1D1YPSU
1D1YPSU
1D1YPSU
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Meet one of your most demanding customers.<br />
When a child needs to be fitted with a<br />
hearing instrument, he or she can be<br />
one of the toughest customers on earth.<br />
Fortunately, nearly 50 years of making custom<br />
earpieces for ears of all shapes and sizes have<br />
taught us a few things.<br />
We understand the challenge of convincing a<br />
youngster that they need to wear their hearing<br />
instruments. The comfort and precise fit of<br />
Westone custom earpieces are the biggest<br />
steps you can take toward that goal.<br />
For most young patients, the instrument and<br />
earpiece have to be cosmetically appealing—<br />
and the smaller the instrument, the better.<br />
Westone’s lightweight, supremely comfortable<br />
earpieces make more open fit and mini BTE<br />
options available to your kiddos. And, our<br />
various venting options allow you to fit<br />
a wider range of hearing losses with<br />
these instruments. A custom-fit earpiece<br />
also offers the retention a young patient<br />
needs and no standard mushroom tip<br />
can match.<br />
Countless Westone customers we served<br />
as children are now grandparents. If you<br />
work with children, contact us and put that<br />
experience to work for you. You’ll find that<br />
satisfying your most demanding customers<br />
can be mere child’s play.<br />
800.525.5071<br />
westone.com<br />
westone@westone.com<br />
ISO 9001:2000
22<br />
32<br />
38<br />
46<br />
58<br />
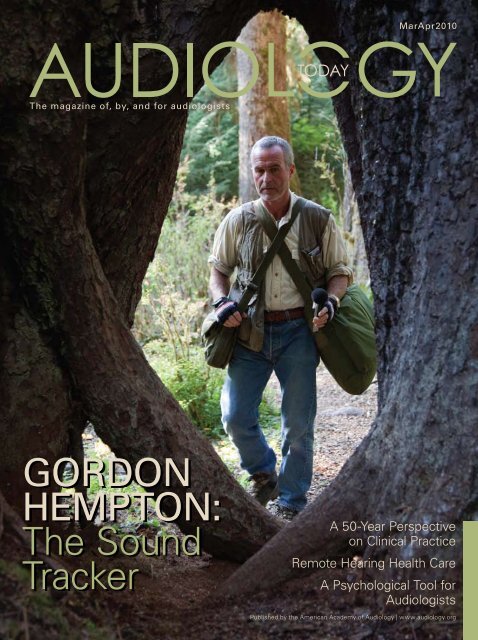
Gordon Hempton,<br />
acoustic ecologist and sound recordist, is this year’s AudiologyNOW! ® General<br />
Assembly keynote speaker. Hempton was able to spend a few tranquil<br />
moments with AT to discuss his search for a nice quiet place to rest.<br />
<br />
With 50<br />
years of active clinical involvement, Luterman discusses his professional life<br />
as a diagnostic and rehabilitative audiologist.<br />
<br />
Tele-audiology, which<br />
may include the full scope of audiological practice, offers one way of<br />
addressing the disparity between the need and the availability of hearing<br />
health services.<br />
<br />
<br />
This opinion editorial provides guiding principles that<br />
recommend that audiology programs and industry work together to identify<br />
and manage potential conflicts of interest to ensure that the relationship<br />
remains both successful and ethical.<br />
<br />
<br />
Audiologists can learn to externalize and personify a patient’s<br />
hearing loss without practicing psychotherapy. This approach causes the<br />
practitioner to focus on the human side of hearing loss and treat the person,<br />
not the disorder.
8 20,000 Hours of Listening By Kris English<br />
10 The Buck Stops Here By Cheryl Kreider Carey<br />
14 How to Bring Metrics to Marketing | Delegate Your Way<br />
to Success<br />
18 Academy and Other Audiology-Related Deadlines<br />
20 What's New on the Academy's Web Site<br />
67 Audiology Beyond the Classroom By Cherysse Lanns<br />
68 What Do Supporting Cells Do By Lisa L. Cunningham<br />
71 Providing Services to Medicare Beneficiaries—<br />
The Options By Annette A. Burton<br />
73 <br />
FAQs About Claims-Based Reporting<br />
76 What Type of Impression Is Your Office Making<br />
By Tracey Irene<br />
78 Suggested Areas of Standardization: AuD Student Clinical<br />
Practicum Experiences By Maureen Valente<br />
81 Higher Education Is on the Move By Doris Gordon<br />
82 I Can See the Future By James W. Hall III<br />
Academy News<br />
84 Become an Advocate at AudiologyNOW! ® By Melissa Sinden<br />
85 Celebrate this Year's Academy Honors Recipients<br />
89 Welcome New Members of the Academy<br />
and Student Academy<br />
90 Practice Guidelines Open for Review | Committee<br />
Accomplishments<br />
92 Partnership with Etymotic | ARO Travel Award Recipients<br />
| University AuD Programs | AudiologyNOW! Events
let your patients<br />
capture every<br />
moment!<br />
The New Passion440 from Widex combines the ultimate performance of<br />
Mind hearing instruments inside a sensationally small Passion RIC model!<br />
Passion440 features include:<br />
Dual Integrated Signal Processing<br />
Directional Microphones – 15 Channel High<br />
Definition Locator<br />
TruSound compression system that enhances clarity<br />
of sound, regardless of input<br />
10 kHz bandwidth – helps patients experience<br />
sounds in greater detail<br />
Multi-Directional Active Feedback Cancelling<br />
Speech Enhancement<br />
Zen – a revolutionary harmonic sound program that<br />
uses fractal technology to help patients relax*<br />
Audibility Extender – helps to extend the<br />
audibility range into high frequencies<br />
SmartSpeak – a signaling mechanism that informs<br />
wearers of hearing aid functions<br />
Stable Sound Delivery TM – the first truly closed<br />
instant-fit solution<br />
Sound Harmony – the unique Widex sound<br />
processing strategy that optimizes hearing aid<br />
performance for open fittings<br />
NanoCare Wax Guard System provides valuable<br />
moisture and wax protection<br />
A wide variety of stylish colors<br />
1.800.221.0188 www.widexPro.com<br />
INDICATIONS FOR USE: The Zen program is intended to provide a relaxing sound background for adults (21 and older) who desire to listen to such a background in quiet. It may be<br />
used as a sound therapy tool in a tinnitus treatment program that is prescribed by a licensed hearing healthcare professional (audiologists, hearing aid specialists, otolaryngologists) who<br />
is trained in tinnitus management.
The American Academy of Audiology promotes quality hearing and balance care<br />
by advancing the profession of audiology through leadership, advocacy, education,<br />
public awareness, and support of research.
Performance.<br />
Design.<br />
Innovation.<br />
Value.<br />
It’s time you heard<br />
of Hansaton.<br />
RED DOT DESIGN AWARD <br />
INTERNATIONAL FORUM DESIGN AWARD <br />
In our 50 years as a European leader in hearing aid design, we’ve<br />
learned a few things about what it means to listen. It’s how we<br />
deliver more of what you want. It’s how we provide the best<br />
available technology and the best possible value. And we do it<br />
simply. Great products. Transparent pricing. Extraordinary service.<br />
We’re listening.<br />
Become a Hansaton dealer today.<br />
The most sound decision you’ll make this year. To learn more about Hansaton products<br />
email info@hansaton.com, call 888.984.7432 or visit www.hansaton-usa.com<br />
Visit our booth at AudiologyNOW! in San Diego April 14-17
Don’t you love how kids love words<br />
First, they want to know the names<br />
of things, and then words that<br />
describe those things (colors, shapes,<br />
ownership—“mine!”). Along the way,<br />
they start noticing the sounds of the<br />
words. Some words have the same<br />
sounds at the end. “Yep,” grown-ups<br />
explain, “those words rhyme.” But,<br />
other words have the same sounds at<br />
the beginning, such as ball, birthday,<br />
beach, boy, beach boy, ba-ba-ba,<br />
ba-Barbara Ann…. Hmm. What’s the<br />
deal with that “buh” sound, anyway<br />
Sometimes, it’s in the middle<br />
of a word, too, like baby. The child<br />
ponders these details, and an amazing<br />
thing starts to happen: the brain<br />
becomes aware of phonemes.<br />
Why is an audiologist talking<br />
about phonemic awareness To<br />
encourage pediatric audiologists to<br />
participate on their patients’ “literacy<br />
team.” To learn to read, our patients’<br />
brains need to engage in five to six<br />
years (about 20,000 hours) of relentless<br />
auditory attention—noticing<br />
speech sounds and contrasting one<br />
sound with another. The brain needs<br />
all that input before it is ready to<br />
make the uniquely human amazing<br />
leap: connecting those sounds to<br />
letters of the alphabet. You’ve heard<br />
Carol Flexer talk about this! Without<br />
those 20,000 hours of listening,<br />
children are less ready to read and<br />
learn with their peers—and they may<br />
never catch up.<br />
Consistent access to sound via<br />
amplification depends on parent commitment,<br />
and we can always improve<br />
our communication with parents<br />
about the hearing-listening-reading<br />
connection. Audiologists are not literacy<br />
experts, but we do need enough<br />
information to convey this connection<br />
to parents. Speech-language pathologists,<br />
early interventionists, and<br />
educators bring their expertise to the<br />
learning process, and we are likely to<br />
“leave it to them” because we lacked<br />
training in preliteracy skill development.<br />
Yet, success ultimately depends<br />
on access to sound, and that’s where<br />
we come in!<br />
The Academy’s “Hear to Read”<br />
initiative was established to support<br />
pediatric audiologists as members<br />
of the literacy team. The first step<br />
was to develop a brochure for audiologists<br />
to share with parents. This<br />
brochure is now available on the<br />
Web site through the Academy Store.<br />
Next steps include expert presentations<br />
at AudiologyNOW! ® (see page<br />
80 for the Marion Downs Lecture in<br />
Pediatric Audiology) and articles in<br />
AT. Eventually we will see chapters<br />
on basic literacy information for<br />
audiologists in pediatric audiology<br />
textbooks.<br />
Fast forward to the near future:<br />
Your patient starts school. Her<br />
teacher says, “Children, this is the<br />
letter B. It makes the sound ‘buh.’<br />
Can you think of some words that<br />
start with that sound” And, your<br />
patient is ready with examples. She’s<br />
ready because she’s been thinking<br />
about “buh” for thousands of hours.<br />
Kris English, PhD<br />
President<br />
American Academy of Audiology<br />
P.S. While you’ve been reading<br />
silently to yourself, your temporal<br />
lobes have been active, as if you<br />
were listening to somebody speak!<br />
It’s called “the silent voice”—see<br />
S. Dehaene, Reading in the Brain:<br />
The Science and Evolution of a Human<br />
Invention (2009).
OAE<br />
“<br />
Testing a child’s hearing is<br />
so much faster and easier<br />
with the Otoport!<br />
”<br />
Whether you need a fast DPOAE handheld<br />
instrument, a clinical quality instrument<br />
with configurable stimulus settings,<br />
or a simple TEOAE newborn screener,<br />
we have an Otoport that will satisfy your<br />
needs for speed and accuracy.<br />
Now with<br />
INDUSTRY LEADING<br />
PROTECTION<br />
2 year<br />
Otoport Warranty<br />
Call for Details!<br />
OAE testing has never been easier. Call or visit www.otodynamics.com today.<br />
Otodynamics<br />
www.otoport.info www.otodynamics.com 1 800 659 7776<br />
Booth 1130
Looking ahead to the annual Academy<br />
Business Meeting (page 94) in San<br />
Diego, I’d like to provide a framework<br />
for the Academy’s business operation.<br />
Serving our membership of 11,000<br />
audiologists with a $7 million budget<br />
and a staff of 34, the Academy has a<br />
robust accounting system to ensure<br />
fiscal responsibility. Here are three<br />
areas I hold paramount in overseeing<br />
the Academy’s finances:<br />
To maintain fiscal<br />
integrity, the internal controls<br />
within our accounting department<br />
ensure separation of duties,<br />
e.g., no one individual both cuts<br />
and signs checks. We undergo an<br />
annual audit by an outside audit<br />
firm that is vetted by the Audit<br />
Committee and approved by the<br />
Board of Directors. Neither the<br />
treasurer nor I are voting members<br />
of the Audit Committee.<br />
Following a<br />
fiscal year (July 1–June 30), Amy<br />
Benham, CPA, senior director<br />
of finance and administration,<br />
produces financial statements<br />
in accordance with Generally<br />
Accepted Accounting Principles.<br />
These financial statements<br />
are reviewed monthly by our<br />
Treasurer, Gary Jacobson, PhD, as<br />
well as the Finance Committee,<br />
and are reviewed quarterly by
®
the board. Amy also oversees<br />
the Academy’s investments, in<br />
accordance with the Academy’s<br />
investment policy. The boardapproved<br />
audit is posted on our<br />
Web site annually (November) for<br />
members to review (go to www.<br />
audiology.org, search key words<br />
“annual report”). Additionally,<br />
the Academy annually submits a<br />
Form 990 (Return of Organization<br />
Exempt from Income Tax) to the<br />
IRS, providing them with our<br />
financial information.<br />
The Academy<br />
staff follows best practices to maximize<br />
the Academy’s resources. We<br />
solicit bids from multiple vendors<br />
before selecting one. Drawing<br />
upon our association management<br />
experience, we negotiate contracts<br />
prudently to provide savings to<br />
the Academy. We are constantly<br />
looking for ways to make the most<br />
of our limited resources. The weak<br />
economy has added a new dimension<br />
to our financial situation. This<br />
year, we have frozen staff salaries<br />
and are not making the discretionary<br />
contribution to their 401k plans.<br />
Incorporated in the state of<br />
Delaware (1997), the American<br />
Academy of Audiology is a not-forprofit<br />
with a 501c(6) designation<br />
from the IRS. In return for not taxing<br />
our revenue, the IRS stipulates what<br />
we “may” and “may not” do as a<br />
not-for-profit. At the end of the year,<br />
any revenue surplus is placed in the<br />
Academy reserves rather than paid<br />
out to stockholders as is done in forprofit<br />
organizations.<br />
We were excited to recently add<br />
the Student Academy of Audiology<br />
to our mix of entities, which<br />
also includes our Political Action<br />
Committee and the American Board<br />
of Audiology. I also serve as the<br />
executive director of our Foundation,<br />
the American Academy of Audiology<br />
Foundation, which has a 501c(3) IRS<br />
tax designation. This necessitates a<br />
separate set of books and Form 990<br />
to the IRS.<br />
As the individual hired by the<br />
Academy’s Board of Directors to<br />
ensure the financial and legal<br />
integrity of the Academy, I take<br />
this responsibility seriously. Using<br />
operating ratios to benchmark the<br />
Academy against other associations,<br />
we strive daily to handle the<br />
Academy’s financial resources in a<br />
most careful manner.<br />
Cheryl Kreider Carey, CAE<br />
Executive Director<br />
American Academy of Audiology
the board. Amy also oversees<br />
the Academy’s investments, in<br />
accordance with the Academy’s<br />
investment policy. The boardapproved<br />
audit is posted on our<br />
Web site annually (November) for<br />
members to review (go to www.<br />
audiology.org, search key words<br />
“annual report”). Additionally,<br />
the Academy annually submits a<br />
Form 990 (Return of Organization<br />
Exempt from Income Tax) to the<br />
IRS, providing them with our<br />
financial information.<br />
The Academy<br />
staff follows best practices to maximize<br />
the Academy’s resources. We<br />
solicit bids from multiple vendors<br />
before selecting one. Drawing<br />
upon our association management<br />
experience, we negotiate contracts<br />
prudently to provide savings to<br />
the Academy. We are constantly<br />
looking for ways to make the most<br />
of our limited resources. The weak<br />
economy has added a new dimension<br />
to our financial situation. This<br />
year, we have frozen staff salaries<br />
and are not making the discretionary<br />
contribution to their 401k plans.<br />
Incorporated in the state of<br />
Delaware (1997), the American<br />
Academy of Audiology is a not-forprofit<br />
with a 501c(6) designation<br />
from the IRS. In return for not taxing<br />
our revenue, the IRS stipulates what<br />
we “may” and “may not” do as a<br />
not-for-profit. At the end of the year,<br />
any revenue surplus is placed in the<br />
Academy reserves rather than paid<br />
out to stockholders as is done in forprofit<br />
organizations.<br />
We were excited to recently add<br />
the Student Academy of Audiology<br />
to our mix of entities, which<br />
also includes our Political Action<br />
Committee and the American Board<br />
of Audiology. I also serve as the<br />
executive director of our Foundation,<br />
the American Academy of Audiology<br />
Foundation, which has a 501c(3) IRS<br />
tax designation. This necessitates a<br />
separate set of books and Form 990<br />
to the IRS.<br />
As the individual hired by the<br />
Academy’s Board of Directors to<br />
ensure the financial and legal<br />
integrity of the Academy, I take<br />
this responsibility seriously. Using<br />
operating ratios to benchmark the<br />
Academy against other associations,<br />
we strive daily to handle the<br />
Academy’s financial resources in a<br />
most careful manner.<br />
Cheryl Kreider Carey, CAE<br />
Executive Director<br />
American Academy of Audiology
Marketing is an essential component<br />
of the success of any practice, yet<br />
without a thorough and quantifiable<br />
system for measuring the effectiveness<br />
of a campaign, marketing is<br />
in danger of becoming a budgetary<br />
black hole. Metrics define the<br />
return on investment of a marketing<br />
campaign, helping practices determine<br />
which initiatives yield the best<br />
results and, equally importantly,<br />
exposing the underperforming<br />
programs that need to be overhauled<br />
or cut altogether. Through<br />
the studied implementation of<br />
metrics, marketing is transformed<br />
from a blind expense into a calculated<br />
investment. Yet measuring the<br />
performance of a marketing initiative<br />
is not a transparent process.<br />
What follows are several strategies<br />
and considerations to introduce<br />
accountability into your marketing<br />
department.<br />
<br />
The first step to implementing a<br />
marketing analytics program is to<br />
cover the basics. Define the target<br />
market and craft a message that<br />
will be distinctly relevant to it. Also<br />
pay close attention to the medium<br />
in which you elect to advertise,<br />
using effectiveness, rather than<br />
cost, as the main arbiter. Approach<br />
your campaign from your potential<br />
patients’ perspective and ask yourself<br />
what message would resonate<br />
with them, and what problem of<br />
theirs you are solving.<br />
<br />
When setting up a marketing<br />
campaign with performance measurement<br />
in mind, it is also critical<br />
to define the goals of the campaign.<br />
How else will you measure its effectiveness<br />
Are you trying to increase<br />
leads Conversions Revenue Or is<br />
it a brand-building exercise Added<br />
precision in pinning down the<br />
goals of your marketing initiatives<br />
will improve the accuracy of your<br />
metrics and bring the goals closer to<br />
becoming a reality.<br />
<br />
Thinking broadly about marketing’s<br />
impact is critical, but, then<br />
again, so is thinking about the<br />
details. Performance metrics should<br />
compile as much data as possible,<br />
ideally through multiple channels so<br />
that the information can be crossreferenced<br />
and synthesized. One<br />
way involves tracking customer<br />
responses with promotion codes.<br />
Every bit of data associated with the<br />
campaign should be recorded, organized,<br />
and analyzed according to the<br />
specific marketing goals to which it<br />
relates.<br />
<br />
Web analytics are slippery, and can<br />
never be relied upon to offer 100<br />
percent accuracy. When selecting<br />
a Web analytics program, be sure<br />
that it filters out internal traffic, as<br />
well as visits from spiders and bots<br />
that could skew the results. Also be<br />
sure that the program uses verified<br />
first-party cookies to track unique<br />
visitors. Also be sure to audit your<br />
system for accuracy, given that Web<br />
analytics applications have been<br />
known to overstate actual results by<br />
as much as 400 percent.<br />
<br />
Finally, it is essential that you act<br />
on the results of your performance<br />
metrics. This means that you must<br />
have the flexibility and humility to<br />
tinker with your strategies, or to pull<br />
the plug on a campaign that simply<br />
isn’t working.<br />
<br />
<br />
It’s like giving to charity—everyone<br />
knows they should do more of<br />
it, and no one can think of a good<br />
reason why they don’t. Delegation
holds the unique value of increasing<br />
your practice’s productivity while<br />
at the same time reducing your<br />
own personal workload. The most<br />
common objections to delegation—<br />
“In the time it takes to explain<br />
how to do it, I could do it myself”<br />
and “If you want a job done right,<br />
do it yourself”—are, at best, shortsighted,<br />
and, at worst, patently false.<br />
Learning how to delegate effectively<br />
is an elusive but essential management<br />
skill that will empower your<br />
employees by demonstrating your<br />
trust and confidence in them, and<br />
it will ultimately help train them to<br />
be effective managers themselves,<br />
ready and poised to transition<br />
into new leadership roles as your<br />
practice grows. Here are six steps<br />
for developing, implementing, and<br />
overseeing your delegation strategy.<br />
<br />
One of the most common fears cited<br />
by managers who refuse to delegate<br />
is that the end product will not be<br />
satisfactory. Managers who have<br />
experienced this firsthand will be<br />
especially gun-shy about delegating<br />
again. An inadequate result is<br />
not necessarily an indicator of poor<br />
workers. It can just as often reflect<br />
poor management, most frequently<br />
rooted in vague communications<br />
and unclear expectations. Define<br />
the goal of the project with the<br />
employee who will be overseeing<br />
it, and make the timetable realistic.<br />
Make sure that the employee understands<br />
both the technical elements<br />
of the project and how it meshes<br />
with the big picture. Without seeming<br />
overbearing or condescending,<br />
overcommunicating at the outset<br />
of a project is not necessarily a bad<br />
thing, as the surest way to guarantee<br />
that a project will fail is to leave<br />
the responsible employee uncertain<br />
of your expectations.<br />
<br />
Delegation means letting go.<br />
Somewhat. When you’re entrusting
one of your employees with a project,<br />
remember that you’re doing<br />
just that—entrusting them. You<br />
hired these people because of their<br />
intelligence, sound judgment, and<br />
competence. When you’re delegating<br />
a project to them, remember<br />
that they are still possessed of<br />
those qualities, and for that reason,<br />
the project will be a success. This<br />
means that you have to let them<br />
find their own way, and trust and<br />
support them as they are doing it.<br />
Within legal and ethical bounds, of<br />
course, it is the end product that<br />
is the yardstick of success, not the<br />
path by which the goal is achieved.<br />
Assuming that yours is the only way<br />
is a hallmark of micromanagement,<br />
and a surefire way to torpedo your<br />
delegation initiative.<br />
<br />
Delegating means that you can let<br />
your employees take the lead in<br />
developing a plan, and, ideally, this<br />
process can be completed with minimal<br />
oversight. That said, it is your<br />
job to make sure that they do, in fact,<br />
have a plan. The methods can be left<br />
up to them, but you will sleep easier<br />
knowing that there is a roadmap<br />
to complete the project, and your<br />
employees will have a much better<br />
chance of succeeding. For complicated<br />
projects, it can be useful to set<br />
reporting schedules to keep employees<br />
on pace. Breaking a single, large<br />
project into smaller, more manageable<br />
tasks is an effective way to<br />
ensure that the ultimate deadline is<br />
met, while simultaneously relieving<br />
you of the anxiety that comes from<br />
micromanaging.<br />
<br />
Set your employees up for success<br />
by pairing them with a project<br />
that is a good match for their skills<br />
and competencies. At the same<br />
time, remember that one of the<br />
main reasons that you delegate is<br />
to develop your employees. Giving<br />
all the challenging projects to one<br />
particularly capable worker will<br />
engender resentment from all<br />
sides. The chosen employee will<br />
feel put upon, while the rest of<br />
your staff will feel neglected and<br />
unappreciated. Know also that<br />
some employees may require more<br />
oversight than others. But part of<br />
your skill as a manager is identifying<br />
your employees’ strengths and<br />
weaknesses, and accentuating the<br />
former while developing the latter.<br />
A finely attuned delegation program<br />
can be your best ally in achieving<br />
this goal.<br />
<br />
<br />
Delegation often fails when<br />
managers dole out tasks and responsibilities<br />
without giving staff the<br />
authority to make decisions. Keeping<br />
a stranglehold on decision-making<br />
authority will undermine the confidence<br />
of your staff, and create the<br />
appearance that, rather than trusting<br />
and believing in your employees,<br />
you simply want to slough off work<br />
on them while keeping overall<br />
control for yourself. This is a flawed<br />
strategy. For your employees to really<br />
develop, they have to be given a long<br />
enough leash to make mistakes and<br />
know that it’s okay—as long as they<br />
fix them and learn from them.<br />
<br />
<br />
This is the fun part! Again, remember<br />
that development is central to<br />
delegation. You’re trying to bring<br />
your employees up and prepare them<br />
for the next level. This means that<br />
feedback must go directly to the<br />
employee whom you have placed<br />
in charge of the project. The natural<br />
tendency of your staff will be to<br />
come to you, but, in keeping with<br />
their status as the project lead, the<br />
employee(s) you have put in charge<br />
must be the hub of all feedback concerning<br />
the project, both positive and<br />
negative.<br />
Whether you can do the job faster<br />
or more effectively than one of your<br />
employees can isn’t the question.<br />
What if you want to take a vacation<br />
Or expand your practice beyond your<br />
ability to manage it single-handedly<br />
Or retire These are all questions<br />
that keep small business owners<br />
up at night, but they are also questions<br />
that have a common answer.<br />
Delegating tasks will demonstrate to<br />
your staff that you trust them, and<br />
your reward will be more capable,<br />
self-assured, and well-rounded<br />
employees ready to take the reins<br />
and drive the business whenever you<br />
call on them.<br />
Articles © Copyright 2010 Information, Inc.<br />
Illustrations by Johanna van der Sterre
Hear.<br />
There and Everywhere.<br />
TM<br />
Every note of the flute solo in a child’s music recital.<br />
The sound of an arriving text message. A toddler’s<br />
first laugh. The cheers from teammates. The peeps,<br />
calls and trills in the backyard.<br />
Life is a composition of finely detailed sounds.<br />
MED-EL’s industry-leading cochlear implant innovations<br />
with FineHearing allow its recipients to hear<br />
*<br />
and appreciate the most obvious and the most<br />
elusive of them all.<br />
It’s a noisy world out there.<br />
Enjoy it.<br />
Help your patients hear life the way it was meant to sound.<br />
Begin their cochlear implant journey with MED-EL.<br />
MAESTRO cochlear implant system<br />
features the thinnest and lightest<br />
speech processor available today.<br />
* FSP is not indicated for use by pre-lingual children in the US.<br />
hearLIFE<br />
COCHLEAR IMPLANTS :: MIDDLE-EAR IMPLANTS<br />
TOLL FREE (888) MEDEL-CI (633-3524) :: V/TDD PHONE (919) 572-2222<br />
www.medel.com
Hear.<br />
There and Everywhere.<br />
TM<br />
Every note of the flute solo in a child’s music recital.<br />
The sound of an arriving text message. A toddler’s<br />
first laugh. The cheers from teammates. The peeps,<br />
calls and trills in the backyard.<br />
Life is a composition of finely detailed sounds.<br />
MED-EL’s industry-leading cochlear implant innovations<br />
with FineHearing allow its recipients to hear<br />
*<br />
and appreciate the most obvious and the most<br />
elusive of them all.<br />
It’s a noisy world out there.<br />
Enjoy it.<br />
Help your patients hear life the way it was meant to sound.<br />
Begin their cochlear implant journey with MED-EL.<br />
MAESTRO cochlear implant system<br />
features the thinnest and lightest<br />
speech processor available today.<br />
* FSP is not indicated for use by pre-lingual children in the US.<br />
hearLIFE<br />
COCHLEAR IMPLANTS :: MIDDLE-EAR IMPLANTS<br />
TOLL FREE (888) MEDEL-CI (633-3524) :: V/TDD PHONE (919) 572-2222<br />
www.medel.com
Hear.<br />
There and Everywhere.<br />
TM<br />
Every note of the flute solo in a child’s music recital.<br />
The sound of an arriving text message. A toddler’s<br />
first laugh. The cheers from teammates. The peeps,<br />
calls and trills in the backyard.<br />
Life is a composition of finely detailed sounds.<br />
MED-EL’s industry-leading cochlear implant innovations<br />
with FineHearing allow its recipients to hear<br />
*<br />
and appreciate the most obvious and the most<br />
elusive of them all.<br />
It’s a noisy world out there.<br />
Enjoy it.<br />
Help your patients hear life the way it was meant to sound.<br />
Begin their cochlear implant journey with MED-EL.<br />
MAESTRO cochlear implant system<br />
features the thinnest and lightest<br />
speech processor available today.<br />
* FSP is not indicated for use by pre-lingual children in the US.<br />
hearLIFE<br />
COCHLEAR IMPLANTS :: MIDDLE-EAR IMPLANTS<br />
TOLL FREE (888) MEDEL-CI (633-3524) :: V/TDD PHONE (919) 572-2222<br />
www.medel.com
Dr. Musiek discusses the<br />
distinction and overlap<br />
of neuropathy/auditory<br />
dys-synchrony and<br />
hyperbilirubinemia.<br />
<br />
<br />
<br />
<br />
<br />
Sexton discusses the<br />
CARE Project (training<br />
in Counseling, Aural<br />
Rehabilitation and<br />
Education), the seven stages<br />
of grieving related to hearing<br />
loss, and more.<br />
<br />
<br />
<br />
<br />
<br />
Soltes discusses service<br />
dogs, hearing dogs, and child<br />
advocacy dogs.
