Spring 2010 - SSM Cardinal Glennon Children's Medical Center
Spring 2010 - SSM Cardinal Glennon Children's Medical Center
Spring 2010 - SSM Cardinal Glennon Children's Medical Center
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong> Children’s <strong>Medical</strong> <strong>Center</strong><br />
<strong>Spring</strong> <strong>2010</strong><br />
www.cardinalglennon.com<br />
FOCUS ON<br />
Pediatrics<br />
MEDICAL NEWS FROM <strong>SSM</strong> CARDINAL GLENNON CHILDREN’S MEDICAL CENTER<br />
AND THE DEPARTMENT OF PEDIATRICS, SAINT LOUIS UNIVERSITY SCHOOL OF MEDICINE<br />
SM
ON THE COVER<br />
Medin Gets His “Picture Taken”<br />
Kristin Casten, RT, helps Medin Grabic, 5, get his<br />
a chest x-ray before his appointment for asthma care at<br />
<strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong> Children’s <strong>Medical</strong> <strong>Center</strong>.<br />
During a typical first-time pulmonary visit, patients<br />
receive an extensive history report, physical exam, lung<br />
function studies and visits with a pulmonologist, nurse<br />
and respiratory therapist. Children often get a chest<br />
x-ray and all patients are taught the proper usage of an<br />
inhaler, nebulizer and peak flow meter.<br />
FOCUS ON<br />
Pediatrics<br />
SM<br />
Editor In Chief<br />
Sherlyn Hailstone<br />
President<br />
<strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong><br />
Children’s <strong>Medical</strong> <strong>Center</strong><br />
<strong>Medical</strong> Editor<br />
Kenneth Haller, MD<br />
Associate Professor of Pediatrics<br />
Saint Louis University<br />
School of Medicine<br />
Editor<br />
Andrew Sutton<br />
Physician Services Manager<br />
<strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong><br />
Children’s <strong>Medical</strong> <strong>Center</strong><br />
Writer & Designer<br />
Katelyn Ideus<br />
Physician Services Assistant<br />
<strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong><br />
Children’s <strong>Medical</strong> <strong>Center</strong><br />
For comments and suggestions, please email FocusOnPeds@ssmhc.com.
Living a Better Life<br />
<strong>Cardinal</strong> <strong>Glennon</strong> Division of Pulmonary Medicine<br />
ACC <strong>Medical</strong> Director and pulmonologist Gary Albers, M.D., examines Natalie Nickels, 7, during her January check up for cystic fibrosis. Find out more about cystic fibrosis on page 11.<br />
6
The blue hallway of <strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong><br />
Children’s <strong>Medical</strong> <strong>Center</strong>’s ACC is<br />
buzzing this morning. Blake Noyes, M.D.,<br />
Gary Albers, M.D., and Anthony Rejent, M.D.,<br />
are writing notes, ordering chest x-rays and performing<br />
exams on their young patients.<br />
Some of the Division’s particular interests include:<br />
• Vocal cord dysfunction<br />
• Abnormalities of surfactant protein metabolism<br />
• Impact of CPAP on children with sleep-disordered<br />
breathing<br />
Photography by Stew Smith<br />
But the hustle of the morning doesn’t stop Dr.<br />
Noyes, Director of the Division of Pulmonary<br />
Medicine, from grabbing the stool in a patient’s<br />
room, pulling it beside the exam table where the<br />
child is sitting and asking about his or her latest<br />
activities.<br />
Sara Rohrbough, 17, tells Dr. Noyes that she<br />
performed in the color guard during the half time<br />
show at the Capitol One<br />
Bowl, and Andria Leezy<br />
talks about her 18-monthold<br />
son’s latest game of<br />
running laps around the<br />
dining room table.<br />
The ease of the conversation<br />
isn’t surprising<br />
considering the time Dr.<br />
Noyes has spent with each<br />
of these patients. Sara is<br />
recovering from a bout of<br />
complicated pneumonia<br />
and Mark Leezy, Jr., was<br />
born with cystic fibrosis.<br />
But no matter the history,<br />
each patient who visits one<br />
of the pulmonary clinics<br />
receives compassionate,<br />
individualized care.<br />
The Division of Pulmonary<br />
Medicine holds clinics for<br />
asthma, general pulmonary<br />
medicine, cystic fibrosis<br />
and sleep disorders. Each patient is seen by a physician,<br />
nurse, respiratory therapist, dietitian and<br />
social worker if necessary.<br />
These clinics provide comprehensive care for all<br />
respiratory disorders, including:<br />
• Asthma<br />
• Complicated pneumonia<br />
• Cystic fibrosis<br />
• Chronic cough<br />
• Recurrent pneumonias<br />
• Recurrent or persistent wheezing<br />
• Sleep disorders<br />
Blake Noyes, M.D., examines cystic fibrosis patient<br />
Mark Leezy, Jr., 18 months.<br />
Dr. Noyes suggests referral to a pediatric pulmonary<br />
specialist for all of the following patients:<br />
