Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
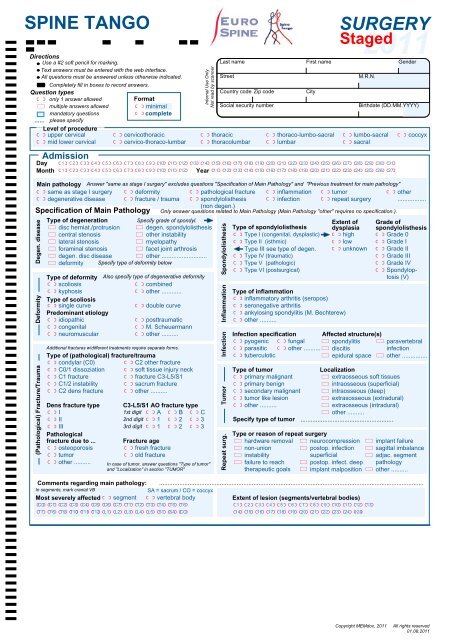
SPINE TANGO<br />
Directions<br />
Use a #2 soft pencil for marking.<br />
Text answers must be entered with the web interface.<br />
All questions must be answered unless otherwise indicated.<br />
)I Completely fill in boxes to record answers.<br />
Question types<br />
I <strong>Form</strong>at<br />
J<br />
only 1 answer allowed<br />
multiple answers allowed I minimal<br />
mandatory questions<br />
complete<br />
...... please specify<br />
Level of procedure<br />
I upper cervical I cervicothoracic<br />
mid lower cervical<br />
cervico-thoraco-lumbar<br />
Day<br />
Month<br />
I<br />
I<br />
IIIIIIIIIIIIIIIIIIIIIIIIIIIIIII<br />
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31<br />
IIIIIIIIIIII<br />
1 2 3 4 5 6 7 8 9 10 11 12 IIIIIIIIIIIIIIIII<br />
11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27<br />
I<br />
I<br />
Internal Use Only<br />
Not read by scanner<br />
Year<br />
Last name<br />
Street<br />
Country code Zip code<br />
Social security number<br />
thoracic<br />
thoracolumbar<br />
SURGERY<br />
2011<br />
Gender<br />
Main pathology Answer "same as stage I surgery" excludes questions "Specification of Main Pathology" and "Previous treatment for main pathology"<br />
same as stage I surgery deformity<br />
pathological fracture inflammation tumor<br />
other<br />
I degenerative disease I fracture / trauma I spondylolisthesis I infection I repeat surgery .................<br />
(non degen.)<br />
Only answer questions related to Main Pathology (Main Pathology "other" requires no specification.).<br />
Specification of Main Pathology<br />
Degen. disease<br />
(Pathological) Fracture/Trauma Deformity<br />
J<br />
J<br />
Type of degeneration<br />
Specify grade of spondyl.<br />
disc herniat./protrusion degen. spondylolisthesis<br />
J central stenosis J other instability<br />
lateral stenosis<br />
myelopathy<br />
J foraminal stenosis J facet joint arthrosis<br />
degen. disc disease<br />
other ...........................<br />
J deformity Specify type of deformity below<br />
Type of deformity Also specify type of degenerative deformity<br />
scoliosis<br />
combined<br />
I kyphosis I other ............<br />
Type of scoliosis<br />
I single curve I double curve<br />
Predominant etiology<br />
I idiopathic I posttraumatic<br />
congenital<br />
M. Scheuermann<br />
I neuromuscular I other ..........<br />
Additional fractures w/different treatments require separate forms.<br />
Type of (pathological) fracture/trauma<br />
I condylar (C0) I C2 other fracture<br />
C0/1 dissoziation<br />
soft tissue injury neck<br />
I C1 fracture I fracture C3-L5/S1<br />
C1/2 instability<br />
sacrum fracture<br />
I C2 dens fracture I other ..........<br />
I<br />
Dens fracture type<br />
I<br />
I II<br />
III<br />
Pathological<br />
fracture due to ...<br />
I osteoporosis<br />
tumor<br />
I other ..........<br />
I<br />
I<br />
I<br />
C3-L5/S1 AO fracture type<br />
1st digit A B C<br />
2nd digit<br />
1<br />
2<br />
3<br />
3rd digit I 1 I 2 I 3<br />
I<br />
Fracture age<br />
fresh fracture<br />
I old fracture<br />
In case of tumor, answer questions "Type of tumor"<br />
and "Localization" in section "TUMOR"<br />
Spondylolisthesis<br />
Inflammation<br />
Infection<br />
Tumor<br />
Repeat surg.<br />
I<br />
I<br />
First name<br />
thoraco-lumbo-sacral<br />
lumbar<br />
I<br />
Staged<br />
I<br />
lumbo-sacral<br />
sacral<br />
Comments regarding main pathology: .............................................................................................................................................................<br />
In segments, mark cranial VB<br />
SA = sacrum / CO = coccyx<br />
Most severely affectedI<br />
