CHN2706 Hemorrhagic Stroke Admission Orders.pdf - Carondelet
CHN2706 Hemorrhagic Stroke Admission Orders.pdf - Carondelet
CHN2706 Hemorrhagic Stroke Admission Orders.pdf - Carondelet
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
P<br />
H<br />
Y<br />
S<br />
I<br />
C<br />
I<br />
A<br />
N<br />
‘<br />
S<br />
O<br />
R<br />
D<br />
E<br />
R<br />
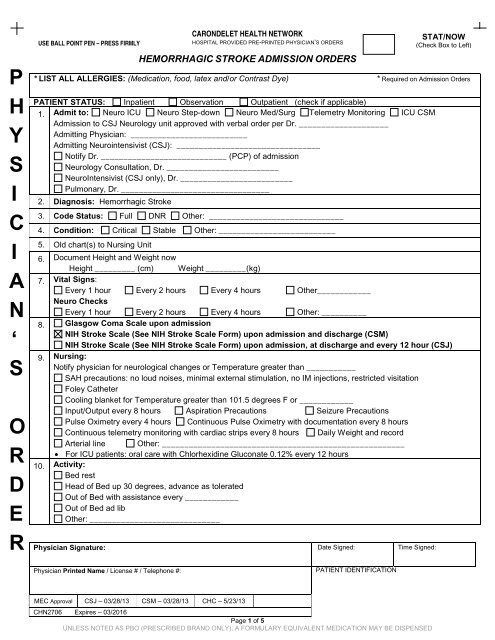
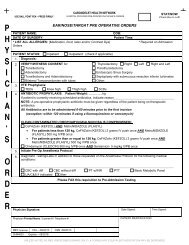
USE BALL POINT PEN – PRESS FIRMLY<br />
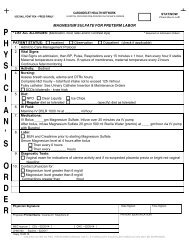
CARONDELET HEALTH NETWORK<br />
HOSPITAL PROVIDED PRE-PRINTED PHYSICIAN’S ORDERS<br />
HEMORRHAGIC STROKE ADMISSION ORDERS<br />
Physician Signature: Date Signed: Time Signed:<br />
STAT/NOW<br />
(Check Box to Left)<br />
* LIST ALL ALLERGIES: (Medication, food, latex and/or Contrast Dye) * Required on <strong>Admission</strong> <strong>Orders</strong><br />
PATIENT STATUS: Inpatient Observation Outpatient (check if applicable)<br />
1. Admit to: Neuro ICU Neuro Step-down Neuro Med/Surg Telemetry Monitoring ICU CSM<br />
<strong>Admission</strong> to CSJ Neurology unit approved with verbal order per Dr. ____________________<br />
Admitting Physician: __________________________<br />
Admitting Neurointensivist (CSJ): ________________________________<br />
Notify Dr. ____________________________ (PCP) of admission<br />
Neurology Consultation, Dr. _________________________<br />
NeuroIntensivist (CSJ only), Dr. _________________________<br />
Pulmonary, Dr. _________________________________<br />
2. Diagnosis: <strong>Hemorrhagic</strong> <strong>Stroke</strong><br />
3. Code Status: Full DNR Other: ______________________________<br />
4. Condition: Critical Stable Other: __________________________<br />
5. Old chart(s) to Nursing Unit<br />
6. Document Height and Weight now<br />
Height _________ (cm)<br />
Weight _________(kg)<br />
7. Vital Signs:<br />
Every 1 hour Every 2 hours Every 4 hours Other____________<br />
Neuro Checks<br />
Every 1 hour Every 2 hours Every 4 hours Other: __________<br />
8. Glasgow Coma Scale upon admission<br />
NIH <strong>Stroke</strong> Scale (See NIH <strong>Stroke</strong> Scale Form) upon admission and discharge (CSM)<br />
NIH <strong>Stroke</strong> Scale (See NIH <strong>Stroke</strong> Scale Form) upon admission, at discharge and every 12 hour (CSJ)<br />
9. Nursing:<br />
Notify physician for neurological changes or Temperature greater than ___________<br />
SAH precautions: no loud noises, minimal external stimulation, no IM injections, restricted visitation<br />
Foley Catheter<br />
Cooling blanket for Temperature greater than 101.5 degrees F or ____________<br />
Input/Output every 8 hours Aspiration Precautions Seizure Precautions<br />
Pulse Oximetry every 4 hours Continuous Pulse Oximetry with documentation every 8 hours<br />
Continuous telemetry monitoring with cardiac strips every 8 hours Daily Weight and record<br />
Arterial line Other: ______________________________________________________<br />