• Cough for more than 4-6 weeks<br />
• Three or more documented pneumonias in<br />
one year<br />
• Wheezing unresponsive to routine asthma<br />
therapy<br />
• Respiratory symptoms associated with poor<br />
growth<br />
Providing the care are <strong>Cardinal</strong><br />
<strong>Glennon</strong>’s experienced<br />
pulmonologists. Dr. Rejent<br />
served as the Director of the<br />
Cystic Fibrosis <strong>Center</strong> for 40<br />
years and helped advance the<br />
services for pediatric cystic<br />
fibrosis patients nationwide.<br />
In the summer of 2009, Dr.<br />
Rejent retired from this position<br />
and passed leadership to<br />
Dr. Noyes.<br />
“The one word that would<br />
describe Dr. Noyes is ‘outstanding,’”<br />
Dr. Rejent says of<br />
his successor. “He is outstanding<br />
in his leadership as<br />
a Division Director, in his<br />
organizational abilities and<br />
in his communication with<br />
every member of the Division<br />
from top to bottom, as<br />
well as his patients.”<br />
Along side Dr. Noyes is Dr.<br />
Albers, who also serves as the <strong>Medical</strong> Director<br />
of the ACC, and Robert Wilmott, M.D., who<br />
sees patients while serving as <strong>Cardinal</strong> <strong>Glennon</strong>’s<br />
Chairman of the Department of Pediatrics. Shalini<br />
Paruthi, M.D., and Glen Fenton, M.D., co-direct<br />
<strong>Cardinal</strong> <strong>Glennon</strong>’s recently-accredited Sleep<br />
<strong>Center</strong>.<br />
“These faculty have a great understanding of these<br />
diseases and this translates into superb care at the<br />
bedside,” Dr. Rejent says. “I continue to learn a<br />
lot from all of them, and we are fortunate to have<br />
them at <strong>Cardinal</strong> <strong>Glennon</strong>.”<br />
7
Marissa Lowe, 18, is used to the injections. She even<br />
smiles occasionally as Kathy Forcelledo, RN, administers<br />
one into each arm.<br />
After several visits to various institutions, Marissa was brought<br />
to <strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong> when she was three years old.<br />
Within a week, <strong>Cardinal</strong> <strong>Glennon</strong> diagnosed her with chronic<br />
asthma. <strong>Cardinal</strong> <strong>Glennon</strong> also found relief for Marissa<br />
through the monthly injections.<br />
“When I was younger, I couldn’t go out and play,” Marissa<br />
says. “But now I feel really good. There have been less hospital<br />
visits over the last couple years.”<br />
Though asthma seems common in children, it is not a benign<br />
diagnosis, and when it goes under-treated or untreated it can<br />
cause permanent airway remodeling, says Susan Mason, RN,<br />
PCNS.<br />
Signs and symptoms of asthma include wheezing, chronic<br />
cough and respiratory distress.<br />
There are several ways to control asthma including:<br />
• Inhaled steroids • Environmental measures<br />
• Albuterol • Avoidance of allergens<br />
• Leukotriene<br />
modifiers<br />
• Elimination of environmental<br />
tobacco smoke exposure<br />
Living With<br />
asthma<br />
However, if these treatments do not help, or when any of the<br />
following occur, it is time to refer to a pediatric pulmonary<br />
specialist:<br />
• Frequent hospital admissions<br />
• Frequent emergency room visits<br />
• Poor control of symptoms<br />
• Any hospital admission where an ICU stay is included<br />
Kathy Forcelledo, RN, administers Marissa Lowe’s monthly injection for chronic asthma.<br />
8<br />
Once brought to <strong>Cardinal</strong> <strong>Glennon</strong>’s asthma clinic, each<br />
patient undergoes an extensive history and physical exam, as<br />
well as lung function studies and often a chest x-ray. A plan<br />
is developed and reviewed, and patients are taught the proper<br />
inhaler or nebulizer and peak flow use. They are then evaluated<br />
by a physician, nurse and respiratory therapist.<br />
“Our quality benchmark is among the best in the National<br />
Association of Children’s Hospitals and Related Institutions<br />
(NACHRI),” says Division Director of Pulmonary Medicine<br />
Blake Noyes, M.D. “The availability of pulmonary to work<br />
with pediatric allergy and immunology specialists is an important<br />
service, and we’ve seen short inpatient stays relative to<br />
NACHRI standards due to our care.”<br />
To consult with one of <strong>Cardinal</strong> <strong>Glennon</strong>’s pulmonary specialists<br />
on any condition, please call the <strong>Cardinal</strong> <strong>Glennon</strong><br />
Access <strong>Center</strong> at 1-888-229-2424.<br />
Blake Noyes, M.D., examines Jazmine Griffin, 11 months, during an asthma check up.<br />
Jazmine was brought in for pneumonia at three months of age but was diagnosed with<br />
asthma.