segment I vertebral body<br />
Extent of lesion (segments/vertebral bodies)<br />
IIIIIIIIIIIIII<br />
C0 C1 C2 C3 C4 C5 C6 C7 T1 T2 T3 T4 T5 T6 IIIIIIIIIIIII<br />
1 2 3 4 5 6 7 8 9 10 11 12 13<br />
IIIIIIIIIIIIII<br />
T7<br />
Admission<br />
I<br />
T8<br />
T9 T10 T11 T12 L1<br />
L2<br />
L3<br />
I<br />
L4<br />
L5<br />
S1<br />
SA<br />
CO<br />
I<br />
I<br />
I<br />
I<br />
City<br />
Type of spondylolisthesis<br />
Type I (congenital, dysplastic)<br />
Type II (isthmic)<br />
Type III see type of degen.<br />
Type IV (traumatic)<br />
Type V (pathologic)<br />
Type VI (postsurgical)<br />
Type of inflammation<br />
inflammatory arthritis (seropos)<br />
I seronegative arthritis<br />
ankylosing spondylitis (M. Bechterew)<br />
I other ..........<br />
I<br />
I<br />
I<br />
J<br />
J<br />
M.R.N.<br />
Birthdate (DD.MM.YYYY)<br />
J<br />
J<br />
I<br />
I<br />
Type of tumor<br />
Localization<br />
primary malignant<br />
extraosseous soft tissues<br />
I primary benign J intraosseous (superficial)<br />
secondary malignant<br />
intraosseous (deep)<br />
I tumor like lesion J extrasosseous (extradural)<br />
other ..........<br />
extraosseous (intradural)<br />
J other ..........<br />
Specify type of tumor .......................................................<br />
coccyx<br />
Infection specification Affected structure(s)<br />
pyogenic fungal spondylitis paravertebral<br />
I parasitic I other .......... J discitis<br />
infection<br />
tuberculotic<br />
epidural space other ...............<br />
J<br />
J<br />
Type or reason of repeat surgery<br />
hardware removal neurocompression<br />
J non-union J postop. infection<br />
instability<br />
superficial<br />
J failure to reach J postop. infect. deep<br />
therapeutic goals<br />
implant malposition<br />
IIIIIIIIIIII<br />
14<br />
15<br />
16<br />
17<br />
18<br />
19<br />
20<br />
21<br />
22<br />
Extent of<br />
dysplasia<br />
I high<br />
low<br />
I unknown<br />
23<br />
24<br />
>24<br />
J<br />
J<br />
J<br />
Grade of<br />
spondylolisthesis<br />
I Grade 0<br />
Grade I<br />
I Grade II<br />
Grade III<br />
I Grade IV<br />
Spondyloptosis<br />
(V)<br />
implant failure<br />
sagittal imbalance<br />
adjac. segment<br />
pathology<br />
other ..........<br />
Copyright MEMdoc, 2011<br />
All rights reserved<br />
01.08.2011
SPINE TANGO<br />
Surgery<br />
Staged<br />
Internal Use Only - Not read by scanner<br />
Surgeon ........................... Assistant ...........................<br />
IIIIIIIIIIIIIIIIIIIIIIIIIIIIIII<br />
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31<br />
IIIIIIIIIIII<br />
Day<br />
Month 1 2 3 4 5 6 7 8 9 10 11 12 YearIIIIIIIIII<br />
11 12 13 14 15 16 17 18 19 20<br />
SURGERY<br />
Page 2 of 2<br />
J<br />
J<br />
J<br />
Therapeutic goals<br />
axial pain relief<br />
peripheral pain relief<br />
functional improvement<br />
motor improvement<br />
sensory improvement<br />
bladder/sex function improv.<br />
J<br />
J<br />
J<br />
spinal stabilization<br />
stop deformity progression<br />
prophylactic decompression<br />
cosmetic improvement<br />
diagnostic measures<br />
other ..............<br />
I<br />
I<br />
I<br />
Anterior access<br />
no anterior access<br />
transoral<br />
anterolateral<br />
cervicothorac. anterolat.<br />
cervicothorac.<br />
w/sternotomy<br />
I<br />
I<br />
I<br />
thoracotomy<br />
thoraco-phrenico-lumbotomy<br />
retroperitoneal<br />
transperitoneal<br />
trans-psoas (XLIF)<br />
other ......................................<br />
I<br />
Components Description not needed if SEDICO implant tracking is used.<br />
none<br />
Supplier:<br />
I<br />
...............................................................<br />
with description<br />