First Senior Friendly Television<br />
With hearing aid connectivity<br />
“1st Senior Friendly TV”<br />
-‐New York Post<br />
<br />
<br />
<br />
“Must Zzz TV”<br />
-‐New York Post<br />
A TV “engineered for <br />
simplicity.”<br />
-‐Senior Housing News<br />
TV Ears TV <br />
Model # 10510<br />
Located in Booth # 1801<br />
at AudiologyNOW<br />
As featured by:<br />
<br />
<br />
Engadget<br />
TV Ears TV is a 32 inch LCD 1080i television that is easy to use, easy to hear, and
The Sound Tracker:<br />
One Man’s Quest<br />
for Natural<br />
silence<br />
BY DAVID FABRY<br />
gordon hempton is an acoustic ecologist<br />
and Emmy award-winning sound recordist.<br />
He will be the General Assembly keynote<br />
and featured session presenter at this year’s<br />
AudiologyNOW! ® AT was able to spend a few<br />
tranquil moments with Hempton recently to<br />
discuss his search for a nice quiet place to rest.
The Sound Tracker: One Man’s Quest for Natural Silence<br />
question:<br />
If a tree falls in the forest but there is too much noise<br />
to hear it, is there still sound Gordon Hempton aims<br />
to find out. Hempton is an acoustic ecologist and<br />
Emmy award-winning sound recordist. For more than<br />
25 years, he has provided professional audio services<br />
to musicians, galleries, museums, and media<br />
producers. He has amassed a three-terrabyte library<br />
of natural sound recordings, with specific expertise<br />
in recording “quiet” environments that has fostered a<br />
passion for preserving what he refers to as “natural<br />
silence” in a noisy world.<br />
On Earth Day 2005, Hempton founded the One<br />
Square Inch Foundation as a means of highlighting<br />
the need for preserving quiet, which in turn helps<br />
us to hear and listen. More than a metaphor, One<br />
Square Inch is indeed a physical location in the<br />
Hoh Rain Forest, part of Olympic National Park—<br />
arguably the quietest place in the United States. It,<br />
too, however, is endangered, and Hempton has<br />
become a tireless advocate for the preservation<br />
of silence in our national parks. Hempton will be<br />
the General Assembly keynote and a featured session<br />
presenter at this year’s AudiologyNOW! ® , one<br />
week prior to the 40-year anniversary of Earth Day.<br />
Audiology Today was able to spend a few tranquil<br />
moments with Hempton recently to discuss his<br />
search for a nice quiet place to rest.
The Sound Tracker: One Man’s Quest for Natural Silence<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
GH: That’s correct. Your meeting presents a particular challenge<br />
for me as a speaker, because I know that everyone in<br />
the audience will be better educated than I am about audiology.<br />
Instead, my role as a speaker will be to bring the fine<br />
line between the hearing and nonhearing world into focus.<br />
<br />
My career has been to develop my listening skills and<br />
record the sounds of wilderness “soundscapes.” My work<br />
as a listener is now 30 years in the making and has taken<br />
me three times around the globe. I have probably the largest<br />
collection of sound recordings of natural places that<br />
have been recorded in this way.<br />
<br />
I record binaurally in digital format, providing a 360 degree<br />
recording under headphones that preserve the cues that<br />
form the acoustic images. It is a very precise art in that<br />
the placement of the binaural head produces profound<br />
differences in terms of what is heard. My presentation will<br />
include a lot of recordings that I think everyone will enjoy<br />
and illustrate my point better than my words can.<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Yes, my interest is in the sounds of what it is like for a<br />
human being to be there and take it all in. Interestingly,<br />
about a year ago, I fell in love with a woman named
The Sound Tracker: One Man’s Quest for Natural Silence<br />
Rebecca. What is interesting about Rebecca, and what she<br />
has really brought into my life, is an understanding not<br />
only of how special my hearing world is, but how profoundly<br />
different the nonhearing world is. While Rebecca<br />
considers herself to be “hearing impaired,” for a hearing<br />
person, she is deaf. She can be in a room with a smoke<br />
alarm going off, with the tea kettle going, while calmly<br />
reading a book because she is unaware of the commotion<br />
going on. On a lighter note, however, she wakes up to my<br />
snoring, so vibrations remain a very strong part of her<br />
sensitivity.<br />
<br />
<br />
It is, however, an example of how profoundly sound<br />
affects the way we think and even organize the world.<br />
We hear 24/7; we don’t have “earlids” that naturally block<br />
out sound. There are no higher vertebrate species that do<br />
not have the ability to hear, although there are vertebrate<br />
species that are blind. Hearing is essential for survival.<br />
But, while animals hear, not all listen, and those that do<br />
not are usually eaten by those that do. Hearing, more than<br />
any other sense, is required for survival.<br />
<br />
<br />
<br />
Just like water may be an unappreciated drink, because it<br />
is so essential, so basic, that we don’t even think about it.<br />
<br />
<br />
In my presentation, we will literally listen to sounds<br />
from all over the planet. I will demonstrate with acoustic<br />
images the way that objects and sounds behave.<br />
Generally, when we look out our window, we see that<br />
there are very few translucent or transparent objects—<br />
generally, most stuff is opaque. If we want to see 360<br />
degrees, we need to actually turn our heads. Therefore,<br />
our view of the world is linear, with one object in front of<br />
the other. There is a timeline, a set of priorities, and this<br />
I have found is the way that “visual” people organize the<br />
world.<br />
<br />
It’s down to the basic essential way of listening. Unlike<br />
vision, very few sounds entirely mask the detection of<br />
another sound. In other words, all these sound events<br />
accommodate each other in arriving at my ears. I use<br />
what I call a “soup pot” method, and I just let everything<br />
arrive, take it all in, and use it to decide how things sound.<br />
It is really beyond hearing—I am listening to the world.<br />
<br />
<br />
<br />
Well, I may challenge some of your members with how I<br />
lost my hearing for an 18-month period. I was surprised
The Sound Tracker: One Man’s Quest for Natural Silence<br />
to discover that as I went through a series of audiologists,<br />
I wasn’t being “heard.” As an audio engineer and acoustic<br />
ecologist, I could describe the frequencies and decibels of<br />
my loss. Statements were made first—not by an audiologist,<br />
but by a physician—that we should test my hearing<br />
to see if I had a hearing loss. I knew I had a hearing loss,<br />
but listening to the world is really a fundamentally different<br />
experience.<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
It was very frustrating, but really only a small frustration<br />
compared to frustration of not hearing. Ultimately, I<br />
recovered on my own after 18 months. When most people<br />
think about listening, they think about listening skills;<br />
they focus their attention on a particular acoustic event,<br />
like tones in a hearing test. When you listen, you let it all<br />
in. What I hope to convey to the audience is that was our<br />
general mode of operation. Before I went to school and was<br />
taught to listen.<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
The basis for this work is that with all the noise present<br />
in the modern world, we have created a lot of meaninglessness.<br />
If we were to simply step outside in New York or<br />
Miami and take all of the sounds in, we would go crazy.<br />
Couplers for<br />
Audiometer<br />
Calibration<br />
Let G.R.A.S. help you with your audiometer<br />
calibration needs. Visit us at AudiologyNOW<br />
– booth 2913 – and see our extensive<br />
program of ear simulators and couplers.<br />
For more information go to gras.dk<br />
US office<br />
2285 East Enterprise Parkway · Twinsburg · OH 44087, USA · E-mail: sales@gras.us · www.gras.us
The Sound Tracker: One Man’s Quest for Natural Silence<br />
When we live in cities, we “close down” our listening<br />
experience. Not so when we visit our national parks and<br />
other places around the planet that are set aside to have<br />
the experience of nature. These places are needed to<br />
restore our senses and “open up.” This is the standard of<br />
“true listening.”<br />
<br />
<br />
<br />
One Square Inch is located in the Hoh Rain Forest, part<br />
of Olympic National Park—arguably the quietest place<br />
in the United States. The exact location is marked by a<br />
experience is almost a supernatural sense of perception.<br />
“Natural silence” is the absence of noise pollution. One of<br />
the things that I will try to convey in my presentation is<br />
that natural silence is not the absence of anything but the<br />
presence of everything.<br />
<br />
<br />
<br />
<br />
Yes, it is very different from the experience of excluding<br />
the noises or your immediate environment for a couple of<br />
minutes. When you live and breathe the environment for<br />
When you live and breathe the environment for<br />
a period of hours or days, you feel remarkably<br />
different; you think different thoughts.<br />
small red-colored stone placed on top of a moss-covered<br />
log at 47° 51.959N, 123° 52.221W, 678 feet above sea level.<br />
Directions to the site can be found in the links section of<br />
the Web site (www.onesquareinch.org).<br />
<br />
<br />
Using my sound level meter (Bruel and Kjaer SLM 2225),<br />
the 60-second Leq is approximately 27 dBA.<br />
<br />
<br />
<br />
<br />
Even at that level, there still is a lot of central sound<br />
occurring. You are still able to hear the murmur of winged<br />
insects, the small hemlock needles lightly falling on the<br />
forest floor, birds singing quarter or half mile away, or<br />
the elk bugling from eight or nine miles away. A listener’s<br />
horizon is really quite distant, and so your sonic view<br />
of the place that you are in is extremely expansive. The<br />
a period of hours or days, you feel remarkably different;<br />
you think different thoughts. All of those trivial items on<br />
my “to-do” list fall off, they simply erode from my being,<br />
and I am left with what essentially matters to me. I leave<br />
the place with just a wonderful feeling.<br />
People ask me how I can think for a moment that I will<br />
be able to preserve a place—save silence—against all the<br />
noise intrusion of the world. And I tell them that silence<br />
tells me so. It is a powerful force of encouragement,<br />
listening to nature. That is essentially what I believe our<br />
National Parks are all about: a place to rejuvenate our<br />
senses and our spirits to become more productive, healthier,<br />
modern people. Unfortunately, although Olympic<br />
National Park is likely the quietest place in the lower 48,<br />
the noise levels have eroded substantially.<br />
<br />
The modern measure of silence today is the “noise free<br />
interval,” in minutes, between audible noise intrusion,<br />
and it has shrunk from several hours just 10 years ago to<br />
about an hour today. In 2008, I experienced 45 minutes<br />
of continuous jet traffic overhead at the One Square Inch
The Sound Tracker: One Man’s Quest for Natural Silence<br />
location. Many of the examples that I will present in<br />
the keynote speech and in the featured session will be<br />
examples of the type of sounds that we would miss with<br />
this elevated noise floor due to the intrusions. I hope that<br />
the recording will serve as an affirmation that we are all<br />
entitled to have a right to quiet.<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Yes. We can trace the increase in listening loss in modern<br />
literature. You can read incredible descriptions of nature’s<br />
music in the 1800s that literally almost evaporates in the<br />
writings of today. I will cite the works of Mark Twain and<br />
of John Muir, who describe “snow melting into music.”<br />
Even as a professional listener and nature sound recordist,<br />
the first time I heard that phrase I thought it was remarkable<br />
poetic license. I’m sure that it doesn’t really melt<br />
into music; it’s nothing that I would want to dance to or<br />
hum all day, but Muir had a neat way of putting words to<br />
it that I could remember. In my presentation, I will play a<br />
recording I made that captures what Muir was describing;<br />
whether we call it reggae or jazz, you won’t play it just<br />
once (also listen at www.audiology.org).<br />
<br />
<br />
<br />
<br />
<br />
Yes, silence has become an endangered species in our<br />
modern world. Alarmingly, in my 30 years of searching,
The Sound Tracker: One Man’s Quest for Natural Silence<br />
natural silence can be found in only a dozen or fewer<br />
remote locations. The evaluation period is right before<br />
dawn, when sound travels the furthest through natural<br />
environments because it is least likely to contain wind and<br />
often the atmospheric layers are set up into temperature<br />
layers, and so sound travels much further than predicted.<br />
There are 12 areas that I have identified, and have made<br />
none public except Olympic National Park because they’re<br />
still virtually unprotected except by their anonymity.<br />
Once we get some laws into place—one in particular<br />
that would ban all aircraft over just a handful of our most<br />
pristine national parks—it would deliver the noise-free<br />
experience that we have all been waiting for. The cost,<br />
according to the figures provided by the Air Transport<br />
Association, would amount to less than a dollar per passenger<br />
to route traffic around Olympic National Park.<br />
Further, this would cost less than a minute in travel time—<br />
far less of a consideration than weather and normal traffic<br />
delays. Presumably, the same figures would generally<br />
apply to avoid flying around other national parks as well.<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
The featured session is not entirely removed from the<br />
keynote address. Basically, the focus of the featured session<br />
will be to get participants to recognize and accept that they<br />
are “listening impaired” even if they have hearing within<br />
the normal range. Once we are willing to accept the fact<br />
that we are listening impaired, the session will focus on<br />
teaching participants to “lip read” nature. I draw a lot of the<br />
inspiration for this session from the special relationship<br />
that I have with my fiancée Rebecca. She shares a love of<br />
Olympic Park as I do—her love is of the scenic wonders, and<br />
mine is of the sonic events. The context of the session will<br />
be to tie in visual events to sonic events.<br />
<br />
<br />
Yes, in plant pathology. My training is in botany, and I<br />
found it worked very well for me with my work as an<br />
acoustic ecologist. Because the land and vegetation form<br />
the structure of the amphitheatre of wildlife, it is closely<br />
associated with the vegetation. From that, you can pretty<br />
much guess what the acoustics are going to be and what<br />
kind of wildlife is going to be audible.<br />
<br />
<br />
<br />
<br />
David Fabry, PhD, is the content editor for Audiology Today.<br />
He is also the managing director of AudioSync Hearing<br />
Technologies.<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
I have recorded underwater whales and dolphins, and will<br />
actually be leaving this week to record the songs of the humpback<br />
whale off the Kona Coast of Hawaii's Big Island. Noise<br />
intrusion certainly applies to aquatic animals as those on land.<br />
References
Visit us at<br />
booth 227<br />
Discover BestSound Technology.<br />
A new dimension in hearing.<br />
Take us for a test drive at AudiologyNOW! 2010.<br />
www.usa.siemens.com/hearing<br />
Copyright © 2010 Siemens Hearing Instruments, Inc. All rights reserved. SHI/11082-10.
RUMINATIONS<br />
OF AN OLD MAN<br />
A<br />
YEAR<br />
PERSPECTIVE<br />
ON CLINICAL<br />
PRACTICE<br />
BY DAVID LUTERMAN
I have been blessed with 50 years of active<br />
clinical involvement. I began my professional<br />
life as a diagnostic audiologist and morphed<br />
into a rehabilitation audiologist, specializing in<br />
helping families of newly diagnosed children<br />
with hearing impairments make the transition<br />
to their new reality. I feel incredibly fortunate to<br />
have stumbled into my life work, and have found<br />
a niche that nourishes me and, at the same<br />
time, benefits others. Immersed in my life journey,<br />
it seemed disjointed; from this vantage point it<br />
seems inevitable. At this stage in my life, I find<br />
myself more reflective with a strong desire to look<br />
back, distill my clinical experience, and pass it<br />
on to current and future generations of clinicians.
Ruminations of an Old Man: A 50-Year Perspective on Clinical Practice<br />
HERE, THEN, IS THE LUTERMAN 10:<br />
<br />
<br />
At heart, we are grief workers. We are dealing with<br />
people undergoing transitions in their lives because they<br />
have lost the life they thought they were going to have,<br />
whether this is the parent of an autistic child, the spouse<br />
of an aphasic patient, or the adult child of a nursing home<br />
patient. Grief is not culture bound or disability specific—it<br />
is endemic to disability. While many things have changed<br />
in our profession, the human equation is unchanging—<br />
we are dealing with clients who are emotionally upset,<br />
not emotionally disturbed. Grieving and the concomitant<br />
feelings are a normal response when a person is suddenly<br />
confronted with a life challenge in which there was no<br />
preparation. As a profession, we need to give ourselves<br />
permission to do the necessary grief work. While technology<br />
may have altered the therapeutic landscape, it<br />
doesn’t bypass the need to interact with our clients on an<br />
emotional plane.<br />
<br />
<br />
When people are emotionally upset they cannot process<br />
information well. I had to learn this the hard way as a<br />
practicing diagnostic audiologist. After making the diagnosis<br />
of hearing loss in a child, my notion of counseling at<br />
that time was to give information. I rapidly developed set<br />
speeches about the audiogram, hearing aid maintenance,<br />
and educational options. I gave these minilectures without<br />
recourse to the parent’s emotional state. What I learned<br />
on subsequent evaluations, much to my dismay, was that<br />
they retained almost nothing of what I had said. They were<br />
much too upset to retain much content, and, in fact, I had<br />
overwhelmed them with information and contributed to<br />
their fear and anxiety. Especially in the early stages of diagnosis<br />
people are helped best by being allowed to grieve.<br />
I have found that people are seldom allowed to grieve,<br />
as most people conspire to make them feel better. They do<br />
this by instilling hope (“They will find a cure”), or by positive<br />
comparisons (“It could be worse, he could have…”).<br />
All this serves to do is to emotionally isolate the person<br />
and deny him or her the right to grieve. What people in<br />
emotional pain often need the most is to be listened to<br />
and have their feelings validated. This is counterintuitive<br />
for most people as the tendency is to want to take<br />
the pain away by solving the problem or distracting them.<br />
I have learned that I cannot take the pain away; these<br />
disabilities represent a loss, and that loss will always be<br />
there despite anything I might say or do. What I can take<br />
away is “feeling bad about feeling bad.”<br />
Once, as I was beginning to facilitate a support group<br />
for parents of newly diagnosed deaf children, one mother<br />
looked at me and said, “you are going to make me cry,”<br />
and I said to her, “No. I am going to give you permission<br />
to cry,” whereupon she started to cry. In the past I would<br />
have felt guilty that I caused that parent to cry. What I<br />
have come to understand is that I am not putting the<br />
feelings in, but creating the conditions that enable the<br />
feelings to emerge. What I have also come to understand<br />
is that feelings just are—you do not have to be responsible<br />
for how you feel but always for how you behave. This<br />
notion has enabled me to enter the realm of feelings with<br />
clients to their benefit because embracing painful feelings<br />
is the first step in healing. The current emphasis on evidence<br />
based practice I find worrisome because emotional<br />
growth does not readily lend itself to measurement, yet it<br />
is in the emotional realm where a great deal of the action<br />
takes place. Communications is best achieved when there<br />
is both content and affect components present. I hope we<br />
can learn as a profession to balance our content counseling<br />
with our affect counseling and value both equally.<br />
<br />
<br />
The purpose of counseling is not necessarily to make<br />
people feel better—the entertainment industry does<br />
that. The goal of counseling should be to empower clients<br />
so that they can make self-enhancing decisions for<br />
themselves and their family members. In the course of<br />
the counseling experience, painful feelings will emerge,<br />
including anger. I have always seen the emergence of the<br />
painful feelings as a positive sign because these clients<br />
are not in denial, and if I am mindful of my role they will<br />
take ownership of the communication disorder. There<br />
can be no meaningful change without ownership of the<br />
problem by the client. Ceding responsibility to the client<br />
is often painful for clients in itself, as frequently they<br />
prefer a passive role in the habilitation process, hoping<br />
and expecting the professional to “fix” it.
