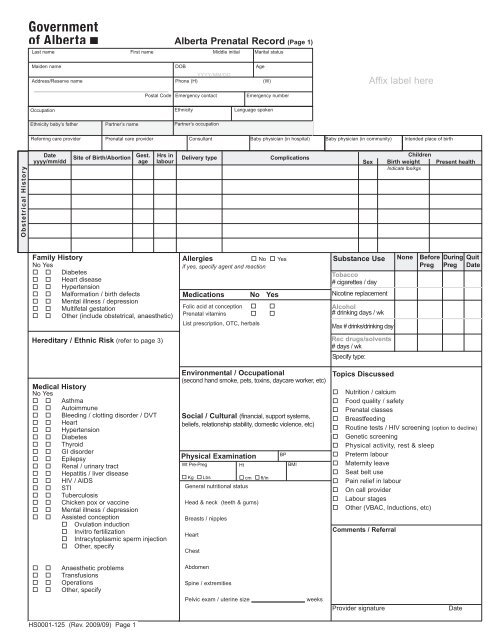
Affix label here Alberta Prenatal Record (Page 1)
Affix label here Alberta Prenatal Record (Page 1)
Affix label here Alberta Prenatal Record (Page 1)
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Alberta</strong> <strong>Prenatal</strong> <strong>Record</strong> (<strong>Page</strong> 1)<br />
Last name First name Middle initial Marital status<br />
Maiden name DOB Age<br />
YYYY/MM/DD<br />
Address/Reserve name Phone (H) (W)<br />
<strong>Affix</strong> <strong>label</strong> <strong>here</strong><br />
Postal Code Emergency contact Emergency number<br />
Occupation<br />
Ethnicity<br />
Language spoken<br />
Ethnicity baby’s father<br />
Partner’s name<br />
Partner’s occupation<br />
Referring care provider<br />
<strong>Prenatal</strong> care provider<br />
Consultant<br />
Baby physician (in hospital)<br />
Baby physician (in community)<br />
Intended place of birth<br />
Obstetrical History<br />
Date<br />
yyyy/mm/dd<br />
Site of Birth/Abortion<br />
Gest.<br />
age<br />
Hrs in<br />
labour<br />
Delivery type<br />
Complications<br />
Sex<br />
Children<br />
Birth weight<br />
Indicate lbs/kgs<br />
Present health<br />
Family History<br />
No Yes<br />
Diabetes<br />
Heart disease<br />
Hypertension<br />
Malformation / birth defects<br />
Mental illness / depression<br />
Multifetal gestation<br />
Other (include obstetrical, anaesthetic)<br />
Allergies<br />
No Yes<br />
if yes, specify agent and reaction<br />
Medications No Yes<br />
Folic acid at conception <br />
<strong>Prenatal</strong> vitamins <br />
List prescription, OTC, herbals<br />
Substance Use<br />
Tobacco<br />
# cigarettes / day<br />
Nicotine replacement<br />
Alcohol<br />
# drinking days / wk<br />
Max # drinks/drinking day<br />
None<br />
Before During<br />
Preg Preg<br />
Quit<br />
Date<br />
Hereditary / Ethnic Risk (refer to page 3)<br />
Rec drugs/solvents<br />
# days / wk<br />
Specify type:<br />
Medical History<br />
No Yes<br />
Asthma<br />
Autoimmune<br />
Bleeding / clotting disorder / DVT<br />
Heart<br />
Hypertension<br />
Diabetes<br />
Thyroid<br />
GI disorder<br />
Epilepsy<br />
Renal / urinary tract<br />
Hepatitis / liver disease<br />
HIV / AIDS<br />
STI<br />
Tuberculosis<br />
Chicken pox or vaccine<br />
Mental illness / depression<br />
Assisted conception<br />
Ovulation induction<br />
Invitro fertilization<br />
Intracytoplasmic sperm injection<br />
Other, specify<br />
Environmental / Occupational<br />
(second hand smoke, pets, toxins, daycare worker, etc)<br />
Social / Cultural (financial, support systems,<br />
beliefs, relationship stability, domestic violence, etc)<br />
Physical Examination<br />
Wt Pre-Preg<br />
Ht<br />
Kg Lbs<br />
cm ft/in<br />
General nutritional status<br />
Head & neck (teeth & gums)<br />
Breasts / nipples<br />
Heart<br />
Chest<br />
BP<br />
BMI<br />
Topics Discussed<br />
Nutrition / calcium<br />
Food quality / safety<br />
<strong>Prenatal</strong> classes<br />
Breastfeeding<br />
Routine tests / HIV screening (option to decline)<br />
Genetic screening<br />
Physical activity, rest & sleep<br />
Preterm labour<br />
