Principles of GCP - UKM Medical Centre
Principles of GCP - UKM Medical Centre
Principles of GCP - UKM Medical Centre
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
OVERVIEW OF <strong>GCP</strong>, ICH<br />
AND MALAYSIAN <strong>GCP</strong><br />
PROF DR ROSLINA A MANAP<br />
Department <strong>of</strong> Medicine<br />
<strong>UKM</strong>MC
Scope <strong>of</strong> Lecture<br />
• Background/definitions<br />
• Evolution <strong>of</strong> <strong>GCP</strong><br />
• <strong>Principles</strong> <strong>of</strong> <strong>GCP</strong><br />
• Common audit findings<br />
• Conclusions<br />
2
Background<br />
• <strong>GCP</strong> certification is mandatory for clinical<br />
researchers<br />
• Pro<strong>of</strong> <strong>of</strong> certification to sponsors/IRB<br />
• Attendance at workshop + assessment<br />
• <strong>GCP</strong> is structured programme/workshop<br />
• cannot be done retrospectively<br />
• <strong>GCP</strong> ensures that research is<br />
• done in a proper way<br />
• <strong>of</strong> high standard<br />
• not associated with foul play, dishonesty, cheating, hiding<br />
<strong>of</strong> data<br />
• not harmful to the participants<br />
3
Good Clinical Practice<br />
A standard for the design, conduct, performance,<br />
monitoring, auditing, recording, analysis, and<br />
reporting <strong>of</strong> clinical trials that provides<br />
assurance that the data and reported results are<br />
credible and accurate (Quality Data), and that<br />
the rights, integrity and confidentiality <strong>of</strong> trial<br />
subjects are protected (Ethics).<br />
Quality Data + Ethics = <strong>GCP</strong>s<br />
ICH <strong>GCP</strong> 1.24 / Malaysian <strong>GCP</strong> 1.28<br />
4
Good Clinical Practice<br />
• Compliance with this standard provides public<br />
assurance:<br />
That the rights, safety, integrity,<br />
confidentiality and well being <strong>of</strong> trial<br />
subjects are protected consistent with the<br />
principles that have their origin in<br />
Declaration <strong>of</strong> Helsinki.<br />
That the data and reported results are<br />
credible and accurate.<br />
5
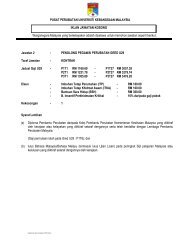
National Document<br />
6
HISTORY<br />
• <strong>GCP</strong> and other rules on human research in drug<br />
development have now been formalized in many<br />
international and national guidelines and regulations.<br />
• FDA guidelines for sponsors and investigators in 1970s<br />
• European Union <strong>GCP</strong> guidelines 1980s<br />
• International Conference on Harmonisation <strong>of</strong><br />
Technical Requirements for Registration <strong>of</strong><br />
Pharmaceuticals for Human Use (ICH) started 1991<br />
7
Researcher/<br />
sponsors<br />
Research Question<br />
Protocol Development<br />
IRB/IEC<br />
Researcher<br />
/monitors/<br />
auditors<br />
Researcher/<br />
sponsors<br />
Scientific & Conflict <strong>of</strong> Interest Reviews<br />
Ethics Review<br />
Recruitment & Enrolment<br />
Data Collection<br />
Data Analysis/Study Close-Out<br />
Dissemination<br />
MUST be<br />
<strong>GCP</strong>-<br />
compliant<br />
8
Steps to reduce research fraud &<br />
misconduct<br />
• Strengthen ethical research guidelines & upgrade<br />
guidelines into Acts <strong>of</strong> Law<br />
• Laws and legislations (e.g. <strong>Medical</strong> Act) must include<br />
research issues<br />
• IRBs made more transparent and accountable for their<br />
decisions<br />
• Role <strong>of</strong> MMC expanded to include research misconduct<br />
• Annual research reports & research findings accessible to<br />
public<br />
9
Steps to reduce research fraud &<br />
misconduct<br />
“Strengthening the number <strong>of</strong> medical personnel<br />
and improving the support system in any particular<br />
academic institution so that medical research is<br />
done by personnel who are not too heavily burdened<br />
by teaching or provision <strong>of</strong> clinical service. A system<br />
where the same, small number <strong>of</strong> staff are expected<br />
