Control of Varicella/ Herpes Zoster Infection - NHS Lanarkshire
Control of Varicella/ Herpes Zoster Infection - NHS Lanarkshire
Control of Varicella/ Herpes Zoster Infection - NHS Lanarkshire
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
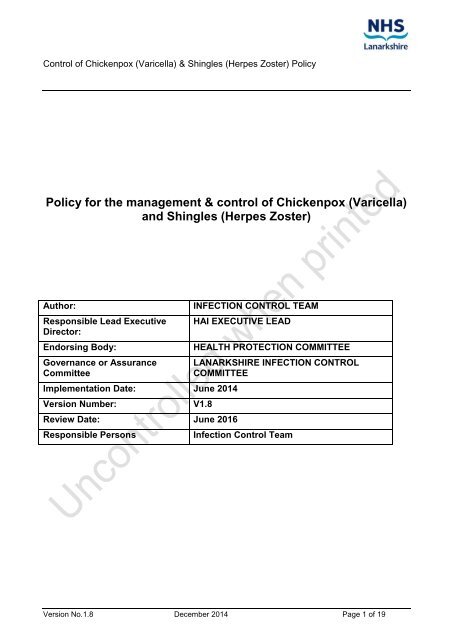
<strong>Control</strong> <strong>of</strong> Chickenpox (<strong>Varicella</strong>) & Shingles (<strong>Herpes</strong> <strong>Zoster</strong>) Policy<br />
Policy for the management & control <strong>of</strong> Chickenpox (<strong>Varicella</strong>)<br />
and Shingles (<strong>Herpes</strong> <strong>Zoster</strong>)<br />
Author:<br />
Responsible Lead Executive<br />
Director:<br />
Endorsing Body:<br />
Governance or Assurance<br />
Committee<br />
Implementation Date: June 2014<br />
Version Number: V1.8<br />
Review Date: June 2016<br />
Responsible Persons<br />
INFECTION CONTROL TEAM<br />
HAI EXECUTIVE LEAD<br />
HEALTH PROTECTION COMMITTEE<br />
LANARKSHIRE INFECTION CONTROL<br />
COMMITTEE<br />
<strong>Infection</strong> <strong>Control</strong> Team<br />
Version No.1.8 December 2014 Page 1 <strong>of</strong> 19
<strong>Control</strong> <strong>of</strong> Chickenpox (<strong>Varicella</strong>) & Shingles (<strong>Herpes</strong> <strong>Zoster</strong>) Policy<br />
CONTENTS<br />
i) Consultation and Distribution Record<br />
ii) Change Record<br />
1. INTRODUCTION<br />
2. AIM, PURPOSE AND OUTCOMES<br />
3. SCOPE, ROLES AND RESPONSIBILITIES<br />
4. CHICKENPOX<br />
5. SHINGLES<br />
6. STANDARD INFECTION CONTROL PRECAUTIONS (SICPs) AND<br />
TRANSMISSION BASED PRECAUTIONS.<br />
7. POST EXPOSURE MANAGEMENT:<br />
7.1 Pregnancy, neonates and infants<br />
7.2 Immunocompromised patients<br />
8. PRACTICALITIES OF ISSUING VARICELLA ZOSTER IMMUNOGLOBULIN<br />
9. MANAGEMENT OF HEALTHCARE WORKERS EXPOSED TO CHICKENPOX OR<br />
SHINGLES INFECTION<br />
10. RESOURCE IMPLICATIONS<br />
11. COMMUNICATION PLAN<br />
12. QUALITY IMPROVEMENT – MONITORING AND REVIEW<br />
13. EQUALITY AND DIVERSITY IMPACT ASSESSMENT<br />
14. SUMMARY OF FREQUENTLY ASKED QUESTIONS<br />
Version No.1.8 December 2014 Page 2 <strong>of</strong> 19
<strong>Control</strong> <strong>of</strong> Chickenpox (<strong>Varicella</strong>) & Shingles (<strong>Herpes</strong> <strong>Zoster</strong>) Policy<br />
15. APPENDIX 1: Appendix 1 – Decision making aid for prescribing VZIG<br />
16. APPENDIX 2: IMMUNOGLOBULIN REQUEST FORM<br />
17. REFERENCES & BIBLIOGRAPHY<br />
Contributing Author /<br />
Authors<br />
CONSULTATION AND DISTRIBUTION RECORD<br />
<br />
<br />
Jacqueline Shookhye-Dickson, <strong>Infection</strong> <strong>Control</strong> Nurse<br />
Dr Christopher Mackintosh, Associate Medical Director<br />
Primary Care<br />
Dr Donald Inverarity, Lead <strong>Infection</strong> <strong>Control</strong> Doctor /<br />
Consultant Microbiologist<br />
<br />
<br />
<br />
<br />
<br />
<br />
Lindsay Guthrie, Senior Health Protection Nurse<br />
Dr Thomas Gillespie, Consultant Microbiologist<br />
Gail Richardson, Head <strong>of</strong> Pharmacy, Wishaw General<br />
Hospital<br />
Steve McCormick, Lead Antimicrobial Pharmacist<br />
Karen Patterson, Head <strong>of</strong> Pharmacy, Hairmyres Hospital<br />
Alexa Wall, Head <strong>of</strong> Pharmacy, Monklands Hospital<br />
Consultation Process /<br />
Stakeholders:<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Microbiologists<br />
Associate Medical Director Primary Care<br />
General Practitioners<br />
Health Protection Nurses<br />
Consultants in Public Health Medicine<br />
<strong>Infection</strong> <strong>Control</strong> Nurses<br />
Occupational Health Nurses<br />
Pharmacists<br />
Antimicrobial Pharmacists<br />
Consultant Haematologist<br />
Consultant in Infectious Diseases<br />
Consultant Paediatrician<br />
Senior Nurses / Midwives<br />
Senior Charge Nurses<br />
Distribution: <strong>NHS</strong> <strong>Lanarkshire</strong> intranet – Firstport<br />
<br />
<strong>NHS</strong> <strong>Lanarkshire</strong> internet<br />
Version No.1.8 December 2014 Page 3 <strong>of</strong> 19
<strong>Control</strong> <strong>of</strong> Chickenpox (<strong>Varicella</strong>) & Shingles (<strong>Herpes</strong> <strong>Zoster</strong>) Policy<br />
CHANGE RECORD<br />
Date Author Change Version No.<br />
20/02/14 J. Shookhye- Content reviewed & updated. New policy V1.0<br />
Dickson template applied<br />
04/04/14 J. Shookhye- Content revised to reflect comments V1.1<br />
Dickson received from stakeholders<br />
15/04/14 J. Shookhye- Final draft for approval V1.2<br />
Dickson<br />
06/05/14 L. Guthrie Changes to VZIG ordering process & form V1.3<br />
included in policy section<br />
21/05/14 L. Guthrie Content revised to reflect comments from V1.4<br />
stakeholders<br />
11/06/14 J. Shookhye- Content revised to reflect final comments V1.5<br />
Dickson and add in contributing authors<br />
12/06/14 L. Guthrie Clarify indications for use <strong>of</strong> VZIG as V1.6<br />
prophylaxis, and not treatment<br />
23/06/14 L. Guthrie Final approved draft V1.7<br />
