INNOVATIONS - National Rural Health Mission
INNOVATIONS - National Rural Health Mission
INNOVATIONS - National Rural Health Mission
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>INNOVATIONS</strong><br />
October 2008<br />
1<br />
Arogyakeralam
2<br />
NRHM Directorate<br />
DHS Compound<br />
Thiruvananthapuram
P.K.SREEMATHI TEACHER<br />
MESSAGE<br />
Arogyakeralam has started making its impact on the heath sector. The visible<br />
changes and trends stand testimony to this. In a state like Kerala where the<br />
health seeking behavior is very high, improving the quality of health care is of<br />
utmost importance. The resource of NRHM came in an opportune time when<br />
the state was finding it difficult to find resources matching the demand.<br />
Though there were many challenges initially in rolling out the activities under<br />
NRHM in the State, these challenges were later on converted to<br />
opportunities through conscious efforts, dedication and commitment. The<br />
initiatives under NRHM are pioneering as well as result oriented.<br />
Arogyakeralam has been successful in adding innovativeness suiting the local<br />
situation that made these initiatives all the more fruitful. The reports<br />
enclosed in this document are examples to this. I congratulate the team led<br />
by Dr. Dinesh Arora I.A.S, who made this happen and I am confident that we<br />
will be able to make lasting impact in the lives of rural poor through more<br />
such initiatives in the future.<br />
Smt. P.K Sreemathy Teacher<br />
Minister for <strong>Health</strong> and Social Welfare<br />
3
Dr. VISHWAS MEHTA IAS<br />
MESSAGE<br />
The success of any programme depends on its flexibility to innovate and<br />
contextualize. NRHM, in this context, is a paragon to other programmes<br />
giving room to innovate and improve. Though a bit late to start off, through<br />
our dedicated efforts we have progressed significantly. Many of the initiatives<br />
mentioned in this document bears testimony to this. I am confident that the<br />
State will become a model to others in implementing NRHM just like in many<br />
other fronts where the state has been a torchbearer. It is heartening to see,<br />
that we were able to do things galore in a short span of time. However, this<br />
never makes us complacent but given us motivation and energy to excel and<br />
improve. Further, I appreciate the hard work and sincerity of all those who<br />
contributed towards making these innovations conceptualize and implement.<br />
4<br />
Dr. Vishwas Mehta I.A.S<br />
Secretary (<strong>Health</strong>)<br />
Govt. Of Kerala
PREFACE<br />
It has been a Challenging and at the same time wonderful experience<br />
implementing NRHM in a state having its own oddities. Though a bit slow at<br />
the beginning, NRHM implementation in the state of Kerala has gained<br />
significant momentum during the last couple of years and we are now in a<br />
position to show case many of the visible changes in the field owing to<br />
earnest efforts made in implementing innovative schemes and activities<br />
which NRHM envisages.<br />
Though Kerala has been in the forefront vis a vis health sector achievements,<br />
a plethora of challenges too engulf us along with our hard‐earned<br />
achievements. For example the burden of communicable and Noncommunicable<br />
diseases is on the rise; the load of cancer patients and ageing<br />
population remains a challenge. However we are now confident of dealing<br />
with all the challenges with the advent of the revolutionary <strong>Rural</strong> <strong>Health</strong><br />
<strong>Mission</strong> initiative.<br />
Like many other states, we too are forging ahead in many fronts. The<br />
innovations enclosed here bears testimony to that and we are quite<br />
confident that we would be able to come up with many other innovative<br />
interventions that could make a lasting impact on the health of millions of<br />
poor in our state. It is a proud moment to present this report which talks<br />
about innovations under the following heads:<br />
Human Resources Management under NRHM<br />
Innovation By Engineering<br />
Accreditation of Hospitals in Kerala<br />
E‐banking practice under NRHM in Kerala<br />
Accreditation of Government Medical Laboratories in Kerala<br />
Telemedicine<br />
ASHA workers ‐ Owning more responsibilities<br />
Debit card scheme for ASHA Volunteers<br />
Immunization Drive – October 2008<br />
Behavioral Change Communication ‐ Innovations<br />
Pain and Palliative Care under NRHM<br />
Radio <strong>Health</strong><br />
Standardizing <strong>Health</strong> Institutions: Ensuring quality services<br />
Effective utilization of untied funds and Annual Maintenance Grants<br />
<strong>Health</strong> Management Information System for Kerala State<br />
School <strong>Health</strong> Programme<br />
Geospatial <strong>Rural</strong> <strong>Health</strong> Information System for Kerala State (G‐RHIS)<br />
5
Information Technology<br />
Three Dimensional Interactive Digital Anotomy: 3D Indiana<br />
Compulsory <strong>Rural</strong> Service: Bridging Critical gap in Manpower<br />
Initiatives on Infection control at Medical College Hospital,<br />
Trivandrum<br />
Ensuring Quality Supply of Medicines in a Transparent and Efficient<br />
way‐ The KMSCL initiative<br />
Improving Efficiency of hospitals‐ the decentralized way<br />
State Disease Control and Monitoring Cell: an innovative initiative<br />
towards the control of Communicable diseases<br />
Comprehensive <strong>Health</strong> Insurance Scheme<br />
We acknowledge the support and guidance of all senior level officials of the<br />
Ministry of <strong>Health</strong> and Family Welfare, without which we would not have<br />
been able to produce results in a way it is envisaged. This unstinted support<br />
from the Ministry will always remain an encouragement for us to innovate<br />
and produce better results.<br />
Dr. Dinesh Arora<br />
State <strong>Mission</strong> Director<br />
NRHM, Kerala<br />
6
Contents<br />
Page<br />
1. HR Management under NRHM<br />
2. HR Management in Nutshell<br />
3. Engineering under NRHM<br />
4. Accreditation of Hospitals in Kerala<br />
5. E‐banking practice under NRHM<br />
6. Accreditation of Government Medical Laboratories<br />
7. Telemedicine<br />
8. ASHA Workers owning more responsibilities<br />
9. Debit Card Scheme for ASHA Volunteers<br />
10. Immunization Drive ‐ October 2008<br />
11. Behavior Change Communication<br />
12. Pain and Palliative Care<br />
13. Radio <strong>Health</strong><br />
14. Standardizing <strong>Health</strong> Institutions<br />
15 Effective Utilisation of untied funds and Annual<br />
Maintenance Grants: with special focus on Malappuram<br />
16 <strong>Health</strong> Management Information System for Kerala State<br />
17 School <strong>Health</strong> Programme<br />
16. Geospatial <strong>Rural</strong> <strong>Health</strong> Information System<br />
17 Information Technology<br />
8<br />
40<br />
44<br />
50<br />
54<br />
62<br />
65<br />
70<br />
75<br />
77<br />
81<br />
85<br />
93<br />
96<br />
104<br />
108<br />
113<br />
124<br />
127<br />
7
18 Three Dimensional Interactive Digital Anotomy: 3D<br />
Indiana<br />
19 Compulsory <strong>Rural</strong> Service: Bridging Critical gap in<br />
Manpower<br />
20 Initiatives on Infection control at Medical College Hospital,<br />
Trivandrum<br />
21 Ensuring Quality Supply of Medicines in a Transparent and<br />
Efficient way‐ The KMSCL initiative<br />
22 Improving Efficiency of hospitals‐ the decentralized way<br />
23 State Disease Control and Monitoring Cell: an innovative<br />
initiative towards the control of Communicable diseases<br />
24 Comprehensive <strong>Health</strong> Insurance Scheme<br />
133<br />
139<br />
144<br />
148<br />
156<br />
161<br />
173<br />
8
Human Resources Management under<br />
NRHM<br />
Human resources pertaining to <strong>Health</strong> Care<br />
Our Mother Land is heading past to occupy number one position in<br />
Population. Certainly it is not an achievement but probably a handicap for<br />
our entire growth and relative development. This ignominious victory on<br />
population growth in fact made so many inconveniences in our development.<br />
But we also must recollect that India is the First country in the Universe in<br />
passing a bill in Parliament on Population control. But, it is an irony that we<br />
still take no strict remedial measures to curb this undesirable growth.<br />
But, when we see the utilization of Human population, Western countries are<br />
standing as specimen for Asian countries. With their minimum population<br />
they create wonders and encourage growth in population. We are still<br />
struggling hard to find out that population is really an asset. In fact it is high<br />
time now to accept; Human Resources are an asset.<br />
As far as <strong>Health</strong> Care is concerned, without the help of trained and able<br />
Human resource, it is impossible to run a <strong>Health</strong> care system. So, broadly we<br />
can classify these groups of <strong>Health</strong> care into two. They are: (1) Clinical and<br />
Non Clinical, who are either directly or indirectly responsible for public health<br />
and Individual <strong>Health</strong>. The maximum benefits on health system is depending<br />
on the performance and the benefits, the system can deliver depend largely<br />
upon the knowledge, skills and motivation of those individuals responsible<br />
for delivering health services.<br />
It is also essential to maintain an appropriate mix between the<br />
different types of health promoters and caregivers to ensure the system's<br />
success. Due to their obvious and important differences, it is imperative that<br />
9
human capital is handled and managed very differently from physical capital.<br />
The relationship between human resources and health care is very complex.<br />
Both the number and cost of health care consumables (drugs, surgical<br />
and equipment) are rising astronomically, which in turn can drastically<br />
increase the costs of health care. In publicly‐funded systems, expenditures in<br />
this area can affect the ability to hire and sustain effective practitioners. In<br />
both government‐funded and employer‐paid systems, HRM practices must<br />
be developed in order to find the appropriate balance of workforce supply<br />
and the ability of those practitioners to practice effectively and efficiently. A<br />
practitioner without adequate tools is as inefficient as having the tools<br />
without the practitioner.<br />
Key questions and issues pertaining to human resources in<br />
health care<br />
When examining health care systems in a global context, many<br />
general human resources issues and questions arise. Some of these issues are<br />
the size, composition and distribution of the health care workforce,<br />
workforce training issues, the attrition rate of health workers, and the level<br />
of economic development and socio demographic, geographical and cultural<br />
factors.<br />
The variation of size, distribution and composition in our county's<br />
health care workforce is of great concern. For example, the number of health<br />
workers available in our country is a key indicator of that country's capacity<br />
to provide delivery and interventions. Factors to consider when determining<br />
the demand for health services include cultural characteristics, socio<br />
demographic characteristics, economic factors and health seeking behaviour.<br />
The factor of health seeking behaviour is especially important in the Kerala<br />
context. The general public tends to approach specialists for all ailments<br />
including minor ailments. The fact that deliveries never take place in sub<br />
10
centres and very rarely takes places in PHC indicates that public prefers<br />
specialists.<br />
Workforce training is another important issue. It is essential that<br />
human resources personnel consider the composition of the health<br />
workforce in terms of both skill categories and training levels. New options<br />
for the education and in‐service training of health care workers are required<br />
to ensure that the workforce is aware of and prepared to meet a particular<br />
country's present and future needs. A properly trained and competent<br />
workforce is essential to any successful health care system.<br />
The migration of health care workers is an issue that arises when<br />
examining global health care systems. Research suggests that the movement<br />
of health care professionals closely follows the migration pattern of all<br />
professionals in that the internal movement of the workforce to urban areas<br />
is common to all countries. Professionals tend to migrate to areas where they<br />
believe their work will be more thoroughly rewarded. <strong>Health</strong> care<br />
professionals look to areas that will provide their families with an abundance<br />
of amenities, including schools for their children, safe neighborhoods and<br />
relatives in close proximity. This has caused a surplus in some areas and a<br />
huge deficit in others. This is more relevant in the Kerala context. In the tribal<br />
district of Wayanad, while only four specialist doctors are working on<br />
contract basis, in the district of Trivandrum, there are 149 specialists working<br />
on contract basis under NRHM. Workforce mobility can create additional<br />
imbalances that require better workforce planning, attention to issues of pay<br />
and other rewards and improved overall management of the workforce. In<br />
these circumstances, it has been decided to give salary incentives, post<br />
graduate quota, difficult and most difficult rural area allowances etc so that<br />
the professionals don’t feel underpaid and dissatisfied.<br />
Another issue that arises when examining health care systems is the<br />
level of economic development. There is evidence of a significant positive<br />
11
correlation between the level of economic development in a country and its<br />
number of human resources for health. States with higher gross domestic<br />
product (GDP) per capita spend more on health care than states with lower<br />
GDP. This is an important factor to consider when examining and attempting<br />
for implementing solutions to problems in health care systems in our country.<br />
Socio‐demographic elements such as age distribution of the<br />
population also play a key role in a country's health care system. An ageing<br />
population leads to an increase in demand for health services and health<br />
personnel. This has specific relevance to the Kerala scenario where it is<br />
expected that the age pyramid in the State will get reversed by the year 2061.<br />
At present, productive age group is highest in Kerala. In the year 2061,<br />
female preponderance will be high and those with age higher than 80 will be<br />
maximum and the productive age group will be lower. The important<br />
implication in this aspect is that additional training of younger workers will be<br />
required to fill the positions of the large number of health care workers that<br />
will be retiring.<br />
It is also essential that cultural and geographical factors be considered<br />
when examining the health care system. Geographical factors such as climate<br />
or topography influence the ability to deliver health services.<br />
The above are just some of the many issues that must be addressed<br />
when examining global health care and human resources that merit further<br />
consideration and study.<br />
12
The impact of human resources on health sector reform<br />
When examining the health care system, it is both useful and<br />
important to explore the impact of human resources on health sector reform.<br />
While the specific health care reform process varies, some trends can be<br />
identified. When NRHM began, Government of India had identified human<br />
resources for health as its key challenge. The performance of the health<br />
system rested upon equitable access, efficiency and quality services in the<br />
rural poor.<br />
One of the main human resources initiative employed in an attempt<br />
to increase efficiency was to get the services of medical and Para medical<br />
personnel on contract basis. While internal contracting was also resorted to<br />
for medical professionals initially during the implementation of the program,<br />
the process has been discontinued consequent on availability of these<br />
professionals in the health institutions.<br />
Some of the human resources initiatives for health sector reform<br />
followed in the State include strategy of attempts to increase equity or<br />
fairness. Some of these strategies include the strategy of payment<br />
commensurate with experience, payment of additional allowances for<br />
specific areas, re‐deployment services etc.<br />
Human resources in health sector reform also seek to improve the<br />
quality of services and patients' satisfaction. <strong>Health</strong> care quality is generally<br />
defined in two ways: technical quality and socio‐cultural quality. Technical<br />
quality refers to the impact that the health services available can have on the<br />
health conditions of a population. Socio‐cultural quality measures the degree<br />
of acceptability of services and the ability to satisfy patients' expectations.<br />
One of the most important obstacle Human resource professionals<br />
face is constraints in budgets, lack of congruence between different<br />
13
stakeholders' values, high rates of turnover, lack of timely capacity building<br />
and low morale of health personnel.<br />
Better use of the spectrum of health care providers and better coordination<br />
of patient services through interdisciplinary teamwork have been<br />
recommended as part of health sector reform. Since all health care is<br />
ultimately delivered by people, effective human resources management will<br />
play a vital role in the success of health sector reform.<br />
Policy approaches in a global approach to health care<br />
delivery<br />
As mentioned earlier, there are three main health system inputs:<br />
human resources, physical capital and consumables. Given that with<br />
sufficient resources any country can obtain the same physical capital and<br />
consumables, it is clear that the main differentiating input is the human<br />
resources. This is the input that is the most difficult to develop, manage,<br />
motivate, maintain and retain, and this is why the role of the human<br />
resources professional is so critical. All health care is delivered by people, so<br />
health care management can really be considered people management; this<br />
is where human resources professionals must make a positive contribution.<br />
Given the significant changes that globalization of health care can<br />
introduce, it is important that human resources professionals be involved at<br />
the highest level of strategic planning, and not merely be positioned at the<br />
more functional, managerial levels. By being actively involved at the strategic<br />
levels, they can ensure that the HR issues are raised, considered and properly<br />
addressed. Therefore, human resources professionals will also need to have<br />
an understanding not only of the HR area, but of all areas of an organization,<br />
including strategy, finance, operations, etc. This need will have an impact on<br />
the educational preparation as well as the possible need to have work<br />
experience in these other functional areas.<br />
14
Human resources initiatives under NRHM in Kerala<br />
Under NRHM, the policy of equitable accessible effective and quality<br />
services has been the base principle for a proper human resource<br />
management in the State. The need for skilled and trained professionals was<br />
utmost felt in the State during the beginning of implementation of the<br />
program in 2005. The main aim of the Government before embarking into a<br />
process of effective human resource management under NRHM was to<br />
ensure that all the sanctioned posts under various health institutions were<br />
filled.<br />
Need Assessment Study<br />
The prime consideration of the department was effective utilization of<br />
the existing work force. However, several shortfalls were felt in the service<br />
delivery model. Consequently, the need of the hour was to have more<br />
qualified and skilled personnel complimenting the existing work force. Before<br />
embarking into a process of recruitment of medical and para medical<br />
personnel in the State through NRHM, the need of the hour was a need<br />
assessment survey in the State through which the critical gaps in Human<br />
Resources could be identified. At the same time, upgradation of the CHCs to<br />
IPHS was essential since facilities available in these institutions hardly<br />
satisfied the norms for the same. The process of upgrading selected CHCs<br />
were initiated in 2006 itself and the same was extended to all CHCs in 2007.<br />
At the same time, based on the need assessment survey, providing quality<br />
maternal health care was proposed and consequently, the contractual<br />
recruitment of medical and para medical personnel was resorted to.<br />
15
Contractual appointment of Doctors & Specialists<br />
Based on the need assessment, it was seen that there is a huge gap<br />
between availability of doctors in the department and the requirement in the<br />
field. Government took a conscious decision of appointing doctors and<br />
specialists in selected health institutions in the State. Doctors were appointed<br />
on contract basis in the State with honorarium commensurate with<br />
experience. On assessment of availability of specialists in the State, it was<br />
noted that specialists, especially Anesthetists, Gynecologists, Physician, and<br />
Pediatrician etc were on shortage in the department. Consequently, it was<br />
decided to appoint these specialists on a contract basis with payment<br />
commensurate with experience.<br />
Sl.<br />
MBBS Doctors Specialty Doctors<br />
District<br />
No<br />
(Contract)<br />
(Contract)<br />
1 Trivandrum 65 30<br />
2 Kollam 28 6<br />
3 Pathanamthitta 24 8<br />
4 Alappuzha 29 6<br />
5 Kottayam 21 8<br />
6 Idukki 33 7<br />
7 Ernakulam 43 25<br />
8 Thrissur 40 27<br />
9 Palakkad 26 7<br />
10 Malappuram 39 11<br />
11 Kozhikode 9 6<br />
12 Wayanad 30 4<br />
13 Kannur 38 2<br />
14 Kasaragod 21 2<br />
Total 446 149<br />
16
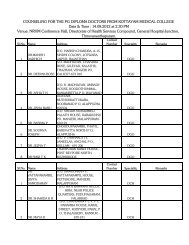
Compulsory <strong>Rural</strong> Service<br />
While the availability of medical personnel was an easy process in<br />
some districts, the same was a laborious one in some backward districts.<br />
Consequently, the Government decided to invoke the clause of compulsory<br />
rural services for doctors studying the various government Medical Colleges<br />
in the State. They were appointed in various health care institutions in the<br />
state with priority to backward districts. MBBS doctors were to serve in<br />
health care institutions for a period of 1 year, PG diploma doctors to serve for<br />
6 months and PG Degree doctors for two years. Even though objections were<br />
raised from several quarters on the compulsory rural service, the government<br />
was bent upon providing medical care to the rural poor especially backward<br />
districts. Government ensured that all the doctors worked in the health<br />
institutions for the prescribed period.<br />
Later, government based on various orders decided to extend the<br />
conditions of compulsory rural services to doctors who passed out from self<br />
financing colleges and cooperative medical colleges in government seats, All<br />
India Quota candidates etc.<br />
The details of doctors now working in health institutions are as follows.<br />
Sl.<br />
Compulsory rural service‐<br />
District<br />
No<br />
MBBS<br />
Bonded PG Diploma / Degree<br />
1 Trivandrum 27 4<br />
2 Kollam 27 5<br />
3 Pathanamthitta 13 1<br />
4 Alappuzha 42 0<br />
5 Kottayam 17 1<br />
6 Idukki 17 0<br />
7 Ernakulam 49 2<br />
8 Thrissur 40 4<br />
9 Palakkad 28 6<br />
10 Malappuram 27 2<br />
17
Sl.<br />
Compulsory rural service‐<br />
District<br />
No<br />
MBBS<br />
Bonded PG Diploma / Degree<br />
11 Kozhikode 13 6<br />
12 Wayanad 22 0<br />
13 Kannur 43 3<br />
14 Kasaragod 27 0<br />
Total 392 34<br />
The best possible outcomes as a result of appointment of doctors are<br />
summarized as follows.<br />
i. More institutions provided with 24 X 7 services<br />
ii. OP increased<br />
iii. OP time in selected institutions extended from 8 AM to 8 PM.<br />
iv. Increase of deliveries as a result of increase of patients from<br />
private to Government health care institutions<br />
In addition, very few specialists are working in Medical Colleges on<br />
bonded obligation under NRHM.<br />
Financing qualified human resources<br />
It was felt at the beginning itself that there should be a good package<br />
on compensation for the Medical & para medical personnel in the State to<br />
ensure that the persons posted in the institutions continue to serve the<br />
Government on a continuous basis. A differential package was evolved for<br />
doctors working in different areas. Even though many of the places in the<br />
State can be classified as semi‐urban or semi‐rural, there are few areas which<br />
have the problem of proper access. These areas have, therefore been,<br />
classified as difficult and most difficult rural areas and doctors posted in these<br />
areas are eligible to get additional honorariums which vary upon the<br />
classification. Also, as mentioned earlier, honorarium was given<br />
commensurate with experience. While doctors who work in health sector are<br />
18
financed by NRHM, those who work in the Medical Colleges (PG Degree<br />
doctors) are paid from State Government budget.<br />
Strengthening Of AYUSH<br />
For Ayurveda, NRHM has taken the initiatives and selected 74<br />
Ayurveda doctors and posted to various institutions by Ayurveda Directorate.<br />
As far as Homoeo is concerned, NRHM has conducted the interview<br />
and forwarded a list of 59 selected candidates to Homoeo Directorate and<br />
they will be placed very soon, Government Order awaited.<br />
Necessity for skilled manpower<br />
While the appointment of qualified professionals in the health<br />
institution was made, the simultaneous need of skilled manpower was felt in<br />
the state. Even though Government had filled up all the vacancies of Staff<br />
Nurses, Lab Technicians, Pharmacists etc., the gaps felt in the health<br />
institutions consequent on patient influx was huge.<br />
Internship of Nurses<br />
Student of BSc Nursing undergoing their course in the Nursing<br />
Colleges under Directorate of Medical Education have to undergo the training<br />
for 4 years and the remaining 1 year as internship. During the internship the<br />
student is paid Rs. 4500/‐ as stipend from NRHM. As of now, NRHM is giving<br />
internship stipend to all the students studying in Nursing Colleges of<br />
Thiruvananthapuram, Kottayam & Kozhikode.<br />
As far as Diploma in General Nursing and Midwifery is concerned,<br />
internship is not part of their curriculum. Instead, after the completion of 3<br />
years training, every student of Government Nursing Schools in Kerala is<br />
given a chance to work in any of the Government Hospitals for the duration<br />
of 2 years and a remuneration of Rs. 7,480/‐.<br />
19
Providing Staff Nurse<br />
Hospitals were crowded and the average OP in the recent times had<br />
increased manifold. The ratio for Bed: Staff nurses which 1: 6 was<br />
overstretched to 1 : 12. NRHM advocates on equitable accessible effective<br />
and quality services. The quality aspect for providing by the skill manpower<br />
was lacking due to the stretch.<br />
Staff nurses who study in Government nursing colleges have to get<br />
into an agreement with government for doing compulsory service for two<br />
years when government calls for the same. This clause has been invoked and<br />
all the bonded nurses are appointed for a period of two years on contract<br />
basis. At present, 1395 Staff Nurses have been appointed in the State on<br />
contract basis. Consequently, the strain in giving quality services has been<br />
reduced to a great extent. Services of Staff Nurses have been ensured to get<br />
24X7 basis and extended OP (upto 8 pm) in selected health institutions in the<br />
State.<br />
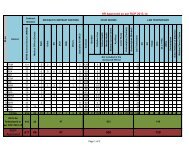
Sl.<br />
No<br />
District<br />
Staff Nurse<br />
1 Trivandrum 264<br />
2 Kollam 94<br />
3 Pathanamthitta 53<br />
