OT OASIS C FOLLOW-UP/RECERT - TriPoint Healthcare
OT OASIS C FOLLOW-UP/RECERT - TriPoint Healthcare
OT OASIS C FOLLOW-UP/RECERT - TriPoint Healthcare
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
WEST PENN ALLEGHENY HOME CARE<br />
<strong>FOLLOW</strong>-<strong>UP</strong>/<strong>RECERT</strong><br />
West Penn Allegheny Health System<br />
<strong>OT</strong> <strong>OASIS</strong> C<br />
Billable Non Billable<br />
__________________________________ _________ _______ _______ ________<br />
____________<br />
Patient Name: Last/First MR# Payor Time In Time Out<br />
Date<br />
___________________________________ _________ _________<br />
______________________________<br />
Address-Street/Apt City Zip Code<br />
Physician/Phone #<br />
Previous Contact Info:<br />
Date of Visit: _____/_____/_____<br />
Staff: __________________________________________ Discipline ___________________<br />
Plan for Visit:
MO32-Resumption of Care Date _____/_____/_____ NA-Not Applicable<br />
MO80-Discipline of person completing assessment: 1-RN 2-PT 3-SLP/ST 4-<strong>OT</strong><br />
MO90-Date Assessment completed: ____/____/____<br />
MO100- This Assessment is Currently Being Completed for the Following Reason:<br />
Follow-Up<br />
04-Recertification (Follow-Up) reassessment<br />
05-Other Follow-up<br />
MO110-Episode Timing: Is the Medicare home health payment episode for which this assessment will define a<br />
case mix group an”early”episode or a “later” episode in the patient’s current sequence of adjacent Medicare home<br />
health payment episodes<br />
1-Early<br />
2-Later<br />
UK-Unknown<br />
NA-Not Applicable No Medicare case mix group to be defined by this assessment<br />
M1020 -Primary & (M1022) Other Diagnoses M1024-Payment Diagnoses (OPTIONAL)<br />
Column 1:Sequencing of Dx should reflect the seriousness of each condition & support disciplines & services<br />
provided)<br />
Column 2:The sequencing of these rating may not match the sequencing of the dx. ICD-9 C M/Symptom Control<br />
rating.<br />
Column 3:Complete if V-code in Col 2 is reported in place of a case mix dx).<br />
Column 4:Complete only if V-code in Col 2 is reported in place of a case mix dx that is a multiple coding situation<br />
(e.g. manifestation code).<br />
M1020) Primary diagnosis (V-code allowed) (V-or E-codes N<strong>OT</strong> allowed)<br />
a. ____________________ _____________ a. ______________ a. ________________<br />
M1022-Other Diagnoses (Vor E codes allowed) (V or E codes N<strong>OT</strong> allowed)<br />
b. ____________________ _____________ b. ______________ b. ________________<br />
c. ____________________ _____________ c. ______________ c. ________________<br />
d. ____________________ _____________ d. ______________ d. ________________<br />
e. ____________________ _____________ e. ______________ e. ________________<br />
f. ____________________ _____________ f. ______________ f. ________________<br />
M1030-Therapies the patient receives at home: (Mark all that apply)<br />
1. Intravenous or infusion therapy ( excludes TPN)<br />
2. Parenteral nutrition (PTN or lipids)<br />
3. Enteral nutrition (nasogastric, gastrostomy, jejunoslomy, or any other artificial entry ino the alimentary<br />
canal)<br />
4. None of the above<br />
Temp: __________ _______________<br />
Pulse: __________Radial ___________Apical __________<br />
Regular Irregular At Rest w/Exercise<br />
Blood Pressure: Systolic Diastolic Units Side Position<br />
B/P #1 _______ _______ _______ _______ _______<br />
B/P #2 _______ _______ _______ _______ _______<br />
B/P #3 _______ _______ _______ _______ _______<br />
Respirations: __________ __________ Easy Labored
Patient Name_____________________________________________Date:_____/_____/_____<br />
3<br />
Lung Sounds: Within Normal Limits L Clear R Clear<br />
Left L Diminished L Rales L Rhonchi L wheezes<br />
Right R.Diminished R Rales R Rhonchi R wheezes<br />
Height __________ Pulse Ox #1 _______ __________ At Rest<br />
Weight __________ w/Exercise RA 02<br />
BMI __________ %_________ Pulse Ox #2 _______ ___________ At Rest<br />
BMI=Weight in Pounds divided by w/Exercise RA 02<br />
Height in Inches squared x 703 BMI Notes:<br />
____________________________________________________<br />
to be recorded in whole numbers only.<br />