• For ICU patients: oral care with Chlorhexidine Gluconate 0.12% every 12 hours<br />
10. Activity:<br />
Bed rest<br />
Head of Bed up 30 degrees, advance as tolerated<br />
Out of Bed with assistance every ____________<br />
Out of Bed ad lib<br />
Other: _____________________________<br />
Physician Printed Name / License # / Telephone #:<br />
PATIENT IDENTIFICATION<br />
MEC Approval CSJ – 03/28/13 CSM – 03/28/13 CHC – 5/23/13<br />
<strong>CHN2706</strong> Expires – 03/2016<br />
Page 1 of 5<br />
UNLESS NOTED AS PBO (PRESCRIBED BRAND ONLY), A FORMULARY EQUIVALENT MEDICATION MAY BE DISPENSED
P<br />
H<br />
Y<br />
S<br />
I<br />
C<br />
I<br />
A<br />
N<br />
‘<br />
S<br />
O<br />
R<br />
D<br />
E<br />
R<br />
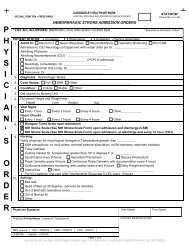
USE BALL POINT PEN – PRESS FIRMLY<br />
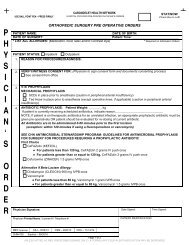
CARONDELET HEALTH NETWORK<br />
HOSPITAL PROVIDED PRE-PRINTED PHYSICIAN’S ORDERS<br />
HEMORRHAGIC STROKE ADMISSION ORDERS<br />
Physician Signature: Date Signed: Time Signed:<br />
STAT/NOW<br />
(Check Box to Left)<br />
11. Diet: Complete Dysphagia Screen prior to ANY oral intake<br />
NPO<br />
STRICT NPO until dysphagia screen completed and documented by RN. If abnormal, NPO and consult speech<br />
therapy<br />
When dysphagia screen completed and cleared, then:<br />
Regular 2 gram Sodium ________ Cal ADA Diet Low Cholesterol Pureed Soft Mechanical<br />
No Caffeine (INCLUDES NO DECAF COFFEE) Other: _____________________________<br />
12. Patient Teaching For:<br />
TIA, <strong>Stroke</strong> and Secondary <strong>Stroke</strong> Risk Prevention<br />
CHF (Also, identify chart as CHF Patient and add Blue Progress Notes)<br />
Diabetes Warfarin (Coumadin) Seizures Asthma<br />
13. IV Fluid:<br />
0.9% Sodium Chloride (NS) IV at _________ mL/hour Saline Lock<br />
Other: ____________________________ at mL/hour with ______mEq Potassium Chloride/Liter<br />
14. Glycemic Control:<br />
Choose one:<br />
Finger stick blood glucose every ______ hours<br />
Finger stick blood glucose before meals and at bedtime<br />
Finger stick – other: _______________________________________________<br />
Use insulin sliding scale to cover:<br />
Meals only<br />
All fingersticks<br />
Other: ______________________________________________<br />
Prescribe one:<br />
Insulin Aspart (NovoLOG) Sliding Scale Protocol – Mild<br />
Insulin Aspart (NovoLOG) Sliding Scale Protocol – Moderate<br />
Insulin Aspart (NovoLOG) Sliding Scale Protocol - Aggressive<br />
15. VTE prophylaxis:<br />
Risk assessment for VTE prophylaxis already completed<br />
Relative or Absolute Contraindications to Anticoagulant and/or Mechanical Prophylaxis (check all that apply)<br />
If contraindications present re-assess in 3-5 days<br />
Active Bleeding<br />
Within 24 hours of neuraxial anesthesia/analgesia<br />
Risk of Bleeding (including but not limited to<br />
History of heparin-induced thrombocytopenia (HIT)<br />
