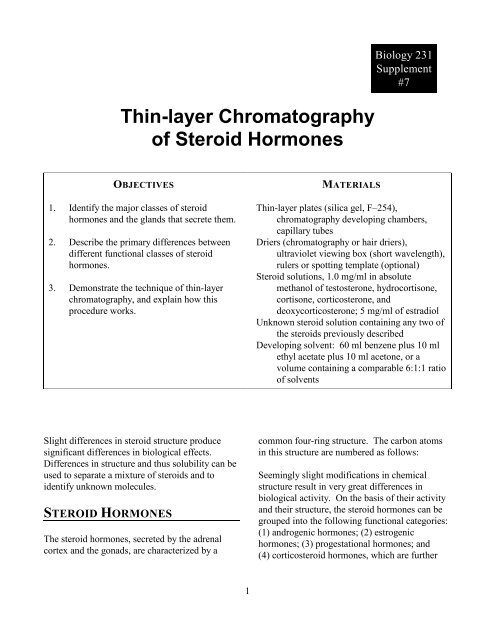
Thin-layer Chromatography of Steroid Hormones
Thin-layer Chromatography of Steroid Hormones
Thin-layer Chromatography of Steroid Hormones
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Thin</strong>-<strong>layer</strong> <strong>Chromatography</strong><br />
<strong>of</strong> <strong>Steroid</strong> <strong>Hormones</strong><br />
Biology 231<br />
Supplement<br />
#7<br />
OBJECTIVES<br />
1. Identify the major classes <strong>of</strong> steroid<br />
hormones and the glands that secrete them.<br />
2. Describe the primary differences between<br />
different functional classes <strong>of</strong> steroid<br />
hormones.<br />
3. Demonstrate the technique <strong>of</strong> thin-<strong>layer</strong><br />
chromatography, and explain how this<br />
procedure works.<br />
MATERIALS<br />
<strong>Thin</strong>-<strong>layer</strong> plates (silica gel, F–254),<br />
chromatography developing chambers,<br />
capillary tubes<br />
Driers (chromatography or hair driers),<br />
ultraviolet viewing box (short wavelength),<br />
rulers or spotting template (optional)<br />
<strong>Steroid</strong> solutions, 1.0 mg/ml in absolute<br />
methanol <strong>of</strong> testosterone, hydrocortisone,<br />
cortisone, corticosterone, and<br />
deoxycorticosterone; 5 mg/ml <strong>of</strong> estradiol<br />
Unknown steroid solution containing any two <strong>of</strong><br />
the steroids previously described<br />
Developing solvent: 60 ml benzene plus 10 ml<br />
ethyl acetate plus 10 ml acetone, or a<br />
volume containing a comparable 6:1:1 ratio<br />
<strong>of</strong> solvents<br />
Slight differences in steroid structure produce<br />
significant differences in biological effects.<br />
Differences in structure and thus solubility can be<br />
used to separate a mixture <strong>of</strong> steroids and to<br />
identify unknown molecules.<br />
STEROID HORMONES<br />
The steroid hormones, secreted by the adrenal<br />
cortex and the gonads, are characterized by a<br />
common four-ring structure. The carbon atoms<br />
in this structure are numbered as follows:<br />
Seemingly slight modifications in chemical<br />
structure result in very great differences in<br />
biological activity. On the basis <strong>of</strong> their activity<br />
and their structure, the steroid hormones can be<br />
grouped into the following functional categories:<br />
(1) androgenic hormones; (2) estrogenic<br />
hormones; (3) progestational hormones; and<br />
(4) corticosteroid hormones, which are further<br />
1
divided into the subcategories <strong>of</strong> glucocorticoids<br />
and mineralocorticoids.<br />
The androgenic hormones are characterized<br />
structurally by the fact that they are nineteencarbon<br />
steroids and functionally by the fact that<br />
they promote the development <strong>of</strong> secondary male<br />
sex characteristics. The most potent androgenic<br />
hormone secreted by the testes is testosterone.<br />
Although the primary source <strong>of</strong> androgens is the<br />
testes, the adrenal cortex also secretes small<br />
amounts. Large amounts <strong>of</strong> androgens are present<br />
in the plasma <strong>of</strong> persons suffering from tumors <strong>of</strong><br />
the testes. Adrenal hyperplasia (Cushing’s<br />
syndrome) and tumors <strong>of</strong> the adrenal cortex can<br />
also cause excessive androgen levels, which can<br />
have a masculinizing effect in females.<br />
Testosterone and the other androgens are secreted<br />
in the testes by the interstitial Leydig cells. This<br />
secretion is stimulated by a gonadotrophic<br />
hormone <strong>of</strong> the anterior pituitary, interstitial cellstimulating<br />
hormone (ICSH), which is identical to<br />
luteinizing hormone (LH).<br />
Although the structural difference between the<br />
androgens and the estrogens is seemingly<br />
slight—the estrogens are eighteen-carbon steroids<br />
with three points <strong>of</strong> unsaturation (double bonds,<br />
see appendix 1) in the A ring—the difference in<br />
biological effects is pleasantly pronounced. The<br />
chief estrogenic hormone is estradiol.<br />
The estrogens are normally secreted in cyclically<br />
increasing and decreasing amounts by the<br />
ovaries, reaching a peak at about the time <strong>of</strong><br />
ovulation. The cyclical secretion <strong>of</strong> estrogens is<br />
stimulated by the cyclical secretion <strong>of</strong> a<br />
