(NPWT) including Vacuum Assisted Closure (Vac) - Royal United ...
(NPWT) including Vacuum Assisted Closure (Vac) - Royal United ...
(NPWT) including Vacuum Assisted Closure (Vac) - Royal United ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Negative Pressure Wound Therapy<br />
(<strong>NPWT</strong>) <strong>including</strong> <strong><strong>Vac</strong>uum</strong> <strong>Assisted</strong><br />
<strong>Closure</strong> (<strong>Vac</strong>) in adults<br />
Reference Number: 745<br />
Author & Title:<br />
Responsible Director:<br />
Kate Purser, Senior Nurse for Tissue Viability<br />
and Nicola Heywood, Tissue Viability Nurse<br />
Specialist<br />
Director of Nursing<br />
Review Date: 6 June 2016<br />
Ratified by:<br />
Mary Lewis<br />
Acting Director of Nursing<br />
Date Ratified: 6 June 2013<br />
Version: 2<br />
Related Policies & Guidelines:<br />
Management of Infected and MRSA wounds<br />
Document name: Negative Pressure Wound Therapy (<strong>NPWT</strong>) Ref.: 745<br />
Issue date: 10 June 2013<br />
Status: Approved<br />
Author: Kate Purser and Nicola Heywood Page 1 of 20
Index:<br />
1. Policy Summary _______________________________________________ 4<br />
2. Policy Statements _____________________________________________ 4<br />
3. Definition of Terms Used _______________________________________ 5<br />
4. Duties and Responsibilities _____________________________________ 5<br />
4.1 Tissue Viability Nurse (TVN) ________________________________________ 5<br />
4.2 Ward/Department Staff ____________________________________________ 6<br />
4.3 Ward/Department Managers ________________________________________ 6<br />
5. How does <strong>NPWT</strong> work __________________________________________ 7<br />
6. Assessing patients for <strong>NPWT</strong> ____________________________________ 7<br />
7. Indications for <strong>NPWT</strong> ___________________________________________ 8<br />
8. Contraindications for <strong>NPWT</strong> _____________________________________ 8<br />
9. Wounds which may be treated with <strong>NPWT</strong> with precautions __________ 9<br />
10. Patients with open abdomens __________________________________ 10<br />
11. Consent ____________________________________________________ 10<br />
12. Potential complications ________________________________________ 11<br />
13. When to discontinue <strong>NPWT</strong> ____________________________________ 12<br />
14. User responsibilities __________________________________________ 12<br />
15. Education / Competency _______________________________________ 13<br />
16. Discharge ___________________________________________________ 14<br />
17. Who to contact for further help/information _______________________ 15<br />
18. Monitoring Compliance ________________________________________ 15<br />
19. Review _____________________________________________________ 15<br />
20. References __________________________________________________ 16<br />
Document Control Information ______________________________________ 18<br />
Ratification Assurance Statement _____________________________________ 18<br />
Consultation Schedule _______________________________________________ 19<br />
Equality Impact: (A) Assessment Screening ____________________________ 20<br />
Document name: Negative Pressure Wound Therapy (<strong>NPWT</strong>) Ref.: 745<br />
Issue date: 10 June 2013<br />
Status: Approved<br />
Author: Kate Purser and Nicola Heywood Page 2 of 20
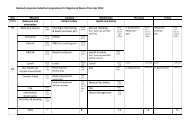
Amendment History<br />
Issue Status Date Reason for Change Authorised<br />
1 Approved March<br />
2009<br />
New Policy<br />
Clinical<br />
Governance<br />
2 Approved 6 June<br />
2013<br />
1. Planned Review<br />
2. Expanded scope. Previously<br />
“<strong><strong>Vac</strong>uum</strong> <strong>Assisted</strong> <strong>Closure</strong><br />
(VAC)” changed to: “(VAC)<br />
Therapy included in the<br />
Negative Pressure Wound<br />
Therapy (<strong>NPWT</strong>) <strong>including</strong><br />
<strong><strong>Vac</strong>uum</strong> <strong>Assisted</strong> <strong>Closure</strong><br />
(<strong>Vac</strong>)”<br />
Committee<br />
Mary Lewis<br />
Acting Director of<br />
Nursing<br />
Document name: Negative Pressure Wound Therapy (<strong>NPWT</strong>) Ref.: 745<br />
Issue date: 10 June 2013<br />
Status: Approved<br />
Author: Kate Purser and Nicola Heywood Page 3 of 20
1. Policy Summary<br />
• The purpose of this policy is to provide guidance for staff within the <strong>Royal</strong> <strong>United</strong><br />