Maternity leave<br />
Seat belt use<br />
Pain relief in labour<br />
On call provider<br />
Labour stages<br />
Other (VBAC, Inductions, etc)<br />
Comments / Referral<br />
Anaesthetic problems<br />
Transfusions<br />
Operations<br />
Other, specify<br />
Abdomen<br />
Spine / extremities<br />
Pelvic exam / uterine size _________________ weeks<br />
Provider signature<br />
Date<br />
HS0001-125 (Rev. 2009/09) <strong>Page</strong> 1
Gravida Term Preterm Number of abortions (by type)<br />
Spon. Induced Ectopic<br />
<strong>Alberta</strong> <strong>Prenatal</strong> <strong>Record</strong> (<strong>Page</strong> 2)<br />
# of living<br />
children<br />
Stillbirths<br />
Neonatal<br />
deaths<br />
<strong>Affix</strong> <strong>label</strong> <strong>here</strong><br />
LMP Sure of dates Cycle EDB by LMP EDB confirmed by U/S<br />
Yes Regular<br />
yyyy mm dd No Irregular<br />
yyyy mm dd yyyy mm dd<br />
Investigations<br />
Test<br />
Pap smear<br />
Date<br />
Date<br />
Result (yyyy/mm/dd) Test Result (yyyy/mm/dd) Test<br />
ABO/Rh<br />
HIV<br />
Last name of mother First name Middle initial<br />
Result<br />
Date<br />
(yyyy/mm/dd)<br />
Chlamydia &<br />
gonorrhea screen<br />
Urinalysis<br />
Urine C&S<br />
Hemoglobin<br />
Blood<br />
antibodies<br />
HBsAG<br />
Rubella<br />
Varicella<br />
Syphilis<br />
serology<br />
Syphilis serology<br />
2nd screen<br />
Gestational<br />
diabetic screen<br />
Group B<br />
strep<br />
mmol/L<br />
Hemoglobin<br />
Other investigations (laboratory, ultrasound) identify date, investigation and results<br />
<strong>Prenatal</strong> genetic investigations Counseled Declined Rh-IG Counseled<br />
1 Test<br />
Result<br />
YYYY/MM/DD Rh IG Ist dose:<br />
YYYY/MM/DD<br />
2 YYYY/MM/DD Rh IG 2nd dose:<br />
YYYY/MM/DD<br />
Date Weight Urine<br />
Gest. Fundus F.H. F.M. Cigs/<br />
(yyyy/mm/dd)<br />
lbs (protein/ BP age Pres.<br />
kg glucose)<br />
(cms) rate 20 wks+ day<br />
wks/days<br />
Comments<br />
Influenza vaccine<br />
Yes No<br />
(yyyy/mm/dd)<br />
Next<br />
Visit<br />
Init.<br />
Fetal movement discussed<br />
Count chart given: Date _________________<br />
Comments / Action plan<br />
Postpartum / Newborn Topics<br />
Breastfeeding Yes No Maybe<br />
Vitamin D supplement<br />
Back to sleep / SIDS prevention<br />
Postpartum depression<br />
Birth control<br />
Follow-up mother/baby<br />
Other (circumcision)<br />
Newborn requires<br />
Hepatitis B Prophylaxis<br />
No<br />
Yes<br />
Provider signature<br />
Date<br />
HS0001-125 (Rev. 2009/09) <strong>Page</strong> 2
<strong>Alberta</strong> <strong>Prenatal</strong> <strong>Record</strong> (<strong>Page</strong> 3)<br />
The <strong>Alberta</strong> <strong>Prenatal</strong> <strong>Record</strong> guides the practitioner in obtaining<br />
the woman’s medical, obstetrical, and family history. It is a record<br />
of the care provided. Refer to the <strong>Alberta</strong> <strong>Prenatal</strong> Care work sheet<br />
on page 4.<br />
The Healthy Mother, Healthy Baby Questionnaire Form HS0285<br />
can be used to obtain additional information on lifestyle and social<br />
history.<br />
