Fall 2010 - SSM Cardinal Glennon Children's Medical Center
Fall 2010 - SSM Cardinal Glennon Children's Medical Center
Fall 2010 - SSM Cardinal Glennon Children's Medical Center
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
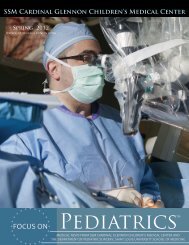
<strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong> Children’s <strong>Medical</strong> <strong>Center</strong><br />
<strong>Fall</strong> <strong>2010</strong><br />
www.cardinalglennon.com<br />
FOCUS ON<br />
Pediatrics<br />
®<br />
MEDICAL NEWS FROM <strong>SSM</strong> CARDINAL GLENNON CHILDREN’S MEDICAL CENTER AND<br />
THE DEPARTMENT OF PEDIATRIC SURGERY, SAINT LOUIS UNIVERSITY SCHOOL OF MEDICINE
ON THE COVER<br />
“I will not cut persons laboring under the stone,<br />
but will leave this to be done by men who are<br />
practitioners of this work.” – Hippocrates<br />
Anand V. Palagiri, M.D., performs laser lithotripsy on Irhad Sehovic, 15, to<br />
remove a large, painful kidney stone. Dr. Palagiri passed a small caliber scope into<br />
Irhad’s urinary tract to reach the painful stone. It was successfully fragmented and<br />
removed with the use of a laser fiber.<br />
Knowledge of stone prevention and treatment has come a long way since<br />
the era of Hippocrates, especially in terms of pediatric stone disease.<br />
In addition to laser lithotripsy, <strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong>’s Pediatric Stone <strong>Center</strong><br />
offers patients an all-inclusive approach to treating urinary stone disease with the<br />
latest technological treatment advances.<br />
FOCUS ON Pediatrics<br />
®<br />
Editor In Chief<br />
Sherlyn Hailstone<br />
President<br />
<strong>Medical</strong> Editor<br />
Kenneth Haller, MD<br />
Associate Professor of Pediatrics<br />
Editor<br />
Andrew Sutton<br />
Physician Services Manager<br />
Writer & Designer<br />
Katelyn Ideus<br />
Physician Communications Specialist<br />
<strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong><br />
Children’s <strong>Medical</strong> <strong>Center</strong><br />
Saint Louis University<br />
School of Medicine<br />
<strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong><br />
Children’s <strong>Medical</strong> <strong>Center</strong><br />
<strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong><br />
Children’s <strong>Medical</strong> <strong>Center</strong><br />
For comments and suggestions, please email FocusOnPeds@ssmhc.com.
Announcements<br />
<strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong> Welcomes Faculty<br />
Jerry<br />
Rosenblum, M.D.<br />
Gastroenterology<br />
The Division of Gastroenterology at<br />
<strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong> Children’s<br />
<strong>Medical</strong> <strong>Center</strong> is pleased to announce<br />
the addition of Jerry Rosenblum, M.D.,<br />
to its team of four gastroenterologists.<br />
Dr. Rosenblum joins <strong>Cardinal</strong> <strong>Glennon</strong><br />
after 18 years in private practice and<br />
30 years of experience. He continues<br />
to see patients at St. Luke’s Hospital in<br />
Chesterfield, Mo., as well as St. Joseph<br />
<strong>Medical</strong> Park in St. Charles, Mo.<br />
Stephen<br />
Braddock, M.D.<br />
Director, <strong>Medical</strong> Genetics<br />
This fall, <strong>Cardinal</strong> <strong>Glennon</strong>’s Division<br />
of <strong>Medical</strong> Genetics welcomed Stephen<br />
Braddock, M.D., as Division Director.<br />
Dr. Braddock joins <strong>Glennon</strong> after serving<br />
as Professor of Clinical Pediatrics<br />
at the University of Virginia School of<br />
Medicine.<br />
Awards<br />
William Keenan, M.D.<br />
American Academy of Pediatrics,<br />
“Virginia Apgar Award.”<br />
Recognizing Dr. Keenan as a<br />
pioneer in the field of neonatal<br />
resuscitation and as one of the<br />
founding members of the Neonatal<br />
Resuscitation Program.<br />
AAP National Conference &<br />
Exhibition; San Francisco, Calif.<br />
October 2, <strong>2010</strong>.<br />
Thomas Foy, M.D.<br />
Shalini Paruthi, M.D.<br />
Ellen Wood, M.D.<br />
<strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong>’s<br />
<strong>2010</strong> St. Luke’s Faithful Healer.<br />
Recognizing physicians for<br />
dedication to our values of<br />
compassion, excellence, stewardship,<br />
community and respect.<br />
Presentations<br />
Alexander<br />
Lin, M.D.<br />
Director, Plastic Surgery<br />
Christina<br />
Plikaitis, M.D.<br />
Plastic Surgery<br />
<strong>Cardinal</strong> <strong>Glennon</strong>’s Division of Plastic<br />
Surgery welcomes Alexander Lin, M.D.,<br />
as Division Director. Dr. Lin received<br />
his M.D. from Johns Hopkins School of<br />
Medicine in Baltimore, Md., and completed<br />
his fellowship in Craniofacial and<br />
Pediatric Plastic Surgery at the University<br />
of Pittsburgh <strong>Medical</strong> <strong>Center</strong>.<br />
Elizabeth<br />
Abraham, M.D.<br />