Living With<br />
Complicated Pneumonia<br />
During her January visit, Sara Rohrbough, 17, completes a pulmonary function test with Pat Lewis, RRT. <strong>Cardinal</strong> <strong>Glennon</strong> helped Sara through complicated pneumonia in the fall.<br />
On New Years Day <strong>2010</strong>, Sara Rohrbough, 17, performed<br />
in the color guard at the half time show of<br />
the Capital One Bowl in Orlando, FL.<br />
Today, Jan. 15, however, she is back in St. Louis at <strong>SSM</strong><br />
<strong>Cardinal</strong> <strong>Glennon</strong>.<br />
Though not one to get sick, Sara got the flu in late October<br />
and stayed sick for more than a month. Finally, she gave in<br />
to her shortness of breath, cough and racing heart and visited<br />
the emergency department at <strong>SSM</strong> St. Clare Health <strong>Center</strong> in<br />
Fenton, MO.<br />
After an exam and chest x-ray, Sara was told a surgeon would<br />
have to drain the fluid that accumulated between her lung<br />
and chest wall through a tube in her back. The mucus, however,<br />
was so thick a pediatric surgeon would have to perform<br />
the procedure.<br />
“I was so scared and it was so overwhelming,” Sara says of<br />
being rolled to the operating room at <strong>Cardinal</strong> <strong>Glennon</strong>. “But<br />
then I just woke up, and it was over and everything was fine.”<br />
Sara suffered from a pneumonia complicated by the development<br />
of an empyema, which is a rare complication relative to<br />
all pneumonias. This type of illness often requires admission<br />
and IV antibiotics. It may also require either a chest tube or<br />
surgical approach to evacuate the fluid.<br />
After her surgery, Sara spent five days at <strong>Cardinal</strong> <strong>Glennon</strong>.<br />
She returned for three follow up visits and will come back this<br />
summer for what Blake Noyes, M.D., anticipates to be her<br />
last visit. During this final check up, Sara will receive a chest<br />
x-ray, an exam and lung function tests.<br />
Then, hopefully, she won’t be back at <strong>Cardinal</strong> <strong>Glennon</strong> any<br />
time soon.<br />
“It wasn’t one of the greatest things<br />
because I had to have surgery. But if<br />
you are going to get stuck in a<br />
hospital, it’s best to get stuck in a good<br />
one like <strong>Cardinal</strong> <strong>Glennon</strong>.”<br />
— Sara Rohrbough, 17<br />
9
10<br />
Mekhi Stokes, 5, rests his head against his mother,<br />
Tankya Hilliard’s shoulder.<br />
“Are you tired” asks board certified Sleep Medicine specialist<br />
Shalini Paruthi, M.D., and Mekhi brightens with a smile.<br />
Mekhi has been visiting <strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong> since 2007,<br />
and he is getting results. After his first sleep study, he had his<br />
adenoids and tonsils taken out and his nose passages shrunk.<br />
He then had a follow-up sleep study in May 2009.<br />
Mekhi no longer wakes up in the middle of the night from<br />
night terrors, he hasn’t complained about his legs feeling tingly<br />
and his snoring has greatly subsided, Hilliard says. Today<br />
Dr. Paruthi reviews his medications and recommends a sinus<br />
wash to help his runny nose.<br />
Mekhi is one of several children seen by the Sleep Services<br />
team, which is led by Co-Directors Dr. Paruthi and Glen Fenton,<br />
M.D. Since Dr. Paruthi joined <strong>Cardinal</strong> <strong>Glennon</strong> in the<br />
fall of 2008, the three-bed Sleep Lab has upgraded all of its<br />
equipment, and the Sleep <strong>Center</strong> received accreditation from<br />
the American Academy of Sleep Medicine in the summer of<br />
2009.<br />
<strong>Cardinal</strong> <strong>Glennon</strong>’s Pediatric Sleep and Research <strong>Center</strong> is<br />
the only accredited and entirely pediatric-focused program<br />
in Missouri, helping patients from age 1 day to 22 years.<br />
With the accreditation, the Sleep <strong>Center</strong> can now guarantee<br />
patients the highest quality of care for all sleep disorders<br />
including:<br />
Living With<br />
Sleep Disorders<br />
Shalini Paruthi, M.D., helps Mekhi Stokes, 5, listen to his heartbeat during his Sleep Services appointment<br />
in January. The <strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong> Sleep <strong>Center</strong> has helped Mekhi with night terrors, restless<br />
