Managment of Urosepsis in a Private Surgical Hospital - anzuns
Managment of Urosepsis in a Private Surgical Hospital - anzuns
Managment of Urosepsis in a Private Surgical Hospital - anzuns
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
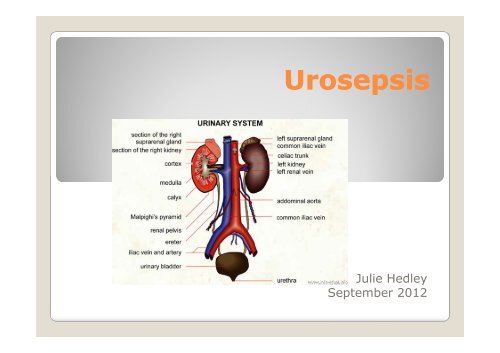
<strong>Urosepsis</strong><br />
Julie Hedley<br />
September 2012
Def<strong>in</strong>ition <strong>of</strong> <strong>Urosepsis</strong><br />
Sepsis caused by<br />
<strong>in</strong>fection <strong>of</strong> the<br />
ur<strong>in</strong>ary tract<br />
and / or male<br />
genital organs<br />
(prostate)
Etiology <strong>of</strong> Sepsis<br />
Elderly patients<br />
The severity <strong>of</strong><br />
sepsis depends<br />
mostly upon the host<br />
response<br />
Diabetics<br />
Immunosuppressed<br />
- transplant recipients<br />
- cancer pts / chemo/steroids<br />
- AIDS
Pathophysiology<br />
For urosepsis to be<br />
established,<br />
pathogens have to<br />
reach the<br />
bloodstream<br />
Risk <strong>of</strong> bacteraemia<br />
is <strong>in</strong>creased <strong>in</strong><br />
- severe UTIs<br />
- obstruction caused by<br />
◦ Stones<br />
◦ Stenosis<br />
◦ Tumours (prostatic or urological)<br />
◦ Pregnancy<br />
◦ Anomalies <strong>of</strong> the Ur<strong>in</strong>ary Tract<br />
◦ Follow<strong>in</strong>g operations
Sepsis <strong>Urosepsis</strong><br />
Bloodstream<br />
Sk<strong>in</strong><br />
Gram negative bacteria<br />
Escherichia coli<br />
Pseudomonas aerug<strong>in</strong>osa<br />
Respiratory tract<br />
Gastro<strong>in</strong>test<strong>in</strong>al tract<br />
Genitour<strong>in</strong>ary tract<br />
Klebsiella<br />
Proteus<br />
Gram positive bacteria<br />
Enetercoccus
Epidemiology<br />
<strong>Urosepsis</strong> accounts<br />
for approx. 25% <strong>of</strong><br />
all sepsis cases<br />
More common <strong>in</strong><br />
men than women<br />
Severe Sepsis:<br />
Pulmonary 50%<br />
Abdom<strong>in</strong>al <strong>in</strong>fections 24%<br />
UTI 5%<br />
Severe sepsis –<br />
UTI’s 5%
Sepsis<br />
Systemic<br />
<strong>in</strong>flammatory<br />
response to <strong>in</strong>fection<br />
Diagnosis when 2 or<br />
more <strong>of</strong> the follow<strong>in</strong>g<br />
criteria are present<br />
Temp > 38 or < 36<br />
HR > 90/m<strong>in</strong><br />
Resps > 20/m<strong>in</strong> or PaCo2 <<br />
32mm Hg<br />
WBC > 12,000 or < 4,000
Sepsis<br />
Sepsis can only be<br />
diagnosed when SIRS<br />
occurs <strong>in</strong> the presence <strong>of</strong><br />
a suspected or confirmed<br />
<strong>in</strong>fection<br />
Severe sepsis (i.e.<br />
multiple organ<br />
dysfunction)<br />
Septic shock (i.e.<br />
severe sepsis with<br />
hypotension despite<br />
adequate fluid<br />
resuscitation) and<br />
death
Cl<strong>in</strong>ical presentation<br />
Sepsis<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Fever or hypothermia<br />
Hyperventilation<br />
Chills<br />
Shak<strong>in</strong>g<br />
Warm sk<strong>in</strong><br />
Sk<strong>in</strong> lesions<br />
Lethagy<br />
Confusion<br />
Coma<br />
Hyperglycaemia<br />
Ileus<br />
Muscle weakness<br />