Nephrology<br />
Adnan<br />
Cutuk, M.D.<br />
Orthopedics<br />
Barbara<br />
Braddock M.D.<br />
Developmental Pediatrics<br />
Kasey<br />
Davis, M.D.<br />
Psychology<br />
Ron Mitchell, M.D.<br />
“Pediatric OSA: Outcomes of<br />
Surgical Therapy.”<br />
Tel-Aviv Sourasky <strong>Medical</strong><br />
<strong>Center</strong>: Department of<br />
Otolaryngology Head and Neck<br />
Surgery. June 18, <strong>2010</strong>.<br />
Miniseminar-Pediatric OSA.<br />
Inter-American Pediatric<br />
Otolaryngology Meeting.<br />
Panama City, Panama.<br />
July 30, <strong>2010</strong>.<br />
Publications<br />
Dr. Christina Plikaitis joins <strong>Glennon</strong><br />
after completing her fellowship in Pediatric<br />
Plastic Surgery at the University of<br />
Chicago.<br />
Vincent<br />
Gibbons, M.D.<br />
Neurology<br />
David<br />
Greenberg, M.D.<br />
Orthopedics<br />
Paruthi S, Chervin RD<br />
“Approaches to the assessment of<br />
arousals and sleep disturbance in<br />
children.” Sleep Med. <strong>2010</strong> Jul 8.<br />
1
Inpatient Satisfaction<br />
Scores Soar in <strong>2010</strong>!<br />
In July <strong>2010</strong>, several of <strong>Cardinal</strong> <strong>Glennon</strong>’s<br />
inpatient satisfaction scores reached the<br />
99th percentile in Press Ganey surveys.<br />
Transitional Care Unit<br />
99 th percentile<br />
Neonatal Intensive Care Unit<br />
99 th percentile<br />
Inpatient Unit: 4-North<br />
99 th percentile<br />
<strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong> building St. Louis’<br />
first pediatric hybrid catheterization lab<br />
<strong>Cardinal</strong> <strong>Glennon</strong> Children’s <strong>Medical</strong> <strong>Center</strong> will elevate children’s<br />
heart care in the metro area with the addition of a pediatric hybrid<br />
catheterization suite, the first in St. Louis.<br />
The suite will allow cardiac cath interventions and heart surgery to<br />
be performed in one session, reducing procedure time and providing<br />
advanced cardiac care at one time rather than an extended period of time.<br />
For many infants, the procedures performed in the hybrid cath lab are lifesaving.<br />
Using catheter-based interventions, surgeons are sometimes able to<br />
address problems without using open cardiac surgery and cardiopulmonary<br />
bypass. For a small infant or those younger than one year, the possibility of<br />
wellness without an invasive procedure is significant.<br />
Fetal Care Institute constructs new space<br />
The St. Louis Fetal Care Institute will open a new clinic suite at <strong>Cardinal</strong><br />
<strong>Glennon</strong>, bringing patients closer to pediatric specialists.<br />
In anticipation of longer stays for out-of-town patients or those meeting<br />
with several specialists in one day, the suite will include two nesting rooms<br />
complete with a couch, recliner, TV and computer. There will also be an<br />
examination and treatment room for ultrasounds and treatments such as<br />
amniocentesis. A monitor on the wall will make sure everyone in the room<br />
can see the images.<br />
Finally, a conference room large enough for a family and several specialists<br />
will provide ample space for consultations.<br />
Wireless Capsule Endoscopy<br />
Gastroenterologist performs first pediatric capsule endoscopes in St. Louis<br />
On June 24, Ajay Jain, M.D., of the Division of Pediatric<br />
Gastroenterology performed the first unique wireless capsule<br />
endoscopy in St. Louis. Since then, Dr. Jain has completed<br />
five capsules for <strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong> patients.<br />
a way to directly visualize the small bowel, thus significantly<br />
helping this large group of patients. This also makes <strong>Cardinal</strong><br />
<strong>Glennon</strong> the only pediatric hospital in the Saint Louis area to<br />
have an in-house capsule endoscopy facility.<br />
2<br />
The capsule provides direct visualization of the small bowel,<br />
an area inaccessible to regular endoscopy and colonoscopy.<br />
Though roughly the size of a Tylenol pill, the swallowed<br />
capsule houses:<br />
• A video camera<br />
• Lenses and battery<br />
• Light source<br />
As it traverses through the digestive system, it takes pictures<br />
and video, which are transmitted to a recorder via electrodes<br />
placed on the patient. Patients are free to move, go home or<br />
go to school during the procedure.<br />
In patients with chronic abdominal pain, small bowel<br />
Crohn’s disease or unidentified GI bleeding who might have<br />
remained undiagnosed or misdiagnosed, the capsule provides<br />
For more information and to earn CME credit from<br />
Saint Louis University, watch Dr. Jain’s presentation,<br />
“Wireless Capsule Endoscopy,” on Pediatrics on Demand!<br />
www.pediatricsondemand.com<br />
Username: ds\r010-online • Password: webcme<br />
Questions Email pediatricsondemand@ssmhc.com.