____________________________________________________<br />
Has the patient had a 10% change in<br />
weight in last 6 Months/____________<br />
Safety Hazards:<br />
No Safety Hazards Structurally Unsound Obstructed Exits/Entrances <br />
Unsafe Mats/Throws<br />
Inadequate Heat Inadequate Lighting Inadequate Plumbing Unsafe Appliances<br />
Lacks Safety Devices Steep Stairs Unsafe Storage of Dangerous Lead Paint<br />
Present<br />
Cluttered Living<br />
Objects/Substances<br />
Arrangements<br />
Other<br />
Fall #1<br />
_____________________ Injury<br />
Location _____________________ MD Notified<br />
____________________________________ Witnessed<br />
Fall #2<br />
_____________________ Injury<br />
Location _____________________ MD Notified<br />
____________________________________ Witnessed<br />
Fall #3<br />
_____________________ Injury<br />
Location _____________________ MD Notified<br />
____________________________________ Witnessed<br />
Reason For Assessment<br />
Admission Recert Post-Fall (Give to Manager when completed)<br />
A. Level of consciousness/Mental Status A. Score: _____<br />
0-Alert and oriented x 3<br />
2-Disoriented x 3 at all times
Patient Name_____________________________________________Date:_____/_____/_____<br />
4<br />
4-Intermittent confusion<br />
B. History of Falls (past 3 months) B. Score _____<br />
0-No falls ( in past 3 months)<br />
2-1-2 falls (in past 3 months)<br />
4-3 or more falls (in past 3 months<br />
C. Ambulation/Elimination Status C. Score _____<br />
0-Ambulatory/continent<br />
2- Chair bound<br />
4-Ambulatory/incontinent<br />
D. Vision Status D. Score: _____<br />
0-Adequate (with or without glasses)<br />
2-Poor (with or without glasses)<br />
4-Legally blind<br />
E. Gait/Balance: to assess the gait/balance, have patient stand on both feet without E. Score: _____<br />
holding onto anything: walk straight forward; walk through a doorway; and<br />
make a turn.<br />
0-Gait/balance normal<br />
1-Balance problem while standing<br />
1-Balance problem while walking<br />
1-Decreased muscular coordination<br />
1-Change in gait pattern when walking through doorway<br />
1-Jerking or unstable when making turns<br />
1-Requires use of assistive device (cane, w/c, furniture..)<br />
F. Orthostatic Changes F. Score: _____<br />
0-No noted drop in blood pressure between lying and standing. No change in cardiac rhythm.<br />
2-Drop 20.<br />
G. Medications: Respond below based on the following types of medications: G. Score: _____<br />
anesthetics, antihistamines, antihypertensives, antiseizure, benzodiazepines,<br />
cathartics, diuretics, hypoglycemics, narcotics, phychotropics, sedatives/hypnotics.<br />
0-None of these medications taken currently on w/in last 7 days<br />
2-Takes 1-2 of these medications currently and/or w/in last 7 days<br />
4-Takes 3-4 of these medications currently and/or w/in 7 days<br />
1-If patient has had a change in medication and/or change in dosage in past 5 days, score + 1 additional point.<br />
H. Medications: Respond below based on the following predisposing conditions: H. Score: ______<br />
hypotension, vertigo, CVA, Parkinson’s disease, loss, of limb(s), seizures, arthritis,<br />
osteoporosis, fractures.<br />
0-None present<br />
2-1-2 present<br />
4-3 or more present<br />
T<strong>OT</strong>AL SCORE: (score of 10 represents High Risk)<br />
______<br />
Patient informed about the safety/falls prevention recommendations listed in the admission packet ____________
Patient Name_____________________________________________Date:_____/_____/_____<br />
5<br />
M1200-Vision (with corrective lenses if the patient usually wears them):<br />
0-Normal vision: sees adequately in most situations; can see medication labels, newsprint<br />
1-Partially impaired: cannot see medication labels or newsprint, but can see obstacles in path, and<br />
the surrounding layout; can count fingers at arm’s length<br />
2-Severely impaired: cannot locate objects without hearing or touching them or patient nonresponsive<br />
M1242-Frequency of Pain: Interfering with patient’s activity or movement:<br />
0-Patient has no pain or pain does not interfere with activity or movement<br />
1-Patient has pain that does not interfere with activity or movement<br />
2-Less often than daily<br />
3-Daily, but not constantly<br />
4-All of the time<br />
Location:<br />
Abdomen Arm Back Chest<br />
