Pelvic Hemorrhage During Gynecologic Surgery
Pelvic Hemorrhage During Gynecologic Surgery
Pelvic Hemorrhage During Gynecologic Surgery
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
GYNECOLOGIC SURGERY<br />
<strong>Pelvic</strong> <strong>Hemorrhage</strong><br />
<strong>During</strong> <strong>Gynecologic</strong> <strong>Surgery</strong><br />
Donald G. Gallup, MD<br />
FOCUSPOINT<br />
Patients at risk<br />
for intraoperative<br />
hemorrhage include<br />
those with a family<br />
history of bleeding<br />
disorders, those<br />
with poor nutrition,<br />
and those who<br />
are obese.<br />
Intraoperative hemorrhage is a serious<br />
complication of gynecologic or obstetric<br />
surgery, and catastrophic hemorrhage<br />
sometimes results in panic. A calm, stepwise<br />
approach, as outlined, will enable<br />
the surgeon, his/her consultants, and the<br />
operating team to successfully manage a<br />
potentially lethal problem.<br />
A29-year-old woman, gravid 2,<br />
para 2, had an emergency hysterectomy<br />
for placenta accreta and<br />
persistent bleeding at a hospital<br />
50 miles from our institution. The<br />
abdomen had been closed, but the cuff was still<br />
“oozing.” She had tachycardia and blood pressure<br />
in the range of 60/40 mm Hg. A helicopter<br />
brought her to our facility. Further<br />
transfusion of packed red<br />
blood cells (RBCs) and fresh<br />
frozen plasma was administered,<br />
and she returned to the<br />
operating room for a left salpingo-oophorectomy<br />
and bilateral<br />
hypogastric artery ligation<br />
through a midline incision.<br />
Bleeding persisted, and a “pack<br />
and go” technique over a hemostatic<br />
agent was used. A vacuum-assisted<br />
closure (VAC)<br />
was used. Neither the skin nor<br />
fascia was closed.<br />
Thirty-six hours later, she<br />
was again reoperated on. No<br />
bleeding was encountered<br />
after removal of the 4″ Kerlex gauze. The abdominal<br />
fascia and skin were closed using<br />
standard sutures and techniques.<br />
Donald G. Gallup, MD, is Professor and Chair, Department of<br />
Obstetrics and Gynecology, Mercer University School of<br />
Medicine (Savannah), Savannah, GA.<br />
RISK FACTORS<br />
Patients at risk for intraoperative hemorrhage<br />
include those with a family history of bleeding<br />
disorders, those with poor nutrition (eg, high<br />
alcohol intake), and those who are obese. The<br />
most common congenital platelet disorder is<br />
von Willebrand disease, and suspect patients,<br />
ie, patients with prior history of bleeding after<br />
surgery on tooth extractions or with family history<br />
of bleeding, should have preoperative<br />
evaluations and management recommendations<br />
from a hematologist. Patients who abuse<br />
alcohol or are malnourished should have preoperative<br />
liver function and coagulation studies.<br />
The primary laboratory test to evaluate potential<br />
bleeding is the platelet count. For any<br />
surgery or invasive procedure, such as insertion<br />
of a central line, a platelet count of 50,000 is<br />
recommended. 1<br />
Patients should stop taking aspirin, NSAIDs,<br />
and medications such as warfarin or clopidogrel<br />
7 days prior to surgery. Certain alternative<br />
medicine products can impair coagulation<br />
(Table 1), so a thorough history should be obtained.<br />
Stop these products 5 to 7 days prior to<br />
surgery. 2<br />
CONTROLLING PELVIC BLEEDING<br />
The first step in controlling bleeding is application<br />
of pressure with a finger or sponge stick.<br />
Then, call for assistance and obtain exposure,<br />
which usually requires extending the incision<br />
and using a fixed table retractor. Pressure on<br />
the aorta with a hand, weighted speculum, or<br />
aortic compressor can be temporarily applied<br />
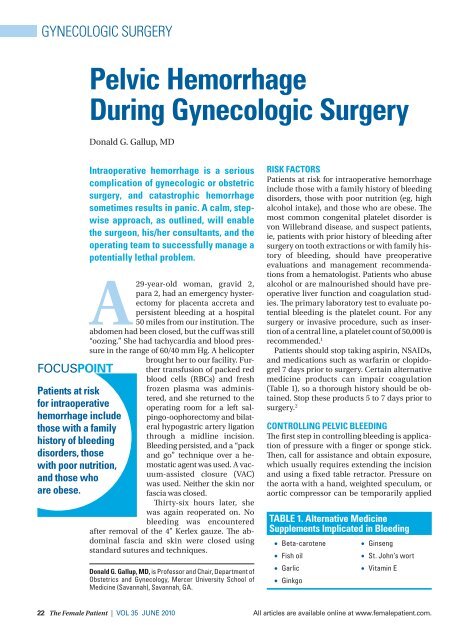
TABLE 1. Alternative Medicine<br />
Supplements Implicated in Bleeding<br />
• Beta-carotene<br />
• Fish oil<br />
• Garlic<br />
• Ginkgo<br />
• Ginseng<br />
• St. John’s wort<br />
• Vitamin E<br />
22 The Female Patient | VOL 35 JUNE 2010 All articles are available online at www.femalepatient.com.
GALLUP<br />
to help locate the source of massive pelvic<br />