Ruminations of an Old Man: A 50-Year Perspective on Clinical Practice<br />
<br />
<br />
As a beginning clinician, I assumed my professional role was<br />
to give information and direction to the client, that I needed<br />
to be a very active participant in the therapeutic process. I<br />
had a “lesson plan” mentality with specific goals in mind,<br />
and my scripted minilectures were designed to ensure that<br />
clients left our encounter with the information I thought they<br />
needed. In retrospect, I can see that the set speeches and<br />
advice giving were a reflection of my own insecurities and<br />
need to limit the clinical interaction in predictable, contentbased<br />
ways that I could manage. By listening to the client<br />
without a preconceived “lesson plan” enables the client to<br />
participate more fully in the therapeutic endeavor—it forces<br />
the client to be active in the relationship. Listening for client<br />
affect and reflecting it back enables the client to identify their<br />
feelings and express them in a safe relationship; this attenuates<br />
client isolation and validates their feelings. Listening<br />
deeply to our clients is a great gift we can give them.<br />
As I have become more self-confident in my clinical skills,<br />
I have been able to cede more and more control of the therapeutic<br />
process to the client. Learning proceeds best when<br />
the learner is an active participant in the process. Listening<br />
enables the clients to reveal themselves, allowing me to find<br />
ways to be most helpful. The client will teach us if we listen. I<br />
had to learn to cultivate the art of not doing and at the same<br />
time being present for the client. The irony here is that often<br />
the less I do, the more the client learns.<br />
<br />
<br />
In the early stages of diagnosis, clients are usually overwhelmed<br />
and feeling inadequate to cope with the disability.<br />
This is a critical juncture for the clinician because the<br />
tendency is to want to rescue the client from their actual<br />
and felt inadequacy. If we rescue by advice giving and taking<br />
responsibility from the client, we can contribute to their<br />
fear and sense of inadequacy. It is very easy to teach helplessness<br />
and create the dependent client who then accepts<br />
a passive role, expecting the clinician to fix it. I have had to<br />
learn how to be responsible to my clients rather than being<br />
responsible for them. Finding the therapeutic equator of<br />
helping is not easy because it is constantly shifting with<br />
each client and at different times with a client. I have had to<br />
learn to trust clients to eventually make the best decision<br />
for them, and that wisdom, which is the best use of information,<br />
resides within the client and not in me. My role is to<br />
judiciously share my information as a client needs and asks<br />
for it. I avoid giving advice and assuming responsibility for<br />
the client at all costs. Enhancing a client’s self-esteem is the<br />
Also of Interest<br />
<br />
<br />
<br />
<br />
<br />
<br />
premier goal of the therapeutic encounter, thereby creating<br />
the independent client who no longer needs us.<br />
Enjoy the<br />
rewards of<br />
practice growth!<br />
Call<br />
(866) 432-7500<br />
or go to<br />
MyEarQ.com<br />
Click on Member Login<br />
User Name: GrowMyPractice<br />
Password: Today<br />
Apply<br />
Today!
Ruminations of an Old Man: A 50-Year Perspective on Clinical Practice<br />
<br />
<br />
It is hard for me to conceive of a program that does not<br />
include a support group. Having a catastrophic event in<br />
your life becomes emotionally isolating because almost<br />
everyone in the client’s everyday life is invalidating their<br />
painful feelings while seldom understanding what the client<br />
is experiencing. The support group is usually the one<br />
place that individuals are understood, feelings can be validated,<br />
and help can be given and received. Professionals,<br />
by nonjudgmental listening, can validate feelings but lack<br />
the instant credibility that members of a support group<br />
have. Support groups are not disability specific.<br />
I think they are especially helpful for the families of<br />
clients who are often on the periphery of clinical services.<br />
Mixed support groups, where there are clients and family<br />
members, are very challenging to facilitate but usually<br />
helpful in promoting family unity. My major clinical role<br />
over the past 45 years has been as a group facilitator for<br />
parents of young children with hearing impairments. I<br />
have found this to be an immensely rewarding activity.<br />
Every group has presented unique challenges and invariably<br />
taught me something valuable<br />
<br />
<br />
It is unfortunate that students in our training programs<br />
are seldom exposed to a family-centered model of service<br />
delivery. The individual pullout model seems to be one<br />
of choice. I think this is an easier model to select for the<br />
beginning therapist as he or she need only focus on the<br />
identified patient. Unfortunately this is the least efficient<br />
way of working with clients. By working with the family<br />
unit we can extend the goals of therapy to the home and<br />
create an environment that is supportive of change. This<br />
model requires a greater skill set of a therapist because it<br />
mandates working with family members who do not have<br />
an overt communication disorder. Families also need<br />
to be broadly defined to include the environment of the<br />
client, whether this is a hospital setting or a classroom.<br />
Training programs need to see that the pull-out model<br />
is a way to start the training, but students need to be<br />
quickly exposed to and trained in the broader model of<br />
a family-centered approach to service delivery. Familycentered<br />
therapy needs to be the gold standard.<br />
<br />
<br />
Words spoken mechanically without feeling and/or out<br />
of context will never be helpful. “This too shall pass”<br />
were the words the wise men came up with for the king<br />
who wanted something to say for all occasions. There<br />
are counseling words that are equally useful, which I<br />
call affirmations. “It must be so hard” is an empathetic<br />
remark that validates the client’s experience, while<br />
“that’s okay” gives sanction to the client’s feelings. Even<br />
more useful is “uh huh,” which says to the client, “I hear<br />
you. Tell me more.” In a long counseling career, probably<br />
the most useful words to the clients are the ones I haven’t<br />
said.<br />
<br />
<br />
I have come to see that clinical mistakes are inevitable.<br />
Even after 50 years, I still have my occasional gaffes. I<br />
have had to learn to be gentle with myself and accept the<br />
fact that errors are an inevitable consequence of clinical<br />
growth. I think any learning and growing clinician needs<br />
to be pushing at the boundaries of their comfort zone;<br />
however, in that boundary region reside errors. I have<br />
learned that the “mistake” is a useful marker for what I<br />
need to learn. I learn best from my blunders, and it is only<br />
a mistake if I do it twice. Fortunately we are not brain surgeons,<br />
clients usually recover from the gaffes, and there<br />
is often an opportunity to apologize, correct the error, and<br />
move on, if the fundamental relationship is strong and<br />
can withstand errors.
Ruminations of an Old Man: A 50-Year Perspective on Clinical Practice<br />
<br />
<br />
On the surface, a counseling relationship looks conventional<br />
in that two people are dialoging. The reality is<br />
that one person—the counselor—is helping the other by<br />
practicing selfless, deep listening. The mantra for the<br />
counselor needs to be “it’s not about me.” Deep listening<br />
requires that the counselor put aside all personal agendas<br />
and be there in the service of the other. This is not<br />
an easy thing to do and is rarely experienced outside of<br />
a counseling relationship. Being in service to the other is<br />
very demanding, and, while in many cases technology<br />
has altered the clinical landscape, the most important<br />
clinical “tool” is still the clinician. Clinical tools need<br />
periodic care, and much like the audiologist sending the<br />
audiometer out to be recalibrated, clinicians must take<br />
periodic timeouts to recalibrate themselves. To be a selfless<br />
listener requires a personal centering that mandates<br />
that clinicians have a fulfilling personal life. We need to<br />
be able to give to our clients from our abundance. Too<br />
often one sees in the helping profession clinicians with<br />
strong needs to be needed that they try to fulfill by<br />
creating dependent relationships. Clinical burnout is a<br />
consequence of clinicians who do not practice good selfcare<br />
and have many dependent relationships.<br />
Fifty years seems like a long time, yet it has gone by bewilderingly fast. It has been a<br />
marvelous ride, much better than I ever expected. I am often asked how I have been<br />
able to remain clinically active for so long amid so much pain and suffering without<br />
burning out. For me it’s a matter of practicing good self-care, avoiding developing<br />
dependent relationships with clients, and, above all, understanding that personal<br />
growth is often forged in the crucible<br />
of the pain of these disabilities. I do not<br />
see these disabilities as tragedies but,<br />
rather, as powerful teachers that promote<br />
transcendence. We give to life what life<br />
demands, and the disabilities often force<br />
clients to develop capacities that would<br />
otherwise lie latent. I love being able to<br />
participate in promoting growth, and when<br />
you love what you do, it is not work. I have<br />
often been amazed that they actually<br />
pay me to do it. To participate in and<br />
facilitate the personal growth of clients<br />
provides moments of grace that make our<br />
profession so worthwhile. I would love to<br />
be around for another 50 years, but the<br />
actuarial tables are against me.<br />
David Luterman, DEd, is professor emeritus at Emerson College<br />
and director of the Thayer Lindsley Family-Centered Program.
PROVIDING REMOTE HEARING HEALTH CARE<br />
BY DE WET SWANEPOEL
The need for audiological services globally far outweighs<br />
the current capacity to deliver these services. Tele-audiology,<br />
which may include the full scope of audiological practice,<br />
offers one way of addressing the disparity between the need<br />
and availability of hearing health services.
Tele-audiolog y: Providing Remote Hearing Health Care<br />
Advances in technology and connectivity<br />
are rapidly changing the<br />
way people live and interact. Health<br />
care is no exception with technologies<br />
revolutionizing the precision<br />
and accuracy of diagnostics and<br />
intervention options. But technology<br />
is not only improving health-care<br />
equipment and devices, it is changing<br />
the very way in which health<br />
services are offered. Using information<br />
and communication technology<br />
(ICT) in health care may improve<br />
access to health care, enhance service<br />
delivery quality, improve public<br />
health and primary care effectiveness,<br />
and address the global<br />
shortage of health professionals<br />
through training (Wootton et al,<br />
2009). One of the uses for information<br />
and communication technology<br />
is telehealth. A variety of terms has<br />
been used to refer to this field of<br />
study, including telemedicine, telecare,<br />
e-health, and so on.<br />
The term telehealth literally means health-care provision<br />
at a distance (Wootton et al, 2009). It encompasses the<br />
full range of health care including screening, diagnosis,<br />
intervention, management, and education of personnel,<br />
patients, and the general population. Services may be provided<br />
in real time through a synchronous model whereby<br />
a live assessment is done with a video link, for example.<br />
Asynchronous services are not provided in real time but<br />
may, as an example, include e-mailing results to a professional<br />
for interpretation. Telehealth service-delivery<br />
models may well incorporate synchronous and asynchronous<br />
aspects, referred to as a “hybrid” model, depending<br />
on the nature of the services required and resources<br />
available (Krumm, 2007).<br />
<br />
Tele-audiology is the utilization of telehealth to provide<br />
audiological services and may include the full scope of<br />
audiological practice. A recent systematic review of teleaudiology<br />
reports have indicated that limited numbers of<br />
studies have been conducted in this field, but those that<br />
are available span audiological services, including screening,<br />
diagnosis, and intervention (Swanepoel and Hall,<br />
forthcoming). Screening applications have included otoacoustic<br />
emissions (OAE), automated auditory brainstem<br />
response (ABR), pure-tone audiometry, and speech-innoise<br />
in a range of populations including infants, children,<br />
and adults using synchronous, asynchronous, and hybrid<br />
models. Reports on diagnostic procedures through<br />
telehealth include video-otoscopy, pure-tone audiometry,<br />
hearing-in-noise testing, ABR, intraoperative monitoring,<br />
and balance evaluation. Intervention services through<br />
telehealth have included reports of hearing aid fitting<br />
and verification, cochlear implant programming, tinnitus<br />
therapy, and hearing aid counseling (Swanepoel and Hall,<br />
forthcoming). Despite the promising findings of initial
Tele-audiolog y: Providing Remote Hearing Health Care<br />
reports, there is a dearth of research reports on audiological<br />
practice and education facilitated through telehealth.<br />
Much work remains to be done to develop and validate<br />
the relatively new field of tele-audiology, but the impetus<br />
is increasingly apparent.<br />
<br />
The need for audiological services globally far outweighs<br />
the current capacity to deliver these services (Swanepoel,<br />
Clark, et al, forthcoming). Globally almost 10 percent of<br />
the world population is estimated to have a mild or greater<br />
degree of hearing loss (World Health Organization [WHO],<br />
2006). One in every four adults globally over the age of 45<br />
has a hearing loss, with 27 percent of men and 24 percent<br />
of women in this age group estimated to be affected<br />
(Lopez et al, 2006; WHO, 2008). It is not surprising that it<br />
is ranked as the most prevalent chronic disability globally,<br />
and with increasing global life expectancy, its prevalence<br />
is expected to increase significantly (WHO, 2008).<br />
In the face of the overwhelming prevalence and<br />
burden of hearing loss on a global scale, there is a severe<br />
paucity of hearing health-care professionals to provide<br />
the necessary services. Surveys indicate that in developing<br />
countries the ratio of audiologists to the general<br />
population varies from 1 to 500,000 to as high as 1 to<br />
6.25 million (Goulios and Patuzzi, 2008; Fagan and Jacobs,<br />
2009). In the continent of Africa, with more than 48 countries,<br />
professional tertiary qualifications in audiology are<br />
only available in two countries. It is not only in developing<br />
countries that there is a dearth of hearing health-care<br />
services, however. A recent report indicated that the<br />
estimated number of audiograms required in the United<br />
States with the capacity of current professionals in the<br />
field showed an annual shortfall of 8 million audiograms,<br />
estimated to increase to 15 million by 2050 (Margolis and<br />
Morgan, 2008). Apart from the mismatch between the<br />
need for, and capacity to deliver, services, the availability<br />
of professionals is often unequally distributed. In the<br />
United States, for example, underserved areas may be in<br />
inner cities or rural communities spread across vast geographical<br />
areas (e.g., Alaska) where professionals are not<br />
available to deliver on-site hearing health care.<br />
Globally it is clear that the demand for audiological<br />
services is extensive and the capacity to deliver these services<br />
limited. Tele-audiology offers one way of addressing<br />
this disparity between need and availability of hearing<br />
health services. The ability to evaluate patients remotely<br />
can increase health-care efficiency but also enables populations<br />
to be reached that may have been unable to access<br />
services previously. Integration of automated testing<br />
for use with asynchronous tele-audiology may further<br />
optimize resources by allowing audiologists to interpret<br />
results remotely while reserving more time-intensive<br />
synchronous testing for complex cases. The possibilities<br />
seem limitless, and the growth in connectivity, especially<br />
through cellular networks, is making access in<br />
remote areas such as central Africa a reality (Swanepoel,<br />
Olusanya, et al, forthcoming).<br />
<br />
<br />
A recent study reported the first systematic validation of<br />
intercontinental pure-tone audiometry using a synchronous<br />
telehealth configuration (Swanepoel, Koekemoer,<br />
et al, forthcoming). The audiologist conducting the<br />
assessment was in Dallas, Texas, and the subjects being<br />
tested were in Pretoria, South Africa. At the patient site,<br />
a facilitator established connectivity, ensuring that the<br />
audiometer, which is PC-based, was operational and that<br />
the earphones were placed correctly ().
Tele-audiolog y: Providing Remote Hearing Health Care<br />
A 3G cellular network Internet connection was used at<br />
the remote site with a netbook running the audiometer<br />
the computer in Pretoria to facilitate remote testing. The<br />
audiologist conducting the test could see the subject and<br />
Initial findings demonstrate that remote<br />
audiometry across continents is feasible and<br />
equivalent to conventional audiometry.<br />
software (). The computers at both sites were<br />
configured with interactive video software, and remote<br />
computing was performed through application sharing<br />
software whereby the audiologist in Dallas controlled<br />
<br />
<br />
<br />
<br />
<br />
gave instructions before commencing pure-tone air-<br />
conduction audiometry ().<br />
Thirty subjects were evaluated remotely and with<br />
a conventional face-to-face setup. The tele-audiology<br />
thresholds corresponded within 5 dB or less of conventional<br />
audiometry thresholds in 96 percent of the 420<br />
comparisons. The threshold correspondence was even<br />
better when compared in cases of hearing loss. The patient<br />
response times were also very similar with a range of 503–<br />
676 msec poststimulus response time for conventional<br />
audiometry and 481–732 msec for remote audiometry. In<br />
terms of time efficiency, the remote testing on average<br />
required a 20 percent longer test duration to complete both<br />
ears and is probably attributable to the slight transmission<br />
delay in the connection (Swanepoel, Koekemoer, et<br />
al, forthcoming). Further investigations using air and bone<br />
conduction are still required, but initial findings demonstrate<br />
that remote audiometry across continents is feasible<br />
and equivalent to conventional audiometry.<br />
<br />
In a certain respect, the mainstay of audiology, pure-tone<br />
audiometry, has always been conducted at a distance.<br />
The patient is seated inside the sound booth while the<br />
audiologist is outside. With tele-audiology, the distance<br />
separating clinician from patient is just increased, and<br />
in some cases they are on opposite sides of the globe.<br />
Conducting services at these distances may require some<br />
adaptation to conventional equipment features. Teleaudiology<br />
assessments or interventions require PC-based<br />
equipment. Objective test procedures like OAE and ABR<br />
may therefore be more easily suited to tele-audiology<br />
since they are software operated from a PC interface.<br />
Remote audiometry therefore ideally requires a<br />
PC-based audiometer. Employing innovative features<br />
can make such an audiometer uniquely telehealth<br />
compliant. The audiometer used in the intercontinental
Tele-audiolog y: Providing Remote Hearing Health Care<br />
<br />
<br />
<br />
<br />
<br />
audiometry study (Figure 1), for example, employs<br />
several novel features that make it especially suited<br />
to remote testing (Swanepoel, Koekemoer, et al, forthcoming).<br />
For quality control purposes, it includes a<br />
microphone on the outside cup of the circumaural<br />
earphone to monitor the environmental noise levels. An<br />
additional microphone on the inside of the earphone<br />
provides a measure of the attenuation of the environmental<br />
noise. This is particularly useful in underserved<br />
areas, where sound booths may be unavailable, and<br />
provides a way of ensuring that the environmental<br />
noise is acceptably low. Additional attenuation is furthermore<br />
provided by using insert earphones covered<br />
by circumaural earphones (Figure 1). Software features<br />
include visual feedback on patient responses; a<br />
green marking on the audiogram means the patient<br />
responded within 1.5 msec after stimulus presentation<br />
while a yellow marking indicates no response within<br />
that time frame (Figure 3). These features provide a<br />
means of quality control and active feedback from the<br />
patient site to bridge the limitations of not being present<br />
on-site with the patient. Similar features may easily be
Tele-audiolog y: Providing Remote Hearing Health Care<br />
employed in other audiological devices for screening,<br />
diagnostic, and intervention purposes.<br />
PC-based audiometry offers a further advantage in<br />
underserved areas with the inclusion of an automated<br />
test paradigm. In a region like Africa where there are very<br />
few audiologists and an overwhelming need for services,<br />
automation can be integrated with an asynchronous<br />
tele-audiology configuration (Swanepoel, Olusanya, et<br />
al, forthcoming). Automated pure-tone audiometry may<br />
be supervised by a facilitator and the results interpreted<br />
by remote audiologists, for example. A recent report<br />
evaluated the effectiveness of automated pure-tone<br />
air-conduction audiometry using a telehealth-compliant<br />
PC-based audiometer (Swanepoel, Mngemane, et al,<br />
forthcoming). Findings demonstrate close correspondence<br />
between manual and automated thresholds, especially in<br />
hearing-impaired subjects where 98 percent of thresholds<br />
corresponded within 5 dB or less of each other. A combination<br />
of asynchronous and synchronous tele-audiology<br />
services must be designed according to the specific needs<br />
of each context. These services are in the very early<br />
stages, however, and pilot studies are required to validate<br />
models of service delivery while providing evidence-based<br />
guidelines.<br />
<br />
Advances in technology and connectivity make tele-<br />
audiology a very real service-delivery option for audiologists.<br />
The advantages include increasing the reach and<br />
capacity of audiological services, distributing services<br />
more equally across regions and into remote or underserved<br />
areas, and conducting humanitarian outreaches<br />
that are sustainable and cost-effective across continents.<br />
Remote audiological services, which can cross state and<br />
national borders, however, also pose a unique set of<br />
questions related to licensure, jurisdictional responsibility,<br />
certification, reimbursement, and quality control<br />
(Swanepoel, Clark, et al, forthcoming). Professional<br />
organizations provide basic guidelines and benchmarks<br />
for tele-audiology but should be expanded to also consider<br />
cross-country service delivery (American Speech-<br />
Language-Hearing Association [ASHA] Working Group<br />
on Telepractice, 2005; American Academy of Audiology<br />
[AAA], 2008). A recently formed nonprofit organization,<br />
the Tele-Audiology Network (www.teleaudiology.org), was<br />
set up with the aim of providing audiologists around the<br />
world the opportunity to volunteer their professional<br />
services through tele-audiology applications to remote<br />
clinics in developing countries (Swanepoel, Clark, et al,<br />
forthcoming).<br />
Nonetheless, the application of telehealth to hearing<br />
health care is an emerging field with a broad scope of exciting<br />
application possibilities including training/education,<br />
screening, diagnosis, and intervention. As audiologists it<br />
is necessary to actively direct and monitor the development<br />
of tele-audiology, rethinking existing service-delivery<br />
models and embracing the potential benefits that improved<br />
connectivity and technology may afford to provide quality<br />
services to as many people, in as many places, as possible.<br />
De Wet Swanepoel, PhD, is associate professor in the<br />
Department of Communication Pathology, University of<br />
Pretoria, South Africa, and adjunct professor in the Callier<br />
Center for Communication Disorders, School of Behavioral and<br />
Brain Sciences, University of Texas at Dallas.<br />
References
Tele-audiolog y: Providing Remote Hearing Health Care<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Also of Interest
Neither academic<br />
programs nor industry<br />
are bound by the same<br />
ethical framework<br />
as members of a<br />
professional organization.<br />
The purpose of this<br />
document is to propose<br />
guidelines that could be<br />
voluntarily adopted by<br />
academic programs and<br />
industry. This article<br />
is an opinion editorial<br />
developed by the<br />
authors listed and has<br />
not been endorsed by<br />
any organization.
Guiding<br />
Interaction<br />
FOR THE<br />
BETWEEN<br />
Programs<br />
Industry<br />
AND<br />
BY IAN M. WINDMILL, BARRY A. FREEMAN, JAMES JERGER,<br />
AND JACK M. SCOTT<br />
IN<br />
It is imperative that both audiology programs and industry work together to identify<br />
and manage potential conflicts of interest to ensure that the relationship remains both<br />
successful and ethical, and thereby assures that the welfare of the consumer (including<br />
students and clinical patients) is paramount in their interactions.
