Cancer Referral form - Breast
Cancer Referral form - Breast
Cancer Referral form - Breast
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
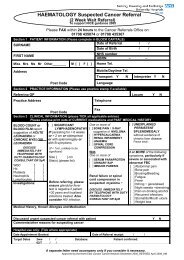
BREAST Suspected <strong>Cancer</strong> <strong>Referral</strong><br />
(2 Week Wait <strong>Referral</strong>)<br />
To support NICE guidance 2005<br />
Please FAX within 24 hours to the <strong>Cancer</strong> <strong>Referral</strong>s Office on:<br />
01708 435074 or 01708 435367<br />
Section 1 PATIENT INFORMATION (Please complete in BLOCK CAPITALS)<br />
SURNAME<br />
Date of <strong>Referral</strong> / /<br />
Date of Birth / /<br />
FIRST NAME<br />
Miss Mrs Ms Mr Other: _________ M [ ] F [ ] Home Tel.<br />
NHS number<br />
UBRN - -<br />
Address<br />
Mobile/Daytime Tel.<br />
Post Code<br />
Language<br />
Section 2 PRACTICE INFORMATION (Please use practice stamp if available)<br />
Transport Y N Interpreter Y N<br />
Referring GP Locum Y N<br />
Practice Address<br />
Telephone<br />
Fax<br />
Post Code<br />
Section 3 CLINICAL INFORMATION (please TICK all applicable entries)<br />
Please enclose print outs of CURRENT medications and PAST MEDICAL HISTORY<br />
Solid lump<br />
Nodularity<br />
Inverted nipple<br />
Skin infiltration or peau d’orange<br />
SIGNS AND SYMPTOMS<br />
Any age<br />
[ ] with discrete, hard lump with fixation, + / - skin tethering<br />
[ ] unilateral eczematous skin or nipple change that does not<br />
respond to topical treatment<br />
[ ] nipple distortion of recent onset<br />
[ ] spontaneous unilateral bloody nipple discharge<br />
[ ] skin distortion/ tethering/ discolouration/ nodule/ ulceration<br />
Female aged > 30 years<br />
[ ] with a discrete lump persisting after period / post menopause<br />
[ ] with fixed, hard or enlarging lump<br />
Male aged > 50 years<br />
[ ] with a unilateral, firm subareolar mass + / - nipple distortion<br />
or associated skin changes<br />
Duration of Signs<br />
and Symptoms and<br />
further in<strong>form</strong>ation<br />
PLEASE REFER PATIENTS WHOSE ONLY SYMPTOM IS BREAST PAIN VIA THE ‘OTHER SYMPTOMS’ PROFORMA<br />
Medical History, Known Allergies and Medication<br />
Family History<br />
Discussed urgent suspected cancer referral with patient Y<br />
Comments/other reasons for suspecting cancer<br />
N<br />
Hospital use only: (Tick where appropriate)<br />
Date Appointment Booked: / / Date of <strong>Referral</strong> receipt: / /<br />
Target Dates 2ww / / Database: Patient confirmed:<br />
62/7 / /<br />
A separate letter need accompany only if you consider it necessary.<br />
Approved by the North East London <strong>Cancer</strong> Network April 2006_REVISED April 2009_AM
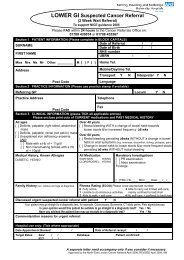
LOCAL CONTACT DETAILS<br />
<strong>Cancer</strong> Waiting Times Co-ordinator Tel. 01708 435169 Queen’s Hospital<br />
CRITERIA 1 FOR URGENT SUSPECTED CANCER REFERRAL<br />
Please FAX the referral <strong>form</strong> within 24 hours<br />
Refer a patient who presents with symptoms suggestive of breast cancer to a team specialising in the<br />
management of breast cancer.<br />
In general:<br />
Convey optimism about the effectiveness of breast cancer treatments and survival of breast<br />
cancer patients<br />
Discuss the in<strong>form</strong>ation and support needs of your patient and respond sensitively<br />
Encourage all patients, including women over 50 years old, to be breast aware²<br />
Always take the patient’s history into account. For example, it may be appropriate, in discussion with<br />
a specialist, to agree referral within a few days in a patient who reports a lump or other symptom that<br />
has been present for several months.<br />
Urgently refer patients with:<br />
• of any age with a discrete, hard lump with fixation, with or without skin tethering<br />
• of any age, with previous breast cancer, who present with a further lump or suspicious symptoms<br />
• female, aged 30 years and older with a discrete lump that persists after their next period, or presents after<br />
menopause<br />
• with unilateral eczematous skin or nipple change that does not respond to topical treatment<br />
• with nipple distortion of recent onset<br />
• with spontaneous unilateral bloody nipple discharge<br />
• male, aged 50 years and older with a unilateral, firm subareolar mass with or without<br />
nipple distortion or associated skin changes.<br />
Please do not use this pro<strong>form</strong>a for non-urgent referrals, but<br />
refer the patient by means of the ‘OTHER SYMPTOMS’ pro<strong>form</strong>a<br />
Incidence<br />
<strong>Breast</strong> cancer is the most common cancer for women with more than 40,000 new cases in the UK in<br />
2000. There are around 250 cases diagnosed in men each year. The strongest risk factor for breast<br />
cancer is age: the older the woman the higher the risk. The full lifetime risk of developing breast cancer<br />
is 1 in 9, see below for age specific risk in<strong>form</strong>ation.<br />
Age Risk Age Risk<br />
25 1 in 15,000 60 1 in 23<br />
30 1 in 1900 70 1 in 15<br />
40 1 in 200 80 1 in 11<br />
50 1 in 50 85 + 1 in 10<br />
Source: <strong>Cancer</strong> Research UK<br />
Most breast cancers detected by screening are stage I tumours with 5 year survival rates over 90% 2.
