Obstetrics - SSM Cardinal Glennon Children's Medical Center
Obstetrics - SSM Cardinal Glennon Children's Medical Center
Obstetrics - SSM Cardinal Glennon Children's Medical Center
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>SSM</strong> Maternity Care SUMMER 2012<br />
FOCUS ON<br />
<strong>Obstetrics</strong><br />
<strong>Medical</strong> News from <strong>SSM</strong> Maternity Care, <strong>SSM</strong> St. Mary’s Health <strong>Center</strong><br />
and the physicians of Saint Louis University School of Medicine<br />
SM
ON THE COVER<br />
Perinatal Genetics<br />
Interventional Geneticist and OB/GYN Dr. Kimberly<br />
Martin and Certified Genetic Counselor Darbey Raible,<br />
MS, CGC, are an integral part of the genetics team at <strong>SSM</strong><br />
Maternity Care, evaluating, educating and supporting<br />
patients who have been referred due to an increased risk for<br />
fetal abnormalities from age, exposures or personal/family<br />
histories. They, along with other specialists in maternal-fetal<br />
medicine, offer consultation and a comprehensive array of<br />
prenatal testing options. For these patients, Dr. Martin says<br />
testing is a choice, and the main objective is to help patients<br />
make an informed decision based on their values and goals.<br />
FOCUS ON<br />
obstetrics<br />
SM<br />
Editor In Chief<br />
Sherlyn Hailstone<br />
President<br />
<strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong><br />
Children’s <strong>Medical</strong> <strong>Center</strong><br />
<strong>Medical</strong> Editor<br />
Gilad Gross, MD<br />
Maternal-Fetal Medicine<br />
Division Director<br />
<strong>SSM</strong> St. Mary’s Health <strong>Center</strong><br />
Editor<br />
Andrew Sutton<br />
Physician Services Team Leader<br />
<strong>SSM</strong> Maternity Care<br />
Writer<br />
Jessica Hedges<br />
Physician Services Communications Specialist<br />
<strong>SSM</strong> Maternity Care<br />
For comments and suggestions, please email FocusOn<strong>Obstetrics</strong>@ssmhc.com.
One-Stop-Shopping<br />
for Continuing<br />
Education<br />
Opportunities<br />
Education<br />
2012<br />
Connections -<br />
a new CME/<br />
CEU guide with<br />
<strong>SSM</strong> <strong>Cardinal</strong><br />
<strong>Glennon</strong>, <strong>SSM</strong><br />
Maternity Care<br />
and Saint Louis<br />
University<br />
School of Medicine educational<br />
opportunities - was mailed to physician<br />
offices in February 2012. If you did not<br />
receive your guide or would like extras,<br />
please e-mail<br />
Jessica_Hedges@ssmhc.com.<br />
To view a printable PDF of<br />
Education Connections, go to<br />
www.ssmhealth.com/maternity,<br />
For Physicians, Education,<br />
Education Connections.<br />
First <strong>SSM</strong><br />
Maternity Care<br />
High-Risk<br />
Pregnancy Guide<br />
Due Out This<br />
Summer<br />
Announcements<br />
Expanded MFM Hours at <strong>SSM</strong> St. Clare<br />
Health <strong>Center</strong> Coming in August<br />
The Maternal-Fetal Medicine Specialists of <strong>SSM</strong> Maternity Care and<br />
Saint Louis University School of Medicine: (top row, from left to right)<br />
Gilad Gross, MD; Raul Artal, MD; Erol Amon, MD; Mike Vlastos, MD;<br />
(bottom row, from left to right) William Holcomb, MD;<br />
Thomas Myles, MD; Jaye Shyken, MD; and Dorothea Mostello, MD.<br />
Beginning in August, MFM appointments will be available on Mondays,<br />
Tuesdays, Wednesdays and Fridays from 7:30 a.m.-5 p.m.<br />
Call 1-888-636-7642 to schedule an appointment with a maternal-fetal<br />
medicine specialist at <strong>SSM</strong> St. Clare Health <strong>Center</strong>.<br />
This<br />
summer, two<br />
additional maternal-fetal<br />
medicine specialists joined<br />
the Division of Maternal-Fetal<br />
Medicine at Saint Louis University<br />
School of Medicine and <strong>SSM</strong> Maternity<br />
Care, comprising a team of 10 MFM<br />
specialists. Look for a postcard about<br />
the new physicians in the mail!<br />
!<br />
<strong>SSM</strong> St. Clare Health <strong>Center</strong><br />
St. Francis Building, Ste. G-10, 1011 Bowles Avenue<br />
Fenton, MO 63026<br />
Appointment Scheduling<br />
Made Easy:<br />
Fax Your Referrals<br />
Look for the first issue of the <strong>SSM</strong><br />
Maternity Care Express Guide in your<br />
mailbox this summer. The guide will be<br />
published annually to include service<br />
descriptions, locations, contacts and<br />
physician information provided by<br />
<strong>SSM</strong> Maternity Care, <strong>SSM</strong> St. Mary’s<br />
Health <strong>Center</strong>, <strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong><br />
Children’s <strong>Medical</strong> <strong>Center</strong> and<br />
Saint Louis University School of<br />
Medicine. To ensure your office is on<br />
our mail list, please contact<br />
Jessica_Hedges@ssmhc.com.<br />
The Maternal Access <strong>Center</strong> Team (from left to right): Denise Hunker; Beth Miles;<br />