bleeding. Individual vessels should be secured<br />
with fine-tipped clamps and clips or smallcaliber<br />
sutures. Never use electrocautery for<br />
large lacerations. Packs (hot or cold) can be<br />
used to temporarily control pelvic bleeding<br />
and should be carefully placed from sidewall to<br />
sidewall and removed sequentially after a period<br />
of at least 5 minutes to allow for adequate<br />
pressure.<br />
Guidelines for component replacement therapy<br />
should be followed after primary volume<br />
expansion. In general, for every 8 units of RBCs<br />
replaced, give 2 units of fresh frozen plasma. If<br />
more than 10 units of RBCs are replaced, give 10<br />
units of platelets. If fibrinogen is low, give 2 units<br />
of cryoprecipate. Using fresh frozen plasma in a<br />
ratio of 1:1 or 1:2 with RBC units earlier has been<br />
shown to improve survival in presence of massive<br />
hemorrhage. 3,4<br />
The Haemonetics Cell Saver should be used<br />
when massive bleeding is anticipated. It is accepted<br />
by many Jehovah’s Witnesses. 5 Relative<br />
contraindications to its use include malignancy,<br />
bacterial contamination from a ruptured abscess,<br />
and inadvertent injury to unprepared<br />
bowel.<br />
TOPICAL AGENTS<br />
If troublesome bleeding persists after packing<br />
and securing arterial bleeders, a topical hemostatic<br />
agent can be used. A less-expensive product<br />
to try initially is Surgicel or Gelfoam. Some<br />
still use Avitene, but this powder substance<br />
works poorly in the presence of thrombocytopenia<br />
and should be used with caution when<br />
applied near the ureter. Ureteral stricture may<br />
occur with excessive amounts. All these agents<br />
require pressure for 3 to 5 minutes, as pressure<br />
may enhance clot formation and inhibits capillary/small<br />
vessel oozing.<br />
Fibrin glue, consisting of equal amounts of<br />
cryoprecipitate and thrombin, has been successfully<br />
used as a local hemostatic agent in<br />
cardiovascular, thoracic, and reconstructive<br />
surgeries and prostatectomy. 6 The fibrin sealants<br />
used in gynecologic surgery are Tisseel VH<br />
and FloSeal. Both are relatively more expensive<br />
than the above agents. The high-viscosity gel<br />
FloSeal may be preferred, as it can be mixed at<br />
the operating room.<br />
HYPOGASTRIC ARTERY LIGATION<br />
If pelvic oozing persists after topical agent application,<br />
consider hypogastric artery ligation<br />
(HAL), which is successful in<br />
about 50% of patients. 7 HAL<br />
works by decreasing pulse<br />
pressure. A safe method to expose<br />
the vessels is to open the<br />
sidewall along the avascular<br />
line of Toldt. The ureter is retracted<br />
out of harm’s way (Figure<br />
1). After clearly identifying<br />
the common iliac vessels, a<br />
right-angle clamp is passed<br />
from lateral to medial, distal to<br />
the posterior division of the artery<br />
or proximal to the uterine<br />
artery. Two large base sutures<br />
are placed in the tip of the<br />
clamp and later tied (Figure 2).<br />
FOCUSPOINT<br />
A calm, stepwise<br />
approach will enable<br />
the surgical team to<br />
successfully manage<br />
a potentially lethal<br />
problem.<br />
A gynecologic oncologist or vascular surgeon<br />
experienced in pelvic surgery may be called to<br />
assist.<br />
PRESACRAL VEIN INJURY<br />
A relatively rare cause of catastrophic pelvic<br />
hemorrhage is inadvertent injury of the presacral<br />
veins. For the gynecologist, this can occur<br />
during presacral neurectomy or sacrocolpopexy.<br />
This bleeding, seldom controlled with<br />
topical agents, has been successfully managed<br />
with insertion of stainless steel thumbtacks di-<br />
Line of Toldt<br />
External<br />
iliac artery<br />
and vein<br />
Common iliac artery<br />
Hypogastric<br />
artery<br />
Hypogastric<br />
vein<br />
Ureter retracted<br />
medially<br />
FIGURE 1. The sidewall is opened along the avascular<br />
line of Toldt. The ureter is identified at the bifurcation of<br />
the common iliac artery and retracted medically.<br />
Illustrated by R. Kelly Gallup.<br />
Follow The Female Patient on and The Female Patient | VOL 35 JUNE 2010 23