10/12/2014 L. Guthrie Review date revised in line with Vale <strong>of</strong><br />
Leven Report recommendation<br />
V1.8<br />
Version No.1.8 December 2014 Page 4 <strong>of</strong> 19
<strong>Control</strong> <strong>of</strong> Chickenpox (<strong>Varicella</strong>) & Shingles (<strong>Herpes</strong> <strong>Zoster</strong>) Policy<br />
1. INTRODUCTION<br />
This policy has been developed for use in <strong>NHS</strong> <strong>Lanarkshire</strong> as part <strong>of</strong> the <strong>Control</strong> <strong>of</strong><br />
<strong>Infection</strong> policy manual and should be read in conjunction with:<br />
Chapter 1 - Standard <strong>Infection</strong> <strong>Control</strong> Precautions (SICPs) and Chapter 2 Transmission<br />
Based Precautions (TBPs).<br />
2. AIM, PURPOSE AND OUTCOMES<br />
To ensure that patients with chickenpox or shingles receive appropriate care and<br />
management in line with current national guidelines and best practice.<br />
To ensure that every effort is made to protect susceptible patients, staff and visitors to<br />
inpatient areas from the risk <strong>of</strong> cross infection from known cases <strong>of</strong> chickenpox or<br />
shingles.<br />
3. SCOPE, ROLES & RESPONSIBILITIES<br />
This policy is designed to safeguard patients / users <strong>of</strong> <strong>NHS</strong> <strong>Lanarkshire</strong> Services and<br />
visitors to inpatient areas.<br />
This policy is aimed at all employees <strong>of</strong> <strong>NHS</strong> <strong>Lanarkshire</strong>, in particular:<br />
<br />
<br />
<br />
<br />
<br />
Nurses, midwives and medical staff working in in-patient & community settings<br />
Domestic staff working in in-patient areas<br />
Health Protection Team<br />
<strong>Infection</strong> <strong>Control</strong> Team<br />
Salus Occupational Health & Safety service<br />
All staff are responsible for implementing and following the information provided in this<br />
policy. Staff must inform their line manager, SALUS and the <strong>Infection</strong> <strong>Control</strong> Team if this<br />
policy cannot be followed.<br />
Stakeholders:<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Microbiologists<br />
Associate Medical Director Primary Care<br />
General Practitioners<br />
Public Health Team<br />
<strong>Infection</strong> <strong>Control</strong> staff<br />
Occupational Health Nurses<br />
Antimicrobial Pharmacists<br />
Consultant in Haematology<br />
Consultant Paediatrician<br />
Senior Nurses / Midwives<br />
SALUS Occupational Health & Safety<br />
Version No.1.8 December 2014 Page 5 <strong>of</strong> 19
<strong>Control</strong> <strong>of</strong> Chickenpox (<strong>Varicella</strong>) & Shingles (<strong>Herpes</strong> <strong>Zoster</strong>) Policy<br />
4. CHICKENPOX<br />
Communicable<br />
disease/ causative<br />
organism<br />
Clinical manifestation<br />
/ diagnosis<br />
Incubation period<br />
Chickenpox / <strong>Varicella</strong> zoster virus (VZV)<br />
May initially begin with cold-like symptoms<br />
Raised temperature<br />
Intensely itchy vesicular rash. Clusters <strong>of</strong> vesicular (blisters) spots<br />
appear over 3-5 days, which start on the face and scalp, spread to<br />
the trunk, abdomen and limbs.<br />
It is possible to be infected but show no symptoms.<br />
Diagnosis can usually be reliably made on physical examination;<br />
swabs/specimens are not usually required.<br />
10-21 days.<br />
Period <strong>of</strong> infectivity 1-2 days before the onset <strong>of</strong> the rash until the vesicles (blisters) are<br />
dry/crusted which is usually 4 - 5 days after the onset <strong>of</strong> rash. This<br />
may be prolonged in immunosuppressed patients.<br />
Mode <strong>of</strong> transmission Direct contact with an infected person,<br />
Droplet or aerosol spread from vesicular fluid from skin lesions.<br />
Secretions from the respiratory tract (the virus enters the individual<br />
through the upper respiratory tract).<br />
Indirectly via contaminated articles e.g. clothing / bedding.<br />
Groups susceptible<br />
to chickenpox<br />
<br />
<br />
Most commonly seen in children under ten years old. In healthy<br />
children the illness is usually mild with no complications.<br />
Non immune adolescents and adults are at increased risk <strong>of</strong><br />
severe disease.<br />
Definition <strong>of</strong> a<br />
significant exposure<br />
to chickenpox<br />
Management <strong>of</strong><br />
patients exposed to<br />
chickenpox<br />
Groups at increased<br />
risk <strong>of</strong> severe disease<br />
Non immune individuals who have had:<br />
Contact in the same room as a person with chickenpox (e.g. in a<br />
house or classroom or a 2-4 bed hospital bay) for a significant<br />
period <strong>of</strong> time (15 minutes or more).<br />
Face to face contact, with a person with chickenpox for example<br />
while having a conversation (remember that they may be infectious<br />
up to 48 hours before the rash appears).<br />
In large open wards, airborne transmission at a distance has<br />