Retha May, RDMS; Kathy Canchola, RN, BSN; and Jenny Michaelree.<br />
With the <strong>SSM</strong> Maternity Care Access <strong>Center</strong>, we answer your calls quickly, but<br />
you can skip the phone call completely with our secure fax scheduling service.<br />
Just fax your patient order to 314-622-6472.<br />
Our Maternal Access <strong>Center</strong> team will take care of the rest.<br />
Go to www.ssmhealth.com/maternity, For Professionals,<br />
Office Resources to print an MFM Referral Form.<br />
1
It’s difficult to stay abreast of the latest high-risk maternal conditions and management options when complicated cases<br />
only arise here and there. From diabetes in pregnancy to congenital heart defect screenings, take a refresher course online,<br />
on your own time, while earning CME credit. And if it couldn’t get any better, it’s free!<br />
New lectures available:<br />
FREE CME!<br />
“Management of Abnormal Pap Smears in Pregnancy”<br />
– C. William Helm, MD, OB/GYN Oncology Specialist, <strong>SSM</strong> Maternity Care and<br />
Saint Louis University School of Medicine<br />
“Benign Thyroid Disease in Pregnancy”<br />
– William Holcomb, MD, MFM Specialist, <strong>SSM</strong> Maternity Care<br />
To view a presentation:<br />
Log on to www.obstetricsondemand.com<br />
Username: ds\r010-online<br />
Password: webcme<br />
To earn 1 CME Credit from St. Louis University School of Medicine:<br />
Choose the link icon above the presenter’s window. Click TEST LINK.<br />
Register (if you haven’t already), take the quiz and finish the evaluation.<br />
Certificates are sent to your e-mail address within 48 hours.<br />
To view neonatology lectures from <strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong> Children’s <strong>Medical</strong> <strong>Center</strong> and Saint Louis University<br />
School of Medicine neonatologists, log on to www.pediatricsondemand.com and follow the instructions above.<br />
New neonatology lectures are posted monthly.<br />
Sign-Up to Receive <strong>SSM</strong> Maternity Care News<br />
on Demand for Obstetrical Updates<br />
<strong>SSM</strong> Maternity Care News on Demand provides community OB/GYNs, nurses and office<br />
staff with regular obstetrical updates that help you and your patients. The electronic newsletter<br />
is e-mailed monthly. To receive the newsletter, send your e-mail address to Jessica_Hedges@ssmhc.com.<br />
NOTE: We respect your privacy and are sensitive to the amount of electronic communication you receive.<br />
Your e-mail address will not be shared with anyone outside the <strong>SSM</strong> Maternity Care Physician Services Department.<br />
2
<strong>SSM</strong> Maternity Care Access <strong>Center</strong><br />
Proves Helpful to OB/GYNs and Staff<br />
The Southern Illinois Healthcare<br />
Foundation (SIHF) Team<br />
From left to right: Dawn Feazel, Licensed Practical Nurse<br />
Team Lead; Darryl Engeljohn, MD, OB/GYN;<br />
Natalie Spruiel, <strong>Medical</strong> Assistant<br />
"The Maternal<br />
Access <strong>Center</strong><br />
process is quick and<br />
simple. The person on<br />
the other end is always<br />
eager to help when we<br />
call. It's a pleasure to<br />
speak with such<br />
friendly people."<br />
- The SIHF Team<br />
Call our dedicated Maternal Access <strong>Center</strong>:<br />
• Maternal transports to <strong>SSM</strong> St. Mary's - The only<br />
24-hour maternal transport team serving Metro<br />
St. Louis, Metro East and the surrounding area<br />
• MFM Consultations - 24/7 consultations with<br />
maternal-fetal medicine specialists<br />
• Direct Inpatient Admissions - Seamless<br />
admission for high-risk patients to<br />
<strong>SSM</strong> St. Mary's Health <strong>Center</strong><br />
• Outpatient Scheduling - Quick and easy<br />
appointment scheduling at any<br />
<strong>SSM</strong> Maternal & Fetal Care <strong>Center</strong><br />
Maternal & Fetal Care <strong>Center</strong>s:<br />
<strong>SSM</strong> St. Mary’s Health <strong>Center</strong> • <strong>SSM</strong> St. Clare Health <strong>Center</strong> • <strong>SSM</strong> St. Joseph Hospital West<br />
<strong>SSM</strong> DePaul Health <strong>Center</strong> • <strong>SSM</strong> St. Joseph Health <strong>Center</strong> • Anderson Hospital<br />
3
<strong>SSM</strong> Maternity Care Launches<br />
‘Your New Happy Born Here’ Campaign<br />
The next time one of your<br />
patients visits an <strong>SSM</strong> hospital<br />
for maternity care, sees an<br />
<strong>SSM</strong> Maternity Care ad in<br />
her favorite magazine The<br />
Bump or a billboard driving<br />
down the highway, she may<br />
notice a brand new look<br />
and feel and messaging that<br />
resonates with all moms and<br />
moms-to-be.<br />
Share our fun<br />
“Which Mommy Are<br />
You” quiz with your<br />
patients and they’ll<br />
receive a free<br />
“Your New Happy”<br />
tote bag.<br />