1 Year Later<br />
Andre Byrd, Jr., has been small since the moment he was born in April 2009.<br />
Now, 17 months old, his size is the least of his mother’s worries.<br />
“He is just so energetic we can barely keep up with him sometimes,” Sahreese<br />
Byrd says. “For everything he’s been through, you think you would be able to<br />
tell, but you can’t. I mean, he’s small, but everything else is great. He is such a<br />
blessing. He really is.”<br />
Andre was born 15 weeks early and without a heartbeat. He was quickly<br />
resuscitated and transferred from <strong>SSM</strong> St. Mary’s Health <strong>Center</strong> to <strong>Cardinal</strong><br />
<strong>Glennon</strong>’s NICU. Neonatologists Michael French, M.D., and Greg Booth, M.D.,<br />
treated Andre for hypotension, Patent Ductus Arteriosus (PDA), sepsis and lung<br />
disease.<br />
Since then, Andre has certainly lived up to how his parents immediately described<br />
him more than a year ago — Andre is a fighter. Not only did he survive, but he<br />
left his NICU bed three weeks before expected, taking only a heart monitor and<br />
1/16 liters of oxygen. He has returned a couple times, once for a week-long stay<br />
in the PICU for an episode that required him to be re-intubated.<br />
Check up with Andre<br />
Check in with the Division of Neonatology<br />
“Compared to how early he was, he actually did really well,” she says. “He didn’t<br />
get any colds this winter, any flu, it has just been the occasional wheezing. He<br />
has come in for some breathing treatments and made lots of friends with the<br />
respiratory staff.”<br />
Andre Byrd, Jr., 17-months, was born at 25 weeks gestation and<br />
without a heart beat. <strong>Cardinal</strong> <strong>Glennon</strong> neonatologists successfully<br />
cared for him, sending him home three weeks early.<br />
Within the last year, the Division of Neonatology has also welcomed a new Director. Richard Cooke, M.D., joined <strong>Glennon</strong>’s<br />
16 neonatologists as Division Director when William Keenan, M.D., stepped down in late 2009. Dr. Cooke says he joined<br />
<strong>Cardinal</strong> <strong>Glennon</strong> because of the hospital’s mission to provide compassionate care to everyone. He was also drawn to the<br />
hospital’s academic relationship with Saint Louis University.<br />
Dr. Cooke’s clinical and research interest is in fetal-infant nutrition. He notes that nutrition plays a critical role in determining<br />
outcomes, but that many unanswered questions remain about feeding high-risk infants.<br />
“Research is simply a way of giving the best possible care,” Dr. Cooke says. “We must know how to feed these infants in order<br />
to ensure they have the best possible short-term and long-term results.”<br />
Though he has stepped down as Division Director, Dr. Keenan<br />
continues to serve babies internationally. In June, the Helping<br />
Babies Breathe program officially launched in Washington, D.C.,<br />
and 100 Master Trainers received training. Dr. Keenan played<br />
a critical role in the development of the program, which was a<br />
restructuring of the Neonatal Resuscitation Program that he helped<br />
develop and has trained 2.2 million providers worldwide.<br />
Sahreese Byrd and her son Andre Byrd, Jr., pose with two of their friends from the<br />
<strong>Cardinal</strong> <strong>Glennon</strong> NICU. From left: neonatologist Greg Booth, M.D., and hospitalist<br />
Stacey Monaco, M.D.<br />
Also, on Oct. 2, Dr. Keenan received the prestigious Virginia<br />
Apgar Award from the American Academy of Pediatrics at the AAP<br />
National Conference & Exhibition in San Francisco, Calif. He was<br />
recognized as a pioneer in the field of neonatal resuscitation and<br />
as one of the founding members of the Neonatal Resuscitation<br />
Program. In the U.S., the death rate for babies has dropped<br />
an estimated 70 percent since the adoption of the Neonatal<br />
Resuscitation Program in 1987.<br />
3
Access <strong>Center</strong> assists an early morning delivery<br />
Shortly after giving birth on Aug. 11, Portia Rushing learned<br />
her son, Padien, was being transferred from Touchette Regional<br />
Hospital to <strong>Cardinal</strong> <strong>Glennon</strong> for “an episode with his<br />
heart.”<br />
At 5:58am, Jason Kesselring, M.D.,<br />
dialed the <strong>Cardinal</strong> <strong>Glennon</strong> Access<br />
<strong>Center</strong> to discuss Padien’s elevated<br />
heart rate of 280 and apparent supraventricular<br />
tachycardia (SVT). To<br />
determine whether or not a transfer<br />
was needed, he quickly consulted<br />
with a neonatologist as well as cardiologist Renuka Peterson,<br />
M.D., who advised medication for the rhythm.<br />
“The Access <strong>Center</strong> just makes everything easier and more efficient,”<br />
Dr. Kesselring says. “You don’t have to remember the<br />
NICU’s number, the ED’s number or the transports team’s<br />
number. You just dial and get someone who knows what they<br />
Do You Know:<br />
How to Use Weight Management<br />
Do you know: “During the past two decades, the prevalence of children who<br />
are obese has doubled, while the number of adolescents who are obese has<br />
tripled.” (American Academy of Pediatrics).<br />
are doing immediately.”<br />
Initially, parents of overweight and obese children should seek advice from<br />
their primary care provider. However, when more intensive weight management<br />
services are needed, it is best to use a pediatric weight management<br />
program, as services for adults or commercial weight loss programs are often<br />
not appropriate for children because of developmental and nutritional issues.<br />
• Due to growth and development, tracking progress in children goes<br />
beyond body weight. Growing children must be carefully weighed<br />
and measured at each visit to calculate BMI and plot this value on a<br />
growth curve or calculate a standard deviation score. In adults, this<br />
is not necessary, as body weight or BMI alone are sufficient to track<br />
progress.<br />
• Children have different nutritional needs than adults, especially in<br />
terms of portion size and daily allowances of nutrients.<br />
• Most importantly, children and many adolescents are not fully independent<br />
in terms of living a healthy lifestyle. They are easily influenced<br />
by adult role models, social cues, advertising, the environment<br />
and peer pressure. It takes a skilled team of pediatric specialists to<br />
recognize these influences and work within the context of the family<br />
and social environment to care for the child.<br />
The Access <strong>Center</strong> was the first in St. Louis and is answered<br />
24 hours a day, 7 days a week by transport-trained nurses.<br />
Physicians are also available any time<br />
to consult on possible transfers or<br />
basic questions. According to Access<br />
<strong>Center</strong> Director Karen Zahn, the<br />
<strong>Center</strong> has made transferring NICU<br />
babies quick and convenient for offsite<br />
locations.<br />
“Physicians can consult directly with<br />
the neonatologist and any other specialist to determine immediately<br />
if the baby needs to be transferred or not, and what<br />
they should do in the mean time,” Zahn says. “It makes everything<br />
more efficient for the physicians, transport team and,<br />
most importantly, the patient.”<br />
Top Row from Left: Kathryn Helling, RD, Clinical Nutrition; Amy<br />
Ford, PsyD, Psychology. Bottom Row from Left: Elizabeth Babusis,<br />
M.D., Lipid Disorders & Weight Loss; Nadim Kanafani, M.D.,<br />
Endocrinology & Diabetes; Kathy Spranaitis, PNP, Gastroenterology;<br />
Joel Nadler, PhD, Psychology<br />
<strong>Cardinal</strong> <strong>Glennon</strong>’s Weight Management Program includes pediatric specialists from endocrinology, lipid disorders, psychology,<br />
nutrition and gastroenterology. Patients work closely with providers who support behavior change through collaborative<br />
goal setting and motivational interviewing techniques. Education focuses on medical, behavioral and nutritional aspects of pediatric<br />
weight management. A patient’s initial visit lasts two to three hours and includes a one-hour nutrition class and healthy<br />
lunch. Depending on individual needs, patients can be seen as often as every three to four weeks.<br />
4<br />
To refer a patient, please have families call (314) 268-2700 ext 1695.