occasionally been reported.<br />
Patients who have had significant contact with a person who has<br />
chickenpox should be assessed by a clinician to determine the risk<br />
they may have <strong>of</strong> contracting chickenpox.<br />
<strong>Varicella</strong> vaccine may be appropriate. Information on prophylaxis<br />
can be found in The Green Book: chapter34<br />
Advice may be sought from a Consultant Microbiologist if required.<br />
If cross infection occurs, the <strong>Infection</strong> <strong>Control</strong> team should be<br />
informed as soon as possible.<br />
Adolescents and adults.<br />
Smokers.<br />
Non immune pregnant women and their baby.<br />
Neonates whose mothers develop chickenpox in the period 7 days<br />
Version No.1.8 December 2014 Page 6 <strong>of</strong> 19
<strong>Control</strong> <strong>of</strong> Chickenpox (<strong>Varicella</strong>) & Shingles (<strong>Herpes</strong> <strong>Zoster</strong>) Policy<br />
before to 7 days after the birth.<br />
Neonates born to non immune mothers who have been exposed to<br />
chickenpox or shingles in the first month <strong>of</strong> the baby’s life.<br />
Immunocompromised patients (see section 7 for definitions and<br />
management).<br />
Complications <strong>of</strong> May include:<br />
Chickenpox<br />
secondary bacterial infections <strong>of</strong> skin lesions<br />
pneumonia,<br />
cerebellar ataxia<br />
encephalitis<br />
haemorrhagic conditions.<br />
Immunity<br />
The majority <strong>of</strong> people are infected in childhood and remain immune to<br />
chickenpox for life. 90% <strong>of</strong> adults raised in the UK are immune.<br />
Vaccine preventable Yes, however this is not a routine part <strong>of</strong> the UK’s childhood<br />
immunisation programme.<br />
Treatment Antiviral treatment started within 24 hours <strong>of</strong> the onset <strong>of</strong> rash may<br />
reduce the duration and severity <strong>of</strong> symptoms in otherwise healthy<br />
adults and adolescents.<br />
Immunocompromised individuals will also certainly benefit from<br />
treatment with IV acyclovir.<br />
See section 8 for guidance regarding prophylaxis with <strong>Varicella</strong><br />
<strong>Zoster</strong> immunoglobulin (VZIG) in asymptomatic individuals at<br />
higher risk <strong>of</strong> developing severe disease.<br />
Notifiable disease No.<br />
Version No.1.8 December 2014 Page 7 <strong>of</strong> 19
<strong>Control</strong> <strong>of</strong> Chickenpox (<strong>Varicella</strong>) & Shingles (<strong>Herpes</strong> <strong>Zoster</strong>) Policy<br />
5. SHINGLES<br />
Communicable<br />
disease/ Causative<br />
organism<br />
Clinical manifestation /<br />
Diagnosis<br />
Period <strong>of</strong> infectivity<br />
Mode <strong>of</strong> transmission<br />
Groups susceptible to<br />
shingles<br />
Definition <strong>of</strong> a<br />
significant exposure to<br />
shingles<br />
Management <strong>of</strong><br />
patients exposed to<br />
shingles<br />
Groups at increased<br />
risk <strong>of</strong> severe disease<br />
Vaccine preventable<br />
Shingles / <strong>Herpes</strong> <strong>Zoster</strong> (HZ)<br />
• Previous infection with chickenpox is necessary before a person<br />
can develop shingles. It appears following reactivation <strong>of</strong><br />
chickenpox virus which lies dormant in dorsal root ganglia (spinal<br />
nerve tissue) – <strong>of</strong>ten for decades.<br />
• Pain in the area <strong>of</strong> the affected nerve is <strong>of</strong>ten the first symptom<br />
followed by a dermatomal (one sided) rash <strong>of</strong> fluid filled vesicles<br />
(blisters).<br />
• Diagnosis can usually be reliably made on physical examination;<br />
swabs/specimens are not usually required.<br />
Until all the lesions have dried/crusted.<br />
Direct contact with the fluid from the vesicles which is then<br />
transferred to the mucous membranes <strong>of</strong> a non immune individual,<br />
usually via the hands.<br />
Individuals who have had chickenpox previously may develop<br />
shingles at any time in their lives although it does seem to be<br />
associated with older age and conditions which suppress the immune<br />
system.<br />
Direct contact with fluid from the rash blisters is required to infect a<br />
person who is not immune to chickenpox (see mode <strong>of</strong> transmission).<br />
Patients who have had significant contact with a person who has<br />
shingles should be assessed by a clinician to determine the risk<br />
they may have <strong>of</strong> contracting chickenpox.<br />
<strong>Varicella</strong> vaccine may be appropriate. Information on prophylaxis<br />
can be found in The Green Book: chapter28a<br />
Advice may be sought from a Consultant Microbiologist if<br />
required.<br />
If cross infection occurs, the <strong>Infection</strong> <strong>Control</strong> team should be<br />
informed as soon as possible.<br />
Pregnant women and their baby, when the woman has no<br />
