Hypoglycemia in the newborn period - New Born Baby
Hypoglycemia in the newborn period - New Born Baby Hypoglycemia in the newborn period - New Born Baby
AIIMS- NICU protocols updated 2007 mg/dl after 24 hours of parentral therapy, the infusion can be tapered off at the rate of 2 mg/kg/min every 6 hours, with glucose monitoring. Tapering has to be accompanied by concomitant increase in oral feeds. Once a rate of 4 mg/kg/min of glucose infusion is reached and oral intake is adequate and the blood sugar values are consistently > 50 mg/dL the infusion can be stopped without further tapering. Ensure continuous glucose infusion without any interruption preferably using infusion pump. Do not stop an IV infusion of glucose abruptly; severe rebound hypoglycemia may occur. Avoid using > 12.5% dextrose infusion through a peripheral vein due to the risk of thrombophlebitis Recurrent / resistant hypoglycemia This condition should be considered when there is a failure to maintain normal blood sugar levels despite a glucose infusion of 12 mg/kg/min or when stabilization is not achieved by 7 days of life. High levels of glucose infusion may be needed in the infants to achieve euglycemia. Table no 4 : Important causes of resistant hypoglycemia and investigations Important causes of resistant hypoglycemia Investigations to be considered Congenital hypopitutarism Serum insulin levels Adrenal insufficiency Hyperinsulenemic states Galactosemia Glycogen storage disorders Maple syrup urine disease Mitochondrial disorders Serum cortisol levels Growth hormone levels Blood ammonia Blood lactate levels Urine ketones and reducing substances Urine and sugar aminoacidogram Besides increasing the rate of glucose infusion, drugs may also be tried in the treatment of resistant hypoglycemia. Before administration of the drugs , take the samples to investigate the cause (Table no 3) . Drugs that are used include the following: Downloaded from www.newbornwhocc.org 8
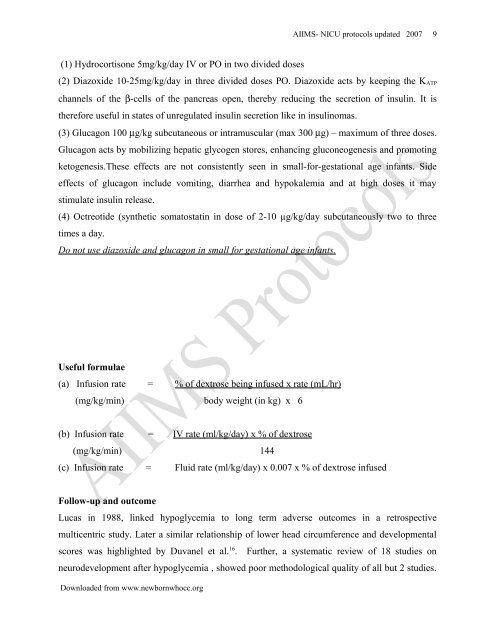
(1) Hydrocortisone 5mg/kg/day IV or PO in two divided doses AIIMS- NICU protocols updated 2007 (2) Diazoxide 10-25mg/kg/day in three divided doses PO. Diazoxide acts by keeping the KATP channels of the β-cells of the pancreas open, thereby reducing the secretion of insulin. It is therefore useful in states of unregulated insulin secretion like in insulinomas. (3) Glucagon 100 μg/kg subcutaneous or intramuscular (max 300 μg) – maximum of three doses. Glucagon acts by mobilizing hepatic glycogen stores, enhancing gluconeogenesis and promoting ketogenesis.These effects are not consistently seen in small-for-gestational age infants. Side effects of glucagon include vomiting, diarrhea and hypokalemia and at high doses it may stimulate insulin release. (4) Octreotide (synthetic somatostatin in dose of 2-10 µg/kg/day subcutaneously two to three times a day. Do not use diazoxide and glucagon in small for gestational age infants. Useful formulae (a) Infusion rate = % of dextrose being infused x rate (mL/hr) (mg/kg/min) body weight (in kg) x 6 (b) Infusion rate = IV rate (ml/kg/day) x % of dextrose (mg/kg/min) 144 (c) Infusion rate = Fluid rate (ml/kg/day) x 0.007 x % of dextrose infused Follow-up and outcome Lucas in 1988, linked hypoglycemia to long term adverse outcomes in a retrospective multicentric study. Later a similar relationship of lower head circumference and developmental scores was highlighted by Duvanel et al. 16 . Further, a systematic review of 18 studies on neurodevelopment after hypoglycemia , showed poor methodological quality of all but 2 studies. Downloaded from www.newbornwhocc.org 9
