- Page 2:
This page intentionally left blank
- Page 8:
Introduction to Fungi JohnWebster U
- Page 12:
To Philip M. Booth
- Page 18:
viii CONTENTS Chapter 6 Chytridiomy
- Page 22:
x CONTENTS 15.4 Rhytismataceae 440
- Page 28:
Preface to the first edition There
- Page 36:
Preface to the third edition Major
- Page 40:
Acknowledgements We are indebted to
- Page 46:
2 INTRODUCTION With photosynthetic
- Page 50:
4 INTRODUCTION Fig1.3 Transmission
- Page 54:
6 INTRODUCTION Fig1.5 Structural fo
- Page 58:
8 INTRODUCTION of mushroom-type fru
- Page 62:
10 INTRODUCTION Fig1.8 Diagrammatic
- Page 66:
12 INTRODUCTION Fig1.9 Tubular cont
- Page 70:
14 INTRODUCTION Fig1.11 Ion fluxes
- Page 74:
16 INTRODUCTION grow alongside each
- Page 78:
18 INTRODUCTION Fig1.15 Rhizomorphs
- Page 82:
20 INTRODUCTION carbon/nitrogen rat
- Page 86:
22 INTRODUCTION well shown by the X
- Page 90:
24 INTRODUCTION Fig1.17 Zoospore ty
- Page 94:
26 INTRODUCTION genera, e.g. Hypocr
- Page 98:
28 INTRODUCTION creating a momentum
- Page 102:
30 INTRODUCTION Fig1.22 Chlamydospo
- Page 106:
32 INTRODUCTION As mentioned on p.
- Page 110:
34 INTRODUCTION the cell wall (Tabl
- Page 114:
36 INTRODUCTION Fig1.24 The spatial
- Page 118:
38 INTRODUCTION Table1.2. The class
- Page 122:
2 Protozoa: Myxomycota (slime mould
- Page 126:
42 PROTOZOA: MYXOMYCOTA (SLIME MOUL
- Page 130:
44 PROTOZOA: MYXOMYCOTA (SLIME MOUL
- Page 134:
46 PROTOZOA: MYXOMYCOTA (SLIME MOUL
- Page 138:
48 PROTOZOA: MYXOMYCOTA (SLIME MOUL
- Page 142:
50 PROTOZOA: MYXOMYCOTA (SLIME MOUL
- Page 146:
52 PROTOZOA: MYXOMYCOTA (SLIME MOUL
- Page 150:
3 Protozoa: Plasmodiophoromycota 3.
- Page 154:
56 PROTOZOA: PLASMODIOPHOROMYCOTA F
- Page 158:
58 PROTOZOA: PLASMODIOPHOROMYCOTA F
- Page 162:
60 PROTOZOA: PLASMODIOPHOROMYCOTA p
- Page 166:
62 PROTOZOA: PLASMODIOPHOROMYCOTA I
- Page 170:
64 PROTOZOA: PLASMODIOPHOROMYCOTA a
- Page 174:
66 PROTOZOA: PLASMODIOPHOROMYCOTA a
- Page 178:
68 STRAMINIPILA: MINOR FUNGAL PHYLA
- Page 182:
70 STRAMINIPILA: MINOR FUNGAL PHYLA
- Page 186:
72 STRAMINIPILA: MINOR FUNGAL PHYLA
- Page 190:
74 STRAMINIPILA: MINOR FUNGAL PHYLA
- Page 194:
76 STRAMINIPILA: OOMYCOTA Fig 5.1 A
- Page 198:
78 STRAMINIPILA: OOMYCOTA Fig 5.3 L
- Page 202:
80 STRAMINIPILA: OOMYCOTA Table 5.1
- Page 206:
82 STRAMINIPILA: OOMYCOTA strains o
- Page 210:
84 STRAMINIPILA: OOMYCOTA Fig 5.5 S
- Page 214:
86 STRAMINIPILA: OOMYCOTA The oogon
- Page 218:
88 STRAMINIPILA: OOMYCOTA Fig 5.9 A
- Page 222:
90 STRAMINIPILA: OOMYCOTA was the f
- Page 226:
92 STRAMINIPILA: OOMYCOTA Fig 5.12
- Page 230:
94 STRAMINIPILA: OOMYCOTA Fig 5.14
- Page 234:
96 STRAMINIPILA: OOMYCOTA that desc
- Page 238:
98 STRAMINIPILA: OOMYCOTA Fig 5.16
- Page 242:
100 STRAMINIPILA: OOMYCOTA In some
- Page 246:
102 STRAMINIPILA: OOMYCOTA haploid
- Page 250:
104 STRAMINIPILA: OOMYCOTA Fig 5.20
- Page 254:
106 STRAMINIPILA: OOMYCOTA Fig 5.22
- Page 258:
108 STRAMINIPILA: OOMYCOTA Fig 5.24
- Page 262:
110 STRAMINIPILA: OOMYCOTA Fig 5.26
- Page 266:
112 STRAMINIPILA: OOMYCOTA firmly t
- Page 270:
114 STRAMINIPILA: OOMYCOTA present,
- Page 274:
116 STRAMINIPILA: OOMYCOTA convinci
- Page 278:
118 STRAMINIPILA: OOMYCOTA Fig 5.29
- Page 282:
120 STRAMINIPILA: OOMYCOTA and pars
- Page 286:
122 STRAMINIPILA: OOMYCOTA sterigma
- Page 290:
124 STRAMINIPILA: OOMYCOTA The spor
- Page 294:
126 STRAMINIPILA: OOMYCOTA Fig 5.35
- Page 298:
128 CHYTRIDIOMYCOTA N-acetylglucosa
- Page 302:
130 CHY TRIDIOMYCOTA Fig 6.2 Flagel
- Page 306:
132 CHY TRIDIOMYCOTA the reproducti
- Page 310:
134 CHY TRIDIOMYCOTA Table 6.1. Ord
- Page 314:
136 CHY TRIDIOMYCOTA Fig 6.7 Synchy
- Page 318:
138 CHY TRIDIOMYCOTA already been d
- Page 322:
140 CHYTRIDIOMYCOTA Fig 6.9 Synchyt
- Page 326:
142 CHYTRIDIOMYCOTA Canter & Jawors
- Page 330:
144 CHYTRIDIOMYCOTA exit tube which
- Page 334:
146 CHYTRIDIOMYCOTA some of the spe
- Page 338:
148 CHYTRIDIOMYCOTA distinguished v
- Page 342:
150 CHYTRIDIOMYCOTA Fig 6.17 Scanni
- Page 346:
152 CHYTRIDIOMYCOTA Fig 6.18 Neocal
- Page 350:
154 CHYTRIDIOMYCOTA Fig 6.19 Blasto
- Page 354:
156 CHYTRIDIOMYCOTA and if dried sa
- Page 358:
158 CHYTRIDIOMYCOTA Fig 6.21 Life c
- Page 362:
160 CHYTRIDIOMYCOTA both thin-walle
- Page 366:
162 CHYTRIDIOMYCOTA pathways. There
- Page 370:
164 CHYTRIDIOMYCOTA Fig 6.25 Monobl
- Page 374:
166 ZYGOMYCOTA Fig 7.1 Recent phylo
- Page 378:
168 ZYGOMYCOTA Fig 7.3 Mucor rouxii
- Page 382:
170 ZYGOMYCOTA Fig 7.5 Sporangiopho
- Page 386:
172 ZYGOMYCOTA The columella is cur
- Page 390:
174 ZYGOMYCOTA Fig 7.8 Phycomyces b
- Page 394:
176 ZYGOMYCOTA Phycomyces, after ar
- Page 398:
178 ZYGOMYCOTA Fig 7.11 Development
- Page 402:
180 ZYGOMYCOTA Fig 7.12 Life cycle
- Page 406:
182 ZYGOMYCOTA Fig 7.14 Mucor racem
- Page 410:
184 ZYGOMYCOTA that many workers co
- Page 414:
186 ZYGOMYCOTA Fig 7.18 Phycomyces
- Page 418:
188 ZYGOMYCOTA the sporangiophore o
- Page 422:
190 ZYGOMYCOTA makes contact with a
- Page 426:
192 ZYGOMYCOTA Fig 7.24 Thamnidium
- Page 430:
194 ZYGOMYCOTA (i.e. striate) wall
- Page 434:
196 ZYGOMYCOTA sporangiospores, eac
- Page 438:
198 ZYGOMYCOTA Fig 7.30 Mortierella
- Page 442:
200 ZYGOMYCOTA Fig 7.32 Mortierella
- Page 446:
202 ZYGOMYCOTA of germ tubes toward
- Page 450:
204 ZYGOMYCOTA Fig 7.34 Basidiobolu
- Page 454:
206 ZYGOMYCOTA Fig 7.36 Basidiobolu
- Page 458:
208 ZYGOMYCOTA Fig 7.37 The eventfu
- Page 462:
210 ZYGOMYCOTA Fig 7.39 Conidiobolu
- Page 466:
212 ZYGOMYCOTA Fig 7.4 0 Carcass of
- Page 470:
214 ZYGOMYCOTA develop. These are t
- Page 474:
216 ZYGOMYCOTA apparent (Fig. 7.43e
- Page 478:
218 ZYGOMYCOTA mycorrhiza (AM). The
- Page 482:
220 ZYGOMYCOTA Fig 7.4 6 Vesicular
- Page 486:
222 ZYGOMYCOTA interest (Allen, 199
- Page 490:
224 ZYGOMYCOTA Fig 7.47 Harpella me
- Page 494:
8 Ascomycota (ascomycetes) 8.1 Intr
- Page 498:
228 ASCOMYCOTA (ASCOMYCETES) Fig 8.
- Page 502:
230 ASCOMYCOTA (ASCOMYCETES) wall a
- Page 506:
232 ASCOMYCOTA (ASCOMYCETES) Fig 8.
- Page 510:
234 ASCOMYCOTA (ASCOMYCETES) Fig 8.
- Page 514:
236 ASCOMYCOTA (ASCOMYCETES) 8.6 De
- Page 518:
238 ASCOMYCOTA (ASCOMYCETES) Fig 8.
- Page 522:
240 ASCOMYCOTA (ASCOMYCETES) Fig 8.
- Page 526:
242 ASCOMYCOTA (ASCOMYCETES) Fig 8.
- Page 530:
244 ASCOMYCOTA (ASCOMYCETES) Fig 8.
- Page 534:
246 ASCOMYCOTA (ASCOMYCETES) formin
- Page 538:
248 ASCOMYCOTA (ASCOMYCETES) Fig 8.
- Page 542:
9 Archiascomycetes 9.1 Introduction
- Page 546:
252 ARCHIASCOMYCETES swollen tips w
- Page 550:
254 ARCHIASCOMYCETES as saprotrophi
- Page 554:
256 ARCHIASCOMYCETES In the followi
- Page 558:
258 ARCHIASCOMYCETES Fig 9.6 The cy
- Page 562:
260 ARCHIASCOMYCETES There are many
- Page 566:
262 HEMIASCOMYCETES (Yarrow, 1998;
- Page 570:
264 HEMIASCOMYCETES organelles and
- Page 574:
266 HEMIASCOMYCETES Fig10.3 Sacchar
- Page 578:
268 HEMIASCOMYCETES Fig10.5 The str
- Page 582:
270 HEMIASCOMYCETES template is una
- Page 586:
272 HEMIASCOMYCETES Following separ
- Page 590:
274 HEMIASCOMYCETES in habitats whi
- Page 594:
276 HEMIASCOMYCETES is extracted ra
- Page 598:
278 HEMIASCOMYCETES Fig10.8 Example
- Page 602:
280 HEMIASCOMYCETES The azole-type
- Page 606:
282 HEMIASCOMYCETES form septa and
- Page 610:
284 HEMIASCOMYCETES Fig10.13 Eremot
- Page 614:
286 PLECTOMYCETES Table 11.1. Class
- Page 618:
288 PLECTOMYCETES Fig11.2 Ascosphae
- Page 622:
290 PLECTOMYCETES Fig11.4 Onygena.
- Page 626:
292 PLECTOMYCETES Histoplasma capsu
- Page 630:
294 PLECTOMYCETES Fig11.5 Ctenomyce
- Page 634:
296 PLECTOMYCETES Fig11.8 Gymnoascu
- Page 638:
298 PLECTOMYCETES they are xerophil
- Page 642:
300 PLECTOMYCETES Fig11.12 Phialoco
- Page 646:
302 PLECTOMYCETES Fig11.13 Conidiop
- Page 650:
304 PLECTOMYCETES Fig11.14 Importan
- Page 654:
306 PLECTOMYCETES Patulin Although
- Page 658:
308 PLECTOMYCETES unicellular chlam
- Page 662:
310 PLECTOMYCETES of the nest-like
- Page 666:
312 PLECTOMYCETES food spoilage (e.
- Page 670:
314 PLECTOMYCETES litter layer unde
- Page 674:
316 HYMENOASCOMYCETES: PYRENOMYCETE
- Page 678:
318 HYMENOASCOMYCETES: PYRENOMYCETE
- Page 682:
320 HYMENOASCOMYCETES: PYRENOMYCETE
- Page 686:
322 HYMENOASCOMYCETES: PYRENOMYCETE
- Page 690:
324 HYMENOASCOMYCETES: PYRENOMYCETE
- Page 694:
326 HYMENOASCOMYCETES: PYRENOMYCETE
- Page 698:
328 HYMENOASCOMYCETES: PYRENOMYCETE
- Page 702:
330 HYMENOASCOMYCETES: PYRENOMYCETE
- Page 706:
332 HYMENOASCOMYCETES: PYRENOMYCETE
- Page 710:
334 HYMENOASCOMYCETES: PYRENOMYCETE
- Page 714:
336 HYMENOASCOMYCETES: PYRENOMYCETE
- Page 718:
338 HYMENOASCOMYCETES: PYRENOMYCETE
- Page 722:
340 HYMENOASCOMYCETES: PYRENOMYCETE
- Page 726:
342 HYMENOASCOMYCETES: PYRENOMYCETE
- Page 730:
344 HYMENOASCOMYCETES: PYRENOMYCETE
- Page 734:
346 HYMENOASCOMYCETES: PYRENOMYCETE
- Page 738:
348 HYMENOASCOMYCETES: PYRENOMYCETE
- Page 742:
350 HYMENOASCOMYCETES: PYRENOMYCETE
- Page 746:
352 HYMENOASCOMYCETES: PYRENOMYCETE
- Page 750:
354 HYMENOASCOMYCETES: PYRENOMYCETE
- Page 754:
356 HYMENOASCOMYCETES: PYRENOMYCETE
- Page 758:
358 HYMENOASCOMYCETES: PYRENOMYCETE
- Page 762:
360 HYMENOASCOMYCETES: PYRENOMYCETE
- Page 766:
362 HYMENOASCOMYCETES: PYRENOMYCETE
- Page 770:
364 HYMENOASCOMYCETES: PYRENOMYCETE
- Page 774:
366 HYMENOASCOMYCETES: PYRENOMYCETE
- Page 778:
368 HYMENOASCOMYCETES: PYRENOMYCETE
- Page 782:
370 HYMENOASCOMYCETES: PYRENOMYCETE
- Page 786:
372 HYMENOASCOMYCETES: PYRENOMYCETE
- Page 790:
374 HYMENOASCOMYCETES: PYRENOMYCETE
- Page 794:
376 HYMENOASCOMYCETES: PYRENOMYCETE
- Page 798:
378 HYMENOASCOMYCETES: PYRENOMYCETE
- Page 802:
380 HYMENOASCOMYCETES: PYRENOMYCETE
- Page 806:
382 HYMENOASCOMYCETES: PYRENOMYCETE
- Page 810:
384 HYMENOASCOMYCETES: PYRENOMYCETE
- Page 814:
386 HYMENOASCOMYCETES: PYRENOMYCETE
- Page 818:
388 HYMENOASCOMYCETES: PYRENOMYCETE
- Page 822:
13 Hymenoascomycetes: Erysiphales 1
- Page 826:
392 HYMENOASCOMYCETES: ERYSIPHALES
- Page 830:
394 HYMENOASCOMYCETES: ERYSIPHALES
- Page 834:
396 HYMENOASCOMYCETES: ERYSIPHALES
- Page 838:
398 HYMENOASCOMYCETES: ERYSIPHALES
- Page 842:
400 HYMENOASCOMYCETES: ERYSIPHALES
- Page 846:
402 HYMENOASCOMYCETES: ERYSIPHALES
- Page 850:
404 HYMENOASCOMYCETES: ERYSIPHALES
- Page 854:
406 HYMENOASCOMYCETES: ERYSIPHALES
- Page 858:
408 HYMENOASCOMYCETES: ERYSIPHALES
- Page 862:
410 HYMENOASCOMYCETES: ERYSIPHALES
- Page 866:
412 HYMENOASCOMYCETES: ERYSIPHALES
- Page 870:
Plate 2 Oomycota. (a) Salmon infect
- Page 874:
Plate 4 Archiascomycetes (a c) and
- Page 878:
Plate 6 Apothecia of operculate dis
- Page 882:
Plate 8 Thalli of lichens. (a) The
