Enteral Tube feeding - Southern Health and Social Care Trust
Enteral Tube feeding - Southern Health and Social Care Trust
Enteral Tube feeding - Southern Health and Social Care Trust
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
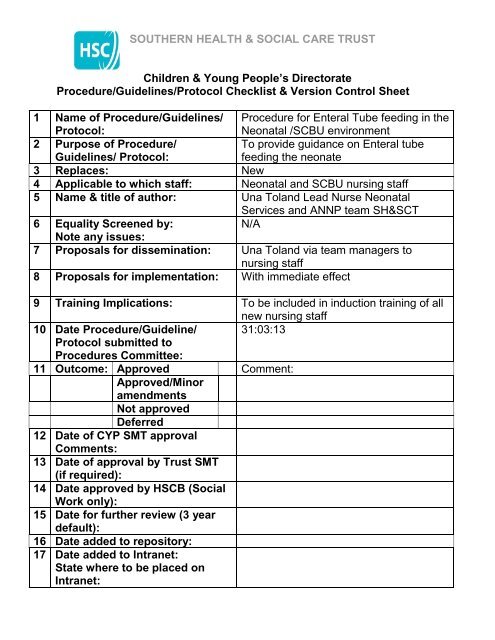
SOUTHERN HEALTH & SOCIAL CARE TRUST<br />
Children & Young People’s Directorate<br />
Procedure/Guidelines/Protocol Checklist & Version Control Sheet<br />
1 Name of Procedure/Guidelines/<br />
Protocol:<br />
Procedure for <strong>Enteral</strong> <strong>Tube</strong> <strong>feeding</strong> in the<br />
Neonatal /SCBU environment<br />
2 Purpose of Procedure/<br />
Guidelines/ Protocol:<br />
To provide guidance on <strong>Enteral</strong> tube<br />
<strong>feeding</strong> the neonate<br />
3 Replaces: New<br />
4 Applicable to which staff: Neonatal <strong>and</strong> SCBU nursing staff<br />
5 Name & title of author: Una Tol<strong>and</strong> Lead Nurse Neonatal<br />
Services <strong>and</strong> ANNP team SH&SCT<br />
6 Equality Screened by:<br />
N/A<br />
Note any issues:<br />
7 Proposals for dissemination: Una Tol<strong>and</strong> via team managers to<br />
nursing staff<br />
8 Proposals for implementation: With immediate effect<br />
9 Training Implications: To be included in induction training of all<br />
new nursing staff<br />
10 Date Procedure/Guideline/ 31:03:13<br />
Protocol submitted to<br />
Procedures Committee:<br />
11 Outcome: Approved Comment:<br />
Approved/Minor<br />
amendments<br />
Not approved<br />
Deferred<br />
12 Date of CYP SMT approval<br />
Comments:<br />
13 Date of approval by <strong>Trust</strong> SMT<br />
(if required):<br />
14 Date approved by HSCB (<strong>Social</strong><br />
Work only):<br />
15 Date for further review (3 year<br />
default):<br />
16 Date added to repository:<br />
17 Date added to Intranet:<br />
State where to be placed on<br />
Intranet:
SOUTHERN HEALTH & SOCIAL CARE TRUST<br />
PROCEDURE FOR ENTERAL TUBE FEEDING IN THE<br />
NEONATAL UNIT<br />
STATEMENT<br />
Within the neonatal environment naso/orogastric tubes are used primarily for the<br />
initiation <strong>and</strong> progression of enteral <strong>feeding</strong>, administration of oral medications<br />
<strong>and</strong> they can also be used for gastric decompression.<br />
The rationale for choice of size of <strong>feeding</strong> tube <strong>and</strong> whether or not it is for<br />
short term or long term use is determined by individualised infant care<br />
plans<br />
Gastric tubes are usually passed nasally for ease of insertion <strong>and</strong> fixation thus<br />
minimising the risk of displacement, but as this occludes one nostril gastric tubes<br />
may be passed orally when there is evidence of respiratory distress<br />
Where thickened feeds are prescribed, larger diameter tubes may be required.<br />
Free drainage of gastric tubes is used when gut decompression is required. To<br />
carry out free drainage, the external end of the tube is inserted into a container<br />
