The Brazilian Journal of Infectious Diseases - Sociedade Brasileira ...
The Brazilian Journal of Infectious Diseases - Sociedade Brasileira ...
The Brazilian Journal of Infectious Diseases - Sociedade Brasileira ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
BJID 2007; 11 (October) 1<br />
ISSN 1413-8670<br />
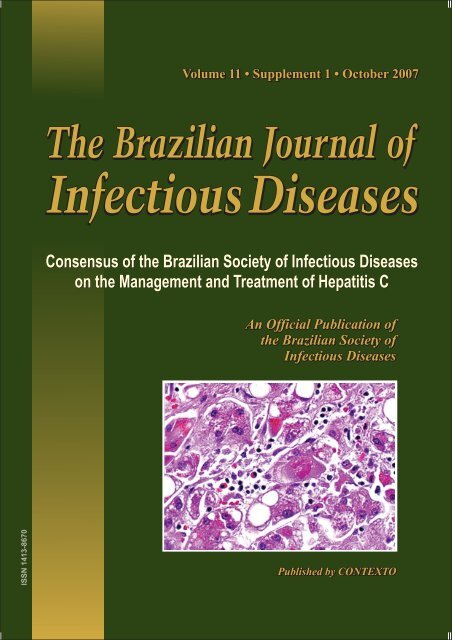
Volume 11 • Supplement 1 • October 2007<br />
THE BRAZILIAN JOURNAL OF<br />
INFECTIOUS DISEASES<br />
An Official Publication <strong>of</strong> the <strong>Brazilian</strong> Society <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong><br />
EDITOR<br />
Anastácio Q. Sousa<br />
Consensus <strong>of</strong> the <strong>Brazilian</strong> Society <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong><br />
on the Management and Treatment <strong>of</strong> Hepatitis C<br />
PUBLISHED BY CONTEXTO<br />
October 2007<br />
Printed in Brazil<br />
www.bjid.com.br
2 BJID 2007; 11 (October)<br />
THE BRAZILIAN SOCIETY OF INFECTIOUS DISEASES<br />
<strong>The</strong> <strong>Brazilian</strong> Society <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> is conducted for scientific purposes, for the advancement<br />
and promulgation <strong>of</strong> knowledge relevant to infectious diseases.<br />
OFFICERS<br />
2007-2008<br />
President<br />
João Silva de Mendonça<br />
Vice President<br />
Denise Vantil Marangoni<br />
First Secretary<br />
Juvêncio José D. Furtado<br />
Second Secretary<br />
Érico Antônio Gomes de Arruda<br />
First Treasurer<br />
Roberto Marcio da Costa Florim<br />
Second Treasurer<br />
Flávio de Queiroz Telles Filho<br />
Federal<br />
Federal<br />
Alagoas - Maria Raquel dos A.S. Guimarães<br />
Amazonas - Eucides Batista da Silva<br />
Bahia - Adriano Oliveira<br />
Ceará - Anastácio de Queiroz Sousa<br />
Distrito Federal - Dea Márcia da Silva M. Pereira<br />
Espírito Santo - Carlos Urbano Gonçalves Ferreira Jr.<br />
Goiás - Marcelo Cecílio Daher<br />
Maranhão - Graça Viana<br />
Mato Grosso do Sul - José Ivan de A. Aguiar<br />
Minas Gerais - Carlos Ernesto Ferreira Starling<br />
Pará - Helena Andrade Zeferino Brígido<br />
Paraíba - Luciana Holmes Simões<br />
Paraná - Alceu Fontana Pacheco Jr.<br />
Pernambuco - Martha Maria Romeiro F. Fonseca<br />
Piauí - Kelsen Dantas Eulálio<br />
Rio de Janeiro - J. Samuel Kierszembaum<br />
Rio Grande do Norte - Hênio Godeiro Lacerda<br />
Rio Grande do Sul - Luciano Goldani<br />
Rondônia - André Luis de Freitas Alves<br />
Santa Catarina - Silvia Cristina C. Flores<br />
São Paulo - Maria Luiza Moretti<br />
Sergipe - Márcia Maria Macedo Lima<br />
Tocantins - Hertz Ward de Oliveira<br />
www.bjid.com.br
BJID 2007; 11 (October) 3<br />
THE BRAZILIAN JOURNAL OF INFECTIOUS DISEASES<br />
An Official Publication <strong>of</strong> the <strong>Brazilian</strong> Society <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong><br />
EDITOR<br />
Anastácio Q. Sousa<br />
ASSOCIATE EDITORS<br />
Adauto Castelo (BR)<br />
André Villela Lomar (BR)<br />
Antônio C. Pignatari (BR)<br />
Carlos Brites Alves (BR)<br />
Hélio Sader (BR)<br />
João Silva de Mendonça (BR)<br />
Márcio Nucci (BR)<br />
Roberto Badaró (BR)<br />
Roberto Focaccia (BR)<br />
EDITORIAL BOARD<br />
Achilea L. Bittencourt (BR)<br />
Antônio Alci Barone (BR)<br />
Antônio Andrade (BR)<br />
Antônio Campos Neto (BR)<br />
Antônio Carlos Nicodemo (BR)<br />
Arnaldo Colombo (BR)<br />
Caio Mendes (BR)<br />
Celso Ramos Filho (BR)<br />
Cláudio Sérgio Pannuti (BR)<br />
Dirceu Grecco (BR)<br />
Edgard Marcelino de Carvalho (BR)<br />
Eduardo Netto (BR)<br />
Érico Antônio Gomes de Arruda (BR)<br />
Esper Georges Kallas (BR)<br />
Eurico de Arruda Neto (BR)<br />
Flávia Rossi (BR)<br />
Guido Levi (BR)<br />
Henry Masur (US)<br />
Jeffrey Shaw (BR)<br />
John R. David (US)<br />
Jorge Arias (BR)<br />
Jorge Luiz Nobre Rodrigues(BR)<br />
Jorge Luiz Sampaio (BR)<br />
José Wellington Oliveira Lima (BR)<br />
Kleber Luz (BR)<br />
Marcelo Ferreira (BR)<br />
Marcos Antônio de Ávila Vitória (BR)<br />
Maria Aparecida Shikanai Yasuda (BR)<br />
Maria Rita Elmor (BR)<br />
Mark Wainberg (CA)<br />
Mauro Schechter (BR)<br />
Mitermayer Galvão dos Reis (BR)<br />
Naftale Katz (BR)<br />
Raimundo Paraná (BR)<br />
Reinaldo Salomão (BR)<br />
Ricardo Diaz (BR)<br />
Richard Guerrant (US)<br />
Richard Locksley (US)<br />
Richard B. Roberts (US)<br />
Robério Dias Leite (BR)<br />
Robert Schooley (US)<br />
Rod Hay (GB)<br />
Rodolfo Teixeira (BR)<br />
Rogério de J. Pedro (BR)<br />
Selma Maria Bezerra Jerônimo (BR)<br />
Sérgio Cimerman (BR)<br />
Sérgio Coutinho (BR)<br />
Sylvia Lemos Hinrichsen (BR)<br />
Timothy Inglis (AUS)<br />
Warren D. Johnson, Jr. (US)<br />
Zilton Andrade (BR)<br />
PRODUCTION STAFF<br />
Luciana Bastianelli, Managing Editor<br />
Andréia Lima, Submissions Manager<br />
Taís Cupertino, Secretary<br />
www.bjid.com.br
4 BJID 2007; 11 (October)<br />
<strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong><br />
<strong>Diseases</strong> is an <strong>of</strong>ficial publication <strong>of</strong> the <strong>Brazilian</strong><br />
Society <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> and is published bimonthly<br />
by Contexto - Rua Alfredo Magalhães, 04/<br />
Barra, 40140-140, Salvador-Bahia-Brazil. <strong>The</strong><br />
editorial <strong>of</strong>fices are at Contexto.<br />
Editorial Office<br />
Correspondence concerning subscriptions,<br />
advertisements, claims for missing issues, changes <strong>of</strong><br />
address and communications to the editors should be<br />
addressed to Dr. Anastácio Q. Sousa, <strong>The</strong> <strong>Brazilian</strong><br />
<strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> - BJID, Rua Alfredo<br />
Magalhães, 04/Barra, 40140-140, Salvador-Bahia-<br />
Brazil; phone: (55 71) 3264-2971; fax (55 71) 3264-<br />
3326; or should be sent by e-mail: bjid@bjid.com.br.<br />
Contributors please consult the Instructions for<br />
Authors in this issue or visit www.bjid.com.br<br />
Sponsors<br />
This supplement was supported by:<br />
• Produtos Roche Químicos e Farmacêuticos S/A<br />
• Schering-Plough do Brasil<br />
<strong>The</strong> opinions expressed in this publication are those<br />
<strong>of</strong> the authors and are not attributable to the<br />
sponsors or to the publisher, editor, associate<br />
editors, or editorial board <strong>of</strong> <strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong><br />
<strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong>.<br />
COVER: Liver cells infected with the hepatitis C virus.<br />
Permissions<br />
Copyright 2007 by <strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong><br />
<strong>Infectious</strong> <strong>Diseases</strong> and Contexto Publishing. All rights<br />
reserved. Except as authorized in the accompanying<br />
statement, no part <strong>of</strong> the BJID may be reproduced in<br />
any form or by any electronic or mechanical means,<br />
including information storage and retrieval systems,<br />
without the publisher's written permission.<br />
Authorization to photocopy items for internal or<br />
personal use, or the internal or personal use by specific<br />
clients is granted by <strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong><br />
<strong>Diseases</strong> and Contexto Publishing for libraries and<br />
other users. This authorization does not extend to<br />
other kinds <strong>of</strong> copying such as copying for general<br />
distribution, for advertising or promotional purposes,<br />
for creating new collective works, or for resale.<br />
Postmaster<br />
Send address changes to BJID, Rua Alfredo<br />
Magalhães, 04/Barra, 40140-140, Salvador-Bahia-Brazil.<br />
Subscriptions<br />
Subscription rates (1 year) for <strong>The</strong> <strong>Brazilian</strong><br />
<strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> (BJID):<br />
Domestic Foreign<br />
(R$) (US$)<br />
Individuals 100 100<br />
Institutions 150 150<br />
Special* 60 60<br />
*Students, interns, residents and fellows.<br />
Information by Contexto:<br />
Home-page: www.bjid.com.br. E-mail: bjid@bjid.com.br<br />
Phone/Fax: (55 71) 3264-2971 / 3264-3326.<br />
© 2007 by <strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> and<br />
Contexto Publishing. All rights reserved.<br />
Now Indexed in INDEX MEDICUS/PUBMED/MEDLINE,<br />
EMBASE/EXCERPTA MEDICA, LATINDEX, LILACS,<br />
SUBIS DATABASE, SIIC, SCIELO, CAS, SOCIEDAD<br />
IBEROAMERICANA DE INFORMACIÓN CIENTIFICA,<br />
ELSEVIER SCIENCE - BIBLIOGRAPHIC DATABASES<br />
DIVISION, CABI PUBLISHING, ULRICH’S<br />
PERIODICALS DIRECTORY<br />
www.bjid.com.br
BJID 2007; 11 (October) 5<br />
THE<br />
BRAZILIAN<br />
JOURNAL<br />
OF INFECTIOUS<br />
DISEASES<br />
Volume 11 • Supplement 1 October 2007<br />
Consensus <strong>of</strong> the <strong>Brazilian</strong> Society <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong><br />
on the Management and Treatment <strong>of</strong> Hepatitis C ........... 1<br />
<strong>Brazilian</strong> Society <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> HCV Consensus Group<br />
Epidemiological Aspects <strong>of</strong> Hepatitis C in Brazil .............. 6<br />
Decio Diament<br />
Sexual Transmission <strong>of</strong> HCV ............................................. 8<br />
Kleber Dias do Prado<br />
Hepatitis C Virus Perinatal Transmission ......................... 10<br />
Umbeliana Barbosa de Oliveira<br />
Hepatitis C: Virological Aspects and Practical<br />
Implications .................................................................... 12<br />
Antonio Alci Barone<br />
Pathogenesis <strong>of</strong> Hepatitis C – HCV Consensus 2007 ...... 14<br />
Ana Tereza R. Viso<br />
Antifibrotic <strong>The</strong>rapy in Chronic Hepatitis C .................... 20<br />
Rinaldo Focaccia Siciliano and Antonio Alci Barone<br />
Laboratory Testing for Hepatitis C ..................................21<br />
Neiva Sellan Lopes Gonçales and Fernando Lopes Gonçales Junior<br />
Hepatitis C: Genotyping ................................................... 25<br />
Norma de Paula Cavalheiro<br />
Noninvasive Means <strong>of</strong> Diagnosing Liver Fibrosis in<br />
Hepatitis C ......................................................................28<br />
Eduardo Sellan Lopes Gonçales, Adriana Flávia Feltrim Angerami<br />
and Fernando Lopes Gonçales Junior<br />
Chronic Hepatitis C: Pathological Anatomy .....................32<br />
Evandro Sobroza de Mello and Venâncio Avancini Ferreira Alves<br />
Co-Infection with Hepatitis B Virus and Hepatitis C<br />
Virus ................................................................................ 37<br />
Heloísa Pedrosa Mitre and João Silva de Mendonça<br />
Co-Infection with Hepatitis C Virus and Human T Lymphocyte<br />
Virus .................................................................................40<br />
Carlos Brites Alves<br />
Basic Guidelines for the Treatment <strong>of</strong> HIV/HVC Co-<br />
Infection ......................................................................... 42<br />
Edgard De Bortholi<br />
Basic Aspects <strong>of</strong> the Treatment for Hepatitis C: Mechanisms<br />
<strong>of</strong> Action <strong>of</strong> Interferon Alpha and Ribavirin and the Bases <strong>of</strong><br />
Individualization ..............................................................47<br />
Carlos Eduardo de Melo, Evaldo Stanislau Affonso de Araújo and<br />
Antonio Alci Barone<br />
<strong>The</strong>rapeutic Approach to Acute Hepatitis C ...................49<br />
Rodrigo Nogueira Angerami and Fernando Lopes Gonçales Júnior<br />
Treatment <strong>of</strong> Chronic Hepatitis C in Treatment-Naïve<br />
Patients ........................................................................... 53<br />
Marcelo Simão Ferreira<br />
Retreatment <strong>of</strong> Hepatitis C Patients Who Previously<br />
Experienced Treatment Failure ......................................... 58<br />
Fernando Lopes Gonçales Jr.<br />
Maintenance Treatment for the Modulation <strong>of</strong> Liver<br />
Fibrosis ........................................................................... 60<br />
Evaldo Stanislau Affonso de Araújo and Antonio Alci Barone<br />
Treatment <strong>of</strong> Patients Infected with Hepatitis C Virus and<br />
Presenting Extrahepatic Manifestations ..........................64<br />
Fátima Mitiko Tengan1 and Antonio Alci Barone<br />
Hepatitis C Treatment Before and After Liver<br />
Transplant..................................................................... 69<br />
Edson Abdala, Daniela Rosa Magalhães Gotardo, Patrícia Rodrigues<br />
Bonazzi and Telésforo Bacchella<br />
Adverse Event Management ...........................................74<br />
Aline Gonzalez Vigani<br />
Treatment Options in the Management <strong>of</strong> Thrombocytopenia<br />
in Patients Infected with HCV .......................................... 79<br />
André Cosme de Oliveira<br />
<strong>The</strong>rapeutic Perspectives for Hepatitis C......................... 81<br />
Evaldo Stanislau Affonso de Araújo, Antonio Alci Barone and Jean-<br />
Michel Pawlotsky<br />
Instructions for Authors<br />
Statement <strong>of</strong> Editorial Policy<br />
Checklist for Submitted Manuscripts<br />
www.bjid.com.br
6 BJID 2007; 11 (October)<br />
BJID on line<br />
<strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> (BJID) is<br />
now present in a new Web Site: www.bjid.com.br. <strong>The</strong><br />
BJID is an <strong>of</strong>ficial publication <strong>of</strong> <strong>The</strong> <strong>Brazilian</strong> Society<br />
<strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> and it is a vehicle for original<br />
publications in this field. <strong>The</strong> BJID is published bimonthly<br />
by Contexto Publishing (Salvador/BA, Brazil)<br />
since 1997. <strong>The</strong> aim <strong>of</strong> this site is to familiarize visitors<br />
with BJID' contents by providing online subscriptions,<br />
review process, submission process, abstracts, past<br />
publications, and extend the BJID´s instructions for<br />
authors to infectious-disease specialists worldwide. Full<br />
instructions for authors are provided in English and<br />
Portuguese. This new website is divided into the<br />
following sections:<br />
Home (A new design was established for BJID,<br />
including spaces for advertising)<br />
Editors (This section includes all the editorial board<br />
<strong>of</strong> BJID)<br />
Subscriptions (In this section, the visitor could<br />
subscribe the BJID online)<br />
Instructions to Authors (This section is in Portuguese<br />
and in English, and can help the authors who want<br />
to submit papers to BJID to follow. <strong>The</strong>re are the<br />
rules for publishing in the <strong>Journal</strong>).<br />
Index Listing (<strong>The</strong> visitors can check the status <strong>of</strong><br />
the BJID in the medicus indexa round the world. In<br />
a nearly future, we will include a service to check<br />
the impact <strong>of</strong> each article published in BJID)<br />
Abstracts (<strong>The</strong> visitors have free access to the<br />
abstracts <strong>of</strong> the current year. For example: every<br />
each issue, the abstracts will be available to be<br />
consulted. If the visitors would like the full text, they<br />
need to ask the permission to our <strong>of</strong>fice).<br />
Publications (In this section, it will be available the<br />
full text <strong>of</strong> last volumes 1997 to 2003 in pdf format)<br />
Sponsors (This space is reserved to the advertising<br />
board <strong>of</strong> the BJID and the institutions that support<br />
the <strong>Journal</strong>. <strong>The</strong> visitors can be addressed directly to<br />
the sponsor they want by a link)<br />
About us (This section inform the visitors about the<br />
production staff <strong>of</strong> the <strong>Journal</strong>, the address, phone<br />
number, e-mail, and the contacts <strong>of</strong> the BJID)<br />
Links (Interesting links about infectious diseases and<br />
institutions)<br />
This website reserved a new space to the authors<br />
who have already submitted papers to the <strong>Journal</strong><br />
and/or those have papers in the submission process<br />
in BJID with the following sections:<br />
On-line Submission Process (<strong>The</strong> authors now could<br />
send the papers by e-mail, following the specific rules<br />
described in this section. Also, the authors now can<br />
consult the review process <strong>of</strong> the submitted articles<br />
via on-line. Immedialely after the submission <strong>of</strong> the<br />
article, the main author will receive a login and a<br />
password, with which the author will be able to<br />
consult the status <strong>of</strong> the article. If other authors want<br />
to check the status <strong>of</strong> their article via on-line, they<br />
can also register a proper login and password.<br />
On-line Review Process (<strong>The</strong> reviewers now can<br />
receive the article and make all the edition process<br />
by internet. <strong>The</strong> reviewer will receive a message<br />
with a login an a password. With them, he could<br />
access the entire article. After he comments in a<br />
specific form, it will be sent to the author<br />
automatically. <strong>The</strong> authors now can consult the<br />
review process <strong>of</strong> the submitted articles via online.<br />
Immediately after the submission <strong>of</strong> the article,<br />
the main author will receive a login and a password,<br />
with which the author will be able to consult the<br />
status <strong>of</strong> the article. If other authors want to check<br />
the status <strong>of</strong> their article via on-line, they can also<br />
register a proper login and password.<br />
www.bjid.com.br
BJID 2007; 11 Supplement 1 (October) 1<br />
Consensus <strong>of</strong> the <strong>Brazilian</strong> Society <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong><br />
on the Management and Treatment <strong>of</strong> Hepatitis C<br />
Evaldo Stanislau Affonso de Araújo, João Silva Mendonça, Antonio Alci Barone, Fernando Lopes Gonçales Junior, Marcelo<br />
Simão Ferreira*, Roberto Focaccia, Jean-Michel Pawlotsky§* and <strong>Brazilian</strong> Society <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> HCV Consensus Group<br />
Each year, and every day, the results <strong>of</strong> clinical trials and basic research provide us with a great deal <strong>of</strong> new<br />
information regarding viral hepatitis. We on the Viral Hepatitis Committee <strong>of</strong> the <strong>Sociedade</strong> <strong>Brasileira</strong> de Infectologia<br />
(SBI, <strong>Brazilian</strong> Society <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong>) have been working to standardize the major issues surrounding dayto-day<br />
practice in treating patients infected with the hepatitis B or C virus (HBV or HCV). We have decided to<br />
address, in alternate years, HBV, together with hepatitis delta (HDV), and HCV, in our annual ‘Consensus’ on<br />
clinical management. Last year, we published the first HBV Consensus (BJID, 2007 (11):2-6). This year, we submit<br />
our HCV Consensus,<br />
which primarily serves to<br />
update the 2002 and 2004<br />
SPI Consensuses. We<br />
distributed the principal<br />
topics among the Committee<br />
members, revised their<br />
work and compiled it into a<br />
Proceedings Supplement<br />
(to be published together<br />
with the BJID), which<br />
elucidates the highlights <strong>of</strong><br />
the Consensus. A deeper<br />
review was written and<br />
referenced (it is our advice<br />
to the reader to read the<br />
Proceedings as well). A<br />
meeting was then held in<br />
Mogi das Cruzes in order<br />
to discuss, in a very practical<br />
and directed way, the<br />
issues most relevant to the<br />
Consensus, from public<br />
policies to the most complex<br />
therapeutic points. <strong>The</strong><br />
results are summarized in a<br />
question/answer, topic/<br />
statement format in this issue<br />
<strong>of</strong> the BJID. <strong>The</strong> main<br />
Figure 1. HCV Consensus Group.<br />
message <strong>of</strong> our statement was<br />
that we need to have the<br />
courage to act in favor <strong>of</strong> life.<br />
Many <strong>of</strong> us have adopted certain practices based on very new knowledge despite a lack <strong>of</strong> formal or <strong>of</strong>ficial policies<br />
to support such practices. Some <strong>of</strong> us have been awaiting new compounds while patients are dying <strong>of</strong> chronic liver<br />
diseases. Unfortunately, the news from the battlefield is not so good. New compounds have been very disappointing<br />
(low potency, viral resistance, ineffective without interferon and various side effects, some serious). It is also difficult<br />
to incorporate new policies into everyday practice. However, strategies such as optimizing the use <strong>of</strong> pegylated<br />
interferon/ribavirin and encouraging treatment compliance, as well as finding new ways to monitor and slow liver<br />
disease progression, are effective and should be put into practice. Most importantly, the low-dose maintenance <strong>of</strong><br />
pegylated interferon seems to be very promising, and the use <strong>of</strong> interferon alpha has saved lives. That is why we<br />
choose to expound upon what we believe to be the current standard <strong>of</strong> care and the gold standard for dealing with<br />
this hard to treat virus, as well as with the chronic complications <strong>of</strong> HCV infection. Our position will be re-evaluated<br />
over the next two years. Until then, we are confident that our guide will be <strong>of</strong> great value to the readers. Finally, we<br />
would like to thank Roche and Schering Plough for the educational grants provided to the SBI. However, we must<br />
stress that neither company attempted to influence any <strong>of</strong> the decisions made by our consensus group.<br />
<strong>The</strong> <strong>Brazilian</strong> Society <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> HCV Consensus Group<br />
Social and Collective Impact <strong>of</strong> the Decision-Making Process<br />
Serologic triage for hepatitis C virus (HCV): When and how?<br />
Diagnosis ‘campaigns’? Most vulnerable groups?<br />
It is recommended that detection ‘campaigns’ be carried<br />
out for more vulnerable groups 1 , individuals in certain<br />
#<strong>Brazilian</strong> Society <strong>Infectious</strong> <strong>Diseases</strong> HCV Consensus Group: Ana<br />
Tereza Rodrigues Viso, Aline Vigani, André Cosme Oliveira, Carlos<br />
Eduardo de Melo, Carlos Brites Alves, Décio Diament, Edson Abdala,<br />
Edgard De Bortholi, Evandro Sobroza de Mello, Eduardo Sellan<br />
Gonçalves, Fátima Mitiko Tengan, Heloísa Pedrosa Mitre*, Kleber<br />
Dias Prado, Neiva Sellan Gonçales, Norma de Paula Cavalheiro, Rinaldo<br />
Focaccia Siciliano, Rodrigo Nogueira Angerami*, Umbeliana Barbosa<br />
de Oliveira, Venâncio Avancini Ferreira Alves*. § Special guest. *Members<br />
who did not participate <strong>of</strong> the Consensus Meeting occurred in the Blue<br />
Tree Park Hotel, Mogi das Cruzes/SP, on August 25 th -26 th , 2007.<br />
occupations (health pr<strong>of</strong>essionals, technicians whose work<br />
potentially puts them in contact with blood), institutionalized<br />
individuals (prisoners, under-age felons, etc.), and the family<br />
members <strong>of</strong> patients with hepatitis C, as well as those infected<br />
with HIV. We emphasize that such individuals should be clearly<br />
informed that the triage diagnosis should be confirmed by a<br />
method with more sensitivity and specificity, as well as that<br />
confirmation <strong>of</strong> the diagnosis will not necessary imply<br />
treatment <strong>of</strong> the infection. Age is a factor to be considered,<br />
1<br />
History <strong>of</strong> blood product transfusion, history <strong>of</strong> major surgery, unsafe<br />
parenteral exposure (reusable syringes, sharing <strong>of</strong> utensils during the<br />
use <strong>of</strong> licit or illicit injected substances, undergoing diagnostic or esthetic<br />
therapeutic procedures involving reusable or inadequately sterilized<br />
material, e.g., tattoo, acupuncture, piercing, manicure, dental<br />
treatment, etc.), and sharing <strong>of</strong> utensils during the use <strong>of</strong> inhaled drugs.<br />
www.bjid.com.br
2 Consensus <strong>of</strong> Hepatitis C Carried Out by SBI<br />
BJID 2007; 11 Supplement 1 (October)<br />
since older people are more likely to have been exposed to the<br />
disease over the course <strong>of</strong> their lifetime.<br />
<strong>The</strong> infected health pr<strong>of</strong>essional: are their activities restricted<br />
in any way?<br />
A priori, the activity <strong>of</strong> health pr<strong>of</strong>essionals with<br />
hepatitis C should not be restricted. However, strict<br />
application and educational measures are recommended<br />
regarding the biosafety guidelines, and it should be noted<br />
that more data are needed before a definitive<br />
recommendation can be made.<br />
Is hepatitis C a sexually transmitted disease (STD)?<br />
Although hepatitis C is not conceptually an STD, sexual<br />
transmission is possible, albeit uncommon, and the risk <strong>of</strong><br />
such transmission increases when the individual presents<br />
genital lesions or HIV positivity, as well as when the<br />
individual engages in risky sexual behavior. In such<br />
situations, the use <strong>of</strong> condoms is recommended.<br />
Heterosexual monogamous couples who present<br />
discrepant serologic results can use condoms <strong>of</strong> their own<br />
accord after being properly instructed. We would like to<br />
issue a warning regarding the risk <strong>of</strong> transmission in the<br />
household through the communal use <strong>of</strong> utensils<br />
contaminated with blood.<br />
Hepatitis C during pregnancy and childbirth: To get pregnant<br />
or not? Cesarean or vaginal delivery? Breastfeeding?<br />
Pregnancy is not contraindicated in women <strong>of</strong><br />
childbearing age infected with HCV, although<br />
contraindications related to the period <strong>of</strong> treatment should<br />
be respected. Regarding the type <strong>of</strong> delivery, the decision<br />
should be made by an obstetrician. It should be noted,<br />
however, that a high viral load <strong>of</strong> HCV can be a relevant<br />
factor in this decision. Nevertheless, at the present, we<br />
cannot recommend a definitive course <strong>of</strong> action.<br />
Breastfeeding is allowed, although the nipple should be<br />
carefully prepared, and breastfeeding should be<br />
discontinued if fissures appear or bleeding occurs. Pregnant<br />
women coinfected with HCV and HIV present a clearly<br />
greater risk <strong>of</strong> perinatal HCV transmission and therefore<br />
constitute an exception to these permissions.<br />
Prevention<br />
Unapparent HCV transmission in society and in the health<br />
care environment: What should we recommend to Health<br />
Oversight Agencies?<br />
We recommend extremely rigorous inspection <strong>of</strong> health<br />
and esthetic institutes, as well as continuing education<br />
<strong>of</strong> the pr<strong>of</strong>essionals who work in this area. We should<br />
also emphasize the need for ongoing education <strong>of</strong> health<br />
pr<strong>of</strong>essionals at all levels <strong>of</strong> patient care – from basic care<br />
to highly complex treatments.<br />
Vaccines: Which and when?<br />
Susceptible individuals with hepatitis C should be<br />
vaccinated against hepatitis A and B. <strong>The</strong>re is a real need to<br />
make vaccines against hepatitis A available in the public health<br />
care system.<br />
<strong>The</strong> Laboratory in the Era <strong>of</strong> Individualized Treatment<br />
Quantification <strong>of</strong> viral loads for all genotypes?<br />
Yes, it is recommended that the viral load <strong>of</strong> all patients be<br />
quantified.<br />
Which quantification method should be used?<br />
It is recommended that the method used be reproducible,<br />
be sensitive, and present ample linearity.<br />
‘Moments <strong>of</strong> decision’: At baseline (One measurement?<br />
When? Several measurements?), as well as at weeks 4, 12, and<br />
24; end-<strong>of</strong>-treatment response (ETR), sustained virologic<br />
response (SVR)...What else?<br />
Baseline viral load should be determined prior to but as<br />
close as possible to the initiation <strong>of</strong> the treatment. It can be<br />
determined only once provided that the test is performed<br />
under ideal technical conditions. At week 4, the same test will<br />
be qualitative in order to define the presence <strong>of</strong> rapid virologic<br />
response (RVR), defined as the detection <strong>of</strong> no viral RNA. At<br />
week 12, it should be quantitative, adopting the criteria <strong>of</strong> no<br />
early virologic response (EVR) (a drop in viral load ≤ 2log10),<br />
partial EVR (drop ≥ 2log10), and complete EVR (no viral RNA<br />
detected). At week 24, the test will be qualitative. If viral RNA<br />
is detected, the treatment instituted exclusively for virologic<br />
purposes will have to be interrupted. Determination <strong>of</strong> the<br />
ETR – emphasizing the differences in duration in different<br />
genotypes and patients – as well as <strong>of</strong> the SVR, must be<br />
qualitative. <strong>The</strong> SVR should be determined at 24 weeks after<br />
the end <strong>of</strong> the treatment.<br />
It should be noted that monitoring will be unnecessary<br />
during the treatment in the cases in which RVR occurred and<br />
adequate treatment compliance is maintained.<br />
‘Week 12’ SVR?<br />
Determination <strong>of</strong> the SVR at 12 weeks after the end <strong>of</strong> the<br />
treatment is not currently considered a useful or valid measure.<br />
Metabolic alterations: Homeostasis model assessment<br />
(HOMA) and glucose tolerance test: when to order, how to<br />
interpret<br />
Various studies indicate the role <strong>of</strong> hepatitis C as a factor<br />
implicated in the development <strong>of</strong> type 2 diabetes in patients at<br />
high risk (male gender, over 40 years <strong>of</strong> age, and overweight).<br />
In experimental models, HCV was found to induce insulin<br />
resistance, including increased production <strong>of</strong> tumor necrosis<br />
factor as one <strong>of</strong> the contributing factors. Insulin resistance is<br />
also associated with the development <strong>of</strong> steatosis and<br />
progression <strong>of</strong> liver fibrosis, principally in patients infected<br />
with HCV genotype 1. <strong>The</strong>refore, there seems to be an<br />
association between insulin resistance and the characteristics<br />
associated with patients presenting a worse response to the<br />
hepatitis C treatment: cirrhosis, obesity, concomitant infection<br />
with HIV (taking antiretroviral drugs), etc.<br />
In summary: HCV promotes insulin resistance, which leads<br />
to steatosis, fibrosis, and resistance to treatment with<br />
interferon alpha (IFN-α).<br />
<strong>The</strong> HOMA mathematical model [(serum levels <strong>of</strong> fasting<br />
insulin vs. serum levels <strong>of</strong> fasting glucose)/22.5] has proven<br />
useful in the evaluation <strong>of</strong> sensitivity to insulin; however, it<br />
www.bjid.com.br
BJID 2007; 11 Supplement 1 (October) Consensus <strong>of</strong> Hepatitis C Carried Out by SBI<br />
3<br />
has not been completely standardized for all clinical situations,<br />
which is why its routine use is not recommended, except in<br />
the situations that will be reviewed now (metabolic alterations)<br />
and in the Proceedings.<br />
Noninvasive monitoring <strong>of</strong> fibrosis<br />
Value <strong>of</strong> simplicity: Thrombocytopenia as a marker <strong>of</strong> liver<br />
cirrhosis<br />
Thrombocytopenia in an individual with hepatitis C<br />
indicates moderate to severe liver fibrosis. <strong>The</strong> sensitivity <strong>of</strong><br />
this diagnostic marker <strong>of</strong> advanced fibrosis increases when it<br />
is used in combination with other biochemical tests, such as<br />
determination <strong>of</strong> the aspartate aminotransferase to platelet<br />
ratio index, calculated using the formula: aspartate<br />
aminotransferase/alanine aminotransferase ratio + platelets.<br />
When is it indicated?<br />
Noninvasive monitoring <strong>of</strong> liver fibrosis should be performed<br />
in cases <strong>of</strong> (i) contraindication or difficult access to liver biopsy,<br />
(ii) the need for such monitoring in order to hasten the performance<br />
<strong>of</strong> a new biopsy in patients at greater risk <strong>of</strong> progression<br />
(immunocompromised patients) or in individuals presenting<br />
stage F1 fibrosis, and (iii) in patients with liver cirrhosis under<br />
treatment for modulation <strong>of</strong> fibrosis (IFN maintenance).<br />
How to measure: Serum panels vs. Fibroscan<br />
Sensitivity and positive predictive value are increased by<br />
combining the methods.<br />
Liver biopsy is dead. . . Long live liver biopsy!<br />
Biopsy for all genotypes? And for all patients?<br />
Yes, except for clinical contraindications, the biopsy<br />
should be performed for all patients presenting detectable<br />
levels <strong>of</strong> HCV RNA.<br />
<strong>The</strong> central issue is the absolute need for the biopsy sample<br />
to be representative <strong>of</strong> the hepatic parenchyma, since<br />
inappropriate biopsies frequently result in understaging <strong>of</strong><br />
the disease. It is highly recommended that a needle biopsy be<br />
performed (wedge biopsies produce subcapsular samples that<br />
cannot be used in the staging <strong>of</strong> fibrosis nor in the staging <strong>of</strong><br />
inflammation); needles that produce very thin biopsies highly<br />
limit architectural staging and should not be used. Trucut 14-<br />
gauge needles or needles that produce samples <strong>of</strong> equivalent<br />
diameter, measuring at least 1.5 cm long and/or 10 represented<br />
portspaces, are recommended. If the biopsy is performed<br />
during a surgical procedure, it should be done at the outset <strong>of</strong><br />
the procedure in order to avoid the artifacts that surgery can<br />
produce in the liver tissue.<br />
<strong>The</strong> biopsy report should include a staging system and<br />
scoring (METAVIR or SBP, preferably). It should be noted,<br />
however, that the pattern <strong>of</strong> inflammatory alterations (portal,<br />
interface, and lobular components) should be described in<br />
detail, since it has become increasingly important in predicting<br />
the evolution <strong>of</strong> the disease as well as in the differential<br />
diagnosis with other diseases. In addition, the principal role<br />
<strong>of</strong> biopsy is to rule out other liver diseases – steatohepatitis<br />
(alcoholic or nonalcoholic), for example, frequently co-exists<br />
with hepatitis C and is known to have a significant impact on<br />
the evolution <strong>of</strong> the disease.<br />
Value <strong>of</strong> the imaging and serum level methods in the diagnosis<br />
<strong>of</strong> liver fibrosis: who needs endoscopy?<br />
Prior to biopsy, patients with indirect evidence <strong>of</strong> portal<br />
hypertension (ultrasonographic signs, thrombocytopenia)<br />
should be submitted to endoscopy <strong>of</strong> the upper digestive tract<br />
for detection <strong>of</strong> esophageal varicose veins that would render a<br />
liver biopsy unnecessary in the diagnosis <strong>of</strong> liver cirrhosis.<br />
Clinical Management in Borderline Situations<br />
Portal hypertension in clinical practice: Clinical management<br />
<strong>of</strong> pretreatment thrombocytopenia<br />
<strong>The</strong>re is no conclusive evidence on the management <strong>of</strong><br />
pretreatment thrombocytopenia; however, some alternatives<br />
can be considered and are reviewed in the Proceedings.<br />
Liver transplant in clinical practice: post-transplant limitations.<br />
Fibrogenesis, treatment after transplant, rejection control and<br />
live donor<br />
Liver disease caused by HCV corresponds to almost half<br />
<strong>of</strong> the indications for liver transplant. Currently, in Brazil, the<br />
distribution <strong>of</strong> the organ follows a criterion <strong>of</strong> severity, using<br />
the model for end-stage liver disease (MELD). After the<br />
transplant, up to 80% <strong>of</strong> the patients experience histologic<br />
recurrence, and the pre-transplant viral load is one <strong>of</strong> the most<br />
significant risk factors. For this reason, pre-transplant<br />
treatment should always be considered, even in patients with<br />
decompensated cirrhosis, provided that the treatment is given<br />
in a specialized center and with an active transplant treatment<br />
team. Post-transplant treatment for chronic hepatitis is<br />
generally indicated when fibrosis is ≥ 2 or when periportal<br />
activity is ≥ 3. Although the duration <strong>of</strong> treatment should be<br />
at least 48 weeks, it should be individualized according to the<br />
virologic response pr<strong>of</strong>ile.<br />
Treatment<br />
Nondrug and nonspecific HCV treatment: metabolic syndrome,<br />
nonalcoholic steatohepatitis, diabetes, obesity – evidence for<br />
the use <strong>of</strong> diet, hypolipidemic agents, and antidiabetic<br />
medication<br />
It is recommended that the conditions associated with<br />
worsening <strong>of</strong> liver fibrosis and lower SVR rate, such as obesity,<br />
type 2 diabetes, nonalcoholic steatohepatitis, steatosis,<br />
dyslipidemia, and metabolic syndrome, be brought under<br />
control before antiviral treatment is instituted.<br />
Patients with concomitant diseases; how to use IFN-α and<br />
specific measures for drug users and patients with mental<br />
disease. Socially marginalized individuals and prisoners.<br />
Individuals with kidney disease in pre- and post-kidney<br />
transplant phases. Individuals with auto-immune disease and<br />
extrahepatic manifestations<br />
At facilities where a multipr<strong>of</strong>essional approach is taken or at<br />
specialized centers, both <strong>of</strong> which allow appropriate monitoring<br />
and control <strong>of</strong> all clinical situations <strong>of</strong> the underlying disease, as<br />
well as <strong>of</strong> those potentiated or triggered by HCV treatment, it is<br />
recommended that HCV treatment be instituted first. It is<br />
noteworthy that, in the case <strong>of</strong> auto-immune manifestations<br />
(cryoglobulinemia and auto-immune hepatitis in particular),<br />
treatment for HCV should be given – observing the premises<br />
www.bjid.com.br
4 Consensus <strong>of</strong> Hepatitis C Carried Out by SBI<br />
BJID 2007; 11 Supplement 1 (October)<br />
above. Corticosteroids and other immunosuppressants can be<br />
used concomitantly when indicated.<br />
Ribavirin: Always a full dose? And how much (0.8 g, 1 g, 11<br />
mg/kg/day, 15 mg/kg/day)?<br />
Ribavirin should always be given in a full dose. <strong>The</strong><br />
recommended dose is 15 mg/kg/day or 1 g for patients who<br />
weigh < 75 kg. <strong>The</strong> minimum dose to be considered in<br />
adjustments is 11 mg/kg/day.<br />
Common adverse effects: how to deal with anemia, neutropenia<br />
and thrombocytopenia before the treatment, during the<br />
treatment, and triggered by the treatment? What are the basal<br />
limits for patients with and without cirrhosis to be treated?<br />
How can the effects be reversed?<br />
<strong>The</strong> minimum criteria for treatment should be hemoglobin<br />
≥ 10 g/dL, neutrophils > 1500/mm 3 and platelets > 60,000/mm 3 .<br />
Patients presenting a drop in hemoglobin to < 10 g/dL or a<br />
drop ≥ 3.5 g/dL with clinical manifestations should be given<br />
Erythropoietin in a dose <strong>of</strong> 40,000 IU/week until the end <strong>of</strong> the<br />
treatment or until anemia is under control. Patients in whom<br />
neutrophils drop to < 750/mm 3 should receive filgrastim in a<br />
dose <strong>of</strong> 300 µg one to three times a week until neutropenia is<br />
under control. In patients presenting a drop in platelets to <<br />
25.000/mm 3 , the treatment should be discontinued. Adjustment<br />
regimens <strong>of</strong> the dose <strong>of</strong> IFN with intermediate values are<br />
presented in the Proceedings.<br />
When to treat: the patient, the doctor, the system ...<br />
<strong>The</strong> patient wants to be treated. How can we deal with this?<br />
<strong>The</strong>re is no definite position on this situation. We<br />
emphasize the need to give clear and exhaustive information<br />
regarding the indications for treatment and the factors<br />
associated with the progression <strong>of</strong> the disease.<br />
Is early indication <strong>of</strong> treatment worthwhile? In which cases?<br />
Treatment can be considered for individuals with level 1<br />
structural lesion (F1 METAVIR), who present incomplete septa,<br />
A3 activity (METAVIR), who are under 60 years <strong>of</strong> age, and<br />
present co-factors associated with risk <strong>of</strong> progression (obesity,<br />
nonalcoholic steatohepatitis, etc.).<br />
Use <strong>of</strong> IFN and ribavirin<br />
<strong>The</strong> patient, the virus, and the medication: Relevant factors<br />
in predicting response before and during the treatment<br />
<strong>The</strong>re has been no relevant alteration regarding the<br />
elements described. Please see the concepts listed below<br />
regarding individualization based on EVR.<br />
Is conventional treatment with IFN-α dead? If not, when<br />
should we use it?<br />
It is the understanding <strong>of</strong> the <strong>Brazilian</strong> Society <strong>of</strong> <strong>Infectious</strong><br />
<strong>Diseases</strong> that treatment with conventional IFN-α is no longer<br />
justifiable and should not be performed.<br />
Dose <strong>of</strong> IFN, the ‘burden’ <strong>of</strong> the ‘weight’<br />
<strong>The</strong> dose <strong>of</strong> pegylated IFN-α-2a (PEG-IFN-α-2a) should<br />
be 270 μg/week for patients weighing > 85 kg and presenting<br />
a high viral load (> 850,000 IU/mL). <strong>The</strong> dose <strong>of</strong> PEG-IFN-α-2b<br />
should be 1.5 μg/kg/week.<br />
Short, long, standard treatment ... Always individualize?<br />
In patients presenting a RVR, no comorbidities (severe<br />
steatosis or cirrhosis), and a low viral load (< 250,000 IU/<br />
mL for genotype 1), the duration <strong>of</strong> the treatment can be<br />
reduced: to 12 weeks for genotypes 2 and 3; and to 24<br />
weeks for genotype 1. Patients with a high viral load and<br />
complete EVR should be treated for the standard duration,<br />
and patients presenting a slow response (no RVR, partial<br />
EVR and negative at week 24) should be treated for an<br />
additional 24 weeks.<br />
<strong>The</strong> fear <strong>of</strong> suspending treatment: How should we deal with<br />
that decision?<br />
We emphasize that, if the objective <strong>of</strong> the treatment is<br />
virologic, the absence <strong>of</strong> EVR and viral detection at week 24<br />
necessarily imply the interruption <strong>of</strong> the treatment.<br />
Maintenance treatment with IFN: When and how? Is<br />
‘watchful waiting’ still a valid concept?<br />
Maintenance treatment with PEG-IFN-α is considered for<br />
the following patients: those with structural lesion > F3 and/<br />
or signs <strong>of</strong> portal hypertension (esophageal varicose veins,<br />
splenomegaly, dilated blood vessels, etc.) and/or platelet<br />
counts < 110,000/mm 3 who are categorized as Child-Pugh class<br />
A or B, with no history <strong>of</strong> severe or potentially uncontrollable<br />
decompensation; those without hepatocellular carcinoma;<br />
relapsers; and partial responders or nonresponders to the<br />
combination <strong>of</strong> PEG-IFN-α and ribavirin (or to IFN only when<br />
ribavirin is contraindicated) administered with adequated<br />
compliance and for a minimum <strong>of</strong> 12 weeks. Maintenance<br />
treatment with PEG-IFN-α should also be considered for<br />
patients for whom the full dose treatment is contraindicated.<br />
Child-Pugh class C patients on the transplant waiting list<br />
should be treated in specialized centers. Proposed regimen 2 :<br />
PEG-IFN-α-2b, 0.5-1.0 μg/kg/week subcutaneously (sc); PEG-<br />
IFN-α-2a, 90 μg/week (sc). Duration 2 : Minimum <strong>of</strong> 24 months,<br />
indefinite, or even until there is an antiviral treatment that is<br />
proven to be safe and efficient. Monitoring the occurrence <strong>of</strong><br />
complications (hepatocellular carcinoma, gastrointestinal<br />
bleeding, encephalopathy, etc.)<br />
Monotherapy with ribavirin, although previously<br />
described, cannot be recommended at the moment, due to<br />
insufficient evidence.<br />
Impact <strong>of</strong> reduction in the dose <strong>of</strong> IFN and/or ribavirin at<br />
various moments <strong>of</strong> the treatment<br />
Every effort should be made to always maintain full<br />
treatment.<br />
Positive and negative predictive values in clinical practice:<br />
patients mono- and co-infected with HIV<br />
Positive predictivity data in the presence <strong>of</strong> RVR and<br />
negative predictivity data in the absence <strong>of</strong> EVR are equally<br />
2<br />
Dose schedule and duration were suggested based on preliminary data<br />
and should be re-evaluated taking into account the results <strong>of</strong> ongoing<br />
studies.<br />
www.bjid.com.br
BJID 2007; 11 Supplement 1 (October) Consensus <strong>of</strong> Hepatitis C Carried Out by SBI<br />
5<br />
valid for HCV mono-infected patients and patients co-infected<br />
with HCV and HIV.<br />
Retreatment: When and how?<br />
Retreatment will always be considered when the previous<br />
treatment was considered suboptimal for the current concepts<br />
(poor compliance, insufficient doses, inappropriate interruptions,<br />
inadequate management <strong>of</strong> adverse events, uncontrolled<br />
comorbidities, etc.) and when there is recurrence. <strong>The</strong> treatment<br />
in true nonresponders to PEG-IFN and ribavirin presents such<br />
a low chance <strong>of</strong> success that it cannot be routinely<br />
recommended.<br />
Due to the fact that relapsers/nonresponders to initial<br />
treatment constitute a quite heterogeneous group, it is<br />
necessary to qualify and carefully select the patients that should<br />
be retreated. Various factors that might have influenced the<br />
nonresponse should be modified before the initiation <strong>of</strong> or even<br />
during the new therapeutic cycle. Currently, patients considered<br />
less likely to respond to retreatment are those who are true<br />
nonresponders, those who are <strong>of</strong> the Black race, those infected<br />
with genotype 1, those with high viral loads, those with<br />
advanced liver disease, and those who present intercurrent<br />
conditions (obesity, etc.)<br />
Patients previously treated with IFN as monotherapy or<br />
with the combination <strong>of</strong> IFN and ribavirin stand a greater chance<br />
<strong>of</strong> presenting an SVR than do nonresponders to the<br />
combination <strong>of</strong> PEG-IFN and ribavirin. Those who experienced<br />
recurrence during the treatment (breakthrough) or after the<br />
treatment fare better than do true nonresponders. Patients who<br />
are noncompliant with previous treatment, as well as those<br />
who required reduced doses <strong>of</strong> IFN or ribavirin due to cytopenia<br />
or other adverse effects, usually respond better to retreatment<br />
than do those who received full doses. Of course, the factors<br />
responsible for noncompliance should be eliminated, and<br />
reductions in medication doses should be properly approached.<br />
In nonresponders, it is recommended that erythropoietin and<br />
filgrastim be started sooner, and further dose reductions should<br />
be avoided at all costs. Users <strong>of</strong> drugs or alcohol who, due to<br />
their addiction, did not adequately comply with all the phases<br />
<strong>of</strong> the previous treatment, can more adequately respond to<br />
retreatment provided that these co-factors are nullified. This<br />
also applies to patients who did not receive adequate social<br />
or cultural support. Patients who suffer from obesity, insulin<br />
resistance, dyslipidemia, steatosis, anemia, or liver diseases<br />
(e.g., hemochromatosis) should be retreated, preferably<br />
after the proper diagnosis and treatment <strong>of</strong> these<br />
concomitant conditions. Doses <strong>of</strong> PEG-IFN should be the<br />
same as those used for treatment-naïve patients. We believe<br />
that, in retreatment regimens, the doses <strong>of</strong> ribavirin should<br />
be as high as possible. Due to the paucity <strong>of</strong> studies with<br />
large patient samples, we recommend that the duration <strong>of</strong><br />
retreatment be 48 weeks for all genotypes. At the moment,<br />
there are no consolidated data in the literature to support<br />
using higher doses <strong>of</strong> PEG-IFN or ribavirin, using induction<br />
doses, or extending the treatment time to more than 48<br />
weeks in retreatment cases. Regarding the week 12 rule,<br />
there is strong evidence that patients who do not present<br />
negativity for HCV RNA by this time will have very little<br />
chance <strong>of</strong> presenting an SVR, and their treatment should be<br />
interrupted.<br />
IFN: Backbone <strong>of</strong> the current treatment. And the future?<br />
Perspectives and frustrations<br />
Preliminary results <strong>of</strong> developing therapies show that IFNα<br />
will still be the active principle <strong>of</strong> the treatment for many<br />
years. For this reason, we have adopted several <strong>of</strong> the practices<br />
that are presented here.<br />
Co-infections<br />
Antiretroviral therapy 2007 and HCV treatment: relevant<br />
interactions<br />
Although ribavirin can reduce the concentration <strong>of</strong> some<br />
antiretroviral nucleoside analog reverse transcriptase inhibitors<br />
(NARTIs), there seem to be no clinical consequences.<br />
<strong>The</strong> adverse effects <strong>of</strong> NARTIs have been associated with<br />
HCV co-infection, female gender, obesity and prolonged exposure<br />
to these drugs. <strong>The</strong> principal combinations with less hepatic<br />
repercussion among NARTIs are as follows: lamivudine + abacavir;<br />
lamivudine + zidovudine; lamivudine + abacavir + zidovudine, and<br />
emtricitabine + ten<strong>of</strong>ovir. However, current studies indicate that<br />
ribavirin interferes with the effect <strong>of</strong> abacavir. <strong>The</strong>refore, ribavirin<br />
should be used with caution in patients receiving the highly active<br />
antiretroviral therapy regimen and being treated for HCV.<br />
Greater toxicity is principally caused by concomitant use <strong>of</strong><br />
didanosine and ribavirin.<br />
CD4 counts: Minimum limits for treatment and decision-making in<br />
patients with reconstituted immunity or immunocompetent patients<br />
Precise indication <strong>of</strong> therapy in HIV/HCV co-infected<br />
patients can be made in patients with CD4 counts > 350 cells/<br />
mm 3 . In patients with CD4 counts between 200 and 350 cells/<br />
.<br />
mm 3 , the decision to treat HCV infection should take into<br />
account other factors, such as the duration <strong>of</strong> HCV infection,<br />
the severity <strong>of</strong> the liver disease, the level <strong>of</strong> HIV suppression<br />
and classical predictors <strong>of</strong> treatment response to HCV, such as<br />
genotype and viral load.<br />
<strong>The</strong> SVR can be predicted when HCV RNA is undetectable<br />
in serum by week 4 <strong>of</strong> treatment. However, a < 2log10 IU/mL<br />
reduction in viral load by week 12 and/or viremia detected at<br />
week 24 predict a lack <strong>of</strong> virologic response, and discontinuation<br />
<strong>of</strong> the treatment is indicated.<br />
Ongoing studies are evaluating 72-week maintenance therapy<br />
in co-infected patients and week-24 nonresponders. This might<br />
be the truly appropriate treatment duration for HIV-positive<br />
patients, even with longer time and smaller fractionated doses.<br />
Is the immunocompetent HIV/HCV co-infected patient ‘monoinfected’?<br />
Yes, the evolution is quite similar.<br />
Multiple viral infections: Who should we treat first and how?<br />
Care should be given to the dominant virus between HBV<br />
and HCV. When treating the dominant virus, the other might<br />
become active. We need to quantify the HBV DNA in order to<br />
manage this situation.<br />
<strong>The</strong> HTLV apparently modulates the host immune<br />
response, a fact that should be considered and which is<br />
detailed in the Proceedings.<br />
<strong>The</strong>re is no consensus regarding the correct course <strong>of</strong><br />
action in multiple co-infections.<br />
www.bjid.com.br
6 BJID 2007; 11 Supplement 1 (October)<br />
Epidemiological Aspects <strong>of</strong> Hepatitis C in Brazil<br />
Decio Diament<br />
Emílio Ribas Institute <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong>; São Paulo, SP, Brazil<br />
<strong>The</strong> true dimension <strong>of</strong> the epidemiological situation <strong>of</strong><br />
chronic hepatitis C in Brazil remains unknown. According to<br />
data from the National Ministry <strong>of</strong> Health, 52,489 cases were<br />
diagnosed in the period from 1994 to 2005. However, the data<br />
regarding the final year <strong>of</strong> this series are incomplete. <strong>The</strong>re is<br />
a trend toward an increase in the number <strong>of</strong> diagnosed cases<br />
during this period, since diagnostic techniques have become<br />
more widely available, both in public and private health care<br />
facilities (Figure 1).<br />
Figure 1. Number <strong>of</strong> diagnosed cases <strong>of</strong> hepatitis C reported<br />
by the National Ministry <strong>of</strong> Health, from 1994 to 2005, totaling<br />
52,489 cases.<br />
This distribution reflects the greater availability <strong>of</strong><br />
resources as well as the highly populated areas in the<br />
southeastern and southern regions <strong>of</strong> the country. However,<br />
serological surveys carried out in the Central-west and<br />
Northeast, as well as in the Federal District, showed prevalence<br />
rates similar to those <strong>of</strong> a previous survey carried out in the<br />
city <strong>of</strong> São Paulo (Figure 3).<br />
Figure 3. Prevalence <strong>of</strong> hepatitis C in serological surveys in<br />
several regions <strong>of</strong> the country (Galizzi Filho J, personal<br />
communication, for the data <strong>of</strong> the surveys on the Centralwest,<br />
Federal District and Northeast; Focaccia R., personal<br />
communication, for the data on São Paulo).<br />
Most diagnosed cases occur in the Southeast, followed<br />
by the South, Central-west, Northeast and North (Figure 2).<br />
Figure 2. Distribution <strong>of</strong> cases by macroregion (National<br />
Ministry <strong>of</strong> Health).<br />
<strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> 2007;11 (5) Suppl. 1:6-7.<br />
© 2007 by <strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> and Contexto<br />
Publishing. All rights reserved.<br />
Data obtained in these serological surveys indicate<br />
prevalence rates from 0.28 to 2.61%. According to the 2000<br />
census taken by the <strong>Brazilian</strong> Institute <strong>of</strong> Geography and<br />
Statistics, Brazil has a population <strong>of</strong> approximately 170 million.<br />
It has been shown that, <strong>of</strong> those testing positive for infection<br />
with the hepatitis C virus (HCV), approximately 80% have the<br />
chronic form <strong>of</strong> hepatitis C. Based on these data, we can<br />
estimate that there are 400,000 to 3,800,000 cases <strong>of</strong> chronic<br />
hepatitis C in Brazil. Comparing these numbers with the data<br />
from the National Ministry <strong>of</strong> Health, we can conclude that<br />
there are a great number <strong>of</strong> undiagnosed cases <strong>of</strong> the disease.<br />
Since there has been a trend toward an increase in the number<br />
<strong>of</strong> diagnosed cases, there will be a significant increase in the<br />
demand for diagnosis and treatment <strong>of</strong> chronic hepatitis C in<br />
the future.<br />
Another interesting fact is that only 17,204 (33%) <strong>of</strong> the<br />
52,493 cases <strong>of</strong> chronic hepatitis reported to the Center for<br />
Epidemiological Surveillance <strong>of</strong> São Paulo, from 1998 to 2006,<br />
were confirmed as being hepatitis C. Another 10,690 cases<br />
(20%) were classified as inconclusive for hepatitis C, 2099<br />
(4%) were excluded, and 416 (0.79%) were cases <strong>of</strong> HBV/HCV<br />
co-infection. <strong>The</strong> remaining cases were confirmed as hepatitis<br />
B, HBV/HDV co-infection, or cases under investigation.<br />
www.bjid.com.br
BJID 2007; 11 Supplement 1 (October) Hepatitis C in Brazil<br />
7<br />
Of the 17,204 confirmed cases, the principal form <strong>of</strong><br />
contamination was parenteral (use <strong>of</strong> injected illicit drugs, as<br />
well as blood and blood product transfusions), followed by<br />
sexual transmission. Work-related accidents accounted for<br />
few <strong>of</strong> the cases (Figure 4).<br />
Figure 4. Distribution <strong>of</strong> cases <strong>of</strong> chronic hepatitis C by form<br />
<strong>of</strong> transmission in 17,204 individuals in the state <strong>of</strong> São Paulo,<br />
from 1998 to 2006 (Source: Center for Epidemiological<br />
Surveillance, São Paulo).<br />
Transmission was classified as unknown in 40% <strong>of</strong> the<br />
reported and confirmed cases, as can be seen in Figure 4. This<br />
suggests that the investigation <strong>of</strong> the form <strong>of</strong> transmission<br />
should be improved, and that items such as administration <strong>of</strong><br />
medication using nondisposable syringes, acupuncture,<br />
tattoos, and piercings should be included in the<br />
epidemiological investigation. Another unusual fact is sexual<br />
transmission in 10% <strong>of</strong> the cases, well above the expected,<br />
which is less than 1%.<br />
Another aspect to be considered is the occurrence <strong>of</strong><br />
hepatitis C in groups <strong>of</strong> differentiated risk, that is, unusual<br />
cases such as those described in Figure 4. <strong>The</strong> first group<br />
would be that <strong>of</strong> the manicurists, since it is supposed that the<br />
community use <strong>of</strong> instruments by these pr<strong>of</strong>essionals would<br />
expose them to a higher risk <strong>of</strong> contamination. <strong>The</strong>re is no<br />
evidence that this could happen, and a recent serological<br />
survey conducted in the city <strong>of</strong> São Paulo in beauty salons<br />
located at shopping malls in various neighborhoods did not<br />
demonstrate prevalence rates different from those <strong>of</strong> the<br />
population in general (Oliveira, ACDS – personal<br />
communication).<br />
Another group is that <strong>of</strong> the dentists. In Brazil, localized<br />
serological surveys with small samples <strong>of</strong> patients have<br />
shown a low prevalence rate, ranging from 0.4 to 0.7%.<br />
However, a study on the level <strong>of</strong> knowledge <strong>of</strong> these<br />
pr<strong>of</strong>essionals about the disease has shown it is very low,<br />
demonstrating the need <strong>of</strong> greater emphasis on training and<br />
continuing education, aiming at making them capable <strong>of</strong><br />
properly protecting themselves, as well as <strong>of</strong> preventing<br />
transmission to patients and perhaps even help the<br />
diagnosis, since several extrahepatic manifestations appear<br />
in the mouth cavity, such as oral liquen planus, erythema<br />
nodosum, etc.<br />
References<br />
1. Bellíssimo-Rodrigues W.T., Machado A.A., Bellíssimo-Rodrigues<br />
F., et al. Prevalence <strong>of</strong> hepatitis B and C among <strong>Brazilian</strong> dentists.<br />
Infect Control Hosp Epidemiol 2006;27:887-8.<br />
2. http://portal.saude.gov.br/portal/saude/<br />
visualizar_texto.cfm?idtxt=25340. Acessado em 24/08/2007.<br />
3. http://www.cve.saude.sp.gov.br/htm/hepa_home.html. Acessado em<br />
24/08/2007.<br />
4. Leão J.C., Teo C.G., Porter S.R. HCV infection: aspects <strong>of</strong><br />
epidemiology and transmission relevant to oral health care<br />
workers. Int J Oral Maxill<strong>of</strong>ac Surg 2006;35(4):295-300.<br />
5. Takahama A.J., Tatsch F., Tannus G., Lopes M.A. Hepatitis C:<br />
incidence and knowledge among <strong>Brazilian</strong> dentists. Community<br />
Dent Health 2005;22(3):184-7.<br />
www.bjid.com.br
8 BJID 2007; 11 Supplement 1 (October)<br />
Sexual Transmission <strong>of</strong> HCV<br />
Kleber Dias do Prado<br />
Emílio Ribas Institute <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong>; São Paulo, SP, Brazil<br />
Although there is evidence that sexual transmission <strong>of</strong><br />
HCV occurs, this form <strong>of</strong> transmission is <strong>of</strong> secondary<br />
epidemiological importance when compared to percutaneous<br />
forms <strong>of</strong> transmission [1]. Among the evidence that supports<br />
the possibility <strong>of</strong> sexual transmission <strong>of</strong> HCV we can list the<br />
following:<br />
1- Case reports <strong>of</strong> acute hepatitis C with anti-HCV<br />
seroconversion in sexual partners <strong>of</strong> individuals infected by<br />
HCV, excluding mechanisms <strong>of</strong> nonsexual transmission and<br />
with high genomic homology among viral strains infecting<br />
sexual partners [2-4].<br />
2- Detection <strong>of</strong> HCV RNA in semen, vaginal secretion and<br />
cervical secretion, despite low titles in most cases [5-8].<br />
3- Data from the Centers for Disease Control and Prevention<br />
demonstrating that, from 1995 to 2000, 18% <strong>of</strong> the cases <strong>of</strong><br />
acute HCV infection in the United States occurred in patients<br />
reporting sexual contact with an individual infected with HCV<br />
in the preceding 6 months or multiple sexual contacts as the<br />
only risk factors for acquiring the infection [1].<br />
<strong>The</strong> risk <strong>of</strong> acquiring HCV through sexual contact differs<br />
among subgroups <strong>of</strong> individuals: We can distinguish two main<br />
risk subgroups:<br />
1. Individuals who have multiple sexual partners or who<br />
engage in sexual practices that might lead to mucosal trauma:<br />
sex pr<strong>of</strong>essionals; men who have sex with men (MSM); and<br />
patients treated in clinics specializing in the treatment <strong>of</strong><br />
sexually transmitted diseases (STDs).<br />
2. Stable monogamous heterosexual sexual partners <strong>of</strong><br />
individuals chronically infected with HCV.<br />
In general, rates <strong>of</strong> anti-HCV incidence and prevalence are<br />
higher in the first subgroup. This may be due to differences in<br />
sexual practices among the groups, but also to nonsexual<br />
factors (sharing personal objects, tattoos, use <strong>of</strong> illicit drugs,<br />
etc.) [1]. Seroprevalence studies in the United States<br />
demonstrated median positive anti-HCV rates in 6% <strong>of</strong> women<br />
who were sex pr<strong>of</strong>essionals, as well as in 4% <strong>of</strong> MSM, 4% <strong>of</strong><br />
clients <strong>of</strong> STD clinics and 4% <strong>of</strong> participants in HIV<br />
surveillance studies. Studies conducted in other parts <strong>of</strong> the<br />
world have obtained similar results [9-15]. <strong>The</strong> following risk<br />
factors were identified: having had a high number <strong>of</strong> recent<br />
and lifetime sex partners; engaging in unsafe sexual practices;<br />
being infected with HIV; and having an STD. This indicates<br />
that sexual activity in general is a risk factor for HCV<br />
<strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> 2007;11 (5) Suppl. 1:8-9.<br />
© 2007 by <strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> and Contexto<br />
Publishing. All rights reserved.<br />
transmission [1].<br />
However it is essential to mention that the results <strong>of</strong> some<br />
studies contradict these findings. Studying the prevalence<br />
and incidence <strong>of</strong> positivity for anti-HCV antibodies in a cohort<br />
<strong>of</strong> 1085 HIV-positive Canadian MSM, Alary et al. found values<br />
<strong>of</strong> 2.9% and 0.038/100 individuals/year, respectively, both<br />
significantly associated with the use <strong>of</strong> injection drugs. <strong>The</strong><br />
authors considered sexual transmission <strong>of</strong> HCV to be rare in<br />
this group [16]. In a study conducted in Thailand, Taketa et al.<br />
assessed the prevalence <strong>of</strong> anti-HCV in injection drug users,<br />
sex pr<strong>of</strong>essionals and individuals with STDs. <strong>The</strong> prevalence<br />
was 85%, 2% and 0%, respectively, with a very low or null<br />
transmission rate in the last two groups [17]. Marincovich et<br />
al. prospectively studied a group <strong>of</strong> 171 couples discordant<br />
for HIV and HCV. <strong>The</strong> index cases were 152 men and 19 women,<br />
whereas the spouses were 152 women and 19 men. Fortythree<br />
per cent had engaged in unprotected vaginal and/or<br />
anal sex, 15% always used a condom but reported incidents in<br />
which the condom broke or slipped <strong>of</strong>f during sexual contact,<br />
and 22% had performed unprotected orogenital sex. <strong>The</strong>re<br />
was only one case <strong>of</strong> HIV seroconversion and no cases <strong>of</strong><br />
HCV seroconversion during the follow-up <strong>of</strong> 529 individuals/<br />
year. <strong>The</strong>re were 31 cases <strong>of</strong> pregnancy, 2 <strong>of</strong> them in women<br />
infected with HCV. This study suggests that the rate <strong>of</strong> HCV<br />
transmission is low or null among heterosexuals, even when<br />
the partner is infected with HIV [18].<br />
For the second subgroup, the best studies are those<br />
excluding percutaneous factors <strong>of</strong> infection and evaluating<br />
genotypes and genomic sequence <strong>of</strong> viral strains in anti-HCV<br />
concordant couples. In those studies, the prevalence <strong>of</strong> HCV<br />
was estimated at 2.8-11% in the Asian Southeast, 0-6.3% in<br />
Northern Europe and 2.7% in the United States [1].<br />
In one <strong>of</strong> the first studies to use genotyping and analysis<br />
<strong>of</strong> the sequence <strong>of</strong> nucleotides <strong>of</strong> the hypervariable E2 region,<br />
Zylberberg et al., studying 24 anti-HCV concordant couples,<br />
reduced to 3 couples the possible cases <strong>of</strong> sexual transmission<br />
<strong>of</strong> HCV. Nevertheless, nonsexual factors could not be ruled<br />
out and might have contributed to HCV transmission between<br />
couples [19]. In Iran, Hajiani et al. studied the HCV transmission<br />
rate for home contacts with no percutaneous risk factors. <strong>The</strong><br />
rates found were 1.33% for the contacts and 1% for the controls<br />
(p>0.06). Only 2 <strong>of</strong> 59 spouses presented evidence <strong>of</strong> infection<br />
(3.39%). <strong>The</strong> authors conclude that intrafamily transmission<br />
is possible, although not common [20].<br />
In a recent study, McMahon et al. determined that the<br />
transmission <strong>of</strong> HCV in 265 heterosexual couples using drugs<br />
in New York City was associated with the use <strong>of</strong> injection<br />
drugs by the couple, although not with the pattern <strong>of</strong> sexual<br />
activity [21]. Along the same lines, Boonyarad et al., studying<br />
160 spouses infected with chronic hepatitis C (106 women<br />
www.bjid.com.br
BJID 2007; 11 Supplement 1 (October) Sexual Transmission <strong>of</strong> HCV<br />
9<br />
and 54 men, all monogamous, stable heterosexual couples),<br />
verified that only 3 individuals (1.88%) tested positive for<br />
anti-HCV antibodies and HCV RNA after a mean period <strong>of</strong> 23<br />
± 5 years <strong>of</strong> unprotected sexual exposure. Nevertheless, in<br />
those 3 individuals, genotyping and sequence analysis did<br />
not clearly identify the same viral strains that infected their<br />
