, and submit documentation <strong>of</strong><br />
such attendance to the NMP; (4) not sign out, dispense or<br />
administer controlled substances without direct supervision<br />
for at least twenty-four (24) months; (5) obtain a worksite<br />
monitor; (6) provide an annual report <strong>of</strong> her progression and<br />
education in recovery; (7) provide annual clinical substance<br />
abuse evaluations/assessments; (8) complete courses in ethics<br />
and pr<strong>of</strong>essional accountability; and (9) provide the terms <strong>of</strong><br />
the Conditional License to present/future employers.<br />
26 <strong>Wyoming</strong> <strong>Nurse</strong> <strong>Reporter</strong>
MARCELLA KNAUB<br />
RN 20430<br />
REVOCATION<br />
On or about November 16, 2010, WSBN entered an Order<br />
<strong>of</strong> Default Judgment and an Order <strong>of</strong> Revocation against<br />
Marcella Knaub, RN. Pursuant to WSBN Rules and<br />
Regulations, Chapter 8, Section 7(a), WSBN may enter an<br />
order <strong>of</strong> default based on the allegations in a petition and<br />
complaint against a respondent/licensee who fails to appear<br />
for a properly noticed hearing. Ms. Knaub failed to appear at<br />
a properly noticed disciplinary hearing. Accordingly, based<br />
on the petition and complaint which alleged violations <strong>of</strong><br />
the <strong>Nurse</strong> Practice Act through Ms. Knaub’s actions related<br />
to chemical dependency/substance abuse while employed at<br />
Indian Health Services, Crow Agency, Montana, and which<br />
rendered her unable to perform nursing duties, WSBN<br />
revoked Ms. Knaub’s RN license.<br />
SAMANTHA LITTLE<br />
RN 28410<br />
LETTER OF REPRIMAND<br />
Samantha Little, RN, entered into a Settlement Agreement,<br />
Stipulation and Order for Letter <strong>of</strong> Reprimand on January<br />
11, <strong>2011</strong>. In September 2010 a complaint was initiated<br />
based upon Ms. Little’s self-report <strong>of</strong> DUI. On September<br />
21, 2010, Ms. Little entered a plea <strong>of</strong> guilty to Driving While<br />
Under the Influence-First Offense, which was suspended<br />
pursuant to W.S. §7-13-301 and was placed on unsupervised<br />
probation for a period <strong>of</strong> twelve (12) months. It is alleged<br />
Ms. Little’s conduct failed to conform to standards <strong>of</strong><br />
nursing practice, as well as constituting criminal conviction,<br />
unfitness due to use <strong>of</strong> drugs or other mind-altering chemical<br />
and substance abuse/impairment. In light <strong>of</strong> Ms. Little’s<br />
cooperation with the investigation, and other mitigating<br />
circumstances, WSBN agreed to issue a Letter <strong>of</strong> Reprimand<br />
to her conduct. Additionally, Ms. Little was required to<br />
complete an ethics course.<br />
KEVIN MADER<br />
RN 24869<br />
SUMMARY SUSPENSION<br />
Kevin Mader, RN, stipulated to an Order for Summary<br />
Suspension on January 11, <strong>2011</strong>. On or about December<br />
23, 2010, a complaint was submitted by Mr. Mader’s<br />
employer, Powell Valley Healthcare (“PVH”) in Powell,<br />
<strong>Wyoming</strong>. Such complaint was based upon allegations<br />
<strong>of</strong> Mr. Mader’s diversion <strong>of</strong> controlled substances for his<br />
personal use. Mr. Mader had presented at North Big<br />
Horn Hospital (“NBHH”) emergency room, with a likely<br />
benzodiazepine overdose as indicated by his own statement<br />
that he had ingested three (3) Lorazepam tablets, which he<br />
had obtained from his employer, PVH. This information<br />
also was communicated by NBHH to PVH. Mr. Mader<br />
was known to PVH as being monitored privately by the<br />
<strong>Wyoming</strong> Pr<strong>of</strong>essional Assistance Program (“WPAP”) and<br />
that prior relapses or non-compliance had been suspected.<br />
Other controlled substances believed to have been taken<br />
from PVH were discovered at NBHH and on Mr. Mader’s<br />
person including approximately sixty-two (62) tablets <strong>of</strong><br />
Tramadol. Further investigation would be undertaken<br />
by PVH in an attempt to determine whether additional<br />
amounts <strong>of</strong> controlled substances and other medications,<br />
including Tramadol, may have been diverted by Mr. Mader.<br />
This self-admitted diversion led to a stipulation between<br />
Mr. Mader and WSBN to summarily suspend his registered<br />
nursing license pending further proceedings by WSBN.<br />
PAMELA MATTSON<br />
CNA 18634<br />
REVOCATION<br />
On or about November 16, 2010, WSBN entered an Order<br />
<strong>of</strong> Default Judgment and an Order <strong>of</strong> Revocation against<br />
Pamela Mattson, CNA. Pursuant to WSBN Rules and<br />
Regulations, Chapter 8, Section 7(a), WSBN may enter<br />
an order <strong>of</strong> default based on the allegations in a petition<br />
and complaint against a respondent/licensee who fails<br />
to appear for a properly noticed hearing. Ms. Mattson<br />
failed to appear at a properly noticed disciplinary hearing.<br />
Accordingly, based on the petition and complaint which<br />
alleged violations <strong>of</strong> the <strong>Nurse</strong> Practice Act through Ms.<br />
Mattson’s actions related to alcohol impairment while<br />
employed at Weston County Health Services <strong>of</strong> Newcastle,<br />
<strong>Wyoming</strong>, WSBN revoked Ms. Mattson’s CNA certificate.<br />
MARY MCBRIDE<br />
RN 17887<br />
LETTER OF REPRIMAND<br />