4 Alappuzha 138<br />
5 Kottayam 115<br />
6 Idukki 60<br />
7 Ernakulam 155<br />
8 Thrissur 96<br />
9 Palakkad 24<br />
10 Malappuram 84<br />
11 Kozhikode 105<br />
12 Wayanad 109<br />
13 Kannur 45<br />
20
14 Kasaragod 53<br />
Total 1395<br />
Other Para-medical personnel<br />
Consequent on extended OP (upto 8 pm), there were small shortages<br />
of other manpower like Lab Technicians, Pharmacists etc. These staff also has<br />
been appointed on contract basis on a need‐basis.<br />
The para medical personnel taken on contract have been funded from<br />
NRHM.<br />
Sl.<br />
No<br />
District Lab Tech Pharmacist<br />
1 Trivandrum 8 1<br />
2 Kollam 0 0<br />
3 Pathanamthitta 6 0<br />
4 Alappuzha 1 7<br />
5 Kottayam 4 0<br />
6 Idukki 0 0<br />
7 Ernakulam 2 10<br />
8 Thrissur 0 0<br />
9 Palakkad 5 0<br />
10 Malappuram 3 9<br />
11 Kozhikode 0 0<br />
12 Wayanad 18 16<br />
13 Kannur 0 0<br />
14 Kasaragod 7<br />
Total 47 50<br />
21
Program Management Professionals – State Level<br />
While the process of appointment of medical and para medical<br />
personnel were carried out in the district, it was imperative that the<br />
management of the program was to be carried in a proper way such that<br />
there occurred no deficiencies in the system. Experts in different fields were<br />
handpicked and appointed in key posts in the State Program Monitoring &<br />
Support Unit. The process of selection was based on criteria of knowledge,<br />
commitment and enthusiasm to work in a <strong>Mission</strong> mode. The staff so<br />
recruited has been used to their best potential, which has delivered desired<br />
results. At present, a well planned mechanism is in place with which the<br />
program is being run in a mission mode.<br />
Program Management Professionals – District Level<br />
Government of India had advised on taking MBA graduates as District<br />
Program Manager (NRHM) in the State. The matter was discussed threadbare<br />
in various forums in the State. While there was a very strong opposition on<br />
appointing an MBA graduate, it was decided to appoint a doctor working in<br />
the health department as the District Program Manager (NRHM). This has<br />
resulted in deriving lots of results since initially many of the department<br />
officials were very skeptical about NRHM. The District Program Manager<br />
(NRHM) were able to integrate the department with program and<br />
consequently, the activities are planned by NRHM and are now being carried<br />
out in a time bound manner jointly by NRHM and Kerala <strong>Health</strong> Services.<br />
Also, accounting personnel with requisite qualification was selected and<br />
appointed in each district to ensure smooth flow of funds as well as proper<br />
monitoring of funds to health as well as Panchayati Raj institutions.<br />
22
Program Management Professionals – Block Level<br />
The need for a person to coordinate all the activities at the block was<br />
felt and hence Block Coordinators for all 234 health blocks were selected in<br />
the State. They are professionals mainly in Social Work or with Master degree<br />
in Business administration.. They coordinate the activities in block level as<br />
well as act as counselors for the general public at large at specific times. The<br />
experience of appointment of block coordinators has derived wonderful<br />
results.<br />
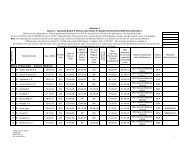
DETAILS OF BLOCK AROGYAKERALAM COORDINATORS AS ON<br />
30‐09‐2008<br />
Sl.no District<br />
Total On On Vacant<br />
Post Contract Deputation<br />
1 Thiruvananthapuram 25 20 03 02<br />
2 Kollam 19 12 04 03<br />
3 Pathanamthitta 13 12 0 01<br />
4 Alappuzha 17 14 02 01<br />
5 Kottayam 19 07 09 03<br />
6 Idukki 08 01 07 0<br />
7 Ernakulam 20 10 10 0<br />
8 Thrissur 28 25 02 01<br />
9 Palakkad 17 10 01 06<br />
10 Malappuram 21 15 02 04<br />
11 Kozhikode 16 14 01 01<br />
12 Wayanad 06 02 04 0<br />
13 Kannur 15 11 02 02<br />
14 Kasargode 10 0 08 02<br />
Total 234 153 55 26<br />
23
Personnel not appointed<br />
As per several guidelines of NRHM, some posts were to be hired and<br />
appointed at State / District / Block / <strong>Health</strong> Institution / Community level.<br />
The broad reasons for not appointing such personnel can be summarized as<br />
follows.<br />
District Data Officers: There is sufficient and perfect coordination between<br />
NRHM officials and Statisticians in the <strong>Health</strong> Services Department who<br />
compliments the activities in the district collecting necessary data from<br />
districts.<br />
Block Program Managers: The Block level Medical Officers with the help of<br />
Block Coordinators ensure that the activities in each block are carried out in a<br />
time bound manner.<br />
Registered Medical Practitioners: The health seeking behaviour of the<br />
community led to the decision of non‐appointment of Registered Medical<br />
Practitioners in the State. The Community opts to see a specialist for even<br />
minor ailments due to which the necessity of RMP was not there.<br />
Trained Birth Attendants: When the State has an Institutional delivery<br />
percentage of more than 99% every year, the need for TBAs does not rise at<br />
all. These were the broad reasons for non‐appointment of some staff under<br />
NRHM.<br />
PRO Cum Liaison Officer<br />
<strong>National</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Mission</strong> is constantly engaged in supporting all the<br />
health care systems of the hospitals. At times it is felt that, many hospitals<br />
do not have adequate staff to work with liaison activities between NRHM &<br />
Hospital and also with various other agencies associated with hospitals. In<br />
this circumstances, NRHM, has appointed 39 MBA/MHA degree holders with<br />
2 years experienced as PRO cum Liaison Officer to work in all major<br />
24
MCH/District and General Hospital across Kerala on an honorarium of Rs.<br />
10000/‐ per month. They are expected to work along with Superintendent<br />
Office and act as per his instruction. He will have a word in implementing<br />
various NRHM activities in the Hospital and also suggest the measures<br />
involved in implementing such schemes.<br />
Bio Medical Engineering<br />
It is felt that on the part of the up gradation of Hospitals and accreditation,<br />
NRHM, needs to have trained manpower on Bio medical field. It is technical<br />
in nature and they can very effectively have a thorough check in Hospital<br />
Equipments and its functioning. People with such quality has been selected,<br />
initially, three in number with Rs.20000/‐ for Bio Medical Officer and<br />
Rs.25000/‐ for Bio Medical Officer one) as monthly payment. Now they are<br />
under training and will be trained further in such activities.<br />
Quality Control Officers<br />
Selection process is over and they will act as one Regional Quality control<br />
Officer and four candidates as Asst. Quality Control Officers. They are yet to<br />
be inducted in NRHM and final selection is just completed on a monthly<br />
payment of Rs. 16000/‐ and Rs.12000/‐ respectively.<br />
Capacity Building under NRHM<br />
Capacity building involves a variety of activities. It includes the<br />
building of skills in the work force to cope with change and adding to the<br />
capacity of officials to build up health institutions. When implementing an<br />
integrated health promotion program, it is important to create optimal<br />
conditions for success. Capacity building involves the development of<br />
sustainable skills, organizational structures, resources and commitment to<br />
health improvement in health and other sectors, to prolong and multiply<br />
25
health gains many times over. It can occur both within a specific program<br />
and as part of broad agency and system development.<br />
In the Kerala context, the capacity building exercise faced a general<br />
slackness during the years 2005‐06 and 2006‐07. However, the importance<br />
of training health staff was realized and during the year 2007‐08, several<br />
training programs were conducted. Further, during the present year, all<br />
categories of staff in districts are being imparted training. Further,<br />
underlining the importance of training program management staff, induction,<br />
financial as well as detailed activity‐wise training was given to program<br />
management staff at various levels.<br />
Admin Training to Superintendent of CHC & all other<br />
Government Hospitals<br />
An initiative has been taken to offer training on various aspects of<br />
health, which is not otherwise part of medical curriculam of Superintendents<br />
of hospitals. As we all are aware, Superintendents of hospitals play a pivotal<br />
role in the day to day functioning of hospitals pertaining to General<br />
Administration, Medical, Laboratory Facilities, Human Resourse Management<br />
and its deployment in addition to all other daily function whether it is clinical<br />
or non clinical. Often it is found that as a single individual who himself is<br />
specially devoted / trained to Medical field, face difficulties in dealing all<br />
these routine functions within the timeframe. This is the general background<br />
on which NRHM thought to provide a very useful and comprehensive training<br />
which provide a deep insight into these aspects and this knowledge is<br />
expected to use to tackle any situation which arises in the normal course of<br />
any hospital, will be master tool to tackle such situation.<br />
26
ACR Lab in Major Hospitals on 24 X 7 basis<br />
Many of the hospitals are now equipped with basic laboratory<br />
facilities which includes men and material. This is very essential for finding<br />
out the proper diagnosis. As the time changes, it is seen that many of the<br />
new diseases are cropping up and often it is becoming an epidemic, which<br />
creates a lot of hue and cry. Recently it is experienced that the diseases<br />
which was either eradicated or vanished have re‐emerged in various part of<br />
our country, which challenges the efficiency of our capacities and claims.<br />
This alarming situation reminds us to have a more advanced version of<br />
laboratory facilities with properly trained technicians and pathologists to find<br />
out the cause behind such kind of disease. Presently ACR Labs are<br />
established only in very few centres mainly Medical Colleges and Regional PH<br />
Labs etc.<br />
The proposal is for the establishment of ACR Labs on 24 hours basis in<br />
Major hospitals of every districts. This will change the total scenario, and the<br />
patients can directly rush up to these labs instead of standing behind the<br />
serpentine queue in the existing ACR Labs. In addition, during the epidemic<br />
situation, re‐appearance of any major disease, the health department<br />
officials can combat and bring out the best results with minimum possible<br />
delay.<br />
Paramedical Education<br />
1. Paramedical Education in Government Sector<br />
Director of Medical Education was conducting about 5 Paramedical courses in<br />
Government Medical/ Dental Colleges from 1985 onwards with about 400<br />
admission/ year. After 2000 many new courses were introduced and<br />
permission was given to self financing colleges for starting paramedical<br />
course. Now there are about 12 paramedical courses which are being<br />
27
conducted in about 20 self financing institutions also. All diploma courses are<br />
conducted by Director of Medical Education and Degree courses like BPT, BSc<br />
MLT etc are conducted by universities. Director of Medical Education is<br />
admitting about 1600 students/ year. Director of Medical Education is<br />
conducting periodical camps to asses the quality of education<br />
2. New courses and institutions.<br />
Numerous request to start new courses and existing courses in new<br />
institutions are pending with Government for sanction of LOI/ NOC and LOP.<br />
3. Paramedical staff in Government hospitals.<br />
Many paramedical post of Government hospitals are having recognized<br />
paramedical courses as basic qualification.<br />
Eg: DMLT for Lab Technicians<br />
DOA for Ophthalmic Assistant<br />
DRT for Radiographers etc.<br />
But to many posts due to lack of specific courses, persons from service<br />
are given in‐service training.<br />
Eg: EEG training<br />
ECG training<br />
MRL training<br />
JLA training etc.<br />
These training are not being done in a scientific way. So steps are being<br />
taken to form in‐service training module for all these posts. One such ie.<br />
Nursing Assistant Training Module is approved by Government.<br />
4. Fixing of qualification of Paramedical posts<br />
Many paramedical posts are remaining unfilled due to lack of fixing of<br />
minimum qualification.<br />
Eg. Theatre Technician<br />
28
Mortuary Technician<br />
Blood Bank Technician<br />
Research Assistant/ Officer<br />
Perfusionist etc.<br />
Now steps are being taken to include new paramedical courses as<br />
minimum qualification for existing paramedical posts.<br />
5. Paramedical Council/ Bill and Registration<br />
Till now there is no system of Registration for Paramedical personnel.<br />
There is no Central Paramedical Council.<br />
State Paramedical Bill was<br />
approved by cabinet in 2007 and waiting for submission to assembly and<br />
approved. State Paramedical Council was formed under Chairmanship of<br />
<strong>Health</strong> Secretary and it is now functioning. Registration of Paramedical<br />
certificate holders of courses conducted by DME, DHS and Universities<br />
approved by Paramedical council were just started.<br />
About 50 lakhs is being sanctioned in this year’s budget for formation of<br />
Paramedical Council. Steps are being taken up to utilize the amount for<br />
renovation of an existing building, post creation and for improvement of<br />
infrastructure facilities<br />
6. Regional Institute of Paramedical Sciences at Medical College,<br />
Calicut<br />
A proposal was given to Central Ministry and a Regional Institute of<br />
Paramedical Sciences was sanctioned attached to Medical College, Calicut<br />
with central funding under this about 54 paramedical courses (Diploma,<br />
PG Diploma, Degree and PG Degree) was proposed. The academic work<br />
like formulation of syllabus, curriculam etc are under progress.<br />
29
7. Paramedical Institutes under SI‐MET<br />
Two institutes are sanctioned under SI‐MET. One at Payyannur and one<br />
at Kuzhalmannam.<br />
8. Priyadarshini Institute of Paramedical Science (PIPMS)<br />
A Paramedical Institute attached to Medical College,<br />
Thiruvananthapuram conducting paramedical courses exclusively for<br />
SC/ST student.<br />
9. One such institute is proposed and under progression at Medical<br />
College, Alappuzha<br />
DRAW BACKS<br />
1. Lack of Central Paramedical Council<br />
2. Lack of State Paramedical Council<br />
3. There is no uniformity in<br />
Nomenclature<br />
Minimum standards<br />
Syllabus<br />
Course donation, curriculum<br />
Exam pattern etc.<br />
of various courses conducted inside and outside the State.<br />
4. Non – recognized institution<br />
<br />
<br />
Various Universities are permitting paramedical courses in May<br />
private institution, which do not have attached hospital or clinical<br />
facilities.<br />
Many private agencies are conducting numerous diploma and<br />
certificate courses with affiliation to any Universities or<br />
Government.<br />
30
In the absence of a Central/ State law legal action against this institution<br />
cannot be initiated.<br />
5. Lack of assessment of need of the State<br />
Requirement of the state with respect to Paramedical personnel for<br />
conduct of Government/ private hospitals and Labs are not yet<br />
assessed.<br />
6. There is no law governing the private hospitals and labs.<br />
Lack of creation of entry cadre post in the Government sector for existing<br />
paramedical courses.<br />
7. Lack of Carrier advancement and training programmes for<br />
Paramedical Technicians who are already there in the service.<br />
Conclusion<br />
It is seen that the relationship between human resources<br />
management and health care is extremely complex. Several research and<br />
analysis have indicated that several key questions must be addressed and<br />
that human resources management can and must play an essential role in<br />
health care sector reform.<br />
The migration of health workers to more affluent regions and/or<br />
countries is a major problem, resulting in citizens in rural areas of developing<br />
countries experiencing difficulties receiving adequate medical care. Since all<br />
health care is ultimately delivered by and to people, a strong understanding<br />
of the human resources management issues is required to ensure the success<br />
of any health care program. Further human resources initiatives are required<br />
in many health care systems, and more extensive research must be<br />
conducted to bring about new human resources policies and practices that<br />
will benefit individuals in the country.<br />
31
HUMAN RESOURCES MANAGEMENT<br />
IN NUTSHELL<br />
Every innovation need a proper planning based upon conditions available in<br />
the location. As far as Kerala is concerned, is a fully literate and highest<br />
achievement holder in <strong>Health</strong> Sector in our country. It is very proud to say<br />
that Kerala has achieved several feats in health, which is on par with World<br />
<strong>Health</strong> Standards. So it became very essential and careful, while selecting<br />
and implementing new methods and innovations of HR in Kerala. NRHM<br />
Kerala put an extra consciousness since the population of Kerala is highly<br />
educated and very spontaneous in actions and re‐actions. So the activities<br />
expected to project as new should have a real and result oriented otherwise<br />
it may boomerang on us, which may tarnished the image of NRHM activities.<br />
Yet the following introductions were either implemented or planned to<br />
implement in near future.<br />
Internship of BSc Nursing Students<br />
It was the introduction of <strong>National</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Mission</strong>. Through this<br />
every student get an opportunity to work in hospitals and can have a hands<br />
on experience from the real life situation in the hospitals. Their course will<br />
be completed only after the fulfillment of this internship programme. The<br />
NRHM is also offering an honorarium of Rs. 4500/‐ per month to these<br />
internees.<br />
32
Introduction of Bonded obligation to General Nursing<br />
Students<br />
<strong>National</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Mission</strong> took a very firm step in implementing<br />
bonded obligation to all students of Government Nursing Schools who are<br />
undergoing Diploma in General Nursing. Their bonded obligation is for two<br />
years on monthly remuneration of Rs. 7480/‐. This scheme has changed the<br />
hospital environment drastically and given awareness to patients that a<br />
trained medical professional will be available on all 365 days in the hospitals.<br />
This introduction is apart from the existing staff strength.<br />
Compulsory <strong>Rural</strong> Service to MBBS Doctors and PG<br />
Doctors<br />
This was another feat launched by NRHM in Kerala. This scheme was<br />
ensured that all the MBBS students are given a chance to work in the<br />
Government Hospitals to test and experienced their knowledge acquired<br />
from the colleges.<br />
NRHM is offering a pay packet of Rs. 15000/‐ for<br />
compulsory rural service and Rs. 20,000/‐ to those who are posted to Difficult<br />
to <strong>Rural</strong> Areas.<br />
Likewise the PG Students also given same opportunity in their field<br />
and they are given Rs. 17,000/‐ as they are posted in Medical Colleges and<br />
Other Major Hospitals.<br />
Strengthening of AYUSH<br />
NRHM selected 74 Ayurveda Doctors and posted to various ayurveda<br />
hospitals across the State by Ayurveda Directorate.<br />
NRHM also selected 59 Homoeo Doctors and their posting is awaited<br />
to get a final nod from Government of Kerala.<br />
33
Block Arogyakeralam Coordinator<br />
Our country is on the threshold of developmental activities and in this<br />
modern era no establishment can survive without the help of management<br />
skilled personnel. This is the background on which NRHM Kerala has selected<br />
a cream of 153 MBA/MSW Graduates with a minimum of 2 years experience<br />
to implement, monitor and project entire range NRHM activities in block<br />
level. Now it is found that this venture by NRHM Kerala is a grand success. In<br />
addition 55 candidates from <strong>Health</strong> Services in the cadre of <strong>Health</strong> Supervisor<br />
/ <strong>Health</strong> Inspector are also selected to work as Block Arogyakeralam<br />
Coordinator.<br />
Public Relations Officer<br />
Another notable feature of NRHM Kerala is the appointment of Public<br />
Relations Officer in all selected Major Hospitals. Their qualification was<br />
either MBA or MHA with 2 years experience in health sector. The output<br />
given by these gentlemen are extremely good and they are an asset to the<br />
hospital and NRHM in implementing programmes in the hospital.<br />
Bio Medical Engineers<br />
Candidates with Degree / Diploma in Bio Medical Engineering /<br />
Instrumentation Egg are qualified for this post. As an initial step 1 (one) Bio<br />
Medical Officer and 4 Assistant Bio Medical Officers are selected and under<br />
training.<br />
Quality Assurance Officers<br />
Initially 1 (one) Regional Quality Assurance Officer and 3 (three)<br />
Assistant Quality Assurance Officers are selected and they are under training.<br />
34
Administrative Training to Superintendent of CHC and all<br />
other Government Hospitals<br />
This is meant for providing training to all Superintendents of the said<br />
hospitals, designed to give training on various aspects of management,<br />
logistics, technical, administration etc. This training is expected to equip all<br />
the Superintendents to handle various problems arising in the hospital from<br />
time to time.<br />
ACR Lab<br />
ACR Lab will be introduced to all major hospitals on 24 hours basis.<br />
The needy will get speedy and accurate clinical facilities within their reach on<br />
an affordable cost. Thereby the private sectors who are grabbing a lion’s<br />
portion with their outdated equipments will automatically wither away.<br />
35
Innovation By Engineering wing of<br />
NRHM, Kerala<br />
Engineering is not an experiment but certainly an art and execution of the art<br />
depends on will power and planning. With regard to Engineering wing of<br />
NRHM in Kerala and its challenging activities undertaken in this tiny state is<br />
most certainly an example of this will power. With in the span of two years it<br />
has undertaken so many projects and brought to a level of perfection in<br />
almost all the work of its inventory. It is an accepted fact that, money alone<br />
will not bring the desired changes but efficiency, sincerity and proper<br />
planning also required to fulfill the dream to a reality. Pertaining to this<br />
situation NRHM, Engineering Wing deserves applaud from all.<br />
The following are the innovations with regard to the work initiated from the<br />
Engineering wing of NRHM.<br />
The up gradation of health care institutions to Indian Public <strong>Health</strong> Standards<br />
(IPHS) is being carried out through external agencies like Hindustan Latex Ltd,<br />
Hindustan Prefab Ltd. and Kerala <strong>Health</strong> Research and Welfare Society. These<br />
agencies are Government owned institutions and conducts necessary surveys<br />
and prepare detailed project reports in conformity with the specifications<br />
and standards. This enables better quality of work, which was earlier absent<br />
when PWD was doing the construction activities.<br />
Community <strong>Health</strong> Centers were the next objects. The up gradations of these<br />
<strong>Health</strong> centers were carried out with the participation of the local authorities,<br />
the hospital authorities and other stakeholders. An institutional level<br />
committee has been constituted for each CHC and this ensured that the<br />
projects prepared by the implementing agencies are thoroughly discussed by<br />
36
all stake holders. The monitoring and evaluation of the work by the ILC was<br />
also ensured in each point.<br />
The only Marmachikitsa Hospital, under the Government sector at<br />
Kanjiramkulam in Thiruvananthapuram district was also selected for up<br />
gradation and work is nearing completion.<br />
Emergency situation call for an urgent attention by the concerned authority.<br />
We recall, the emergency situation cropped up in the SAT Hospital and<br />
Renovation and infection prevention work was carried out in record time,<br />
when there was an incidence of outbreak of Sepsis at the SAT Hospital at<br />
Thiruvananthapuram. Another example is the completion of an idle building<br />
at Sabarimala by PWD during the Pilgrim season on a record time. The<br />
renovation work undertaken to repair the building for the benefit of pilgrim is<br />
a classic example of this.<br />
All the agencies have been directed to prepare a master plan for the hospitals<br />
and any further expansion would be based on such master plans.<br />
It is decided to complete a sewage treatment plant at Kozhikode MCH. At<br />
present there is no such system and the people in the vicinity of MCH, are<br />
facing pollution and unhygienic situations due to this. This situation is taken<br />
with utmost seriousness and within a short time, a fully functional sewage<br />
treatment plant will come up to alleviate the era of such pollution. The work<br />
will form part of the up gradation of IMCH Kozhikode and is nearing<br />
completion.<br />
The Bio‐ Medical waste disposal from each health care institution is a big<br />
challenge before the Government and <strong>Health</strong> conscious Population. This is<br />
presently being carried out in some major institutions through IMAGE, an<br />
organization under the Kerala chapter of IMA. It is now proposed to extend<br />
the agreement with IMAGE to all the other institutions, which are being<br />
upgraded.<br />
37
A proposal for Emergency Management of health and accident related issues<br />
was prepared and forwarded to the Government for consideration. This is<br />
now with the Government for approval.<br />
The Tsunami Rehabilitation Programme under the <strong>Health</strong> Department is<br />
being implemented by the Engineering wing of the Sate NRHM through the<br />
State <strong>Mission</strong> Director who is the nodal officer of the Project Implementation<br />
Unit. The progress is relatively fast when compared with other departments<br />
and also the works are in conformity with the IPHS specifications, carried out<br />
through implementing agencies like HLL, HPL, and KHRWS etc.<br />
In all construction activities priority is given to renovate/modify existing<br />
usable buildings, including heritage buildings and demolition is adhered to<br />
only in unavoidable circumstances. This will surely, save time, money and<br />
energy.<br />
Bio‐Medical engineers have been appointed to take care of the equipment<br />
needs in the <strong>Health</strong> sector and they are preparing the requirement of each<br />
institution in the state. Once this work is completed procurement is planned<br />
through the Government owned Kerala Medical Services Corporation.<br />
38
Progress of Engineering Works at various Districts<br />
CHC Enadhimangalam<br />
(Before renovation )<br />
CHC Enadhimangalam<br />
(work in progress )<br />
CHC Thamarassery<br />
(Before renovation )<br />
CHC Thamarassery<br />
(Work in progress )<br />
CHC Neendakara Old OP Block<br />
(Before Renovation )<br />
CHC Neendakara Old OP Block<br />
(After Renovation )<br />
39
CHC Kanjettukara old building<br />
(Before Renovation )<br />
CHC Kanjettukara old building<br />
(Work in progress )<br />
CHC Kadakkal<br />
(Before renovation )<br />
CHC Kadakkal<br />
(work in progress )<br />
CHC Anchal Old OP Block<br />
(Before renovation )<br />
CHC Anchal New OP Block<br />
(work in progress )<br />
40
CHC Mayyanad Old OP Block &<br />
Entrance Zone (Before Renovation)<br />
CHC Mayyanad Old OP Block &<br />
Entrance Zone (work in progress)<br />
CHC Kalpetta (After Renovation)<br />
CHC Perambra (Upgraded)<br />
CHC Vadanappally (Before Renovation)<br />
CHC Vadanappally (work in progress)<br />
41
Accreditation of Hospitals in Kerala<br />