respective partners. <strong>The</strong> authors concluded that sexual<br />
transmission <strong>of</strong> HCV is rare [22].<br />
Finally, Vandelli et al. conducted a large prospective study<br />
in which 895 monogamous and stable heterosexual couples<br />
were evaluated for 10 years [23]. Among the spouses, the<br />
authors identified 3 cases <strong>of</strong> seroconversion, none <strong>of</strong> which<br />
were attributed to sexual contact with the partner: in one case,<br />
the genotypes were different; in the other two, there were<br />
discrepancies in the sequence and phylogenetic analysis).<br />
<strong>The</strong>refore, the authors conclude that the rate <strong>of</strong> sexual<br />
transmission <strong>of</strong> HCV is very low or even null in these patients.<br />
<strong>The</strong>refore, it seems unnecessary to recommend condom use<br />
in this population. <strong>The</strong>se couples did not practice anal sex,<br />
neither sex during menstruation nor used condoms [23].<br />
<strong>The</strong> risk <strong>of</strong> sexual transmission <strong>of</strong> HCV ranges from 0-<br />
0.6%/year for heterosexual couples in monogamous, stable<br />
relationships to 1%/year to individuals with several sex<br />
partners [1]. <strong>The</strong>refore, the formal, systematic recommendation<br />
<strong>of</strong> condom use is only necessary for the latter group. Condom<br />
use is also justified in HCV-positive individuals presenting<br />
concomitant STDs, having sex during menstruation or<br />
engaging in sexual practices that can traumatize the mucosal<br />
surfaces (anal sex, fisting, etc.) In conclusion, the sharing <strong>of</strong><br />
objects potentially contaminated with blood, such as razor<br />
blades, scissors, nail clippers, cuticle trimmers and tooth<br />
brushes, is not recommended [1].<br />
References<br />
1. Terrault N.A. Sexual activity as a risk factor for hepatitis C.<br />
Hepatology 2002;36:S99-105.<br />
2. Halfon P., Riflet H., Renou C., et al. Molecular evidence <strong>of</strong> maleto-female<br />
sexual transmission <strong>of</strong> hepatitis C virus after vaginal<br />
and anal intercourse. J Clin Microbiol 2001;39:1204-6.<br />
3. Nakayama H., Sugai Y., Ikeya S., et al. Molecular investigation <strong>of</strong><br />
interspousal transmission <strong>of</strong> hepatitis C virus in two Japanese<br />
patients Who acquired acute hepatitis C after 40 or 42 years <strong>of</strong><br />
marriage. J Med Virol 2005;75(2):258-66.<br />
4. Lai K.W., Young K.C., Cheng P.N., et al. Interspousal transmission<br />
<strong>of</strong> hepatitis C virus: application <strong>of</strong> comparing the variability <strong>of</strong><br />
HVR1 nucleotide region. Hepatogastroenterology<br />
2004;51(57):791-5.<br />
5. Leruez-Ville M., Kunstmann J.M., De Almeida M., et al. Detection<br />
<strong>of</strong> hepatitis C virus in the semen <strong>of</strong> infected men. Lancet<br />
2000;356:42-3.<br />
6. Manavi M., Watkins-Riedel T., Kucera E., et al. Evidence <strong>of</strong><br />
hepatitis C virus in cervical smears. J Infect 1999;38:60-1.<br />
7. Pekler V.A., Robbins W.A., Nyamathi A., et al. Use <strong>of</strong> versant<br />
TMA and bDNA 3.0 assays to detect and quantify hepatitis C<br />
virus in semen. J Clin Lab Anal 2003;17(6):264-70.<br />
8. Bélec L., Leg<strong>of</strong>f J., Si-Mohamed A., et al. Cell-associated, nonreplicating<br />
strand (+) hepatitis C virus-RNA shedding in<br />
cervicovaginal secretions from chronically HCV-infected<br />
women. J Clin Virol 2003;27(3):247-51.<br />
9. Van de Laar T.J., Van der Bij A.K., Prins M., et al. Increase in HCV<br />
incidence among men who have sex with men in Amsterdam<br />
most likely caused by sexual transmission. J Infect Dis<br />
2007;196(2):230-8.<br />
10. Danta M., Brown D., Bhagani S., et al. Recent epidemic <strong>of</strong> acute<br />
hepatitis C virus in HIV-positive men who have sex with<br />
men linked to high-risk sexual behaviours. AIDS<br />
2007;21(8):983-91.<br />
11. Götz H.M., Van Doornum G., Niesters H.G., et al. A cluster <strong>of</strong> acute<br />
hepatitis C virus infection among men who have sex with men:<br />
results from contact tracing and public health implications.<br />
AIDS 2005;19(9):969-74.<br />
12. D’Oliveira A. Jr., Voirin N., Allard R., et al. Prevalence and sexual<br />
risk <strong>of</strong> hepatitis C virus infection when human immunodeficiency<br />
virus was acquired through sexual intercourse among patients <strong>of</strong><br />
the Lyon University Hospitals, France, 1992-2002. J Viral Hepat<br />
2005;12(3):330-2.<br />
13. De los Angeles Pando M., Biglione M.M., Toscano M.F., et al.<br />
Human immunodeficiency virus type 1 and other viral coinfections<br />
among young heterosexual men and women in<br />
Argentina. Am J Trop Med Hyg 2004;71(2):153-9.<br />
14. Marx M.A., Murugavel K.G., Tarwater P.M., et al. Association <strong>of</strong><br />
hepatitis C virus infection with sexual exposure in southern<br />
India. Clin Infect Dis 2003;37(4):514-20.<br />
15. Russi J.C., Serra M., Viñoles J., et al. Sexual transmission <strong>of</strong> hepatitis<br />
B virus, hepatitis C virus, and human immunodeficiency virus<br />
type 1 infections among male transvestite commercial sex<br />
workers in Montevideo, Uruguay. Am J Trop Med Hyg<br />
2003;68(6):716-20.<br />
16. Alary M., Joly J.R., Vincelette J., et al. Lack <strong>of</strong> evidence <strong>of</strong> sexual<br />
transmission <strong>of</strong> hepatitis C virus in a prospective cohort study<br />
<strong>of</strong> men who have sex with men. Am J Public Health<br />
2005;95(3):502-5.<br />
17. Taketa K., Ikeda S., Suganuma M., et al. Differential<br />
seroprevalences <strong>of</strong> hepatitis C virus, hepatitis B virus and human<br />
immunodeficiency virus among intravenous drug users,<br />
commercial sex workers and patients with sexually transmitted<br />
diseases in Chiang Mai, Thailand. Hepatol Res 2003;27(1):6-12.<br />
18. Marincovich B., Castilla J., Del Romero J., et al. Absence <strong>of</strong> hepatitis<br />
C virus transmission in a prospective cohort <strong>of</strong> heterosexual<br />
serodiscordant couples. Sex Transm Infect 2003;79(2):160-2.<br />
19. Zylberberg H., Thiers V., Lagorce D., et al. Epidemiological and<br />
virological analysis <strong>of</strong> couples infected with hepatitis C virus.<br />
Gut 1999;45(1):112-6.<br />
20. Hajiani E., Masjedizadeh R., Hashemi J., et al. Hepatitis c virus<br />
transmission and its risk factors within families <strong>of</strong> patients<br />
infected with hepatitis C virus in southern Iran: Khuzestan.<br />
World J Gastroenterol 2006;12(43):7025-8.<br />
21. McMahon J.M., Pouget E.R., Tortu S. Individual and couple-level<br />
risk factors for hepatitis C infection among heterosexual drug<br />
users: a multilevel dyadic analysis. J Infect Dis<br />
2007;195(11):1556-9.<br />
22. Boonyarad V., Chutaputti A., Choeichareon S., et al. Interspousal<br />
transmission <strong>of</strong> hepatitis C in Thailand. J Gastroenterol<br />
2003;38(11):1053-9.<br />
23. Vandelli C., Renzo F., Romanò L., et al. Lack <strong>of</strong> evidence <strong>of</strong> sexual<br />
transmission <strong>of</strong> hepatitis C among monogamous couples: results<br />
<strong>of</strong> a 10-year prospective follow-up study. Am J Gastroenterol<br />
2004;99(5):855-9.<br />
www.bjid.com.br
10 BJID 2007; 11 Supplement 1 (October)<br />
Hepatitis C Virus Perinatal Transmission<br />
Umbeliana Barbosa de Oliveira<br />
Emílio Ribas Institute <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong>; São Paulo, SP, Brazil<br />
<strong>The</strong> hepatitis C virus (HCV) is the most frequent cause <strong>of</strong><br />
chronic hepatic disease. Its principal route <strong>of</strong> transmission is<br />
exposure to contaminated blood. Perinatal transmission is one<br />
<strong>of</strong> the less common modes <strong>of</strong> infection with HCV.<br />
Incidence<br />
Vertical transmission <strong>of</strong> HCV has been reported in<br />
numerous studies. However, the estimated rate <strong>of</strong> vertical<br />
transmission varies considerably due to several factors:<br />
• Study methodology;<br />
• Selection <strong>of</strong> maternal population;<br />
• Risks involved in the transmission, such as coinfection<br />
with HIV and high levels <strong>of</strong> HCV RNA.<br />
A review <strong>of</strong> the literature carried out in 1998 identified 976<br />
children from 28 studies with follow-up periods that were<br />
sufficiently long to estimate the transmission rate. In those<br />
studies, the vertical transmission rate was below 10% in cases<br />
involving HIV-negative mothers. <strong>The</strong> risk <strong>of</strong> vertical<br />
transmission increased significantly in cases involving HIVpositive<br />
mothers. It is believed that, in these cases, the mother<br />
tends to present higher levels <strong>of</strong> HCV viremia, increasing the<br />
risk <strong>of</strong> transmission.<br />
In a more recent review (published in 2001), the authors<br />
searched through studies published in the 1992-2000 period<br />
and identified 77 studies. <strong>The</strong>y found clinical and demographic<br />
variables that influenced the transmission rate. <strong>The</strong>y<br />
concluded that co-infection with HIV is the most significant<br />
factor associated with the risk <strong>of</strong> vertical HCV transmission.<br />
Findings regarding other possible risk factors, such as HCV<br />
genotype, type <strong>of</strong> delivery, and breastfeeding, have been<br />
inconclusive.<br />
Risk Factors<br />
As previously mentioned, the principal risk factor for vertical<br />
transmission <strong>of</strong> HCV is concomitant infection with HIV.<br />
Viremia Level<br />
Some studies have shown that viral load can be an<br />
important determinant factor for vertical transmission <strong>of</strong> HCV.<br />
It has been demonstrated that women with viral loads lower<br />
than 1 × 10 5 copies per mL have a lower risk <strong>of</strong> vertical<br />
transmission, whether co-infected with HIV or not. One study<br />
that compared viral loads among HCV RNA-positive mothers<br />
whose children were infected with HCV or not showed that, in<br />
cases <strong>of</strong> probable vertical transmission, the maternal viral load<br />
was ten times higher than in those cases in which transmission<br />
did not occur.<br />
However, there are also inconsistent data in two large<br />
studies that found no significant differences between the HCV<br />
RNA levels <strong>of</strong> the mothers who transmitted HCV and those <strong>of</strong><br />
mothers who did not.<br />
<strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> 2007;11 (5) Suppl. 1:10-11.<br />
© 2007 by <strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> and Contexto<br />
Publishing. All rights reserved.<br />
Co-Infection with HIV<br />
Numerous studies have shown that the HCV vertical<br />
transmission rate is higher among HIV-positive women that<br />
among those who are HIV-negative (19% vs. 4%). This is in<br />
part explained by the fact that HIV-positive women present<br />
higher viral loads <strong>of</strong> HCV.<br />
One study showed that the average level <strong>of</strong> HCV RNA in<br />
women co-infected with HIV was ten times higher than in<br />
women mono-infected with HCV. This shows that the increase<br />
in the co-infection risk can be nullified after adjusting the risk<br />
for the viral load, and antiretroviral therapy for HIV can reduce<br />
the risk <strong>of</strong> HCV transmission.<br />
One study that compared HIV-positive women and HIVnegative<br />
women with similar viral loads <strong>of</strong> HCV showed that the<br />
risk <strong>of</strong> HCV transmission was similar in both groups. In that study,<br />
all HIV-positive women were receiving antiretroviral therapy.<br />
Another study showed that children infected with HIV<br />
are at a higher risk <strong>of</strong> being infected with HCV than are those<br />
who are HIV-negative (17.1% vs. 5.4%). <strong>The</strong> explanation for<br />
these data remains unclear.<br />
Genotype<br />
<strong>The</strong>re is no evidence that HCV genotype influences<br />
vertical transmission. <strong>The</strong> data collected to date do not allow<br />
us to establish a relationship between HCV genotype and<br />
vertical transmission risk.<br />
Breastfeeding<br />
It is possible to detect HCV RNA in breast milk and<br />
colostrum. However, HCV transmission through breastfeeding<br />
has not been documented. A likely explanation would be that<br />
HCV is inactivated by the effect <strong>of</strong> gastric acidity and that the<br />
HCV RNA levels in breast milk are very low.<br />
<strong>The</strong>refore, breastfeeding does not increase the risk that<br />
HCV will be transmitted from an infected mother to her child.<br />
<strong>The</strong> American College <strong>of</strong> Obstetricians and Gynecologists, as<br />
well as the American Academy <strong>of</strong> Pediatrics, allows<br />
breastfeeding by mothers who are infected with HCV.<br />
It is important to emphasize that breastfeeding is not<br />
recommended in case <strong>of</strong> nipple fissure, due to the<br />
possibility <strong>of</strong> bleeding.<br />
Type <strong>of</strong> Delivery<br />
<strong>The</strong> impact that the type <strong>of</strong> delivery has on perinatal<br />
transmission <strong>of</strong> HCV is completely unknown. Vaginal delivery<br />
has been associated with an increase in the transmission risk.<br />
In a study carried out by Lin et al. in 1994, 70 pregnant women<br />
were evaluated. <strong>The</strong> vertical transmission rate among children<br />
who were born by vaginal delivery was 32%, compared to 6%<br />
in cases <strong>of</strong> cesarean section. However, the high transmission<br />
rate in the Lin et al. study was associated with the fact that a<br />
large proportion <strong>of</strong> the women evaluated (76%) were coinfected<br />
with HIV and HCV. <strong>The</strong>refore, cesarean section is<br />
associated with a decrease in the HCV transmission risk in co-<br />
www.bjid.com.br
BJID 2007; 11 Supplement 1 (October) Hepatitis C Virus Perinatal Transmission<br />
11<br />
infected women. <strong>The</strong> higher risk <strong>of</strong> transmission in vaginal<br />
delivery might be associated with exposure <strong>of</strong> the newborn to<br />
HCV-contaminated blood during its passage through the<br />
vagina. However, the exposure to blood can sometimes be<br />
greater in cesarean section.<br />
Many studies are needed in order to estimate the risk <strong>of</strong><br />
perinatal transmission <strong>of</strong> HCV. Currently, cesarean sections<br />
are not recommended for pregnant women infected with HCV.<br />
Other risk factors associated with delivery are rupture <strong>of</strong> the<br />
placental membrane six hours or more before delivery and<br />
invasive procedures such as internal monitoring <strong>of</strong> the fetus<br />
(Blood 2000; 96:2045).<br />
Clinical Manifestations<br />
Newborns infected with HCV are generally asymptomatic.<br />
In these cases, a significant proportion presents normal<br />
alanine aminotransferase (ALT) levels.<br />
One study monitored 104 children with vertical<br />
transmission upon birth for approximately 49 months (J Infect<br />
Dis 2000;181:419). Although HCV RNA levels were positive<br />
for HCV in 90% <strong>of</strong> these children, the clinical manifestations<br />
were rare. None <strong>of</strong> them presented hepatic insufficiency. <strong>The</strong><br />
majority presented persistent or transitory increase in ALT<br />
levels. Levels <strong>of</strong> ALT were, in general, normal or slightly<br />
increased at birth, evolving to an increase in the fourth to<br />
sixth months <strong>of</strong> age, remaining high for two years, and declining<br />
significantly thereafter.<br />
In that study, 20 children were submitted to hepatic biopsy.<br />
In all cases, evidence <strong>of</strong> chronic hepatitis was found. <strong>The</strong><br />
degree <strong>of</strong> inflammation varied from mild to moderate. In three<br />
cases some level <strong>of</strong> fibrosis was found.<br />
Other studies suggest that children infected with verticallytransmitted<br />
HCV are generally asymptomatic. However, such<br />
transmission is <strong>of</strong>ten accompanied by an increase in ALT<br />
levels during the first 6 to 12 months <strong>of</strong> life.<br />
One large study monitored 266 perinatally HCV-infected<br />
children for an average <strong>of</strong> 4.2 years. In that study, approximately<br />
20% <strong>of</strong> the children presented spontaneous clearance <strong>of</strong> HCV,<br />
and 80% evolved to chronic infection.<br />
Clearance <strong>of</strong> HCV is defined as a loss in the polymerase<br />
chain reaction positivity for HCV RNA in those children who<br />
maintained detectable HCV RNA in the first year <strong>of</strong> life. Most<br />
<strong>of</strong> those children were asymptomatic.<br />
Further studies involving long-term follow-up evaluation<br />
are needed in order to determine what proportion <strong>of</strong> children<br />
with chronic hepatitis C caused by vertical transmission will<br />
develop hepatic insufficiency and hepatocarcinoma.<br />
Diagnosis<br />
<strong>The</strong> initial diagnosis <strong>of</strong> infection with HCV in adults is<br />
made through anti-HCV antibody testing. However, this test<br />
presents limitations when used in children.<br />
This is primarily due to the passage <strong>of</strong> IgG from the mother<br />
to the child through the placental barrier. <strong>The</strong>refore, the<br />
presence <strong>of</strong> anti-HCV in the serum <strong>of</strong> the child does not<br />
necessarily indicate HCV infection. Clearance <strong>of</strong> the anti-HCV<br />
passively acquired from the mother can take more than 12<br />
months, although it occurs within 12 months in 95% <strong>of</strong> the<br />
cases.<br />
Second, the presence <strong>of</strong> maternal anti-HCV does not<br />
necessarily mean that the mother is chronically infected with<br />
HCV.<br />
A diagnosis <strong>of</strong> vertical transmission is made by identifying<br />
HCV RNA in the mother and child.<br />
It is important to emphasize that the HCV RNA test can<br />
also present false-positive or false-negative results. A falsepositive<br />
result can occur as a result <strong>of</strong> contamination <strong>of</strong> positive<br />
samples. A false-negative result occurs due to a loss <strong>of</strong> RNA<br />
during sample storage or to an error in RNA extraction.<br />
A consensus from the National Institutes <strong>of</strong> Health<br />
recommends that children born to mothers testing positive<br />
for HCV should be submitted to the HCV RNA test on two<br />
occasions: between 2 and 6 months <strong>of</strong> life and after 15<br />
months <strong>of</strong> life (together with anti-HCV tests on the latter<br />
occasion).<br />
Conclusions<br />
<strong>The</strong> incidence <strong>of</strong> vertical transmission by HCV is<br />
approximately 2% to 5%. <strong>The</strong> risk is higher in the following<br />
situations: co-infection with HIV; and high maternal viral load<br />
<strong>of</strong> HCV.<br />
<strong>The</strong>re are still no effective interventions to reduce the risk<br />
<strong>of</strong> HCV transmission from the mother to the child. As yet,<br />
HCV testing is not recommended for pregnant women.<br />
References<br />
1. Manzini P., Saracco G., Cerchier A., et al. Human<br />
immunodeficiency virus infection as risk factor for mother-tochild<br />
hepatitis C virus transmission; persistence <strong>of</strong> anti-hepatitis<br />
C virus in children is associated with the mother’s anti-hepatitis<br />
C virus immunoblotting pattern. Hepatology 1995;21:328.<br />
2. Thomas S.L., Newell M.L., Peckham C.S., et al. A review <strong>of</strong><br />
hepatitis C virus (HCV) vertical transmission: risks <strong>of</strong><br />
transmission to infants born to mothers with and without HCV<br />
viraemia or human immunodeficiency virus infection. Int J<br />
Epidemiol 1998;27:108.<br />
3. Yeung L.T., King S.M., Roberts E.A. Mother-to-infant transmission<br />
<strong>of</strong> hepatitis C virus. Hepatology 2001;34:223.<br />
4. Terrault N. Epidemiological evidence for perinatal transmission<br />
<strong>of</strong> hepatitis C virus. Viral Hepatitis Reviews 1998;4:245.<br />
5. Lin H.H., Kao J.H., Hsu H.Y., et al. Possible role <strong>of</strong> high-titer<br />
maternal viremia in perinatal transmission <strong>of</strong> hepatitis C virus.<br />
J Infect Dis 1994;169:638.<br />
6. Kumar R.M., Shahul S. Role <strong>of</strong> breast-feeding in transmission <strong>of</strong><br />
hepatitis C virus to infants <strong>of</strong> HCV-infected mothers. J Hepatol<br />
1998;29:191.<br />
7. Azzari C., Resti M., Moriondo M., et al. Vertical transmission <strong>of</strong><br />
HCV is related to maternal peripheral blood mononuclear cell<br />
infection. Blood 2000;96:2045.<br />
8. Tovo P.A., Pembrey L.J., Newell M.L. Persistence Rate and<br />
Progression <strong>of</strong> Vertically Acquired Hepatitis C Infection. J Infect<br />
Dis 2000;181:419.<br />
9. Vogt M., Lang T., Frosner G., et al. Prevalence and clinical outcome<br />
<strong>of</strong> hepatitis C infection in children who underwent cardiac surgery<br />
before the implementation <strong>of</strong> blood-donor screening. N Engl J<br />
Med 1999;341:866.<br />
10. Three broad modalities in the natural history <strong>of</strong> vertically acquired<br />
hepatitis C virus infection. Clin Infect Dis 2005;41:45.<br />
www.bjid.com.br
12 BJID 2007; 11 Supplement 1 (October)<br />
Hepatitis C: Virological Aspects and Practical Implications<br />
Antonio Alci Barone<br />
Laboratory <strong>of</strong> Hepatitis, LIM 47 DMIP-HC-FMUSP; São Paulo, SP, Brazil<br />
<strong>The</strong> hepatitis C virus (HCV) is a member <strong>of</strong> the Hepacivirus<br />
genus <strong>of</strong> the family Flaviviridae.<br />
Other important pathogens for humans, such as the<br />
dengue virus and the yellow fever virus, belong to this family,<br />
as do infectious agents in animals, such as the bovine viral<br />
diarrhea virus and the classical swine flu virus.<br />
<strong>The</strong> shape <strong>of</strong> HCV is spherical (50 nm in diameter), and it<br />
has an enveloped nucleocapsid and a single-stranded RNA<br />
genome <strong>of</strong> positive polarity. <strong>The</strong> HCV genome, with<br />
approximately 10,000 nucleotides, consists <strong>of</strong> a single long<br />
open reading frame (ORF) flanked by two noncoding regions<br />
(NCRs) at the initial 5’ end, at which the internal ribosome<br />
entry segment (IRES) is located, and at the 3’ end. Its<br />
translation yields a large polyprotein (with nearly 3000 amino<br />
acids) that is processed by viral and host cell proteases into<br />
structural proteins, including the core, envelope 1 (E1), E2,<br />
and p7 proteins, as well as the nonstructural proteins NS2,<br />
NS3, NS4, and NS5. Recently, an alternate reading frame that<br />
codifies an F protein with more than 160 amino acids has been<br />
identified. However, its expression in natural HCV infection<br />
has not been confirmed.<br />
Structural proteins are cleaved by enzymes <strong>of</strong> the<br />
parasitized cell. Envelope proteins are extensively glycosylated<br />
and are involved in the binding with receptors as well as in<br />
the entrance and fusion <strong>of</strong> the virus. <strong>The</strong> function <strong>of</strong> p7 protein<br />
remains unknown. Nonstructural proteins, initially NS2 and<br />
subsequently NS3, undergo self-cleavage and position<br />
themselves in transmembrane domains across the host cell<br />
membrane and into the cytosol or lumen (Figure 1).<br />
Unlike that <strong>of</strong> the hepatitis B virus (HBV), the HCV genome<br />
does not invade the infected cell nucleus. After the binding<br />
through receptors (CD81, a tetraspanin, and the low density<br />
lipoprotein receptor), the HCV genome acts directly as an<br />
mRNA in the cytoplasm, where the translation is initiated<br />
through the IRES in the 5’ NCR. <strong>The</strong> protein produced is<br />
subsequently processed by the cell enzymes and by the<br />
enzymes within the virus itself, yielding structural and<br />
nonstructural proteins. After synthesis and maturation, these<br />
nonstructural proteins and the RNA form replication complexes<br />
that combine with the membrane and catalyze the translation<br />
<strong>of</strong> intermediate negative strands <strong>of</strong> RNA, from which positivestrand<br />
progeny are generated. <strong>The</strong> genomic RNA and capsid<br />
proteins unite, forming the nucleocapsid, which is transported<br />
in cytoplasmic vesicles. While passing through the Golgi<br />
complex, these vesicles assemble with the other particles and<br />
undergo exocytosis and cell release (Figure 2).<br />
<strong>The</strong> study <strong>of</strong> the HCV genome, even in samples obtained<br />
from a single individual, reveals great heterogeneity among<br />
the HCV genotypes. Genotypes in which multiple mutants<br />
<strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> 2007;11 (5) Suppl. 1:12-13.<br />
© 2007 by <strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> and Contexto<br />
Publishing. All rights reserved.<br />
coexist have been designated quasispecies. <strong>The</strong> multiple<br />
mutations represent a rapid and very efficient mechanism for<br />
the virus to evade the immune response and persist in the<br />
host. <strong>The</strong> selection process and the process <strong>of</strong> adaptation<br />
to the host have led to the evolution to different HCV<br />
genotypes. <strong>The</strong> classification system most commonly used<br />
is that proposed by Simmonds et al. and is based on the<br />
similarity <strong>of</strong> the sequence <strong>of</strong> nucleotides using the following<br />
criteria: similarity lower than 72% characterizes a new<br />
genotype; similarity between 75 and 86% characterizes a<br />
new subgenotype. <strong>The</strong>re are 6 genotypes, which are<br />
numbered from 1 to 6, with subgenotypes 1a, 1b, 1c, 2a, 2b,<br />
2c, 3a, 3b, 4a, 5a, and 6a. Although the criterion is based on<br />
molecular biology, this classification has practical,<br />
pathogenetic, epidemiological, and treatment-related<br />
implications. <strong>The</strong>refore, subgenotype 1a is more prevalent<br />
in the USA, 1b in Japan, 3a in Scotland, and 4a in Egypt/<br />
Zaire. In Brazil, genotype 1 is found in approximately 60% <strong>of</strong><br />
the patients, followed by genotype 3, which is found in 20 to<br />
30%, and genotype 2, which is found in a lower percentage.<br />
Subgenotype 1b can cause severe forms <strong>of</strong> the infection<br />
and, similar to genotype 4, does not respond as well to<br />
treatment with IFN-α. <strong>The</strong>refore, genotypes 1 and 4 should<br />
be treated for 48 weeks.<br />
<strong>The</strong> important advances in the knowledge <strong>of</strong> viral hepatitis<br />
B and C are a consequence <strong>of</strong> some facts that will be discussed<br />
herein.<br />
<strong>The</strong> Use <strong>of</strong> Chimpanzees as a Model for the Study <strong>of</strong> Viral<br />
Hepatitis<br />
Although chimpanzees are not natural hosts for these<br />
viruses, they reproduce the disease, thus allowing important<br />
discoveries:<br />
• Epidemiological studies: knowledge <strong>of</strong> these diseases<br />
as communicable;<br />
• Infectivity and titers <strong>of</strong> pools <strong>of</strong> HCV and HBV,<br />
obtained from the infected animals;<br />
• Infectivity <strong>of</strong> the molecular clones <strong>of</strong> HCV and<br />
importance <strong>of</strong> genetic elements specific to HCV;<br />
• Neutralization capacity <strong>of</strong> antibodies specific for HBV<br />
and HCV;<br />
• Protective immunity, tested through re-exposure to the<br />
viruses;<br />
• Mutants that escape to humoral and cellular immunity<br />
could be recognized.<br />
However, the use <strong>of</strong> nonhuman primates has advantages<br />
and disadvantages.<br />
Advantages<br />
<strong>The</strong> only animal susceptible to the acute and chronic forms<br />
<strong>of</strong> the disease; non-selected population; and sequential<br />
biopsies.<br />
www.bjid.com.br
BJID 2007; 11 Supplement 1 (October) Virological Aspects <strong>of</strong> Hepatitis C<br />
13<br />
Figure 1. Organization <strong>of</strong> the HCV genome, polyprotein<br />
processing, and protein topology [1].<br />
Figure 2. HCV cycle in the host cell [1].<br />
Figure 3. Systems used in the HCV in vitro study [1].<br />
Disadvantages<br />
Ethical considerations regarding the use <strong>of</strong> primates; cost<br />
and availability; rarity <strong>of</strong> vertical transmission; more benign<br />
disease presentation; and weaker, more limited immune<br />
response<br />
Use <strong>of</strong> Replicons<br />
In HCV, subgenomic RNA replicons are those in which the<br />
structural region has been replaced by the neomycin<br />
phosphotransferase gene, and the translation <strong>of</strong> the<br />
nonstructural proteins is regulated by the IRES <strong>of</strong> the<br />
encephalomyocarditis virus. Through this experimental<br />
approach, it became possible for the first time to effectively<br />
and efficiently replicate HCV in vitro in cultured Huh-7 human<br />
hepatoma cells. Interestingly, some simple amino acid<br />
substitutions can increase the replication efficiency by up to<br />
10,000 times in all <strong>of</strong> the nonstructural proteins. <strong>The</strong> replicon<br />
system allowed the clarification <strong>of</strong> important aspects <strong>of</strong> the<br />
virus life cycle, as well as simplifying the evaluation <strong>of</strong> new<br />
antiviral strategies. However, some aspects <strong>of</strong> the virus life<br />
cycle cannot be studied using this system.<br />
Efficient Cell Culture Systems for HCV<br />
A 32-year-old male patient <strong>of</strong> Asian origin presented a<br />
pr<strong>of</strong>ile consistent with fulminant hepatitis. Using reverse<br />
transcriptase polymerase chain reaction, HCV RNA was<br />
detected in the serum during the acute phase and not during<br />
the remission phase.<br />
Using these samples, the complete HCV genome was<br />
recovered and cloned. This strain, designated JFH1, has 9678<br />
bp in the genome, with a single long ORF (nt 341-9439), and<br />
encodes 3033 amino acids <strong>The</strong> transfection <strong>of</strong> this sample<br />
into HUH-7.5.1 cultured cells allowed three independent<br />
groups <strong>of</strong> researchers to obtain HCV infecting particles, for<br />
tissue culture as well as for chimpanzee. <strong>The</strong>se studies [2-4]<br />
were published, between June and July <strong>of</strong> 2005, in the following<br />
journals: Proceedings <strong>of</strong> the National Academy <strong>of</strong> Sciences,<br />
Nature Medicine, and Science.<br />
<strong>The</strong> infectious virions <strong>of</strong> HCV obtained in this way have<br />
been used to infect laboratory animals and naïve cells. Such<br />
infection can be monitored by the detection <strong>of</strong> the expression<br />
<strong>of</strong> the NS5A, through analysis <strong>of</strong> reporter genes, or by direct<br />
measurement <strong>of</strong> viral RNA (Figure 3).<br />
In conclusion, more recent findings regarding the<br />
virological aspects <strong>of</strong> HCV have greatly increased the<br />
possibility <strong>of</strong> thoroughly studying this agent and especially<br />
its relationship with the human host. Based on this approach,<br />
it will be possible to better understand how to combat the<br />
virus in chronically infected patients, thus preventing the<br />
progression <strong>of</strong> the disease and its consequences.<br />
References<br />
1. Tellinghuissen T.L., et al. Studying Hepatitis C virus: making the<br />
best <strong>of</strong> a bad virus. <strong>Journal</strong> <strong>of</strong> Virology 2007;81(17):8853-67.<br />
2. Barthenschlager B., et al. Efficient hepatitis C virus cell culture:<br />
what a difference the host cell makes. PNAS 2005;102(28):9739-<br />
40.<br />
3. Wakita T., et al. Production <strong>of</strong> infectious hepatitis C virus in<br />
tissue culture from a cloned viral genome. Nature medicine<br />
2005;11(7):791-6.<br />
4. Lindenbach B.D., et al. Complete replication <strong>of</strong> hepatitis C virus<br />
in cell culture. Science 2005;309:623-6.<br />
5. Kato T., et al. Sequence analysis <strong>of</strong> Hepatitis C virus isolated from<br />
a fulminant hepatitis patient. J Med Virol 2001;64:334-9.<br />
www.bjid.com.br
14 BJID 2007; 11 Supplement 1 (October)<br />
Pathogenesis <strong>of</strong> Hepatitis C – HCV Consensus 2007<br />
Ana Tereza R. Viso<br />
Laboratory <strong>of</strong> Hepatitis, LIM 47 DMIP-HC-FMUSP; São Paulo, SP, Brazil<br />
<strong>The</strong> chronic hepatitis C virus (HCV) infects approximately<br />
130 million people worldwide [1]. It is estimated that<br />
approximately 15% <strong>of</strong> HCV-infected individuals eliminate the<br />
virus spontaneously, that 25% develop a mild form <strong>of</strong> the<br />
disease, and that 60% develop the chronic progressive form<br />
[2]. <strong>The</strong> elimination or persistence <strong>of</strong> HCV infection depends<br />
on the balance between the effectiveness, specificity and<br />
rapidity <strong>of</strong> the innate and adaptive immune responses, as well<br />
as on the HCV replication rate [3]. Persistence <strong>of</strong> HCV can<br />
also be caused by infection at privileged (extrahepatic) sites,<br />
viral inhibition <strong>of</strong> antigen presentation, selective immune<br />
suppression, negative regulation <strong>of</strong> HCV gene expression,<br />
viral mutations, immune exhaustion <strong>of</strong> T cells and the<br />
incomplete differentiation <strong>of</strong> memory T cells [4,5].<br />
Fibrosis is the principal complication <strong>of</strong> chronic hepatitis<br />
C, and it is estimated that 20% <strong>of</strong> patients develop cirrhosis<br />
over a period <strong>of</strong> 10, 20 or 30 years [2,6]. <strong>The</strong> progression <strong>of</strong><br />
fibrosis increases morbidity and mortality in chronic hepatitis<br />
C [7], since it can lead to death due to complications caused<br />
by cirrhosis or hepatocarcinoma [2].<br />
Various studies have associated the progression <strong>of</strong> fibrosis<br />
in hepatitis C with diverse factors such as: the kinetics and<br />
pathogenicity <strong>of</strong> HCV; host-HCV interaction; intrinsic host<br />
factors such as demographic pr<strong>of</strong>ile, body mass index and<br />
diabetes mellitus; host exposure to external factors; and the<br />
form <strong>of</strong> HCV acquisition.<br />
Life Cycle and Pathogenicity <strong>of</strong> HCV<br />
Belonging to the Flaviviridae family, HCV is a small<br />
enveloped virus [8]. Its genome consists <strong>of</strong> one RNA molecule<br />
that is composed <strong>of</strong> two terminal regions, 5’- and 3’-<br />
untranslated regions, and between these there is a single open<br />
reading frame that encodes a polyprotein with approximately<br />
3000 amino acids. This polyprotein cleaves at the N-terminal<br />
side <strong>of</strong> three structural proteins, the nucleocapsid (core),<br />
envelope 1 (E1) and envelope 2 (E2), all <strong>of</strong> which are involved<br />
in the architectural organization <strong>of</strong> HCV. At the carboxylterminal<br />
side, the polyprotein cleaves to six nonstructural<br />
proteins, NS2, NS3, NS4 (NS4A and NS4B), NS5 (NS5A and<br />
NS5B) and NS6, which are responsible for the life cycle <strong>of</strong> the<br />
virus [9].<br />
After entering a susceptible host, HCV invades, infects<br />
and replicates within the blood stream, repeating the process<br />
in various tissues, as well as in peripheral B and T lymphocytes,<br />
as it proceeds to the liver by tropism, passing through various<br />
tissues such as those <strong>of</strong> the pancreas, thyroid, adrenal glands,<br />
<strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> 2007;11 (5) Suppl. 1:14-19.<br />
© 2007 by <strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> and Contexto<br />
Publishing. All rights reserved.<br />
spleen and bone marrow [10-12]. Since HCV can also directly<br />
infect the lymphatic tissue, its stimulation can lead to the<br />
development <strong>of</strong> B-cell lymphomas [13]. It is known that the<br />
liver is the principal site <strong>of</strong> HCV replication, and various studies<br />
have shown that this virus infects approximately 10% <strong>of</strong><br />
hepatic cells [5]. Infection with HCV at extrahepatic sites can<br />
promote the appearance <strong>of</strong> HCV variants [14,15], thereby<br />
decreasing the chance that the immune system will recognize<br />
the virus.<br />
To enter the host cell, HCV E2 and E1 proteins recognize<br />
and bond with the CD81 receptors present on the surface <strong>of</strong><br />
hepatocytes and lymphocytes [16,17]. Circulating HCV<br />
particles are accompanied by low-density and very lowdensity<br />
lipoproteins, which prompts discussion in the<br />
literature regarding the possibility that low-density lipoprotein<br />
is also a viral receptor [15]. After the interaction <strong>of</strong> the virus<br />
envelope with the host cell membrane, HCV enters the cell<br />
through endocytosis. In the cytoplasm, the messenger RNA<br />
then undergoes translation, and polyproteins are processed;<br />
the HCV RNA then replicates, after which the new viral ‘RNA’s<br />
are packaged and transported to the surface <strong>of</strong> the host cell<br />
so that they can disseminate and complete a new cycle [18].<br />
<strong>The</strong> HCV replication rate is high, approximately 1 × 10 12 virions<br />
per day; this, together with its high mutation rate, estimated at<br />
10 -3 nucleotide substitutions per year, leads to great<br />
heterogeneity in its presentations, which are known as<br />
quasispecies [8]. <strong>The</strong> selection <strong>of</strong> and host adaptation to HCV<br />
quasispecies have given rise to distinct genotypes [19] whose<br />
classification is based on the similarity <strong>of</strong> the sequence <strong>of</strong><br />
nucleotides: similarity below 69% characterizes a new viral type;<br />
and similarity between 75 and 80% characterizes a subtype [20].<br />
<strong>The</strong> progression <strong>of</strong> fibrosis in chronic hepatitis C has been<br />
associated with the diversity <strong>of</strong> HCV quasispecies [21]. <strong>The</strong><br />
production <strong>of</strong> new viruses is counterbalanced by the<br />
destruction <strong>of</strong> infected cells through tissue apoptosis or<br />
degradation in peripheral blood, since the half-life <strong>of</strong> the virus<br />
in peripheral blood is approximately 2.7 hours [7]. Experimental<br />
studies have shown that NS3 and NS5 proteins induce<br />
apoptosis in infected hepatocytes [22].<br />
In individuals infected with HCV, the persistence <strong>of</strong> the<br />
virus can be attributed the large inoculum and the high rate <strong>of</strong><br />
viral replication, which allow the virus to evade the host<br />
immune response [4,23]. <strong>The</strong>re is controversy over whether<br />
the sequence <strong>of</strong> nucleotides is directly associated with more<br />
intense hepatic lesions [6,24,25].<br />
<strong>The</strong>re is some evidence <strong>of</strong> direct cytopathic lesion caused<br />
by HCV, including HCV-induced histological lesions with scant<br />
inflammatory infiltrate [26-28], fulminant hepatitis C after<br />
chemotherapy in liver transplants [29] and HCV-related acute<br />
cholestatic syndrome after renal transplantation [30].<br />
www.bjid.com.br
BJID 2007; 11 Supplement 1 (October) Pathogenesis <strong>of</strong> Hepatitis C<br />
15<br />
Studies suggest that specific genotypes, such as genotype<br />
1, can be more cytopathic [31] or can induce more rapid<br />
progression <strong>of</strong> the disease than do other genotypes [32].<br />
Genotype 1 has been shown to be the genotype most strongly<br />
associated with chronic HCV infection [33]. <strong>The</strong> risk <strong>of</strong><br />
cirrhosis and hepatocarcinoma has been shown to be greater<br />
in individuals presenting genotype 1b than in those presenting<br />
genotypes 2 and 3 [34]. However, other authors have stated<br />
that HCV genotype and viral load do not influence the<br />
progression <strong>of</strong> the disease [2,6].<br />
It is known that steatosis is a c<strong>of</strong>actor that influences the<br />
progression <strong>of</strong> fibrosis in chronic hepatitis C [35]. Various<br />
studies have directly associated steatosis with HCV genotype<br />
3 [36,37]. <strong>The</strong>refore, genotype 3 is considered cytopathic<br />
[38,39]. Kumar et al. identified the reduction <strong>of</strong> steatosis as<br />
the only variable predictive <strong>of</strong> the virological response to the<br />
treatment <strong>of</strong> chronic hepatitis C in individuals infected with<br />
HCV genotype 3 [38].<br />
Innate Immune Response to HCV<br />
<strong>The</strong> innate immune response to HCV is responsible for<br />
the activation <strong>of</strong> cytokines such as interferon (IFN) which<br />
activate antiviral proteins that inhibit the replication <strong>of</strong> the<br />
virus while the adaptive immune response to HCV neutralizes<br />
viral particles and destroys infected cells [40]. Studies <strong>of</strong> HCVinfected<br />
chimpanzees that eliminate the virus without the<br />
specific T-cell immune response suggest that, in some cases,<br />
the innate immune response might be sufficient to destroy<br />
the infection [41].<br />
<strong>The</strong> RNA <strong>of</strong> HCV is recognized by the innate immune<br />
response through the Toll-like receptor which responds with<br />
the production <strong>of</strong> IFN-1α and IFN-1β [5,42]. IFN-1 stimulates<br />
the nitric oxide synthase enzyme that is expressed in<br />
hepatocytes and macrophages as the is<strong>of</strong>orm inducible nitric<br />
oxide synthase [43]. Patients with HCV who are treated with<br />
IFN present higher levels <strong>of</strong> inducible nitric oxide synthase,<br />
which have been correlated with lower serum levels <strong>of</strong> alanine<br />
aminotransferase [44].<br />
In addition, IFN-1 induces the production <strong>of</strong> various<br />
proteins such as protein kinase (PKR), 2’,5’-oligoadenylate<br />
synthetase (OAS) and the Mx protein [44]. <strong>The</strong>se proteins are<br />
responsible for the expression <strong>of</strong> the genes that inhibit the<br />
replication <strong>of</strong> this virus within hepatocytes in an attempt to destroy<br />
the infection [7,40]. When IFN bonds with the IFN receptor on<br />
the surface <strong>of</strong> the infected cell, it activates the Janus kinase,<br />
which induces phosphorylation <strong>of</strong> cytoplasmic proteins known<br />
as signal transducers and activators <strong>of</strong> transcription (STATs),<br />
specifically STAT 1 and STAT 2. <strong>The</strong> STATs form a dimer that<br />
directs itself to the cell nucleus where it forms a complex with<br />
the p48 protein, which is a stimulation factor for IFN-stimulated<br />
gene factor 3. That complex bonds with the IFN-stimulated<br />
response element ISRE, which is an RNA-polymerase promoter<br />
complex, and there is a stimulus <strong>of</strong> the genes responsible for the<br />
production <strong>of</strong> antiviral response proteins and <strong>of</strong> major<br />
histocompatibility complex (MHC) proteins [44].<br />
Some individuals present genetic alterations in the STATs<br />
or in the Janus kinase that would impede the formation <strong>of</strong><br />
antiviral proteins [45].<br />
Various viral proteins have shown a capacity to escape<br />
the effect <strong>of</strong> IFN, as evidenced by the high rate <strong>of</strong> resistance<br />
to treatment with IFN-α seen among individuals with hepatitis<br />
C [44,45].<br />
<strong>The</strong>re are various characteristics <strong>of</strong> HCV that allow it to<br />
evade the innate immune response:<br />
• <strong>The</strong> viral replication complex appears to be composed<br />
<strong>of</strong> a membrane that is highly resistant to in vitro<br />
proteases and nucleases, which protects HCV from<br />
detection by the innate immune response [40].<br />
• <strong>The</strong> HCV core protein interacts with diverse cell factors,<br />
including the tumor necrosis factor (TNF) receptor,<br />
which decreases the cytolytic activity <strong>of</strong> T cells [46]<br />
• Core proteins impede the antiviral activity <strong>of</strong> IFN, as<br />
do NS3/4A and NS5A proteins [40].<br />
• <strong>The</strong> NS3/4A proteins can impede the recognition <strong>of</strong><br />
the Toll-like receptor [5].<br />
• <strong>The</strong> NS5A and E2 proteins can bind to PKR, thereby<br />
blocking its activity [5].<br />
• Multiple mutations in the IFN-sensitivity-determining<br />
region (ISDR) modify the NS5A region, which inhibits<br />
the phosphorylation <strong>of</strong> PKR, thereby impeding its<br />
antiviral activity [45].<br />
• <strong>The</strong> E2 region <strong>of</strong> HCV contains a sequence <strong>of</strong> eight<br />
amino acids identical to those <strong>of</strong> PKR, and this<br />
sequence is more common in genotype 1 than in<br />
genotypes 2 and 3, which probably accounts for the<br />
fact that individuals infected with genotype 1 present<br />
greater resistance to treatment with IFN [44].<br />
• Mutations in the ISDR sequence <strong>of</strong> NS5A suppress<br />
the antiviral action <strong>of</strong> OAS.<br />
• Levels <strong>of</strong> this protein are lower in nonresponders to<br />
treatment with IFN [44].<br />
<strong>The</strong> liver cell populations that participate in the innate<br />
immune response are the natural killer (NK) cells, NK T cells,<br />
Kupffer cells and dendritic cells [5]. <strong>The</strong> NK cells respond<br />
minutes or hours after HCV infection by polarizing <strong>of</strong> the<br />
granules in the direction <strong>of</strong> the infected cells as well as by<br />
releasing perforins that fragment the nuclei <strong>of</strong> infected cells<br />
and induce apoptosis [47]. <strong>The</strong>y inhibit viral replication with<br />
the production <strong>of</strong> IFN gamma (IFN-γ), which recruits intrahepatic<br />
inflammatory cells and stimulates the T-helper 1 (Th1) response<br />
[48], thereby inducing the necrosis or apoptosis <strong>of</strong> the HCVinfected<br />
cell [49]. Studies suggest that HCV inhibits receptor<br />
genes in the activation <strong>of</strong> NK cells, decreasing the activity <strong>of</strong><br />
these cells by reducing their number and function in chronically<br />
infected individuals [40]. <strong>The</strong> NK cells also have the capacity<br />
to increase the functions <strong>of</strong> dendritic cells in the presence <strong>of</strong><br />
hepatic cells, although that capacity is impaired in NK cells<br />
derived from patients with chronic hepatitis C, in which the<br />
production <strong>of</strong> interleukin (IL)-10 and transforming growth factor<br />
beta (TGF-β) can inhibit the activity <strong>of</strong> dendritic cells [50].<br />
www.bjid.com.br
16 Pathogenesis <strong>of</strong> Hepatitis C<br />
BJID 2007; 11 Supplement 1 (October)<br />
After HCV enters the host cell, the binding <strong>of</strong> the E2<br />
glycoprotein with the CD81 receptor <strong>of</strong> NK cells inhibits the<br />
function <strong>of</strong> the NK cells [7,51], which alters the immune<br />
response to HCV infection. <strong>The</strong> E2 glycoprotein also inhibits<br />
cytotoxicity and the production <strong>of</strong> IFNγ by NK cells [40].<br />
Various studies have suggested that the failure <strong>of</strong> dendritic<br />
cells to recognize HCV contributes to the persistence <strong>of</strong><br />
hepatitis C [50,52-54].<br />
Humoral Immune Response to HCV<br />
After HCV infection, there is expression <strong>of</strong> the<br />
hypervariable NS1/E2 region on the surface <strong>of</strong> the virus, which<br />
stimulates B cells to produce high antibody titers <strong>of</strong> antibodies<br />
with the objective <strong>of</strong> destroying the permanence <strong>of</strong> the virus<br />
[44]. <strong>The</strong> appearance <strong>of</strong> anti-HCV antibodies is significantly<br />
delayed, and these antibodies can first be detected from 7 to<br />
31 weeks after infection [7]. <strong>The</strong> host applies selective pressure<br />
on HCV, and this stimulates high nucleotide variation, as well<br />
as the appearance <strong>of</strong> mutations in the envelope proteins, from<br />
which the virus selects genomic variants in an attempt to<br />
eliminate the site <strong>of</strong> immune response recognition [55]. <strong>The</strong><br />
great quantity <strong>of</strong> HCV quasispecies formed allows the virus<br />
to evade the humoral immune response, and the effect <strong>of</strong> HCVneutralizing<br />
antibodies appears to be insufficient to control<br />
the infection [7], which therefore persists [15].<br />
Similar to what occurs in auto-immune type 2 hepatitis,<br />
HCV can mimic the immune system, leading to viral escape or<br />
postinfection immunity [4,56]. Anti-HCV antibodies have been<br />
implicated in tissue damage due to the formation <strong>of</strong><br />
immunocomplexes such as antinuclear antibodies [57], autoantibodies<br />
that act against cytochrome P450 and antibodies<br />
that act against the liver and kidney [4]. <strong>The</strong> deposition <strong>of</strong><br />
immunocomplexes has been related to the appearance <strong>of</strong><br />
extrahepatic manifestations, such as arthritis,<br />
cryoglobulinemia [58], vasculitis, glomerulonephritis, Sicca<br />
syndrome and itchiness, all <strong>of</strong> which cause considerable<br />
morbidity [57].<br />
<strong>The</strong>re is evidence that HCV infection can be resolved by<br />
the cell response with specific CD4+ and CD8+ T cells when<br />
there is no formation <strong>of</strong> antibodies against this virus [59,60],<br />
showing that the humoral immune response is not always<br />
involved in the response to HCV infection.<br />
Cell Response to HCV<br />
Since there is a weak humoral immune response to HCV, it<br />
is believed that the reactivity <strong>of</strong> cytotoxic T-lymphocytes<br />
(CTLs) or CD8+ T cells is fundamental to viral elimination<br />
[61,62], and that impairment <strong>of</strong> this reactivity is one <strong>of</strong> the<br />
factors responsible for the chronicity <strong>of</strong> the infection<br />
[7,63,64]. <strong>The</strong> CD8+ T cells can eliminate HCV from the liver<br />
through two mechanisms: inducement <strong>of</strong> apoptosis in<br />
infected hepatocytes; and suppression <strong>of</strong> replication by the<br />
production <strong>of</strong> IFN-γ [22,65]. <strong>The</strong> CTL response is less<br />
vigorous in chronically infected patients than in those<br />
presenting acute infection [4]. This can be the result <strong>of</strong><br />
immunologic tolerance or exhaustion <strong>of</strong> the CD8+ T cell<br />
response to the high viral load that persists in individuals<br />
chronically infected with HCV [4].<br />
In addition to CD8+ T cells, CD4+ T cells seem to be<br />
involved in the viral damage mediated by the increased<br />
expression <strong>of</strong> MHC class II molecules. Some studies have<br />
attributed the vigorous and long-lasting response <strong>of</strong> CD4+ T<br />
cells to the elimination <strong>of</strong> HCV in the acute form the infection<br />
[4,66]. However, the loss <strong>of</strong> the specific CD4+ T cell reactivity<br />
to HCV has been associated with the persistence <strong>of</strong> the virus<br />
and the progression <strong>of</strong> liver damage [67,68].<br />
In acute HCV infection, the peak in serum levels <strong>of</strong><br />
transaminases corresponds with the cell response, which<br />
suggests that the hepatic lesion is immune-mediated [5,64]. It<br />
is known that, after activation, T cells initiate clonal<br />
proliferation by secreting cytokines and other substances that<br />
can affect hepatic function in a variety <strong>of</strong> ways [69].<br />
Various cytokines act as mediators in the inflammation<br />
caused by chronic hepatitis C and have been related to<br />
hepatocyte death, i.e. cholestasis and fibrosis, and<br />
paradoxically play a role in regeneration following hepatic<br />
injury [69,70]. It is argued that the imbalance between the<br />
production <strong>of</strong> Th1 and Th2 cytokines is related to the<br />
progression <strong>of</strong> chronic hepatitis C. <strong>The</strong> expression <strong>of</strong> Th1<br />
cytokines such as IL-2 and TNF-α has been shown to be<br />
related to the more aggressive presentation <strong>of</strong> hepatic disease,<br />
whereas the expression <strong>of</strong> Th2 cytokines such as IL-10 has<br />
been shown to be related to the milder presentation [71].<br />
<strong>The</strong> production <strong>of</strong> TNF-α is one <strong>of</strong> the earliest events in<br />
hepatic injury and is the ‘trigger’ for the production <strong>of</strong> other<br />
cytokines [72], as well as being implicated in the inducement<br />
<strong>of</strong> hepatocyte apoptosis in viral hepatitis [73].<br />
<strong>The</strong> levels <strong>of</strong> cytokines such as IFN-γ, TNF-α, IL-6 and<br />
IL-8 are elevated in individuals with chronic hepatitis C [74-<br />
82], and some authors have shown that this increase is<br />
proportional to the extent <strong>of</strong> the damage, histologically<br />
[26,76,83,84].<br />
<strong>The</strong>re is evidence that IL-4 can modulate the immune<br />
response in HCV-infected individuals [75], principally through<br />
the activity <strong>of</strong> Th2 cells.<br />
It has been shown that IL-10 can suppress proliferation in<br />
the Th1 and Th2 responses, as well as inducing anergy [85].<br />
<strong>The</strong>re is evidence that IL-10 levels increase in chronic hepatitis<br />
C [75]. Some studies report reduced inflammatory activity [86],<br />
and others report that administration <strong>of</strong> IL-10 to such patients<br />
causes fibrosis [87].<br />
Various studies have shown that TGF-β is increased in<br />
chronic hepatitis C and is involved in the progression <strong>of</strong><br />
fibrosis, which has been challenged by other authors [88,89].<br />
It has been suggested that TGF-β and IL-10 act as<br />
immunosuppressive agents in the liver [90]. In addition, both<br />
have been shown to inhibit the immune response and regulate<br />
the activity <strong>of</strong> dendritic cells [91], which can establish a<br />
balance between the Th1 and Th2 responses in chronic<br />
diseases [92].<br />
www.bjid.com.br
BJID 2007; 11 Supplement 1 (October) Pathogenesis <strong>of</strong> Hepatitis C<br />
17<br />
Host Factors Associated with the Persistence and<br />
Progression <strong>of</strong> Hepatitis C<br />
In HCV infection, the genetic constitution and immune<br />
‘status’ <strong>of</strong> the host are important factors in the persistence<br />
and progression <strong>of</strong> the virus [23,93], since they influence<br />
antigen recognition and presentation, as well as the type <strong>of</strong><br />
Th response [94].<br />
Some MHC class II alleles, such as DR5, have been<br />
associated with a lower incidence <strong>of</strong> cirrhosis in individuals<br />
chronically infected with HCV [94]. Rehermann et al. [95]<br />
identified CTLs restricted by histocompatibility leukocyte<br />
antigen A2 in 97% <strong>of</strong> chronic hepatitis C patients, compared<br />
with 2% <strong>of</strong> anti-HCV-negative controls. It is speculated that<br />
the MHC class II molecule presentation <strong>of</strong> antigens is deficient<br />
in HCV-infected cells, since some viral proteins inhibit the<br />
presentation <strong>of</strong> the antigen through IFN-induced negative<br />
immunoregulation [44].<br />
Some pro-inflammatory cytokines appear to be associated<br />
with the viral infection response as well as with the expression<br />
<strong>of</strong> specific haplotypes [94], such as IL-10 haplotypes, which<br />
can be predictors <strong>of</strong> spontaneous elimination <strong>of</strong> HCV [96].<br />
However, there is disagreement in the literature, since other<br />
authors did not find evidence for polymorphism in the studied<br />
genes being considered as a relevant factor in the elimination<br />
<strong>of</strong> HCV or in the response to treatment [97-99].<br />
<strong>The</strong> influence <strong>of</strong> demographic data such as age, gender<br />
[6,34] and ‘race’ [100,101] in the progression <strong>of</strong> hepatitis C<br />
can be due to genetic variations existent among those. Some<br />
studies report that HCV positivity increases with age [34,101],<br />
thereby leading to a greater chance <strong>of</strong> progression <strong>of</strong> the<br />
disease [6,34]. <strong>The</strong> male gender is more prevalent in most<br />
studies on hepatitis C [6,101] and, in addition, it was associated<br />
with the progression <strong>of</strong> the disease to cirrhosis [6,34]. Some<br />
studies suggest that Afro-Americans, due to a greater<br />
propensity to chronicity, resistance to treatment (higher<br />
percentage <strong>of</strong> genotype 1) and development <strong>of</strong><br />
hepatocarcinoma, present a worse evolution <strong>of</strong> hepatitis C<br />
than do Caucasian-Americans [100,102]. Analyzing 99 chronic<br />
HCV-infected individuals and 31 individuals who had<br />
spontaneously eliminated HCV, Sugimoto et al. [103] found<br />
evidence that the CD4+ T-cell response was less vigorous in<br />
Afro-Americans than in Caucasian-Americans, with a<br />
predominance <strong>of</strong> the Th2 response and maintenance <strong>of</strong> the<br />
infection. <strong>The</strong> evolution <strong>of</strong> hepatitis C in different ethnicities<br />
could be due to genetic factors, such as the presence <strong>of</strong> HLA<br />
class II alleles, which could define the spontaneous elimination<br />
<strong>of</strong> HCV [104].<br />
<strong>The</strong>re are various extrinsic host factors that are related to<br />
the progression <strong>of</strong> chronic hepatitis C: alcohol abuse; smoking<br />
[6,34,105-109]; the endovenous acquisition <strong>of</strong> HCV; and<br />
coinfection with other viruses such as HIV, HBV and human<br />
T-cell lymphotropic virus [6,110,111].<br />
<strong>The</strong> prevalence <strong>of</strong> HCV infection is higher among<br />
individuals who consume alcohol [112,113]. Studies suggest<br />
that alcohol increases the ability <strong>of</strong> HCV to enter and persist<br />
within the organism [112]. Other studies argue that alcohol<br />
intake affects some components <strong>of</strong> the immune response<br />
[112] and can alter the inflammatory response <strong>of</strong> cytokines,<br />
thereby increasing viremia, which can be an important<br />
c<strong>of</strong>actor in the development <strong>of</strong> hepatocarcinoma [114]. In<br />
addition, alcohol intake in HCV-infected individuals<br />
increases hepatic steatosis and induces apoptosis<br />
[107,112,115].<br />
Smoking, in addition to increasing inflammatory activity<br />
and hepatic fibroses [109], can induce direct injury to the<br />
liver, as well as causing indirect damage (toxic effect), and<br />
can have immunological effects (production <strong>of</strong> IL-1, IL-6 and<br />
TNF-a, which cause liver damage).<br />
References<br />
1. Alter M.J. Epidemiology <strong>of</strong> hepatitis C virus infection. World J<br />
Gastroenterol 2007;13(17):2436-41.<br />
2. EASL International Consensus Conference on Hepatitis C: Paris<br />
26-28, February 1999. Consensus Statement. J Hepatology<br />
1999;30:956-61.<br />
3. Brown P.M.J., Neuman M.G. Immunopathogenesis <strong>of</strong> hepatitis C<br />
viral infection: Th1/Th2 responses and the role <strong>of</strong> cytokines.<br />
Clin Biochemistry 2001;34:167-71.<br />
4. Cerny A., Chisari F.V. Pathogenesis <strong>of</strong> chronic hepatitis C:<br />
Immunological features <strong>of</strong> hepatic injury and viral persistence.<br />
Hepatology 1999;30:595-601.<br />
5. Dustin L.B., Rice C.M. Flying under the radar: the immunobiology<br />
<strong>of</strong> hepatitis C. Annu Rev Immunol 2007;25:71-99.<br />
6. Poynard T., et al. Natural history <strong>of</strong> liver fibrosis progression in<br />
patients with chronic hepatitis C. <strong>The</strong> OBSVIRC, METAVIR,<br />
CLINIVIR, and DOSVIRC groups. Lancet 1997;394:825-32.<br />
7. Pawlotsky J.M. Pathophysiology <strong>of</strong> hepatitis C infection and<br />
related liver disease. Trends Microbiol 2004;12(2):96-102.<br />
8. Major M.E., et al. Hepatology 1997;25:1527-38.<br />
9. McGarvey M.J., et al. Structure and molecular virology. In:<br />
Zuckerman AJ, Toma HC, editors. Viral hepatitis. 2 nd ed. London:<br />
Churchill Livingstone; 1998. p.253-70.<br />
10. Koziel M.J., et al. Intrahepatic cytotoxic T Lymphocytes specific<br />
for hepatitis C virus in persons with chronic hepatitis. J Immunol<br />
1992;149(10):3339-44.<br />
11. Gowans E.J. Distribution <strong>of</strong> markers <strong>of</strong> hepatitis C virus infection<br />
throughout the body. Semm Liver Dis 2000;20:85-102.<br />
12. MacDonald A.J., et al. CD4 T helper type 1 and regulatory T cells<br />
induced against the same epitopes on the core protein in hepatitis<br />
C virus-infected persons. J Infect Dis 2002;185:720-7.<br />
13. Ferri C., et al. Hepatitis C vírus infection and B-cell lymphomas.<br />
Eur J Can 1994;30:1591-2.<br />
14. Maggi F., et al. Differences in hepatitis C virus quasispecies<br />
composition between liver, peripheral blood mononuclear cells<br />
and plasma. J Gen Virol 1997;78(Pt 7):1521-5.<br />
15. Giannini C., Bréchot C. Hepatitis C virus biology. Cell Death and<br />
Differentiation 2003;(10):S27-38.<br />
16. Pileri P., et al. Binding <strong>of</strong> hepatitis C virus to CD81. Science<br />
1998;282:938-41.<br />
17. Polyak S.J. Hepatitis C virus-cell interactions and their role in<br />
pathogenesis. Clin Liver Dis 2003; 7:67-88.<br />
18. Lindenbach B.D., Rice C.M. Unravelling hepatitis C virus<br />
replication from genome to function. Nature<br />
2005;436(18):933-8.<br />
19. Simmonds P., et al. Classification <strong>of</strong> hepatitis C virus into six major<br />
genotypes and a series <strong>of</strong> subtypes by phylogenetic analysis <strong>of</strong><br />
the NS-5 region. J General Virology 1993;74:2391-9.<br />
20. Simmonds P., et al. Consensus Proposals for a unified system <strong>of</strong><br />
nomenclature <strong>of</strong> hepatitis C virus genotypes. Hepatology<br />
2005;42(4):963-73.<br />
www.bjid.com.br
18 Pathogenesis <strong>of</strong> Hepatitis C<br />
BJID 2007; 11 Supplement 1 (October)<br />
21. Wang X.H., et al. Progression <strong>of</strong> fibrosis during chronic hepatitis<br />
C is associated with rapid virus evolution. J Virol<br />
2007;81(12):6513-22.<br />
22. Herzer K., et al. Hepatitis viruses: live and let die. Liver Int<br />
2007;27(3):293-301.<br />
23. Gremion C., Cerny A. Hepatitis C virus and the immune system: a<br />
concise review. Rev Med Virol 2005;15(4):235-68.<br />
24. Haruna Y., et al. Detection <strong>of</strong> hepatitis C virus RNA in liver tissues by<br />
an in situ hybridization technique. J Hepatol 1993;18(1):96-100.<br />
25. Brillanti S., et al. Persistent hepatitis C viraemia without liver<br />
disease. Lancet 1993;341(8843):464-5.<br />
26. Miller R.H., Purcell R.H. Hepatitis C virus shares amino acid<br />
sequence similarity with pestiviruses and flaviviruses as well as<br />
members <strong>of</strong> two plant virus supergroups. Proc Natl Acad Sci<br />
USA 1990;87:2057-61.<br />
27. Gonzalez-Peralta R.P., et al. Optimization for the detection <strong>of</strong><br />
hepatitis C virus antigens in the liver. J Hepatol 1994;20:143-47.<br />
28. Barone A.A., et al. Response in patients with chronic HCV hepatitis<br />
to treatment with interferon-alpha. Braz J Infect Dis<br />
1999;3(3):118-28.<br />
29. Naoumov N.V. Hepatitis C virus-specific CD4+ T cells: do they<br />
help or damage? Gastroenterology 1999;117:1012-4.<br />
30. Delladetsima J.K., et al. Cholestatic syndrome with bile duct damage<br />
and loss in renal transplant recipients with HCV infection. Liver<br />
2001;21(2):81-8.<br />
31. Dusheiko G., et al. Hepatitis C virus genotypes: an investigation<br />
<strong>of</strong> typo-specific differences in geographic origin and disease.<br />
Hepatology 1994;19:13-8.<br />
32. Kobayashi M., et al. <strong>The</strong> natural course <strong>of</strong> chronic hepatitis C: a<br />
comparison between patients with genotypes 1 and 2 hepatitis<br />
C viruses. Hepatology 1996;23(4):695-9.<br />
33. Amoroso P., et al. Correlation between virus genotype and chronicity<br />
rate in acute hepatitis C. J Hepatology 1998;28:936-44.<br />
34. Bellentani S., et al. Clinical course and risk factors <strong>of</strong> hepatitis C<br />
virus related liver disease in the general population: report from<br />
the Dionysos study. Gut 1999;44(6):874-80.<br />
35. Cholet et al. Factors associated with liver steatosis and fibrosis in<br />
chronic hepatitis C patients. Gastroenterol Clin Biol<br />
2004;28:272-8.<br />
36. Rubbia-Brandt L., et al. Steatosis affects chronic hepatitis C<br />
progression in a genotype specific way. Gut 2004;53(3):406-12.<br />
37. Sharma P., et al. Hepatic steatosis in hepatitis C virus genotype 3<br />
infection: does it correlate with body mass index, fibrosis, and<br />
HCV risk factors? Dig Dis Sci 2004;49(1):25-9.<br />
38. Kumar D., et al. Hepatitis C virus genotype 3 is cytopathic to<br />
hepatocytes: reversal <strong>of</strong> hepatic steatosis after sustained<br />
therapeutic response. Hepatology 2002;36:1466-72.<br />
39. Negro F. Mechanisms and significance <strong>of</strong> liver steatosis in hepatitis<br />
C virus infection. World J Gastroenterol 2006;12(42):6756-65.<br />
40. Thimme R., et al. A target on the move: innate and adaptive<br />
immune escape strategies <strong>of</strong> hepatitis C virus. Antiviral Res<br />
2006;69(3):129-41.<br />
41. Lloyd A.R., et al. Host and viral factors in the immunopathogenesis<br />
<strong>of</strong> primary hepatitis C virus infection. Immunol Cell Biol<br />
2007;85(1):24-32.<br />
42. Mizukoshi E., Rehermann B. Immune responses and immunity in<br />
hepatitis C virus infection. J Gastroenterol 2001;36(12):799-808.<br />
43. Samuel C.E. Antiviral actions <strong>of</strong> interferons. Clin Microbil Rev<br />
2001;14(4):778-809.<br />
44. Taylor D.R., et al. Hepatitis C virus and interferon resistance.<br />
Microbes and Infection 2000;2:1743-56.<br />
45. Tan S.-L., Katze M.G. How hepatitis C virus counteracts the<br />
interferon response: the jury is still out on NS5A. Virology<br />
2001;284:1-12.<br />
46. Chen C.M., et al. Direct interaction <strong>of</strong> hepatitis C virus core<br />
protein with the cellular lymphotoxin-beta receptor modulates<br />
the signal pathway <strong>of</strong> the lymphotoxin-beta receptor. J Virol<br />
1997;71(12):9417-26.<br />
47. Rehermann B., Chisari F.V. Cell mediated immune response to<br />
the hepatitis C virus. Curr Top Microbiol Immunol<br />
2000;242:299-325.<br />
48. Janeway C.A., et al. Imunobiologia: o sistema imune na saúde e na<br />
doença. Tradução Ana Cristina Arámburu da Silva, Cristina<br />
Bonorino, Denise Cantarelli Machado, Gaby Renard, Isabel<br />
Cristina Ribas Werlang, Moisés Evandro Bauer. 6ª ed. Porto<br />
Alegre: Artmed, 2007. Cap. 1, p.37-101: Imunidade Inata.<br />
49. Winnock M., et al. Liver-associated lymphocytes: role in tumor<br />
defense. Semin Liver Dis 1993;13:81-92.<br />
50. Jinushi M., et al. Negative regulation <strong>of</strong> NK cell activities by<br />
inhibitory receptor CD94/NKG2A leads to altered NK cell-induced<br />
modulation <strong>of</strong> dendritic cell functions in chronic hepatitis C virus<br />
infection. J Immunol 2004;15;173(10):6072-81.<br />
51. Crotta S., et al. Inhibition <strong>of</strong> natural killer cells through engagement<br />
<strong>of</strong> CD81 by the major hepatitis C virus envelope protein. J Exp<br />
Med 2002;195(1):35-41.<br />
52. Longman R.S., et al. Presence <strong>of</strong> functional dendritic cells in<br />
patients chronically infected with hepatitis C virus. Blood<br />
2004;103(3):1026-9.<br />
53. Bain C., et al. Impaired Assostimulatory function <strong>of</strong> dendritic cells<br />