Mary McBride, RN, entered into a Settlement Agreement,<br />
Stipulation and Order for Letter <strong>of</strong> Reprimand on November<br />
17, 2010. In June 2010, WSBN received a complaint from<br />
Ms. McBride’s employer, Goshen Care Center (“GCC”) in<br />
Torrington, <strong>Wyoming</strong>, which generally alleged abuse and<br />
unpr<strong>of</strong>essional conduct. Specifically, Ms. McBride allegedly<br />
was abusive to two GCC residents. Ms. McBride allegedly<br />
restrained one resident by holding their hands after the<br />
patient was slapping their hands on the dinner table. In<br />
addition, when another resident was verbally rude while in<br />
the dining room, Ms. McBride placed the resident in the<br />
sun room by herself where she was left for approximately<br />
fifteen minutes. Such conduct is alleged to constitute<br />
unsafe client care; abuse; neglect; unpr<strong>of</strong>essional conduct;<br />
and failure to conform to nursing standards. In light <strong>of</strong> Ms.<br />
McBride’s cooperation with the investigation, and other<br />
mitigating circumstances, WSBN agreed to issue a Letter <strong>of</strong><br />
Reprimand to her conduct. Additionally, Ms. McBride was<br />
required to complete courses in ethics, critical thinking, and<br />
pr<strong>of</strong>essional accountability.<br />
AMANDA NAPOLETANO<br />
CNA 12470<br />
LETTER OF REPRIMAND<br />
Amanda Napoletano, CNA, entered into a Settlement<br />
Agreement, Stipulation and Order for Letter <strong>of</strong> Reprimand<br />
on January 11, <strong>2011</strong>. On or about February 12, 2010,<br />
the <strong>Board</strong> received a report from <strong>Wyoming</strong> Department<br />
<strong>of</strong> Family Services (“DFS”) <strong>of</strong> alleged abuse towards a<br />
male patient <strong>of</strong> the <strong>Wyoming</strong> <strong>State</strong> Hospital (“WSH”).<br />
A complaint was initiated against Ms. Napoletano.<br />
Subsequently, on February 24, 2010, the <strong>Board</strong> received a<br />
complaint initiated by Donna Aspuria, Interim Director<br />
<strong>of</strong> <strong>Nursing</strong> for the WSH in Evanston, <strong>Wyoming</strong>, alleging<br />
acts <strong>of</strong> abuse, unpr<strong>of</strong>essional conduct and sexual boundary<br />
violations towards the same male patient, in which Ms.<br />
Napoletano also was the subject. WSBN agreed to issue<br />
a Letter <strong>of</strong> Reprimand to Ms. Napoletano’s conduct.<br />
Additionally, Ms. Napoletano was required to complete<br />
courses in ethics and pr<strong>of</strong>essional boundaries, along with<br />
reading “Games Criminals Play” by Juanita Allen and<br />
completing an authorized test on said book.<br />
ANDREW NEMEC<br />
RN 27678<br />
VOLUNTARY SURRENDER<br />
Andrew Nemec, RN, entered into a Settlement Agreement,<br />
Stipulation and Order for Voluntary Surrender on December<br />
6, 2010. WSBN initiated a complaint based upon<br />
disciplinary action relating to Mr. Nemec’s Illinois license,<br />
as reflected by an Order dated July 19, 2010 (“Illinois<br />
Order”), by the <strong>State</strong> <strong>of</strong> Illinois Department <strong>of</strong> Financial<br />
and Pr<strong>of</strong>essional Regulation. The Illinois Order reflected<br />
that Mr. Nemec diverted Dilaudid during the period<br />
December 6 through 8, 2009, and was subjected to a drug<br />
screen which tested positive, while employed as a registered<br />
nurse with Alexian Brothers Medical Center in Elk Grove<br />
Village, Illinois (“ABMC”). Mr. Nemec admitted the<br />
diversion and was terminated from employment at ABMC.<br />
Mr. Nemec also held a Registered <strong>Nurse</strong> license in the state<br />
<strong>of</strong> California, the status <strong>of</strong> which is “inactive” due to failure<br />
to provide continuing education. Mr. Nemec subsequently<br />
notified WSBN <strong>of</strong> his intent to let his <strong>Wyoming</strong> license<br />
expire and agreed to voluntarily surrender his registered<br />
nursing license.<br />
DELORIS PARKER<br />
RN 20501<br />
LETTER OF REPRIMAND<br />
Deloris Parker, RN, entered into a Settlement Agreement,<br />
Stipulation and Order for Letter <strong>of</strong> Reprimand on January<br />
11, <strong>2011</strong>. In February 2009 Ms. Parker’s employer initiated<br />
a complaint alleging inappropriate delegation, as well<br />
as fraud and deceit. Specifically, on February 16, 2009,<br />
a report was submitted <strong>of</strong> an incident on February 12,<br />
2009, in which Ms. Parker, in violation <strong>of</strong> safety protocol<br />
regarding medication administration, directed a first-year<br />
nursing student to give an oral opiate medication without<br />
the nursing instructor or a supervising preceptor nurse being<br />
present. Although the medication was administered by the<br />
nursing student, Ms. Parker documented that she herself<br />
had administered the medication (hydrocodone). Internal<br />
investigation at PVH also confirmed this report. Ms. Parker<br />
subsequently confirmed the allegations, acknowledging<br />
that she asked a nursing student to deliver medication to<br />
a patient, whom she did not accompany because <strong>of</strong> other<br />
nursing duties and fire alarm distractions at the time. It is<br />
alleged this conduct violated standards <strong>of</strong> nursing practice<br />
and constituted unpr<strong>of</strong>essional conduct as well as fraud and<br />
deceit in signing a report/record as a registered nurse. In<br />