gonadotrophic hormone <strong>of</strong> the anterior pituitary,<br />
follicle-stimulating hormone (FSH).<br />
Abnormally high concentrations <strong>of</strong> circulating<br />
estrogenic hormones may be due to tumors <strong>of</strong> the<br />
adrenal cortex or the gonads. This can have a<br />
feminizing effect in males.<br />
In the normal female cycle, the estrogens<br />
stimulate growth and development <strong>of</strong> the inner<br />
lining <strong>of</strong> the uterus (the endometrium). The final<br />
maturation <strong>of</strong> the endometrium is under the<br />
control <strong>of</strong> the hormone progesterone, secreted in<br />
the phase <strong>of</strong> the cycle after ovulation (luteal<br />
phase) by the corpus luteum <strong>of</strong> the ovaries. The<br />
cyclical secretion <strong>of</strong> progesterone is stimulated<br />
by the cyclical secretion <strong>of</strong> luteinizing hormone<br />
(LH) from the anterior pituitary. (LH and ICSH<br />
are two names for the same hormone, which has<br />
different effects in the two sexes.)<br />
During pregnancy, the placenta secretes<br />
increasing amounts <strong>of</strong> progesterone, which is<br />
correlated with the development <strong>of</strong> the fetus.<br />
Progesterone is a twenty-one-carbon steroid.<br />
2
The glucocorticoids, secreted by the zona<br />
fasciculata and the zona reticularis, stimulate the<br />
breakdown <strong>of</strong> muscle proteins and the conversion<br />
<strong>of</strong> amino acids into glucose (gluconeogenesis).<br />
The secretions <strong>of</strong> the z. fasciculata and the<br />
z. reticularis are stimulated by the anterior<br />
pituitary hormone, adrenocorticotrophin<br />
(ACTH). The most potent glucocorticoids are<br />
corticosterone, hydrocortisone (cortisol), and<br />
cortisone.<br />
The steroid hormones <strong>of</strong> the adrenal cortex<br />
(corticosteroids) also contain twenty-one carbons<br />
but differ from progesterone by the presence <strong>of</strong><br />
three or more oxygen groups. These hormones<br />
are divided into two functional classes and are<br />
secreted by two functionally distinct regions <strong>of</strong> the<br />
cortex.<br />
The mineralocorticoids, secreted by the zona<br />
glomerulosa, are involved in the regulation <strong>of</strong><br />
sodium and potassium balance. The secretion <strong>of</strong><br />
aldosterone (a mineralocorticoid) is stimulated by<br />
angiotensin II and is thus regulated by the<br />
secretion <strong>of</strong> renin from the kidneys. The most<br />
potent mineralocorticoids are aldosterone and, to<br />
a lesser degree, deoxycorticosterone (DOC).<br />
An abnormal secretion <strong>of</strong> the mineralocorticoids<br />
is usually associated with hypertension and may<br />
be produced by primary aldosteronism or by<br />
secondary aldosteronism due to low blood<br />
sodium, high blood potassium, hypovolemia,<br />
cardiac failure, kidney failure, or cirrhosis <strong>of</strong> the<br />
3
liver. An increased secretion <strong>of</strong> the<br />
glucocorticoids is found in Cushing’s syndrome<br />
(adrenal hyperplasia), pregnancy, and stress due to<br />
disease, surgery, and burns.<br />
carry others. If the process is halted before all<br />
the steroids have been washed <strong>of</strong>f the top <strong>of</strong> the<br />
plate, some will have migrated farther from the<br />
origin than others.<br />
THIN-LAYER<br />
CHROMATOGRAPHY<br />
In this exercise, an attempt will be made to<br />
identify two unknown steroids that are present in<br />
the same solution. To do this, you must<br />
(1) separate and (2) identify these steroids by<br />
comparing their behavior with that <strong>of</strong> known<br />
steroids.<br />
Since each steroid has a different structure, each<br />
will have a different solubility (ability to be<br />
dissolved) in a given solvent. These differences<br />
will be used to separate and identify the steroids<br />
on a thin-<strong>layer</strong> plate.<br />
The thin-<strong>layer</strong> plate consists <strong>of</strong> a thin <strong>layer</strong> <strong>of</strong><br />
porous material (in this procedure, silica gel) that<br />
is coated on one side <strong>of</strong> a plastic glass, or<br />
aluminum plate. The solutions <strong>of</strong> steroids are<br />
applied on different spots <strong>of</strong> the plate (a procedure<br />
called “spotting”), and the plate is placed in a<br />