Hospital (RUH), Bath NHS Trust about the requirements and processes for<br />
<strong>NPWT</strong>.<br />
• <strong>NPWT</strong> involves the use of a medical device to obtain negative pressure or a<br />
vacuum within a wound via a foam or gauze interface to promote healing. Both<br />
the suction effect and the mechanical forces generated in the wound lead can<br />
positively influence the wound healing process.<br />
• <strong>NPWT</strong> also assists in the removal of excess exudate thereby reducing local<br />
oedema. As such, <strong>NPWT</strong> can improve wound healing and health related quality<br />
of life.<br />
• The RUH currently uses <strong><strong>Vac</strong>uum</strong> <strong>Assisted</strong> <strong>Closure</strong> (V.A.C.®) to deliver <strong>NPWT</strong>.<br />
2. Policy Statements<br />
• The use of <strong>NPWT</strong> should be guided by informed clinical judgment and only<br />
commenced following a full assessment by a practitioner who has completed<br />
RUH <strong>NPWT</strong> training and completed self-assessment competencies following<br />
supervision by an experienced colleague.<br />
• This policy will identify what types of wounds are suitable for <strong>NPWT</strong>, who can<br />
use the therapy and how it is to be managed.<br />
• This policy aims to ensure the safe and effective use of <strong>NPWT</strong> in the RUH.<br />
• This policy also aims to ensure that no act or omission on the part of clinical<br />
professionals leads to the inappropriate management of a patient’s wound<br />
(Nursing and Midwifery Council (NMC), 2008).<br />
Document name: Negative Pressure Wound Therapy (<strong>NPWT</strong>) Ref.: 745<br />
Issue date: 10 June 2013<br />
Status: Approved<br />
Author: Kate Purser and Nicola Heywood Page 4 of 20
3. Definition of Terms Used<br />
<strong>NPWT</strong>: is a generic term used to describe vacuum assisted therapy that is not<br />
associated with any particular brand/company.<br />
<strong><strong>Vac</strong>uum</strong> assisted closure (V.A.C.®) therapy: is one of the most established<br />
negative pressure systems and uses a vacuum to create continuous or<br />
intermittent negative pressure at the wound bed to remove fluid, exudate and<br />
infectious materials as well as stimulating perfusion and new tissue growth<br />
(World Union Wound Healing Society, 2008).<br />
4. Duties and Responsibilities<br />
This policy applies to all members of staff involved in any aspect of <strong>NPWT</strong>. They<br />
have responsibility for ensuring that the principles outlined within this document<br />
are universally applied. The responsibility for the delivery of care of the patient<br />
remains with trust staff and the nurse in charge of ward<br />
4.1 Tissue Viability Nurse (TVN)<br />
• The TVN will assist ward staff to assess and manage patients with<br />
complex wounds requiring <strong>NPWT</strong>.<br />
• The TVN will ensure that regular training is available for appropriate<br />
staff. The <strong>NPWT</strong> training will be regularly reviewed to ensure that it is<br />
current. Registered nurses have a responsibility to ensure that their<br />
knowledge and skills are up to date, in order to maintain and develop<br />
their competence (NMC, 2008).<br />
• The TVN will ensure that self-assessment competencies are available<br />
for those who have undertaken <strong>NPWT</strong> training.<br />
Document name: Negative Pressure Wound Therapy (<strong>NPWT</strong>) Ref.: 745<br />
Issue date: 10 June 2013<br />
Status: Approved<br />
Author: Kate Purser and Nicola Heywood Page 5 of 20
4.2 Ward/Department Staff<br />
• Will at all times follow the Trust procedure for <strong>NPWT</strong>.<br />
• Must complete a comprehensive wound assessment which will be<br />
documented on the Trust wound assessment form.<br />
• Following assessment, ward/department staff will refer the patient to<br />
the TVN if required.<br />
• The patient’s suitability for <strong>NPWT</strong> will be assessed by either the TVN<br />
or a trained registered nurse who has completed the full RUH <strong>NPWT</strong><br />
training and competencies. Please note that although the term<br />
registered nurse is used throughout this document it is acknowledged<br />
that other registered allied health professionals may undertake <strong>NPWT</strong><br />
after appropriate training. For further clarification, please contact the<br />
TVN. This assessment will be clearly and accurately documented in<br />
the patient’s medical notes by the registered nurse (NMC, 2009).<br />