Guiding Principles for the Interaction Between Academic Programs in Audiology and Industry<br />
he American Association of Medical<br />
Colleges (AAMC, 2008) recently<br />
published a report titled Industry<br />
Funding of Medical Education. The AAMC<br />
recognized the necessity of an<br />
effective relationship between<br />
medical schools and industry, and<br />
produced a set of guidelines that<br />
could be used by member schools<br />
to reduce potential conflicts of<br />
interest and to establish rules<br />
that define appropriate interaction<br />
with industry. The report of the AAMC focuses on issues<br />
between clinical faculty and pharmaceutical companies<br />
but also includes sections on relationships with manufacturers<br />
of medical devices.<br />
Members of professional organizations are subject<br />
to codes of ethics and ethical practice guidelines. While<br />
individual faculty or employees of industry may be members<br />
of a professional organization, and therefore subject<br />
to these codes of ethics, neither academic programs nor<br />
industry are “members,” and thus are not similarly bound<br />
to the same ethical framework. Therefore, academic<br />
programs and industry must voluntarily adopt guidelines<br />
that assure appropriate interaction. In addition, those<br />
guidelines should assure that those individual faculty or<br />
employees of industry who are members of professional<br />
organizations are not placed in positions whereby their<br />
individual ethical standing is compromised.<br />
The AAMC report served as a template for the development<br />
of these guidelines for the relationship between<br />
academic programs in audiology and industry. More<br />
importantly, these guidelines were developed with input<br />
and consensus of individuals from both academia and<br />
industry. The purpose of these guidelines is to provide a<br />
framework by which academic programs and industry can<br />
continue to work together to advance the diagnosis and<br />
treatment of hearing and balance disorders, to provide<br />
educational support for future generations of audiologists,<br />
and to assure public confidence in the relationship.<br />
<br />
Over the past 20 years, the relationship between universities<br />
and various forms of commercial enterprises has<br />
grown substantially. While there are the more obvious<br />
partnerships for sponsorship of football stadiums and<br />
basketball arenas, there are many more partnerships<br />
that have evolved as the direct result of partnering with<br />
industry for teaching and research endeavors. In fact,<br />
universities are actively engaging business ventures and<br />
partnerships both for expanded funding and for increasing<br />
academic standing.<br />
Therefore, it is not surprising that partnerships have<br />
also evolved between academic programs in audiology and<br />
industry. Many of the product development advancements<br />
and clinical enhancements realized over the past 40 years<br />
would not have been possible without a close working relationship<br />
between industry and universities. The emphasis<br />
on development of evidence-based clinical practice and<br />
research necessarily encompasses a relationship between<br />
engineers, scientists, clinicians, and consumers. Those<br />
industries that serve the hearing and balance areas are recognized<br />
leaders in the development of both new techniques<br />
and technologies and partner with universities in product<br />
development and validation. Restrictions on these relationships<br />
can seriously hamper technological advancements.<br />
In addition, industry often provides economic and<br />
other resources for training programs and research<br />
within audiology programs. In a broad sense, this partnership<br />
is fundamentally necessary to ensure continued<br />
advances in the prevention, diagnosis, and treatment of<br />
hearing and balance disorders. Examples of some of the<br />
health benefits derived from the close working relationships<br />
between academe and industry include advances in<br />
amplification, cochlear implants, and electrophysiologic<br />
test procedures.<br />
<br />
Audiology programs have increasingly sought industry<br />
support for many aspects of their core educational<br />
missions. While support is most commonly sought for<br />
research activities, financial or in-kind support has also<br />
been sought for student scholarships, learning labs, guest<br />
lectures, teaching equipment (e.g., computers, projectors,<br />
software, etc.), clinical equipment (e.g., audiometers,<br />
verification systems, etc.), furniture, and even bricks and<br />
mortar. This relationship, though common, must be conducted<br />
in such a manner as to assure the objectivity and<br />
integrity of academic teaching, learning, and practice.<br />
Both audiology programs and industry require public<br />
confidence and trust to be successful and, therefore,<br />
must be mindful to avoid those activities that may create<br />
an apparent conflict of interest. In addition, industry<br />
and university relationships should be transparent to<br />
students. The university must present an ethical model<br />
that can serve as a model for students who will graduate<br />
and may have similar relationships with industry<br />
in their careers. As there are fundamental differences<br />
between academic programs and commercial enterprises<br />
in terms of both missions and financial obligations, it is
Guiding Principles for the Interaction Between Academic Programs in Audiology and Industry<br />
possible that potential conflicts of interest could arise in<br />
the course of their interactions. It is imperative that both<br />
audiology programs and industry work together to identify<br />
and manage these potential conflicts to ensure that<br />
the relationship remains both successful and ethical, and<br />
thereby assures that the welfare of the consumer (including<br />
students and clinical patients) is paramount in their<br />
interactions.<br />
While the relationship between pharmaceutical<br />
companies and physicians has received much attention<br />
over the past several years, practitioner relationships<br />
with other sectors of industry, including medical device<br />
manufacturers, also have the potential for conflict of<br />
interest. While pharmaceuticals and medical devices<br />
are fundamentally different, there is a risk of inappropriate<br />
influence on students and patients if guidelines are<br />
not developed to assure a fair and balanced approach to<br />
education. Clinical and academic content decisions must<br />
be made by university faculty based on student education<br />
and clinical training needs rather than on the relationship<br />
with the commercial enterprise. Universities must avoid<br />
a perception of motivation for financial gain rather than<br />
objective, patient-centered practice and clinical education.<br />
<br />
The relationship between academic programs and<br />
industry is more complex than that between private<br />
practitioners and industry. There are four areas in which<br />
potential conflicts of interest may arise for academic<br />
programs in their interactions with industry: (1) with<br />
academic and clinical faculty; (2) with students; (3) with<br />
the clinics associated with the program; and (4) with the<br />
program itself.<br />
<br />
The relationship between individual faculty and industry<br />
is perhaps the most obvious and common relationship.<br />
Faculty often relies on industry to provide funding for<br />
research activities and publications, a practice that has<br />
occurred for decades. These opportunities for faculty<br />
often lead to advancements in the university, including<br />
promotion and tenure. Conversely, industry relies on<br />
ES3 Automatic<br />
In a tough economy, get the most for your money!<br />
You can with every Earscan® audiometer.<br />
Coming Soon...<br />
arscan4<br />
®<br />
Optional Dual station automatic audiometry– conduct<br />
2 tests at once.<br />
Integrated bioacoustic simulator– no other<br />
hardware to buy.<br />
USB connectivity & audio capability– hook up as<br />
many audiometers as you need with USB hubs.<br />
ES3M Manual<br />
Optional sound room monitoring.<br />
ES3S Screening<br />
Audiometer control software included.<br />
Optional database management software.<br />
www.microaud.com<br />
866-327-7226<br />
Micro Audiometrics<br />
C O R P O R A T I O N<br />
®<br />
Designed & Manufactured in the USA.<br />
See us at Booth #2437<br />
AudiologyNOW! 2010<br />
San Diego, CA<br />
A family owned business since 1980.<br />
Celebrating our 30th Anniversary!
Guiding Principles for the Interaction Between Academic Programs in Audiology and Industry<br />
faculty to conduct independent research, often with an<br />
eye toward verification of findings or development of new<br />
strategies that may benefit the commercial enterprises<br />
of the company. In this regard, faculty and industry must<br />
strive to manage these relationships to ensure the integrity<br />
of the results of such ventures.<br />
Beyond the obvious relationship of funding for<br />
research, faculty can have other relationships with industry.<br />
These include being an invited speaker for continuing<br />
education courses, providing consultation with industry,<br />
or being an instructor on recently developed technologies.<br />
In each of these cases, the opportunities for conflicts of<br />
interest arise as they can with the other more historically<br />
commonplace practices. Whether it be accepting royalties<br />
from a textbook that then becomes a required text in<br />
a course taught by the author, or accepting desk copies<br />
of textbooks considered for adoption for classes, these<br />
activities all present a potential conflict of interest.<br />
<br />
Paradoxically, the impressionable nature of students<br />
would appear to make them most vulnerable to conflicts<br />
of interest from industry, yet they are not, for the<br />
most part, in any position to exercise decisions regarding<br />
industry. Students could be influenced by gifts, trips,<br />
scholarships, and other benefits from industry, but as<br />
they are unlicensed and hold no decision-making roles<br />
within academic programs or clinics, they are perhaps<br />
not in a position to be conflicted, but they certainly may<br />
be impressionable. However, the potential does exist that<br />
relationships established prior to graduation may carry<br />
over to practice after graduation. Therefore, university<br />
programs and preceptors have a responsibility to discuss<br />
ethical guidelines and to model best practices to students,<br />
to assure that students understand the potential impact of<br />
relationships that could be established prior to graduation.<br />
<br />
The one area that would seem most likely to give rise<br />
to conflicts is the patient care activities associated with<br />
academic programs. While academic programs may operate<br />
a teaching clinic as part of their training program, and<br />
clinical faculty may provide services in those clinics, it is<br />
most often the case that neither the clinic nor the faculty<br />
operates as a traditional for-profit business. That is, the purpose<br />
of the clinic is not to maximize profits, but rather, to<br />
provide a consistent and controlled teaching environment<br />
for students. Similarly, faculty compensation is generally<br />
not tied to the profitability of the clinic and therefore<br />
would be less likely to be influenced by industry or other<br />
external forces. However, exceptions do exist, such as faculty<br />
practices. These issues will, however, likely pertain to<br />
clinical environments external to the university as well as<br />
to preceptors within those environments. As it is possible<br />
that students may rotate through these clinical environments,<br />
preceptors should be advised of their responsibility<br />
to model best ethical practices for the students.<br />
<br />
Universities, in general, and academic programs specifically,<br />
establish relationships with industry, often with an<br />
eye toward funding basic teaching endeavors. Academic<br />
programs will solicit donations from industry to fund<br />
faculty salaries, continuing education programs, classroom<br />
technology, scholarship programs, or teaching<br />
laboratories. Industry often provides funding or in-kind<br />
gifts in this regard. The question is whether these gifts<br />
could influence a program in a way that might influence<br />
patient care activities or students. The obvious concern<br />
to academic programs in audiology is that the program<br />
may exert influence on the clinical entities of the program<br />
to make patient care decisions based on these gifts.<br />
For example, a gift from a hearing instrument manufacturer<br />
for classroom technology may result in patients<br />
being counseled toward that particular device or students<br />
gravitating toward those manufacturers and their<br />
products, rather than other devices that may be available,<br />
after graduation.<br />
<br />
<br />
Audiology programs and industry share the goal of<br />
educating students to provide quality hearing and balance<br />
care to patients, as well as advancing knowledge in<br />
auditory and vestibular sciences. The basic principles that<br />
should guide decisions regarding interactions between<br />
academic programs in audiology and industry include:<br />
• The interaction should serve the interests and legitimate<br />
missions of both the academic program and industry.<br />
• From the academic program’s perspective, the interactions<br />
must serve legitimate educational or research<br />
purposes.<br />
• Any interactions should serve to enhance the hearing<br />
or balance health of the public.<br />
• All interactions should be disclosed and transparent.
LEADING THE WAY<br />
ONE INNOVATION AT A TIME<br />
© 2009 Starkey Laboratories, Inc. All Rights Reserved. 6/09<br />
StarkeyPro.com
Guiding Principles for the Interaction Between Academic Programs in Audiology and Industry<br />
• The interactions should involve open communication<br />
between knowledgeable parties.<br />
• The interactions should support and enable the free<br />
exchange of information in appropriate settings in a<br />
manner consistent with professional behaviors.<br />
• Interactions should not involve any quid pro quo<br />
between the program and industry beyond that consistent<br />
with fair market value of products used by the<br />
academic program and/or clinic and associated services.<br />
<br />
<br />
• Audiology programs should adopt and implement guidelines<br />
that address specific interactions between faculty,<br />
students, clinical sites, and industry. These guidelines<br />
should be designed to assure that a principled relationship<br />
occurs that promotes the educational mission of<br />
programs, enhances the experiences of students, and<br />
advances knowledge of hearing and balance disorders.<br />
• Guidelines should be applied with fairness and consistency,<br />
keeping in mind that relationships evolve over<br />
time. Guidelines should govern all interactions with<br />
any sector of industry and should not discriminate<br />
based on the size of the company, the financial opportunities<br />
involved, or personal relationships.<br />
• “Industry” includes all vendors and/or prospective<br />
vendors including manufacturers of diagnostic equipment<br />
or treatment technologies, classroom or learning<br />
technologies, publishing companies, or other such<br />
industries that are related to student education, clinical<br />
services, or research.<br />
• Guidelines should adhere to the rules and regulations<br />
of the institution of the academic program.<br />
<br />
<br />
• Compensation for services, including reimbursement<br />
for expenses, honoraria, or serving in an advisory<br />
capacity, should be at fair market value and commensurate<br />
with the participation of the faculty or program.<br />
• Industry must recognize their obligation to permit<br />
university programs and faculty to make independent<br />
decisions regarding industry products.<br />
• There is a recognized and necessary interaction<br />
between manufacturers and practitioners (which<br />
includes university faculty), including<br />
<br />
<br />
<br />
The collaborative processes in the innovative and<br />
creative development of devices;<br />
The training, instruction, education, services, and<br />
technical support provided to practitioners to<br />
assure the safe and effective use of products; and<br />
The needed support for research and education<br />
provided to develop technologies that better serve<br />
the public.<br />
<br />
<br />
<br />
There is a growing body of evidence from the social sciences<br />
that gifts of any value may affect the objectivity of clinical<br />
decision making. One-on-one gifting relationships of all<br />
kinds engender feelings of reciprocity that can unwittingly<br />
bias decision making, by recipients in favor of donors’ interests.<br />
These concerns are particularly targeted at clinical<br />
decision making whereby the objectivity of the audiologist<br />
in patient care activities could be called into question.<br />
The clinical arm of audiology programs is not immune<br />
to the potential of bias in clinical decision making.<br />
However, many academic audiology clinics are often operated<br />
in a manner that is atypical of for-profit clinics and<br />
often rely on a variety of resources to maintain their operations,<br />
including direct state funding, grants, in-kind gifts,<br />
donations of equipment, and direct or indirect financial<br />
gifts. Important in this regard is to separate “gifts” that<br />
are provided for legitimate educational purposes versus<br />
gifts that potentially induce bias, particularly if the gift<br />
is directed at an individual (e.g., clinical audiologists) as<br />
opposed to the academic program as a whole. Individuals<br />
who provide clinical service, even within this environment,<br />
must maintain objectivity in clinical decision making and<br />
in regard to the preparation of future clinicians.<br />
<br />
• Audiology programs should establish and implement<br />
guidelines on the type and extent of gifts that may be<br />
accepted by faculty from industry. These guidelines
Guiding Principles for the Interaction Between Academic Programs in Audiology and Industry<br />
should include a definition of what constitutes a gift<br />
(e.g., dinner with industry representatives, anatomical<br />
models, textbooks, travel grants, etc.), as well as any<br />
value limits on those gifts.<br />
• Gifts provided to the academic program in general<br />
should serve a legitimate educational purpose. In this<br />
regard, such benefits may include, but not be limited<br />
to, enhancing the curriculum, expanding service<br />
delivery, developing research programs, improving<br />
infrastructure, or augmenting faculty development<br />
programs.<br />
• Any gift that establishes a quid pro quo should be<br />
prohibited.<br />
• All gifts should serve legitimate educational purposes.<br />
• Honoraria for services provided should not be considered<br />
gifts but should be equivalent to fair market<br />
values for compensation for the services or time<br />
rendered.<br />
<br />
Equipment and devices are used extensively in the<br />
provision of services to patients with hearing or balance<br />
disorders. Representatives of industry can play an<br />
important role in introducing new technologies as well as<br />
provide training and support on the proper use of devices<br />
by practitioners, and thus may have legitimate reasons<br />
to be present in the clinics or classrooms of academic<br />
programs in audiology. Frequently, their presence is<br />
essential when devices are initially used with patients.<br />
Also, industry representatives may participate in the educational<br />
mission of an academic program through direct<br />
or indirect instruction. Nonetheless, there is the potential<br />
that certain interactions with industry representatives<br />
can also compromise independence of decision making<br />
and professionalism.<br />
<br />
<br />
• Student interaction with industry representatives<br />
should be primarily for the purpose of education.<br />
• Industry representatives who are invited to observe or<br />
participate in interactions between patients and the<br />
faculty and staff of an audiology program clinic, or<br />
participate directly or indirectly in the instructional<br />
endeavors, should be identified by the program as<br />
consultants and not as part of the faculty. Industry<br />
representatives in patient care activities should be<br />
sanctioned by the program, and their presence should<br />
be fully disclosed and consented to by patients before<br />
the representatives are permitted to be present during<br />
patient care interactions.<br />
<br />
<br />
Industry is a common source of funding or speakers for<br />
continuing education activities associated with academic<br />
programs in audiology. The credibility of audiology<br />
programs requires that CE programs sponsored by the<br />
academic program be legitimate, academically oriented,<br />
and open to a variety of viewpoints.<br />
<br />
<br />
• Academic programs and industry should be able to<br />
sponsor and/or plan CE programs together. Programs<br />
that serve as marketing vehicles for industry should be<br />
identified as such.<br />
• Industry funding sources should be directly acknowledged<br />
in all announcements and literature about<br />
particular CE offerings, in the presentations and<br />
forums as required by CE agency standards, and in all<br />
publications about the programs.<br />
• Meals, travel, and lodging can be provided for participants<br />
so long as those items are consistent to the<br />
scope of the program and are offered without expectation<br />
of quid pro quo.<br />
• Access for industry representatives should be based<br />
on guidelines and procedures that are well considered,<br />
clearly interpreted, and consistently and fairly<br />
applied. Faculty, staff, and students of an audiology<br />
program, along with industry representatives must be<br />
made aware of and held accountable for abiding by the<br />
guidelines and procedures in this regard.<br />
• Academic programs offering CE programs should<br />
familiarize themselves with standards for continuing<br />
education and strive to assure programs with industry<br />
sponsorship or participation meet those standards.<br />
Approved continuing education credit should be<br />
offered when available. Programs not approved for CE<br />
credits should be identified as such.
Guiding Principles for the Interaction Between Academic Programs in Audiology and Industry<br />
<br />
<br />
Industry often takes the lead in the development of new<br />
technologies, expanded applications of existing technologies,<br />
or advances in the diagnosis and/or treatment<br />
of hearing and balance disorders. The dissemination of<br />
this information to the audiology community is critical<br />
to assuring appropriate understanding and use of these<br />
developments. As such, industry has a responsibility to<br />
provide educational programs to faculty whose role it is<br />
to teach the next generation of practitioners. Educational<br />
events in which information is transferred between<br />
industry and academic faculty and students, whether at<br />
the academic institution or at another location, serves to<br />
assure that advances in knowledge and technology are<br />
available in a timely manner. Thus, students have the<br />
opportunity to learn about the most contemporary developments<br />
in hearing and balance health care.<br />
Faculty are often called upon to participate in industrysponsored<br />
educational programs due to their expertise or<br />
experience. In fact, the credibility of these programs may<br />
be enhanced due to the reputations of the faculty speakers<br />
and their academic institutions. These programs may<br />
provide legitimate educational opportunities to those<br />
in attendance. However, faculty should be cautious in<br />
participating in industry-sponsored programs whose sole<br />
purpose is marketing, the enhancement of the reputation<br />
of the company, or for which a quid pro quo is expected.<br />
It is important to note that this caution does not extend<br />
to programs where faculty present to peers the results of<br />
industry-sponsored research provided there is the opportunity<br />
for critical review and discussion.<br />
Students can benefit from the expertise, clinical skills,<br />
and technology available from industry. To not allow students<br />
to attain these benefits is to deny the contributions<br />
of industry to auditory and vestibular science. However,<br />
students are also vulnerable and impressionable, so it is<br />
the responsibility of the faculty, academic programs, and<br />
industry to protect students from those situations that<br />
could potentially exploit their naïveté.<br />
<br />
<br />
• Audiology programs should develop guidelines that<br />
define appropriate and acceptable levels of involvement<br />
of faculty and students in industry-sponsored<br />
educational programs.<br />
<br />
<br />
appropriate use of faculty names and affiliations<br />
for use in industry-sponsored educational activities.<br />
Audiology programs should require full transparency<br />
and disclosure by their faculty with respect<br />
to their role in industry-sponsored educational<br />
programs.<br />
Audiology programs should develop guidelines<br />
with respect to faculty participation in speakers<br />
bureaus.<br />
• Academic programs should assist students in differentiating<br />
those industry-sponsored programs that serve<br />
a legitimate educational purpose from those that do<br />
not. Faculty should also provide insight and advice to<br />
students to assure they understand the purpose of their<br />
participation.<br />
• Audiology programs should require that payments<br />
to faculty for participation in industry-sponsored<br />
Upcoming Web Seminars<br />
MARCH 2010<br />
Global Audiology: Humanitarian Audiology<br />
for Beginners<br />
APRIL 2010 (LIVE FROM AUDIOLOGYNOW!)<br />
Marion Downs Lecture: Optimizing Early Word<br />
Learning In Infants with Hearing Loss<br />
Multidisciplinary Clinical Model for Managing<br />
Patients with Tinnitus (Tier 1)<br />
MAY 2010<br />
The Internet Pharmacy—Looking for Drug<br />
Information in All the Right and Wrong Places<br />
JULY 2010<br />
CEUs<br />
Hearing Aid Reality Check .2<br />
Visit www.eAudiology.org for dates and to register.<br />
.1<br />
.1<br />
.3<br />
.2<br />
<br />
Programs should develop guidelines regarding the
Guiding Principles for the Interaction Between Academic Programs in Audiology and Industry<br />
educational activities be only at fair market value and<br />
consistent with models of compensation for the services<br />
or time provided.<br />
teaching material, etc.) when the faculty member,<br />
program, or student is providing a legitimate service for<br />
which the expenses are necessary should be permitted.<br />
• Meals, travel, lodging, and other trip-related expenses<br />
should be at levels that are commensurate with the participation<br />
of the faculty in the programs.<br />
<br />
<br />
Industry has historically been a source of financial support<br />
for students, most commonly in the form of scholarships<br />
or assistantships associated with research endeavors.<br />
University programs and preceptors have a responsibility to<br />
discuss ethical issues with respect to this financial support<br />
to assure that the support is offered without strings<br />
attached and serves a legitimate academic purpose.<br />
<br />
<br />
<br />
• Industry should be free to offer financial or in-kind support<br />
to academic programs for research funding, student<br />
scholarships, or educational funding.<br />
• To ensure transparency, such services should be rendered<br />
in accordance with terms specified in professional<br />
services agreements, which may include compensation<br />
for services that are customary and reasonable in academic<br />
practice.<br />
<br />
Ghostwriting is defined as the provision of written material<br />
that is officially credited to someone other than the<br />
writer(s) of the material. Transparent writing collaboration<br />
with attribution between faculty and persons in industry<br />
is not considered to be ghostwriting, provided each author<br />
legitimately contributes to the endeavor.<br />
<br />
• Academic programs in audiology should not permit their<br />
faculty or students to allow their presentations or publications<br />
to be written by others. Faculty and students<br />
should not receive credit for work to which they did not<br />
substantially contribute.<br />
• All scholarships or other educational funds from<br />
industry should either be given directly to the audiology<br />
program or, if given directly to the student, clearly identified<br />
as a scholarship or assistantship to support their<br />
academic training.<br />
• Universities that allow students to accept any assistantship,<br />
scholarship, or educational fund must assure that<br />
there are no expectations of a quid pro quo. Any funding<br />
that establishes a quid pro quo should be prohibited.<br />
<br />
Expenses associated with CE programs, teaching activities,<br />
or research endeavors may accrue to faculty, students, or<br />
the program in audiology in general. While these may be<br />
covered in a professional services agreement with a specific<br />
company, many times they can occur with no more than a<br />
verbal understanding between industry and the faculty or<br />
academic programs.<br />
<br />
• Reimbursement of expenses associated with travel<br />
or the provision of services (e.g., copying expenses,<br />
• Industry should not permit their employees to receive<br />
credit for work to which they did not substantially<br />
contribute.<br />
<br />
Purchasing decisions made by audiology programs may<br />
present major challenges in efforts to prevent the intrusion<br />
of financial self-interest and inappropriate bias. In the case of<br />
the purchase of devices and equipment, those with experience<br />
and information relevant to purchasing decisions may<br />
have financial or other ties to the manufacturer or provider.<br />
<br />
• At a minimum, audiology programs should ensure that<br />
each participant in the purchasing process discloses all<br />
potential conflicts of interest.<br />
• To the extent an individual’s expertise is necessary in<br />
evaluating any product, that individual’s financial ties to<br />
any manufacturer of that or any related product should<br />
be disclosed to those charged with the responsibility for<br />
making the decision.
Guiding Principles for the Interaction Between Academic Programs in Audiology and Industry<br />
<br />
<br />
There is value in permitting audiology faculty to interact<br />
with industry, including faculty participation on industry<br />
boards of directors and scientific advisory boards as well as<br />
through professional services agreements and consulting<br />
contracts, provided such activities are conducted with full<br />
disclosure and in compliance with the rules and regulations<br />
of the parent institution.<br />
<br />
<br />
• Faculty should provide full disclosure of participation<br />
on boards of directors or advisory boards of industry, or<br />
consulting services for industry.<br />
• Compensation for these activities should reflect the fair<br />
market value of the services provided.<br />
Acknowledgments. This document began with a discussion by the<br />
faculty at the Starkey Student Summer program (2008) in response<br />
to the AAMC’s report, Industry Funding of Medical Education. That<br />
publication served as the starting point for a discussion regarding the<br />
complex yet symbiotic relationship between industry and academic<br />
programs in audiology, and with respect to evolving ethical standards<br />
that impact such relationships. The authors would like to thank the<br />
following individuals who contributed to the thought process and<br />
stimulated the writing of this document: Patricia Dabrowski, AuD;<br />
David Berkey, PhD; Jason Galster, PhD; Brandon Sawalich; Paul<br />
Pessis, AuD; Jerry Northern, PhD; and Jerry Yanz, PhD.<br />
Reference<br />
<br />
<br />
<br />
<br />
Ian M. Windmill, PhD, is chief of the Division of Communicative<br />
Sciences at the University of Mississippi Medical Center. Barry<br />
A. Freeman, PhD, is senior director of education and training<br />
for Starkey Laboratories. James Jerger, PhD, is a distinguished<br />
scholar-in-residence at the University of Texas at Dallas. Jack M.<br />
Scott, PhD, is an assistant professor and clinical supervisor in the<br />
School of Communication Sciences and Disorders at the University<br />
of Western Ontario.<br />
Also of Interest<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Help<br />
PUSH<br />
the<br />
PAC.<br />
Stop by the<br />
Advocacy Booth at<br />
AudiologyNOW! ® 2010<br />
or contribute online.<br />
Visit www.audiology.org,<br />
search key words<br />
“PUSH the PAC.”