coagulopathy, recent intracranial or intraocular<br />
(unfractionated heparin and enoxaparin contraindicated)<br />
surgery, hemorrhagic stroke or traumatic head injury<br />
Clinically significant thrombocytopenia<br />
Other: _________________________________<br />
Physician <strong>Orders</strong>: See assessment tool on last page<br />
Sequential Compression Devices to bilateral lower extremities (caution in peripheral arterial insufficiency)<br />
Enoxaparin (LOVENOX) 40 mg subcutaneous daily<br />
Enoxaparin (LOVENOX) 30 mg subcutaneous twice daily<br />
Enoxaparin (LOVENOX) 30 mg subcutaneous daily (renal insufficiency CrCL less than 30 mL/min, not on dialysis)<br />
Fondaparinux (ARIXTRA) 2.5 mg subcutaneous daily (HIT patients only; contraindicated if weight less than 50 kg<br />
or CrCl less than 30 mL/minute<br />
Other: ______________________________________________________<br />
Physician Printed Name / License # / Telephone #:<br />
PATIENT IDENTIFICATION<br />
MEC Approval CSJ – 03/28/13 CSM – 03/28/13 CHC – 5/23/13<br />
<strong>CHN2706</strong> Expires – 03/2016<br />
Page 2 of 5<br />
UNLESS NOTED AS PBO (PRESCRIBED BRAND ONLY), A FORMULARY EQUIVALENT MEDICATION MAY BE DISPENSED
P<br />
H<br />
Y<br />
S<br />
I<br />
C<br />
I<br />
A<br />
N<br />
‘<br />
S<br />
O<br />
R<br />
D<br />
E<br />
R<br />
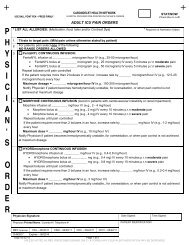
USE BALL POINT PEN – PRESS FIRMLY<br />
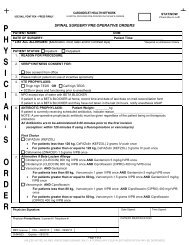
CARONDELET HEALTH NETWORK<br />
HOSPITAL PROVIDED PRE-PRINTED PHYSICIAN’S ORDERS<br />
HEMORRHAGIC STROKE ADMISSION ORDERS<br />
Physician Signature: Date Signed: Time Signed:<br />
STAT/NOW<br />
(Check Box to Left)<br />
16. Medications:<br />
Pravastatin (PRAVACHOL) ________ mg PO every evening<br />
Laxatives<br />
Milk of Magnesia Concentrate 10 mL PO daily PRN mild constipation<br />
Bisacodyl (DULCOLAX) 10 mg PR daily PRN severe constipation<br />
Sodium Phosphate (FLEETS) enema PR daily PRN severe constipation<br />
Anxiety:<br />
Lorazepam (ATIVAN) 0.5 mg IV/PO every 6 hours PRN anxiety<br />
Dyspepsia:<br />
Famotidine (PEPCID) 20 mg IV/PO every 12 hours Stress Ulcer Prophylaxis<br />
Famotidine (PEPCID) 20 mg IV/PO once daily (if CrCl less than 50 mL/minute) Stress Ulcer Prophylaxis<br />
Aluminum Hydroxide/Magnesium Hydroxide/Simethicone 30 mL PO 4 times daily PRN dyspepsia<br />
Calcium Carbonate (TUMS) 500 mg 2 tabs PO every 4 hours PRN heartburn<br />
Pain:<br />
Morphine 2 mg ______ mg IV every 1 hour PRN severe pain<br />
OXYcodone/Acetaminophen 5mg/325 mg (PERCOCET) 2 tablets PO every 4 hours PRN moderate pain<br />
Acetaminophen (TYLENOL) 650 mg PO every 4 hours PRN for pain<br />
Acetaminophen not to exceed<br />
Acetaminophen (TYLENOL) 650 mg suppository PR every 4 hours PRN for pain 4 grams per 24 hours<br />
Nausea:<br />
Ondansetron (ZOFRAN) 4mg IV every 6 hours PRN nausea/vomiting<br />
Promethazine (PHENERGAN) 12.5 mg PO/IV every 4 hours PRN nausea/vomiting<br />
