atoll ESC V6 final for HLpres
atoll ESC V6 final for HLpres
atoll ESC V6 final for HLpres
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
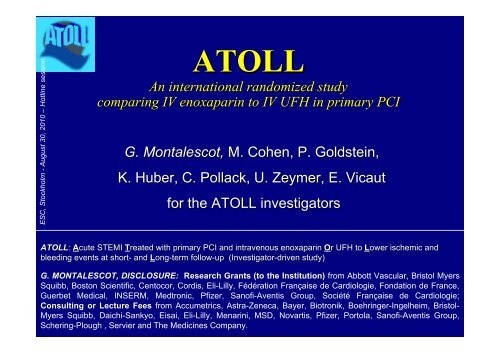
<strong>ESC</strong>, Stockholm - August 30, 2010 – Hotline session<br />
ATOLL<br />
An international randomized study<br />
comparing IV enoxaparin to IV UFH in primary PCI<br />
G. Montalescot, M. Cohen, P. Goldstein,<br />
K. Huber, C. Pollack, U. Zeymer, E. Vicaut<br />
<strong>for</strong> the ATOLL investigators<br />
ATOLL: Acute STEMI Treated with primary PCI and intravenous enoxaparin Or r UFH to Lower ischemic and<br />
bleeding events at short- and Long-term follow-up (Investigator-driven study)<br />
G. MONTAL<strong>ESC</strong>OT, DISCLOSURE: Research Grants (to the Institution) from Abbott Vascular, Bristol Myers<br />
Squibb, Boston Scientific, Centocor, Cordis, Eli-Lilly, Fédération Française de Cardiologie, Fondation de France,<br />
Guerbet Medical, INSERM, Medtronic, Pfizer, Sanofi-Aventis Group, Société Française de Cardiologie;<br />
Consulting or Lecture Fees from Accumetrics, Astra-Zeneca, Bayer, Biotronik, Boehringer-Ingelheim, Bristol-<br />
Myers Squibb, Daichi-Sankyo, Eisai, Eli-Lilly, Menarini, MSD, Novartis, Pfizer, Portola, Sanofi-Aventis Group,<br />
Schering-Plough , Servier and The Medicines Company.
Intravenous 0.5mg/kg Enoxaparin<br />
Anti-Xa IU/mL<br />
1.2<br />
0.8<br />
0.4<br />
0<br />
PD experience<br />
0.5 mg/kg IV<br />
1 mg/kg SC<br />
0 2 4 6 8 10 12 14 16 18 20<br />
Time (hours)<br />
Sanchez-Pena P. Br J Clin Pharmacol. 2005;60:364-73.<br />
Clinical experience<br />
•Choussat et al (elective PCI)<br />
•Miller et al (ACS-PCI)<br />
•Carnendran et al (elective PCI)<br />
•STEEPLE (elective PCI)<br />
•PROTECT –TIMI30 (ACS-PCI)<br />
•Silvain et al (elective PCI)<br />
•FINESSE (primary PCI)<br />
•Brieger et al. (Primary PCI)<br />
Choussat et al. JACC. 2002;40:1943-50.<br />
Miller L. J Invasive Cardiol. 2002;14:247-50<br />
Carnendran et al. J Invasive Cardiol. 2003;15:235-8.<br />
Montalescot et al. N Engl J Med. 2006;355:1006-17.<br />
Gibson et al. JACC. 2006;47:2364-2373<br />
Silvain et al. JACC. 2010;55:617-25<br />
Montalescot et al. JACC Cardiovasc Interv. 2010;3:203-12<br />
Brieger et al. Catheter Cardiovasc Interv. 2010 [in press]
ATOLL Trial design<br />
Randomization as early as possible (MICU +++)<br />
Real life population (shock, cardiac arrest included)<br />
No anticoagulation and no lytic be<strong>for</strong>e Rx<br />
Similar antiplatelet therapy in both groups<br />
STEMI Primary PCI<br />
ENOXAPARIN IV<br />
0.5 mg/kg<br />
with or without GPIIbIIIa<br />
ENOXAPARIN SC<br />
IVRS<br />
Primary PCI<br />
UFH IV<br />
50-70 IU with GP IIbIIIa<br />
70-100IU without GP IIbIIIa<br />
(Dose ACT-adjusted)<br />
UFH IV or SC<br />
30-day results
Trial organization<br />
ACTION Study Group (Academic Research Organization, Paris):<br />
1-Coordinating Center: Institute of Cardiology, Pitié-Salpêtrière Hospital, Paris<br />
2-Sponsor:<br />
AP-HP (Assistance Publique-Hôpitaux de Paris)<br />
3-Data center, Statistics: Unité Recherche Clinique, Lariboisière Hospital, Paris<br />
4-International CRO: Pierrel-Hyperphar<br />
5-Funding: AP-HP and unrestricted research grant from Sanofi-Aventis Group<br />