immunity to chickenpox (a pregnant woman who has shingles<br />
presents no risk to her unborn baby).<br />
Neonates born to non immune mothers who come into direct<br />
contact with a person with shingles may develop chickenpox (see<br />
section 7).<br />
Immunocompromised individuals may suffer more severe and<br />
prolonged symptoms (see section 7 for definitions and<br />
management).<br />
Yes. In 2013 a vaccination programme for those <strong>of</strong> 70 years <strong>of</strong> age<br />
began, in conjunction with a catch up programme.<br />
Treatment Shingles can be effectively treated with oral antiviral drugs;<br />
systemic antiviral treatment can reduce the severity and duration<br />
<strong>of</strong> pain, reduce complications, and reduce viral shedding.<br />
Treatment should be started within 72 hours <strong>of</strong> the onset <strong>of</strong> rash<br />
Version No.1.8 December 2014 Page 8 <strong>of</strong> 19
<strong>Control</strong> <strong>of</strong> Chickenpox (<strong>Varicella</strong>) & Shingles (<strong>Herpes</strong> <strong>Zoster</strong>) Policy<br />
Notifiable disease<br />
and is usually continued for 7–10 days, see The Green Book:<br />
chapter28a<br />
Immunocompromised patients at high risk <strong>of</strong> disseminated or<br />
severe infection should be treated with a parenteral antiviral drug.<br />
See sections 7 & 8 for guidance regarding prophylaxis with<br />
<strong>Varicella</strong> <strong>Zoster</strong> immunoglobulin (VZIG) and antivirals in<br />
asymptomatic individuals at higher risk <strong>of</strong> developing severe<br />
disease.<br />
No.<br />
6. STANDARD INFECTION CONTROL PRECAUTIONS (SICPs) & TRANSMISSION<br />
BASED PRECAUTIONS<br />
Patient placement The patient should be nursed in a single side room (for chickenpox a<br />
negative pressure room should be used if available) until all the<br />
vesicles have dried/crusted (and no new crops are appearing if it is<br />
chickenpox).<br />
Immunocompromised patients may require a longer period <strong>of</strong><br />
isolation.<br />
Patients with chickenpox in their own homes should avoid contact<br />
with non immune people until their lesions are dried and crusted.<br />
Patients with shingles in their own homes may not necessarily<br />
require to be <strong>of</strong>f <strong>of</strong> work e.g. if the rash is not on the extremities, can<br />
be covered, the patient will comply with hand hygiene advice and is<br />
not working with people at high risk <strong>of</strong> contracting chickenpox and<br />
complications from same.<br />
A risk assessment can be carried out by the <strong>Infection</strong> <strong>Control</strong> team /<br />
Health Protection team.<br />
Patient care Patients should only be cared for by staff who are immune to chickenpox.<br />
Hand hygiene<br />
Personal Protective<br />
Equipment<br />
Healthcare Waste<br />
Laundry<br />
Equipment<br />
Decontamination<br />
Patient transfers<br />
between hospitals/<br />
With soap and water or alcohol gel as per SICP /TBP Policy on Firstport.<br />
Patients should also be encouraged to carry out hand hygiene.<br />
As per SICP /TBP Policy on Firstport:<br />
Waste should be designated as clinical / healthcare waste and placed in<br />
an orange bag. Waste Policy is available on Firstport<br />
Linen should be treated as infected. Laundry Policy is available on<br />
Firstport.<br />
The patient should be allocated their own equipment which should not be<br />
shared with other patients. Where this is not possible, equipment must<br />
be thoroughly cleaned with a chlorine based detergent before being used<br />
on another patient. Decontamination Policy Section I is available on<br />
Firstport.<br />
The patient’s room and equipment should be cleaned at least once daily<br />
by Nursing and Domestic staff with a chlorine based detergent.<br />
Once the patient is no longer infectious / is discharged, a terminal clean<br />
<strong>of</strong> the room may be required. Please discuss with the <strong>Infection</strong> <strong>Control</strong><br />
Team.<br />
Transfer <strong>of</strong> infectious patients should be prevented where possible. If it is<br />
essential then the receiving area must be informed prior to moving the<br />
Version No.1.8 December 2014 Page 9 <strong>of</strong> 19
<strong>Control</strong> <strong>of</strong> Chickenpox (<strong>Varicella</strong>) & Shingles (<strong>Herpes</strong> <strong>Zoster</strong>) Policy<br />
wards<br />
patient in order that the appropriate facilities can be prepared for them.<br />
Refer to SICP /TBP Policy and consult the <strong>Infection</strong> <strong>Control</strong> Team for<br />
advice if required.<br />
7. MANAGEMENT OF AT- RISK INDIVIDUALS FOLLOWING SIGNIFICANT<br />
EXPOSURE<br />
People at higher risk <strong>of</strong> developing serious complications from chickenpox or shingles may<br />
be given antiviral drugs and/or prophylactic immunoglobulin (VZIG), which may prevent<br />
severe illness developing.<br />