<strong>Glennon</strong> Expands Cochlear Implant Program<br />
The Division of Otolaryngology and the<br />
Department of Audiology have recently<br />
expanded their services, offering comprehensive<br />
hearing assessments to patients,<br />
full ENT and Audiology services at two<br />
locations — <strong>Cardinal</strong> <strong>Glennon</strong> and St. Anthony’s<br />
<strong>Medical</strong> <strong>Center</strong> in St. Louis — and<br />
dedicated cochlear implant audiologists.<br />
The Cochlear Implant Program, led by<br />
ENT surgeon Anita Jeyakumar, M.D.,<br />
cares for all children with moderate to<br />
severe hearing loss. Prior to making the<br />
decision to implant, each patient visits<br />
extensively with surgeons, audiologists,<br />
social workers and experienced nurses.<br />
The comprehensive approach also ensures<br />
coordinated visits with other specialities;<br />
hearing tests with or without sedation;<br />
communication with referring physician<br />
Cochlear Implant Program Director Anita Jeyakumar,<br />
M.D., performs a cochlear implant.<br />
Diversions<br />
within 24 hours of appointment; and education<br />
for parents.<br />
“Our goal is to be a resource to parents<br />
and children as they navigate through the<br />
child’s hearing loss,” Dr. Jeyakumar says.<br />
“For some, implantation is the solution,<br />
but for others it is not. Our belief is that<br />
every child deserves to hear, and we will do<br />
everything we can to provide a solution.”<br />
Full ENT and Audiology Services @<br />
<strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong><br />
1465 S. Grand Blvd, St. Louis, MO 63104<br />
ENT: 314.268.4010<br />
Audiology: 314.577.5671<br />
St. Anthony’s <strong>Medical</strong> <strong>Center</strong><br />
10010 Kennerly Rd., St. Louis, MO 63128<br />
ENT: 314.842.3535<br />
Audiology: 314.577.5671<br />
Andrew Sutton Physician Services Team Leader<br />
Dining<br />
Acero<br />
www.fialafood.com<br />
314.644.1790<br />
I’m hesitant to tell you about Acero.<br />
Not because the food or the service<br />
falls short of outstanding. Quite the<br />
contrary, this place is so fantastic,<br />
and so small, I want to keep it all to<br />
myself.<br />
Tucked at the end of a row of shops in Maplewood, this<br />
quaint spot focuses on perfecting the rustic Italian meal. Acero<br />
is owned by Jim Fiala (Liluma, Terrace View, The Crossing)<br />
and excels in providing a memorable experience through<br />
house-made pasta, imaginative dishes and attentive service.<br />
The three courses for $30 has to be the best deal in town. I’ve<br />
been twice, and I honestly feel I’m committing a crime for<br />
not paying more for my meal.<br />
Tricia and I both enjoyed the three course option during our<br />
last visit. We shared a couple “quartinos” of Soave, a crisp,<br />
citrus-forward wine from Italy, and kicked things off with the<br />
Acero salad, a blend of romaine, egg, onion, salumi and herb<br />
vinaigrette. The saltiness of the salumi, the heartiness of the<br />
egg and the zest of the vinaigrette all sing together in a delightful<br />
chorus. The delight carried through in to my second<br />
course, tagliatelle with morel mushrooms. The freshness of<br />
the house made pasta shines through and plays against the<br />
olive oil and earthiness of the mushrooms. Honestly, I could<br />
eat the tagliatelle as a meal, and I’m sure many people do.<br />
Tricia raved about her entree, a fresh-caught walleye, and I<br />
was blown away by my scallops. An imaginative presentation,<br />
the scallops are prepared with mandarin oranges, which lend a<br />
pleasing citrus flavor.<br />
Desserts are quite tasty. The highlights include the affagato -<br />
a shot of espresso poured on top of vanilla ice cream, and the<br />
warm chocolate torte, which also comes with a side of vanilla<br />
ice cream.<br />
Acero is small. The food is excellent. The service is personable.<br />
Reservations are recommended.<br />
Beverages<br />
Tricia and I recently popped open a bottle of 2007 Delas “St.<br />
Esprit” Cotes-du-Rhone. The Delas is a fine example of the<br />
outstanding Rhone wines cranked out in the 2007 vintage.<br />
An excellent value ($15.00), this blend of 75% Syrah and<br />
25% Grenache paints the glass a deep garnet color. The nose<br />
reveals chocolate, cedar, caramel and cola. Fruit-forward,<br />
layered, and with moderate tannins, black cherry stands out<br />
as the dominant player on the palate. A pleasing, medium<br />
finish rounds out this very enjoyable wine. Get some soon.<br />
The word is out on the value and quality of the 2007 Rhone<br />
vintage.<br />
5
What is independence For many children it’s<br />
the first few moments away from their parents’<br />
grasp, a slumber party in a friend’s basement<br />
or the first time they get the car keys. But for the patients<br />
within the Division of Pediatric Urology, it’s a lot of things<br />
people don’t want to talk about.<br />
Voiding dysfunction, incontinence and genital anomalies<br />
separate children from social norms and severely affect self<br />
esteem, bodily function and social interaction. So why<br />
doesn’t anyone want to talk about it<br />
“Many times, it is difficult for parents to find a venue to be<br />
heard and to thoroughly discuss these issues,” says Division<br />
Director Anand Palagiri, M.D. “But they are extremely<br />
important to quality of life and social acceptance, hence our<br />
mission to bridge the gap and address the problems either<br />
medically or surgically.”<br />
Dr. Palagiri and partner Casimir Firlit, M.D., provide comprehensive<br />
care, commonly treating conditions such as:<br />
• Undescended Testicle (Cryptorchidism)<br />
• Hypospadias (Abnormal urethral opening)<br />
The Silen<br />
<strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong> Div<br />
• Hernia<br />
• Hydrocele<br />
• Vesicoureteral Reflux<br />
• Obstructed Kidneys (UPJ obstruction)<br />
• Hydronephrosis (Prenatal/Postnatal)<br />
• Kidney Stones<br />
• Nocturnal Enuresis (Bed Wetting)<br />