Steering Committee: G. Montalescot (Chair,, France), M. Cohen (USA), P. Goldstein<br />
(France), K. Huber (Austria), C. Pollack (USA), E. Vicaut (France), U. Zeymer<br />
(Germany)<br />
Data Safety Monitoring Board: A. Cohen (Chair(<br />
Chair, , France), M. Cucherat (France), A.<br />
Gitt (Germany)<br />
Core Laboratory: R. Dumaine, , A. Samadi<br />
Clinical Event Committee: F. Philippe, P. Sabouret, , F. Boccara, , A. Bellemain, , O.<br />
Gournay
Main objectives<br />
• 1° EP:<br />
– All-cause mortality at D30,<br />
– Complications of MI at D30 [resuscitated cardiac arrest,<br />
recurrent MI/ACS, urgent revascularization, stroke, peripheral or<br />
pulmonary embolism],<br />
– Procedure failure [definite stent thrombosis; B.O. use of<br />
GpIIB/IIIa; Non-TIMI 3 flow after PCI; ST resolution < 50% after PCI],<br />
– Non-CABG major bleeding during hospitalization<br />
• Main 2° EP: All-cause mortality, Recurrent MI/ACS or<br />
Urgent revascularization at D30<br />
• Main safety EP: Non-CABG major bleeding (STEEPLE<br />
definition) during hospitalization
Other objectives<br />
Efficacy<br />
• Death or complication of MI<br />
• Death, re-MI or urgent revascularization<br />
• Death; Death or resuscitated cardiac arrest<br />
Safety<br />
• Major or minor bleeding<br />
• Transfusion<br />
Net<br />
Benefit<br />
• Death, complication of MI or Major bleeding
Statistics<br />
• Study had a 80% statistical power to detect a difference<br />
between a group UFH proportion of 0.30 and a group<br />
enoxaparin proportion of 0.216 (RRR 28%, OR of 0.643)<br />
when the sample size in each group is 425.<br />
• Sample size reassessment after 75% recruitment based<br />
on conditional power calculation (Addplan software).<br />
• Analysis done on all randomized patients. Multiple<br />
imputation procedures <strong>for</strong> missing values done <strong>for</strong><br />
sensitivity analysis of the main criteria (Proc MI SAS).<br />
• Chisquare test <strong>for</strong> frequency comparisons and logrank<br />
<strong>for</strong> survival analysis (SAS version 9.2).
RESULTS
Baseline characteristics<br />
UFH ENOXAPARIN<br />
(n=460)<br />
(n=450)<br />
Male sex 78% (359) 78% (353)<br />
Age, median (Q1;Q3)<br />
60 (52; 70) 59 (52; 71)<br />
Age > 75<br />
17% (80) 19% (85)<br />
Pre-hospital randomization 71% (325) 70% (318)<br />
Current smoker, % (n) 47% (218) 44% (199)<br />
Diabetes, % (n) 15% (69) 14% (63)<br />
Hypertension, % (n) 45% (207) 46% (205)<br />
Hyperlipidemia, % (n) 40% (184) 40%(180)<br />
Prior myocardial infarction, % (n) 10% (44) 6% (28)<br />
Prior stroke, % (n) 2% (10) 3% (12)<br />
Shock and/or cardiac arrest be<strong>for</strong>e sheath, % (n) 5% (24) 4% (17)<br />
Time from symptom onset to randomization—hr,<br />
median (Q1;Q3)<br />
2h19<br />
(1h26; 4h37)<br />
2h33<br />
(1h29; 4h50)
Procedure and study medications<br />
Radial artery access, % (n)<br />
Other artery access, % (n)<br />
Stent implanted (among PCI patients) , % (n)<br />
Thrombectomy (among PCI patients) , % (n)<br />
Glycoprotein IIb/IIIa be<strong>for</strong>e start of PCI,% (n)<br />
Abciximab<br />
Eptifibatide<br />
Tirofiban<br />
Medications be<strong>for</strong>e/during hospitalization — % (n)<br />
Aspirin<br />
Clopidogrel<br />
< 300mg<br />
> 300 and < 600mg<br />