Other: _____________________________________________________________________________<br />
Other Medications:<br />
Fosphenytoin 15 mg/kg IV load _______ mg now STAT, then _________ mg IV every 8 hours starting at _______<br />
Nimodipine 60 mg PO/NGT every 4 hours<br />
Keppra (LEVETIRACETAM) 500 mg PO every 12 hours<br />
17. Oxygen at ________ liters/minute via Nasal Cannula Face Mask<br />
18. **ICU ONLY**<br />
Blood Pressure Medications:<br />
If systolic B/P is greater than180 mmHg or ____________, MAP greater than 130, or __________, give:<br />
Labetalol 10 mg IV slow push over 2 minutes, then<br />
Repeat Labetalol 20 mg IV slow push every 10 minutes PRN up to 300 mg<br />
OR<br />
After first dose start Labetalol IV drip at 2 mg/minute and titrate in increments of 0.5 mg every 2 minutes<br />
(max rate 8 mg/minute) to maintain systolic B/P less than _________ mmHg<br />
OR<br />
Start NiCARdipine (CARDENE) IV drip at 5mg/hour and titrate in increments of 2.5 mg/hour every 5 minutes<br />
(max rate 15 mg/hour) to maintain a systolic BP less than _________ mmHg<br />
OR<br />
Enalaprilat (VASOTEC) 0.625 mg 1.25 mg 2.5 mg IV slow push every 6 hours PRN. to maintain<br />
systolic BP less than __________ mmHg<br />
Esmolol 250 micrograms/kg loading dose IV, then 50 microgram/kg/minute maintenance infusion<br />
If SBP or MAP uncontrolled, Notify Physician<br />
Other:____________<br />
19. For treatment of coagulopathy:<br />
Physician to complete Emergency Management of the Coagulopathic ICH Patient Order<br />
Physician Printed Name / License # / Telephone #:<br />
PATIENT IDENTIFICATION<br />
MEC Approval CSJ – 03/28/13 CSM – 03/28/13 CHC – 5/23/13<br />
<strong>CHN2706</strong> Expires – 03/2016<br />
Page 3 of 5<br />
UNLESS NOTED AS PBO (PRESCRIBED BRAND ONLY), A FORMULARY EQUIVALENT MEDICATION MAY BE DISPENSED
P<br />
H<br />
Y<br />
S<br />
I<br />
C<br />
I<br />
A<br />
N<br />
‘<br />
S<br />
USE BALL POINT PEN – PRESS FIRMLY<br />
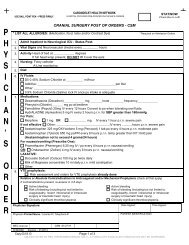
CARONDELET HEALTH NETWORK<br />
HOSPITAL PROVIDED PRE-PRINTED PHYSICIAN’S ORDERS<br />
HEMORRHAGIC STROKE ADMISSION ORDERS<br />
STAT/NOW<br />
(Check Box to Left)<br />
20. Labs:<br />
CBC with diff<br />
Basic Metabolic Panel<br />
UA Urine Culture Urine Pregnancy<br />
Toxicology Screen<br />
PT/INR and PTT<br />
HgbA 1 C<br />
Fasting lipid panel/LDL (Direct)<br />
Other: ___________________<br />
21. Skin Care:<br />
If Braden Scale 18 or less, Consult Skin Care Team and initiate protocol<br />
• Aloe Vesta every 4 hours to coccyx, heels, elbows and any other bony prominences<br />
• Turn patient every 2 hours<br />
• Elevate heels off bed<br />
Lateral rotational therapy mattress replacement or bed<br />
22. Diagnostic tests:<br />
MRI brain CT head in AM __________ 2D Echocardiogram<br />
MRA brain and neck CTA Brain and neck Carotid Doppler<br />
ECG Chest X-Ray PA and lateral Other: _________________________________<br />
23. Evaluate and Treat:<br />
