Self-Administered Drug - WPS Medicare
Self-Administered Drug - WPS Medicare
Self-Administered Drug - WPS Medicare
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
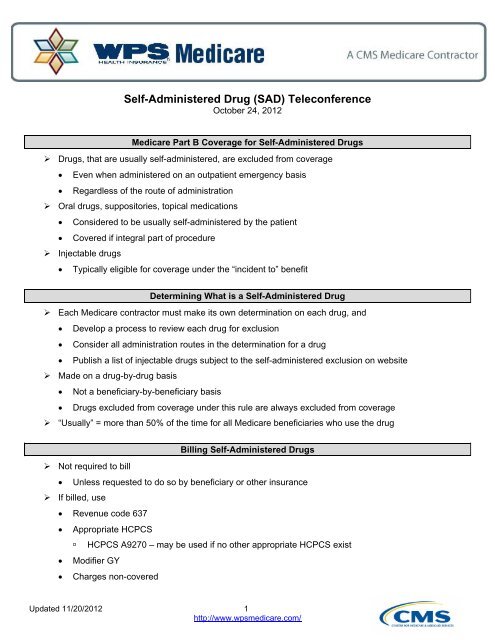
<strong>Self</strong>-<strong>Administered</strong> <strong>Drug</strong> (SAD) Teleconference<br />
October 24, 2012<br />
<strong>Medicare</strong> Part B Coverage for <strong>Self</strong>-<strong>Administered</strong> <strong>Drug</strong>s<br />
‣ <strong>Drug</strong>s, that are usually self-administered, are excluded from coverage<br />
Even when administered on an outpatient emergency basis<br />
Regardless of the route of administration<br />
‣ Oral drugs, suppositories, topical medications<br />
Considered to be usually self-administered by the patient<br />
Covered if integral part of procedure<br />
‣ Injectable drugs<br />
Typically eligible for coverage under the “incident to” benefit<br />
Determining What is a <strong>Self</strong>-<strong>Administered</strong> <strong>Drug</strong><br />
‣ Each <strong>Medicare</strong> contractor must make its own determination on each drug, and<br />
Develop a process to review each drug for exclusion<br />
Consider all administration routes in the determination for a drug<br />
Publish a list of injectable drugs subject to the self-administered exclusion on website<br />
‣ Made on a drug-by-drug basis<br />
Not a beneficiary-by-beneficiary basis<br />
<strong>Drug</strong>s excluded from coverage under this rule are always excluded from coverage<br />
‣ “Usually” = more than 50% of the time for all <strong>Medicare</strong> beneficiaries who use the drug<br />
Billing <strong>Self</strong>-<strong>Administered</strong> <strong>Drug</strong>s<br />
‣ Not required to bill<br />
Unless requested to do so by beneficiary or other insurance<br />
‣ If billed, use<br />
Revenue code 637<br />
Appropriate HCPCS<br />
HCPCS A9270 – may be used if no other appropriate HCPCS exist<br />
Modifier GY<br />
Charges non-covered<br />
Updated 11/20/2012 1<br />
http://www.wpsmedicare.com/
<strong>Drug</strong>s Treated as Hospital Outpatient Supplies<br />
‣ <strong>Medicare</strong> pays for drugs that may be considered usually self-administered by the patient when such<br />
drugs function as supplies<br />
<strong>Drug</strong>s provided are an integral component of a procedure or are directly related to it<br />
‣ Except for the applicable copayment, hospitals may not bill beneficiaries for these types of drugs<br />
‣ Report coded and uncoded drugs with their charges under appropriate revenue code<br />
Cost center under which the hospital accumulates the costs for the drugs<br />
Appealing <strong>Self</strong>-<strong>Administered</strong> <strong>Drug</strong>s<br />
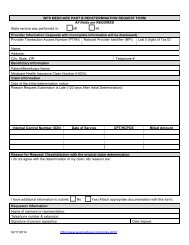
‣ Beneficiaries may appeal the denial<br />
Because it is a “benefit category” denial, an ABN is not required<br />
‣ Providers may also appeal the denial<br />
References<br />
‣ CMS Internet-Only Manual (IOM)<br />
Publication 100-02, <strong>Medicare</strong> Benefit Policy Manual, Chapter 15, Section 50.2<br />
Publication 100-04, <strong>Medicare</strong> Claims Processing Manual, Chapter 1, Section 60.4.2<br />
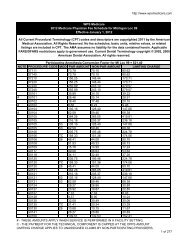
‣ <strong>WPS</strong> <strong>Medicare</strong> SAD listing and policy<br />
http://wpsmedicare.com >> Appropriate Part A contract >> Policy >> <strong>Self</strong>-<strong>Administered</strong> <strong>Drug</strong><br />
Exclusion List (SAD List)<br />
This program is presented for informational purposes only. Current <strong>Medicare</strong> regulations will always prevail.<br />
Page 2 of 2