Go to<br />
www.whichmommy.com<br />
to take the quiz.<br />
4
Renovated Maternal & Fetal Care<br />
<strong>Center</strong> at <strong>SSM</strong> St. Mary’s Health <strong>Center</strong><br />
Renovated Maternal & Fetal Care <strong>Center</strong> at <strong>SSM</strong> St. Mary’s Health <strong>Center</strong> (Page 5) (photo: St.<br />
Mary’s MFCC, this should take up most of the article … since it’s just one sentence)<br />
To schedule your patient to see a maternal specialist at the new Maternal & Fetal Care <strong>Center</strong><br />
space at <strong>SSM</strong> St. Mary’s Health <strong>Center</strong>, please call the Maternal Access <strong>Center</strong> at 1-888-636-7642.<br />
To schedule your patient to see a maternal specialist at the<br />
new Maternal & Fetal Care <strong>Center</strong> space at <strong>SSM</strong> St. Mary’s Health<br />
<strong>Center</strong>, please call the Maternal Access <strong>Center</strong> at 1-888-636-7642.<br />
Diversions<br />
Andrew Sutton<br />
Physician Services Team Leader<br />
2008 Nalle Winery Reserve Chardonnay<br />
The weather is warming up, and it’s time for long evenings on the patio with a group of good friends. One of the<br />
friends you should bring to the party is the 2008 Nalle Reserve Chardonnay.<br />
Nalle Winery is a tiny, family-owned operation in the Dry Creek Valley in Sonoma’s wine country. So tiny, in fact,<br />
that it’s literally a mother, father and son that run the winery and make the wine. I had a chance to visit them this past<br />
summer and fell in love with their laid-back attitude, and their simply outstanding Burgundy style wines.<br />
The grapes are sourced from the Hopkins Ranch in Russian River Valley, where cool temperatures and fog allow the<br />
grapes to develop slowly with just the right amount of acidity, and elegance. This wine shows fantastic nose of ripe<br />
fruit, with a touch of vanilla, and a little bit of apple. Its mouth feel sways a little toward medium than light, showing<br />
the kiss of oak from a short barrel fermentation, balanced by a touch of crispness and acidity. This is a very wellbalanced<br />
wine that is an absolute joy to consume. Available through the Nalle website for $42, I would put this wine<br />
up against a Premier Cru Burgundy any day of the week. YUM! www.nallewinery.com<br />
5
Perinatal Genetics<br />
Expert, Comprehensive Support through<br />
Education, Diagnosis and Treatment<br />
Pregnancy is a wonderfully exciting time for most<br />
women, but the question “What if there’s something<br />
wrong with my baby” crosses every mother’s mind,<br />
even just once. At <strong>SSM</strong> Maternity Care, our team<br />
of geneticists is available to you and your patients<br />
for guidance, counseling, education, diagnosis and<br />
treatment.<br />
“We recognize that genetic testing is a choice,” says<br />
Kimberly Martin, MD, SLUCare/<strong>SSM</strong> Maternity Care<br />
Interventional Geneticist and OB/GYN. “We don’t<br />
usually recommend specific testing. Instead, we help<br />
each family understand their options and encourage<br />
them to choose testing that’s right for them. Sometimes,<br />
that’s no test at all.”<br />
Dr. Martin and her team see up to 40 patients a day.<br />
Some of these patients have been referred by their OB/<br />
GYN because they are considered at increased risk for<br />
a birth defect, while others may not be considered “at<br />
risk,” but are interested in learning more about available<br />
testing to determine whether their baby is healthy.<br />
According to Dr. Martin, at least 3 percent of babies are<br />
born with some type of birth defect or handicapping<br />
condition. No matter the situation, the referring<br />
obstetrician and patient can be assured that the utmost<br />
importance is placed on communication and personal<br />
coordination between the health care team.<br />
“Because we offer such a wide variety of services, and<br />
we see patients for a wide variety of indications, our<br />
Looking up at the flat screen monitor of her baby boy in utero, Heather Hipkins can’t believe how much her son has grown since<br />
her last ultrasound just a few weeks before.<br />
SLUCare/<strong>SSM</strong> Maternity Care Maternal-Fetal Medicine Specialist Gilad Gross, MD, was happy to report that Heather’s little<br />
guy is progressing well and at 16 weeks, anatomically, everything looks great.<br />
6<br />
Because of Heather and her baby’s hereditary bone condition, Trichorhinophalangeal Syndrome (TRPS), both mom and baby<br />
will be monitored closely and co-managed by a multidisciplinary team that includes her primary obstetrician, an MFM, maternal<br />
geneticist and certified genetic counselor. She sees Dr. Gross at the Maternal & Fetal Care <strong>Center</strong> at <strong>SSM</strong> St. Joseph Hospital<br />
West (one of six locations) every few weeks, which is conveniently located near her home and office.