Increased cardiac output<br />
Severe sepsis/septic<br />
shock<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Liver dysfunction (jaundice)<br />
Cool sk<strong>in</strong><br />
Pancreatitis<br />
Renal failure<br />
Decreased cardiac output<br />
Acute respiratory distress<br />
syndrome<br />
Multiple-organ dysfunction<br />
syndrome<br />
Encephalopathy<br />
Neuropathy<br />
DIC
Diagnosis & Management<br />
A rapid diagnosis is<br />
critical to meet the<br />
requirements <strong>of</strong> early<br />
goal directed therapy<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Nurs<strong>in</strong>g assessment<br />
Observations/record<strong>in</strong>gs<br />
Medical <strong>in</strong>tervention<br />
O2 Therapy<br />
Fluid resuscitation<br />
Exam<strong>in</strong>ation uro-genital<br />
tract<br />
Ur<strong>in</strong>alysis<br />
Blood test<br />
Ur<strong>in</strong>e & blood cultures<br />
Antibiotic Therapy
Case Study<br />
Optical Urethrotomy<br />
……<strong>Urosepsis</strong><br />
Mr C – age 83yrs<br />
Medical History:<br />
IHD<br />
CABG<br />
PE- post cholecystectomy<br />
40yrs ago<br />
Observations:<br />
BMI 41 Weight 110kgs<br />
T 37, HR 70, BP 163/85,<br />
R/R 16, O2 sats 98%
Optical Urethrotomy<br />
Telescopic <strong>in</strong>spection<br />
<strong>of</strong> the urethra and<br />
bladder with <strong>in</strong>cision<br />
<strong>of</strong> a stricture<br />
<br />
<br />
<br />
<br />
Operation time 60 m<strong>in</strong>s<br />
Recovery uneventful<br />
Perfalgan & Clexane <strong>in</strong><br />
PACU<br />
Obs stable
RTW<br />
After return<strong>in</strong>g to the<br />
ward at 1020hrs Mr C<br />
was comfortable and<br />
settled, was tak<strong>in</strong>g<br />
oral fluids and had<br />
managed a light diet.<br />
His wife was present<br />
Temp 36.9<br />
HR 58 (regular)<br />
RR 16<br />
B/P 130/69<br />
O2 Sats 95% on room air<br />
Pa<strong>in</strong> score 2/10<br />
Analgesia decl<strong>in</strong>ed<br />
IDC light haematuria<br />
At 1120 the status quo<br />
rema<strong>in</strong>ed
At 12midday…<br />
A member <strong>of</strong> the<br />
kitchen staff alerted<br />
the RN that Mr C had<br />
asked her for another<br />
blanket….she said he<br />
appeared to be<br />
shiver<strong>in</strong>g<br />
The RN immediately went to<br />
check her patient…Mr C<br />
Flushed <strong>in</strong> the face<br />
Shiver<strong>in</strong>g severely<br />
Experienc<strong>in</strong>g a rigor<br />
Temp 37.1<br />
Pulse 84<br />
B/P 195/116<br />
Resps 20<br />
O2 Sats on room air 92%
Immediate action…<br />
The RN’s immediate<br />
response was to start<br />
a nurs<strong>in</strong>g assessment<br />
to establish why Mr C<br />
was experienc<strong>in</strong>g<br />
these symptoms<br />
ABCDE<br />
O2 via nasal prongs @ 3L<br />
Circulatory status<br />
Pa<strong>in</strong> score rema<strong>in</strong>ed 2/10<br />
No <strong>in</strong>crease <strong>in</strong> resp effort<br />
respiratory <strong>in</strong>fection<br />
catheter blocked<br />
full bladder<br />
<strong>in</strong>fection somewhere<br />
2hrs post op – too early<br />
to be surgery related!!