Audiologists can learn to externalize<br />
and personify a patient’s hearing loss<br />
without practicing psychotherapy. This<br />
approach causes the practitioner to<br />
focus on the human side of hearing loss<br />
and treat the person, not the disorder.<br />
Emphasizing that hearing loss affects<br />
a person but is not part of that person<br />
helps to reduce the patient’s shame for<br />
being hearing impaired.
Externalizing and Personifying Hearing Loss: A Psychological Tool for Audiologists<br />
Howard” was a 67-year-old man with a progressive<br />
severe-to-profound hearing loss, beginning approximately<br />
10 years prior. He came, in his words, “to get my wife off<br />
my back.” A familiar refrain.<br />
“What’s your wife on your back about” I asked.<br />
“Oh, she wants me to get hearing aids.”<br />
I knew where this was going, and I suspected Howard<br />
did as well. Sure enough, he complained that “Betty”<br />
yells at him to turn down the TV volume, to stop asking<br />
“What” all the time, to stop being so irritable, and to get<br />
therapy.<br />
“It sounds like a battle between you and your wife,” I said.<br />
“I hear fine,” Howard protested. “It’s really her problem.<br />
She often mumbles and speaks to me with her back<br />
turned.”<br />
This wasn’t going to work. And if I suggested too<br />
quickly that Betty was absolutely right—that getting evaluated<br />
for hearing aids would be a good idea—he would<br />
politely, or not so politely, thank me for my time and give<br />
me a version of “Don’t call me, I’ll call you.”<br />
A new approach: I assured Howard that I wouldn’t try<br />
to badger him to get hearing aids, and instead I asked him<br />
if he thinks he’s affected by hearing loss.<br />
“Yeah, sure, I have hearing loss, but who doesn’t have it<br />
at my age”<br />
“Not many people,” I replied. “But it sounds like it has<br />
you, not that you have it.”<br />
“Huh”<br />
“Bear with me, would you Imagine, please, that the<br />
hearing loss is sitting in the empty seat in front of you. It’s<br />
so smart that it can even sit! What does it look like How<br />
big is it What color What’s it wearing Is it friendly or<br />
mean What’s its name”<br />
Howard didn’t expect these rather strange questions,<br />
and I’m sure he became dubious of my mental stability at<br />
this point. Nevertheless, with a fair amount of prodding,<br />
he accommodated my line of questioning. “It’s dark and<br />
heavy, real strong, over six feet tall, has bulging muscles,<br />
and is wearing an Army uniform. And it’s mean, real<br />
mean. His name is ‘Joker.’” Howard let out a smile.<br />
In this manner, I personified Howard’s hearing loss<br />
and externalized it as separate from him.<br />
I then asked him to switch seats and to role-play the<br />
hearing loss. By this time, he was enjoying this “unorthodox<br />
approach,” as he now put it, and was in a more playful,<br />
imaginative mood. He flexed his muscles, scowled, and<br />
made mean, intimidating faces. It would have made the<br />
Joker proud. In turn, I role-played an investigative reporter<br />
whose task was to ask the hearing loss about all the ways<br />
that it had succeeded in disrupting Howard’s life:<br />
• Its influence in the different areas of the Howard’s life<br />
(e.g., its effects on his relationships with others, its<br />
impact on his feelings, its interference in his thoughts,<br />
its effects on Howard’s story about who he is a person,<br />
and so on);<br />
• The strategies, the techniques, the deceits, and the<br />
tricks that the hearing loss has resorted to in its<br />
efforts to get the upper hand in Howard’s life;<br />
• The special qualities possessed by the hearing loss<br />
that it depends on to undermine Howard’s knowledge<br />
and skills, including an inquiry into the powerful<br />
ways that the hearing loss imposes its authority on<br />
his life; and<br />
• The plans that the hearing loss has ready to put into<br />
action should its dominance be threatened.<br />
Initially, Howard responded to my question with the<br />
familiar phrase, “my hearing loss,” and I immediately<br />
countered, “The hearing loss clearly affects you but isn’t<br />
you.” That refrain would become important in our work.<br />
The hearing loss is a condition that influences him but is<br />
separate from him. An important tenet: The person is not<br />
the problem; the problem is the problem.<br />
Howard responded: “You wanna know how the hearing<br />
loss has succeeding in disrupting my life It turns my wife<br />
into a nag, shuts me out from family gatherings, makes<br />
me feel lousy and depressed and angry and makes the<br />
title of the story of my life ‘Howard Is a Loser.’ I don’t know<br />
how the hearing loss gets the upper hand, as you say.<br />
Maybe one of the hearing loss’s strategies or tricks is that<br />
it makes me think that people are mumbling, not talking<br />
loud enough, purposely trying to make my life difficult, or<br />
don’t care about me.<br />
“The hearing loss is very smart and real tricky. I can’t<br />
put my finger on him. Like sometimes I can understand<br />
people, and other times I can’t. It’s random. So sometimes<br />
I don’t think I have a hearing loss, and others doubt me<br />
as well. The hearing loss wants control of me, probably<br />
because it has nothing better to do or wants to feel more<br />
powerful. He screws up my relationships so even my<br />
wife makes me come here to play this stupid game—no<br />
offense, doc.” He gave a half smile.<br />
“No offense taken,” I smiled back.<br />
It was time to switch gears. I then asked him to continue<br />
role-playing the hearing loss, but at this juncture, I<br />
would begin to investigate how the hearing loss had failed<br />
to disrupt Howard’s life:
Externalizing and Personifying Hearing Loss: A Psychological Tool for Audiologists<br />
• The aspects of Howard’s life that Howard still controls,<br />
despite the hearing loss’s influences;<br />
• The countertechniques, counterstrategies, and tricks<br />
that Howard has developed that have at times been<br />
effective in preventing the hearing loss from getting<br />
the upper hand and imposing its authority;<br />
• The special qualities, knowledge, skills, and “self-talk”<br />
that Howard uses that have proven difficult for the<br />
hearing loss to undermine and disqualify;<br />
• Who stands with Howard (relatives, friends, acquaintances,<br />
teachers, therapists, and so on), and the part<br />
they have played in denying the hearing loss’s desires<br />
and wishes; and<br />
• The options that are available to Howard for taking<br />
advantage of the hearing loss’s vulnerabilities and for<br />
reclaiming his own life.<br />
Predictably, Howard had fewer responses than he did<br />
with the previous discussion. After a long silence, he<br />
finally said, “It took away my music, but it hasn’t stopped<br />
me from collecting stamps or taking pictures of my<br />
grandkids so they’ll have a photo album of their lives. My<br />
‘countertechnique’ against the hearing loss, as you put it,<br />
is to do things that I don’t need hearing for.”<br />
“What do you say to the hearing loss while you employ<br />
this strategy”<br />
“You can’t control everything!” he shouted toward the<br />
empty seat with his fist raised and a smirk.<br />
“This doesn’t sound like part of the ‘Howard Is a Loser’<br />
story,” I remarked.<br />
Howard nodded his head somewhat tentatively. I then<br />
asked, “When you succeed in outsmarting the hearing<br />
loss like that, what do you title your story”<br />
“Maybe something like ‘Sometimes, Howard Is a Fighter.’”<br />
One’s story or narrative about oneself is inextricably<br />
related to one’s identity (White, 2007). Howard’s dominant<br />
narrative had been that he is a loser. But now, for the first<br />
time, we excavated another narrative of himself, another<br />
“title” for his identity—sometimes a fighter. It would be<br />
important to embellish this previously dormant narrative<br />
with details, to make it more dominant, to put more “meat”<br />
on it. Any version of “Tell me more” would’ve done, but<br />
typically one’s narrative or identity is related to a previous<br />
relationship that has the capacity to be useful in the present.<br />
I therefore asked Howard, “Who taught you to fight”<br />
After a pause, Howard told me that his long-decreased<br />
grandfather had been a second lieutenant in World War I.<br />
I asked Howard several questions about his grandfather’s<br />
life, about why he joined the armed forces, about his<br />
bravery, what his fears might have been, how he might<br />
have felt going to battle. We spent over half a session<br />
on old war stories. He commented that he often thought<br />
of his grandfather when watching footage of the war in<br />
Iraq. Finally, I wondered aloud whether his grandfather<br />
was psychologically present when Howard was able to<br />
shout to the hearing loss, “You can’t control everything!”<br />
Howard looked at me quizzically but, after some thought,<br />
tentatively nodded his head.<br />
I asked him if he would talk to his grandfather about<br />
how he could help him prepare for battle against the<br />
hearing loss. I motioned to the last remaining empty chair<br />
in my office. Again, after some awkwardness and nervous<br />
laughter, he complied with my request. “Do you have any<br />
advice for me” he asked the empty seat.<br />
At this point, I asked him to switch seats and be his<br />
grandfather while I took over asking the questions. “You<br />
must have some advice for your grandson on how he can<br />
prevent the hearing loss [I motioned to the hearing loss<br />
seat] from getting the upper hand in his life.”<br />
“Howard, you should learn as much as you can about<br />
its weaknesses, its vulnerabilities,” he responded, with<br />
a deep voice, confidence, and conviction. His advice<br />
reminded me of General Westmoreland’s famous statement<br />
that the inability to understand the enemy was “the<br />
basic error” in the conduct of the war in Vietnam.<br />
“What weaknesses of the hearing loss can Howard<br />
exploit” I asked.<br />
He shrugged his shoulders, “I don’t know.”<br />
“Guess.” (My standard response when anyone says, “I<br />
don’t know.”)<br />
“Hmmm, well the hearing loss doesn’t do well with soft<br />
noises. So Howard can maybe get people to speak louder,<br />
he can turn the volume up on the TV, get his wife to stop<br />
calling him from the other room.”<br />
“A good start,” I responded. “Speaking of Howard’s wife,<br />
help me understand something about your grandson. He<br />
came to therapy to get Betty off his back about hearing<br />
aids. In your opinion, would getting hearing aids be an<br />
effective weapon against the hearing loss”<br />
Pause. “Yeah, probably,” he said, somewhat hesitantly.<br />
“So why won’t Howard listen to Betty” I asked.<br />
“Howard’s always been a bit stubborn. He digs in his<br />
heels. He never has wanted to lose a battle—just like me.”<br />
“Chip off the old block. But Howard’s fighting the battle<br />
against the wrong person!”<br />
“What do you mean”
Externalizing and Personifying Hearing Loss: A Psychological Tool for Audiologists<br />
“The enemy is the hearing loss, not Betty! You know<br />
what I bet that one of hearing loss’s tricks is to get<br />
Howard to fire artillery at his own forces!”<br />
“The hearing loss is very cunning,” the lieutenant<br />
agreed, now nodding his head.<br />
“Exactly. The real war is Howard and Betty against the<br />
hearing loss! Do you have any thoughts about some of the<br />
other tricks and deceits that the hearing loss uses against<br />
Howard”<br />
“It makes him feel ashamed, very down on himself, and<br />
it makes him think that hearing aids will make him more<br />
ashamed and even depressed.”<br />
“Astute observation, lieutenant! How do you think<br />
Howard could maneuver around the forces of the hearing<br />
loss to get hearing aids”<br />
“Shock and awe!” he yelled, now enjoying this discussion.<br />
“Regime change! He could blow hearing loss out of<br />
the water!” the Lieutenant proclaimed. I had a foreboding<br />
sense that Donald Rumsfeld had just entered the room.<br />
“I bet he would! What strategy do you think the hearing<br />
loss is using to prevent Howard from blowing it out of the<br />
water with hearing aids”<br />
“Oh, I bet the hearing loss is convincing Howard that<br />
hearing aids will make him look old, that people will pity<br />
him, that they cost too much.“<br />
“The hearing loss is a formidable enemy. Simple sanctions<br />
obviously aren’t going to work. Howard, Betty, and<br />
you need to join forces and launch a full-scale military<br />
campaign with covert and overt special combat operations<br />
against the hearing loss! Maximize your firepower<br />
with air, naval, and land invasions to strategic targets.” I,<br />
too, was enjoying myself at this point. I asked him, “Can<br />
the three of you be ready to present a comprehensive<br />
battle plan in my office tomorrow at 14 hundred hours”<br />
“Yes sir!” he saluted. I saluted him back.<br />
The next day at 14 hundred hours, I entered the waiting<br />
room, not knowing who would be present: Howard, his<br />
grandfather, Rumsfeld, the hearing loss, or Betty. It was<br />
Howard and Betty. We formulated a battle plan:<br />
<br />
How is this clinical vignette relevant to audiologists I’m<br />
not necessarily suggesting that you buy more office chairs<br />
so you can stage imaginary discussions with hearing<br />
losses and patients’ deceased relatives, but it might not<br />
be a bad idea. In another publication (Harvey, 2009), I propose<br />
that the first step to motivating resistant adolescents<br />
is to connect beyond the presenting problem, to share a<br />
fun moment or commonality that doesn’t have to do with<br />
hearing or amplification. This principle isn’t restricted to<br />
that age group but applies to treating any patient who is<br />
“dragged” to our offices.<br />
Howard introduced himself to me by saying that his<br />
wife made him come. My immediate internal reaction<br />
was “Ugh, here we go again. One of a thousand unmotivated<br />
men who start therapy this way,” and I felt mild<br />
irritation and boredom. Undoubtedly, Howard also felt<br />
mild irritation and boredom with me, and due to audiological<br />
factors and/or to his psychological resistance, he<br />
didn’t understand my speech. I privately predicted that<br />
he expected me to ask about his feelings, perhaps to talk<br />
• Receiving an audiological evaluation to learn more<br />
about the hearing loss (“reconnaissance mission”);<br />
• Putting aside monies to purchase hearing aids (“weaponry”)<br />
and batteries (“ammunition”);<br />
• Taking speech reading classes (“combat training”); and<br />
• Negotiating communication rules (“code of conduct”).
Externalizing and Personifying Hearing Loss: A Psychological Tool for Audiologists<br />
about his childhood, and to side with Betty about his<br />
needing to get hearing aids. But if I followed this predicted<br />
script, our reciprocal irritation and boredom with<br />
each other would only have increased, and therapy would<br />
have been doomed from the start.<br />
Therefore, my first task was to introduce an element<br />
of surprise that is beyond the presenting problem, that is<br />
“fun,” and that would also be potentially beneficial. In this<br />
case, I used a psychotherapy technique of externalizing<br />
and personifying a problem (White, 2007): Howard’s hearing<br />
loss. Humor was important and deliberately utilized.<br />
Soon enough, we were both smiling. We achieved what<br />
would be the first building block of our alliance or rapport.<br />
This technique of externalizing and personifying<br />
Howard’s hearing loss can be used by audiologists<br />
Externalizing and personifying a patient’s hearing<br />
loss can effectively illustrate how the person is not<br />
the problem, the hearing loss is the problem.<br />
without exceeding their level of expertise by practicing<br />
psychotherapy. Although not initially apparent, this<br />
approach is consistent with audiologist David Luterman’s<br />
(2008) reminder to look at the human side of hearing<br />
loss and treat the person, not the disorder. Emphasizing<br />
that hearing loss affects a person but is not part of that<br />
person—the person is not the problem; the problem is the<br />
problem—helps to reduce one’s shame for being hearing<br />
impaired. Stated differently, externalizing Howard’s<br />
hearing loss, in addition to introducing levity and humor,<br />
was an effective means of reducing what psychologist<br />
Beatrice Wright (1983) referred to as “spread”. Howard’s<br />
hearing loss had “spread” to nullify his competencies and<br />
therefore cause him to experience shame. In contrast,<br />
when his hearing loss became the hearing loss, he could<br />
begin changing his relationship with it. He could put the<br />
hearing loss in its place and reclaim his own integrity.<br />
I became an “investigative reporter” whose job it was to<br />
learn about how the hearing loss sabotaged Howard’s life<br />
and how Howard could resist its influences. This investigative<br />
stance is critical for audiologists who work with people<br />
who deny the need for amplification. The task was to learn<br />
more about how the hearing loss operated, including its<br />
successes and failures; the task was not to help at this<br />
point. A reporter’s job is to seek information, not to help.<br />
The importance of listening and curiosity—investigative<br />
reporting—is an important principle of Motivational<br />
Interviewing by Miller and Rollnick (2002). Premature<br />
attempts to offer advice are not helpful and often backfire<br />
by increasing a patient’s denial or resistance (Beck and<br />
Harvey, 2009). In that regard, it is important to note that<br />
Howard was at the “Contemplation Stage”: he acknowledged<br />
his hearing loss but was ambivalent, at best, to<br />
address it. It would have been an error to jump on the<br />
change bandwagon by attempting to convince him to get<br />
hearing aids, as I would have been colluding with Betty<br />
against Howard.<br />
Methods of determining the cast of characters in a<br />
patient’s “relevant system” (nuclear family, extended<br />
family, friends, etc.) and then connecting with the “protagonist”<br />
who has the clout to effectively support your<br />
audiologic recommendations have been described elsewhere<br />
(Harvey, 2003a, 2003b, 2009). A standard question<br />
is to ask patients whether other family members have<br />
benefited from amplification, with the goal of increasing<br />
the credibility of your recommendations, “If hearing<br />
aids helped Uncle George, maybe they’ll help me.” Taking<br />
this line of questioning a step further, you can also ask<br />
a patient to imagine what advice an influential family<br />
member, living or deceased, would give, or might have<br />
given, to the patient about amplification, for example,<br />
“What might Uncle George say to you about getting hearing<br />
aids”<br />
When Howard shouted to the hearing loss in the seat,<br />
“You can’t control everything!” his countenance changed;<br />
he raised his fist, seemingly inspired to fight. Something<br />
had shifted! I privately wondered what phantom people<br />
had entered the room. Who else was now psychologically<br />
present with Howard, the hearing loss, and me Could<br />
they help Howard outsmart the hearing loss Stated<br />
more technically, what past or present protagonists in his<br />
family or relevant system could assist him in doing battle<br />
with the now externalized and personified hearing loss<br />
It was when he referred to himself as “sometimes<br />
a fighter” that I considered using a battle metaphor to
Externalizing and Personifying Hearing Loss: A Psychological Tool for Audiologists<br />
inquire about a protagonist. When I asked Howard who<br />
taught him to fight, he introduced me to his grandfather.<br />
With Howard then thinking like his grandfather, I solidified<br />
a collusion of Betty, Howard, and his grandfather<br />
against the hearing loss.<br />
The importance of matching a patient’s metaphors<br />
cannot be overstated. Consistent with the self-world view<br />
narrative of Howard’s grandfather, which was shaped by<br />
the military, battle metaphors were abundant in Howard’s<br />
emerging narrative of his own identity. He emerged as a<br />
fighter like his grandfather. Howard was strongly supportive<br />
of the United States invading Iraq, so it was no<br />
surprise that, while role-playing his grandfather, he<br />
envisioned “shock and awe” tactics against the hearing<br />
loss. My reference to Donald Rumsfeld was reflective of<br />
my own negative bias against that war. Here my task was<br />
to ensure that my sentiments did not interfere with my<br />
alliance with Howard. On the contrary, I spent some time<br />
between our sessions Googling military terms, such as<br />
“reconnaissance mission,” “full-scale military campaign,”<br />
and “special combat operations.”<br />
In summary, this illustration seems relevant for<br />
audiologists in that it offers possibilities of how to playfully<br />
connect with those patients who are “dragged” in<br />
by a significant other. Externalizing and personifying a<br />
patient’s hearing loss, in whatever adaptation fits your<br />
style, can effectively illustrate how the person is not<br />
the problem, the hearing loss (in the empty chair) is the<br />
problem. It can properly demarcate that the participants<br />
in the power struggle do not include you or the spouse<br />
of the person with hearing impairment but that the<br />
struggle is, in fact, between the individual patient and<br />
the hearing loss. As a result, you will increase the likelihood<br />
that previously resistant patients will follow your<br />
recommendations.<br />
<br />
Howard and I met for eight visits, and interestingly<br />
enough, the final meeting was with his wife—previously<br />
the enemy, now his ally. They had been successful in<br />
battle. Howard showed me his hearing aids and, while<br />
playfully rolling his eyes, remarked that the audiologist<br />
had two empty seats in her office reserved for the hearing<br />
loss and his grandfather! (I had given her a heads-up).<br />
As we prepared to say our goodbyes, he hesitated a<br />
bit and asked Betty to open her pocketbook. He took out<br />
several photos of his grandfather and the medals he was<br />
awarded, one by one, taking time to show me all the<br />
details. Perhaps he was trying to teach me about military<br />
honor. I don’t know, but I said to Howard that I wish<br />
Attending<br />
AudiologyNOW ® <br />
Searching for a<br />
Job<br />
Need to Hire an<br />
Audiologist<br />
The HEARCareers<br />
Employment Center at<br />
AudiologyNOW! 2010 provides<br />
employers and job seekers a<br />
place to connect.<br />
Job Seekers:<br />
ß View HEARCareers job postings<br />
ß Find employer contact information<br />
ß Leave your contact information for employers<br />
ß Post resumes on-site<br />
Employers:<br />
ß View attendee resumes<br />
ß Find job seeker contact information<br />
ß Leave your contact information for job<br />
seekers<br />
ß Post jobs on-site<br />
Visit www.audiologynow.org to<br />
learn more about the HEARCareers<br />
Employment Center at AudiologyNOW!
Externalizing and Personifying Hearing Loss: A Psychological Tool for Audiologists<br />
I could have met his grandpa. Betty quickly responded,<br />
“You’ve already met him several times.”<br />
<br />
<br />
<br />
Michael A. Harvey, PhD, ABPP, is a clinical psychologist and a<br />
consultant faculty at Salus University. His most recent books<br />
are The Odyssey of Hearing Loss: Tales of Triumph and<br />
Listen with the Heart: Relationships and Hearing Loss,<br />
both published by Dawnsign Press. Feedback is welcome at<br />
mharvey2000@comcast.net.<br />
References<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Exclusive Savings.<br />
Without the firewall.<br />
See how much you could save on auto, home, renters insurance and more.<br />
AAA members could get an additional discount<br />
on car insurance. Get a free quote today.<br />
1-800-368-2734
Hometown: Pickering,<br />
Ontario, Canada<br />
Education: BS, Biology,<br />
Susquehanna University,<br />
Selinsgrove, PA<br />
Current School: Northeast<br />
Ohio AuD Consortium –<br />
The University of Akron,<br />
Akron, OH<br />
About Me: I’m currently<br />
doing my fourth-year<br />
externship in a hospital<br />
setting and enjoying the<br />
diversity of cases that we<br />
see, so my next step is to<br />
look for a job placement<br />
that offers the same type<br />
of variety.<br />
Quote to Live By: “Learn<br />
from yesterday, live for<br />
today, hope for tomorrow.<br />
The important thing is<br />
not to stop questioning.”<br />
—Albert Einstein<br />
hat I have valued about my program at the Northeast Ohio AuD Consortium<br />
(NOAC) is the faculty encouraged me to go beyond the classroom and participate<br />
in other opportunities, such as conventions, membership in audiology<br />
organizations, and, most importantly, doing service in the community. Expanding my<br />
horizons outside of class has been a priceless experience for my growth as a future<br />
audiologist.<br />
By doing service projects in my neighborhood, I have gained a better perspective<br />
about the impact of audiology in the community. Since my first year in graduate school, I<br />
have participated in the NOAC audiology student group, which gave me the opportunity<br />
to volunteer at local events. These occasions allowed me to teach others about hearing,<br />
but also gave me the chance to witness the exceptional commitment that families have<br />
for their hearing-impaired children. Being outside of clinic also provided a relaxed environment<br />
for parents to express their accomplishments and struggles with hearing loss. It<br />
did not take much effort for us to spend an afternoon with the community, but the effect<br />
it had on the parents and children was encouraging.<br />
I am currently finishing my fourth-year externship in a metropolitan city hospital.<br />
At one of our clinics, we see a large cultural population who lack trust of health-care<br />
professionals and are resistant to the idea of hearing aids. This can be frustrating, as we<br />
often see children fall through the cracks, despite our counseling about the benefits of<br />
immediate intervention.<br />
One day, my supervisor had the audiologists participate in screenings at the local<br />
health fair. We were able to meet neighborhood residents and counsel them on their<br />
hearing concerns. I was impressed that the adults were open to learning about audiology<br />
services and enlightened by our advice. The few minutes counseling them provided<br />
tools to follow up for further assistance. Our interaction was short, but I feel that the<br />
time spent was absolutely worthwhile if we influenced only one person to seek a better<br />
quality of life. Additionally, it made a step toward fostering a trusting relationship with<br />
the community.<br />
It has been personally gratifying to volunteer in the community throughout graduate<br />
school. As a member of society, I believe it is everybody’s responsibility to spend time<br />
contributing to helping the lives of those we can serve.