At 36 weeks of gestation the <strong>Alberta</strong> <strong>Prenatal</strong> <strong>Record</strong> should be<br />
given to the woman to carry with her or a copy sent to the intended<br />
site for delivery.<br />
Hereditary/Ethnic Risk Assessment*<br />
Offer genetic counseling and/or carrier screening to biological<br />
parents with a relevant personal or family history of the<br />
following conditions, or to members of an at risk ethnic group.*<br />
Is t<strong>here</strong> any blood relationship between the biological parents<br />
No Yes <br />
A. Is t<strong>here</strong> a personal or family history (either side of the baby’s<br />
family) of the following:<br />
Thalassemia<br />
Tay Sachs disease<br />
Sickle cell anemia or trait<br />
Cystic fibrosis<br />
Hemophilia/bleeding disorder<br />
Intellectual disability/developmental delay<br />
Neuromuscular disease or muscular dystrophy<br />
Fragile X syndrome<br />
Major birth defect (e.g. spina bifida, cleft lip/palate)<br />
Metabolic disorder (e.g. PKU)<br />
Other inherited disease or chromosome abnormality,<br />
specify:<br />
No <br />
No <br />
No <br />
No <br />
No <br />
No <br />
No <br />
No <br />
No <br />
No <br />
No <br />
Yes <br />
Yes <br />
Yes <br />
Yes <br />
Yes <br />
Yes <br />
Yes <br />
Yes <br />
Yes <br />
Yes <br />
Yes <br />
Pregnancy Risk Profile for Specific Outcomes<br />
This risk profile summarizes the likelihood of specific adverse<br />
pregnancy outcomes (preterm, preterm SGA, SGA and LGA) in the<br />
presence of risk factors. The numbers are evidence-based odds<br />
ratios, representing the likelihood of occurrence of the adverse<br />
pregnancy outcomes in the presence of the specific risk factors.<br />
Circle all that apply.<br />
Risk Factor<br />
Demographic / Social<br />
Aboriginal<br />
Black<br />
Single<br />
Nulliparity<br />
Multiparity (> G3)<br />
Height < 152cm<br />
Pre-pregnancy Wt 80kg<br />
Age >35<br />
Cigarettes<br />
Substance Use<br />
Pre-existing Illness<br />
Diabetes<br />
Hypertension<br />
Chronic renal disease<br />
Endocrine disorder<br />
Medical disorder<br />
Cervical conization / surgery<br />
Preterm<br />
3<br />
2<br />
13<br />
2<br />
3<br />
4<br />
2<br />
4<br />
3<br />
3<br />
7<br />
Preterm<br />
SGA<br />
2<br />
2<br />
3<br />
2<br />
2<br />
2<br />
2<br />
5<br />
4<br />
Term<br />
SGA<br />
2<br />
2<br />
2<br />
2<br />
2<br />
2<br />
Term<br />
LGA<br />
> 4000g<br />
3<br />
3<br />
2<br />
2<br />
B. Offer genetic counseling / carrier screening for ethnic risk or<br />
positive family history:<br />
Ethnic Group<br />
Asian, African, Middle Eastern<br />
Mediterranean, Hispanic<br />
Carrier screening<br />
Thalassemia, hemoglobinopathy<br />
(e.g. sickle cell)<br />
Obstetrical History<br />
Previous SGA<br />
Previous preterm birth<br />
Prior > 3 abortions<br />
2<br />
4<br />
2<br />
12<br />
2<br />
2<br />
8<br />
Ashkenazi Jew<br />
French Canadian, Acadian, Cajun<br />
Tay-Sachs disease, Canavan<br />
Disease, familial dysautonomia<br />
Tay-Sachs disease<br />
* For additional information, contact Medical Genetics at:<br />