light <strong>of</strong> Ms. Parker’s cooperation with the investigation,<br />
and other mitigating circumstances, WSBN agreed to issue<br />
a Letter <strong>of</strong> Reprimand to her conduct. Additionally, Ms.<br />
Parker was required to complete courses in ethics, effective<br />
delegation, and detection and prevention <strong>of</strong> medication<br />
errors.<br />
JEANNE PAYTON<br />
RN 16924<br />
CONDITIONAL LICENSE<br />
Jeanne Payton, RN, entered into a Settlement Agreement,<br />
Stipulation and Order for Conditional License on November<br />
17, 2010. Ms. Payton made a self-report <strong>of</strong> on-the-job<br />
alcohol use on April 21, 2010, stemming from a report she<br />
made to her employer, Cheyenne Regional Medical Center<br />
(“CRMC”) in October 2009. Ms. Payton also reported a<br />
relapse in March 2010 to WSBN, which she also reported<br />
to CRMC. Ms. Payton immediately entered residential<br />
treatment at Cedar <strong>Spring</strong>s, after which she participated<br />
in an Intensive Outpatient Program (“IOP”) provided by<br />
CRMC until successful discharge on May 17, 2010. The<br />
terms <strong>of</strong> the Conditional License include a stayed suspension<br />
for ninety (90) days and require Ms. Payton to: (1) enroll<br />
in the <strong>Nurse</strong> Monitoring Program (“NMP”) for not less<br />
than sixty (60) months; (2) submit to random drug screens;<br />
(3) regularly attend AA or NA meetings, and submit<br />
documentation <strong>of</strong> such attendance to the NMP; (4) not sign<br />
out, dispense or administer controlled substances without<br />
direct supervision for at least twenty-four (24) months; (5)<br />
obtain a worksite monitor; (6) provide an annual report<br />
<strong>of</strong> her progression and education in recovery; (7) provide<br />
annual clinical substance abuse evaluations/assessments; (8)<br />
complete courses in ethics and pr<strong>of</strong>essional accountability;<br />
and (9) provide the terms <strong>of</strong> the Conditional License to<br />
present/future employers.<br />
LAURIE PENDERGRAFT<br />
LPN 4315<br />
VOLUNTARY SURRENDER<br />
Laurie Pendergraft, LPN, entered into a Settlement<br />
Agreement, Stipulation and Order for Voluntary Surrender<br />
on January 11, <strong>2011</strong>. In June 2010, a complaint was<br />
submitted to WSBN by Ms. Pendergraft’s employer, Pioneer<br />
Manor (“PM”), the long-term care unit <strong>of</strong> Campbell County<br />
Memorial Hospital, located in Gillette, <strong>Wyoming</strong>. Such<br />
complaint generally alleged alcohol or chemical impairment<br />
and concerns regarding unsafe care. Specifically, Ms.<br />
Pendergraft reported to work on May 29, 2010 with a blood<br />
alcohol level <strong>of</strong> 117, which was reported by an outside lab<br />
testing as showing blood alcohol content (“BAC”) <strong>of</strong> 0.092.<br />
Ms. Pendergraft was subsequently terminated from her<br />
employment with PM. It is alleged that Ms. Pendergraft’s<br />
conduct failed to conform to standards <strong>of</strong> nursing practice<br />
and constituted unfitness/incompetency due to use <strong>of</strong> drugs<br />
or other mind-altering chemical, as well as unpr<strong>of</strong>essional<br />
Continued on page 28<br />
<strong>Wyoming</strong> <strong>Nurse</strong> <strong>Reporter</strong> 27
conduct and impairment. WSBN agreed to accept Ms.<br />
Pendergraft’s voluntary surrender <strong>of</strong> her LPN license.<br />
SHARI (LONG) ROMERO<br />
RN 21612<br />
LETTER OF REPRIMAND/CONDITIONAL<br />
LICENSE<br />
On or about January 10, <strong>2011</strong>, WSBN entered an Order<br />
Issuing Letter <strong>of</strong> Reprimand and Issuing Conditional License<br />
against Shari (Long) Romero, RN, following a contested<br />
hearing held on September 21-22, 2010. It was generally<br />
alleged that Ms. (Long) Romero had violated provisions <strong>of</strong><br />
the <strong>Nurse</strong> Practice Act related to unpr<strong>of</strong>essional conduct,<br />
disciplinary action in another jurisdiction, substance abuse/<br />
chemical impairment and criminal convictions. Specifically,<br />
it was alleged that Ms. (Long) Romero had failed to disclose<br />
certain disciplinary information from another jurisdiction<br />
to WSBN and had been twice arrested for driving while<br />
under the influence. Further, it was alleged that Ms. (Long)<br />
Romero had an on-going impairment related to substance/<br />
chemical abuse. WSBN issued a reprimand for Ms. (Long)<br />
Romero’s conduct in failing to disclose information on<br />
the <strong>Board</strong>’s application documents. In addition, WSBN<br />
issued a Conditional License to Ms. (Long) Romero with<br />
the following conditions: (1) indefinite participation in<br />
the <strong>Nurse</strong> Monitoring Program (NMP); (2) shall not work<br />
as a registered nurse while taking a prescription for any<br />
controlled substance, as defined in the <strong>Wyoming</strong> Controlled<br />
Substances Act, and demonstrate to the NMP the proper<br />
waste <strong>of</strong> any unused controlled substance; (3) administration<br />
<strong>of</strong> any medication by any route, or participation in any<br />
procedures, including PICC line placement, while employed<br />
as a registered nurse shall be monitored by her worksite<br />
monitor through direct supervision; (4) no duties that<br />
allow exposure to medical waste containers without direct<br />
supervision from her worksite monitor; and (5)submit to a<br />