approach is absolutely tailored to each patient’s specific<br />
needs. Obstetricians referring to our team can be sure<br />
that we will work closely with them to provide the<br />
appropriate, high quality and comprehensive care their<br />
patients deserve,” says SLUCare/<strong>SSM</strong> Maternity Care<br />
Certified Genetic Counselor Darbey Raible, MS, CGC.<br />
Dr. Martin supports this notion. “Open communication<br />
and a partnership with the primary health care provider<br />
is critical,” she says. “Our goal is to keep the patient’s<br />
care with the primary provider unless the condition<br />
requires complete or specialized care.”<br />
At 41 years of age, patient Heather Hipkins is at<br />
increased risk to have a baby with a chromosome<br />
abnormality, such as Down syndrome. But<br />
Trichorhinophalangeal Syndrome (TRPS), the rare,<br />
inherited bone disease she was born with, is the<br />
main reason Heather was referred to <strong>SSM</strong> Maternity<br />
Care. The disease does not allow Heather to properly<br />
absorb calcium, which is cause for her numerous<br />
hospitalizations, multiple surgeries and concern for<br />
her developing baby. It is inherited in an autosomal<br />
dominant fashion, meaning there is a 50/50 chance that<br />
Heather’s baby will inherit the changed gene causing<br />
TRPS. Heather first met with SLUCare/<strong>SSM</strong> Maternity<br />
Care Maternal-Fetal Medicine Specialist Gilad Gross,<br />
MD, to address her calcium intake while pregnant and<br />
physical ability to carry and deliver her child. Her next<br />
appointment was with the genetics team.<br />
“I saw Darbey first,” Heather says. “We discussed<br />
my family history and she explained what they try to<br />
accomplish and broke down the details of my genetic<br />
disorder. It was phenomenal, so detailed and interesting.”<br />
Because most of the<br />
information presented<br />
to patients during the<br />
genetics counseling session<br />
is new and sometimes<br />
overwhelming, Darbey<br />
sets a conversational<br />
tone and only discusses<br />
information applicable<br />
to the patient. “Assessing<br />
what information is going<br />
to be most important to<br />
the patient I am working<br />
with allows me to tailor<br />
the discussion so that it is<br />
personal and relevant to<br />
them,” she says. “We often<br />
use pictures and diagrams<br />
to help make the concepts less abstract and make the<br />
counseling session a conversation, where I’m not the<br />
only one talking but the patient is explaining to me their<br />
A chorionic villus sampling (CVS) taken by Dr. Martin in<br />
Heather’s first trimester confirmed that her baby is affected<br />
with the same rare bone disease she lives with.<br />
Dr. Gross reviews Heather’s lab work that shows her<br />
increased calcium supplements are working. Because of the<br />
TRPS, she has difficulty retaining calcium.<br />
Heather was relieved to know that Dr. Gross discussed her<br />
prenatal care plan with her endocrinologist of nearly 30<br />
years. “It’s important to me that he stays in the loop. He<br />
knows a lot about my history and may be able to give Dr.<br />
Gross some helpful information,” she says.<br />
understanding of what has been discussed.” In addition,<br />
take-away materials are provided so that the patient has<br />
more time to digest the information after the meeting<br />
and share with their partner, family, and other health<br />
care providers if desired.<br />
Based upon the information Darbey provided and after<br />
meeting with Dr. Martin, Heather opted to go forward<br />
with a test called chorionic villus sampling (CVS).<br />
Performed as early as 10 weeks of pregnancy, the test<br />
would determine whether the baby has the correct<br />
number of chromosomes, and the sample could be tested<br />
to determine if the baby<br />
had inherited the TRPS<br />
gene.<br />
Dr. Martin explained<br />
to Heather that it is not<br />
unusual to have some<br />
spotting after the CVS,<br />
and that she could call<br />
the <strong>SSM</strong> Maternity<br />
Care team if she had<br />
any worries. Heather<br />
did have spotting and<br />
naturally, was worried.<br />
The Maternal & Fetal<br />
Care <strong>Center</strong> (MFCC) at<br />
<strong>SSM</strong> St. Joseph Hospital<br />
West got Heather in to<br />
see an MFM immediately. “I love Becky the ultrasound<br />
technician,” Heather says. “She knew I was scared, so<br />
she showed me right away that everything looked okay<br />
7
on the ultrasound.” Heather also saw Dr. Gross who<br />
reassured her that the light bleeding was normal and not<br />
causing any trouble for the baby.<br />
A few days later when Heather was still spotting, she<br />
called the after hours physician exchange. Heather<br />
continues, “Within minutes, Dr. Nguyen called me<br />
back. He explained that since the blood was dark in<br />
color, it was just my body recovering from the test.”<br />
[Dr. Thinh Nguyen joined the SLUCare/<strong>SSM</strong> Maternity<br />
Care MFM team this summer.] This team approach<br />
to the care of one patient is everyday practice at <strong>SSM</strong><br />
Maternity Care.<br />
“The team of SLUCare/<strong>SSM</strong> Maternity Care providers<br />
are a compassionate, collegial group,” Dr. Martin says.<br />
“With no exception, we all agree that the patient comes<br />
first.”<br />
Daily communication and monthly case conferences<br />
are just a couple ways the team keeps the patient at the<br />
forefront. “Our provision of patient care is very much<br />
a collaborative effort,” Darbey says. “We frequently<br />
consult one another on cases, which I believe raises the<br />
