Update Myelodysplastic syndrome MDS - å°ä¸æ¦®æ°ç¸½é«é¢
Update Myelodysplastic syndrome MDS - å°ä¸æ¦®æ°ç¸½é«é¢
Update Myelodysplastic syndrome MDS - å°ä¸æ¦®æ°ç¸½é«é¢
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
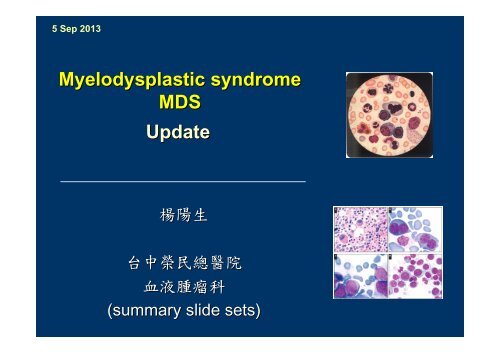
5 Sep 2013<br />
<strong>Myelodysplastic</strong> <strong>syndrome</strong><br />
<strong>MDS</strong><br />
<strong>Update</strong><br />
楊 陽 生<br />
台 中 榮 民 總 醫 院<br />
血 液 腫 瘤 科<br />
(summary slide sets)
<strong>MDS</strong>: a stem cell disorder
What is <strong>MDS</strong><br />
“clonal disorder affecting hematopoietic maturation,<br />
characterized by ineffective hematopoiesis and bone<br />
marrow failure with resultant cytopenias, often<br />
culminating in florid acute leukemia”<br />
Huh
<strong>MDS</strong>: History - long ago<br />
• Reports of cytopenic disorders began appearing in<br />
the early 20th century<br />
• 1942: “odo-leukemia”<br />
odo = threshold<br />
• 1949: “preleukemic anemia”<br />
(Chevalier et al)<br />
(Hamilton-Paterson)<br />
• 1953: expanded definition to include all blood lines<br />
“clonal myeloid hemopathy”<br />
(Block et al)
Variety of Term in history<br />
other terms used over the last 50 years:<br />
•Herald state of leukemia<br />
•Refractory anemia<br />
•Sideroachrestic anemia<br />
•Idiopathic refractory sideroblastic anemia<br />
•Pancytopenia with hyperplastic marrow<br />
•Oligoblastic leukemia
Confusion<br />
• No surprise that there is confusion and ignorance<br />
about this disorder:<br />
Historical coupling of <strong>MDS</strong> to acute myeloid leukemia<br />
• There is a relationship<br />
• Has hindered consideration of <strong>MDS</strong> as a distinct<br />
entity<br />
– biased investigational and therapeutic efforts towards<br />
the leukemia
<strong>MDS</strong>: History - more recent<br />
• Paris,1975: hemopoietic dysplasia<br />
– subsequently shortened to myelodysplasia<br />
• 1982: French-American<br />
American-British classification scheme<br />
(FAB)<br />
• 1999-2002: World Health Organization classification<br />
scheme<br />
• 2000~: Approaching a molecular classification !
What is myelodysplasia<br />
• Disordered production of one or more cell lines<br />
“dysplasia”<br />
• Abnormal growth and differentiation of hematopoietic<br />
precursors<br />
• Abnormal appearance under the microscope
Causes of <strong>MDS</strong><br />
• May follow exposures to bone marrow toxins<br />
– chemotherapy<br />
– radiation<br />
– organic compounds<br />
• Some follow inherited tendencies<br />
– Fanconi anemia, disorders of DNA repair<br />
• > 80% have no identifiable exposure or cause
Cytogenetic abnormalities and epigenetic<br />
changes are key drivers of <strong>MDS</strong><br />
pathogenesis<br />
Stromal/<br />
angiogenic<br />
factors 2<br />
Direct<br />
environmental<br />
toxicity 1<br />
Epigenetic changes<br />
e.g. DNA<br />
hypermethylation 3<br />
Immune<br />
dysfunction 1,2<br />
Stem cell<br />
dysfunction<br />
<strong>MDS</strong><br />
Cytogenetic<br />
abnormalities/<br />
DNA damage 1<br />
Impaired<br />
apoptosis 1<br />
1. List AF, Doll DC. in: Lee RG, et al. eds. Wintrobe’s Clinical Hematology. 10th ed. 1999:2320–41<br />
2. Greenberg PL, et al. Hematology Am Soc Educ Program 2002;136–61<br />
3. Leone G, et al. Haematologica 2002;87:1324–41
• Affect people of any age<br />
– including children<br />
<strong>MDS</strong>: Epidemiology<br />
• Overall incidence: approx. 4/per 100,000 in general<br />
population<br />
• More common in advancing age<br />
– North America: mid-late 60’s<br />
• Peak incidence occurs at 60-90 years of age<br />
> 20 per 100,000 at age of 70-85 years<br />
> 30 per 100,000 at age 85+ years
<strong>MDS</strong>: Epidemiology<br />
• 10000-15000 15000 new diagnosis per year in USA<br />
• About 8200 patients with <strong>MDS</strong> in Germany<br />
• <strong>MDS</strong> Foundation estimates that in people older than<br />
70 there are 15 - 50 new diagnoses/100,000 persons<br />
per year<br />
– extrapolating USA estimates, perhaps 3000-6000<br />
Canadians have an <strong>MDS</strong> diagnosis at any given time
Diagnosis of <strong>MDS</strong>
• Requires suspicion<br />