Calgary Ph: 403-955-7373 or Edmonton Ph: 780-407-7333<br />
Resource: Society of Obstetricians and Gynecologists of Canada<br />
(SOGC) guidelines. www.sogc.org/guidelines<br />
Definitions and Abbreviations:<br />
Expected Date of Birth (EDB) - Calculated by date of LMP and<br />
confirmed by early ultrasound<br />
Small for Gestational Age (SGA) - birth weight of less than 10th percentile<br />
Large for Gestational Age (LGA) - birth weight greater than 90th percentile<br />
PIH - Pregnancy Induced Hypertension (gestational hypertension)<br />
PPROM - Preterm Prelabour Rupture Of Membranes<br />
HELLP - Hemolysis, Elevated Liver enzyme levels and a Low<br />
Platelet count<br />
Current Pregnancy<br />
Multifetal gestation<br />
Poly / oligohydramnios<br />
Blood antibodies<br />
Acute medical disorder<br />
PIH<br />
PIH / proteinuria / HELLP<br />
Placenta abruptio<br />
Placenta previa<br />
Vaginal bleeding >20 wks<br />
PPROM<br />
<strong>Prenatal</strong> visits < 4<br />
Wt gain 41 wks<br />
Net wt gain > 15 kg<br />
Risk Factor<br />
Circle outcome risk<br />
20<br />
4<br />
4<br />
4<br />
2<br />
5<br />
5<br />
10<br />
5<br />
80<br />
4<br />
Preterm<br />
47<br />
13<br />
5<br />
6<br />
3<br />
5<br />
12<br />
69<br />
Preterm<br />
SGA<br />
3<br />
2<br />
3<br />
Term<br />
SGA<br />
4<br />
3<br />
Term<br />
LGA<br />
<strong>Page</strong> 3
<strong>Prenatal</strong> Care Worksheet<br />
This prenatal worksheet outlines the examinations, investigations and counseling the physician or midwife should consider in providing prenatal care.<br />
Significant effort has been made to ensure the accuracy of information presented. This worksheet should not be considered a substitute for clinical judgement and clinical advice.<br />
TIMING<br />
First prenatal visit<br />
6 - 10 weeks<br />
At each visit<br />
(Schedule visits every 4<br />
weeks up to 28-30 weeks,<br />
every 2 weeks up to 36<br />
weeks and then weekly after<br />
36 weeks until birth or more<br />
frequently if indicated)<br />
11-14 Weeks<br />
16-20 Weeks<br />
HISTORY & PHYSICAL<br />
INVESTIGATIONS TO CONSIDER<br />
Complete history & physical, including preconception: CBC<br />
Wt, Ht, and BMI.<br />
ABO/Rh & antibodies<br />
Obtain environmental/occupational, social/cultural and Rubella & varicella titre<br />
substance use history by interview or have mother complete Hepatitis B antigen<br />
Healthy Mother, Healthy Baby Questionnaire<br />
HIV serology<br />
(HMHB) HS0285.<br />
Pap smear<br />
Assess current medical status<br />
Chlamydia & gonorrhea screen<br />
Determine <strong>here</strong>ditary / ethnic risk - page 3<br />
Urinalysis & urine C&S<br />
Review current medications / herbal / OTC<br />
Genetic screening - schedule 1st<br />
Complete risk profile - page 3<br />
trimester aneuploidy screen<br />
Assign EDB (expected date of birth)<br />
Carrier screening<br />
Complete <strong>Prenatal</strong> Testing - Initial Screen for Pregnant Glucose testing<br />
Woman Lab Requisition<br />
TSH<br />
Schedule dating ultrasound<br />
Viral serology (e.g. toxoplasmosis)<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Inquire as to general well-being<br />