• The nurse undertaking <strong>NPWT</strong> will ensure that a photograph is taken<br />
of the wound (with patient consent) prior to and after <strong>NPWT</strong>.<br />
• The nurse undertaking <strong>NPWT</strong> will gain informed consent prior to<br />
commencement of the therapy and this will be documented in the<br />
Medical Notes. Patients will be advised of the potential benefits and<br />
complications and a patient information leaflet given to them and fully<br />
explained (NMC, 2008).<br />
• The nurse undertaking <strong>NPWT</strong> will ensure that the RUH <strong>NPWT</strong><br />
assessment and Care Plan is fully completed.<br />
4.3 Ward/Department Managers<br />
• Ward managers are responsible for ensuring that there is adherence<br />
with the policy by their staff.<br />
• Ward managers will ensure that they have adequate numbers of staff<br />
who have completed <strong>NPWT</strong> training. This includes full <strong>NPWT</strong><br />
training <strong>including</strong> the completion of competencies and the shorter<br />
ward based training on the management of <strong>NPWT</strong> devices for those<br />
Document name: Negative Pressure Wound Therapy (<strong>NPWT</strong>) Ref.: 745<br />
Issue date: 10 June 2013<br />
Status: Approved<br />
Author: Kate Purser and Nicola Heywood Page 6 of 20
managing patients with <strong>NPWT</strong>, but not undertaking assessments or<br />
dressing changes.<br />
5. How does <strong>NPWT</strong> work<br />
The following are suggested mechanisms of action:<br />
• Change in microvascular blood flow improving local perfusion<br />
• Removal of fluid exudate and reduction of oedema<br />
• Stimulation of the formation of granulation tissue<br />
• Reduction in bacterial colonisation<br />
• Mechanical closure of wound by reverse tissue expansion<br />
• Maintenance of a moist wound healing environment (Kinetic Concepts inc.<br />
(KCI), 2007).<br />
6. Assessing patients for <strong>NPWT</strong><br />
<strong>NPWT</strong> may only be used following a formal <strong>NPWT</strong> SBAR assessment (see Tissue<br />
Viability intranet site for latest assessment documents) by a competent registered<br />
nurse who has completed RUH <strong>NPWT</strong> training and competencies, a TVN or the<br />
patient’s medical registrar or consultant.<br />
The rationale for <strong>NPWT</strong> must be clearly documented in the patient’s medical notes.<br />
All patients receiving <strong>NPWT</strong> will have a <strong>NPWT</strong> SBAR care-plan commenced (see<br />
Tissue Viability Intranet site for documents)<br />
There are no <strong>NPWT</strong> systems that are cleared for use in newborns, infants or<br />
children. This policy only applies to adults (Food and Drug Administration (FDA),<br />
2011).<br />
Document name: Negative Pressure Wound Therapy (<strong>NPWT</strong>) Ref.: 745<br />
Issue date: 10 June 2013<br />
Status: Approved<br />
Author: Kate Purser and Nicola Heywood Page 7 of 20
7. Indications for <strong>NPWT</strong><br />
• Wounds free from slough or eschar (KCI, 2007)<br />
• Acute and traumatic wounds (KCI, 2007)<br />
• Venous or diabetic ulcers (Xie et al. 2010; Armstrong et al. 2002; Philbeck et al.<br />
2001).<br />
• Grade 3 or 4 pressure ulcers (Xie et al. 2010; Baynham et al. 1999)<br />
• Dehisced surgical wounds (KCI, 2007)<br />
• Flaps and skin grafts (Scherer et al. 2002; Lee et al. 2011)<br />
• Full-thickness debrided wounds (KCI, 2007)<br />
8. Contraindications for <strong>NPWT</strong><br />
Standard <strong>NPWT</strong> should not be used for any of the following wounds:<br />
• Non enteric or unexplored fistulas<br />
• Open abdomens<br />
• Cavity / sinus of unknown depth or origin<br />
• Wound with local malignancy<br />
• Necrotic tissue/eschar<br />
• Untreated osteomyelitis<br />
• Actively bleeding wounds<br />
• Wounds with exposed blood vessels, nerves, structures or organs<br />
• Vascular anastomosis & exposed anastomotic sites<br />
• The patient is unable to understand what the therapy entails, or comply with<br />
treatment (refer to Mental Capacity Act (Department of Health, 2005), sections 2,<br />
3 and 4)<br />
• The patient has capacity and declines <strong>NPWT</strong>, ensure this is fully documented<br />
and discussed with the consultant, TVN and ward manager.<br />
Document name: Negative Pressure Wound Therapy (<strong>NPWT</strong>) Ref.: 745<br />
Issue date: 10 June 2013<br />
Status: Approved<br />
Author: Kate Purser and Nicola Heywood Page 8 of 20