- Page 886:
Plate10 Fruitbodies of Homobasidiom
- Page 890:
Plate12 Urediniomycetes (a g) and U
- Page 894:
14 Hymenoascomycetes: Pezizales (op
- Page 898:
416 HYMENOASCOMYCETES: PEZIZALES (O
- Page 902:
418 HYMENOASCOMYCETES: PEZIZALES (O
- Page 906:
420 HYMENOASCOMYCETES: PEZIZALES (O
- Page 910:
422 HYMENOASCOMYCETES: PEZIZALES (O
- Page 914:
424 HYMENOASCOMYCETES: PEZIZALES (O
- Page 918:
426 HYMENOASCOMYCETES: PEZIZALES (O
- Page 922:
428 HYMENOASCOMYCETES: PEZIZALES (O
- Page 926:
430 HYMENOASCOMYCETES: HELOTIALES (
- Page 930:
432 HYMENOASCOMYCETES: HELOTIALES (
- Page 934:
434 HYMENOASCOMYCETES: HELOTIALES (
- Page 938:
436 HYMENOASCOMYCETES: HELOTIALES (
- Page 942:
438 HYMENOASCOMYCETES: HELOTIALES (
- Page 946:
440 HYMENOASCOMYCETES: HELOTIALES (
- Page 950:
442 HYMENOASCOMYCETES: HELOTIALES (
- Page 954:
444 HYMENOASCOMYCETES: HELOTIALES (
- Page 958:
16 Lichenized fungi (chiefly Hymeno
- Page 962:
448 LICHENIZED FUNGI (CHIEFLY HYMEN
- Page 966:
450 LICHENIZED FUNGI (CHIEFLY HYMEN
- Page 970:
452 LICHENIZED FUNGI (CHIEFLY HYMEN
- Page 974:
454 LICHENIZED FUNGI (CHIEFLY HYMEN
- Page 978:
456 LICHENIZED FUNGI (CHIEFLY HYMEN
- Page 982:
458 LICHENIZED FUNGI (CHIEFLY HYMEN
- Page 986:
460 LOCULOASCOMYCETES Fig17.1 Sexua
- Page 990:
462 LOCULOASCOMYCETES Fig17.2 Lepto
- Page 994:
464 LOCULOASCOMYCETES Fig17.4 Stago
- Page 998:
466 LOCULOASCOMYCETES Fig17.7 Phoma
- Page 1002:
468 LOCULOASCOMYCETES Fig17.9 Pleos
- Page 1006:
470 LOCULOASCOMYCETES Fig17.10 Lewi
- Page 1010:
472 LOCULOASCOMYCETES Table 17.2. S
- Page 1014:
474 LOCULOASCOMYCETES Fig17.13 Bipo
- Page 1018:
476 LOCULOASCOMYCETES Fig17.15 Toxi
- Page 1022:
478 LOCULOASCOMYCETES is commonly f
- Page 1026:
480 LOCULOASCOMYCETES Fig17.18 Spor
- Page 1030:
482 LOCULOASCOMYCETES Fig17.19 Myco
- Page 1034:
484 LOCULOASCOMYCETES incompatible
- Page 1038:
486 LOCULOASCOMYCETES Fig17.24 Clad
- Page 1042:
488 BASIDIOMYCOTA (Figs. 18.1d,e).
- Page 1046:
490 BASIDIOMYCOTA wall is indeed th
- Page 1050:
492 BASIDIOMYCOTA Fig18.4 Life cycl
- Page 1054:
494 BASIDIOMYCOTA dikaryotic ballis
- Page 1058:
496 BASIDIOMYCOTA mushroom Agaricus
- Page 1062:
498 BASIDIOMYCOTA Fig18.9 Diagramma
- Page 1066:
500 BASIDIOMYCOTA Fig18.11 Diagramm
- Page 1070:
502 BASIDIOMYCOTA Fig18.13 Hyphal a
- Page 1074:
504 BASIDIOMYCOTA Auricularia auric
- Page 1078:
506 BASIDIOMYCOTA fungus Bulbillomy
- Page 1082:
508 BASIDIOMYCOTA A 3 B 3 , A 3 B 4
- Page 1086:
510 BASIDIOMYCOTA the small number
- Page 1090:
512 BASIDIOMYCOTA Fig18.21 Phylogen
- Page 1094:
19 Homobasidiomycetes 19.1 Introduc
- Page 1098:
Fig19.2 The eight-clade phylogeneti