expertise of everyone’s practice. In addition, our monthly<br />
conferences allow us to review and critically assess recent<br />
cases to identify ways to improve patient care.” Like the<br />
old saying goes, “It takes a village to raise a child” – the<br />
same could be said for a pregnancy.<br />
“It takes a village to care for a pregnant woman,” Dr.<br />
Martin says to Jarita Sanders during her latest visit to the<br />
MFCC at <strong>SSM</strong> St. Mary’s Health <strong>Center</strong>.<br />
Jarita is pregnant with her third child, and for the third<br />
time was diagnosed with gestational diabetes early in her<br />
pregnancy. She is being treated by the diabetes team of<br />
SLUCare/<strong>SSM</strong> Maternity Care specialists that include a<br />
maternal-fetal medicine specialist, diabetes educator and<br />
dietician. Dr. Martin and Darbey met Jarita after one<br />
of her first trimester ultrasounds showed a large nuchal<br />
translucency measurement.<br />
“Our team has had extra training and certification in<br />
ultrasound evaluation for babies with birth defects,”<br />
Dr. Martin says. “All babies have some fluid under the<br />
skin at the back of the neck in the first trimester; but<br />
“Congratulations! We were so worried about this little one, and now we are just checking things off the list,”<br />
SLUCare/<strong>SSM</strong> Maternity Care Interventional Geneticist Kimberly Martin, MD, tells Jarita during an appointment.<br />
Jarita’s baby girl had an abnormally large nuchal translucency measurement taken during a first trimester ultrasound<br />
examination, but a CVS and later ultrasound revealed a structurally normal baby. Dr. Martin referred Jarita<br />
to Fetal Cardiologist Renuka Peterson, MD, at <strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong> Children’s <strong>Medical</strong> <strong>Center</strong> for a fetal<br />
echocardiogram, which also proved normal.<br />
“Dr. Peterson was wonderful,” Jarita says. “She explained everything she was looking for during the echo and said<br />
everything looked fine.”<br />
8
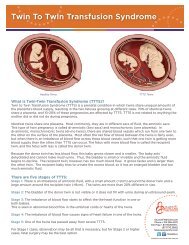
most babies have a small amount, the average being less<br />
than 2 mm. Babies with chromosome abnormalities and<br />
some other birth defects tend to have more fluid. To use<br />
this measurement to determine individual risks for fetal<br />
abnormalities, the nuchal translucency measurement has<br />
to be very precise, and the <strong>SSM</strong> Maternity Care team has<br />
extensive experience with this evaluation.” The nuchal<br />
translucency measurement for Jarita’s baby was 4.6 mm.<br />
“I was in utter shock when I learned this measurement<br />
could mean my baby has Down syndrome,” Jarita says.<br />
“Darbey and Dr. Martin were very kind and explained<br />
the causes, risks and options for testing. Darbey said it<br />
was completely up to me if I wanted to do the CVS and<br />
that I should think about it.” Jarita did decide to have<br />
the CVS performed by Dr. Martin and within a week,<br />
she received good news. The CVS was normal and an<br />
ultrasound 6 weeks later showed a nuchal measurement<br />
of 5 mm, normal for the baby’s size.<br />
“Families who are referred to me due to known or<br />
suspected abnormalities are often very anxious. The<br />
ultrasound test is not definitive, and that’s why some<br />
families choose to go the extra step with CVS or<br />
amniocentesis,” Dr. Martin says. “Most of the time I’m<br />
able to give families a lot of reassurance, and then call<br />
them with the normal results of diagnostic testing. If I<br />
didn’t have the opportunity to call families with good<br />
news, I couldn’t have stayed in this field of medicine for<br />
20 years!”<br />
Dr. Martin discusses how results will be communicated<br />
with the family before the testing takes place. How and<br />
when they want to receive the information is completely<br />
up to them. “When there is a significant chance that<br />
the results will be abnormal, I know it is often best that<br />
the call come at a time when the couple is together, and<br />
we are all at a time and place in our day when we can<br />
talk openly,” she says, adding, “I notify their primary<br />
OB/GYN provider first and then contact the family. If<br />
the patient’s primary provider would like to deliver the<br />
news, I make sure they know I’m available for questions.<br />
The most important thing is that the family does not<br />
feel alone. It’s not unusual for me to give the family and<br />
Ultrasound photo of Jarita’s baby’s nuchal translucency<br />
measurement in the first trimester. Since Jarita has early onset<br />
gestational diabetes, and the measurement is large compared<br />
to the baby’s size, Dr. Martin says the baby is at an increased<br />
risk for birth defects.<br />
An ultrasound six weeks later shows Jarita’s baby to have a<br />
normal nuchal skin thickness in comparison to the baby’s<br />
increased size.<br />
SLUCare/<strong>SSM</strong> Maternity Care Certified Genetic<br />
Counselor Darbey Raible, MS, CGC, uses a photo<br />
to show Jarita what an enlarged nuchal translucency<br />
measurement looks like and discusses the possible<br />
chromosome abnormalities that might be present.<br />
As a genetic counselor, Darbey collects and interprets patient histories and assists them in understanding the risks<br />
for their babies and options available for prenatal screening or testing. “Throughout the entire process, we remain<br />
available to patients as a source of information and support to make their situation a bit easier to navigate,”<br />
Darbey says.<br />
9
Molecular Cytogenetics Lab<br />
at <strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong><br />