9. Wounds which may be treated with <strong>NPWT</strong> with<br />
precautions<br />
For the following wounds, <strong>NPWT</strong> may only be used in consultation with the TVN<br />
and/or the patient’s consultant:<br />
• Wounds with unstable fractures, open joints or sharp / loose fragments of bone.<br />
• Enteric fistulae of known origin for closure (Alvarez et al. 2001).<br />
• Wounds with exposed tendon (Heugel et al. 2002).<br />
• Infected wounds – daily dressings may be required in conjunction with<br />
antimicrobial wound liners and treatment with systemic antibiotics if appropriate.<br />
• Patients who are taking anti-coagulants, have haemostasis problems or a friable<br />
wound – seek specialist TVN advice and line the wound with a non-adherent<br />
dressing prior to application of the foam. Paraffin tulle should never be used. The<br />
patient’s clotting times must be monitored closely during <strong>NPWT</strong> and lower<br />
pressures may be required.<br />
• Wound near organs or irradiated, sutured or weakened blood vessels – seek<br />
specialist TVN advice and protect these with at least 3 layers of a non-adherent<br />
dressing and consider using lower pressures.<br />
• Chronic wounds – <strong>NPWT</strong> should only be considered after an appropriate wound<br />
management plan <strong>including</strong> modern wound dressings has failed (Azad &<br />
Nishikawa, 2002; Joseph et al. 2000).<br />
Discuss any queries with the TVN or the appropriate company prior to application of<br />
<strong>NPWT</strong>.<br />
Document name: Negative Pressure Wound Therapy (<strong>NPWT</strong>) Ref.: 745<br />
Issue date: 10 June 2013<br />
Status: Approved<br />
Author: Kate Purser and Nicola Heywood Page 9 of 20
10. Patients with open abdomens<br />
• The open abdomen is a technique also known as laparostomy, in which the<br />
fascia is left open intentionally to avoid elevation of intra-abdominal pressure and<br />
where surgical re-exploration is desirable. Temporary abdominal closure can be<br />
achieved using a dressing or technology intended to protect the exposed viscera<br />
(KCI, 2009; Garner, 2001).<br />
• The abdominal dressing <strong>NPWT</strong> system can assist to stabilise the abdominal<br />
wall, quantify and collect exudate, protect the intra-abdominal viscera and keeps<br />
the fascia intact and the cutaneous plane for subsequent closure (Caro et al.<br />
2011).<br />
• Patients with open abdomens must be referred to the TVN via Millennium within<br />
24 hours for consideration of specialized <strong>NPWT</strong> pumps & dressings designed<br />
specifically for the open abdomen.<br />
• Ward staff will not perform <strong>NPWT</strong> assessments or apply <strong>NPWT</strong> to the open<br />
abdomen, this must be managed by the patients’ consultant with appropriate<br />
involvement of the TVNs. Each patient will be managed individually (KCI, 2009).<br />
• All patients with <strong>NPWT</strong> insitu over an open abdomen who are well enough to<br />
mobilise should be assessed for corsetry and mobilized cautiously. This is to<br />
ensure that the <strong>NPWT</strong> seal is maintained.<br />
• For further information on the open abdomen and <strong>NPWT</strong>, please refer to the<br />
‘Clinical guidelines for the management of the open abdomen with KCI systems<br />
for active abdominal therapy’ (KCI, 2009) (See Tissue Viability intranet site).<br />
11. Consent<br />
• Verbal consent must be gained from the patient and this will be documented in<br />
the patient’s medical notes.<br />
• A patient information leaflet should be given and discussed with all appropriate<br />
patients and carers and is available on the Tissue Viability intranet. Patients<br />
MUST be monitored for any signs of bleeding and be educated on the<br />
importance of seeking assistance promptly in the case of haemorrhage (FDA,<br />
2009; 2011).<br />
Document name: Negative Pressure Wound Therapy (<strong>NPWT</strong>) Ref.: 745<br />
Issue date: 10 June 2013<br />
Status: Approved<br />
Author: Kate Purser and Nicola Heywood Page 10 of 20
12. Potential complications<br />
Rarely, complications may occur which require that the therapy is discontinued.<br />
These include:<br />
• Pressure necrosis from the tubing<br />
• Trauma of peri-wound skin<br />
• Growth of granulation tissue into foam - this may be avoided by using the white<br />
foam dressings (Versafoam) or by lining the wound with a non-adherent dressing<br />
• Allergic reaction to the drape<br />
• Fistula formation<br />