- Page 1 and 2: Hypoglycemia in the Newborn AIIMS-
- Page 3 and 4: Introduction AIIMS- NICU protocols
- Page 5 and 6: Clinical signs associated with hypo
- Page 7: AIIMS- NICU protocols updated 2007
- Page 11 and 12: AIIMS- NICU protocols updated 2007
(1) Hydrocortisone 5mg/kg/day IV or PO <strong>in</strong> two divided doses<br />
AIIMS- NICU protocols updated 2007<br />
(2) Diazoxide 10-25mg/kg/day <strong>in</strong> three divided doses PO. Diazoxide acts by keep<strong>in</strong>g <strong>the</strong> KATP<br />
channels of <strong>the</strong> β-cells of <strong>the</strong> pancreas open, <strong>the</strong>reby reduc<strong>in</strong>g <strong>the</strong> secretion of <strong>in</strong>sul<strong>in</strong>. It is<br />
<strong>the</strong>refore useful <strong>in</strong> states of unregulated <strong>in</strong>sul<strong>in</strong> secretion like <strong>in</strong> <strong>in</strong>sul<strong>in</strong>omas.<br />
(3) Glucagon 100 μg/kg subcutaneous or <strong>in</strong>tramuscular (max 300 μg) – maximum of three doses.<br />
Glucagon acts by mobiliz<strong>in</strong>g hepatic glycogen stores, enhanc<strong>in</strong>g gluconeogenesis and promot<strong>in</strong>g<br />
ketogenesis.These effects are not consistently seen <strong>in</strong> small-for-gestational age <strong>in</strong>fants. Side<br />
effects of glucagon <strong>in</strong>clude vomit<strong>in</strong>g, diarrhea and hypokalemia and at high doses it may<br />
stimulate <strong>in</strong>sul<strong>in</strong> release.<br />
(4) Octreotide (syn<strong>the</strong>tic somatostat<strong>in</strong> <strong>in</strong> dose of 2-10 µg/kg/day subcutaneously two to three<br />
times a day.<br />
Do not use diazoxide and glucagon <strong>in</strong> small for gestational age <strong>in</strong>fants.<br />
Useful formulae<br />
(a) Infusion rate = % of dextrose be<strong>in</strong>g <strong>in</strong>fused x rate (mL/hr)<br />
(mg/kg/m<strong>in</strong>) body weight (<strong>in</strong> kg) x 6<br />
(b) Infusion rate = IV rate (ml/kg/day) x % of dextrose<br />
(mg/kg/m<strong>in</strong>) 144<br />
(c) Infusion rate = Fluid rate (ml/kg/day) x 0.007 x % of dextrose <strong>in</strong>fused<br />
Follow-up and outcome<br />
Lucas <strong>in</strong> 1988, l<strong>in</strong>ked hypoglycemia to long term adverse outcomes <strong>in</strong> a retrospective<br />
multicentric study. Later a similar relationship of lower head circumference and developmental<br />
scores was highlighted by Duvanel et al. 16 . Fur<strong>the</strong>r, a systematic review of 18 studies on<br />
neurodevelopment after hypoglycemia , showed poor methodological quality of all but 2 studies.<br />
Downloaded from www.<strong>newborn</strong>whocc.org<br />
9