Government has initiated steps for Standardization of Hospitals and<br />
Public <strong>Health</strong> Institutions in the State. Up gradation and Standardization of<br />
services including diagnostic facilities in the Government Hospitals need to be<br />
implemented as a prelude. Specialty cadre is also being implemented in the<br />
state. This will rationalize the posting of doctors especially Specialists.<br />
Government of Kerala has implemented the scheme of<br />
Comprehensive <strong>Health</strong> Insurance Scheme from October, 2008. Government<br />
Hospitals and other health facilities with desired infrastructure for inpatient<br />
and day care facilities will be empanelled with the selected insurance<br />
company. Accreditation of Public <strong>Health</strong> Institutions can help us achieving the<br />
above mentioned points especially the Up gradation and Standardization of<br />
services.<br />
Quality council of India (QCI) is an autonomous body set up by<br />
Government of India to establish and operate the <strong>National</strong> Accreditation<br />
Structure in the country. <strong>National</strong> Accreditation Board for Hospitals &<br />
<strong>Health</strong>care Providers (NABH) is a constituent board of Quality Council of<br />
India, set up to establish and operate accreditation programme for<br />
healthcare organizations. Initiating the process of accreditation will help the<br />
<strong>Health</strong> Department to assess the existing service delivery standards of the<br />
said facilities, to identify the baseline level of all quality indicators; to<br />
benchmark the indicators, to suggest alterations in structural designs of the<br />
facilities to meet the requirement.<br />
It was decided to include one hospital from one district for<br />
accreditation with NABH. The hospitals selected for the accreditation process<br />
are given below.<br />
42
S.No District Name Hospital Name Bed Strength<br />
1. Trivandrum W and C Hospital, Trivandrum 428<br />
2. Kollam District Hospital, Kollam 471<br />
3.<br />
4.<br />
Pathanamthitta<br />
Alappuzha<br />
General Hospital,<br />
Pathanamthitta<br />
Taluk Head Quarters Hospital,<br />
Cherthala<br />
414<br />
251<br />
5. Kottayam District Hospital, Kottayam 374<br />
6.<br />
Idukki<br />
Taluk Head Quarters Hospital,<br />
Thodupuzha<br />
304<br />
7. Ernakulam General Hospital, Ernakulam 779<br />
8.<br />
Thrissur<br />
Taluk Head Quarters Hospital,<br />
Chavakkad<br />
140<br />
9. Palakkad District Hospital, Palakkad 562<br />
10. Malappuram District Hospital, Manjeri 501<br />
11. Kozhikode W and C Hospital, Kozhikode 295<br />
12. Wayanad<br />
Taluk Head Quarters Hospital,<br />
Sulthan Bathery<br />
13. Kannur District Hospital, Kannur 616<br />
14. Kasaragod District Hospital, Kanhangad 400<br />
57<br />
An agreement has been signed between Government of Kerala and<br />
Quality Council of India for accreditation of hospitals in Kerala. The Quality<br />
Council of India, New Delhi shall carry out the activities specified as follows:‐<br />
►<br />
►<br />
►<br />
►<br />
To understand the existing level of health care delivery by discussion<br />
with policy makers and senior officers and other stake holders;<br />
To review the secondary data available like bed occupancy rate,<br />
OPD Attendance, No. of Discharges, Average length of stay, number<br />
of samples etc.;<br />
To have a sensitization workshop for policy makers and officials of<br />
the Dept. of <strong>Health</strong> and Family Welfare;<br />
To suggest any basic minimal civil structural alteration, if required in<br />
the identified hospitals and labs;<br />
43
►<br />
►<br />
►<br />
►<br />
►<br />
►<br />
►<br />
►<br />
►<br />
►<br />
►<br />
►<br />
►<br />
To study the manpower deployment against any pre set norms<br />
appropriate to the needs as per the requirement of NABH;<br />
To indicate the gap in the terms of manpower, equipments and<br />
drugs<br />
To study the equipment and instrument functionality, maintenance<br />
and calibration of the same;<br />
To identify senior and potential trainers from within the facilities at<br />
all the facilities;<br />
To conduct training of trainers of various facilities;<br />
To do the training needs assessment of all personnel in relation to<br />
achieving NABH standards;<br />
To prepare training modules based on Training needs assessment<br />
(TNA) and the Accreditation standards of NABH;<br />
To assist in organizing Training Program for all personnel;<br />
To observe and analyze the effectiveness of such training by<br />
carrying out patient satisfaction survey, employee satisfaction<br />
surveys and hospital utilization rates coupled with analyzing the<br />
health indicators;<br />
To assist to create signage, work instructions, manuals etc.<br />
necessary for the facilities;<br />
To facilitate carrying out internal audit as per NABH Standards for<br />
the facilities;<br />
To assist in carrying out the self assessment as per NABH standards;<br />
and<br />
To assist in follow up action after preliminary assessment and final<br />
assessment by Assessors.<br />
Under NRHM, for accreditation, equipping the hospitals with medical<br />
equipments and providing other facilities like cots, linen etc., has been<br />
decided in principle by the Government that henceforth the equipment<br />
purchase in all the institutions shall be under the aegis of Kerala Medical<br />
Services Corporation for which Bio Medical Engineers are appointed. It has<br />
also decided to modify the State and District Quality Assurance Committees<br />
to widen the scope from only sterlisation and Family Planning services to up<br />
44
gradation and quality assurance of hospital inpatient care and diagnostic<br />
services.<br />
After completion of this phase the hospitals will have to apply for<br />
accreditation with NABH. Accreditation process includes application for<br />
accreditation, pre assessment visit by NABH, final assessment of hospitals,<br />
scrutiny of the assessment report by NABH secretariat and recommendation<br />
for accreditation by Accreditation Committee, approval for accreditation by<br />
Chairman NABH and issue of accreditation certificate by NABH secretariat.<br />
45
E-banking practice under NRHM in<br />
Kerala<br />
Achieving heights with new experiments and the implementation of<br />
the said results in the existing scene is the collective effort of many. As we all<br />
are aware that Finance is the<br />
backbone of any activity in motion, it<br />
is essential that a strict monitoring<br />
about its movement is mandatory to<br />
have a control over it. During the<br />
introduction of NRHM in Kerala, it<br />
was the big concern of finance<br />
department to have a day‐to‐day control over the inflow and outflow of<br />
money in NRHM activities. This has led to the innovation of e‐banking in<br />
Kerala thus became the pioneer among NRHM states. When the NRHM was<br />
initiated in 2005‐06, Kerala<br />
was the first state to<br />
understand that the<br />
conventional way of<br />
transacting money was no<br />
longer feasible. Innovation<br />
was needed and on an<br />
experimental basis a pilot<br />
programme was launched<br />
in Kerala. The response from the state was overwhelming and with many<br />
months of hard work put in all the financial transactions under NRHM have<br />
been put under the e‐ Banking platform in Kerala. What is unique about this<br />
46
innovation is that, this is the first time to happen anywhere in the country in<br />
the health sector. This is a ground‐breaking change and will go a long way in<br />
establishing a firm grip over the finances of the mission at the national level.<br />
The experiment was initiated around 2 years back, and through a<br />
progression of feedback from the grass root, continuous improvements were<br />
made on the software. As a result, today the software is user friendly, flexible<br />
and is an effective financial information tool. Not only are the transactions<br />
under the e ‐ banking platform faster and safe, but the exquisiteness of the<br />
system is the online information system.<br />
e‐ Banking solution for<br />
NRHM has been put in place in<br />
Kerala, through Customized<br />
software developed by ICICI on<br />
a consultative process with the<br />
users. The software is named<br />
“i‐check pay software”. The<br />
state is now completely online<br />
in transacting funds under<br />
NRHM at both the state headquarters as well as in the 14 districts. The users<br />
are finding the online system not only user friendly but also has given the<br />
state with the desired freedom of flexibility along with increased control over<br />
transactions and minimal delays in transfer of funds. The ease, speed and<br />
increased control over transactions are found to be very effective in the<br />
financial management of NRHM considering that over 70% of funds are<br />
devolved to the institutions at the grass root level. The simple, safe and easy<br />
to use solution for transfer of funds has proved as a boon to NRHM,<br />
considering that adequate and timely devolution of funds are essential to<br />
support the massive works taken up under NRHM on a scale never seen<br />
before. Currently, the solution is offered up to the district level, but<br />
47
eventually it is the desire of the state to enlarge the solution up to the block<br />
level.<br />
From the Ministry, Grants are released online to the designated bank<br />
account of the State with ICICI Bank, and sanction order is posted on the web<br />
site. Grants are booked under main heads: RCH – II / <strong>Mission</strong> Flexible<br />
Pool/Immunization/Ayush/Others as the case may be. A single bank account<br />
with ICICI is maintained at state<br />
level and district level for RCH<br />
Flexi pool + <strong>Mission</strong> Flexible<br />
Pool+ Immunization. Below<br />
district level, the beneficiary<br />
institution maintains bank<br />
account with any scheduled<br />
commercial bank. Similarly, each<br />
of <strong>National</strong> Disease Control Program has one bank account at state<br />
level/district level with ICICI Bank<br />
Fund transfer from the state to districts and vendors are done online<br />
from the designated bank<br />
account. Each release is<br />
captured from the main heads:<br />
RCH – II / <strong>Mission</strong> Flexible<br />
Pool/Immunization/Ayush/othe<br />
rs as the case may be, and this<br />
enables at any point of time the<br />
bank balance in the main<br />
heads. Also automatic computation of expenditure and advances is made<br />
possible.<br />
The traditional system of writing cheque has been totally<br />
discontinued at the state level and in the districts. From the state, funds are<br />
48
eleased online to the designated bank account of the district and sanction<br />
order is posted on the web site. The district gets the amount within 24 Hours<br />
to the Bank Account. The districts are enabled at any point of time to have<br />
the bank balance in the main heads, and automatic computation of<br />
expenditure and advances is done. Not only the districts, but to employees<br />
and any other vendor each payment is electronically transferred to the bank<br />
account of beneficiary/recipient. Accountant is the first level operator to<br />
enter the transactions on line. Authorized signatory 1 and Authorized<br />
signatory 2 approves the transactions. Once transactions are approved,<br />
transfer of money to the designated bank account of the beneficiary/vendor<br />
is done within 24 hours<br />
Along with the transfer of funds, the system captures the transfer<br />
either as an advance or as expenditure as the case may be, into the<br />
designated programme (RCH‐II/<strong>Mission</strong> Flexible Pool/Immunization). The<br />
advance when settled is captured and adjusted from that of advance to the<br />
expenditure. The software is so user friendly that it is very easy to track<br />
pending transactions and understand the balance position of different<br />
segments. Transactions Reports and advance positions are generated by the<br />
system. SOE positions and utilization reports are generated on line.<br />
49
How it has helped the state of Kerala …<br />
Example: Because more than 1000 Doctors and 1500 Staff Nurses are<br />
in place, substantial amounts were being devolved from the District<br />
Societies to PHC/CHC etc. for salary payment – getting back UC was<br />
problem. With e‐ Banking all the Doctors/Staff Nurse/Lab<br />
Technicians/Block Coordinators have been asked to intimate their<br />
personal bank account details so that on the basis of attendance<br />
certificate from Medical Officer, the District Societies can directly<br />
credit the salary to the bank account of the employee. THIS WILL<br />
ENABLE INSTANT CAPTURE OF EXPENDITURE RATHER THAN WAITING<br />
FOR SOE/UC FROM THE PHC/CHC.<br />
Example: More than 8000 ASHAS have been selected and trained in<br />
Kerala. The number will be much higher in the days ahead. Rather<br />
than following the conventional route of transfer of funds to PHC/CHC<br />
ASHAS will be issued a CARD and payment to ASHA will be routed by<br />
the Districts through CARD System. This enables immediate capture of<br />
SOE and is also more secure. It is also user friendly as the CARD can be<br />
used through ATMs of any bank<br />
Con‐Current Auditing<br />
The Financial Management system in NRHM was further strengthened<br />
and better internal controls established both at State as well as Districts. A<br />
fool proof system of capturing the monthly expenditure was put in place. As a<br />
new initiative, Concurrent Audit was set up at Head quarters and all the<br />
districts. The purpose of Con current audit is to determine whether the<br />
financial management arrangements including internal control mechanism as<br />
developed are working effectively, identify areas for improvement and<br />
enhancing efficiency.<br />
1. The focus of the concurrent audit is to see that:<br />
a. Accuracy is ensured in maintenance of books of account<br />
and these are maintained on a timely basis;<br />
b. Advances are tracked, followed up and settle on a priority<br />
basis;<br />
50
c. Exclude advances being shown as expenditure in the FMRs;<br />
d. Bring in accuracy to the monthly/quarterly Financial<br />
Monitoring Reports based on books of accounts;<br />
e. Ensure voucher/evidence based payments to improve<br />
transparency.<br />
f. Enable timely and accurate submission of financial MIS to<br />
the management.<br />
g. Improve the accuracy and timeliness of financial reporting<br />
from sub‐District levels; and<br />
h. Improve the internal control systems in the society.<br />
The monthly concurrent audit report includes:<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Audited Receipts & Payments Account,<br />
Audited Income and Expenditure Account,<br />
Audited Balance Sheet,<br />
Audited Statement of Expenditure,<br />
Bank reconciliation,<br />
Age‐wise report of Advances,<br />
Visited block’s Report, (one or two blocks per month),<br />
Comparison of physical Vs financial,<br />
Reporting in the checklist format,<br />
Auditor’s comments,<br />
Actions taken on previous month’s observations.<br />
In addition to the audit report a “Management Letter” is also to be furnished<br />
which contains the following:<br />
a. Comments and observation on the notes to the accounts,<br />
accounting policy, accounting records, systems and internal<br />
controls.<br />
b. Identify specific deficiencies and areas of weaknesses in the<br />
systems and internal controls and make recommendations for<br />
their improvement.<br />
c. Communicate matters that have come to the attention of the<br />
auditors, which may have a significant impact on the project<br />
implementation.<br />
d. Bring to attention any other matters that the auditor considers<br />
pertinent.<br />
51
Accreditation of Government Medical<br />
Laboratories in Kerala<br />
Quality council of India (QCI) is an autonomous body set up by<br />
Government of India to establish and operate the <strong>National</strong> Accreditation<br />
Structure in the country. <strong>National</strong> Accreditation Board for laboratories (NABL)<br />
is a constituent board of Quality Council of India, set up to establish and<br />
operate accreditation programme for healthcare organizations.<br />
There are 348 Government Medical Laboratories in Kerala. This<br />
includes large laboratories, medium laboratories and small laboratories. Most<br />
of the Laboratories under <strong>Health</strong> department in Kerala are devoid of essential<br />
standard inspection, enforcement and public accountability regulation of<br />
diagnosis services. These Medical Laboratories need specific essential<br />
standards for diagnostic services at all levels. Accreditation of QCI certified<br />
standards, ISO certification and eventually NABL accreditation of Laboratory<br />
Diagnostic Services will improve the quality of health care services.<br />
<strong>Health</strong> care traditionally has been physician focused. Evidence based<br />
medical laboratory diagnostic services play key role in improving quality of<br />
health care services. This can be made possible only by adopting state‐of‐the<br />
art laboratory facilities along with competent technicians, supervisory and<br />
managerial staff. Medical Laboratories are central function for clinical<br />
diagnosis and treatment.<br />
More over Government of Kerala has decided to implement the<br />
scheme of Comprehensive <strong>Health</strong> Insurance Scheme from October, 2008 in<br />
Kerala. Government Hospitals and other health facilities with desired<br />
52
infrastructure for inpatient and day care facilities will need to be empanelled<br />
with the selected insurance company.<br />
A Memorandum of Agreement has been signed between Government<br />
of Kerala and Quality Council of India (QCI), for Accreditation of Laboratories<br />
in Kerala. QCI, will begin the execution of lab awareness programme and the<br />
lab application process soon. QCI will implement a customer service<br />
telephone helpline prior to the commencement of awareness programming<br />
to answer lab process implementation. QCI will provide to the State, a<br />
complete set of the QCI Programme manuals, educational guidelines, criteria,<br />
templates and forms to be provided to the labs. QCI will prepare and provide<br />
online access for State personnel to its lab database.<br />
Initiating the process of Accreditation will help the <strong>Health</strong> Department<br />
to assess the existing laboratory service delivery standards of the said<br />
facilities, to identify the baseline level of all quality indicators and to suggest<br />
alterations in structural designs of the facilities to meet the requirement. A<br />
review of facilities including laboratory space and laying down standard<br />
operating procedures for various activities, training of the key personnel will<br />
help in getting ISO/ NABL Accreditation.<br />
Under NRHM, for accreditation, equipping the hospitals with medical<br />
equipments and providing other facilities like cots, linen etc., it has been<br />
decided in principle by the Government that henceforth the equipment<br />
purchase in all the institutions shall be under the aegis of Kerala Medical<br />
Services Corporation for which Bio Medical Engineers were appointed. It has<br />
also been decided to modify the State and District Quality Assurance<br />
Committees to widen the scope from only sterilization and Family Planning<br />
services to up gradation and quality assurance of hospital care and diagnostic<br />
services.<br />
It was decided to include all Government Laboratories in Kerala<br />
namely State Public <strong>Health</strong> Laboratory, Regional Public <strong>Health</strong> Laboratories,<br />
53
District Public <strong>Health</strong> Laboratories, Medical Laboratories attached to District<br />
Hospitals, General Hospitals, Women and Children Hospitals, Specialty<br />
Hospitals, Thaluk Head Quarters Hospitals, Government Hospitals, CHCs,<br />
Block PHC, PHCs and Medical College Hospitals for accreditation.<br />
54
Telemedicine<br />
Introduction<br />
Telemedicine is the use of<br />
electronic signals to transfer<br />
medical data (photographs, x‐ray<br />
images, audio, patient records,<br />
videoconferences, etc.) from one<br />
site to another via the Internet,<br />
Intranets, satellites, or<br />
videoconferencing telephone<br />
equipment in order to improve access to health care. Real time telemedicine<br />
could be a simple telephone call, video‐conferencing, remote monitoring or<br />
consultation using tele‐otoscope, a tele‐stethoscope, Teleradiology, remote<br />
microscope etc.<br />
History<br />
In 1906 Einthoven, inventor of electrocardiography first investigated on ECG<br />
transmission over telephone lines. During 1920s, radios were used to link<br />
physicians at shore stations to assist ships at sea that had medical<br />
emergencies. First large‐scale telemedicine project, Space Technology<br />
Applied to <strong>Rural</strong> Papago Advanced <strong>Health</strong> Care (STARPAHC), was developed<br />
and demonstrated by NASA in 1973. NASA initially used telemedicine to<br />
transmit basic physiological data from astronauts to understand the effects of<br />
launch, spaceflight, and reentry on the human body. During 1960s Moon<br />
programme accelerated telemedicine and telescience systems development.<br />
55
In developed countries constraints on time and resources will make<br />
face to face consultation increasingly expensive, and telemedicine has the<br />
potential to produce major efficiencies in the diagnostic process. In<br />
developing countries telemedicine will help the rural people to access<br />
specialty health care services.<br />
Indian Space Research Organization, Department of Information<br />
Technology, Centre for Development of Advanced Computing and <strong>National</strong><br />
<strong>Rural</strong> <strong>Health</strong> <strong>Mission</strong> Supporting the Telemedicine projects in India.<br />
Telemedicine projects started in Kerala as early as 2002 to provide<br />
follow‐up treatment to cancer patients. The success of the Cancernet leads to<br />
development and deploy of many telemedicine projects in Kerala.<br />
Coordination and inter liking of all<br />
telemedicine projects in Kerala is<br />
envisaged under NRHM. More over<br />
the same network can be used for<br />
patient care, follow‐up treatment,<br />
diagnosis, continuing medical<br />
education, teleconferencing, patient<br />
education, behavioral change communication and communication and case<br />
discussion.<br />
56
Telemedicine Projects in Kerala<br />
Sl. No Name of project Funding Agency Implementing<br />
Agency<br />
1<br />
CANCERNET – later changed to<br />
Onconet<br />
DIT‐ Govt of India<br />
2 ONCONET – Kerala<br />
&<br />
CDAC<br />
ISRO<br />
3<br />
DIT‐Govt of India<br />
Telemedicine and Tele‐<br />
CDAC<br />
&<br />
Education Facilities in Kerala<br />
Govt of Kerala<br />
4<br />
Tele <strong>Health</strong> and Medical EducationISRO &<br />
Project Kerala<br />
GoK<br />
ISRO<br />
5<br />
<strong>Rural</strong> <strong>Health</strong> Care Delivery systemMedia Lab Asia<br />
through Telemedicine<br />
(DIT)<br />
CDAC<br />
6 Mobile Telemedicine<br />
Media Lab Asia<br />
(DIT)<br />
CDAC<br />
Revitalisation of existing<br />
7<br />
telemedicine centres and scaling up<br />
NRHM<br />
telemedicine facility to more<br />
CDAC<br />
primary care centres in Kerala.<br />
1. Cancernet<br />
Cancernet was the first endeavor in India in the area of tele‐oncology,<br />
which was successfully commissioned in 2002. Cancernet was an oncology<br />
network for providing telemedicine services in cancer detection, treatment,<br />
pain‐relief, and patient follow up and continuity of care through peripheral<br />
hospital. It provided great help to the cancer patients who needs continuous<br />
follow up and treatment. Success of cancernet paved the way for the fullfledged<br />
Telemedicine project Onconet.<br />
Onconet<br />
Cancernet later converted to Onconet, which consist of teleconsultation<br />
clinics at Regional Cancer Centre (RCC) and its peripheral centers<br />
at Kochi, Kannur, Palakkad, Kozhenchery and Chavara. High bandwidth<br />
57
connectivity is available between RCC and peripheral centers through<br />
satellite link. It includes tele‐pathology and radiology system at RCC and two<br />
nodes for capture, storage, transmission and online sharing of images. There<br />
is also an oncology resource centre, which provides cancer related<br />
information to clinicians, researchers, health planners and administrators on<br />
the telemedicine network and Intranet.<br />
It is a web based telemedicine system with hospital information<br />
system as the back end and telemedicine software tightly integrated with<br />
Hospital Information System. It is a multi‐tier web application runs on Java<br />
and J2EE Technologies, Oracle 10g database and an application server.<br />
Connectivity is provided with 384 Kbps V‐SAT and 128 Kbps ISDN.<br />
Main components of oncology telemedicine systems includes a video<br />
conferencing system , connectivity between RCC with nodal centres and a<br />
central server containing patient data, accessible through LAN within the RCC<br />
as well as at nodal centres through a WAN.<br />
Telemedicine provides a way for cancer patients to get follow‐up near<br />
their home town.<br />
2. Telemedicine And Tele Education Facilities In Kerala.<br />
Four Taluk Hospitals, Mental <strong>Health</strong> Centre Trivandrum, Medical<br />
College Hospital, Trivandrum, Sree Chithira Thirunal Institute, and RCC form<br />
this telemedicine network. This network is functioning using the Mercury<br />
Telemedicine software developed by C‐DAC.<br />
3. Tele <strong>Health</strong> and Medical Education Project Kerala.<br />
This project connects 6 Medical colleges, Regional Cancer Centre,<br />
SCTIMST, all District Hospitals and one CHC. This project has been developed<br />
and implemented by<br />
ISRO, IIITMK, Govt. of Kerala and CDAC.<br />
58
4. <strong>Rural</strong> <strong>Health</strong> Care Delivery through Telemedicine<br />
This project is being implemented in Kerala. Aim of the project is to<br />
develop a resources sharing, integrated, rural healthcare delivery system<br />
through Telemedicine using Information and Communication Technology<br />
(ICT) at Tirur Taluk of Malappuram District, Kerala using available network<br />
coverage provided by Akshaya Network. System study completed and<br />
specialty and nodal centres are identified which included 9 CHC and one<br />
THQH. Web based Telemedicine Software is under development in open<br />
source.<br />
5. Mobile Telemedicine<br />
This project is being implemented, which includes development of<br />
low cost mobile telemedicine facility and deploy the prototype in Cherthala,<br />
Alappuzha district with the objectives of extending specialist care to the rural<br />
areas for early detection of diseases like Tuberculosis, diabetes, hypertension<br />
etc. It also includes follow up of patients with chronic diseases, early<br />
detection of cancers, comprehensive care for the cancer patients, follow‐up<br />
consultation and provision of maternal and child health services.<br />
6. NRHM Telemedicine Proposal‐ Project for revitalisation of existing<br />
telemedicine centres and scaling up telemedicine facility to more primary<br />
care centres in Kerala.<br />
Memorandum of Agreement has been signed between NRHM and<br />
CDAC for the implementation of the project. Objectives of the project are to<br />
make all the telemedicine centres set up under the different projects fully<br />
operational, to promote the usage of the telemedicine centres for patient<br />
care, to bring all the telemedicine centres in Kerala in a common frame work<br />
and to establish more telemedicine centres in health care institutions. It is<br />
also decided to start telemedicine centres at General Hospital Trivandrum<br />
and Malabar Cancer Centre.<br />
59
ASHA workers - Owning more<br />
responsibilities<br />
The ASHA was earlier planned to be implemented in the States<br />
with poor <strong>Health</strong> Indicators. However, after a detailed assessment on the<br />
special needs of the states Government of India approved ASHA scheme for<br />
the whole population in the state of Kerala. Further, it was planned to deploy<br />
32853 ASHA volunteers in fourteen districts by 2010. Around 20,000 ASHA<br />