• Voiding Dysfuntion<br />
• Circumcision and its complications<br />
• Urinary/Fecal Incontinence<br />
But they certainly don’t do it alone. Within their division<br />
they call upon clinical coordinator Kelly Lepsky, RN, surgical<br />
physician assistant Jenny Deyto, PA, and clinical nurse Louisa<br />
Salvin, RN. With more than 20 years of experience, nurse<br />
practitioners Jeanne Hermann, PNP, and Nancy VanCleave,<br />
PNP, offer high-quality care as they triage patients through<br />
weekly clinics and address dysfunctional voiding.<br />
This group also works tirelessly to ensure care to expectant<br />
mothers whose prentatal ultrasounds reveal urinary tract mal-<br />
Treating Vesicoureteral Reflux<br />
6<br />
After his first day of kindergarten, Donald Horvath, 5, receives a<br />
renal and bladder ultrasound at his first appointment with urology<br />
nurse practitioner Jeanne Hermann, PNP. Donald was fully toilet<br />
trained when he was 2 years old, but within the last year he has<br />
experienced several accidents along with a urinary tract infection. In<br />
her effort to rule out any anatomical abnormalities, Jeanne utilizes<br />
diagnostic imaging in the form of a renal ultrasound and a voiding<br />
cystogram.<br />
James Shipley, 5, awaits his turn for surgery. Dr. Palagiri<br />
and his team schedule a day for endoscopic injection<br />
procedures every eight to ten weeks. Today they completed 11<br />
cases. Nurse practitioner Nancy VanCleave, PNP, diagnosed<br />
James with VUR and addressed his dysfunctional voiding.<br />
With no improvement from conservative management,<br />
Dr. Palagiri suggested the minimally invasive injection<br />
procedure.<br />
Dr. Palagiri completes James Shipley’s 20<br />
deflux injection procedure. He inserts an<br />
through the urethra and up into the blad<br />
he passes a tiny needle through the endo<br />
dispenses the gel (deflux ) around the ur<br />
ing to create a mound that stops urinary<br />
Over time, the gel combines with fibrobl<br />
collagen, which stabilize the position an<br />
implant. Afterward, Dr. Palagiri met wi<br />
family. He told them James will have no<br />
restrictions and can return to school the
t Service<br />
ision of Pediatric Urology<br />
formations such as hydronephrosis, posterior urethral valves<br />
and bladder extrophy. For many mothers, early diagnosis<br />
and a prenatal consultation with pediatric urologists provides<br />
comfort as they know their baby is going to be cared for possibly<br />
prior to delivery or quickly thereafter.<br />
Many of urology issues also require the expertise of other<br />
pediatric specialists such as Nephrology, Radiology, Sleep<br />
Medicine, Neurology, Gastroenterology, Anesthesiology and<br />
Neonatology.<br />
When seeing a patient in clinic with nocturnal enuresis (bedwetting),<br />
Jeanne and Nancy often consider whether or not<br />
the patient is a candidate for Sleep Medicine Specialist Shalini<br />
Paruthi, M.D., especially if everything anatomically is working<br />
properly.<br />
“It’s important we work together to ensure we provide the<br />
most comprehensive diagnosis,” Dr. Paruthi says. “Complications<br />
such as enuresis can be devastating to a child’s self<br />
esteem and restrict their activities. I recently had a teenage<br />
patient who had never been on a sleep over because of nightly<br />
enuresis. She was very ashamed.”<br />
The Division of Urology also stays on the leading-edge of care<br />
with education about the newest techniques and technologies<br />
available to pediatric surgeons. This winter, Dr. Palagiri<br />
and Dr. Firlit will begin using the robotic da Vinci Surgical<br />
System for routine surgeries that, in the past, were only performed<br />
through an open incision. Pediatric urology procedures<br />
such as pyeloplasty, ureteral reimplantation and partial<br />
or total nephrectomy can now be performed in a minimally<br />
invasive fashion with the use of the robot.<br />
However, these surgical advances do not overshadow the fact<br />
that many of the Division’s patients need much more than<br />
surgical care, Dr. Palagiri says.<br />
“When we take a patient under our care we understand we<br />
are responsible for the entire patient — medically, surgically<br />
and emotionally,” Dr. Palagiri says. “We also understand that<br />
a lot of the conditions we address are extremely taxing on the<br />
child’s family, and we pride ourselves on comforting parents<br />
and openly discussing any of their concerns.”<br />
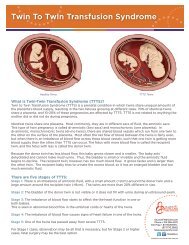
Vesicoureteral reflux is a condition in which urine backs up from the bladder into the kidney. For many children, this is caused by a faulty valve at the junction of the ureter<br />
and the bladder. It should operate as a one-way valve. Instead, it operates as a two-way valve and can allow urine in the bladder to flow backwards (reflux) into one or both<br />
ureters and kidneys. Reflux is dangerous when there is an infection in the bladder because it makes it much easier for bacteria to travel up the ureters and enter the kidneys<br />
where it may infect and scar them. Treatment for persistent reflux include both endoscopic injection for minor reflux and open surgery (reimplant surgery) for severe reflux.<br />
-minute<br />
endoscope<br />
der. Then<br />
scope and<br />
eteral openreflux.<br />
asts and<br />
d size of<br />
th James’<br />
physicial<br />
next day.<br />
Kaitlyn Wright, 8, models an anesthesia mask prior to her surgery. Kaitlyn<br />
would undergo a Bilateral Extravesical Ureteral Reimplant. With a success<br />
rate of 98 percent, this is a common procedure for Dr. Palagiri and his team to<br />
perform for a child with severe reflux.<br />
Dr. Palagiri isolates the ureter as he performs an ureteral reimplantation to<br />
correct severe VUR.<br />
7
Silent Service<br />
Reconstruction for Acceptance<br />
The moment her son, Gavin, was born, Nikki Mitchell knew<br />
something was wrong. An obstetric nurse from Hannibal,<br />
Mo., Nikki knows what a male baby’s body should look like,<br />