Children’s <strong>Medical</strong> <strong>Center</strong><br />
State-of-the-art technology,<br />
thorough testing, reliable results<br />
The goal of the Molecular Cytogenetics Lab at <strong>SSM</strong><br />
<strong>Cardinal</strong> <strong>Glennon</strong> Children’s <strong>Medical</strong> <strong>Center</strong> is to<br />
provide patients with the best diagnostic testing<br />
in the shortest time possible. “We are fortunate to<br />
have a molecular cytogenetics lab,” Dr. Martin says,<br />
adding, “We work well together to determine the best<br />
diagnostic testing for each family and provide reliable<br />
and timely results.”<br />
provider my cell phone number or to spend an hour on<br />
the phone in the evening with a family.”<br />
Whether the baby requires surgery or will need to see<br />
a pediatric geneticist after birth, <strong>SSM</strong> Maternity Care<br />
supports patients during and after pregnancy with<br />
a multidisciplinary team of obstetric and pediatric<br />
geneticists, maternal-fetal medicine specialists, fetal<br />
surgeons, counselors and other pediatric sub-specialists.<br />
The initial results of Heather’s CVS showed that her<br />
baby did not have any chromosome abnormalities such<br />
as Down syndrome, and that she was having a baby boy.<br />
A few weeks later, the test for TRPS showed that the<br />
baby had inherited Heather’s changed gene. Like most<br />
genetic disorders, it is not possible to determine the exact<br />
difficulties he will face until after he is born and begins<br />
to grow. “We pass 75,000 genes to our kids and have<br />
no control over which ones they get,” Dr. Martin says.<br />
“Heather’s little boy is lucky to have such a remarkable<br />
mother, and we will follow her baby closely to try to<br />
avoid some of the difficulties Heather has conquered<br />
with such courage and grace.”<br />
Heather was disappointed to learn that her little boy will<br />
face many of the same challenges she has throughout her<br />
life, but her outlook remains positive. “This news won’t<br />
change my pregnancy,” Heather says. “I will continue<br />
to work out, eat healthy, get plenty of sleep and stay as<br />
positive as possible.”<br />
For someone who spent her childhood in a hospital and<br />
has had seven surgeries in the last seven years, Heather<br />
knows a thing or two about quality care. “I absolutely<br />
love Dr. Martin and Darbey. Both my husband and I<br />
have learned so much from them,” she says. “They are<br />
very professional, extremely intelligent and helpful with<br />
any questions that we have. I would recommend them to<br />
anyone who may need their assistance.”<br />
Genetic<br />
Services Available<br />
at <strong>SSM</strong> Maternity Care<br />
High-resolution ultrasound<br />
Diagnostic testing in pregnancy – chorionic<br />
villus sampling, amniocentesis<br />
First and second trimester screening for Aneuploidy<br />
Fetal blood sampling and transfusion<br />
10<br />
Prenatal fetal surgery and therapy
The St. Louis Fetal Care Institute<br />
at <strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong><br />
Children’s <strong>Medical</strong> <strong>Center</strong><br />
Dr. Martin sees patients for genetic disorders at the<br />
Maternal & Fetal Care <strong>Center</strong> at <strong>SSM</strong> St. Mary’s Health<br />
<strong>Center</strong> as well as the St. Louis Fetal Care Institute (FCI)<br />
at <strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong> Children’s <strong>Medical</strong> <strong>Center</strong>.<br />
“Patients I see at the Fetal Care Institute have often<br />
received information that their baby has a birth defect or<br />
other condition. They are referred to the FCI so they can<br />
meet with the variety of specialists who may be involved<br />
in the care of their baby,” Dr. Martin says. Typically,<br />
the multidisciplinary team includes a fetal surgeon,<br />
maternal-fetal medicine specialist, geneticist, patient-care<br />
coordinator and in most cases a neonatologist and other<br />
sub-specialized pediatric providers. Dr. Martin adds, “At<br />
(From left to right) Pediatric and Fetal Surgeon Ed<br />
Yang, MD, and Maternal-Fetal Medicine Specialist<br />
Mike Vlastos, MD, co-direct the St. Louis Fetal<br />
Care Institute, providing state-of-the-art diagnostic<br />
services, evidence-based prognostic information and<br />
appropriate fetal interventions. In this photo, Drs.<br />
Yang and Vlastos perform a tracheal occlusion for a<br />
fetus with Congenital Diaphragmatic Hernia (CDH).<br />
They are the first in the world to successfully inject a<br />
dissolvable hydrogel in the fetus’ trachea instead of a<br />
detachable balloon.<br />
<strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong> we offer fetal MRI, which is often helpful in evaluating specific types of birth defects such<br />
as those involving the Central Nervous System. We also have the expertise of two gifted pediatric cardiologists, Dr.<br />
Renuka Peterson and Dr. Angela Sharkey, who provide detailed assessments of baby’s hearts before birth, and can<br />
help families understand any abnormalities that are found and what is expected for their child after delivery.”<br />
As the most comprehensive fetal care center in middle-America, the St. Louis Fetal Care Institute has provided<br />
innovative, compassionate care to mothers whose babies have congenital, structural and genetic anomalies since<br />
2009. The FCI is led by a nationally recognized, expert team of physicians who are experienced in leading-edge<br />
treatments and technologies, ensuring the best possible results for patients. The new clinical suite at <strong>SSM</strong> <strong>Cardinal</strong><br />