to perform “miracles” by being able to undertake<br />
good research in the background <strong>of</strong> a multitude <strong>of</strong><br />
other commitments (teaching, clinical service or<br />
administrative duties) may inadvertently encourage<br />
a medical researcher to be fraudulent for his<br />
“academic survival”.<br />
Zabidi Azhar Hussin, National Ethics Seminar, 2 Dec 2006<br />
10
Why develop <strong>GCP</strong><br />
• Fraud & misconduct<br />
• Nuremberg code<br />
• Clinical trial tragedies<br />
11
Fraud & misconduct<br />
• Defined as “the deliberate reporting <strong>of</strong><br />
false or misleading data or the<br />
withholding <strong>of</strong> reportable data”<br />
• 3 general types:<br />
• Altered data<br />
• Omitted data<br />
• Manufactured data<br />
12
Nuremberg Code 1947<br />
• 10 points pertaining to human<br />
experimentation<br />
• Including, “voluntary<br />
consent is absolutely<br />
essential”<br />
• Result <strong>of</strong> 140 days <strong>of</strong> American<br />
military tribunal against 23<br />
leading German physicians/<br />
administrators for crimes<br />
against humanity including<br />
human experimentation<br />
without consent<br />
• Thousands died or permanently<br />
crippled<br />
• 16 found guilty; 7 executed on<br />
2.6.48<br />
Dr Leo Alexander points to scars on the<br />
leg <strong>of</strong> Jadwiga Dzido’s, a Polish<br />
underground and victim <strong>of</strong> medical<br />
experiments at the Ravensbrueck<br />
concentration camp<br />
13
The Ellen Roche Story<br />
Johns Hopkins University<br />
Garland Hall, JHU<br />
• 24-year-old female lab<br />
technician<br />
• Healthy volunteer in<br />
asthma study<br />
• Died on 2/7/01 after<br />
inhalation <strong>of</strong> a non-<br />
approved drug<br />
• Autopsy revealed lung<br />
destruction<br />
14
Evolution <strong>of</strong> <strong>GCP</strong><br />
• 1930’s – US Food Drug & Cosmetic Act<br />
• 1947 – Nuremberg Code<br />
• 1960’s – Clinical trial tragedies<br />
• 1964 – Declaration <strong>of</strong> Helsinki<br />
• 1970’s – Sponsor/monitor obligations (US)<br />
• 1980’s – Informed Consent Regulations (US)<br />
• 1980’s – IRB Regulations (US)<br />
• 1986 - ABPI Guidelines (UK)<br />
• 1987 – Bonne Pratiques Cliniques (France)<br />
16
Evolution <strong>of</strong> <strong>GCP</strong><br />
• 1989 – Nordic and Japanese Guidelines<br />
• 1990 – Huriet Law (France)<br />
• 1991 – European CPMP Guidelines<br />
• 1992 – Australian Guidelines<br />
• 1992 – WHO Guidelines<br />
• 1996 – ICH Guidelines issued<br />
• 1997 – ICH becomes LAW in some countries<br />
• 1990’s European Guidelines, Asian countries<br />
• Oct 1999 – Malaysian <strong>GCP</strong><br />
17
Declaration <strong>of</strong> Helsinki<br />
• Adopted by World <strong>Medical</strong> Association<br />
General Assembly, Helsinki, Finland, June<br />
1964<br />
• Amended 5 times, most recently in October<br />
2000 in Edinburgh, Scotland<br />
18
Declaration <strong>of</strong> Helsinki<br />
• 32 points, including:<br />
• “…the health <strong>of</strong> my patients will be my first<br />
consideration”<br />
• “…to protect the life, health, privacy and dignity<br />
<strong>of</strong> the human subject”<br />
• “…the well-being <strong>of</strong> the human subject should take<br />
precedence over the interests <strong>of</strong> science and<br />
society”<br />
• “…the responsibility <strong>of</strong> the human subject must<br />
always rest with a medically qualified person and<br />
never rest on the subject <strong>of</strong> the research, even<br />
though the subject has given consent”<br />
19
ICH and Malaysian <strong>GCP</strong><br />
• International Conference on Harmonisation Guideline for Good<br />
Clinical Practice<br />
• Tripartite harmonisation initiatives (EU, USA, Japan)<br />
• Drafted 17/8/95, endorsed 30/4/96, and effective from 9/5/97<br />
• M<strong>GCP</strong> very similar to ICH <strong>GCP</strong> but with modifications to cater for<br />
local needs – drafted 6/99, finalised 9/99, launched 2/11/99, and<br />