The aim <strong>of</strong> post-exposure management is to protect individuals at high risk <strong>of</strong> suffering<br />
from severe chickenpox and those who might transmit infection to those at high risk. There<br />
is no benefit once chickenpox is present.<br />
See Appendix 1: Decision making aid for prescribing VZIG.<br />
In these circumstances seek advice from an Infectious Diseases Specialist (Monklands<br />
Hospital 01236 748 748 or local Microbiologist).<br />
Further treatment information is available in the Green Book: Chapter 28a and Chapter 34<br />
and the British National Formulary.<br />
VZIG is a blood product, therefore the nature <strong>of</strong> this preventative treatment MUST be<br />
discussed with the patient by the clinician prior to prescription. The patient may<br />
then provide verbal consent or refuse the product. This discussion and outcome<br />
should be recorded in the patient’s care record.<br />
VZIG can be given within 10 days <strong>of</strong> exposure. Therefore most prescriptions for<br />
VZIG can be requested within standard working hours and is not a clinical<br />
emergency. Patients should be reassured <strong>of</strong> this, and provided with a prescription<br />
as soon as is reasonably practical.<br />
7.1 PREGNANCY, NEONATES & INFANTS<br />
Management <strong>of</strong> a pregnant woman exposed to chickenpox or shingles should be<br />
discussed with an Obstetrician and/ or midwife, who will contact the Microbiologist and, if<br />
appropriate, arrange for the booking blood to be tested.<br />
The management <strong>of</strong> neonates or infants should be decided by a Paediatrician, in<br />
conjunction with a Consultant in Infectious Diseases and Microbiologist.<br />
<strong>Varicella</strong>–zoster immunoglobulin (VZIG) is recommended for individuals who have been<br />
exposed:<br />
<br />
<br />
<br />
who are at increased risk <strong>of</strong> severe chickenpox, and<br />
who have no antibodies to varicella–zoster virus (VZV), and<br />
who have had significant exposure to chickenpox or herpes zoster.<br />
However it should be noted that chickenpox can still develop in infants who have received<br />
VZIG.<br />
Version No.1.8 December 2014 Page 10 <strong>of</strong> 19
<strong>Control</strong> <strong>of</strong> Chickenpox (<strong>Varicella</strong>) & Shingles (<strong>Herpes</strong> <strong>Zoster</strong>) Policy<br />
Those at increased risk during pregnancy, or the neonatal period include:<br />
Patients at increased risk<br />
Neonates whose mothers<br />
develop chickenpox rash in<br />
the period 7 days before to 7<br />
days after delivery.<br />
Susceptible neonates exposed<br />
in the first 7 days <strong>of</strong> life.<br />
Neonates born to non immune<br />
mothers, exposed within the<br />
first month <strong>of</strong> life.<br />
Neonates / infants exposed<br />
during intensive/prolonged<br />
special care.<br />
Non immune women exposed<br />
at any stage <strong>of</strong> pregnancy.<br />
Babies born to immune<br />
mothers but who are being<br />
discharged home where a<br />
household member has<br />
chickenpox or shingles.<br />
Babies born at
<strong>Control</strong> <strong>of</strong> Chickenpox (<strong>Varicella</strong>) & Shingles (<strong>Herpes</strong> <strong>Zoster</strong>) Policy<br />
2mg/kg/day for at least one week, or 1mg/kg/day for one month. For adults, an<br />
equivalent dose is harder to define but immunosuppression should be considered in<br />
those who, in the previous 3 months, have received 40mg <strong>of</strong> prednisolone per day for<br />
more than one week. Occasionally, there may be individuals on lower doses <strong>of</strong><br />
steroids who may be immunosuppressed, and are at increased risk from infections.<br />
Therefore, live vaccines should be considered with caution in discussion with a<br />
relevant specialist physician.<br />
<br />
<br />
<br />
<br />
<br />
<br />
All patients currently being treated for malignant disease with immunosuppressive<br />
chemotherapy or radiotherapy, and for at least six months after terminating such<br />
treatment.<br />
All patients who have received a solid organ transplant and are currently on<br />
immunosuppressive treatment.<br />
Patients who have had a bone marrow transplant within the previous 6 months, and<br />
until at least 12 months after finishing all immunosuppressive treatment, or longer<br />
where the patient has developed graft-versus-host disease.<br />
Patients receiving other types <strong>of</strong> immunosuppressive drugs (e.g. azathioprine,<br />
cyclosporine, methotrexate, cyclophosphamide, leflunomide and the newer cytokine<br />
inhibitors) alone or in combination with lower doses <strong>of</strong> steroids. The advice <strong>of</strong> the<br />
physician or immunologist in charge should be sought for at least six months after<br />
treatment.<br />
Patients with evidence <strong>of</strong> severe primary immunodeficiency, e.g. severe combined<br />
immunodeficiency (SCID), Wiskott-Aldrich syndrome and other combined<br />