<strong>Glennon</strong> offers patient-centered care with two nesting rooms, an ultrasound examination and treatment room, and a<br />
large conference/consultation room to allow the family to meet with a larger care team.<br />
Available Fetal Interventions<br />
for appropriate fetal diagnoses<br />
Fetoscopic procedures:<br />
• Laser photocoagulation for Twin-Twin Transfusion<br />
Syndrome<br />
• Fetal cystoscopy and posterior urethral valve<br />
ablation for bladder outlet obstruction<br />
• Resection of constricting Amniotic bands<br />
Open fetal procedures:<br />
• Open repair of open neural tube defects<br />
• Resection of sacrococcygeal teratomas<br />
• Resection of giant lung lesions<br />
• EXIT procedure – Ex utero intrapartum treatment<br />
for airway obstruction and unstable congenital<br />
heart defects<br />
Other therapeutic fetal procedures:<br />
• Fetal transfusions<br />
• Thoracic or vesicoamniotic shunt placement<br />
To contact the St. Louis Fetal Care Institute at <strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong> Children’s <strong>Medical</strong> <strong>Center</strong>,<br />
please call 314-268-4037 or 877-776-3385 or e-mail fetalcare@ssmhc.com. To learn more about<br />
the St. Louis Fetal Care Institute, go to www.stlouisfetalcare.com.<br />
11
Q&A<br />
Kim Martin, MD<br />
Interventional Geneticist and OB/GYN, <strong>SSM</strong> Maternity Care<br />
Adjunct Associate Professor of <strong>Obstetrics</strong> and<br />
Gynecology, Saint Louis University School of Medicine<br />
Q: Why did you choose to specialize in genetics What is it about<br />
Saint Louis University and <strong>SSM</strong> Maternity Care that made you want to practice here<br />
A: When I was a resident, ultrasound was becoming a much more important tool in obstetrics and gynecology, and<br />
I really enjoyed doing it. I realized that the ability to identify healthy babies and babies with birth defects/genetic<br />
disorders was going to increase, and I wanted to be a part of this emerging technology. Similarly, an explosion in genetic<br />
information was taking place at that time. I decided to specialize in genetics because this knowledge seemed to blend<br />
perfectly with ultrasound. Saint Louis University and <strong>SSM</strong> Maternity Care is a natural fit for me because there is a<br />
large ultrasound practice. The Division of Maternal-Fetal Medicine is very strong, but it did not have a board-certified<br />
medical geneticist. My skill set complements the other members of my division well. I truly love my job here.<br />
Q: What do you like best about your job<br />
A: Like most doctors, my job is different every day. I never know what we will find with our ultrasound machine, and<br />
every family I meet is unique. This daily variety keeps me interested and enthusiastic. I am happy to get up and go to<br />
work every day, and this is good for me and my patients. Despite almost 20 years in practice, I am still amazed by how<br />
much there is to learn. Saint Louis University and <strong>SSM</strong> provides a very stimulating atmosphere.<br />
Q: How does the genetics team stay up-to-date on the latest research, diagnostic testing and technology available<br />
A: Like all areas in medicine, knowledge continues to increase exponentially. Genetics is no different, and with<br />
completion of the Human Genome Project, the number of genetic disorders for which specific testing is available,<br />
is rapidly growing. Just last week we sent blood from a couple which will be used to sequence all known functional<br />
regions of their genomes! We attend national conferences and routinely read publications, but we also work closely with<br />
other geneticists here at SLU and <strong>SSM</strong>, and around the world. Laboratories often specialize in one or two disorders,<br />
so almost every week we interact with other institutions. Right now we are corresponding with a lab in Taiwan and<br />
may be shipping some samples there. Fortunately, there are several online databases that we can utilize to research the<br />
particular disorder and find the best laboratory to do the testing. We often consult with several labs before making a<br />
decision about where a particular test will be performed.<br />
Q: Do you have a particular patient care philosophy that has guided you throughout your career<br />
12<br />
A: There are two basic principles that I think exemplify what I strive to achieve in my practice. The first is that the right<br />
thing to do in any situation is what is best for the patient; and that takes precedence over my schedule, and usually<br />
my private life. When I enter a patient’s room, I am 100 percent in the room, and do my very best to meet whatever<br />
needs they have and ensure that their questions are answered, even if the answer is “I don’t know, but I will try to find<br />
the answer for you.” The second principle is that it is essential that families understand their genetic and obstetrical<br />
risk factors so that they can make informed choices about the options that are available to diagnose and/or treat them.<br />
Something that distinguishes a geneticist from other medical specialists is that our counseling of patients is, above<br />
all, non-directive. Our responsibility is to educate families so that they are empowered to make choices that are best<br />
for themselves within the context of their personal, professional, moral, and religious community and to support and<br />
affirm those choices.<br />
To reach Dr. Martin or to make an appointment at an<br />
<strong>SSM</strong> Maternal & Fetal Care <strong>Center</strong>, please call 1-888-636-7642.