- Page 1102:
518 HOMOBASIDIOMYCETES There are th
- Page 1106:
520 HOMOBASIDIOMYCETES basidiocarp
- Page 1110:
522 HOMOBASIDIOMYCETES agar media,
- Page 1114:
524 HOMOBASIDIOMYCETES Fig19.9 Diff
- Page 1118:
526 HOMOBASIDIOMYCETES An equally i
- Page 1122:
528 HOMOBASIDIOMYCETES Fig19.11 Car
- Page 1126:
530 HOMOBASIDIOMYCETES are common o
- Page 1130:
532 HOMOBASIDIOMYCETES biotechnolog
- Page 1134:
534 HOMOBASIDIOMYCETES 2 million to
- Page 1138:
536 HOMOBASIDIOMYCETES Breeding of
- Page 1142:
538 HOMOBASIDIOMYCETES In culture,
- Page 1146:
540 HOMOBASIDIOMYCETES is used in a
- Page 1150:
542 HOMOBASIDIOMYCETES edible and s
- Page 1154:
544 HOMOBASIDIOMYCETES Fig19.17 Sch
- Page 1158:
546 HOMOBASIDIOMYCETES in a sinuous
- Page 1162:
548 HOMOBASIDIOMYCETES growth often
- Page 1166:
550 HOMOBASIDIOMYCETES agg. (Fig. 1
- Page 1170:
552 HOMOBASIDIOMYCETES to form the
- Page 1174:
554 HOMOBASIDIOMYCETES phylogenetic
- Page 1178:
556 HOMOBASIDIOMYCETES Fig19.21 Bas
- Page 1182:
558 HOMOBASIDIOMYCETES fungus is ac
- Page 1186:
560 HOMOBASIDIOMYCETES monokaryons
- Page 1190:
562 HOMOBASIDIOMYCETES logs, they m
- Page 1194:
564 HOMOBASIDIOMYCETES of peroxidas
- Page 1198:
566 HOMOBASIDIOMYCETES and their po
- Page 1202:
568 HOMOBASIDIOMYCETES Fig19.27 Ste
- Page 1206:
570 HOMOBASIDIOMYCETES non-outcross
- Page 1210:
572 HOMOBASIDIOMYCETES (Talbot, 197
- Page 1214:
574 HOMOBASIDIOMYCETES P. pomaceus
- Page 1218:
576 HOMOBASIDIOMYCETES independentl
- Page 1222:
578 HOMOBASIDIOMYCETES: GASTEROMYCE
- Page 1226:
580 HOMOBASIDIOMYCETES: GASTEROMYCE
- Page 1230:
582 HOMOBASIDIOMYCETES: GASTEROMYCE
- Page 1234:
584 HOMOBASIDIOMYCETES: GASTEROMYCE
- Page 1238:
586 HOMOBASIDIOMYCETES: GASTEROMYCE
- Page 1242:
588 HOMOBASIDIOMYCETES: GASTEROMYCE
- Page 1246:
590 HOMOBASIDIOMYCETES: GASTEROMYCE
- Page 1250:
592 HOMOBASIDIOMYCETES: GASTEROMYCE
- Page 1254:
594 HETEROBASIDIOMYCETES Table 21.1
- Page 1258:
596 HETEROBASIDIOMYCETES Simple app
- Page 1262:
598 HETEROBASIDIOMYCETES (Uetake et
- Page 1266:
600 HETEROBASIDIOMYCETES 21.3.1 Dac
- Page 1270:
602 HETEROBASIDIOMYCETES Fig 21.6 A
- Page 1274:
604 HETEROBASIDIOMYCETES the hymeni
- Page 1278:
606 HETEROBASIDIOMYCETES Fig 21.10
- Page 1282:
608 HETEROBASIDIOMYCETES Fig 21.13
- Page 1286:
610 UREDINIOMYCETES: UREDINALES (RU
- Page 1290:
612 UREDINIOMYCETES: UREDINALES (RU
- Page 1294:
614 UREDINIOMYCETES: UREDINALES (RU
- Page 1298:
616 UREDINIOMYCETES: UREDINALES (RU
- Page 1302:
618 UREDINIOMYCETES: UREDINALES (RU
- Page 1306:
620 UREDINIOMYCETES: UREDINALES (RU
- Page 1310:
622 UREDINIOMYCETES: UREDINALES (RU
- Page 1314:
624 UREDINIOMYCETES: UREDINALES (RU
- Page 1318:
626 UREDINIOMYCETES: UREDINALES (RU
- Page 1322:
628 UREDINIOMYCETES: UREDINALES (RU
- Page 1326:
630 UREDINIOMYCETES: UREDINALES (RU
- Page 1330:
632 UREDINIOMYCETES: UREDINALES (RU
- Page 1334:
634 UREDINIOMYCETES: UREDINALES (RU
- Page 1338:
23 Ustilaginomycetes: smut fungi an
- Page 1342:
638 USTILAGINOMYCETES: SMUT FUNGI A
- Page 1346:
640 USTILAGINOMYCETES: SMUT FUNGI A
- Page 1350:
642 USTILAGINOMYCETES: SMUT FUNGI A
- Page 1354:
644 USTILAGINOMYCETES: SMUT FUNGI A
- Page 1358: 646 USTILAGINOMYCETES: SMUT FUNGI A
- Page 1362: 648 USTILAGINOMYCETES: SMUT FUNGI A
- Page 1366: 650 USTILAGINOMYCETES: SMUT FUNGI A
- Page 1370: 652 USTILAGINOMYCETES: SMUT FUNGI A
- Page 1374: 654 USTILAGINOMYCETES: SMUT FUNGI A
- Page 1378: 656 USTILAGINOMYCETES: SMUT FUNGI A
- Page 1382: 24 Basidiomycete yeasts 24.1 Introd
- Page 1386: 660 BASIDIOMYCETE YEASTS (Heterobas
- Page 1390: 662 BASIDIOMYCETE YEASTS in that it
- Page 1394: 664 BASIDIOMYCETE YEASTS 5-fluorocy
- Page 1398: 666 BASIDIOMYCETE YEASTS and Xantho
- Page 1402: 668 BASIDIOMYCETE YEASTS Fig 24.5 S
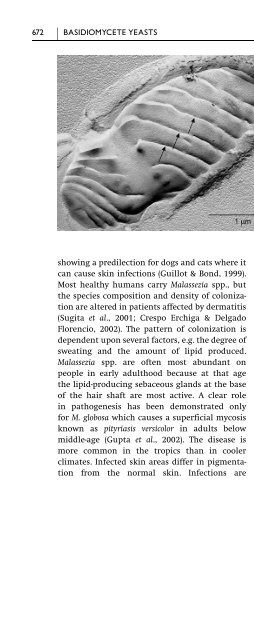
- Page 1406: 670 BASIDIOMYCETE YEASTS Fig 24.7 P
- Page 1412: 25 Anamorphic fungi (nematophagous
- Page 1416: NEMATOPHAGOUS FUNGI 675 We owe much
- Page 1420: NEMATOPHAGOUS FUNGI 677 Fig 25.3 Ar
- Page 1424: NEMATOPHAGOUS FUNGI 679 Fig 25.5 Da
- Page 1428: NEMATOPHAGOUS FUNGI 681 Fig 25.7 Ne
- Page 1432: NEMATOPHAGOUS FUNGI 683 (group 1),
- Page 1436: AQUATIC HYPHOMYCETES (INGOLDIAN FUN
- Page 1440: AQUATIC HYPHOMYCETES (INGOLDIAN FUN
- Page 1444: AQUATIC HYPHOMYCETES (INGOLDIAN FUN
- Page 1448: AQUATIC HYPHOMYCETES (INGOLDIAN FUN
- Page 1452: AQUATIC HYPHOMYCETES (INGOLDIAN FUN
- Page 1456: AQUATIC HYPHOMYCETES (INGOLDIAN FUN
- Page 1460:
AERO-AQUATIC FUNGI 697 Table 25.3.
- Page 1464:
AERO-AQUATIC FUNGI 699 Fig 25.22 Pr
- Page 1468:
AERO-AQUATIC FUNGI 701 means of dis
- Page 1472:
REFERENCES 703 Aist, J. R. & Israel
- Page 1476:
REFERENCES 705 Arnold, D. L., Blake
- Page 1480:
REFERENCES 707 Barr, D. J. S. (1987
- Page 1484:
REFERENCES 709 Beakes, G. W. & Gloc
- Page 1488:
REFERENCES 711 Beuchat, L. R. (1995
- Page 1492:
REFERENCES 713 Bourett, T. M., Czym
- Page 1496:
REFERENCES 715 Brown, J. S., Whan,
- Page 1500:
REFERENCES 717 Callac, P. (1995). B
- Page 1504:
REFERENCES 719 Castlebury, L. A., R
- Page 1508:
REFERENCES 721 Chiu, S. W. & Moore,
- Page 1512:
REFERENCES 723 Cooke, L. R. & Littl
- Page 1516:
REFERENCES 725 Culvenor, C. C., Bec
- Page 1520:
REFERENCES 727 Degousée, N., Gupta
- Page 1524:
REFERENCES 729 Dissing, H. (1986).