• Neoplasm caused by an increase in blood flow and rate of healing<br />
• Retained foam in wound, practitioners should always ensure that they have<br />
removed all foam pieces from the wound<br />
<strong>NPWT</strong> may also need to be discontinued if the patient experiences:<br />
• Psychological intolerance / non–concordance with <strong>NPWT</strong><br />
• No healing response within one week of commencing <strong>NPWT</strong><br />
• Frank pus in the dressing or canister<br />
<strong>NPWT</strong> will need to be discontinued immediately if the patient experiences:<br />
• Uncontrolled / excessive bleeding or haematoma under the dressing<br />
• Excessive pain: Patients may complain of mild increased pain when <strong>NPWT</strong> is<br />
initially commenced. This is usually due to the vacuum effect as the foam or<br />
gauze collapses and should settle down soon after application (Krasner, 2002).<br />
Pain may also be caused by high pressures, so consider reducing the pressure<br />
setting. The use of white Versafoam or non-adherent dressings under <strong>NPWT</strong><br />
black foam (Granufoam) may also help reduce pain. However, if the pain is<br />
continuous or severe then discontinue the therapy (Fraccalvieri et al. 2011).<br />
Document name: Negative Pressure Wound Therapy (<strong>NPWT</strong>) Ref.: 745<br />
Issue date: 10 June 2013<br />
Status: Approved<br />
Author: Kate Purser and Nicola Heywood Page 11 of 20
13. When to discontinue <strong>NPWT</strong><br />
• <strong>NPWT</strong> is associated with a significant cost implication, therefore there should be<br />
regular reassessments of the need to continue <strong>NPWT</strong>. Reviews should be<br />
undertaken by registered nurses with RUH <strong>NPWT</strong> competencies & occur at least<br />
weekly. The TVN can be contacted for advice and or assistance with<br />
reassessments.<br />
• <strong>NPWT</strong> should be only be discontinued in discussion with the TVN or the patients’<br />
medical team. However, if there is a serious problem such as<br />
excessive/uncontrolled bleeding or pain, stop the therapy immediately.<br />
• Discontinue <strong>NPWT</strong> therapy if it no longer appears to be effective and the wound<br />
has become ‘static’ i.e. there is no new granulation tissue after one week.<br />
Discuss with TVN whether <strong>NPWT</strong> should be continued.<br />
• Exudate levels are so low that the wound is drying out.<br />
• The wound has reached a stage at which <strong>NPWT</strong> therapy is no longer required i.e.<br />
has granulated up to the level of the surrounding skin.<br />
• The patient is unable to be discharged / transferred with <strong>NPWT</strong> therapy.<br />
14. User responsibilities<br />
It is the responsibility of the clinical staff that use <strong>NPWT</strong> to:<br />
• Refer all patients on <strong>NPWT</strong> to the Tissue Viability team through Millennium.<br />
• Only use <strong>NPWT</strong> once they have received approved RUH <strong>NPWT</strong> training and<br />
completed the <strong>NPWT</strong> competencies.<br />
• Be familiar with RUH policies and protocols, relevant company information and<br />
instructions, prior to using the therapy (see Tissue Viability intranet for the latest<br />
resources).<br />
• Ensure that the <strong>NPWT</strong> policy and all relevant literature are available for all<br />
members of the multidisciplinary team responsible for the patient.<br />
Document name: Negative Pressure Wound Therapy (<strong>NPWT</strong>) Ref.: 745<br />
Issue date: 10 June 2013<br />
Status: Approved<br />
Author: Kate Purser and Nicola Heywood Page 12 of 20
• Ensure that the consumables used are those recommended by the company and<br />
are compatible with the machine.<br />
• Obtain the consumables required for the therapy and where areas regularly use<br />
<strong>NPWT</strong>, to ensure that an adequate supply of these is maintained.<br />
• Ensure that Infection Control and user safety measures are adhered to with<br />
reference to manufacturing instructions and RUH infection control policy.<br />
• Ensure that the Medical Equipment Library (if the pump is RUH owned) or the<br />
relevant company (if a rental pump is used) is informed of any patient transfers.<br />
• Accept the cost of the therapy when it is being used in their area.<br />
15. Education / Competency<br />
Staff may only use <strong>NPWT</strong> following attendance at an RUH <strong>NPWT</strong> workshop<br />
completion of the <strong>NPWT</strong> self-assessment competency framework.<br />