in chronic hepatitis C infection. Gastroenterlol<br />
2001;120(2):512-24.<br />
54. Sarobe P., et al. Abnormal priming <strong>of</strong> CD4+ T cells by dendritic<br />
cells expressing hepatitis C virus core and E1 proteins. J Virol<br />
2002;76(10):5062-70.<br />
55. Botarelli P., et al. T-Lymphocyte response to hepatitis C virus in<br />
different clinical courses <strong>of</strong> infection. Gastroenterology<br />
1993;104:580-7.<br />
56. Cerny A., Chisari F.V. Hepatitis C and Autoimmune Hepatitis.<br />
Hepatology 2000;31(3):811-2.<br />
57. Cacoub P., et al (Multivirc Group). Extrahepatic manifestations<br />
<strong>of</strong> chronic hepatitis C. Arthritis Rheum 1999;42:2204-12.<br />
58. Agnello V. Mixed cryoglobulinemia and hepatitis C virus. Hosp<br />
Pract 1995;30(3):35-42.<br />
59. Takaki A., et al. Cellular immune responses persist and humoral<br />
responses decrease two decades after recovery from a singlesource<br />
outbreak <strong>of</strong> hepatitis C. Nat Med 2000; 6(5):578-82.<br />
60. Lechner et al. Analysis <strong>of</strong> successful immune responses in persons<br />
infected with hepatitis C virus. J Exp Med 2000;191(9):1499-<br />
1512.<br />
61. Missale G., et al. Different clinical behaviors <strong>of</strong> acute hepatitis C<br />
virus infection associated with different vigor <strong>of</strong> the anti-viral<br />
cell-mediated immune response. J Clin Invest 1996;98:706-14.<br />
62. Gruner N.H., et al. Association <strong>of</strong> hepatitis C virus-specific CD8+<br />
T cells with viral clearance in acute hepatitis C. J Infect Dis<br />
2000;181(5):1528-36.<br />
63. Chisari F.V. Cytotoxic T cells and viral hepatitis. J Clin Invest<br />
1997;100(12):S19-S24.<br />
64. Thimme R., et al. Determinants <strong>of</strong> viral clearance and persistence<br />
during acute hepatitis C virus infection. J Exp Med<br />
2001;194(10):1395-406.<br />
65. Kanto T., Hayashi N. Immunopathogenesis <strong>of</strong> hepatitis C virus<br />
infection: multifaceted strategies subverting innate and adaptive<br />
immunity. Intern Med 2006;45(4):183-91.<br />
66. Wertheimer A.M., et al. Novel CD4+ and CD8+ T-cell determinants<br />
within the NS3 protein in subjects with spontaneously resolved<br />
HCV infection. Hepatology 2003;37(3):577-89.<br />
67. Carucci P., et al. Hepatitis C virus-specific T helper cell responses<br />
in recurrent hepatitis C after liver transplantation. J Hepatol<br />
1997;26(suppl):145.<br />
68. Gerlach J.T., et al. Recurrence <strong>of</strong> hepatitis C virus after loss <strong>of</strong><br />
virus-specific CD4+ T-cell response in acute hepatitis C.<br />
Gastroenterology 1999;117:933-41.<br />
69. Kerr J.F.R., et al. <strong>The</strong> nature <strong>of</strong> piecemeal necrosis in chronic<br />
active hepatitis. Lancet 1979;20:827-8.<br />
70. Marcellin P., et al. Fibrosis and disease progression in hepatitis C.<br />
Hepatology 2002;36:S47-56.<br />
www.bjid.com.br
BJID 2007; 11 Supplement 1 (October) Pathogenesis <strong>of</strong> Hepatitis C<br />
19<br />
71. Napoli J., et al. Progressive liver injury in chronic hepatitis<br />
C infection correlates with increased intrahepatic<br />
expression <strong>of</strong> Th1-associated cytokines. Hepatology<br />
1996;24:759-65.<br />
72. Tilg H., et al. How to modulate inflammatory cytokines in liver<br />
diseases. Liver Int 2006;26(9):1029-39.<br />
73. Ding W.X., Yin X.M. Dissection <strong>of</strong> the multiple mechanisms <strong>of</strong><br />
TNF-alpha-induced apoptosis in liver injury. J Cell Mol Med<br />
2004;8(4):445-54.<br />
74. Tilg H., et al. Serun levels <strong>of</strong> cytokines in chronic liver diseases.<br />
Gastroenterology 1992;103:264-74.<br />
75. Cacciarelli T.V., et al. Immunoregulatory cytokines in chronic<br />
hepatitis C virus infection: pre- and posttreatment with<br />
interferon alfa. Hepatology 1996;24:6-9.<br />
76. Malaguarnera M., et al. Serum interleukin 6 concentrations in<br />
chronic hepatitis C patients before and after interferon-alpha<br />
treatment. Int J Clin Pharmacol <strong>The</strong>r 1997;35(9):385-8.<br />
77. Oyanagi Y., et al. Enhanced expression <strong>of</strong> interleukin-6 in chronic<br />
hepatitis C. Liver 1999;19(6):464-72.<br />
78. Biró L., et al. Changes in the acute phase complement component<br />
and IL-6 levels inpatients with chronic hepatitis C receiving<br />
interferon alfa-2b. Immunol Lett 2000;72:69-74.<br />
79. Polyak S.J., et al. Elevated levels <strong>of</strong> interleukin-8 in serum are<br />
associated with hepatitis C virus infection and resistance to<br />
interferon therapy. J Virol 2001;75(13):6209-11.<br />
80. Lapinski T.W. <strong>The</strong> levels <strong>of</strong> IL-1 beta, IL-4 and IL-6 in the serum<br />
and the liver tissue <strong>of</strong> chronic HCV-infected patients. Arch<br />
Immunol <strong>The</strong>r Exp. (Warsz) 2001;49(4):311-6.<br />
81. Kasprzak et al. Expression <strong>of</strong> cytokines (TNF-α, IL-1 α, and IL-<br />
2) in chronic hepatitis C: comparative hybridocytochemical<br />
and immunocytochemical study in children and adult patients. J<br />
Histochemistry and Cytochemistry 2004;52(1):29-38.<br />
82. Kamal S.M., et al. Kinetics <strong>of</strong> Intrahepatic hepatitis C virus (HCV)-<br />
specific CD4+ T cell responser in HCV and Schistosoma mansoni<br />
coinfection: relation to progression <strong>of</strong> liver fibrosis. J Infect<br />
Dis 2004;189:1140-50.<br />
83. Shimoda K., et al. Interleukin-8 and hIRH (SDF1-alpha/PBSF)<br />
mRNA expression and histological activity index in patients<br />
with chronic hepatitis C. Hepatology 1998;28(1):108-15.<br />
84. Neuman M.G., et al. Kinetics <strong>of</strong> serum cytokines reflect changes<br />
in the severity <strong>of</strong> chronic hepatitis C presenting minimal fibrosis.<br />
J Viral Hepat 2002;9:134-40.<br />
85. Taylor A., et al. Mechanisms <strong>of</strong> immune suppression by interleukin-<br />
10 and transforming growth factor-beta: the role <strong>of</strong> T regulatory<br />
cells. Immunology 2006;117(4):433-42.<br />
86. Nelson D.R., et al. Long-term interleukin 10 therapy in chronic<br />
hepatitis C patients has a proviral and anti-inflammatory effect.<br />
Hepatology 2003;38(4):859-68.<br />
87. Nelson D.R., et al. Interleukin 10 treatment reduces fibrosis in<br />
patients with chronic hepatitis C: a pilot trial <strong>of</strong> inferferon<br />
nonresponders. Gastroenterology 2000;118:655-60.<br />
88. Roulot D., et al. Quantitative analysis <strong>of</strong> transforming<br />
growth factor beta 1 messenger RNAin the liver <strong>of</strong><br />
patients with chronic hepatitis C. Absence <strong>of</strong> correlation<br />
between high levels and severity <strong>of</strong> disease. Hepatology<br />
1995;21:298-304.<br />
89. Nelson D.R., et al. Transforming growth factor-beta 1 in chronic<br />
hepatitis C. J Viral Hepat 1997;4(1):29-35.<br />
90. Knolle P.A., Gerken G. Local control <strong>of</strong> the immune response in<br />
the liver. Immunol Rev 2000;174:21-34.<br />
91. Racanelli V., Rehermann B. <strong>The</strong> liver as an immunological organ.<br />
Hepatology 2006;43:S54-62.<br />
92. Yazdanbakhsh M., et al. Allergy, parasites, and the hygiene<br />
hypothesis. Science 2002;296(5567):490-4.<br />
93. Chitturi S., George J. Predictors <strong>of</strong> liver-related complications in<br />
patients with chronic hepatitis C. Ann Med 2000;32:588-91.<br />
94. Thursz M.R., et al. Host factors in chronic viral hepatitis. Semin<br />
Liver Dis 1997;17:345-50.<br />
95. Rehermann B., et al. Quantitative analysis <strong>of</strong> the peripheral blood<br />
cytotoxic T lymphocyte response in patients with chronic<br />
hepatitis C virus infection. J Clin Invest 1996;98:1432-40.<br />
96. Mangia A., et al. IL-10 haplotypes as possible predictors <strong>of</strong><br />
spontaneous clearance <strong>of</strong> HCV infection. Cytokine<br />
2004;25(3):103-9.<br />
97. Bozkaya H., et al. Circulating IL-2 and IL-10 in chronic active<br />
hepatitis C with respect to the response to IFN treatment.<br />
Infection 2000;28:309-13.<br />
98. Constantini P.K., et al. Interleukin-1, interleukin-10 and tumour<br />
necrosis factor-alpha gene polymorphisms in hepatitis C virus<br />
infection: an investigation <strong>of</strong> the relationships with spontaneous<br />
viral clearance and response to alpha-interferon therapy. Liver<br />
2002;22(5):404-12.<br />
99. Minton E.J., et al; Trent Hepatitis C Study Group. Clearance <strong>of</strong><br />
hepatitis C virus is not associated with single nucleotide<br />
polymorphisms in the IL-1, -6, or -10 genes. Hum Immunol<br />
2005;66(2):127-32.<br />
100.Reddy K.R., et al. Racial differences in responses to therapy with<br />
interferon in chronic hepatitis C. Consensus Interferon Study<br />
Group. Hepatology 1999;30:787-93.<br />
101.Lepe R., et al. Ethnic differences in the presentation <strong>of</strong> chronic<br />
hepatitis C. J Viral Hepat 2006;13(2):116-20.<br />
102.El-Serag H.B. Epidemiology <strong>of</strong> hepatocellular carcinoma. Clin<br />
Liver Dis 2001;5:87-107.<br />
103.Sugimoto K., et al. Influence <strong>of</strong> ethnicity in the outcome <strong>of</strong><br />
hepatitis C virus infection and cellular immune response.<br />
Hepatology 2003;37:590-9.<br />
104.Azocar J., et al. MHC class II genes in HCV viral clearance <strong>of</strong><br />
hepatitis C infected Hispanic patients. Hum Immunol<br />
2003;64(1):99-102.<br />
105.Pessione F., et al. Cigarette smoking and hepatic lesions in patients<br />
with chronic hepatitis C. Hepatology 2001;34:121-5.<br />
106.Campollo R O. Hepatitis C virus infection and alcohol. Rev<br />
Gastroenterol Mex 2002;67 Suppl 2:S80-3.<br />
107.Vento S., Cainelli F. Does hepatitis C virus cause severe liver<br />
disease only in people who drink alcohol? Lancet <strong>Infectious</strong> Dis<br />
2002;2(5):303-9.<br />
108.Monto A., et al. Risks <strong>of</strong> a range <strong>of</strong> alcohol intake on hepatitis c-<br />
related fibrosis. Hepatology 2004;39:826-34.<br />
109.El-Zayadi A.R. Heavy smoking and liver. World J Gastroenterol<br />
2006;12(38):6098-101.<br />
110.Kishihara Y., et al. Human T lymphotropic virus type I infection<br />
influences hepatitis C virus clearance. J Infect Dis<br />
2001;184:1114-9.<br />
111.Einav S., Koziel M.J. Immunopathogenesis <strong>of</strong> hepatitis C virus in the<br />
immunosuppressed host. Transpl Infect Dis 2002;4(2):85-92.<br />
112.Campollo R.O. Hepatitis C virus infection and alcohol. Rev<br />
Gastroenterol Mex 2002;67(Suppl 2):S80-3.<br />
113.Sanchez Avila J.F. Hepatitis C and addictions. Rev Gastroenterol<br />
Mex 2002;67(Suppl2):S84-7.<br />
114.Schiff E. <strong>The</strong> alcoholic patient with hepatitis C virus infection.<br />
Am J Med 1999;107(6B):95S-9.<br />
115.Bhattacharya R., Shuhart M.C. Hepatitis C and alcohol:<br />
interactions, outcomes, and implications. J Clin Gastroenterol<br />
2003;36(3):242-52.<br />
www.bjid.com.br
20 BJID 2007; 11 Supplement 1 (October)<br />
Antifibrotic <strong>The</strong>rapy in Chronic Hepatitis C<br />
Rinaldo Focaccia Siciliano and Antonio Alci Barone<br />
Laboratory <strong>of</strong> Hepatitis, LIM 47 DMIP-HC-FMUSP; São Paulo, SP, Brazil<br />
<strong>The</strong> most pronounced histological characteristics <strong>of</strong><br />
chronic hepatitis C are hepatocellular necrosis, inflammatory<br />
infiltrate and fibrosis. Unlike the first two, which present<br />
fluctuations, the evolution <strong>of</strong> liver fibrosis progressively<br />
evolves toward pathological sequelae due to the chronic liver<br />
injury induced by hepatitis C virus (HCV). Fibrosis results<br />
from the accumulation <strong>of</strong> extracellular matrix components,<br />
which leads to distortion <strong>of</strong> the liver architecture, alterations<br />
in hepatic microcirculation, and cellular dysfunction. This<br />
pathological hepatic process develops slowly and<br />
progressively, producing clinical repercussions only in its final<br />
stage, liver cirrhosis, which can take decades. <strong>The</strong>refore,<br />
determination <strong>of</strong> the degree <strong>of</strong> fibrosis through liver biopsy<br />
or progression rate is crucial to the understanding <strong>of</strong> the natural<br />
history <strong>of</strong> chronic hepatitis C.<br />
Some authors have identified host factors that are<br />
associated with the accelerated progression <strong>of</strong> liver fibrosis<br />
in HCV infection. <strong>The</strong> most important are being over 40 years<br />
<strong>of</strong> age at the time <strong>of</strong> HCV infection, being male, consuming<br />
excessive quantities <strong>of</strong> alcohol, and presenting conditions<br />
that lead to immunodeficiency, such as HIV infection or<br />
transplant. Other factors also seem to contribute to a more<br />
rapid progression toward fibrosis, such as liver steatosis, coinfection<br />
with hepatitis B virus (HBV), obesity, and diabetes<br />
mellitus.<br />
Recent advances in clinical studies and basic science have<br />
brought new perspectives to the development <strong>of</strong> therapies<br />
that can curb the progression <strong>of</strong> the fibrogenic process or<br />
even promote reversion <strong>of</strong> liver fibrosis. <strong>The</strong>se advances<br />
occurred after the recognition <strong>of</strong> fibrogenic cell types in the<br />
liver, as well as <strong>of</strong> the principal sites <strong>of</strong> fibrosis formation and<br />
its reversibility potential.<br />
Fibrosis seems to result from an imbalance between the<br />
synthesis and degradation <strong>of</strong> the extracellular matrix, resulting<br />
in the accumulation <strong>of</strong> conjunctive tissue in the liver. This<br />
process is triggered and sustained by the chronic liver damage<br />
caused by HCV and leads to the disruption <strong>of</strong> the normal liver<br />
architecture, culminating in the development <strong>of</strong> cirrhosis/<br />
hepatic insufficiency. Stellate cells are the principal source <strong>of</strong><br />
extracellular matrix in the damaged liver tissue. In a normal<br />
liver, they are present in the Disse space and are the principal<br />
reservoirs <strong>of</strong> vitamin A. Chronic hepatic injury secondary to<br />
HCV, through the increase <strong>of</strong> free radicals and fibrogenic<br />
mediators, leads to the activation <strong>of</strong> stellate cells, as well as to<br />
their proliferation and differentiation into my<strong>of</strong>ibroblasts, when<br />
they acquire contractile, pro-inflammatory and fibrogenic<br />
properties. Once activated, they migrate to the sites <strong>of</strong> injury<br />
<strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> 2007;11 (5) Suppl. 1:20-21.<br />
© 2007 by <strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> and Contexto<br />
Publishing. All rights reserved.<br />
with the objective <strong>of</strong> effecting repair by secreting a large<br />
quantity <strong>of</strong> extracellular matrix. Activated stellate cells also<br />
produce cytokines that perpetuate their activation status, as<br />
well as being stimulated by the apoptosis <strong>of</strong> damaged<br />
hepatocytes. <strong>The</strong> leukocytes attracted into the hepatic<br />
inflammatory process secondary to HCV infection also induce<br />
the production <strong>of</strong> collagen by stellate cells. <strong>The</strong>se activated<br />
cells, in turn, have a pro-inflammatory effect that feeds a<br />
vicious cycle.<br />
Under physiological conditions, the excess extracellular<br />
matrix is degraded through regulation by metalloproteinases.<br />
Activated hepatic my<strong>of</strong>ibroblasts, in addition to producing<br />
large quantities <strong>of</strong> Type I and Type III collagen, secrete tissue<br />
inhibitors <strong>of</strong> metalloproteinases, which block the<br />
collagenolytic activity. We have begun to comprehend various<br />
parts <strong>of</strong> this process <strong>of</strong> accumulation <strong>of</strong> extracellular matrix in<br />
the liver tissue, although there are still many gaps in our<br />
understanding. In addition to the efficient collagenolytic<br />
activity <strong>of</strong> the metalloproteinases, the degradation <strong>of</strong> the<br />
extracellular matrix in the liver can also occur through the<br />
activities <strong>of</strong> neutrophils, macrophages and stellate cells<br />
themselves; however, the importance and modulation <strong>of</strong> each<br />
have yet to be clarified. <strong>The</strong> activation <strong>of</strong> stellate cells, as well<br />
as their proliferation and fibrogenic activity, is regulated by<br />
various soluble growth factors, such as platelet-derived<br />
growth factor, transformation growth factor beta, and<br />
endothelin-1.<br />
Determining the mechanisms involved in the process <strong>of</strong><br />
liver fibrosis has led to a new perspective on the development<br />
<strong>of</strong> antifibrotic drugs in animal models. However, there is still<br />
an obstacle to be transposed before positive laboratory results<br />
can be reproduced in humans. New lines <strong>of</strong> research attempt<br />
to attenuate the activation <strong>of</strong> stellate cells, inhibit some <strong>of</strong><br />
their properties when activated, promote their apoptosis, or<br />
stimulate the degradation <strong>of</strong> the extracellular matrix. No specific<br />
antifibrotic therapies have been approved for use in humans;<br />
however, considerable effort has been made in laboratory<br />
studies in this promising area.<br />
In clinical practice, the treatment <strong>of</strong> hepatitis C with the<br />
combination <strong>of</strong> pegylated interferon alpha and ribavirin is the<br />
only pharmacological regimen currently available that can<br />
modify the natural evolution <strong>of</strong> liver fibrosis. This does not<br />
simply occur by suppressing the viremia (achieving a<br />
sustained virological response) but possibly by the antifibrotic<br />
role <strong>of</strong> pegylated interferon alpha. Recent clinical studies show<br />
remission <strong>of</strong> liver fibrosis or reduction <strong>of</strong> its progression rate<br />
in patients under treatment with therapeutic regimens<br />
containing interferon alpha or pegylated interferon. This effect<br />
is even more apparent among hepatitis C patients presenting<br />
a biochemical or virological response after therapy. Notably,<br />
www.bjid.com.br
BJID 2007; 11 Supplement 1 (October) Antifibrotics and Chronic Hepatitis C<br />
21<br />
most <strong>of</strong> these studies are retrospective, and their principal<br />
objective was the evaluation <strong>of</strong> the virologic response to the<br />
treatment with interferon alpha.<br />
Although liver fibrosis is a dynamic process, its remission<br />
is slow and demands prolonged therapy and follow-up<br />
evaluation. Multicentric prospective comparative studies that<br />
evaluate the histological impact <strong>of</strong> maintenance treatment with<br />
pegylated interferon in low doses versus placebo in patients<br />
with hepatitis C who are nonresponsive to treatment are<br />
currently being carried out. Preliminary results <strong>of</strong> these<br />
studies are quite promising; reduction <strong>of</strong> fibrosis or clinical<br />
complications resulting from liver cirrhosis can be seen after<br />
approximately two years <strong>of</strong> therapy with pegylated<br />
interferon. <strong>The</strong> final results, with histological analysis, after<br />
long-term follow-up treatment and inclusion <strong>of</strong> a large<br />
number <strong>of</strong> patients, will consolidate an evaluation <strong>of</strong> safety,<br />
clinical and histological benefits, and cost-effectiveness ratio<br />
<strong>of</strong> the prolonged use <strong>of</strong> pegylated interferon in low doses in<br />
hepatitis C.<br />
<strong>The</strong> role <strong>of</strong> the physician in the positive modification <strong>of</strong><br />
the natural history <strong>of</strong> hepatitis C-related liver fibrosis should<br />
not be restricted to the removal <strong>of</strong> HCV as a hepatic aggressive/<br />
pro-inflammatory factor (achieving a sustained virologic<br />
response) or to the use <strong>of</strong> interferon as a potential antifibrotic<br />
agent. In daily practice, other strategies aimed at attenuating<br />
the progression <strong>of</strong> liver fibrosis are based on the effects on<br />
modifiable factors that can alter the natural history <strong>of</strong> HCV:<br />
drinking cessation; prevention and control <strong>of</strong> obesity; and<br />
prevention <strong>of</strong> HIV or HBV co-infection.<br />
Much progress has been achieved in basic science<br />
regarding the understanding <strong>of</strong> the biological mechanisms<br />
that lead to the development <strong>of</strong> liver fibrosis. However, clinical<br />
trials to validate new drugs or antifibrotic strategies are<br />
warranted.<br />
References<br />
1. Albanis E, Friedman S,L. Antifibrotic agents for liver disease. Am<br />
J Transplant 2006;6(1):12-9.<br />
2. Friedman S.L., Rockey D.C., Bissell D.M. Hepatic fibrosis 2006:<br />
report <strong>of</strong> the Third AASLD Single Topic Conference.<br />
Hepatology 2007;45(1):242-9.<br />
3. Bataller R., Brenner D.A. Liver fibrosis. J Clin Invest<br />
2005;115(2):209-18.<br />
4. Marcellin P., Asselah T., Boyer N. Fibrosis and disease progression<br />
in hepatitis C. Hepatology 2002;36(5 Suppl 1):S47-56.<br />
5. Friedman S.L., Bansal M.B. Reversal <strong>of</strong> hepatic fibrosis - fact or<br />
fantasy? Hepatology 2006;43(2 Suppl 1):S82-8.<br />
6. Everson G.T., Hoefs J.C., Seeff L.B., et al. Impact <strong>of</strong> disease severity<br />
on outcome <strong>of</strong> antiviral therapy for chronic hepatitis C: Lessons<br />
from the HALT-C trial. Hepatology 2006;44(6):1675-84.<br />
7. Kaiser P., Hass H., Lutze B., et al. Long-term low dose treatment<br />
with pegylated interferon alpha 2b leads to a significant reduction<br />
in fibrosis and inflammatory score in chronic hepatitis C<br />
nonresponder patients with fibrosis or cirrhosis. 57th Annual<br />
Meeting <strong>of</strong> the American Association for the Study <strong>of</strong> Liver<br />
<strong>Diseases</strong>. Massachusetts – USA 2006.<br />
8. Afdhal N., Freilich B., Levine R., et al. Colchicine versus peginterferon<br />
long-term (COPILOT) trial: interim analysis <strong>of</strong> clinical<br />
outcomes at year 2. Hepatology 2004;40:238A.<br />
www.bjid.com.br
22 BJID 2007; 11 Supplement 1 (October)<br />
Laboratory Testing for Hepatitis C<br />
Neiva Sellan Lopes Gonçales and Fernando Lopes Gonçales Junior<br />
Hepatitis Study Group – MI/FCM/UNICAMP; Campinas, SP, Brazil<br />
Serological Detection <strong>of</strong> Hepatitis C Virus<br />
Serological diagnosis <strong>of</strong> patients infected with the hepatitis<br />
C virus (HCV) can be performed using two categories <strong>of</strong> tests:<br />
indirect tests, which detect antibodies against HCV; and direct<br />
tests, which detect, quantify, or characterize components <strong>of</strong><br />
the viral particle, such as HCV RNA testing and testing for<br />
detection <strong>of</strong> the HCV core antigen.<br />
Anti-HCV antibodies are usually detected using third- and<br />
fourth-generation immunoenzymatic assays – enzyme<br />
immunoassay (EIA)/enzyme-linked immunosorbent assay<br />
(ELISA) 3 and EIA/ELISA 4, respectively – which contain<br />
HCV core antigens and HCV nonstructural genes. <strong>The</strong><br />
specificity <strong>of</strong> the EIA tests available on the market that detect<br />
anti-HCV was determined to be higher than 99%, whereas<br />
their sensitivity, which was more difficult to determine due to<br />
the lack <strong>of</strong> gold standard tests with high sensitivity, was 95-<br />
99% [1]. However, false-positive results for anti-HCV can<br />
occasionally occur, especially in populations with prevalence<br />
rates below 10% [2-4].<br />
<strong>The</strong>re are many reasons why laboratories do not routinely<br />
use a supplementary test based on immunoblot analysis, such<br />
as the recombinant immunoblot assay, to complement the<br />
diagnosis <strong>of</strong> HCV infection. In addition to the high cost <strong>of</strong><br />
such a test, the lack <strong>of</strong> laboratory standards that can evaluate<br />
its performance and interpretation, in conjunction with its<br />
actual accuracy, is among the principal reasons. Furthermore,<br />
this type <strong>of</strong> test does not distinguish past from present<br />
infection, and its use is only indicated for confirmation <strong>of</strong> EIA<br />
results.<br />
In contrast, the use <strong>of</strong> nucleic acid testing (NAT) makes it<br />
possible to differentiate between viremic and nonviremic<br />
individuals by detection <strong>of</strong> HCV RNA, allowing the clinician a<br />
differentiated approach to anti-HCV-positive individuals.<br />
However, there can be situations in which HCV RNA is not<br />
detected (negative HCV RNA) and the individual has active<br />
infection with HCV. This can occur in individuals in whom<br />
anti-HCV antibody titers are high and RNA titers are low [5].<br />
<strong>The</strong>refore, HCV RNA might not be detectable in certain<br />
individuals in the acute phase <strong>of</strong> the disease. However, these<br />
findings are transient, and chronic infection can develop [6].<br />
In addition, HCV RNA intermittent positivity has been<br />
observed in individuals chronically infected with HCV [6-8].<br />
Negativity <strong>of</strong> HCV RNA results can indicate resolved infection.<br />
In 15 to 25% <strong>of</strong> those anti-HCV positive individuals who<br />
acquired the infection after 45 years <strong>of</strong> age, the infection<br />
resolves spontaneously. This percentage increases to 40-45%<br />
in those who acquired the HCV infection in childhood or<br />
young adulthood [9].<br />
Different tests based on polymerase chain reaction (PCR)<br />
have been developed to directly detect the viral particle. One<br />
characteristic <strong>of</strong> real-time PCR is amplification coupled with<br />
<strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> 2007;11 (5) Suppl. 1:22-24.<br />
© 2007 by <strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> and Contexto<br />
Publishing. All rights reserved.<br />
detection, which allows the evaluation <strong>of</strong> the number <strong>of</strong> viral<br />
genomes at the onset <strong>of</strong> and throughout the reaction.<br />
Qualitative detection <strong>of</strong> HCV RNA by reverse transcriptase<br />
(RT)-PCR is generally accepted as the most sensitive and<br />
standardized test to date [10,11]. Nevertheless, there is variability<br />
among the results from different laboratories, as evidenced by<br />
the use <strong>of</strong> international panels <strong>of</strong> pr<strong>of</strong>iciency. <strong>The</strong> accuracy<br />
and reliability <strong>of</strong> the results are directly related to the laboratory<br />
procedures adopted in the performance <strong>of</strong> the tests [12]. <strong>The</strong><br />
lack <strong>of</strong> preliminary care in sample collection, in conjunction<br />
with the time involved in preparing and separating the samples,<br />
can result in incorrect results. It is extremely important that all<br />
laboratory procedures comply with Good Laboratory Practice<br />
and strictly follow the protocols standardized by the<br />
manufacturers <strong>of</strong> the diagnostic kits and reagents.<br />
<strong>The</strong> gold standard consists <strong>of</strong> the careful use <strong>of</strong> NAT,<br />
standardized for detection <strong>of</strong> HCV RNA, together with EIAs<br />
(specificity in conjunction with sensitivity).<br />
An alternative to aid diagnosis is the use <strong>of</strong> the ratio<br />
between optical density and cut-<strong>of</strong>f value (OD/COV) or the<br />
sample/cut-<strong>of</strong>f ratio as an indicator <strong>of</strong> the true positivity <strong>of</strong><br />
the test. Studies carried out in Brazil show that, in EIAs,<br />
reagents with OD/COV greater than 3 are repeatedly associated<br />
with 100% true-positive results (positive predictive value) and<br />
present approximately 92% positivity for HCV RNA by RT-<br />
PCR [13]. In terms <strong>of</strong> the population studied, the positive<br />
predictive value is increased when accompanied by risk<br />
factors, high levels <strong>of</strong> alanine aminotransferase (ALT), or liver<br />
disease.<br />
In immunocompetent patients, EIAs present excellent<br />
reproducibility; however, in hemodialyzed or<br />
immunocompromised patients, EIA sensitivity is significantly<br />
reduced [14].<br />
In low-risk populations, such as blood donors, or in<br />
random population screening, i.e., in populations that do not<br />
present risk factors for the acquisition <strong>of</strong> HCV infection,<br />
negative EIA results are sufficient to rule out the presence <strong>of</strong><br />
HCV. However, false-positive results can occur in these<br />
populations. In such cases, a qualitative study <strong>of</strong> HCV RNA<br />
should be performed to confirm the diagnosis.<br />
In high-risk populations, when there is clinical suspicion <strong>of</strong><br />
HCV infection, positive EIA results confirm the exposure to<br />
HCV. A qualitative study <strong>of</strong> HCV RNA should be performed to<br />
distinguish individuals with chronic infection from those who<br />
have eliminated the HCV spontaneously.<br />
In patients with chronic hepatitis <strong>of</strong> unknown cause and<br />
negative anti-HCV EIA results, especially in<br />
immunocompromised patients [14], a qualitative study <strong>of</strong> HCV<br />
RNA should be performed. <strong>The</strong> presence <strong>of</strong> HCV RNA confirms<br />
the diagnosis, although a negative result does not rule out<br />
HCV infection. In such cases, it is recommended that a new<br />
HCV RNA study be performed six months after the first study.<br />
Detection <strong>of</strong> the HCV core antigen by EIA can be an alternative<br />
for early diagnosis <strong>of</strong> HCV infection.<br />
www.bjid.com.br
BJID 2007; 11 Supplement 1 (October) Laboratory Testing for Hepatitis C<br />
23<br />
<strong>The</strong> HCV core antigen ELISA was developed to be used<br />
as a serological screening test to detect the HCV core antigen,<br />
especially during the immunological window period, when<br />
antibodies are not detected. This assay was found to have<br />
sensitivity close to that <strong>of</strong> NAT, with a mean difference in<br />
detection <strong>of</strong> one to two days [15].<br />
Based on this assay, a new assay was developed to detect<br />
and quantify HCV core antigen. <strong>The</strong> modifications made to<br />
this new assay, such as the dissociation <strong>of</strong> immune complexes,<br />
which allows the detection <strong>of</strong> free antigens and core antigen<br />
antibodies, and the change in the signal amplification, through<br />
the modification <strong>of</strong> the conjugate, have increased the<br />
sensitivity <strong>of</strong> the test. Studies have demonstrated that this<br />
test can reduce the immunological window by 3.3 days in<br />
comparison with the previous test (i.e., the HCV core antigen<br />
ELISA). This increase in sensitivity has led to a significant<br />
(58-day) decrease in the size <strong>of</strong> the immunological window.<br />
<strong>The</strong> difference between this EIA and PCR was only 0.24<br />
days [16].<br />
This test can be considered a viable alternative to<br />
detecting viremia directly when NAT cannot be used for<br />
reasons <strong>of</strong> cost, organization, emergency, or logistic difficulties.<br />
Tests that allow simultaneous or combined detection <strong>of</strong> HCV<br />
core antigen and antibody in a single assay are currently<br />
available on the market. <strong>The</strong>se tests, known as HCV Ag/Ab<br />
combo assays, have high sensitivity and specificity, reducing<br />
the duration <strong>of</strong> the immunological window (during which<br />
antibodies are not detected) by up to 12 days [17]. Studies<br />
carried out using this assay showed sensitivity close to that<br />
<strong>of</strong> NAT, with a mean difference in detection <strong>of</strong> 1 to 2 days [18].<br />
<strong>The</strong> use <strong>of</strong> NAT in the diagnosis <strong>of</strong> HCV infection makes it<br />
possible to distinguish viremic from nonviremic individuals<br />
through the detection <strong>of</strong> HCV RNA.<br />
<strong>The</strong>refore, these tests can be considered a plausible future<br />
solution in the screening <strong>of</strong> blood donors, organ<br />
transplantation programs, and cases <strong>of</strong> occupational exposure,<br />
in which a rapid and low-cost diagnosis is necessary.<br />
In order to standardize the tests, the World Health<br />
Organization and the United States National Institute for<br />
Biological Standards and Controls have established a standard<br />
measure known as the international unit (IU). Assays for<br />
qualitative detection <strong>of</strong> HCV RNA are important tools because<br />
they are significantly more sensitive than are most quantitative<br />
tests. Qualitative assays are based on the principle <strong>of</strong> target<br />
amplification using either PCR or transcription-mediated<br />
amplification. <strong>The</strong> cut-<strong>of</strong>f value <strong>of</strong> the lower limit <strong>of</strong> detection<br />
<strong>of</strong> HCV RNA <strong>of</strong> these commercial assays is 50 IU/mL and 6 IU/<br />
mL, respectively [19]. <strong>The</strong> specificity <strong>of</strong> these essays exceeds<br />
99%. A positive test for HCV RNA confirms active replication<br />
<strong>of</strong> HCV. Clinical and laboratory follow-up with study <strong>of</strong> HCV<br />
RNS should be performed to confirm the absence <strong>of</strong> active<br />
replication <strong>of</strong> HCV. Once HCV infection is confirmed,<br />
performing further qualitative tests for HCV RNA in patients<br />
submitted to clinical follow-up evaluation but not receiving<br />
treatment has no diagnostic utility.<br />
<strong>The</strong> quantification <strong>of</strong> HCV RNA can be performed by<br />
target amplification using PCR or by signal amplification using<br />
branched DNA (bDNA). In these commercial assays, the cut<strong>of</strong>f<br />
value <strong>of</strong> the lower limit <strong>of</strong> quantification <strong>of</strong> HCV RNA<br />
ranges from 600 to 615 IU/mL, and the upper linear limit ranges<br />
from 850,000 to 7,700,000 IU/mL [20]. <strong>The</strong> standardization in<br />
IU does not represent the actual number <strong>of</strong> viral particles in<br />
the preparation. <strong>The</strong>re are significant variations among<br />
commercial assays. <strong>The</strong> dynamics <strong>of</strong> each assay should be<br />
observed, and appropriate dilutions <strong>of</strong> the material being<br />
analyzed should be performed to ensure the accuracy <strong>of</strong> the<br />
quantification.<br />
<strong>The</strong> ideal assay for HCV RNA should have a lower<br />
detection limit <strong>of</strong> 5 to 50 IU/mL and a linearity curve <strong>of</strong> 6 to 7<br />
log 10<br />
. Traditional assays for detection <strong>of</strong> viral load, such as<br />
bDNA and Roche Monitor, present detection limits <strong>of</strong> 615 IU/<br />
mL and 600 IU/mL respectively [21,22], which are inadequate<br />
to define end-<strong>of</strong>-treatment response or sustained virological<br />
response. Real-time PCR assays are a promising tool due to<br />
their sensitivity and broad range <strong>of</strong> linearity. Cobas Taqman<br />
48 HCV assay is a quantitative assay that has a detection limit<br />
<strong>of</strong> 10 to 100 IU/mL, which makes it well suited for use in followup<br />
treatment (at the initiation and at week 12) [23].<br />
Acute Infection and Cutting/Piercing Accidents<br />
After exposure to HCV, anti-HCV antibodies can be<br />
detected by EIA in 50 to 70% <strong>of</strong> the patients at the onset <strong>of</strong><br />
symptoms, this percentage increasing to approximately 90%<br />
after 3 months. Routinely, HCV RNA can be detected between<br />
post-exposure weeks 1 and 3, remaining at detectable levels<br />
when symptom onset occurs. From post-infection week 2 to<br />
post-infection week 8, levels <strong>of</strong> ALT rise, and this increase is<br />
accompanied by the appearance <strong>of</strong> hepatocytic lesions.<br />
Vertical Transmission<br />
An important question is that <strong>of</strong> exactly how mother-tochild<br />
transmission <strong>of</strong> the HCV infection is defined. In many<br />
children born to mothers with chronic hepatitis C, anti-HCV<br />
(IgG) is detectable in the blood. <strong>The</strong>se antibodies are acquired<br />
through passive transplacental transfer. <strong>The</strong>se passively<br />
acquired antibodies will remain detectable for the first 12 to 15<br />
months <strong>of</strong> life. <strong>The</strong>refore, the criterion to identify mother-tochild<br />
transmission <strong>of</strong> HCV infection is the detection <strong>of</strong> anti-<br />
HCV and HCV RNA in the blood <strong>of</strong> the child after the age <strong>of</strong> 18<br />
months.<br />
Chronic Infection<br />
In patients with chronic hepatitis C, the diagnosis <strong>of</strong><br />
chronicity is based on the detection <strong>of</strong> anti-HCV and HCV<br />
RNA in the blood, using techniques <strong>of</strong> high sensitivity, and is<br />
confirmed through liver biopsy.<br />
Loss <strong>of</strong> anti-HCV and isolated presence <strong>of</strong> HCV RNA are<br />
uncommon in immunocompetent patients with chronic<br />
hepatitis C. However, these findings can occur in<br />
hemodialyzed patients and in severely immunocompromised<br />
patients<br />
Follow-Up Treatment<br />
Some patients with detectable HCV RNA should be<br />
considered for treatment. Genotyping should be performed<br />
at the initiation <strong>of</strong> treatment in order to define treatment<br />
duration, since, according to treatment protocols, patients<br />
infected with genotype 2 or 3 should be treated for 24<br />
www.bjid.com.br
24 Laboratory Testing for Hepatitis C<br />
BJID 2007; 11 Supplement 1 (October)<br />
weeks, whereas those infected with genotype 1 should be<br />
treated for 48 weeks [24].<br />
A considerable limitation in the evaluation <strong>of</strong> patients<br />
with chronic infection with HCV has been the lack <strong>of</strong><br />
standardization <strong>of</strong> the tests for detection <strong>of</strong> HCV RNA. A<br />
significant difference has been observed in the assays used,<br />
both in terms <strong>of</strong> sensitivity (upper limit <strong>of</strong> detection) and in<br />
terms <strong>of</strong> dynamics. <strong>The</strong>se differences are observed not only<br />
among the different assays but also among different<br />
laboratories performing a given assay. <strong>The</strong>refore, it is<br />
important that, throughout the clinical follow-up <strong>of</strong> a patient<br />
receiving specific treatment, the same assays and, if<br />
possible, the same laboratory always be used [25-28].<br />
Quantification <strong>of</strong> HCV RNA should be performed in<br />
the pretreatment sample and in the week-12 sample in<br />
order to evaluate the predictive value <strong>of</strong> the treatment<br />
response.<br />
Since the qualitative study <strong>of</strong> HCV RNA presents a<br />
lower limit <strong>of</strong> detection <strong>of</strong> 50 IU/mL, it should be used at<br />
week 4 <strong>of</strong> treatment, as a predictor <strong>of</strong> sustained virologic<br />
response (SVR), then again, to detect the SVR, at the<br />
end <strong>of</strong> treatment and at 6 months after the end <strong>of</strong><br />
treatment. <strong>The</strong>refore, presenting negative PCR results<br />
by week 4 <strong>of</strong> treatment has a high predictive value for<br />
achieving an SVR.<br />
References<br />
1. Alter M.J., Kuhnert W.L., Finelli L. Guidelines for Laboratory<br />
Testing and Result Reporting <strong>of</strong> antibody to hepatitis C Virus.<br />
MMWR 2003;52:1-15.<br />
2. Kleinman S., Alter H., Bush M., et al. Increased detection <strong>of</strong> hepatitis<br />
C virus (HCV) – infected blood donors by a multiple-antigen HCV<br />
enzyme immunoassay. Transfusion 1992;32:805-613.<br />
3. Conry-Cantilena C., VanRaden M., Gibble J., et al. Route <strong>of</strong> infection,<br />
viremia, and liver disease in blood donors found to have hepatitis<br />
C virus infection. N Engl J Med 1996;334:1691-6.<br />
4. Hyams K.C., Riddle J., Rubertone M., et al. Prevalence and<br />
incidence <strong>of</strong> hepatitis C virus infection in the US military: a<br />
seroepidemiologic survey <strong>of</strong> 21000 troops. Am J Epidemiol<br />
2001;153:764-70.<br />
5. Busch M.P., Kleinmam S.H., Jackson B., et al. Nucleic acid testing<br />
<strong>of</strong> blood donors for transfusion-transmitted infectious diseases:<br />
report <strong>of</strong> Interorganization Task Force on Nucleic Acid<br />
Amplification <strong>of</strong> Blood Donors. Transfusion 2000;40:143-59.<br />
6. Thomas D.L., Astemborski J., Rai R.M., et al. Natural history <strong>of</strong><br />
hepatitis C virus infection: host, viral, and environmental<br />
factors. JAMA 2000;284:450-6.<br />
7. Alter M.J., Margolis H.S., Krawczynski K., et al. Natural history<br />
<strong>of</strong> community-acquired hepatitis C in the United States. N Engl<br />
J Med 1992;327:1899-905.<br />
8. Larghi A., Zuin M., Crosignani A., et al. Outcome <strong>of</strong> an out break<br />
<strong>of</strong> acute hepatitis C among healthy volunteers participating in<br />
pharmacokinetics studies. Hepatology 2002;36:993-1000.<br />
9. Alter H.J., Seef L.B. Recovery, persistence, and sequelae in hepatitis<br />
C virus infection: a perspective on long term outcome. Semin<br />
Liver Dis 2000;20:17-35.<br />
10. Pawlotsky J.M. Molecular diagnosis <strong>of</strong> viral hepatitis.<br />
Gastroenterology 2002;122:1554-68.<br />
11. Pawlotsky J.M. Use and interpretation <strong>of</strong> virological tests for<br />
hepatitis C. Hepatology 2002;36:S65-S73.<br />
12. Callendo A.M., Valsamakis A., Zhou Y., et al. Multilaboratory<br />
comparison <strong>of</strong> hepatitis C virus viral load assays. J Clin Microbiol<br />
2006;44:1726-32.<br />
13. Gonçales N.S.L., Costa F.F., Vassalo J., Gonçales Jr., F.L. Diagnosis<br />
<strong>of</strong> hepatitis C in <strong>Brazilian</strong> blood donors using a reverse<br />
transcriptase nested polymerase chain reaction: comparison<br />
with enzyme immunoassay and recombinant protein immunoblot<br />
assay. Rev Inst Med trop S Paulo 2000;42(5):263-7.<br />
14. Lakshmi V., Reddy A.K., Dakshinamurty K.V. Evaluation <strong>of</strong><br />
commercially available third-generation anti-hepatitis C virus<br />
enzyme-linked immunosorbent assay in patients on<br />
haemodialysis. Indian J Med Microbiol 2007;25:140-2.<br />
15. Tanaka E.C., Ohue K., Aoyagi K., et al. Evaluation <strong>of</strong> a new<br />
enzyme immunoassay for hepatitis C virus (HCV) core antigen<br />
with clinical sensitivity approximating that <strong>of</strong> genomic<br />
amplification <strong>of</strong> HCV RNA. Hepatology 2000;32:388-93.<br />
16. Laperche S., Le Marrec N., Simon N., et al. A new HCV core<br />
antigen assay based on disassociation <strong>of</strong> immune complexes: an<br />
alternative to molecular biology in the diagnosis <strong>of</strong> early HCV<br />
infection. Transfusion 2003;43:958-62.<br />
17. Laperche S., Elghouzzi M.-H., More P., et al. Is an assay for<br />
simultaneous detection <strong>of</strong> hepatitis C virus core antigen and<br />
antibody a valuable alternative to nucleic acid testing?<br />
Transfusion 2005;45:1965-72.<br />
18. Laperche S., Le Marrec N., Girault A., et al.. Simultaneous detection<br />
<strong>of</strong> hepatitis C virus (HCV) core antigen and anti-HCV antibodies<br />
improves the early detection <strong>of</strong> HCV infection. J Clin Microbiol<br />
2005;43:3877-83.<br />
19. Desombere I., Van Vlierberghe H., Couvert S., et al. Comparison<br />
<strong>of</strong> qualitative (COBAS AMPLICOR HCV 2.0 versus VERSANT<br />
HCV RNA) and quantitative (COBAS AMPLICOR HCV monitor<br />
2.0 versus VERSANT HCV RNA 3.0) assays for hepatitis C<br />
virus (HCV) RNA detection and quantification: impact on<br />
diagnosis and treatment <strong>of</strong> HCV infections. J Clin Microbiol<br />
2005;43(6):2590-2.<br />
20. Elbeik T, Surtihadi J, Destree M et al. Multicenter evaluation <strong>of</strong><br />
performance characteristics <strong>of</strong> the Bayer VERSANT HCV RNA<br />
3.0 assay (bDNA). J Clin Microbiol 2004;42:563-9.<br />
21. Veillon P., Payan C., Picchio G., et al. Comparative<br />
evaluation <strong>of</strong> the total hepatitis C virus core antigen,<br />
branched-DNA, and Amplicor Monitor assays in<br />
determining viremia for patients with chronic hepatitis C<br />
during interferon plus ribarin combination therapy. J Clin<br />
Microbiol 2003;41:3212-20.<br />
22. Nolte F.S., Fried M.W., Shiffman M.L., et al. Prospective<br />
multicenter clinical evaluation <strong>of</strong> AMPLICOR and COBAS<br />
AMPLICOR hepatitis C virus tests. J Clin Microbiol<br />
2001;39:4005-12.<br />
23. Konnick E.Q., Willians S., Ashwood E.R., et al. Evaluation <strong>of</strong><br />
Cobas hepatitis C virus (HCV) Taqman anlyte –specific reagent<br />
assay nd comparison to the Cobas Amplicor HCV monitor v2.0<br />
and Versant HCV bDNA 3.0 assays. J Clin Microbiol<br />
2005;43:2133-40.<br />
24. Fried M.W., Shiffman M.L., Reddy C., et al. Peginterferon alfa-2a<br />
plus ribavirin for chronic hepatitis C virus infection. N Engl J<br />
Med 2002;347:975-92.<br />
25. Shiffman M.L., Ferreira-Gonzalez A., Reddy K.R., et al.<br />
Comparison <strong>of</strong> three commercially available assays for HCV<br />
RNA using the International Units standard: Implications for<br />
management <strong>of</strong> patients with chronic hepatitis C virus infection<br />
in clinical practice. Am J Gastroenterol 2003;98:1159-66.<br />
26. Podzorski R.P. Molecular testing in the diagnosis and management<br />
<strong>of</strong> hepatitis C virus infection. Arch Pathol Lab Med<br />
2002;126:285-90.<br />
27. Schirm J., van Loon A.M., Valentine-Thon E., et al. External<br />
quality assessment program for qualitative and quantitative<br />
detection <strong>of</strong> hepatitis C virus in diagnostic virology. J Clin<br />
Microbiol 2002;40:2973-80.<br />
28. Pawlotsky J.M. Diagnostic testing in hepatitis C virus infection:<br />
viral kinetics and genomics. Semin Liver Dis 2003;23:3-11.<br />
www.bjid.com.br
BJID 2007; 11 Supplement 1 (October) 25<br />
Hepatitis C: Genotyping<br />
Norma de Paula Cavalheiro<br />
Laboratory <strong>of</strong> Hepatitis, LIM 47 DMIP-HC-FMUSP; São Paulo, SP, Brazil<br />
<strong>The</strong> heterogeneity <strong>of</strong> the hepatitis C virus (HCV) genome<br />
was described at the beginning <strong>of</strong> the 1990s. Subsequently,<br />
genotyping tests were developed in order to delineate and<br />
differentiate these variants, leading to various classifications<br />
in different parts <strong>of</strong> the world. However, in 1994, in a consensus<br />
publication, criteria were established and a universal<br />
classification was consolidated, comprising the identification<br />
<strong>of</strong> 6 large groups or viral genotypes, in addition to over 70<br />
different subtypes distributed worldwide. It was established<br />
that genotypes differ from one another in 31% to 33%, as do<br />
the subtypes in 20% to 25%.<br />
<strong>The</strong> standardization in HCV classification was in<br />
accordance with the uniformity <strong>of</strong> data published in scientific<br />
and epidemiological studies on evolution and pathogenesis.<br />
Due to genomic peculiarities <strong>of</strong> different populations in the<br />
world, databases for centralization and collection <strong>of</strong><br />
information on HCV circulating genomes were created, by<br />
region: the first in Japan by Pr<strong>of</strong>. Masashi Mizokami et al.<br />
(http://s2as02.genes.nig.ac.jp/); the second in the European<br />
Union by Pr<strong>of</strong>. Gilbert Deleage et al. (http://euhcvdb.fr/); and<br />
the third in the United States by Dr. Carla Kuiken et al. (http:/<br />
/hcv.lanl.gov/ or http://hcv-db.org). <strong>The</strong> accessibility <strong>of</strong> these<br />
databases, which are consulted and updated by researchers<br />
worldwide, helps standardize terms for HCV viral genotypes<br />
and subtypes [1].<br />
Prior to 1994, new variants were identified in Vietnam,<br />
Thailand, Burma and Indonesia. <strong>The</strong>se viral genotypes were<br />
originally classified as genotypes 7, 8, 9, 10 and 11. <strong>The</strong>se<br />
variants were reclassified in 2005; genotype 10a came to be<br />
denominated subtype 3k, and genotypes 7a, 7d, 7b, 7e/7c,<br />
11a, 9a, 9b, 9c, 8b and 8a became subtypes 6e, 6c, 6d, 6f, 6g,<br />
6h, 6i, 6j, 6k and 6l, respectively [1].<br />
In Brazil, HCV genotype 1 is predominant, being identified<br />
in 70% <strong>of</strong> the infected population, followed by genotypes 3<br />
(in 25%) and 2 (in approximately 5%). In the southern region,<br />
the pr<strong>of</strong>ile is differentiated, the prevalence <strong>of</strong> genotype 3 being<br />
comparable to that <strong>of</strong> genotype 1 [2,3].<br />
<strong>The</strong> HCV viral genotype can be determined in a clinical<br />
sample in different forms, and the regions <strong>of</strong> HCV genome<br />
considered appropriate include the core, E1, NS4 and NS5<br />
regions, as well as the 5’UTR, as mentioned in innumerable<br />
studies [4,5].<br />
<strong>The</strong> most direct method, considered the gold standard, is<br />
the sequencing <strong>of</strong> the HCV genome in a certain region,<br />
sufficiently divergent for different genotypes and subtypes<br />
to be distinguished [5].<br />
<strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> 2007;11 (5) Suppl. 1:25-27.<br />
© 2007 by <strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> and Contexto<br />
Publishing. All rights reserved.<br />
In practice, there are two categories <strong>of</strong> assays for the<br />
diagnosis <strong>of</strong> HCV viral types: serotyping and genotyping [6,7].<br />
<strong>The</strong> enzyme-linked immunosorbent assay, also known as<br />
the indirect method (serotyping), commercialized only for<br />
research, discriminates among the six HCV genotypes, and<br />
not the subtypes. It presents genotype-specific antibodies<br />
for different HCV genotypes (Serotype HCV 5’NC – Abbott-<br />
Murex) in the NS4 region <strong>of</strong> the genome. This test omits the<br />
determination <strong>of</strong> the quantity <strong>of</strong> circulating viral particles and<br />
presents lower sensitivity and specificity in the diagnosis <strong>of</strong><br />
HCV genotypes, when compared with genotyping. Its<br />
performance is also limited in the evaluation <strong>of</strong><br />
immunocompromised patients [3,7,8].<br />
Genotyping (the direct method) analyzes the sequences<br />
<strong>of</strong> various regions <strong>of</strong> the genome in the differentiation <strong>of</strong> HCV<br />
genotypes and subtypes. <strong>The</strong>refore, it depends on samples<br />
that present viral particles for analysis. <strong>The</strong>se techniques are:<br />
sequencing, hybridization with genotype-specific probes, and<br />
real-time polymerase chain reaction (PCR) [5,7,9].<br />
Reverse hybridization, distributed under the commercial<br />
name Line Probe Assay (LIPA - Versant HCV Genotype assay<br />
1.0/2.0; Innogenetics, Ghent, Belgium; distributed by Siemens<br />
Medical Solutions Diagnostics, Tarrytown, NY, USA), as<br />
described by Lieven Stuyver et al. in 1993, uses nitrocellulose<br />
tapes, on which oligonucleotide probes <strong>of</strong> region 5’NC,<br />
complementary to each specific HCV genotype/subtype, are<br />
immobilized. <strong>The</strong>se tapes are hybridized under high stringency<br />
conditions, and the PCR product is marked with biotinylated<br />
primers in the amplification process. After hybridization, an<br />
avidin conjugate will bind to the biotinylated hybrid. <strong>The</strong><br />
substrate will yield the formation <strong>of</strong> a colored product, which<br />
will be deposited on the tape and reveal the viral genotype<br />
present in the sample. Genotypes 1 through 6, as well as<br />
subtypes 1a, 1b, 1a/1b, 2a/2c, 2b, 3a-c, 4a-h, 5a, 6a and 10a, are<br />
discriminated. <strong>The</strong> results are evaluated through visual<br />
assessment.<br />
A new version <strong>of</strong> LIPA (version 2.0) adds probes <strong>of</strong> the<br />
core region <strong>of</strong> HCV and enables distinction <strong>of</strong> subtypes 1c <strong>of</strong><br />
6 and subtypes 1a and 1b, which, in the former version, was<br />
not possible for all the samples analyzed, since region 5’NC is<br />
extremely conserved and may not present sufficient diversity<br />
for the distinction <strong>of</strong> these subtypes. <strong>The</strong> interpretation <strong>of</strong><br />
results is also performed by assessing the nitrocellulose tapes<br />
with a scanner, and the images are analyzed using a computer<br />
program. <strong>The</strong> new version is in the registration phase for<br />
distribution in Brazil [7,10,11].<br />
Direct sequencing is the most complete information on<br />
the variations <strong>of</strong> the sequences analyzed. In addition, it is an<br />
ideal and definitive method for the study <strong>of</strong> viral genetic<br />
variability. Moreover, the study <strong>of</strong> viral dynamics in the context<br />
www.bjid.com.br
26 Hepatitis C: Genotyping<br />
BJID 2007; 11 Supplement 1 (October)<br />
<strong>of</strong> quasispecies, during the natural history <strong>of</strong> the disease or<br />
as consequence <strong>of</strong> antiviral therapy, depends principally on<br />
the direct sequencing <strong>of</strong> certain regions <strong>of</strong> the HCV genome.<br />
Furthermore, it is considered the gold standard for determining<br />
HCV genotypes and subtypes [7].<br />
<strong>The</strong> sequencing technique for HCV genotyping consists<br />
<strong>of</strong> PCR amplification <strong>of</strong> part <strong>of</strong> the viral genome, especially <strong>of</strong><br />
the 5’NC, NS5B and core regions. <strong>The</strong>se regions are<br />
sufficiently conserved for the development <strong>of</strong> reliable primers<br />
and, at the same time, present diversity for the discrimination<br />
<strong>of</strong> viral genotypes and subtypes. <strong>The</strong> PCR employed for<br />
sequencing comes from PCR-HCV qualitative or<br />
quantitative PCR HCV products, the volume <strong>of</strong> DNA and<br />
the high purity <strong>of</strong> the resulting tapes being essential for<br />
the success <strong>of</strong> the analyses. This second PCR is performed<br />
specifically to adjust or mark these products for reading in<br />
sequencers. <strong>The</strong> assessment <strong>of</strong> both tapes, positive and<br />
negative, is essential in order to resolve possible<br />
ambiguities during the evaluation <strong>of</strong> the sequencings [7].<br />
<strong>The</strong> sequences provided by the equipment should be<br />
analyzed, and there are international databases available<br />
for consultation, for this purpose. <strong>The</strong>se databases are also<br />
used for the centralization and collection <strong>of</strong> sequences<br />
worldwide. <strong>The</strong> database recommended for Brazil is the<br />
European site http://euhcvdb.fr/, probably because <strong>of</strong> the<br />
epidemiological pathway followed during the <strong>Brazilian</strong><br />
colonization period.<br />
<strong>The</strong> genotyping test TRUGENE-SIEMENS HCV 5’NC<br />
Genotyping Kit (Siemens Medical Solutions Diagnostics,<br />
Tarrytown, NY, USA) <strong>of</strong>fers s<strong>of</strong>tware used in conjunction<br />
with the equipment, with a previously selected genomic<br />
library that analyzes the sequences <strong>of</strong> region 5’NC<br />
immediately after sequencing. In addition to the genotyping<br />
results, it presents the homology with patterns <strong>of</strong> HCV<br />
genotypes and subtypes based on region 5’NC. This<br />
methodology is only available to researchers [1,7,12].<br />
<strong>The</strong> real time PCR-HCV method is a quantitative<br />
molecular diagnostic test that uses TaqMan technology.<br />
In this test, genotype-specific probes marked for HCV<br />
typing were employed in order to identify genotypes 1, 2<br />
and 3a. Another test, also based on TaqMan technology,<br />
can identify genotypes 1 to 4 and presents specific probes<br />
for subtypes 1a/b, 2a/b/c, 3a and 4b/c/d. Both<br />
methodologies are based on region 5’NC [9,13-16].<br />
Commercially, but only for research, there is the Abbott<br />
Real-Time PCR HCV Assay (Abbott Diagnostics Europe,<br />
Wiesbaden, Germany) test, which also determines the viral<br />
genotype <strong>of</strong> the samples for HCV genotypes 1a, 1b, 2a, 2b, 3,<br />
4, 5 and 6. This methodology for the genotyping <strong>of</strong> HCV is<br />
associated with viral quantification, levels below 6053 IU/mL<br />
compromising the efficiency and sensitivity <strong>of</strong> the test [9].<br />
<strong>The</strong> identification <strong>of</strong> genotypes is clinically important, and<br />
treatment protocols recommend that genotype information<br />
be obtained in order to delineate the duration and type <strong>of</strong> the<br />
medication to be used. <strong>The</strong> literature mentions that genotypes<br />
1 and 4 are considered more resistant than are genotypes 2<br />
and 3, and that the standard treatment consists <strong>of</strong> interferon<br />
combined with ribavirin. Another disadvantage <strong>of</strong> genotypes<br />
1 and 4 is that they present a worse prognosis <strong>of</strong> evolution <strong>of</strong><br />
the disease. For treatment-naïve patients, infection with<br />
genotype 1, 4 or 5 should be treated for 12 months, compared<br />
with 6 months for infection with genotype 2 or 3. <strong>The</strong><br />
Consensus Group recommends pegylated interferon<br />
combined with ribavirin for genotype 1. For re-treatment,<br />
pegylated interferon associated with ribavirin is<br />
recommended, regardless <strong>of</strong> the genotype, in the usual doses,<br />
respecting the duration recommended for genotype 1 for other<br />
genotypes. In cases <strong>of</strong> HIV/HCV co-infection, the response<br />
to antiviral therapy for HCV is not favorable: 14%-38% for<br />
genotype 1; and 43%-73% for genotypes 2 and 3 [1,7,17,18].<br />
<strong>The</strong> advantages <strong>of</strong> genotyping methods include reliability<br />
and the opportunity to obtain important information on the<br />
molecular pathogenesis <strong>of</strong> HCV [7].<br />
<strong>The</strong> impact <strong>of</strong> HCV heterogeneity and its different<br />
genotypes on the everyday clinical management <strong>of</strong> HCV<br />
chronic infection has not been completely established, nor<br />
has its role as an epidemiological marker been clarified.<br />
<strong>The</strong> sensitivity and specificity <strong>of</strong> serological and virological<br />
tests can also be influenced by the heterogeneity <strong>of</strong> HCV,<br />
which justifies constant evolution in the study <strong>of</strong> patients<br />
and differentiation techniques <strong>of</strong> HCV genotypes and<br />
subtypes [4].<br />
References<br />
1. Simmonds P., Bukh J., Combet C., et al. Consensus proposals for<br />
a unified system <strong>of</strong> nomenclature <strong>of</strong> hepatitis C virus genotypes.<br />
Hepatology 2005;42:962-73.<br />
2. Campiotto S., Pinho J.R.R., Carrilho F.J., et al. Geographic<br />
distribution <strong>of</strong> hepatitis C virus genotypes in Brazil. <strong>Brazilian</strong><br />
<strong>Journal</strong> <strong>of</strong> Medical and Biological Research 2005;38:41-9.<br />
3. Cavalheiro N.P., Barone A.A., Tengan F.M. HCV Serotypes in<br />
brazilian patients. Int J Infect Dis 2002;6:228-32.<br />
4. Pawlotsky J.-M. Diagnostic tests for hepatitis C. J Hepatol<br />
1999;31 Suppl. 1:71-9,.<br />
5. Laperche S., Lunel F., Izopet J., et al. Comparison <strong>of</strong> Hepatitis C<br />
Virus NS5b and 5_ Noncoding Gene Sequencing Methods in a<br />
Multicenter Study. <strong>Journal</strong> <strong>of</strong> Clinical Microbiology 2005:733-9.<br />
6. Pawlotsky J.-M., Prescott L., Simmonds P., et al. Serological<br />
determination <strong>of</strong> hepatitis C virus genotype: Comparison with<br />
a standardized genotyping assay. J Clin Microbiol<br />
1997;35:1734-9.<br />
7. Stéphane C., Pawlotsky J.-M. Hepatitis C virus: Virology, diagnosis<br />
and management <strong>of</strong> antiviral therapy. World J Gastroenterol<br />
2007;13(17):2461-6.<br />
8. Prescott L.E., Simmonds P. Serological genotyping using synthetic<br />
peptides derived from the NS4 region. In: LAU, JOHNSON<br />
YIU-NAM. Hepatitis C protocols: methods in molecular<br />
medicine. Totowa, Humana Press, cap.17, p.199-205, 1998.<br />
9. Raymond H.W., Carol Cimmins. Evaluation <strong>of</strong> the Abbott<br />
Molecular Diagnostics Real Time PCR Assay for HCV<br />
Quantitative Viral Load and HCV Genotyping. Poster S30,<br />
Clinical Virology Symposium, 2004.<br />
10. Nadarajah R., Khan Y., Miller S.A., Brooks G.F. Evolution <strong>of</strong> a<br />
new generation Line-Probe Assay that detects 5’untranslated<br />
and Core regions to genotype and subtype Hepatitis C Virus. Am<br />
J Clin Pathol 2007;128:300-4.<br />
www.bjid.com.br
BJID 2007; 11 Supplement 1 (October) Hepatitis C: Genotyping<br />
27<br />
11. Bouchardeau F., Cantaloube J.F., Chevaliez S., et al. Improvement<br />
<strong>of</strong> Hepatitis C Virus (HCV) Genotype Determination with the<br />
New Version <strong>of</strong> the INNO-LiPA HCV Assay. <strong>Journal</strong> <strong>of</strong> Clinical<br />
Microbiology 2007;45:1140-5.<br />
12. Nolte F.S., Green A.M., Fiebelkorn K.R., et al. Clinical evaluation<br />
<strong>of</strong> two methods for genotyping Hepatitis C virus based on<br />
analysis <strong>of</strong> the 5’noncoding region. <strong>Journal</strong> <strong>of</strong> Clinical<br />
Microbiology 2003;41:1558-64.<br />
13. Lindh M., Hannoun C. Genotyping <strong>of</strong> hepatitis C virus by Taqman<br />
real-time PCR. <strong>Journal</strong> <strong>of</strong> Clinical Virology 2005;34:108-14.<br />
14. Moghaddam A., Reinton N., Dalgard O. A rapid real-time PCR<br />
assay for determination virus genotypes 1, 2 and 3a. <strong>Journal</strong> <strong>of</strong><br />
Viral Hepatitis 2006;13:222-9.<br />
15. Rolfe K.J., Alexander G.J.M., Tim G.W., et al. A real-time Taqman<br />
method for hepatitis C virus genotyping. <strong>Journal</strong> <strong>of</strong> Clinical<br />
Virology 2005;34:115-21.<br />
16. Mukaide M., Tanaka Y., Kakuda H., et al. New combination test<br />
for hepatitis C virus genotype and viral load determination<br />
using Amplicor GT HCV MONITOR test v2.0. World J<br />
Gastroenterol 2005;11(4):469-75.<br />
17. Poynard T., Marcellin P., Lee S.S., et al. Randomized trial <strong>of</strong> interferon<br />
alfa 2b plus ribavirin for 48 weeks or for 24 weeks versus interferon<br />
alfa 2bplus placebo for 48 weeks for treatment <strong>of</strong> chronic infectious<br />
hepatitis C virus. Lancet 1998;352:1426-32.<br />
18. Tom Wong, Samuel S.L. Hepatitis C: a review for primary care<br />
physicians. CMAJ 2006;174(5):649-59.<br />
www.bjid.com.br
28 BJID 2007; 11 Supplement 1 (October)<br />
Noninvasive Means <strong>of</strong> Diagnosing Liver Fibrosis in Hepatitis C<br />
Eduardo Sellan Lopes Gonçales, Adriana Flávia Feltrim Angerami and Fernando Lopes Gonçales Junior<br />
Study Group on Hepatitis, <strong>Infectious</strong> <strong>Diseases</strong> Division, UNICAMP; Campinas,SP<br />
Liver biopsy is still considered the gold standard for<br />
staging fibrosis in chronic liver diseases. However, liver<br />
biopsy is an invasive procedure, and complications occur in<br />
0.6%-5% <strong>of</strong> patients [1,2]. In addition, to perform the procedure<br />
there is a need for additional resources such as<br />
ultrasonography. <strong>The</strong>refore, as a rule, patients undergoing<br />
liver biopsy are hospitalized for at least 6 hours [3].<br />
Recent studies involving patients with chronic hepatitis<br />
C showed that fragments <strong>of</strong> technically inadequate hepatic<br />
tissue frequently lead to the underestimation <strong>of</strong> the stage <strong>of</strong><br />
liver fibrosis [4]. That rate <strong>of</strong> diagnostic error can vary from<br />
10%-30% depending on the study [5]. In addition, in<br />
developed countries, there is greater patient resistance to<br />
undergoing biopsy.<br />
In Brazil there is an additional factor, which is that patients<br />
are obligated to submit to liver biopsy for indication <strong>of</strong><br />
treatment, except in clinically confirmed cases <strong>of</strong> hepatic<br />
cirrhosis according to the Ministry <strong>of</strong> Health guidelines.<br />
For all <strong>of</strong> these reasons, an increasing number <strong>of</strong> studies<br />
are being conducted in order to evaluate the effectiveness <strong>of</strong><br />
noninvasive markers for staging liver fibrosis. <strong>The</strong><br />
noninvasive methods used in the largest number <strong>of</strong> published<br />
studies are the calculation <strong>of</strong> two indices - the aspartate<br />
aminotransferase (AST) to platelet ratio index (APRI) and<br />
the FibroTest index - and the FibroScan test.<br />
<strong>The</strong> effectiveness <strong>of</strong> the various methods evaluated in<br />
various studies revealed quite heterogeneous results. <strong>The</strong><br />
APRI method and the Forns index are unable to stage a large<br />
percentage <strong>of</strong> patients, and their accuracies do not exceed<br />
80-85%. <strong>The</strong>refore, a considerable number <strong>of</strong> patients are<br />
required to undergo liver biopsy. Otherwise, approximately<br />
20% would be incorrectly diagnosed. <strong>The</strong> efficacy <strong>of</strong> those<br />
methods encounters difficulty regarding standardization and<br />
the definition <strong>of</strong> cut-<strong>of</strong>f values for each degree <strong>of</strong> fibrosis.<br />
cut-<strong>of</strong>f values are used. <strong>The</strong> absence <strong>of</strong> cirrhosis (Ishak stage<br />
0-4) is defined as values lower than 1, and cirrhosis (Ishak<br />
stage 5-6) is defined as values higher than 2 [6]. <strong>The</strong> formula<br />
for calculating the APRI test is as follows:<br />
APRI = AST(/LSN) × 100 / Platelets (10 9 /L)<br />
Table 1 shows the APRI values obtained.<br />
Table 1. <strong>The</strong> aspartate aminotransferase to platelet ratio index<br />
results obtained by Wai et al.<br />
Cut-Off PPV NPV<br />
No Fibrosis < 0.5 64% 90%<br />
Fibrosis > 1.5 91% 65%<br />
No Cirrhosis < 1.0 35% 100%<br />
Cirrhosis > 2.0 65% 95%<br />
PPV=positive predictive value; NPV=negative predictive value.<br />
<strong>The</strong>refore, the aforementioned Wai et al. showed that the<br />
APRI has a high positive predictive value to identify patients<br />
with significant fibrosis and a high negative predictive value<br />
to rule out cirrhosis. That study also showed that it is possible<br />
to predict the presence or absence <strong>of</strong> significant fibrosis in<br />
51% <strong>of</strong> patients and to predict the presence or absence <strong>of</strong><br />
cirrhosis in 81% <strong>of</strong> patients [6].<br />
FibroTest<br />
FibroTest combines and analyzes the serum levels <strong>of</strong> five<br />
factors in patients with chronic hepatitis C. Those five factors<br />
are bilirubin, gamma-glutamyl transferase, apolipoprotein A1,<br />
alpha-2-macroglobulin and haptoglobin. <strong>The</strong> results obtained<br />
are evaluated through a formula which predicts and classifies<br />
them as F0-1, F2-3 and F4 [7].<br />
APRI<br />
<strong>The</strong> APRI was developed by Wai et al. [6] and is calculated<br />
based on AST levels and platelet counts. According to the<br />
results obtained in that study, the lower and upper cut-<strong>of</strong>f<br />
values for the definition <strong>of</strong> significant fibrosis and cirrhosis<br />
are determined. Through analysis <strong>of</strong> the results, the positive<br />
and negative predictive values for the presence or absence<br />