revised 2004<br />
20
Aims <strong>of</strong> International Conference on<br />
Harmonisation (ICH)<br />
1. Unify registration requirements for new products<br />
2. Reduce medicinal product development costs: more<br />
economical use <strong>of</strong> animal, human and material<br />
resources.<br />
3. Accelerate medicinal product licensing times: avoid<br />
repeat testing in different regions.<br />
4. Increases patent protection times through reducing<br />
delay in licensing times.<br />
21
Malaysian <strong>GCP</strong> Subcommittee<br />
2 nd Edition 2004<br />
• Tan Sri Datuk Dr Mohd Ismail Merican<br />
• Pr<strong>of</strong> Dr Abd Rashid Abd Rahman<br />
• Dr Nor Shahidah Khairullah<br />
• Pr<strong>of</strong> Dr Lang Chim Choy<br />
• Pr<strong>of</strong> Dr Tariq bin Abdul Razak<br />
• Pr<strong>of</strong> Dato’ Dr Khalid bin Yus<strong>of</strong>f<br />
• Dr Muruga Vadivale<br />
• Dr Lokman Hakim Sulaiman<br />
• Dato’ Dr Zaki Morad Mohd Zaher<br />
• Ms Fudziah Dato Ariffin<br />
• Ms Norhayati Hanafiah<br />
22
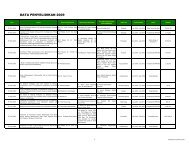
• 2nd edition <strong>of</strong> Malaysian<br />
<strong>GCP</strong> Guidelines – Jan 2004<br />
• The guideline is developed<br />
in line with the current<br />
local regulatory<br />
requirements on the<br />
manufacture <strong>of</strong><br />
Investigational medicinal<br />
products, prerequisite <strong>of</strong><br />
an approved <strong>GCP</strong> training<br />
and the current ICH <strong>GCP</strong><br />
guidelines<br />
• (CPMP/ICH/135/95)<br />
• This guideline is available<br />
at<br />
http://www.bpfk.gov.my<br />
23
Malaysian vs. ICH <strong>GCP</strong><br />
Amendments & additions<br />
Comprehensively addresses:<br />
• Use <strong>of</strong> alternative medicine (1.29)<br />
<br />
Plant/animal-derived materials or products with<br />
therapeutic or other human health benefits which<br />
contain either raw or processes ingredients from one or<br />
more plants/animals.<br />
• Role/authority <strong>of</strong> DCA (1.26, 5.20.3)<br />
<br />
A regulatory authority established for the purpose <strong>of</strong><br />
regulatory the control <strong>of</strong> drugs and cosmetics<br />
regulations, 1984 24
Malaysian vs. ICH <strong>GCP</strong><br />
• Importance <strong>of</strong> approved training in <strong>GCP</strong>,<br />
NCCR (1.6)<br />
• Training which is approved by the National<br />
Committee for Clinical Research (NCCR).<br />
The content <strong>of</strong> the training must<br />
incorporate the co-curriculum curriculum as stipulated<br />
by the committee<br />
25
Malaysian vs. ICH <strong>GCP</strong><br />
• Clinical trial import licence/exemption/customs (1.14,<br />
1.13, 5.14.2)<br />
• A license in Form 4 in the schedule <strong>of</strong> The Control <strong>of</strong><br />
Drugs and Cosmetics Regulations <strong>of</strong> 1984,<br />
authorizing the licensee to import any product for<br />
purposes <strong>of</strong> clinical trials, notwithstanding that the<br />
product is not a registered product.<br />
• An approval by the DCA authorizing the applicant<br />
to manufacture any local product for the purpose <strong>of</strong><br />
clinical trial.<br />
26
Malaysian vs. ICH <strong>GCP</strong><br />
• Role <strong>of</strong> IRB/IEC <strong>of</strong> MOH (3.2.7)<br />
• An institution without IRB/IEC may request IRB/IEC <strong>of</strong><br />
Ministry <strong>of</strong> Health<br />
• Malaysia or the Universities to make decisions on<br />
behalf <strong>of</strong> the said institution<br />
National Committee for Clinical Research (NCCR) (1.46)<br />
• A committee established for the purpose <strong>of</strong><br />
coordinating and promoting clinical research in<br />
Malaysia, chaired by the Deputy Director <strong>of</strong> Health<br />
(Research & Technical Support), MOH<br />
27
Investigator<br />
• (4.1.1) The investigator(s) should be qualified by<br />
education, approved training in Good Clinical Practice and<br />
experience to assume responsibility for the proper<br />