and<br />
There are three levels of <strong>NPWT</strong> competency:<br />
• Novice practitioner: Has the ability to renew an existing <strong>NPWT</strong> dressing safely.<br />
This level may be undertaken by registered nurses, NVQ 3’s and student nurses.<br />
NVQ 3’s and student nurses must complete their competencies with the TVNs.<br />
Registered nurses may complete their competencies with a registered nurse in<br />
their area who has already gained the ‘experienced’ competencies.<br />
• Competent practitioner: Has the ability to initiate and manage <strong>NPWT</strong> on a patient<br />
within their own clinical specialty. This level may be undertaken by appropriate<br />
registered staff.<br />
• Experienced practitioner: Is able to assess a patient’s suitability for <strong>NPWT</strong> and<br />
can initiate and manage <strong>NPWT</strong> in a variety of clinical situations. This level can<br />
be undertaken by Band 6 and above registered staff. They will assess ‘Novice’<br />
and ‘Competent’ staff. It is recommended that all areas using <strong>NPWT</strong> therapy<br />
have at least one ‘Experienced’ practitioner. Competency at this level can only<br />
be assessed by the TVN.<br />
Document name: Negative Pressure Wound Therapy (<strong>NPWT</strong>) Ref.: 745<br />
Issue date: 10 June 2013<br />
Status: Approved<br />
Author: Kate Purser and Nicola Heywood Page 13 of 20
16. Discharge<br />
A patient may only be discharged home with a <strong>NPWT</strong> pump following discussion<br />
with the patient’s consultant and/or the TVN.<br />
The team responsible for the patient will ensure that prior to discharge:<br />
• Agreement is obtained from the relevant GP / community nursing team that<br />
they will assume responsibility for the <strong>NPWT</strong>. Ward staff should contact the<br />
community teams with plenty of notice if a discharge is imminent. At least 48<br />
hours’ notice is usually required.<br />
• The RUH TVN is contacted with the following details:<br />
o Type of unit in use <strong>including</strong> rental number<br />
o Type of dressing in use<br />
o Expected discharge date<br />
o Type of wound<br />
o Any relevant medical/surgical history<br />
• The TVN will contact the relevant community tissue viability team to agree<br />
funding the therapy.<br />
• Patients will not be discharged with RUH owned pumps. Those patients with a<br />
trust owned pump will be allocated a rental pump.<br />
• The relevant company is informed on the day of discharge, in order to cancel /<br />
transfer the rental agreement.<br />
• The patient is discharged home with enough consumables to enable two<br />
complete changes of <strong>NPWT</strong> dressings.<br />
Document name: Negative Pressure Wound Therapy (<strong>NPWT</strong>) Ref.: 745<br />
Issue date: 10 June 2013<br />
Status: Approved<br />
Author: Kate Purser and Nicola Heywood Page 14 of 20
17. Who to contact for further help/information<br />
• Tissue Viability Nurse: Ext. 1112/1837 or page through switchboard<br />
• KCI helpline (24 hours – 0800 980 8880)<br />
• Tissue Viability intranet site: http://webserver.ruhbath.swest.nhs.uk/clinical_directory/clinical_depts/tissue_viability/index.asp<br />
menu_id=10<br />
18. Monitoring Compliance<br />
The Tissue Viability service will review any incidents of non-concordance with this policy.<br />
Key themes of any non-concordance will be reported to Divisional Governance<br />
Meetings. Ward managers have a responsibility to ensure that all staff under their<br />
supervision are concordant with this policy. RUH employees have a responsibility to<br />
ensure that they follow RUH policies and protocols in order that their care is based on<br />
the best available evidence and, as such, risks are minimised.<br />
19. Review<br />
This policy will be in effect for three years, unless otherwise stated. Prior to the third<br />
anniversary of the policy the author will be asked to review it and make any<br />
necessary changes prior to further ratification.<br />
Document name: Negative Pressure Wound Therapy (<strong>NPWT</strong>) Ref.: 745<br />
Issue date: 10 June 2013<br />
Status: Approved<br />
Author: Kate Purser and Nicola Heywood Page 15 of 20
20. References<br />
• Alvarez, A.A. et al. (2001). Case report vacuum-assisted closure for cutaneous<br />
gastrointestinal fistula management. Gynaecologic Oncology, 80, pp. 413-16.<br />
• Armstrong, D.G. et al. (2002). Outcomes of sub-atmospheric pressure dressing<br />
therapy on wounds of the diabetic foot. Ostomy Wound Management, 48(4),<br />