Diagnosis<br />
• Typically 2 settings where <strong>MDS</strong> should be suspected:<br />
1. Signs or symptoms of a blood disorder<br />
– fatigue, exercise intolerance, pale<br />
– serious or recurrent infections<br />
– inappropriate bleeding and bruising<br />
2. Unexpected finding in blood suggesting <strong>MDS</strong>:<br />
– low blood count of any kind<br />
• > 80% have anemia ± others<br />
• 30 - 45% have low platelets<br />
– macrocytosis (large red cells)<br />
– high monocyte count<br />
– abnormal appearing blood cells
Diagnostic evaluation (required)<br />
• complete history and examination<br />
• complete blood counts and differentials<br />
• iron, B12 and folate levels<br />
• bone marrow aspirate & biopsy<br />
– chromosome analysis: “cytogenetics”<br />
• serum erythropoietin levels<br />
– prior to transfusions
Diagnostic tests as needed<br />
Tests that are useful in some clinical circumstances<br />
•Flow cytometric study<br />
•HLA tissue typing (if stem cell transplant(BMT) a<br />
consideration)<br />
•HIV testing<br />
•Specific disease related gene identification (molecular<br />
diagnosis)<br />
•other specific tests<br />
– PNH<br />
– other HLA determinations
<strong>MDS</strong> diagnosis<br />
• No perfect diagnostic test<br />
• No absolute diagnostic criteria<br />
• Combination of findings:<br />
– Appearance of dysplasia in blood and marrow<br />
– Abnormal cytogenetic testing<br />
– Abnormal flow cytometry findings<br />
– Abnormal molecular study
Classification<br />
and<br />
Risk stratification
IPSS calculation
Molecular Changes in <strong>MDS</strong>
Genetic alterations of epigenetic pathways<br />
in <strong>MDS</strong>
Frequency and clinical consequences of<br />
recurrent gene mutations in patients with<br />
<strong>MDS</strong>
Epigenetic changes<br />
• There are 3 known mechanisms of epigenetic<br />
changes<br />
– DNA methylation<br />
– Histone modification<br />
– RNA-associated silencing<br />
• Changes are potentially reversible<br />
• Changes are a target for therapy<br />
Egger G, et al. Nature. 2004;429:457-463.<br />
Jones PA, et al. Nat Rev Genet. 2002;3:415-428.
Epigenetics<br />
DNA methylation and gene expression<br />
• CpG islands<br />
– Hypermethylation is the most well-recognized<br />
epigenetic change<br />
– Located near the promoter regions<br />
– Most CpG islands are nonmethylated<br />
CpG=cytosine-phosphodiester-guanine.<br />
Jones PA, et al. Nat Rev Genet. 2002;3:415-428.<br />
Esteller M, et al. EMBO Rep. 2006;6:624-628.
DNA methylation<br />
N<br />
NH 2<br />
DNA<br />
methyltransferase<br />
N<br />
NH 2<br />
CH 3<br />
O<br />
N<br />
O<br />
N<br />
Cytosine<br />
Cytosine + methyl group<br />
• DNA methylation maintained by DNA methyltransferases<br />
(DNMTs)<br />
• Methylation occurs at CpG dinucleotides in DNA (CpG rich<br />
islands, located in promoter region)<br />
Esteller M. N Engl J Med 2008;358:1148–59
DNA methylation silences genes in cancer<br />
including tumour-suppressor genes<br />
Normal tissue<br />
Transcription factor<br />
Gene ON (gene transcription → protein expression)<br />
Promoter region<br />
Many hundreds of CpG Islands become<br />
aberrantly methylated in all types of cancer cells<br />
Tumour<br />
Gene OFF<br />
Esteller M. N Engl J Med 2008;358:1148–59
<strong>MDS</strong>: Therapy Overview
Conventional <strong>MDS</strong> treatment<br />
• Many potential therapies available to<br />
and tried in <strong>MDS</strong> patients<br />
• Most show some benefit<br />
• Most benefits are<br />
– small<br />
– only in a minority subset of patients<br />
• Hard to know who should receive<br />
them and what to expect
Therapy Options<br />
• Blood transfusions<br />
• Management of Iron Overload<br />
• Infection control<br />
• Growth factors: EPO, rG-CSF;<br />
Danazol<br />
• Chemotherapy<br />
• Epigenetic Therapy (Vidaza, Dacogen)<br />
• IMiD
The Role of the Specialty Clinic<br />
1. Provide guidance for primary<br />
caregivers<br />
2. Maximize supportive care<br />
3. Optimize individualized management<br />
4. Clinical trials and data collection<br />
5. Dissemination of current state of<br />
knowledge