hair sample for drug screening purposes every six months,<br />
beginning one month from the effective date <strong>of</strong> the order.<br />
KRISTINE SCOTT<br />
CNA 19728<br />
REVOCATION<br />
On or about November 16, 2010, WSBN entered an Order<br />
<strong>of</strong> Revocation against Kristine Scott, CNA, following a<br />
contested hearing held on September 21, 2010. It was<br />
generally alleged that Ms. Scott had violated provisions<br />
<strong>of</strong> the Act related to chemical impairment and criminal<br />
violations. Specifically, it was alleged that Ms. Scott<br />
had been terminated from her employment as a CNA<br />
for being under the influence <strong>of</strong> methamphetamines at<br />
work; had been criminally convicted <strong>of</strong> unauthorized use<br />
<strong>of</strong> a controlled substance; and had subsequent relapses to<br />
substances. Accordingly, following deliberations which<br />
considered the evidence presented at the hearing, WSBN<br />
revoked Ms. Scott’s CNA certificate.<br />
WILLIAM STEWART<br />
RN 22821<br />
CONDITIONAL LICENSE<br />
William Stewart, RN, entered into a Settlement Agreement,<br />
Stipulation and Order for Conditional License on November<br />
17, 2010. When Mr. Stewart submitted his application for<br />
a registered pr<strong>of</strong>essional nurse license by endorsement in<br />
2005, he voluntarily revealed that he had been the subject<br />
<strong>of</strong> prior disciplinary action by the Montana <strong>State</strong> <strong>Board</strong><br />
<strong>of</strong> <strong>Nursing</strong> on the basis <strong>of</strong> drug diversion and narcotics<br />
addiction and had received treatment for addiction. Mr.<br />
Stewart subsequently filed a self-complaint with WSBN in<br />
August 2009, admitting drug diversion and substance abuse/<br />
dependency. At that time, Mr. Stewart indicated that in<br />
1998 he had developed a substance abuse problem when<br />
working as a nurse in Montana and received treatment.<br />
He also indicated that he was drug free until working in<br />
Lander, WY, when he was prescribed medication for back<br />
pain. He developed an addiction and began diverting<br />
medication waste and abusing opioids. He further indicated<br />
that he returned to treatment at Rimrock Foundation<br />
Treatment Center in Montana on an in-patient basis. In<br />
September2009, WSBN received a complaint from Lander<br />
Regional Hospital (“LRH”), which reported that on August<br />
25, 2009, Mr. Stewart was perceived to be impaired toward<br />
the end <strong>of</strong> his shift in the ER. It was also reported at that<br />
time the department in which Mr. Stewart was assigned had<br />
been under investigation for drug diversion. On the basis <strong>of</strong><br />
an initiated internal complaint and preliminary investigation<br />
by LRH, Mr. Stewart was drug tested, which yielded a<br />
positive screen, as well as admissions <strong>of</strong> his involvement<br />
in drug diversion in an interview with law enforcement<br />
<strong>of</strong>ficers. Mr. Stewart was charged with 3 felony counts <strong>of</strong><br />
possession <strong>of</strong> a Schedule II controlled substance – Fentanyl<br />
Citrate. Mr. Stewart admitted to law enforcement <strong>of</strong>ficers<br />
to taking controlled substances and provided a statement<br />
regarding his history <strong>of</strong> addiction to Tramadol, which led to<br />
his diverting unused portions <strong>of</strong> controlled substance vials,<br />
including Morphine, Demerol, and Dilaudid. Mr. Stewart<br />
further admitted that his addiction was so strong that when<br />
there was not waste, he began diverting these opioids from<br />
the supply and using them, and that on August 25, 2009,<br />
he injected himself with Morphine, Dilaudid and Fentanyl.<br />
On April 13, 2010, two <strong>of</strong> three felony counts <strong>of</strong> possession<br />
<strong>of</strong> a controlled substance were dismissed and Mr. Stewart’s<br />
guilty plea for the remaining count was not accepted and<br />
entry <strong>of</strong> conviction was deferred pursuant to Wyo. Stat. §<br />
7-13-301, and he was placed on supervised probation for<br />
a period <strong>of</strong> five (5) years, subject to indicated terms and<br />
conditions. The terms <strong>of</strong> the Conditional License require<br />
Mr. Stewart to: (1) enroll in the <strong>Nurse</strong> Monitoring Program<br />
(“NMP”) for not less than sixty (60) months; (2) submit<br />
to random drug screens; (3) regularly attend AA or NA<br />
meetings, and submit documentation <strong>of</strong> such attendance<br />
to the NMP; (4) not sign out, dispense or administer<br />
controlled substances without direct supervision for at least<br />
twenty-four (24) months; (5) obtain a worksite monitor; (6)<br />
provide an annual report <strong>of</strong> his progression and education<br />
in recovery; (7) provide annual clinical substance abuse<br />
evaluations/assessments; (8) complete courses in ethics,<br />
critical thinking and pr<strong>of</strong>essional accountability; and (9)<br />
provide the terms <strong>of</strong> the Conditional License to present/<br />
future employers.<br />
JESSE TAYLOR<br />
CNA 18499<br />
REPRIMAND/SUSPENSION<br />
On or about February 1, <strong>2011</strong>, WSBN entered an Order<br />
<strong>of</strong> Default Judgment and an Order <strong>of</strong> Suspension and<br />
Reprimand against Jesse Taylor, CNA. Pursuant to WSBN<br />
Rules and Regulations, Chapter 8, Section 7(a), WSBN<br />