volunteers have been selected so far of which 10,000 have been deployed in<br />
the state. First Phase of training has been completed for the selected ASHA<br />
volunteers.<br />
The roles and responsibilities envisaged for are as follows:<br />
Identify pregnant women as a beneficiary of the Scheme and report /<br />
facilitate registration at the sub centre for ANC.<br />
Assist the pregnant woman to obtain necessary certifications where<br />
necessary.<br />
Provide and / or help the women in receiving at least 3 ANC, TT<br />
injections, IFA tablets.<br />
Identify a functional Government <strong>Health</strong> Centre for referral & delivery<br />
and acquaint the women with<br />
the details of the same.<br />
Counsel for Institutional<br />
delivery<br />
Escort the beneficiary women<br />
to the pre‐determined health<br />
centre and stay with her till the<br />
woman is discharged.<br />
Arrange to immunize the<br />
newborn till the age of 9<br />
months<br />
Register birth or death of the<br />
child or mother.<br />
Post natal visit within 7 days of delivery and track mothers health<br />
Counsel for initiation of breastfeeding to the newborn within 1 hour<br />
of delivery and its continuance till 3‐6 months<br />
Roles and responsibilities: A paradigm shift<br />
60
Considering the health scenario in the state of Kerala where the<br />
burden of non‐communicable diseases is on the rise, it has been decided to<br />
extend the role of ASHA to the management of Communicable & Non‐<br />
Communicable diseases. The areas where their services are planned to be<br />
extended are Prevention & Control of Communicable diseases, Identification<br />
& Control of NCD’s, Palliative care and Community based Mental <strong>Health</strong><br />
Programme.<br />
Towards the Prevention and control of Communicable diseases ASHA<br />
volunteers are made responsible for the following<br />
‣ Reporting of outbreaks/ cases to Sub centre/PHC/CHC<br />
‣ House to house campaigns and other IEC activities<br />
‣ House visits with teams for Source Reduction activities and<br />
chlorination and acted as volunteers for the same<br />
‣ Lead Source Reduction activities by house visits<br />
Improving Immunization through ASHA<br />
As a part of strengthening immunization the field level activities need<br />
to be strengthened using ASHA/link workers and also by making the use of<br />
local level events like the Ward <strong>Health</strong> Nutrition Days (WHNDs). WHND,<br />
which is organised every month in a ward, is the right platform to strengthen<br />
immunization under the leadership of ASHA.<br />
done by ASHA<br />
As a part of social mobilization for WHND the following has to be<br />
Visit all the household and get<br />
to know all the families. Make<br />
it a point to visit all the poor<br />
households, especially SC/St<br />
families<br />
Make a list of infants who<br />
need immunisation, were left<br />
out or dropped out<br />
61
Find out the reason for dropouts or un immunized<br />
Review and plan activities to mobilize the dropouts and un immunized<br />
children<br />
Make a list of children who need care for malnutrition<br />
Make a list of children who were missed<br />
Also ASHA workers should find out and note down the reasons for not<br />
taking immunization or missing out immunization or dropping.<br />
ASHA/JPHN should make a note on the people who did not attend the<br />
session as per their list. This should be discussed in the monthly review<br />
meetings at PHC and Special awareness/BCC drives should be launched based<br />
on the nature of resistance of the population.<br />
Special NCD Management Programme through ASHA<br />
As a part of NCD management though ASHA, during the detailed<br />
training given to ASHA volunteers, classes on prevention of Non‐<br />
Communicable Disease are given. Along with this, it is also planned to give<br />
necessary drugs / kits to ASHAs<br />
At grassroots level they are expected to take up the following<br />
activities<br />
1. Initial Home Visit to all households<br />
of there are & Collection of details<br />
of all persons above 35 in the<br />
prescribed format. For this she will<br />
be paid Rs. 2/‐ per form. (500<br />
persons out of the 1000 population for ASHA are expected to be<br />
above 50)<br />
2. Bring all those with suspicion of NCD to the Subcentre / PHC for initial<br />
Checkup. (50% of the surveyed population i.e. 200 persons are<br />
expected to be brought for initial Check up) For this she will be paid<br />
Rs. 20/‐ per person.<br />
62
3. Of the persons brought for Checkup, those who are diagnosed to have<br />
any NCD will need regular follow up. ASHA is expected to arrange for<br />
a minimum of 2 follow up visits during 1 year for each of these cases.<br />
(Almost all of the 100 persons brought by ASHA are expected to need<br />
regular follow up visits) For this she will be paid Rs. 10/‐ per follow up.<br />
63
Debit card scheme for ASHA Volunteers<br />
The background<br />
Like other states, Kerala too is deploying one ASHA volunteer for<br />
every 1000 population. Around 20,000 volunteers have been selected and<br />
half of them received the necessary training. In Thiruvananthapuram district<br />
around 2000 ASHA volunteers are already deployed. The performance of<br />
ASHA volunteers are monitored by Junior Public <strong>Health</strong> Nurse at field level<br />
and report to PHC Medical Officer. PHC Medical Officer verifies this report<br />
and effect payment to ASHA Volunteers.<br />
The issue<br />
Complaints regarding timely payment of incentives to ASHA volunteers,<br />
owing to reasons enlisted below:<br />
As the incentives are to the paid from different heads, based on the activities<br />
of ASHA workers, the PHC Medical Officers find it difficult to debit the<br />
amount from different heads. The fear of audit objection is also a reason,<br />
which causes delay in releasing the payment in time.<br />
This delay some times affects the motivation and achievement levels of ASHA<br />
workers.<br />
The solution - Debit card- a<br />
revolutionary idea<br />
To ward off delay in making payments to<br />
ASHA volunteers, Thiruvananthapuram<br />
64
district designed and implemented a novel scheme for paying incentives to<br />
ASHA Volunteers through a debit card system.<br />
Through this system, the incentives are credited to the respective accounts of<br />
AHSA volunteers from the district NRHM office. The performance report<br />
verified by the PHC Medical Officer is sent to the districts, based on which<br />
payment is made by way of crediting the amount to the respective ICICI bank<br />
account of ASHA volunteers from the district headquarters. This not only<br />
helps avoiding delay in payment but also helps in generating SOEs<br />
immediately.<br />
Features of the debit card<br />
The ICICI Bank Pay Direct Card is a pre‐paid card with magnetic strips, which<br />
can be loaded in rupees. The card does not have any minimum balance<br />
requirement and it offers the flexibility of using it at all the VISA ATM outlets.<br />
<br />
<br />
<br />
<br />
Bulk uploading and reloading facility<br />
The Card holder can upload and reload any number of cards at any<br />
time unlike with cheques, which need to be signed and distributed to<br />
each employee separately.<br />
Web‐based MIS<br />
The Card owner can check all the transactions online, which gives the<br />
advantage of better tracking of their accounts.<br />
Instant SMS alerts on every upload<br />
The Bank also provide a facility where the cardholder receives an SMS<br />
alert on his mobile phone whenever money is uploaded onto the card.<br />
24 x 7 Customer Care assistance<br />
ICICI Bank has created a dedicated helpline number that remains<br />
active 24x7. So let it be a balance inquiry, lost‐card reporting or<br />
activating the replacement card, this number remains available for<br />
help anytime.<br />
65
Immunization Drive – October 2008<br />
Background<br />
Reviewing the present scenario of Vaccine Preventable Diseases<br />
(VPDs) of the state and to save the future generation from the threats of<br />
VPDs, it has been decided to strengthen immunization coverage through<br />
intensification of IEC/BCC activities. The month of October shall be observed<br />
as ‘Immunization Month’, every year from the year 2008 onwards. The<br />
campaign will be a joint venture by the <strong>Health</strong> and Education department and<br />
District Medical officer (<strong>Health</strong>) and District Programme Manager, will ensure<br />
that all possible steps have been taken for smooth implementation of the<br />
programme.<br />
Planning and review<br />
Inter‐sectoral Co‐ordination Committees will be constituted at District,<br />
Education District, Sub district and School levels by involving officials from<br />
related departments like <strong>Health</strong>, Education, Social Welfare and LSGIs and<br />
representatives of Parent Teachers Association, IMA, IAP, Opinion leaders,<br />
religious leaders, NGOs etc., and any person suitable for strengthening<br />
immunization. District Collector will be the Chairperson. DMO(<strong>Health</strong>) will be<br />
the Convener and RCH Officer will be the Joint Convener of the District level<br />
Committee. The committee will plan and review the overall campaign.<br />
State level Launch<br />
The campaign was launched at the state level<br />
by the Minister of <strong>Health</strong> and Social Welfare in<br />
the presence of Minister for Education and<br />
66
other officials and Peoples' representatives on October 03, 2008.<br />
Campaign methodology<br />
It is proposed to hold the following IEC BCC Campaigning throughout the<br />
month of October.<br />
a. Pledge to read in School Assembly.<br />
b. Special talk once in a week in the school assembly by MO<br />
Supervisory Staff.<br />
c. Since all Wednesdays are Immunization Days, a Key Message<br />
on Immunization may be exhibited in the Notice Board of<br />
every School on 1 st , 8 th , 15 th , 22 th and 29 th of October 2008<br />
and the Class Teachers may be asked to copy the message and<br />
to convey to students of the concerned classes.<br />
d. Brochure depicting the message on immunization should be<br />
distributed to all students. Brochure, Posters, Stickers, Flip<br />
Chart and Pledge will be produced and supplied from HQ.<br />
e. Students will be given<br />
an opportunity to<br />
clarify doubts on<br />
Immunization. They<br />
will be asked to write<br />
their doubts on a piece<br />
of paper and handed<br />
over to the concerned class teachers before 25 th October<br />
2008. The written doubts so collected should be handed over<br />
to the <strong>Health</strong> Personnel through <strong>Health</strong>/Science Club of the<br />
school. <strong>Health</strong> Personnel will prepare the answers to the<br />
doubts raised by the students in consultation with the MO and<br />
Supervisory staff. The answers thus written will be submitted<br />
67
to the Headmaster concerned with the questions before 29 th<br />
October 2008 and a copy of the same should be kept in the<br />
PHC, CHC etc. The Headmaster will be asked to take necessary<br />
steps to gather all students who raised the doubts in a suitable<br />
room and arrangements may be done to read the Answers to<br />
the Questions on or before 31 st October 2008.<br />
f. Most catching awareness programmes like Ventriloquism<br />
(Monkey show)/ Magic show shall be conducted at school<br />
level where immunization coverage is low.<br />
g. Most suitable Cultural/ Folk Media Programme shall be<br />
played for the general public where the immunization<br />
coverage is low.<br />
h. Press releases on VPDs.<br />
i. Rally shall be arranged at school level and the consequences<br />
of VPD’s may be highlighted among the general public where<br />
immunization coverage is low.<br />
j. Quiz/Elocution/Essay writing/Poster making/Slogan/Poem<br />
writing competitions shall be conducted at school, sub‐district<br />
and Education district levels and the winners should be<br />
appreciated and Awards may be presented.<br />
k. Half‐day Orientation Training shall be given to all<br />
Headmasters at Sub‐district level and teachers. PTA members,<br />
selected members from <strong>Health</strong> Science Club at school level. A<br />
handbook Module may be prepared and issued to all<br />
participants.<br />
l. Efforts will be made to make Immunization as a point of<br />
discussion in all conversations and meetings.<br />
68
m. A circular is prepared and circulated to all <strong>Health</strong> institutions<br />
explaining the role and responsibilities of all levels of staff<br />
during the Immunization Month.<br />
n. Regular Press releases shall be given on the activities planned<br />
and activities performed at District and Block levels.<br />
o. Coverage through local TV channels will be ensured<br />
69
Behavioural Change Communication -<br />
Innovations<br />
Initiative 1: Compilation of Government Orders –<br />
publishing a booklet on Arogyakeralam<br />
Since the inception of Arogyakeralam in the state of<br />
Kerala, various government orders have been issued<br />
related to the implementation of the programme in the<br />
state. Previous year’s orders were printed and circulated<br />
as and when required and mostly the orders were in<br />
English. This practice did not enable easy reference of<br />
government orders. Thus to tide over this difficulty,<br />
Arogyakeralam decided to translate all the orders<br />
in local language, compile it and print together as a<br />
booklet with a brief description on NRHM and the<br />
activities. Thus a booklet named ‘Arogyakeralam‐ a<br />
guideline’ was printed and circulated widely till the<br />
ward level. This was appreciated by GoI, PRIs and<br />
the health workers at all levels and is being used as<br />
an easy reference manual for implementing NRHM activities in the state.<br />
70
Initiative 2: Local specific health melas<br />
<strong>Health</strong> Melas are envisaged under NRHM, towards sensitizing the public on<br />
available health services and creating a demand on such health services.<br />
Detailed guidelines were issued from GoI towards the conduct of this.<br />
However, considering the local demand and its peculiarity, minor<br />
modifications with necessary policy support was made, for the successful<br />
implementation of such <strong>Health</strong> Melas.<br />
Considering the popularity and impact of health melas it has been decided to<br />
hold health melas in all Legislative Assembly Constituencies in the State for<br />
which an amount of Rs. 1,00,000/ ‐<br />
(Rupees One lakh Only) per<br />
constituency, has been allotted<br />
through NRHM. 114 out of 140<br />
Melas have been organized in the<br />
year 2007‐08. Almost all of the<br />
health melas have been a grand success in terms of community participation,<br />
organization and response from the common mass, who participated in<br />
Melas. It is worth mentioning that Rs. one lakh, per constituency has been<br />
devolved from NRHM towards the conduct of the mela, an equal amount or<br />
more, has been raised through sponsorship. The ownership and involvement<br />
shown by the Members of Legislative Assembly is commendable. Apart from<br />
the amount allotted per constituency, the elected representatives were able<br />
to raise more amounts making the Melas a grand success.<br />
71
Initiative 3: Local Specific IEC campaign: Bodhana Nauka<br />
(Information Boat)<br />
NRHM, Alappuzha and AIR, jointly organized a Bodhana Nauka or Information<br />
Boat for conveying the health awareness among water logged Kuttanad<br />
region in Alappuzha, which was really a grand success and caught the<br />
attention of everyone.<br />
The life of Kuttanadan folks are<br />
mostly like fish, who take birth in<br />
water and continue their life in<br />
water. This has caused them to<br />
be affected by water borne<br />
diseases as well as vector borne<br />
diseases like chikungunya,<br />
Leptospirosis, diarrhea etc. The programme called 'Bodhana Nauka' was<br />
focused to give more attention on creating health awareness especially on<br />
preventive measures for different communicable diseases among the people<br />
by joining hands with health professionals, people's representatives ,<br />
community leaders, educational Institutions, religious institutions, ASHA<br />
volunteers etc. The programme included street plays, awareness classes, quiz<br />
competitions for public and school children, Special radio programmes etc.<br />
Initiative 4: Promoting the brand Image of NRHM<br />
The society registered for implementing NRHM in the state has been named<br />
AROGYAKERALAM towards popularizing the brand image of NRHM. The<br />
name AROGYAKERALAM was placed in NRHM logo and was used widely to<br />
have maximum mileage. Moreover a slogan ‐ AROGYAKERALAM<br />
AISWARYAKERALAMI‐ was also coined as a part of popularizing brand image.<br />
72
<strong>Health</strong> messages placed through newspapers, journals, weeklies, souvenirs,<br />
events, electronic media etc carried the logo and the slogan with<br />
prominence.<br />
Initiative 5: Caller ring tone<br />
Title song with health message as the lyrics has been designed and<br />
produced. This is now being used as caller ring tones in all corporate<br />
mobile connections of NRHM. The song having a message is also<br />
played during all functions/events of NRHM. This has helped in<br />
popularizing the brand image of NRHM as well as increasing the<br />
visibility of the programme.<br />
73
Pain and Palliative Care under NRHM<br />
CARE of the incurably ill, Dying and Chronically Bedridden<br />
PATIENTS<br />
Background<br />
Most countries in the Developing world are experiencing health transitions<br />
with a rapidly rising burden of chronic and incurable diseases, which are<br />
currently, the major cause of death among adults.<br />
In India, in 2005, 53 percent of deaths were due to chronic diseases 43 % of<br />
disability adjusted life‐years ( DALY’s) lost. According to WHO estimates,<br />
about 5.4 million of them would benefit from Palliative Care. Palliative care<br />
is the active total care of patients<br />
whose disease is not responsive to<br />
curative treatments. Palliative<br />
Care responds to physical,<br />
psychological, social and spiritual<br />
need of the patient and the family<br />
and extends if necessary to<br />
support in bereavement. It is<br />
patient centered and not disease<br />
focused. The goal of palliative care is the achievement of the best possible<br />
quality of life for patients and their families.<br />
Palliative care services, if implemented in a rational public health way<br />
improves the quality of life for cancer suffers, patients dying of chronic<br />
diseases, the elderly terminally ill and people suffering from AIDS.<br />
74
The Neighbourhood Network in Palliative Care (NNPC), a community owned<br />
project in Kerala has exceptionally a good coverage. NNPC offers proof to the<br />
theory that communication ownership can work wonders and the results of<br />
the performance could be outstanding if the project is in collaboration with<br />
the local government.<br />
The basic concept behind NNPC is that networks provide social support, selfesteem,<br />
identity and perceptions of control. This network of trained<br />
community volunteers with the support of health care professionals brings<br />
together individuals from diverse backgrounds. Such groups in the<br />
community have shown better understanding and cooperation in response to<br />
the challenges faced by the community.<br />
The methodology of NNPC involves getting people from a region together,<br />
discussing problems of chronic, incurable and bedridden patients in their area<br />
enlisting the support of those who are willing to spend minimum of two<br />
hours every week for helping these patients and giving the structured<br />
trainings and encouraging them to plan and organize locally relevant services.<br />
Groups of these trained volunteers are linked to the Palliative Care<br />
professional and health care institutions in the area. Community groups and<br />
health care professionals make an action plan which clearly defines individual<br />
and institutional roles and responsibilities.<br />
The funds necessary for the project are mobilized locally. The region where<br />
NNPC is in place, local governments (Panchayaths) in Kerala’s three‐tier<br />
decentralized governance have also been offering financial support for the<br />
project<br />
75
In less than eight years, the NNPC initiatives has resulted in an estimated<br />
coverage of more than 70 percent in Palliative Care and long term care in the<br />
region as against a national average of around one percent in Palliative Care.<br />
The result of NNPC has proved that the delivery of sustainable good quality<br />
palliative care and long term care is possible with community participation<br />
The new Palliative Care Policy declared by the Government of Kerala is<br />
unique in many ways:‐<br />
(i)<br />
(ii)<br />
(iii)<br />
(iv)<br />
It is the first time in Asia that any government has put forth a policy<br />
for Palliative Care<br />
This policy emphasizes the community based approach to palliative<br />
care and considers home based care as the “Corner stone” of<br />
palliative care services<br />
It highlights the need for integrating palliative care with primary<br />
health care and disease effective programme for effective coverage<br />
Integrating the existing services with the main stream health care and<br />
Local Self Government Institutions<br />
The Policy envisages the guiding principle of home based care. It considers<br />
palliative care as part of general health care and aims to ensure adequate<br />
orientation of available man power and existing institutions in the health care<br />
field to this area.<br />
The Palliative care policy of Government of Kerala validates the NNPC<br />
approach in palliative care and also endorses the WHOs recently formulated<br />
policy of community participation in the area of Non‐ Communicable<br />
diseases.<br />
76
NRHM pain and palliative care project<br />
NRHM, Kerala has initiated the project aimed at the development of<br />
community based care services for the bed ridden, elderly, chronically and<br />
incurably ill people in the state. This unique initiative is expected to have<br />
wide positive implications in the care of these marginalized groups of people<br />
in the state and also nationally. With a budget of more than 4 crore rupees,<br />
this is the largest palliative care project in India so far. This is also the only<br />
palliative care project in NRHM in any state in India.<br />
Then new NRHM project is exactly in the same lines as the government of<br />
Kerala's palliative care policy and is expected to act as the main implementing<br />
arm of this policy. The project aims at awareness and capacity building in the<br />
general community, health care professionals in government and private<br />
sector, local self government officials, the student community and grassroots<br />
level political leaders. A series of demonstration projects in the background<br />
of these awareness and training activities are expected to facilitate the<br />
evolution of a social movement in the care of the incurably and terminally ill<br />
patients in the state, well integrated to the existing health care system.<br />
Preparation<br />
<br />
<br />
<br />
As part of the preparation for<br />
the project, networking with the<br />
existing palliative care initiatives<br />
in all the districts was<br />
completed. First round of district<br />
level meetings of stake holders<br />
were finished in July 2008<br />
Recruitment of field staff for the project has been finished and the list<br />
of selected candidates published<br />
The process of establishment of the coordinating unit and resource<br />
centre at IPM is now on<br />
77
Training of the field coordinators is now on. The trained coordinators<br />
will be reporting to the corresponding DPMs after training on 18 th<br />
August.<br />
Awareness / training programs in districts will start by the third week<br />
of August<br />
The doctors and nurses selected for the project will start their training<br />
by end of August and report for work by mid October<br />
Media support:<br />
A major campaign by Malayala Manorama in association with IPM to build<br />
awareness among various sections of the people is already on. The campaign<br />
is for a period of one year and is expected to cover the whole period of the<br />
project. Malayala Manorama has agreed on continued support for the<br />
project.The news paper has promised that the new webpage launched by it<br />
and linked to its online page (third largest in the world in terms of number of<br />
hits) will have a definite space allotted for the Arogyakeralam –Palliative Care<br />
Project. This space can in future be used to reach out to wider Malayalee<br />
community all over the world.<br />
Organisations:<br />
Indian Association of Palliative Care, (IAPC) the umbrella organization of<br />
palliative care initiatives has pledged unconditional support to the project.<br />
Support from IAPC will ensure that all the existing groups in palliative care are<br />
with the project<br />
Other groups/ departments:<br />
Involvement of students and youth have been ensured (see below)<br />
Other government departments like Local Self Government Department,<br />
Department of Youth welfare and the Home Department have expressed<br />
interest in collaborating at the grass root level.<br />
78
Work done in so far:<br />
We have already started moving ahead.<br />
<br />
<br />
First state level workshop for trainers in palliative care in Kerala was<br />
conducted on 8th and 10th August 2008, Calicut. More than 100<br />
volunteer trainers from all over the state were briefed on the project.<br />
This team expected to work as resource persons for the awareness /<br />
training programs in the project<br />
All the six centres offering training in palliative care in the state<br />
brought on a common platform under the project.<br />
o RCC, Trivandrum<br />
o TIPS, Trivandrum<br />
o Amrita, Cochin<br />
o IPC, Trichur<br />
o CRCPC, Manjeri<br />
o IPM, Calicut<br />
Background work for facilitating the involvement of the students in the<br />
project is on<br />
o All NSS (national Service Scheme) units under Calicut<br />
University getting involved this year<br />
o All NSS units under technical cell (Engineering Colleges and<br />
Polytechnics) getting involved this year<br />
o Selected units under Kerala University getting involved this<br />
year<br />
<br />
Groundwork for facilitating the involvement of the youth has also<br />
been done.<br />
79
o Government of Kerala’s Youth Welfare Board has taken a<br />
decision to collaborate with the activities<br />
o Nehru Yuvak Kendras and affiliated youth clubs (more than 50<br />
clubs in each district) will collaborate with the project<br />
o This will mean awareness / training for more than 25,000<br />
young men and women in the state<br />
o Kerala Police getting involved<br />
o 20 police stations with community policing will cooperate with<br />
the project as pilot<br />
o 4th Battalain of Kerala Armed Police (more than 800<br />
personnel) in Kannur District getting palliative care training<br />
under the project next month<br />
80
RADIO HEALTH<br />
<strong>Health</strong> Literacy and Community<br />
participation have played a significant role<br />
in the development of the famed Kerala<br />
<strong>Health</strong> Model. <strong>Health</strong> care demands have<br />
been increasing over the past 50 years due<br />
to transitions in population structure<br />
(increasing old age population) and disease pattern (increasing life style<br />
diseases like Diabetes, Heart disease, hypertension, stroke, accidents and<br />
traumatic and emerging infections). The attitude and behavior of general<br />
population hence needs to be modified to maintain the public health gains.<br />
The present situation demands a need of new and innovative health<br />
communication strategies to communicate with the target audience, without<br />
which assuring people’s participation will be difficult.<br />
With the intention to have a healthy and well fit population, Radio<br />
<strong>Health</strong> is such an innovative Community <strong>Health</strong> Education and<br />
Communication model designed and produced by NRHM (<strong>National</strong> rural<br />
<strong>Health</strong> <strong>Mission</strong>) and initiated by Thiruvananthapuram district team of NRHM<br />
