MD - Health Care Compliance Association
MD - Health Care Compliance Association
MD - Health Care Compliance Association
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
OIG 2006 Work Plan ...continued from page 7<br />
■ Documented medical necessity and actual<br />
receipt of durable medical equipment<br />
■ Medicare drug reimbursement generally,<br />
including focus on acquisition and reimbursement<br />
under the average sales price,<br />
oral antiemetic medications, and duplicate<br />
payments for Part B drugs<br />
■ Prior approval for services provided, physician<br />
supervision, and licensure of personnel<br />
performing tests in Independent<br />
Diagnostic Testing Facilities (IDTFs)<br />
■ Documented medical necessity for appropriate<br />
services provided in Comprehensive<br />
Outpatient Rehabilitation Facilities<br />
(CORFs)<br />
■ Part B payments for inpatient radiology<br />
services<br />
■ Pricing of laboratory services provided to<br />
Medicare patients vs. patients covered by<br />
other payors<br />
■ Controls for identifying inappropriate<br />
payments for or utilization of covered preventive<br />
care services<br />
■ Physicians’ roles in over prescribing<br />
OxyContin and other prescription drugs<br />
Finally, in addition to these focus areas, in<br />
light of the recent advisory opinions, fraud<br />
alerts, corporate integrity agreements, and<br />
ongoing investigations, physicians should take<br />
the opportunity in 2006 to catalogue their<br />
current relationships with other providers and<br />
suppliers in the health care industry and consult<br />
qualified counsel to determine whether<br />
those relationships are compliant with federal<br />
and state laws, particularly the federal Anti-<br />
Kickback Statute and Stark II. ■<br />
1. The OIG Fiscal Year 2006 Work Plan is available at<br />
http://www.oig.hhs.gov/publications/docs/workplan/2006/<br />
WorkPlanFY2006.pdf<br />
2. The OIG first issued a CPG for hospitals in 1998 (“1998<br />
CPG”). See OIG <strong>Compliance</strong> Program Guidance for<br />
Hospitals, 63 Fed. Reg. 8987 (February 23, 1998). The 1998<br />
CPG was primarily intended to encourage hospitals to design<br />
and implement corporate compliance plans and programs. As a<br />
supplement to this early guidance, the OIG issued the<br />
“Supplemental <strong>Compliance</strong> Program Guidance for Hospitals”<br />
on January 31, 2005 (“Supplemental CPG”). See OIG<br />
Supplemental <strong>Compliance</strong> program Guidance for Hospitals, 70<br />
Fed. Reg. 4858 (January 31, 2005). The Supplemental CPG is<br />
focused on measuring and improving the effectiveness of existing<br />
compliance efforts, identifies specific fraud and abuse risk<br />
areas that hospitals should actively monitor, and describes the<br />
OIG’s expectations regarding compliance program design and<br />
guidelines for monitoring existing compliance programs.<br />
3. See HHS and DOJ, <strong>Health</strong> <strong>Care</strong> Fraud and Abuse Control<br />
Program (HCFAC) Annual Report For FY 2004 available at<br />
http://www.oig.hhs.gov/publications/docs/hcfac/hcfacreport2004.htm.<br />
During 2004, the federal government won or<br />
negotiated approximately $605 million in judgments and settlements,<br />
and it attained additional administrative impositions in<br />
health care fraud cases and proceedings. The Medicare Trust<br />
Fund received transfers of more than $1.51 billion during this<br />
period as a result of these efforts, as well as those of preceding<br />
years, and an additional $99 million in federal Medicaid money<br />
was similarly transferred to the Centers for Medicare and<br />
Medicaid Services (CMS) as a result of these efforts. The<br />
HCFAC account has returned over $7.3 billion to the Medicare<br />
Trust Fund since the inception of the program in 1997.<br />
4. Specifically, in the 2006 Work Plan, the OIG noted that during<br />
a recent audit it found that hospitals admitted patients for<br />
dialysis treatment, which lasted from 24 to 48 hours in which<br />
medical reviewers indicated that the stays were for the purpose<br />
of observation rather than treatment. The CMS Intermediary<br />
Manual requires the physician’s order to clearly state that the<br />
level of care the patient requires; e.g., “admission to inpatient<br />
status” or “admission to observation status.” Accordingly, the<br />
OIG intends in 2006 to examine whether payments made for<br />
“inpatient admissions” related to dialysis services were appropriate<br />
given the physicians’ orders in the case.<br />
Helpful Hints<br />
Eight steps to take in using the OIG<br />
Work Plan in your compliance program<br />
■ Review the table of contents. It lists<br />
the specific topics of concern of the<br />
OIG by the type of organization<br />
■ Highlight those areas that are potential<br />
applicable concerns and high priorities<br />
for your organization<br />
■ Review, in detail, the OIG’s concerns<br />
with the specific risk area<br />
■ Analyze your organization’s<br />
compliance program based on<br />
those stated concerns<br />
■ Determine whether your organization’s<br />
compliance program is meeting its<br />
established objectives and addressing<br />
these particular risk areas for your<br />
organization<br />
■ Discuss this analysis with key individuals<br />
of the organization’s compliance<br />
team to focus your compliance program<br />
on the specific areas of interest<br />
of the OIG for the coming year<br />
■ Educate the organization’s staff about<br />
these identified risk areas<br />
■ Ensure that an effective monitoring<br />
system is established and put in place<br />
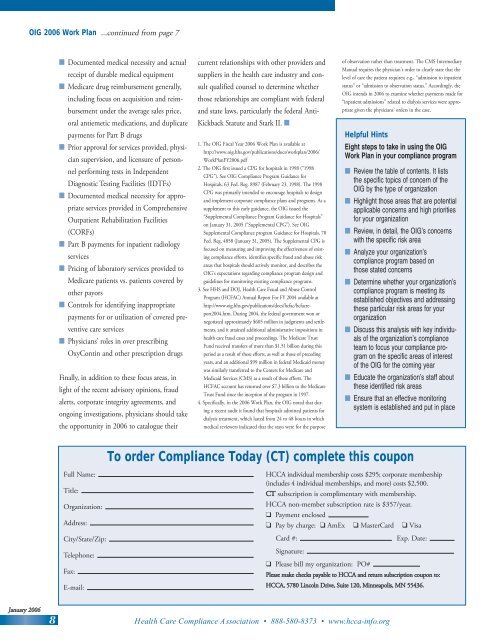
To order <strong>Compliance</strong> Today (CT) complete this coupon<br />
Full Name:<br />
Title:<br />
Organization:<br />
Address:<br />
City/State/Zip:<br />
Telephone:<br />
Fax:<br />
E-mail:<br />
HCCA individual membership costs $295; corporate membership<br />
(includes 4 individual memberships, and more) costs $2,500.<br />
CT subscription is complimentary with membership.<br />
HCCA non-member subscription rate is $357/year.<br />
❑ Payment enclosed<br />
❑ Pay by charge: ❑ AmEx ❑ MasterCard ❑ Visa<br />
Card #:<br />
Exp. Date:<br />
Signature:<br />
❑ Please bill my organization: PO#<br />
Please make checks payable to HCCA and return subscription coupon to:<br />
HCCA, 5780 Lincoln Drive, Suite 120, Minneapolis, MN 55436.<br />
January 2006<br />
8<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org