but for her son, something was different.<br />
Gavin was born with a genital anomaly known as hypospadias.<br />
Hypospadias is a common birth defect, occurring in one<br />
out of every 150 to 300 boys.<br />
It is a condition in which the urethral opening does not form<br />
completely to the tip of the penis. Instead, the opening may<br />
be located anywhere along the underside of the penis. While<br />
the urethral opening is most often found near the head, it also<br />
may be located from the middle of the penile shaft to the base<br />
of the penis or even behind the scrotum. Gavin’s hypospadias<br />
was of the latter, occurring in only 20% of all hypospadias. In<br />
severe cases such as Gavin’s, the penis will also have downward<br />
curvature, a condition called chordee.<br />
for Dr. Palagiri, specifically about anesthesia and pain.<br />
Dr. Palagiri told her he calls daily on the expertise of<br />
<strong>Cardinal</strong> <strong>Glennon</strong>’s pediatric-trained anesthesiologists who<br />
not only provide top-level care during the procedure, but<br />
manage pain post-operatively as well.<br />
From a mother’s point of view, Nikki asked about Gavin’s<br />
emotions – will he be scared Before going to the operating<br />
room, Child Life Specialist Colleen Brone, meets with<br />
children to find ways to calm their nerves or make their<br />
trip to the operating room easier. Also, <strong>Cardinal</strong> <strong>Glennon</strong>’s<br />
operating rooms allow children to watch movies as they fall<br />
asleep.<br />
“I’m coming from the perspective of a mother and a nurse,”<br />
Nikki says before Gavin goes to the operating room, “and I<br />
feel comfortable from both perspectives with the care<br />
Dr. Palagiri and his team have provided Gavin.<br />
“I always emphasize to parents, especially mothers, that they<br />
did nothing wrong,” Dr. Palagiri says. “Sometimes it’s difficult<br />
for parents to understand how something like this can<br />
happen, and that’s why we take the time to explain everything<br />
and insist that there are no silly questions.”<br />
Due to her nursing background, Nikki had several questions<br />
“You can tell Dr. Palagiri has a family. He is so understanding<br />
and takes the time to meet with us and then walk us<br />
out, carrying Gavin the whole way. How often do you really<br />
get that kind of care from a surgeon”<br />
During the 3-hour hypospadias repair, Dr. Palagiri finally<br />
puts Nikki’s worries to rest for the first time in 20 months.<br />
First, he works out the mechanics, straightening the penis<br />
and creating a tube from the hole to where it should be.<br />
Then he focuses on the cosmetics.<br />
“It is one thing for the hole to be brought to the tip of the<br />
penis, however, what the penis looks like afterwards is a<br />
whole other ball game,” Dr. Palagiri says. “It’s extremely<br />
important to the esteem of a male child. We live in a society<br />
where it matters to have a normal-looking penis, and my<br />
goal is to make sure the children I work with have no idea<br />
anything was ever an issue.”<br />
8<br />
Gavin Mitchell, 17 months, smiles with his parents prior to surgery.<br />
Gavin was born with a severe hypospadias, which Dr. Palagiri corrected<br />
in a 3-hour hypospadias repair.<br />
“You can tell Dr. Palagiri has a<br />
family. He is so understanding<br />
and takes the time to meet with<br />
us and then walk us out, carrying<br />
Gavin the whole way. How often<br />
do you really get that kind<br />
of care from a surgeon”<br />
— Nikki Mitchell, mother
Silent Service<br />
Reconstruction for Independence<br />
Treon McKinzie, 12, is ready for independence, but first she<br />
must depend on pediatric urologist Casimir Firlit, M.D.<br />
Born with myelomeningocele, lumbar lesion, with hydrocephalus,<br />
Treon has a VP shunt for hydrocephalus, which was<br />
placed at birth. Despite medical management and intermittent<br />
bladder catheterization, at 3 years old she had increased<br />
dilation of both kidneys as well as development of bilateral<br />
severe vesicoureteral reflux with frequent urinary tract infections.<br />
In order to protect her kidneys from damage, a vesicostomy<br />
was completed in which the bladder wall was brought to the<br />
abdominal wall and an opening was created in the lower abdominal<br />
wall below the umbilicus to allow urine to flow out<br />
of the bladder continuously. This has protected the kidneys<br />
well, but required her to wear diapers at all times due to the<br />
continuous, unobstructed flow of urine out of the bladder.<br />
“It’s important for children like Treon that we find solutions<br />
for issues like continence,” Dr. Firlit says. “She has a right to<br />
live like any other child and have that independence. She is<br />
the reason I do what I do.”<br />
Dr. Firlit, Treon and Treon’s mother elected to complete two<br />
stages of reconstructive surgery to maximize the outcome.<br />
During Stage 1, the vesicostomy was closed and a suprapubic<br />
tube was place in the bladder, exiting through the abdominal<br />
wall in her left lower abdomen. The tube is connected to a<br />
drainage bag for approximately four weeks, allowing the bladder<br />
to fully heal.<br />
Stage 1 also included the creation of a tubulzarized Appendico<br />
Cecostomy, often referred to as an ACE. This surgery uses the<br />
appendix to create a continent channel and a small opening in<br />
the right lower abdomen. Through this opening, Treon will be<br />
able to give herself a low volume enema while sitting on the<br />
toilet, emptying her entire colon of stool and allowing her to<br />
be continent of stool between treatments. With teaching and<br />
practice, she will be able to do this procedure independently,<br />
allowing her the opportunity for a self-directed and responsible<br />
quality of life.<br />
After healing of her bladder is confirmed by radiologic<br />
cystogram, the bladder catheter will be plugged for increasing<br />
lengths of time to train her bladder to hold urine for four<br />