leg syndrome and snoring.<br />
Insomnia: Two main types: (1) difficulty falling asleep or (2)<br />
difficulty staying asleep. Insomnia causes and treatments vary<br />
by age. For younger children, bedtime routines, regular bedtimes<br />
and wake times and special techniques can help. Older<br />
children can use strategies to help them relax. Medications are<br />
used when necessary.<br />
Sleep Apnea: 3 to 5 percent of children have obstructive sleep<br />
apnea, in which a blockage of the airway exists during sleep,<br />
often due to large tonsils and adenoids.<br />
• Night time symptoms: snoring, breathing pauses,<br />
sweating, tossing and turning or bedwetting.<br />
• Daytime symptoms: hyperactivity, headaches,<br />
heartburn/reflux and excessive daytime sleepiness.<br />
• Treatment may involve outpatient surgery to remove<br />
adenoids and tonsils or the use of a CPAP (Continuous<br />
Positive Airway Pressure) machine when sleeping.<br />
Restless Leg Syndrome: Occurs in 2 percent of children and<br />
is a significant contributor to insomnia. It is often confused<br />
with growing pains. Children often describe pain or sensations<br />
in their legs at bedtime or during the night, saying it<br />
improves with movement or rubbing the legs, and is worse<br />
with inactivity. Often due to low iron stores in the body and<br />
can be treated with iron supplementation. Caffeine intake or<br />
vigorous exercise can worsen condition.<br />
Night Terrors and Nightmares:<br />
Terrors: Children appear awake, but are asleep as they run,<br />
kick and scream through the house. Episodes typically occur<br />
during partial awakenings/arousals from sleep. Treatment<br />
focuses on the underlying cause of the arousal, such as sleep<br />
apnea or restless leg syndrome. Parents should make<br />
the house safer by removing sharp corners and<br />
using door alarms.<br />
Nightmares: Typically happen in later hours of<br />
sleep and most children remember them vividly. If a<br />
particular dream recurs, imagery rehearsal is recommended,<br />
in which the child and parent talk about<br />
the bad dream(s), and come up with alternate,<br />
satisfactory endings. This is done for 10 to 15<br />
minutes before bed for four weeks.<br />
Narcolepsy or Other Hypersomnias:<br />
Narcolepsy is now understood to be an autoimmune<br />
disorder, with an environmental trigger and a<br />
peak incidence near 15 or 16 years of age. It can be<br />
diagnosed and treated successfully in most children<br />
using lifestyle modifications and stimulant medication.<br />
Watch Dr. Paruthi’s Sleep Services presentations on<br />
Pediatrics on Demand and earn CME credit.<br />
www.PediatricsonDemand.com<br />
Username: ds\r010-online, Password: webcme
Living With<br />
Cystic Fibrosis<br />
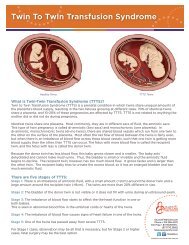
At 18 months, Mark Leezy, Jr., never stays still. With<br />
his blond hair matted down from sweat and his cheeks<br />
red from his last sprint across <strong>SSM</strong> <strong>Cardinal</strong> <strong>Glennon</strong>’s<br />
ACC lobby, it’s hard believe Mark spent the first three months<br />
of his life in <strong>Cardinal</strong> <strong>Glennon</strong>’s NICU.<br />
He was born with a meconium perforation, an intestinal obstruction<br />
caused by mucus build up in his bowels, and a red<br />
flag for cystic fibrosis. When an ultrasound early in Andria<br />
Leezy’s pregnancy showed the meconium perforation, Andria<br />
and her husband, Mark Leezy, Sr., were tested and found to<br />
be carriers of cystic fibrosis. But it wasn’t until Mark Jr. was<br />
born that it was confirmed he had the chronic lung disease.<br />
“I guess we are one of the lucky ones because we’ve known<br />
and been able to treat him early,” Andria says. “Some parents<br />
don’t find out until their kids are much older.”<br />
Though a life-threatening disease, cystic fibrosis can go misdiagnosed<br />
as chronic cough, asthma or pneumonia, thus going<br />
untreated.<br />
However, as of December 2009, all states are required to perform<br />
newborn screenings for cystic fibrosis, as early detection<br />
can greatly improve a child’s quality of life.<br />
An infant with a positive screening should be immediately<br />
referred to a Cystic Fibrosis Foundation accredited center like<br />
