October - LRS Institute of Tuberculosis & Respiratory Diseases
October - LRS Institute of Tuberculosis & Respiratory Diseases
October - LRS Institute of Tuberculosis & Respiratory Diseases
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
160 D.D.S. KULPATI<br />
During the ‘shock-lung” which<br />
follws<br />
are as<br />
Phase I: Traumatic shock necessitating<br />
resuscitation, blood and plasma infusion:<br />
spontaneous hyperventilation and hypocapnia<br />
(no hypoxaemia). This is followed by<br />
stabilization <strong>of</strong> circulation and respiration.<br />
Phase II: Early respiratory distress and<br />
V/Q imbalance. Hypoxaemia accompanied<br />
by 10-20% pulmonary AV shunting,<br />
hyperventilation and hypocapnia.<br />
Phase III: Hypoxia necessitating mechanical<br />
ventilation. Alveolar infiltrates on radiograph.<br />
Phase IV: Terminal hypoxia and hypercarbia<br />
(greater than 30% AV shunting).<br />
Diagnosis<br />
The diagnosis <strong>of</strong> ARDS is easier when all<br />
the characteristic clinical, radiographie,<br />
laboratory and physiological abnormalities<br />
are present (Table III) but it may remain<br />
extremely obscure when various features are<br />
evolving in seriously ill patients, ARDS occurs<br />
following a catastrophic injury or risk factors.<br />
Usually after a latent period <strong>of</strong> 12 to 48 hours,<br />
laboured breathing, intercostal retractions,<br />
tachypnoea due to decreased lung compliance<br />
and gas transfer abnormalities become manifest.<br />
The radiograph <strong>of</strong> the chest shows a<br />
chacteristic diffuse and rapidly progressive infiltrate<br />
which is interstitial at first and becomes<br />
bilateral, <strong>of</strong>ten symmetrical alveolar infiltrate<br />
later on, usually sparing the costophrenic<br />
and cardiophrenic angles. A few patients may<br />
never require intubation since nasal or high<br />
flow mask oxygen is adequate. However, the<br />
vast majority <strong>of</strong> patents require endotracheal<br />
intubation to establish a reliable flow <strong>of</strong> high<br />
oxygen concentration. An increase in the<br />
concentration <strong>of</strong> complement fragment C5a<br />
or the fibrin degradation product “D” has<br />
been detected in those who finally developed<br />
the syndrome (Haynes et al, 1980). Certain<br />
hemodynamic changes can also provide a<br />
reliable diagnostic guide (Shoemaker et al,<br />
1980).<br />
Cardiogenic edema is usually associated with<br />
cardiac enlargement, heart murmur, galloprhythm<br />
and raised jugular venous pressure.<br />
The radiograph <strong>of</strong> the chest shows parahilar<br />
butterfly pattern <strong>of</strong> pulmonary edema including<br />
pleural effusions and prominence <strong>of</strong> pulmonary<br />
lymphatic channels <strong>of</strong>ten called ‘Kerley linos’.<br />
However, the most sensitive method is to<br />
demonstrate raised pulmonary capillary wedge<br />
pressure (>16 mm Hg.) The protein eoncen-<br />
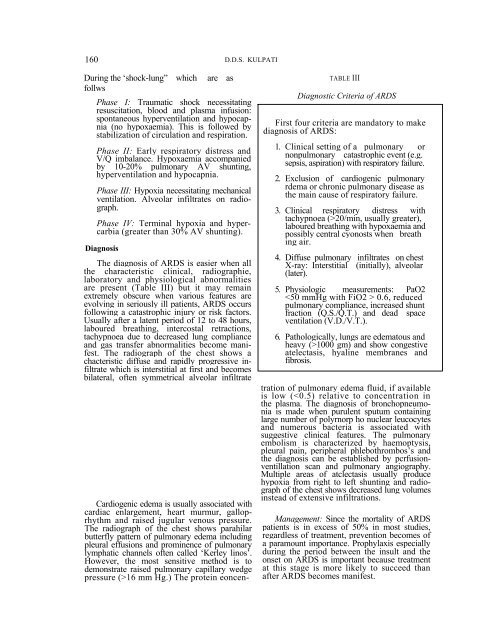
TABLE III<br />
Diagnostic Criteria <strong>of</strong> ARDS<br />
First four criteria are mandatory to make<br />
diagnosis <strong>of</strong> ARDS:<br />
1. Clinical setting <strong>of</strong> a pulmonary or<br />
nonpulmonary catastrophic event (e.g.<br />
sepsis, aspiration) with respiratory failure.<br />
2. Exclusion <strong>of</strong> cardiogenic pulmonary<br />
rdema or chronic pulmonary disease as<br />
the main cause <strong>of</strong> respiratory failure.<br />
3. Clinical respiratory distress with<br />
tachypnoea (>20/min, usually greater),<br />
laboured breathing with hypoxaemia and<br />
possibly central cyonosts when breath<br />
ing air.<br />
4. Diffuse pulmonary infiltrates on chest<br />
X-ray: Interstitial (initially), alveolar<br />
(later).<br />
5. Physiologic measurements: PaO2<br />
0.6, reduced<br />
pulmonary compliance, increased shunt<br />
fraction (Q.S./Q.T.) and dead space<br />
ventilation (V.D./V.T.).<br />
6. Pathologically, lungs are edematous and<br />
heavy (>1000 gm) and show congestive<br />
atelectasis, hyaline membranes and<br />
fibrosis.<br />
tration <strong>of</strong> pulmonary edema fluid, if available<br />
is low (