in collaboration with AIR<br />
Radio <strong>Health</strong> aims (i) to build up an innovative and comprehensive<br />
health literacy model through the medium of RADIO by assuring wider<br />
community participation for mass appeal (ii) to create awareness among the<br />
audience the importance of health and the need to lead the life as an healthy<br />
individual;(iii) to create a friendly and open atmosphere for audience<br />
interaction through innovative ideas; (iv) to create a positive change in the<br />
81
health habits and behavior of people (v) To ensure the idea/ message<br />
conveyed, reach every nook and corner to gain targeted feedback.<br />
Radio <strong>Health</strong> is the first ever concept<br />
of its kind of where FM Radio works as<br />
a medium for health literacy<br />
campaign. It will be the best platform<br />
to coordinate majority of <strong>Health</strong><br />
Practitioners ranging from Specialists<br />
Doctors to the peripheral health<br />
workers and Asha Workers. It will mainly focus on Primary <strong>Health</strong> Care and<br />
Preventive aspects of health by giving importance to all Medical Systems<br />
(AYUSH) and Alternate <strong>Health</strong> Practices. It is mission for solving health<br />
problems both physical and mental through interactive programmes by cocoordinating<br />
different agencies of <strong>Health</strong> Care System, NGO’s and Radio<br />
<strong>Health</strong> Clubs.<br />
Radio <strong>Health</strong> Clubs will be introduced in Schools, Colleges, Residential<br />
Associations, Cultural Groups etc. Radio <strong>Health</strong> Club members can function as<br />
RJs and Programme Producers. This concept will be an effective mode of<br />
propaganda for Radio <strong>Health</strong> as a whole.<br />
Radio <strong>Health</strong> has been launched on 25th September 2008. The<br />
Frequency of Transmission is 101.9 MHz; Ananthapuri FM .The transmission<br />
time is 3 to 3.30 pm, 4 days/week.<br />
Contents of the Programme is prepared under the direct supervision<br />
of Expert Doctors, Public <strong>Health</strong> Experts and executed by Creative persons<br />
and Radio <strong>Health</strong> Club Members. An approval committee has been<br />
constituted who will approve the programmes to be aired periodically.<br />
82
Standardizing <strong>Health</strong> Institutions:<br />
Ensuring quality services<br />
The background<br />
The Hospitals existing in Kerala under govt. services is not having a uniform<br />
pattern and the required minimum standards have not been clearly specified.<br />
This has created various types of regional imbalances in the availability of<br />
health care instituions, which invariably and adversely affects the availability<br />
of services in the backward districts /areas. In the absence of clear‐cut<br />
standardization criteria, systematic and uniform institutional development<br />
strategies have not been followed in the state. Based on some of the<br />
fundamental principles of Public <strong>Health</strong> Planning followed in the<br />
standardization committee report, the recently developed Indian public<br />
<strong>Health</strong> Standards (IPHS), giving due consideration to the special features of<br />
the public health scenario and institutional development pattern of Kerala, it<br />
has been decided to standardize health institutions coming under the <strong>Health</strong><br />
Services Department.<br />
The process<br />
As per the standardization process the institutions will be classified,<br />
based on the bed strength. Accordingly the Institutions will be classified as<br />
follows with the mentioned facilities and staff strength.<br />
83
i. Primary <strong>Health</strong> centers (PHC)<br />
Primary <strong>Health</strong> Centers are basically Grama panchayat level health<br />
Instituions intended for providing the basic promotive and preventive health<br />
care services including the implementation of the national and state level<br />
Public <strong>Health</strong> programmes along with minimum curative services. Though<br />
observation beds are provided in these institutions but elaborate in‐ patient<br />
care is not expected at this level.<br />
However, at present there are many PHCs (i.e. Panchayath level <strong>Health</strong><br />
instituions) having in patient services, Lab Services, Vehicles with driver etc.<br />
In these instituions existing pattern will be continued. But considering the<br />
fact that, the efforts for making the inpatient facilities into real functioning<br />
components in many of these institutions have repeatedly failed, if required<br />
the nonfunctioning sanctioned bed strength and additional staff created in<br />
some of these institutions may be transferred into other intuitions requiring<br />
additional staff and bed strength.<br />
Staff pattern.‐Minimum staff required<br />
1. Medical Officers 2 (Preferably one male and one female ‐ increased from<br />
existing one, the remaining 1 can be provided from NRHM till sanctioned<br />
posts are created)<br />
1. Pharmacist 1<br />
2. Staff nurse 3<br />
(increased from existing 1, the remaining 2 can be provided on contract basis<br />
with NRHM funding till sanctioned posts are created)<br />
3. Nursing Assistant 1<br />
4. Hosp. Attendant 1<br />
5. Part time sweeper 1<br />
84
Public <strong>Health</strong> wing<br />
One Junior Public health Nurse & Junior <strong>Health</strong> Inspector each for one sub<br />
Center (i.e. for 5000 Population in plains and for 3000 population in tribal and<br />
hilly areas.)<br />
One <strong>Health</strong> Inspector<br />
One Lady <strong>Health</strong> Inspector<br />
Office<br />
One LD/ UD Clerk<br />
One peon<br />
ii. Primary <strong>Health</strong> Centers with 24 Hr on call service (24x 7 PHCs).<br />
After upgrading the eligible Block PHCs into CHCs as per the<br />
standardization criteria, the remaining block PHCs with functioning in patient<br />
facilities along with other existing Mini PHCs with functioning IP facilities will<br />
be categorized as 24 Hr PHCs as per Indian Public <strong>Health</strong> Standard. One<br />
hospital in each block will be designated as 24 X 7 PHC and should have bed<br />
strength of up to 30.<br />
Staff strength:<br />
1. Medical Officers 4<br />
2. Pharmacist 2<br />
3. Lab Technician 2<br />
4. Staff nurse 9<br />
5. Nursing Assistant 3<br />
6. Hosp. Attendant 3<br />
7. Part time sweeper 2<br />
Preferably a vehicle, which can be taken by outsourcing<br />
85
Staff nurse and other category of staff is to be provided as per the existing<br />
bed strength and other facilities.<br />
The institution will have OPD services, emergency 24 X 7 services that<br />
could be attended by nurses and one Medical Officer. Well functioning HDCs,<br />
co‐location of AYUSH doctors, referral services, in‐patient services, minor<br />
surgeries, management of would and fracture, MCH care including FP<br />
services including facility for MTP, nutritional services, School <strong>Health</strong><br />
Programs, Monitoring & Supervision of <strong>National</strong> <strong>Health</strong> Programs including<br />
ASHA. Full laboratory facilities shall be available and availability of drugs &<br />
key diagnostic tests is to be ensured.<br />
iii. Community <strong>Health</strong> Centers (CHC)<br />
Community <strong>Health</strong> Centers are Block level <strong>Health</strong> care institutions<br />
providing basic Secondary Care <strong>Health</strong> Care services along with the planning,<br />
implementation and coordination of the public <strong>Health</strong> programmes at the<br />
Block level. There will be one community <strong>Health</strong> center each in all the <strong>Health</strong><br />
Blocks in the State. All the existing Block PHCs and the prevailing CHCs shall<br />
be renamed as Block CHCs. At present some of the CD blocks are not having a<br />
CHC .In such cases one block PHC/ Govt. Hospitals will be upgraded into CHC<br />
and with the support of GoI these centers along with presently existing CHCs<br />
shall be upgraded to Indian Public <strong>Health</strong> Standards (IPHS). In case if any of<br />
the CD blocks are currently having two CHCs, one of them shall be renamed<br />
as 24 hr PHC. The CHCs will have bed strength of 30 to 100 with theater<br />
facility, Laboratory, X‐ray, ECG, and Ultrasound<br />
Staff required<br />
Doctors –specialists (Junior Medical consultants) in General Medicine,<br />
General Surgery, Obstetrics & Gynecology, pediatrics, Anesthesiology<br />
86
Other non specialists (general category) based on the total bed strength.<br />
Paramedical staff and other staff based on the bed strength and other<br />
facilities available.<br />
Block level Public <strong>Health</strong> staff<br />
<strong>Health</strong> Supervisors 1<br />
Lady <strong>Health</strong> Supervisors 1<br />
Staff Nurse 12<br />
JPHN 2<br />
Pharmacist 2<br />
Lab Technician 2<br />
Radiographer<br />
Ophthalmic Assistant<br />
1 security<br />
Other ministerial posts as per norms<br />
The institution shall have proper waste management system, laundry<br />
facilities, full emergency services, shall have a minimum of 7 doctors and 1<br />
Block Coordinator cum PRO. The institution shall provide 24 X 7 services, shall<br />
have separate male and female wards, and shall provide emergency obstetric<br />
care including surgical interventions like caesarian section, new born care,<br />
emergency care of sick children, lapro services, MTP services, essential lab<br />
services, blood storage services and transport services. Shall have ECG<br />
facilities, X‐ray facility and preferably USS facility, shall have fully functional<br />
OT with surgical items. Minimum of two vehicles one especially<br />
administrative control over the PHCs and SCs, One statistical assistant as<br />
block will be the first level of monitoring / MIS. Minimum one computer with<br />
internet connection; shall have computerized pharmacy, training & skill<br />
development of PRIs, ASHAs, JPHNs, Nurses etc., fully functional HDCs,<br />
residential accommodation for the staff<br />
87
iv. Taluk Hospitals.<br />
There will be one Taluk Hospital each in all the taluks. Taluks, which are not<br />
having a Taluk Hospital, the biggest CHC/ Govt Hospital, will be upgraded as<br />
Taluk Hospital. In some places Taluk hospitals, which were previously<br />
designated as CHCs shall again be re‐designated as CHC, if that particular<br />
Taluk has got two Hospitals of taluk level status.<br />
Taluk Hospital will have minimum bed strength of 100. All the Taluk Head<br />
Quarters Hospital having more than 100 bed strength will continue to have<br />
the existing facilities and staff.<br />
v. District Hospital/General hospital<br />
There will be one District / General hospital in each district with<br />
minimum bed strength of 250.<br />
vi. Women & Children’s Hospital & specialty hospital.<br />
The existing Women and children’s hospitals will continue as Women &<br />
Children Hospital. The minimum bed strength of W&C will be 200, and the<br />
bed strength of W&Cs with less than 200 bed strength will be increased<br />
accordingly. Considering the fact that W &Cs are needed in every district for<br />
providing quality Maternal and Child <strong>Health</strong>, W &Cs will be started in all<br />
districts.<br />
Specialty hospitals of Mental <strong>Health</strong>, Leprosy and Tuberculosis will<br />
continue as specialty Hospitals. Strengthening and development of these<br />
Hospitals will be taken up in due course separately.<br />
88
Effective utilization of untied funds and<br />
Annual Maintenance Grants: with<br />
special focus on Malappuram<br />
Untied funds and Annual maintenance grants are a boon to many of<br />
the institutions, which had been reeling under shortage of resources. Many<br />
of the institutions are making the best use out of it Malappuram district has<br />
become a model on this.<br />
In terms of health indicators Malappuram is the backward district in<br />
the state of Kerala. The 2004 DLHS survey puts the district at 180th place.<br />
However visible changes are seen almost two years since the implementation<br />
of NRHM in the district. Malappuram is the district where the highest number<br />
of health institutions are there with 11 Community <strong>Health</strong> Centres, 88<br />
Primary <strong>Health</strong> Centres, 589 Subcentres and 5 Taluk Head Quarters Hospital.<br />
NRHM untied funds has become a boon to Malappuram as most of<br />
the institutions that were in a bad shape are getting a facelift because of<br />
NRHM funds. Innovative and patient friendly services were initiated using<br />
untied funds and maintenance grants.<br />
Some of the changes that were made using untied funds and annual<br />
maintenance grants are enlisted below:<br />
89
Token system in a PHC using untied funds<br />
Token system was introduced<br />
in a PHC called Chaliyar in<br />
Malappuram district owing to<br />
which a more systematic<br />
delivery of services could be<br />
put in place. This PHC situated<br />
in the tribal area caters to<br />
more than 250 patients every<br />
Before token system was introduced<br />
day. Seeing the success of this system the executive committee, district<br />
health and family welfare society has decided to scale up this system to more<br />
institutions.<br />
Improving facilities in subcentres<br />
Owing to improved facilities in subcentres, more<br />
Public <strong>Health</strong> Nurses are staying at the centres<br />
and giving services. Around 10% increase in the<br />
numbers of JPHN staying in the centres is noted<br />
Patients availing Token System<br />
90
Improving facilities at Sub Centres<br />
- Post Situation<br />
JPHN Attending a patient at a<br />
modified sub centre at Malappuram<br />
Well dug using WHSC Funds - a<br />
proud panchayat president<br />
standing beside<br />
IP Ward - Pre situation<br />
IP Ward - Post situation<br />
Water Purifier put in place<br />
Visiting Room with TV & IEC<br />
Materials<br />
91
<strong>Health</strong> Management Information System<br />
for Kerala State<br />
Events are taking place every day. Be it at <strong>Health</strong> or any department.<br />
The events so happened is to be recorded for our study and future reference<br />
, so that our planners can have a scientific and reliable study for formulating<br />
and implementing plan to evolve remedial and suitable measures to make<br />
our future safe. In olden days, the recording was only manual and there by a<br />
huge data collection and its analysis was simply not easy. Now we are living in<br />
a modern era and with most modern equipments in our hands. The<br />
computers can be of very useful and big and long data can be stored and<br />
analyzed so easily. This information will be the base in taking important<br />
policy matters pertaining to that subject.<br />
This is the background on which, health<br />
department decided to implement certain<br />
schemes and HISP is one among that. This<br />
is basically meant to record child and<br />
maternal activities, immunization,<br />
communicable diseases and record its movement.<br />
The <strong>Health</strong> Management<br />
Information System for reporting of<br />
Maternal and Child <strong>Health</strong> activities for<br />
the State of Kerala is being scaled up<br />
from Thiruvananthapuram district taken<br />
for pilot implementation and extended to<br />
remaining districts in the State. The scaling up will be effected in the HMIS<br />
92
formats customized to the<br />
requirements of the State<br />
adopting the HMIS Model and<br />
Toolkit by NHSRC and the<br />
project is rolled out in the State<br />
from October ’08 with<br />
technical support from NHSRC.<br />
The scaling up of HMIS implementation in Kerala is also entrusted to<br />
HISP, India, after the successful implementation of pilot by them for<br />
Thiruvananthapuram district. Arogyakeralam (NRHM), under the <strong>Health</strong> Dept<br />
will monitor the implementation.<br />
The salient and unique features of the project are:-<br />
The <strong>Health</strong> Information<br />
Systems Programme (HISP) software<br />
is developed on FOSS (Free & Open<br />
Source Software) in accordance with<br />
the State IT Policy was piloted in<br />
Thiruvananthapuram district in<br />
Kerala by HISP India who was<br />
entrusted the task of setting up<br />
computer supported HMIS in public health facilities – the District <strong>Health</strong><br />
Information Systems (DHIS) in 2005.<br />
HISP is provided with facilities for Data Management on Maternal &<br />
Child <strong>Health</strong> related activities, Immunization coverage, Communicable<br />
Diseases monitoring etc., generation of reports on same and various<br />
analyses. Provisions are also there in HISP to keep the collected data in order,<br />
93
in every respect, for future requirements. The data thus collected will be<br />
analyzed and used for planning and decision‐making purposes in the <strong>Health</strong><br />
sector.<br />
The HISP software has systematic provisions for organized entry,<br />
access, retrieval and management of data also facilitating automatic data<br />
consolidation and validation. Improved data quality coupled with enhanced<br />
scope of raw data to be processed for accurate information promises to be<br />
new and innovative for the State’s <strong>Health</strong> Sector.<br />
Vizhinjam PHC Map<br />
Antenatal, Delivery, Live Birth<br />
Oct 05 - Oct 06<br />
Vellar ANC= 45 :Delv=42 :Births=42<br />
M angalathukonam ANC= 33 :Delv= 30 :Birt hs= 30<br />
Katt ukulam ANC= 78 :Delv= 69 :Births= 69<br />
Peringamala ANC= 35 :Delv=31 :Births=31<br />
Muttakkad ANC= 25 :Delv= 24 :Births=20<br />
Venniyur ANC= 85 :Delv=70 :Births=70<br />
Kattachalkuzhi ANC= 60 :Delv=65 :Births=65<br />
Main Centre ANC= 53 :Delv=39 :Births=39<br />
Total Population<br />
43<br />
ANC<br />
Del<br />
LIBI<br />
1. The State wide implementation will be Web based and approximately<br />
1,215 health facilities in the State including all PHCs, CHCs, District Hospitals,<br />
Government Hospitals, General Hospitals, W & C Hospitals, Medical Colleges,<br />
Taluk Hospitals and Specialty hospitals will be uploaded to the web for data<br />
entry and management in customized formats collecting and processing data<br />
from all institutions up to peripheral Sub Centres and even Private health<br />
facilities.<br />
94
The computers installed in all the <strong>Health</strong> Institutions over the State<br />
will be connected to the Server proposed to collocate at the Data Centre of<br />
the State through Kerala State Wide Area Network (KSWAN) / Broad band<br />
Vizhinjam PHC Map<br />
% Full Immunization<br />
Oct 05 - Oct 06<br />
Vellar 105%<br />
Kattukulam 94%<br />
M angalat hukonam 100%<br />
Peringamala 106%<br />
Muttakkad 170%<br />
Venniyur 89%<br />
Kattachalkuzhi 98%<br />
Main Centre 110%<br />
Total Population<br />
fullimm<br />
89<br />
90 - 94<br />
95 - 100<br />
101 - 110<br />
111 - 170<br />
connection of BSNL. The data will be collected to the Central Server on‐line.<br />
Capacity building of the Staff at different levels of <strong>Health</strong> Dept will be<br />
a by product of HISP implementation. The programme mainly focuses on<br />
equipping all levels of <strong>Health</strong> staff to enter and manage the application<br />
through intensive trainings across the State. Nearly 12,000 staff belonging to<br />
<strong>Health</strong> department will be trained under the programme.<br />
Serving as an effective MIS tool, HISP proposes to collect vital inputs<br />
from a variety of health units reporting for Maternal and Child <strong>Health</strong><br />
activities and IDSP to present raw data and mainly covert the same into<br />
processed formats for information.<br />
HISP is set to change the face of data reporting in State’s <strong>Health</strong><br />
Sector as we switch to digital reporting and management of <strong>Health</strong> related<br />
data for better information. Getting equipped the <strong>Health</strong> facilities and<br />
personnel for managing the data as web application through large scale<br />
95
trainings covering a spectrum of resources is also a matter of pride to the<br />
State. Ultimately, making use of the same for better monitoring, planning and<br />
decision make will prove vital for development of the State.<br />
The project is expected to finish by 2010.<br />
96
School <strong>Health</strong> Programme<br />
Kerala is the most literate state in India there by the emphasis on<br />
school health is immense since<br />
most of the children attend<br />
school till 12th standard unlike<br />
other states. These students<br />
carry lot of information to their<br />
home and families situated even<br />
in the far‐flung areas. Now,<br />
NRHM has taken a step ahead in<br />
bringing these children under one<br />
net: that is “School <strong>Health</strong><br />
Programme”. It is known to all<br />
that today’s children are<br />
tomorrow’s citizen and their<br />
health is paramount concern of<br />
any welfare State. The selected schools will be tested with the first doze of<br />
this scheme by this year and in the coming years; entire schools of the state<br />
will be brought under this umbrella.<br />
There are 14000 government and Aided schools in Kerala including<br />
higher secondary and VHSS with around 50lakh students. No doubt, it is a<br />
massive programme, by which these huge populations get hands on<br />
information on health and hygiene and its necessity. This will reflect in the<br />
future years and they will easily cooperate in building up a better and healthy<br />
NATION. The students spend, twelve years in schools and a continuous<br />
pouring of information on <strong>Health</strong> and Hygiene is going to reflect in their way<br />
97
of life. And this is definitely a good media rather than spending much on<br />
other media. Similarly focus on the health of the students’ at school will<br />
finally yield a healthy, well‐informed and productive generation. The<br />
academic performance of the<br />
children, which is the main focus of<br />
the school authorities, will also<br />
improve and show considerable<br />
changes when the both physical<br />
and mental health of the students<br />
and their coping up skills during<br />
stress is enhanced.<br />
Keeping the above<br />
objective in mind the <strong>National</strong><br />
<strong>Rural</strong> <strong>Health</strong> <strong>Mission</strong> Under the<br />
<strong>Health</strong> Department has joined<br />
hands with the Education<br />
Department in chalking out a School health Programme aiming at the<br />
comprehensive growth and well being of students for a better, well informed<br />
and healthy generation. The stepping‐stone for achieving this goal was on<br />
December 1st 2007 at the Cotton Hill Girls Higher Secondary School<br />
Thiruvananthapuram.<br />
The school health clinic, the first of its kind, was set up at one of the<br />
largest girls’ school in Asia namely Cotton Hill Girls Higher Secondary school<br />
on the 1st of December 2007 and is functioning extremely well with a full<br />
time Doctor and a staff nurse. There has been a tremendous positive<br />
response from the students, teachers and the PTA of the school since a lot of<br />
time and energy and manpower were being wasted for taking children who<br />
are ill to the nearest medical institution.<br />
The main objectives of the School <strong>Health</strong> Programme are<br />
98
Clinical examination: The<br />
primary, preventive and<br />
minor clinical problems are<br />
dealt and referred as per<br />
need by a full time<br />
dedicated JPHN (ANM)<br />
appointed for 5 schools<br />
each. A <strong>Health</strong> Calendar<br />
with a chart will be set up<br />
in each class to know at a<br />
glance the absenteeism<br />
due to illness.<br />
Counseling: The services of a clinical psychologist/ MSW are present<br />
at regular intervals in a month for general and specific counseling<br />
according to the need. Both Individual and Group counseling would be<br />
conducted. The children needing counseling at individual level will be<br />
decided on voluntary basis and through the recommendation of the<br />
Class Teacher or JPHN.<br />
<strong>Health</strong> education to the students is conveyed by setting up of health<br />
information charts, placing an anonymous question box and health<br />
messages placed and rotated per class. Frequently asked questions<br />
would be compiled at the end of one year to prepare a booklet so that<br />
it will be useful for the other students. Students deliver a health<br />
message daily after the prayer in the school assembly as “<strong>Health</strong><br />
thought of the day”. Taking into consideration an average of 35 weeks<br />
of school 35 health messages will be printed and hung at the class<br />
room. One message per week to be circulated in each class on a<br />
rotation basis so that it is most cost effective. A question box will be<br />
placed in all schools for children to clear their doubts on any topics<br />
99
without mentioning their name. The box will be opened once a week<br />
and the answers to the questions will be compiled and put up on the<br />
notice board. The box will be placed in the school <strong>Health</strong> Club.<br />
<br />
<br />
Involvement of the parents and teachers: Classes on parenting,<br />
support during academic backwardness in children, organizing<br />
interactive sessions in the class with parents of the students from<br />
different professions during which they will not only tell about their<br />
professions but will also highlight the health risks they face due to<br />
their profession and what steps can be taken to prevent them. This<br />
has a three fold advantage like the students get an orientation about<br />
that profession i.e. career guidance, and to know the health problems<br />
related to a profession and how to prevent it. In addition, a sense of<br />
ownership develops among the parents when they address their own<br />
children’s class. The parents and teachers will also benefit during the<br />
Medical Camps held in the schools twice a year.<br />
Comprehensive health database of students: Formulating a health<br />
database of each and every student of the school with updated<br />
information on their comprehensive health. The new and innovative<br />
“School‐ TC & <strong>Health</strong> Record” is introduced by the “Arogyakeralam”<br />
(NRHM), Department of <strong>Health</strong>, Government of Kerala, for the overall<br />
physical, mental and social health development of school children.<br />
Information regarding the comprehensive health of the student is<br />
noted in this Record. The programme is named ‘‐2 to +2’ as it is meant<br />
for children from Pre‐Primary (LKG) to the Higher Secondary levels<br />
(Plus Two). This is also an authentic Transfer Certificate (TC) because<br />
the TC is a part of the <strong>Health</strong> Record. The Conduct Certificate is also<br />
included in the ““School‐ TC & <strong>Health</strong> Record.”<br />
100
This Record is an authentic and comprehensive one covering general<br />
information, health details of the child and members of his/her family, details<br />
of fitness program, TC & conduct certificate, extracurricular achievements<br />
and List of free text books. This <strong>Health</strong> record is jointly brought out by the<br />
Departments of <strong>Health</strong> and NRHM, Education, Local Self Government and<br />
Sports & Youth Affairs with the active participation and support of Parent‐<br />
Teachers’ organizations. As ‘Prevention is better than cure,’ it is best, if<br />
children are made to imbibe healthy habits and attitudes at an early age,<br />
which would help them later in their lives as well. Many of the diseases can<br />
be cured completely if they are diagnosed and treated in the initial stages.<br />
This may prevent its spread& progress, minimizing treatment expenditure<br />
and reducing absenteeism of the students from schools and parents from<br />
their offices.<br />
This <strong>Health</strong> Record is filled and maintained in schools. Every child will<br />
undergo a Primary <strong>Health</strong> examination and screening once a year and those<br />
who require further medical treatment will be referred to specialized doctors<br />
in the special medical camps. The details of students who require further<br />
investigations and treatment is promptly entered in the <strong>Health</strong> Record and<br />