immunodeficiency syndromes<br />
Patients with immunosuppression due to HIV infection.<br />
VZIG MANAGEMENT IN IMMUNOSUPPRESSED PATIENTS<br />
Whenever possible, immunosuppressed patients exposed to chickenpox / shingles should<br />
be tested irrespective <strong>of</strong> their history <strong>of</strong> chickenpox.<br />
However, VZIG administration should not be delayed past seven days after initial contact<br />
while an antibody test is done. Under these circumstances, VZIG should be given on the<br />
basis <strong>of</strong> a negative history <strong>of</strong> chickenpox. If the patient has a positive history <strong>of</strong><br />
chickenpox, wait for the antibody results. Those with a positive history in whom VZ<br />
antibody is not detected by a sensitive assay should be given VZIG.<br />
VZIG is not indicated in immunosuppressed contacts with detectable antibody as the<br />
amount <strong>of</strong> antibody provided by VZIG will not significantly increase VZ antibody titres in<br />
those who are already positive.<br />
Version No.1.8 December 2014 Page 12 <strong>of</strong> 19
<strong>Control</strong> <strong>of</strong> Chickenpox (<strong>Varicella</strong>) & Shingles (<strong>Herpes</strong> <strong>Zoster</strong>) Policy<br />
Second attacks <strong>of</strong> chickenpox can occasionally occur in immunosuppressed VZ antibody<br />
positive patients, but these are likely to be related to defects in cell-mediated immunity.<br />
VZ antibody detected in patients who have been transfused or who have received<br />
intravenous immunoglobulin in the previous three months may have been passively<br />
acquired. Although VZIG is not indicated if antibody from other blood products is<br />
detectable, re-testing in the event <strong>of</strong> a subsequent exposure will be required, as the patient<br />
may have become antibody negative.<br />
8. PRACTICALITIES OF ISSUING VZIG<br />
<br />
<br />
<br />
<br />
<br />
<br />
VZIG is a Prescription only medicine (POM) and needs to be prescribed in the<br />
casenotes / kardex.<br />
VZIG stock release from pharmacy requires completion <strong>of</strong> specific VZIG request<br />
form (see Appendix 2) by the requesting/prescribing physician.<br />
Requests for the issue <strong>of</strong> VZIG within <strong>NHS</strong> <strong>Lanarkshire</strong> should be discussed<br />
with a <strong>NHS</strong> <strong>Lanarkshire</strong> Consultant Microbiologist.<br />
VZIG will be issued when there is laboratory evidence <strong>of</strong> a lack <strong>of</strong> immunity to<br />
chickenpox in an 'at risk' individual who has had significant contact with a patient<br />
diagnosed as having active varicella infection. Stocks <strong>of</strong> VZIG are held by<br />
Pharmacy at Wishaw General Hospital, Hairmyres Hospital and at the Blood<br />
Transfusion Service (BTS) at Monklands Hospital.<br />
VZIG will be detectable in the blood for 3 months. But if a second exposure<br />
occurs after 3 weeks <strong>of</strong> administration <strong>of</strong> VZIG, a further dose is indicated but<br />
does not require additional laboratory testing.<br />
Patients who receive VZIG are potentially incubating the illness and therefore<br />
may still develop chickenpox. Administration <strong>of</strong> VZIG may extend the incubation<br />
period up to 28 days. Therefore such patients should avoid contact with<br />
susceptible others from day 10 to day 28 following their own exposure.<br />
Please note that a separate local arrangement has been approved for the supply <strong>of</strong> VZIG<br />
in Haematology at Monklands District General Hospital.<br />
Version No.1.8 December 2014 Page 13 <strong>of</strong> 19
<strong>Control</strong> <strong>of</strong> Chickenpox (<strong>Varicella</strong>) & Shingles (<strong>Herpes</strong> <strong>Zoster</strong>) Policy<br />
9. MANAGEMENT OF HEALTHCARE WORKERS EXPOSED TO CHICKENPOX OR<br />
SHINGLES INFECTION<br />
Healthcare workers<br />
with chickenpox<br />
Healthcare workers<br />
with shingles<br />
Immune Healthcare<br />
workers exposed<br />
to Chickenpox or<br />
shingles<br />
Non immune<br />
Healthcare workers<br />
exposed to<br />
chickenpox or<br />
shingles<br />
Pregnant<br />
Healthcare workers<br />
Treatment <strong>of</strong> non<br />
immune Healthcare<br />
workers exposed<br />
to chickenpox or<br />
shingles<br />
Should inform Occupational Health and be excluded from work until no<br />
new crops are appearing and all lesions have dried and crusted.<br />
Should inform Occupational Health who will carry out a risk<br />
assessment.<br />
May be able to continue to work if the lesions can be covered with a<br />
dressing, do not impede hand hygiene and do not work with high risk<br />
patients (patients in oncology/ haematology, transplant and maternity<br />
units for e.g.)<br />
Healthcare workers with either a definite history <strong>of</strong> chickenpox/<br />
shingles or who have been vaccinated against varicella, should be<br />
considered protected and be allowed to continue working.<br />