may enter an order <strong>of</strong> default based on the allegations in<br />
a petition and complaint against a respondent/licensee<br />
who fails to appear for a properly noticed hearing. Ms.<br />
Taylor failed to appear at a properly noticed disciplinary<br />
hearing. Accordingly, based on the petition and complaint<br />
which alleged violations <strong>of</strong> the <strong>Nurse</strong> Practice Act through<br />
Ms. Taylor’s actions related to sexual boundary violations<br />
and unpr<strong>of</strong>essional conduct while employed at <strong>Wyoming</strong><br />
<strong>State</strong> Hospital, WSBN reprimanded Ms. Taylor’s CNA<br />
certificate. Additionally, Ms. Taylor’s CNA certificate is<br />
suspended pending completion <strong>of</strong> <strong>Board</strong>-approved ethics<br />
and boundaries courses.<br />
CARLENE THAYER<br />
RN 19703<br />
REPRIMAND<br />
On or about February 1, <strong>2011</strong>, WSBN entered an Order<br />
<strong>of</strong> Default Judgment and an Order <strong>of</strong> Reprimand against<br />
Carlene Thayer, RN. Pursuant to WSBN Rules and<br />
Regulations, Chapter 8, Section 7(a), WSBN may enter an<br />
order <strong>of</strong> default based on the allegations in a petition and<br />
complaint against a respondent/licensee who fails to appear<br />
for a properly noticed hearing. Ms. Thayer failed to appear at<br />
a properly noticed disciplinary hearing. Accordingly, based<br />
on the petition and complaint which alleged violations <strong>of</strong><br />
the <strong>Nurse</strong> Practice Act through Ms. Thayer’s actions related<br />
to fraud and deceit, and unpr<strong>of</strong>essional conduct while<br />
employed at Western Medical Associates, PC, in Casper,<br />
<strong>Wyoming</strong>, WSBN reprimanded Ms. Thayer’s RN license.<br />
LEA THOMPSON<br />
RN 22822<br />
REVOCATION<br />
On or about February 1, <strong>2011</strong>, WSBN entered an Order <strong>of</strong><br />
Default Judgment and an Order <strong>of</strong> Revocation against Lea<br />
Thompson, RN. Pursuant to WSBN Rules and Regulations,<br />
Chapter 8, Section 7(a), WSBN may enter an order <strong>of</strong><br />
default based on the allegations in a petition and complaint<br />
against a respondent/licensee who fails to appear for a<br />
properly noticed hearing. Ms. Thompson failed to appear at<br />
a properly noticed disciplinary hearing. Accordingly, based<br />
on the petition and complaint which alleged violations <strong>of</strong><br />
the <strong>Nurse</strong> Practice Act through Ms. Thompson’s actions<br />
related to nurse license discipline in other jurisdictions,<br />
fraud and deceit/failure to disclose, and unpr<strong>of</strong>essional<br />
conduct, WSBN revoked Ms. Thompson’s RN license.<br />
KATRINA TOLBERT<br />
LPN 6890<br />
REVOCATION<br />
On or about February 1, <strong>2011</strong>, WSBN entered an Order<br />
<strong>of</strong> Default Judgment and an Order <strong>of</strong> Revocation against<br />
Katrina Tolbert, LPN. Pursuant to WSBN Rules and<br />
Regulations, Chapter 8, Section 7(a), WSBN may enter an<br />
order <strong>of</strong> default based on the allegations in a petition and<br />
complaint against a respondent/licensee who fails to appear<br />
for a properly noticed hearing. Ms. Tolbert failed to appear at<br />
a properly noticed disciplinary hearing. Accordingly, based<br />
on the petition and complaint which alleged violations <strong>of</strong><br />
the <strong>Nurse</strong> Practice Act through Ms. Tolbert’s actions<br />
related to drug diversion and unpr<strong>of</strong>essional conduct while<br />
employed at Valley View Rehabilitation and Care Center<br />
in Saratoga, <strong>Wyoming</strong>, WSBN revoked Ms. Tolbert’s LPN<br />
license.<br />
KORTNEY TOWNS<br />
CNA 21290<br />
REVOCATION<br />
On or about February 4, <strong>2011</strong>, WSBN entered an Order<br />
<strong>of</strong> Default Judgment and an Order <strong>of</strong> Revocation against<br />
Kortney Towns, CNA. Pursuant to WSBN Rules and<br />
Regulations, Chapter 8, Section 7(a), WSBN may enter<br />
an order <strong>of</strong> default based on the allegations in a petition<br />
and complaint against a respondent/licensee who fails<br />
to appear for a properly noticed hearing. Ms. Towns<br />
failed to appear at a properly noticed disciplinary hearing.<br />
Accordingly, based on the petition and complaint which<br />
alleged violations <strong>of</strong> the <strong>Nurse</strong> Practice Act through Ms.<br />
Towns’ actions related to abandonment and unpr<strong>of</strong>essional<br />
conduct while employed at the <strong>Wyoming</strong> Medical Center,<br />
in Casper, <strong>Wyoming</strong>, WSBN revoked Ms. Towns’ CNA<br />
certificate.<br />
TRINA WATERMAN<br />
RN 26297<br />
REVOCATION<br />
On or about November 16, 2010, WSBN entered an Order<br />
<strong>of</strong> Default Judgment and an Order <strong>of</strong> Revocation against<br />
Trina Waterman, RN. Pursuant to WSBN Rules and<br />
Regulations, Chapter 8, Section 7(a), WSBN may enter<br />
an order <strong>of</strong> default based on the allegations in a petition<br />
and complaint against a respondent/licensee who fails to<br />
appear for a properly noticed hearing. Ms. Waterman<br />
failed to appear at a properly noticed disciplinary hearing.<br />
Accordingly, based on the petition and complaint which<br />
alleged violations <strong>of</strong> the <strong>Nurse</strong> Practice Act through Ms.<br />
Waterman’s actions related to violation <strong>of</strong> the Medication<br />