Generalized Head/Neck Leg Shoulder Other<br />
Patient Describes Pain as: Ache Burning Dull Sharp Stabbing Throbbing<br />
Pain Intensity Level Now: 0 01 02 03 04 05 06 07 08 09 10<br />
Pain Intensity at Worst: 0 01 02 03 04 05 06 07 08 09 10<br />
Pain Intensity at Best: 0 01 02 03 04 05 06 07 08 09 10<br />
Acceptable Level of Pain: 0 01 02 03 04 05 06 07 08 09 10<br />
Pain Quality:<br />
Bone Nerve Somatic Visceral Other Other<br />
Onset: _______________________________________________________________<br />
Frequency: ___________________________________________________________<br />
Duration: Constant Intermittent Occasional With Movement<br />
Note:<br />
Barriers to Pain Control<br />
Culture Education Philosophy of caregiver Physical<br />
Emotional Spiritual Financial Other
Patient Name_____________________________________________Date:_____/_____/_____<br />
6<br />
Pain Relief measures<br />
Rest Other<br />
Current Meds:<br />
Pain Relief Medications & Response:<br />
Effects of Pain Relief Measures ________<br />
Impact on Functional Activity:<br />
Location:<br />
Abdomen Arm Back Chest<br />
Generalized Head/Neck Leg Shoulder Other<br />
Patient Describes Pain as: Ache Burning Dull Sharp Stabbing Throbbing<br />
Pain Intensity Level Now: 0 01 02 03 04 05 06 07 08 09 10<br />
Pain Intensity at Worst: 0 01 02 03 04 05 06 07 08 09 10<br />
Pain Intensity at Best: 0 01 02 03 04 05 06 07 08 09 10<br />
Acceptable Level of Pain: 0 01 02 03 04 05 06 07 08 09 10<br />
Pain Quality:<br />
Bone Nerve Somatic Visceral Other Other<br />
Onset: ______________________________________________________________<br />
Frequency: __________________________________________________________<br />
Duration:<br />
Note:
Patient Name_____________________________________________Date:_____/_____/_____<br />
7<br />
Barriers to Pain Control<br />
Culture Education Philosophy of caregiver Physical<br />
Emotional Spiritual Financial Other<br />
Pain Relief measures<br />
Rest Other<br />
Current Meds:<br />
Pain Relief Medications & Response:<br />
Effects of Pain Relief Measures ________<br />
Impact on Functional Activity:<br />
Location:<br />
Abdomen Arm Back Chest<br />
Generalized Head/Neck Leg Shoulder Other<br />
Patient Describes Pain as:<br />
Ache Burning Dull Sharp Stabbing Throbbing<br />
Pain Intensity Level Now: 0 01 02 03 04 05 06 07 08 09 10<br />
Pain Intensity at Worst: 0 01 02 03 04 05 06 07 08 09 10<br />
Pain Intensity at Best: 0 01 02 03 04 05 06 07 08 09 10<br />
Acceptable Level of Pain: 0 01 02 03 04 05 06 07 08 09 10
Patient Name_____________________________________________Date:_____/_____/_____<br />
8<br />
Pain Quality:<br />
Bone Nerve Somatic Visceral Other Other<br />
Onset: _________________________________________________________________________<br />
Frequency:<br />
Duration:<br />
Note:<br />
____________________________________________________________________<br />
Constant Intermittent Occasional With Movement<br />
Barriers to Pain Control<br />
Culture Education Philosophy of caregiver Physical<br />
Emotional Spiritual Financial Other<br />
Pain Relief measures<br />
Rest Other<br />
Current Meds:<br />
Pain Relief Medications & Response:<br />
Effects of Pain Relief Measures ________<br />
Impact on Functional Activity:<br />
Sensory Perception: Ability to respond meaningfully to pressure-related<br />
Score<br />
discomfort. 1. Completely Limited __________<br />
2. Very Limited<br />
3. Slightly Limited<br />
4. No Improvement<br />
Moisture Degree to which skin is exposed to moisture. 1. Constantly Moist __________
Patient Name_____________________________________________Date:_____/_____/_____<br />
9<br />
2. Very Moist<br />
3. Occasionally Moist<br />
4. Rarely Moist<br />
Activity: Degree of physical activity 1. Bedfast __________<br />
2. Chairfast<br />
3. Walks Occasionally<br />
4. Walks Frequently<br />
Mobility: Ability to change and control body position. 1. Completely Immobile __________<br />
2. Very Limited<br />
3. Slightly Limited<br />
4. No Limitations<br />
Nutrition: Usual food intake pattern. 1. Very Poor __________<br />
2. Probably Inadequate<br />
3. Adequate<br />
4. Excellent<br />
Friction/Shear: 1. Problem ___________<br />
2. Potential Problem<br />
3. No Apparent Problem<br />
Total Branden Risk Score<br />
_____________<br />
Total Branden Risk Score<br />