sent for specialized treatment to referral hospitals along with their parents<br />
through a referral card.<br />
The introduction of “School ‐TC & <strong>Health</strong> Record” is a very significant<br />
step by the State’s <strong>Health</strong> sector and first of its kind in the country. This<br />
programme is initially introduced in selected Government and Aided schools<br />
in the State and will be scaled up in the coming years.<br />
<br />
Monthly reports will be compiled by the JPHN and submitted to DPM<br />
with copy to head office. This data may be used for research.<br />
Frequently asked questions of the students would be compiled every<br />
6months ‐1yr as small booklets “FAQs of students in schools”. <strong>Health</strong><br />
education classes and messages circulated can also be compiled at the<br />
year‐end as a school health booklet for students, teachers and<br />
101
parents. The database from each district will be compiled centrally<br />
and maintained as a comprehensive health profile of all Government<br />
school going children in the State. The district school health<br />
programme would be jointly monitored by the District Programme<br />
manager, Block medical Officer in charge and District medical Officer.<br />
Keeping the above objectives in mind the school health programme<br />
has been chalked out for all districts covering 1 school per<br />
panchayath/municipality/corporation. In this phase, covering 1100schools in<br />
the first pilot phase option to the local self‐government to fund the same<br />
program in another school in the same panchayath.<br />
The school health Team is planned under the Medical Officer of the<br />
Block CHC or PHC or Taluk Hospital nearest to the school and the team<br />
includes<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<strong>Health</strong> Supervisor<br />
Lady <strong>Health</strong> Supervisor<br />
<strong>Health</strong> Inspector<br />
Lady <strong>Health</strong> Inspector<br />
Junior <strong>Health</strong> Inspector<br />
Junior Public <strong>Health</strong> Nurse<br />
Block Arogya coordinator<br />
Ophthalmic Assistant<br />
Teacher Coordinator / Teacher counselor (Male/Female)<br />
PTA representative<br />
ASHA/AWW<br />
Dental Hygienist<br />
Fitness coordinator<br />
The school health team will visit the selected schools at regular intervals and<br />
would assist the JPHN and school authorities in conducting the <strong>Health</strong><br />
education Classes, Observance of health Days and Medical Camps. The School<br />
health Team will assist in promoting immunization program, facilitate blood<br />
group checking, measure height, weight, BMI and physical & psychological<br />
health status, re‐organization of school health clubs, conduct referral services<br />
and propagation of health message. <strong>Health</strong> Education classes in the schools<br />
102
and data analysis and compiling with monthly reports to the block<br />
coordinator/CHC Medical Officer In‐charge/DPM.<br />
A full time dedicated JPHN will be appointed for 5schools to facilitate<br />
all the school health activities namely planned health check‐up one day per<br />
week of the selected school, promotion of immunization program, facilitating<br />
blood group checking, measuring height, weight, BMI and physical &<br />
psychological health status using screening questionnaire to be filled by<br />
respective class‐teachers, re‐organization of school health clubs, referral<br />
services and propagation of health message in the schools. One JPHN in<br />
charge of 5 schools in an area and will visit each school once per week.<br />
Medical Camps<br />
One screening camp by the JPHN and a lady Doctor in July followed by a<br />
special medical camp in December/ January including specialist doctors will<br />
be conducted in each selected school. Organizations like Indian academy of<br />
Paediatrics, Indian Medical Association, Indian Dental Association and<br />
Federation of Obstetrics and Gynecologic Society of India have partnered in<br />
the program for health education and health check up of the students free of<br />
cost. Counseling services will be made available according to the need by<br />
hiring a counsellor and also making use of the counselors being hired under<br />
the education department. The disability‐trained teachers of Sarva Siksha<br />
Abhayaan will also be trained in this programme for their contribution in<br />
screening the students. The Block Resource Centre of SSA will be utilized for<br />
further follow up of students with problems along with their parents. Referral<br />
services from the school to the local health facility and follow up counseling<br />
when needed will be provided.<br />
103
Activities planned for 2008-09<br />
Printing of School – TC & <strong>Health</strong> Card<br />
Printing of health education posters and calendars<br />
Appointment of JPHNs (1JPHN/5 schools, 220 JPHNs for 1100 schools)<br />
Identification of schools 1per panchayath/nagarasabha totally to 1100<br />
schools and list of selected schools from Education Department.<br />
GO from education department to the schools for cooperation with<br />
the programme.<br />
Joint meeting of the <strong>Health</strong> and Education departments.<br />
Formal inauguration of the programme with launching of the <strong>Health</strong><br />
Card<br />
Signing of letters with IAP, IMA, IDA and FOGSI.<br />
Development of training modules.<br />
Identification of school health MOs and formation of school health<br />
team.<br />
Training of JPHNs, Teachers, School health team, ASHAs, Block Arogya<br />
Coordinators based on modules developed.<br />
Development of annual schedule of weekly visits, screening and<br />
health education classes in consultation with the school authorities.<br />
Distribution of <strong>Health</strong> Cards/Calendars/<strong>Health</strong> messages to the<br />
selected schools and monitoring to see that all cards are filled<br />
according to the guidelines<br />
Revival of the <strong>Health</strong> clubs of the schools<br />
Regular and timely health education classes in schools selected<br />
initiated by the JPHN/School health Team with involvement of parents<br />
& teachers<br />
Regular monitoring by Block Arogya Coordinators and quarterly field<br />
visits by the DPMs/RCH Officers/ State officers<br />
The cooperation from the Education Department is:<br />
Government Order from Education departments issued to all<br />
schools<br />
o Assign one period per week for health Education Classes<br />
o Conduct 2 camps‐ 1 screening and 1 special medical camp in school<br />
in one academic year<br />
o Have the active cooperation of the PTA and management<br />
o Revive the health Clubs in schools<br />
o Provide space for counseling and to conduct health education<br />
classes<br />
104
o Provide all support and cooperation to the JPHN assigned and the<br />
school health Team<br />
o Make provision for the JPHN and Medical Officer to sign<br />
attendance in a special attendance register maintained at the<br />
Principal’s office<br />
o Allow JPHN the use of the computer at school for maintaining data<br />
and records and reporting.<br />
Maintenance of health cards and other IEC materials provided to<br />
the school<br />
The disability trained teachers to be trained in School <strong>Health</strong><br />
Programme<br />
To approve the utilization of the Block Resource Centre for<br />
programmes under the School health programme<br />
Cooperation from DPI & DHSE in owning the programme along with<br />
<strong>Health</strong> Department<br />
This School <strong>Health</strong> Programme is a unique programme and first of its<br />
kind focusing on inculcating healthy attitudes and habits in the future<br />
generation “Catching Them Young” by making health a part of their<br />
curriculum. The schools are a medium to reach the whole society through the<br />
students and their families. School <strong>Health</strong> programme not only encompasses<br />
the comprehensive health and academic growth of the students but also<br />
focuses on public health issues like environmental sanitation, source<br />
reduction activities and in general a healthy lifestyle for the general<br />
population. We look forward to a healthier and vibrant Kerala through this<br />
programme.<br />
105
Geospatial <strong>Rural</strong> <strong>Health</strong> Information<br />
System for Kerala State (G-RHIS)<br />
Geospatial <strong>Rural</strong> <strong>Health</strong> Information System (G‐RHIS) is being developed for<br />
<strong>Health</strong> & Family Welfare Department and Arogyakeralam with a view to<br />
enhance efficiency in health services delivery at various levels especially<br />
peripheral areas to enable monitoring of services, identification of gaps and<br />
decision making.<br />
The G‐RHIS is developed in a Geographic Information Systems platform with<br />
Spatial Information on all government <strong>Health</strong> Institutions in the State. The<br />
web enabled query G‐RHIS will provide spatial information on the locations of<br />
1,274 <strong>Health</strong> Institutions including PHCs, BPHCs, CHCs, District hospitals,<br />
Government hospitals, General hospitals, Specialty hospitals, W and C<br />
hospitals, Medical Colleges, and others and also approx. 5,500 Sub Centres in<br />
Kerala.<br />
Spatial themes on Administrative Boundaries, road and drainage networks,<br />
places developed in GIS will be provided in the software.<br />
Advantages of G-RHIS<br />
• The software will facilitate query and identification to provide spatial<br />
and non spatial information of the basic details of <strong>Health</strong> Institution,<br />
availability of medical, paramedical and other staff, hospital facilities,<br />
equipments and various services.<br />
• Facilitate spatial information on the allocation and availability of<br />
Community Functionaries under NRHM viz Accredited Social <strong>Health</strong><br />
106
Activist (ASHA), Junior Public <strong>Health</strong> Nurse (JPHN) and Anganwadi<br />
workers (AWW) along with the names, addresses and phone.<br />
• It will also enable Spatial monitoring of the performance of various<br />
State and <strong>National</strong> <strong>Health</strong> Programmes (<strong>National</strong> Blindness Control<br />
Programme, <strong>National</strong> Leprosy Eradication Programme, RNTCP, Iodine<br />
Deficiency Diseases Control Programme, FW Programme, NVBDCP,<br />
Universal Immunization Programme, Malaria Control Programme) at<br />
Institutional and area levels with respect to area, population and<br />
time.<br />
• Provide spatial query and information on trends in occurrence of<br />
Communicable diseases with respect to area, population and time.<br />
• Facilitate spatial information on generation of Panchayat <strong>Health</strong><br />
Plans, District Action Plans, Ward <strong>Health</strong> and Sanitation Committees,<br />
Hospital Management Committees.<br />
• Facilitate spatial information on Fund allocation to Sub centres and<br />
expenditure with respect to time and purpose.<br />
• Facilitate spatial information on JSY, amount handed over by hospitals<br />
to various categories of beneficiaries.<br />
• Provide Routing information to <strong>Health</strong> Institutions.<br />
• The GRHIS software will also provide analytical information in<br />
graphical format besides spatial and non spatial reports all of which<br />
can be printed for use.<br />
• The software is also provided with Zoom‐in, Zoom‐out, Pan, Identify<br />
functions.<br />
Plan for Uploading And Data Entry<br />
All health institutions in the State except Sub centres will be uploaded to<br />
access the G‐RHIS software and data entry will be done at institutional level.<br />
107
Present Status<br />
• 5,250 <strong>Health</strong> Institutions covering eleven districts in the State are<br />
mapped using GPS. Palakkad, Kasargode and Wayanad districts are<br />
being mapped.<br />
• Data structure designing of GRHIS software is completed.<br />
• Data coding is in progress.<br />
• First version of Software to be ready by December 2008<br />
The implementation of G‐RHIS in the State will revolutionize planning and<br />
decision making in <strong>Health</strong> Sector using Geospatial Technology through<br />
effective performance monitoring of all <strong>Health</strong> institutions and <strong>Health</strong><br />
programmes, facilitating allocation of resources and personnel and various<br />
Epidemiological analysis.<br />
108
Information Technology<br />
More than a dozen Scheme/ Programme/ Projects in <strong>Health</strong> and Family<br />
Welfare Dept in Kerala are backed with Information Technology. They are<br />
HISP, SPARK, MESSAGE, IDEAS, Video Conference, IHMS, School <strong>Health</strong>,<br />
RSBY, Tele Medicines,<br />
Keralam Website ,etc<br />
Video Conference, Geo‐ spatial <strong>Rural</strong> HIS, Aarogya<br />
The innovative programmes under the H&FW Dept are explained below<br />
1. Arogyakeralam Website<br />
This Exclusive website is developed for publishing information about the<br />
health and social welfare activities of Govt of Kerala. The website developed<br />
by M/S <strong>National</strong> Informatic Center(NIC) was recently converted to FOSS (Free<br />
Open Source Software) as per State’ IT Policy. In order to have a<br />
decentralized content Generation, NRHM opted CMD (Content Management<br />
Frame work). This enables content generation at any levels of scheme/<br />
project implementation. The content after its approval can be uploaded to<br />
the site by the generated staff itself, but with access permission of the<br />
administrator. A state owned IT organization, C‐DIT is the agency identified<br />
for the training and support the website<br />
2. SPARK (Service and Payroll Administrative<br />
Repository for Kerala)<br />
SPARK is a web based application software developed by NIC under IT Dept<br />
for the whole State for the Management of Payroll, Human Resources and<br />
109
Other payments, of government employees. The monthly routine work, the<br />
salary bill preparation is made simple through SPARK.<br />
Digitization of Service book is the first phase of SPARK<br />
implementation. This is done with help of the Govt Organisation, Keltron, in<br />
<strong>Health</strong> and Family welfare dept.<br />
In H& FW, 23000 out of the 45000 service books have been digitized.<br />
Implementation work is progressing in association with State IT Dept &<br />
expected to finish before December 2008<br />
Infrastructure development, such as installation of Computers,<br />
Printers, Connectivity, Network & power wiring in about 2000 health<br />
institution is the biggest task connected to implementation of SPARK. Giving<br />
training to all the Self Drawing Officers and staffs in establishment section is<br />
the next biggest task.<br />
SPARK is integrated with TIS (Treasury Information Software) aiming to e‐<br />
transaction of salary and other payments.<br />
3. MESSAGE (Modern Electronic Systems and Services<br />
Agility & Governance in Enterprises)<br />
MESSAGE is a web based application developed by NIC for state IT Dept , for<br />
Less‐ paper, Electronic file flow management for Govt Offices. This<br />
Transparent file management , as it is web based broaden access to the<br />
office work. Any time /anywhere file processing results fast file movement.<br />
Searching for the file usually result time loss. The file search and Monitoring<br />
made simple in MESSAGE. Public search is also possible which support Right<br />
to Information rules.<br />
Training to staff is over, and NRHM is waiting for the action of IT <strong>Mission</strong> for<br />
implementation of MESSAGE.<br />
110
4. IDEAS (Information and Data Exchange Advanced<br />
System)<br />
IDEAS aims the Service Delivery to Citizen. This Web based application<br />
gives information about the file status to staff and public through web<br />
search. It contains modules such as tapal entry, file transit, meeting<br />
management etc.<br />
IDEAS is implemented in <strong>Health</strong> and Family Welfare Dept in Govt<br />
Secretariat and running in full swing. As it runs in other Govt Depts also the<br />
file follow up became easy. Provision to register the file no enables delivery<br />
of file status through e‐mail and SMS at free of cost.<br />
5. IHMS (Internal Hospital Management System)<br />
IHMS is an application software for management of information within the<br />
Hospital like OP& IP management, generating history of treatment,<br />
communicable diseases, etc. It is implemented and running successfully in<br />
Trivandrum Medical College and will be replicated in all other Medical<br />
Colleges and major hospitals, subject to approval of Govt.<br />
6.RSBY (Rashtriya Swastic Bima Yojana)<br />
The Scheme envisages better health coverage to the public, especially the<br />
BPL citizen. It enable freedom to patient to approach any empanelled<br />
Hospitals, including Govt Hospital, for better treatment. Cashless treatment,<br />
Smart Card based operation, etc are envisaged in the scheme.<br />
111
Software package for managing the insurance part, at Hospital level is under<br />
Development . Bonus of the scheme is that Govt Hospital facility needs to be<br />
upgraded to bring them to IPHS Standard for empanelment.<br />
5. AASTHI<br />
It is a Web based inventory management information system, which target to<br />
maintain the statewide IT inventories. Hardware and OS (Operating Software)<br />
protection is the added advantage of the programme. Preparation of<br />
installation and commissioning certificate, fault reporting , etc are the<br />
modules available with the software. <strong>Health</strong> dept will implement it in<br />
association with the IT Dept.<br />
6. Video Conference facility<br />
Conferences and meetings are necessity of the department like H&FW,<br />
handling sensitive areas related to <strong>Health</strong> services. In order to minimize the<br />
strain and cost in participating and conducting the meetings/ conferences,<br />
Video Conference Facility is a solution. NRHM took the initiatives to connect<br />
all the District Centres through Video Conference Facility. Equipments are<br />
ISDN based also so that worldwide conference will be possible.<br />
One Centre set up at ' XANADU ' Trivandrum and another Centre is under<br />
set up at Kerala NRHM HQ. Centres under NRHM will be linked with the<br />
existing state facility under IT Dept<br />
The VC Facility could support Tele Medicine also.<br />
112
Three Dimensional Interactive Digital<br />
Anatomy: 3 D INDIANA – An NRHM Initiative<br />
Background<br />
Towards making MBBS studies more interactive and practical oriented<br />
NRHM is now contemplating on putting into use three dimensional<br />
interactive digital anatomy model software which has been developed by a<br />
doctor at an Alappuzha clinic, Jerome Kalister, has with the help of a 15<br />
member team. This software has been approved by Anatomical Society of<br />
India. This software has been submitted before Medical Council of India.<br />
3 D Indiana, an interactive digital anatomy model of the human body,<br />
could help Medical students. 3D Indiana is an anatomy aid to medicos not a<br />
substitute for a cadaver. Indiana, an acronym for<br />
interactive digital anatomy, will help the user<br />
navigate the inside of the virtual human body and<br />
study internal organs, their location,<br />
interconnection, size and texture.<br />
Headed by Kalister, a team of medical<br />
experts, software engineers and structural<br />
engineers has been working on the project for<br />
years, using 10 computer systems. Presently<br />
students get to see a cadaver in the first year of<br />
MBBS only. Second and third year, there’s only a<br />
fleeting glance because the specimen would have<br />
been dismembered in the first year itself. So<br />
113
medicos spend hours with diagrams and pictures instead of a cadaver. 3D<br />
Indiana is a replica of the human with every organ, bone, muscle, nerve and<br />
blood vessel. 3D Indiana will really help medical students, doctors, surgeons,<br />
medical researchers.<br />
Specialties of 3D Indiana<br />
In this software each and every structure in the human body is<br />
digitally sculpted and deployed in its true anatomical<br />
positions, based on CTs, MRIs, real time dissections<br />
and authentic text books. As per the brochure of the<br />
software, 3 D Indiana is a fully navigable and<br />
delightfully user‐friendly 3D environment lets the user<br />
cruise amongst the rich details of the body. Every<br />
structure is constructed with its ultimate details and<br />
can be rotated, hidden, zoomed, made transparent,<br />
grouped and viewed in either their systemic or<br />
regional<br />
orientations.<br />
To begin with, this virtual interactive medium of the human body is<br />
one of a kind in the arena of modern day, medical teaching aids marked by its<br />
sophisticated and state of art character.<br />
It offers a multidimensional view of the remotest of areas of the<br />
human anatomical framework, equipped to zoom in on the smallest of<br />
114
structure with precision and clarity. Richly detailed, visually resplendent,<br />
anatomically precise and spatially accurate, it affords the most<br />
comprehensive insight into the human body.<br />
At the undergraduate level, emphasis is on dissecting on real cadavers<br />
considering that the sight, smell, touch and feel of real bodies, their various<br />
organs, bones, cartilages and other structure is very much integral and<br />
fundamental to the learning of the human body. This software would be<br />
useful as a complementary learning tool for undergraduates considering the<br />
visual impact & possibilities of the software.<br />
As the software presupposes that the user should have a prior<br />
thorough understanding of human anatomy, which in fact can only be<br />
accrued through meticulous real time dissections on the cadaver, it could<br />
serve as an excellent aid for research and advanced learning.<br />
<br />
3 D INDIANA in its basic form is an ultimate reference in anatomy. It is<br />
a powerful tool in teaching and leaning anatomy. It presents itself as a<br />
fully navigable full body where each and every structure in the body is<br />
oriented in its true anatomical position.<br />
<br />
Virtual surgical with a game engine added it can be used to stimulate<br />
and give training on any surgical procedure.<br />
<br />
With a little programming normal body responses could be elicited<br />
from the virtual body hopefully enabling clinical trials of drugs and<br />
chemicals in it.<br />
115
The evolution of pathological process and body response to it can be<br />
programme into 3 D Indiana.<br />
<br />
Animated surgeries – hundreds of surgical procedures may be<br />
simulated by animation on the 3d Indiana.<br />
<br />
Combined with volumetric anatomy (a new concept in anatomy,<br />
proposed by 3dindiana team, that gives a mathematical system of<br />
location of each and every point in the 3d volume of the body‐refer<br />
www.volumetricanatomy.com) it becomes an extremely accurate<br />
virtual body from which measurements could be taken and be used<br />
for multitudes of research purposes including planning of new surgical<br />
access etc., etc.<br />
<br />
3D Interactive Digital Anatomy is a scientifically accurate and<br />
artistically perfect 3D rendition of the human body in its ultimate<br />
detail. It is the most detailed and delightfully user friendly software<br />
designed for assisting the study, teaching and research on human<br />
anatomy. Every named structure in the body is digitally sculpted in its<br />
richest details and deployed in their true anatomical positions in the<br />
body based on CTs, MRIs real time dissections and authentic text<br />
books.<br />
<br />
Touch any structure with the mouse, its name is displayed then and<br />
there. It can be isolated, zoomed, rotated so as to peruse it from any<br />
angle. It can be grouped with any number of structures to view their<br />
inter‐relations. Any one of them may be made transparent so that the<br />
structures underneath is visible through.<br />
116
It lets you take any number of sections in any plane of your fancy. Any<br />
piece can be disarticulated and put back fro any number of times. And<br />
of course it is a fat free; yielding itself to a clutter less, clear view of<br />
even the smallest structure.<br />
<br />
The programmed index and annotations are quite cool. A user may<br />
cruise amongst the various structures in the fully navigable body or<br />
may follow a dissection mode that guides him through the minute<br />
details<br />
Putting the software into effective use<br />
Sensing the importance of concept, after detailed deliberations with<br />
the team who developed this, NRHM suggested the introduction of the<br />
software in the Government Medical Colleges which could be introduced as a<br />
trial in a medical college before the Medical Council of India approves it for<br />
use in colleges throughout the country. A demonstration of the software has<br />
been held at Medical College, Alappuzha. The field study of 3D Indiana Digital<br />
interactive software, a unique creation by Dr. Jerome Kalister was held in the<br />
presence of experts from the discipline of Anatomy. The NRHM has<br />
constituted a committee which is now contemplating on distributing the<br />
software to all Medical Colleges based on the field study report. The<br />
committee will negotiate with the software company for supplying it at a<br />
subsidized rate for the Government medical colleges.<br />
117
COMPULSORY RURAL SERVICE:<br />
BRIDGING CRITICAL GAP IN<br />
MANPOWER: DIFFICULT RURAL<br />
AREA ALLOWANCES<br />
Background<br />
From the year 1998 onwards, a provision has been incorporated in<br />
the prospectus for admission to the MBBS course to the effect that those<br />
students who successfully complete MBBS course from Govt. Medical<br />
Colleges in Kerala are liable to serve in rural areas for a period of 3 years, if<br />
required by the govt. In the prospectus it is further stipulated that out of the<br />
3 years, one year service should be in Difficult <strong>Rural</strong> Areas. Likewise, from<br />
the year 2004 onwards the prospectus for admission to the Medical PG<br />
course specifies that those students who successfully complete PG course<br />
from Government Medical Colleges other than the All India Quota and<br />
Government service doctors are liable to serve <strong>Health</strong> Services / Medical<br />
Education Services for a period of 2 years, if required by the Government.<br />
Clause XII (c) provision of prospectus for Admission to Medical PG Degree/<br />
DNB/ Diploma courses 2004 stipulates that the applicants selected to PG<br />
course will have to execute a bond at the time of joining the course to the<br />
effect that they will serve the Government for 2 years after completion of the<br />
course, if the Government requires so.<br />
Towards bridging the critical gap<br />
While the availability of medical personnel was an easy process in<br />
some districts, the same was a laborious one in some backward districts.<br />
Consequently, the Government decided to invoke the clause of compulsory<br />
rural services from the year 2007 onwards for doctors studying the various<br />
118
government Medical Colleges in the State. They were appointed in various<br />
health care institutions in the state with priority to backward districts. MBBS<br />
doctors have to serve in health care institutions for a period of 1 year, PG<br />
diploma doctors to serve for 1 year and PG Degree doctors for two years.<br />
Even though objections were raised from several quarters on the compulsory<br />
rural service, the government was assertive in providing medical care to the<br />
rural poor especially backward districts. Government ensured that all the<br />
doctors worked in the health institutions for the prescribed period.<br />
Later, government based on various orders decided to extend the<br />
conditions of compulsory rural services to doctors who passed out from self<br />
financing colleges and cooperative medical colleges in government seats, All<br />
India Quota candidates etc.<br />
Outcome<br />
The best possible outcomes as a result of appointment of doctors are<br />
summarized as follows.<br />
v. More institutions provided with 24 X 7<br />
services<br />
vi. OP increased<br />
400000<br />
350000<br />
300000<br />
Increase in O.P<br />
vii.<br />
OP time in selected institutions extended<br />
from 8 AM to 8 PM.<br />
250000<br />
200000<br />