conduct <strong>of</strong> the trial, should meet all the qualifications<br />
specified by the applicable regulatory requirement(s), and<br />
should provide evidence <strong>of</strong> such qualifications through up-<br />
to-date curriculum vitae and/ or other relevant<br />
documentation requested by the sponsor, the IRB/IEC,<br />
and /or the regulatory authority(ies) 28
Investigator<br />
• Both the informed consent discussion and the<br />
written informed consent form and any other<br />
written information to be provided to subjects<br />
should include explanations <strong>of</strong> (a)-(u):<br />
29
Investigator<br />
• All serious adverse events (SAEs) detected or being notified<br />
should be reported within 2 working days to the sponsor<br />
except for those SAEs that the protocol or other document<br />
(eg., Investigator’s Brochure) identifies as not needing<br />
immediate reporting. The immediate report should be<br />
followed within 7 days by detailed, written report. The<br />
investigator must comply with the applicable regulatory<br />
requirement(s) related to the reporting <strong>of</strong> unexpected<br />
serious adverse drug reactions to the regulatory<br />
authority(ies) and IRB/IEC<br />
30
Investigator<br />
• Alternative use <strong>of</strong> thumbprint for consent<br />
(4.8.9) If a subject is unable to read or if a legally<br />
acceptable representative is unable to read, an<br />
impartial witness should be present……. …………….<br />
the subject or the subject’s legally acceptable<br />
representative orally consented to the subject’s<br />
participation in the trial and, if capable <strong>of</strong> doing so,<br />
has signed and/or thumbprinted and personally<br />
dated the informed consent form, the witness<br />
should sign and personally date the consent form.<br />
4.8.10 (u) The source <strong>of</strong> the investigational product<br />
that may be culturally unacceptable. 31
Sponsor<br />
• 5.6.1 The sponsor is responsible for selecting the investigator (s)/<br />
institution(s). Each investigator should be qualified by training<br />
(including approved <strong>GCP</strong> training) and should have adequate<br />
resources to properly conduct the trial for which the investigator is<br />
selected.<br />
• 5.8.1 If required by the applicable regulatory requirement(s), the<br />
sponsor must provide insurance or must indemnify (legal and<br />
financial coverage) the investigator/ institution against claims<br />
arising from the trial, except for claims that arise from malpractice<br />
and/or negligence<br />
32
Sponsor<br />
• 5.14.2 The sponsor should not supply an<br />
investigator/institution with the investigational<br />
product(s) until the sponsor obtains all required<br />
documentation (e.g. approval/favourable<br />
opinion from<br />
IRB/IEC and regulatory authority(ies). All importation<br />
<strong>of</strong> clinical trial drugs should go through customs even<br />
though a clinical trial import licence has been<br />
obtained.<br />
33
<strong>Principles</strong> <strong>of</strong> <strong>GCP</strong><br />
Safety and Protection <strong>of</strong> Subjects<br />
• “The health <strong>of</strong> my patient will be<br />
my first consideration” Declaration<br />
<strong>of</strong> Helsinki<br />
<br />
Trials should be conducted in<br />
accordance with the ethical<br />
principles that have their origin in<br />
the Declaration <strong>of</strong> Helsinki, and<br />
that are consistent with <strong>GCP</strong> and<br />
regulatory requirement(s).<br />
34
<strong>Principles</strong> <strong>of</strong> <strong>GCP</strong><br />
Safety and Protection <strong>of</strong> Subjects<br />
• The rights, safety, and well-being <strong>of</strong> the trial<br />
subjects are the most important<br />
considerations and should prevail over<br />
interests <strong>of</strong> science and society<br />
<br />
Before a trial is initiated, foreseeable risks<br />
and inconveniences should be weighed<br />
against the anticipated benefit for the<br />
individual subject and society.<br />