_____________<br />
BRADEN SCORING: Patients with a score of 16 or less are considered to be at risk of developing pressure ulcers. (15 or 16 +<br />
low risk; 13 or 14+ moderate risk; 12 or less + high risk)<br />
Do you want to attach the Mini Nutritional (MNA) Assessment as a secondary profile<br />
M1306-Does this patient have a least one Unhealed Pressure Ulcer at Stage 11 or Higher or designated as “unstageable”<br />
0-No (go to M1322)<br />
1-Yes<br />
M1308-Current Numbers of Unhealed (non-epithelialized) Pressure Ulcers at Each Stage: (Enter “0" if none; excludes Stage 1<br />
pressure ulcers)<br />
Column 1<br />
Complete at<br />
SOC/ROC/FU/DC<br />
Stage description<br />
Number Currently<br />
Unhealed pressure ulcers<br />
Present<br />
a. Stage 11: Partial thickness loss of dermis presenting as a shallow open ulcer with red pink wound bed, without slough, May<br />
also present as an intact or open/ruptured serum-filled blister.<br />
Column 1: _______ Column 2: _____<br />
b. Stage 111: Full thickness tissue loss. Subcutaneous fat may be visible but bone, tendon, or muscles are not exposed. Slough<br />
may be present but does not obscure the depth of tissues loss. May include undermining and tunneling.<br />
Column 1: _______ Column 2: _____<br />
c. Stage IV: Full thickness tissue loss with visible bone, tendon, or muscle. Slough or eschar may be present on some parts of the<br />
wound bed. Often includes undermining and tunneling.<br />
Column 1: _______ Column 2: _____<br />
d1. Unstageable: Known or likely but unstageable due to non-removable dressing or device.
Patient Name_____________________________________________Date:_____/_____/_____<br />
10<br />
Column 1: _______ Column 2: _____<br />
d2. Unstageable: Known or likely but unstageable due to coverage of wound bed by slough and/or eschar.<br />
Column 1: _______ Column 2: _____<br />
d3. Unstageable: Suspected deep tissue injury in evolution.<br />
Column 1: _______ Column 2:_____<br />
M1322-Current Number of Stage 1 Pressure Ulcers: Intact skin with non-blanchable redness of a localized area usually over a<br />
bony prominence. The area may be painful, firm, soft, warmer or cooler as compared to adjacent tissue.<br />
0 1 2 3 4 or more<br />
M1324-Stage of Most Problematic Unhealed (Observable) Pressure Ulcer:<br />
1-Stage 1 2-Stage 11 3-Stage 111 4-Stage IV<br />
M1330-Does this patient have a Stasis Ulcer<br />
0-No (Go to M1340)<br />
1-Yes, patient has B<strong>OT</strong>H observable and unobservable stasis ulcers.<br />
2-Yes, patient has observable stasis ulcers ONLY<br />
3-Yes, patient has unobservable stasis ulcers ONLY (known but not observable due to non-removable<br />
dressing) (Go to M1340)<br />
M1332-Current Number of (Observable) Stasis Ulcer(s):<br />
1-One 2-Two 3-Three 4-Four or more<br />
M1334-Status of Most Problematic (Observable) Stasis Ulcer:<br />
0-Newly 1-Fully 2-Early/partial 3-Not healing<br />
epithelialized granulating granulating<br />
M1340-Does this patient have a Surgical Wound<br />
0-No (Go to M1350)<br />
1-Yes, patient has a least one (observable) surgical wound<br />
2- Surgical wound known but not observable due to non-removable dressing (Go to M1350)<br />
M1342-Status of Most Problematic (Observable) Surgical Wound:<br />
0-Newly 1-Fully 2-Early/partial 3-Not healing<br />
epithelialized granulating granulating<br />
M1350-Does this patient have a Skin Lesion or Open Wound, excluding bowel ostomy, other than those described above that<br />
is receiving intervention by the home health agency.<br />
0-No 1-Yes<br />
M1400-When is the patient dyspneic or noticeabley short of breath<br />
0-Patient is not short of breath<br />
1-When walking more than 20 feet, climbing stairs.<br />
2-With Moderate exertion (e.g., while dressing, using commode or bedpan, walking distances less than 20<br />
3-With minimal exertion (while eating, talking or performing other ADLs), or with agitation<br />
4- At rest (during day or night)<br />
M1610-Urinary Incontinence or Urinary Catheter Presence:<br />
0-No Incontinence or catheter (includes anuria or ostomy for urinary drainage) -(Go to M1620)<br />
1-Patient is Incontinent<br />
2-Patient requires a urinary catheter (i.e, external, indwelling, intermittent, suprapubic)-(Go to M1620)<br />
M1620-Bowel Incontinence Frequency:<br />