<strong>Cardinal</strong> <strong>Glennon</strong>. However, the threshold for testing older<br />
children should remain low as infants can be missed on the<br />
newborn screen.<br />
Kevin Powell, M.D., exams cystic fibrosis inpatient Alando Harris, 15.<br />
Through the leadership of Anthony Rejent, M.D., <strong>Cardinal</strong><br />
<strong>Glennon</strong> has been at the forefront of quality improvements,<br />
such as infant screenings, for the last 40 years. In 2004, <strong>Cardinal</strong><br />
<strong>Glennon</strong> was one of the first centers to initiate quality<br />
improvement efforts for the delivery of care and processes.<br />
“I want to continue the impressive quality efforts initiated under<br />
Dr. Rejent’s leadership through an ongoing review of our<br />
patient registry data and combining that with care recommendations<br />
put forward by the Cystic Fibrosis Foundation,” says<br />
Blake Noyes, M.D., who became the director of the Cystic<br />
Fibrosis <strong>Center</strong> after Dr. Rejent’s retirement in the summer of<br />
2009.<br />
But beyond delivery and processes, is the care provided by<br />
<strong>Cardinal</strong> <strong>Glennon</strong>’s pulmonologists.<br />
Alando Harris, 15, has spent several days and nights at <strong>Cardinal</strong><br />
<strong>Glennon</strong> battling illness due to the condition. He also<br />
suffers from cystic fibrosis related diabetes mellitus.<br />
Alando has worked with all of <strong>Cardinal</strong> <strong>Glennon</strong>’s<br />
pulmonologists including Dr. Noyes, Dr. Rejent and<br />
Dr. Gary Albers.<br />
“Dr. Albers always tries to make Alando laugh because<br />
he is so quiet,” Alando’s mother Tanya Bridges said.<br />
“Somehow, Dr. Albers succeeds with one of his silly<br />
jokes.”<br />
And while Bridges appreciates the work of the physicians,<br />
nurses and staff, it seems the care givers are just<br />
as touched by the effort of the patients and families<br />
they care for.<br />
Judy Brussatti, RN, CPNP, shows Mark Leezy, Jr., 18 months, a book about breathing during his visit<br />
to the <strong>Cardinal</strong> <strong>Glennon</strong> Cystic Fibrosis <strong>Center</strong>.<br />
“You become so involved with the whole family,”<br />
Judy Brusatti, RN, CPNP says. “I stay in this because<br />
the diagnosis and treatment are challenging, but also<br />
because caring for these children has made me a better<br />
nurse, a better person and a better parent. They are<br />
truly inspiring.”<br />
11
Q&A<br />
Blake Noyes, M.D.<br />
Division Director of<br />
Pulmonary Medicine<br />
12<br />
Q: How do the years of experience of the faculty in your<br />
division affect the care you are able to provide<br />
A: Within the division, there is a collective experience of more<br />
than 150 years of taking care of patients with pulmonary<br />
disorders, so there is little that the pulmonary physicians have<br />
not encountered in their careers.<br />
The faculty also routinely collaborate on the approach and<br />
care of patients with complicated respiratory disorders, which<br />
provides each patient with a broad range of experiences.<br />
Finally, the division has had terrific stability over the years<br />
with our nursing, respiratory therapy and social services staff,<br />
which provides a tremendous amount of continuity for the<br />
patients and families.<br />
Q: Why did you choose to specialize in pediatric<br />
pulmonary medicine<br />
A: I was always drawn to patients with cystic fibrosis and<br />
always admired their resolute determination and courage in<br />
the face of a disease which, at the time, was often fatal before<br />
adulthood. The opportunity to follow patients and families<br />
over a long time was always appealing to me as well.<br />
Q: What is the most difficult part of your job<br />
A: Without a doubt, experiencing the death of a child from a<br />
respiratory disorder. The impact on the parents and extended<br />
family members and the loss of the tremendous potential all<br />
children have is always extraordinarily difficult. Making a<br />
diagnosis of cystic fibrosis and giving that news to the parents<br />
is always emotionally challenging since the effect on family<br />
dynamics, lifestyle and child rearing can be so devastating.<br />
To reach DR. Noyes<br />
Please Call:<br />
(314) 268-6439.