> 600 and < 900mg<br />
> 900mg<br />
Beta-blockers<br />
ACE-inhibitors<br />
Statins<br />
UFH<br />
(n=460)<br />
66% (305)<br />
34% (155)<br />
94% (366)<br />
44% (173)<br />
77% (357)<br />
64% (295)<br />
11% (54)<br />
2% (8)<br />
94% (434)<br />
93% (427)<br />
37% (171)<br />
37% (172)<br />
25% (113)<br />
1% (4)<br />
84% (385)<br />
72% (333)<br />
83% (382)<br />
ENOXAPARIN<br />
(n=450)<br />
69% (309)<br />
31% (141)<br />
96% (364)<br />
48% (184)<br />
71% (313)<br />
62% (277)<br />
8% (34)<br />
0.4% (2)<br />
96% (431)<br />
94% (422)<br />
37% (168)<br />
39% (174)<br />
22% (101)<br />
2% (7)<br />
88% (398)<br />
75% (336)<br />
87% (392)
Primary Endpoint<br />
Death, Complication of MI, Procedure Failure or Major Bleeding<br />
40<br />
ts<br />
n<br />
tie<br />
a<br />
p<br />
f<br />
o<br />
35<br />
30<br />
25<br />
20<br />
15<br />
%<br />
10<br />
33.7<br />
28<br />
RRR = 17%<br />
P = 0.07<br />
UFH<br />
ENOX<br />
5<br />
0
Main Secondary Endpoint (ischemic)<br />
Death, Recurrent MI/ACS or Urgent Revascularization<br />
30d rate (%)<br />
te<br />
ra<br />
P<br />
E<br />
ry<br />
a<br />
d<br />
n<br />
c<br />
o<br />
e<br />
s<br />
in<br />
a<br />
M<br />
5<br />
.1<br />
0<br />
0<br />
.1<br />
0<br />
5<br />
.0<br />
0<br />
UFH<br />
ENOX<br />
Log-Rank Test<br />
p=0.01<br />
41%<br />
11.3%<br />
6.7%<br />
0<br />
.0<br />
0<br />
0 5 10 15 20 25 30<br />
Days
Death or Complication of MI<br />
Death, resuscitated cardiac arrest, recurrent MI/ACS, Urg Revasc,<br />
stroke, peripheral or pulmonary embolism<br />
30d rate (%)<br />
te<br />
I<br />
ra<br />
f<br />
M<br />
o<br />
n<br />
tio<br />
a<br />
lic<br />
p<br />
m<br />
o<br />
C<br />
r<br />
o<br />
th<br />
a<br />
e<br />
D<br />
5<br />
.1<br />
0<br />
0<br />
.1<br />
0<br />
5<br />
.0<br />
0<br />
0<br />
.0<br />
0<br />
UFH<br />
ENOX<br />
Log-Rank Test<br />
p=0.02 12.4%<br />
0 5 10 15 20 25 30<br />
Days<br />
37%<br />
7.8%
Triple Ischemic Endpoint<br />
Death, re-MI or Urgent Revascularization<br />
30d rate (%)<br />
te<br />
ra<br />
c<br />
s<br />
a<br />
v<br />
e<br />
R<br />
rg<br />
U<br />
r<br />
I<br />
o<br />
-M<br />
,<br />
re<br />
th<br />
a<br />
e<br />
D<br />
0<br />
.1<br />
0<br />
8<br />
.0<br />
0<br />
6<br />
.0<br />
0<br />
4<br />
.0<br />
0<br />
2<br />
.0<br />
0<br />
0<br />
.0<br />
0<br />
UFH<br />
ENOX<br />
Log-Rank Test<br />
p=0.04 8.5%<br />
0 5 10 15 20 25 30<br />
Days<br />
40%<br />
5.1%
Death (any)<br />
Death or<br />
resuscitated cardiac arrest<br />
te<br />
ra<br />
th<br />
a<br />
e<br />
D<br />
0<br />
.1<br />
0<br />
8<br />
.0<br />
0<br />
6<br />
.0<br />
0<br />
4<br />
.0<br />
0<br />
2<br />
.0<br />
0<br />
0<br />
.0<br />
0<br />
UFH<br />
ENOX<br />
te<br />
t<br />
r<br />
a<br />
s<br />
r<br />
re<br />
Log-Rank Test a<br />
c<br />
ia<br />
p=0.08 6.3%<br />
r<br />
d<br />
a<br />
c<br />
40% d<br />
te<br />
3.8%<br />
ita<br />
c<br />
s<br />
u<br />
s<br />
re<br />
r<br />
o<br />
th<br />
a<br />
e<br />
Days<br />
D<br />
0 5 10 15 20 25 30<br />
30d rate (%)<br />
0<br />
.1<br />
0<br />
8<br />
.0<br />
0<br />
6.3%<br />
6<br />
.0<br />
0<br />
4<br />
.0<br />
0<br />
3.8%<br />
2<br />
.0<br />
0<br />
0<br />
.0<br />
0<br />
UFH<br />
ENOX<br />
Log-Rank Test<br />