pp.64-68.<br />
• Azad, S. & Nishikawa H. (2002). Topical negative pressure may help chronic<br />
wound healing. BMJ, 324, pp.1100.<br />
• Baynham, S. A. et al. (1999). Treating stage IV pressure ulcers with negative<br />
pressure therapy: A case report. Ostomy/Wound Management 45 (4), pp. 28-35.<br />
• Caro, A. et al. 2011. Treatment of the open abdomen with topical negative<br />
pressure therapy: a retrospective study of 46 cases. International Wound<br />
Journal 8 (3), pp. 274-9.<br />
• Department of Health, 2005. Mental Capacity Act. London: Department of<br />
Health.<br />
• FDA (2011). FDA safety communication: Update on serious complications<br />
associated with negative pressure wound therapy systems [Online]. Available<br />
at: http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm244211.htm<br />
[Accessed 16 Nov. 2012]<br />
• FDA (2009). Preliminary public health notification: Serious complications<br />
associated with negative pressure wound therapy systems [Online]. Available at:<br />
http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/PublicHealthNotificat<br />
ions/ucm190658.htm[Accessed 16 Nov 2012].<br />
• Fraccalvieri, M. et al. 2011. Patients pain feedback using negative pressure<br />
wound therapy with foam and gauze. International Wound Journal 8 (5), pp. 492-<br />
9.<br />
• Garner, G. B. (2001). <strong><strong>Vac</strong>uum</strong>-assisted wound closure provides early fascial reapproximation<br />
in trauma patients with open abdomens. The American Journal of<br />
Surgery, 182 pp.630-638<br />
• Heugel, J.R. et al. (2002). Treatment of the exposed Achilles tendon using<br />
negative pressure wound therapy: a case report. Journal of Burn Care &<br />
Rehabilitation, 23 (3), pp. 167-71.<br />
• Joseph, E. et al. (2000). A prospective, randomised trial of vacuum-assisted<br />
closure versus standard therapy of chronic non-healing wounds. Wounds, 12(2):<br />
60-7.<br />
• KCI (2009). Clinical Guidelines for the Management of the Open Abdomen with<br />
KCI Systems for Active Abdominal Therapy. London: MEP.<br />
• KCI (2007). V.A.C. ® Therapy Clinical guidelines. London: MEP.<br />
• Krasner, D.L. (2002). Managing wound pain in patients with vacuum-assisted<br />
closure devices. Ostomy Wound Management, 48 (5) pp.38-43.<br />
Document name: Negative Pressure Wound Therapy (<strong>NPWT</strong>) Ref.: 745<br />
Issue date: 10 June 2013<br />
Status: Approved<br />
Author: Kate Purser and Nicola Heywood Page 16 of 20
• Lee, D. L. et al. 2011. Negative Pressure Wound Therapy: An adjuvant to<br />
surgical reconstruction of large or difficult skin and soft tissue defects.<br />
International Wound Journal 8 (4), pp. 406-11.<br />
• Philbeck, T. E. et al. (2001). <strong><strong>Vac</strong>uum</strong>-assisted closure therapy for diabetic foot<br />
ulcers: clinical and cost analyses. Home Health Care Consultant, 46 (3) pp.250-<br />
54.<br />
• Scherer, L. A. et al. (2002). The vacuum assisted closure device: a method of<br />
securing skin grafts and improving graft survival. Archives of Surgery, 137 (8),<br />
pp.930-934.<br />
• Nursing and Midwifery Council, 2009. Record Keeping: Guidance for Nurses and<br />
Midwives. London: NMC.<br />
• Nursing and Midwifery Council, 2008. The Code: Standards of Conduct,<br />
Performance and Ethics for Nurses and Midwives. London: NMC.<br />
• World Union Wound Healing Society, 2008. Principles of Best Practice: <strong><strong>Vac</strong>uum</strong><br />
<strong>Assisted</strong> <strong>Closure</strong>: Recommendations for Use. A Consensus Document. MEP Ltd,<br />
London.<br />
• Xie, X. et al., (2010). The clinical effectiveness of negative pressure wound<br />
therapy: A systematic review. Journal of Wound Care 19 (11), pp. 491-7.<br />
Document name: Negative Pressure Wound Therapy (<strong>NPWT</strong>) Ref.: 745<br />
Issue date: 10 June 2013<br />
Status: Approved<br />
Author: Kate Purser and Nicola Heywood Page 17 of 20
Document Control Information<br />
Ratification Assurance Statement<br />
Dear<br />
Mary<br />
Please review the following information to support the ratification of the below named<br />
document.<br />
Name of document:<br />
Name of author:<br />
Negative Pressure Wound Therapy<br />
Kate Purser & Nicola Heywood<br />
Job Title:<br />
I, the above named author confirm that:<br />
Tissue Viability Nurse Specialist<br />
• The Policy presented for ratification meets all legislative, best practice and other<br />
guidance issued and known to me at the time of development of the Policy;<br />