If however they develop any symptoms consistent with chickenpox<br />
they should report to Occupational Health for assessment before<br />
having further patient contact.<br />
Healthcare workers without a definite history <strong>of</strong> chickenpox and who<br />
have not been vaccinated against it should report to their<br />
Occupational Health department before having further patient<br />
contact.<br />
May require to be excluded from contact with high-risk patients<br />
(patients in oncology/ haematology, transplant and maternity units for<br />
e.g.) until their immune status is known.<br />
Occupational Health can provide advice and take blood for<br />
serological testing where immunity is uncertain.<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Pregnant staff who have previously had chickenpox / were previously<br />
vaccinated against it are likely to be immune and at less risk;<br />
regardless they should discuss this with Occupational Health and<br />
their own Obstetrician/ Midwife without delay.<br />
Pregnant staff that have not had chickenpox / were not previously<br />
vaccinated against it may be at increased risk and should discuss<br />
this with Occupational Health and their own Obstetrician / Midwife<br />
without delay.<br />
• Occupational Health can provide advice and take blood for<br />
serological testing where immunity is uncertain.<br />
Should be discussed with the Occupational Health team.<br />
There is some evidence that varicella vaccine administered within<br />
three days <strong>of</strong> exposure may be effective in preventing chickenpox.<br />
Irrespective <strong>of</strong> the interval since exposure, vaccine should be <strong>of</strong>fered<br />
to reduce the risk <strong>of</strong> the healthcare workers being exposed /<br />
exposing patients to chickenpox virus in the future.<br />
Exceptions: <strong>Varicella</strong> vaccine is not suitable for pregnant or<br />
immunocompromised people.<br />
In pregnancy, treatment with immunoglobulin may be indicated; see<br />
section 7 for information and speak to Occupational Health and own<br />
Obstetrician/Midwife for guidance without delay.<br />
• Immunocompromised staff should speak to Occupational Health for<br />
advice. Sections 7 and 8 contain information regarding definitions<br />
and treatment with antivirals and / or immunoglobulin.<br />
Version No.1.8 December 2014 Page 14 <strong>of</strong> 19
<strong>Control</strong> <strong>of</strong> Chickenpox (<strong>Varicella</strong>) & Shingles (<strong>Herpes</strong> <strong>Zoster</strong>) Policy<br />
10. RESOURCE IMPLICATIONS<br />
There are no resource implications.<br />
11. COMMUNICATION PLAN<br />
This policy will be launched using the weekly staff briefing and will be accessible on<br />
Firstport.<br />
This policy will be discussed at the relevant management team meetings and the local<br />
partnership meetings.<br />
12. QUALITY IMPROVEMENT<br />
Compliance with this policy will be monitored by the <strong>Infection</strong> <strong>Control</strong> Team.<br />
13. EQUALITY AND DIVERSITY IMPACT ASSESSMENT<br />
This policy meets <strong>NHS</strong> <strong>Lanarkshire</strong>’s EDIA<br />
√<br />
(tick box)<br />
14. SUMMARY OF FREQUENTLY ASKED QUESTIONS (FAQS)<br />
If you have any questions about this policy or how to implement it, please contact the<br />
<strong>Infection</strong> <strong>Control</strong> Team to discuss your query.<br />
Version No.1.8 December 2014 Page 15 <strong>of</strong> 19
<strong>Control</strong> <strong>of</strong> Chickenpox (<strong>Varicella</strong>) & Shingles (<strong>Herpes</strong> <strong>Zoster</strong>) Policy<br />
15. Appendix 1 – Decision making aid for prescribing VZIG Prophylaxis<br />
YES to any<br />
INITIAL ASSESSEMENT<br />
Has the patient had a significant exposure to varicella or zoster (as per section 4 or 5 <strong>of</strong> CIM)?<br />
House hold contact<br />
Face to face exposure<br />
Open ward exposure<br />
AND was the exposure to a case:<br />
within 48 <strong>of</strong> the onset <strong>of</strong> rash until crusting <strong>of</strong> lesions (Chickenpox) OR<br />
between day <strong>of</strong> onset <strong>of</strong> rash until crusting (Shingles)<br />
NO to all<br />
Is the patient:<br />
Pregnant?<br />
Immunocompromised?<br />
A neonate/infant where:<br />
Mother has developed<br />
Chickenpox 7 days before or<br />
after delivery<br />
Neonate is antibody negative<br />
AND exposed to chickenpox<br />
or zoster in first 7 days <strong>of</strong> life<br />
Neonate requires intensive<br />
care?<br />
NO to all<br />
YES to any<br />
Patient (or mother in case <strong>of</strong> neonates) has<br />
a previous history <strong>of</strong> Chickenpox infection<br />
OR known antibody positive status?<br />
NO or UNCERTAIN<br />
YES<br />
Reassure patient. No further<br />
action required.<br />
Check antibody status (either stored booking blood (obstetrics) or fresh blood sample<br />
Antibody positive<br />
Antibody negative<br />