hours – this capacity has not been there for nine years. Once<br />
this training is complete in about three to four months, Treon<br />
will return to the operating room for Stage 2 – the Monti procedure<br />
and, if necessary, a bladder neck sling should leakage<br />
of urine from the urethra persist.<br />
After healing from the Monti surgery, Treon will be able to<br />
catheterize her bladder intermittently through a small opening<br />
in the left lower abdomen, with improved continence between<br />
catheterizations.<br />
Fereius Casimir et pliquo Firlit, te velicate M.D., (right) culla quae performs mod Treon’s que nihitatium Stage 1 procedure, coris mo et, which velles includes mo inum the dolorer creation ferrore of the hentis tubulzarized sundund Appendico empellatinto Cecostomy. cupid ut rere quam ipsandi beatur<br />
sum reris atur Abo. Ut molestiur Genectur<br />
9
Left: Using a video screen, Anand Palagiri, M.D., navigates through the ureter to the kidney to find Irhad Sehovid’s kidney stone. Using a laser fiber, he disintegrates the<br />
kidney stone and pulls out the smaller pieces. Right: Dr. Palagiri directs the laser fiber to the kidney stone and blasts it apart.<br />
It was a Monday morning at 5:00am when Irhad Sehovic, 15,<br />
woke up with a terrible pain in his left side.<br />
Silent Service<br />
Pediatric Stone <strong>Center</strong><br />
factors is initiated. What we do now will impact these children<br />
positively for the rest of their lives.”<br />
10<br />
“I tried eating something, but it wouldn’t go away,” he says.<br />
“It was the worst pain I have ever experienced.”<br />
When Irhad began vomiting, his parents rushed him to the<br />
emergency room. When his vomiting persisted even after<br />
medication, he was sent to <strong>Cardinal</strong> <strong>Glennon</strong> via ambulance.<br />
Emergency physicians diagnosed him with a kidney stone.<br />
Little did Irhad know he had been taken to the right place. In<br />
2007, <strong>Cardinal</strong> <strong>Glennon</strong> launched the Midwest’s first Pediatric<br />
Kidney Stone <strong>Center</strong> to address the painful problem that<br />
is increasing among young children.<br />
Kidney stones are caused by diet, dehydration or genetic<br />
factors, which must be addressed to keep stones from reoccurring.<br />
However, for children, once a stone has formed, they<br />
are usually difficult to pass due to the smaller caliber of the<br />
urinary tract. According to Dr. Palagiri, there is no stone the<br />
<strong>Center</strong> can’t remove in any child.<br />
“Kids have a bright future ahead of them when we deal with<br />
and treat the stones early on,” Dr. Palagiri says. “Currently, we<br />
offer state-of-the-art, minimally invasive techniques to remove<br />
stones. In collaboration with Dr. Ellen Wood and her team of<br />
nephrologists, a thorough evaluation of the etiology and risks<br />
To treat kidney stones, Dr. Palagiri established a protocol specifically<br />
tailored to children given the delicate nature of their<br />
urinary tract. It usually follows these steps and requires up to<br />
three separate procedures:<br />
1. Placement of a ureteral stent: The stent protects the<br />
kidney and ureter and alleviates the obstruction caused<br />
by the stone. At the same time, it dilates the ureter prior<br />
to the second procedure.<br />
2. Procedures:<br />
• Holmium Laser: Using a tiny camera and a scope,<br />
Dr. Palagiri inserts a small laser fiber that targets<br />
and breaks apart the stone so it can be removed in<br />
multiple pieces.<br />
• Extracorporeal Shock Wave Lithotripsy (ESWL):<br />
If the stone is in the kidney and can be seen on<br />
diagnostic x-ray, the <strong>Center</strong> may elect to use sound<br />
waves to target the stone. The stone is pulverized<br />
into sand and is much easier to pass. This option<br />
requires no invasion of the body.<br />
3. Stent Removal: When a stone requires manipulation to<br />
be removed, often times the ureter can swell shut after<br />
the intervention. In these cases, Dr. Palagiri will leave a<br />
stent behind to protect the ureter. He then removes it
da Vinci Surgical System<br />
This winter, the Division of Pediatric Urology<br />
at <strong>Cardinal</strong> <strong>Glennon</strong> will begin using the da<br />
Vinci Surgical System.<br />
The robotic system offers even smaller<br />
instruments, which are beneficial for the<br />
smaller bodies of pediatric patients. Anand<br />
Palagiri, M.D., says the da Vinci is especially<br />
useful for procedures that require fine sewing,<br />
such as kidney procedures.<br />
The da Vinci also allows for procedures once<br />
performed openly, to be completed minimally<br />
invasively. These include:<br />
• Pyeloplasty<br />
• Ureteral reimplantation<br />
• Partial or total nephrectomy<br />
Features of the da Vinci Surgical System<br />
include:<br />
• High-resolution, 3D video<br />
• Fully articulating instruments<br />
• State of the art robotic technology<br />
Benefits for patients include:<br />
• Shorter length of stay<br />
• Lower complication rates<br />
• Less post-op pain<br />
• Superior outcomes<br />
one week later.<br />
4. Testing: Once the stone is removed, it is sent for stone<br />
analysis. A 24-hour urine collection is also completed by<br />
the patients several weeks after the surgery. These values<br />
often help determine whether there are any metabolic<br />
abnormalities. Urology works closely with the Division<br />
of Nephrology based on the results of this testing. If<br />
there are concerns on the molecular level, the patient<br />
will work with nephrologists and possibly clinical nutritionists<br />
to determine the needed course.<br />
5. Basic Preventions: To avoid stones, Dr. Palagiri suggests<br />
limiting dark-colored sodas, iced tea and salt. The stone<br />
center’s motto is as follows: “The solution to pollution is<br />
dilution,” so drink lots of water and remain hydrated.<br />
One week after his painful morning, Irhad underwent laser<br />
