Fall 2010 - SSM Cardinal Glennon Children's Medical Center
Fall 2010 - SSM Cardinal Glennon Children's Medical Center
Fall 2010 - SSM Cardinal Glennon Children's Medical Center
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Silent Service<br />
Reconstruction for Independence<br />
Treon McKinzie, 12, is ready for independence, but first she<br />
must depend on pediatric urologist Casimir Firlit, M.D.<br />
Born with myelomeningocele, lumbar lesion, with hydrocephalus,<br />
Treon has a VP shunt for hydrocephalus, which was<br />
placed at birth. Despite medical management and intermittent<br />
bladder catheterization, at 3 years old she had increased<br />
dilation of both kidneys as well as development of bilateral<br />
severe vesicoureteral reflux with frequent urinary tract infections.<br />
In order to protect her kidneys from damage, a vesicostomy<br />
was completed in which the bladder wall was brought to the<br />
abdominal wall and an opening was created in the lower abdominal<br />
wall below the umbilicus to allow urine to flow out<br />
of the bladder continuously. This has protected the kidneys<br />
well, but required her to wear diapers at all times due to the<br />
continuous, unobstructed flow of urine out of the bladder.<br />
“It’s important for children like Treon that we find solutions<br />
for issues like continence,” Dr. Firlit says. “She has a right to<br />
live like any other child and have that independence. She is<br />
the reason I do what I do.”<br />
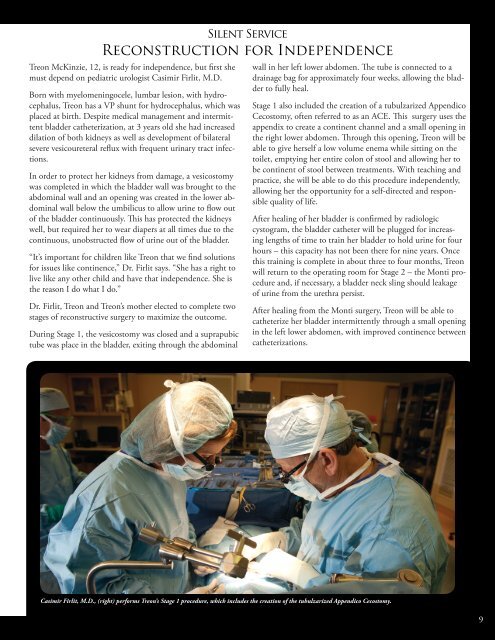
Dr. Firlit, Treon and Treon’s mother elected to complete two<br />
stages of reconstructive surgery to maximize the outcome.<br />
During Stage 1, the vesicostomy was closed and a suprapubic<br />
tube was place in the bladder, exiting through the abdominal<br />
wall in her left lower abdomen. The tube is connected to a<br />
drainage bag for approximately four weeks, allowing the bladder<br />
to fully heal.<br />
Stage 1 also included the creation of a tubulzarized Appendico<br />
Cecostomy, often referred to as an ACE. This surgery uses the<br />
appendix to create a continent channel and a small opening in<br />
the right lower abdomen. Through this opening, Treon will be<br />
able to give herself a low volume enema while sitting on the<br />
toilet, emptying her entire colon of stool and allowing her to<br />
be continent of stool between treatments. With teaching and<br />
practice, she will be able to do this procedure independently,<br />
allowing her the opportunity for a self-directed and responsible<br />
quality of life.<br />
After healing of her bladder is confirmed by radiologic<br />
cystogram, the bladder catheter will be plugged for increasing<br />
lengths of time to train her bladder to hold urine for four<br />
hours – this capacity has not been there for nine years. Once<br />
this training is complete in about three to four months, Treon<br />
will return to the operating room for Stage 2 – the Monti procedure<br />
and, if necessary, a bladder neck sling should leakage<br />
of urine from the urethra persist.<br />
After healing from the Monti surgery, Treon will be able to<br />
catheterize her bladder intermittently through a small opening<br />
in the left lower abdomen, with improved continence between<br />
catheterizations.<br />
Fereius Casimir et pliquo Firlit, te velicate M.D., (right) culla quae performs mod Treon’s que nihitatium Stage 1 procedure, coris mo et, which velles includes mo inum the dolorer creation ferrore of the hentis tubulzarized sundund Appendico empellatinto Cecostomy. cupid ut rere quam ipsandi beatur<br />
sum reris atur Abo. Ut molestiur Genectur<br />
9