• I am not aware of any omissions to the Policy, and I will bring to the attention of the<br />
Executive Director any information which may affect the validity of the Policy<br />
presented as soon as this becomes known;<br />
• The Policy meets the requirements as outlined in the document entitled Trust-wide<br />
Policy for the Development and Management of Policies (v4.0);<br />
• The Policy meets the requirements of the NHSLA Risk Management Standards to<br />
achieve as a minimum level 2 compliance, where applicable;<br />
• I have undertaken appropriate and thorough consultation on this Policy and I have<br />
documented the names of those individuals who responded as part of the<br />
consultation within the document. I have also fed back to responders to the<br />
consultation on the changes made to the Policy following consultation;<br />
• I will send the Policy and signed ratification checklist to the Policy Coordinator for<br />
publication at my earliest opportunity following ratification;<br />
• I will keep this Policy under review and ensure that it is reviewed prior to the review<br />
date.<br />
Signature of Author: Date: 3 June 2013<br />
Name of Person<br />
Ratifying this policy: Mary Lewis<br />
Job Title:<br />
Director of Nursing<br />
Signature: Date: 6 June 2013<br />
To the person approving this policy:<br />
Please ensure this page has been completed correctly, then print, sign and<br />
post this page only to: The Policy Coordinator, John Apley Building.<br />
The whole policy must be sent electronically to: ruh-tr.policies@nhs.net<br />
Document name: Negative Pressure Wound Therapy (<strong>NPWT</strong>) Ref.: 745<br />
Issue date: 10 June 2013<br />
Status: Approved<br />
Author: Kate Purser and Nicola Heywood Page 18 of 20
Consultation Schedule<br />
Name and Title of Individual<br />
Date Consulted<br />
Miss Langdon 25/3/2013<br />
Mr Bishay 25/3/2013<br />
Mr Dalton 25/3/2013<br />
Mr Chadwick 25/3/2013<br />
Mr Krystopic 25/3/2013<br />
Mr Williamson 25/3/2013<br />
Mr Budd 25/3/2013<br />
Mr Pai 25/3/2013<br />
Miss Winterborn 25/3/2013<br />
Jan Lynn 25/3/2013<br />
Rosemary Griffiths 25/3/2013<br />
Judith Sparkes 25/3/2013<br />
Lisa Valentine 25/3/2013<br />
Clare Warren 25/3/2013<br />
Brenda Duckett 25/3/2013<br />
Jo Flint 25/3/2013<br />
Sue Kennedy 25/3/2013<br />
Caroline Ficke 25/3/2013<br />
The following people have submitted responses to the consultation process:<br />
Name and Title of Individual<br />
Date Responded<br />
Name of Committee/s (if applicable)<br />
Date of<br />
Committee<br />
Document name: Negative Pressure Wound Therapy (<strong>NPWT</strong>) Ref.: 745<br />
Issue date: 10 June 2013<br />
Status: Approved<br />
Author: Kate Purser and Nicola Heywood Page 19 of 20
Equality Impact: (A) Assessment Screening<br />
To be completed when submitted to the appropriate Executive Director for<br />
consideration and approval.<br />
Person responsible for the assessment:<br />
Name:<br />
Nicola Heywood<br />
Job Title:<br />
Tissue Viability Nurse Specialist<br />
Does the document/guidance affect one<br />
group less or more favourably than another<br />
on the basis of:<br />
Yes/No<br />
Comments<br />
Race Yes No<br />
Ethnic origins (<strong>including</strong> gypsies and travellers) Yes No<br />
Nationality Yes No<br />
Gender (<strong>including</strong> gender reassignment) Yes No<br />
Culture Yes No<br />
Religion or belief Yes No<br />
Sexual orientation Yes No<br />
Age Yes No<br />
Disability<br />
(learning disabilities, physical disability, sensory impairment and<br />
mental health problems)<br />
Yes<br />
No<br />
Is there any evidence that some groups are affected<br />
differently<br />
Yes No<br />
If you have identified potential discrimination, are there<br />
any valid exceptions, legal and/or justifiable<br />
Yes No<br />
Is the impact of the document/guidance likely to be<br />
negative<br />
Yes No<br />
If so, can the impact be avoided Yes No<br />
What alternative is there to achieving the<br />
document/guidance without the impact<br />
Yes No<br />
Can we reduce the impact by taking different action Yes No<br />
If you answered NO to all the above questions, the assessment is now complete, and no<br />
further action is required.<br />
If you answered YES to any of the above please complete the<br />
Equality Impact: (B) Full Analysis<br />
Document name: Negative Pressure Wound Therapy (<strong>NPWT</strong>) Ref.: 745<br />
Issue date: 10 June 2013<br />
Status: Approved<br />
Author: Kate Purser and Nicola Heywood Page 20 of 20