w/o description Article name: .........................................................<br />
For article numbers or multiple implants use form "Implant documentation" @ www.eurospine.org<br />
I<br />
I<br />
Posterior access<br />
no posterior access<br />
midline<br />
paramedian<br />
posterolateral<br />
I<br />
I<br />
percutaneous<br />
para-coccygeal (AxiALIF)<br />
other<br />
....................<br />
I<br />
I<br />
I<br />
J<br />
J<br />
J<br />
Decompression<br />
none<br />
anterior<br />
specify ...<br />
posterior}<br />
Location in spine, choose at least one!<br />
J<br />
Fusion promoting measu.<br />
none<br />
J anterior<br />
posterior}<br />
specify ...<br />
Location in spine, choose at least one!<br />
J<br />
J<br />
Stabilization rigid<br />
none<br />
anterior<br />
specify ...<br />
posterior}<br />
Location in spine, choose at least one!<br />
I<br />
Surgical Measures<br />
J<br />
J<br />
J<br />
J<br />
J<br />
J<br />
J<br />
J<br />
J<br />
I<br />
Surgeon credentials Morbidity state<br />
specialized spine<br />
unknown<br />
board certif. orthopaedic I ASA1 (no disturbance)<br />
board certified neuro<br />
ASA2 (mild/moderate)<br />
orthopaedic in training I ASA3 (severe)<br />
neuro in training<br />
ASA4 (life threatening)<br />
other .................... I ASA5 (moribund)<br />
Prophylaxis<br />
none J thrombembolism J other<br />
infection<br />
ossification<br />
J<br />
discectomy partial/total<br />
vertebrectomy partial<br />
vertebrectomy full<br />
osteotomy<br />
interbody fusion (ALIF)<br />
interbody fusion (PLIF)<br />
interbody fusion (TLIF)<br />
interbody fusion (XLIF)<br />
Note: "anterior" / "posterior" refers to location of MEASURES in the spine, NOT to access!<br />
J<br />
J<br />
interbody stabil. with cage<br />
interbody stabil. with auto-/allograft<br />
vertebral body replacement by cage<br />
plates<br />
pedicle screws with rod<br />
I<br />
Extent of surgery - indicate as: (from cranial to caudal)<br />
segments from C0 C1 C2 C3 C4 C5 C6<br />
I vertebral bodies toIC0<br />
C1 C2 C3 C4 C5 C6<br />
J<br />
J<br />
other interbody fusion<br />
posterolat. fusion<br />
posterior fusion<br />
other ................<br />
J<br />
J<br />
J<br />
J<br />
J<br />
J<br />
J<br />
Fusion material<br />
none<br />
autol. bone harvested<br />
autol. bone locally procured<br />
allog. bone<br />
facet screws<br />
transarticular screw C1-C2<br />
laminar hooks with rod<br />
pedicle hooks with rod<br />
lateral mass screw with rod<br />
J<br />
J<br />
J<br />
J<br />
bone subst.<br />
cement<br />
BMP or similar<br />
other .............<br />
odontoid screws<br />
laminar screws<br />
other<br />
............................<br />
SA = sacrum / CO = coccyx<br />
IIIIIIIIIIIIIIIIIIIIIIIIIIII<br />
C7 T1 T2 T3 T4 T5 T6 T7 T8 T9 T10 T11 T12 L1 L2 L3 L4 L5 S1 SA CO<br />
IIIIIIIIIIIIIIIIIIIIIIIIIII<br />
C7<br />
J<br />
J<br />
Technology<br />
conventional<br />
MISS/LISS<br />
loops<br />
endoscope<br />
I<br />
I<br />
Blood loss<br />
unknown<br />
< 100 ml<br />
100 - 500 ml<br />
laminotomy<br />
hemi-laminectomy<br />
laminectomy<br />
facet joint resec. partial<br />
T1<br />
T2<br />
T3<br />
T4<br />
T5<br />
J<br />
J<br />
I<br />
I<br />
T6<br />
CASS<br />
microscope<br />
neuromonitoring<br />
other ................<br />
500 - 1000 ml<br />
1000 - 2000 ml<br />
> 2000 ml<br />
T7<br />
J<br />
J<br />
T8<br />
I<br />
I<br />
I<br />
facet joint resection full<br />
sequestrectomy<br />
flavectomy<br />
flavotomy<br />
T9 T10 T11 T12 L1<br />
Operation time<br />
unknown<br />
< 1 hr.<br />
1-2 hrs.<br />
2-3 hrs.<br />
3-4 hrs.<br />
J<br />
L2<br />
J<br />
L3<br />
I<br />
I<br />
I<br />
J<br />
J<br />
L4<br />
4-5 hrs.<br />
5-6 hrs.<br />
6-8 hrs.<br />
8-10 hrs.<br />
> 10 hrs.<br />
Blood transfusion<br />
none >=2 units<br />