solvent bath with the spots above the solvent.<br />
If this chromatography were repeated using the<br />
same steroids and the same solvent, the final<br />
pattern (chromatogram) would be the same as<br />
obtained previously. In other words, the distance<br />
that a given steroid migrates in a given solvent,<br />
relative to the solvent front, can be used as an<br />
identifying characteristic <strong>of</strong> that steroid. We can<br />
give this identity a numerical value by calculating<br />
the distance the steroid traveled relative to the<br />
front (the R value) follows.<br />
f<br />
We can identify the unknown steroid by<br />
comparing its R f value in a given solvent with the<br />
Rf values <strong>of</strong> known steroids in the same solvent.<br />
As the solvent creeps up the plate by capillary<br />
action, it will wash the steroids <strong>of</strong>f their original<br />
spots (the origin) and carry them upward toward<br />
the other end <strong>of</strong> the plate. Since the solubility <strong>of</strong><br />
each steroid is different, it takes longer for the<br />
solvent to wash and carry some than to wash and<br />
4
CLINICAL SIGNIFICANCE<br />
The chromatographic separation and<br />
identification <strong>of</strong> steroid hormones has revealed<br />
much about endocrine physiology that is clinically<br />
useful. It was learned, for example, that the<br />
placenta secretes estrogens that are more polar<br />
(water soluble) than the predominant ovarian<br />
estrogen, estradiol. These polar placental<br />
estrogens—estriol and estetrol—are now<br />
measured clinically during pregnancy to assess the<br />
health <strong>of</strong> the placenta.<br />
<strong>Chromatography</strong> <strong>of</strong> androgens recovered from<br />
their target tissues (such as the prostate) has<br />
revealed that these tissues convert testosterone<br />
into other products. Further, these products<br />
appear to be more biologically active (more<br />
androgenic) than testosterone itself. Testosterone<br />
secreted by the testes is thus a prehormone, which<br />
is enzymatically converted in the target tissue into<br />
more active products — dihydrotestosterone<br />
(DHT), in many tissues. Males who have a<br />
congenital deficiency in 5-reductase, the enzyme<br />
responsible for this conversion, therefore, show<br />
many symptoms <strong>of</strong> androgen deficiency even<br />
though their testes secrete large amounts <strong>of</strong><br />
testosterone.<br />
Procedure<br />
1. Using a pencil, make a tiny notch on the left margin <strong>of</strong> the thin-<strong>layer</strong> plate, approximately<br />
1½ inches from the bottom. The origin <strong>of</strong> all the spots will lie on an imaginary line extending<br />
across the plate from this notch.<br />
2. Using a capillary pipette, carefully spot steroid solution 1 (estradiol) about ½ inch in from the lefthand<br />
margin <strong>of</strong> the plate, along the imaginary line. Repeat this procedure, using the same steroid at<br />
the same spot, two more times. Allow the spot to dry between applications.<br />
3. Repeat step 2 with each <strong>of</strong> the remaining steroid solutions (2, testosterone; 3, hydrocortisone;<br />
4, cortisone; 5, corticosterone; 6, deoxycorticosterone; 7, unknown), spotting each steroid<br />
approximately ½ inch to the right <strong>of</strong> the previous steroid, along the imaginary line.<br />
4. Observe the steroid spots at the origin under an ultraviolet lamp. (Note: Do not look directly at the<br />
UV light.)<br />
5
5. Place the thin-<strong>layer</strong> plates in a developing chamber filled with solvent (benzene/ethyl<br />
acetate/acetone, 6:1:1), and allow the chromatogram to develop for 1 hour.<br />
6. Remove the thin-<strong>layer</strong> plate, dry, and observe it under the UV light. Using a pencil, outline the<br />
spots observed under the UV light.<br />
7. In the laboratory report below, record the R f values <strong>of</strong> the known steroids, and determine the<br />
steroids present in the unknown solution.<br />
DATA FROM EXERCISE 7<br />
Record your data in the table below and calculate the R f value <strong>of</strong> each spot.<br />
<strong>Steroid</strong><br />
Distance<br />
to Front<br />
Distance<br />
to Spot<br />
Rf<br />
1. Estradiol<br />
2. Testosterone<br />
3. Hydrocortisone<br />
4. Cortisone<br />
5. Corticosterone same<br />
6. Deoxycorticosterone<br />
7. Unknown 1<br />
Unknown 2<br />
6