0-Very rarely or never has bowel incontinence 4-On a daily basis<br />
1-Less than once weekly<br />
5-More often than once daily<br />
2-Once to three times weekly<br />
NA-Patient has ostomy for bowel elimination<br />
3-Four to six times weekly<br />
M1630-Ostomy for Bowel Elimination: Does this patient have an ostomy for bowel elimination that (within the last 14 days): a)<br />
was related to an inpatient facility stay, or b)necessitated a change in medical or treatment<br />
feet
Patient Name_____________________________________________Date:_____/_____/_____<br />
11<br />
regimen:<br />
0-Patient does not have an ostomy for bowel elimination<br />
1-Patient’s ostomy was not related to an inpatient stay and did not necessitate change in medical or<br />
treatment regimen<br />
2-The ostomy was related to an inpatient stay or did necessitate change in medical or treatment regimen<br />
M1810-Current ability to Dress Upper Body safely (with or without dressing aids), including undergarments, pullovers,<br />
front-opening shirts and blouses, managing zippers, buttons, and snaps:<br />
0-Able to get clothes out of closets and drawers, put them on and remove them from the upper body without<br />
assistance.<br />
1-Able to dress upper body without assistance if clothing is laid out or handed to the patient.<br />
2-Someone must help the patient put on upper body clothing.<br />
3-Patient depends entirely upon another person to dress the upper body.<br />
M1820-Current ability to Dress Lower Body (with or without dressing aids) including undergarments, slacks, socks or nylons,<br />
shoes:<br />
0-Able to obtain, put on and remove clothing and shoes without assistance.<br />
1-Able to dress lower body without assistance if clothing is laid out or handed to the patient.<br />
2-someone must help the patient put on undergarments, slacks, socks or nylons, and shoes.<br />
3-Patient depends entirely upon another person to dress the lower body.<br />
M1830-Bathing: Current ability to wash entire body. Excludes grooming (washing face washing hands and shampooing hair):<br />
0-Able to bathe self in shower or tub independently, including getting in and out of tub/shower.<br />
1-With the use of devices, is able to bathe self in shower or tub independently including getting in and out<br />
of tube/shower.<br />
2-Able to bathe in shower or tub with the assistance of anther person:<br />
(a)for intermittent supervision or encouragement or reminders, OR<br />
(b)to get in and out of the shower or tube, OR<br />
(c)for washing difficult to reach areas.<br />
3-Able to participates in bathing self in shower or tub, but requires presence of another person throughout the bath<br />
for assistance or supervision.<br />
4-Unable to participate in bathing self in shower or tub, but able to bathe self independently with or without<br />
the use of devices at the sink, in chair, or on commode.<br />
5-Unable to use the shower or tub, but able to participate in bathing self in bed, at the sink, in bedside chair, or on<br />
commode, with the assistance or supervision of another person throughout the bath.<br />
6-Unable to participate effectively in bathing and is bathed totally by another person.<br />
M1840-Toilet transferring: Current ability to get to and from the toilet or bedside commode safely and transfer on and off<br />
toilet/commode.<br />
0-Able to get to and from the toilet independently with or without a device.<br />
1-When reminded, assisted or supervised by another person, able to get to and from the toilet and transfer.<br />
2-Unable to get to and from the toilet but is able to use a bedside commode (with or without assistance).<br />
3-Unable to get to and from the toilet or bedside commode but is able to use a bedpan/urinal independently.<br />
4-Is totally dependent in toileting<br />
M1850-Transferring: Current ability to move safely from bed to chair, or ability to turn and position self in bed if patient in<br />
bedfast.<br />
0-Able to independently transfer.<br />
1-Able to transfer with minimal human assistance or with use of assistive device.<br />
2-Able to bear weight and pivot during transfer process but unable to transfer self.<br />
3-Unable to transfer self and is unable to bear weight or pivot when transferred by another person.<br />
4- Bedfast, unable to transfer but is able to turn and position self in bed.