By Lisa L. Cunningham<br />
earing scientists have long<br />
focused on sensory hair cells<br />
of the inner ear because these<br />
cells are sensitive to death caused<br />
by a variety of stressors—including<br />
noise trauma, exposure to ototoxic<br />
drugs, and even aging. In the mammalian<br />
inner ear, these cells are not<br />
regenerated, so their death results<br />
in permanent hearing loss and/or<br />
balance disorder. Of course, hair cells<br />
aren’t the only cells in the inner ear,<br />
but they seem to be the ones that<br />
receive the most attention. What<br />
about all those other cells Hair cells<br />
in both the auditory and vestibular<br />
systems are surrounded by supporting<br />
cells. What do those cells do<br />
The cochlea contains several<br />
types of supporting cells, including<br />
Deiters’ cells, Hensen cells, Claudius<br />
cells, pillar cells, and phalangeal cells.<br />
They provide basic structural framework<br />
and rigidity to the organ of Corti.<br />
The main structural support is provided<br />
by pillar cells and Deiters’ cells.<br />
Supporting cells are often referred<br />
to as “glia-like” cells, because they<br />
surround, support, and electrically<br />
isolate hair cells in a fashion that<br />
is similar to the way glia surround,<br />
support, and isolate neurons in the<br />
central nervous system. Hair cells<br />
quickly die in zebrafish mutants that<br />
lack supporting cells, indicating that<br />
supporting cells are required for hair<br />
cell survival (Haddon et al, 1999).<br />
Supporting cells are critical for<br />
proper potassium homeostasis in the<br />
cochlea. Endolymph contains high<br />
concentrations of potassium relative<br />
to perilymph. Movement of the<br />
basilar membrane results in deflection<br />
of the stereocilia and opening of<br />
the mechanoelectrical transduction<br />
channel. Potassium from endolymph<br />
then rushes into the hair cell via<br />
these channels, resulting in hair cell<br />
depolarization and neurotransmitter<br />
release. However, all that potassium<br />
has to then be returned to<br />
endolymph. Hair cells release potassium<br />
into perilymph at their basal<br />
surfaces. Supporting cells are then<br />
thought to participate in potassium<br />
recycling by taking up potassium<br />
from perilymph and transporting<br />
it from cell to cell, via a network of<br />
“gap junctions” that connect supporting<br />
cells to one another (Spicer and<br />
Schulte, 1996; Wangemann, 2002).<br />
Potassium is routed via these gap<br />
junctions toward the stria vascularis,<br />
where it is used to generate the endocochlear<br />
potential as it is resecreted<br />
into endolymph.<br />
Cochlear supporting cells are also<br />
important for the survival of primary<br />
auditory neurons (called spiral ganglion<br />
neurons, or SGNs). Molecular<br />
signaling between supporting cells<br />
and SGNs is carried out by a family of<br />
molecules called neuregulins. Loss of<br />
neuregulin signaling results in death<br />
of SGNs, indicating that supporting<br />
cells are required for the survival of<br />
SGNs and thus the maintenance of<br />
cochlear innervation (Stankovic et<br />
al, 2004). Survival of SGNs is critical<br />
to the success of cochlear implants,<br />
which are designed to directly stimulate<br />
SGNs in the absence of hair cells.<br />
Recent evidence suggests that<br />
supporting cells also actively mediate<br />
hair cell death. In the neonatal<br />
rat cochlea, hair cell damage results<br />
in activation of a stress-induced
protein called ERK1/2 in Deiters’ cells<br />
(Lahne and Gale, 2008). ERK1/2 is not<br />
activated in hair cells in response to<br />
this damage. Chemical inhibition of<br />
ERK1/2 signaling in supporting cells<br />
suppressed aminoglycoside-induced<br />
hair cell death (Lahne and Gale, 2008).<br />
These data suggest that supporting<br />
cells can actually promote hair cell<br />
death and possibly even kill hair cells.<br />
Taken together, these data suggest<br />
that supporting cells are much more<br />
than passive structural components<br />
of the cochlea. Instead they are active<br />
participants in sensory transduction,<br />
and they can directly influence<br />
the survival of both spiral ganglion<br />
neurons and hair cells. Scientists are<br />
currently investigating the cell-to-cell<br />
communication that occurs between<br />
supporting cells and other cochlear<br />
cell types. Understanding these<br />
signals may open doors to new therapeutic<br />
strategies aimed at protecting<br />
hair cells and/or SGNs by targeting<br />
supporting cells.<br />
Lisa L. Cunningham, PhD, is an assistant<br />
professor with the Department of<br />
Pathology and Laboratory Medicine at<br />
the Medical University of South Carolina.<br />
References<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
You can have confidence<br />
in the OAE capabilities and<br />
reliability of your Echoport<br />
Now with<br />
INDUSTRY LEADING<br />
PROTECTION<br />
3 year<br />
Echoport Warranty<br />
Call for Details!<br />
The #1 choice for clinical OAE testing,<br />
the ILO292 DP Echoport provides all the<br />
OAE tests you need: full screen analysis<br />
for TEOAE, DPOAE, contralateral<br />
suppression, Spontaneous OAEs,<br />
DP Growth and binaural capability.<br />
It also helps to know that you can safely<br />
rely on the most trouble-free system in the<br />
industry.<br />
No breakdowns ... No worries!<br />
Otodynamics<br />
www.otodynamics.com 1 800 659 7776<br />
Booth 1130
“<br />
I lost my aid,<br />
am I covered<br />
”<br />
With ESCO Reminder Care there is no question.<br />
Insurance coverage for everyone.<br />
www.earserv.com / 800-992-3726
By Annette A. Burton<br />
he Coding and Reimbursement<br />
Committee has received<br />
numerous questions regarding<br />
participation in the Medicare program.<br />
We would like to take this opportunity<br />
to review the enrollment options for<br />
the Medicare program as they pertain<br />
to the profession of audiology.<br />
<br />
<br />
Current regulatory language in the<br />
Social Security Act demonstrates the<br />
intent for Medicare beneficiaries to<br />
have widespread access to diagnostic<br />
and therapeutic services within the<br />
United States. Although the Centers<br />
for Medicare and Medicaid (CMS) cannot<br />
currently require most providers<br />
to accept assignment for services,<br />
CMS does require that claims for<br />
covered services are submitted on<br />
behalf of Medicare beneficiaries,<br />
if requested. Claims for covered<br />
services for Medicare beneficiaries<br />
are to be submitted by all providers,<br />
except in cases where the provider<br />
has opted out of the Medicare program<br />
and has entered into a private<br />
contract with the beneficiary.<br />
<br />
<br />
Each provider type has a set of<br />
defined options of participation for<br />
Medicare:<br />
<br />
Also of Interest<br />
Mandated to participate and<br />
accept assignment.<br />
Enroll as either a participating or<br />
nonparticipating provider.<br />
Opt out of the Medicare program<br />
for a renewable, two-year period<br />
and enter into a private contractual<br />
arrangement with the<br />
beneficiary to not submit claims<br />
or receive reimbursement from<br />
Medicare.<br />
Audiologists currently fall within<br />
the second category, if treating<br />
Medicare beneficiaries; they must<br />
enroll in Medicare and submit claims<br />
for covered services. Audiologists<br />
have the option to enroll as either<br />
a participating provider who must<br />
accept assignment of Medicare<br />
benefits for all covered services or<br />
as a nonparticipating provider who<br />
<br />
<br />
<br />
may choose to accept assignment of<br />
Medicare claims on a case-by-case<br />
basis. Audiologists are currently not<br />
allowed to opt out of the Medicare<br />
program and enter into private contractual<br />
arrangements with Medicare<br />
beneficiaries.<br />
There are advantages and disadvantages<br />
to becoming either a<br />
participating or a nonparticipating<br />
provider. To learn more about the<br />
differences between participating<br />
and nonparticipating status, there<br />
are many resources available. The<br />
Medicare Physician Guide: A Resource<br />
for Residents, Practicing Physicians and<br />
Other Health Care Professionals is a free<br />
and very helpful reference guide that<br />
is produced by the Medicare Learning<br />
Network. It may be downloaded at<br />
www.cms.hhs.gov/MLNProducts/<br />
downloads/physicianguide.pdf, or a<br />
free copy on CD can be obtained from<br />
CMS by visiting http://cms.meridianksi.com/kc/pfs/pfs_lnkfrm_fl.aspl<br />
gnfrm=reqprod&function=pfs.<br />
<br />
It is important to remember that the<br />
mandatory claim submission requirement<br />
refers only to covered services<br />
as defined by Medicare. Many<br />
services may not meet Medicare’s<br />
definition of a covered service.<br />
Routine procedures, services that are<br />
directly related to the provision of<br />
amplification, therapeutic services<br />
that are within an audiologist’s scope
of practice but fall outside of the<br />
narrowly defined diagnostic benefit<br />
category determined by Medicare, are<br />
all considered noncovered services<br />
under the Medicare benefit.<br />
Please remember that Medicare<br />
does not prohibit an audiologist from<br />
providing noncovered services to a<br />
Medicare beneficiary. Medicare does<br />
not restrict or prohibit billing the<br />
beneficiary for noncovered services;<br />
however, the beneficiary must be<br />
notified in advance that the service<br />
is noncovered.<br />
<br />
There is no submission requirement<br />
for services that are free. It is important<br />
to note that provision of free<br />
services cannot be only offered to<br />
certain types of patients. For example,<br />
it would not be permissible to avoid<br />
the mandatory reporting requirements<br />
just for Medicare beneficiaries<br />
and submit claims for the same diagnostic<br />
services to other third-party<br />
payers. It is good practice to have<br />
consistent billing practices for all<br />
patients, regardless of the payer.<br />
Annette A. Burton, AuD, is the chair<br />
of the Coding and Reimbursement<br />
Committee, and is the director of the<br />
Easter Seals Centers for Better Hearing<br />
in Connecticut.<br />
Disclaimer. The purpose of the information<br />
provided in this column by the<br />
American Academy of Audiology Coding<br />
and Reimbursement Committee is to<br />
provide general information and educational<br />
guidance to audiologists. Action<br />
taken with respect to the information<br />
provided is an individual choice. The<br />
American Academy of Audiology hereby<br />
disclaims any responsibility for the<br />
consequences of any action(s) taken by<br />
any individual(s) as a result of using the<br />
information provided, and reader agrees<br />
not to take action against, or seek to hold,<br />
or hold liable, the American Academy<br />
of Audiology for the reader’s use of the<br />
information provided. As used herein,<br />
the “American Academy of Audiology”<br />
shall be defined to include its directors,<br />
officers, employees, volunteers, members,<br />
and agents.<br />
The Hugh Knowles Center<br />
for Clinical and Basic Science in Hearing and Its Disorders<br />
at Northwestern University welcomes its two newest fellows<br />
Andrew FishmanPamela Souza<br />
Feinberg School of Medicine School of Communication<br />
The center fosters interdisciplinary research, scholarship, training, and clinical services<br />
to help people recover and protect the joy of hearing. Fellows are distinguished Northwestern<br />
faculty who contribute their research, clinical, and educational efforts in this mission.<br />
Current fellows<br />
James Bartles<br />
Ann Bradlow<br />
Mary Ann Cheatham<br />
Peter Dallos<br />
Sumitrajit Dhar<br />
Jaime Garcia-Añoveros<br />
Dean Garstecki<br />
Nina Kraus<br />
Alan Micco<br />
Ernest Moore<br />
Claus-Peter Richter<br />
Mario Ruggero<br />
Jonathan Siegel<br />
Catherine Warrier<br />
Donna Whitlon<br />
Richard Wiet<br />
Patrick Wong<br />
Beverly Wright<br />
Inquiries from potential<br />
doctoral students,<br />
postdoctoral fellows,<br />
and research scientists about the<br />
center’s activities are welcome.<br />
knowlescenter@northwestern.edu<br />
www.communication.northwestern<br />
.edu/departments/csd/<br />
research/hugh_knowles_center
he Tax Relief and Health Care<br />
Act of 2006 established the<br />
Physician Quality Reporting<br />
Initiative (PQRI), which included<br />
incentivized payments for eligible<br />
providers for quality measures<br />
furnished to Medicare beneficiaries.<br />
Since December 2007, 10 audiology<br />
organizations have worked collaboratively<br />
as the Audiology Quality<br />
Consortium in developing reportable<br />
measures under PQRI.<br />
As of January 1, 2010, this voluntary<br />
program allows Medicare Part<br />
B-enrolled audiologists to participate<br />
in the reporting of up to four<br />
measures. Providers who meet the<br />
threshold for the accurate reporting<br />
of these measures may be eligible for<br />
a two percent incentive payment.<br />
Medicare patients of any age<br />
referred to a physician after an<br />
audiologic assessment determined by<br />
one of the qualified conditions, and<br />
who are not currently under the care<br />
of a physician for that condition, are<br />
measures eligible to be reported on.<br />
However, Medicare beneficiaries are<br />
required to have a physician referral<br />
for a medically necessary reason.<br />
<br />
Congenital or traumatic<br />
deformity of the ear<br />
have disease of the ear and mastoid<br />
processes)<br />
A history of sudden<br />
or rapidly progressive hearing loss<br />
Otitis Media with<br />
Effusion (OME): Diagnostic<br />
Evaluation-Assessment of<br />
Tympanic Membrane Mobility, is<br />
also reportable, but will have a<br />
very limited use as it will be applicable<br />
for those pediatric patients<br />
who are Medicare beneficiaries, an<br />
uncommon occurrence; the two<br />
percent bonus will not apply.<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
You should report on these measures<br />
to help maintain audiology’s<br />
commitment to high quality care for<br />
Medicare beneficiaries while simultaneously<br />
supporting the recognition<br />
of the profession as a member of the<br />
health-care coordination process.<br />
Care coordination is intended to<br />
increase communication among<br />
those professionals providing services<br />
to Medicare patients to ensure<br />
a standard of care and to avoid<br />
duplication. In addition, there is an<br />
opportunity to capture additional<br />
A history of active<br />
drainage from the ear within the<br />
previous 90 days (for patients who
evenue with the two percent reporting<br />
bonus on qualifying measures.<br />
<br />
<br />
<br />
Successful reporting requires the following<br />
components:<br />
You will need to report on at<br />
least three measures during the<br />
reporting period. For each of the<br />
measures, you are required to<br />
report on 80 percent of patients<br />
who have conditions that are<br />
applicable to those measures.<br />
Each measure has a numerator<br />
and a denominator specific to<br />
that measure. The numerator is<br />
the action the measure requires<br />
for reporting and the denominator<br />
specifies the eligible patients<br />
for each measure. There are also<br />
denominator exclusions: patients<br />
who are not eligible for the measure<br />
for specific reasons.<br />
For each measure, except for measure<br />
#94, audiologists are required<br />
to refer the patient to a physician<br />
after the audiologic evaluation<br />
reveals a condition unless the<br />
condition meets the criteria for an<br />
exclusion.<br />
You will need a National Provider<br />
Identifier (NPI) number and a<br />
Medicare Provider Transaction<br />
Account Number (PTAN), formerly<br />
known as the Provider Identifier<br />
Number (PIN).<br />
<br />
<br />
To obtain an NPI, go to https://nppes.<br />
cms.hhs.gov/NPPES/StaticForward.<br />
doforward=static.instructions.<br />
To obtain a PTAN, go to https://<br />
pecos.cms.hhs.gov/pecos/login.do.<br />
If you prefer, you may file a hard<br />
copy of the 855I (www.cms.hhs.gov/<br />
CMSforms/downloads/CMS855I.pdf)<br />
to obtain your PTAN. If you are an<br />
employee of, or contract with a physician,<br />
you will need to file the 855R, to<br />
reassign benefits to the employer or<br />
contracted entity: www.cms.hhs.gov/<br />
cmsforms/downloads/cms855r.pdf.<br />
Note: If you are enrolled in Medicare<br />
but have not submitted a CMS-855I since<br />
2003, you are required to submit a complete<br />
application. Providers and suppliers<br />
should follow the instructions for completing<br />
an initial enrollment application.<br />
<br />
<br />
You will find the numerators,<br />
denominators, and exclusions<br />
for each measure in detail at<br />
www.asha.org/uploadedFiles/<br />
ReportingMeasuresStepByStep.pdf.<br />
<br />
<br />
As a Part B-enrolled Medicare provider,<br />
you will file your claim on a CMS<br />
1500 form as is currently done for<br />
Medicare and other third-party payer<br />
claims. There are specific CPT, ICD-9,<br />
and G-codes or Healthcare Common<br />
Procedure Coding System (HCPCS)<br />
codes that correspond with each<br />
of the measures and can be found<br />
here: www.asha.org/uploadedFiles/<br />
ReportingMeasuresStepByStep.pdf.<br />
The CPT codes describe the procedures<br />
performed; the ICD-9 codes are<br />
the diagnostic codes and the G/HCPCS<br />
codes are Category II CPT codes; or<br />
HCPCS codes. Audiology procedures<br />
are Category I codes. It is required that<br />
the G/HCPCS codes be reported on<br />
the same claim as that of the patient’s<br />
procedures and diagnosis codes.<br />
The CPT codes are placed in box<br />
24D, the ICD-9 codes are inserted in<br />
box 21, and the G/HCPCS codes go in<br />
box 24D on the CMS 1500 form.<br />
<br />
<br />
<br />
Let’s use measure Measure #190<br />
(history of sudden or rapidly progressive<br />
hearing loss) as our example.<br />
First choose one of the following CPT<br />
codes for this particular measure and<br />
mark it in box 24D:<br />
• 92557<br />
• 92567<br />
• 92568<br />
• 92575<br />
*At the time of publication, CPT codes<br />
92550 and 92570 were not finalized for<br />
inclusion. A request to the Centers for<br />
Medicare and Medicaid Services to include<br />
them has been made by the Audiology<br />
Quality Consortium.<br />
Then you will need to choose one<br />
of the following ICD-9 codes for this<br />
particular measure for box 21:<br />
• 389.00-389.06 inclusive<br />
• 389.08<br />
• 389.10-389.18 inclusive
• 389.20-389.22 inclusive<br />
• 389.8<br />
• 389.9<br />
Finally, locate the denominator<br />
(G/HCPCS code), which will describe<br />
the eligible patients for this measure.<br />
For measure #190, it is “Patients aged<br />
birth and older with verification and<br />
documentation of sudden or rapidly<br />
progressive hearing loss,” and mark<br />
that code in box 24D.<br />
December 31, 2010. The payment will<br />
be calculated based on the qualified<br />
claims submitted at the end of the<br />
reporting period and will result in<br />
a payment to you, typically within<br />
the first six months post–reporting<br />
year. Remember that you must report<br />
correctly on at least 80 percent of<br />
applicable patients to receive the<br />
incentive payment.<br />
<br />
PQRI claims reporting process questions<br />
may be addressed to Debbie<br />
Abel, AuD, the Academy’s director of<br />
reimbursement, at dabel@audiology.<br />
org. Questions regarding other PQRI<br />
processes should be addressed to<br />
Victoria Keetay, PhD, the Academy’s<br />
senior director of education, at<br />
vkeetay@audiology.org.<br />
<br />
<br />
<br />
Audiologists have an option of<br />
reporting for the calendar year<br />
2010—January 1 to December 31,<br />
2010, or for the last six months of<br />
the calendar year, from July 1 to<br />
Also of Interest<br />
<br />
<br />
THE BENEFITS OF<br />
ACADEMY MEMBERSHIP<br />
AKA VIP STATUS<br />
CONFERENCE<br />
CALLING<br />
Discounted<br />
member prices<br />
available for<br />
unlimited and<br />
reservationless<br />
conference calling.<br />
FELLOW LOGO<br />
Promote your<br />
commitment to<br />
hearing health<br />
care through your<br />
affiliation with<br />
the Academy.<br />
Download the<br />
logo for FREE.<br />
AUTO<br />
INSURANCE<br />
Discounted<br />
member prices<br />
may apply to you<br />
for outstanding<br />
rates and<br />
24/7/365 service.<br />
MEMBERSHIP HAS ITS BENEFITS<br />
Learn more about all of the benefits available to Academy<br />
members at www.audiology.org. Search key word BENEFITS.
By Tracey Irene<br />
e often evaluate the<br />
impression that we are<br />
making on our patients<br />
in terms of our professionalism, services,<br />
and skill. A first impression can<br />
set the stage for the entire visit. It is<br />
important to consider the experience<br />
you provide patients before they are<br />
even called back for their appointment.<br />
Is your waiting room warm and<br />
inviting Are your patients greeted<br />
when they walk in the door Is there<br />
appropriate information available on<br />
your practice, services, and staff<br />
One way to evaluate this experience<br />
is to spend some time sitting<br />
in your waiting room. What do you<br />
hear, see, and feel Is there sufficient<br />
seating available How long<br />
has it been since the carpet was<br />
cleaned Is the literature in your<br />
waiting room current, clean and<br />
organized Can you overhear the<br />
conversations your receptionist is<br />
having on the phone Is the temperature<br />
comfortable and lighting<br />
ample Are the acoustics friendly to<br />
individuals with hearing loss<br />
Remember, patients will form<br />
an impression of your office within<br />
minutes of their arrival. You have<br />
one opportunity to make a first<br />
impression, so make sure it is a good<br />
one. Here are some things to consider<br />
when evaluating your waiting room<br />
and patient experience:<br />
Is your receptionist greeting<br />
your patients when they arrive in<br />
your office Is the wait time for your<br />
patients reasonable Are they made<br />
to feel welcome and comfortable Is<br />
the check-in process clear, and have<br />
the patients been informed of what<br />
is needed for the appointment Is<br />
confidentiality maintained during<br />
the check-in process<br />
Is the seating in your office comfortable<br />
and functional Consider<br />
seats with armrests so patients can<br />
lift themselves from the chairs with<br />
ease. Also, consider some seating<br />
without armrests for those patients<br />
who may require additional space.<br />
Are the lighting and acoustics<br />
appropriate for individuals with<br />
hearing loss and vision loss You<br />
may want to keep in mind that television<br />
or music may deteriorate the<br />
acoustics of the office; however, this
could be used as an opportunity for<br />
your patients to try assistive listening<br />
devices. You will need to weigh<br />
these considerations and decide what<br />
will work best in your office.<br />
Is your waiting room clean and tidy<br />
Do you have any mysterious stains on<br />
furniture or carpet Do you have hand<br />
sanitizer, tissues, and trash cans available<br />
to your patients Are your surfaces<br />
covered in dust or fingerprints<br />
Is the reading material current<br />
Educational materials should be current<br />
and patient friendly. Magazines<br />
should also be current, clean, and<br />
organized. Consider magazines that<br />
appeal to men, women, and children.<br />
Try to reduce the amount of clutter<br />
on the surfaces of counters and tables.<br />
Is there a restroom available to<br />
your patients near the waiting room<br />
If not, consider a sign detailing the<br />
restroom location.<br />
If you find yourself overwhelmed<br />
by this process, understand that you<br />
are not alone. Start by making small<br />
changes and monitor the impact it<br />
makes on your patients. Consider<br />
surveying your patients to determine<br />
what areas you could improve<br />
upon. If you are in need of a complete<br />
redesign, an interior designer can<br />
be helpful in determining the layout,<br />
color scheme, size, lighting, and<br />
furnishings of your office. Use this<br />
opportunity as a way to improve your<br />
patient’s experience and satisfaction<br />
in your practice. Satisfied patients<br />
can be invaluable to your practice,<br />
as they may generate a number of<br />
referrals through word-of-mouth<br />
marketing.<br />
Tracey Irene, AuD, is a senior audiologist<br />
with Professional Hearing Services,<br />
A Division of Moreland Ear, Nose, and<br />
Throat Group, LTD, in Milwaukee, WI.<br />
She is also a member of the Academy’s<br />
BEST Committee.<br />
<br />
<br />
<br />
<br />
<br />
<br />
auction4audiology<br />
Preview Auction Items<br />
Online Today<br />
Bidding Is Open April 5–17<br />
If interested in donating an item to the auction,<br />
contact Auction HQ: tconte@audiology.org.<br />
Proceeds from Auction 4 Audiology<br />
support research, education, and<br />
public awareness in the hearing<br />
sciences through the American<br />
Academy of Audiology Foundation.<br />
Visit w w w.biddingforgood.com/auction4audiology<br />
to v iew a nd bid on auction items.