<br />
Ethics committee<br />
• Freely given informed consent should be<br />
obtained from every subject prior to clinical<br />
trial participation<br />
35
<strong>Principles</strong> <strong>of</strong> <strong>GCP</strong><br />
Safety and Protection <strong>of</strong> Subjects<br />
• The available non clinical and clinical<br />
information on an investigational product<br />
should be adequate to support the proposed<br />
clinical trial.<br />
• Clinical trials should be scientifically sound, and<br />
described in a clear, detailed protocol.<br />
• A trial should be conducted in compliance with<br />
the protocol that has received prior institutional<br />
review board (IRB)/independent ethics<br />
committee (IEC) approval/favourable<br />
opinion<br />
36
<strong>Principles</strong> <strong>of</strong> <strong>GCP</strong><br />
Safety and Protection <strong>of</strong> Subjects<br />
• A trial should be initiated and<br />
continued only if the anticipated<br />
benefits justify the risks<br />
• All clinical trial information should be<br />
recorded, handled, and stored in a way<br />
that allows its accurate reporting,<br />
interpretation and verification<br />
37
<strong>Principles</strong> <strong>of</strong> <strong>GCP</strong><br />
Safety and Protection <strong>of</strong> Subjects<br />
• The confidentiality <strong>of</strong> records that<br />
could identify subjects should be<br />
protected, respecting the privacy and<br />
confidentiality rules in accordance with<br />
the applicable regulatory<br />
requirement(s)<br />
• The medical care given to, and medical<br />
decisions made on behalf <strong>of</strong>, subjects<br />
should always be the responsibility <strong>of</strong> a<br />
qualified physician or, when<br />
appropriate, <strong>of</strong> a qualified dentist 38
<strong>Principles</strong> <strong>of</strong> <strong>GCP</strong><br />
Safety and Protection <strong>of</strong> Subjects<br />
• Each individual involved in conducting a<br />
trial should be qualified by education,<br />
training, and experience to perform his<br />
or her respective task(s).<br />
• Investigational products should be<br />
manufactured, stored and handled in<br />
accordance to GMP, and should only be<br />
used as per approved protocol<br />
• Systems with procedures that assure<br />
the quality <strong>of</strong> every aspect <strong>of</strong> the trial<br />
should be implemented 39
Written Informed Consent<br />
• Study specific procedures performed before consent<br />
• Wrong version being used (LANGUAGE)<br />
• Backdating/dated by site staff<br />
• Not re-consenting following protocol amendment<br />
• Copy not given to patient<br />
• Missing consent forms<br />
40
Study Protocol/Amendments<br />
• Recruiting ineligible subjects<br />
• Protocol procedures not done/done properly<br />
• Additional procedures performed<br />
• Implementation <strong>of</strong> amendment prior to ethics approval<br />
• Amendments not distributed to investigational staff at sites<br />
• Incorrect version used<br />
41
Study Drug<br />
• Inadequate drug accountability<br />
• Inadequate storage conditions<br />
• Lack <strong>of</strong> restricted access<br />
• Inadequate temperature monitoring<br />
42
AE/SAE Reporting<br />
• Delays in reporting <strong>of</strong> SAEs<br />
• AEs not thought to be drug-related related not reported in case<br />
report forms (CRF)<br />
• AEs on CRF not recorded in medical records<br />
• AEs not followed up at next visit or after study<br />
• Doctor not understanding definitions <strong>of</strong> AE/SAE<br />
43
Conclusions<br />
• Being <strong>GCP</strong> compliant ensures that:<br />
• Subjects are properly protected<br />
• Studies are based on good science, well<br />
designed, and properly analyzed<br />
• Study procedures are properly undertaken and<br />
adequately documented<br />
• Being non-<strong>GCP</strong> compliant results in:<br />
• Subjects being at risk<br />
• Data collection being unreliable<br />
• Risk <strong>of</strong> rejection by regulatory bodies<br />
44