<strong>and</strong> the stopper opened.<br />
Wide bore tubes (usually PVC) are for short term use only <strong>and</strong> generally<br />
size 6fg <strong>and</strong> size 8fg are used.<br />
Infants 1500g will usually have a size 8fg gastric tube passed<br />
PVC tubes should be replaced every 7 days if indwelling or more often if<br />
clinically indicated<br />
If tube is not indwelling a new tube is inserted with every feed.<br />
Fine bore tubes (polyurethane) are intended for long term use<br />
The most common length used in the Neonatal unit is 56cms <strong>and</strong> size 6fg<br />
<strong>and</strong> size 8fg. These tubes should be replaced as per manufacturer’s<br />
instructions.<br />
Equipment – non indwelling orogastric tube<br />
Gastric <strong>feeding</strong> tube<br />
Appropriate milk feed <strong>and</strong>/ or medication<br />
Syringes – 1 for aspiration<br />
- 1 for bolus feed<br />
pH indicator strips
SOUTHERN HEALTH & SOCIAL CARE TRUST<br />
Equipment – indwelling nasogastric tube<br />
Gastric <strong>feeding</strong> tube size<br />
Syringes – 1 for aspiration (5ml or 10ml)<br />
- 1 for bolus feed (size depends on feed volume)<br />
Appropriate milk feed<br />
pH indicator strips<br />
Hydrocolloid<br />
Tegaderm<br />
Sterile scissors<br />
NB -if infant is distressed during insertion of <strong>feeding</strong> tube a soother may be<br />
offered. Or alternatively if clinically indicated oral sucrose may be offered as per<br />
Pain Management Guidelines.<br />
ACTION<br />
Explain procedure to parents/carers<br />
Preparation<br />
Decontaminate h<strong>and</strong>s as per local<br />
policy adhering to 7 step technique<br />
<strong>and</strong> 5 moments.<br />
Collect appropriate equipment, place<br />
at cot side in preparation for<br />
procedure.<br />
Decontaminate h<strong>and</strong>s again..<br />
Wear appropriate PPE -disposable<br />
apron <strong>and</strong><br />
Risk assess each situation. If there<br />
is a risk of contamination with<br />
bodily fluids, ie gastric aspirate or<br />
breast milk then non sterile gloves<br />
should be worn.<br />
Orogastric Insertion using ANTT<br />
approach<br />
Hold the <strong>feeding</strong> tube approx.<br />
5cms from the end<br />
Use the natural bend of the<br />
tube to follow the natural curves<br />
of the mouth <strong>and</strong> throat<br />
Insert the tube in the mouth <strong>and</strong><br />
towards the back of the throat,<br />
gently pushing it down the<br />
oesophagus until it reaches the<br />
RATIONALE<br />
To ensure parental/carers<br />
underst<strong>and</strong>ing, <strong>and</strong> gain informed<br />
consent.<br />
To prevent cross contamination <strong>and</strong><br />
to have all requirements readily<br />
available.<br />
Ensures correct positioning of<br />
<strong>feeding</strong> tube.<br />
End of <strong>feeding</strong> tube should remain<br />
inside pack until point of use. Do not<br />
touch key part—tip of <strong>feeding</strong> tube<br />
<strong>and</strong> syringe tips.