Reassure patient. No further<br />
action required.<br />
DISCUSS TREATMENT OPTIONS WITH PATIENT. IF<br />
PATIENT CONSENTS: Complete VZIG request form &<br />
proceed with administration within 10 days <strong>of</strong> exposure.<br />
Continue to observe for signs <strong>of</strong> rash.<br />
Version No.1.8 December 2014 Page 16 <strong>of</strong> 19
<strong>Control</strong> <strong>of</strong> Chickenpox (<strong>Varicella</strong>) & Shingles (<strong>Herpes</strong> <strong>Zoster</strong>) Policy<br />
16. Appendix 2 – <strong>Varicella</strong>-<strong>Zoster</strong> Immunoglobulin Pharmacy Request Form<br />
<strong>Varicella</strong>-<strong>Zoster</strong> Immunoglobulin (VZIG) Pharmacy Request Form<br />
VZIG is recommended for individuals who are at increased risk <strong>of</strong> severe<br />
chickenpox and who have NO antibodies to varicella–zoster virus (VZV) and who have<br />
had significant exposure * to chickenpox or shingles (herpes zoster).<br />
* See Section P <strong>of</strong> <strong>NHS</strong>L <strong>Control</strong> <strong>of</strong> <strong>Infection</strong> Manual or ‘The Green Book’ for full guidance<br />
Location<br />
Hospital VZIG Stock Process<br />
Wishaw Pharmacy Complete this form<br />
Hairmyres Pharmacy Complete this form<br />
Monklands Blood Bank Lab Contact directly<br />
Appropriate Use<br />
N.B. VZIG is rarely required urgently<br />
The aim <strong>of</strong> post-exposure VZIG administration is to protect individuals (pregnant, neonate, infant,<br />
immunocompromised patients) at high risk <strong>of</strong> suffering from severe chickenpox. The dose should be given<br />
within 10 days <strong>of</strong> exposure, preferably within normal working hours<br />
All requests must be discussed with an <strong>NHS</strong> <strong>Lanarkshire</strong> Consultant Microbiologist,<br />
Microbiology Speciality Doctor or ID Consultant prior to requesting stock release.<br />
Name <strong>of</strong> Consultant Microbiologist, Microbiology<br />
Speciality Doctor or ID Consultant authorising supply:<br />
Patient Details<br />
Addressograph<br />
Consultant/GP:<br />
Name:<br />
Speciality:<br />
CHI Number:<br />
Ward/Clinic:<br />
Date <strong>of</strong> Birth: Inpatient Outpatient *<br />
Please Circle<br />
Supply Details [Pharmacy Only]<br />
Number <strong>of</strong> VZIG<br />
250mg Vials Supplied:<br />
Batch Number:<br />
Expiry Date:<br />
Dispensed by:<br />
Date:<br />
Checked by:<br />
0-5 years - 250mg (one vial)<br />
6-10 years - 500mg (two vials)<br />
11-14 years - 750mg (three vials)<br />
15 years and over - 1000mg (four vials)<br />
Collected by[signature and block capitals]:<br />
Date:<br />
Version No.1.8 December 2014 Page 17 <strong>of</strong> 19
<strong>Control</strong> <strong>of</strong> Chickenpox (<strong>Varicella</strong>) & Shingles (<strong>Herpes</strong> <strong>Zoster</strong>) Policy<br />
17. REFERENCES AND BIBLIOGRAPHY<br />
British National Formulary (Feb 2014) http://www.bnf.org/bnf/index.htm<br />
Centers for Disease <strong>Control</strong> and Prevention: Chickenpox:<br />
http://www.cdc.gov/chickenpox/<br />
Centers for Disease <strong>Control</strong> and Prevention: Shingles:<br />
http://www.cdc.gov/shingles/index.html<br />
Health Protection Agency: Chickenpox<br />
http://www.hpa.org.uk/Topics/InfectiousDiseases/<strong>Infection</strong>sAZ/Chickenpox<strong>Varicella</strong><strong>Zoster</strong>/<br />
GeneralInformation/<br />
Health Protection Agency: Shingles<br />
http://www.hpa.org.uk/Topics/InfectiousDiseases/<strong>Infection</strong>sAZ/Shingles/GeneralInformatio<br />
nShingles/<br />
Health Protection Scotland (2012) <strong>Infection</strong> Prevention and <strong>Control</strong> Manual for Scotland<br />
http://www.documents.hps.scot.nhs.uk/hai/infection-control/ic-manual/ipcm-p-v2-3.pdf<br />
<strong>NHS</strong> GGC (2009) Chickenpox Policy:<br />
http://library.nhsggc.org.uk/mediaAssets/<strong>Infection</strong>%20<strong>Control</strong>/Chickenpox%20Policy%20-<br />
%2011.01.10.pdf<br />
<strong>NHS</strong> GGC (2011) Shingles Policy:<br />
http://library.nhsggc.org.uk/mediaAssets/<strong>Infection</strong>%20<strong>Control</strong>/26.07.11%20-<br />
%20Shingles%20V3.pdf<br />
<strong>NHS</strong> Scotland (2013) Protect yourself against Shingles.<br />
http://firstport2/staffsupport/immunisation/Documents/Shingles/Protect%20yourself%20against%20shingles_p<br />
atient%20leaflet.pdf<br />
Version No.1.8 December 2014 Page 18 <strong>of</strong> 19
<strong>Control</strong> <strong>of</strong> Chickenpox (<strong>Varicella</strong>) & Shingles (<strong>Herpes</strong> <strong>Zoster</strong>) Policy<br />
Public Health England (2013) The Green Book Chapter 28 Shingles.<br />
https://www.gov.uk/government/publications/shingles-herpes-zoster-the-green-bookchapter-28a<br />
Public Health England (2013) The Green Book Chapter 34 <strong>Varicella</strong>:<br />
https://www.gov.uk/government/publications/varicella-the-green-book-chapter-34<br />
Version No.1.8 December 2014 Page 19 <strong>of</strong> 19