Administration Policy and improper wasting practices/drug<br />
diversion while employed at <strong>Wyoming</strong> Medical Center in<br />
Casper, <strong>Wyoming</strong>, WSBN revoked Ms. Waterman’s RN<br />
license.<br />
JAMEY LEA WEICKUM<br />
CNA 4929<br />
LETTER OF REPRIMAND<br />
Jamey Lea Weickum, CNA, entered into a Settlement<br />
Agreement, Stipulation and Order for Letter <strong>of</strong> Reprimand<br />
on December 11, 2010. In July 2010, a complaint was<br />
initiated based upon information obtained following Ms.<br />
Weickum’s application for renewal <strong>of</strong> her CNA certificate,<br />
28 <strong>Wyoming</strong> <strong>Nurse</strong> <strong>Reporter</strong>
which information was not disclosed in such application.<br />
Ms. Weickum provided negative answers on her application<br />
to the question whether in the past two years she had been<br />
“charged, arrested, cited, or convicted for any criminal<br />
<strong>of</strong>fense (including DUI).” However, an investigation<br />
disclosed that Ms. Weickum entered a plea <strong>of</strong> nolo<br />
contendere to a felony charge <strong>of</strong> “Accessory after the Fact,”<br />
pursuant to WYO. STAT. § 6-50202(a) & (b)(ii)(B),<br />
which was deferred pursuant to WYO. STAT. § 7-13-301.<br />
Such conduct is alleged to have failed to conform to nursing<br />
standards and constitute unpr<strong>of</strong>essional conduct. WSBN<br />
agreed to issue a Letter <strong>of</strong> Reprimand to Ms. Weickum’s<br />
conduct and, additionally, require completion <strong>of</strong> courses in<br />
ethics and pr<strong>of</strong>essional accountability.<br />
CRISTINA WILLIAMS<br />
RN 26995<br />
REVOCATION<br />
On or about November 16, 2010, WSBN entered an Order<br />
<strong>of</strong> Default Judgment and an Order <strong>of</strong> Revocation against<br />
Christina Williams, RN. Pursuant to WSBN Rules and<br />
Regulations, Chapter 8, Section 7(a), WSBN may enter<br />
an order <strong>of</strong> default based on the allegations in a petition<br />
and complaint against a respondent/licensee who fails<br />
to appear for a properly noticed hearing. Ms. Williams<br />
failed to appear at a properly noticed disciplinary hearing.<br />
Accordingly, based on the petition and complaint which<br />
alleged violations <strong>of</strong> the <strong>Nurse</strong> Practice Act through Ms.<br />
Williams’ actions: (1) reported by the Texas <strong>State</strong> <strong>Board</strong> <strong>of</strong><br />
<strong>Nursing</strong> in an Agreed Order dated June 3, 2009, indicating<br />
numerous instances <strong>of</strong> drug diversion, falling asleep on<br />
duty, presenting improper patient care, misappropriation<br />
<strong>of</strong> narcotic medication for personal use, and a positive<br />
drug screen for opiates, and chemical dependency; and<br />
(2) <strong>of</strong> providing false information on her application for<br />
a <strong>Wyoming</strong> registered nurse license, WSBN revoked Ms.<br />
Williams’ RN license.<br />
Denials <strong>of</strong> Applicants Seeking Licensure or Certification<br />
The <strong>Nurse</strong> Practice Act, 33-21-146 identifies the following reasons that an application may be denied:<br />
“(a) The board <strong>of</strong> nursing may refuse to issue or renew, or may suspend or revoke<br />
the license, certificate or temporary permit <strong>of</strong> any person, or to otherwise discipline a<br />
licensee, upon pro<strong>of</strong> that the person:<br />
(i) Has engaged in any act inconsistent with uniform and reasonable standards <strong>of</strong><br />
nursing practice as defined by board rules and regulations;<br />
(ii) Has been found guilty by a court, has entered an Alford plea or has entered a plea<br />
<strong>of</strong> nolo contendere to a misdemeanor or felony that relates adversely to the practice <strong>of</strong><br />
nursing or to the ability to practice nursing;<br />
(iii) Has practiced fraud or deceit:<br />
(A) In procuring or attempting to procure a license to practice nursing;<br />
(B) In filing or reporting any health care information, including but not limited to client<br />
documentation, agency records or other essential health documents;<br />
(C) In signing any report or record as a registered nurse or as a licensed practical<br />
nurse;<br />
(D) In representing authority to practice nursing; or<br />
(E) In submitting any information or record to the board. (iv) Is unfit or incompetent<br />
to practice nursing by reason <strong>of</strong> negligence, habits or other causes including but not<br />
limited to:<br />
(A) Being unable to practice nursing with reasonable skill and safety to patients by<br />
reason <strong>of</strong> physical or mental disability, or use <strong>of</strong> drugs, narcotics, chemicals or any other<br />
mind-altering material; or<br />
(B) Performance <strong>of</strong> unsafe nursing practice or failure to conform to the essential<br />
standards <strong>of</strong> acceptable and prevailing nursing practice, in which case actual injury need<br />
not be established.<br />
(v) Has engaged in any unauthorized possession or unauthorized use <strong>of</strong> a controlled<br />
substance as defined in the <strong>Wyoming</strong> Controlled Substances Act [§§ 35-7-1001 through<br />
35-7-1057];<br />
(vi) Has had a license to practice nursing or to practice in another health care discipline<br />
in another jurisdiction, territory or possession <strong>of</strong> the United <strong>State</strong>s denied, revoked,<br />