<strong>of</strong> significant fibrosis or cirrhosis are also determined.<br />
To evaluate significant fibrosis, the following cut-<strong>of</strong>f<br />
values are used: lower than 0.5 (absence <strong>of</strong> significant fibrosis,<br />
Ishak stage 0-2); and higher than 1.5 (presence <strong>of</strong> significant<br />
fibrosis, Ishak stage 3-6)[6]. To evaluate cirrhosis, different<br />
<strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> 2007;11 (5) Suppl. 1:28-31.<br />
© 2007 by <strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> and Contexto<br />
Publishing. All rights reserved.<br />
FibroScan - A New Noninvasive Method<br />
<strong>The</strong> evaluation <strong>of</strong> the degree <strong>of</strong> liver fibrosis is <strong>of</strong><br />
fundamental importance to the prognosis, follow-up and<br />
therapeutic decision-making for patients with chronic liver<br />
disease. Biopsy is an invasive method and occasionally<br />
(although rarely) results in complications. In addition, the<br />
biopsy results, from an anatomical-pathological point <strong>of</strong> view,<br />
are <strong>of</strong>ten evaluated subjectively [8,9]. Nevertheless, biopsy<br />
continues to be the gold standard by which fibrosis is staged<br />
and evaluated<br />
<strong>The</strong>re are various studies on noninvasive options in the<br />
staging, evaluation and monitoring <strong>of</strong> liver fibrosis. FibroScan<br />
is a new method, still only available on a small scale, which<br />
presents better results in various studies with respect to<br />
differentiating between cirrhotic and noncirrhotic patients. It<br />
www.bjid.com.br
BJID 2007; 11 Supplement 1 (October) Noninvasive Diagnosis <strong>of</strong> Fibrosis in Hepatitis C<br />
29<br />
Figure 1. Algorithm proposed by Sebastiani et al. (EASL) [14], in which the aspartate aminotransferase to platelet ratio index<br />
(APRI) method is used in conjunction with FibroTest. ALT=alanine aminotransferase; UDE=upper digestive tract endoscopy;<br />
US=ultrasound.<br />
Chronic hepatitis C with elevated ALT levels<br />
APRI<br />
F0-F1<br />
Unclassified<br />
F≥2<br />
FibroTest<br />
F0-F1<br />
F≥2<br />
Biopsy<br />
F0-F1<br />
Significant fibrosis (≥F2)<br />
is considered a quick and easy noninvasive procedure for<br />
diagnosing cirrhosis and has been presented as an alternative<br />
to liver biopsy in patients with a formal contraindication [8].<br />
FibroScan measures hepatic elasticity through a transducer<br />
positioned intercostally on the skin over the right lobe <strong>of</strong> the<br />
liver. <strong>The</strong> transducer transmits low amplitude and low<br />
frequency vibration pulses to the hepatic tissue. This<br />
vibration pulses propagate an elastic wave whose velocity is<br />
directly related to the elasticity <strong>of</strong> the tissue. Results are<br />
given in kilopascals (kPa).<br />
Some studies have shown that body mass index and age<br />
<strong>of</strong> the patient, as well as the level <strong>of</strong> experience on the part <strong>of</strong><br />
the health pr<strong>of</strong>essional, can influence the FibroScan results<br />
<strong>of</strong> patients with chronic hepatitis C. <strong>The</strong> body mass index<br />
and steatosis can affect the evaluation <strong>of</strong> fibrosis, although<br />
some studies have shown that those factors are minimized<br />
if the test is repeated a fair number <strong>of</strong> times. Some studies<br />
recommend a total <strong>of</strong> five measurements to validate the<br />
results [10].<br />
For the detection <strong>of</strong> fibrosis ≥ F2, FibroScan presents<br />
85.2% sensitivity, 90.7% specificity, 93.8% positive<br />
predictive value, 78.8% negative predictive value and 87.7%<br />
diagnostic power. For the detection <strong>of</strong> cirrhosis, the test<br />
presents 78.3% sensitivity, 98.2% specificity, 97.8% positive<br />
predictive value, 81.6% negative predictive value and 88.2%<br />
diagnostic power [11-13].<br />
Despite the reasonable quantity <strong>of</strong> published studies, few<br />
have compared the methods in a randomized manner. <strong>The</strong>re<br />
are two studies that propose algorithms for evaluation. <strong>The</strong><br />
first study, published by the European Association for the<br />
www.bjid.com.br
30 Noninvasive Diagnosis <strong>of</strong> Fibrosis in Hepatitis C<br />
BJID 2007; 11 Supplement 1 (October)<br />
Figure 2. Algorithm proposed by Castéra et al. [15], in which the FibroTest results are evaluated together with the FibroScan<br />
results.<br />
Detectable HCV<br />
RNA<br />
FibroScan/<br />
FibroTest<br />
Concordance<br />
between the two<br />
methods<br />
No<br />
Yes<br />
Liver biopsy<br />
No liver biopsy<br />
Treatment or<br />
monitoring<br />
Fibrosis absent or<br />
minimal (
BJID 2007; 11 Supplement 1 (October) Noninvasive Diagnosis <strong>of</strong> Fibrosis in Hepatitis C<br />
31<br />
<strong>The</strong> study conducted by Castéra et al. proposes the<br />
combination <strong>of</strong> FibroScan and FibroTest as a screening<br />
method for significant fibrosis. When there was concordance<br />
between the methods, which occurred in 70%-80% <strong>of</strong> patients,<br />
the compatibility with the liver biopsy was 84% in diagnosing<br />
fibrosis ≥ F2, 95% in diagnosing fibrosis ≥ F3, and a 94% in<br />
diagnosing cirrhosis (F4).<br />
<strong>The</strong>refore, much still needs to be studied in relation to<br />
the noninvasive methods for estimating the degree <strong>of</strong><br />
fibrosis, which is why it is necessary to carry out randomized<br />
comparative studies involving different patient populations.<br />
Table 2. FibroScan results<br />
Variable Degree <strong>of</strong> fibrosis<br />
≥F2 ≥F3 F4<br />
Sensitivity 67% 73% 87%<br />
Specificity 89% 91% 91%<br />
PPV 95% 87% 77%<br />
NPV 48% 81% 95%<br />
PPV=positive predictive value; NPV=negative predictive value.<br />
to the fact that the majority <strong>of</strong> patients presented significant<br />
fibrosis. <strong>The</strong> principal limitation <strong>of</strong> these markers is the<br />
difficulty in obtaining confirmation for patients with F0-F1<br />
fibrosis. <strong>The</strong>refore, an algorithm for the evaluation <strong>of</strong> fibrosis<br />
that attempts to define which patients are not required to<br />
undergo liver biopsy was developed.<br />
Another study conducted by Castéra et al. [15] compared<br />
the effectiveness <strong>of</strong> transitory hepatic elastography<br />
(FibroScan, Echosens, Paris, France) in relation to the APRI<br />
and FibroTest. It succeeded in showing that FibroScan has a<br />
great capacity to diagnose significant fibrosis (≥ F2). <strong>The</strong><br />
results can be seen in Table 2.<br />
<strong>The</strong>refore, it can be seen that FibroScan presents a high<br />
positive predictive value for patients with fibrosis ≥ F2 and<br />
an excellent negative predictive value for patients with hepatic<br />
cirrhosis. It is undoubtedly a good method for demonstrating<br />
significant fibrosis or for ruling out hepatic cirrhosis.<br />
References<br />
1. Perrault J., McGill D.B., Ott B.J., Taylor W.F. Liver biopsy:<br />
complications in 1000 inpatients. Gastroenterology<br />
1978;74:103-6.<br />
2. Gunneson T.J., Menon K.V., Wiesner R.H., et al. Ultrasoundassisted<br />
percutaneous liver biopsy perfomed by a physician<br />
assistant. Am J Gastroenterol 2002;97:1472-5.<br />
3. Wong J.B., K<strong>of</strong>f R.S. Watchful waiting with periodic liver biopsy<br />
versus immediate empirical therapy for histologically mild<br />
chronic hepatitis C. A cost-effectiveness analysis. Ann Intern<br />
Med 2000;133:665-75.<br />
4. Colloredo G., Guido M., Sonzogni A., Leandro G. Impact <strong>of</strong> liver<br />
biopsy size on histological evaluation <strong>of</strong> chronic viral hepatitis:<br />
the smaller the sample, the milder the disease. J Hepatol<br />
2003;39:239-44.<br />
5. Poniachik J., Bernstein D.E., Reddy K.R., et al. <strong>The</strong> role <strong>of</strong><br />
laparoscopy in the diagnosis <strong>of</strong> cirrhosis. Gastrointest Endosc<br />
1996;43:568-71.<br />
6. Wai C.T., Greenson J.K., Fontana R.J., et al. A simple<br />
noninvasive índex can predict both significant fibrosis and<br />
cirrhosis in patients with chronic hepatitis C. Hepatology<br />
2003;38:518-26.<br />
7. Poynard T., McHutchison J., Manns M., et al. Biochemical<br />
surrogate markers <strong>of</strong> liver fibrosis and activity in a randomized<br />
trial <strong>of</strong> peginterferon alfa-2b and ribavirin. Hepatology<br />
2003;38:481-92.<br />
8. Transient elastography: a new surrogate marker <strong>of</strong> liver fibrosis<br />
influenced by major changes <strong>of</strong> transaminases. <strong>Journal</strong> <strong>of</strong> Viral<br />
Hepatitis 2007;14:360-9.<br />
9. Diagnosis <strong>of</strong> hepatic steatosis and fibrosis by transient<br />
elastography in asymptomatic healthy individuals: a<br />
prospective study <strong>of</strong> living related potencial liver donors.<br />
<strong>Journal</strong> <strong>of</strong> Gastroenterol 2007;42:382-8.<br />
10. Usefulneness <strong>of</strong> elastometry in evaluating the extents <strong>of</strong> liver<br />
fibrosis in hemophiliacs coinfected with hepatitis C and<br />
human immunodeficiency virus. Hepatology research<br />
2006;35:135-9.<br />
11. Features associated with success rate and performance <strong>of</strong> fibroscan<br />
measurements for the diagnosis <strong>of</strong> cirrhosis in HCV patients: a<br />
prospective study <strong>of</strong> 935 patients. <strong>Journal</strong> <strong>of</strong> Hepatology<br />
2007;46:628-34.<br />
12. Transient elastography: a valid alternative to biopsy in patients<br />
with chronic liver disease. <strong>Journal</strong> compilation 2006;24:513-8.<br />
13. Do not trivialize the Fibroscan examination, value its accuracy.<br />
<strong>Journal</strong> <strong>of</strong> Hepatology 2007;46.<br />
14. Sebastiani G., Vario A., Guido M., et al. Stepwise combination<br />
algorithms <strong>of</strong> non-invasive markers to diagnose significant<br />
fibrosis in chronic hepatitis C. <strong>Journal</strong> <strong>of</strong> Hepatology<br />
2006;44:686-93.<br />
15. Castéra L., Vergniol J., Foucher J., et al. Gastroenterology<br />
2005;128:343-50.<br />
www.bjid.com.br
32 BJID 2007; 11 Supplement 1 (October)<br />
Chronic Hepatitis C: Pathological Anatomy<br />
Evandro Sobroza de Mello and Venâncio Avancini Ferreira Alves<br />
Pathological Anatomy Division, Hospital das Clínicas <strong>of</strong> São Paulo; LIM-14: Hepatic Pathology,<br />
University <strong>of</strong> São Paulo School <strong>of</strong> Medicine; CICAP – Hospital Alemão Oswaldo Cruz; São Paulo, SP, Brazil<br />
In infections with the hepatitis C virus (HCV), there is a<br />
wide spectrum <strong>of</strong> histological alterations that can affect the<br />
liver, from acute hepatitis to mild reactive phenomena to more<br />
severe forms, including chronic hepatitis with varying degrees<br />
<strong>of</strong> inflammation/fibrosis, cirrhosis, and hepatocellular<br />
carcinoma. In cases <strong>of</strong> acute hepatitis C, biopsies are rare,<br />
pathologists focusing their attention on the chronic form <strong>of</strong><br />
the disease. <strong>The</strong> histological diagnosis <strong>of</strong> chronic hepatitis<br />
through liver biopsy remains extremely important in the<br />
management <strong>of</strong> patients infected with HCV, since it is the<br />
cornerstone <strong>of</strong> the detection <strong>of</strong> liver disease caused by the<br />
virus as well as the determination <strong>of</strong> the intensity <strong>of</strong> this<br />
disease. It should therefore be added to the diagnosis <strong>of</strong><br />
infection made using serologic methods.<br />
<strong>The</strong> basic parameter for the histological diagnosis <strong>of</strong><br />
chronic hepatitis is the presence <strong>of</strong> portal inflammatory<br />
infiltrate, with predominance <strong>of</strong> lymphocytes, usually with<br />
variations in the number <strong>of</strong> plasmocytes and histiocytes. This<br />
inflammation is accompanied by periportal activity <strong>of</strong> varying<br />
degrees (also denominated interface activity or piecemeal<br />
necrosis), parenchymal activity (lobular) and fibrosis.<br />
<strong>The</strong>re are various classification systems using in the<br />
scoring and staging <strong>of</strong> chronic hepatitis [4,9,11,13,18,21,34].<br />
Many <strong>of</strong> those systems are <strong>of</strong> historical importance. According<br />
to directive no. 863, issued by the São Paulo State Secretary<br />
<strong>of</strong> Health on November 4, 2002, it is recommended that one <strong>of</strong><br />
two chronic hepatitis classification systems be used: the<br />
<strong>Sociedade</strong> <strong>Brasileira</strong> de Patologia (SBP, <strong>Brazilian</strong> Society <strong>of</strong><br />
Pathology) system [13] or the METAVIR system [1,4]. <strong>The</strong>se<br />
two systems are in fact very similar, and they both take into<br />
account the previously mentioned basic aspects <strong>of</strong> chronic<br />
hepatitis: periportal activity, lobular activity, and fibrosis. In<br />
addition to these, the classification system proposed by Ishak<br />
in 1995 [18] has been widely used in international literature.<br />
<strong>The</strong> Ishak system is an update <strong>of</strong> the system proposed by the<br />
same author in 1981, which gained popularity and was<br />
commonly referred to as the Knodell system [21] (a designation<br />
that should no longer be used), has been widely used in<br />
international literature. Table 1 shows an approximate<br />
correspondence between these systems, both for fibrosis<br />
(architectural alteration) and for periportal/lobular activity.<br />
<strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> 2007;11 (5) Suppl. 1:32-36.<br />
© 2007 by <strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> and Contexto<br />
Publishing. All rights reserved.<br />
Protocol <strong>of</strong> Histological Evaluation for Liver Biopsies <strong>of</strong><br />
Patients with Chronic viral Hepatitis<br />
This protocol can be applied to several etiologies <strong>of</strong><br />
chronic hepatitis, including, in addition to HCV, HBV, autoimmune<br />
hepatitis and, less frequently, Wilson’s disease or<br />
some forms <strong>of</strong> drug-induced hepatitis. <strong>The</strong> protocol is based<br />
on the criteria <strong>of</strong> the SBP National Consensus <strong>of</strong> Chronic<br />
Hepatitis [13].<br />
1) Sample type (needle biopsy, wedge biopsy, resected<br />
surgical sample, other):<br />
2) Sample size<br />
Number <strong>of</strong> portal spaces in the biopsy: _____<br />
3) Histological variables:<br />
• Portal fibrosis:<br />
( ) 0 (absent)<br />
( ) 1 (discrete, without septum formation)<br />
( ) 2 (with portal-portal septa)<br />
( ) 3 (with portal-portal and portal-central septa, with<br />
formation <strong>of</strong> nodules – in ‘nodular transformation’)<br />
( ) 4 (cirrhosis)<br />
• Portal inflammation<br />
( ) 0 (absent)<br />
( ) 1 (discrete)<br />
( ) 2 (moderate)<br />
( ) 3 (pronounced)<br />
( ) 4 (very pronounced)<br />
• Periportal activity (interface activity)<br />
( ) 0 (absent)<br />
( ) 1 (presence <strong>of</strong> spillover only)<br />
( ) 2 (discrete piecemeal necrosis – occasional foci in<br />
some portal spaces)<br />
( ) 3 (moderate piecemeal necrosis – occasional foci in<br />
many portal spaces or innumerable foci in few portal<br />
spaces)<br />
( ) 4 (pronounced piecemeal necrosis - innumerable foci<br />
in many portal spaces)<br />
• Parenchymal activity<br />
( ) 0 (absent)<br />
( ) 1 (tumefaction, lymphocyte sinusoidal infiltrate and<br />
occasional foci <strong>of</strong> lytic hepatocytic necrosis)<br />
( ) 2 (innumerable foci <strong>of</strong> lytic hepatocytic necrosis)<br />
( ) 3 (occasional areas <strong>of</strong> confluent necrosis)<br />
( ) 4 (innumerable areas <strong>of</strong> confluent necrosis or areas<br />
<strong>of</strong> panacinar necrosis)<br />
• Histological evidence <strong>of</strong> association with other conditions:<br />
( ) level ______ siderosis<br />
( ) steatohepatitis markers<br />
( ) others:______<br />
Nature and Size <strong>of</strong> the Liver Biopsy<br />
Surgical biopsies performed with forceps generate<br />
subcapsular samples and should be discouraged, since the<br />
portal spaces in this location are frequently large, and it is<br />
www.bjid.com.br
BJID 2007; 11 Supplement 1 (October) Chronic Hepatitis C – Pathological Anatomy<br />
33<br />
Table 1. Approximate equivalence <strong>of</strong> the most widely used classification systems for the staging and scoring <strong>of</strong> chronic hepatitis<br />
difficult or impossible to correctly evaluate the presence <strong>of</strong><br />
fibrosis. Even during the surgical procedure, therefore, liver<br />
biopsy should be performed with a needle. In addition, the<br />
biopsy should preferably be performed at the outset <strong>of</strong> the<br />
surgery in order to prevent alterations secondary to surgical<br />
manipulation.<br />
Data in the literature demonstrate that the size <strong>of</strong> the needle<br />
biopsy greatly influences the result <strong>of</strong> the analysis<br />
[8,10,15,33,35]. Samples measuring 3.0 cm or more in length,<br />
show hepatitis with mild activity, as a result, in only 50% <strong>of</strong><br />
the cases; 1.5-cm long samples, in 60%; and those measuring<br />
1.0 cm or less, in almost 90% <strong>of</strong> the cases [8]. Other authors<br />
have also considered 1.5 cm as the minimum size for diagnosis<br />
in needle liver biopsy [35]. Thin needles have also provided<br />
inferior results [8,33]. Bedossa et al. [3] only achieved a<br />
precision plateau with 2.5-cm long biopsies. <strong>The</strong>refore, 1.5-<br />
cm long biopsies should be considered the minimum<br />
necessary size and, ideally, they should measure 2.5 cm or<br />
more. Larger diameter needles, such as Tru-Cut needles, are<br />
also recommended.<br />
Steatosis<br />
Approximately 50% <strong>of</strong> the biopsy samples collected from<br />
patients with HCV present steatosis [17,40]. <strong>The</strong> evaluation<br />
<strong>of</strong> the presence <strong>of</strong> steatosis, its scoring, and the evaluation <strong>of</strong><br />
the presence <strong>of</strong> associated steatohepatitis has gradually<br />
become more important [6,7,12,16,19,20,24,29-32,36,40].<br />
<strong>The</strong> spectrum <strong>of</strong> steatosis, steatohepatitis and cirrhosis has<br />
been denominated nonalcoholic fatty liver disease (NAFLD).<br />
Although NAFLD is common in the population in general,<br />
concomitance between NAFLD and HCV is 2-3 times greater<br />
Architectural Alteration (Fibrosis)*<br />
SBP, 2000 METAVIR, 1994 Ishak, 1995<br />
0 0 0<br />
1<br />
2<br />
1<br />
2<br />
1 or 2<br />
3<br />
3 3 4 or 5<br />
4 4 6<br />
Parenchymal activity<br />
Inflammatory Activity**<br />
SBP, 2000 and Ishak, 1995 METAVIR, 1994<br />
Periportal activity<br />
A<br />
0 or 1 0 0<br />
0 or 1<br />
2<br />
1 or 2<br />
0–1<br />
1<br />
1<br />
2 2 2<br />
2<br />
3<br />
3–4<br />
0–2<br />
3<br />
2<br />
3 3–4 3<br />
4 0–4 3<br />
SBP= <strong>Sociedade</strong> <strong>Brasileira</strong> de Patologia (SBP, <strong>Brazilian</strong> Society <strong>of</strong> Pathology). *Maximum Ishak<br />
score, 6; maximum METAVIR score, 4; maximum SBP score, 4. **Corresponds to periportal and<br />
parenchymal activity, independently, for SBP and Ishak, and mixed periportal and lobular for METAVIR;<br />
in the METAVIR classification, the activity score reaches 3, whereas in Ishak and SBP it reaches 4.<br />
than what would be expected only at random [24]. In patients<br />
with chronic HCV infection, steatosis has been attributed to a<br />
series <strong>of</strong> factors usually associated with NAFLD, including<br />
high body mass index, insulin resistance and old age [16,26,31].<br />
Evidence also indicates that steatosis contributes to the<br />
progression <strong>of</strong> fibrosis in a pattern similar to that seen in NAFLD<br />
[7,16,17,40].<br />
It has been suggested that steatosis can also result from<br />
the viral cytopathic effect, especially in patients infected with<br />
genotype 3. In a series <strong>of</strong> patients with genotype 3 and steatosis,<br />
a sustained virological response led to regression <strong>of</strong> steatosis in<br />
91% <strong>of</strong> the cases, a much higher index than the 19% observed for<br />
those who did not present sustained virological response [6],<br />
making the cytopathic effect a more consistent cause <strong>of</strong> steatosis.<br />
Other authors have reported similar results [22,36].<br />
In HCV-positive patients, it is currently essential to<br />
characterize steatosis and related injuries, especially the<br />
presence and quantification <strong>of</strong> perisinusoidal and centrilobular<br />
fibrosis, which characterizes steatohepatitis. <strong>The</strong> lesson we learn<br />
from steatosis is that, in HCV-infected patients, biopsy is an<br />
instrument for the detection <strong>of</strong> liver diseases, whether associated<br />
with the virus or not, and that we should be prepared for other<br />
(probably less common) liver diseases that might be present in<br />
a particular case.<br />
Histopathological Aspects <strong>of</strong> Post-Transplant HCV<br />
Recurrence<br />
Immediate post-transplant virological recurrence <strong>of</strong> HCV<br />
is universal, and the progression <strong>of</strong> the disease is more rapid<br />
www.bjid.com.br
34 Chronic Hepatitis C – Pathological Anatomy<br />
BJID 2007; 11 Supplement 1 (October)<br />
than in non-transplanted patients [22A]. Long-term studies have<br />
shown that 70-90% <strong>of</strong> cases will present histological recurrence<br />
<strong>of</strong> the disease [20A,23A]. In most cases, hepatitis C<br />
histologically manifests in the same manner before the<br />
transplant: with portal and parenchymal inflammation,<br />
aggression <strong>of</strong> the interface with piecemeal necrosis, and fibrosis<br />
at portal spaces. Steatosis and ductal injury are also common<br />
findings. Earlier findings are <strong>of</strong>ten predominantly lobular, with<br />
inflammation and apoptotic bodies (acute hepatitis), and<br />
steatosis is occasionally the first histological manifestation<br />
[4A]. In a small proportion <strong>of</strong> cases, hepatitis C can result in a<br />
severe, rapidly progressive cholestatic pattern, which leads to<br />
loss <strong>of</strong> the graft [36A,41,42]. Due to the low tolerance <strong>of</strong><br />
transplanted individuals to the treatment with interferon and<br />
ribavirin [24A,45], the evaluation <strong>of</strong> the biopsy is crucial for<br />
indication <strong>of</strong> treatment. Some anatomopathological aspects can<br />
be useful in predicting its evolution: histological recurrence in<br />
less than six months [46]; level <strong>of</strong> inflammatory activity [23A,44];<br />
marked ballooning <strong>of</strong> hepatocytes; and cholestasis [43].<br />
Histopathological Criteria for Possible Predictive Value <strong>of</strong><br />
Worse Evolution<br />
In chronic hepatitis, the contribution <strong>of</strong> the<br />
histopathological analysis <strong>of</strong> the samples collected by liver<br />
biopsy is currently considered decisive for diagnosis, for<br />
staging <strong>of</strong> the architectural damage, and for determining the<br />
level <strong>of</strong> necroinflammatory activity, assuming a decisive role<br />
in indicating the therapy with antiviral agents.<br />
In our view, in addition to reports on that decision, as<br />
summarized in the METAVIR, Ishak, Scheuer, and Desmet<br />
classification systems, or, among us, the SBP/<strong>Brazilian</strong> Society<br />
<strong>of</strong> Hepatology consensus led by Gayotto, most recent<br />
evidence brings back the need <strong>of</strong> a detailed report <strong>of</strong> each <strong>of</strong><br />
the principal forms <strong>of</strong> liver damage, and there have been<br />
studies that demonstrate a more rapid evolution <strong>of</strong> cases that<br />
present, among other predictive factors, more interface activity,<br />
confluent necrosis <strong>of</strong> hepatocytes, and steatosis [47,48].<br />
A study involving 106 patients with initial biopsy<br />
presenting architectural staging 0 or 1 and re-biopsied after a<br />
mean interval <strong>of</strong> 7.8 years (minimum <strong>of</strong> 48 months) [48] revealed<br />
progression <strong>of</strong> architectural damage in 64 cases (60.4%),<br />
suggesting the need for therapeutic intervention, even in<br />
infected individuals not yet presenting significant alterations<br />
to the hepatic architecture. Among the predictive factors for<br />
progression <strong>of</strong> the injury, those authors highlight the level <strong>of</strong><br />
necroinflammatory activity: 31.2% <strong>of</strong> the cases with moderate<br />
activity (A2) presented progression, which only occurred in<br />
2.3% <strong>of</strong> those without activity (A0) and the presence <strong>of</strong><br />
steatosis (progression in 87.5% <strong>of</strong> the cases with > 30% cells<br />
with steatosis, in 80% <strong>of</strong> those with < 30% steatosis, and in<br />
only 48.6% without steatosis).<br />
Other authors also emphasize the presence and extent <strong>of</strong><br />
steatosis as a risk factor for progression <strong>of</strong> injuries in chronic<br />
hepatitis C, either resulting from viral cytopathic effect, as<br />
proposed for genotype 3a [49], or associated with coexistent<br />
steatohepatitis, alcoholic [50] or nonalcoholic [47]. A recent<br />
meta-analysis including 3068 Italian patients infected with<br />
HCV and submitted to biopsy [51] confirmed that steatosis is<br />
independently associated with genotype 3, fibrosis, diabetes,<br />
inflammatory liver activity, drinking, body mass index, and<br />
older age.<br />
Important experience was brought to debate in the most<br />
recent European Hepatology Congress: analyzing predictive<br />
factors <strong>of</strong> damage progression in 563 cases <strong>of</strong> HCV with mean<br />
intervals between biopsies <strong>of</strong> 5.4 years [52], it was determined<br />
that, in contrast to generic approaches that suggested that<br />
liver damage progress in a relatively uniform, linear manner, the<br />
speed <strong>of</strong> progression varied considerably in each patient. <strong>The</strong>se<br />
authors, selecting statistically significant variables, identified<br />
the risk <strong>of</strong> progression associated with various architectural<br />
alterations (Table 2).We find, therefore, that important current<br />
studies demonstrate the outstanding contribution <strong>of</strong><br />
histopathological findings in the discrimination <strong>of</strong> differentiated<br />
progression risk in patients chronically infected with HCV. More<br />
than dividing patients in classes that deserve antiviral treatment<br />
or not, most recent evidence point to the need <strong>of</strong> reviewing the<br />
systems <strong>of</strong> histological scoring, and the pathologist should<br />
inform, in addition to the stage <strong>of</strong> architectural alteration, the<br />
level <strong>of</strong> each type <strong>of</strong> necroinflammatory damage in each acinar<br />
compartment <strong>of</strong> the liver.<br />
Table 2. Progression risks <strong>of</strong> architectural alterations<br />
Factor<br />
Relative Risk<br />
Age > 50 years 1.6<br />
Brindging necrosis 4.0<br />
Confluent necrosis 3.4<br />
Piecemeal necrosis 2.9<br />
Steatosis<br />
Moderate/Pronounced 3.8<br />
Discrete 2.1<br />
Perivenular fibrosis 2.6<br />
References<br />
1. <strong>The</strong> French METAVIR Cooperative Study Group. Intraobserver<br />
and interobserver variations in liver biopsy interpretation in<br />
patients with chronic hepatitis C. Hepatology 1994;20:15-20.<br />
2. Bain V.G., Bonacini M., Govindarajan S., et al. A multicentre study<br />
<strong>of</strong> the usefulness <strong>of</strong> liver biopsy in hepatitis C. J Viral Hepat<br />
2004;11:375-82.<br />
3. Bedossa P., Dargere D., Paradis V. Sampling variability <strong>of</strong> liver<br />
fibrosis in chronic hepatitis C. Hepatology 2003;38:1449-57.<br />
4. Bedossa P., Poynard T. An algorithm for the grading <strong>of</strong> activity in<br />
chronic hepatitis C. <strong>The</strong> METAVIR Cooperative Study Group.<br />
Hepatology 1996;24:289-93.<br />
4a.Baiocchi L., Tisone G., Palmieri G., et al. Hepatic steatosis: a<br />
specific sign <strong>of</strong> hepatitis C reinfection after liver transplantation.<br />
Liver Transpl Surg 1998;4:441-7.<br />
5. Berg T., Sarrazin C., Hinrichsen H., et al. Does noninvasive staging<br />
<strong>of</strong> fibrosis challenge liver biopsy as a gold standard in chronic<br />
hepatitis C? Hepatology 2004;39:1456-7; author reply 1457-<br />
1458.<br />
www.bjid.com.br
BJID 2007; 11 Supplement 1 (October) Chronic Hepatitis C – Pathological Anatomy<br />
35<br />
6. Castera L., Hezode C., Roudot-Thoraval F., et al. Effect <strong>of</strong><br />
antiviral treatment on evolution <strong>of</strong> liver steatosis in<br />
patients with chronic hepatitis C: indirect evidence <strong>of</strong> a<br />
role <strong>of</strong> hepatitis C virus genotype 3 in steatosis. Gut<br />
2004;53:420-4.<br />
7. Cholet F., Nousbaum J.B., Richecoeur M., et al. Factors associated<br />
with liver steatosis and fibrosis in chronic hepatitis C patients.<br />
Gastroenterol Clin Biol 2004;28:272-8.<br />
8. Colloredo G., Guido M., Sonzogni A., Leandro G. Impact <strong>of</strong> liver<br />
biopsy size on histological evaluation <strong>of</strong> chronic viral hepatitis:<br />
the smaller the sample, the milder the disease. J Hepatol<br />
2003;39:239-44.<br />
9. De Groote J., Desmet V.J., Gedigk P., et al. A classification <strong>of</strong><br />
chronic hepatitis. Lancet 1968;2:626-8.<br />
10. Demetris A.J., Ruppert K. Pathologist’s perspective on liver needle<br />
biopsy size? J Hepatol 2003;39:275-7.<br />
11. Desmet V.J., Gerber M., Ho<strong>of</strong>nagle J.H., et al. Classification <strong>of</strong><br />
chronic hepatitis: diagnosis, grading and staging. Hepatology<br />
1994;19:1513-20.<br />
12. Fiore G., Fera G., Napoli N., et al. Liver steatosis and chronic<br />
hepatitis C: a spurious association? Eur J Gastroenterol Hepatol<br />
1996;8:125-9.<br />
13. Gayotto L.C.C., Alves V.A., Cerski C.T., et al. Visão Histórica e<br />
consenso nacional sobre a classificação das hepatites crônicas -<br />
projeto do clube de patologia hepática da <strong>Sociedade</strong> brasileira de<br />
Patologia aprovado pela <strong>Sociedade</strong> <strong>Brasileira</strong> de Hepatologia.<br />
GED 2000;19:137-40.<br />
14. Giannini E., Testa R. Noninvasive diagnosis <strong>of</strong> fibrosis: the truth<br />
is rarely pure and never simple. Hepatology 2003;38:1312-13;<br />
author reply 1313.<br />
15. Holund B., Poulsen H., Schlichting P. Reproducibility <strong>of</strong> liver<br />
biopsy diagnosis in relation to the size <strong>of</strong> the specimen. Scand J<br />
Gastroenterol 1980;15:329-35.<br />
16. Hu K.Q., Kyulo N.L., Esrailian E., et al. Overweight and obesity,<br />
hepatic steatosis, and progression <strong>of</strong> chronic hepatitis C: a<br />
retrospective study on a large cohort <strong>of</strong> patients in the United<br />
States. J Hepatol 2004;40:147-54.<br />
17. Hwang S.J., Luo J.C., Chu C.W., et al. Hepatic steatosis in chronic<br />
hepatitis C virus infection: prevalence and clinical correlation.<br />
J Gastroenterol Hepatol 2001;16:190-5.<br />
18. Ishak K., Baptista A., Bianchi L., et al. Histological grading and<br />
staging <strong>of</strong> chronic hepatitis. J Hepatol 1995;22:696-9.<br />
19. Ismail F.W., Hamid S.S. Hepatic steatosis and hepatitis C. J Pak<br />
Med Assoc 2004;54:108-9.<br />
20. Khokhar N., Mushtaq M., Mukhtar A.S., Ilahi F. Steatosis and<br />
chronic hepatitis C virus infection. J Pak Med Assoc<br />
2004;54:110-2.<br />
20a. Feray C., Gigou M., Samuel D., et al. <strong>The</strong> course <strong>of</strong> hepatitis C<br />
virus infection after liver transplantation. Hepatology<br />
1994;20:1137-43.<br />
21. Knodell R.G., Ishak K.G., Black W.C., et al. Formulation and<br />
application <strong>of</strong> a numerical scoring system for assessing<br />
histological activity in asymptomatic chronic active hepatitis.<br />
Hepatology 1981;1:431-5.<br />
22. Kumar D., Farrell G.C., Fung C., George J. Hepatitis C virus<br />
genotype 3 is cytopathic to hepatocytes: Reversal <strong>of</strong> hepatic<br />
steatosis after sustained therapeutic response. Hepatology<br />
2002;36:1266-72.<br />
22a. Gane E. <strong>The</strong> natural history and outcome <strong>of</strong> liver transplantation<br />
in hepatitis C virus-infected recipients. Liver Transpl<br />
2003;9:S28-34.<br />
23. Lebensztejn D.M., Kaczmarski M., Sobaniec-Lotowska M.,<br />
Barwijuk-Machala M. Blind liver biopsy in children-diagnostic<br />
significance and complications in authors’ own material. Med<br />
Sci Monit 2000;6:1155-8.<br />
23a. Gane E.J., Portmann B.C., Naoumov N.V., et al. Long-term<br />
outcome <strong>of</strong> hepatitis C infection after liver transplantation. N<br />
Engl J Med 1996;334:815-20.<br />
24. Lonardo A., Adinolfi L.E., Loria P., et al. Steatosis and hepatitis C<br />
virus: mechanisms and significance for hepatic and extrahepatic<br />
disease. Gastroenterology 2004;126:586-97.<br />
24a. Garcia-Retortillo M., Forns X. Prevention and treatment <strong>of</strong><br />
hepatitis C virus recurrence after liver transplantation. J Hepatol<br />
2004;41:2-10.<br />
25. Lu L.G., Zeng M.D., Wan M.B., et al. Grading and staging <strong>of</strong><br />
hepatic fibrosis, and its relationship with noninvasive diagnostic<br />
parameters. World J Gastroenterol 2003;9:2574-8.<br />
26. Monto A., Alonzo J., Watson J.J., et al. Steatosis in chronic<br />
hepatitis C: relative contributions <strong>of</strong> obesity, diabetes mellitus,<br />
and alcohol. Hepatology 2002;36:729-36.<br />
27. Myers R.P., Benhamou Y., Imbert-Bismut F., et al. Serum<br />
biochemical markers accurately predict liver fibrosis in HIV and<br />
hepatitis C virus co-infected patients. AIDS 2003;17:721-5.<br />
28. Myers R.P., Tainturier M.H., Ratziu V., et al. Prediction <strong>of</strong> liver<br />
histological lesions with biochemical markers in patients with<br />
chronic hepatitis B. J Hepatol 2003;39:222-30.<br />
29. Negro F. Hepatitis C virus and liver steatosis: when fat is not<br />
beautiful. J Hepatol 2004;40:533-5.<br />
30. Patton H.M., Patel K., Behling C., et al. <strong>The</strong> impact <strong>of</strong> steatosis<br />
on disease progression and early and sustained treatment response<br />
in chronic hepatitis C patients. J Hepatol 2004;40:484-90.<br />
31. Ramalho F. Hepatitis C virus infection and liver steatosis. Antiviral<br />
Res 2003;60:125-7.<br />
32. Rubbia-Brandt L., Fabris P., Paganin S., et al. Steatosis affects<br />
chronic hepatitis C progression in a genotype specific way. Gut<br />
2004;53:406-12.<br />
33. Scheuer P.J. Liver biopsy size matters in chronic hepatitis: bigger<br />
is better. Hepatology 2003;38:1356-8.<br />
34. Scheuer P.J. <strong>The</strong> nomenclature <strong>of</strong> chronic hepatitis: time for a<br />
change. J Hepatol 1995;22:112-4.<br />
35. Schlichting P., Holund B., Poulsen H. Liver biopsy in chronic<br />
aggressive hepatitis. Diagnostic reproducibility in relation to<br />
size <strong>of</strong> specimen. Scand J Gastroenterol 1983;18:27-32.<br />
36. Sharma P., Balan V., Hernandez J., Rosati M, Williams J, Rodriguez-<br />
Luna H, Schwartz J, Harrison Eet al. Hepatic steatosis in hepatitis<br />
C virus genotype 3 infection: does it correlate with body mass<br />
index, fibrosis, and HCV risk factors? Dig Dis Sci 2004;49:25-9.<br />
36a. Kaneko J., Sugawara Y., Akamatsu N., et al. Cholestatic hepatitis<br />
due to hepatitis C virus after a living donor liver transplantation.<br />
Hepatogastroenterology 2004;51:243-4.<br />
37. Terjung B., Lemnitzer I., Dumoulin F.L., et al. Bleeding<br />
complications after percutaneous liver biopsy. An analysis <strong>of</strong><br />
risk factors. Digestion 2003;67:138-45.<br />
38. Wai C.T., Greenson J.K., Fontana R.J., et al. A simple noninvasive<br />
index can predict both significant fibrosis and cirrhosis in patients<br />
with chronic hepatitis C. Hepatology 2003;38:518-26.<br />
39. Wawrzynowicz-Syczewska M., Kruszewski T., Boron-Kaczmarska<br />
A. Complications <strong>of</strong> percutaneous liver biopsy. Rom J<br />
Gastroenterol 2002;11:105-7.<br />
40. Wyatt J., Baker H., Prasad P., et al. Steatosis and fibrosis in patients<br />
with chronic hepatitis C. J Clin Pathol 2004;57:402-6.<br />
41. Pessoa M.G., Bzowej N., Berenguer M., et al. Evolution <strong>of</strong> hepatitis<br />
C virus quasispecies in patients with severe cholestatic hepatitis<br />
after liver transplantation. Hepatology 1999;30:1513-20.<br />
42. Troppmann C., Rossaro L., Perez R.V., McVicar J.P. Early, rapidly<br />
progressive cholestatic hepatitis C reinfection and graft loss<br />
after adult living donor liver transplantation. Am J Transplant<br />
2003;3:239-40.<br />
43. Pelletier S.J., Iezzoni J.C., et al. Prediction <strong>of</strong> liver allograft<br />
fibrosis after transplantation for hepatitis C virus:<br />
persistent elevation <strong>of</strong> serum transaminase levels versus<br />
necroinflammatory activity. Liver Transpl 2000;6:44-53.<br />
44. Prieto M., Berenguer M., Rayon J.M., et al. High incidence<br />
<strong>of</strong> allograft cirrhosis in hepatitis C virus genotype 1b<br />
infection following transplantation: relationship with<br />
rejection episodes. Hepatology 1999;29:250-6.<br />
www.bjid.com.br
36 Chronic Hepatitis C – Pathological Anatomy<br />
BJID 2007; 11 Supplement 1 (October)<br />
45. Samuel D., Bizollon T., Feray C., et al. Interferon-alpha 2b plus<br />
ribavirin in patients with chronic hepatitis C after liver<br />
transplantation: a randomized study. Gastroenterology<br />
2003;124:642-50.<br />
46. Testa G., Crippin J.S., Netto G.J., et al. Liver transplantation for<br />
hepatitis C: recurrence and disease progression in 300 patients.<br />
Liver Transpl 2000;6:553-61.<br />
47. Westin J., Nordlinder H., Lagging M., et al. Steatosis accelerates<br />
fibrosis development over time in hepatitis C vírus genotype 3<br />
infected patients. J Hepatol 2002;37:837-42.<br />
48. Boccato S., Pistis R., Noventa F., et al. Fibrosis Progression in initially<br />
mild chronic hepatitis C. J Viral Hepat 2006;13:297-302.<br />
49. Rubbia-Brandt L., Leandro G., Spahr L., et al. Liver steatosis in<br />
chronic hepatitis C: a morphological sign suggesting infection<br />
with HCV genotype 3. Histopathology 2001;39:119-24.<br />
50. Pessione F., Degos F., Marcellin P., et al. Effect <strong>of</strong> alcohol<br />
consumption on serum hepatitis C virus RNA and histological<br />
lesions in chronic hepatitis C. Hepatology 1998;27:1717-22.<br />
51. Leandro G., Mangia A., Hui J., et al. Relationship between steatosis,<br />
inflammation, and fibrosis in chronic hepatitis C: a meta-analysis<br />
<strong>of</strong> individual patient data. Gastroenterology 2006;130:1636-42.<br />
52. Silini E.M., Cavallero A., Dal Bello B., et al. Modelling liver fibrosis<br />
progression in chronic hepatitis C: A study <strong>of</strong> 563 patients with<br />
sequential liver biopsies. J. Hepatol 2006;44(S2):S36-81.<br />
www.bjid.com.br
BJID 2007; 11 Supplement 1 (October) 37<br />
Co-Infection with Hepatitis B Virus and Hepatitis C Virus<br />
Heloísa Pedrosa Mitre and João Silva de Mendonça<br />
<strong>Infectious</strong> <strong>Diseases</strong> Division <strong>of</strong> the Hospital for State Civil Servants; São Paulo, SP, Brazil<br />
<strong>The</strong> hepatitis B virus (HBV) and the hepatitis C virus (HCV)<br />
share common transmission pathways. <strong>The</strong>refore, co-infection<br />
can be expected. <strong>The</strong> World Health Organization estimates<br />
that, worldwide, 170 million people are infected with HCV, and<br />
350 million people are infected with HBV. However, the number<br />
<strong>of</strong> individuals co-infected with both viruses is unknown.<br />
Although various studies have evaluated small numbers<br />
<strong>of</strong> co-infected individuals, the inclusion criteria, parameters<br />
assessed, and study designs are not uniform. In addition,<br />
ethnicity, local epidemiology, and viral genotypes are also<br />
diverse. <strong>The</strong>refore, the conclusions <strong>of</strong> a specific study, in<br />
principle, should not be widespread.<br />
In cases <strong>of</strong> co-infection with HBV and HCV, the replication <strong>of</strong><br />
either virus can be inhibited, just as either virus can be dominant<br />
or the dominance can alternate between the two. It is more common<br />
for HBV to appear to be suppressed by HCV. <strong>The</strong> chronologies<br />
<strong>of</strong> the two infections have an influence on which virus will be<br />
dominant. Molecular biology techniques (to determine levels <strong>of</strong><br />
HCV RNA and HBV DNA) have facilitated the definition <strong>of</strong> the<br />
interaction between the two viruses.<br />
Co-infections can appear in various manners:<br />
a) Simultaneous acute infection with HBV and HCV:<br />
presupposes same source and transmission pathway. <strong>The</strong><br />
number <strong>of</strong> studies is small, but indicates that the interaction<br />
between the two viruses is similar to that which occurs in<br />
chronic infections. <strong>The</strong>re are descriptions <strong>of</strong> cases in which<br />
there is a delay in the identification <strong>of</strong> the Hepatitis B surface<br />
antigen (HBsAg), lower levels <strong>of</strong> alanine aminotransferase<br />
(ALT), and lower HBV antigenemia, which can be attributed<br />
to suppression <strong>of</strong> HBV activity by HCV.<br />
b) Superinfection by one virus, the other virus being<br />
chronically present: it should be suspected above all in<br />
individuals with risk factors, such as the use <strong>of</strong> illicit<br />
intravenous drugs, multi-transfused individuals, and those<br />
living in areas <strong>of</strong> high HBV prevalence.<br />
Superinfection by HCV: infection by HCV in a patient that<br />
is already infected with HBV. This is known in Asian countries,<br />
where the prevalence <strong>of</strong> HBV is high.<br />
<strong>The</strong> viral suppression <strong>of</strong> the HCV may occur, although the<br />
viral suppression <strong>of</strong> the HBV is more frequent, noted by lower<br />
levels <strong>of</strong> HBV DNA and lower DNA polymerase activity, as<br />
well as by the hepatic expression <strong>of</strong> HBsAg and hepatitis B<br />
core antigen (HBcAg), clearance <strong>of</strong> the hepatitis B e antigen<br />
(HBeAg) or even <strong>of</strong> the HBsAg.<br />
<strong>The</strong> HCV core antigen seems to affect the transcription <strong>of</strong><br />
HBV and, as a result, its replication, which is reported to be<br />
more accentuated for the HCV genotype 1.<br />
<strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> 2007;11 (5) Suppl. 1:37-39.<br />
© 2007 by <strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> and Contexto<br />
Publishing. All rights reserved.<br />
After HBV clearance, HCV can persist, resulting in chronic<br />
hepatitis. In addition, there is the possibility <strong>of</strong> evolution to<br />
severe disease, with a risk <strong>of</strong> death.<br />
Superinfection by HBV: infection by HBV in an individual<br />
that is already chronically infected with HCV. <strong>The</strong> HCV RNA<br />
levels are lower, and, in a study conducted in Italy, HCV<br />
clearance was higher in co-infected individuals (71%) than in<br />
mono-infected individuals (14%).<br />
However, the HBV DNA levels can be lower than those <strong>of</strong><br />
mono-infected individuals, indicating HCV interference.<br />
<strong>The</strong>refore, one virus can induce the clearance <strong>of</strong> another.<br />
<strong>The</strong> evolution to severe forms <strong>of</strong> the disease, with<br />
fulminant hepatitis pr<strong>of</strong>iles, has also been described.<br />
c) Asymptomatic infection with HBV: there are reports <strong>of</strong><br />
patients infected with HCV, with low levels <strong>of</strong> HBV DNA,<br />
reactive anti-HBc, however, non-reactive HBsAg, HBeAg,<br />
anti-HBe, and anti-HBs, configuring co-infection with HCV<br />
with asymptomatic HBV.<br />
<strong>The</strong>se individuals evolve with high ALT levels and high<br />
histological activity. <strong>The</strong>re are reports in which biopsies<br />
from such patients were evaluated, and cirrhosis was found<br />
in 33% <strong>of</strong> the cases, compared with 19% for patients<br />
presenting chronic mono-infections.<br />
<strong>The</strong> data suggest that the evolution <strong>of</strong> the disease is more<br />
severe in co-infected individuals.<br />
<strong>The</strong>re are various potential outcomes:<br />
a) Clearance <strong>of</strong> both viruses: negative HBsAg and,<br />
eventually, appearance <strong>of</strong> anti-HBs. <strong>The</strong> anti-HCV remains<br />
reactive. However, both HBV DNA and HCV RNA become<br />
undetectable. This is the best evolution for both viruses.<br />
b) Fulminant hepatitis: several studies indicate that<br />
individuals co-infected with HBV and HCV have a higher<br />
risk <strong>of</strong> evolution to fulminant hepatitis. In a prospective<br />
study involving patients with acute hepatitis C, <strong>of</strong> those<br />
who died, 23% were chronically infected with HBV, whereas<br />
only 2.9% were infected with HBV (OR=10.2).<br />
In a study conducted in France, among 40 patients with<br />
fulminant or sub-fulminant hepatitis, 12.5% presented acute<br />
hepatitis B or C, and 7.5% presented superinfection with<br />
HCV.<br />
c) Chronic hepatitis: <strong>of</strong> all possible events, this is the one<br />
that occurs most frequently and presents treatment<br />
possibilities. Among the chronic cases <strong>of</strong> hepatitis, several<br />
immunological and molecular-biological pr<strong>of</strong>iles can be<br />
identified:<br />
Active HBV and HCV: detectable HBV DNA and HCV RNA<br />
in serum. This situation has higher possibility <strong>of</strong> evolution to<br />
cirrhosis and hepatic decompensation. In these cases,<br />
treatment may be considered, either with interferon (IFN) +<br />
ribavirin (RBV) or IFN + lamivudine (LMV).<br />
www.bjid.com.br
38 HBV/HCV Co-Infection<br />
BJID 2007; 11 Supplement 1 (October)<br />
Inactive HBV and active HCV: with evolution to undetectable<br />
HBV DNA and detectable HCV RNA. If treatment is indicated,<br />
IFN + RBV is the treatment <strong>of</strong> choice.<br />
Active HBV and inactive HCV or previous infection with<br />
HCV: with reactive HBsAg and HBeAg, detectable HBV DNA<br />
and undetectable HCV RNA.<br />
If indicated, therapeutic options may be IFN or IFN + LMV.<br />
Cirrhosis: co-infected individuals have a higher risk <strong>of</strong><br />
evolution to cirrhosis if compared with mono-infected<br />
individuals (44% and 21%, respectively) as well as a higher<br />
risk <strong>of</strong> chronic hepatitis decompensation.<br />
Hepatocellular carcinoma: evidence indicates that the<br />
possibility <strong>of</strong> evolution to hepatocellular carcinoma (HCC) is<br />
higher in co-infected individuals. A prospective study<br />
comprising 290 individuals with cirrhosis concluded that, in<br />
the univariate and multivariate analyses, co-infection with<br />
HBV and HCV is a predictive factor for the development <strong>of</strong><br />
HCC. <strong>The</strong>se conclusions were confirmed in subsequent<br />
studies, in which the incidence <strong>of</strong> HCC in individuals coinfected<br />
with HBV and HCV was 2 and 3.7 cases/100<br />
individuals/year, respectively.<br />
<strong>The</strong> cumulative risk <strong>of</strong> HCC development in 10 years was<br />
45% in co-infected individuals, 16% in individuals monoinfected<br />
with HBV, and 28% in individuals mono-infected with<br />
HCV.<br />
Treatment<br />
<strong>The</strong> treatment guidelines have been defined in monoinfected<br />
individuals, among others, by pr<strong>of</strong>essional associations<br />
<strong>of</strong> liver researchers, such as the Asian-Pacific Association for<br />
the Study <strong>of</strong> the Liver, the European Association for the Study<br />
<strong>of</strong> the Liver, and the American Association for the Study <strong>of</strong><br />
Liver <strong>Diseases</strong>. According to these guidelines, the choice <strong>of</strong><br />
pegylated interferon over conventional interferon was defined<br />
in association with ribavirin in cases <strong>of</strong> chronic infection with<br />
HCV, and, in isolation, in cases <strong>of</strong> chronic infection with HBV,<br />
when the administration <strong>of</strong> antiviral drugs is also considered.<br />
On the other hand, the treatment <strong>of</strong> individuals co-infected<br />
with HBV and HCV is complex due to the interaction between<br />
both viruses, and between both viruses and the host<br />
immunologic system. Standards for these treatments are not<br />
yet available. However, the therapeutic regimen should be<br />
carefully chosen and should be based on serologic markers,<br />
viremia levels, histology, and, above all, definition <strong>of</strong> the<br />
dominant virus.<br />
Individuals with uncompensated cirrhosis should be<br />
referred to facilities specializing in liver transplantation.<br />
Interferon<br />
Since IFN is an immunomodulating drug, with antiviral<br />
and antiproliferative effect, it is effective against HBV and<br />
HCV. It is also the most widely studied therapeutic option.<br />
<strong>The</strong> first study in co-infected individuals, carried out in the<br />
1990s, suggests that higher doses (9 MU 3 times a week) are<br />
more effective for the clearance <strong>of</strong> HBV or HCV.<br />
If suppression <strong>of</strong> one <strong>of</strong> the viruses is achieved, there is<br />
the possibility <strong>of</strong> reactivation <strong>of</strong> the other, since the suppressor<br />
effect <strong>of</strong> the former has been removed. Pegylated IFN, which<br />
is more effective in mono-infected individuals, can have a<br />
similar effect in co-infected individuals.<br />
In the infection with HCV and asymptomatic HBV<br />
infection, the histological changes and activity are typically<br />
pronounced. <strong>The</strong> response to treatment is less favorable and<br />
respondents present recurrence (downregulation?).<br />
IFN + RBV: this is the regimen that performs best in<br />
individuals mono-infected with HCV. <strong>The</strong>re have been various<br />
studies, involving small samples <strong>of</strong> co-infected individuals,<br />
reporting rates <strong>of</strong> sustained biochemical response and<br />
sustained virologic response (SVR) that are comparable to<br />
those <strong>of</strong> mono-infected individuals, especially if HCV is the<br />
dominant virus.<br />
Due to the viral interaction, it is extremely important that<br />
HBV activity is monitored. It is known that at least half <strong>of</strong> the<br />
patients present HBV reactivation at the beginning <strong>of</strong> the<br />
treatment, and that 45% will have ‘flare-ups’. <strong>The</strong>refore, we<br />
should pay attention to HBV, even if HBV DNA is undetectable<br />
at the beginning <strong>of</strong> the treatment. Over the course <strong>of</strong> the<br />
disease, HBV DNA can become undetectable in 10% to 30%<br />
<strong>of</strong> the patients.<br />
IFN + LMV: small studies suggest that the addition <strong>of</strong> LMV<br />
is useful, above all in patients with active HBV. One such study<br />
described eight HBeAg-reactive patients, in whom HBV DNA<br />
and HCV RNA were detected, submitted to a 12-month course<br />
<strong>of</strong> IFN + LMV, followed by an additional six months <strong>of</strong> treatment<br />
with LMV. In approximately one-third <strong>of</strong> the patients, there was<br />
HBV and HBeAg clearance. In half <strong>of</strong> the patients, there was<br />
normalization <strong>of</strong> ALT, HCV clearance, and an SVR.<br />
It would be premature to venture an opinion on what is<br />
the most appropriate regimen, considering that further studies,<br />
involving larger patient samples, are still needed.<br />
Adefovir and entecavir: there have been no studies involving<br />
co-infected individuals. <strong>The</strong>se might be good options in<br />
patients with dominant HBV.<br />
Liver transplantation: little experience with co-infected<br />
individuals.<br />
<strong>The</strong>re are reports <strong>of</strong> higher survival compared with<br />
individuals mono-infected with HBV, with suggestion <strong>of</strong> the<br />
benefit <strong>of</strong> HCV suppression over HBV in immunosuppression<br />
after transplantation.<br />
In order to define the risks and benefits, it is necessary to<br />
await the results <strong>of</strong> further, larger studies.<br />
Triple Co-Infection<br />
a) HBV, HCV, and hepatitis D virus (HDV): only patients<br />
who are already infected with HBV can acquire HDV. <strong>The</strong><br />
triple infection can occur in certain geographic areas where<br />
the prevalence <strong>of</strong> infection with HBV is high.<br />
<strong>The</strong> evolution to severe disease is described, the desired<br />
treatment being that that consists <strong>of</strong> high doses <strong>of</strong> IFN for a<br />
long period and, still, with poor responses.<br />
www.bjid.com.br
BJID 2007; 11 Supplement 1 (October) HBV/HCV Co-Infection<br />
39<br />
<strong>The</strong>re are few relevant studies in the literature, and all <strong>of</strong><br />
those involved small study samples, which precludes the<br />
standardization <strong>of</strong> the procedure in these cases. <strong>The</strong>re are<br />
reports <strong>of</strong> treatment <strong>of</strong> seven patients with achievement <strong>of</strong><br />
sustained biochemical response in two patients, and<br />
worsening with side effects in two other patients.<br />
b) HBV, HCV, and HIV: in these cases, the complexity <strong>of</strong><br />
the HBV/HCV interaction is added to the effect <strong>of</strong> the HIV on<br />
the host immunologic system.<br />
It is known that, in HCV/HIV and HBV/HIV co-infections,<br />
the evolution <strong>of</strong> the hepatic disease is faster and potentially<br />
more severe. In addition, after the introduction <strong>of</strong> the highdose<br />
anti-HIV therapy known as highly active antiretroviral<br />
therapy, the mortality rate for chronic liver diseases has<br />
increased.<br />
<strong>The</strong>re are few studies on the treatment <strong>of</strong> individuals coinfected<br />
with HBV, HCV, and HIV. <strong>The</strong> rate at which an SVR is<br />
achieved has been reported to be 17% with the use <strong>of</strong> IFN,<br />
compared with 25% for IFN + RBV.<br />
It must be borne in mind that, due to the frequent use <strong>of</strong><br />
LMV in the antiretroviral therapy for HIV, HBV resistance to<br />
LMV is high in co-infected individuals.<br />
In one small study, the effect against the dominant virus,<br />
HBV or HCV, did not lead to the reactivation <strong>of</strong> the other,<br />
except in one case involving a patient with a very low CD4<br />
lymphocyte count.<br />
Studies <strong>of</strong> new antiviral drugs that are more effective<br />
against HBV (ten<strong>of</strong>ovir, entecavir, adefovir, etc.) in HBV/<br />
HIV or HBV/HCV/HIV co-infected individuals might inform<br />
therapeutic decisions regarding the complex treatment <strong>of</strong><br />
co-infections involving HBV.<br />
References<br />
1. Chakravarti A., et al. Characteristics <strong>of</strong> dual infection <strong>of</strong> hepatitis B<br />
and C viruses among patients with chronic liver disease: a study<br />
from tertiary care hospital. Trop Gastroenterol 2005;26:183-7.<br />
2. Crockett S.D., et al. Natural story and treatment <strong>of</strong> hepatitis B<br />
virus and hepatitis C virus coinfection. Ann Clin Microbiol<br />
Antimicrob 2005;4:1-12.<br />
3. French A.L., et al. Isolated hepatitis B core antibody is associated<br />
with HIV and ongoind but not resolved hepatitis C virus infection<br />
in a cohort <strong>of</strong> US women. JID 2007;195:1437-41.<br />
4. Liu Z., et al. Hepatitis B virus (HBV) and hepatitis C virus (HCV)<br />
dual infection. Int J Med Sci 2006;3:57-62.<br />
5. Sagnelli E., et al. Virologic and clinical expressions <strong>of</strong> reciprocal<br />
inhibitory effect <strong>of</strong> hepatitis B, C, and Delta viruses in patients<br />
with chronic hepatitis. Hepatology 2000;32:1106-10.<br />
6. Sagnelli E., et al. HBV superinfection in hepatitis C cirus chronic carriers,<br />
viral interaction, and clinical course. Hepatology 2002;36:1285-91.<br />
7. Sagnelli E., et al. Hepatitis C virus superinfection in hepatitis B<br />
virus chronic carriers: a reciprocal viral interaction and a variable<br />
clinical course. J Clin Virol 2006;35:317-20.<br />
8. Soriano V., et al. Treatment <strong>of</strong> chronic hepatitis B or C in HIVinfected<br />
patients with dual viral hepatitis. JID 2007;195:1181-3.<br />
9. Wang Y.M., et al. Suppression <strong>of</strong> hepatitis C virus by hepatitis B<br />
virus in coinfected patients at the National University Hospital<br />
<strong>of</strong> Singapore. J Gastroenterol 1999;34:481-5.<br />
www.bjid.com.br
40 BJID 2007; 11 Supplement 1 (October)<br />
Co-Infection with Hepatitis C Virus and Human T Lymphocyte Virus<br />
Carlos Brites Alves<br />
Federal University <strong>of</strong> Bahia, School <strong>of</strong> Medicine; Salvador, BA, Brazil<br />
Most individuals infected with human T lymphocyte virus<br />
(HTLV) type 1 or 2 will not develop the disease related to this<br />
virus, remaining asymptomatic for the rest <strong>of</strong> their lives. This<br />
fact has important implications for prospective counseling<br />
and evaluation <strong>of</strong> this population. Individuals infected with this<br />
virus, once identified, should be submitted to anamnesis and<br />
complete physical examination (in order to identify early<br />
manifestations <strong>of</strong> the disease and probable forms <strong>of</strong> acquiring<br />
the infection) and should be periodically evaluated every 6-12<br />
months. It is recommended that injection drug users be tested for<br />
other pathogens common to this population, such as the hepatitis<br />
B virus, the hepatitis C virus (HCV), HIV, etc. It is recommended<br />
that partners <strong>of</strong> sexually active individuals be tested for HTLV.<br />
Children <strong>of</strong> women infected with HTLV-1 should be tested.<br />
Follow-up evaluations should include the following<br />
periodic laboratory tests (every 6-12 months): complete blood<br />
workups with platelet counts; parasitological stool<br />
examination (testing for Strongyloides); urine and urine<br />
sediment test (urinary infection). Although the proviral load<br />
<strong>of</strong> HTLV-1 is still under evaluation and has yet to be validated,<br />
some studies recommend annual quantification.<br />
Special Situations<br />
• In asymptomatic cases that present evidence <strong>of</strong> HTLVrelated<br />
systemic disease, such as dermatological<br />
alterations, hyperreflexia, clone or Babinski sign:<br />
• Serum calcium level, immunophenotyping <strong>of</strong> T<br />
lymphocytes (CD3, CD4, CD8, histocompatibility<br />
leukocyte antigen-DR, CD38 and CD56); diffuse<br />
histiocytic lymphoma, creatine phosphokinase, folate<br />
and vitamin B12 levels; free thyroxine 4 and thyroid<br />
stimulating hormone; and study <strong>of</strong> somatosensitive<br />
evoked potentials.<br />
Healthy individuals infected with HTLV-1 should be<br />
counseled regarding the transmission mechanisms <strong>of</strong> the<br />
infection and be reassured that the probability <strong>of</strong> developing<br />
the disease in the future is low. If necessary, they should be<br />
referred for specialized psychological follow-up evaluation.<br />
Currently, there is no indication – based on scientific<br />
evidence – that any certain type <strong>of</strong> specific anti-HTLV-1<br />
pharmacological intervention plays a role in the prophylaxis<br />
<strong>of</strong> HTLV-related diseases. <strong>The</strong>refore, there is no indication for<br />
the use <strong>of</strong> immunomodulatory, immunosuppressant or<br />
antiretroviral drugs in asymptomatic individuals infected with<br />
HTLV (National Ministry <strong>of</strong> Health, guide <strong>of</strong> clinical<br />
management <strong>of</strong> the HTLV-infected patient, 2004).<br />
<strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> 2007;11 (5) Suppl. 1:40-41.<br />
© 2007 by <strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> and Contexto<br />
Publishing. All rights reserved.<br />
HTLV/HCV Co-Infection<br />
Infection with HCV is frequently detected in HTLV-infected<br />
individuals and vice versa, as seen in other commonly<br />
transmitted pathogens.<br />
Co-infection with HTLV-2 and HCV in patients who are<br />
drug users has been reported, principally in cohorts in the<br />
northern hemisphere [1]. A study carried out in Paraná, Brazil<br />
revealed a strong association (OR=22.60; 95% CI: 10.35-49.35)<br />
between these two pathogens, probably reflecting shared<br />
transmission forms [2].<br />
<strong>The</strong> prevalence <strong>of</strong> co-infection also seems to increase in<br />
individuals infected with HIV in Brazil. Segurado et al. [3]<br />
demonstrated that HCV infection was an independent risk<br />
factor for HTLV infection (adjusted OR=6.43, p=0.02).<br />
Interactions Between HCV and HTLV in Co-Infected<br />
Individuals: Potential Clinical Implications<br />
<strong>The</strong>re are few studies on the effects <strong>of</strong> co-infection with HCV<br />
and HTLV. Hisada et al. [4] demonstrated that the co-infection<br />
with HTLV is associated with greater viral load <strong>of</strong> HCV.<br />
In a study conducted in Japan, HCV/HTLV-1 co-infected<br />
individuals were found to be at a higher risk <strong>of</strong> incidental liver<br />
disease (RR = 5.9), hepatocarcinoma and death (RR = 21.9), as<br />
well as for developing diabetes [5]. In addition, co-infected<br />
individuals have been shown to present a higher frequency<br />
<strong>of</strong> anergy to purified protein derivative, although with no<br />
statistical significance, suggesting a differentiated<br />
immunomodulatory effect in this population [6].<br />
A recent study conducted in the state <strong>of</strong> Bahia, Brazil<br />
revealed a high prevalence <strong>of</strong> HTLV/HCV co-infection.<br />
Although it did not evaluate the clinical impact, it showed the<br />
relevance <strong>of</strong> this association.<br />
In practical terms, there is no established recommendation<br />
for the management <strong>of</strong> HCV/HTLV co-infection. Nevertheless,<br />
the analysis what evidence there is suggests that this<br />
association can result in significant modifications in the natural<br />
history <strong>of</strong> HCV, increasing the viral load <strong>of</strong> HCV, as well as<br />
increasing the morbidity and mortality associated with this<br />
infection. <strong>The</strong>refore, the co-infected patient requires special<br />
attention regarding the clinical evolution <strong>of</strong> hepatitis C and<br />
the markers <strong>of</strong> the infection.<br />
In addition to monitoring the parameters related to HTLV<br />
infection, especially the neurologic alterations secondary to<br />
the infection, we should carefully evaluate the stage <strong>of</strong> the<br />
liver disease, and routinely evaluate the viral load <strong>of</strong> HCV.<br />
Attention should be given to potential alterations <strong>of</strong> glucose<br />
metabolism, since there seems to be an increased tendency<br />
toward these problems in the co-infected individual. For coinfected<br />
patients, routine evaluations <strong>of</strong> fasting glycemia, as<br />
well as glucose tolerance tests, could be necessary.<br />
www.bjid.com.br
BJID 2007; 11 Supplement 1 (October) HCV/HTLV Co-Infection<br />
41<br />
References<br />
1. Zunt J.R., Tapia K., Thiede H., et al. HTLV-2 infection in injection<br />
drug users in King County, Washington, Scand J Infect Dis<br />
2006;38(8):654-63.<br />
2. Morimoto H.K., Caterino-De-Araujo A., Morimoto A.A., et al.<br />
Seroprevalence and risk factors for human T cell lymphotropic<br />
virus type 1 and 2 infection in human immunodeficiency virusinfected<br />
patients attending AIDS referral center health units in<br />
Londrina and other communities in Paraná, Brazil (AIDS Res<br />
Hum Retroviruses 2005;21(4):256-62.<br />
3. Segurado A.C., Braga P., Etzel A., Cardoso M.R. Hepatitis C virus<br />
coinfection in a cohort <strong>of</strong> HIV-infected individuals from Santos,<br />
Brazil: seroprevalence and associated factors. AIDS Patient Care<br />
STDS 2004;18(3):135-43.<br />
4. Hisada M., Chatterjee N., Zhang M., et al. Increased<br />
hepatitis C virus load among injection drug users infected<br />
with human immunodeficiency virus and human T<br />
lymphotropic virus type II. J Infect Dis<br />
2003;188(6):891-7.<br />
5. Boschi-Pinto C., Stuver S., Okayama A., et al. A follow-up<br />
study <strong>of</strong> morbidity and mortality associated with hepatitis<br />
C virus infection and its interaction with human T<br />
lymphotropic virus type I in Miyazaki, Japan. J Infect Dis<br />
2000;182(1):379-80.<br />
6. Hisada M., Shima T., Okayama A., et al. Suppression <strong>of</strong> skin<br />
reactivity to purified protein derivative by hepatitis C virus<br />
among HTLV-1 carriers in Japan.J Acquir Immune Defic Syndr<br />
Hum Retrovirol 1998;19(4):421-5.<br />
www.bjid.com.br
42 BJID 2007; 11 Supplement 1 (October)<br />
Basic Guidelines for the Treatment <strong>of</strong> HIV/HVC Co-Infection<br />
Edgard De Bortholi<br />
Emílio Ribas Institute <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong>; São Paulo, SP, Brazil<br />
<strong>The</strong> treatment <strong>of</strong> HIV/HCV co-infection presents many<br />
questions that have not yet been answered or on which there<br />
is no consensus. Since it is a recently introduced issue, the<br />
guidelines in the literature are divergent on some points. <strong>The</strong><br />
still fragmented knowledge and lack <strong>of</strong> long-term worldwide<br />
experience in the treatment <strong>of</strong> such co-infections has forced<br />
referral facilities to constantly update their approaches.<br />
Some guidelines for the management <strong>of</strong> the HIV/HCV coinfected<br />
patient have been proposed, and new<br />
recommendations are particularly necessary:<br />
• Management <strong>of</strong> patients with persistently normal<br />
aminotransferase levels.<br />
• Definition and quantification <strong>of</strong> liver fibrosis: when<br />
and how?<br />
• Predictors <strong>of</strong> the response to anti-HCV therapy in coinfected<br />
patients.<br />
• <strong>The</strong>rapeutic doses <strong>of</strong> pegylated interferon and ribavirin.<br />
• Treatment duration.<br />
• Treatment <strong>of</strong> nonresponsive and recidivist patients.<br />
• Treatment <strong>of</strong> acute infection in HIV-positive patients.<br />
• HIV/HCV/HBV co-infected patients.<br />
• Interaction between antiretroviral drugs and anti-HCV<br />
therapeutics.<br />
• Antiretroviral hepatotoxicity in co-infected patients.<br />
• Antiretroviral drugs and recommended doses in<br />
hepatic insufficiency.<br />
Management <strong>of</strong> Patients with Persistently Normal<br />
Aminotransferase<br />
Establishing the persistence <strong>of</strong> normal aminotransferase<br />
levels in HCV-infected patients is difficult, especially in coinfected<br />
patients. Fluctuations in the levels <strong>of</strong> aspartate<br />
aminotransferase and alanine aminotransferase are common<br />
in this group <strong>of</strong> patients due to several factors, among<br />
which are the use <strong>of</strong> drugs <strong>of</strong> hepatotoxic potential, alcohol<br />
abuse, and infection with other opportunistic agents. In<br />
contrast to mono-infected patients, who present<br />
persistently normal alanine aminotransferase levels (~25%),<br />
co-infected patients present levels <strong>of</strong> 7-9%. However, <strong>of</strong><br />
such patients, 25-40% present advanced liver fibrosis,<br />