FOCUS ON<br />
FACULTY<br />
Genetic Specialists<br />
Kimberly Martin, MD<br />
Adjunct Associate Professor of <strong>Obstetrics</strong> and Gynecology,<br />
Saint Louis University School of Medicine<br />
MD: McGill University, Montreal, Quebec<br />
Internship: University of Western Ontario<br />
Residency in <strong>Obstetrics</strong> and Gynecology:<br />
University of Western Ontario<br />
Fellowship in <strong>Medical</strong> Genetics: University of British Columbia<br />
Rachael Bradshaw, MS, CGC<br />
BA, Biology: Earlham College<br />
MS, <strong>Medical</strong> Genetics: University of Cincinnati<br />
Meg Hefner, MS, CGC<br />
BS, Zoology and Psychology: University of Toronto<br />
MS, Human Genetics: University of Michigan<br />
Darbey Raible, MS, CGC<br />
BS, Biological Sciences: University of Notre Dame<br />
MS, <strong>Medical</strong> Genetics: University of Cincinnati<br />
Maternal-Fetal<br />
Medicine Specialists<br />
Raul Artal, MD<br />
Chairman, Department of <strong>Obstetrics</strong>, Gynecology and Women’s<br />
Health at Saint Louis University School of Medicine<br />
Professor of <strong>Obstetrics</strong> and Gynecology,<br />
Saint Louis University School of Medicine<br />
MD: Sackler School of Medicine, University of Tel-Aviv, Israel<br />
Rotating Internship: Beilinson Hospital, Israel<br />
Residency in <strong>Obstetrics</strong> and Gynecology: Beilinson Hospital,<br />
Israel; Case Western Reserve University/Metro General Hospital<br />
Fellowship in Maternal-Fetal Medicine:<br />
Harbor-UCLA <strong>Medical</strong> <strong>Center</strong><br />
Gilad Gross, MD<br />
Division Director, Maternal-Fetal Medicine at<br />
<strong>SSM</strong> St. Mary’s Health <strong>Center</strong><br />
<strong>Medical</strong> Director, Labor and Delivery, Antepartum and<br />
Postpartum at <strong>SSM</strong> St. Mary’s Health <strong>Center</strong><br />
Professor of <strong>Obstetrics</strong> and Gynecology,<br />
Saint Louis University School of Medicine<br />
MD: Saint Louis University School of Medicine<br />
Residency in <strong>Obstetrics</strong> and Gynecology:<br />
University of Missouri-Kansas City<br />
Fellowship in Maternal-Fetal Medicine, OB/GYN:<br />
Washington University School of Medicine<br />
Erol Amon, MD<br />
Director, Maternal-Fetal Medicine Fellowship at<br />
Saint Louis University School of Medicine<br />
Professor of <strong>Obstetrics</strong> and Gynecology,<br />
Saint Louis University School of Medicine<br />
MD: Northwestern University <strong>Medical</strong> School<br />
Internship and Residency in <strong>Obstetrics</strong> and Gynecology:<br />
Saint Joseph Hospital, Northwestern University <strong>Medical</strong> School<br />
Fellowship in Maternal-Fetal Medicine:<br />
University of Tennessee <strong>Center</strong> for Health Sciences<br />
William Holcomb, MD<br />
Maternal-Fetal Medicine Specialist, <strong>SSM</strong> Maternity Care<br />
MD: Indiana University<br />
Residency in <strong>Obstetrics</strong> and Gynecology:<br />
Washington University School of Medicine<br />
Fellowship in Maternal-Fetal Medicine:<br />
Washington University School of Medicine<br />
Dorothea Mostello, MD<br />
Director, Diabetes in Pregnancy Program at<br />
Saint Louis University School of Medicine<br />
Associate Professor of <strong>Obstetrics</strong> and Gynecology,<br />
Saint Louis University School of Medicine<br />
MD: The Johns Hopkins School of Medicine<br />
Residency in <strong>Obstetrics</strong> and Gynecology:<br />
University of Colorado Health Sciences <strong>Center</strong> and<br />
Affiliated Hospitals<br />
Fellowship in Maternal-Fetal Medicine:<br />
University of Cincinnati<br />
Thomas Myles, MD<br />
Director, Maternal-Fetal Medicine Outreach Program at<br />
<strong>SSM</strong> St. Mary’s Health <strong>Center</strong><br />
Professor of <strong>Obstetrics</strong> and Gynecology,<br />
Saint Louis University School of Medicine<br />
MD: Saint Louis University School of Medicine<br />
Residency in <strong>Obstetrics</strong> and Gynecology:<br />
Illinois Masonic <strong>Medical</strong> <strong>Center</strong><br />
Fellowship in Maternal-Fetal Medicine: Rush-Presbyterian,<br />
St. Luke’s <strong>Medical</strong> <strong>Center</strong><br />
Jaye Shyken, MD<br />
Associate Professor of <strong>Obstetrics</strong> and Gynecology,<br />
Saint Louis University School of Medicine<br />
MD: University of Missouri School of Medicine<br />
Residency in <strong>Obstetrics</strong> and Gynecology:<br />
University of Missouri and Clinics<br />
Fellowship in Maternal-Fetal Medicine:<br />
Washington University School of Medicine<br />
Mike Vlastos, MD<br />
Co-Director, St. Louis Fetal Care Institute<br />
Assistant Professor of <strong>Obstetrics</strong> and Gynecology,<br />
Saint Louis University School of Medicine<br />
MD: Creighton University<br />
Residency in Family Practice: University of Wyoming<br />
Residency in <strong>Obstetrics</strong> and Gynecology: Regions Hospital<br />
Fellowship in Maternal-Fetal Medicine:<br />
Washington University School of Medicine<br />
13
Physician Services Department<br />
1465 South Grand Blvd.<br />
Saint Louis, Missouri 63104-1095<br />
Non Profit Org<br />
U.S. Postage<br />
PAID<br />
St. Louis, MO<br />
Permit No. 2412