FAMILY HISTORY INFORMATION 3<br />
Please make symptomatic MEDIUM or HIGH risk family history referrals<br />
via the ‘OTHER SYMPTOMS’ pro<strong>form</strong>a<br />
For advice, see ‘local contacts section’ or contact the <strong>Cancer</strong> Genetics clinic,<br />
Chris Harocopos, CNS <strong>Cancer</strong> Genetics, on 020 7905 2138<br />
Low risk women do not need to be seen<br />
<strong>Breast</strong> awareness in<strong>form</strong>ation should be offered to the patient 4<br />
In patients aged > 50 yrs participation in the NHSBSP should be encouraged<br />
Before a decision on referral is made, primary care professionals should note that a woman outside the 40–49 year age<br />
group who is estimated to be at moderate risk (e.g., she has only one relative with breast cancer diagnosed at any age, or<br />
she has two relatives diagnosed with breast cancer older than an average age of 50 years) will not generally be offered<br />
additional mammography.<br />
Women at moderate risk outside the 40–49 year age group may be referred for risk counselling and advice on risk<br />
management or consideration for prevention trials. Advice should be sought from the designated contact in secondary care<br />
about the appropriateness of referral.<br />
Women who meet the following criteria should be offered referral to secondary care:<br />
one 1 st degree female relative diagnosed with breast cancer < 40<br />
one 1 st degree male relative diagnosed with breast cancer at any age<br />
one 1 st degree relative with bilateral breast cancer where the 1st primary was diagnosed < 50<br />
or<br />
two 1 st degree relatives, or one 1 st degree AND one 2 nd degree relative, diagnosed with breast cancer at any age, or<br />
one 1 st degree or 2 nd degree relative diagnosed with breast cancer at any age AND one 1 st degree or 2 nd degree<br />
relative diagnosed with ovarian cancer at any age (one of these should be a 1 st degree relative)<br />
or<br />
three 1 st degree or 2 nd degree relatives diagnosed with breast cancer at any age<br />
Advice should be sought from the designated secondary care contact if any of the following are present in the family history<br />
in addition to breast cancers in relatives not fulfilling the above criteria:<br />
• bilateral breast cancer<br />
• male breast cancer<br />
• ovarian cancer<br />
• Jewish ancestry<br />
• sarcoma in a relative younger than age 45 years<br />
• glioma or childhood adrenal cortical carcinomas<br />
• complicated patterns of multiple cancers at a young age<br />
• paternal history of breast cancer (two or more relatives on the father’s side of the family)<br />
Discussion with the designated secondary care contact should take place if the primary care health professional is uncertain<br />
about the appropriateness of referral because the family history presented is unusual or difficult to make clear decisions<br />
about, or where the woman is not sufficiently reassured by the standard in<strong>form</strong>ation provided.<br />
Direct referral to a specialist genetics service should take place where a high-risk predisposing gene mutation has been<br />
identified (for example, BRCA1, BRCA2 or TP53).<br />
1 Based on <strong>Referral</strong> Guidelines for Suspected <strong>Cancer</strong> (NICE, 2005)<br />
Notes in grey refer to the evidence grading used in the NICE guidelines, for more in<strong>form</strong>ation see<br />
www.nice.org.uk/cg027NICEguideline<br />
2 <strong>Breast</strong> <strong>Cancer</strong> Factsheet (<strong>Cancer</strong> Research UK, Feb 2004)<br />
3 National Institute for Clinical Excellence (2004) Familial breast cancer: the classification and care of women at risk of<br />
familial breast cancer in primary, secondary and tertiary care. NICE Clinical Guideline No. 14. London: National<br />
Institute for Clinical Excellence. Available from: www.nice.org.uk/CG014<br />
4 <strong>Breast</strong> awareness means the woman knows what her breasts look and feel like normally. Evidence suggests that there<br />
is no need to follow a specific or detailed routine such as breast self examination, but women should be aware of any<br />
changes in their breasts ~see website below for further in<strong>form</strong>ation:<br />
www.cancerscreening.nhs.uk/breastscreen/breastawareness



![[4] Biopsy Leaflet.pub - Barking, Havering and Redbridge University ...](https://img.yumpu.com/51285530/1/190x134/4-biopsy-leafletpub-barking-havering-and-redbridge-university-.jpg?quality=85)