which leads to liver cirrhosis.<br />
<strong>The</strong> rapid evolution <strong>of</strong> fibrosis in co-infected patients,<br />
even in those with normal transaminase levels, indicates<br />
treatment, based on patient motivation, duration <strong>of</strong> the disease,<br />
fibrosis stage, and viral load <strong>of</strong> HCV.<br />
<strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> 2007;11 (5) Suppl. 1:42-46.<br />
© 2007 by <strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> and Contexto<br />
Publishing. All rights reserved.<br />
Definition and Quantification <strong>of</strong> Liver Fibrosis: When and<br />
How?<br />
Various studies have demonstrated the rapidity <strong>of</strong> liver<br />
fibrosis progression in HIV/HCV co-infected patients. Such<br />
patients, even those presenting little or no fibrosis, should<br />
undergo histological evaluation at least every two years.<br />
Unfortunately, since it is an invasive procedure, liver<br />
biopsy might present complications resulting from technical<br />
performance. Pathologist reports are <strong>of</strong>ten made difficult by<br />
the small size <strong>of</strong> the liver fragments obtained in the biopsy,<br />
which has repercussions for the indication <strong>of</strong> anti-HCV<br />
therapy.<br />
Despite the disadvantages <strong>of</strong> liver biopsy, it remains the<br />
principal technique for determining the severity <strong>of</strong> hepatic<br />
injury.<br />
Noninvasive procedures to assess the level <strong>of</strong> the liver<br />
fibrosis are currently divided into two categories: imaging<br />
techniques, such as elastometry (FibroScan); and the use <strong>of</strong><br />
biochemical markers (Fibrotest, APRISHASTA, FIB-4, and<br />
Forn Index). <strong>The</strong>se procedures are accurate at discriminating<br />
between the absence <strong>of</strong> fibrosis and advanced fibrosis but<br />
are not very precise at evaluating the intermediate stages <strong>of</strong><br />
the fibrosis. <strong>The</strong>y present good predictive value for advanced<br />
liver fibrosis and cirrhosis.<br />
Biochemical marker determination in co-infected patients<br />
is <strong>of</strong> little utility, given the inflammatory nature <strong>of</strong> the HIV<br />
disease and the fact that, in this population, hepatotoxic drugs<br />
are used. Such drugs interfere with the serum markers <strong>of</strong><br />
fibrosis in various ways: atazanavir elevates bilirubin levels;<br />
non-nucleoside analog reverse transcriptase inhibitors affect<br />
gamma glutamyl-transferase levels; and some protease<br />
inhibitors elevate cholesterol levels.<br />
Due to technical difficulties, complications and the number<br />
<strong>of</strong> times that the degree <strong>of</strong> fibrosis must be determined, liver<br />
biopsy might soon be replaced by FibroScan for the evaluation<br />
<strong>of</strong> co-infected patients, at least in one <strong>of</strong> their follow-up visits.<br />
Predictors <strong>of</strong> the Response to Anti-HCV <strong>The</strong>rapy in Co-<br />
Infected Patients<br />
<strong>The</strong> current trend in the treatment <strong>of</strong> HCV infection is to<br />
individualize the approach.<br />
All HIV/HCV co-infected patients should undergo HCV<br />
genotyping before any therapeutic decision is made.<br />
Since the first attempts at treatment <strong>of</strong> HCV infection in<br />
HIV-positive patients, a small percentage <strong>of</strong> patients presenting<br />
a sustained virological response at the end <strong>of</strong> the treatment<br />
has been demonstrated, especially those with manifested<br />
immunosuppression with low CD4 counts. <strong>The</strong>se patients<br />
present high viral loads <strong>of</strong> HCV, lower CD8 anti-HCV<br />
responses, greater frequency <strong>of</strong> liver steatosis caused by the<br />
www.bjid.com.br
BJID 2007; 11 Supplement 1 (October) Treatment <strong>of</strong> HIV/HCV Co-Infection<br />
43<br />
use <strong>of</strong> alcohol and hepatotoxic drugs (resulting from a lower<br />
kinetic response to HCV treatment), a higher percentage <strong>of</strong><br />
adverse effects, and worse treatment compliance.<br />
In order to achieve an early virological response, it is<br />
necessary to interfere with the natural and adaptive responses,<br />
which are reduced in co-infected patients, inducing a delay in<br />
viral clearance, which translates to a late virological response.<br />
High levels <strong>of</strong> HCV RNA in co-infected patients might also explain<br />
the low rate at which a sustained virological response is achieved.<br />
Approximately 30% <strong>of</strong> co-infected patients do not present<br />
a significant reduction in HCV viremia during the first month<br />
<strong>of</strong> treatment with pegylated interferon and ribavirin.<br />
<strong>The</strong> precise indication for treatment in HIV/HCV coinfected<br />
patients is CD4 counts greater than 350 cells/mm 3 . In<br />
patients with CD4 counts between 200 and 350 cells/mm 3 , the<br />
decision to treat the HCV infection should take other factors<br />
into account, such as the duration <strong>of</strong> the HCV infection, the<br />
severity <strong>of</strong> the liver disease, the degree <strong>of</strong> HIV suppression,<br />
and the classic predictors <strong>of</strong> the response to the HCV<br />
treatment (genotype and viral load).<br />
A sustained virological response can be predicted based<br />
on the HCV RNA serum negativity in week 4 <strong>of</strong> treatment.<br />
However, a reduction <strong>of</strong> less than 2 log IU/mL in the viral load<br />
<strong>of</strong> HCV in week 12 or the presence <strong>of</strong> detectable viremia in<br />
week 24 predicts the absence <strong>of</strong> a virological response, and<br />
the treatment should be discontinued.<br />
Ongoing studies focus on the maintenance <strong>of</strong> the treatment<br />
for 72 weeks in co-infected patients who are nonresponsive<br />
at week 24. Perhaps this, or even a longer time with smaller<br />
and fractionated doses, is the real treatment time for HIVpositive<br />
patients.<br />
Contraindications and Special Populations<br />
<strong>The</strong> patients with hepatic decompensation (ascites,<br />
digestive bleeding, hepatic encephalopathy, etc.) cannot be<br />
treated with interferon due to the high risk <strong>of</strong> developing<br />
serious complications. In these patients, the possibility <strong>of</strong> a<br />
liver transplant should be considered, even though this<br />
possibility is still remote because <strong>of</strong> the inherent difficulties<br />
<strong>of</strong> immunosuppression and HIV infection.<br />
However, the patients with compensated (Child-Pugh class<br />
A or B) cirrhosis can be treated since they are the ones that<br />
benefit most from the treatment.<br />
As to intravenous drug users and chronic alcoholics, the<br />
treatment should be postponed until the habits are controlled,<br />
and such patients should be referred to a detoxification<br />
program.<br />
<strong>The</strong>rapeutic Doses <strong>of</strong> Pegylated Interferon and Ribavirin<br />
To date, the efficacy <strong>of</strong> high doses <strong>of</strong> pegylated interferon<br />
in the treatment <strong>of</strong> HIV/HCV co-infected patients has not been<br />
confirmed, and we should therefore await the results <strong>of</strong> future<br />
investigations.<br />
Ribavirin induces errors in the viral replication cycle, and<br />
this effect is relevant, principally in HIV-positive patients, in whom<br />
the mediated immune response is impaired. Various authors have<br />
demonstrated that the dose <strong>of</strong> ribavirin is directly related to<br />
achieving a sustained virological response. High doses <strong>of</strong> this<br />
drug are fundamental to the maintenance <strong>of</strong> viral suppression,<br />
especially in the first weeks <strong>of</strong> the treatment. <strong>The</strong>refore, the<br />
recommended dose for the treatment <strong>of</strong> HCV is 15 mg/kg/day<br />
(the minimal dose for adjustment is 11 mg/kg/dose).<br />
Treatment Duration<br />
<strong>The</strong> current consensuses recommend that the duration <strong>of</strong><br />
treatment for HIV/HCV co-infected patients be 48 weeks<br />
regardless <strong>of</strong> the genotype. However, values <strong>of</strong> HCV RNA > 2<br />
log IU/mL at week 12 have a negative predictive value similar<br />
to that observed for mono-infected patients. Nevertheless,<br />
recent studies have questioned this simplistic view <strong>of</strong> the<br />
treatment time. When patients infected with genotype 2 or 3<br />
test negative for HCV RNA in week 4 and maintain their<br />
negativity until week 12, the treatment time is reduced to 24<br />
weeks. When patients infected with genotype 1 or 4 are in the<br />
same situation, the duration <strong>of</strong> treatment is extended to 48 weeks.<br />
For the patients who, despite positivity in week 4, present a<br />
drop in HCV RNA > 2 log IU/mL by week 12, the polymerase<br />
chain reaction (PCR) for qualitative HCV should be repeated in<br />
week 12. If the PCR is negative, and the genotype is 2 or 3, the<br />
treatment should continue to week 48. However, if the genotype<br />
is 1 or 4, the treatment should be maintained until week 72.<br />
If the qualitative PCR for HCV is still positive at week 24,<br />
or there is an HCV RNA reduction < 2 log IU/mL in week 12,<br />
the treatment should be discontinued, regardless <strong>of</strong> the<br />
genotype.<br />
Using erythropoietin and filgrastim has been a good<br />
strategy, even in co-infected patients, for the treatment <strong>of</strong><br />
anemia and neutropenia, respectively.<br />
Treatment <strong>of</strong> Nonresponsive and Recidivist Patients<br />
At least to date, the HIV/HCV co-infected patients, in<br />
contrast with mono-infected patients, are not candidates for<br />
liver transplant, due to the disease progression and the<br />
absence <strong>of</strong> a therapeutic response.<br />
A growing number <strong>of</strong> co-infected patients who have<br />
already undergone treatment with standard interferon with or<br />
without ribavirin, especially those with progression <strong>of</strong> the<br />
fibrosis staging, can now be retreated with pegylated interferon<br />
and ribavirin.<br />
For the patients who have already used pegylated<br />
interferon and ribavirin and did not respond to the treatment<br />
or presented recurrence, there is currently no regimen for<br />
infection control.<br />
Despite the absence <strong>of</strong> a virological response in these<br />
patients, 35-43% <strong>of</strong> them present a reduction in the degree <strong>of</strong><br />
liver fibrosis, demonstrating the antifibrotic effect <strong>of</strong><br />
interferon. <strong>The</strong>se data provide a rationale if the maintenance<br />
<strong>of</strong> interferon, even in small doses, for a prolonged time, has<br />
no effect on the progression <strong>of</strong> the fibrosis, even in the patients<br />
in whom HCV has not been eradicated.<br />
www.bjid.com.br
44 Treatment <strong>of</strong> HIV/HCV Co-Infection<br />
BJID 2007; 11 Supplement 1 (October)<br />
New anti-HCV drugs are urgently needed, especially for this<br />
group <strong>of</strong> patients, who depend exclusively on clinical treatment.<br />
Treatment <strong>of</strong> Acute Infection in HIV-Positive Patients<br />
Outbreaks <strong>of</strong> acute HCV infection in homosexuals have<br />
been reported in some European cities. Despite the knowledge<br />
<strong>of</strong> the low transmissibility <strong>of</strong> HCV through sex, sexual practices<br />
that generate traumatic lesions and genital ulcerations have<br />
been associated with the infection.<br />
<strong>The</strong> natural history <strong>of</strong> HCV infection in HIV patients has<br />
demonstrated its evolution to chronicity. <strong>The</strong>refore, early<br />
therapeutic intervention (in the acute phase <strong>of</strong> infection) is<br />
particularly indicated in these cases, although treatment should<br />
not be instituted earlier than 12 weeks after the exposure, due<br />
to the possibility <strong>of</strong> spontaneous viral clearance. However, a<br />
delay in starting treatment might result in a reduction <strong>of</strong> the<br />
therapeutic response.<br />
<strong>The</strong> treatment <strong>of</strong> acute HCV infection in HIV-positive<br />
patients seems to provide a pattern <strong>of</strong> lower virological<br />
response when compared to HIV-negative patients. However,<br />
the viral clearance pattern obtained in HIV-positive patients<br />
in the acute phase is greater than that seen in those presenting<br />
chronic infection.<br />
Acute infection in HIV-positive patients should be treated<br />
with pegylated interferon and ribavirin for 24 weeks.<br />
HIV/HCV/HBV Co-Infected Patients<br />
In HIV-positive patients living in developed countries, the<br />
prevalence <strong>of</strong> multiple viral hepatitis (HBV/VCV; VBV/VDV; VBV/<br />
HCV/HDV) is lower than 3%. However, this is still higher than<br />
that seen in the general population. Patients presenting HBV/<br />
HCV co-infection seem to present reciprocal inhibition <strong>of</strong> viral<br />
replication, with one <strong>of</strong> the viruses being predominant. However,<br />
this predominance might oscillate from one virus to the other.<br />
Nevertheless, in patients with severe immunosuppression,<br />
replication <strong>of</strong> all <strong>of</strong> the viruses might occur simultaneously. In<br />
HIV-positive patients with good immune status, the interference<br />
seems to favor HCV, to the detriment <strong>of</strong> HBV.<br />
<strong>The</strong> progression <strong>of</strong> the liver disease seems to be more<br />
accelerated in HIV-positive patients infected with both HBV<br />
and HCV. In addition, these individuals are more likely to<br />
develop hepatocarcinoma.<br />
Using interferon to treat chronic HDV in HIV-positive<br />
patients is rarely effective.<br />
<strong>The</strong>re is no established consensus as to the approach to<br />
treating multiple viral hepatitis. Few studies have examined<br />
the efficacy and safety <strong>of</strong> the combination <strong>of</strong> pegylated<br />
interferon and ribavirin for treating multiple infections in HIVpositive<br />
patients. When possible, all <strong>of</strong> the viruses involved<br />
in the hepatitis should be treated.<br />
Interaction between Antiretroviral Medications and Anti-<br />
HCV <strong>The</strong>rapy<br />
<strong>The</strong> highly active antiretroviral therapy (HAART) regimen<br />
is associated with increased survival due to the fact that it<br />
controls HIV and slows the progression <strong>of</strong> the hepatic disease.<br />
<strong>The</strong> better prognosis that the HAART regimen confers on HIV/<br />
HCV co-infected patients is probably due to deceleration <strong>of</strong> the<br />
progression <strong>of</strong> hepatic fibrosis. This has principally been<br />
demonstrated in HIV patients treated with protease inhibitors.<br />
Some studies have suggested the early introduction <strong>of</strong><br />
antiretroviral therapy in HIV/HCV co-infected patients,<br />
considering the beginning <strong>of</strong> the HAART regimen in patients<br />
with CD4 counts > 350 cells/mm 3 , particularly in male patients<br />
and in those who acquired HCV at an advanced age, which<br />
would decrease the effects resulting from immune<br />
reconstitution and the slowing <strong>of</strong> the progression <strong>of</strong> HCVinduced<br />
hepatic disease.<br />
<strong>The</strong> principal complication in the treatment <strong>of</strong> HIV-infected<br />
patients is the interaction between ribavirin and some<br />
antiretroviral drugs.<br />
Ribavirin can decrease the concentrations <strong>of</strong> some<br />
nucleoside analog reverse transcriptase inhibitors (NRTIs),<br />
although there seem to be no clinical consequences.<br />
<strong>The</strong> adverse effects <strong>of</strong> the NRTIs have been associated<br />
with HCV co-infection, female gender, obesity, and prolonged<br />
exposure to these drugs. <strong>The</strong> principal NRTI combinations<br />
associated with lower impact on the liver are as follows:<br />
lamivudine+abacavir (3TC/ABC); 3TC+zidovudine (AZT);<br />
3TC+ABC+AZT; and emtricitabine + ten<strong>of</strong>ovir. However,<br />
recent studies have indicated that ribavirin interferes with the<br />
effects <strong>of</strong> ABC, and, therefore, its use in the HAART regimen<br />
for HCV patients should be considered with caution.<br />
<strong>The</strong> greatest toxicity is that resulting from the concomitant<br />
use <strong>of</strong> didanosine and ribavirin, worsening with the addition<br />
<strong>of</strong> stavudine. <strong>The</strong>se combinations increase the possibility <strong>of</strong><br />
mitochondrial toxicity and are potentiated by the presence <strong>of</strong><br />
HIV and HCV. In patients treated with these antiretroviral drugs<br />
combined with ribavirin, lactic acidosis, pancreatitis and<br />
hepatic decompensation have been reported. <strong>The</strong>refore, it is<br />
recommended that replacements for these antiretroviral drugs<br />
be found for patients who will initiate the treatment for HCV.<br />
In addition, AZT should be replaced, when possible, due to<br />
frequent, severe anemia and neutropenia when AZT is<br />
administered together with ribavirin.<br />
It is important to emphasize that the antiretroviral drugs,<br />
as well as the drugs used in the treatment and prophylaxis <strong>of</strong><br />
the various opportunistic infections, are metabolized by the<br />
liver and, therefore, many <strong>of</strong> these metabolites can increase<br />
the risk <strong>of</strong> hepatic lesion.<br />
<strong>The</strong> chart below shows the principal interactions between<br />
the drugs used, facilitating the choice <strong>of</strong> antiretroviral drugs<br />
in the clinical approach to co-infected patients.<br />
<strong>The</strong> combination <strong>of</strong> ritonavir and saquinavir has proven<br />
to be highly hepatotoxic, and its use is not currently<br />
recommended, especially in HIV/HCV co-infected patients<br />
with concomitant tuberculosis, in whom noncompliance with<br />
treatment and, principally, the elevation <strong>of</strong> transaminase levels<br />
result from the discontinuation <strong>of</strong> the treatment with<br />
antituberculosis drugs or the introduction <strong>of</strong> alternative<br />
www.bjid.com.br
BJID 2007; 11 Supplement 1 (October) Treatment <strong>of</strong> HIV/HCV Co-Infection<br />
45<br />
Chart 1. Drug interactions<br />
Antiretroviral drugs Adverse effects <strong>The</strong>rapeutic alternative Interaction with anti-HCV therapy<br />
Zidovudine Anemia and neutropenia Stavudine Potentiates the probability <strong>of</strong> anemia<br />
caused by ribavirin<br />
Didanosine Hepatotoxicity Lamivudine or efavirenz Ribavirin inhibits the<br />
Mitochondrial toxicity<br />
phosphorylation <strong>of</strong> this drug<br />
Stavudine Hepatotoxicity Lamivudine or efavirenz Should not be combined with<br />
Mitochondrial toxicity<br />
didanosine due to potentiation <strong>of</strong><br />
mitochondrial toxicity<br />
Nevirapine Hepatotoxicity Efavirenz Do not combine with didanosine and<br />
stavudine; potentiation <strong>of</strong><br />
mitochondrial toxicity<br />
Ribavirin Hepatotoxicity Tolerated in low doses Increases the probability <strong>of</strong><br />
HCV=hepatitis C virus.<br />
Chart 2. Antiretrovirals and recommended doses in liver failure<br />
when used in combination<br />
with other protease inhibitors<br />
Name Hepatic metabolism Recommendations<br />
intolerance to the antiretroviral<br />
therapy.<br />
NRTIs<br />
Abacavir Yes Mild (A*)=200 mg twice a day / moderate/severe=contraindicated<br />
Didanosine Yes Not recommended<br />
Emtricitabine No No need for dose adjustment -recommended<br />
Lamivudine No No need for dose adjustment -recommended<br />
Stavudine Unknown No need for dose adjustment -recommended<br />
Zalcitabine No No need for dose adjustment -recommended<br />
Zidovudine Yes No need for dose adjustment -recommended<br />
NtRTIs<br />
Ten<strong>of</strong>ovir No No need for dose adjustment -recommended<br />
NNRTIs<br />
Delavirdine Yes Not recommended<br />
Efavirenz Yes Not recommended<br />
Nevirapine Yes Mild (A*)/moderate (B*)=No need for dose adjustment -recommended<br />
Severe (C*)=contraindicated<br />
Protease inhibitors<br />
Atazanavir Yes Mild (A*)=No need for dose adjustment - recommended<br />
Moderate (B*)=300 mg/day. Severe (C*)=contraindicated<br />
Fosamprenavir Yes Mild/moderate=700 mg 2xday<br />
Severe=contraindicated (because the dose cannot be reduced to<br />
lower than 700 mg)<br />
Indinavir Yes Mild/moderate=600 mg 3× day. Severe=not recommended<br />
Nelfinavir Yes Not recommended<br />
Ritonavir Yes Mild/moderate=No need for dose adjustment -recommended<br />
Severe=not recommended<br />
Saquinavir Yes Mild/ moderate=not recommended. Severe=contraindicated<br />
Boosters w/ ritonavir<br />
Atazanavir/ritonavir Yes<br />
Not recommended at some levels <strong>of</strong> hepatic insufficiency because<br />
it has not been adequately studied<br />
Fosamprenavir/ritonavir Yes Not recommended<br />
Lopinavir/ritonavir Yes Not recommended<br />
Saquinavir/ritonavir Yes<br />
Mild/moderate=Not recommended. Severe=contraindicated<br />
Tipranavir/ritonavir Yes<br />
Mild=No need for dose adjustment - recommended<br />
Moderate/severe=contraindicated<br />
Fusion inhibitors<br />
Enfuvirtide Unknown Not recommended<br />
*Child-Pugh class. NRTIs=nucleoside analog reverse transcriptase inhibitors; NtRTIs=nucleotide analog reverse transcriptase inhibitors;<br />
NNRTIs=non-nucleoside analog reverse transcriptase inhibitors.<br />
www.bjid.com.br
46 Treatment <strong>of</strong> HIV/HCV Co-Infection<br />
BJID 2007; 11 Supplement 1 (October)<br />
regimens that are less efficient in the resolution <strong>of</strong> infection<br />
with Mycobacterium tuberculosis.<br />
<strong>The</strong> data currently available are insufficient to determine the<br />
nature <strong>of</strong> the interaction <strong>of</strong> atazanavir, ten<strong>of</strong>ovir, fosamprenavir,<br />
and tipranavir with the therapeutic regimen in HCV infection.<br />
References<br />
1. Arends J.E., Boucher C.A.B., Hoepelman A.I.M. Hepatitis C virus<br />
and human imunodeficiency virus coinfected: where do we<br />
stand? <strong>Journal</strong> <strong>of</strong> Medicine 2005;63:156-63.<br />
2. Lai, et al. Antiretroviral medication considerations for individuals<br />
coinfected with HIV and hepatitis C virus. AIDS Patient Care<br />
and STDs 2006;20(10):678-92.<br />
3. Rockstroh J.K. Influence <strong>of</strong> viral hepatitis on HIV infection.<br />
<strong>Journal</strong> <strong>of</strong> Hepatology 2006;44:S25-S7.<br />
4. Sancho A.R., Soriano Vicente. Coinfección por el VIH y el virus de<br />
la hepatitis C. http//www.doyma. Acessado em 26/02/2007.<br />
5. Soriano V., et al. Care <strong>of</strong> patients coinfected with HIV and hepatitis<br />
C virus: 2007 updated recomendations from the HCV-HIV<br />
international panel. AIDS 2007,21:1073-89.<br />
6. Thomas L.D. Options for treatment <strong>of</strong> hepatitis C in HIV-infected<br />
persons. <strong>Journal</strong> <strong>of</strong> Hepatology 2006;44:S40-S3.<br />
www.bjid.com.br
BJID 2007; 11 Supplement 1 (October) 47<br />
Basic Aspects <strong>of</strong> the Treatment for Hepatitis C: Mechanisms <strong>of</strong> Action <strong>of</strong> Interferon Alpha and<br />
Ribavirin and the Bases <strong>of</strong> Individualization<br />
Carlos Eduardo de Melo, Evaldo Stanislau Affonso de Araújo and Antonio Alci Barone<br />
Laboratory <strong>of</strong> Hepatitis, LIM 47 DCMIP-HC-FMUSP; São Paulo, SP, Brazil<br />
Pharmacological Characteristics <strong>of</strong> Interferons and<br />
Ribavirin<br />
<strong>The</strong> treatment <strong>of</strong> patients with chronic hepatitis C has<br />
developed considerably in recent years. However, it is still<br />
based on the use <strong>of</strong> interferon alpha (IFN-α) as an antiviral<br />
and immunomodulatory agent against the hepatitis C virus<br />
(HCV).<br />
<strong>The</strong> IFNs are a family <strong>of</strong> proteins that are naturally<br />
produced by the cells <strong>of</strong> the immune system. <strong>The</strong> IFN-á protein<br />
presents antiviral, antiproliferative and immunomodulatory<br />
activity [1-3]. Its mechanism <strong>of</strong> biological action occurs<br />
through the activation <strong>of</strong> specific genes, influencing cell<br />
growth and division, as well as modulating some immune<br />
system activities. <strong>The</strong>refore, IFNs have an indirect antiviral<br />
effect on HCV [2,4].<br />
Commercially, IFN-α is produced by means <strong>of</strong> recombinant<br />
DNA techniques and is available in preparations <strong>of</strong> two distinct<br />
subtypes (IFN-α 2a or IFN-α 2b), which can be combined<br />
with other molecules, such as polyethylene glycolor, more<br />
recently, albumin [5,6]. <strong>The</strong> only difference between IFN-α 2a<br />
and IFN-α 2b is in the amino acid present at position 23 <strong>of</strong> the<br />
protein: IFN-α 2a has a lysine at that position, whereas IFN-α<br />
2b has an arginine [7].<br />
After the binding with its specific receptor (IFNAR) on<br />
the surface <strong>of</strong> the target cells, IFN-α activates an intracellular<br />
signaling cascade, which takes the induction <strong>of</strong> IFN-stimulated<br />
genes (ISGs), establishing a non-virus-specific antiviral state<br />
inside the cell [3,7]. <strong>The</strong> principal signaling mechanism used<br />
by IFN-α is the so-called Janus kinase/signal transducers and<br />
activators <strong>of</strong> transcription (Jak/STAT) pathway [3]. <strong>The</strong>refore,<br />
two cytoplasmatic proteins with the activity <strong>of</strong> tyrosine kinase<br />
associated with IFNAR, activated Jak1 and tyrosine kinase 2<br />
(Tyk2), are activated by the dimerization <strong>of</strong> the receptors.<br />
Activated Jak1 and Tyk2 perform the phosphorylation <strong>of</strong><br />
STAT1 and STAT2, respectively. <strong>The</strong> phosphorylated STAT1<br />
and STAT2 bond with the protein p48 forming IFN-stimulated<br />
gene factor 3 (ISGF3), which translocates into the nucleus<br />
and bonds with IFN-stimulated regulatory element in the<br />
sequences which promote a variety <strong>of</strong> genes inducible by<br />
IFN-α including antiviral proteins such as 2’5’-oligoadenylate<br />
synthetase (2’5’OAS), protein kinase RNA, and Mx protein<br />
[1,3,7,8].<br />
<strong>The</strong> absorption <strong>of</strong> IFN-α (2a or 2b) is high (above 80%)<br />
when administrated intramuscularly or subcutaneously. <strong>The</strong><br />
concentration typically peaks at 3-12 h after administration [9].<br />
<strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> 2007;11 (5) Suppl. 1:47-48.<br />
© 2007 by <strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> and Contexto<br />
Publishing. All rights reserved.<br />
<strong>The</strong> metabolism and elimination <strong>of</strong> IFN-α occurs principally<br />
via the kidneys, with a half-life <strong>of</strong> 3-8 h [9].<br />
Pharmacological Characteristics <strong>of</strong> the Pegylated<br />
Interferons<br />
Pegylated IFNs (PEG-IFNs) are produced through the<br />
binding <strong>of</strong> an inert molecule <strong>of</strong> polyethylene glycol to the<br />
recombinant IFN-á, thus reducing the renal clearance, altering<br />
the metabolism and increasing the half-life <strong>of</strong> the IFN molecule,<br />
although maintaining all <strong>of</strong> its immunostimulatory<br />
characteristics [10,11].<br />
<strong>The</strong> two PEG-IFNs currently available are produced with<br />
polyethylene glycol molecules <strong>of</strong> different complexities. PEG-<br />
IFN-α 2b consists <strong>of</strong> the binding <strong>of</strong> IFN-α 2b with a linear PEG<br />
chain, forming a 12-kDa molecule. PEG-IFN-α 2a is formed by<br />
the binding <strong>of</strong> two 20-kDa chains with IFN-α 2a, resulting in a<br />
complex 40-kDa molecule [6].<br />
<strong>The</strong> differences in the chemical structure <strong>of</strong> the two PEG-<br />
IFN-α formulations are associated with significant<br />
differences in the pharmacological characteristics <strong>of</strong> the<br />
two drugs. <strong>The</strong> PEG-IFN-α 2b (12 kDa) is more rapidly<br />
absorbed (with an absorption half-life <strong>of</strong> 4.6 h), presents a<br />
wide volume <strong>of</strong> body distribution (approximately 0.99 L/<br />
kg) and a mean elimination time <strong>of</strong> 40 h. However, PEG-IFNα<br />
2a (40 kDa) is absorbed more slowly (absorption half-life,<br />
50 h), its distribution is restricted to well-vascularized<br />
organs with good perfusion, such as the liver, and it remains<br />
detectable in the serum for one week (approximately 65 h<br />
elimination half-life) [6,12,13].<br />
Pharmacological Characteristics <strong>of</strong> Ribavirin<br />
Ribavirin is a synthetic nucleoside which is structurally<br />
similar to guanosine [14,15]. Ribavirin enters into the<br />
eukaryotic cells rapidly and, after it undergoes intracellular<br />
phosphorylation, shows virustatic activity against a broad<br />
spectrum <strong>of</strong> DNA and RNA viruses [14,15].<br />
<strong>The</strong> exact mechanism <strong>of</strong> the antiviral action <strong>of</strong> ribavirin<br />
has not yet been totally elucidated [1,16]. However, some<br />
studies suggest the following possible mechanisms:<br />
a) direct inhibition <strong>of</strong> HCV replication;<br />
b) inhibition <strong>of</strong> the enzyme inosine monophosphate<br />
dehydrogenase <strong>of</strong> the host;<br />
c) induction <strong>of</strong> mutagenesis in the viral RNA;<br />
d) immunomodulation by the induction <strong>of</strong> a T helper 1<br />
(Th1)-type immune response Ribavirin is rapidly<br />
absorbed (half-life <strong>of</strong> approximately 2 h) and widely<br />
distributed throughout the body after its oral<br />
administration; its metabolization occurs principally<br />
via the kidneys [16].<br />
www.bjid.com.br
48 Treatment for Hepatitis C: Basic Aspects<br />
BJID 2007; 11 Supplement 1 (October)<br />
Treatment with IFN-α has as a success-defining<br />
characteristic, progressively more extensive and vigorous<br />
immune stimulation. <strong>The</strong> more rapid the stimulation is, the<br />
greater are the chances <strong>of</strong> success. <strong>The</strong> study <strong>of</strong> mononuclear<br />
cells ex vivo and in vivo demonstrated that, 3-6 h after the<br />
administration <strong>of</strong> conventional IFN-α, 516 genes were<br />
upregulated, <strong>of</strong> which 88 with actions directly linked to immune<br />
functions [17]; the same phenomenon was observed for PEG-<br />
IFN, also differentiating responders from nonresponders using<br />
the intensity <strong>of</strong> expression in certain IFN-inducible genes<br />
(2’5’OAS, MX1, IRF-7 and TLR-7), greater in the responders<br />
and lesser in the Afro-Americans [18,19].<br />
<strong>The</strong> final pathway <strong>of</strong> the phenomenon triggered in the cell<br />
nucleus is the activation <strong>of</strong> effector cells. An initial activation<br />
<strong>of</strong> the innate immunity (natural killer cells) is supposedly<br />
necessary for the early reduction <strong>of</strong> the viremia – the greater<br />
and the more rapid it is, the more closely it associates with<br />
achieving a sustained virological response (also differentiating<br />
rapid responders from slow responders). Progressively, as <strong>of</strong><br />
week 4 <strong>of</strong> the treatment, the effective immune stimulation induced<br />
by IFN with the respective reduction <strong>of</strong> the viremia would enable<br />
the specific defense mechanisms (CD4+ and CD8+ cells) which,<br />
in turn, would be in charge <strong>of</strong> disposing <strong>of</strong> the residual infected<br />
cells (hepatocytes and extrahepatic cells) [20]. In fact, Pillai et<br />
al. clearly showed that the magnitude and diversity <strong>of</strong> the cellular<br />
response was associated with early and sustained virological<br />
responses [21], in contrast to other authors who only associated<br />
the Th1-type cellular response with the initial viremia [22]. At<br />
any rate, it is clear that patients presenting a rapid and vigorous<br />
initial response have greater chances <strong>of</strong> success. However,<br />
patients presenting a slower response need more long-term<br />
stimulation. <strong>The</strong>rein reside the bases for the individualization<br />
<strong>of</strong> treatment. It is equally clear that this initial virological<br />
response depends on the gene stimulus induced by IFN-α.<br />
Whether or not these phenomena imply differences associated<br />
with the different types <strong>of</strong> IFNs used in clinical practice has yet<br />
to be answered. However, initial evidence was provided by the<br />
analysis <strong>of</strong> the expression <strong>of</strong> mRNA <strong>of</strong> inducible IFN genes in<br />
two groups <strong>of</strong> patients exposed to the two existing types <strong>of</strong><br />
PEG-IFN, suggesting that, despite lower plasma exposure, the<br />
patients who used PEG-IFN-α 2b expressed their genes more<br />
vigorously, emphasizing the relevance <strong>of</strong> the intracellular<br />
environment in the response to HCV treatment [23].<br />
References<br />
1. Feld J.J., Ho<strong>of</strong>nagle J.H. Mechanism <strong>of</strong> action <strong>of</strong> interferon and<br />
ribavirin in treatment <strong>of</strong> hepatitis C. Nature<br />
2005;436(7053):967-72.<br />
2. Peters M. Actions <strong>of</strong> cytokines on the immune response and viral<br />
interactions: an overview. Hepatology 1996,23(4):909-16.<br />
3. Wohnsland A., H<strong>of</strong>mann W.P., Sarrazin C. Viral determinants <strong>of</strong><br />
resistance to treatment in patients with hepatitis C. Clin<br />
Microbiol Rev 2007,20(1):23-38.<br />
4. Souvignet C., Lejeune O., Trepo C. Interferon-based treatment <strong>of</strong><br />
chronic hepatitis C. Biochimie 2007;89(6-7):894-8.<br />
5. Chemmanur A.T., Wu G.Y. Drug evaluation: Albuferon-alpha—an<br />
antiviral interferon-alpha/albumin fusion protein. Curr Opin<br />
Investig Drugs 2006;7(8):750-8.<br />
6. Foster G.R. Review article: pegylated interferons: chemical and clinical<br />
differences. Aliment Pharmacol <strong>The</strong>r 2004;20(8):825-30.<br />
7. Pestka S. <strong>The</strong> human interferon alpha species and receptors.<br />
Biopolymers 2000;55(4):254-87.<br />
8. Pawlotsky J.-M. Mechanisms <strong>of</strong> antiviral treatment efficacy and<br />
failure in chronic hepatitis C. Antiviral Res 2003;59(1):1-11.<br />
9. USP DI® Volume I: Drug Information for the Health Care<br />
Pr<strong>of</strong>essional [database on CD-ROM]. Version 5.1. Greenwood<br />
Village, Colo: Thomson Micromedex.<br />
10. Reddy K.R., Wright T.L., Pockros P.J., et al. Efficacy and safety<br />
<strong>of</strong> pegylated (40-kd) interferon alpha-2a compared with<br />
interferon alpha-2a in noncirrhotic patients with chronic<br />
hepatitis C. Hepatology 2001;33(2):433-8.<br />
11. Strader D.B., Wright T., Thomas D.L., et al. Diagnosis,<br />
management, and treatment <strong>of</strong> hepatitis C. Hepatology<br />
2004,39(4):1147-71.<br />
12. Bailon P., Palleroni A., Schaffer C.A., et al. Rational design <strong>of</strong> a<br />
potent, long-lasting form <strong>of</strong> interferon: a 40 kDa branched<br />
polyethylene glycol-conjugated interferon alpha-2a for the<br />
treatment <strong>of</strong> hepatitis C. Bioconjug Chem 2001;12(2):195-202.<br />
13. Glue P., Fang J.W., Rouzier-Panis R., et al. Pegylated interferonalpha2b:<br />
pharmacokinetics, pharmacodynamics, safety, and<br />
preliminary efficacy data. Hepatitis C Intervention <strong>The</strong>rapy<br />
Group. Clin Pharmacol <strong>The</strong>r 2000;68(5):556-67.<br />
14. Graci J.D., Cameron C.E. Mechanisms <strong>of</strong> action <strong>of</strong> ribavirin against<br />
distinct viruses. Rev Med Virol 2006;16(1):37-48.<br />
15. Leyssen P., De Clercq E., Neyts J. Perspectives for the treatment<br />
<strong>of</strong> infections with Flaviviridae. Clin Microbiol Rev<br />
2000;13(1):67-82.<br />
16. Parker W.B. Metabolism and antiviral activity <strong>of</strong> ribavirin. Virus<br />
Res 2005;107(2):165-71.<br />
17. Ji X., Cheung R., Cooper S., et al. Interferon alfa regulated gene<br />
expression in patients initiating interferon treatment for chronic<br />
hepatitis C. Gastroenterology 2003;37:610-21.<br />
18. Taylor M.W., Tsukahara T., Brodsky L., et al. Changes in gene<br />
expression during pegylated interferon and ribavirin therapy <strong>of</strong><br />
chronic hepatitis C virus distinguish responders from non<br />
responders to antiviral therapy. <strong>Journal</strong> <strong>of</strong> Virology<br />
2007;81(7):3391-3401.<br />
19. He X.-S., Ji X., Hale M.B., et al. Global transcriptional response to<br />
interferon is a determinant <strong>of</strong> HCV treatment outcome and is<br />
modified by race. Hepatology 2006;44:352-9.<br />
20. Tang K.H., Herrmann E., Cooksley H., et al. Relationship between<br />
early HCV kinetics and T-cell reactivity in chronic hepatitis C<br />
genotype 1 during peginterferon and ribavirin therapy. <strong>Journal</strong><br />
<strong>of</strong> Hepatology 2005;43:776-82.<br />
21. Pillai V., Lee W.M., Thiele D.L., et al. Clinical responders to<br />
antiviral therapy <strong>of</strong> chronic HCV infection show elevated<br />
antiviral CD4+ and CD8+ T-cell responses. <strong>Journal</strong> <strong>of</strong> Viral<br />
Hepatitis 2007;14:318-29.<br />
22. Aberle J.H., Perstinger G., Weseslindtner L., et al. CD4+ T cell<br />
responses in patients with chronic hepatitis C undergoing<br />
peginterferon/ribavirin therapy correlate with faster, but not<br />
sustained, viral clearance. <strong>The</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong><br />
2007;195:1315-9.<br />
23. Silva M., Poo J., Wagner F., et al. A randomized trial to compare<br />
the pharmacokinetic, pharmacodynamic, and antiviral effects<br />
<strong>of</strong> peginterferon alfa-2b and peginterferon alfa-2a in patients<br />
with chronic hepatitis C (COMPARE). <strong>Journal</strong> <strong>of</strong> Hepatology<br />
2006;45:204-13.<br />
www.bjid.com.br
BJID 2007; 11 Supplement 1 (October) 49<br />
<strong>The</strong>rapeutic Approach to Acute Hepatitis C<br />
Rodrigo Nogueira Angerami 1 and Fernando Lopes Gonçales Júnior 2<br />
1<br />
Epidemiological Surveillance Unit, Hospital Epidemiology Service, Hospital das Clínicas, State University at Campinas and Campinas<br />
Referral Center for STD/AIDS; 2 Study Group on Hepatitis, <strong>Infectious</strong> <strong>Diseases</strong> Division, Clinical Medicine Department, School <strong>of</strong> Medical<br />
Sciences, State University at Campinas; Campinas, Brazil<br />
It is estimated that 150 to 200 million individuals are currently<br />
infected with the hepatitis C virus (HCV) [1-3], and that, annually,<br />
there are 3 to 4 million new cases <strong>of</strong> infection worldwide [4]. In<br />
view <strong>of</strong> the impossibility <strong>of</strong> immunoprevention [5] - either through<br />
vaccines or the use <strong>of</strong> post-exposure immunoglobulin - and the<br />
risk <strong>of</strong> chronicity in individuals exposed to the disease, which is<br />
estimated to be between 50% and 85% [2,4,6-9,33], the definition<br />
<strong>of</strong> strategies aimed at early detection and treatment <strong>of</strong> infected<br />
individuals, preferably during the acute phase <strong>of</strong> the infection<br />
[2,4], has been widely discussed in recent years.<br />
In individuals presenting symptoms consistent with acute<br />
hepatitis C (AHC), it is known that the possibility <strong>of</strong><br />
spontaneous viral clearance, among various factors, depends<br />
especially on a potent initial cellular immune response<br />
mediated by cytotoxic T lymphocytes - initially by HCVspecific<br />
CD8+ T lymphocytes and, subsequently, CD4+ T<br />
lymphocytes [10-12]. Other factors associated with a higher<br />
rate <strong>of</strong> sustained virological response (SVR) are the specific<br />
characteristics <strong>of</strong> the patients. Individuals who are Asian or<br />
Caucasian, female, young, and HIV-negative, as well as<br />
presenting a rapid drop in HCV RNA levels and presenting<br />
specific human leukocyte antigen class II alleles, together<br />
with the previously mentioned T cytotoxic response, also<br />
respond better to treatment [16,17,33]. Better responses are<br />
also found in cases <strong>of</strong> infections with shorter incubation<br />
period produced by smaller inoculates. In addition, in a<br />
prospective study conducted by Santantoni et al., a higher<br />
rate <strong>of</strong> spontaneous viral clearance was observed in patients<br />
infected with genotype 3 [7].<br />
A diagnosis <strong>of</strong> acute infection with HCV remains a rare<br />
event in clinical practice. In 70-80% <strong>of</strong> infected patients, AHC<br />
is asymptomatic, and 75% are anicteric [4,8,13-15,33].<br />
Individuals with AHC present elevated serum levels <strong>of</strong> alanine<br />
aminotransferase (ALT) and aspartate aminotransferase<br />
(AST), with or without a clinical pr<strong>of</strong>ile <strong>of</strong> acute hepatitis,<br />
detection <strong>of</strong> (previously undetectable) HCV RNA and<br />
seroconversion for anti-HCV antibodies. It is estimated that<br />
infection with HCV accounts for only 20% <strong>of</strong> all diagnosed<br />
cases <strong>of</strong> acute hepatitis [13]. In the United States, there are<br />
40,000 cases <strong>of</strong> AHC annually [12], and only a small<br />
percentage <strong>of</strong> those are clinically diagnosed in this phase.<br />
Considering the high risk <strong>of</strong> developing chronic hepatitis<br />
C and the favorable evidence, in terms <strong>of</strong> therapeutic response,<br />
it is fundamental to improve our capacity to properly detect<br />
and treat cases <strong>of</strong> acute infection with HCV [12].<br />
At-Risk Populations<br />
Currently, it is thought that, in 90% <strong>of</strong> cases <strong>of</strong> infection<br />
with HCV, it is possible to identify the associated risk factors<br />
[14].<br />
<strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> 2007;11 (5) Suppl. 1:49-52.<br />
© 2007 by <strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> and Contexto<br />
Publishing. All rights reserved.<br />
In the last two decades, especially after serologic triage<br />
was adopted as obligatory for blood donors, and due to the<br />
increased accuracy <strong>of</strong> serologic tests, there has been a drastic<br />
reduction in the number <strong>of</strong> new infections with HCV through<br />
blood and blood products. This resulted in significant<br />
changes in the epidemiological pattern <strong>of</strong> the disease [2,16,18].<br />
However, new infections still occur via parenteral route, and,<br />
less frequently, by sexual or vertical transmission. Currently,<br />
the principal groups at risk for infection with HCV are as<br />
follows: health pr<strong>of</strong>essionals exposed through cut or<br />
puncture accidents involving sharp objects contaminated<br />
with infectious material; intravenous drug users; individuals<br />
engaging in sex with HCV-positive partners; patients on<br />
hemodialysis; and patients submitted to various invasive<br />
procedures [4,12,14,18-21].<br />
In the United States, intravenous drug users account for<br />
68% <strong>of</strong> the new cases <strong>of</strong> HCV infection, compared with 18% for<br />
individuals engaging in sex with HCV-positive partners, 4% for<br />
health pr<strong>of</strong>essionals exposed through cut or puncture accidents,<br />
1% for individuals infected through other routes, and 9% for<br />
those in whom the source <strong>of</strong> infection cannot be identified [22].<br />
Currently, it is believed that the risk <strong>of</strong> vertical transmission is<br />
significantly potentialized in cases <strong>of</strong> HIV/HCV co-infection, in<br />
which the rate <strong>of</strong> such transmission can be as high as 17% [37].<br />
Special attention has been given to the occupational risk<br />
<strong>of</strong> infection with HCV in health pr<strong>of</strong>essionals, and the<br />
estimated risk <strong>of</strong> cut or puncture accidents with sharp objects<br />
contaminated with infectious materials ranges from 1% to<br />
2% [5,22].<br />
Although risks, impacts and recommendations are still<br />
controversial, it is estimated that the risk <strong>of</strong> sexual transmission<br />
ranges from 0% to 3% [34,37], increasing especially in specific<br />
situations, such as co-infection with HIV or other sexually<br />
transmitted diseases, and between homosexual partners.<br />
It is also known that the risk <strong>of</strong> HCV infection is higher in<br />
individuals with chronic kidney disease under treatment with<br />
hemodialysis. It is believed that, among such individuals<br />
treated in the United States, the prevalence <strong>of</strong> anti-HCV<br />
reactivity ranges from 15% to 50% [37].<br />
<strong>The</strong> definition <strong>of</strong> protocols for clinical and laboratory<br />
periodic follow-up evaluation in these segments at increased<br />
risk is fundamental in order to improve the detection <strong>of</strong> AHC.<br />
Laboratory Diagnosis<br />
<strong>The</strong> laboratory techniques most commonly used in the<br />
detection <strong>of</strong> anti-HCV antibodies are fundamentally based<br />
on third- and fourth-generation enzyme-linked<br />
immunosorbent assays. Such serologic tests have<br />
demonstrated great specificity (> 99%) and sensitivity (95%-<br />
99%) [38]. However, one <strong>of</strong> the possible limitations in the<br />
diagnosis <strong>of</strong> acute infection with HCV results from the<br />
possibility <strong>of</strong> late seroconversion, occurring at 4 to 10 weeks<br />
after exposure [23]. Regarding detection <strong>of</strong> anti-HCV<br />
www.bjid.com.br
50 <strong>The</strong>rapeutic Approach to Acute Hepatitis C<br />
BJID 2007; 11 Supplement 1 (October)<br />
antibodies, we observe 50% to 70% positivity at symptom<br />
onset; in addition, from postinfection month 3 onward,<br />
antibodies are detected in 90% <strong>of</strong> the cases [38].<br />
However, HCV RNA determination constitutes an<br />
important tool for early detection <strong>of</strong> acute infections, since<br />
HCV is detectable by 1 to 3 weeks after transmission [23,38].<br />
Immediately after HCV RNA detection and concomitantly with<br />
the appearance <strong>of</strong> possible signs and symptoms - 2 to 8 weeks<br />
after infection - it is possible to observe increased ALT levels<br />
[38]. Detection <strong>of</strong> HCV RNA, in the absence <strong>of</strong> anti-HCV<br />
antibodies, strongly suggests acute infection, especially<br />
when subsequent anti-HCV seroconversion is observed. <strong>The</strong><br />
use <strong>of</strong> transcription-mediated amplification (TMA), together<br />
with other available techniques, constitutes an additional<br />
strategy for early detection <strong>of</strong> acute HCV infection [23].<br />
<strong>The</strong>rapeutic Approaches<br />
<strong>The</strong> high rate <strong>of</strong> chronicity observed after infection with<br />
HCV justifies the increasing interest in possible therapeutic<br />
approaches in cases <strong>of</strong> acute infection.<br />
Various approaches have been proposed in literature, all<br />
<strong>of</strong> which aim at preventing the progression to chronic disease.<br />
Nevertheless, to date, the ideal treatment regimen to be<br />
adopted in clinical practice has not been established<br />
[4,6,8,9,14,18,19,24]. Comparing results from different clinical<br />
trials is difficult for the following reasons: acute hepatitis C is<br />
frequently asymptomatic; different criteria are used in case<br />
definition; samples <strong>of</strong> patients are small and heterogeneous;<br />
there are no control groups; different types and doses <strong>of</strong><br />
interferon (IFN) are used; there are different end points, and<br />
follow-up time varies enormously. <strong>The</strong>refore, it is impossible<br />
to define an ideal therapeutic regimen.<br />
When we evaluate the data available in literature, we<br />
observe excellent results in patients treated in the acute phase<br />
<strong>of</strong> the infection, even under monotherapy [15,16]. <strong>The</strong> principal<br />
post-treatment outcome measure is the rate at which patients<br />
achieve an SVR, defined as the absence <strong>of</strong> HCV RNA detected<br />
in serum by qualitative polymerase chain reaction (PCR) at 24<br />
weeks after the end <strong>of</strong> the treatment [25,26]. Among patients<br />
treated in the acute phase <strong>of</strong> the infection, this rate ranges<br />
from 37% to 98% [2,4,8,18,20,24], which is higher than the 54%-<br />
56% observed among patients with chronic hepatitis C, even<br />
among those under combined therapy with pegylated IFN (PEG-<br />
IFN) and ribavirin (RBV) [25,26].<br />
Various trials evaluate the efficacy <strong>of</strong> different regimens<br />
using conventional IFN alpha (IFN α) in the treatment <strong>of</strong><br />
AHC. <strong>The</strong> best results to date were those reported by Jaeckel<br />
et al., whose treatment regimen consisted <strong>of</strong> monotherapy<br />
with IFN α-2b with inducement - 5 million IU/day, s.c., for 4<br />
weeks, followed by 5 million IU, 3 times a week, for 20 weeks<br />
[2]. In that study, the use <strong>of</strong> IFN, even without RBV, made it<br />
possible to obtain high SVR levels. However, the Jaeckel et<br />
al. study raises the following considerations: 68% <strong>of</strong> the<br />
patients included in the study were icteric and therefore<br />
presented a higher probability <strong>of</strong> having self-limited infection,<br />
which could, in part, explain the high SVR rate reported. As<br />
previously mentioned, symptomatic individuals can evolve<br />
to spontaneous viral clearance. In addition, Kamal et al.<br />
observed a higher SVR rate in treated symptomatic individuals<br />
when compared to those asymptomatic individuals treated<br />
with the same therapeutic regimen (96% and 76%,<br />
respectively) [8]. However, Santantonio et al. reported an<br />
SVR rate <strong>of</strong> 94% among individuals who did not present<br />
spontaneous viral clearance by week 12 after acute symptom<br />
onset, when treated with PEG-IFN α-2b, in monotherapy, for<br />
24 weeks [12]. Such finding corroborates other reports<br />
demonstrating that it is safe to adopt the expected conduct<br />
up to week 21 in order to await possible spontaneous viral<br />
clearance [15,16,20,28,36].<br />
In view <strong>of</strong> these facts, it should be noted that, among<br />
individuals acutely infected with HCV, those who are<br />
asymptomatic, especially those who are anicteric and present<br />
normal ALT levels, are more likely to present spontaneous<br />
viral clearance [8,12,14,18,20] - typically between weeks 5<br />
and 12 [27,28]. This viral clearance can occur, in rare situations<br />
(in 10%-50% <strong>of</strong> cases), up to 24 weeks after symptom onset<br />
[8,9,12-15,17,18,21]. Various authors suggest that the treatment<br />
be initiated, at most, 12 to 16 weeks after symptom onset,<br />
avoiding unnecessary exposure to IFN in patients who can<br />
clear HCV spontaneously [4,10,12,18,33].<br />
However, some authors suggest that, in cases <strong>of</strong><br />
asymptomatic acute infection, treatment should be<br />
introduced at the time <strong>of</strong> diagnosis [12].<br />
It should be noted, however, that lower SVR rates have<br />
been observed in cases <strong>of</strong> late treatment. <strong>The</strong>se rates were<br />
initially described by Nomura et al. [18] who, using IFN α (6<br />
million IU, i.m., daily, for four weeks), reported an SVR in 87%<br />
<strong>of</strong> early treated individuals - 8 weeks after detection <strong>of</strong><br />
symptoms - and in 40% <strong>of</strong> patients treated after AHC symptom<br />
onset. This study demonstrated that early introduction <strong>of</strong><br />
treatment enabled a high SVR rate, even in short-term treatment<br />
regimen. More recently, in a study conducted by Kamal et al.,<br />
the SVR rate in individuals treated after week 20 was 76.6%,<br />
whereas, in individuals who started therapy at weeks 8 and 10,<br />
the rates were, respectively, 95.3% and 93.2% [20].<br />
Similarly to what was observed in the treatment <strong>of</strong> chronic<br />
hepatitis C [14,29,30], negative HCV RNA at treatment week 1<br />
was associated with a greater probability <strong>of</strong> achieving an<br />
SVR [31]. In the study carried out by Kamal et al., achieving<br />
a rapid virological response (RVR), defined as HCV RNA<br />
negativity or a ≥ 2 log 10<br />
drop in HCV RNA, by treatment week<br />
4, was found to have positive and negative predictive values<br />
<strong>of</strong> 88% and 98%, respectively, for achieving an SVR. In<br />
another study, involving individuals with AHC treated with<br />
IFN as monotherapy in daily doses for 4 weeks, HCV RNA<br />
negativity in the first week <strong>of</strong> treatment was found to have a<br />
positive predictive value <strong>of</strong> 87% for achieving an SVR [18].<br />
<strong>The</strong> combination <strong>of</strong> PEG-IFN α and RBV is currently<br />
considered the first-line treatment regimen for patients with<br />
chronic hepatitis C, those infected with genotype 2 or 3 and<br />
treated thusly achieving an SVR at a rate <strong>of</strong> 82% [20]. However,<br />
the efficacy, safety, duration and appropriate timing <strong>of</strong> PEG-IFN<br />
treatment in cases <strong>of</strong> AHC have not yet been well established.<br />
A multicenter, prospective, randomized controlled study,<br />
using PEG-IFN α-2b and involving a 48-week post-treatment<br />
follow-up period, reported SVR rates <strong>of</strong> 95.3% and 93.2%,<br />
respectively, in groups <strong>of</strong> patients in which treatment was<br />
initiated at week 8 or week 12 after symptom onset [20]. Studies<br />
that compared treatment results obtained with conventional<br />
IFN to those obtained with PEG-IFN found similarly high<br />
www.bjid.com.br
BJID 2007; 11 Supplement 1 (October) <strong>The</strong>rapeutic Approach to Acute Hepatitis C<br />
51<br />
efficacy in both formulations [4]. Kamal et al., comparing the<br />
efficacy <strong>of</strong> PEG-IFN α, with and without RBV, reported 85%<br />
and 80% SVR rates, respectively [20]. It should be highlighted,<br />
however, that no evidence justifies the routine use <strong>of</strong> the<br />
combination with RBV up to the present moment.<br />
In a multicenter study, patients with acute hepatitis C<br />
received PEG-IFN α-2b (in a dose <strong>of</strong> 1.0-1.5 μg/kg/week)<br />
initiated at the time <strong>of</strong> diagnosis and continued for 12 weeks;<br />
HCV RNA negativity was found in 87% at treatment week 4,<br />
in 91% at the end <strong>of</strong> the treatment (week 12), and in 73% at 24<br />
weeks after the end <strong>of</strong> the treatment [9]. In patients treated<br />
with higher doses <strong>of</strong> PEG-IFN (≥ 1.2 μg/kg/week for 12 weeks),<br />
the same authors reported an 84% SVR rate, comparable to<br />
that found for 24-week regimens [9]. In a prospective,<br />
uncontrolled study, De Rosa et al., using PEG-IFN α-2b (1.0-<br />
1.6 μg/kg/week, during 12 weeks) initiated immediately after<br />
diagnosis, reported an overall rate <strong>of</strong> 74%, although higher<br />
rates were reported when higher doses <strong>of</strong> PEG-IFN were used<br />
(82% when ≥ 1.33 μg/kg/week doses were used) [21].<br />
Similar to what was observed in the treatment for chronic<br />
hepatitis C, compliance to treatment regimen has proven an<br />
important SVR predictive factor in the treatment <strong>of</strong> AHC. This<br />
was demonstrated in a multicenter study, in which a 71% overall<br />
response rate was found, compared with an 89% rate found in<br />
the population with expected compliance to treatment [32].<br />
When SVR rates were evaluated in difficult-to-treat<br />
populations, two studies involving intravenous drug users<br />
reported SVR rates between 72% and 74% [9.21]. In both<br />
situations, regular follow-up and multidisciplinary approach<br />
were used in order to provide adequate compliance to the<br />
proposed treatment regimen.<br />
Kamal et al. reported that HCV genotype is also an element<br />
to be considered as an SVR predictive factor in patients with<br />
AHC. <strong>The</strong>refore, similar to what was reported in cases <strong>of</strong> chronic<br />
hepatitis C, there were associations among genotypes,<br />
treatment time, and SVR rates, in patients with acute hepatitis<br />
C. Distinct SVR rates were found, according to the genotype<br />
involved: 63.8% for genotype 1; and 100% for genotypes 2<br />
and 3. However, when a prolonged (24-week) treatment regimen<br />
was adopted, an SVR rate <strong>of</strong> 88% was observed in patients<br />
infected with genotype 1, higher than the 38% and 60% reported<br />
for 8-week and 12-week regimens, respectively [8].<br />
In addition to genotypes other than genotype 1, relevant<br />
positive predictive factors for achieving an SVR include lower<br />
viral load at the start <strong>of</strong> treatment, early initiation <strong>of</strong> treatment,<br />
and rapid negative HCV RNA after the initiation <strong>of</strong> treatment<br />
[8,18]. Calleri et al. reported that, in addition to achieving an<br />
RVR (by week 4 <strong>of</strong> treatment) and low pre-treatment viremia,<br />
PEG-IFN doses ≥ 1.2 mg/kg/week were positive predictive<br />
factors for achieving an SVR [9].<br />
It is not currently possible to determine the best treatment<br />
regimen for AHC cases. Nor can we establish a minimum<br />
follow-up time to be adopted after the end <strong>of</strong> the treatment.<br />
Wiegand et al., in a prospective study using biochemical,<br />
ultrasound, and virological monitoring (HCV-PCR, TMA and<br />
RNA detection in peripheral mononuclear cells) <strong>of</strong> patients<br />
treated with IFN α, in monotherapy, did not report any<br />
evidence <strong>of</strong> viral recurrence or hepatocytic lesion during the<br />
period studied (mean, 135 weeks; range, 52-224 weeks) [10].<br />
However, as suggested by Alberti et al. [16] in a meta-analysis<br />
and subsequently by other authors, the minimum clinical,<br />
biochemical, and virological follow-up time should not be<br />
less than 48 weeks.<br />
Conclusions<br />
High SVR rates have been reported in patients treated for<br />
acute hepatitis C. In view <strong>of</strong> this, various national and<br />
international consensuses have recommended the treatment<br />
<strong>of</strong> this infection [6,14,19,34,35]. However, there is no<br />
consensus regarding the proper timing <strong>of</strong> the initiation <strong>of</strong><br />
treatment onset duration <strong>of</strong> treatment. <strong>The</strong> best treatment<br />
regimen to be used, as well as the length <strong>of</strong> the post-treatment<br />
follow-up period, is also debatable.<br />
Taking into account the fact that acute hepatitis C is<br />
generally asymptomatic, serologic triage and <strong>of</strong>ten HCV RNA<br />
testing are universally recommended strategies for correct<br />
diagnostic approach <strong>of</strong> intravenous drug users, patients<br />
infected with HIV, patients on hemodialysis, children <strong>of</strong><br />
mothers with HCV, sexual partners <strong>of</strong> HCV-positive<br />
individuals, and health pr<strong>of</strong>essionals having been exposed<br />
to HCV. <strong>The</strong>se segments are currently considered the principal<br />
at-risk groups for acute infection with HCV and, therefore,<br />
potentially considered for treatment.<br />
Diagnostic laboratory tests should include anti-HCV<br />
antibody tests (detectable between post-infection weeks 4 and<br />
10), determination <strong>of</strong> serum levels <strong>of</strong> aminotransferases such<br />
as ALT (high between post-exposure weeks 2 and 5) and<br />
especially detection <strong>of</strong> HCV RNA (detectable by 1 week after<br />
infection). <strong>The</strong> performance <strong>of</strong> liver biopsy for the diagnosis<br />
<strong>of</strong> acute hepatitis C is restricted to situations in which the<br />
clinical pr<strong>of</strong>ile is consistent, although anti-HCV seroconversion<br />
or recent HCV RNA detection are not characteristic.<br />
Individuals with acute hepatitis C are those who present<br />
increased ALT, accompanied or not by clinical pr<strong>of</strong>ile<br />
consistent with acute hepatitis, with detection <strong>of</strong> (previously<br />
undetectable) HCV RNA and seroconversion for anti-HCV.<br />
Taking into account the possibility <strong>of</strong> spontaneous viral<br />
clearance <strong>of</strong> HCV, especially reported in symptomatic<br />
individuals with acute infection, it is recommended that, in<br />
symptomatic individuals, the treatment be initiated from week<br />
12 after symptom onset onward.<br />
In the case <strong>of</strong> asymptomatic patients with acute infection,<br />
treatment should be initiated at the time <strong>of</strong> diagnosis, since<br />
there is less probability <strong>of</strong> spontaneous viral clearance and<br />
due to the fact that late specific therapy is associated with a<br />
lower SVR rate.<br />
Both IFN formulations - conventional IFN and PEG-IFN -<br />
are considered efficacious options for the treatment <strong>of</strong> acute<br />
hepatitis C. However, there has been an increasing tendency<br />
toward using PEG-IFN as a first option, especially in<br />
individuals infected with genotype 1. <strong>The</strong> option <strong>of</strong> high<br />
doses <strong>of</strong> PEG-IFN should be especially considered in<br />
situations in which short-course treatment regimens are used<br />
or in cases <strong>of</strong> infection with genotype 1. When there is an<br />
option for using the conventional IFN treatment regimen,<br />
adopting a daily induction dose, followed by reduction <strong>of</strong><br />
the number <strong>of</strong> doses, up to the end <strong>of</strong> the treatment, seems to<br />
be the most efficacious option. <strong>The</strong>re is as yet no conclusive<br />
evidence that the combination <strong>of</strong> IFN and RBV is superior to<br />
monotherapy with IFN.<br />
www.bjid.com.br
52 <strong>The</strong>rapeutic Approach to Acute Hepatitis C<br />
BJID 2007; 11 Supplement 1 (October)<br />
<strong>The</strong>refore, as observed in studies <strong>of</strong> chronic hepatitis C<br />
with HCV genotype 1, prolonged treatment regimens are<br />
recommended in cases <strong>of</strong> acute hepatitis C with HCV genotype<br />
1, although 24-week treatments can also be considered. In acute<br />
infections with genotype 2 or 3, short-course treatments (e.g.,<br />
12-week courses) can be feasible options.<br />
Prolonged (24-week) treatment or combined therapy with<br />
RBV can be considered for patients who do not present an<br />
early virological response in the first 4 weeks <strong>of</strong> treatment.<br />
Monotherapy regimens, with shorter duration and supervised<br />
administration <strong>of</strong> IFN, especially in groups <strong>of</strong> difficult-totreat<br />
patients, would be desirable.<br />
<strong>The</strong> ideal duration <strong>of</strong> post-treatment evaluation - clinical,<br />
biochemical (ALT levels) and virological (detection <strong>of</strong> HCV<br />
RNA) - has not yet been well established. However, durations<br />
<strong>of</strong> at least 48 weeks should be considered.<br />
References<br />
1. Alter M.J., Kruszon-Moran D., Nainan O.V. et al. <strong>The</strong><br />
prevalence <strong>of</strong> hepatitis C virus infection in the United States,<br />
1988 through 1994. N Engl J Med 1999;341:556-62.<br />
2. Jaeckel E., Cornberg M., Wedemeyer H., et al. Treatment <strong>of</strong><br />
acute hepatitis C with interferon alfa-2b. N Engl J Med<br />
2001;345:1452-7.<br />
3. Kamal S.M., Ismail A., Graham C.S., et al. Pegylated interferon<br />
alpha therapy in acute hepatitis C: relation to hepatitis C<br />
virus-specific T cell response kinetics. Hepatology<br />
2004;39:1721-31.<br />
4. Weigrand K., Stremmel W., Encke J. Treatment <strong>of</strong> hepatitis C<br />
virus infection. World <strong>Journal</strong> <strong>of</strong> Gastroenterology<br />
2007;13(13):1897-1905.<br />
5. Updated US Public Health Service guideline for the management<br />
<strong>of</strong> occupational exposures to HBV, HCV and HIV and<br />
recommendations for postexposure prophylaxis. MMWR<br />
2001;50: RR1.<br />
6. EASL International Consensus Conference on Hepatitis C,<br />
Consensus Statement, 1999. J Hepatol 1999;30:956-61.<br />
7. Santantonio T., Fasano M., Sinisi E., et al. Efficacy <strong>of</strong> a 24-<br />
week course <strong>of</strong> peg-interferon a-2b monotherapy in patients<br />
with acute hepatitis C after failure <strong>of</strong> spontaneous clearance.<br />
J Hepatol 2005;42:329-33.<br />
8. Kamal S.M., Moustafa K.N., Chen J., et al. Duration <strong>of</strong><br />
peginterferon therapy in acute hepatitis C: a randomized<br />
trial. Hepatology 2006;43:923-31.<br />
9. Calleri G., Cariti G., Gaiottino F., et al. A short course <strong>of</strong><br />
pegylated interferon-a in acute hepatitis C. <strong>Journal</strong> <strong>of</strong> Viral<br />
Hepatitis 2007;14:116-21.<br />
10. Wiegand J., Jäckel E., Cornberg M., et al. Long-term followup<br />
after successful interferon therapy <strong>of</strong> acute hepatitis C.<br />
Hepatology 2004;40:98-107.<br />
11. McKiernan S.M., Hagan R., Curry M., et al. Distinct MHC<br />
class I and II alleles are associated with hepatitis C viral<br />
clearance, originating from a single source. Hepatology<br />
2004;108-14.<br />
12. Santantonio T., Medda E., Ferrari C., et al. Risk factors and<br />
outcome among a large patient cohort with communityacquired<br />
acute hepatitis C in Italy. Clin Infect Dis<br />
2006;43:1154-9.<br />
13. Afdhal N.H. <strong>The</strong> natural history <strong>of</strong> hepatitis C. Seminars in<br />
Liver <strong>Diseases</strong> 2004;24,suppl. 2:3-8.<br />
14. Strader D.B., Wright T., Thomas D.L., Seeff L.B. AASLD<br />
Practice Guideline – Diagnosis, Management and Treatment<br />
<strong>of</strong> Hepatitis C. Hepatology 2004;39:1147-71.<br />
15. Heller T., Rehermann B. Acute hepatitis C: a multifaceted<br />
disease. Seminars in Liver <strong>Diseases</strong> 2005;25:7-17.<br />
16. Alberti A., Boccato S., Vario A., Benvegnù L. <strong>The</strong>rapy <strong>of</strong><br />
acute hepatitis. Hepatology 2002;5:S195-S200.<br />
17. Micallef J.M., Kaldor J.M., Dore G.J. Spontaneous viral clearance<br />
following acute hepatitis C infection: a systematic review <strong>of</strong><br />
longitudinal studies. <strong>Journal</strong> <strong>of</strong> Viral Hepatitis, 2006;13:34-41.<br />
18. Nomura H., Sou S., Tanimoto H., et al. Short-term interferonalfa<br />
therapy for acute hepatitis C: a randomized controlled<br />
trial. Hepatology 2004;39:1213-19.<br />
19. Consensus Statements on the Prevention and Management <strong>of</strong><br />
Hepatitis B and Hepatitis C in the Asia-Pacific Region. <strong>Journal</strong><br />
<strong>of</strong> Gastroenterology and Hepatology 2000;15:815-41.<br />
20. Kamal S.M., Fouly A.E., Kamel R.R., et al. Peginterferon alfa-2b<br />
therapy in acute hepatitis C: impact <strong>of</strong> onset <strong>of</strong> therapy on<br />
sustained virologic response. Gastroenterology 2006;130:632-8.<br />
21. De Rosa F.G., Bargiacchi O., Audagnotto S., et al. Twelveweek<br />
treatment <strong>of</strong> acute hepatitis C virus with pegylated<br />
interferon-a-2b in injection drug users. Clinical <strong>Infectious</strong><br />
<strong>Diseases</strong> 2007;45:583-8.<br />
22. Alter M.J. Prevention <strong>of</strong> spread <strong>of</strong> hepatitis C. Hepatology<br />
2002;36:suppl.1:593-8.<br />
23. Mondelli M.U., Cerino A., Cividini A. Acute hepatitis C:<br />
diagnosis and management. J Hepatol 2005;42:S108-S14.<br />
24. Corey K.E., Ross A.S., Wurcel A., et al. Outcomes and treatment<br />