150000<br />
No:s.<br />
viii.<br />
Increase of deliveries as a result of increase<br />
of patients from private to Government<br />
health care institutions<br />
100000<br />
50000<br />
0<br />
2005-06 2006-07 2007-08<br />
In addition, very few specialists are working in<br />
Medical Colleges on bonded obligation under NRHM.<br />
Increased O.P in Peripheral hospitals owing to increased manpower<br />
119
This scheme not only bridged the critical gap but also ensured that all<br />
the MBBS students are given a chance to work in the Government Hospitals<br />
to test and experienced their knowledge acquired from the colleges. NRHM<br />
is offering a pay package of Rs. 15000/‐ for compulsory rural service and Rs.<br />
20,000/‐ to those who are posted to Difficult to <strong>Rural</strong> Areas.<br />
Call allowance<br />
Apart from this Government specialists will be eligible for call allowance<br />
between 8 PM to 8 AM (subject to certain terms and conditions) for<br />
rendering additional work during night hours while NOT on call duty as<br />
detailed below.<br />
For each call Rs.100<br />
For Gynecologist Rs.200 – Normal delivery<br />
Rs.500 – Assisted delivery<br />
Rs.1000 – Cesarean section / Emergency<br />
hysterotomy/hysterctomy<br />
For Surgeon / Ophthalmic / ENT / Ortho<br />
Rs.200 – minor surgeries<br />
Rs.500 – Major surgeries<br />
For Anesthetist Rs.1000 per case for general & spinal anaesthesia and<br />
long procedures<br />
Rs.500 for minor procedures under block anaesthesia<br />
However, Government Doctors can be appointed on additional shift duty<br />
(3 PM to 8 PM and 8 PM to 8 AM) if there is absolute necessity. This is to be<br />
decided by a committee consisting of District Medical Officer (<strong>Health</strong>), RCH<br />
Officer and District Program Manager based on request from the local<br />
Panchayat.<br />
120
The details of doctors working in health institutions under CRS as on October<br />
01, 2008 are as follows.<br />
Sl.<br />
Compulsory rural Bonded PG Diploma /<br />
District<br />
No<br />
service‐MBBS<br />
Degree<br />
1 Trivandrum 27 4<br />
2 Kollam 27 5<br />
3 Pathanamthitta 13 1<br />
4 Alappuzha 42 0<br />
5 Kottayam 17 1<br />
6 Idukki 17 0<br />
7 Ernakulam 49 2<br />
8 Thrissur 40 4<br />
9 Palakkad 28 6<br />
10 Malappuram 27 2<br />
11 Kozhikode 13 6<br />
12 Wayanad 22 0<br />
13 Kannur 43 3<br />
14 Kasaragod 27 0<br />
Total 392 34<br />
121
Initiatives on Infection Control at<br />
Medical College Hospital, Trivandrum<br />
The context<br />
A hospital is a place where sick people come mainly for treatment<br />
and investigation owing to which infectious diseases are constantly in<br />
transition; new diseases are emerging and older diseases are re‐emerging. It<br />
had been noted that in Medical Colleges, over the past few years, there have<br />
been increased outbreaks of diseases that were earlier controlled. The<br />
reasons for these outbreaks are multiple and complex‐some of them being<br />
rapid population growth, expansion of population in to the remote areas,<br />
environmental degradation, improved transportation leading to easier spread<br />
of diseases, climate change, inadequate or deteriorating public health<br />
infrastructure, and poor infection‐control& infection prevention practices.<br />
In general, infections that occur more than 48‐72 hours after<br />
admission and within 10 days after discharge are considered to be hospital<br />
acquired infections or nosocomial infections. Hospitalized patients are more<br />
vulnerable to infection than other healthy individuals, since the host is<br />
immuno suppressed and the environment is conducive to growth of resistant<br />
bacteria. Moreover the transmission of these bacteria is very much facilitated<br />
by the activities of the healthcare workers and other patients. Some times<br />
there is a large increase in the commonly occurring types of infections or<br />
appearance of a new infection for e.g., Methicill‐ in resistant staphylococcus<br />
aureus (MRSA) in the Surgery/Orthopedics ward<br />
122
The need to control<br />
Approximately10% of hospitalized patients develops infection every<br />
year. In developing countries this may go up to 25%. One third of these<br />
infections are preventable. Diagnosing and treating there infections puts<br />
intense pressure on the health care service and health budget. In short,<br />
healthcare facilities can be potential setting for transmission of diseases‐The<br />
reasons being,<br />
large no of persons with infections come to the healthcare<br />
setting for services<br />
services are provided in limited physical space<br />
Providers of health care services are exposed to various<br />
types of infections.<br />
Availability of limited number of<br />
instruments/equipments/essentials.<br />
Hence proper precautions in the health care facilities are pertinent for<br />
the prevention of nosocomical infections.<br />
Persons at risk<br />
All personnel in the healthcare setup who come in contact with<br />
patients or their investigative procedures are at potential risk of developing<br />
nosocomial infections. This includes<br />
o Doctors<br />
o Nurses<br />
o Lab Technicians<br />
o Attenders<br />
o Nursing assistants<br />
o Other paramedical<br />
staff,<br />
o Patients<br />
123
o Bystanders &the community.<br />
Measures initiated to prevent infection in Medical College Hospital,<br />
Thiruvananthapuram<br />
Medical College Hospital, Thiruvananthapuram is a premier tertiary care<br />
teaching institution with 1600 in –patients and 22 different specialties. On an<br />
average the referral O.P comes to about 450 new cases and 1000 review<br />
cases per day. New O.P in causality comes to 600 per day and review cases 70<br />
per day.<br />
Following an outbreak of infections in early 2007, the Infection<br />
Control Committee of Medical College Hospital, Thiruvananthapuram<br />
decided to implement a slew of measures to control the infection which<br />
included mainly the training component and continued awareness and<br />
ensuring adherence to standard protocol on Infection Prevention Practices<br />
Training to all level of staff Infection prevention was organized with the<br />
following objectives:<br />
Prevention of infection within and outside the hospital<br />
To bring about a positive change in the attitude and behaviour<br />
of health care providers with regard to infection prevention<br />
practices.<br />
A Handbook for the participants was prepared in the vernacular<br />
language by the State PEID Cell based on the WHO guidelines. The<br />
participants were trained in:<br />
1. Hand wash& use of gloves<br />
2. Surgical hand scrub& use of protective attires.<br />
3. Processing of instruments &their storage<br />
4. House keeping and maintaining a sterile field.<br />
5. Use & disposal of Sharps<br />
124
6. Waste Disposal.<br />
Eminent faculties from various hospitals handled the sessions and around<br />
1650 participants were trained in different batches covering 56 days<br />
The State PEID Cell is now in the process of preparing posters for<br />
wards and theatre on standard Precautions and developing a Protocol on<br />
Infection Prevention Practices for Medical College Hospital, Trivandrum<br />
based on WHO guidelines 2003.<br />
125
Ensuring quality supply of medicines in<br />
a transparent and efficient way- the<br />
KMSCL initiative<br />
The beginning<br />
In order to make available quality medicines, supplies, equipments &<br />
diagnoistic services to the poorest of poor of the population in the state,<br />
Government of Kerala has constituted Kerala Medical Services Corporation<br />
Ltd. (KMSCL) as a fully Government owned company with authorized share<br />
capital of Rs. Ten Crore with its headquarters in Thiruvananthapuram. The<br />
company got registered on 28.12.2007 with the <strong>Health</strong> Secretary has its<br />
Chairman and Special Secretary (<strong>Health</strong>), State <strong>Mission</strong> Director (NRHM),<br />
Director of <strong>Health</strong> Services, Director of Medical Education, Addl. Secretary<br />
(Finance), an expert in Pharmaceutical Sciences nominated by Government<br />
and the Managing Director, KMSCL are as Directors.<br />
Objectives of the Corporation<br />
The main objectives of the Corporation are the following.<br />
1. To implement a transparent system for<br />
procurement, storage and distribution of<br />
quality drugs, supplies, equipments etc.<br />
required for the hospitals at reasonable<br />
competitive price.<br />
2. To ensure adequate savings in the drug<br />
budget by efficient forecasting system.<br />
126
3. To avoid loss due to expiry of drugs and medical items and to optimize<br />
accountability at all levels.<br />
4. To achieve constant quality control monitoring of drugs and medical<br />
items by establishing adequate quality assurance measures.<br />
5. To adopt a streamlined procedure for procurement, storage and<br />
distribution through IT enabled services.<br />
6. To improve infrastructure of the existing Drug Warehouse in District.<br />
7. To provide diagnostic and other miscellaneous services to Government<br />
health care institutions.<br />
8. To enhance Public <strong>Health</strong> Care Service delivery by providing excellent<br />
management control and constant vigil.<br />
The Corporation started functioning with effect from 1st April, 2008<br />
by establishing District Drug Warehouses in all 14 districts in the State to<br />
cater the needs of 1316 <strong>Health</strong> Care Institutions under the State <strong>Health</strong><br />
Services Department and 16 institutions under six Government Medical<br />
Colleges in the State.<br />
Procurement of Medicines for Hospitals<br />
Government have constituted a Technical Committee (Expert<br />
Committee) in the Corporation consisting of Director of <strong>Health</strong> Services,<br />
Director of Medical Education, State <strong>Mission</strong> Director (NRHM), Drugs<br />
Controller, Senior Doctors nominated by DHS & DME and an expert in<br />
Pharmaceutical Sciences to prepare the list of medicines to be procured by<br />
Corporation. On the basis of the recommendations of the Technical<br />
Committee, Corporation has finalized the List of Essential Drug which consist<br />
of 527 items of generic medicines, sutures, surgical and other items. Based<br />
on the annual requirement of medicines & supplies furnished by the DHS<br />
and DME, Corporation floated its first tender on 30.01.2008 in which a record<br />
127
number of 173 reputed companies from all over the country participated.<br />
The tender processing were done in a transparent manner by publishing all<br />
details in its official web site www.arogyakeralam.gov.in in due course<br />
giving no chance of complaints from the bidders as well as the general public.<br />
Factory facilities of 20 new firms, who had participated in the tender<br />
for the first time in the state, were inspected by the team of inspectors<br />
appointed by the Corporation and six firms were rejected as they were not<br />
complying Good Manufacturing Practices (GMP) stipulated under the Drugs<br />
and Cosmetic Rules, 1945.<br />
Corporation finalized tenders with 103 firms, including State owned<br />
Kerala State Drugs and Pharmaceuticals Ltd. (KSDPL), for supply of medicines<br />
for the year 2008‐09 at a competitive rate. So far Corporation has issued<br />
purchase orders for procurement of medicines worth Rs.97.08 lakhs to<br />
ensure uninterrupted supply of all essential items.<br />
Ensuring Quality<br />
Each and every batch of Drug procured by the Corporation is being<br />
tested through Empanelled Analytical Laboratories to ensure the prescribed<br />
standards before release to hospitals. Corporation has empanelled Eleven<br />
(11) approved laboratories from all over India for testing the samples<br />
collected from the delivery received in the various District Drug Warehouses<br />
of the Corporation. Government Drug Testing Laboratory,<br />
Thiruvananthapuram is the appellate authority in the case of disputes<br />
regarding quality testing.<br />
Samples of supplies in each batch are chosen at the point of supply or<br />
distribution/ storage points for testing. Payment to the suppliers is released<br />
only upon receipt of quality analysis report from laboratories. Samples which<br />
do not meet quality requirements are rejected, treating them as Not Of<br />
Standard quality. So far Corporation has sent 2,809 samples of medicines for<br />
128
analysis and obtained results for 2,023 samples. Sixteen samples have been<br />
declared as Not Of Standard quality.<br />
Distribution to Hospitals<br />
The medicines received from the suppliers are collected in the District<br />
Drug Warehouses of the Corporation for delivery to hospital as per their<br />
requirements. The delivery schedule for various categories of hospitals has<br />
been designed as follows.<br />
<br />
Medical College Institutions ‐ Thrice in a<br />
month<br />
District /General Hospital ‐ Twice in a month<br />
Taluk Hospitals ‐ Once in a month<br />
BPHC/ CHC/ PHC ‐ Once in 2 months<br />
Mini PHC ‐ Once in 3 months<br />
In addition to this emergency supplies are also given to hospitals as<br />
per necessity. For each hospital budget allotment is provided for purchase<br />
of medicines from the Corporation and a Pass book is also maintained to<br />
record the transactions.<br />
All the District Drug Warehouses and Head Office of the Corporation<br />
are connected through online network by a data processing system named as<br />
Drug Distribution Management System (DDMS) for monitoring the stock<br />
position, details of samples collected for testing and to watch the<br />
performance of suppliers, etc.<br />
Other Projects under processing<br />
Apart from supplying medicines, surgical and supplies to hospitals,<br />
Corporation has initiated action for supply of coats, beds, bed sheets etc. for<br />
129
the hospitals. Action has also taken for fixing rate contract for supply of<br />
consumables and disposables, Reagents and Chemicals, X‐ray items, Linen,<br />
Medical gases, Glass wares, Dental Materials and specialized surgical and<br />
sutures required for the hospitals.<br />
Corporation is supplying medicines to<br />
hospitals which are availing funds provided by<br />
the Local Self Governments for purchase of<br />
medicines.<br />
Corporation has start action for supply of<br />
32,200 ICDS kits consisting of 10 items of<br />
medicines as per the requirement of the Sate<br />
Social Welfare Department as per the Central Sector Scheme.<br />
Negotiations are on with the State Animal Husbandry Department for<br />
the procurement and supply of around 100 items of veterinary medicines.<br />
Corporation is also supplying certain medicines to the Kerala State<br />
AIDS Control Society and the State ESI Department.<br />
Advantages<br />
Disadvantages of earlier system<br />
Lack of inventorisation of the<br />
entire system.<br />
No centralised computer<br />
network system to monitor and<br />
coordinate the procurement and<br />
distribution functions.<br />
Unscientific indenting, and<br />
lack of proper quality check<br />
Non‐adherence of First expiry<br />
First out (FEFO) system.<br />
<br />
Excess administration costs,<br />
Advantages of the present<br />
system<br />
Procure and stock quality<br />
drugs and supplies<br />
Follow essential drug<br />
guideline of WHO<br />
Ensure ready availability of all<br />
essential drugs and supplies<br />
throughout the state, in proper<br />
quality.<br />
Ensure adequate savings in<br />
Drug Budget by efficient<br />
forecasting system.<br />
Avoid loss of drugs owing to<br />
expiry.<br />
130
no market standing of products.<br />
Chances of duplication of<br />
invoices.<br />
Manipulation of quantity,<br />
higher procurement costs.<br />
Agents acting as cartel,<br />
bargaining for higher prices, &<br />
dictating terms.<br />
Poor delivery system to the<br />
peripheral hospitals<br />
Constant quality control<br />
monitoring of drugs.<br />
Enhance public service by<br />
providing<br />
excellent<br />
management control.<br />
Adopt a streamlined procedure<br />
for procurement, storage and<br />
distribution<br />
Medicines and Supplies are procured at a reasonable and competitive rate<br />
much lower than the market rate. The following are some of the examples.<br />
Sl. No. Name of the Drug KMSCL<br />
Rate*<br />
Market<br />
Rate*<br />
1 Isosorbide Dinetrate Tab 6.90 89.00<br />
2 Nifedipine Tab 6.60 40.00<br />
3 Atenalol Tab 12.25 40.00<br />
4 Ciprofloxacin Tab 83.00 120.00<br />
5 Amoxycillin Dispersible Tab 34.99 60.00<br />
6 Amoxycillin Cap 74.05 120.00<br />
7 Ampicillin Cap 68.34 122.00<br />
8 Ranitidine Tab 19.60 32.00<br />
9 Insulin Human Rapid Acting 55.85 120.00<br />
10 Anti‐Snake venom 140.04 333.00<br />
11 Anti‐Rabies Vaccine 205.70 316.00<br />
12 Paracetamol Tab 13.68 24.00<br />
*Rate for 100 tablets<br />
131
Ensures timely and uninterrupted supply of quality medicines,<br />
surgicals, sutures etc. to hospitals.<br />
Significant reductions in procurement cost of medicines and there by<br />
savings in budgetary allotment.<br />
Better inventory control.<br />
Pre‐decided delivery schedule to hospitals ensures regular supply of<br />
medicines and reduces rush in District Drug Warehouses.<br />
Computerized Drug Distribution Management System (DDMS) enables<br />
stock monitoring, re‐ordering and order placing of items easier.<br />
Batch wise quality testing of medicines at the point of delivery<br />
ensures quality assurance of medicines supplied to hospitals.<br />
Suppliers’ bill passing and payments become prompt and regular.<br />
132
Improving efficiency of Hospitals- the<br />
decentralized way<br />
The context<br />
People’s representatives and common population having a stake on<br />
the development of their health institutions is of great significance in this era<br />
of community led planning and monitoring. The true essence of this concept<br />
was captured through a public contact programme (Janasamparkaparipadi)<br />
organised at the districts led by the Minister for <strong>Health</strong> and Social Welfare<br />
and Coordinated by NRHM. The initiative titled ‘janasamparkaparipadi‐2008’<br />
covered the districts of Wayanad, Kannur and Kasaragode districts of the<br />
state on 23 rd , 24 th and 25 th of October 2008. The rest of the districts will be<br />
covered the end of December 2008. The aim of the programme is to get<br />
suggestions and opinions from the peoples’ representatives, NGOs and the<br />
general public towards improving the functioning of the hospitals and to<br />
chart out a concrete plan of action based on the suggestions. The<br />
stakeholders were asked to submit suggestions/grievances to their nearest<br />
health institutions till two days before the programme day.<br />
The process<br />
The programme had a preparatory and an action phase. A slew of<br />
preparatory activities were done as detailed below:<br />
• Financial review of the districts was done the following heads<br />
were reviewed:<br />
• Expenditure against funds given under RCH‐II/<strong>Mission</strong> Flexible<br />
Pool and Immunization<br />
133
• Expenditure against funds devolved for HMS/AMG/Untied funds.<br />
• Expediting utilization of funds for HMS/AMG/Untied funds.<br />
• JSY Funds utilization<br />
• Progress of CHC up‐gradation<br />
Detailed report on the progress of the civil works in institutions and layout<br />
plans were prepared.<br />
The public were informed about the campaign through:<br />
• Public Address system<br />
• Road show<br />
• Bit notices to be distributed through ASHA volunteers<br />
• Through TV as scroll messages<br />
• Spot news through FM/Radio<br />
• Press releases/news through Print and electronic media<br />
• Banners/posters to be placed at major public places/offices/health<br />
institutions<br />
• Notice inviting grievances exhibited in all Primary Level <strong>Health</strong><br />
Institutions<br />
• SMS to mobiles through a special news portal and major mobile<br />
service providers in the state<br />
Publicity was given for 5 days prior to the programme date and the<br />
grievances received were consolidated, classified based on the nature.<br />
The needs for the requested equipment from the Institutions were analyzed<br />
with regard to:<br />
• The availability of space for all the big (physically) equipment.<br />
• The availability of specialist to operate sophisticated equipments.<br />
• The input electrical supply for high load equipments.<br />
• the patient load<br />
• availability of existing similar equipments and its condition<br />
134
• range and capacity of machine suitable to the institution<br />
On the Programme day<br />
Public relations activities<br />
• ASHA volunteers and the health staff guided the gathering<br />
• Kiosk on NRHM was put up at the entrance<br />
• Banners put up at different locations at the campaign site<br />
• Leaflets on various health topics and NRHM distributed<br />
• Ventriloquism/monkey shows/puppet shows organized at different<br />
locations of the venue<br />
• Wide Media coverage was given<br />
• Media publicity through PIB and dept. of field publicity<br />
• Reporting and documenting the event<br />
• Awareness films/video spots through Plasma TV<br />
• A big balloon with message 'jana samparka paripadi' flown at the<br />
campaign site towards distant visibility of the venue<br />
135
The outcome<br />
The sorted out suggestions and<br />
grievances were sorted out discussed<br />
and solutions suggested with a definite<br />
action plan for implementation. Later in<br />
the day review of NRHM implementation<br />
in the districts was carried out. A press<br />
conference was organized wherein the<br />
action plan was detailed out.<br />
Feedback from the participants (25 samples) were collected and analysed. As<br />
shown in the graph below majority who participated<br />
136
State Disease Control and Monitoring<br />
Cell (SDCMC): an innovative initiative<br />
towards the control of communicable<br />
diseases<br />
The background<br />
Emergence and resurgence of vector borne diseases, including Chikungunya,<br />
has become a serious threat to Kerala – to the people and to the health care<br />
management system. Since May‐June 2006, Kerala has reported outbreaks of<br />
Chikungunya in many localities of Alappuzha, Kozhikode, and Trivandrum,<br />
Ernakulam, Kottayam and Pathanamthitta districts. This has resulted not only<br />
in health cost but also economic loss due to the number of man days lost.<br />
NRHM Kerala has been working on possible options to prevent Chikungunya<br />
and other vector borne diseases, on a war footing basis and has formed the<br />
State Disease Control and Monitoring Cell (SDCMC) to coordinate various<br />
interventions in disease control and management.<br />
Role of SDCMC<br />
SDCMC will be actively involved in the disease surveillance, monitoring and<br />
control activities and at the same time coordinating the efforts of a wide<br />
variety of stakeholders towards the prevention of outbreaks in the State. In<br />
addition to collaborating with these stakeholders for the successful<br />
implementation of the programme, SDCMC is also supporting various<br />
projects being implemented to strengthen the disease control activities all<br />
through the State. An action plan has already been prepared for the year<br />
2008. A multifaceted approach with active participation from all the<br />
stakeholders will help in preventing the catastrophic effects of the outbreak.<br />
137
The primary function of SDCMC is to act as the coordinating body between<br />
these different stakeholders and to play a central role in the development<br />
and implementation of disease control and monitoring activities in the state.<br />
Standard Management Protocol developed<br />
138
Stakeholders of SDCMC<br />
NRHM<br />
KGMOA<br />
IMA<br />
KGMCT<br />
HLFPPT<br />
NICD<br />
SDCMC<br />
NIV<br />
KERALA<br />
UNIT<br />
DHS<br />
KSIVID<br />
DME<br />
Addl. DHS (PH)<br />
Entomology teams<br />
IDSP<br />
NVBDCP<br />
14 Districts<br />
DMO (H)<br />
District Malaria Officer<br />
DPMS<br />
District Level VC teams<br />
State PEID cell<br />
Regional PEID cell<br />
Medical colleges<br />
Government<br />
Private<br />
Cooperative<br />
KGMOA ‐ Kerala Government Medical Officers Associations<br />
KGMCT ‐ Kerala Government Medical College Teachers Association<br />
NICD ‐ <strong>National</strong> Institute of Communicable Diseases<br />
KSIVD ‐ Kerala State Institute of Virology Diseases<br />
HLFPPT ‐ Hindustan Latex Family Planning Promotion Trust<br />
DHS‐ Directorate of <strong>Health</strong> Services<br />
DME ‐ Directorate of Medical Education<br />
139
The core strategies in addressing vector borne diseases, as specified by the<br />
State Disease Control and Monitoring Cell (SDCMC) are<br />
<br />
<br />
<br />
Strengthening of the surveillance system.<br />
Integrated vector management.<br />
Enhanced monitoring and supervision<br />
Key supporting interventions planned for disease control and monitoring are<br />
1. Capacity building<br />
2. Behaviour change communication<br />
3. Intersectoral collaboration<br />
Activities of SDCMC at a glance<br />
Daily Communicable Disease Reporting From All District<br />
Headquarters/ Medical Colleges and consolidation<br />
Daily report of Communicable Diseases in the state sent to <strong>Health</strong><br />
Minister, Secretary (H), <strong>Mission</strong> Director, DHS, DME via email and SMS<br />
by 6 pm<br />
Strengthening Of Surveillance System through Medical Colleges With<br />
the Support Of State & Regional PEID Cells<br />
Local Media Scanning<br />
Visual Media<br />
Print Media<br />
24 X 7 Reporting & Monitoring<br />
Lab Surveillance through NIV Field Unit, Alappuzha<br />
Students engaging in source reduction activities<br />
KSIVD (Kerala State Institute of Infectious and Viral Diseases),<br />
Alappuzha, Microbiology Depts, Medical Colleges<br />
140
Developed and Implemented State and Block Level Action Plan for<br />
the Control Of Chikungunya/ Dengue.<br />
Developed Standard Management Protocol for Suspected<br />
Chikungunya<br />
Organizing Workshops on Monitoring And Supervision Strategies for<br />
Prevention & Control Of Chikungunya, Dengue in Kerala<br />
Integrated Vector Management: Developed Handbook on Integrated<br />
Vector Management for <strong>Health</strong> Workers.<br />
Pre‐monsoon Aedes Survey in the State<br />
Intersectoral Coordintation With LSGIs<br />
ToT Of ASHA Workers and volunteers on Source Reduction Activities<br />
and and Observation of Dry Days.<br />
Undertaking Research/studies<br />
Feepok Study‐ Chikungunya Sequlae Study.<br />
Situational Analysis of Chikungunya Epidemic In Kasargode District.<br />
Study On Increasing Number Of Hepatitis B Cases From<br />
Pathanamthitta District.<br />
Source reduction activities<br />
Epidemic Response<br />
Started 24 X 7 Epidemic Control Cell and field stations in Kasargode to<br />
control the outbreak<br />
Held interstate Meeting‐ Kerala, Karnataka, Tamilnadu.<br />
Held Inter district Meeting‐ Kasargode, Kannur, Dakshin Kannada,<br />
Kudagu<br />
Started Border Fever Depots<br />
Organised Medical Camps‐ Allopathy, Ayurveda And Homoeo<br />
Intensified Source Reduction By Arogyarakshak (Volunteers)<br />
141
BCC Initiatives<br />
Focused Campaign using a slogan and campaign colour: Nithantha<br />
Jagratha Veeduthorum<br />
Nodal Agency: Hindustan Latex Family Planning Promotion Trust<br />
Campaign initiated In Northern Districts<br />
Set of IEC tools developed<br />
Target specific leaflets for awareness generation amongst the public and students<br />
Posters developed for awareness creation<br />
142
Platforms for Sharing and learning‐ Organizing workshops<br />
A. <strong>National</strong> Workshop on Emerging Fevers with Focus on Chikungunya<br />
The need<br />
India witnessed a massive outbreak of Chikungunya in 2006 and 2007.<br />
Kerala is reported to be one of the worst affected states in India during the<br />
2007 epidemic. Though the health care community could address the<br />
epidemic to an extent, this called for an effective action strategy to contain<br />
the outbreak. The <strong>National</strong> Workshop on Emerging Fevers with Focus on<br />
Chikungunya is an offspring of such a conscious and responsible thought.<br />
Objectives of the workshop<br />
<br />
<br />
<br />
To act as a forum for sharing<br />
<strong>National</strong>/ International<br />
experiences in containing<br />
emerging fevers.<br />
To provide opportunities for<br />
