Spring 2010 - SSM Cardinal Glennon Children's Medical Center
Spring 2010 - SSM Cardinal Glennon Children's Medical Center
Spring 2010 - SSM Cardinal Glennon Children's Medical Center
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
10<br />
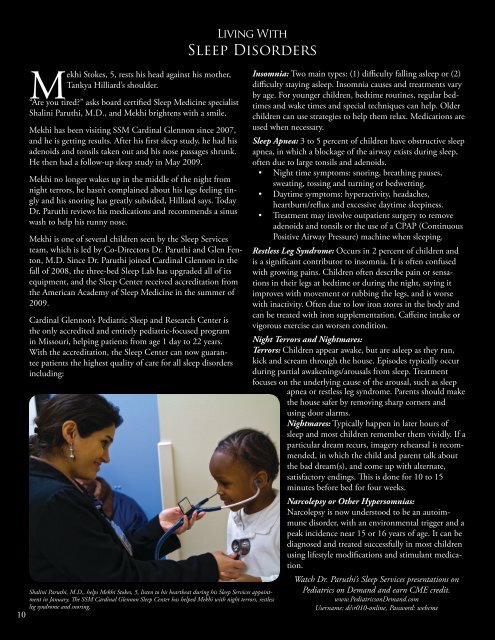
Mekhi Stokes, 5, rests his head against his mother,<br />
Tankya Hilliard’s shoulder.<br />
“Are you tired” asks board certified Sleep Medicine specialist<br />
Shalini Paruthi, M.D., and Mekhi brightens with a smile.<br />
Mekhi has been visiting <strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong> since 2007,<br />
and he is getting results. After his first sleep study, he had his<br />
adenoids and tonsils taken out and his nose passages shrunk.<br />
He then had a follow-up sleep study in May 2009.<br />
Mekhi no longer wakes up in the middle of the night from<br />
night terrors, he hasn’t complained about his legs feeling tingly<br />
and his snoring has greatly subsided, Hilliard says. Today<br />
Dr. Paruthi reviews his medications and recommends a sinus<br />
wash to help his runny nose.<br />
Mekhi is one of several children seen by the Sleep Services<br />
team, which is led by Co-Directors Dr. Paruthi and Glen Fenton,<br />
M.D. Since Dr. Paruthi joined <strong>Cardinal</strong> <strong>Glennon</strong> in the<br />
fall of 2008, the three-bed Sleep Lab has upgraded all of its<br />
equipment, and the Sleep <strong>Center</strong> received accreditation from<br />
the American Academy of Sleep Medicine in the summer of<br />
2009.<br />
<strong>Cardinal</strong> <strong>Glennon</strong>’s Pediatric Sleep and Research <strong>Center</strong> is<br />
the only accredited and entirely pediatric-focused program<br />
in Missouri, helping patients from age 1 day to 22 years.<br />
With the accreditation, the Sleep <strong>Center</strong> can now guarantee<br />
patients the highest quality of care for all sleep disorders<br />
including:<br />
Living With<br />
Sleep Disorders<br />
Shalini Paruthi, M.D., helps Mekhi Stokes, 5, listen to his heartbeat during his Sleep Services appointment<br />
in January. The <strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong> Sleep <strong>Center</strong> has helped Mekhi with night terrors, restless<br />
leg syndrome and snoring.<br />
Insomnia: Two main types: (1) difficulty falling asleep or (2)<br />
difficulty staying asleep. Insomnia causes and treatments vary<br />
by age. For younger children, bedtime routines, regular bedtimes<br />
and wake times and special techniques can help. Older<br />
children can use strategies to help them relax. Medications are<br />
used when necessary.<br />
Sleep Apnea: 3 to 5 percent of children have obstructive sleep<br />
apnea, in which a blockage of the airway exists during sleep,<br />
often due to large tonsils and adenoids.<br />
• Night time symptoms: snoring, breathing pauses,<br />
sweating, tossing and turning or bedwetting.<br />
• Daytime symptoms: hyperactivity, headaches,<br />
heartburn/reflux and excessive daytime sleepiness.<br />
• Treatment may involve outpatient surgery to remove<br />
adenoids and tonsils or the use of a CPAP (Continuous<br />
Positive Airway Pressure) machine when sleeping.<br />
Restless Leg Syndrome: Occurs in 2 percent of children and<br />
is a significant contributor to insomnia. It is often confused<br />
with growing pains. Children often describe pain or sensations<br />
in their legs at bedtime or during the night, saying it<br />
improves with movement or rubbing the legs, and is worse<br />
with inactivity. Often due to low iron stores in the body and<br />
can be treated with iron supplementation. Caffeine intake or<br />
vigorous exercise can worsen condition.<br />
Night Terrors and Nightmares:<br />
Terrors: Children appear awake, but are asleep as they run,<br />
kick and scream through the house. Episodes typically occur<br />
during partial awakenings/arousals from sleep. Treatment<br />
focuses on the underlying cause of the arousal, such as sleep<br />
apnea or restless leg syndrome. Parents should make<br />
the house safer by removing sharp corners and<br />
using door alarms.<br />
Nightmares: Typically happen in later hours of<br />
sleep and most children remember them vividly. If a<br />
particular dream recurs, imagery rehearsal is recommended,<br />
in which the child and parent talk about<br />
the bad dream(s), and come up with alternate,<br />
satisfactory endings. This is done for 10 to 15<br />
minutes before bed for four weeks.<br />
Narcolepsy or Other Hypersomnias:<br />
Narcolepsy is now understood to be an autoimmune<br />
disorder, with an environmental trigger and a<br />
peak incidence near 15 or 16 years of age. It can be<br />
diagnosed and treated successfully in most children<br />
using lifestyle modifications and stimulant medication.<br />
Watch Dr. Paruthi’s Sleep Services presentations on<br />
Pediatrics on Demand and earn CME credit.<br />
www.PediatricsonDemand.com<br />
Username: ds\r010-online, Password: webcme