<strong>of</strong> acute hepatitis C virus infection in a United States population.<br />
Clinical Gastroenterology and Hepatology 2006;4:1278-82.<br />
25. Manns M.P., Mc Hutchison J.G., Gordon S.C., et al.<br />
Peginterferon alfa-2b plus ribavirin compared with interferon<br />
alfa-2b plus ribavirin for initial treatment <strong>of</strong> chronic hepatitis<br />
C: a randomized trial. Lancet 2001;358:958-65.<br />
26. Fried M.W., Shiffman M.L., Reddy K.R., et al. Peginterferon<br />
alfa-2a plus ribavirin for chronic hepatitis C virus infection.<br />
N Engl J Med 2002;347:975-82.<br />
27. H<strong>of</strong>er H., Watkins-Riedel T., Janata O., et al. Spontaneous<br />
viral clearance in patients with acute hepatitis C can be<br />
predicted by repeated measurements <strong>of</strong> serum viral load.<br />
Hepatology 2003;37:60-4.<br />
28. Gerlach J.T., Diepolder H.M., Zachoval R., et al. Acute<br />
hepatitis C: high rate <strong>of</strong> both spontaneous and treatmentinduced<br />
viral clearance. Gastroenterology 2003;125:80-8.<br />
29. Davis G.I., Wong J.B., McHutchinson J.G., et al. Early virologic<br />
response to treatment with peginterferon alfa-2b plus<br />
ribavirin in patients with chronic hepatitis C. Hepatology<br />
2003;38:645-52.<br />
30. Firenci P. Predicting the therapeutic response in patients with<br />
chronic hepatitis C: the role <strong>of</strong> viral kinetics studies. J<br />
Antimicrob Chemother 2004;53:15-8.<br />
31. Yamaji K., Hayashi J., Kawakami Y., et al. Hepatitis C viral<br />
RNA status at two weeks <strong>of</strong> therapy predicts the eventual<br />
response. J Clin Gastroenterol 1998;26:193-9.<br />
32. Wiegand J., Baggish P., Boecher W., et al. Early monotherapy with<br />
pegylated interferon alpha-2b for acute hepatitis infection: the<br />
HEP-NET acute-HCV II study. Hepatology 2006;43:250-6.<br />
33. Jaeckel E., Cornberg M., Waldemeyer H., et al. Acute hepatitis<br />
C: to treat or not to treat? Hepatology 2002;35:1538-40.<br />
34. Management <strong>of</strong> hepatitis C: 2002. NIH Consensus<br />
Development Conference, 2002.<br />
35. Angerami R.N., Stucchi R., Gonçales N.S.L., Gonçales Jr. F.L.G.<br />
Hepatite C aguda. II Consenso da <strong>Sociedade</strong> Paulista de<br />
Infectologia para Manuseio e Terapia da Hepatite C 2004:34-6.<br />
36. Zekry A., Patel K., Mc Hutchison J.G. Treatment <strong>of</strong> acute<br />
hepatitis C infection: more pieces <strong>of</strong> the puzzle. J Hepatol<br />
2005;42:293-6.<br />
37. Focaccia R., Galante V.C., Oliveira U.B. Hepatite C –<br />
Epidemiologia. In: Tratado de Hepatites Virais. Ed Roberto<br />
Focaccia, 2ª Edição, Editora Atheneu, 2007:211-16.<br />
38. Consenso da <strong>Sociedade</strong> Paulista de Infectologia para Manuseio<br />
e Terapia da Hepatite C, 2004.<br />
www.bjid.com.br
BJID 2007; 11 Supplement 1 (October) 53<br />
Treatment <strong>of</strong> Chronic Hepatitis C in Treatment-Naïve Patients<br />
Marcelo Simão Ferreira<br />
Federal University <strong>of</strong> Uberlândia School <strong>of</strong> Medicine; Uberlândia, MG, Brazil<br />
After the initial acute phase <strong>of</strong> infection, 50-85% <strong>of</strong> patients<br />
infected with the hepatitis C virus (HCV) develop the chronic<br />
form <strong>of</strong> the disease, which, in 20-30% <strong>of</strong> cases, will evolve to<br />
cirrhosis, liver failure or hepatocellular carcinoma, albeit after<br />
several decades. Once this infection has been established, it<br />
rarely resolves spontaneously. It is known that, during the<br />
chronic phase, the more severe forms <strong>of</strong> this viral infection<br />
can be induced by various c<strong>of</strong>actors: chronic alcoholism; coinfection<br />
with HIV or the hepatitis B virus; liver biopsy-proven<br />
steatosis (or steatohepatitis); and advanced age. <strong>The</strong> main<br />
objective for treating this disease is, therefore, to prevent the<br />
occurrence <strong>of</strong> late complications, by means <strong>of</strong> the eradication<br />
<strong>of</strong> HCV, which can be achieved in just over half <strong>of</strong> the cases<br />
treated with the currently available drugs.<br />
Treatment for Chronic Hepatitis C: Drugs and Treatment<br />
Response Patterns<br />
<strong>The</strong> currently recommended treatment for the chronic<br />
forms <strong>of</strong> hepatitis C is the combination <strong>of</strong> interferon alpha<br />
(IFN-α) and ribavirin. <strong>The</strong> former is a cytosine that is a<br />
component <strong>of</strong> the innate response <strong>of</strong> the human host. Various<br />
genes involved in the immune response are induced/stimulated<br />
by IFN-α, resulting in the activation <strong>of</strong> natural killer cells,<br />
maturation <strong>of</strong> dendritic cells, and proliferation <strong>of</strong> memory cells,<br />
as well as in the prevention <strong>of</strong> apoptosis <strong>of</strong> T cells. <strong>The</strong><br />
hepatocellular injury seen in chronic hepatitis C is not due to<br />
the cytopathic effect <strong>of</strong> HCV. It is immunomediated by natural<br />
killer cells and CD8 T lymphocytes, which are activated by<br />
the action <strong>of</strong> IFN-α.<br />
Ribavirin is an oral nucleoside analog with antiviral effects<br />
against various pathogens (respiratory syncytial virus,<br />
arenavirus, etc.) Although its mechanism <strong>of</strong> action in HCV<br />
remains unclear, it seems that ribavirin causes the virus to<br />
mutate rapidly to forms that are more easily killed, as well as<br />
depleting intracellular adenosine triphosphate, which is<br />
essential for the synthesis <strong>of</strong> viral RNA. Immunomodulatory<br />
effects have been also attributed to this drug.<br />
<strong>The</strong> use <strong>of</strong> IFN-α was approved for hepatitis C treatment<br />
in 1991. At that time, the response to this immunotherapy was<br />
very low (< 20%). However, when the combination <strong>of</strong> ribavirin<br />
and IFN-α began to be used, the proportion <strong>of</strong> patients in<br />
whom a sustained virological response (SVR) was achieved<br />
grew to 40-45%. Even at that time, treatment responses were<br />
confirmed by detecting HCV RNA through molecular tests<br />
such as polymerase chain reaction (PCR). In this context, the<br />
infection is considered eradicated when there is an SVR, which<br />
is defined as the absence <strong>of</strong> serum HCV RNA in a sensitive<br />
test (qualitative PCR) at the end <strong>of</strong> treatment and at six months<br />
<strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> 2007;11 (5) Suppl. 1:53-57.<br />
© 2007 by <strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> and Contexto<br />
Publishing. All rights reserved.<br />
after the end <strong>of</strong> treatment. Patients who achieve an SVR almost<br />
always show a dramatic decrease in HCV RNA levels, defined<br />
as a ≥ 2 log 10<br />
drop or the absence <strong>of</strong> HCV RNA by 12 weeks<br />
after the initiation <strong>of</strong> treatment. This response is designated<br />
the early virological response (EVR) and has been widely used<br />
for treatment follow-up <strong>of</strong> patients infected with HCV<br />
genotype 1. <strong>The</strong> maintenance <strong>of</strong> the undetectable viral load<br />
status at the end <strong>of</strong> the treatment is designated the end-<strong>of</strong>treatment<br />
response (ETR). A patient is considered recidivist<br />
when HCV RNA becomes undetectable during treatment but<br />
becomes positive again after the end <strong>of</strong> the treatment, whereas<br />
a patient is considered a nonresponder when HCV RNA levels<br />
remain stable or decrease < 2 log 10<br />
during treatment with the<br />
combined regimen.<br />
<strong>The</strong> most recent advance in the treatment <strong>of</strong> hepatitis C<br />
has been the development <strong>of</strong> long-acting, pegylated<br />
formulations <strong>of</strong> IFN-α (PEG-IFN-α), produced by the covalent<br />
addition <strong>of</strong> a polyethylene glycol molecule to the IFN-α<br />
molecule. This combination decreased absorption, reduced<br />
the clearance <strong>of</strong> the drug and increased its half-life. With this<br />
increased half-life, PEG-IFN-α can be administered in weekly<br />
doses. Two pegylated formulations have now been approved<br />
for the treatment <strong>of</strong> hepatitis C: PEG-IFN-α 2a (Pegasys-<br />
Roche), with a molecular weight <strong>of</strong> 40 kDa, and PEG-IFN-α 2b<br />
(PEG-INTRON; Schering-Plough), with a molecular weight <strong>of</strong><br />
12 kDa.<br />
Table 1 shows the names and doses <strong>of</strong> the drugs that are<br />
currently used for the treatment <strong>of</strong> chronic hepatitis C.<br />
Viral Kinetics After the Beginning <strong>of</strong> Treatment<br />
<strong>The</strong> most important objective <strong>of</strong> chronic hepatitis C<br />
treatment is HCV eradication. <strong>The</strong> introduction <strong>of</strong> treatment<br />
leads to a biphasic drop in the viral population. <strong>The</strong> speed at<br />
which the quantity <strong>of</strong> HCV drops differs among the treated<br />
patients, and the drops can therefore be classified as rapid<br />
or slow. Patients in whom there are rapid drops at the<br />
beginning <strong>of</strong> treatment more <strong>of</strong>ten achieve an SVR. During<br />
this rapid response phase, which generally occurs within<br />
the first 48 h <strong>of</strong> HCV treatment, the viral load decreases<br />
rapidly, which reflects the IFN-α inhibition <strong>of</strong> replication and<br />
the degradation <strong>of</strong> the drug in the serum. <strong>The</strong> HCV RNA<br />
titers begin to decline 8 to 12 h after the administration <strong>of</strong> the<br />
first IFN-α dose, and the drop ranges from 0.5 to 1.5 log 10<br />
within the first 48 h. <strong>The</strong>reafter, the rate <strong>of</strong> viral load reduction<br />
slows, reflecting the clearance <strong>of</strong> the virus in the infected<br />
cells. <strong>The</strong> complete elimination <strong>of</strong> viral particles requires<br />
combined treatment for several months. During this second<br />
phase, ribavirin seems to play a crucial role in HCV<br />
depuration. Negative HCV viral load during treatment is<br />
generally followed by alanine aminotransferase<br />
normalization and improvement in the necroinflammatory<br />
activity in liver biopsy.<br />
www.bjid.com.br
54 Chronic Hepatitis C in Treatment-Naïve Patients<br />
BJID 2007; 11 Supplement 1 (October)<br />
Table1. Drugs used for the treatment <strong>of</strong> chronic hepatitis C<br />
Drugs<br />
Conventional interferon<br />
Alpha 2a<br />
Alpha 2b<br />
Consensus<br />
Pegylated interferon<br />
Peginterferon α 2a (40 kDa)<br />
Peginterferon α 2b (12 kDa)<br />
Nucleoside analogs<br />
Ribavirin<br />
MU: million units; sc: subcutaneous.<br />
Recommended doses<br />
3 MU sc 3 × week<br />
3 MU sc 3 × week<br />
9 μg sc 3 × week<br />
180 μg SC / week<br />
1.5 μg/kg SC / week<br />
From 1,000 mg (≤ 75 kg) to<br />
1250 mg (> 75 kg), oral, daily<br />
Treatment Protocols<br />
For adults diagnosed with chronic hepatitis C and<br />
presenting detectable serum levels <strong>of</strong> HCV RNA, together<br />
with persistent elevation <strong>of</strong> aminotransferases, histological<br />
evidence <strong>of</strong> progressive hepatic disease, no severe<br />
comorbidities, and no contraindications, treatment is<br />
recommended. All patients should be initially submitted to<br />
viral load quantification (quantitative PCR), HCV genotype<br />
identification (genotypes 1 to 6) and liver biopsy for the<br />
evaluation <strong>of</strong> necroinflammatory activity (intensity) and<br />
fibrosis (staging). <strong>The</strong> two most common methods for<br />
histological evaluation are the METAVIR and Ishak scoring<br />
systems, in which fibrosis is scored as absent (F0), only portal<br />
(F1), portal with septum formation (F2), hepatic with portalcentral<br />
and portal-portal bridging (F3), or cirrhosis (F4).<br />
Treatment is recommended for patients who present a score<br />
<strong>of</strong> at least F2.<br />
It must be borne in mind that liver biopsy is an invasive,<br />
costly, and potentially fatal procedure. For patients presenting<br />
HCV genotype 1, this procedure is useful for therapeutic<br />
decisions when there is no evidence <strong>of</strong> advanced fibrosis<br />
detected by other methods (ultrasound, etc.) However, for<br />
those presenting genotype 2 or 3 and high treatment response<br />
rates, liver biopsy might be unnecessary and might not<br />
influence the therapeutic decision, especially for those<br />
individuals who present persistently high levels <strong>of</strong><br />
aminotransferases.<br />
<strong>The</strong> combination <strong>of</strong> PEG-IFN-α and ribavirin is the<br />
treatment currently recommended for patients with chronic<br />
hepatitis C; its efficacy in achieving an SVR is greater than<br />
that <strong>of</strong> the conventional treatment with IFN-α in isolation or<br />
with the combination <strong>of</strong> IFN-α and ribavirin (56% vs. 16% vs.<br />
42%). As demonstrated in Table 1, subcutaneous PEG-IFN-a<br />
is administered weekly, and oral ribavirin is administered in<br />
two daily doses. <strong>The</strong> recommended dose <strong>of</strong> PEG-IFN-α 2a is<br />
180 μg per week and that <strong>of</strong> PEG-IFN-α 2b is 1.5 μg/kg per<br />
week. Treatment duration and ribavirin dosing vary according<br />
to HCV genotype. Patients presenting HCV genotype 1 must<br />
be treated with either 1,000-mg or 1,250-mg doses <strong>of</strong> ribavirin<br />
(body weight ≤ 75 kg or > 75 kg, respectively) for 48 weeks.<br />
Patients infected with HCV genotype 2 or 3 must receive 800<br />
mg <strong>of</strong> ribavirin daily for 24 weeks. In Brazil, ribavirin capsules<br />
contain 250 mg, and so it is not possible to administer the<br />
recommended 800-mg doses. <strong>The</strong>refore, we believe it is<br />
prudent to prescribe 1000-mg doses for all patients infected<br />
with these genotypes. <strong>The</strong>re is little information on the<br />
treatment against hepatitis C genotypes 4, 5, and 6 (which are<br />
rare in Brazil). It has been recommended that the 48-week<br />
treatment regimen be used in these cases.<br />
In the treatment for infection with HCV genotype 1, the<br />
possibility <strong>of</strong> achieving an SVR is based on the EVR, as<br />
previously defined. Negative results or a significant (≥ 2 log 10<br />
)<br />
drop in HCV viral load by week 12 <strong>of</strong> treatment is indicative <strong>of</strong><br />
an SVR, which appears in 65% <strong>of</strong> the patients treated with<br />
PEG-IFN-α 2a and in 72% <strong>of</strong> those treated with PEG-IFN-α 2b.<br />
However, among those who have not achieved an EVR by<br />
week 12 using either formulation, only 3% achieve an SVR.<br />
<strong>The</strong>refore, the EVR is a strong negative predictor <strong>of</strong> the SVR.<br />
All patients who continue to present positivity (based on<br />
viral loads) at week 12 should be re-assessed at week 24, at<br />
which point a qualitative PCR should be performed. If results<br />
are negative, treatment should be maintained up to week 48. If<br />
is the results are still positive, treatment should be<br />
discontinued. For HCV genotypes 2 and 3, it is not generally<br />
recommended that molecular tests be performed during the<br />
24-week treatment regimen. At the end <strong>of</strong> the combined<br />
treatment, regardless <strong>of</strong> the genotype, a qualitative PCR should<br />
be performed in order to evaluate the ETR.<br />
Chart 1 shows the algorithm for the follow-up <strong>of</strong> patients<br />
with chronic hepatitis C during the treatment with PEG-IFN-α<br />
and ribavirin.<br />
With the current treatment protocols, the rate at which an<br />
SVR is achieved ranges from 54% to 56% after the use <strong>of</strong> the<br />
combination <strong>of</strong> PEG-IFN-α (either formulation) and ribavirin,<br />
which is considerably higher than that seen with older<br />
conventional treatments (Chat 1). Among patients infected<br />
with HCV genotype 2 or 3, the rate at which an SVR is achieved<br />
ranges from 75% to 80%, compared with 40% to 61% among<br />
those infected with HCV genotype 1. Among patients with<br />
HCV genotype 1, the rate at which an SVR is achieved is lower<br />
in blacks (28%) than in Caucasians (52%). Other factors that<br />
influence treatment response, leading to lower cure rates, are<br />
high viral load levels (> 600,000 IU/mL), male gender, high<br />
body mass index, biopsy showing advanced fibrosis and high<br />
iron levels in the hepatic parenchyma. In patients infected<br />
with HCV genotype 2 or 3 and treated with a conventional<br />
regimen involving the combination <strong>of</strong> IFN-α (3 million units 3<br />
times a week) and ribavirin, the rate at which an SVR is achieved<br />
can be similar to that <strong>of</strong> those treated with pegylated<br />
formulations and ribavirin. <strong>The</strong>refore, this regimen is still<br />
recommended in Brazil (directive 863/2002). For such patients,<br />
the use <strong>of</strong> this treatment regimen for six months is less costly<br />
and better tolerated.<br />
Patients with liver cirrhosis have lower chances to eliminate<br />
HCV by means <strong>of</strong> the current treatment than do noncirrhotic<br />
patients. This might be due to the fact that the former present<br />
more advanced age, greater alterations in hepatic<br />
microcirculation (which prevent the adequate interaction<br />
between IFN and infected cells), and lower treatment<br />
www.bjid.com.br
BJID 2007; 11 Supplement 1 (October) Chronic Hepatitis C in Treatment-Naïve Patients<br />
55<br />
Chart 1. Chronic hepatitis treatment strategies<br />
Table 2. Drugs for the treatment <strong>of</strong> chronic hepatitis C<br />
Genotype PEG-IFN-α Ribavirin Duration Treatment evolution SVR<br />
(dose) (dose) (weeks) (%)<br />
1 α 2a: 180 μg/week 1.0 g (< 75 kg) 48 a) No response: ¯HCV RNA at week 12 40-61<br />
(4, 5, 6) α 2b: 1.5 μg/kg/week 1.25 g (> 75 kg) < 2 log 10<br />
IU/mL or HCV RNA ⊕ by week 24<br />
b) Rapid response: treat for 24 weeks if<br />
HCV RNA Θ by week 4 and low initial<br />
viral load (< 600,000 IU/mL)<br />
2, 3 Same as above 1.0 g 24 a) No response: uncommon 75-80<br />
b) Rapid response: treat for 12-16 weeks<br />
if HCV RNA Θ by week 4<br />
PEG-IFN=pegylated interferon; SVR=sustained virological response; HCV=hepatitis C virus.<br />
www.bjid.com.br
56 Chronic Hepatitis C in Treatment-Naïve Patients<br />
BJID 2007; 11 Supplement 1 (October)<br />
compliance rates. <strong>The</strong>se patients should be treated carefully<br />
due to the risk <strong>of</strong> decompensation <strong>of</strong> the disease during<br />
treatment and the worsening <strong>of</strong> pre-existing hematological<br />
parameters (leukopenia and platelet reduction). Patients with<br />
compensated cirrhosis should be treated if they present the<br />
minimum criteria to receive these medications:<br />
a) Total bilirubin < 1.5 g/dL<br />
b) Albumin > 3.4 g/dL<br />
c) Platelets > 75,000/mm 3<br />
d) Hemoglobin > 13 g/dL; neutrophils > 1500/mm 3<br />
e) Creatinine < 1.5 mg/dL<br />
f) Absence <strong>of</strong> ascites, together with hepatic encephalopathy.<br />
In patients with advanced fibrosis and treated with the<br />
PEG-IFN-α/ribavirin combination, the rate at which an SVR is<br />
achieved ranges from 37% to 50%, being higher (70%-75%) in<br />
those presenting HCV genotype 2 or 3, as well as in those<br />
with low viral loads. Side effects, especially thrombocytopenia<br />
and neutropenia, are more common in these patients. At this<br />
stage <strong>of</strong> the disease, cirrhotic patients who achieved an SVR<br />
are not totally protected against the risk <strong>of</strong> developing<br />
hepatocellular carcinoma. Two recent studies have confirmed a<br />
limited reduction in the risk <strong>of</strong> hepatocellular carcinoma in<br />
patients who successfully responded to the combined<br />
regimen; however, some degree <strong>of</strong> risk remains due to the<br />
carcinogenic effect <strong>of</strong> hepatic fibrosis. In addition, the<br />
complications <strong>of</strong> advanced liver disease, in these cases,<br />
occur less frequently, mortality is lower, and there will<br />
obviously be no re-infection <strong>of</strong> the organ after the liver<br />
transplant. In order to prevent re-infection in transplanted<br />
patients, those who are on a liver transplant waiting list and<br />
present decompensated cirrhosis have been treated with<br />
IFN-α or PEG-IFN-α and ribavirin for periods ranging from<br />
three to fourteen months. In these individuals, the rate at<br />
which an SVR is achieved has been low (from 20% to 25%),<br />
and morbidity/mortality due to the treatment have been<br />
considerably high. Bacterial infections, severe cytopenias,<br />
and even mortality have been reported during treatment.<br />
However, in those patients who responded to treatment, with<br />
the elimination <strong>of</strong> HCV, there was improvement in liver<br />
function, fewer episodes <strong>of</strong> decompensation and lower<br />
mortality. Benefits seem to be higher, as expected, for patients<br />
infected with HCV genotype 2 or 3, who traditionally respond<br />
better to the treatment regimen.<br />
Not every patient whose HCV RNA levels become<br />
undetectable during treatment achieves an SVR. In 10% <strong>of</strong><br />
the treated patients, this molecular marker reappears in the<br />
serum during treatment, whereas in 20% <strong>of</strong> the treated patients,<br />
it reappears after the end <strong>of</strong> treatment (recurrence); in this<br />
context, HCV RNA becomes detectable a few weeks after the<br />
interruption <strong>of</strong> treatment, and aminotransferase levels again<br />
increase. Recurrence is more common with short treatment or<br />
when there is a delay in achieving negative HCV RNA results.<br />
In those patients who responded to treatment and achieved<br />
an SVR, long-term follow-up evaluations have shown that<br />
HCV RNA results remain negative in more than 95% <strong>of</strong> these<br />
patients, confirming the cure and the improvement in<br />
histological parameters.<br />
Modifications During the Course <strong>of</strong> Treatment <strong>of</strong> Chronic<br />
Hepatitis C<br />
In patients infected with HCV genotype 1, a 72-week<br />
combined regimen (PEG-IFN-α + ribavirin) may be beneficial<br />
for slow responders, who fail to present negative HCV RNA<br />
results by week 4 or week 12 <strong>of</strong> treatment (EVR). In a randomized<br />
study, 326 patients still presented positive results for the virus<br />
at week 4 <strong>of</strong> treatment. <strong>The</strong>se patients received the<br />
medications for either 48 or 72 weeks. <strong>The</strong> rate at which an<br />
SVR was achieved was significantly higher in the group<br />
receiving the longer-duration regimen (45% vs. 32%; p = 0.01).<br />
In another randomized study, patients who did not achieve an<br />
EVR were submitted to either 48 or 72 weeks <strong>of</strong> treatment. <strong>The</strong><br />
results showed that 29% (31/106) <strong>of</strong> the patients in the 72-<br />
week group achieved an SVR, compared with only 17% (17/<br />
100) <strong>of</strong> those in the 48-week group (p = 0.04). <strong>The</strong>refore,<br />
selected patients who present slow initial response to antiviral<br />
medications can be treated for longer periods.<br />
However, the treatment duration can be shortened if<br />
patients develop a rapid virological response (RVR), defined<br />
as presenting a response by week 4 <strong>of</strong> treatment. Various<br />
studies have demonstrated that negative results in the<br />
qualitative PCR by week 4 <strong>of</strong> treatment have a positive<br />
predictive value for SVR. Studies involving patients infected<br />
with HCV genotype 2 or 3 who achieve an RVR with the use <strong>of</strong><br />
PEG-IFN-α 2b and ribavirin have demonstrated that treatment<br />
can be discontinued at 12 to 16 weeks after the beginning <strong>of</strong><br />
treatment, since these patients presented SVR rates that were<br />
similar to those seen in the control group, which was submitted<br />
to the 24-week regimen. Recurrences were especially more<br />
common among patients infected with HCV genotype 2 and<br />
in those with high viral loads before treatment. In a recent<br />
randomized study, 150 patients infected with HCV genotype 2<br />
were treated with PEG-IFN-α and ribavirin for either 16 or 24<br />
weeks. <strong>The</strong> comparison showed that both groups presented<br />
high SVR rates (94% and 95%, respectively), indicating that<br />
patients infected with HCV genotype 2 can be treated for a<br />
shorter period <strong>of</strong> time. In a similar study, involving patients<br />
infected with HCV genotype 1, good results were<br />
demonstrated using a 24-week course <strong>of</strong> treatment. Patients<br />
achieving an RVR and a low viral load (< 600,000 IU/mL),<br />
treated for this short period <strong>of</strong> time, presented a high cure rate<br />
(89%), confirming the hypothesis that, even in patients<br />
infected with the more difficult to treat genotypes, it is possible<br />
that treatment can be shortened if patients are adequately<br />
selected regarding short-term regimens.<br />
Although further studies are necessary to confirm the<br />
efficacy <strong>of</strong> less prolonged therapies for the treatment <strong>of</strong><br />
chronic hepatitis C, these current studies have already<br />
indicated that it is possible to use this strategy for patients<br />
achieving an RVR, significantly improving treatment<br />
compliance and quality <strong>of</strong> life <strong>of</strong> the patients, as well as<br />
reducing the frequency <strong>of</strong> side effects and increasing the<br />
cost-effectiveness ratio. Table 2 summarizes the current<br />
recommendations for the treatment <strong>of</strong> chronic hepatitis C,<br />
showing the recommended medications and doses, together<br />
with treatment durations and responses.<br />
www.bjid.com.br
BJID 2007; 11 Supplement 1 (October) Chronic Hepatitis C in Treatment-Naïve Patients<br />
57<br />
Contraindications to and Side Effects <strong>of</strong> Treatment<br />
Absolute contraindications to the PEG-IFN-α and ribavirin<br />
treatment include pregnancy, breastfeeding and<br />
hypersensitivity to either drug. Relative contraindications,<br />
due to potential side effects are as follows: decompensated<br />
liver disease (jaundice, ascites, hepatic encephalopathy,<br />
severe coagulopathy, etc.); neuropsychiatric, pulmonary,<br />
cerebrovascular or coronary diseases; severe autoimmune<br />
diseases; malignant neoplasms; convulsions; and history<br />
<strong>of</strong> solid organ transplants. Patients addicted to injection<br />
drugs, as well as chronic alcoholics, should be advised to<br />
abandon the habit (for at least six months) prior to the<br />
beginning <strong>of</strong> the antiviral therapy. Patients diagnosed with<br />
anemia, leukopenia and platelet reduction should be treated<br />
with care, and hematological parameters should be closely<br />
monitored throughout the treatment.<br />
Side effects <strong>of</strong> interferon and ribavirin affect practically<br />
all <strong>of</strong> the patients. Table 3 shows these side effects, which<br />
are organized by their frequency.<br />
<strong>The</strong> most common side effects are fatigue, myalgia,<br />
psychological alterations (depression, anxiety, insomnia, and<br />
irritability) and worsening <strong>of</strong> hematological parameters<br />
(anemia, platelet reduction, and leukopenia). Ribavirin<br />
induces hemolytic anemia, which frequently requires dose<br />
reduction. In addition, ribavirin is teratogenic, which requires<br />
strict contraceptive control during treatment. Only 1% to<br />
2% <strong>of</strong> patients will develop severe side effects, requiring the<br />
interruption <strong>of</strong> one or both medications. Recombinant<br />
erythropoietin (for anemia) and filgrastim (for neutropenia)<br />
should be routinely used for the control <strong>of</strong> treatment-induced<br />
cytopenias. Patients suffering from depression or mood<br />
disorders can use antidepressants or anxiolytics, with<br />
variable success.<br />
References<br />
1. Ho<strong>of</strong>nagle J.H., Seef L.B. Peginterferon and Ribavirin for chronic<br />
hepatitis C. New England <strong>Journal</strong> <strong>of</strong> Medicine 2006;355:2444-<br />
51.<br />
2. Strader D.B., Wright T., Thomas D.L., Seef L.B. Diagnosis,<br />
management and treatment <strong>of</strong> hepatitis C. Hepatology<br />
2004;4:1147-71.<br />
3. Iacobellis A., Siciliano M., Perri F., et al. Peginterferon alfa-2b<br />
and ribavirin in patients with hepatitis C virus and<br />
decompensated cirrhosis: a controlled study. <strong>Journal</strong> <strong>of</strong><br />
Hepatology 2007;46:206-12.<br />
4. Bruno S., Str<strong>of</strong>folini T., Colombo M., et al. Sustained virological<br />
response to Interferon a is associated with improved outcome in<br />
HCV-related cirrhosis: a retrospective study 2007;45:579-87.<br />
5. Schiff E.R. Emerging strategies for pegylated interferon<br />
combination therapy. Gastroenterology & Hepatology<br />
2007;4(1):517-21.<br />
6. Navasa M., Forns X. Antiviral therapy in HCV decompensated<br />
cirrhosis: to treat or not to treat? <strong>Journal</strong> <strong>of</strong> Hepatology<br />
2007;46:185-8.<br />
7. Everson G.T., Hoefs J.C., Seef L.B., et al. Impact <strong>of</strong> disease severity<br />
on outcome <strong>of</strong> antiviral therapy for chronic hepatitis C: lessons<br />
from the HALT-C trial. Hepatology 2006;44:1675-84.<br />
8. Tan J., Lok A.S.F. Update on viral hepatitis: 2006. Current Opinion<br />
in Gastroenterology 2007;263-7.<br />
Table 3. Side effects <strong>of</strong> interferon and ribavirin<br />
Side effects<br />
Interferon α (including PEG-IFN)<br />
Flu symptoms (greater with PEG-IFN-α 2a)<br />
Neutropenia<br />
Thrombocytopenia<br />
Depression, acute psychosis,<br />
suicide attempts<br />
Irritability<br />
Visual disorders<br />
Fatigue, myalgia<br />
Hypothyroidism/hyperthyroidism<br />
Headache<br />
Nausea, vomiting<br />
Itching<br />
Fever, weight loss<br />
Hearing loss<br />
Alopecia<br />
Pulmonary interstitial fibrosis<br />
Angina/myocardial infarction<br />
Bacterial infections (in cirrhotic patients)<br />
PEG-IFN=pegylated interferon.<br />
Ribavirin<br />
Hemolytic anemia<br />
Fatigue<br />
Pruritus<br />
Skin rash<br />
Sinusitis<br />
Fetal malformations<br />
Gout<br />
9. Hadzyiannis S.J., Sette H., Morgan T.R., et al. Peginterferon a 2a<br />
and Ribavirin combination therapy in chronic hepatitis C. Annals<br />
<strong>of</strong> Internal Medicine 2004;140:346-55.<br />
10. Pawlotsky J.-M. Current and future concepts in hepatitis C<br />
therapy. Seminars in Liver Disease 2005;25:72-83.<br />
11. Mangia A., Santoro R., Minerva N., et al. Peginterferon alfa 2b<br />
and Ribavirin for 12 vs 24 weeks in HCV genotype 2 or 3. <strong>The</strong><br />
New England <strong>Journal</strong> <strong>of</strong> Medicine 2005;325:2609-17.<br />
12. Zenzem S., Buti M., Ferenci P., et al. Efficacy <strong>of</strong> 24 weeks treatment<br />
with chronic hepatitis C infected with genotype 1 and low<br />
pretreatment viremia. <strong>Journal</strong> <strong>of</strong> Hepatology 2006;44:97-103.<br />
13. Delgard O., Bjoro K., Hellum K.B., et al. Treatment with pegylated<br />
interferon and ribavirin in HCV infection with genotype 2 or 3<br />
for 14 weeks: a pilot stydy Hepatology 2004;40:1260-5.<br />
14. Manns M., Waldemeyer H., Cornberg M. Treating viral hepatitis C:<br />
efficacy, side effects and complications. Gut 2006;55:1350-9.<br />
15. Davis G.L. Monitoring <strong>of</strong> viral levels during therapy <strong>of</strong> hepatitis<br />
C. Hepatology 2002;36:5145-51.<br />
16. Manns M.P., McHutchison J.G., Gordon S.C., et al. Peginterferon<br />
alfa 2b plus ribavirin for initial treatment <strong>of</strong> chronic hepatitis<br />
C: a randomized trial. Lancet 2001;358:958-65.<br />
17. H<strong>of</strong>mann W.P., Zeuzem S., Sarrazin C. Towards individualized<br />
antiviral therapy <strong>of</strong> patients infected with hepatitis C virus<br />
genotypes 2 and 3. Hepatology Reviews 2006;3:3-10.<br />
18. Abergel A., Hezode C., Leroy V., et al. Peginterferon alpha-2b<br />
plus ribavirin for treatment <strong>of</strong> chronic hepatitis C with severe<br />
fibrosis: a multicentre randomized controlled trial comparing<br />
two doses <strong>of</strong> peginterferon alpha 2b. <strong>Journal</strong> <strong>of</strong> Viral Hepatitis<br />
2006;13:811-20.<br />
19. Hung C.H., Lee C.M., Lu S.N., et al. Long term effect <strong>of</strong> interferon<br />
alpha 2b plus ribavirin therapy on incidence <strong>of</strong> hepatocellular<br />
carcinoma in patients with hepatitis C virus-related cirrhosis.<br />
<strong>Journal</strong> <strong>of</strong> Viral Hepatitis 2006;13:409-14.<br />
20. EASL International Consensus Conference on hepatitis C. Paris,<br />
26-27 February 1999. Consensus statement. <strong>Journal</strong> <strong>of</strong><br />
Hepatology 1999;3151:3-8.<br />
www.bjid.com.br
58 BJID 2007; 11 Supplement 1 (October)<br />
Retreatment <strong>of</strong> Hepatitis C Patients Who Previously Experienced Treatment Failure<br />
Fernando Lopes Gonçales Jr.<br />
Department <strong>of</strong> Viral Hepatitis Studies, State University <strong>of</strong> Campinas (Unicamp); Campinas, SP, Brazil<br />
In its different formulations, interferon (IFN) alpha<br />
combined with ribavirin (RBV) is the best treatment alternative<br />
for patients infected with the hepatitis C virus (HCV) [1]. In<br />
such patients, the objective is to achieve an end-<strong>of</strong>-treatment<br />
virological response – negative serum HCV ribonucleic acid<br />
(RNA) – followed by a sustained virological response (SVR),<br />
which is defined as HCV RNA negativity for six months after<br />
the suspension <strong>of</strong> treatment.<br />
<strong>The</strong> treatment regimens for HCV infection have evolved<br />
from monotherapy with conventional IFN alpha to combined<br />
therapy with IFN and RBV and, more recently, to combined<br />
therapy with pegylated IFN (PEG-IFN alpha-2a or alpha-2b)<br />
and RBV [2,3]. It is known that approximately 60% <strong>of</strong> the<br />
patients infected with HCV genotype 1 and nearly 40% <strong>of</strong><br />
those infected with genotype 3 do not achieve an SVR when<br />
treated with the conventional regimen <strong>of</strong> IFN and RBV [2-7].<br />
<strong>The</strong> availability <strong>of</strong> PEG-IFNs has reduced the percentage <strong>of</strong><br />
patients experiencing treatment failure. In large international<br />
trials involving treatment-naïve patients, regimens that include<br />
the combination <strong>of</strong> PEG-IFN and RBV have produced<br />
significantly higher rates <strong>of</strong> SVR than those observed with<br />
the use <strong>of</strong> the conventional combination <strong>of</strong> IFN and RBV (54-<br />
56% vs. 44-47%) [5-7].<br />
Similar to what occurs in treatment-naïve patients,<br />
retreatment provides the patient with a new chance to achieve<br />
an SVR. Long-term studies have proven that the vast majority<br />
<strong>of</strong> the patients who achieve an SVR usually remain negative<br />
for HCV RNA for a long time [8].<br />
<strong>The</strong> arguments in favor <strong>of</strong> retreating patients would be<br />
the possibility <strong>of</strong> eradicating HCV, reducing fibrosis, and<br />
decreasing the risk <strong>of</strong> evolving to hepatocarcinoma. With<br />
regard to the new antiviral agents, we do not know when they<br />
will be available or whether all patients will be able to wait<br />
several years to initiate retreatment.<br />
It is known that patients who experience relapse after<br />
treatment with conventional IFN, with or without RBV, respond<br />
better to retreatment with PEG-IFN alpha and RBV than do<br />
those presenting no response to treatment with conventional<br />
IFN (with or without RBV). Krawitt et al. observed an SVR rate<br />
<strong>of</strong> 55% in 66 relapsing patients who were retreated with PEG-<br />
IFN alpha-2b (100-150 µg/week) and RBV (1000 mg/day),<br />
compared with only 20% in 116 previous nonresponders<br />
treated with the same regimen [9]. An SVR was observed in<br />
53% <strong>of</strong> the relapsing patients infected with genotype 1,<br />
compared with 59% <strong>of</strong> the relapsing patients infected with<br />
genotypes 2 or 3. <strong>The</strong>re were, therefore, no significant<br />
differences between these groups <strong>of</strong> patients. This was not<br />
<strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> 2007;11 (5) Suppl. 1:58-59.<br />
© 2007 by <strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> and Contexto<br />
Publishing. All rights reserved.<br />
observed in the previous nonresponders receiving retreatment.<br />
Of those, only 17% <strong>of</strong> the individuals infected with genotype<br />
1, in comparison with 57% <strong>of</strong> the individuals infected with<br />
genotypes 2 or 3, achieved an SVR. <strong>The</strong>refore, genotype had<br />
an influence on SVR in the previous nonresponders who<br />
underwent retreatment.<br />
Studies conducted in Brazil and involving nonresponders<br />
to IFN/RBV demonstrated SVR rates resulting from retreatment<br />
with the PEG-IFN alpha-2a + RBV regimen [10], as well as with<br />
the PEG-IFN alpha-2b + RBV regimen [11], that were higher<br />
than those reported in international studies. Of the relapsers<br />
treated, 57% [10] and 62% [11] achieved an SVR. <strong>The</strong>se SVR<br />
rates in relapsers are higher than, for example, the rates <strong>of</strong><br />
41% and 59% obtained, respectively, in Canada (by Sherman<br />
et al.) and in France (by Moucari et al.) [12,13]. In analyzing<br />
the response in relapsers by genotype, the <strong>Brazilian</strong><br />
researchers found that an SVR was achieved in 69-70% <strong>of</strong><br />
those infected with genotype 3, compared with 43-44% <strong>of</strong><br />
those infected with genotype 1 [10,11].<br />
True nonresponders, that is, patients who never presented<br />
viral negativity during or at the end <strong>of</strong> the treatment, are the<br />
most difficult group to retreat. Some authors showed that,<br />
after previous treatment with conventional IFN, with or without<br />
RBV, relapsers have significantly higher SVR when retreated<br />
with PEG-IFN alpha-2b and RBV than do nonresponders to<br />
previous treatment (55% vs. 20%; p
BJID 2007; 11 Supplement 1 (October) Retreatment <strong>of</strong> Hepatitis C Patients<br />
59<br />
IFN alpha-2a in the first 12 weeks, achieved an SVR at a rate<br />
<strong>of</strong> 30-37%, which is practically twice as high as the SVR rate<br />
<strong>of</strong> 18% observed in those treated with normal doses <strong>of</strong> PEG-<br />
IFN alpha-2a [16].<br />
Since nonresponders to initial treatment/relapsers<br />
constitute a very heterogeneous group, it is necessary to<br />
carefully qualify and select the patients who should be<br />
retreated. <strong>The</strong> various factors that might have been<br />
responsible for the lack <strong>of</strong> a response should be modified/<br />
nullified prior to the initiation <strong>of</strong> or even during the new<br />
treatment cycle. Currently, the patients who are considered<br />
the least likely to respond to retreatment are the true<br />
nonresponders, as well as those who are black, infected<br />
with genotype 1, presenting a high viral load, having<br />
advanced liver disease, or presenting intercurrent diseases,<br />
such as obesity, HIV coinfection, and coinfection with<br />
hepatitis B virus.<br />
Those who were previously treated with IFN as<br />
monotherapy or with the combination <strong>of</strong> IFN and RBV are<br />
more likely to achieve an SVR than are the nonresponders<br />
to the combination <strong>of</strong> PEG-INF and RBV. Those who had<br />
relapses during (breakthrough) or after the previous<br />
treatment also fare better than do those who are true<br />
nonresponders. Patients who were noncompliant with the<br />
previous treatment or those who needed to undergo IFN or<br />
RBV dose reduction due to cytopenias or other adverse<br />
effects usually respond better to retreatment than do those<br />
who received full doses. It is clear that the factors<br />
responsible for noncompliance should be corrected. In<br />
addition, medication dose reductions should be adequately<br />
addressed. In nonresponders, erythropoietin and filgrastim<br />
should be used earlier and further dose reductions should<br />
be avoided at all costs. Drug and alcohol users who, due to<br />
their dependence, did not satisfactorily complete all phases<br />
<strong>of</strong> the previous treatment might respond better to<br />
retreatment if these c<strong>of</strong>actors are removed. This also applies<br />
to the patients who did not have adequate social or cultural<br />
support. Obese patients, insulin-resistant patients,<br />
dyslipidemic patients, patients with steatosis, and patients<br />
with liver diseases, such as hemochromatosis, should be<br />
retreated, preferably after the diagnosis and treatment <strong>of</strong><br />
these accompanying conditions have been appropriately<br />
addressed. <strong>The</strong> doses <strong>of</strong> PEG-IFN should be the same as<br />
those used in treatment-naïve patients. We recommend that,<br />
in retreatment, the doses <strong>of</strong> RBV be as high as possible.<br />
Due to the paucity <strong>of</strong> studies <strong>of</strong> large population samples,<br />
the duration <strong>of</strong> retreatment should be 48 weeks for all<br />
genotypes. At the moment, there are no conclusive data in<br />
the literature to support the use <strong>of</strong> higher doses <strong>of</strong> PEG-<br />
IFN and RBV, the use <strong>of</strong> induction doses, or the extension<br />
<strong>of</strong> treatment duration to more than 48 weeks in such<br />
patients. With regard to the week-12 rule, there is strong<br />
evidence that patients who do not present HCV RNA<br />
negativity by that time are much less likely to achieve an SVR,<br />
and that their treatment should therefore be discontinued.<br />
References<br />
1. National Institutes <strong>of</strong> Health Consensus Development Conference<br />
Statement: Management <strong>of</strong> hepatitis C: 2002-June 10-12,<br />
2002. Hepatology 2002;36:S3-20.<br />
2. McHutchison J.G., Gordon S.C., Schiff E.R., et al. Interferon<br />
alfa-2b alone or in combination with ribavirin as initial<br />
treatment for chronic hepatitis C. N Engl J Med<br />
1998;339:1485-92.<br />
3. Poynard T., Marcellin P., Lee S.S., et al. Randomised trial <strong>of</strong><br />
interferon alpha-2b plus ribavirin for 48 weeks or for 24<br />
weeks versus interferon alpha-2b plus placebo for 48 weeks<br />
for treatment <strong>of</strong> chronic infection with hepatitis C virus.<br />
Lancet 1998;352:1426-32.<br />
4. Poynard T., McHutchison J., Goodman Z., et al. Is an “a la<br />
carte” combination interferon alfa-2b plus ribavirin regimen<br />
possible for the first line treatment in patients with chronic<br />
hepatitis C? Hepatology 2000;31:211-8.<br />
5. Fried M.W., Shiffman M.L., Reddy K.R., et al. Peginterferon<br />
alfa-2a plus ribavirin for chronic hepatitis C virus infection.<br />
N Engl J Med. 2002;347:975-82.<br />
6. Manns M.P., McHutchison J.G., Gordon S.C., et al.<br />
Peginterferon alfa-2b plus ribavirin compared with interferon<br />
alfa-2b plus ribavirin for initial treatment <strong>of</strong> chronic hepatitis<br />
C: a randomised trial. Lancet 2001;358:958-65.<br />
7. Hadziyannis S.J., Sette H., Morgan T.R., et al. Peginterferonalpha2a<br />
and ribavirin combination therapy in chronic<br />
hepatitis C: a randomized study <strong>of</strong> treatment duration and<br />
ribavirin dose. Ann Intern Med 2004;140:346-55.<br />
8. Marcellin P., Boyer N., Gervais A., et al. Long-term<br />
histologic improvement and loss <strong>of</strong> detectable intrahepatic<br />
HCVRNA in patients with chronic hepatitis C and sustained<br />
response to interferon-alpha therapy. Ann Int Med<br />
1997;127:875-81.<br />
9. Krawitt E.L., Ashikaga T., Gordon S.R., et al. Peginterferon<br />
alpha-2b and ribavirin for treatment-refractory chronic<br />
hepatitis C. J Hepatol 2005;43:243-9.<br />
10. Parise E., Cheinquer H., Crespo D., et al. Peginterferon alfa-2<br />
a (40 KD) (PEGASYS) plus ribavirin (COPEGUS) in<br />
retreatment <strong>of</strong> chronic hepatitis C patients, nonresponders<br />
and relapsers to previous conventional interferon plus<br />
ribavirin therapy. Braz J Infect Dis 2006;10:11-6.<br />
11. Gonçales F.L. Jr., Vigani A., Gonçales N., et al. Weight–based<br />
combination therapy with peginterferon alpha-2b and<br />
ribavirin for naïve, relapser and non-responder patients with<br />
chronic hepatitis C. Braz J Infect Dis 2006;10:311-6.<br />
12. Sherman M., Yoshida E.M., Deschenes M., et al. Peginterferon<br />
alfa-2a (40KD) plus ribavirin in chronic hepatitis C<br />
patients who failed previous interferon therapy. Gut<br />
2006;55:1631-8.<br />
13. Moucari R., Ripault M.P., Oules V., et al. High predictive value<br />
<strong>of</strong> early viral kinectics in retreatment with peginterferon and<br />
ribavirin <strong>of</strong> chronic hepatitis C patients non-responders to<br />
standard combination therapy. J Hepatol 2007;46:596-604.<br />
14. Shiffman M.L., Di Bisceglie A.M., Lindsay K.L., et al.<br />
Peginterferon alfa-2a and ribavirin in patients with chronic<br />
hepatitis C who have failed prior therapy. Gastroenterology<br />
2004;126:1015-23.<br />
15. Poynard T., Schiff E., Terg R., et al. Sustained virologic<br />
response (SVR) in the EPIC3 trial: week 12 virology predicts<br />
SVR in previous interferon/ribavirin treatment failures<br />
receiving Peg-Intron/Rebetol weight based dosing. J Hepatol<br />
2005;42 (Suppl. 2):40.<br />
16. Diago M. Peginterferon alfa-2a (40kd) (Pegasys®) and<br />
ribavirin (Copegus®) in patients infected with HCV<br />
genotype 1 who failed to respond to interferon and ribavirin:<br />
final results <strong>of</strong> the Spanish high-dose induction pilot trial.<br />
Presented at the 55 th AASLD; October 29-November 2,<br />
2004; Boston, MA.<br />
www.bjid.com.br
60 BJID 2007; 11 Supplement 1 (October)<br />
Maintenance Treatment for the Modulation <strong>of</strong> Liver Fibrosis<br />
Evaldo Stanislau Affonso de Araújo and Antonio Alci Barone<br />
Laboratory <strong>of</strong> Hepatitis, LIM 47 DMIP-HC-FMUSP; São Paulo, SP, Brazil<br />
In many cases, the evolution <strong>of</strong> chronic infection with the<br />
hepatitis C virus (HCV) is favorable. However, progression to<br />
liver fibrosis is a common phenomenon and can lead to liver<br />
cirrhosis. Phenomena associated with liver fibrosis have been<br />
previously reviewed and are more related to the host than to<br />
viral factors [1]. In brief, the onset <strong>of</strong> fibrosis is caused by the<br />
activation <strong>of</strong> stellate cells, which acquire the shape <strong>of</strong><br />
my<strong>of</strong>ibroblasts and become the source <strong>of</strong> collagen deposition,<br />
as well as <strong>of</strong> protein matrix formation. Activated stellate cells<br />
rapidly undergo apoptosis, after which the collagen matrix is<br />
degraded and removed by the activity <strong>of</strong> metalloproteinases.<br />
<strong>The</strong>re is a complex balance between the procollagen and<br />
antifibrotic factors, although the mechanisms <strong>of</strong> fibrosis<br />
regression are not fully understood [2]. However, it appears<br />
that the tissue inhibitor <strong>of</strong> metalloproteinase-1 [3] and stellate<br />
cell apoptosis [4] are crucial to maintaining this balance. <strong>The</strong><br />
mechanism through which HCV triggers fibrosis is little<br />
understood. Apparently, hepatocyte infection triggers a state<br />
<strong>of</strong> oxidative stress and induces inflammatory cell recruitment.<br />
<strong>The</strong>se phenomena lead to the activation <strong>of</strong> stellate cells and<br />
collagen deposition. In addition, HCV proteins directly activate<br />
stellate cells [4].<br />
Liver cirrhosis and the preceding transition stage are<br />
marked phenomena in the clinical evolution <strong>of</strong> patients and<br />
have been associated with morbidity/mortality due to chronic<br />
hepatitis C. A study involving a cohort <strong>of</strong> patients chronically<br />
infected with HCV, monitored from 1991 onward, with a mean<br />
infection period <strong>of</strong> 22 years, provided evidence that, five years<br />
after the diagnosis <strong>of</strong> cirrhosis (Ishak score ≥ 4), the survival<br />
rate was 80% [5]. This rate decreased to 19% after the first<br />
hepatic decompensation [5]. In the multivariate analysis,<br />
treatment with the combination <strong>of</strong> conventional or pegylated<br />
interferon alpha with ribavirin was found to be favorably<br />
associated with survival. In other words, the treatment was<br />
associated with the most important outcome: survival! In<br />
addition, subjects presenting a virological response, whether<br />
sustained or not, presented better evolution when compared<br />
to nonresponders. This fact suggests that even transitory<br />
negative viremia levels are a favorable phenomenon and may<br />
imply lower structural alterations and activity in the liver [5].<br />
One relevant aspect <strong>of</strong> this study was that the interruption <strong>of</strong><br />
alcohol consumption from the moment <strong>of</strong> diagnosis on<br />
prevented the previous ingestion from having an unfavorable<br />
influence on the disease progression. This fact reinforces the<br />
importance <strong>of</strong> alcohol abstinence for patients with hepatitis<br />
C. Poynard et al. [6] retrospectively analyzed data from 3,010<br />
patients treated with either conventional or pegylated<br />
<strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> 2007;11 (5) Suppl. 1:60-63.<br />
© 2007 by <strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> and Contexto<br />
Publishing. All rights reserved.<br />
interferon alpha, using various therapeutic regimens . <strong>The</strong><br />
authors concluded that the treatment with pegylated interferon<br />
and ribavirin resulted in significant improvement in histology,<br />
inflammatory activity and structural alterations (fibrosis).<br />
<strong>The</strong>re was improvement in the ‘fibrosis progression rate’,<br />
which is a valid concept, although reproducibility was<br />
jeopardized by the risks <strong>of</strong> sample variation. <strong>The</strong> least<br />
worsening <strong>of</strong> fibrosis was found in the optimized group<br />
receiving pegylated interferon and ribavirin (8%), and greatest<br />
degree <strong>of</strong> such worsening was found in the group receiving<br />
interferon for 24 weeks (23%) [6]. In general, fibrosis stabilized<br />
or improved even in those patients not achieving a sustained<br />
virological response (SVR). However, sample variations, a high<br />
percentage <strong>of</strong> patients with mild initial fibrosis (over 70%<br />
classified as F1), lack <strong>of</strong> paired biopsy results from all<br />
participants, lack <strong>of</strong> a control group, and principally, a relatively<br />
short follow-up period (20 months between biopsies, on<br />
average) were limitations <strong>of</strong> this analysis. Nevertheless,<br />
Poynard et al. [6] addressed the concept <strong>of</strong> cirrhosis<br />
‘reversion’, or as the authors designated it, the ‘reversible<br />
cirrhosis stage’. This group was composed <strong>of</strong> young patients,<br />
whose structural staging changed, regressing from F4. This<br />
phenomenon occurred in 75 (49%) <strong>of</strong> the 153 cirrhotic patients<br />
[6]. <strong>The</strong> authors postulated that this stage <strong>of</strong> fibrosis would<br />
still be ‘easily’ reversed. Some <strong>of</strong> the factors that were found<br />
to be associated with the regression <strong>of</strong> fibrosis after treatment<br />
are, obviously, the initial degree <strong>of</strong> fibrosis, minimal baseline<br />
activity, achieving an SVR, being less than 40 years <strong>of</strong> age,<br />
initial viral load lower than 3.5 million copies/mL, and (a new<br />
concept at that time) body mass index (BMI) < 27 kg/m 2 [6]. In<br />
another relevant meta-analysis, Cammà et al [7,8]. evaluated<br />
three randomized clinical studies comprising 1441 patients,<br />
paired biopsies being available for 1013 (70.3%). Similarly to<br />
Poynard et al. [6], these authors demonstrated improvement<br />
in hepatic fibrosis in the patients treated with pegylated<br />
interferon alpha-2a, when compared to those treated with<br />
conventional interferon, who achieved an SVR or even<br />
experienced recurrence. However, there was no improvement<br />
among nonresponders. <strong>The</strong> authors also found that a BMI<br />
higher than 30 kg/m 2 was associated with the worsening <strong>of</strong><br />
hepatic fibrosis. However, in a more representative sample –<br />
447 (44%) <strong>of</strong> 1013 cirrhotic patients – no ‘regression <strong>of</strong><br />
cirrhosis’ was found. Only 33% <strong>of</strong> the cirrhotic patients<br />
presented improvement in fibrosis. However, the observation<br />
period between biopsies was also short. Finally, high alanine<br />
aminotransferase level was another factor that was associated<br />
with histological improvement. More recently, Di Marco et al.<br />
[9] prospectively evaluated cirrhotic patients with portal<br />
hypertension and no previous decompensation who received<br />
pegylated interferon alpha-2b (1.0 μg/kg/week) with or without<br />
www.bjid.com.br
BJID 2007; 11 Supplement 1 (October) Maintenance Treatment for Liver Fibrosis<br />
61<br />
ribavirin (0.8 g/day). Patients infected with genotype 2 or 3<br />
showed rapid response, with negative viral RNA results by<br />
week 4 <strong>of</strong> treatment, and achieved an SVR. However, only 10<br />
<strong>of</strong> the patients infected with genotype 1 or 4 achieved an<br />
SVR. Nevertheless, for this subgroup <strong>of</strong> patients, the<br />
predictability <strong>of</strong> early response by week 12, but not by week<br />
4, was also valid, and high baseline viral load was a negative<br />
predictive marker for SVR. <strong>The</strong> occurrence <strong>of</strong> cytopenias was<br />
high; however, stimulating factors were not used with these<br />
patients. If stimulating factors had been available, the SVR<br />
rate associated with treatment maintenance would have<br />
certainly been better. Treatment compliance is even more<br />
critical for this group <strong>of</strong> patients and was associated with<br />
SVR [9]. Finally, it was clear that SVR is associated with better<br />
evolution. Only 6% <strong>of</strong> the patients achieving an SVR<br />
deteriorated, compared with 38% <strong>of</strong> the nonresponders [9].<br />
Bruno et al. [10] conducted a retrospective multicenter study<br />
comprising 920 patients with compensated cirrhosis who were<br />
treated with conventional interferon alpha (from 3 to 6 million<br />
IU/3 times a week) for a year. Similarly to the prospective<br />
study conducted by Di Marco et al. [9], the authors<br />
demonstrated benefits for those who achieved an SVR, with a<br />
reduction in the risk <strong>of</strong> decompensation, occurrence <strong>of</strong><br />
hepatocellular carcinoma (HCC) and death. <strong>The</strong>y also found<br />
that a platelet count <strong>of</strong> 109,000/mL is an independent predictor<br />
<strong>of</strong> decompensation <strong>of</strong> the liver disease [10]. This factor is<br />
extremely relevant for clinical practice and could be used as a<br />
cut-<strong>of</strong>f point in order to define the use <strong>of</strong> more aggressive<br />
measures, or even those that still need to be validated.<br />
Specifically regarding HCC, Cammà et al. [7,8] in 2001, pointed<br />
out that the benefit <strong>of</strong> the reduction in the incidence <strong>of</strong> HCC,<br />
albeit modest, is also more relevant among those who achieve<br />
an SVR after being treated with interferon alpha. Other authors<br />
have also reproduced data regarding the effective and<br />
tolerable treatment [11], fewer complications, reduction or<br />
negative incidence <strong>of</strong> HCC among cirrhotic patients monoinfected<br />
with HCV who achieved an SVR after the treatment<br />
with interferon alpha [12-14], and even histological response<br />
<strong>of</strong> patients co-infected with HIV [12]. Finally, even patients<br />
with severe cirrhosis under individualized, ascending-dose<br />
regimens benefit from treatment and can achieve an SVR, albeit<br />
a modest one [15-17]. Despite the innumerable benefits <strong>of</strong> the<br />
treatment with interferon alpha, we must emphasize that<br />
surveillance regarding the incidence <strong>of</strong> HCC is highly<br />
recommended, even in cirrhotic patients who have achieved<br />
an SVR [10].<br />
<strong>The</strong>re is clear evidence <strong>of</strong> improvement in fibrosis (a<br />
quantitative decrease, as well as functional gains such as<br />
lower portal hypertension) [3], greater survival, potential<br />
decrease in the incidence <strong>of</strong> HCC and hepatic complications,<br />
and even ‘cirrhosis reversion’ [6], even for nonresponders [6]<br />
or for those who presented recurrence [5-8]. <strong>The</strong>refore, we<br />
should ask why we do not treat even those patients with more<br />
severe cirrhosis [15-17], and why we do not use the treatment<br />
with interferon alpha for objectives other than the virological.<br />
In order to answer these questions, it is initially important<br />
that recent knowledge on viral kinetics and the concepts <strong>of</strong><br />
treatment individualization – dose and duration –be<br />
considered in the therapeutic decision-making, and that the<br />
same concepts are not clearly validated for cirrhotic patients.<br />
<strong>The</strong>refore, if our goal is to achieve an SVR, extending the<br />
treatment <strong>of</strong> nonresponders to at least 24 weeks <strong>of</strong> ‘ideal’<br />
treatment is considered ‘futile’ [1]. However, is this true from<br />
a histological point <strong>of</strong> view, or from the perspective <strong>of</strong> the<br />
need to modulate the natural history <strong>of</strong> the disease? In order<br />
to answer these questions and in view <strong>of</strong> the previously<br />
described evidence, physicians began to consider the use <strong>of</strong><br />
maintenance treatment with interferon alpha. However, for a<br />
conclusive analysis, a prospective evaluation would be ideal,<br />
since differences in methodologies would greatly affect the<br />
quality <strong>of</strong> the results [17]. Three principal studies (Table 1)<br />
have addressed this issue: the Hepatitis C Antiviral Long-<br />
Term Treatment against Cirrhosis (HALT-C) trial, conducted<br />
by the NIH; the Evaluation <strong>of</strong> Peg-Intron in Control <strong>of</strong><br />
Hepatitis C Cirrhosis (EPIC)3 trial; and the Colchicine versus<br />
Peg-Interferon Long-Term (COPILOT) trial. Other, smaller,<br />
studies, such as the PROFIC-C trial, have also addressed this<br />
issue [18].<br />
<strong>The</strong> COPILOT study evaluates patients with fibrosis<br />
classified as greater than Ishak 3 and previous nonresponders<br />
to interferon/ribavirin or pegylated interferon/ribavirin,<br />
comparing, in two branches, colchicine to pegylated interferon<br />
alpha-2b at 0.5 μg/kg/week. Preliminary analyses after a twoyear<br />
follow-up period revealed that the group using interferon<br />
presented significantly fewer hepatic complications,<br />
especially portal hypertension and upper gastrointestinal tract<br />
bleeding [6]. Alterations in HCV quantification were minimal.<br />
<strong>The</strong> EPIC3 trial has yet to produce preliminary results.<br />
However, the HALT-C study has provided a consistent amount<br />
<strong>of</strong> information. Nevertheless, data regarding the main objective<br />
<strong>of</strong> the study, fibrosis modulation, are still unavailable but<br />
should be presented at the upcoming congress <strong>of</strong> the American<br />
Association for the Study <strong>of</strong> Liver <strong>Diseases</strong> (AASLD; Afdhal,<br />
personal communication). Using the available results from<br />
HALT-C, Everson et al. [15], in 2006, emphasized the need to<br />
‘optimize’ the treatment <strong>of</strong> cirrhotic patients, for whom the<br />
SVR rate was lower, regardless <strong>of</strong> platelet counts or the need<br />
to reduce interferon doses – or even the influence <strong>of</strong> previous<br />
treatment response. <strong>The</strong>refore, cirrhosis is a determining factor<br />
<strong>of</strong> a lower SVR rate. Among the therapy ‘optimization’ measures<br />
that are currently available, should we consider treatment prior<br />
to the establishment <strong>of</strong> cirrhosis? What would be the criteria?<br />
We still cannot answer that, but if we consider some preliminary<br />
results <strong>of</strong> new therapies, we can predict that interferon alpha<br />
will still be the backbone <strong>of</strong> hepatitis treatment for many years.<br />
<strong>The</strong>refore, we should certainly attempt to gain a better<br />
understanding <strong>of</strong> the potential <strong>of</strong> these treatments and use<br />
them wisely.<br />
Among the minor studies, Erhardt et al. preliminarily<br />
showed that the maintenance <strong>of</strong> a 0.35-1.0 μg/kg/week dose<br />
www.bjid.com.br
62 Maintenance Treatment for Liver Fibrosis<br />
BJID 2007; 11 Supplement 1 (October)<br />
Table 1. Maintenance studies with pegylated interferon<br />
Study HALT-C COPILOT EPIC3<br />
Disease stage Ishak 4-6 Ishak 3-6 METAVIR 2-4<br />
CTP ≤ 6 CTP ≤ 7 CTP ≤ 6<br />
Patients (n) 1400 800 1700 (700 cirrhotic)<br />
Treatment arms Placebo, IFN-α, Peg-IFN-α-2a (90 μg) Peg-IFN-α-2b (0.5 μg)<br />
Colchicine (0.6 mg bid) Peg-IFN á-2b (0.5 μg)<br />
Duration 3.5 years 4 years 3-5 years<br />
HALT-C=Hepatitis C Antiviral Long-Term Treatment against Cirrhosis (trial); COPILOT= Colchicine versus Peg-Interferon Long-Term<br />
(trial); EPIC3=Evaluation <strong>of</strong> Peg-Intron in Control <strong>of</strong> Hepatitis C Cirrhosis (trial) 3; CTP=Child-Turcotte-Pugh score; IFN=interferon;<br />
Peg=pegylated.<br />
<strong>of</strong> pegylated interferon alpha-2b significantly reduced, after<br />
48 weeks, the incidence <strong>of</strong> HCC and complications due to<br />
cirrhosis when compared to the control group. In a similar<br />
study, Kaiser et al. [19] demonstrated that, in the intervention<br />
group, the fibrosis score dropped from 3.58 to 2.59 after 18<br />
months <strong>of</strong> treatment, and to 2.36 by six months after the end<br />
<strong>of</strong> treatment. In the control group, the fibrosis score increased<br />
from 3.88 to 4.07 and to 4.79 by the same time points. <strong>The</strong>refore,<br />
monotherapy with lower doses <strong>of</strong> pegylated interferon alpha-<br />
2b effectively reduced and modulated hepatic fibrosis. <strong>The</strong><br />
mechanism for the improvement induced by interferon is<br />
unknown and is certainly multifactorial. <strong>The</strong> elimination <strong>of</strong><br />
the triggering agent is undoubtedly crucial, but, since even<br />
patients who suffer recurrence get better, it is possible that<br />
interferon alpha has an intrinsic antifibrotic effect, as well as<br />
inhibiting the activation <strong>of</strong> stellate cells [4]. Other possible<br />
approaches that are positively associated with the<br />
improvement <strong>of</strong> hepatic fibrosis in nonresponders – or as a<br />
coadjuvant – are the use <strong>of</strong> renin-angiotensin inhibitors<br />
(inhibiting the activation <strong>of</strong> stellate cells) and the control <strong>of</strong><br />
metabolic syndrome [4]. Other substances that are potentially<br />
active against hepatic fibrosis are interleukin-10 and the natural<br />
herb known as Sho-saiko-to [4]. <strong>The</strong> maintenance treatment<br />
with ribavirin is clearly a discarded alternative since there are<br />
no positive effects [20]. Finally, the use <strong>of</strong> controlled<br />
phlebotomies may be an alternative in selected cases.<br />
Excessive iron in the hepatocytes, increased by the effect <strong>of</strong><br />
HCV, has been associated with greater tissue damage [20].<br />
<strong>The</strong> field <strong>of</strong> antifibrogenesis is in full development and has<br />
been recently reviewed in an AASLD symposium [3].<br />
Considering all the reviewed aspects, we should finally<br />
evaluate who would benefit from the maintenance treatment.<br />
<strong>The</strong>se would be the patients with extensive fibrosis (F3/F4) or<br />
cirrhosis that does not respond to the optimal standard<br />
treatment. In view <strong>of</strong> the risk <strong>of</strong> disease progression and the<br />
onset <strong>of</strong> HCC, as well as the body <strong>of</strong> evidence available, simply<br />
monitoring the progression <strong>of</strong> the disease is not an acceptable<br />
approach, neither for the patient nor for the physician [20].<br />
<strong>The</strong>refore, what is the ideal dose and how long should we<br />
maintain the treatment with interferon? <strong>The</strong> period has yet to<br />
be defined, and it may be indefinite (or until the appearance <strong>of</strong><br />
a definitely efficacious, safe therapy). Biopsy monitoring every<br />
two years in association with HCC and screening for<br />
www.bjid.com.br<br />
esophageal varices are acceptable standards, although<br />
normalization <strong>of</strong> alanine aminotransferase levels and HCV<br />
reduction will rarely be seen [20]. <strong>The</strong> advent <strong>of</strong> noninvasive<br />
methods <strong>of</strong> monitoring fibrosis [21,22] has transformed<br />
maintenance into an even more alternative strategy. Regarding<br />
the adopted dose, in ongoing and published studies,<br />
pegylated interferon alpha has been used in smaller-thanhabitual<br />
doses, once a week. Tolerance and safety have proven<br />
adequate. Doses from one-third to one-half <strong>of</strong> the standard<br />
size seem to be satisfactory for hepatic fibrosis modulation.<br />
However, definitive results, which are still unavailable, could<br />
alter this perception.<br />
In summary:<br />
1. Hepatic fibrosis is a potentially reversible<br />
phenomenon, which can even provide functional<br />
benefits.<br />
2. Even for cirrhotic patients, treatment with interferon<br />
alpha is possible, efficient and safe, although it is less<br />
efficacious if we consider the SVR.<br />
3. Treatment with pegylated interferon alpha, even when<br />
it is ineffective, is associated with greater survival,<br />
fewer complications and lower incidence <strong>of</strong> HCC.<br />
4. Interferon alpha has a modulatory effect on hepatic<br />
fibrosis.<br />
5. Maintenance treatment with reduced doses <strong>of</strong><br />
pegylated interferon alpha proved to be effective in<br />
modulating hepatic fibrosis as well as in altering the<br />
natural history <strong>of</strong> the disease.<br />
6. Antifibrogenesis is a field that is still in development,<br />
and, in addition to interferon alpha, other measures<br />
can be adopted, such as control <strong>of</strong> metabolic syndrome<br />
and the use <strong>of</strong> renin-angiotensin inhibitors.<br />
Considering the reviewed aspects, together with the facts<br />
that the number <strong>of</strong> antiviral therapies currently in development<br />
is smaller than expected, and that none <strong>of</strong> those are yet<br />
clinically available, as well as the fact that they will still need<br />
to be combined with interferon alpha, I believe that the<br />
optimization <strong>of</strong> interferon alpha will continue to be crucial. A<br />
pharmaco-economic analysis must be certainly considered as<br />
a supporting tool in the collective decision-making. However,<br />
considering the physician-patient relationship, some<br />
reflections are pertinent and should be debated by the<br />
Hepatitis Committee <strong>of</strong> the <strong>Brazilian</strong> Society <strong>of</strong> Infectology.