Patient Name_____________________________________________Date:_____/_____/_____<br />
12<br />
5-Bedfast, unable to transfer and is unable to turn and position self.<br />
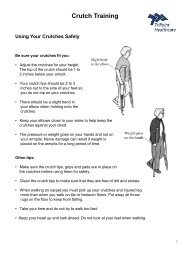
M1860-Ambulation/Locomotion: Current ability to walk safely, once in a standing position, or use a wheelchair, once in a seated<br />
position, on a variety of surfaces.<br />
0-Able to independently walk on even and uneven surfaces and negotiate stairs with or without railings (i.e.<br />
needs no human assistance or assistive device).<br />
1-With the use of a one-handed device (e.g. cane, single crutch, hemi-walker), able to independently walk<br />
on even and uneven surfaces and negotiate stairs with or without railings.<br />
2-Requires use of a two-handed device (e.g. walker or crutches) to walk alone on a level surface and/or<br />
requires human supervision or assistance to negotiate stairs with or steps or uneven surfaces.<br />
3-Able to walk only with the supervision or assistance of another person at all times.<br />
4-Chairfast, unable to ambulate but is able to wheel self independently.<br />
5-Chairfast, unable to ambulate and is unable to wheel self.<br />
6-Bedfast, unable to ambulate or be up in a chair.<br />
M2030-Management of Injectable medications: Patient’s current ability to prepare and take all prescribed injectable medications<br />
reliably and safely, including administration of correct dosage at the appropriate times/intervals. Excludes IV medications.<br />
0-Able to independently take the correct medication(s) and proper dosage(s) at the correct times.<br />
1-Able to take injectable medication(s) at correct times if: (a) individual syringes are prepared in advance by<br />
another person; OR (b)another person develops a drug diary or chart.<br />
2-Able to take medication(s) at the correct times if given reminders by another person based on the<br />
frequency of the injection.<br />
3-Unable to take injectable medications unless administered by another person.<br />
NA-No injectable medications prescribed.<br />
ADL’s: 0- Independent 1. SBA 2. Min A 3. Mod A 4. Max A 5. Dependent enter in first<br />
column.<br />
Grooming (M1800): ________________ ______________________________________________<br />
Dressing UB (M1810): ________________ ______________________________________________<br />
Dressing LB (M1820): ________________ ______________________________________________<br />
Bathing (M1830): ________________ ______________________________________________<br />
Toileting/Transfer (M1840): ________________ ______________________________________________<br />
Toileting/Hygiene (M1845): ________________ ______________________________________________<br />
Tub/Shower (M1850): ________________ ______________________________________________<br />
Feeding/Eating (M1870): ________________ ______________________________________________<br />
IADL’s:<br />
Cooking/Meal Prep (M1880): _________________ _______________________________________________<br />
Laundry: _________________ _______________________________________________<br />
Household Mgmnt: _________________ _______________________________________________<br />
ADL/IADL’s Notes: _________________ _______________________________________________<br />
Leisure: ___________________________________________________________________________________<br />
Social participation: _________________________________________________________________________________<br />
Therapeutic Exercises:
Patient Name_____________________________________________Date:_____/_____/_____<br />
13<br />
PRE Stretching Muscle Re-Ed<br />
Posture:<br />
Endurance:<br />
Sensation:<br />
Muscle Grade<br />
Range of Motion<br />
AROM PROM AAROM<br />
Choose from the following for<br />
muscle grade 0=Zero, 1-, 1=Trace, 1+, 2-, 2=Gravity min, 2+, 3-<br />
Shoulder:<br />
Flexion Left Left ______ ______ _______<br />
Right Right ______ ______ _______<br />
Extension Left Left ______ ______ _______<br />
Right Right ______ ______ _______<br />
Abduction Left Left ______ ______ _______<br />