Pulmonary Medicine<br />
Faculty<br />
Gary M. Albers, M.D.<br />
<strong>Medical</strong> Director of Ambulatory Care<br />
M.D.: Saint Louis University, St. Louis, MO<br />
Pediatrics/Internal Medicine Internship: Saint Louis University, <strong>Cardinal</strong><br />
<strong>Glennon</strong> Children’s <strong>Medical</strong> <strong>Center</strong>, St. Louis, MO<br />
Pediatrics/Internal Medicine Residency: Saint Louis University, <strong>Cardinal</strong><br />
<strong>Glennon</strong> Children’s <strong>Medical</strong> <strong>Center</strong>, St. Louis, MO<br />
Pediatric Pulmonary Medicine Fellowship: University of North Carolina,<br />
Chapel Hill, NC<br />
Blake E. Noyes, M.D.<br />
Division Director of Pulmonary Medicine and Director of Cystic Fibrosis <strong>Center</strong><br />
M.D.: Saint Louis University, St. Louis, MO<br />
Pediatric Internship: St. Louis University, <strong>Cardinal</strong> <strong>Glennon</strong> Children’s<br />
<strong>Medical</strong> <strong>Center</strong>, St. Louis, MO<br />
Pediatric Residency: Saint Louis University, <strong>Cardinal</strong> <strong>Glennon</strong> Children’s<br />
<strong>Medical</strong> <strong>Center</strong>, St. Louis, MO<br />
Pulmonary Fellowship: University of Pittsburgh, Children’s Hospital of<br />
Pittsburgh, Pittsburgh, PA<br />
Research Scholar: University of Pittsburgh, Children’s Hospital of Pittsburgh,<br />
Pittsburgh, PA<br />
Shalini Paruthi, M.D.<br />
Co-Director of Sleep Services<br />
M.D.: University of Missouri-Kansas City, Kansas City, MO<br />
Preliminary Year in Internal Medicine: Saint Joseph Mercy Hospital, Ann<br />
Arbor, MI<br />
Residency in Internal Medicine: University of Michigan <strong>Medical</strong> <strong>Center</strong>,<br />
Ann Arbor, MI<br />
Fellowship in Sleep Medicine: University of Michigan <strong>Medical</strong> <strong>Center</strong>,<br />
Ann Arbor, MI<br />
Kevin T. Powell, M.D.<br />
M.S. in Chemical Engineering: Massachusetts Institute of Technology,<br />
Boston, MA<br />
PhD in <strong>Medical</strong> Engineering: MIT/Harvard <strong>Medical</strong> School, Boston, MA<br />
M.D.: Tufts University School of Medicine, Boston, MA<br />
Residency in Pediatrics: University of Wisconsin, Madison, WI<br />
Anthony J. Rejent, M.D.<br />
M.D.: Creighton University School of Medicine, Omaha, NE<br />
Internship: St. Vincent’s Hospital and <strong>Medical</strong> <strong>Center</strong>, Toledo, OH<br />
Pediatric Residency: Saint Louis University, <strong>Cardinal</strong> <strong>Glennon</strong> Children’s<br />
<strong>Medical</strong> <strong>Center</strong>, St. Louis, MO<br />
Chief Resident, Division of Pediatrics: United States Air Force Hospital,<br />
Columbus, MS<br />
Robert W. Wilmott, M.D.<br />
IMMUNO Professor and Chair of the Department of Pediatrics<br />
M.D.: University College Hospital <strong>Medical</strong> School, London, England<br />
Residency: University College Hospital, London, England<br />
Fellowship in Pulmonary Medicine: Hospital for Sick Children and Institute<br />
of Child Health, London, England<br />
Pediatrics on Demand<br />
March 15<br />
“Vocal Cord Dysfunction”<br />
Blake Noyes, M.D.<br />
March 29<br />
“Managing the Child with a Chronic Cough”<br />
Robert Wilmott, M.D.<br />
www.pediatricsondemand.com<br />
Username: ds\r010-online<br />
Password: webcme<br />
13