BJID 2007; 11 Supplement 1 (October) Maintenance Treatment for Liver Fibrosis<br />
63<br />
<strong>The</strong>refore, we propose the following:<br />
Individualization<br />
<strong>The</strong> dose and duration <strong>of</strong> treatment with the combination<br />
<strong>of</strong> pegylated interferon and ribavirin should be defined based<br />
on patient body weight and on the early response during<br />
therapy for patients with minimal lesions (F1) who nevertheless<br />
are at risk for progression: moderate peri-portal activity, from<br />
40 to 60 years <strong>of</strong> age and comorbidities (nonalcoholic<br />
steatohepatitis, HIV infection or metabolic syndrome).<br />
Maintenance Treatment<br />
Considering maintenance treatment with pegylated<br />
interferon alpha for patients with structural lesions greater<br />
than F3 or portal hypertension signs (esophageal varices,<br />
enlarged spleen, dilation <strong>of</strong> vessels) or platelet counts lower<br />
than 110,000/mm 3 , classified as Child-Pugh class A or B, no<br />
evidence <strong>of</strong> severe or potentially uncontrollable<br />
decompensation, with no HCC, no recurrence, partial<br />
responders or nonresponders to pegylated interferon alpha<br />
in association with ribavirin (or only to interferon when there<br />
are contraindications regarding ribavirin) whose compliance<br />
can be confirmed for at least 12 weeks. This treatment should<br />
also be considered for patients who present contraindications<br />
regarding the use <strong>of</strong> full doses. Child-Pugh class C patients<br />
could be treated in specialized centers when on a transplant<br />
waiting list.<br />
Proposed regimen*: subcutaneous pegylated<br />
interferon alpha-2b at 0.5-1.0 μg/kg/week;<br />
subcutaneous pegylated interferon alpha-2a at 90 μg/<br />
week.<br />
Duration*: at least 24 months, indefinite, or until the<br />
appearance <strong>of</strong> a definitely efficacious, safe antiviral<br />
therapy.<br />
Follow-up evaluation: Monitoring the onset <strong>of</strong><br />
complications (HCC, digestive tract hemorrhage,<br />
encephalopathy, etc.)<br />
*Dose schedule and duration were suggested based on preliminary data<br />
and should be reassessed depending on the results <strong>of</strong> ongoing studies.<br />
References<br />
1. Ho<strong>of</strong>nagle J.H., Seef L.B. Peginterferon and ribavirin for chronic<br />
hepatitis C. New England <strong>Journal</strong> <strong>of</strong> Medicine<br />
2006;355(23):2444-51.<br />
2. Arthur M.J.P.Reversibility <strong>of</strong> liver fibrosis and cirrhosis following<br />
treatment for hepatitis C.Gastroenterology 2002;122(5):1525-<br />
8.<br />
3. Friedman S.L., Rockey D.C., Bissel M. Hepatic fibrosis 2006:<br />
report <strong>of</strong> the third AASLD single topic conference. Hepatology<br />
2007;45:242-9.<br />
4. Bataller R., Brenner D.A. Liver fibrosis. <strong>The</strong> <strong>Journal</strong> <strong>of</strong> Clinical<br />
Investigation 2005;115:209-18.<br />
5. Lawson A., Hagan S., Rye K., et al. <strong>The</strong> natural history <strong>of</strong> hepatitis<br />
C with severe hepatic fibrosis. <strong>Journal</strong> <strong>of</strong> Hepatology<br />
2007;47:37-45.<br />
6. Poynard T., McHutchinson J., Manns M., et al. Impact <strong>of</strong> pegylated<br />
interferon alfa-2b and ribavirin on liver fibrosis in patients with<br />
chronic hepatitis C. Gastroenterology 2002;122:1303-13.<br />
7. Cammà C., Di Bona D., Schepis F., et al. Effect <strong>of</strong> peginterferon<br />
alfa-2a on liver histology in chronic hepatitis C: a meta-analysis<br />
<strong>of</strong> individual patient data. Hepatology 2004;39:333-42.<br />
8. Cammà C., Giunta M., Andreone P., Craxì A. Interferon and<br />
prevention <strong>of</strong> hepatocellular carcinoma in viral cirrhosis: an<br />
evidence-based approach. <strong>Journal</strong> <strong>of</strong> Hepatology 2001;34:593-<br />
602.<br />
9. Di Marco V., Almasio P.L., Ferraro D., et al. Peg-Interferon alone<br />
or combined with ribavirin in HCV cirrhosis with portal<br />
hypertension: a randomized controlled trial. <strong>Journal</strong> <strong>of</strong><br />
Hepatology 2007 (in press).<br />
10. Bruno S., Str<strong>of</strong>folini T., Colombo M., et al. Sustained Virological<br />
Response to interferon-á is associated with improved outcome<br />
in HCV-related cirrhosis: a retrospective study. Hepatology<br />
2007;45:579-87.<br />
11. Helbling B., Jochum W., Stamenic I., et al. HCV-Related advanced<br />
fibrosis/cirrhosis: randomization controlled trial <strong>of</strong> pegylated<br />
interferon á-2a and ribavirin. <strong>Journal</strong> <strong>of</strong> Viral Hepatitis<br />
2006;13:762-9.<br />
12. Sarmento-Castro R., Horta A., Vasconcelos O., et al. Impacto f<br />
peginterferon alpha-2b and ribavirin treatment on liver tissue<br />
in patients with HCV or HCV-HIV co-infection. <strong>Journal</strong> <strong>of</strong><br />
Infection 2007;54:609-16.<br />
13. Veldt B.J., Saracco G., Boyer N., et al. Long term clinical outcome<br />
<strong>of</strong> chronic hepatitis C patients with sustained virological<br />
response to interferon monotherapy. Gut 2004;53:1504-8.<br />
14. Coverdale S.A., Khan M.H., Byth K., et al. Effects <strong>of</strong> interferon<br />
treatment response on liver complications <strong>of</strong> chronic hepatitis<br />
C: 9-year follow-up study. American <strong>Journal</strong> <strong>of</strong><br />
Gastroenterology 2004.<br />
15. Everson T.G., Hoefs J.C., Seef L.B., et al. Impact <strong>of</strong> disease severity<br />
on outcome <strong>of</strong> antiviral therapy for chronic hepatitis C: lessons<br />
from the HALT-C Trial. Hepatology 2006;44:1675-84.<br />
16. Everson T.G., Trotter J., Forman L., et al. Treatment <strong>of</strong> advanced<br />
hepatitis C with low accelerating dosage regimen <strong>of</strong> antiviral<br />
therapy. Hepatology 2005;42:255-62.<br />
17. Everson G.T. Maintenance Interferon for chronic hepatitis C:<br />
more issues than answers? Hepatology 2000;32:436-8.<br />
18. Schuppan D., Krebs A., Bauer M., Hahn E.G. Hepatitis C and liver<br />
fibrosis. Cell Death and Differentiation 2003;10:S59-S67.<br />
19. Kaiser S., Hass H., Luize B., et al. Long term, low dose treatment<br />
with pegylated interferon alfa 2b leads to a significant reduction<br />
in fibrosis and inflammatory score in chronic hepatitis C<br />
nonresponder patients with fibrosis or cirrhosis.41 st EASL, 2006.<br />
20. Kelleher T.B., Afdhal N.H. Maintenance therapy for chronic<br />
hepatitis C. Current Gastroenterology Reports 2005;7:50-3.<br />
21. Afdhal N.H., Kowdley K.V., Llovet J.M. CCO Independent<br />
Conference Coverage <strong>of</strong> the 2007 Annual Meeting <strong>of</strong> EASL.<br />
Interim analisys: peginterferon alfa-2b maintenance therapy<br />
may reduce incidence <strong>of</strong> HCV-related HCC, Cirrhosis<br />
complications, 2007.<br />
22. Afdhal N.H., Nunes D. Evaluation <strong>of</strong> liver fibrosis: a concise review.<br />
American <strong>Journal</strong> <strong>of</strong> Gastroenterology 2004;1160-70.<br />
www.bjid.com.br
64 BJID 2007; 11 Supplement 1 (October)<br />
Treatment <strong>of</strong> Patients Infected with Hepatitis C Virus and Presenting Extrahepatic Manifestations<br />
Fátima Mitiko Tengan1 and Antonio Alci Barone<br />
University <strong>of</strong> São Paulo School <strong>of</strong> Medicine; São Paulo, SP, Brazil<br />
HCV and Mixed Cryoglobulinemia<br />
Antiviral treatment should be performed with the same<br />
medications (standard or pegylated interferon alpha (PEG-<br />
IFN-α, with or without ribavirin) and similar regimens, until<br />
additional controlled studies provide further information on<br />
the treatment <strong>of</strong> mixed cryoglobulinemia (MC) related to<br />
infection with the hepatitis C virus (HCV).<br />
Data regarding antiviral treatment <strong>of</strong> MC (Table 1) show<br />
that this therapeutic approach should be the first choice due<br />
to the antiproliferative and immunomodulatory effects <strong>of</strong> IFN<br />
and the usefulness <strong>of</strong> antiviral treatment, as demonstrated in<br />
most studies. In addition, the strict correlation between<br />
virological and clinical response, as well as the positive effect<br />
<strong>of</strong> inhibiting viral replication in the expanded B-cell clones,<br />
which is considered the pathogenic basis <strong>of</strong> MC, are reasons<br />
to make this choice. However, IFN-α can also trigger or worsen<br />
autoimmune diseases [6,7].<br />
Renal insufficiency and neuropathies can occur or be<br />
worsened, and ulcer cicatrization may be prolonged. <strong>The</strong>refore,<br />
treatment with IFN-α should be restricted to symptomatic<br />
patients, with or without renal involvement, after the careful<br />
evaluation <strong>of</strong> clinical and laboratory characteristics regarding<br />
autoimmunity during this period.<br />
In comparison with the antiviral treatment <strong>of</strong> chronic<br />
hepatitis C, the antiviral treatment <strong>of</strong> MC is more complex due<br />
to various reasons, such as the lack <strong>of</strong> standardized treatment<br />
protocols, the higher incidence <strong>of</strong> recurrence and the<br />
contraindications to antiviral treatment (old age, severe hepatic<br />
disease, acute nephritis and disseminated vasculitis). In<br />
addition, the interpretation <strong>of</strong> laboratory findings seems to be<br />
more complex than in chronic HCV infection. In fact,<br />
biochemical markers <strong>of</strong> MC response (cryocrit, rheumatoid<br />
factor or complement activity) can be more independent <strong>of</strong><br />
the virological response than are alanine aminotransferase<br />
(ALT) levels.<br />
At the moment, antiviral treatment is suggested as the<br />
treatment <strong>of</strong> choice for this condition, even when there is no<br />
indication <strong>of</strong> hepatic pathology. Patients with apparently<br />
benign manifestations <strong>of</strong> the disease (palpable purpura,<br />
arthralgia and mild fatigue) should not be treated or can be<br />
symptomatically treated with nonsteroidal anti-inflammatory<br />
drugs. Special attention must be given to the treatment <strong>of</strong><br />
patients with severe MC (with acute nephritis and<br />
disseminated vasculitis).For these cases, the data are<br />
insufficient to guarantee the safety <strong>of</strong> IFN administration, and<br />
we therefore strongly suggest a cautious approach. It is<br />
preferable to use an alternative therapeutic approach to all<br />
patients for whom antiviral treatment is contraindicated or<br />
not tolerated, as well as for those who did not respond to<br />
previous treatment. Possible alternatives include the use <strong>of</strong><br />
corticosteroids, immunosuppressants, plasmapheresis and a<br />
hypo-antigenic, or low-antigen-content, diet [8].<br />
Treatment should be individualized for each patient<br />
according to the severity <strong>of</strong> clinical symptoms, considering<br />
other factors involved (age, comorbidities, etc.) and for a<br />
limited period <strong>of</strong> time (weeks or months) until the remission <strong>of</strong><br />
symptoms. Any therapeutic approach must be avoided for<br />
clinically asymptomatic patients.<br />
Table 1. <strong>The</strong>rapeutic regimens used for mixed cryoglobulinemia associated with hepatitis C virus infection<br />
Author Year Number<br />
Treatment<br />
Treatment duration<br />
End-<strong>of</strong>-treatment<br />
Sustained<br />
(months) response virological response<br />
Zuckerman [1] 2000 9 NR 3 M IU IFN 3×/week 6 78% NA<br />
+ RBV<br />
Mazzaro [2] 2003 27 NR or 3 M IU IFN 3×/week 12 85% NA<br />
Relapsers + RBV<br />
Alric [3] 2004 18 3 M IU IFN 3×/week ≥ 18 NA 70%<br />
or PEG-IFN + RBV<br />
Cacoub [4] 2005 9 1.5 μg/kg/week PEG-IFN ≥ 10 88%<br />
+ RBV<br />
Mazzaro [5] 2005 18 1.0 μg/kg/week PEG-IFN 12 89% 44%<br />
+ RBV<br />
CS: corticosteroid; NR: Nonresponders; IFN: interferon; PEG: pegylated; RBV: Ribavirin; NA: not available.<br />
<strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong><br />
Publishing. All rights reserved.<br />
2007;11 (5) Suppl. 1:64-68. © 2007 by <strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> and Contexto<br />
www.bjid.com.br
BJID 2007; 11 Supplement 1 (October) Treating Extrahepatic Manifestations <strong>of</strong> Hepatitis C<br />
65<br />
Prior to the identification <strong>of</strong> HCV, corticosteroid therapy<br />
was the treatment <strong>of</strong> choice for MC, since corticosteroids,<br />
even in small doses, control most <strong>of</strong> the symptoms. However,<br />
corticosteroids can favor HCV replication, cause various side<br />
effects and not induce significant changes in the cryocrit or<br />
in the natural history <strong>of</strong> the disease. Cytostatic,<br />
immunosuppressive drugs (e.g., cyclophosphamide,<br />
chlorambucil and azathioprine) are mainly used, in combination<br />
with plasmapheresis, when there is no response to<br />
corticosteroids and during acute phases <strong>of</strong> MC (acute<br />
nephritis evolving to renal insufficiency and hyperviscosity<br />
syndrome). Various studies showed that rituximab (anti-CD20<br />
antibody, a specific B-cell surface antigen) is efficacious for<br />
most patients with MC, with the significant improvement or<br />
resolution <strong>of</strong> MC – particularly skin lesions – and regression<br />
<strong>of</strong> clonal expansion <strong>of</strong> B cells [9].<br />
Plasmapheresis is indicated for the removal <strong>of</strong> circulating<br />
cryoglobulins and immunocomplexes.<br />
Due to its efficacy and fast action, plasmapheresis is<br />
especially recommended in the presence <strong>of</strong> acute<br />
manifestations (cryoglobulinemic nephritis, severe sensorymotor<br />
neuropathies, skin ulcers and hyperviscosity syndrome).<br />
Combined with cyclophosphamide, it has been shown to<br />
effectively reduce the rebound effect at the end <strong>of</strong> apheresis.<br />
<strong>The</strong> low-antigen-content diet has low macromolecule content<br />
with high antigenic properties, resulting in more efficient<br />
removal <strong>of</strong> cryoglobulins by the reticuloendothelial system.<br />
This diet can improve the minor manifestations <strong>of</strong> the disease<br />
(purpura, arthralgia and paresthesias) and is generally<br />
prescribed during the initial phase <strong>of</strong> the disease.<br />
HCV and Lymphoma<br />
<strong>The</strong> inclusion <strong>of</strong> antiviral treatment seems to be rational in<br />
therapeutic regimens for non-Hodgkin’s lymphomas (NHLs)<br />
and HCV infection. This approach is supported by recent<br />
studies on low-grade lymphomas [10], and, in particular, on<br />
marginal zone lymphomas [11,12].<br />
Vallisa et al. [10] treated 13 patients diagnosed with<br />
concomitant low-grade NHL-B and HCV infection,<br />
characterized by an indolent evolution, with PEG-IFN and<br />
ribavirin. A hematologic response was seen in most patients<br />
(complete and partial response, 75%), and this was strongly<br />
associated with the clearance or reduction <strong>of</strong> HCV viral load<br />
in serum, after the treatment, which proved to be useful for<br />
treating this pathology.<br />
Hermine et al. [11] reported that patients with concomitant<br />
HCV infection and splenic lymphoma with villous lymphocytes<br />
presented complete remission after being treated with IFN.<br />
<strong>The</strong> inclusion <strong>of</strong> a control group with patients diagnosed with<br />
the same disease but presenting no HCV infection<br />
demonstrated that, unlike the patients with HCV infection,<br />
the HCV-negative patients did not respond to the treatment<br />
with IFN. Similarly, remission <strong>of</strong> polyclonal proliferation in<br />
response to the antiviral treatment proved to be clearly<br />
associated with virological response [13].<br />
Although antiviral response seems to be an attractive tool<br />
for low-grade NHL and positive HCV, chemotherapy might be<br />
necessary for intermediate- or high-grade NHL, and the<br />
antiviral treatment can be maintained after chemotherapy [14].<br />
<strong>The</strong> use <strong>of</strong> rituximab in NHL associated with HCV, alone or in<br />
combination (with antiviral treatment or with chemotherapy),<br />
seems very promising, especially for low-grade NHL [15-17].<br />
Despite the limited number <strong>of</strong> described cases, it is reasonable<br />
to consider rituximab a safe and efficacious treatment for<br />
indolent B-cell lymphomas accompanied by HCV infection.<br />
HCV and the Presence <strong>of</strong> Autoantibodies<br />
From a clinical point <strong>of</strong> view, the major concern is<br />
represented by the use <strong>of</strong> IFN. It has been reported that the<br />
administration <strong>of</strong> IFN can have a negative effect on<br />
autoimmune hepatitis. Significant increases in ALT activity –<br />
even if transitory, corrected with corticosteroids and not<br />
associated with deterioration <strong>of</strong> liver function – have also<br />
been reported in HCV/anti-liver-kidney-microsomal type 1<br />
(anti-LKM1)-positive cases treated with IFN [18,19].<br />
Initial treatment for CS is recommended when there are<br />
high antibody titers (≥ 1:320), high globulin titers, anti-LKM1<br />
antibodies, anti-human microsomal cytochrome P450 (CYP)<br />
IID6 257-279 antibodies and interface hepatitis with various<br />
plasmocytes. In the case <strong>of</strong> initial treatment with IFN, rigorous<br />
monitoring <strong>of</strong> ALT levels is suggested, especially in patients<br />
who are anti-LKM1-positive.<br />
HCV and Sjogren’s Syndrome<br />
In one study, 12 patients diagnosed with concomitant<br />
Sjögren’s syndrome and HVC infection were treated with IFN<br />
alone or with the combination <strong>of</strong> IFN and ribavirin [20]. Half <strong>of</strong><br />
the patients presented improvement <strong>of</strong> the dry syndrome using<br />
the associated regimen, but none responded to IFN in<br />
isolation. Various patients presented adverse immunologic<br />
events during treatment.<br />
HCV and Arthritis<br />
Treatment decisions must be made case by case. Etiologic<br />
treatment with IFN-a and ribavirin is recommended when there<br />
is hepatic or systemic involvement, since it can occasionally<br />
induce or worsen autoimmune disturbances. <strong>The</strong> treatment<br />
leads to a significant improvement in HCV-related arthritis,<br />
even without a complete biochemical or virological response.<br />
Cryoglobulinemia-related arthritis generally responds to<br />
antiviral treatment. Considering there are few data available at<br />
the moment, the usually non-aggressive evolution <strong>of</strong> HCVrelated<br />
arthritis does not justify the use <strong>of</strong> antiviral medications<br />
as a standard treatment.<br />
HCV and Porphyria Cutanea Tarda<br />
Treatment with IFN-a seems to be less efficacious in<br />
patients with concomitant chronic HCV infection and<br />
porphyria cutanea tarda than in those with chronic HCV<br />
infection alone. [21]. <strong>The</strong> disease also responds to iron<br />
www.bjid.com.br
66 Treating Extrahepatic Manifestations <strong>of</strong> Hepatitis C<br />
BJID 2007; 11 Supplement 1 (October)<br />
depletion by phlebotomy, which can be performed prior to<br />
antiviral treatment. However, porphyria can be triggered in<br />
genetically predisposed patients treated with the association<br />
<strong>of</strong> IFN-a and ribavirin, as a consequence <strong>of</strong> hemolysis<br />
induced by ribavirin, which causes an increase in serum iron<br />
levels [22].<br />
HCV and Lichen Planus<br />
Doutre et al. [23] reported improvement in lesions <strong>of</strong> two<br />
patients treated with IFN-α. Other authors [24-28] also<br />
reported that lesions disappeared during treatment with IFNá<br />
for several months after the end <strong>of</strong> treatment. Protzer et al.<br />
[29] reported oral and cutaneous lichen planus (LP)<br />
exacerbations during the treatment with IFN-α. Treatment was<br />
discontinued because local measures did not improve the<br />
lesions.<br />
It is generally recommended that stricter control measures<br />
be taken when patients with previous manifestations <strong>of</strong> LP<br />
receive IFN. <strong>The</strong>re are no detailed reports on the effect <strong>of</strong> the<br />
combination <strong>of</strong> IFN and ribavirin in patients with concomitant<br />
LP and HCV infection.<br />
HCV and Thyroid<br />
<strong>The</strong> treatment with IFN-α may trigger the formation <strong>of</strong><br />
autoantibodies in patients with HCV and exacerbate thyroid<br />
dysfunction in patients with pre-existing antibodies [30-33].<br />
Changes are generally detected after three months <strong>of</strong> treatment<br />
and disappear when treatment is discontinued [34].<br />
In severe cases, treatment must be discontinued,<br />
particularly in patients with hypothyroidism. Alternatively, in<br />
patients previously receiving thyroid medications, it can be<br />
useful to increase the dose during the antiviral treatment [35].<br />
Low antibody titers are not an indication for treatment<br />
discontinuation. <strong>The</strong> possibility <strong>of</strong> good treatment control<br />
generally allows the continuity <strong>of</strong> antiviral treatment. Prior to<br />
treatment, levels <strong>of</strong> thyroid hormones, including thyroidstimulating<br />
hormone (TSH), as well as anti-thrombopoietin<br />
antibodies, must be monitored. In addition, it is opportune to<br />
perform regular TSH monitoring during treatment. When there<br />
are altered values, the decision <strong>of</strong> continuing or discontinuing<br />
the treatment must be made case by case.<br />
HCV and Type 2 Diabetes Mellitus<br />
Considering that hyperglycemia was considered an<br />
independent risk factor for the ‘nonresponse’ to antiviral<br />
treatment <strong>of</strong> chronic hepatitis C [36], and that abnormal glucose<br />
levels can be associated with host-related factors, such as<br />
age, gender, alcohol use, ethnicity, obesity and resistance to<br />
insulin, it is recommended that glucose levels in blood be<br />
controlled (by means <strong>of</strong> medications or changes in lifestyle),<br />
prior to the administration <strong>of</strong> antiviral treatment.<br />
HCV and Nephropathies<br />
<strong>The</strong> treatment options for HCV and nephropathies are<br />
essentially the same as those described for MC [37-40].<br />
However, during the acute phase <strong>of</strong> kidney disease (when<br />
renal insufficiency and systemic manifestations are present),<br />
it is recommended that antiviral treatment be avoided or<br />
discontinued. In this case, measures aimed at reducing the<br />
inflammatory activity <strong>of</strong> renal lesions (corticosteroid therapy),<br />
removing circulating cryoglobulins (plasmapheresis) and<br />
reducing the formation <strong>of</strong> new antibodies (cyclophosphamide<br />
administration) are used [41-45]. Under these conditions,<br />
favorable outcomes have been achieved with mycophenolate<br />
m<strong>of</strong>etil and, more recently, with anti-CD20 antibody (rituximab).<br />
Regarding the use <strong>of</strong> ribavirin, lower proteinuria and improved<br />
kidney function have been reported in patients treated with<br />
IFN + ribavirin [1, 46,47]. It must be highlighted that ribavirin<br />
clearance is reduced in patients with renal insufficiency, and<br />
that dialysis does not eliminate the medication. <strong>The</strong>refore, the<br />
use <strong>of</strong> this antiviral drug in standard doses is not<br />
recommended for patients who present with creatinine<br />
clearance < 50 mL/min.<br />
HCV and Neuropathies<br />
Treatment with IFN-a is not efficacious and can worsen<br />
peripheral neuropathy in patients with chronic hepatitis C<br />
and MC [48]. A detailed review <strong>of</strong> available studies on patients<br />
with both HCV infection and peripheral neuropathy was<br />
inconclusive. <strong>The</strong>re were patients who responded to<br />
corticosteroids, endovenous immunoglobulin or<br />
plasmapheresis combined with antiviral treatment [49].<br />
HCV and Resistance to Insulin<br />
When treating patients with HCV infection, the physician<br />
has the challenge <strong>of</strong> differentiating patients with good<br />
prognoses from those with poor prognoses, especially<br />
regarding the intervention measures available. At the moment,<br />
the available data allow us to infer that the treatment <strong>of</strong> insulin<br />
resistance (reducing hyperinsulinemia) and <strong>of</strong> those factors<br />
that surely contribute to the onset and maintenance <strong>of</strong><br />
steatosis can increase the rate at which a sustained virological<br />
response is achieved in patients with HCV infection who were<br />
treated with the combination <strong>of</strong> PEG-IFN and ribavirin.<br />
Comments<br />
Decisions regarding the treatment <strong>of</strong> the abovementioned<br />
pathologies must be taken on a case-by-case basis, since the<br />
pathogeneses <strong>of</strong> most <strong>of</strong> these clinical manifestations are<br />
unknown. Cumulative knowledge on each <strong>of</strong> the pathologies<br />
must be considered regarding the immunomodulatory effect<br />
<strong>of</strong> IFN-α, which is the standard treatment for HCV infection.<br />
One option would be the use <strong>of</strong> an immunosuppressive agent<br />
in conjunction with interferon when there are autoimmune<br />
phenomena.<br />
References<br />
1. Zuckerman E., Keren D., Slobodin G., et al. Treatment <strong>of</strong><br />
refractory, symptomatic, hepatitis C virus related mixed<br />
cryoglobulinemia with ribavirin and interferon-alpha. J<br />
Rheumatol 2000; 27: 2172-8.<br />
www.bjid.com.br
BJID 2007; 11 Supplement 1 (October) Treating Extrahepatic Manifestations <strong>of</strong> Hepatitis C<br />
67<br />
2. Mazzaro C., Zorat F., Comar C., et al. Interferon plus ribavirin in<br />
patients with hepatitis C virus positive mixed cryoglobulinemia<br />
resistant to interferon. J Rheumatol 2003;30:1775-81.<br />
3. Alric L., Plaisier E., <strong>The</strong>bault S., et al. Influence <strong>of</strong> antiviral<br />
therapy in hepatitis C virus-associated cryoglobulinemic MPGN.<br />
Am J Kidney Dis 2004;43:617-23.<br />
4. Cacoub P., Saadoun D., Limal N., et al. PEGylated interferon alfa-<br />
2b and ribavirin treatment in patients with hepatitis C virusrelated<br />
systemic vasculitis. Arthritis Rheum 2005;52:911-5.<br />
5. Mazzaro C., Zorat F., Caizzi M., et al. Treatment with peginterferon<br />
alfa-2b and ribavirin <strong>of</strong> hepatitis C virus-associated<br />
mixed cryoglobulinemia: a pilot study. J Hepatol<br />
2005;42:632-8.<br />
6. Cid M.C., Hernandez-Rodriguez J., Robert J., et al. Interferonalpha<br />
may exacerbate cryoglobulinemia-related ischemic<br />
manifestations: an adverse effect potentially related to its antiangiogenic<br />
activity. Arthritis Rheum 1999;42:1051-5.<br />
7. Suzuki H., Takei T., Tsuji H., Nishikawa T. Membranoproliferative<br />
glomerulonephritis and demyelinating neuropathy caused by<br />
type II mixed cryoglobulinemia associated with HCV infection.<br />
Intern Med 2000;39:397-400.<br />
8. Ferri C., Giuggioli D., Cazzato M., et al. HCV-related<br />
cryoglobulinemic vasculitis: an update on its etiopathogenesis<br />
and therapeutic strategies. Clin Exp Rheumatol 2003;21:S78-<br />
S84.<br />
9. Zaja F., De Vita S., Mazzaro C., et al. Efficacy and safety <strong>of</strong><br />
rituximab in type II mixed cryoglobulinemia. Blood<br />
2003;101:3827-34.<br />
10. Vallisa D., Bernuzzi P., Arcaini L., et al. Role <strong>of</strong> anti-hepatitis C<br />
virus (HCV) treatment in HCV-related, low-grade, B-cell, non-<br />
Hodgkin’s lymphoma: a multicenter Italian experience. J Clin<br />
Oncol 2005;23:468-73.<br />
11. Hermine O., Lefrere F., Bronowicki J.P., et al. Regression <strong>of</strong> splenic<br />
lymphoma with villous lymphocytes after treatment <strong>of</strong> hepatitis<br />
C virus infection. N Engl J Med 2002;347:89-94.<br />
12. Kelaidi C., Rollot F., Park S., et al. Response to antiviral treatment<br />
in hepatitis C virus-associated marginal zone lymphomas.<br />
Leukemia 2004;18:1711-6.<br />
13. Zuckerman E., Zuckerman T., Sahar D., Streichman S. Attias<br />
therapy on t(14;18) translocation and immunoglobulin gene<br />
rearrangement in patients with chronic hepatitis C virus<br />
infection. Blood 2001;97:1555-9.<br />
14. Gisbert J.P., Garcia-Buey L., Pajares J.M., Moreno-Otero R.<br />
Systematic review: regression <strong>of</strong> lymphoproliferative disorders<br />
after treatment for hepatitis C infection. Aliment Pharmacol<br />
<strong>The</strong>r 2005;21:653-62.<br />
15. Hainsworth J.D., Litchy S., Burris H.A., et al. Rituximab as firstline<br />
and maintenance therapy for patients with indolent non-<br />
Hodgkin’s lymphoma. J Clin Oncol 2002;20:4261-7.<br />
16. Somer B.G., Tsai D.E., Downs L., et al. Improvement in Sjogren’s<br />
syndrome following therapy with rituximab for marginal zone<br />
lymphoma. Arthritis Rheum 2003;49:394-8.<br />
17. Ramos-Casals M., Lopez-Guillermo A., Brito-Zeron P., et al.<br />
Treatment <strong>of</strong> B-cell lymphoma with rituximab in two patients<br />
with Sjogren’s syndrome associated with hepatitis C virus<br />
infection. Lupus 2004;13:969-71.<br />
18. Muratori L., Lenzi M., Cataleta M., et al. Interferon therapy in<br />
liver/kidney microsomal antibody type 1-positive patients with<br />
chronic hepatitis C. J Hepatol 1994;21:199-203.<br />
19. Garcia-Buey L., Garcia-Monzon C., Rodriguez S., et al. Latent<br />
autoimmune hepatitis triggered during interferon therapy in<br />
patients with chronic hepatitis C. Gastroenterology<br />
1995;108:1770-7.<br />
20. D<strong>of</strong>foel-Hantz V., Loustaud-Ratti V., Ramos-Casals M., et al.<br />
Evolution <strong>of</strong> Sjogren syndrome associated with hepatitis C virus<br />
when chronic hepatitis C is treated by interferon or the<br />
association <strong>of</strong> interferon and ribavirin. Rev Med Interne<br />
2005;26:88-94.<br />
21. Fernandez I., Castellano G., Salamanca R.D., et al. Porphyria<br />
cutanea tarda as a predictor <strong>of</strong> poor response to interferon alfa<br />
therapy in chronic hepatitis C. Scand J Gastroenterol<br />
2003;38(3):314-9.<br />
22. Jessner W., Der-Petrossian M., Christiansen L., et al. Porphyria<br />
cutanea tarda during interferon/ribavirin therapy for chronic<br />
hepatitis C. Hepatology 2002;36(5):1301-2.<br />
23. Doutre M.S., Beylot C., Couzigou P., et al. Lichen planus and virus<br />
C hepatitis: disappearance <strong>of</strong> the lichen under interferon alfa<br />
therapy. Dermatology 1992;184:229.<br />
24. Boccia S., Gamberini S., Dalla Libera M., et al. Lichen planus and<br />
interferon therapy for hepatitis C. Gastroenterology<br />
1993;105:1921-2.<br />
25. Barreca T., Corsini G., Franceschini R., et al. Lichen planus induced<br />
by interferon- alpha-2a therapy for chronic active hepatitis<br />
C.Eur. J. Gastroenterol. Hepatol 1995;7:367-8.<br />
26. Nagao Y., Sata M., Ide T., et al. Development and exacerbation <strong>of</strong><br />
oral lichen planus during and after interferon therapy for<br />
hepatitis C. Eur J Clin Invest 1996;26:1171-4.<br />
27. Schlesinger T.E., Camisa C., Gay J.D., Bergfeld W.F. Oral erosive<br />
lichen planus with epidermolytic hyperkeratosis during<br />
interferon alfa-2b therapy for chronic hepatitis C virus infection.<br />
J Am Acad Dermatol 1997;36:1023-5.<br />
28. Dalekos G.N., Christodoulou D., Kistis K.G., et al. A prospective<br />
evaluation <strong>of</strong> dermatological side-effects during alpha-interferon<br />
therapy for chronic viral hepatitis. Eur J Gastroenterol Hepatol<br />
1998;10:933-9.<br />
29. Protzer U., Ochsendorf F.R., Leopolder-Ochsendorf A.,<br />
Holtermuller K.H. Exacerbation <strong>of</strong> lichen planus during<br />
interferon alfa-2a therapy for chronic active hepatitis C.<br />
Gastroenterology 1993;104:903-5.<br />
30. Di Bisceglie A.M., Martin P., Kassianides C., et al. Recombinant<br />
interferon alfa therapy for chronic hepatitis C. A randomized,<br />
double-blind, placebo-controlled trial. N Engl J Med<br />
1989;321(22):1506-10.<br />
31. Lisker-Melman M., Bisceglie A.D., Usala S., et al. Development<br />
<strong>of</strong> thyroid disease during therapy <strong>of</strong> chronic viral hepatitis with<br />
interferon alfa. Gastroenterology 1992;102(6):2155-60.<br />
32. Marazuela M., Garcia-Buey L., Gonzalez-Fernandez B., et al.<br />
Thyroid autoimmune disorders in patients with chronic hepatitis<br />
C before and during interferon-alpha therapy. Clin Endocrinol<br />
(Oxf) 1996;44(6):635-42.<br />
33. Deutsch M., Dourakis S., Manesis E., et al. Thyroid abnormalities<br />
in chronic viral hepatitis and their relationship to interferon<br />
alfa therapy. Hepatology 1997;26(1):206-10.<br />
34. Mazziotti G., Sorvillo F., Stornaiuolo G., et al. Temporal<br />
relationship between the appearance <strong>of</strong> thyroid autoantibodies<br />
and development <strong>of</strong> destructive thyroiditis in patients undergoing<br />
treatment with two different type-1 interferons for HCV-related<br />
chronic hepatitis: a prospective study. J Endocrinol Invest<br />
2002;25(7):624-30.<br />
35. Willson R.A. Extrahepatic manifestations <strong>of</strong> chronic viral<br />
hepatitis. Am J Gastroenterol 1997;92(1):3-17.<br />
36. Lecoub A., Hernandez C., Simó R., et al. Glucose abnormalities are<br />
na independent risk factor for nonresponse to antiviral treatment<br />
in chronic hepatitis C. Am J Gastroentreol 2007;102:1-7.<br />
37. Johnson R.J., Gretch D.R., Yamabe H., et al. Membranoproliferative<br />
glomerulonephritis associated with hepatitis C virus infection.<br />
N Engl J Med 1993;328:465-70.<br />
38. Diego J.M., Roth D. Treatment <strong>of</strong> hepatitis C infection in patients<br />
with renale disease. Curr Opin Nephrol Hypert 1988;7:557.<br />
39. Misiani R., Bellavita P., Baio P., et al. Successful treatment <strong>of</strong>HCVassociated<br />
cryoglobulinaemic glomerulonephritis with a<br />
combination <strong>of</strong> interferon-alpha and ribavirin. Nephrol Dial<br />
Transplant 1999;14:1558-60.<br />
40. Mazzaro C., Panarello G., Carniello S., et al. Interferon versus steroids<br />
in patients with hepatitis C virus-associated cryoglobulinaemic<br />
glomerulonephritis. Dig Liver Dis 2000;32:708-15.<br />
www.bjid.com.br
68 Treating Extrahepatic Manifestations <strong>of</strong> Hepatitis C<br />
BJID 2007; 11 Supplement 1 (October)<br />
41. Dammacco F., Sansonno D., Han J.H., et al. Natural interferonalpha<br />
versus its combination with 6-methyl-prednisolone in<br />
the therapy <strong>of</strong> type II mixed cryoglobulinemia: a long-term,<br />
randomized, controlled study. Blood 1994;84:3336-43.<br />
42. D’Amico G. Renal involvement in hepatitis C infection:<br />
cryoglobulinemic glomerulonephritis. Kidney Int<br />
1998;54:650-71.<br />
43. Bombardieri S., Ferri C., Paleologo G., et al. Prolonged plasma<br />
exchange in the treatment <strong>of</strong> renal involvement in essential<br />
mixed cryoglobulinemia. Int J Artif Organs 1983;6(Suppl.<br />
1):47-50.<br />
44. Ferri C., Moriconi L., Gremignai G., et al. Treatment <strong>of</strong> the renal<br />
involvement in mixed cryoglobulinemia with prolonged plasma<br />
exchange. Nephron 1986;43:246-53.<br />
45. Madore F., Lazarus J.M., Brady H.R. <strong>The</strong>rapeutic plasma exchange<br />
in renal diseases. J Am Soc Nephrol 1996;7:367-86.<br />
46. Jefferson J.A., Johnson R.J. Treatment <strong>of</strong> hepatitis C-associated<br />
glomerular disease. Semin Nephrol 2000;20:286-92.<br />
47. Reed M.J., Alexander G.J., Thiru S., Smith K.G. Hepatitis C-<br />
associated glomerulonephritis—a novel therapeutic approach.<br />
Nephrol Dial Transplant 2001;16:869-71.<br />
48. Scelsa S.N., Herskovitz S., Reichler B. Treatment <strong>of</strong><br />
mononeuropathy multiplex in hepatitis C virus and<br />
cryoglobulinemia. Muscle Nerve 1998;21(11):1526-9.<br />
49. Ramos-Casals M., Trejo O., Garcia-Carrasco M., Font J.<br />
<strong>The</strong>rapeutic management <strong>of</strong> extrahepatic manifestations in<br />
patients with chronic hepatitis C virus infection. Rheumatology<br />
[Oxford) 2003;42(7):818-28.<br />
www.bjid.com.br
BJID 2007; 11 Supplement 1 (October) 69<br />
Hepatitis C Treatment Before and After Liver Transplant<br />
Edson Abdala 1,2 , Daniela Rosa Magalhães Gotardo 1 , Patrícia Rodrigues Bonazzi 1,2 and Telésforo Bacchella 1<br />
1<br />
Liver Transplant Section, Department <strong>of</strong> Gastroenterology, University <strong>of</strong> São Paulo School <strong>of</strong> Medicine; 2 Department <strong>of</strong> <strong>Infectious</strong> and<br />
Parasitic <strong>Diseases</strong>, University <strong>of</strong> São Paulo School <strong>of</strong> Medicine; São Paulo, SP, Brazil<br />
Advanced hepatic disease, either in the form <strong>of</strong> cirrhosis<br />
or hepatocellular carcinoma, caused by infection with the<br />
hepatitis C virus (HCV), is currently the main indication for<br />
liver transplant worldwide [1,2]. Hepatitis C also appears as<br />
an etiologic factor for terminal hepatic disease. However,<br />
although this procedure is defined as a standard therapy in<br />
both situations, recurrence <strong>of</strong> HCV infection is universally<br />
recognized. <strong>The</strong> potential for HCV infection to evolve in a<br />
more aggressive manner is greater among transplant patients<br />
than among immunocompetent individuals, and the reestablishment<br />
<strong>of</strong> hepatic cirrhosis in these patients can occur<br />
within five to ten years after the transplant. <strong>The</strong> progression<br />
to cirrhosis also occurs at a more accelerated pace in these<br />
patients, with decompensation rates higher than 40% a year<br />
after diagnosis [3].<br />
Despite the risk <strong>of</strong> recurrence, cirrhosis caused by HCV<br />
has long represented a disease with good post-transplant<br />
evolution potential and low recurrence rates. In the mid 1990s,<br />
there was an increase in the rate <strong>of</strong> recurrence, which impairs<br />
the function <strong>of</strong> the graft and reduces the survival <strong>of</strong> the patient.<br />
Studies to determine the risk factors began to be carried out,<br />
and the adoption <strong>of</strong> certain measures has enabled better<br />
outcomes [4].<br />
Natural History <strong>of</strong> Hepatitis C After Transplant<br />
Early recurrence <strong>of</strong> the HCV infection after the transplant,<br />
defined as the detection <strong>of</strong> HCV RNA in the serum or graft, is<br />
a practically universal event, observed in more than 95% <strong>of</strong><br />
the cases. Hepatic disease recurrence is represented by a wide<br />
range <strong>of</strong> histopathological aspects, and the differential<br />
diagnosis with acute cellular rejection can delay its detection.<br />
In these cases, there is overlapping <strong>of</strong> histopathological<br />
standards, as well as immunopathogenic phenomena in<br />
common [5,6].<br />
In the recurrence context, acute hepatitis generally occurs<br />
between one and six months after the liver transplant, at a<br />
frequency <strong>of</strong> approximately 70%. Its histopathological<br />
findings are characterized by hepatocyte edema, large-droplet<br />
steatosis, moderate lobular inflammation, and acidophilic<br />
corpuscles. Although spontaneous resolution <strong>of</strong> acute<br />
hepatitis C occurs in up to 15% <strong>of</strong> immunocompetent<br />
individuals, it is rarely observed in the transplant context [3,4].<br />
Severe progressive cholestatic hepatitis can occur early,<br />
between one and three months after the transplant. This kind<br />
<strong>of</strong> recurrence is rarer, occurring only in 10% <strong>of</strong> the cases. Its<br />
severe evolution pattern is characterized by high levels <strong>of</strong><br />
<strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> 2007;11 (5) Suppl. 1:69-73.<br />
© 2007 by <strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> and Contexto<br />
Publishing. All rights reserved.<br />
serum bilirubin (over 6 mg/dL), high serum levels <strong>of</strong> HCV RNA,<br />
central ballooning in the liver biopsy, low inflammatory<br />
infiltrate, and cholangiolar proliferation, without associated<br />
ductopenia, suggesting that HCV has a direct cytopathic effect.<br />
<strong>The</strong>se patients evolve to rapid graft loss, and death occurs<br />
even before a new transplant attempt can be made [4].<br />
In most cases, however, the hepatitis C recurrence is<br />
diagnosed as chronic hepatitis, with a more accelerated<br />
progression <strong>of</strong> fibrosis than that observed in the<br />
immunocompetent population, resulting in cirrhosis in 8% to<br />
30% <strong>of</strong> patients within five years. Cirrhosis is also more<br />
aggressive in these patients, with a 65% cumulative risk <strong>of</strong><br />
complications within three years. <strong>The</strong> histopathological<br />
findings found in the graft are similar to those found in the<br />
native liver <strong>of</strong> an individual with hepatitis C and include mixed<br />
portal infiltrate with lymphoid aggregates, periportal<br />
inflammation, varied lobular inflammation, and steatosis. <strong>The</strong>se<br />
findings can be detected in 70% to 90% <strong>of</strong> patients one year<br />
after the transplant [7].<br />
In all <strong>of</strong> these cases, however, the real recurrence rate can<br />
only be estimated through routine serial biopsies, considering<br />
that 20% to 30% <strong>of</strong> patients do not evolve to increased<br />
aminotransferase levels, and that such an increase lacks<br />
specificity, potentially resulting from other events, such as<br />
rejection, ischemia or opportunistic infections [8]. In the Liver<br />
Transplant Sector <strong>of</strong> the Hospital das Clínicas da Faculdade<br />
de Medicina da Universidade de São Paulo (HCFMUSP,<br />
University <strong>of</strong> São Paulo School <strong>of</strong> Medicine Hospital das<br />
Clínicas), protocol biopsies are carried out every six months in<br />
the first year after the transplant, every year between the second<br />
and forth year after the transplant, and every three years after<br />
the sixth year <strong>of</strong> the transplant. An evaluation <strong>of</strong> 43 patients<br />
demonstrated histological recurrence caused by chronic<br />
hepatitis in 80% <strong>of</strong> cases in an average period <strong>of</strong> 9.9 months [9].<br />
Risk Factors for the Severity <strong>of</strong> Post-Transplant HCV<br />
Recurrence <strong>of</strong> Hepatitis C<br />
<strong>The</strong> factors that determine the evolution <strong>of</strong> hepatitis C in<br />
patients submitted to liver transplant can be variables related<br />
to the donor and receptor, viral factors, and events associated<br />
with the transplant, resulting in greater severity <strong>of</strong> the disease<br />
and higher rates <strong>of</strong> graft loss. <strong>The</strong> factors that are more<br />
consistently associated with the severity <strong>of</strong> the disease are:<br />
advanced age <strong>of</strong> donors, treatment for acute cellular rejection<br />
involving pulse therapy with corticosteroids or administration<br />
<strong>of</strong> OKT3, and infection with the cytomegalovirus [3,5,7,10]. A<br />
better understanding <strong>of</strong> the factors that contribute to the<br />
progression <strong>of</strong> the disease may indicate the potentially<br />
modifiable mechanisms <strong>of</strong> its evolution.<br />
www.bjid.com.br
70 Liver Transplant and Hepatitis C Treatment<br />
BJID 2007; 11 Supplement 1 (October)<br />
Donor and Receptor Factors<br />
<strong>The</strong> use <strong>of</strong> older liver donors is a factor that negatively<br />
affects the fibrosis progression rate. Recent studies show a<br />
tendency toward a ten-year increase in the age <strong>of</strong> donors in the<br />
last decade. This measure, although applied to compensate for<br />
the low availability <strong>of</strong> organs, has been shown to have a direct<br />
influence on the degree <strong>of</strong> fibrosis in recurrent hepatitis C.<br />
Recent studies have shown that the ten-year difference in donor<br />
age (40 versus 50 years) has been associated with greater fibrosis<br />
progression (from 0.6 to 2.1 units a year) and with a decrease in<br />
the interval <strong>of</strong> appearance <strong>of</strong> cirrhosis (<strong>of</strong> up to eight years).<br />
Donor age seems to influence graft survival only in HCVpositive<br />
patients. However, there is little chance that this will<br />
change, since very few transplant programs are able to pair<br />
younger donors with HCV-positive receptors [11,12].<br />
<strong>The</strong> involvement <strong>of</strong> immunogenetic factors is also<br />
considered, with studies that observed the association<br />
between HLA-B14 and HLA-DRB104 as beneficial to hepatitis<br />
C evolution, and the mismatch between the donor/receptor<br />
HLA-DRB1 with an increased recurrence risk [13,14].<br />
Other donor factors that require further investigation<br />
include the use <strong>of</strong> live donors, hepatic iron content, and hepatic<br />
steatosis [15,16].<br />
Viral Factors<br />
Some studies have associated high viral load before or<br />
soon after the transplant with the severity <strong>of</strong> post-transplant<br />
HCV recurrence. An analysis involving 284 North-American<br />
and Spanish patients showed that the pre-transplant viral load<br />
is an independent factor in the progression <strong>of</strong> fibrosis. In<br />
another study carried out in the United States, the five-year<br />
survival <strong>of</strong> patients submitted to transplant for HCV was found<br />
to be lower in patients with viral loads higher than one million<br />
mEq/mL [7].<br />
<strong>The</strong> importance <strong>of</strong> the HCV genotype in the progression<br />
<strong>of</strong> the disease remains controversial. Although most <strong>of</strong> the<br />
studies conducted in the United States failed to show this<br />
association, a large collaborative European study showed a<br />
higher rate <strong>of</strong> progression and severity in transplant patients<br />
infected with HCV genotype 1b. One hypothesis is that, in<br />
the liver transplant context, the host immune response to HCV<br />
is stronger for the 1b genotype than for other genotypes, and<br />
that the tissue lesion is associated with this response [17].<br />
Factors Associated with the Transplant<br />
<strong>The</strong> treatment <strong>of</strong> acute rejection episodes with the use <strong>of</strong><br />
corticosteroid pulse therapy or anti-lymphocyte preparations<br />
has been associated with greater severity <strong>of</strong> hepatitis C<br />
recurrence. However, for such patients, the use <strong>of</strong><br />
immunosuppressive regimens is recommended, which is<br />
sufficient to prevent moderate or severe rejection, as is the<br />
subsequent use <strong>of</strong> corticosteroid pulse therapy or OKT3<br />
administration, but not to the point <strong>of</strong> exacerbating the<br />
hepatitis C progression or causing other long-term<br />
complications [5].<br />
Considering that one <strong>of</strong> the hypotheses put forth to explain<br />
the more severe HCV recurrence observed in recent years is<br />
the increased potency <strong>of</strong> immunosuppressive agents, several<br />
studies have been carried out to minimize or even abandon<br />
the use <strong>of</strong> the immunosuppressive regimen. <strong>The</strong>se studies<br />
have shown diverging results. However, there were differences<br />
among the studies in terms <strong>of</strong> the initial immunosuppressive<br />
doses and the dose reduction rates. In some studies, the<br />
prolonged use <strong>of</strong> maintenance corticosteroid therapy was<br />
associated with lesser severity <strong>of</strong> the hepatic disease<br />
recurrence. In this case, the method <strong>of</strong> reducing the dose was<br />
important, and gradual reductions have been associated with<br />
less aggressive forms <strong>of</strong> hepatitis C [18,19].<br />
<strong>The</strong> use <strong>of</strong> azathioprine or mycophenolate m<strong>of</strong>etil has not<br />
been shown to have any consistent effect on HCV recurrence.<br />
Although cyclosporine has been shown to have antiviral<br />
properties in vitro, it has not shown to have any advantage<br />
over tacrolimus in clinical practice [20,21]. <strong>The</strong> long-term use<br />
<strong>of</strong> sirolimus can provide some benefit, since it has antifibrotic<br />
and potential antiviral effects, although such studies are still<br />
preliminary and do not support its preferential use in this<br />
group <strong>of</strong> patients. <strong>The</strong> use <strong>of</strong> new drugs, such as sirolimus<br />
and the interleukin 2 receptor antagonist, requires controlled<br />
and prospective studies. <strong>The</strong>refore, the general<br />
immunosuppression status seems to be one <strong>of</strong> the possible<br />
determinant events in the course <strong>of</strong> recurrent hepatitis C<br />
[20,22,23].<br />
Another factor that is associated with the transplant and<br />
negatively influences the post-transplant evolution <strong>of</strong> hepatitis<br />
C is the presence <strong>of</strong> infection with the cytomegalovirus, which<br />
leads to the worsening <strong>of</strong> fibrosis [24].<br />
Pre- and Post-Transplant Approach to Treating HCV-Positive<br />
Patients<br />
Antiviral therapy is the main strategy used in treating HCVpositive<br />
patients. However, the ideal moment at which to<br />
intervene remains unknown. <strong>The</strong> authors <strong>of</strong> most studies have<br />
initiated the treatment for HCV recurrence when there is<br />
histological evidence <strong>of</strong> the disease. Alternative treatments<br />
include the use <strong>of</strong> antiviral therapy before or soon after the<br />
transplant, when there is still no clinical evidence <strong>of</strong> recurrent<br />
disease. This is known as pre-emptive therapy. Antiviral<br />
therapy is generally less efficient and less well tolerated in the<br />
transplant patient than in the immunocompetent patient.<br />
Treatment <strong>of</strong> Patients with Cirrhosis Who are on the<br />
Transplant Waiting List<br />
Viral clearance in the patient with cirrhosis, in addition to<br />
providing better expectations for the transplant (increased<br />
graft survival), can even interrupt the progression <strong>of</strong> fibrosis<br />
in these patients, and, in some cases, preclude the need for<br />
the liver transplant.<br />
Studies have proven that, although the side effect rates<br />
are high, the rate at which a sustained virological response is<br />
achieved in patients with compensated cirrhosis treated with<br />
www.bjid.com.br
BJID 2007; 11 Supplement 1 (October) Liver Transplant and Hepatitis C Treatment<br />
71<br />
progressively higher doses <strong>of</strong> conventional interferon and<br />
ribavirin is approximately 22%, and can be even higher in those<br />
infected with genotype 2 or 3. When submitted to transplant,<br />
such patients do not present recurrence <strong>of</strong> the disease,<br />
confirming the validity <strong>of</strong> this therapeutic strategy [25].<br />
In one study, carried out by Forns et al., 30 transplant<br />
waiting list patients <strong>of</strong> different functional classes were<br />
submitted to antiviral treatment. In that study, the efficacy <strong>of</strong><br />
the treatment was evaluated on the basis <strong>of</strong> the virological<br />
response throughout the treatment period, as well as on the<br />
rate at which a sustained virological response was achieved.<br />
<strong>The</strong> simple reduction in the HCV viral load before the<br />
transplant was sufficient to avoid recurrence after the<br />
transplant (efficacy <strong>of</strong> approximately 66%). In addition, none<br />
<strong>of</strong> the patients achieving a sustained virological response<br />
experienced disease recurrence [26].<br />
Most <strong>of</strong> the studies involving this population <strong>of</strong> patients<br />
have evaluated the efficacy <strong>of</strong> conventional interferon. Overall,<br />
they concluded that the treatment is recommended for patients<br />
with Child-Turcotte-Pugh class A or B cirrhosis and a model<br />
for end-stage liver disease (MELD) score lower than 18, or<br />
even in patients with decompensated cirrhosis. However, in<br />
the last case, following the treatment protocol in a center with<br />
support and possibility <strong>of</strong> immediate transplant [26].<br />
In a recent study <strong>of</strong> data collected in the HCFMUSP Liver<br />
Transplant Sector, 37 transplant waiting list patients with HCVinduced<br />
cirrhosis were submitted to antiviral treatment. This<br />
population was composed <strong>of</strong> 46% women and 54% men, with<br />
a mean age <strong>of</strong> over 50 years. <strong>The</strong> predominant genotypes<br />
were 1 and 3. <strong>The</strong>re was history <strong>of</strong> ascites and hepatic<br />
encephalopathy in 43.2% and 8.1% <strong>of</strong> the patients infected<br />
with genotypes 1 and 3, respectively. History <strong>of</strong> varicose<br />
digestive hemorrhage two months before the treatment was<br />
present in 5.4% <strong>of</strong> patients, and a history <strong>of</strong> spontaneous<br />
bacterial peritonitis was common (in 8.1%). Pegylated<br />
interferon was used in only five patients (all infected with<br />
genotype 1), and conventional interferon was used in the<br />
remaining patients. Both were used in combination with<br />
ribavirin. <strong>The</strong> mean duration <strong>of</strong> treatment was 7.9 months.<br />
<strong>The</strong> most common side effect associated with the treatment<br />
discontinuation was neutropenia (in 37.7%). Of the 37 patients,<br />
14 (37.8%) presented viral load reduction <strong>of</strong> at least 2 log. In<br />
that study, the presence <strong>of</strong> compensated or decompensated<br />
cirrhosis did not affect the treatment response [27].<br />
Recent studies describe the treatment with pegylated<br />
interferon and ribavirin in patients with decompensated<br />
cirrhosis. Although they present a considerable virological<br />
response, the frequency <strong>of</strong> severe complications necessarily<br />
leads to the need to always analyze the risk/benefit ratio before<br />
the decision to initiate treatment is made, also considering the<br />
feasibility <strong>of</strong> an emergency transplant [28,29].<br />
Pre-Emptive <strong>The</strong>rapy<br />
Antiviral therapy before the establishment <strong>of</strong> histologically<br />
confirmed disease presents theoretical advantages,<br />
considering that, immediately after the transplant, the HCV<br />
viral load and the degree <strong>of</strong> hepatic fibrosis tend to be lower.<br />
This could provide a better response to the treatment, similar<br />
to what occurs in nontransplant patients. However, this is a<br />
moment at which the immunosuppression is still high, interfering<br />
with the antiviral response, and the antiviral regimen tolerability<br />
is too low in view <strong>of</strong> all <strong>of</strong> the other post-transplant clinical<br />
complications, such as infections and cytopenias. In addition,<br />
the immunomodulatory effect <strong>of</strong> interferon can increase the<br />
risk <strong>of</strong> acute cellular rejection, which is higher in this phase <strong>of</strong><br />
the transplant process. Another criticism <strong>of</strong> pre-emptive<br />
treatment is that it does not distinguish patients who will actually<br />
evolve to a more significant recurrence <strong>of</strong> the disease and for<br />
whom treatment is indicated, from those who might have no<br />
need <strong>of</strong> antiviral therapy after the transplant [30,31].<br />
Controlled studies have shown that treatment with the<br />
combination <strong>of</strong> conventional interferon and ribavirin has an<br />
advantage over monotherapy with interferon. <strong>The</strong>re was a<br />
delay in the appearance <strong>of</strong> recurrence in those patients, who<br />
presented viral load reduction and better histological pr<strong>of</strong>iles.<br />
Studies involving the use <strong>of</strong> pegylated interferon and ribavirin<br />
have also demonstrated histological improvement, although<br />
their results are generally disappointing, with sustained<br />
virological response rates <strong>of</strong> 7-13% with the use <strong>of</strong> isolated<br />
interferon, 16-33% with interferon and ribavirin, and 9% with<br />
isolated pegylated interferon [32].<br />
This strategy is not applicable to all patients. Those with<br />
better MELD scores before the transplant seem to be the best<br />
candidates. <strong>The</strong> need to reduce the dose or even discontinue<br />
the treatment is common, typically caused by cytopenias and<br />
concomitant renal dysfunction, with secondary anemia, which<br />
makes the use <strong>of</strong> ribavirin particularly difficult [33].<br />
Post-Transplant Treatment<br />
In general, most patients submitted to transplant for<br />
cirrhosis caused by HCV are treated after the transplant, when<br />
recurrence is already an established event. Unfortunately, most<br />
studies that support this treatment strategy have been<br />
uncontrolled, preventing the determination <strong>of</strong> the treatment<br />
risks, acute/chronic rejection rates, and even the evaluation<br />
<strong>of</strong> the therapeutic efficacy.<br />
This is a population that, in principle, presents the worst<br />
prognostic factors <strong>of</strong> evolution and treatment response, since<br />
it comprises older patients who are infected with genotype 1,<br />
have high viral loads and present more extensive fibrosis, as<br />
well as more <strong>of</strong>ten having a history <strong>of</strong> previous treatment.<br />
<strong>The</strong>se characteristics are also associated with the fact that<br />
transplant patients present comorbidities that frequently<br />
prevent the use <strong>of</strong> full-dose therapies [34].<br />
In this group <strong>of</strong> patients, protocol biopsies are an essential<br />
means <strong>of</strong> assessing the degree <strong>of</strong> hepatic fibrosis and should<br />
be carried out whenever clinically indicated (by an increase in<br />
aminotransferase levels) or at least on an annual basis, with<br />
the specific purpose <strong>of</strong> detecting and monitoring HCV<br />
recurrence [35].<br />
www.bjid.com.br
72 Liver Transplant and Hepatitis C Treatment<br />
BJID 2007; 11 Supplement 1 (October)<br />
<strong>The</strong> results <strong>of</strong> this group are no less disappointing, with a<br />
sustained virological response rate <strong>of</strong> 12.5% with isolated<br />
interferon, 21% with interferon and ribavirin, and 9% with<br />
isolated pegylated interferon. In uncontrolled studies the<br />
combined use <strong>of</strong> pegylated interferon and ribavirin proved<br />
to be the best strategy, with responses between 30% and<br />
45% [2,36-38].<br />
<strong>The</strong> optimal duration <strong>of</strong> antiviral therapy remains<br />
undefined. Although most recent studies established<br />
treatment periods <strong>of</strong> 48 to 52 weeks, the validity <strong>of</strong><br />
prolonging treatment in patients who achieved virological<br />
response by the end <strong>of</strong> the standard treatment period is still<br />
in question [39-41].<br />
<strong>The</strong> advantages <strong>of</strong> therapy that begins within 6 to 24<br />
months after the transplant, compared with pre-emptive<br />
therapy, is that these patients require less<br />
immunosuppression, present better clinical status, and are<br />
at lower risk <strong>of</strong> acute or chronic rejection [7].<br />
<strong>The</strong> occurrence <strong>of</strong> acute or chronic rejection has not<br />
been a limiting factor to the treatment, although there are<br />
some reports on this subject [42].<br />
<strong>The</strong> use <strong>of</strong> ribavirin as isolated therapy or as maintenance<br />
after the combined use with interferon has no subside in the<br />
literature [43].<br />
Use <strong>of</strong> Adjuvant <strong>The</strong>rapy<br />
In this group <strong>of</strong> patients, one <strong>of</strong> the central issues is the<br />
high rate <strong>of</strong> side effects from antiviral drugs, especially<br />
cytopenia, which <strong>of</strong>ten requires dose reduction or even<br />
discontinuation <strong>of</strong> the treatment. <strong>The</strong> risk/benefit ratio <strong>of</strong> the<br />
use <strong>of</strong> erythropoietin or granulocyte colony-stimulating factor<br />
has not been well established. However, its use has facilitated<br />
the maintenance <strong>of</strong> antiviral treatment and the use <strong>of</strong> optimal<br />
doses <strong>of</strong> ribavirin and interferon [44]. Efforts have been made<br />
to investigate the use <strong>of</strong> ribavirin substitutes that do not cause<br />
hemolysis, such as viramidine, although controlled studies<br />
are still needed in order to determine the best strategy in<br />
relation to the adverse effects <strong>of</strong> the therapy [5].<br />
Second Transplants in Cases <strong>of</strong> Hepatitis C Recurrence<br />
Although a second transplant is always an option in<br />
patients presenting hepatitis C recurrence, this strategy is<br />
historically associated with disappointing results. Receptor<br />
age, total bilirubin, high prothrombin time, older donor age,<br />
admission to the intensive care unit, high creatinine level,<br />
and high MELD score are predictive factors <strong>of</strong> short survival<br />
after a new transplant. Second transplants remain<br />
controversial and require comprehensive discussions in view<br />
<strong>of</strong> the low availability <strong>of</strong> organs and the use <strong>of</strong> MELD score<br />
as an organ allocation criterion, which implies that second<br />
transplants will be given to recurrent patients presenting<br />
more severe clinical pr<strong>of</strong>iles. In general, a second transplant<br />
is recommended if one <strong>of</strong> the variables related to recurrence,<br />
and thus the natural history <strong>of</strong> HCV recurrence, can be altered<br />
[45-47].<br />
References<br />
1. Gane E. <strong>The</strong> natural history and outcome <strong>of</strong> liver transplantation<br />
in hepatitis C virus-infected recipients. Liver Transplant 2003;9<br />
(suppl3):S28-S34.<br />
2. Teixeira R., Menezes E.G., Schiano T.D. <strong>The</strong>rapeutic management<br />
<strong>of</strong> recurrent hepatitis C after liver transplantation. Liver Int<br />
2007;27:302-12.<br />
3. Samuel D., Forns X., Berenguer M., et al. Report <strong>of</strong> the<br />
monothematic EASL conference on liver transplantation for<br />
viral hepatitis. J Hepatol 2006;45:127-43.<br />
4. Rodriguez-Luna H., Douglas D.D. Natural history <strong>of</strong> hepatitis C<br />
following Liver Transplant 2004;17:363-71.<br />
5. Wiesner R.H., Sorrell M., Villamil F., et al. Liver Transplantation<br />
Society Expert Panel. Report <strong>of</strong> the first international liver<br />
transplantation expert panel consensus conference on liver<br />
transplantation and hepatitis C. Liver Transplant 2003;9<br />
(suppl3):S1-S9.<br />
6. Guido M., Fagiuoli S., Tessari G., et al. Histology predicts<br />
cirrhotic evolution <strong>of</strong> post transplant hepatitis C. Gut<br />
2002;50:697-700.<br />
7. Terrault N.A., Berenguer M. Treating hepatitis C infection in liver<br />
transplant recipients. Liver Transplant 2006;12:1192-204.<br />
8. Charlton M. Liver biopsy, viral kinetics and the impact <strong>of</strong> viremia<br />
on severity <strong>of</strong> hepatitis C virus recurrence. Liver Transplant<br />
2003;9 (Suppl. 3):S58-S62.<br />
9. Campos S.V., Bonazzi P.R., Abdala E., et al. Chronic hepatitis C<br />
recurrence after liver transplantation. Liver Transplant 2007;13<br />
(suppl.1):S213-S14.<br />
10. Cameron A.M., Ghobrial R.M., Hiatt J.R., et al. Effect <strong>of</strong> nonviral<br />
factors on hepatitis C recurrence after liver transplantation.<br />
Ann Surg 2006;244:563-71.<br />
11. Berenguer M., Prieto M., San Juan F., et al. Contribution <strong>of</strong><br />
donor age to the recent decrease in patient survival among<br />
HCV-infected liver transplant recipients. Hepatology<br />
2002;36:202-10.<br />
12. Machicao V., Bonatti H., Krishna M., et al. Donor age affects<br />
fibrosis progression and graft survival after liver transplantation<br />
for hepatitis C. Transplantation 2004;77:84-92.<br />
13. Langrehr J.M., Puhl G., Bahra M., et al. Influence <strong>of</strong> donor/recipient<br />
HLA-matching on outcome and recurrence <strong>of</strong> hepatitis C after<br />
liver transplantation. Liver Transplant 2006;12:644-51.<br />
14. Belli L.S., Burra P., Poli F., et al. HLA-DRB1 donor-recipient<br />
mismatch affects the outcome <strong>of</strong> hepatitis C disease<br />
recurrence after liver transplantation. Gastroenterology<br />
2006;130:695-702.<br />
15. Imber C.J., St.Peter S.D., Handa A., Friend P. Hepatic steatosis<br />
and its relationship to transplantation. Liver Transplant<br />
2002;8:415-23.<br />
16. Guo L., Orrego M., Rodriguez-Luna H., et al. Living donor liver<br />
transplantation for hepatitis C-related cirrhosis: no difference in<br />
histological recurrence when compared to deceased donor liver<br />
transplantation recipients. Liver Transplant 2006;12: 560-5.<br />
17. Féray C., Caccamo L., Alexander G.J.M., et al. European<br />
Collaborative Study on factors influencing outcome after liver<br />
transplantation for hepatitis C. Gastroenterology<br />
1999;117:619-25.<br />
18. McCaughan G.W., Zekry A. Impact <strong>of</strong> immunosuppression on<br />
immunopathogenesis <strong>of</strong> liver damage in hepatitis C virus-infected<br />
recipients following liver transplantation. Liver Transplant<br />
2003;9 (suppl3):S21-S7.<br />
19. Lladó L., Xiol X., Figueras J., et al. Immunosuppression without<br />
steroids in liver transplantation is safe and reduces infection<br />
and metabolic complication: results from a prospective<br />
multicenter randomized study. J Hepatol 2006;44:710-6.<br />
20. Berenguer M., Aguilera V., Prieto M., et al. Effect <strong>of</strong> calcineurin<br />
inhibitors on survival and histologic disease severity in HCVinfected<br />
liver transplant recipients. Liver Transplant<br />
2006;12:762-7.<br />
www.bjid.com.br
BJID 2007; 11 Supplement 1 (October) Liver Transplant and Hepatitis C Treatment<br />
73<br />
21. Hilgard P., Kahraman A., Lehmann N., et al. Cyclosporine versus<br />
tacrolimus in patients with hepatitis C infection after liver<br />
transplantation: effects on virus replication and recurrent<br />
hepatitis. World J Gastroenterol 2006;7:697-702.<br />
22. Jain A., Kashyap R., Demetris A.J., et al. A prospective randomized<br />
trial <strong>of</strong> mycophenolate m<strong>of</strong>etil in liver transplant recipients<br />
with hepatitis C. Liver Transplant 2002;8:40-6.<br />
23. Tisone G., Orlando G., Cardillo A., et al. Complete weaning <strong>of</strong>f<br />
immunosuppression in HCV liver transplant recipients is feasible<br />
and favourably impacts on the progression <strong>of</strong> disease recurrence.<br />
<strong>Journal</strong> <strong>of</strong> Hepatology 2006;44:702-9.<br />
24. Chopra K.B., Demetris A.J., Blakolmer K., et al. Progression <strong>of</strong><br />
liver fibrosis in patients with chronic hepatitis C after orthotopic<br />
liver transplantation. Transplantation 2003;76:1487-91.<br />
25. Crippin J.S., McCashland T., Terrault N., et al. A pilot study <strong>of</strong> the<br />
tolerability and efficacy <strong>of</strong> antiviral therapy in hepatitis C virusinfected<br />
patients awaiting liver transplantation. Liver Transplant<br />
2002;8:350-5.<br />
26. Forns X., Garcia-Retortillo M., Serrano T., et al. Antiviral therapy<br />
<strong>of</strong> patients with decompensated cirrhosis to prevent recurrence<br />
<strong>of</strong> hepatitis C after liver transplantation. J <strong>of</strong> Hepatol<br />
2003;39:905-15.<br />
27. Oliveira P.R.D., Freitas A.C., Tengan F.M., et al. Hepatitis C antiviral<br />
therapy in cirrhotic patients. J Clin Virol 2006;38(suppl):S135-S6.<br />
28. Horoldt B., Haydon G., O’Donnell K., et al. Results <strong>of</strong> combination<br />
treatment with pegylated interferon and ribavirin in cirrhotic<br />
patients with hepatitis C infection. Liver Int 2006;26:650-9.<br />
29. Iacobellis A., Siciliano M., Perri F., et al. Peginterferon alfa-2b<br />
and ribavirin in patients with hepatitis C virus and decompensated<br />
cirrhosis: a controlled study. J Hepatol 2007;46:206-12.<br />
30. Shiffman M.L., Vargas H.E., Everson G.T. Controversies in the<br />
management <strong>of</strong> hepatitis C virus infection after liver<br />
transplantation. Liver Transplant 2003;9(suppl3):S1129-S44.<br />
31. Kuo A., Terrault N.A. Management <strong>of</strong> hepatitis C in liver<br />
transplant recipients. Am J Transplant 2006;6:449-58.<br />
32. Szabo G., Katz E., Bonkowsky H.L. Management <strong>of</strong> recurrent<br />
hepatitis C after liver transplantation: a concise review. American<br />
J Gastroenterol 2000;95:2164-70.<br />
33. Davis G.L. New approaches and therapeutic modalities for the<br />
prevention and treatment <strong>of</strong> recurrent HCV after liver<br />
transplantation. Liver Transplant 2003;9(suppl3):S114-S19.<br />
34. Berenguer M., Palau A., Fernandez A., et al. Efficacy, predictors<br />
<strong>of</strong> response and potential risks associated with antiviral therapy<br />
in liver transplant recipients with recurrent hepatitis C. Liver<br />
Transplant 2006;12:516-19.<br />
35. Sebagh M., Rifai K., Féray C., et al. All liver recipients benefit<br />
from the protocol 10-year liver biopsies. Hepatology<br />
2003;37:1293-301.<br />
36. Wang C.S., Ko H.H., Yoshida E.M., et al. Interferon-based<br />
combination anti-viral therapy for hepatitis C virus after liver<br />
transplantation: a review and quantitative analysis. Am J<br />
Transplant 2006;6:1586-99.<br />
37. Murkherjee S., Lyden E. Impact <strong>of</strong> pegylated interferon alpha-2b<br />
and ribavirin on hepatic fibrosis in liver transplant patients<br />
with recurrent hepatitis C: an open-label series. Liver Int<br />
2006;26:539-5.<br />
38. Heydtmann M., Freshwater D., Dudley T., et al. Pegylated<br />
interferon alpha-2b for patients with HCV recurrence and graft<br />
fibrosis following liver transplantation. Am J Transplant<br />
2006;6:825-33.<br />
39. Lavezzo B., Franchello A., Smedile A., et al. Treatment <strong>of</strong> recurrent<br />
hepatitis C in liver transplants: efficacy <strong>of</strong> a six versus a twelve<br />
month course <strong>of</strong> interferon alfa-2b with ribavirin. J Hepatol<br />
2002;37:247-52.<br />
40. Rodriguez-Luna H., Khatib A., Sharma P., et al. Treatment <strong>of</strong><br />
recurrent hepatitis C infection after liver transplantation<br />
with combination <strong>of</strong> pegylated interferon alpha-2b and<br />
ribavirin: an open-label series. Transplantation<br />
2004:77:190-4.<br />
41. Bizzolon T., Ahmed S.N.S., Radenne S., et al. Long term histological<br />
improvement and clearance <strong>of</strong> intrahepatic hepatitis C virus<br />
RNA following sustained response to interferon-ribavirin<br />
combination therapy in liver transplanted patients with hepatitis<br />
C recurrence. Gut 2003;52:283-7.<br />
42. Khalili M., Vardanian A.J., Hamerski C.M., et al. Management <strong>of</strong><br />
hepatitis C-infected liver transplant recipients at large North<br />
American centres: changes in recent years. Clin Transplant<br />
2006;20:1-9.<br />
43. Schiano T.D., Martin P. Management <strong>of</strong> HCV infection and liver<br />
transplantation. Int J Med Sci 2006;3:79-83.<br />
44. Gotardo D.R.M., Abdala E., Bonazzi P.R., et al. Safety <strong>of</strong> recurrent<br />
hepatitis C treatment after liver transplantation with use <strong>of</strong><br />
adjuvants. Liver Transplant 2007;13(suppl 1):S152.<br />
45. McCashland T.M. Retransplantation for recurrent hepatitis C:<br />
positive aspects. Liver Transplant 2003;9(suppl 3.):S67-S72.<br />
46. Wall W.J., Khakhar A. Retransplantation for recurrent hepatitis C:<br />
the argument against. Liver Transplant 2003;9(suppl 3):S73-S8.<br />
47. Ercolani G., Grazi G.L., Ravaioli M., et al. Histological recurrent<br />
hepatitis C after liver transplantation: outcome and role <strong>of</strong><br />
retransplantation. Liver Transplant 2006;12:1104-11.<br />
www.bjid.com.br
74 BJID 2007; 11 Supplement 1 (October)<br />
Adverse Event Management<br />
Aline Gonzalez Vigani<br />
Department <strong>of</strong> Viral Hepatitis Studies, State University <strong>of</strong> Campinas (Unicamp); Campinas, SP, Brazil<br />
<strong>The</strong> treatment <strong>of</strong> hepatitis C involves combining<br />
conventional interferon (IFN) or pegylated IFN (PEG-IFN) with<br />
ribavirin (RBV). <strong>The</strong>se therapeutic regimens are associated<br />
with numerous adverse events, among which constitutional<br />
and neuropsychiatric symptoms, as well as hematological<br />
abnormalities, stand out [1,2]. <strong>The</strong> adverse events observed<br />
with the use <strong>of</strong> PEG-IFN or conventional IFN are similar, and<br />
the frequencies <strong>of</strong> those events are shown in Table 1 [3-5].<br />
Adverse events resulting from the treatment <strong>of</strong> hepatitis C<br />
can jeopardize the quality <strong>of</strong> life <strong>of</strong> patients and their response<br />
to treatment. <strong>The</strong> control <strong>of</strong> those events involves medicinal<br />
and non-medicinal interventions. <strong>The</strong> latter include a<br />
reduction in the dosage <strong>of</strong> IFN or RBV and discontinuation <strong>of</strong><br />
the treatment.<br />
A temporary or permanent reduction in the dosage <strong>of</strong> PEG-<br />
IFN, conventional IFN or RBV as a result <strong>of</strong> an adverse event<br />
is necessary in approximately 30% <strong>of</strong> patients. In 10% <strong>of</strong><br />
patients it is necessary to discontinue the treatment [4].<br />
Hematological abnormalities (neutropenia, anemia and<br />
thrombocytopenia) and depression are the most common<br />
causes <strong>of</strong> dose reduction.<br />
<strong>The</strong> maintenance <strong>of</strong> the dosages <strong>of</strong> medications used in<br />
the treatment <strong>of</strong> hepatitis C and <strong>of</strong> the recommended course<br />
<strong>of</strong> treatment are important for the effectiveness <strong>of</strong> the therapy,<br />
as shown in Figure 1 [6]. Dose reduction is associated with<br />
lowering the rate at which a sustained viral response (SVR) is<br />
achieved. Early identification and strategies for controlling<br />
adverse events are important in the prevention <strong>of</strong> moderate<br />
and severe complications. <strong>The</strong>se practices also attenuate the<br />
deleterious effects on the quality <strong>of</strong> life <strong>of</strong> patients and maximize<br />
the effectiveness <strong>of</strong> treatment for hepatitis C.<br />
Constitutional Symptoms<br />
Constitutional symptoms such as fatigue, headache and<br />
myalgia are the most common adverse events in patients<br />
Figure 1. Effect <strong>of</strong> dose reduction <strong>of</strong> pegylated interferon<br />
(PEG-IFN) and ribavirin (RBV) in relation to the sustained<br />
viral response (SVR) rate.<br />
Table 1. Adverse events associated with using the pegylated<br />
interferon-ribavirin combination in the treatment <strong>of</strong> hepatitis C<br />
Adverse event<br />
Approximate<br />
incidence (%)<br />
Reaction at the site <strong>of</strong> injection 36-58<br />
Fatigue 50-64<br />
Headache 50-62<br />
Myalgia 42-56<br />
Fever 43-56<br />
Chills 24-48<br />
Alopeica 28-36<br />
Artralgia 27-35<br />
Irritability 24-35<br />
Depression 21-34<br />
Anorexia 14-32<br />
Dermatitis 16-21<br />
Anemia 12-22<br />
Neutropenia 17-20<br />
Thrombocytopenia 3-6<br />
<strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> 2007;11 (5) Suppl. 1:74-78.<br />
© 2007 by <strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> and Contexto<br />
Publishing. All rights reserved.<br />
treated with the combination <strong>of</strong> IFN and RBV (Table 1).<br />
Practically all patients manifest at least one such event during<br />
the administration <strong>of</strong> the initial doses <strong>of</strong> IFN. <strong>The</strong>se symptoms<br />
typically disappear or become less intense after the first month<br />
<strong>of</strong> treatment. Paracetamol, acetaminophen and ibupr<strong>of</strong>en taken<br />
immediately before the injection <strong>of</strong> IFN alleviate the symptoms.<br />
Adequate hydration, together with light to moderate exercise,<br />
can help minimize these side effects.<br />
Hematological Effects<br />
In approximately 25% <strong>of</strong> patients, it is necessary at least<br />
to reduce the dosage <strong>of</strong> IFN or RBV due to abnormalities in<br />
laboratory test results [4]. Conventional IFN and PEG-IFN<br />
have both been associated with the suppression <strong>of</strong><br />
hematopoiesis. In addition, hemolytic anemia occurs in all<br />
patients treated with RBV, although the intensity <strong>of</strong> that anemia<br />
is variable.<br />
Anemia<br />
Anemia resulting from the treatment <strong>of</strong> hepatitis C is a<br />
multifactorial side effect. Those factors increase the<br />
destruction <strong>of</strong> red blood cells and reduce their production.<br />
<strong>The</strong> increased destruction <strong>of</strong> red blood cells occurs due to<br />
hemolysis triggered by RBV, and the reduction in red blood<br />
www.bjid.com.br