Right Right ______ ______ _______<br />
Adduction Left Left ______ ______ _______<br />
Right Right ______ ______ _______<br />
Int Rotation Left Left ______ ______ _______<br />
Right Right ______ ______ _______<br />
Ext Rotation Left Left ______ ______ _______<br />
Right Right ______ ______ _______<br />
Elbow/Forearm<br />
Flexion Left Left ______ ______ _______<br />
Right Right ______ ______ _______<br />
Extension Left Left ______ ______ _______<br />
Right Right ______ ______ _______<br />
Supination Left Left ______ ______ _______
Patient Name_____________________________________________Date:_____/_____/_____<br />
14<br />
Right Right ______ ______ _______<br />
Pronation Left Left ______ ______ _______<br />
Right Right ______ ______ _______<br />
Wrist<br />
Flexion Left Left ______ ______ _______<br />
Right Right ______ ______ _______<br />
Extension Left Left ______ ______ _______<br />
Right Right ______ ______ _______<br />
Ulnar Deviation Left Left ______ ______ _______<br />
Right Right ______ ______ _______<br />
Radical Deviation Left Left ______ ______ _______<br />
Right Right ______ ______ _______<br />
Thumbs<br />
MP Flexion Left Left ______ ______ _______<br />
Right Right ______ ______ _______<br />
IP Extension Left Left ______ ______ _______<br />
Right Right ______ ______ _______<br />
Abduction Left Left ______ ______ _______<br />
Right Right ______ ______ _______<br />
Extension Left Left ______ ______ _______<br />
Right Right ______ ______ ________<br />
Opposition Left Left ______ ______ ________<br />
Right Right ______ ______ ________<br />
Left Fingers Right<br />
Index Middle Ring Little Little Ring Middle Index<br />
MP Flex <br />
PIP Flex <br />
DIP Flex <br />
Abd <br />
Tip-DPC <br />
Functional Hand Strength<br />
Trial #1 Trial #2 Trial #3 Trial #1 Trial #2 Trial #3<br />
Grip <br />
<br />
Tip Pinch <br />
<br />
Lateral Pinch
Patient Name_____________________________________________Date:_____/_____/_____<br />
15<br />
<br />
3 Jaw Chuck <br />
<br />
Patient<br />
CG/Other Status Comments<br />
ADL ____________________________________________<br />
Techniques ____________________________________________<br />
Energy ____________________________________________<br />
Conservation ____________________________________________<br />
HEP ____________________________________________<br />
<br />
____________________________________________<br />
Safety ____________________________________________<br />
Measures ____________________________________________<br />
Community ____________________________________________<br />
Resources ____________________________________________<br />
Use of ____________________________________________<br />
Adaptive<br />
Equipment _____________________________________________<br />
Other _______________________________________<br />
<br />
_______________________________________<br />
M2200-Therapy Need: In the home health plan of care for the Medicare payment episode for which this assessment will define a<br />
case mix group, what is the indicated need for therapy visits (total of reasonable and necessary physical, occupational, and<br />
speech-language pathology visits combined) (Enter zero “000" if no therapy visits indicated.)<br />
Number of therapy visits indicated (total of physical, occupational and speech-language<br />
pathology combined).<br />
<br />
NA-Not applicable: No case mix group defined by this assessment.<br />
Homebound Limitations:<br />
Bed Bound Chair bound Medically restricted to home Other<br />
Unable to ambulate Unable to ambulate None<br />
more than 10ft<br />
more than 20ft<br />
Requires Assistance:<br />
Frequent rest periods Ambulance to leave home Assist of 1 person to ambulate/transfer<br />
Assist of 2 people to Mechanical device for transfer Requires assistance due to mental confusion None<br />
ambulate/transfer<br />
Patient requires following assistive device(s)<br />
Cane Pronged Walker Walker<br />
Wheeled walker Wheelchair Crutches<br />
Specialized Orthotics Prosthesis Oxygen