SOUTHERN HEALTH & SOCIAL CARE TRUST<br />
pre-measured mark on the tube<br />
Establishing correct placement of<br />
the <strong>feeding</strong> tube<br />
Gently aspirate tube using 5-10ml<br />
syringe. Test reaction of aspirate using<br />
pH indicator strips.<br />
Securing the <strong>feeding</strong> tube in place<br />
If there is a clinical decision made to<br />
keep the <strong>feeding</strong> tube in place it<br />
should be secured using a<br />
hydrocolloid base dressing placed on<br />
the infant’s skin onto which the <strong>feeding</strong><br />
tube is secured in place. Always check<br />
the correct positioning of the <strong>feeding</strong><br />
tube before commencing each feed.<br />
An external sticker should be attached<br />
to the stopper end of the tube<br />
indicating the date the tube was<br />
inserted <strong>and</strong> the length of insertion.<br />
Procedure for giving a tube feed<br />
Always check the expiry date of<br />
the feed <strong>and</strong> that the type <strong>and</strong><br />
amount of feed required is<br />
correct.<br />
Remove the plunger of a 10,20<br />
or 50ml sterile syringe<br />
Connect the barrel of the<br />
syringe to the end of the gastric<br />
tube<br />
Pinch the <strong>feeding</strong> tube while<br />
filling the syringe<br />
Fill the barrel with the correct<br />
volume of milk<br />
Let milk flow under gravity<br />
Hold the syringe 5-10cms<br />
above the infant until the<br />
syringe is empty.<br />
It should take approx. 10<br />
minutes for the milk to flow into<br />
the infant’s stomach. Changing<br />
the height of the syringe will<br />
also affect the speed of milk<br />
To check tube position following<br />
insertion. 5-10ml syringe generates<br />
lower pressure on stomach wall.<br />
(Syringe size still under NPSA<br />
review)<br />
NB: if unable to obtain aspirate<br />
consult NPSA Guidelines, 2005 for<br />
checking position of <strong>feeding</strong> tubes in<br />
babies.<br />
Use of hydrocolloid tape limits<br />
disruption of skin integrity.<br />
Accidental dislodgement can occur<br />
between feeds.<br />
Gravity feeds prevent pressure rises<br />
within the stomach thus decreasing<br />
the risk of regurgitation.<br />
Lowering the syringe slows the milk<br />
flow raising the syringe makes the<br />
milk flow faster.
SOUTHERN HEALTH & SOCIAL CARE TRUST<br />
<br />
<br />
flow.<br />
Observe the infant during the<br />
entire gastric feed. Do not leave<br />
the infant unattended. Stop the<br />
tube feed if the infant shows<br />
any sign of breathing difficulty,<br />
colour change, looks blue,<br />
becomes floppy, or vomits.<br />
Pinch the <strong>feeding</strong> tube during<br />
removal or cap the end of the<br />
gastric tube between feeds.<br />
Documentation<br />
Document relevant information in care<br />
pathway to include<br />
Who inserted the <strong>feeding</strong> tube<br />
Feeding tube size <strong>and</strong> position<br />
at the lips/nares<br />
Is tube secure<br />
Route of administration of the<br />
feed<br />
pH <strong>and</strong> amount <strong>and</strong> colour of<br />
aspirate<br />
Time <strong>and</strong> volume of feed<br />
administered.<br />
Type of feed administered<br />
To comply with NMC St<strong>and</strong>ards for<br />
record keeping <strong>and</strong><br />
recommendations from NPSA alert<br />
―Reducing the harm caused by<br />
misplaced gastric <strong>feeding</strong> tubes in<br />
babies under the care of neonatal<br />
units August 2005‖<br />
Continuous <strong>feeding</strong> via a Syringe<br />
pump connected to an indwelling<br />
<strong>feeding</strong> tube<br />
<br />
<br />
<br />
<br />
Only draw up <strong>and</strong> attach a<br />
syringe containing the volume<br />
of milk required for a 4 hour<br />
period.<br />
Use a new syringe to draw up<br />
milk at every 4 hourly change.<br />
Discard any unused milk <strong>and</strong><br />
the syringe at the end of the 4<br />
hour period<br />
The syringe should be labelled<br />
with the date <strong>and</strong> time of<br />
erection, the infant’s name,<br />
DOB, the type of milk used <strong>and</strong><br />
the date <strong>and</strong> time of the expiry<br />
of the milk.<br />
To reduce risk of microbial growth in<br />
milk or syringe containing milk over<br />
period of time<br />
To ensure the infant receives the<br />
right milk <strong>and</strong> the milk is within date.