BJID 2007; 11 Supplement 1 (October) Adverse Event Management<br />
75<br />
cell production occurs due to IFN-induced suppression <strong>of</strong><br />
bone marrow erythroid precursors [7,8].<br />
<strong>The</strong> RBV penetrates erythrocytes, in which<br />
monophosphate, diphosphate and triphosphate are<br />
phosphorylated. Those pharmacologically active forms are<br />
incapable <strong>of</strong> passing through the erythrocyte membrane, and<br />
so remain intracellularly retained at a concentration 60 times<br />
greater than that <strong>of</strong> plasma [7,8]. <strong>The</strong> accumulated<br />
phosphorylated derivates are slowly eliminated from the<br />
erythrocytes, which have a half-life <strong>of</strong> 40 days. In contrast,<br />
the elimination <strong>of</strong> RBV from plasma is rapid, since it has a halflife<br />
<strong>of</strong> 24 hours.<br />
<strong>The</strong> mechanisms by which IFN can exacerbate RBVinduced<br />
anemia include suppression <strong>of</strong> hematopoiesis in bone<br />
marrow and an increase in the destruction <strong>of</strong> erythroid<br />
precursor cells [9].<br />
Anemia starts and develops almost immediately after<br />
the initiation <strong>of</strong> therapy, becoming more intense after 4 to 6<br />
weeks <strong>of</strong> treatment. <strong>The</strong> average decrease in the level <strong>of</strong><br />
hemoglobin (Hb) is 2.5 to 3.0 g/dL, but more intense degrees<br />
<strong>of</strong> hemolysis can occur. Anemia associated with combined<br />
therapy can exacerbate other side effects resulting from<br />
the treatment <strong>of</strong> hepatitis C such as dyspnea, fatigue,<br />
dizziness and headache.<br />
Non-pharmacological control <strong>of</strong> the treatment <strong>of</strong> anemia<br />
involves dose reduction or permanent discontinuation <strong>of</strong> RBV<br />
[9]. In patients without heart disease, a reduction in the dosage<br />
<strong>of</strong> ribavirin when the levels <strong>of</strong> Hb fall below 10 g/dL is<br />
recommended, and discontinuation is recommended when Hb<br />
levels are under 8.5 g/dL (Table 2) [10]. Those<br />
recommendations are more restricted to patients with stable<br />
heart disease. In rare cases, when the level <strong>of</strong> Hb is lower than<br />
8.5 g/dL, a transfusion <strong>of</strong> packed red blood cells, in<br />
conjunction with discontinuation <strong>of</strong> the treatment for hepatitis<br />
C, might be necessary.<br />
Between 9 and 22% <strong>of</strong> patients receiving combined<br />
treatment for hepatitis C require an RBV dose reduction due<br />
to anemia [3,4].<br />
However, the strategy <strong>of</strong> RBV dose reduction has been<br />
associated with a modest increase in the level <strong>of</strong> Hb (˜1 g/dL)<br />
at 4-8 weeks after the reduction, as well as with a decrease in<br />
the rate at which an SVR is achieved (Figure 1) [6,11].<br />
Hematopoietic growth factors such as alpha erythropoietin<br />
can be an alternative in relation to RBV dose reduction for the<br />
treatment <strong>of</strong> anemia arising during the treatment <strong>of</strong> hepatitis C.<br />
Alpha erythropoietin is a synthetic glycoprotein that has a<br />
mechanism <strong>of</strong> action similar to that <strong>of</strong> endogenous erythropoietin,<br />
which is a hormone produced by the renal peritubular capillaries<br />
that stimulates erythropoiesis in bone marrow.<br />
Studies indicate that therapy with erythropoietin at the<br />
dosage <strong>of</strong> 40,000 IU once a week elevates the level <strong>of</strong> Hb after<br />
one week <strong>of</strong> use and thus permits the maintenance <strong>of</strong> RBV<br />
dosage in patients that become anemic during combined<br />
therapy for hepatitis C [12,13]. In the study conducted by<br />
Afdhal et al., the initial dose <strong>of</strong> RBV was maintained in 88% <strong>of</strong><br />
the patients who received erythropoietin during treatment for<br />
hepatitis C, and Hb levels increased (from 10.6 ± 0.9 to 13.2 ±<br />
1.2 g/dL) in those same patients [13]. <strong>The</strong> initial dose <strong>of</strong> RBV<br />
was maintained in 66% <strong>of</strong> the patients who received a placebo.<br />
<strong>The</strong> cost <strong>of</strong> alpha erythropoietin is high, but it is a therapeutic<br />
option for patients who develop an Hb level < 10 g/dL during<br />
treatment <strong>of</strong> hepatitis C [14].<br />
Neutropenia<br />
A decrease in neutrophil counts to below normal values<br />
occurs in the majority <strong>of</strong> patients receiving conventional IFN<br />
or PEG-IFN and results from the suppression <strong>of</strong> bone marrow<br />
caused by those medications [15]. Neutropenia (neutrophil<br />
count
76 Adverse Event Management<br />
BJID 2007; 11 Supplement 1 (October)<br />
Table 2. Dose modifications for adverse events resulting from therapy with interferon and ribavirin according to manufacturer<br />
recommendations<br />
Hematological parameters PEG-IFN-α 2b PEG-IFN-α 2a IFN RBV<br />
Hemoglobin a
BJID 2007; 11 Supplement 1 (October) Adverse Event Management<br />
77<br />
bone marrow suppression. A drop in platelet counts during<br />
combined treatment for hepatitis C is common, but IFN dose<br />
reduction or discontinuation <strong>of</strong> treatment as a result <strong>of</strong> that<br />
drop is uncommon [2,3]. Thrombocytopenia requiring IFN<br />
dose reduction is more common in patients treated with PEG-<br />
IFN and RBV than in those treated with conventional IFN and<br />
RBV, with frequency rates <strong>of</strong> 4% and 1%, respectively [18].<br />
Recommendations for the discontinuation <strong>of</strong> PEG-IFN or<br />
conventional IFN as a result <strong>of</strong> thrombocytopenia are shown<br />
in Table 2. Platelet counts generally return to pretreatment<br />
levels by 4 weeks after the discontinuation <strong>of</strong> treatment [2].<br />
<strong>The</strong>re are ongoing studies that aim to evaluate the effectiveness<br />
and safety <strong>of</strong> growth factors that stimulate the production<br />
and maturation <strong>of</strong> megakaryocytes in thrombocytopenic<br />
patients undergoing treatment for hepatitis C.<br />
Rare cases <strong>of</strong> autoimmune thrombocytopenic purpura have<br />
been described during the treatment for hepatitis C, and the<br />
presence <strong>of</strong> that disorder should be investigated in rare cases<br />
involving an intense decrease in platelet counts.<br />
Neuropsychiatric Symptoms<br />
Approximately 20% to 30% <strong>of</strong> patients report depressive<br />
symptoms during treatment for hepatitis C [19]. <strong>The</strong> control <strong>of</strong><br />
depression in patients who are candidates to receive treatment<br />
for hepatitis C is shown in Figure 2 [20]. In the pretreatment<br />
phase, it is important to establish the psychiatric status <strong>of</strong> the<br />
patient, which involves determining whether there is a history<br />
<strong>of</strong> depression, assessing the mood state and identifying abuse<br />
<strong>of</strong> illegal substances. Patients who abuse drugs or who have a<br />
complex psychiatric history involving disorders such as<br />
schizophrenia and bipolar disorder or who are receiving<br />
psychiatric treatment should be jointly accompanied by a<br />
psychiatrist during treatment for hepatitis C. Patients with<br />
current or previous depression should be evaluated before the<br />
initiation <strong>of</strong> treatment for hepatitis C, preferably through the<br />
use <strong>of</strong> scales that infer the intensity <strong>of</strong> depression. In patients<br />
with moderate depression, antidepressant medication can be<br />
given 4 weeks before the initiation <strong>of</strong> treatment for hepatitis C.<br />
Antidepressants belonging to a class <strong>of</strong> selective<br />
serotonin reuptake inhibitors (SSRIs) constitute the treatment<br />
<strong>of</strong> choice for IFN-associated depression [19]. Such<br />
antidepressants are safe and well-tolerated in patients with<br />
hepatic disease. In addition, the treatment success rate in<br />
patients with depression during treatment for hepatitis C is<br />
near 90% [18]. Fluoxetine, sertraline, citalopram, paroxetine<br />
and other SSRIs can have a slightly sedative effect, and the<br />
choice <strong>of</strong> SSRI to be used should be based on that effect and<br />
on the predominant symptomatology <strong>of</strong> the patient [21]. In<br />
patients with fatigue or cognitive slowness, fluoxetine or<br />
sertraline can be preferred over paroxetine, which tends to be<br />
less stimulating. In case <strong>of</strong> suicidal ideation or attempted<br />
suicide, the treatment <strong>of</strong> hepatitis C should be immediately<br />
suspended [22]. <strong>The</strong> dose <strong>of</strong> antidepressant medication started<br />
during treatment <strong>of</strong> hepatitis C should be slowly reduced over<br />
a 6 to 12 month period after the end <strong>of</strong> the treatment.<br />
Thyroid Disease<br />
Approximately 1-6% <strong>of</strong> individuals treated with IFN<br />
develop thyroid abnormalities [23]. In all patients, an<br />
evaluation <strong>of</strong> thyroid function is recommended. Levels <strong>of</strong><br />
thyroid-stimulating hormone should be determined before the<br />
initiation <strong>of</strong> treatment for hepatitis C, every 12 weeks during<br />
treatment and once after the end <strong>of</strong> the treatment. Individuals<br />
who develop hypothyroidism while undergoing treatment<br />
should receive hormonal replacement therapy.<br />
Pulmonary Side Effects<br />
Dry cough, which can occur during treatment, has been<br />
associated with the use <strong>of</strong> RBV. In most cases the cough is<br />
tolerable, but occasionally it is necessary to discontinue the<br />
use <strong>of</strong> RBV. Cases in which cough becomes productive or is<br />
accompanied by abnormal pulmonary auscultation findings<br />
or fever, pneumonia should be investigated. Interstitial<br />
pneumonia can be severe, but it is normally reversible with<br />
the discontinuation <strong>of</strong> therapy [19].<br />
Retinopathy<br />
<strong>The</strong> use <strong>of</strong> IFN can trigger or aggravate prior retinopathy.<br />
Subconjunctival hemorrhage and retinal hemorrhage have<br />
been reported during treatment with IFN [19]. Patients with<br />
risk factors for retinopathy such as systemic arterial<br />
hypertension and diabetes mellitus should undergo<br />
ophthalmological examination before and during therapy under<br />
the supervision <strong>of</strong> an ophthalmologist. Treatment should be<br />
discontinued in individuals who present either retinal lesions<br />
during treatment or the worsening <strong>of</strong> a prior lesion.<br />
References<br />
1. Maddrey W.C. Safety <strong>of</strong> combination interferon alfa-2b/ribavirin<br />
therapy in chronic hepatitis C-relapsed and treatment-naive<br />
patients. Semin Liver Dis 1999;19 Suppl 1:67-75.<br />
2. Fried M.W. Side effects <strong>of</strong> therapy <strong>of</strong> hepatitis C and their<br />
management. Hepatology 2002;36(5 Suppl 1):S237-44.<br />
3. Manns M.P., McHutchison J.G., Gordon S.C., et al. Peginterferon<br />
alfa-2b plus ribavirin compared with interferon alfa-2b plus<br />
ribavirin for initial treatment <strong>of</strong> chronic hepatitis C: a<br />
randomised trial. Lancet 2001;22:958-65.<br />
4. Fried M.W., Hadziyannis S.J. Treatment <strong>of</strong> chronic hepatitis C<br />
infection with peginterferons plus ribavirin. Semin Liver Dis<br />
2004;24 Suppl 2:47-54.<br />
5. Hadziyannis S.J., Sette H. Jr., Morgan T.R., et al. Peginterferonalpha2a<br />
and ribavirin combination therapy in chronic hepatitis<br />
C: a randomized study <strong>of</strong> treatment duration and ribavirin dose.<br />
Ann Intern Med 2004;2;140(5):346-55.<br />
6. Shiffman M.L., Di Bisceglie A.M., Lindsay K.L., et al. Hepatitis C<br />
Antiviral Long-Term Treatment Against Cirrhosis Trial Group.<br />
Peginterferon alfa-2a and ribavirin in patients with chronic<br />
hepatitis C who have failed prior treatment. Gastroenterology<br />
2004;126(4):1015-23.<br />
7. Bodenheimer H.C. Jr., Lindsay K.L., Davis G.L., et al. Tolerance<br />
and efficacy <strong>of</strong> oral ribavirin treatment <strong>of</strong> chronic hepatitis C:<br />
a multicenter trial. Hepatology 1997;26(2):473-7.<br />
8. De Franceschi L., Fattovich G., Turrini F., et al. Hemolytic anemia<br />
induced by ribavirin therapy in patients with chronic hepatitis<br />
C virus infection: role <strong>of</strong> membrane oxidative damage.<br />
Hepatology 2000;31(4):997-1004.<br />
www.bjid.com.br
78 Adverse Event Management<br />
BJID 2007; 11 Supplement 1 (October)<br />
9. Kowdley K.V. Hematologic side effects <strong>of</strong> interferon and ribavirin<br />
therapy. J Clin Gastroenterol 2005;39(1 Suppl):S3-8.<br />
10. Afdhal N.H. Role <strong>of</strong> epoetin alfa in maintaining ribavirin dose.<br />
Gastroenterol Clin North Am 2004;33(1 Suppl):S25-35.<br />
11. Sulkowski M.S., Wasserman R., Brooks L., et al. Changes in<br />
haemoglobin during interferon alpha-2b plus ribavirin<br />
combination therapy for chronic hepatitis C virus infection. J<br />
Viral Hepat 2004;11(3):243-50.<br />
12. Dieterich D.T., Wasserman R., Brau N., et al. Once-weekly epoetin<br />
alfa improves anemia and facilitates maintenance <strong>of</strong> ribavirin<br />
dosing in hepatitis C virus-infected patients receiving ribavirin<br />
plus interferon alfa. Am J Gastroenterol 2003;98(11):2491-9.<br />
13. Afdhal N.H., Dieterich D.T., Pockros P.J., et al. Epoetin alfa<br />
maintains ribavirin dose in HCV-infected patients: a prospective,<br />
double-blind, randomized controlled study. Gastroenterology<br />
2004;126(5):1302-11.<br />
14. Devine E.B., Kowdley K.V., Veenstra D.L., Sullivan S.D.<br />
Management strategies for ribavirin-induced hemolytic anemia<br />
in the treatment <strong>of</strong> hepatitis C: clinical and economic<br />
implications. Value Health 2001;4(5):376-84.<br />
15. Collantes R.S., Younossi Z.M. <strong>The</strong> use <strong>of</strong> growth factors to manage<br />
the hematologic side effects <strong>of</strong> PEG-interferon alfa and ribavirin.<br />
J Clin Gastroenterol 2005;39(1 Suppl):S9-13.<br />
16. Sulkowski M.S. Management <strong>of</strong> the hematologic complications<br />
<strong>of</strong> hepatitis C therapy. Clin Liver Dis 2005;9(4):601-16.<br />
17. Soza A., Everhart J.E., Ghany M.G., et al. Neutropenia during<br />
combination therapy <strong>of</strong> interferon alfa and ribavirin for chronic<br />
hepatitis C. Hepatology 2002;36(5):1273-9.<br />
18. Aspinall R.J., Pockros P.J. <strong>The</strong> management <strong>of</strong> side-effects during<br />
therapy for hepatitis C. Aliment Pharmacol <strong>The</strong>r<br />
2004;20(9):917-29.<br />
19. Russo M.W., Fried M.W. Side effects <strong>of</strong> therapy for chronic hepatitis<br />
C. Gastroenterology 2003;124(6):1711-9.<br />
20. Raison C.L., Demetrashvili M., Capuron L., Miller A.H.<br />
Neuropsychiatric adverse effects <strong>of</strong> interferon-alpha:<br />
recognition and management. CNS Drugs 2005;19(2):105-23.<br />
21. Edwards J.G., Anderson I. Systematic review and guide to selection<br />
<strong>of</strong> selective serotonin reuptake inhibitors. Drugs<br />
1999;57(4):507-33.<br />
22. Janssen H.L., Brouwer J.T., van der Mast R.C., Schalm S.W. Suicide<br />
associated with alfa-interferon therapy for chronic viral<br />
hepatitis. J Hepatol 1994;21(2):241-3.<br />
23. Huang M.J., Tsai S.L., Huang B.Y., et al. Prevalence and significance<br />
<strong>of</strong> thyroid autoantibodies in patients with chronic hepatitis C<br />
virus infection: a prospective controlled study. Clin Endocrinol<br />
(Oxf) 1999;50(4):503-9.<br />
www.bjid.com.br
BJID 2007; 11 Supplement 1 (October) 79<br />
Treatment Options in the Management <strong>of</strong> Thrombocytopenia in Patients Infected with HCV<br />
André Cosme de Oliveira<br />
Liver Transplant Section <strong>of</strong> the Clinical Hospital <strong>of</strong> University <strong>of</strong> São Paulo School <strong>of</strong> Medicine (HC-FMUSP); São Paulo, SP, Brazil<br />
Thrombocytopenia (platelet count < 80,000/mm 3 ) in<br />
patients with chronic hepatitis has been associated with two<br />
factors: the first is hypersplenism resulting from splenomegaly<br />
in portal hypertension [1]. <strong>The</strong> spleen continuously<br />
sequesters one-third <strong>of</strong> circulating platelets, so that<br />
splenomegaly increases the fraction <strong>of</strong> platelets trapped in<br />
the splenic sinusoids, especially when resulting from passive<br />
congestion or an increase in venous portal pressure [1].<br />
Hypersplenism seems to be the most common cause <strong>of</strong><br />
thrombocytopenia associated with liver cirrhosis and portal<br />
hypertension.<br />
<strong>The</strong> second mechanism is related to the decreased<br />
production <strong>of</strong> thrombopoietin, a hormone produced by<br />
hepatocytes, which regulates the development <strong>of</strong> the<br />
megakaryocyte. In cirrhosis, due to the reduction in the mass<br />
<strong>of</strong> functioning hepatocytes, there can be a reduction <strong>of</strong><br />
thrombopoiesis in the bone marrow, leading to<br />
thrombocytopenia in the peripheral blood [1].<br />
In some situations, patients who are otherwise eligible for<br />
HCV treatment with interferon and ribavirin cannot be so<br />
treated because their platelets counts are low, which<br />
jeopardizes the treatment [2,3].<br />
Nevertheless, hepatitis C patients treated with interferon and<br />
ribavirin also present a drop in the platelet count as a side<br />
effect [2,3].<br />
<strong>The</strong>re is as yet no treatment consensus in the literature for<br />
the management <strong>of</strong> these patients. We therefore present some<br />
related studies that address the management <strong>of</strong> these patients,<br />
in the pre-treatment and intra-treatment phases.<br />
Patients receiving interferon alpha or peginterferon alpha<br />
can present a 30-50% reduction in the baseline platelet count,<br />
and a dose reduction is necessary in approximately 4% <strong>of</strong> the<br />
patients [2,3]. We should consider possible reduction <strong>of</strong> the<br />
dose when platelet counts drop to < 50,000/mm 3 , and<br />
discontinuation <strong>of</strong> treatment when < 25,000/mm 3 .<br />
When using peginterferon alpha-2, the weekly dose can<br />
be reduced from 180 μg to 135 μg, or even to 90 μg. While<br />
using peginterferon alpha-2b, the weekly dose can be reduced<br />
from 1.5 μg/kg to 1.0 μg/kg, or even to 0.5 μg/kg [2,3].<br />
Human recombinant interleukin (IL)-11 (oprelvekin,<br />
Neumega ® ; Wyeth Laboratories, Collegeville, PA, USA) can<br />
be used as a way to stimulate the increase in the number <strong>of</strong><br />
platelets at a dose <strong>of</strong> 5 μg/kg/day, subcutaneously, initially<br />
for 7 days. If necessary, maintenance can consist <strong>of</strong> 1 to 3<br />
doses per week during HCV drug therapy, similarly to what is<br />
recommended for filgrastim (granulocyte colony-stimulating<br />
factor) [4].<br />
<strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> 2007;11 (5) Suppl. 1:79-80.<br />
© 2007 by <strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> and Contexto<br />
Publishing. All rights reserved.<br />
Administration <strong>of</strong> IL-11 has multiple effects on the<br />
hematopoietic system, specifically promoting the proliferation<br />
and maturation <strong>of</strong> megakaryocytes and inducement <strong>of</strong><br />
neutrophilia and thrombocytosis [5].<br />
In patients with cirrhosis, its use should be restricted to<br />
those with Child-Pugh class A or B cirrhosis [5].<br />
In a study conducted by Ghalib et al. [6], none <strong>of</strong> the<br />
patients presented increased platelet counts until day 4 <strong>of</strong><br />
daily use <strong>of</strong> the medication, and the maximal therapeutic<br />
response was observed near day 13 (Figure 1). At 6 to 8 days<br />
after the initiation <strong>of</strong> treatment, 89% <strong>of</strong> the patients presented<br />
duplication <strong>of</strong> the initial number <strong>of</strong> platelets, and 78% <strong>of</strong> the<br />
patients presented platelet counts > 80,000/mm 3 .<br />
Another treatment option for thrombocytopenia in these<br />
patients is splenic embolization.<br />
Figure 1. Ratio between platelet counts and duration <strong>of</strong><br />
treatment with interleukin-11.<br />
Splenic embolization should preferably be performed with<br />
injection <strong>of</strong> polyvinyl alcohol particles between 355 and 500<br />
µm (Trufill PVA Embolization Particles; Cordis Corp., Johnson<br />
& Johnson Co., Miami Lakes, FL, USA) into the splenic artery<br />
and should not exceed an embolization volume <strong>of</strong> 30% <strong>of</strong> the<br />
initial spleen volume [7].<br />
<strong>The</strong> most severe complications after embolization can be<br />
ascites, thrombosis <strong>of</strong> the splenic vein or portal vein,<br />
spontaneous bacterial peritonitis, and splenic abscess.<br />
Abdominal pain and fever are typically present postembolization<br />
[8].<br />
Splenic embolization presented 50% <strong>of</strong> complication in<br />
embolizations < 30% <strong>of</strong> splenic volume, whereas, in<br />
embolizations > 30%, 100% <strong>of</strong> the patients presented<br />
complications [9].<br />
Abdominal computed tomography scans can be performed<br />
2 to 3 weeks after embolization for assessment <strong>of</strong> effectiveness<br />
<strong>of</strong> the procedure and to identify complications [10].<br />
www.bjid.com.br
80 Thrombocytopenia in Patients Infected with HCV<br />
BJID 2007; 11 Supplement 1 (October)<br />
All patients should be previously vaccinated against<br />
pneumococci before embolization. In addition, antibiotic<br />
therapy should be initiated and maintained during<br />
hospitalization <strong>of</strong> the patient. We suggest the use <strong>of</strong> cefotaxime<br />
and ampicillin in these cases [11]. <strong>The</strong> combined treatment<br />
with interferon and ribavirin should not be initiated or reinitiated<br />
until 8 weeks after splenic embolization [12].<br />
<strong>The</strong> use <strong>of</strong> human recombinant interleukin-11 (IL-11)<br />
(oprelvekin) and splenic embolization are both feasible<br />
treatments for these patients, taking into account the<br />
characteristics <strong>of</strong> the individual health care facilities at which<br />
the follow-up treatment is administered.<br />
References<br />
1. Moreno A., Bárcena R., Blázquez J., et al. Thrombocytopenia can<br />
be found in patients with chronic hepatitis related to hepatitis C<br />
virus (HCV). Both hypersplenism and decreased liver production<br />
<strong>of</strong> thrombopoietin (TPO) have been hypothesized as<br />
mechanisms responsible for thrombocytopenia. Hospital Ramón<br />
y Cajal, Madrid, Spain.<br />
2. Manns M.P., et al. Peginterferon alfa-2b plus ribavirin compared<br />
with interferon alfa-2b plus ribavirin for initial treatment <strong>of</strong> chronic<br />
hepatitis C: a randomised trial. Lancet 2001;358:958-65.<br />
3. Fried M.W. Peginterferon alfa-2a plus ribavirin for chronic hepatitis<br />
C virus infection. N Engl J Med 2002;347:975-82.<br />
4. Hennepin County Medical Center. Management <strong>of</strong> HCV and<br />
treatment side effects. April 10, 2005.<br />
5. Lawitz E., Hepburn M., Casey T. A Pilot Study <strong>of</strong> Interleukin-<br />
11 in Subjects with Chronic Hepatitis C and Advanced Liver<br />
Disease Nonresponsive to Antiviral <strong>The</strong>rapy.<br />
Gastroenterology Service; <strong>Infectious</strong> <strong>Diseases</strong> Service;<br />
Pathology Department; Brooke Army Medical Center, San<br />
Antonio, Texas.<br />
6. Ghalib R., Levine C., Hassan M., et al. Recombinant Human<br />
Interleukin-11 Improves Thrombocytopenia in Patients With<br />
Cirrhosis. Hepatology 2003:1165-71.<br />
7. Zhu K., Meng X., Li Z., et al. Partial splenic embolization using<br />
polyvinyl alcohol particles for hypersplenism in cirrhosis: A<br />
prospective randomized study. Eur J Radiol 2007;24.<br />
8. Lee C.M., Leung T.K., Wang H.J., et al. Evaluation <strong>of</strong> the effect<br />
<strong>of</strong> partial splenic embolization on platelet values for liver<br />
cirrhosis patients with thrombocytopenia. World J<br />
Gastroenterol 2007;13(4):619-22.<br />
9. Hayashi H., Beppu T., Masuda T., et al. Predictive factors for<br />
platelet increase after partial splenic embolization in liver<br />
cirrhosis patients. J Gastroenterol Hepatol 2007;7.<br />
10. Lee C.M., Leung T.K., Wang H.J., et al. Evaluation <strong>of</strong> the effect<br />
<strong>of</strong> partial splenic embolization on platelet values for liver<br />
cirrhosis patients with thrombocytopenia. World J<br />
Gastroenterol 2007;13(4):619-22.<br />
11. Foruny J.R., Blázquez J., Moreno A., et al. Safe use <strong>of</strong> pegylated<br />
interferon/ribavirin in hepatitis C virus cirrhotic patients with<br />
hypersplenism after partial splenic embolization. Eur J<br />
Gastroenterol Hepatol 2005;17(11):1157-64.<br />
12. Pålsson B., Verbaan H. Partial splenic embolization as pretreatment<br />
for antiviral therapy in hepatitis C virus infection. Eur J<br />
Gastroenterol Hepatol 2005;17(11):1153-5.<br />
www.bjid.com.br
BJID 2007; 11 Supplement 1 (October) 81<br />
<strong>The</strong>rapeutic Perspectives for Hepatitis C<br />
OVERVIEW<br />
Evaldo Stanislau Affonso de Araújo and Antonio Alci Barone<br />
Laboratory <strong>of</strong> Hepatitis, LIM 47 DMIP-HC-FMUSP; São Paulo, SP, Brazil<br />
NEW THERAPIES FOR HEPATITIS C<br />
Jean-Michel Pawlotsky<br />
French National Reference Center for Viral Hepatitis B, C and Delta; Department <strong>of</strong> Virology,<br />
and INSERM U841, Hôpital Henri Mondor, Université Paris 12, Créteil, France<br />
Overview<br />
Hepatitis C virus (HCV) is represented by a single open<br />
reading frame <strong>of</strong> single-stranded RNA comprising<br />
approximately 3000 AA, positioned between 3’ and 5’<br />
noncoding extremities. Transcription from the 5’ end results<br />
in a compound polyprotein, generated by structural proteins<br />
in the amino-terminal region extremity and by nonstructural<br />
proteins in the opposing terminal region. Post-transcription<br />
cleavage by viral and host cell proteases generates 10<br />
individual HCV proteins [1]. <strong>The</strong> HCV cDNA clone was first<br />
described in 1989. Subsequently, counter to the expectations<br />
<strong>of</strong> an enormous breakthrough, there was a hiatus in the growth<br />
<strong>of</strong> knowledge regarding the molecular virology <strong>of</strong> this virus.<br />
Only in 1997 was the first functioning and complete HCV cDNA<br />
clone described and used in animal models (chimpanzees) for<br />
preliminary analyses <strong>of</strong> the viral expression using<br />
biotechnological tools. A milestone in the study <strong>of</strong> viral<br />
molecular biology was the description, in 1999, <strong>of</strong> a viral culture<br />
model in tumor cells (Huh 7) using a HCV 1b subgenomic<br />
replicon. Based on this model, despite strict limitations, other<br />
viral fragments were used in order to evaluate the dynamics<br />
<strong>of</strong> viral replication in different settings and with exposure to<br />
antiviral agents. Nevertheless, the inability to obtain a complete<br />
HCV sequence remains an obstacle to be overcome [1].<br />
One characteristic <strong>of</strong> HCV is that is has minimal cytopathic<br />
effects, with immunomediated hepatotropic injury. However,<br />
it is also found in extrahepatic sites, where it has a short halflife<br />
(approximately 3 hours) and high serum turnover [2].<br />
Standard treatment involves the administration <strong>of</strong> pegylated<br />
interferon alpha together with ribavirin. This treatment regimen<br />
has had modest success, a little over 50% [3], reaching 71% in<br />
cases <strong>of</strong> dose optimization and full compliance [4]. However,<br />
it could be much less, if we consider real life data, as well as<br />
characteristics <strong>of</strong> the host (race, comorbidities, immune state),<br />
<strong>of</strong> the liver disease (level <strong>of</strong> fibrosis and steatosis), <strong>of</strong> the<br />
medication (dose, interferon type) and <strong>of</strong> the virus itself. In<br />
addition, it is well known that genotype 1 has a lower response<br />
rate, and certain viral proteins can subvert the stimulus induced<br />
by interferon and ribavirin [3]. Viral kinetics, the evaluation <strong>of</strong><br />
the decay pattern <strong>of</strong> the viremia – in terms <strong>of</strong> intensity and<br />
<strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> 2007;11 (5) Suppl. 1:81-87.<br />
© 2007 by <strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> and Contexto<br />
Publishing. All rights reserved.<br />
speed – after the initiation <strong>of</strong> the therapy, has proven to be a<br />
useful tool in the management <strong>of</strong> patients. It demonstrates<br />
the interaction among virus, drug, and host, in a relatively<br />
simple way: intense, rapid decay indicates a favorable case;<br />
insignificant, slow decay indicates cases that are unfavorable,<br />
moderate or intermediate. Such kinetic patterns allow<br />
patients to be characterized as rapid responders, slow<br />
responders, or nonresponders. This approach allows the<br />
treatment to be individualized, with ideal doses per weight<br />
and shorter, standard, or extended duration. In addition, it<br />
allows early prediction <strong>of</strong> treatment response. <strong>The</strong>refore,<br />
individualized therapy constitutes the best therapeutic tool<br />
at the moment [5].<br />
Of course, for the sake <strong>of</strong> effectiveness, safety, and<br />
tolerability, the current therapy is insufficient to confront the<br />
present hepatitis C epidemic. <strong>The</strong>refore, from a therapy with<br />
poorly understood mechanisms <strong>of</strong> action that function<br />
through essentially indirect means [6], we have evolved to<br />
the specifically targeted antiviral therapy for hepatitis C [7],<br />
that is, the search for compounds that have a direct effect on<br />
the HCV life cycle. However, the preliminary results <strong>of</strong> current<br />
clinical studies have demonstrated worrisome aspects<br />
regarding safety, tolerability, and efficacy for some <strong>of</strong> these<br />
compounds [7], which is why we believe that treatment with<br />
interferon alpha will continue to lead the field for many years<br />
to come, and studies involving combinations <strong>of</strong> new<br />
compounds including interferon and, occasionally, ribavirin<br />
are already underway. A good example <strong>of</strong> this fact are the<br />
preliminary results <strong>of</strong> the PROVE-1 study recently presented<br />
in Barcelona [8], in which the group that used the combination<br />
<strong>of</strong> pegylated interferon alpha-2a 180 μg + ribavirin 1-1.2 g +<br />
telaprevir 750 mg every 8 hours, in an intention-to-treat<br />
analysis, showed a markedly greater response than that<br />
observed for the control group (receiving pegylated interferon<br />
+ ribavirin), despite the fact that the subjects were infected<br />
with genotype 1. At week 4, 79% presented viremia < 10 IU/<br />
mL. At week 12, 70% presented viremia < 10 IU/mL, whereas<br />
39% presented viremia ≥ 10 IU/mL, emphasizing the loss <strong>of</strong><br />
cases and the intention-to-treat analysis. Nevertheless, the<br />
incidence <strong>of</strong> rash, gastrointestinal effects, and anemia was<br />
significantly higher in the telaprevir group.<br />
<strong>The</strong> new therapeutic options are divided into ‘smallmolecule’<br />
(protease and viral polymerase inhibitors and<br />
www.bjid.com.br
82 <strong>The</strong>rapeutic Perspectives for Hepatitis C<br />
BJID 2007; 11 Supplement 1 (October)<br />
protein inhibitors <strong>of</strong> the host – glucosidase) [9] – data<br />
summarized in Table 1 – and drugs whose targets are still<br />
indirect. In this second group, there are several that are<br />
currently in Phase I trials, specifically the Toll-like receptor<br />
agonists 7 and 9 (ANA 245 – Isatoribine – ANA 975 and<br />
Actilon) [10] whose mechanism <strong>of</strong> immune stimulation is<br />
broader than that induced by interferon alpha. <strong>The</strong> modulation<br />
<strong>of</strong> the inflammation and apoptosis by caspase inhibition is<br />
also under evaluation, and preliminary results demonstrate<br />
that aspartate aminotransferase normalizes in the patients who<br />
received it during trials ranging from Phase II to IDN-6556<br />
[11]. <strong>The</strong>re are other forms <strong>of</strong> interferon in phase I and II trials:<br />
albuferon (interferon alpha-2b fused to albumin, with more<br />
favorable posology regimen and similar efficacy to that <strong>of</strong><br />
pegylated interferon); omega interferon; gamma interferon;<br />
interferon for oral use; and oral interferon inducers<br />
(resiquimod and imiquimod). In addition, there are nucleoside<br />
analogs similar to ribavirin (viramidine, now known as<br />
taribavirin) in Phase III, inosine monophosphate<br />
dehydrogenase inhibitors– VX98-497 (merimepodib) in Phase<br />
II for previous nonresponders [12], mycophenolate m<strong>of</strong>etil,<br />
also in Phase II for nonresponders, broad spectrum antiviral<br />
agents in Phase II (amantadine and rimantadine) and other<br />
immunomodulators in Phases I to III (histamine, thymosin<br />
alpha-1, IL-10 and IL-12). Finally, therapeutic vaccines are<br />
being studied in pre-clinical phases (E1/E2) I or II (E1, NS3-<br />
NS4-NS5-core, IC41) [10].<br />
After a brief review <strong>of</strong> developing drugs, we should bear<br />
in mind the problems and disappointments already<br />
encountered regarding the resistance developed in vitro or in<br />
vivo, in addition to the already mentioned weaknesses related<br />
to posology tolerance and complexity. Posology regimens, as<br />
already described for HIV, can be facilitated by the association<br />
with the protease inhibitor ritonavir, acting as a potent<br />
inhibitor <strong>of</strong> the enzyme system function <strong>of</strong> cytochrome P450,<br />
which would enable, in preliminary analyses, simplified<br />
posology regimens for some <strong>of</strong> the small molecules [13].<br />
Regarding other problems, further review will bring up some<br />
relevant issues, in addition to the already evident necessary<br />
maintenance <strong>of</strong> interferon, and even ribavirin, in future<br />
therapeutic regimens.<br />
New <strong>The</strong>rapies for Hepatitis C<br />
<strong>The</strong> current standard <strong>of</strong> care for patients with chronic<br />
hepatitis C is the combination <strong>of</strong> pegylated interferon (IFN)<br />
alpha and ribavirin. This treatment is effective in<br />
approximately 80% <strong>of</strong> patients with hepatitis C virus (HCV)<br />
genotype 2 or 3 infection, but less than 50% <strong>of</strong> those with<br />
HCV genotype 1 [14]. Many new HCV drugs are at the<br />
preclinical developmental stage and several are in clinical<br />
development. Novel HCV therapies currently in development<br />
schematically belong to four categories: novel IFNs,<br />
alternatives to ribavirin, immune therapies, and specific and<br />
nonspecific inhibitors <strong>of</strong> the HCV lifecycle.<br />
Novel <strong>The</strong>rapies for Hepatitis C<br />
Novel IFNs<br />
New IFN alpha molecules are currently being developed.<br />
<strong>The</strong>y are expected to yield more potent antiviral effects, and<br />
eventually more potent immunomodulatory effects, with<br />
improved pharmacokinetic and pharmacodynamic properties<br />
and, if possible, better tolerance. <strong>The</strong> potential interest in nonalpha<br />
IFNs is also being studied.<br />
Albumin-linked IFN alpha<br />
Albumin-linked IFN alpha (Albuferon ® , Human Genome<br />
Sciences and Novartis) is an IFN alpha-2b molecule attached<br />
to a human albumin moiety which has a prolonged half-life<br />
that allows dosing at intervals <strong>of</strong> 2 to 4 weeks. Albumin-linked<br />
IFN alpha is able to induce an antiviral response in previous<br />
nonresponders to pegylated IFN and ribavirin combination.<br />
Results presented at the 42 nd Annual Meeting <strong>of</strong> the European<br />
Association for the Study <strong>of</strong> the Liver (EASL) have shown no<br />
significant difference in the rates <strong>of</strong> sustained virological<br />
response between patients receiving pegylated IFN alpha-2a<br />
and ribavirin or various doses <strong>of</strong> albumin-linked IFN alpha<br />
administered every two or four weeks with ribavirin.<br />
Consensus IFN alpha<br />
IFN alphacon-1 (Infergen, Amgen and InterMune-<br />
Yamanouchi) is a synthetic recombinant “consensus” IFN<br />
(cIFN) created by scanning the sequences <strong>of</strong> several natural<br />
alpha IFNs and assigning the most frequently observed amino<br />
acid in each corresponding position to the recombinant<br />
molecule [15]. <strong>The</strong>re is no clear evidence that cIFN is superior<br />
to other alpha IFNs when both are given in equivalent doses<br />
in terms <strong>of</strong> sustained virological response.<br />
Other alpha IFNs in development<br />
Multiferon (Viragen) is a highly purified, multi-subtype<br />
natural human IFN alpha derived from human leukocytes<br />
which has already been approved for use in HCV therapy in<br />
several countries. Medusa ® (Flamel Technologies) is a selfassembled<br />
poly-aminoacid nanoparticles system that can be<br />
used as a protein carrier for the development <strong>of</strong> novel longacting<br />
native protein drugs. Medusa IFN alpha-2a and Medusa<br />
IFN beta are currently in early clinical development. Various<br />
types <strong>of</strong> orally administered IFNs alpha are also currently<br />
being developed. Whether similar efficacy as with<br />
subcutaneous administration can be achieved is under study.<br />
Non-type I IFNs<br />
IFN omega, like IFN alpha or beta, is a type 1 IFN. It shares<br />
70% homology with IFN alpha and binds to the same receptor.<br />
A stable, glycosylated form <strong>of</strong> IFN omega has been developed<br />
(Intarcia) and has been administered to patients with chronic<br />
hepatitis C in phase I and II trials. <strong>The</strong> results <strong>of</strong> a phase II trial<br />
presented at the 42 nd EASL Annual Meeting have shown<br />
sustained virological response rates (HCV RNA below 50<br />
international units (IU)/mL at week 12 post-therapy) <strong>of</strong> 36% in<br />
www.bjid.com.br
BJID 2007; 11 Supplement 1 (October) <strong>The</strong>rapeutic Perspectives for Hepatitis C<br />
83<br />
Table 1. Developing drugs that have a direct effect on HCV (adapted from [7,10])<br />
Site <strong>of</strong> action<br />
Compound<br />
Commercial<br />
name<br />
Development<br />
phase<br />
Posology<br />
Comments<br />
Input inhibitors Anti HCV Immunoglobulin Civacir Phase II 200-400 mg/kg Poor preliminary results<br />
(HCIg)<br />
Monoclonal antibodies — Phase I — Transitory reduction <strong>of</strong><br />
(HCV-AB 68, HCV AB 65)<br />
viremia<br />
HCV-RNA Antisense oligonucleotides — Phase II Interrupted<br />
transcription ISIS 14803<br />
inhibitors AVI-4065 — Phase I Current<br />
RNA that catalyzes the Heptazyme Phase I — Interrupted<br />
cleavage <strong>of</strong> the target RNA<br />
(Ribozymes)<br />
IRES small-molecule VGX-410C Phase I — Current<br />
inhibitors<br />
Small Interfering RNA TT033 Pre-clinical — Parenteral use<br />
(siRNA) or short hairpin<br />
RNA (shRNA)<br />
Post-transcription Serum proteinase inhibitors BILN 2061 — — Interrupted<br />
processing to NS3-4A ACH-806/Gs-9132<br />
inhibitors VX-950 Phase II VO 450-750 mg PROVE –Telaprevir +<br />
(telaprevir) every 8 h RBV+PEG-IFN: 88%<br />
with RNA < 10 IU in 12<br />
without vs. 52% PEG+RBV<br />
Resistance<br />
Rash<br />
SCH 503034 Phase II VO 200-400 mg SCH+PEG-IFN-α-2b +<br />
(boceprevir) every 8 h RBV current<br />
ACH-806 — — Interrupted<br />
and GS-9132<br />
ITMN 191 Phase I — —<br />
ACH 1095 To initiate — —<br />
HCV replication Polymerase inhibitors NS5B Nucleoside NM283 VO Potent, but GI effects<br />
inhibitors (RdRp) analogs/ (Valopicitabine)<br />
Nucleotides –An.Nucleos.<br />
Phase II<br />
R1626 – VO Marked reduction<br />
An.Nucl. 1.5-4.5g PEG-IFN-RBV<br />
Phase II BID combination under study<br />
Anemia<br />
MK-0608<br />
Pre-clinical<br />
Non-nucleoside HCV-796 — Marked reduction<br />
inhibitors Phase II with PEG-IFN without resistance<br />
XTL 2125 Phase I<br />
R7128 Phase I<br />
Cyclophilin B inhibitors DEBIO-025 Phase I — Reduction <strong>of</strong> viremia<br />
NIM 811 Phase I<br />
NS5A inhibitors A 689 Pre-clinical — —<br />
A-831 Pre-clinical — —<br />
Helicase inhibitors QU633 — — —<br />
recombinant human antibodies<br />
Viral assembly Glucosidase inhibitor UT-231B Phase II future — Poor results<br />
and release (Iminosugar) MX-3253 Phase II — PEG-IFN/RBV<br />
(celgosivir)<br />
combination<br />
www.bjid.com.br
84 <strong>The</strong>rapeutic Perspectives for Hepatitis C<br />
BJID 2007; 11 Supplement 1 (October)<br />
the IFN omega-ribavirin combination arm versus 6% in patients<br />
treated with IFN omega alone. <strong>The</strong> manufacturer plans to<br />
develop an implantable infusion pump that will release a steady<br />
amount <strong>of</strong> IFN omega for approximately four weeks.<br />
In spite <strong>of</strong> in vitro results that would support a potentiating<br />
effect <strong>of</strong> IFN gamma on IFN alpha [16], the pro<strong>of</strong> <strong>of</strong> concept<br />
that IFN gamma could have a utility in the treatment <strong>of</strong> chronic<br />
hepatitis C still remains to be made.<br />
IFN lambda-1 (interleukin 29 or IL-29) is a member <strong>of</strong> a<br />
novel family <strong>of</strong> cytokines that are distantly related to the IL-<br />
10 family and type 1 IFNs. IFN lambda-1 exhibits dose- and<br />
time-dependent inhibition <strong>of</strong> HCV replication in various<br />
models, independent <strong>of</strong> types 1 and 2 IFN receptors and<br />
induced pathways [17]. A pegylated form <strong>of</strong> IFN lambda will<br />
soon enter clinical evaluation.<br />
Alternatives to Ribavirin<br />
Alternatives to ribavirin are needed that would have the same<br />
effects as ribavirin on infection in combination with pegylated<br />
IFN or other IFN molecules without its hemolytic properties.<br />
However, the challenge for discovering such molecules is<br />
hampered by the fact the antiviral mechanisms <strong>of</strong> ribavirin remain<br />
poorly understood. Taribavirin (Valeant Pharmaceuticals) is an<br />
amidine prodrug <strong>of</strong> ribavirin converted into ribavirin by adenosine<br />
deaminases, which are primarily present in hepatocytes.<br />
Taribavirin is thus preferentially taken up in the liver where it<br />
serves for ribavirin delivery to the major site <strong>of</strong> HCV replication,<br />
whereas it is not transported efficiently into red blood cells [18].<br />
In two recent phase III trials in combination with pegylated IFN<br />
alpha 2a and 2b, respectively, taribavirin at a flat dose <strong>of</strong> 600 mg<br />
twice a day failed to achieve similar efficacy as weight-based<br />
dosed ribavirin in patients with chronic hepatitis C <strong>of</strong> various<br />
genotypes. <strong>The</strong> incidence <strong>of</strong> hemolytic anemia was however<br />
significantly lower with taribavirin. New trials with higher doses<br />
<strong>of</strong> taribavirin have been planned.<br />
Immune <strong>The</strong>rapies<br />
Various nonspecific immunomodulatory agents, including<br />
thymosin alpha-1 (Thymalphasin, SciClone), IL-10 or histamine<br />
(Maxym Pharmaceuticals) have been administered to patients<br />
with chronic hepatitis C, with little success.<br />
Vaccines can induce CD4+ and CD8+ T-cell responses to<br />
HCV. Preclinical and early human studies indicate that<br />
therapeutic vaccines using different forms <strong>of</strong> recombinant HCV<br />
proteins together with various adjuvants could upregulate<br />
both cellular and humoral immune responses in patients with<br />
chronic hepatitis C [19]. However, there is currently no<br />
evidence that therapeutic vaccines alone can result in changes<br />
in HCV RNA levels. It remains to be determined whether<br />
therapeutic vaccines could be useful in combination with<br />
potent antiviral molecules.<br />
Inhibitors <strong>of</strong> the HCV Life Cycle<br />
Every step <strong>of</strong> the HCV lifecycle constitutes a potential target<br />
for specific or nonspecific antiviral molecules. Many drugs are<br />
at the preclinical developmental stage and several are in clinical<br />
development, but initial trials using some <strong>of</strong> these inhibitors<br />
alone have raised concerns about their tolerability and the<br />
development <strong>of</strong> viral resistance. A number <strong>of</strong> specifically targeted<br />
therapies are now also being tested in combination with<br />
pegylated IFN alpha with or without ribavirin.<br />
Inhibitors <strong>of</strong> the early steps <strong>of</strong> the HCV life cycle<br />
Inhibition <strong>of</strong> HCV entry can be based on the use <strong>of</strong> specific<br />
antibodies that neutralize infectious particles and prevent their<br />
attachment to the receptor molecules. <strong>The</strong>se include polyclonal<br />
hepatitis C immune globulins, that have been administered to<br />
prevent HCV infection in HCV-infected liver transplant recipients<br />
with little success [20], and anti-HCV monoclonal antibodies<br />
with high-affinity HCV neutralizing properties that reduce viral<br />
replication by 0.3 to 1.0 log [21,22]. Small molecule entry<br />
inhibitors can theoretically belong to two groups <strong>of</strong> drugs:<br />
molecules that specifically fix onto the HCV surface structures<br />
and neutralize the virus, or molecules that compete with<br />
infectious viral particles at the receptor level. Unfortunately,<br />
our understanding <strong>of</strong> HCV entry mechanisms remains<br />
rudimentary, hampering the development <strong>of</strong> such molecules<br />
inhibitors. Fusion could also become an interesting target for<br />
novel therapies when its mechanisms are better understood.<br />
HCV RNA translation inhibitors<br />
Several nucleic acid-based strategies have been tested,<br />
including antisense oligodeoxynucleotides,<br />
phosphorodiamidate morpholino oligomers (PMO), or<br />
ribozymes. All <strong>of</strong> them have been shown to potently inhibit<br />
HCV translation in vitro, but have been disappointing in vivo<br />
[23,24]. RNA interference initiated by small interfering RNAs<br />
(siRNA) or short hairpin RNAs (shRNA) is very specific and<br />
<strong>of</strong>fers a potential to be used as antiviral against HCV. However,<br />
because <strong>of</strong> their size and chemical composition, siRNAs and<br />
shRNAs currently are not orally bioavailable and require<br />
parenteral administration. Alternative strategies currently<br />
target the three-dimensional functional internal ribosome entry<br />
site (IRES) complexed with ribosomal subunits and viral and<br />
cellular proteins with small molecule inhibitors.<br />
Inhibitors <strong>of</strong> HCV post-translational processing<br />
Highly selective, potent peptidomimetic inhibitors <strong>of</strong> HCV<br />
NS3/4A proteinase have been designed. VX-950 or telaprevir<br />
(Vertex Pharmaceuticals) and SCH 503034 or boceprevir<br />
(Schering-Plough Corporation) have now advanced to phase<br />
II clinical trials. Patients who received 750 mg <strong>of</strong> telaprevir<br />
alone every 8 hours experienced a median 4.4-log reduction in<br />
HCV RNA levels [25]. <strong>The</strong> drug is well tolerated over shortterm<br />
administration. However, viral breakthroughs occur<br />
during the second week <strong>of</strong> telaprevir administration in patients<br />
with low exposure to the drug. <strong>The</strong>y are due to selection <strong>of</strong><br />
telaprevir-resistant variants. Combination with pegylated IFN<br />
alpha with or without ribavirin could theoretically at least partly<br />
prevent telaprevir resistance. This hypothesis is currently<br />
www.bjid.com.br
BJID 2007; 11 Supplement 1 (October) <strong>The</strong>rapeutic Perspectives for Hepatitis C<br />
85<br />
under study in two phase II trials. Boceprevir appears to have<br />
less potent antiviral properties than telaprevir in vivo at the<br />
doses used to date [26]. In combination, the antiviral effect <strong>of</strong><br />
boceprevir appears to be additive to that <strong>of</strong> pegylated IFN<br />
alpha-2b [26]. A phase II clinical trial is ongoing in combination<br />
with pegylated IFN alpha and ribavirin, where high doses <strong>of</strong><br />
boceprevir are administered to treatment-naïve patients.<br />
Other approaches have been developed to inhibit the NS3/<br />
4A serine proteinase function. ACH-806/GS-9132 (Achillion<br />
Pharmaceuticals and Gilead Sciences) inhibits binding <strong>of</strong><br />
NS4A to the NS3 proteinase, therefore inhibiting polyprotein<br />
processing by preventing the formation <strong>of</strong> the active<br />
proteinase complex. ACH-806/GS-9132 has potent in vitro<br />
activity against HCV genotype 1 and administration <strong>of</strong> 300<br />
mg twice daily for 5 days resulted in an average change in<br />
HCV RNA level from baseline <strong>of</strong> -0.9 log [27]. <strong>The</strong> development<br />
<strong>of</strong> this drug has been halted because <strong>of</strong> nephrotoxicity [27].<br />
Inhibitors <strong>of</strong> HCV replication<br />
Inhibitors <strong>of</strong> the RNA-dependent RNA polymerase (RdRp)<br />
belong to two categories: nucleoside/nucleotide inhibitors,<br />
that target the catalytic site <strong>of</strong> the enzyme, and non-nucleoside<br />
inhibitors that target allosteric sites <strong>of</strong> the RdRp. Three RdRp<br />
inhibitors have been administered to patients in clinical trials,<br />
including two nucleoside and one non-nucleoside inhibitor.<br />
Two have been withdrawn due to toxicity. R1626 (Roche<br />
Products) induces a dose-dependent HCV RNA level reduction<br />
[28]. At very high doses, HCV RNA level decrease reaches<br />
more than 3 logs, but side-effects are frequent. R1626 in<br />
combination with pegylated IFN alpha and ribavirin has<br />
recently progressed into phase II <strong>of</strong> clinical development. Other<br />
drugs have entered phase I clinical development.<br />
<strong>The</strong> HCV RdRp has been reported to bind cyclophilin B, a<br />
cellular peptidyl-prolyl cis-trans isomerase that apparently<br />
regulates HCV replication through modulation <strong>of</strong> the RNA<br />
binding capacity <strong>of</strong> RdRp. Synthetic, non-immunosuppressive<br />
cyclophylin B inhibitors have been developed and are being<br />
tested in patients with chronic HCV infection [29]. Side-effect<br />
were however frequent and led to treatment withdrawal in<br />
several cases [16]. Another cyclophilin B inhibitor, NIM 811<br />
(Novartis) is currently being tested in a phase I trial [30,31].<br />
Inhibitors <strong>of</strong> virus assembly and release<br />
Iminosugars have been suggested to be able to cross<br />
cellular membranes and concentrate in the endoplasmic<br />
reticulum where they could competitively inhibit envelope<br />
proteins glycosylation and interfere with viral assembly [32].<br />
MX-3253 or celgosivir (Migenix) has a modest antiviral effect<br />
on HCV in monotherapy. It is currently administered in<br />
combination with pegylated IFN alpha and ribavirin in a phase<br />
II clinical trial.<br />
Questions and Issues with New <strong>The</strong>rapies<br />
Among the many new avenues being explored, orally<br />
administered antiviral drugs that specifically inhibit a step <strong>of</strong><br />
the HCV lifecycle have come under the spotlight. However,<br />
although encouraging results have been published, serious<br />
issues have been raised as to the antiviral potency <strong>of</strong> these<br />
drugs, their tolerability, and the crucial problem <strong>of</strong> viral<br />
resistance.<br />
Antiviral Potency<br />
Antivirals usually enter development as soon as they show<br />
some degree <strong>of</strong> antiviral efficacy in one <strong>of</strong> the existing in vitro<br />
models. However, in vitro antiviral activity does not always<br />
translate into antiviral efficacy in vivo. <strong>The</strong>re are several<br />
examples <strong>of</strong> drugs that were highly potent in vitro but failed<br />
when administered to patients. Unfortunately, studies with<br />
“negative” results are rarely published, even though they<br />
could teach us a lot. <strong>The</strong>re are several possible reasons for<br />
these in vitro/in vivo discrepancies, including the use <strong>of</strong><br />
poorly relevant preclinical models, misinterpretation <strong>of</strong><br />
preclinical data, poor pharmacokinetics, poor delivery <strong>of</strong> a<br />
potentially potent drug to its target site, or the fact that the<br />
target is not physically accessible in infected cells in vivo.<br />
Tolerability<br />
Small-molecule viral inhibitors have been under close<br />
scrutiny for potential toxicity. <strong>The</strong> clinical development <strong>of</strong><br />
BILN 2061 (Boehringer-Ingelheim, Ingelheim, Germany), a<br />
potent HCV NS3 serine protease inhibitor and the first drug <strong>of</strong><br />
this type to be administered to infected patients, has been<br />
suspended because <strong>of</strong> myocardial toxicity in animals [33,34].<br />
<strong>The</strong> development <strong>of</strong> an enormous number <strong>of</strong> potentially active<br />
HCV drug candidates was stopped before they were given to<br />
patients, owing to concerns raised by preclinical toxicity<br />
studies in vitro and in animal models. <strong>The</strong> clinical development<br />
<strong>of</strong> several drugs has been stopped because <strong>of</strong> their side-effect<br />
pr<strong>of</strong>ile, including valopicitabine (digestive side-effects), HCV-<br />
796 (ALT elevations) and ACH-806 (nephrotoxicity). Other<br />
drugs are still being developed in spite <strong>of</strong> serious side-effects.<br />
R1626 has been shown to induce a dose-dependent reduction<br />
<strong>of</strong> blood cell counts and hemoglobin levels after two weeks <strong>of</strong><br />
administration at high doses [28], and the outcome <strong>of</strong> these<br />
effects is unknown if therapy is prolonged or if ribavirin is<br />
used in combination. Apparent safety during short-term<br />
administration does not guarantee that no serious adverse<br />
effects will occur when the drug is given for several weeks or<br />
months. Reesink et al. observed no serious adverse events<br />
during 14 days <strong>of</strong> telaprevir administration [25]. However, a<br />
recent commercial press release from Vertex Pharmaceuticals<br />
(December 13, 2006) states that, in the PROVE 1 study, a phase<br />
2b twelve-week clinical trial <strong>of</strong> the triple combination <strong>of</strong><br />
pegylated IFN alpha, ribavirin and telaprevir in treatment-naive<br />
patients, 3% <strong>of</strong> the patients discontinued telaprevir because<br />
<strong>of</strong> rash (rash was the most common reason for treatment<br />
discontinuation). Drug-drug interactions may also be a<br />
problem when HCV inhibitors are used in combination with<br />
pegylated IFN, with or without ribavirin. In addition, although<br />
synergy or additive efficacy may be expected, antagonism<br />
www.bjid.com.br
86 <strong>The</strong>rapeutic Perspectives for Hepatitis C<br />
BJID 2007; 11 Supplement 1 (October)<br />
can also occur. Here again, in vitro studies may give clues as<br />
to likely adverse effects but they cannot replace in vivo<br />
studies.<br />
Resistance<br />
A surprising finding has been the frequency and early<br />
timing <strong>of</strong> the emergence <strong>of</strong> resistance with all classes <strong>of</strong> anti-<br />
HCV drugs. <strong>The</strong>se results suggest that resistant variants are<br />
preexisting, fit, and ready to be selected by any specific HCV<br />
inhibitor. <strong>The</strong>se findings disqualify HCV inhibitor<br />
monotherapy and raise major ethical issues as to whether<br />
naive or nonresponder patients should now be included in<br />
trials <strong>of</strong> these drugs in monotherapy, as there is a risk that<br />
they will be disqualified from future trials and therapies with<br />
drug combinations.<br />
Conclusion<br />
At this point, it is clear that specific HCV inhibitors should<br />
not be used alone. Combination therapy with oral antiviral<br />
drugs will require company portfolios to contain more than<br />
one such drug. And appropriate preclinical drug-drug<br />
interaction studies will have to be performed before clinical<br />
trials are initiated. This may take several years. In the<br />
meantime, new strategies are needed to improve the results<br />
<strong>of</strong> current HCV therapy. <strong>The</strong> “conservative“ approach aimed<br />
at optimizing pegylated interferon-ribavirin therapy should<br />
not be neglected. Preliminary results have shown that<br />
increasing the dose and/or the number <strong>of</strong> injections <strong>of</strong><br />
pegylated IFN increases the response rate, and this is being<br />
further explored in ongoing trials. Likewise, increasing the<br />
dose <strong>of</strong> ribavirin has been shown to significantly improve<br />
the cure rate, and the adverse effects <strong>of</strong> ribavirin can now be<br />
partly controlled by using erythropoietin. Other trials are<br />
addressing the best way <strong>of</strong> tailoring the duration <strong>of</strong> treatment<br />
to the early virologic response (i.e. the HCV RNA decline at<br />
week 4 or even week 2). Another option is to enhance<br />
pegylated IFN-ribavirin efficacy by adding antiviral drugs<br />
with an additive or synergistic antiviral effect. Such<br />
combinations have the advantage <strong>of</strong> theoretically preventing<br />
the onset <strong>of</strong> resistance to the inhibitor, through the antiviral<br />
effect <strong>of</strong> IFN alpha. This may indeed happen in good IFN<br />
responders, although it is unclear whether IFN inhibition<br />
will be sufficient to avoid the emergence <strong>of</strong> resistance. In<br />
addition, patients with little or no response to IFN will in<br />
effect be receiving inhibitor monotherapy. Preliminary data<br />
are encouraging and ongoing trials will show how well double<br />
and triple combinations are tolerated, and whether the<br />
responses persist.<br />
References<br />
1. Tellinghusein T.L., Evans M.J., Hahn T., et al. Studying Hepatitis<br />
C Virus: making the best <strong>of</strong> a bad virus. <strong>Journal</strong> <strong>of</strong> Virology<br />
2007;81(17):8853-67.<br />
2. Lindenbach B.D., Rice C.M. Unravelling hepatitis C virus<br />
replication from genome to function. Nature<br />
2005;436(18):933-7.<br />
3. Wohnsland A., H<strong>of</strong>mann W.P., Sarrazin C. Viral determinants <strong>of</strong><br />
resistance to treatment in patients with hepatitis C. Clinical<br />
Microbiologogy Reviews 2007;20(1):23-38.<br />
4. Pawlotsky J.-M. Mechanisms <strong>of</strong> antiviral treatment efficacy<br />
and failure in chronic hepatitis C. Antiviral Research<br />
2003;59:1-11.<br />
5. Marcellin P., et al. Which patients with genotype 1 chronic<br />
hepatitis C can benefit from prolonged treatment with the<br />
‘accordion’ regimen? J Hepatology 2007 (in press).<br />
6. Goodbourn S., Didcock L., Randall R.E. Interferons: cell signalling,<br />
immune modulation, antiviral responses and virus<br />
countermeasures. <strong>Journal</strong> <strong>of</strong> General Virology<br />
2000;(81):2341-64.<br />
7. Pawlotsky J.-M., Chevaliez S., McHutchison J.G. <strong>The</strong> hepatitis C<br />
virus life cycle as a target for new antiviral therapies.<br />
Gastroenterology 2007;132:1979-98.<br />
8. McHutchinson J.G., et al. EASL 2007 Late Breaker 786.<br />
9. Harrison S.A. Small Molecule and novel treatments for chronic<br />
hepatitis C virus infection. American <strong>Journal</strong> <strong>of</strong> Gastroenterology<br />
2007;102:1-7.<br />
10. McHutchinson J.G., Bartenschlager R., Patel K., Pawlotsky J.-M.<br />
<strong>The</strong> face <strong>of</strong> future hepatitis C antiviral drug development: recent<br />
biological and virologic advances and their translation to drug<br />
development and clinical practice. <strong>Journal</strong> <strong>of</strong> Hepatology<br />
2006;44:411-21.<br />
11. Walters L., Nelson M. New therapeutic options for hepatitis C.<br />
Current Opinion on <strong>Infectious</strong> <strong>Diseases</strong> 2006;19:615-22.<br />
12. Marcellin P., Horsmans Y., Nevens F., et al. Phase 2 study <strong>of</strong> the<br />
combination <strong>of</strong> merimepodib with peginterferon-a2b, and<br />
ribavirin in nonresponders to previous therapy for chronic<br />
hepatitis C. J Hepatology 2007 (in press).<br />
13. Kempf D.J., Chen H.-J., Yeung J.T., et al. Pharmacokinetic<br />
boosting <strong>of</strong> VX-950, an inhibitor <strong>of</strong> HCV protease, by co-dosing<br />
with ritonavir. <strong>Journal</strong> <strong>of</strong> Hepatology 2006;44(2):S4.<br />
14. NIH Consensus Statement on Management <strong>of</strong> Hepatitis C: 2002.<br />
NIH Consens State Sci Statements 2002;19:1-46.<br />
15. Keeffe E.B., Hollinger F.B. <strong>The</strong>rapy <strong>of</strong> hepatitis C: consensus<br />
interferon trials. Consensus Interferon Study Group. Hepatology<br />
1997;26:101S-7S.<br />
16. Larkin J., Jin L., Farmen M., et al. Synergistic antiviral activity <strong>of</strong><br />
human interferon combinations in the hepatitis C virus replicon<br />
system. J Interferon Cytokine Res 2003;23:247-57.<br />
17. Marcello T., Grakoui A., Barba-Spaeth G., et al. Interferons alpha<br />
and lambda inhibit hepatitis C virus replication with distinct<br />
signal transduction and gene regulation kinetics.<br />
Gastroenterology 2006;131:1887-98.<br />
18. Wu J.Z., Lin C.C., Hong Z. Ribavirin, viramidine and adenosinedeaminase-catalysed<br />
drug activation: implication for nucleoside<br />
prodrug design. J Antimicrob Chemother 2003;52:543-6.<br />
19. Leroux-Roels G., Batens A.H., Desombere I., et al. Immunogenicity<br />
and tolerability <strong>of</strong> intradermal administration <strong>of</strong> an HCV E1-<br />
based vaccine candidate in healthy volunteers and patients with<br />
resolved or ongoing chronic HCV infection. Hum Vaccin<br />
2005;1:61-5.<br />
20. Davis G.L., Nelson D.R., Terrault N., et al. A randomized, openlabel<br />
study to evaluate the safety and pharmacokinetics <strong>of</strong> human<br />
hepatitis C immune globulin (Civacir) in liver transplant<br />
recipients. Liver Transpl 2005;11:941-9.<br />
21. Schiano T.D., Charlton M., Younossi Z., et al. Monoclonal antibody<br />
HCV-AbXTL68 in patients undergoing liver transplantation<br />
for HCV: results <strong>of</strong> a phase 2 randomized study. Liver Transpl<br />
2006;12:1381-9.<br />
22. Galun E., Terrault N.A., Eren R., et al. Clinical evaluation (Phase<br />
I) <strong>of</strong> a human monoclonal antibody against hepatitis C virus:<br />
safety and antiviral activity. J Hepatol 2007;46:37-44.<br />
23. McHutchison J.G., Patel K., Pockros P., et al. A phase I trial <strong>of</strong> an<br />
antisense inhibitor <strong>of</strong> hepatitis C virus (ISIS 14803), administered<br />
to chronic hepatitis C patients. J Hepatol 2006;44:88-96.<br />
www.bjid.com.br
BJID 2007; 11 Supplement 1 (October) <strong>The</strong>rapeutic Perspectives for Hepatitis C<br />
87<br />
24. Soler M., McHutchison J.G., Kwoh T.J., et al. Virological effects<br />
<strong>of</strong> ISIS 14803, an antisense oligonucleotide inhibitor <strong>of</strong><br />
hepatitis C virus (HCV) internal ribosome entry site (IRES),<br />
on HCV IRES in chronic hepatitis C patients and<br />
examination <strong>of</strong> the potential role <strong>of</strong> primary and secondary<br />
HCV resistance in the outcome <strong>of</strong> treatment. Antivir <strong>The</strong>r<br />
2004;9:953-68.<br />
25. Reesink H.W., Zeuzem S., Weegink C.J., et al. Rapid decline <strong>of</strong><br />
viral RNA in hepatitis C patients treated with VX-950: a phase<br />
Ib, placebo-controlled, randomized study. Gastroenterology<br />
2006;131:997-1002.<br />
26. Sarrazin C., Rouzier R., Wagner F., et al. SCH 503034, a novel<br />
hepatitis C virus protease inhibitor, plus pegylated interferon<br />
á-2b for genotype 1 non-responders. Gastroenterology<br />
2007;in press.<br />
27. Pottage J.C., Lawitz E., Mazur D., et al. Short-term antiviral<br />
activity and safety <strong>of</strong> ACH-806 (GS-9132), an NS4A<br />
antagonist, in HCV genotype 1 infected individuals. J<br />
Hepatol 2007;in press.<br />
28. Roberts S., Cooksley G., Dore G., et al. Results <strong>of</strong> a phase 1b,<br />
multiple dose study <strong>of</strong> R1626, a novel nucleoside analogue<br />
targeting HCV polymerase in chronic HCV genotype 1 patients.<br />
Hepatology 2006;44 (suppl. 1):692A.<br />
29. Flisiak R., Orban A., Kierkus J., et al. <strong>The</strong> cyclophilin inhibitor<br />
DEBIO-025 has a potent dual anti-HIV and anti-HCV activity<br />
in treatment-naïve HIV/HCV co-infected subjects. Hepatology<br />
2006;44 (suppl. 1):609A.<br />
30. Ma S., Boerner J.E., Tiong Yip C., et al. NIM811, a cyclophilin<br />
inhibitor, exhibits potent in vitro activity against hepatitis C<br />
virus alone or in combination with alpha interferon. Antimicrob<br />
Agents Chemother 2006;50:2976-82.<br />
31. Goto K., Watashi K., Murata T., et al. Evaluation <strong>of</strong> the antihepatitis<br />
C virus effects <strong>of</strong> cyclophilin inhibitors, cyclosporin<br />
A, and NIM811. Biochem Biophys Res Commun<br />
2006;343:879-84.<br />
32. Durantel D., Carrouee-Durantel S., Branza-Nichita N., et al. Effects<br />
<strong>of</strong> interferon, ribavirin, and iminosugar derivatives on cells<br />
persistently infected with noncytopathic bovine viral diarrhea<br />
virus. Antimicrob Agents Chemother 2004;48:497-504.<br />
33. Hinrichsen H., Benhamou Y., Wedemeyer H., et al. Short-term<br />
antiviral efficacy <strong>of</strong> BILN 2061, a hepatitis C virus serine<br />
protease inhibitor, in hepatitis C genotype 1 patients.<br />
Gastroenterology 2004;127:1347-55.<br />
34. Reiser M., Hinrichsen H., Benhamou Y., et al. Antiviral efficacy <strong>of</strong><br />
NS3-serine protease inhibitor BILN-2061 in patients with chronic<br />
genotype 2 and 3 hepatitis C. Hepatology 2005;41:832-5.<br />
www.bjid.com.br
88 BJID 2007; 11 Supplement 1 (October)<br />
INSTRUCTIONS FOR AUTHORS<br />
Manuscripts for submission to <strong>The</strong> <strong>Brazilian</strong><br />
<strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong> should be sent to<br />
Anastácio Queiroz de Sousa, Editor-in-Chief, Rua<br />
Alfredo Magalhães, 04/Barra, 40140-140, Salvador-<br />
Bahia-Brazil. Each manuscript will be assigned a<br />
registration number, and the author notified that the<br />
manuscript is complete and appropriate to begin the<br />
review process.<br />
Authors must indicate in a cover letter the address,<br />
telephone number, fax number, and e-mail <strong>of</strong> the<br />
corresponding author. <strong>The</strong> corresponding author will<br />
be asked to make a statement confirming that the<br />
content <strong>of</strong> the manuscript represents the views <strong>of</strong> the<br />
co-authors, that neither the corresponding author nor<br />
the co-authors have submitted duplicate or<br />
overlapping manuscripts elsewhere, and that the items<br />
indicated as personal communications in the text are<br />
supported by the referenced person.<br />
Each manuscript is to be submitted as an original<br />
with three copies and four sets <strong>of</strong> illustrations. For<br />
submission to Letters to the Editor or the Editor's<br />
Corner, an original and one copy are required. For<br />
submission to Clinical <strong>Infectious</strong> <strong>Diseases</strong> Images,<br />
which are not intended as a vehicle for case reports,<br />
all text should be in one double-spaced electronic<br />
document, title (no more than eight words in the<br />
title; no more than five authors may be listed,<br />
inclusing name, highest academic degree, address,<br />
e-mail address, telephone and fax number <strong>of</strong> each<br />
author; the text should contain no more than 300<br />
words. <strong>The</strong> other manuscripts are to be typed<br />
double-spaced, including text, tables, references<br />
and legends. All pages are to be numbered, with<br />
the order <strong>of</strong> presentation as follows: title page,<br />
abstract, text, acknowledgements, references,<br />
tables, figure legends and figures. A running title <strong>of</strong><br />
not more than 40 characters should be at the top <strong>of</strong><br />
each page. <strong>The</strong> abstract should not exceed 250<br />
words. References should be listed consecutively in<br />
the text and recorded as follows in the reference list.<br />
Authors (when there are fewer than five, record all<br />
authors; when there are five or more, record the first<br />
three, followed by et al.), title, journal, year, volume,<br />
pages (first and last).<br />
www.bjid.com.br<br />
References must follow the format <strong>of</strong> the National<br />
Library <strong>of</strong> Medicine as in Index Medicus and "Uniform<br />
Requirements". Titles <strong>of</strong> journals not listed in Index<br />
Medicus should be spelled out in full. Several examples<br />
<strong>of</strong> specific references follow:<br />
Article<br />
(If the journal is not listed in Index Medicus)<br />
Smith J.C., Charles R.S. Microbes and water filters.<br />
<strong>Journal</strong> <strong>of</strong> Water Purification 1996;20:165-170.<br />
(If the journal is in Index Medicus)<br />
Watson B.M., Gupta R., Randal T., Starr S.<br />
Persistence <strong>of</strong> cell-mediated immune responses<br />
post-VZV immunization. J Infect Dis<br />
1994;169:197-9.<br />
Book Chapter<br />
Taylor D.M., Personnet J. Epidemiology and natural<br />
history <strong>of</strong> Helicobacter pylori infection. In: Blaser<br />
M.J., Smith P.D., Ravdin J. eds. Infections <strong>of</strong> the<br />
gastrointestinal tract. New York: Raven Press,<br />
1994.<br />
Book<br />
Polak J.M., Van Noordan S. An introduction to<br />
immunochemistry: current techniques and problems.<br />
Oxford, UK: Oxford University Press, 1987.<br />
Abstract<br />
Blatt S.P., Butzin C.A., Lucey D.R., Melcher G.P.,<br />
Hendrix C.R. Anergy status and CD4 CD29<br />
memory T-cells predict progression to AIDS<br />
(abstract PoB 3480). In: Program and abstracts:<br />
VIII International Conference on AIDS<br />
(Amsterdam) Amsterdam: CONGREX Holland,<br />
1992.<br />
Figures may be submitted as glossy photographs<br />
or as high-quality laser prints on bond paper.<br />
Manuscript style should follow accepted standards.<br />
Please refer to the BJID for guidance. <strong>The</strong> final style will<br />
be determined by the Medical Editor after it is reviewed<br />
and accepted by the manuscript's corresponding author.
BJID 2007; 11 Supplement 1 (October) 89<br />
STATEMENT OF<br />
EDITORIAL POLICY<br />
<strong>The</strong> <strong>Brazilian</strong> <strong>Journal</strong> <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong><br />
(BJID) is organized, guided and sponsored by the<br />
<strong>Brazilian</strong> Society <strong>of</strong> <strong>Infectious</strong> <strong>Diseases</strong>.<br />
Communications published in the BJID are to be<br />
relevant in the broadest sense to all aspects <strong>of</strong><br />
microbiology, infection and immune response to<br />
infectious agents.<br />
Manuscripts may be submitted within designated<br />
categories <strong>of</strong> communication including:<br />
Evaluation <strong>of</strong> Manuscripts<br />
<strong>The</strong> Editor will obtain reviews <strong>of</strong> each submitted<br />
manuscript by two expert consultants, usually from<br />
the Editorial Board <strong>of</strong> the BJID. Exceptions will be<br />
made to this policy by the Editor only in cases in<br />
which the content <strong>of</strong> the manuscript is not consistent<br />
with the editorial policy <strong>of</strong> the <strong>Journal</strong>. Authors may<br />
suggest appropriate consultants for review <strong>of</strong> the<br />
manuscript. <strong>The</strong> review process will ordinarily<br />
require two months.<br />
• original basic or clinical investigation;<br />
• case presentation and discussion;<br />
• brief reports <strong>of</strong> new methods or observations;<br />
• clinical infectious diseases images;<br />
• state-<strong>of</strong>-the-art presentations or reviews;<br />
• letters to the editor concerning previous publications;<br />
• editor's corner containing ideas, hypotheses and<br />
comments.<br />
Supplements to the BJID include articles under a<br />
unifying theme, such as those summarizing presentations<br />
<strong>of</strong> symposia or focusing on a specific pathogenic<br />
process or antimicrobial agent. <strong>The</strong>se will be added to<br />
the regular bi-monthly publication as appropriate and<br />
will be peer reviewed in the same manner as submitted<br />
manuscripts.<br />
Publication<br />
<strong>The</strong> BJID is published bi-monthly (February,<br />
April, June, August, October, December) by<br />
Contexto Publishing Inc., Rua Alfredo Magalhães,<br />
04/Barra, 40140-140, Salvador-Bahia-Brazil. <strong>The</strong><br />
editors <strong>of</strong> the <strong>Journal</strong> reserve the right to edit<br />
manuscripts for clarity, grammar and style. Authors<br />
will have an opportunity to review these changes<br />
prior to creation <strong>of</strong> galley pro<strong>of</strong>s. Changes in content<br />
after galley pro<strong>of</strong>s are sent for review will require<br />
charges to the author. <strong>The</strong> BJID does not accept<br />
articles which duplicate or overlap publications<br />
elsewhere.<br />
www.bjid.com.br
90 BJID 2007; 11 Supplement 1 (October)<br />
Checklist for Submitted Manuscripts<br />
1. Please provide a cover letter with your submission, specifying the corresponding author as well as an<br />
address, telephone and facsimile number.<br />
2. Submit four copies <strong>of</strong> your manuscript (original plus three copies and a disk <strong>of</strong> the manuscript - Word<br />
Perfect/Word for Windows), each with a complete set <strong>of</strong> original illustrations.<br />
3. <strong>The</strong> entire manuscript (including tables and references) must be typed double-spaced and printed on standardsized<br />
paper. <strong>The</strong> left and right margins must be at least 3 cm.<br />
4. <strong>The</strong> entire manuscript must be typed in a font size <strong>of</strong> at least 12 points.<br />
5. Please number pages beginning with the title page (title page is page 1).<br />
6. <strong>The</strong> order <strong>of</strong> appearance <strong>of</strong> material in all manuscripts should be as follows: title page, abstract, text,<br />
acknowledgements, references, tables, legends for figures, figures.<br />
7. <strong>The</strong> title page must include a title <strong>of</strong> not more than three printed lines (250 letters and spaces), authors (no<br />
titles or degrees), institutional affiliations, a running headline <strong>of</strong> not more than 40 letters and spaces, a name and<br />
complete address to which correspondence and reprint requests should be sent, and footnotes indicating sources<br />
<strong>of</strong> financial support and changes <strong>of</strong> address.<br />
8. Abstract (maximum 250 words) must be on a separate page before the introduction. Do not submit an<br />
abstract with correspondence.<br />
9. Acknowledgements <strong>of</strong> persons who assisted the authors should be included on the page preceding the<br />
references.<br />
10. References must begin on a separate page.<br />
11. References must be cited on (not above) the line <strong>of</strong> text and in brackets instead <strong>of</strong> parentheses, e.g., [7,8].<br />
12. References must be numbered in the order in which they appear in the text. References not cited in the text<br />
cannot appear in the reference section. References that are only or are first cited in a table or figure are numbered<br />
according to where the table or figure is cited in the text. For instance, if a table is placed after reference 8, a new<br />
reference cited in table 1 would be reference 9.<br />
13. Reference citations must follow the format established by the "Uniform Requirements for Manuscripts<br />
Submitted to Biomedical <strong>Journal</strong>s" (see examples in Instructions to Authors).<br />
14. If you reference your own unpublished work (i.e., an "in press" article) in the manuscript that you are<br />
submitting, you must enclose three copies <strong>of</strong> the "in press" article and an acceptance letter from the journal.<br />
15. If you cite unpublished data that are not your own, you must provide a letter <strong>of</strong> permission from the author<br />
<strong>of</strong> that publication.<br />
16. Please provide four glossy or laser-produced prints <strong>of</strong> each figure that you are submitting. Label all figures<br />
clearly with first author's name and figure number (place typed label on the back <strong>of</strong> the figure).<br />
17. Provide a figure legend for each figure. Figure legends must be on a separate page at the end <strong>of</strong> the<br />
manuscript.<br />
Please refer to Instructions to Authors for further information regarding the section to be submitted<br />
the manuscript, title page, abstract, references, tables and figures, and style.<br />
www.bjid.com.br