Patient Name_____________________________________________Date:_____/_____/_____<br />
16<br />
Slideboard None Other<br />
Note:<br />
With activity of leaving home the patient may experience:<br />
Dizziness/vertigo Angina/chest pain Pain<br />
Swelling Respiratory distress/ Unsteady gait/Frequent falls/<br />
dyspnea/SOB<br />
Mental confusion<br />
Serious risk of infection Incontinence of urine<br />
Incontinence of stool None Other<br />
poor balance<br />
Homebound status is primarily due to:<br />
Infected/Drainage/Large/Painful wound Profound generalized weakness Morbid obesity<br />
Orthopedic condition Cardiac condition Neurologic condition<br />
Lung condition Immunosupression Psychological impairment<br />
Peripheral vascular disease Urinary condition Bowel condition<br />
None<br />
Other<br />
Note:<br />
CHHA Name<br />
______________________________________________________________________________<br />
Agency<br />
________________________________________________________________________________________________<br />
Schedule<br />
Orientation to Care<br />
Care Plan Instruction Given<br />
Services Supervised<br />
Services Evaluated<br />
_______/_______/_______Next Scheduled Supervisory Visit<br />
Review of Vulnerabilities:<br />
None Noted Cognition Impairment Substance Abuse
Patient Name_____________________________________________Date:_____/_____/_____<br />
17<br />
Sensory Deficit Impaired Mobility Functional Limitations<br />
Environmental Concerns Dependent upon Caregiver<br />
Other:<br />
Rehab Potential: _____________________________<br />
To Achieve Goals by<br />
Next Visit Date<br />
_______/_______/_______<br />
_______/_______/_______<br />
Plan:<br />
Phone Call Made to: ________________________________________<br />
Details:<br />
____________________________________________________________________________________________<br />
____<br />
Visit Narrative:<br />
To use this form: 1) Select an Active Problem. Based upon this selection, 2) select Active Goals & Interventions 3)<br />
Check “Add Selected G/I” to populate the G/I Addressed This visit text box 4) Return to the Active Problem, select<br />
new Problem 5) Select new G/I 6) Re-check the “Add Selected” box<br />
Active Problems<br />
Active Goals:<br />
Add Selected Goals
Patient Name_____________________________________________Date:_____/_____/_____<br />
18<br />
Goals Addressed This Visit<br />
Active Interventions:<br />
Add Selected intervention<br />
Interventions Addressed This Visit
Patient Name_____________________________________________Date:_____/_____/_____<br />
19<br />
MOO10-CMS Certification Number 397076<br />
MOO14-Branch State PA<br />
MOO16-Branch ID Number (N)<br />
MOO18-National Provider ID 1811997315<br />
MOO20-Patient ID Number<br />
MOO30 Start of care date _______/_______/_______<br />
MOO40-Patient Name (First):____________________(Last): _______________________ (MI): ____<br />
MOO50-Patient State of Residence____________________<br />
MOO60-Patient Zip Code ____________<br />
MOO63-Medicare Number _________________<br />
(Including suffix, if any)<br />
NA-No Medicare<br />
MOO64-Social Security Number ____________<br />
UK-Unknown or Not Available<br />
MOO65-Medicaid Number_________________
Patient Name_____________________________________________Date:_____/_____/_____<br />
20<br />
NA-No Medicaid<br />
MOO66-Birth Date _______/_______/_______<br />
MOO69- 1-Male 2-Female<br />
MO150-Current Payment Sources for Home Care: (Mark all that apply.)<br />
0-None; no charge for current services<br />
9-Private HMO/managed care<br />
1-Medicare (traditional fee-for-service)<br />
10-Self-pay<br />
2-Medicare (HMO/managed care)<br />
11-Other (specify) __________________<br />
3-Medicaid (traditional fee-for-service)<br />
4-Medicaid (HMO/managed care)<br />
5-Workers’ compensation<br />
6-Title programs (e.g., title III, V, or XX)<br />
7-Other government (e.g., CHAMPUS, VA, etc.)<br />
8-Private insurance<br />
Occupational Therapist Signature _______________________________________________________________________