By Maureen Valente<br />
he doctor of audiology (AuD)<br />
degree is a rigorous, four-year<br />
clinical degree whereby rich<br />
practicum experiences are interwoven<br />
with challenging course work and<br />
exposure to research and the corresponding<br />
literature. Students develop<br />
skills, knowledge, and competencies<br />
throughout the intensive program to<br />
ultimately serve as highly competent,<br />
autonomous, compassionate clinicians<br />
upon graduation. The Academy’s<br />
Education Committee is delighted to<br />
have formulated a new Subcommittee<br />
on Research in Audiology Education,<br />
so that research in professional education<br />
may be enhanced and so that<br />
the profession may move forward<br />
based on the evidence. Initiatives will<br />
collaboratively dovetail with other<br />
research- and education-oriented<br />
outcomes of the recent Gold Standards<br />
Summit (GSS) and similar conferences.<br />
Much discussion has taken place,<br />
casually and within more formal<br />
venues, regarding the possibility of<br />
a greater degree of standardization<br />
with regard to clinical education.<br />
These discussions appear to primarily<br />
center around the fourth-year externship.<br />
Until we have an opportunity<br />
to view and make transformations<br />
based on research outcomes, it may<br />
be beneficial to continue brainstorming<br />
and discussing via venues such as<br />
this Audiology Today column and many<br />
others. As the Education Committee<br />
has held conference calls to help<br />
provide leadership in carrying out the<br />
many, massive initiatives suggested<br />
after meetings such as the GSS, one<br />
recurring reminder discussed is “that<br />
we have to roll up our sleeves, dig in,<br />
and begin somewhere.”<br />
In this spirit and with the above<br />
foundation, this co-chair wishes to<br />
put forth these thoughts based on<br />
personal experience within her own<br />
AuD program in managing clinical<br />
practicum experiences of all four<br />
years and in placing an average of<br />
12 fourth-year externs per year at<br />
various sites across the country. In<br />
addition, thoughts stem from a more<br />
global, national perspective following<br />
much discussion with teams of<br />
professionals across the country<br />
(students, preceptors, and faculty),<br />
after much committee discussion on<br />
a national level, and following recent<br />
Council on Academic Accreditation<br />
in Audiology and Speech-Language<br />
Pathology and Accreditation<br />
Commission for Audiology Education<br />
accreditation processes. Thoughts<br />
expressed are only that, intended to<br />
suggest guidelines without becoming<br />
too narrowly focused, with further<br />
discussion highly encouraged.<br />
<br />
<br />
Types and number of experiences<br />
may vary from program to program,<br />
although some best practice guidelines<br />
may include:<br />
Begin with clinical practicum<br />
experiences as soon as possible<br />
upon enrollment.<br />
Develop close integration of clinical<br />
practicum experiences with<br />
course work.
Provide specified development and<br />
assessment of skills, knowledge,<br />
and competencies as a function of<br />
each academic year of study,<br />
Include diagnostic and (re)habilitative<br />
services across the life span<br />
and audiology’s scope of practice.<br />
The program should not rely upon<br />
the fourth-year externship for the<br />
majority of its clinical education.<br />
Create and enable ongoing<br />
teamwork among the student,<br />
preceptor, site, and university.<br />
This includes extensive teamwork<br />
during the placement process and<br />
also during the academic term.<br />
Criteria for site selection should<br />
be predetermined by the educational<br />
program and may include<br />
such factors as environment<br />
conducive to learning, learning<br />
opportunities available, state-ofthe-art<br />
equipment and techniques,<br />
population diversity, utilization<br />
of best practice, and geographic<br />
proximity.<br />
Specify criteria for selection and<br />
include such factors as experience<br />
in the profession, area(s) of<br />
expertise, communication and<br />
interpersonal skills, precepting<br />
and mentoring skills, and<br />
accessibility.<br />
Assessment of the student should<br />
take place via daily feedback, formative<br />
assessment, and summative<br />
assessment. The student should play<br />
a key role in assessment, performing<br />
self-assessment of his/her own<br />
progress and assessment of the<br />
preceptor(s). An affiliation agreement<br />
should always be in place<br />
between the site and the university;<br />
all parties, including the student,<br />
should be aware of and have access<br />
to its contents.<br />
<br />
The fourth-year externship has<br />
replaced the clinical fellowship year<br />
(CFY) model, with the fundamental<br />
difference being that the student is<br />
still a student during the externship<br />
year. By this time, the student has<br />
successfully completed earlier practicum<br />
rotations, most if not all course<br />
work, and (very likely) any capstone<br />
project that may be required.<br />
<br />
The spirit of the externship is for<br />
the student to immerse himself<br />
or herself in a full-time clinical<br />
experience. A depth and breadth of<br />
experiences is optimal, although this<br />
depth and breadth should also have<br />
been achieved via earlier rotations,<br />
whenever possible. If this is the case,<br />
discussion and advising may take<br />
place if the student wishes to specialize.<br />
The educational program should<br />
not rely upon the fourth-year externship<br />
placement for the majority of its<br />
clinical education.<br />
<br />
Continued teamwork is essential<br />
among all parties, including the<br />
student, site, preceptor, and university.<br />
Sites are strongly encouraged<br />
to make use of the Academy’s<br />
Externship Registry and universities/<br />
students are encouraged to seek valuable<br />
site information through this<br />
and other resources. The university<br />
should guarantee student placement<br />
(and extensive support in securing<br />
placement), and students should not<br />
be left to secure their own externship<br />
sites. University personnel should<br />
make first contacts and should provide<br />
ongoing mentoring throughout,<br />
including resume writing, interviewing<br />
skills, and other important<br />
aspects. Protocols and timelines may<br />
vary from university to university,<br />
with some encouraging a year-long<br />
rotation at one facility and others<br />
encouraging rotation at several facilities<br />
throughout the year.<br />
<br />
Much variability continues to exist<br />
with regard to timelines implemented<br />
by sites and by university<br />
programs. Areas where variability<br />
exists include submission/acceptance<br />
of applications, review of applications,<br />
interviewing, and making/accepting<br />
of offers. The Academy has developed<br />
a recommended timeline for externship<br />
placement (see Figure 1). It would<br />
be optimal if such a timeline could<br />
be followed closely for standardization<br />
purposes; if this is not possible,<br />
feedback for possible revision and<br />
updating should be forwarded to the<br />
Academy. Criteria for site selection<br />
and preceptor qualifications should<br />
follow the same guidelines as outlined<br />
above. There is a great need for<br />
ongoing preceptor training, according<br />
to feedback received after the GSS<br />
and other conferences, especially in<br />
the area of supervision. This should<br />
continue to be addressed by the profession<br />
as an ongoing initiative.<br />
<br />
Several years ago, an Academy task<br />
force was formulated to explore<br />
issues related to payment for the<br />
fourth year. A white paper was written,<br />
resulting in many controversial<br />
comments and little consensus.<br />
Although there is great variability at<br />
the current time regarding payment,<br />
it was decided at that time that this<br />
issue should be one between university<br />
and site. General suggestions put<br />
forth by this author at the current<br />
time included:<br />
That any payment should be made<br />
with the clear stipulation that<br />
the student is clearly known as a<br />
student and not an employee.
That a site be selected based on<br />
its merit, depth, and breadth of<br />
experience. A site should not be<br />
selected based solely on financial<br />
merit, nor should an excellent site<br />
be disregarded solely because of<br />
an inability to pay.<br />
That the student not be placed in<br />
uncomfortable or risky situations<br />
regarding third-party reimbursement<br />
or other professional issues.<br />
<br />
Teamwork should continue and the<br />
university should be in touch with<br />
the student and preceptor on a very<br />
regular basis. This author implements<br />
such contact on at least a monthly<br />
basis. The university representative<br />
should visit the site whenever<br />
feasible, and contact should be<br />
more frequent if difficulties arise.<br />
Assessment of the student should<br />
occur as outlined above and within<br />
the framework of fourth-year student<br />
competencies, skills, and knowledge.<br />
It has often been suggested by<br />
preceptors that a uniform assessment<br />
tool should be developed for use<br />
among programs, and this possibility<br />
is currently being explored by the<br />
Clinical Education Subcommittee.<br />
Level of direct supervision should<br />
diminish throughout the fourth year,<br />
as the student approaches graduation<br />
and is well on his or her way toward<br />
becoming a competent and independent<br />
clinician.<br />
<br />
This very dynamic process will,<br />
undoubtedly, further evolve as we<br />
collectively discuss and gather the<br />
evidence related to “what is currently<br />
working” and “what areas are in need<br />
of constructive change.”<br />
Maureen Valente, PhD, is the director<br />
of Audiology Studies, Program in<br />
Audiology and Communication Sciences, at<br />
Washington University School of Medicine.<br />
She is also the cochair of the Academy<br />
Education Committee.<br />
LIVE FROM AUDIOLOGYNOW! ® IN SAN DIEGO!<br />
2010 MARION DOWNS<br />
LECTURE IN PEDIATRIC<br />
AUDIOLOGY<br />
OPTIMIZING EARLY WORD LEARNING<br />
IN INFANTS WITH HEARING LOSS<br />
FRIDAY, APRIL 16, 10:00 AM PT<br />
PRESENTED BY MARY PAT MOELLER, PHD,<br />
Center for Childhood Deafness at Boys Town<br />
National Research Hospital<br />
FREE Web seminar available through eAudiology.<br />
Visit www.eAudiology.org to register.<br />
Funded by the AAA Foundation with a<br />
grant from the Oticon Foundation.
By Doris Gordon<br />
responsibility of an<br />
accrediting agency, such as<br />
key<br />
ACAE, is monitoring changes,<br />
reforms, and general trends in higher<br />
education today. We need to be ahead<br />
of the curve in transforming audiology<br />
education. Why Because we’re<br />
evaluators who not only confirm that<br />
academic programs are in compliance<br />
with educational standards but<br />
enable them to adapt to changes that<br />
bring about genuine improvements<br />
in student learning.<br />
Former U.S. Secretary of<br />
Education Margaret Spellings established<br />
the Commission for the Future<br />
of Higher Education in 2004–2005<br />
to review what was happening in<br />
universities and colleges at all levels.<br />
Valid questions about the accountability,<br />
access, and cost/affordability<br />
of education were asked by the commission.<br />
The present U.S. Secretary<br />
of Education, Arne Duncan, is passionate<br />
about preparing students for<br />
higher education, mandating that<br />
secondary educational institutions<br />
throughout the country focus on<br />
excellence in teaching and achieve<br />
higher scores on standardized tests.<br />
Molly Corbett Broad, the recent<br />
CEO of the prestigious American<br />
Council on Education urges us “to<br />
think big…this is a time when the<br />
game is changing…hunkering down<br />
is not a smart option.”<br />
So what is changing Our worldview,<br />
for one. As Thomas Friedman<br />
explains in his book, The World is Flat,<br />
U.S. businesses, corporate structures,<br />
and educational institutions need to<br />
cooperate with nations around the<br />
globe. During this past year, the rise<br />
in international students attending<br />
universities for postsecondary<br />
and graduate education within the<br />
United States has been impressive.<br />
The Chinese are leading the way.<br />
They have funds for tuition and<br />
board and bring ideas and different<br />
perspectives to graduate programs.<br />
The international influence benefits<br />
education for all.<br />
Learning is changing. Robert<br />
Zemsky, in his recent book, Making<br />
Reform Work, reinforces the notion<br />
that learning is the “academy’s core<br />
business and the traditional method<br />
of learning with detailed content is<br />
changing to a more well-executed<br />
learning process.” Static learning<br />
is decreasing and dynamic learning<br />
is more evident, in the sense<br />
that learning processes change as<br />
the learner gains new knowledge<br />
and tackles new problems. Zemsky<br />
notes that “the academy today<br />
argues that the successful student is<br />
much more a clever librarian—that<br />
is, someone who knows how to ask<br />
the right questions and to recognize<br />
good answers.”<br />
Technology is revolutionizing education.<br />
In an interesting article, “How<br />
the iPhone Can Reboot Education,”<br />
(www.wired.com/gadgetlab/2009/12/<br />
iphone-university-abilene/) a small<br />
university in Abilene, Texas, recently<br />
completed a pilot program for the<br />
purchase of iPhones for its students.<br />
“The traditional classroom, where<br />
an instructor assigns a textbook, is<br />
heading toward obsolescence. Why<br />
listen to a single source talk about a<br />
printed textbook that will inevitably<br />
be outdated in a few years That<br />
setting seems stale and hopelessly<br />
limited when pitted against the internet,<br />
which opens a portal to a live<br />
stream of information provided by<br />
billions of minds.”<br />
What do these changes tell us<br />
about audiology education Will we<br />
have the vision to place audiology<br />
on the cutting-edge of science and<br />
education As a member of a rigorous<br />
academic discipline, audiology has<br />
no choice but to embrace these ideas<br />
and include them in the learning<br />
environment.<br />
Doris Gordon, MS, MPH, is the executive<br />
director of ACAE.
By James W. Hall III<br />
BOARD OF GOVERNORS<br />
James “Jay” W. Hall III, PhD, Chair<br />
John A. Coverstone, AuD<br />
Antony Joseph, AuD, PhD<br />
Beth Longnecker, AuD<br />
Yvonne S. Sininger, PhD<br />
Therese Walden, AuD<br />
Gail M. Whitelaw, PhD<br />
American Academy<br />
of Audiology Board of<br />
Directors Liaison<br />
Karen Jacobs, AuD<br />
Past Chair<br />
Ex Officio Member<br />
James A. Beauchamp, AuD<br />
ore than 20 years have passed since the now legendary “Future of<br />
Audiology” session at the 1987 ASHA Convention in New Orleans.<br />
During the session, James Jerger, PhD, spontaneously proffered an<br />
idea that brought the standing-room-only crowd to their feet—audiologists<br />
should form their own professional organization. This pivotal event in the<br />
development of the profession of audiology was summarized in a retrospective<br />
article published in the May/June 2008 issue of Audiology Today titled “The<br />
Future of Audiology…20 Years Later.”<br />
At the 1989 session, I took the opportunity to focus on two topics that were,<br />
in my opinion, central to the future of audiology—education and certification.<br />
On the topic of education of audiologists, I outlined a plan for a four-year<br />
doctoral program incorporating a supervised clinical experience, which was<br />
both extensive and intensive. The idea was not original. Even then, a number<br />
of audiologists were enthusiastically developing plans for a doctor of<br />
audiology-type degree. And, citing a recommendation of Raymond Carhart<br />
made back in the 1960s, I suggested that audiology develop two levels of<br />
<br />
<br />
<br />
Public Representative<br />
Patty A. Keffer, MBA<br />
Managing Director<br />
Ex Officio Member<br />
Sara Blair Lake, JD, CAE<br />
For ABA information, contact:<br />
American Board of Audiology<br />
11730 Plaza America Drive<br />
Suite 300<br />
Reston, VA 20190<br />
800-881-5410<br />
aba@audiology.org<br />
Hails From: Twin Cities of Minnesota<br />
(currently), Portland, OR (originally)<br />
Year Certified: 2006<br />
Degree: AuD, PCO School of Audiology<br />
What I Do for the ABA: Members of<br />
the board set policy and direction for<br />
the ABA, approve new applicants for<br />
certification, and oversee specialty certification<br />
programs. I am the new chair<br />
of the ABA Marketing Committee and a<br />
member of the ABA Ethics Committee.<br />
In My Free Time: I enjoy spending<br />
time with my family and try to play<br />
with my two children every day. I<br />
also enjoy softball, golf, and skiing. I<br />
usually have a few home improvement<br />
projects half-finished at any<br />
time, and several Web site projects<br />
pending. I also try to work in some<br />
time on the guitar or piano so I don’t<br />
completely forget how to play!<br />
Quote to Live By: “Live a balanced<br />
life—learn some, and think some,<br />
and draw, and paint, and sing, and<br />
dance, and play, and work every day<br />
some.” —Robert Fulghum
certification—general certification and specialty certification.<br />
We now have both. As I begin my term as chair of<br />
the ABA Board of Governors, it seems like a good time to<br />
once again prognosticate about the future of audiology.<br />
The future of audiology is all around us and easy to see.<br />
We can see the future of audiology in the clinic, sitting<br />
in early morning patient conferences, and in the classroom.<br />
At the Academy’s convention, AudiologyNOW! ® , we<br />
glimpse the future of the profession hundreds of times.<br />
The future is on duty early in the morning at the registration<br />
desks outside lecture rooms, presenting research<br />
posters, and especially at the ABA-sponsored Meet &<br />
Greet event. Doctor of audiology students are the future<br />
of audiology. Audiology tomorrow is embodied in our<br />
students today. Embracing our future, the ABA will significantly<br />
expand student-related activities and initiatives<br />
throughout 2010.<br />
The ABA’s popular Meet & Greet function, generously<br />
supported by Thieme Publishing, grows larger each<br />
year. Audiology students are matched with audiologists,<br />
including some of the “big names” in our profession. In<br />
an informal setting over lunch, mentors and mentees<br />
have the opportunity to converse and get to know each<br />
other. Speaking from experience, the ABA Meet & Greet<br />
is one of the most enjoyable and stimulating events of<br />
AudiologyNOW! Recognizing that some students will be<br />
unable to travel to San Diego in April, the ABA will offer<br />
a “virtual” option for the Meet & Greet event. Audiology<br />
student mentees will be connected with audiologist mentors<br />
to become electronically acquainted and to exchange<br />
ideas. I encourage ABA-certified audiologists to “adopt<br />
a student” for some virtual meeting and greeting. Go to<br />
the ABA Web site (www.americanboardofaudiology.org)<br />
to sign up for participation in the Meet & Greet event, or<br />
e-mail the ABA at aba@audiology.org.<br />
Another student-related initiative for 2010 is the<br />
promotion and expansion of the provisional ABA certification.<br />
Students approaching the last year of their<br />
doctor of audiology program are encouraged to apply for<br />
provisional certification, to set themselves apart as they<br />
seek fourth-year externships and their first postgraduate<br />
employment as an audiologist. I strongly encourage all<br />
audiology students to pursue the provisional certification<br />
option by downloading an application from the ABA Web<br />
site. Speaking of the ABA Web site, it’s about to undergo<br />
a major makeover. The improved ABA Web site will have<br />
a fresh, user-friendly appearance. One of the exciting<br />
new features of the Web site is a page devoted to student<br />
activities and opportunities. If you’re a student, I invite<br />
you to help us develop the student page on the ABA Web<br />
site. We value your ideas and your creativity. Please contact<br />
us now via e-mail at aba@audiology.org.<br />
I’m looking forward to another very good year for<br />
the ABA. Please join the Board of Governors, the ABA<br />
staff, and me in contributing to the essential work of the<br />
American Board of Audiology.<br />
James W. Hall III, PhD, is the chair of the American Board of<br />
Audiology.<br />
<br />
<br />
Register Your<br />
Clinical Site<br />
A free tool for universities, students, and clinical sites<br />
To register your site today, visit<br />
www.audiology.org, search<br />
key words “Externship Registry.”
By Melissa Sinden<br />
he Government Relations<br />
Committee, in conjunction<br />
with the Academy’s advocacy<br />
team, is excited to announce a variety<br />
of new, interactive, informational<br />
events at AudiologyNOW! 2010 in San<br />
Diego. These sessions are designed to<br />
educate Academy members on how to<br />
become active advocates, and provide<br />
valuable tips on engaging elected officials<br />
and shaping public policy.<br />
After the great success of the<br />
inaugural Advocacy Summit last year<br />
in Dallas, the Academy will host a<br />
larger meeting to allow more Academy<br />
members and interested advocates<br />
to attend. While the summit last year<br />
was limited to only a handful of states<br />
to kick off the Key Contacts initiative,<br />
this year, invitations have been<br />
extended to all Academy members<br />
interested in becoming the “go-to”<br />
person in their state or congressional<br />
district. These Key Contacts represent<br />
the voice of audiology on issues affecting<br />
the profession in their districts. For<br />
more information on the Key Contacts<br />
initiative, visit www.audiology.org,<br />
key words “key contacts.”<br />
This year’s AudiologyNOW! will also<br />
feature a learning module titled “Your<br />
Role in the Legislative Process.” Erin<br />
Miller, AuD, chair of the Academy’s<br />
Government Relations Committee;<br />
John Williams, the Academy’s federal<br />
lobbyist; and Melissa Sinden, senior<br />
director of government relations for<br />
the Academy, will host this interactive<br />
presentation. Participants will learn<br />
the “ins and outs” of the legislative<br />
processes at the state and federal levels,<br />
and what to expect when meeting<br />
with elected representatives. Those in<br />
attendance will learn how to become a<br />
lobbyist for the profession and how to<br />
become involved to ensure the voice of<br />
audiology is heard.<br />
Be sure to stop by the new and<br />
improved advocacy booth in Academy<br />
Central for all the latest advocacy<br />
and PAC (Political Action Committee)<br />
information. There, you can learn<br />
more about the Academy’s legislative<br />
issues, view exciting merchandise,<br />
and find out how to PUSH the PAC!<br />
Contributions to the PAC may be<br />
made through the Academy Web site,<br />
by mail, or directly at the Advocacy<br />
Booth by cash, check, or credit<br />
card. Remember that donors in the<br />
President’s Circle ($500+/year) receive<br />
an invitation to an “Insider’s Briefing”<br />
and VIP admission to the PAC event at<br />
AudiologyNOW! This year’s PAC event<br />
will offer contributors the opportunity<br />
to sample California wines at the San<br />
Diego Wine and Culinary Center!<br />
For more information about the<br />
PAC, visit www.audiology.org/<br />
advocacy/pac/Pages/default.aspx.<br />
We look forward to seeing you at<br />
one of our many advocacy events in<br />
San Diego!<br />
Melissa Sinden is senior director of<br />
government relations for the American<br />
Academy of Audiology.
Join us <br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Dr. Chermak’s name is synonymous<br />
to many audiologists with research<br />
in the diagnosis and management of<br />
central auditory processing disorder<br />
(APD). She began her pioneering work<br />
in the 1980s, and her contributions<br />
to the field’s knowledge base have<br />
been seminal. It is virtually impossible<br />
to delve into APD literature<br />
without repeatedly encountering<br />
her influence in the form of refereed<br />
articles, edited monographs, book<br />
chapters, and books. What makes<br />
her academic record more remarkable<br />
is that it was generated while<br />
she was simultaneously distinguishing<br />
herself as a teacher, university<br />
administrator, and international<br />
advocate for the field of audiology. As<br />
a Fulbright Scholar in 1989, she studied<br />
international models of health<br />
care and shared that knowledge<br />
through international presentations,<br />
workshops, and articles. Her<br />
excellence in administration and<br />
teaching has been recognized over<br />
and over again through awards such<br />
as the Distinguished Faculty Award,<br />
the Edward R. Meyer Distinguished<br />
Professor Award, and the Faculty<br />
Excellence Award. Dr. Chermak<br />
has been chair of the Department<br />
of Speech and Hearing Sciences at<br />
Washington State University since<br />
1990. She has made notable and<br />
lasting contributions to our profession,<br />
her students, and research in<br />
audiology.<br />
<br />
Dr. Compton-Conley has had a<br />
distinguished career as an educator<br />
and consumer advocate. She is<br />
best known for expanding awareness<br />
of assistive technology for<br />
hearing-impaired persons. An<br />
acclaimed expert in this specialty<br />
area, her counsel and advice are<br />
sought worldwide. Dr. Compton-<br />
Conley is currently a professor of<br />
audiology and the director of the<br />
Assistive Devices Center at Gallaudet<br />
University. She participates on<br />
numerous audiology review boards,<br />
task forces, and committees. During<br />
her career, she has advised over<br />
20 governmental agencies, worked<br />
with rehabilitative institutions in<br />
the public and private sector, and<br />
consulted for the telecommunications,<br />
automotive, transportation,<br />
entertainment, retail, construction,<br />
and hearing aid industries. The core<br />
of Dr. Compton-Conley’s clinical and<br />
research work has concentrated on<br />
improving signal-to-noise ratio for<br />
hearing-impaired listeners. Her classic<br />
video and workbook Doorways to<br />
Independence earned her international<br />
recognition. In describing her contributions,<br />
Dr. James Jerger remarked<br />
that she “has forgotten more about<br />
assistive technology than the rest<br />
of us will ever know.” Dr. Compton-<br />
Conley demonstrates a tireless<br />
commitment to hearing-impaired<br />
consumers. She has motivated and<br />
inspired students for decades and is<br />
highly esteemed by colleagues for<br />
contributions in the lab, the classroom,<br />
and the community.