deliberations of studies done<br />
through oral and poster<br />
presentations<br />
Presentation and finalization of an action plan for the state in the<br />
areas of<br />
a. Prevention and control<br />
b. Management<br />
c. Follow‐up<br />
143
Major stakeholders of the workshop<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Govt. of Kerala<br />
<strong>National</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Mission</strong>, Kerala<br />
Directorate of <strong>Health</strong> Services<br />
Directorate of Medical Education<br />
Kerala Govt. Medical College Teachers Association<br />
Kerala Govt. Medical Officers Association<br />
Indian Medical Association<br />
AYUSH Departments<br />
Two pre workshop meetings were held to sensitize major stakeholders about<br />
the forthcoming national workshop and ensure their participation in the<br />
workshop, mobilize maximum number of research papers on Chikungunya<br />
and emerging fevers and to prepare a draft action plan for the state. The<br />
meetings focused on the limitations and gaps in the current practice and<br />
threw light into strategies to strengthen the efforts to contain emerging<br />
fevers.<br />
The process and outcome<br />
The national workshop was attended by 450 delegates from across the<br />
country. Scientific sessions deliberated on the national scenario on the<br />
Chikungunya epidemic and measures taken to contain the epidemic;<br />
experiences of various states in the country; preventive and management<br />
strategies were discussed in detail. The key aspects of preventive strategies<br />
of the Kerala; state action plan for containing emerging fevers evolved in the<br />
pre workshop meetings and the time bound strategic plan for the prevention<br />
of Chikungunya and other emerging fevers; the management strategies. The<br />
workshop concluded with the finalization of an action plan for the state in the<br />
areas of prevention, management and follow‐up.<br />
144
B. Workshop on Intra Dermal Rabies Vaccination<br />
The need<br />
Rabies is a major public health issue in many parts of the world<br />
causing an estimated 55,000 deaths every year. India suffers a casualty of<br />
about 22,000 deaths per year due to rabies and in Kerala Rabies claims about<br />
30‐40 lives per year. Timely and appropriate post exposure prophylaxis can<br />
prevent deaths in this one hundred percent fatal disease. Approximately 3<br />
million people receive post exposure prophylaxis in India. Nervous Tissue<br />
Vaccine (NTV) has been replaced by more safe and effective Cell Culture<br />
Vaccines (CCVs) in India since December 2004. WHO estimates that a full<br />
course of Post Exposure Prophylaxis (PEP) requires 31 days of wages for an<br />
Asian citizen thereby making it unaffordable to many. Intradermal post<br />
exposure regimen has been approved by WHO as early as in 1992 and has<br />
now undergone extensive evaluations in India. It is found to be equally<br />
effective and at the same time cost effective (60‐70% cost reduction). This<br />
regimen has been approved by the Govt. of India in 2006. NICD, Delhi has<br />
formulated and published guidelines for intradermal vaccination for Govt. of<br />
India and is already being implemented in states like Uttar Pradesh, Orissa,<br />
Andhra Pradesh, Karnataka, West Bengal, Tamilnadu and Uttaranchal.<br />
Proceedings of the workshop<br />
In this context a workshop on<br />
developing guidelines for IDRV<br />
(Intra Dermal Rabies Vaccine)<br />
in Kerala was held during the<br />
month of September 2008. The<br />
workshop was enriched by the<br />
145
presence of experts of International and <strong>National</strong> repute from within and<br />
outside the state. Faculties from 8 states, who had already implemented the<br />
IDRV regimen in their states, shared their experiences in the workshop. The<br />
workshop was attended by key stakeholders from all over the state. There<br />
were representatives from <strong>Health</strong> Services Department, Medical Education<br />
Department and also Service Unions in <strong>Health</strong> Services. More than 320<br />
delegates attended the workshop during which the faculties shared their<br />
experiences regarding IDRV implementation in their states. The workshop<br />
was followed by a core group meeting on the next day during which the<br />
<strong>National</strong> Guidelines put forward by NICD in 2007 was discussed in detail and<br />
was adopted to suit Kerala scenario. The core group had the presence of<br />
nearly 50 experts from within and outside the state.<br />
Outcome<br />
There were 3 post workshop core group meetings as a result of which the<br />
draft guidelines for implementation of IDRV and draft operational guidelines<br />
have been prepared. It was decided to implement IDRV in a planned phase in<br />
the state with the support of Kerala Medical Services Corporation Ltd<br />
(KMSCL). As the first step IDRV will be implemented in the Anti Rabies Clinics<br />
attached to the 5 Govt. Medical Colleges in the state and also General<br />
Hospital, Thiruvananthapuram. It is also planned to impart training to the<br />
stakeholders at three levels‐ <strong>National</strong> level training from Hyderabad, State<br />
level training and District level training.<br />
At present Kerala is following the IM regimen for Anti rabies vaccination and<br />
only the bite victims belonging to BPL category are given the costly IM<br />
treatment free of cost that too subject to availability. With the adoption of ID<br />
regimen we will be able to cater to almost five times the patient load with<br />
the present quantity of vaccine. This will surely help in improving the<br />
146
acceptability of the more cost effective IDRV regimen thereby increasing the<br />
accessibility of the common man for treatment against this deadly disease.<br />
The workshop IDRV KERALA 2008 is believed to be the first step in the<br />
direction of a crucial policy change by Govt. of Kerala.<br />
147
COMPREHENSIVE HEALTH<br />
INSURANCE SCHEME (CHIS)<br />
1. Rashtriya Swasthya Bima Yojana<br />
1.1. The Rashtriya Swasthya Bima Yojana scheme of Government of India<br />
announced by Prime Minister, Manmohan Singh on Aug 15th 2007, is<br />
introduced in the State alongwith Comprehensive <strong>Health</strong> Insurance<br />
Scheme for (CHIS).<br />
1.2. The objective of RSBY is to protect below poverty line (BPL) households<br />
from major health shocks that involve hospitalization. Specifically, BPL<br />
families are entitled to more than 700 in‐patient procedures with a cost<br />
of up to 30,000 rupees per annum for a nominal registration fee of 30<br />
rupees.<br />
2. Comprehensive <strong>Health</strong> Insurance Scheme for (CHIS)<br />
2.1. Provision of effective and free healthcare to the poorest 30 % families is<br />
taken up in the Eleventh 5 year Plan of the State by way of strengthening the<br />
Public <strong>Health</strong> System. As per the estimates of Planning Commission, there<br />
are 11.79 lakhs BPL (absolute poor) families in Kerala and all of whom will be<br />
covered under RSBY. In addition, the State government has estimated<br />
another 10 lakhs BPL (poor) families in Kerala. According to the recent<br />
enumeration there are 12,66,207 “absolute poor” and 11.01,206 “poor”<br />
families in the State.<br />
148
2.2. In this scenario the Government of Kerala has extended the benefits of<br />
Insurance scheme to the ‘Poor’ BPL population and All others included under<br />
“Above Poverty Line” by introducing alongside the CHIS with slight variation<br />
in premium. Hon’ble Minister for Finance, Dr. T.M.Thomas Issac in his Budget<br />
Speech for 2008‐09, announced the implementation of the Comprehensive<br />
<strong>Health</strong> Insurance Scheme for (CHIS) to all the families other than those<br />
covered under the RSBY.<br />
2.3. Thus the non –RSBY population covering more than 3/4 th families of the<br />
State are divided into two categories (a) those belonging to BPL (poor) list of<br />
the State Government but do not to the list of Central Planning Commission<br />
and (b) the APL families belonging neither to list of State Govt nor prepared<br />
as per guidelines of Planning Commission.<br />
Accordingly the State Govt. issued orders on 4 th July 2008 for implementing<br />
CHIS in the State. The scheme was launched on 2 nd October 2008 and<br />
Alappuzha district was taken up as the first district. The RSBY and CHIS is<br />
introduced in all the 14 districts of the State.<br />
3. Premium and Registration fees for CHIS<br />
In RSBY, 75% of the premium is met by the Central Government and 25% by<br />
State Government while under CHIS (BPL poor), the State Government bears<br />
100% premium. The beneficiary pays Rs 30/‐ towards registration fees/<br />
family in both cases. In case of APL, the beneficiary bears the premium<br />
amount as well as registration fees. The competitive premium per family<br />
quoted is Rs.506/‐ inclusive of service tax and cost of smart card for all 13<br />
districts except Palakkad where it is Rs.498/‐<br />
3. Implementation of the Schemes in Kerala<br />
149
3.1. The Scheme is jointly implemented by departments of Labour &<br />
Rehabilitation, <strong>Health</strong> & Family Welfare, <strong>Rural</strong> Development, and Local Self<br />
Govt. The Labour Department is the Nodal dept. for implementation of CHIS.<br />
3.2. A separate agency “Comprehensive <strong>Health</strong> Insurance Agency of Kerala”<br />
(CHIAK) is created for implementation of the scheme.<br />
3.3. “United India Insurance Company Limited” is the insurance provider for<br />
all 14 districts.<br />
4. Benefits of the scheme<br />
First, the scheme provides the beneficiary a choice between public and<br />
private hospitals and makes him a potential client worth attracting and<br />
keeping due to the significant revenues that hospitals stand to earn through<br />
the scheme.<br />
‣ Cashless medical treatment up to Rs.30,000/‐ per annum<br />
‣ Coverage of existing diseases<br />
‣ No age limit<br />
‣ Coverage extends to the head of household, spouse three dependants<br />
(Children/Parents)<br />
Second and related to this point, the overall design of the scheme involves<br />
incentives that are conducive both to the expansion of the scheme as well as<br />
long run sustainability. In the case of enrolment, the insurer is compensated<br />
for each household enrolled and issued a smart card.<br />
Other benefits to beneficiaries<br />
‣ Free OPD consultation (No OP treatment)<br />
‣ Accident death benefit of Rs.25000/‐ for head of family and spouse<br />
(extra benefit offered free by the insurance company)<br />
‣ Transport expenses up to Rs. 100/‐ trip with a maximum of Rs.1000/‐<br />
150
Apart from this Incentives would be granted to Hospital staff attending to the<br />
patient @ 15% of claim amount received, Field Key Officers @Rs.2/‐ per card<br />
and District Key Managers @ Rs.1000/‐ per month for 3 months<br />
5. Empanelment of Hospitals<br />
5.1. Criteria<br />
‣ At least 10 inpatient medical beds for primary inpatient health care<br />
‣ Should have an operational pharmacy and diagnostic service, or<br />
should be able to link with the same. (Testing of clinical specimens, X‐<br />
rays and ECG etc.)<br />
‣ Fully equipped Operation theatre<br />
‣ Fully qualified doctors and nursing staff under its employment round<br />
the clock<br />
‣ Maintenance and providing of necessary records<br />
‣ Registration with Income Tax Department<br />
‣ Telephone/Fax, 64KBPS connectivity, Personal Computer with 2 smart<br />
card readers and a finger print verification machine or a stand‐alone<br />
machine<br />
‣ Agree to the cost of packages for each identified<br />
intervention/procedure as approved under the Scheme.<br />
‣ Bed charges (General Ward), Nursing and Boarding charges, Surgeons,<br />
Anesthetists, Medical Practitioner, Consultants fees, Anesthesia,<br />
Blood, Oxygen, O.T. Charges, Cost of Surgical Appliances, Medicines<br />
and drugs, X‐rays, food to patient etc.<br />
‣ Expenses incurred for diagnostic test and medicine up to 1 day before<br />
the admission of the patient and cost of<br />
medicine up to 5 days after the discharge<br />
‣ Offer free OPD consultation<br />
diagnostic tests and<br />
151
‣ Provide fixed discounts on diagnostic and medical treatment required<br />
for beneficiaries<br />
‣ Agree to display the CHIS status at their reception / admission<br />
counter<br />
‣ Agree to provide a separate help desk and have a dedicated officer in<br />
the administration dept.<br />
5.2. Indicative list of day care treatments<br />
Due to the advances in the treatment techniques the following health<br />
services will be treated on a day care basis<br />
Haemo – Dialysis<br />
Parenteral Chemotherapy<br />
Radiotherapy<br />
Eye surgery<br />
Lithotripsy (Kidney stone removal)<br />
Tonsillectomy<br />
D&C<br />
Dental surgery following an accident<br />
Surgery of Hydrocele<br />
Surgery of prostrate<br />
Few gastrointestinal Surgery<br />
Genital Surgery<br />
Surgery of Nose<br />
Surgery of Throat<br />
Surgery of Ear<br />
Surgery of Urinary System<br />
Treatment of fractures/dislocation (excluding hair line fracture),<br />
Contracture releases and minor reconstructive procedures of limbs<br />
which otherwise require hospitalization<br />
Laparoscopic therapeutic surgeries that can be done in day care<br />
Identified surgeries under General anesthesia<br />
Any disease/ procedure mutually agreed upon<br />
5.3. Common exclusions<br />
(Conditions that do not require hospitalisation)<br />
Congenital external diseases<br />
Drug and Alcohol induced illnesses<br />
152
Sterilisation and Fertility related procedures<br />
Vaccination<br />
War, nuclear invasion<br />
Suicide<br />
Naturopathy, Unani, Sidha, Ayurveda<br />
6. Transaction at hospitals<br />
Beneficiaries are entitled to a list of pre‐specified in‐patient services from the<br />
second month following enrollment. Upon discharge, the pre‐specified cost<br />
of the procedure is deducted from Rs. 30,000/‐. A receipt is printed and<br />
provided to the beneficiary Actual travel cost up to a maximum of Rs.100/‐<br />
per visit would be given to the beneficiary at the time of discharge.<br />
7. Operation of the System<br />
Enrollment<br />
The List of eligible BPL households is provided to the insurer in RSBY format.<br />
The list is posted in each village prior to the enrollment. The date and<br />
location of enrollment booths is publicized in advance and stations equipped<br />
with the hardware for the issue of smart cards. The smart card along with an<br />
information pamphlet describing the scheme and the list of empanelled<br />
hospitals is provided on the spot and the beneficiary has to pay Rs.30 as<br />
registration fee. The Schemes operates through a biometric Smart Card with<br />
Provision to split the card to more than one among the beneficiaries. On loss<br />
of card, a new card can be issued but beneficiary will have to bear the cost of<br />
the duplicate card.<br />
153
154
8. Gearing up for the scheme by NRHM<br />
8.1. A technical committee headed by Superintendent with RMO, 2 to 3 Unit<br />
heads / HODs, Nursing officer, Nursing Superintendent as members and PRO<br />
as convener would be formed in all institutions. This committee will be<br />
responsible for sorting out issues if in connection with incentives of doctors<br />
and other staffs.<br />
8.2. The Medical Officer in Charge is arranged to submit Insurance claims for<br />
all the patients for the procedure services covered to the Insurance company,<br />
with all required documents and the money received against the claim would<br />
be utilized by the hospital with approval of Hospital Management Committee<br />
155
(HMC)/ Hospital Development Society (HDS). The Medical Officer‐incharge/Superintendents<br />
of the respective hospitals would be responsible to<br />
provide the additional requirement if any in equipping the critical<br />
components for implementing the CHIS Scheme through the Hospital<br />
Management Committee/Hospital Development Society. The Medical Officerin<br />
charge/Superintendents would ensure that proper records are maintained<br />
for all the OP/IP cases handled in the hospitals to ensure timely submission of<br />
insurance claims to the insurance company and realization of reimbursement.<br />
8.3. Insurance money received from Insurance company will be deposited in<br />
separate bank account started by HMC/HDS. All payments from this account<br />
would be paid through bank cheques except transportation allowance to<br />
patients upto Rs 100/‐ at a time. Payments of incentives to doctors to<br />
Doctors and other staff will be through cheques. Only generic drugs would<br />
be prescribed by Doctors as far as possible. And Kerala Medical Services Corp.<br />
Ltd. (KMSCL) will make all efforts to ensure regular supply of the same.<br />
8.4. 85% of the insurance amount flowing into the account would be<br />
earmarked as HMC/HDS share and remaining 15% as incentive share. 85% of<br />
the insurance amount earmarked as HMC/HDS share would be utilized for<br />
filling critical gaps in providing quality medical care in various service delivery<br />
areas of hospital namely OP, IP sections, OT for providing various drugs and<br />
consumables, for essential lab investigations hiring manpower especially<br />
doctors like anesthetist/ surgeon etc. Remuneration for Computer operator/<br />
Data entry operator would be also met through this.<br />
8.5. Utilization of the staff incentive : 15% of the Insurance money share<br />
earmarked as the staff incentive share would be distributed as per the<br />
following general guidelines.<br />
Incentive break up as percentage of total incentive amount per case.<br />
156
1. Surgeon / main physician / doctor treating the case.<br />
30%<br />
2. Surgeon assisting the surgery / other physician / doctors involved<br />
in treating the case<br />
10%<br />
3. Anesthetist / doctors of other departments actively involved in<br />
case management of medical cases<br />
20%<br />
4. Consultations / call duty etc<br />
5%<br />
5. Staff Nurses<br />
12%<br />
6. Nursing Assistants / Hospital Attendant Gr.1 &2<br />
8%<br />
7. Lab Technician<br />
2%<br />
8. X‐ray / Ultra Sound CT Scan Technician<br />
2%<br />
9. Record Keeping / system management<br />
1%<br />
10. Others if any<br />
10%<br />
Staff Nurses /hospital Attendants Gr.1 &2 of IP Wards, OT, Post<br />
Operator Wards, and Observation wards would be eligible for incentive as<br />
per no. of cases managed. Lab technicians would be eligible for incentives if<br />
lab investigations are done in hospital lab for these cases. Doctors involved in<br />
the Ultra sound CT Scan would be covered as consultation component of<br />
incentive.<br />
8.6. One Computer each has already been procured and allotted to 1,033<br />
Hospitals under <strong>Health</strong> Services, including the hospitals selected for the<br />
scheme. These computers would be utilized for the implementation of this<br />
scheme. A telephone with 64 Kbps connectivity is to be provided in the<br />
hospital if not available already.<br />
System Administrator and State Data Manager of NRHM will take care of the<br />
connectivity aspect of this component.<br />
157
8.7. Rs. 15,000/‐ (Rupees Fifteen thousand only) each would be given through<br />
HMC/HDS for all the selected institutions for the procurement of additional<br />
of facilities/equipment. The Untied fund Maintenance Grant and the fund<br />
provided to the HMCs through NRHM would be utilized for meeting the<br />
additional requirement if any.<br />
8.8. The procurement procedure of the finial print reader, smart card reader<br />
etc. would be done by NRHM through the insurance company in centralized<br />
manner after rate negotiations. The payment of the same woulld be made by<br />
the HMC/HDS, at the local level after successful installation of the same.<br />
8.9. In Medical College Hospitals, General Hospitals and Specially/District<br />
Hospitals. CHIS counters will be functioning round the clock specifically to<br />
take care of the CHIS patients. In other major Hospitals and smaller hospitals,<br />
after the routine working hours, registration of casually patients will be done<br />
by the staff nurse in charge/other designated staff in charge of the casualty.<br />
They would also be eligible for incentive from the category of "others"<br />
earmarked in the incentive guidelines ordered separately.<br />
8.10. One Public Relation Officer (PRO) preferably with MBA qualification will<br />
be posted through NRHM in selected institutions identified, and they will be<br />
made responsible for looking after the implementation of the scheme (ie.<br />
institutional level nodal officer) under the supervision and guidance of the<br />
Superintendent/Medical Officer‐in‐charge of the institution.<br />
8.11. A Computer Operator would be posted through NRHM for taking care<br />
of the routine functioning of the CHIS scheme. In bigger institutions which<br />
require additional staff to run the CHIS counter data entry operators if<br />
required, would be engaged on contract basis through Kudumbasree units<br />
with the approval of the HMC/HDS.<br />
8.12. For the first 3 months the payment of the Public Relation Officer and<br />
Computer Operator will be met by the NRHM. Thereafter it will be the<br />
responsibility of the HMC/HDS to pay the remuneration of these staff.<br />
158
8.13. Facility Survey based filling of Critical Gaps: Facility Survey would be<br />
completed immediate in the selected hospitals, for filling the Critical Gaps of<br />
infrastructure, equipments and staff of all these institutions based on the<br />
survey report should be completed through NRHM/immediately.<br />
8.14. Facilities of remaining Hospitals selected: The facilities available under<br />
plan fund, TRP, ACA, LSGI fund HMC fund etc would be utilized as per IPH<br />
standard/standardization guidelines in time bound manner.<br />
8.15. Strengthening the Lab facilities. The Lab facilities of the selected<br />
institutions including Medical College Hospitals will be assessed and to fill up<br />
based on IPGS/standardization Committee report in time bound manner.<br />
The QCI norms and procedures will be followed in this regard.<br />
9. Database Management Software<br />
Software is proposed to be developed by C‐DAC for regular record keeping<br />
generation of weekly and monthly reports and tabulation of incentive for<br />
individual staff members. An additional RSBY / CHIS incentive recording<br />
format will be designed and attached to all case sheets. Individual doctors<br />
and other staffs attending CHIS cases would be putting the date wise<br />
signature and staff nurse / head nurse in charge would be responsible for<br />
record maintenance counter signed by unit chief every day.<br />
Latest progress from field‐ Report by CHIAK<br />
Field Key Officers issue 5,000 smart cards in Alappuzha under the two<br />
schemes after the launch on 2 nd October 2008. Remaining districts to<br />
be taken up in November.<br />
Private hospitals are being consulted by Insurer and District Collectors<br />
are monitoring the progress.<br />
159
District level workshops for 9 districts completed. Remaining being<br />
taken up.<br />
Meetings of Panchayat Presidents and other Panchayat<br />
representatives in progress.<br />
Kudumbasree is validating the BPL list of all districts other than<br />
Alappuzha and the data will be handed over to CHIAK. C‐Dit would be<br />
entrusted with the task of converting the same to RSBY format for<br />
forwarding to Government of India’s approval.<br />
One Hospital in each district will be called a Model Hospital and these<br />
hospitals will have facilities equivalent to that of Medical Colleges in the<br />
State. Facility surveys have been completed for major institutions<br />
(District/General/Speciality/Taluk Hospitals) towards identifying the critical<br />
infrastructure/manpower gaps which can be filled immediately as short term<br />
plan and over a period of two years as long term plan. The up gradation of<br />
119 CHCs in the state are on and nearly 50 will get upgraded by December<br />
2008 and the remaining by March 2009. The empanelled hospitals for<br />
implementing insurance scheme will be upgraded in a shortest time<br />
regarding infrastructure, equipments, diagnostic and other facilities through<br />
empanelled agencies. An amount of Rs. 18 crores (10 crores from Maternal<br />
<strong>Health</strong> Rs. 5 crores from Child <strong>Health</strong> and Rs. 3 crores from Urban <strong>Health</strong>)<br />
from RCH‐II and Rs. 22 crores (Rs. 10 crores from upgradation works and 12<br />
crores from EMRI) from Additional ties has been set apart for upgradation of<br />
selected hospitals in the state for implementing the insurance scheme.<br />
List of Hospitals where the insurance scheme will be implemented is annexed<br />
160
Annexure‐1<br />
LIST OF INSTITUTIONS<br />
TRIVANDRUM<br />
1. General Hospital, Trivandrum<br />
2. W & C Hospital, Thycaud<br />
3. Government Hospital, Peroorkada<br />
4. THQH Nedumangad<br />
5. THQH Chirayinkil<br />
6. THQH Neyyattinkara<br />
7. Government Hospital, Fort<br />
8. Govt. hospital, Parassala<br />
9. CHC Kanyakulangara<br />
10. CHC Kesavapuram<br />
11. CHC Vithura<br />
12. GH Varkala<br />
13. ICD Pulayanarkotah<br />
14. CHC Poovar<br />
15. CHC Vizhinjam<br />
KOLLAM<br />
1. District Hospital, Kollam<br />
2. W & C Hospital, Kollam (Victoria Hospital)<br />
3. THQH Sasthamkotta<br />
4. THQH Karunagapally<br />
5. THQH Punalur<br />
6. THQH Kottarakara<br />
7. CHC Neendakara<br />
8. CHC Kadakkal<br />
9. CHC Nedumgolam<br />
10. GH Nedumpana<br />
11. Chest Hospital, Karunagappally<br />
PATHANAMTHITTA<br />
1. General Hospital, Pathanamthitta<br />
2. District Hospital, Kozhencherry<br />
3. Specialty Hospital, Adoor<br />
4. THQH Tiruvalla<br />
5. THQH Ranni<br />
6. THQH Mallappally<br />
ALAPUZHA<br />
1. General Hospital, Alapuzha<br />
2. W & C Hospital, Alapuzha<br />
161
3. THQH Cherthala<br />
4. THQH Haripad<br />
5. THQH Mavelikkara<br />
6. CHC Chengannur<br />
7. GH Kayamkulam<br />
KOTTAYAM<br />
1. District Hospital, Kottayam<br />
2. General Hospital, Pala<br />
3. THQH Kanjirapally<br />
4. THQH Changanassery<br />
5. CHC Vaikom<br />
6. THQH Pampady<br />
IDUKKI<br />
1. District Hospital, Idukki<br />
2. THQH Peerumedu<br />
3. THQH Thodupuzha<br />
4. CHC Adimali<br />
5. CHC Nedumkantam<br />
6. PHC Marayoor<br />
7. PHC Devikulam<br />
ERNAKULAM<br />
1. General Hospital, Ernakulam<br />
2. W & C Hospital, Mattancherry<br />
3. THQH Fort Kochi<br />
4. THQH Aluva<br />
5. THQH Perumbavoor<br />
6. THQH N.Paravoor<br />
7. THQH Tripunithura<br />
8. THQH Moovattupuzha<br />
9. CHC Kothamangalam<br />
10. GH Karuvelipady<br />
11. CHC Piravam<br />
12. CHC Kalady<br />
THRISSUR<br />
1. District Hospital, Thrissur<br />
2. THQH Kodungalloor<br />
3. THQH Irinjalakuda<br />
4. THQH Chavakkad<br />
162
5. THQH Vadakkanchery<br />
6. THQH Chalakkudy<br />
7. Govt. hospital, Kunnamkulam<br />
8. GH Mala<br />
9. CHC Cherppu ( to be upgraded)<br />
10. CHC Valappad<br />
PALAKKAD<br />
1. District Hospital, Palakkad<br />
2. THQH Chitoor<br />
3. CHC Alathur<br />
4. THQH Mannarkkad<br />
5. THQH Ottapalam<br />
6. Tribal Specialty Hospital, Kottathara, Attapady<br />
7. CHC Nenmara<br />
MALAPPURAM<br />
1. District Hospital, Manjeri<br />
2. THQH Nilambur<br />
3. THQH Tirurangadi<br />
4. THQH Perinthalmanna<br />
5. THQH Tirur<br />
6. THQH Ponnani<br />
7. CHC Malappuram<br />
8. CHC Purathur<br />
9. CHC Areecode<br />
10. CHC Kondotty<br />
11. CHC Vandoor<br />
12. CHC Tanur ( to be upgraded)<br />
13. Block PHC Melattur<br />
14. PHC Edappal<br />
KOZHIKODE<br />
1. General Hospital, Kozhikode<br />
2. W & C Hospital, Kozhikode<br />
3. THQH Koilandi<br />
4. THQH Vadakara<br />
5. CHC Thamarassery<br />
6. GH Nadapuram<br />
7. CHC Kuttiyadi<br />
8. CHC Balusserry<br />
WAYANAD<br />
1. General Hospital, Kalpetta<br />
163
2. District Hospital, Mananthavady<br />
3. THQH Sultan Bathery<br />
4. THQH Vythiri<br />
5. CHC Meenangady<br />
6. CHC Pulpally<br />
KANNUR<br />
1. General Hospital, Thalassery<br />
2. District Hospital, Kannur<br />
3. THQH Thaliparamba<br />
4. GH Payyannoor<br />
5. GH Kuthuparambu<br />
6. CHC Peravoor<br />
7. CHC Pappinisserry<br />
8. CHC Panoor<br />
KASARAGODE<br />
1. District Hospital, Kanhangad<br />
2. THQH Kasaragod<br />
3. CHC Panathady<br />
4. CHC Nileswar<br />
5. GH Manjeswar<br />
6. PHC Kumbala<br />
7. CHC Cheruvathoor ( to be upgraded)<br />
8. CHC Trikkarippur<br />
164