Assign gestational age<br />
Weight<br />
Blood pressure<br />
Symphysis - fundal height in cm<br />
Fetal heart sounds<br />
Presence of fetal movements<br />
Discuss results of genetic screening<br />
Arrange for diagnostic investigations<br />
Urine for glucose<br />
Urine for protein<br />
Blood antibody titres every 4<br />
weeks if Rh sensitized<br />
<br />
<br />
<br />
<br />
Genetic screening (1st trimester)<br />
Diagnostic genetic testing (CVS)<br />
Genetic screening (2nd trimester)<br />
Amniocentesis<br />
COUNSELING<br />
Review (HMHB-Q) with mother and/or identify concerns<br />
through interview<br />
Nutrition (including folic acid supplementation)<br />
Nausea & vomiting<br />
Food quality / safety<br />
Exercise / sleep<br />
Work / environmental concerns<br />
Smoking<br />
Alcohol and drug use<br />
Screening for infections in pregnancy<br />
Genetic screening options<br />
18-20 Weeks<br />
Ultrasound anatomical & fetal growth<br />
Confirm EDB for entire pregnancy<br />
24-28 Weeks<br />
Commence fetal movement counts<br />
Hemoglobin<br />
Discuss importance of fetal movement awareness and<br />
Provide copy of Fetal Movement Chart Form HS0001-132 Diabetic screening<br />
maternal response to a decrease in fetal movement<br />
Complete <strong>Prenatal</strong> - Testing Universal Syphilis<br />
Syphilis rescreening<br />
Signs & symptoms of preterm labour<br />
Rescreening Lab Requisition<br />
HIV screening / rescreening<br />
Obtain VBAC consultation / documentation<br />
ABO/Rh & antibodies (if Rh negative)<br />
Offer HIV screening / rescreening<br />
28-32 Weeks Add fetal presentation to routine visit<br />
Give Rh immune globulin (if Rh neg)<br />
Importance of fetal movement awareness<br />
30-36 Weeks Importance of fetal movement awareness<br />
Labour & birth concerns<br />
Hospital admission procedures<br />
Newborn issues and testing<br />
Breastfeeding<br />
Postpartum planning<br />
35-36 Weeks Confirm presentation of fetus<br />
GBS culture<br />
Ensure record available to L&D unit<br />
41-42 Weeks Pelvic examination Fetal assessment / NST Biophysical profile Importance of fetal movement awareness<br />
Syphilis & HIV screening / re-screening Induction plans<br />
Birth & Postpartum Pelvic examination<br />
Give Rh immune globulin (if Rh neg)<br />
Labour & birth concerns<br />
Postpartum (6 weeks) Breastfeeding evaluation<br />
Pap smear<br />
Sexuality & Contraception<br />
Assess for postpartum depression<br />
Hemoglobin<br />
Review immune status<br />
Arrange for newborn follow-up<br />
Coping strategies<br />
Risk for postpartum depression<br />
<strong>Page</strong> 4<br />
Newborn well-being / follow-up<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Seatbelt use<br />
Domestic violence / relationship stability<br />
Refer to SOGC - Intimate Partner Violence<br />
consensus statement (2005) for screening questions.<br />
<strong>Prenatal</strong> classes<br />
Sexuality<br />
Breastfeeding<br />
Counsel for common symptoms at this<br />
gestation<br />
Review results of investigations<br />
2nd trimester genetic screening<br />
Diagnostic genetic testing aminocentesis