- Page 1528:
REFERENCES 731 Edgar, J. A., Frahn,
- Page 1532:
REFERENCES 733 Falk, S. P., Gadoury
- Page 1536:
REFERENCES 735 Foster, S. J. & Fitt
- Page 1540:
REFERENCES 737 Gauger, W. L. (1975)
- Page 1544:
REFERENCES 739 Haptoglossa heteromo
- Page 1548:
REFERENCES 741 Griffith, J. M., Dav
- Page 1552:
REFERENCES 743 Hampson, M. C. (1988
- Page 1556:
REFERENCES 745 Heath, M. C. & Skala
- Page 1560:
REFERENCES 747 Hohl, H. R. & Iselin
- Page 1564:
REFERENCES 749 Huang, B., Li, Z. G.
- Page 1568:
REFERENCES 751 Ingold, C. T. & Zobe
- Page 1572:
REFERENCES 753 Jiang, J., Stephenso
- Page 1576:
REFERENCES 755 Kendrick, B., ed. (1
- Page 1580:
REFERENCES 757 Ko, W. H. (1980). Ho
- Page 1584:
REFERENCES 759 concern: cytological
- Page 1588:
REFERENCES 761 Latunde-Dada, A. O.,
- Page 1592:
REFERENCES 763 Lingappa, B. T. (195
- Page 1596:
REFERENCES 765 Luttrell, E. S. (198
- Page 1600:
REFERENCES 767 Markovich, N. A. & K
- Page 1604:
REFERENCES 769 Menge, J. A. (1984).
- Page 1608:
REFERENCES 771 Molina, R., Trappe,
- Page 1612:
REFERENCES 773 Moss, M. O. & Long,
- Page 1616:
REFERENCES 775 inoperculaten Discom
- Page 1620:
REFERENCES 777 Obermayer, W. & Poel
- Page 1624:
REFERENCES 779 Ott, S., Meier, T. &
- Page 1628:
REFERENCES 781 Percudani, R., Trevi
- Page 1632:
REFERENCES 783 Pommer, E.-H. (1995)
- Page 1636:
REFERENCES 785 Raper, J. R. (1939).
- Page 1640:
REFERENCES 787 Reynolds, D. R. (197
- Page 1644:
REFERENCES 789 Roncal, T., Cordobé
- Page 1648:
REFERENCES 791 Sánchez, C. (2004).
- Page 1652:
REFERENCES 793 K. A. Powell, A. Ren
- Page 1656:
REFERENCES 795 Silliker, M. E., Mon
- Page 1660:
REFERENCES 797 Solla, A. & Gil, L.
- Page 1664:
REFERENCES 799 Stensrud, Ø., Hywel
- Page 1668:
REFERENCES 801 Swann, E. C. & Taylo
- Page 1672:
REFERENCES 803 Thines, E., Weber, R
- Page 1676:
REFERENCES 805 Uchida, W., Matsunag
- Page 1680:
REFERENCES 807 Verstrepen, K. J., D
- Page 1684:
REFERENCES 809 Waters, H., Butler,
- Page 1688:
REFERENCES 811 Weeks, R. J., Padhye
- Page 1692:
REFERENCES 813 Willetts, H. J. & Bu
- Page 1696:
REFERENCES 815 Xu, J.-T. & Mu, C. (
- Page 1700:
Index Page numbers with images are
- Page 1704:
INDEX 819 ascospore-delimiting memb
- Page 1708:
INDEX 821 Candida parapsilosis 227,
- Page 1712:
INDEX 823 Cordyceps capitata 362 Co
- Page 1716:
INDEX 825 Erysiphe polygoni 402 Ery
- Page 1720:
INDEX 827 hemicellulose 528 Hemilei
- Page 1724:
INDEX 829 Leveillula taurica 407 Le
- Page 1728:
INDEX 831 mycosporine-alanine 387 m
- Page 1732:
INDEX 833 Phallus ravenelii 591 Pha
- Page 1736:
INDEX 835 Puccinia coronata 476, 61
- Page 1740:
INDEX 837 scolytid beetles 366 Scop
- Page 1744:
INDEX 839 thallic conidiogenesis 30
- Page 1748:
INDEX 841 yeasts 3; see Archiascomy