Cemented vs Uncemented Total hip Arthroplasty ANZCVS Resident ...
Cemented vs Uncemented Total hip Arthroplasty ANZCVS Resident ...
Cemented vs Uncemented Total hip Arthroplasty ANZCVS Resident ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
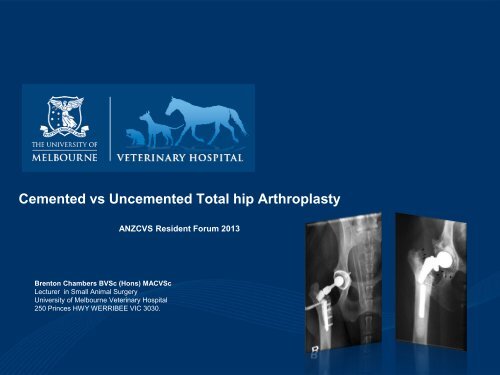
<strong>Cemented</strong> <strong>vs</strong> <strong>Uncemented</strong> <strong>Total</strong> <strong>hip</strong> <strong>Arthroplasty</strong><br />
<strong>ANZCVS</strong> <strong>Resident</strong> Forum 2013<br />
Brenton Chambers BVSc (Hons) MACVSc<br />
Lecturer in Small Animal Surgery<br />
University of Melbourne Veterinary Hospital<br />
250 Princes HWY WERRIBEE VIC 3030.
Lecture Outline<br />
• Previous Exam Questions<br />
• Indications<br />
• Techniques<br />
• <strong>Cemented</strong> CFX<br />
• <strong>Uncemented</strong> BFX, Kyon, Helica<br />
• Complications<br />
• Operative<br />
• Early<br />
• Late
Previous Exam Questions<br />
2008 Part1<br />
2. Discuss two (2) only of the following:<br />
• The proposed aetiology and pathogenesis of<br />
nonseptic loosening of cemented <strong>hip</strong><br />
prostheses. Include in your answer a<br />
discussion of cytokine involvement and<br />
cellular changes
Indications for <strong>Total</strong> Hip <strong>Arthroplasty</strong><br />
• THR is a salvage procedure replacing the diseased<br />
joint components (acetabulum and femoral head)<br />
with commercially available prostheses divided into<br />
cemented and non-cemented systems<br />
• Indications: (Skeletally mature or near mature only)<br />
– OA unresponsive to appropriate medical management<br />
– Failed FHNE<br />
– Traumatic or chronic coxofemoral luxation<br />
– Irreparable/failed /malunion Acetabular fracture<br />
– Irreparable/failed/malunion Femoral head and neck fracture<br />
– Avascular necrosis of femoral head/neck (Jankovits 2011)<br />
– Slipped Femoral Capital Physis (Gemmill 2012)
Contra-Indications<br />
• Animals with concurrent active<br />
infectious disease:<br />
• Local<br />
• Distant<br />
• Animals with systemic illness<br />
predisposing to infectious disease or<br />
delayed healing<br />
• Concurrent neurologic disease (Olmsted<br />
1987)<br />
• Size NOT contra-indication (Warnock 2003)
Commercial Systems<br />
• Biomedtrix – CFX / BFX/ Hybrid<br />
– Modular system:<br />
• Acetabular cup UHMWPE<br />
• Femoral Head<br />
• Femoral Stem<br />
– Universal, micro, nano<br />
• Kyon/Zurich – <strong>Uncemented</strong> (Screw<br />
Fixation)<br />
• Helica – novel screw prosthesis<br />
• Amplitude – Dual Mobility
Published Complications<br />
• Luxation<br />
• Septic loosening<br />
• Aseptic loosening<br />
• Fracture<br />
• Implant failure<br />
• Sciatic Neuropraxia<br />
• Pulmonary Embolism<br />
• Overall complication rate 7-22%
<strong>Cemented</strong> Technique<br />
• Pre-operative Implant templating<br />
radiographs<br />
• Implant stability result of PMMA<br />
cohesive<br />
• Cementing technique influences mantle<br />
quality and stability (Ota 2005, Wixon<br />
1997)<br />
• Antibiotic combined with cement<br />
beneficial for prophylaxis
<strong>Cemented</strong> Technique Acetabular Preparation<br />
• Acetabular reaming<br />
• Establish appropriate surface for cement cohesion<br />
• Sufficient Dorsal Support<br />
• Sufficient Medial Support<br />
• Alignment: (Cross 2000a,b, Dyce 2000)<br />
• 5-10 deg closed<br />
• 10-20 deg retroversion<br />
• Association with luxation (Hunter 2003, Konde 1982,<br />
Massat 1984, Dyce 2000, Nelson 2007)<br />
• Recommended ALO 35-45 degrees
<strong>Cemented</strong> technique - Femoral Preparation<br />
• External rotation of femur<br />
• Trochanteric osteotomy not recommended<br />
(Wylie 1997)<br />
• Reamers and broaches used to prepare<br />
femur:<br />
• Filling of bony irregularities with debris<br />
• Pulsatile lavage suction increases cohesion by 185%<br />
(Askew 1984)<br />