suspended or otherwise restricted;<br />
(vii) Has practiced nursing within this state without a valid current license or temporary<br />
permit or as otherwise permitted under this act;<br />
(viii) Has knowingly and willfully failed to report to the board any violation <strong>of</strong> this act<br />
or <strong>of</strong> board rules and regulations;<br />
(ix) Has been found by the board to have violated any <strong>of</strong> the provisions <strong>of</strong> this act or <strong>of</strong><br />
board rules and regulations; or<br />
(x) Has knowingly engaged in an act which the licensee knew was beyond the scope <strong>of</strong><br />
the individual’s nursing practice prior to committing the act, or performed acts without<br />
sufficient education, knowledge, or ability to apply nursing principles and skills; or<br />
(xi) Has failed to submit to a mental, physical or medical competency examination<br />
following a proper request by the board made pursuant to board rules and regulations and<br />
the <strong>Wyoming</strong> Administrative Procedure Act.<br />
(b) Upon receipt from the department <strong>of</strong> family services <strong>of</strong> a certified copy <strong>of</strong> an order<br />
from a court to withhold, suspend or otherwise restrict a license issued by the board, the<br />
board shall notify the party named in the court order <strong>of</strong> the withholding, suspension<br />
or restriction <strong>of</strong> the license in accordance with the terms <strong>of</strong> the court order. No appeal<br />
under the <strong>Wyoming</strong> Administrative Procedure Act shall be allowed for a license<br />
withheld, suspended or restricted under this subsection” (pg 12-13 <strong>of</strong> 18).<br />
DENIALS OF APPLICANTS SEEKING LICENSURE OR CERTIFICATION<br />
BRITTANIA STONER CNA APPLICANT DISMISSAL<br />
On or about February 1, <strong>2011</strong>, WSBN entered an Order <strong>of</strong> Dismissal against Brittania Stoner, CNA Applicant. Ms. Stoner’s application for certification as a CNA was denied<br />
by WSBN application review committee based upon information indicating a criminal history. Ms. Stoner notified WSBN she no longer wished to pursue her request for a<br />
hearing. The preliminary denial is confirmed as a final denial <strong>of</strong> Ms. Stoner’s application, and the proceedings related thereto have been dismissed for failure to prosecute.<br />
AMANDA STEPHENS CNA APPLICANT DISMISSAL<br />
On or about February 1, <strong>2011</strong>, WSBN entered an Order <strong>of</strong> Dismissal against Amanda Stephens, CNA Applicant. Ms. Stephens’ application for certification as a CNA was<br />
denied by WSBN application review committee based upon information indicating a criminal history. Subsequent to filing her request for a hearing, Ms. Stephens failed to<br />
appear at scheduled pre-hearing conferences or other pursue her request for a hearing. The preliminary denial is confirmed as a final denial <strong>of</strong> Ms. Stephens’ application, and<br />
the proceedings related thereto have been dismissed for failure to prosecute.<br />
WILLIAM CARSON<br />
CNA APPLICANT<br />
Mr. Carson’s application for certification as a CNA was denied by WSBN application review committee based upon information indicating a criminal history and impairment<br />
issues.<br />
KASSIDY FALKENBURG<br />
CNA APPLICANT<br />
Ms. Falkenburg’s application for certification as a CNA was denied by WSBN application review committee based upon information indicating a criminal history and related<br />
impairment issues.<br />
HOLLIE GUERRERo<br />
CNA APPLICANT<br />
Ms. Guerrero’s application for certification as a CNA was denied by WSBN application review committee due based upon information indicating a criminal history and related<br />
impairment issues.<br />
<strong>Wyoming</strong> <strong>Nurse</strong> <strong>Reporter</strong> 29
Gems Worth Sharing...<br />
Pearls <strong>of</strong> Practice<br />
Everyone has a nursing secret…..a special<br />
method <strong>of</strong> doing something they learned<br />
along the way from another nurse, a mentor,<br />
a clinical instructor or by trial and error. It<br />
might be evidence based practice or an old<br />
“nurses” tale, but if it works and makes things<br />
easier for you or your patient the WSBN is<br />
interested in hearing from YOU. Any CNA,<br />
LPN, RN, or APRN can submit. Share your<br />
experience or creativity. Send in your Pearls<br />
<strong>of</strong> Practice to wynursing@state.wy.us and if<br />
selected for publication you will receive a<br />
special gift.<br />
This issue we feature Pearls from the<br />
<strong>Board</strong>. We asked each board member to<br />
submit their favorite Pearls.<br />
NG tubes. Before inserting a salem NG,<br />
try soaking it briefly in some very warm water.<br />
This makes the tube s<strong>of</strong>ter and more flexible<br />
and better able to snake through the sinuses<br />
without tissue damage. Just don’t get it so<br />
hot that it burns the nasal tissue.<br />
Having trouble getting an NG to go down<br />
the esophagus instead <strong>of</strong> the trachea? Just as<br />
you use the natural curve <strong>of</strong> the tubing to go<br />
through the sinus, when you pass it through<br />
the back <strong>of</strong> the throat twist the tube 180<br />
degrees so the natural curve <strong>of</strong> the tubing is<br />
posterior. That will keep the tip <strong>of</strong> the NG<br />
away from the windpipe and right down into<br />