Dr. Hawkins is one of those rare<br />
individuals who can function just<br />
as easily in the research laboratory,<br />
classroom, or clinic. He has<br />
not only functioned in each of these<br />
capacities, but also excelled. The<br />
early portions of his career were in<br />
academia, with a greater emphasis<br />
on teaching and research, but never<br />
to the exclusion of his interests in<br />
clinical audiology. In fact, a hallmark<br />
of the first 15 to 20 years of Dr.<br />
Hawkins’ career is the application of<br />
good science and research skills to<br />
clinical issues confronting audiology,<br />
especially in the area of amplification.<br />
During the past 15 years of Dr.<br />
Hawkins’ career, while serving as the<br />
head of the audiology section and the<br />
director of the Hearing Aid Clinic at<br />
Mayo Clinic in Jacksonville, Florida,<br />
greater emphasis has been placed on<br />
clinical audiology, but never to the<br />
exclusion of research and teaching.<br />
Hallmarks of this more recent<br />
period include many presentations<br />
and publications on professional<br />
ethics, group approaches to aural<br />
rehabilitation, amplification, and<br />
diagnostic audiology. Of course,<br />
countless patients with whom he<br />
has worked have also benefited<br />
greatly from his services as a master<br />
clinician. Perhaps the only thing surpassing<br />
his many accomplishments<br />
in research, teaching, and clinical<br />
service is his great humility about<br />
these accomplishments.<br />
<br />
Dr. Kujawa is one of the field’s most<br />
active and accomplished audiologists.<br />
She is director of audiology<br />
at Massachusetts Eye and Ear<br />
Infirmary, associate professor of<br />
otology and laryngology at Harvard<br />
Medical School, and adjunct faculty<br />
at Harvard-MIT Health Sciences and<br />
Technology. Dr. Kujawa has made<br />
major contributions to the fields<br />
of audiology and hearing science.<br />
Highlights of her service to the field<br />
include two terms on the executive<br />
board of the Academy, as well as the<br />
board of directors of the American<br />
Auditory Society, editorial board<br />
and section editor for Ear & Hearing,<br />
member of the Working Group<br />
on Translational Research for the<br />
NIDCD, and chair of the Academy<br />
Research Committee. Dr. Kujawa’s<br />
research record is stellar. Her current<br />
work on the interactive effects of<br />
noise exposure and aging on auditory<br />
function has added important information<br />
to our understanding of the<br />
causes and progression of hearing<br />
loss. She also studies the genetics,<br />
intracochlear drug delivery systems,<br />
and the efferent system. She has<br />
published more than 40 scholarly<br />
papers in the field’s most prestigious<br />
journals. Finally, Dr. Kujawa is a<br />
consummate teacher of audiology,<br />
medical, and basic science students.<br />
<br />
<br />
<br />
<br />
<br />
<br />
Dr. Saunders is a leader in the<br />
development of new technologies for<br />
cochlear implants and hearing aids.<br />
Her academic qualifications include<br />
a BS (Hon) in chemical physics and<br />
MSc in clinical audiology from the<br />
University of Manchester. After<br />
completing her PhD at the University<br />
of Southampton, she worked in<br />
England as a clinical audiologist<br />
and lecturer in audiology until she<br />
moved to Australia in 1984, where<br />
she continued her career as a clinical<br />
and research audiologist. In 1996, she<br />
became a project leader for commercialization<br />
of new hearing-related<br />
technologies at the Co-operative<br />
Research Center for Cochlear<br />
Implant and Hearing Aid Innovation<br />
in Melbourne. As an example, Dr.<br />
Saunders was part of the team that<br />
developed and patented a shaped<br />
implantable cochlear implant electrode,<br />
subsequently commercialized<br />
as the Nucleus ® Contour Electrode TM .
She has participated in the publication<br />
of several scientific articles<br />
regarding this device. Her most<br />
recent business responsibility was<br />
CEO and director of Dynamic Hearing<br />
Pty (Australia), which develops sound<br />
processing and DSP technology for<br />
hearing aids and headsets. She has<br />
recently left this position and is now<br />
on the faculty of Monash University<br />
in Melbourne, Australia.<br />
<br />
<br />
<br />
<br />
<br />
<br />
Dr. Davis has a list of accomplishments<br />
so long that there is not<br />
enough room to present them here.<br />
He initiated, developed, and still<br />
manages the National Hearing<br />
Service Newborn Hearing Screening<br />
Program for England, a model that<br />
set the benchmark for programs<br />
all over the world. He and his colleagues<br />
completed a national study<br />
of hearing, which investigated the<br />
prevalence of deafness and lifestyle<br />
influences impacting the hearing<br />
impaired in England. He initiated,<br />
developed, and still manages the<br />
NHS Hearing Aid Program for<br />
England, which provides appropriate<br />
and properly fitted hearing aids for<br />
citizens of England, Scotland, and<br />
Wales. Dr. Davis is known worldwide<br />
as a scientist and researcher, with<br />
over 200 referreed publications. He<br />
serves on the managing council of<br />
the International Journal of Audiology.<br />
He is a frequent attendee and speaker<br />
at AudiologyNOW!, and the ICA, and<br />
in Asia, Europe, and South America.<br />
He is so well respected and appreciated<br />
in his own country that Queen<br />
Elizabeth II awarded him the Order of<br />
the British Empire.<br />
<br />
<br />
<br />
<br />
<br />
<br />
Dr. Northrup is a bilingual audiologist<br />
and faculty associate at Callier<br />
Center for Communicative Disorders,<br />
at the University of Texas, Dallas.<br />
Her humanitarianism is expressed<br />
daily in her work as an advocate for<br />
children who have hearing loss but<br />
cannot afford amplification. She has<br />
fought for countless underserved<br />
children with hearing impairment in<br />
the Dallas area, and has led numerous<br />
trips to her native Panama to<br />
fit hearing aids on children. She<br />
organized a team of experts from<br />
North America to implant and program<br />
cochlear implants for children<br />
in Panama. As the president of the<br />
Pan-American Society of Audiology,<br />
she has connected colleagues from<br />
Central and South America with<br />
leaders in audiology from North<br />
America and Europe. She has visited<br />
many universities and professional<br />
organizations in different countries<br />
to aid in their development and<br />
production of exchange materials.<br />
Her approach is to “teach the teachers.”<br />
Dr. Northrup started The Global<br />
Village, a project designed to translate<br />
audiological terms from English<br />
to Spanish and Portuguese. She<br />
has devoted her life to underserved<br />
children with hearing impairment<br />
and the international development<br />
of audiology.
Dr. Fausti’s remarkable and prolific<br />
career in audiology began with<br />
research on human high-frequency<br />
sensitivity and its assessment. He<br />
has explored normal and abnormal<br />
function, as well as the effects of<br />
various physical and chemical toxins.<br />
This led to the development of new<br />
strategies, protocols, and equipment<br />
for early identification of ototoxicity,<br />
which has been a major focus in his<br />
career. More recently, his research<br />
has focused on tinnitus, which is<br />
of course a major issue with the<br />
veteran population that he serves. A<br />
central theme in his research is rehabilitation,<br />
and perhaps his proudest<br />
achievement is the establishment of<br />
the National Center for Rehabilitative<br />
Auditory Research (NCRAR) in 1997,<br />
located at the VA Medical Center in<br />
Portland Oregon, where he currently<br />
serves as director. Through<br />
this Center of Excellence, Dr. Fausti<br />
and his colleagues have continued<br />
to produce vital research in the field<br />
of auditory rehabilitation. He also<br />
serves as associate chief of staff for<br />
the Portland VA Medical Center, professor<br />
at Oregon Health and Science<br />
University, and adjunct professor at<br />
Portland State University and the<br />
University of Oregon.
Dr. Fausti’s remarkable and prolific<br />
career in audiology began with<br />
research on human high-frequency<br />
sensitivity and its assessment. He<br />
has explored normal and abnormal<br />
function, as well as the effects of<br />
various physical and chemical toxins.<br />
This led to the development of new<br />
strategies, protocols, and equipment<br />
for early identification of ototoxicity,<br />
which has been a major focus in his<br />
career. More recently, his research<br />
has focused on tinnitus, which is<br />
of course a major issue with the<br />
veteran population that he serves. A<br />
central theme in his research is rehabilitation,<br />
and perhaps his proudest<br />
achievement is the establishment of<br />
the National Center for Rehabilitative<br />
Auditory Research (NCRAR) in 1997,<br />
located at the VA Medical Center in<br />
Portland Oregon, where he currently<br />
serves as director. Through<br />
this Center of Excellence, Dr. Fausti<br />
and his colleagues have continued<br />
to produce vital research in the field<br />
of auditory rehabilitation. He also<br />
serves as associate chief of staff for<br />
the Portland VA Medical Center, professor<br />
at Oregon Health and Science<br />
University, and adjunct professor at<br />
Portland State University and the<br />
University of Oregon.
The Clinical Practice Guidelines for the Diagnosis, Treatment, and<br />
Management of Children and Adults with Central Auditory Processing<br />
Disorder are open for widespread peer review until March 12,<br />
2010. Send your comments to Task Force Chair Frank Musiek,<br />
PhD. To review the document, visit www.audiology.org,<br />
Publications and Resources, Document Library, CAPD.<br />
<br />
<br />
The Academy wishes to thank the Ototoxicity Monitoring<br />
Task Force (under the Strategic Documents Committee)<br />
for their dedication and support with the development of<br />
this position statement and practice guidelines.<br />
Task Force Members: John D. Durrant, PhD, University<br />
of Pittsburgh (chair); Kathleen Campbell, PhD, Southern<br />
Illinois University; Stephen Fausti, PhD, Portland VA Medical<br />
Center; O’Neil Guthrie, Duke University; Gary Jacobson, PhD,<br />
Vanderbilt University; Brenda L. Lonsbury-Martin, PhD, VA<br />
Loma Linda Healthcare System and Loma Linda University<br />
Medical Center; Gayla Poling, PhD, Ohio State University<br />
<br />
The first half of FY2010 marked many accomplishments and<br />
initiatives from our committees. Review a snapshot of the<br />
list below and read more in the Academy’s Annual Report at<br />
www.audiology.org (search key words “Annual Report”).<br />
<br />
•<br />
•<br />
•<br />
•<br />
Planned and finalized the invited sessions.<br />
Reviewed submissions for Learning Modules, Exhibitor<br />
Courses, Student Hands-On Labs, Industry Updates,<br />
Research Pods, and Research and Clinical Posters.<br />
Developed special events and on-site activities.<br />
Planned educational activities for San Diego outreach.<br />
<br />
<br />
•<br />
Worked on updating several member resources to<br />
include The BEST Way: Reaching Physicians, Frontline<br />
Office Training Kit, Audiogram of Familiar Sounds, and<br />
Hearing Aid Checklist.<br />
• Developed and contributed to a column in Audiology<br />
Today on practice management.<br />
<br />
• Participated in CMS meeting regarding the new<br />
bundled and current single vestibular codes with representatives<br />
from ASHA and AAO-HNS.<br />
• Submitted responses to the proposed and final<br />
Medicare Physician Fee Schedule rules.<br />
• Fielded questions from members and provided updates<br />
to FAQs for Web site.<br />
• As members of the Audiology Quality Consortium,<br />
continue to provide education for members for the<br />
Physician Quality Reporting Initiative.<br />
• Researched Medicare Opt Out issue, resulting in report to<br />
Executive Committee, Board and member education article.<br />
• Participated in meetings with other audiology associations<br />
and in anti-trust training.<br />
<br />
• Continued ongoing discussion on next steps related<br />
to the Gold Standards Summit outcomes.<br />
• Created Research in Audiology Education<br />
Subcommittee to focus on the development of evidenced-based<br />
instruction in AuD education.<br />
• Created education column in Audiology Today.<br />
• Recommended the development of a JAAA supplement<br />
on evidence-based instruction.<br />
• Clinical Education Subcommittee promoted and<br />
further developed the Externship Registry.<br />
<br />
• Revised the Guidelines for Financial Relationships with<br />
Manufacturers of Hearing Devices in preparation for peer<br />
review.<br />
• Initiated revision of the Ethics in Audiology (Green) book.<br />
• Responded to a multitude of inquiries from members.<br />
<br />
• Continued to push for direct access, gaining 53 cosponsors<br />
during the 65 days Congress was in session since<br />
its introduction.<br />
• Created a public policy resolution on pediatric audiology.<br />
• Developed Key Contacts training materials and<br />
resources.<br />
• Hosted a Virtual Advocacy Day to promote direct access.<br />
<br />
• Received and reviewed a total of 13 nominations;<br />
selected eight honorees for 2010.
• Submitted nomination packages for the International<br />
Award in Hearing.<br />
• Supported the recommendation that Dr. John Durrant<br />
from the University of Pittsburgh represent the<br />
Academy and ASHA at the Affiliated Societies meeting<br />
of the International Society of Audiologists.<br />
• Supported the travel expenses of Academy representative<br />
to the Pan-American Society of Audiologists<br />
Conference.<br />
<br />
• The Welcoming Subcommittee welcomed 141 new<br />
members to the Academy.<br />
• The Member Assistance Program Subcommittee reviewed<br />
and approved 11 applications for AudiologyNOW! 2010.<br />
• Announced that at year end 2009 the Academy had<br />
reached 11,012 members—the highest in Academy history!<br />
<br />
• Developed and launched a new fundraising campaign<br />
titled “PUSH the PAC.”<br />
• Planned a new fundraising event for AudiologyNOW!,<br />
redesigned existing contributor circles, identified new<br />
ways to thank contributors, and redesigned the PAC<br />
portion of the Academy's Web site.<br />
• Engaged students and provided more opportunities<br />
for students to become involved with fundraising<br />
initiatives.<br />
<br />
• Attended RUC meeting and CPT Editorial Panel meeting<br />
in October 2009.<br />
• Participated in a CPT Panel Workgroup on<br />
Intraoperative Monitoring.<br />
<br />
• Identified, developed, and scheduled eAudiology Web<br />
seminars six to eight months in advance.<br />
<br />
• Participated in activities of the Audiology Quality<br />
Consortium supporting PQRI.<br />
• Drafted Standards of Practice document (to be finalized<br />
April 2010).<br />
<br />
•<br />
•<br />
Rolled out new member tools for National Audiology<br />
Awareness Month and National Protect Your Hearing<br />
Month.<br />
The Recruitment Subcommittee launch on www.<br />
audiology.org, with tips and tools for audiologists to<br />
use when recruiting into the field in their local area.<br />
<br />
•<br />
•<br />
Reviewed www.howsyourhearing.org Web site for<br />
design, layout, and content.<br />
Reviewed content of “Hearing Aids” and “Newborn<br />
Hearing Screening” brochures.<br />
<br />
•<br />
•<br />
•<br />
Selected recipients of the Research Grants in Hearing<br />
and Balance.<br />
The ARC 2010 Program Committee continued to plan<br />
the Academy Research Conference (ARC) on aging and<br />
hearing health.<br />
The ARC 2010 Program Chair and the staff liaison<br />
successfully submitted an NIH conference grant<br />
application.<br />
<br />
•<br />
•<br />
•<br />
•<br />
Worked with the SAA board to recruit SAA chapters (38<br />
chapters as of 12/31/09 ; 42 as of 2/9/10).<br />
Restructured the advising process to merge the positions<br />
of SAA Advisory Committee Chair with SAA<br />
National Advisor.<br />
Participated in the SAA’s strategic planning.<br />
Worked with the SAA to develop a relationship with<br />
the Special Olympics Healthy Hearing Program.<br />
<br />
• Prepared for the 10th Annual State Leaders Workshop.<br />
• Promoted the Active Advocate of the Year Award.<br />
• Conducted a review of state licensure laws for the<br />
AMA SOP Task Force.<br />
<br />
• Five subcommittees made up of 19 task forces continue<br />
to develop practice guidelines, position statements,<br />
and reports.<br />
• Published Ototoxicity Monitoring Practice Guidelines<br />
and Position Statement in October 2009.
tymotic Research joined forces with the<br />
Academy and the American Academy<br />
of Audiology Foundation (AAAF) to<br />
advocate for listening safety at the Midwest<br />
Clinic, an international band and orchestra<br />
conference which has been held in Chicago<br />
every December for the past 64 years. The<br />
conference attracts over 15,000 members of<br />
the instrumental music education community<br />
and is a great venue to promote the Turn<br />
It to the Left message about noise-induced<br />
hearing loss (NIHL).<br />
Etymotic exhibits at the clinic every year,<br />
and uses the conference as an opportunity<br />
to speak to music educators and students<br />
about the dangers of loud listening. Last fall,<br />
Gail Gudmundsen, AuD, director of sales and<br />
marketing at Etymotic, realized that youth<br />
who attend the Midwest Clinic are the perfect<br />
audience for Turn It to the Left, the soft-rap CD<br />
with the message: “Protect your ears when<br />
you’re near loud sounds, Get your hearing<br />
tested and memorize this song…turn it to the<br />
left, turn it to the left!”<br />
“Awareness about the risks of musicinduced<br />
hearing loss has grown exponentially<br />
in the past few years, due to efforts of many<br />
people in the audiology and hearing conservation<br />
communities,” Gudmundsen said. “Since<br />
the clinic exists exclusively<br />
for educational purposes,<br />
we were able to reach<br />
music teachers,<br />
directors, and students all in one setting. The<br />
Turn It to the Left CD was another great way to<br />
promote the message.”<br />
In its efforts to increase public awareness<br />
about NIHL, Etymotic made a generous gift to<br />
the AAAF’s fund in support of noise-induced<br />
hearing loss research. This contribution<br />
ensured that copies of the CD were available<br />
to students at the clinic at no charge. The<br />
CDs not distributed at the Midwest Clinic<br />
were given to audiologists and attendees of<br />
the Illinois Academy of Audiology annual<br />
meeting in Chicago, held January 20–22,<br />
2010. Etymotic staff also provided Midwest<br />
Clinic attendees with information on the<br />
importance of audiological care, careers in<br />
audiology, and other facts about healthy<br />
hearing. For more information on the AAAF’s<br />
NIHL research funding, contact Kathleen<br />
Devlin Culver, director of development, at<br />
800-226-2336, x1049 or<br />
kculver@audiology.org.<br />
Many thanks to our friends and colleagues<br />
at Etymotic for helping the Academy and<br />
AAAF increase awareness about how important<br />
it is to Turn It to the Left!
Wednesday, April 14, 2010, 5:30 – 10:00pm at<br />
AudiologyNOW! 2010 in San Diego.<br />
Graciously hosted by Sadanand and Angie<br />
Singh of Plural Publishing at their La Jolla home.<br />
Sample fine wines from the Singh’s cellar and<br />
enjoy the Pacific views at this elegant benefit<br />
dinner party.<br />
Limited number of tickets still available; call<br />
703-226-1049 for more information.<br />
Complimentary transportation from the<br />
Hilton San Diego Bayfront underwritten by<br />
HearUSA Hearing Care Network.<br />
Proceeds to support audiology research<br />
and education.<br />
<br />
<br />
The AAAF challenges university AuD programs<br />
to donate an item showcasing their<br />
state or school spirit to our annual Auction<br />
4 Audiology at AudiologyNOW! ® 2010. The<br />
program whose item generates the most<br />
bids will win a gift certificate for a celebration.<br />
Have a night of food, fun, and a break<br />
from the books. Interested in making a<br />
STATEment Contact Tara Conte at tconte@<br />
audiology.org.<br />
<br />
• <br />
• <br />
<br />
<br />
• <br />
<br />
• <br />
<br />
• <br />
<br />
<br />
• <br />
<br />
<br />
<br />
• <br />
<br />
• <br />
<br />
• <br />
<br />
• <br />
<br />
• <br />
<br />
•
HOW CAN THE ACADEMY<br />
HELP YOU<br />
Come to the 2010 business meeting and help us put the pieces together.<br />
The 2010 Academy Business meeting<br />
provides all members the opportunity to voice<br />
their ideas on improving the Academy to staff<br />
and leaders in round table discussions. It is<br />
the responsibility of all members to help shape<br />
the future of the Academy. The Academy is an<br />
association of, by, and for audiologists, and we<br />
need your help.<br />
Mark your calendars for Saturday, April 17,<br />
2010, at 1:00pm during AudiologyNOW! ® in<br />
San Diego. Visit www.audiologynow.org for<br />
more information.<br />
Attendees will be entered to win one<br />
complimentary registration to AudiologyNOW!<br />
2011 (April 6–9, Chicago, IL).<br />
Members can view the FY09 audited financials<br />
and committee accomplishments on line.<br />
Visit www.audiology.org search key word<br />
“Annual Report”.
CHESTER COUNTY<br />
OTOLARYNGOLOGY<br />
& ALLERGY ASSOCIATES<br />
Full-time and/or part-time Audiologist<br />
needed for private practice in beautiful<br />
Chester County, PA. Our practice<br />
encompasses pediatric and adult care and<br />
includes a growing hearing aid patient base.<br />
Areas of Focus Include:<br />
- Standard Audiologic Testing<br />
- Vestibular Testing with VNG<br />
- Hearing Aid Dispensing<br />
Interested candidates please forward<br />
resume to ccofps@comcast.net or<br />
fax to 610-345-0986.<br />
Ohio<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
WORK AND PLAY IN NEW ZEALAND<br />
INTERNATIONAL OPPORTUNITIES FOR AUDIOLOGISTS<br />
Have you got the spirit of<br />
adventure<br />
Bay Audiology is New Zealand’s<br />
largest private practice, with over<br />
60 clinics nationwide. This is a<br />
well established company. Our<br />
Audiologists provide hearing tests,<br />
screenings, industrial monitoring,<br />
hearing aid fitting, access to<br />
rehabilitation programmes and<br />
hearing aid accessories.<br />
Opportunities<br />
Opportunities for experienced<br />
Audiologists with hearing aid<br />
dispensing experience in<br />
private practice.<br />
Lifestyle<br />
New Zealand’s reputation for<br />
breathtaking scenery is unrivalled,<br />
with expansive coastlines,<br />
geothermal backdrops and alpine<br />
peaks. You will have an adventure<br />
playground on your doorstop, and<br />
be welcomed by an existing network<br />
of US Audiologists who have<br />
relocated. New Zealand, a country<br />
that is both family-friendly and<br />
peaceful. Go to www.purenz.com for<br />
a taste of what our beautiful country<br />
has to offer.<br />
When you join Bay Audiology<br />
When you join, we’ll provide you<br />
with:<br />
• A strong commitment to<br />
clinical development and<br />
patient excellence<br />
• A structured induction and<br />
training program<br />
• Succession planning with in<br />
house training and development<br />
programmes to enhance your<br />
audiology and personal skills<br />
• Further Education funding<br />
• Variety<br />
• Tailored benefits package<br />
• Relocation assistance<br />
Contact us now, and confidentially discuss your<br />
future in Audiology. Join Bay Audiology and<br />
Experience Life at Full Volume!<br />
Contact: Alison Redfern-Daly<br />
Senior HR Advisor<br />
Mobile: 00 64 21 384707<br />
Phone: 00 9 308 3723<br />
Email: a.redfern-daly@bayaudiology.co.nz<br />
Web: www.bayaudiology.co.nz
Classified and Employment Line Listing<br />
Rates for Audiology Today<br />
<br />
<br />
<br />
Classified and Employment Display<br />
Advertising for Audiology Today<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Web Employment Postings<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Advertiser Index<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Academy Products Index
April 14, 2010 | San Diego, CA | The first day of AudiologyNOW! ®<br />
FEATURED TOPICS<br />
ß Age-Related Hearing Loss: Demographics<br />
and Risk Factors<br />
ß Aging and the Auditory Periphery<br />
ß Aging, Auditory Perception, and Hearing Aids<br />
ß Aging and Central Auditory Neurobiology<br />
ß<br />
ß<br />
ß<br />
Aging and Clinical Electrophysiology<br />
Age-Related Changes in Cognition:<br />
Implications for Speech Perception<br />
Implications of Cognitive Factors for Aural<br />
Rehabilitation<br />
SPACE IS STILL AVAILABLE! Save Money—Register by March 30<br />
www.AcademyResearchConference.org<br />
<br />
<br />
<br />
<br />
<br />
AUDIOLOGYNO W! APRIL 14—17, 2010
He’s one of the most renowned Audiologists of his time, and his musical talents are just as revered. The one<br />
and only Charles “Chuck” Berlin, a Pioneer, an Audiologist and a Performer is about to come to a town near<br />
you, first stop ....... San Diego.<br />
On April 15th - 17th get a glimpse of what Persona Medical’s World Tour has to offer by stopping by booth<br />
#1938. Listen to Chuck play classical piano and speak about new innovations in Audiology. Chuck will be<br />
performing half past every hour during regular convention hours and will be available to answer questions<br />
throughout the event. Get educated and entertained all at once by visiting Persona Medical at booth #1938.<br />
Not attending AudiologyNow Don’t worry, Persona Medical’s World Tour featuring Chuck Berlin (with<br />
special guest Michael Poe) is coming to a town near you. Please visit personamedical.com for locations,<br />
dates and times. Limited seating is available and C.E.U. hours are provided.<br />
personamedical.com | 800.789.6543