lithotripsy with the homenum laser. Dr. Palagiri inserted a<br />
scope through Irhad’s urinary tract and into his kidney. He<br />
located the stone and inserted the laser fiber, which successfully<br />
disintegrated the stone. The remaining pieces were then<br />
removed from the urinary tract.<br />
“My advice would be to not do what I<br />
did,” Irhad says. “Drink all the water<br />
you can. But, if you do end up here<br />
at <strong>Cardinal</strong> <strong>Glennon</strong>, you’ll probably<br />
end up having a good time.”<br />
11
Q&A<br />
Anand Palagiri, M.D.,<br />
Division Director, Pediatric Urology<br />
Front from left: Nurse Practitioners Nancy VanCleave, PNP, and Jeanne Hermann, PNP;<br />
clinical coordinator Kelly North-Lepsky, RN. Back: Anand Palagiri, M.D.<br />
Q: What is the most challenging part of your job<br />
A: In pediatrics, parents entrust you with the care of their<br />
child and that is not something we take lightly. We want to<br />
make sure that child has a great future. It’s a daunting task,<br />
but I look forward to the challenge. I want to do everything<br />
and anything in my power to make sure the parent has<br />
absolute trust in the services we provide.<br />
Q: Why is your Division important to the health care of<br />
children<br />
A: Continence equals independence. It is extremely important<br />
to parents and their children and has a lot of social impact.<br />
Urology also has an evolving role as diets change, not always<br />
for the better, creating issues such as kidney stones that we are<br />
witnessing at younger ages. These issues need to be addressed<br />
at an early age so we can equip these children with what they<br />
need to ensure a healthy future.<br />
Q: Why did you choose pediatric urology<br />
A: As a urologist, my father played a pivotal role in my career<br />
choice. I grew up watching him care for patients and make<br />
their quality of life better. During medical school and urology<br />
residency, I had an excellent exposure to colleagues in the field<br />
specific to pediatric urology.<br />
I’ve always enjoyed the surgical reconstruction as well as<br />
the challenges urologic problems pose in children. Urologic<br />
problems are not widely known because of the personal<br />
nature of the issues. Those who are in the specialty dedicate<br />
their time to the patient and their families to validate their<br />
concerns. We understand these concerns are never trivial,<br />
especially in terms of reconstruction of the genitalia and<br />
voiding issues. These are a huge part of a child’s self esteem in<br />
today’s society.<br />
Q: How has technology impacted your specialty and how<br />
will it in the future<br />
A: Technology has improved significantly in terms of size of<br />
instruments. Because of this, we are tackling procedures that<br />
were once foreign to pediatric urologists due to the lack of<br />
instrumentation. We as technicians should strive to improve<br />
just not our skills, but our tools for surgical perfection.<br />
To reach DR. Palagiri<br />
Please Call:<br />
(314) 268-2700<br />
ext 6843.<br />
12
Pediatric Urology<br />
Faculty<br />
Anand Palagiri, M.D.<br />
Division Director, Pediatric Urology<br />
B.A. Music/B.A. Biology: Washington University, St. Louis, MO<br />
M.D. with Distinction in Research: Saint Louis University School of<br />
Medicine, St. Louis, MO<br />
Residency in Urology: Saint Louis University School of Medicine,<br />
St. Louis, MO<br />
Fellowship in Pediatric Urology: Saint Louis University School of Medicine,<br />
St. Louis, MO<br />
Diplomate, American Board of Urology &<br />
Certificate of Added Qualification, Pediatric Urology<br />
Clinical Assistant Professor of Urology: Saint Louis University School of<br />
Medicine, St. Louis, MO<br />
Casimir Firlit, M.D., Ph.D.<br />
M.S. in Pharmacology: Loyola University of Chicago, Chicago, IL<br />
M.D.: Loyola University of Chicago, Chicago, IL<br />
Ph.D. in Pharmacology: Loyola University of Chicago, Chicago, IL<br />
Fellowship: Lederle <strong>Medical</strong> Student Fellowship in Research, Loyola University<br />
of Chicago <strong>Medical</strong> School, Chicago, IL<br />
Clinical Fellowship in Pediatric Urology: Children’s Memorial Hospital/<br />
Northwestern University, Chicago, IL<br />
Clinical Preceptorship in Pediatric Renal Transplantation: Children’s<br />
Memorial Hospital/Northwestern University, Chicago, IL<br />
Jenny Deyto, PA C<br />
Bachelor of Arts - International Affairs: The George Washington University,<br />
Washington, D.C.<br />
Master of <strong>Medical</strong> Science - Physician Assistant Studies: Saint Louis<br />
University, St. Louis, MO<br />
Pediatric Urology<br />
Staff<br />
Jeanne Hermann, RN, CPNP<br />
Bachelor of Arts-Biology: Webster University, St. Louis, MO<br />
Bachelor of Science in Nursing: Saint Louis University, St. Louis, MO<br />
P.N.P. Certification: <strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong> Children’s <strong>Medical</strong> <strong>Center</strong>,<br />
Saint Louis University, St. Louis, MO<br />
Nancy VanCleave, RN, CPNP<br />
Bachelors of Science in Nursing: St. Louis University, St. Louis, MO<br />
P.N.P. Certification: <strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong> Children’s <strong>Medical</strong> <strong>Center</strong>,<br />
Saint Louis University, St. Louis, MO<br />
Kelly North-Lepsky, RN<br />
Clinical Coordinator<br />
Associates Degree in Nursing: St. Louis Community College, St. Louis, MO<br />
Bachelor of Science - Criminal Justice Studies: University of Missouri Saint<br />
Louis, St. Louis, MO<br />
Louisa Salvin, RN<br />
Urodynamics, Myelomeningocele Clinical Nurse<br />
Bachelor of Arts: Wellesley College, Wellesley, MA<br />
Diploma - Nursing: Newton Wellesley School of Nursing, Newton, MA<br />
To reach our faculty or staff, please call (314) 577-5334.<br />
13
Physician Services Department<br />
1465 South Grand Blvd.<br />
Saint Louis, Missouri 63104-1095<br />
Non Profit Org<br />
U.S. Postage<br />
PAID<br />
St. Louis, MO<br />
Permit No. 2412