the stomach. (X-ray is still gold standard for<br />
verifying placement).<br />
When you enter a patient’s room for<br />
the first time, take a moment to establish a<br />
personal connection before launching into<br />
your assessment routine. Try to establish eye<br />
level communication rather than standing<br />
over the patient. Sit on a stool or the edge<br />
<strong>of</strong> the bed when you introduce yourself and<br />
ask a few questions. This will humanize your<br />
further interactions and help establish trust.<br />
Remember your ABCs when interpreting<br />
a chest X-ray.<br />
A= airway (is the ET tube in the correct<br />
position, any deviations <strong>of</strong> airway not related<br />
to positioning)<br />
B= bones (are the clavicles intact, correct<br />
number <strong>of</strong> ribs, etc)<br />
C= cardiac (what is the shape <strong>of</strong> the heart)<br />
D= diaphragm (what’s the level, is it present<br />
all the way across)<br />
E/F= Equal lung Fields (are the fields<br />
homogenous, hyperinflation vs.<br />
hypoinflation)<br />
G= gas pattern <strong>of</strong> bowels (is it present all the<br />
way to colon, any abnormal dilation)<br />
H= hardware (central lines and leads, is the<br />
NG tube in the correct position)<br />
NEXT ISSUE: What are your favorite<br />
mnemonics?<br />
1/2<br />
Director <strong>of</strong> <strong>Nursing</strong><br />
5K Sign-On Bonus (Guidelines Apply)<br />
Montana NURSE<br />
O F F I C I A L P U B L I C A T I O N O F T H E M O N T A N A S T A T E B O A R D O F N U R S E S<br />
Worland Healthcare & Rehab, a FiveStar skilled nursing &<br />
rehab community in Worland, WY, has an opportunity for<br />
an experienced DON (2+yrs). WY RN license required<br />
with knowledge <strong>of</strong> state, federal regulations.<br />
Please apply online at www.5sqc.com EOE<br />
Edition 1<br />
Nu<br />
The<br />
Reach every n<br />
Attention:<br />
Your <strong>Nursing</strong> License<br />
Expires on Dec. 31, 2010<br />
1-<br />
25% Relocation/Recruitment Bonus<br />
<strong>Nurse</strong> Manager (OR) at<br />
VA Montana Health System<br />
This is a FT Permanent opportunity in<br />
beautiful Helena MT. Primarily M-F, day shift.<br />
Great salary, benefits, and career path.<br />
Apply at www.usajobs.gov or contact<br />
Human Resources at (406) 447-7933<br />
<strong>Nursing</strong> Program<br />
Administrators<br />
Recruit <strong>Nursing</strong><br />
Faculty Here<br />
Victor Horne<br />
(800) 561-4686 ext. 114<br />
“If you have the courage to ask,<br />
I have the courage to answer.”<br />
The Color <strong>of</strong> SunlighT<br />
A rural nurse’s story <strong>of</strong> unconditional<br />
love and acceptance, and a factual<br />
account <strong>of</strong> a relationship trancending<br />
the barriers <strong>of</strong> class, gender and<br />
disability.<br />
by Michelle AlexAnder, rn And<br />
Michelle diAne rose<br />
Please visit www.tcosl.com to order.<br />
R<br />
N<br />
re<br />
n<br />
vho<br />
30 <strong>Wyoming</strong> <strong>Nurse</strong> <strong>Reporter</strong>
Breathe new life into your career.<br />
THERE IS OPPORTUNITY IN THE AIR.<br />
At Banner Health’s <strong>Wyoming</strong> facilities, we understand the vital role our nurses play in our success.<br />
We provide an environment that is rich in opportunities, <strong>of</strong>fers growth and development and is<br />
equipped with the latest in life-saving technology. We are committed to making a difference in<br />
our employees’ lives so they can make a difference in the lives <strong>of</strong> others.<br />
<strong>Nursing</strong> Opportunities Available<br />
Community Hospital and Goshen Care Center – Torrington<br />
Platte County Memorial Hospital – Wheatland<br />
Washakie Medical Center – Worland<br />
Breathe new life into your career. Call 307-534-7157 or visit:<br />
www.BannerHealth.com<br />
Banner Health has been named as a Top 10 Health System in the U.S.<br />
based on clinical performance according to Thomson Reuters.<br />
Connect with Banner Health Careers:<br />
EOE/AA Banner Health supports a drug-free work environment.
<strong>Wyoming</strong> <strong>State</strong> <strong>Board</strong> <strong>of</strong> <strong>Nursing</strong><br />
1810 Pioneer Ave.<br />
Cheyenne, <strong>Wyoming</strong> 82002<br />
Presorted Standard<br />
U.S. Postage Paid<br />
Little Rock, AR<br />
Permit No. 1884<br />
TO OUR STATE’S WONDERFUL NURSING COMMUNITY:<br />
THANKS FOR YOUR SERVICE<br />
AND ALL THAT YOU DO!<br />
Remember, wherever you work or volunteer as a nurse,<br />
you can speak up about colorectal cancer.<br />
Colorectal Cancer is the only cancer that is preventable<br />
with screening!<br />
Help us spread the word about prevention.<br />
Save a life - one colon at a time!<br />
Letha Buller, RN,<br />
Patient Care Coordinator<br />
Downtown Clinic, Laramie, WY<br />
The <strong>Wyoming</strong> Colorectal Cancer<br />
Screening Program would like<br />
to express gratitude and<br />
admiration for the state’s free<br />
clinic nurses. You Make This<br />
World A Better Place!<br />
Not pictured:<br />
Teton Free Clinic<br />
Jackson, <strong>Wyoming</strong><br />
Margie Schauland, RN<br />
Heart Mountain Volunteer Medical Clinic<br />
Cody, <strong>Wyoming</strong><br />
Marty Kethman, LPN and Cyndy Rankin RN<br />
Free Clinic <strong>of</strong> Sheridan County, Sheridan, WY<br />
TO APPLY FOR A FREE COLONOSCOPY<br />
Call 1-866-205-5292<br />
or visit https://ccedp.health.wyo.gov<br />
Sadie Hockenhull, RN<br />
Heart Mountain Volunteer Medical Clinic<br />
Powell, WY