<strong>Pelvic</strong> <strong>Hemorrhage</strong> <strong>During</strong> <strong>Gynecologic</strong> <strong>Surgery</strong><br />
Right angle<br />
clamp<br />
External<br />
iliac artery<br />
and vein<br />
FIGURE 3. The VAC is placed in the operating room in a<br />
patient who was operated for catastrophic hemorrhage.<br />
Courtesy of Donald G. Gallup, MD.<br />
Hypogastric vein<br />
rectly into the sacrum. 8 Harvesting a 2×1 cm of<br />
rectus abdominus muscle fragment, pressing it<br />
against the presacral veins, and indirectly coagulating<br />
them with pure cutting current (welding)<br />
for 2 minutes has also been successful. 9<br />
“PACK AND GO”<br />
If intraoperative bleeding persists despite HAL<br />
and other measures, a pelvic pack should be<br />
placed. Some prefer a Logothetopolous (parachute)<br />
pack. 10 The disadvantages of this pack,<br />
which is brought out through the vagina, are<br />
possible unrecognized further bleeding or injury<br />
to bowel on later removal. We prefer a fast,<br />
simple method used by many trauma surgeons.<br />
11 Tightly packed 2″ to 4″ Kerlex gauze is<br />
TABLE 2. “Pack and Go” Steps<br />
Hypogastric artery<br />
FIGURE 2. A right-angle clamp is passed gently<br />
posterior to the artery with aid of a Babcock clamp.<br />
The artery should be “hugged” in order to prevent<br />
injury to underlying hypogastric vein.<br />
Illustrated by R. Kelly Gallup.<br />
1. Pack Kerlex gauze from sidewall to sidewall.<br />
2. Close skin only with towel clips or running suture.<br />
3. Transfer patient to ICU and correct hypothermia,<br />
acidosis, and coagulopathy.<br />
4. Reoperate and remove pack in 36 to 48 hours.<br />
placed over previously applied FloSeal (Table 2).<br />
The pack should be removed with saline drip assistance.<br />
An alternative to closing the skin is use<br />
of a modified VAC (Figure 3). This closure kit is<br />
available in most operating rooms associated<br />
with trauma services. With this damage control<br />
surgery, upon reoperation, the pelvis is free of active<br />
bleeding, and repacking is seldom needed.<br />
The author reports no actual or potential conflict<br />
of interest in relation to this article.<br />
REFERENCES<br />
1. Nolan TE, Gallup DG. Massive transfusion: a current<br />
review. Obstet Gynecol Surv. 1991;46(5):289-295.<br />
2. Ang-Lee MK, Moss J, Yuan CS. Herbal medicines and perioperative<br />
care. JAMA. 2001;286(2):208-216.<br />
3. Gonzalez EA, Moore FA, Holcomb JB, et al. Fresh frozen<br />
plasma should be given earlier to patients requiring massive<br />
transfusion. J Trauma. 2007;62(1):112-119.<br />
4. Holcomb JB, Wade CE, Michalek JE, et al. Increase plasma<br />
and platelet to red blood cell ratios improves outcome in<br />
466 massively transfused civilian trauma patients. Ann<br />
Surg. 2008;248(3):447-458.<br />
5. deCastro RM. Bloodless surgery: establishment of a<br />
program for the special medical needs of the Jehovah’s<br />
Witness community: the gynecologic surgery experience<br />
at a community hospital. Am J Obstet Gynecol.<br />
1999;180(6 Pt 1):1491-1498.<br />
6. Abala DM, Lawson JH. Recent clinical and investigational<br />
applications of fibrin sealant in selected surgical<br />
specialties. J Am Coll Surg. 2006;202(4):685-697.<br />
7. Papp Z, Toth-Pal E, Papp C, et al. Hypogastric artery ligation<br />
for intractable pelvic hemorrhage. Int J Gynecol Obstet.<br />
2006;92(1):27-31.<br />
8. Patsner B, Orr JW Jr. Intractable venous hemorrhage: use<br />
of stainless steel thumbtacks to obtain hemostasis. Am J<br />
Obstet Gynecol. 1990;162(2):452.<br />
9. Harrison JL, Hooks VH, Pearl RK, et al. Muscle fragment<br />
welding for control of massive presacral bleeding during<br />
rectal mobilization: a review of eight cases. Dis Colon Rectum.<br />
2003;46(8):115-119.<br />
10. Howard RJ, Straughn JM Jr, Huh WK, Rouse DJ. <strong>Pelvic</strong><br />
umbrella pack for refractory obstetric hemorrhage secondary<br />
to posterior uterine rupture. Obstet Gynecol. 2002;<br />
100(5 Pt 2):1061-1063.<br />
11. Rotondo MF, Zonies DH. The damage control sequence<br />
and underlying logic. Surg Clin North Am. 1997;77(4):<br />
761-777.<br />
24 The Female Patient | VOL 35 JUNE 2010 All articles are available online at www.femalepatient.com.