1220 hrs<br />
Follow<strong>in</strong>g a nurs<strong>in</strong>g<br />
assessment, the RN<br />
phoned the<br />
anaesthetist<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Suspected sepsis<br />
Verbal order for stat dose<br />
<strong>of</strong> ABs (Amoxicill<strong>in</strong>)<br />
Urgent bloods<br />
CBC & Urea & Electrolyes<br />
Advise surgeon<br />
Confirmed anaesthetist’s<br />
suspicion – bacteraemia<br />
Verbal order for stat dose<br />
<strong>of</strong> Gentamyc<strong>in</strong><br />
Urgent blood cultures,<br />
TNT, CSU
Team work<br />
Consulted with the<br />
Team Leader &<br />
decision made to<br />
transfer Mr C to<br />
HDW.<br />
Ward nurses took<br />
over the care <strong>of</strong> RNs<br />
other patients<br />
T/L arranged for the<br />
urgent specimens to<br />
be taken
Rapid deterioration…<br />
After transfer to HDW<br />
Mr C’s condition<br />
began to rapidly<br />
deteriorate and by<br />
1330 he was show<strong>in</strong>g<br />
signs <strong>of</strong> confusion<br />
and irritability<br />
Temp 38.9 – 39.1<br />
B/P 232/106<br />
HR 92<br />
Resps 29<br />
O2 sats 99% @ 3L<br />
ABs @ 1230<br />
IV fluids @ 500mls/hr<br />
Oral Paracetomol<br />
Cool<strong>in</strong>g cares<br />
Support for Mrs C
Test results…<br />
At 1340hrs the<br />
surgeon phoned to<br />
advise the<br />
prelim<strong>in</strong>ary test<br />
results –<br />
Enterococcus<br />
Bacteraemia…<br />
sensitive to<br />
Amoxycill<strong>in</strong><br />
<br />
Possible that the<br />
organism was already <strong>in</strong><br />
Mr C’s ur<strong>in</strong>ary system<br />
before hav<strong>in</strong>g surgery
By 1500hrs…<br />
Mr C rema<strong>in</strong>ed<br />
febrile, confused,<br />
and irritable.<br />
UO began to drop –<br />
struggl<strong>in</strong>g to ma<strong>in</strong>ta<strong>in</strong><br />
30ml/hr<br />
His UO from RTW was<br />
800mls – however…<br />
<br />
<br />
O2 sats fall<strong>in</strong>g even with<br />
O2 @ 4-6L/m<strong>in</strong> (94-96%)<br />
HR & RR elevated
Transfer to the DHB<br />
Follow<strong>in</strong>g a review by<br />
the surgeon a<br />
decision was made to<br />
transfer Mr C to the<br />
DHB for further<br />
assessment &<br />
management
Discharge summary<br />
Full recovery<br />
Discharged after<br />
5 days<br />
Optical Urethrotomy<br />
and <strong>in</strong>sertion <strong>of</strong> SPC<br />
Discharge diagnosis –<br />
<strong>Urosepsis</strong> post Optical<br />
Urethrotomy<br />
2° diagnosis –<br />
- delirium<br />
- atelectasis<br />
- mild hypokalaemia<br />
- sweat rash<br />
Discharge meds <strong>in</strong>cluded<br />
10 days <strong>of</strong> oral antibiotics<br />
IDC <strong>in</strong> situ on discharge<br />
F/U appt with urologist
Reflection<br />
This case study<br />
reflects on the<br />
management <strong>of</strong> a<br />
unexpected complex<br />
cl<strong>in</strong>ical situation and<br />
the skill <strong>in</strong> which it<br />
was handled<br />
<br />
<br />
<br />
<br />
<br />
<br />
Communication<br />
Assessment<br />
Teamwork<br />
Nurs<strong>in</strong>g knowledge<br />
Efficiency<br />
Cultural needs met
To conclude…<br />
The shorter the<br />
time to effective<br />
treatment, the<br />
higher the success<br />
rate<br />
<br />
<br />
<br />
<br />
<br />
Early recognition <strong>of</strong><br />
symptoms<br />
Early diagnosis<br />
Early oxygen treatment<br />
Early fluid treatment<br />
Early antibiotic therapy<br />
<br />
Comprehensive teamwork
References<br />
Baird, N. (2012) Cl<strong>in</strong>ical Care Reflection. An unpublished<br />
refection<br />
Cystoscopy and Optical Internal Urethrotomy Peri-op<br />
Instructions. Retrieved from<br />
http://www.usadelaware.com/medicalbriefs/cystoscop<br />
yandoptical<strong>in</strong>ternalurethr...<br />
Wagenlehner F.M.E, Wolfgang W, Naber K.G. (2007)<br />
Pharmocok<strong>in</strong>etic Caracteristics <strong>of</strong> Antimicrobials and<br />
Optimal Treatment <strong>of</strong> <strong>Urosepsis</strong>. Cl<strong>in</strong> Pharmacolk<strong>in</strong>et<br />
2007; 46(4)<br />
Wagenlehner F.M.E, Pilatz A, Naber K.G. Weidner W. (2008)<br />
Therapeutic challenges <strong>of</strong> urosepsis. European Journal<br />
<strong>of</strong> Cl<strong>in</strong>ical Investigation 2008; 38: 45-49