p=0.049<br />
0 5 10 15 20 25 30<br />
Days<br />
7.0%<br />
42%<br />
4.0%<br />
30d rate (<br />
7.0%<br />
4.0%
Death finding Chance finding<br />
REGISTRIES<br />
RANDOMIZED<br />
%<br />
te<br />
ra<br />
th<br />
a<br />
e<br />
D<br />
Zeymer et al. Eurointervention 2009;4:524-8. Li et al. Am Heart J 2010;159:684-90.<br />
Montalescot et al. JACC CI 2010;3:203-12. Brieger et al. CCI 2010 (DOI:10.1002/ccd.22674)
Main Safety Endpoint<br />
Non-CABG Major Bleeding (STEEPLE definition)<br />
ts<br />
n<br />
tie<br />
a<br />
p<br />
f<br />
o<br />
%<br />
P = NS
All Safety Endpoints<br />
ts<br />
n<br />
tie<br />
a<br />
p<br />
f<br />
o<br />
%<br />
P = NS <strong>for</strong> all<br />
14<br />
12<br />
10<br />
8<br />
6<br />
4<br />
2<br />
0<br />
2.4 2.9 2.7<br />
2.3<br />
Protocole definitions<br />
(STEEPLE)
Death, , Complication of MI or Major bleeding<br />
16<br />
Net clinical benefit<br />
ts<br />
n<br />
tie<br />
a<br />
p<br />
f<br />
o<br />
14<br />
12<br />
10<br />
%<br />
8<br />
6<br />
4<br />
15<br />
10,2<br />
RRR = 32%<br />
P = 0.03<br />
UFH<br />
ENOX<br />
2<br />
0
Study Limitations<br />
o Not a pivotal registration<br />
trial<br />
o Medium size trial<br />
Independent trial led by the<br />
investigators<br />
« Real life » population<br />
(>70% Rx in the field) and<br />
no prior anticoagulation<br />
o Misses its primary EP, a<br />
mix of ischemic, safety<br />
and « classic » surrogate<br />
EP<br />
Effective on hard ischemic EP<br />
o Reflects practice in a<br />
limited number of<br />
countries<br />
Contemporary study (>70% of<br />
GPIIbIIIa, >60% high dose<br />
clopidogrel, >66% radial)
Conclusions<br />
In this 1 st pure head-to-head comparison between<br />
two anticoagulants in primary PCI, i.v. enoxaparin:<br />
• Did not reduce procedural failure<br />
• Reduced serious ischemic events, on top of<br />
intense antiplatelet therapy<br />
• Had a good safety profile, with a superior net<br />
clinical benefit
Special Thank to:<br />
INVESTIGATORS – Austria: WR. Benzer, K. Huber, F. Leisch, F. Weidinger –<br />
France: F. Adnet, M. Angioi, B. Barberon, JF. Benezet, JL. Bonnet, J. Boschat,<br />
B. Boulanger, D. Carrie, T. Chouihed, P. Coste, Y. Cottin, H. Courcoux, C.<br />
Cuvier, N. Danchin, JL. Ducasse, F. Duclos, P. Ecollan, S. Elhadad, E. Filippi,<br />
M. Freysz, F. Funck, S. Gallula, B. Gelée, A. Greffet, P. Henry, A. Jacquemin, T.<br />
Joseph, JM. Lablanche, H. Lardoux, H. Le Breton, B. Lederman, A. Margenet,<br />
G. Mehu, O. Nallet, F. Paganelli, M. Pansieri, L. Payot, C. Pouges, E. Salengro,<br />
C. Spaulding, G. Steg, O. Stibbe, E. Teiger, M. Thicoipe, C. Thuaire, J. Treuil, O.<br />
Wittenberg, O. Wolf – Germany: D. Andresen, C. Axthelm, Fischer, E. Girth, E.<br />
Hauptmann, U. Zeymer – USA: M.Cohen, F. Shamoon<br />
COMMITTEES – A Appaix-Bellemain, F Boccara, A Cohen, M. Cohen, M<br />
Cucherat, R Dumaine, A Gitt, P Goldstein, O Gournay, K Huber, F Philippe, C<br />
Pollack, P Sabouret, A Samadi, E Vicaut, U Zeymer<br />
PIERREL Research– L. Basso, L. Merlini, M. Mazzoleni<br />
ACTION study Group – ME. Assossou, M. Aout, B. Bertin, D. Brugier, JP.<br />
Collet, M. Courreges-Viaud, V. Gallois, P. Gallula, V. Jouis, S. Kabla, C. Misse,<br />
G. Ngouala, A. Pena, S. Paulsrud, N. Vignolles