SOUTHERN HEALTH & SOCIAL CARE TRUST<br />
<br />
<br />
The syringe pump should be<br />
clearly labelled MILK using the<br />
designated milk labels.<br />
A MILK sticker alert should be<br />
placed on the <strong>feeding</strong> tube<br />
close to the syringe pump <strong>and</strong> a<br />
further label placed close to the<br />
infant’s nares.<br />
To alert staff that this pump is for<br />
administration of MILK only<br />
To allow staff to track <strong>feeding</strong> tube<br />
from source to pump as part of<br />
safety checks<br />
March 2013<br />
REFERENCES<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Bradford City Teaching Primary <strong>Care</strong> <strong>Trust</strong> (2006) Community Children’s<br />
Team Nasogastric Feeding Policy <strong>and</strong> Procedure. Bradford City Teaching<br />
Primary <strong>Care</strong> <strong>Trust</strong>.<br />
Bradford Teaching Hospitals NHS <strong>Trust</strong> (2004) Children <strong>and</strong> Neonatal<br />
Services Nasogastric tube policy. Bradford City NHS <strong>Trust</strong>.<br />
S.H.S.C.T. (2009) Policy on Gaining Consent.<br />
Knox, T <strong>and</strong> Davie J, (2009) Nasogastric tube <strong>feeding</strong> – which syringe size<br />
produces lower pressure <strong>and</strong> is safest to use Nursing Times, 105:27<br />
National Patient Safety Agency (2007) Patient Safety Alert 19. Promoting<br />
safer measurement <strong>and</strong> administration of liquid medicines via oral <strong>and</strong><br />
other enteral routes. London: NPSA<br />
National Patient Safety Agency (2005) Patient Safety Alert 05. How to<br />
confirm the correct position of nasogastric <strong>feeding</strong> tubes in infants,<br />
children <strong>and</strong> adults. London: NPSA<br />
Great Ormond Street Hospital NHS <strong>Trust</strong> (2009). Clinical Guideline:<br />
nasogastric <strong>and</strong> orogastric tube management<br />
NMC (2008) Guidelines for Record Keeping.<br />
National Patient Safety Agency (2005) Patient Safety Alert 09. Reducing<br />
the harm caused by misplaced naso <strong>and</strong> orogastric <strong>feeding</strong> tubes in<br />
babies under the care of neonatal units. London: NPSA.<br />
Freer, Y. <strong>and</strong> Lyon, A. (2005) Nasogastric tube aspirate pH values<br />
associated with typical enteral <strong>feeding</strong> patterns in infants admitted to an<br />
NICU, Journal of Neonatal Nursing, 11, 106-109.<br />
ReferenceNewborn Services Clinical Guideline<br />
http://www.adhb.govt.nz/guidelines/nutrition/withholding feeds.htm
SOUTHERN HEALTH & SOCIAL CARE TRUST<br />
FEED TOLERANCE GUIDE FOR NEONATES RECEIVING TUBE FEEDS<br />
Frequency of tube feeds Frequency of aspiration of tube<br />
to assess feed tolerance<br />
hourly<br />
6 hourly<br />
2 hourly 4 hourly<br />
3 hourly 3 hourly<br />
4 hourly 4 hourly<br />
When assessing aspirate volumes always consider<br />
Colour of aspirate<br />
Indicative Colour Chart for Assessing Aspirate Colour<br />
Milk Lemon Mustard Wasabi Lime Avocado Spinach<br />
1 2 3 4 5 6 7<br />
Aspirate colour 4 - 7 Seek medical /ANNP advise before proceeding with feed<br />
Consistency of aspirate -- altered milk appearance<br />
Volume of aspirate<br />
Frequency of feeds<br />
Evidence of possits<br />
Stool pattern, amount, consistency, evidence of blood <strong>and</strong>/or mucous in<br />
stool. Consider need for glycerine suppository.<br />
Evidence of abdominal distension, discoloration, abdominal tenderness.<br />
Consider need for AXR.<br />
General clinical condition, cardio respiratory instability, temperature<br />
instability.<br />
If aspirate<br />
50% of 3 or<br />
4 hourly total<br />
feed volume<br />
Return<br />
aspirate if<br />
altered milk<br />
Aspirate<br />
stomach<br />
contents<br />
Alert ANNP /Medical<br />
staff, clinically assess<br />
review <strong>feeding</strong> plan,<br />
document changes..<br />
Alert ANNP / Medical<br />
staff clinically assess.<br />
Review <strong>feeding</strong> plan<br />
<strong>and</strong> document changes.<br />
Do not increment<br />
feed.