Physical Therapy Occupational Therapy Speech Therapy Social Worker Nutrition/Dietary<br />
Rehab/Psychology Other: __________________________________<br />
24. Physiatry Consultation, Dr. _______________________________________<br />
O<br />
R<br />
D<br />
E<br />
R<br />
Physician Signature: Date Signed: Time Signed:<br />
Physician Printed Name / License # / Telephone #:<br />
PATIENT IDENTIFICATION<br />
MEC Approval CSJ – 03/28/13 CSM – 03/28/13 CHC – 5/23/13<br />
<strong>CHN2706</strong> Expires – 03/2016<br />
Page 4 of 5<br />
UNLESS NOTED AS PBO (PRESCRIBED BRAND ONLY), A FORMULARY EQUIVALENT MEDICATION MAY BE DISPENSED
USE BALL POINT PEN – PRESS FIRMLY<br />
CARONDELET HEALTH NETWORK<br />
HOSPITAL PROVIDED PRE-PRINTED PHYSICIAN’S ORDERS<br />
HEMORRHAGIC STROKE ADMISSION ORDERS<br />
STAT/NOW<br />
(Check Box to Left)<br />
VTE Risk Assessment<br />
Risk Assessment (Use the highest applicable risk category) Risk Level Suggested Prophylaxis Options<br />
By Condition: Very High Enoxaparin 40 mg subq daily OR<br />
• Total hip replacement 10 days of Enoxaparin 30 mg subq twice daily<br />
• Hip fracture<br />
prophylaxis is<br />
suggested Enoxaparin 40 mg subq daily<br />
• Total knee replacement Enoxaparin 30 mg subq twice daily<br />
By High Risk Group:<br />
Very High Enoxaparin 30 mg subq twice daily<br />
• History of VTE<br />
• Thrombophilia<br />
• Immobility, paresis<br />
By Risk Factor Assessment:*<br />
• Surgery – general (high risk)<br />
• Surgery – intracranial<br />
neurosurgery, spinal,<br />
gynecologic, urologic<br />
(moderate risk)<br />
• Age greater than 40 years<br />
• Heart failure<br />
• Inflammatory bowel disease<br />
• Ischemic CVA with<br />
paresis/plegia<br />
• Nephrotic syndrome<br />
• Obesity (BMI of 30 kg/m 2 or<br />
greater)<br />
• Sepsis/pneumonia<br />
• Central line<br />
• Severe respiratory distress<br />
• Spinal cord injury within 1 month<br />
• Trauma (major or lower<br />
extremity)<br />
• Pelvic fracture<br />
• Estrogen/SERM** within 2<br />
weeks<br />
• Malignancy or cancer therapy<br />
• Mechanical ventilation<br />
• Pregnancy or post-partum<br />
period<br />
• Acute MI<br />
• History of spinal cord injury<br />
• Smoking<br />
• Varicose veins<br />
*List of risk factors is not all-inclusive<br />
**SERM= selective estrogen receptor modulator<br />
High<br />
(3 or more risk<br />
factors)<br />
Moderate<br />
(1 or 2 risk<br />
factors)<br />
Low<br />
(0-1 risk factors)<br />
Enoxaparin 40 mg subq daily<br />
± mechanical prophylaxis<br />
OR<br />
Heparin 5000 units subq every 8 hour<br />
± mechanical prophylaxis<br />
Heparin 5000 units subq every 8 hour<br />
OR<br />
Mechanical prophylaxis<br />
Early ambulation<br />
********************************************************THIS PAGE FOR REFERENCE ONLY***********************************************************<br />
Copy 05.17.12 Page 5 of 5<br />
UNLESS NOTED AS PBO (PRESCRIBED BRAND ONLY), A FORMULARY EQUIVALENT MEDICATION MAY BE DISPENSED