• Important Factors:<br />
• Appropriate prosthesis size (2mm cement mantle)<br />
• Correct final positioning of stem
<strong>Cemented</strong> technique - Femoral Preparation<br />
• Prewarming stem prevents expansion/contraction with<br />
exothermic PMMA polymerisation (Bishop 1996)<br />
• Stem Centraliser prevents endosteal contact and<br />
maximises uniformity of cement mantle (Schulz 1999)<br />
• Retrograde cement fill and slow stem insertion minimises<br />
cement mantle void formation<br />
• Maximum collar contact reduces stress and implant failure<br />
(Manley 1995, Shatzker 1989)<br />
• Normo to slight anteversion<br />
• Modular head components allow adjustment:<br />
– Short neck predisposes to luxation<br />
– Long neck results in external rotation and abduction<br />
• Hip skids for reduction damage heads – aseptic loosening
<strong>Uncemented</strong> <strong>Total</strong> Hip <strong>Arthroplasty</strong><br />
• Short term stability provided by:<br />
• Precise press fit (BFX)<br />
• Monocortical screws (Kyon)<br />
• Screw prosthesis (Helica)<br />
• Long term Stability provided by:<br />
• Osseous ingrowth into porous incorporated surfaces
<strong>Uncemented</strong> <strong>Total</strong> Hip <strong>Arthroplasty</strong><br />
• Advantages:<br />
• Longer implant life (reduced aseptic loosening)<br />
• Decreased post-operative/late infection<br />
• Better stability (bone ingrowth)<br />
• Disadvantages:<br />
• Increased risk intra-operative femoral<br />
fracture/fissure<br />
• Precise preparation required
Technique Differences BFX <strong>vs</strong> CFX<br />
• Higher Osteotomy location (isthmus)<br />
• Acetabular reaming to EXACT templated size<br />
• Orientation during reaming maintained for press fit<br />
• Broaches but no reaming for femoral stem<br />
component<br />
• Observe cortex as final size approached:<br />
• Circlage applied if fissures detected and size<br />
increases abandoned<br />
• Fractures revised with CFX – advantage of biomedtix<br />
cross compatibility
THR in Smaller Dogs & Cats – Mini/Micro/Nano<br />
• Technique variations:<br />
• Burr for acetabular preparation cf reamer<br />
• Craniodorsal capsular prosthesis due to laxity<br />
– (Warnock 2003, Marino 2012)<br />
• Luxation rates:<br />
• Similar to THR in larger dogs<br />
• 4% after falling from owners arms (Marino 2012)<br />
• Outomes:<br />
• Excellent to good in<br />
• No sig difference in forceplate data btn<br />
contralateral limb (Jankovits 2011)
Kyon/ Zurich<br />
• Cup:<br />
• Perforated double shell outer<br />
titanium shell allows osseous<br />
integration (Convection currents)<br />
• Inner UHMWPE contact surface<br />
• Geometry reduces contact<br />
pressures<br />
• Initial press-fit augmented by<br />
screw fixation<br />
• Modular head system<br />
• Amorphous Diamond coating<br />
reduces wear particles
Kyon/Zurich<br />
• Argued press-fit, canal filling<br />
systems cannot be stable at all<br />
contact areas and motion (tension<br />
on lateral, compression medial<br />
during weight bearing) prevents<br />
osseous integration<br />
• Initial stability provided by bi- and<br />
monocortical locking screw fixation<br />
to medial cortex alone – no lateral<br />
cortical contact allows more<br />
effective bone ingrowth (reduces<br />
stress shielding)
Kyon/Zurich - Complications<br />
• Hummel (2010):<br />
• Most common complications were intraoperative<br />
femoral fracture, luxation and septic<br />
loosening<br />
• Higher overall rates than for previously reported<br />
cemented and other cemented techniques plus<br />
higher than previously reported for Zurich THR<br />
• Previously performed <strong>Cemented</strong> THR or FHNA<br />
assoc with success.
Helica<br />
• Bone preserving prosthesis<br />
• Self-cutting threaded titanium<br />
alloy femoral implant screws<br />
into femoral neck<br />
• UHMWPE acetabular<br />
prosthesis enclosed in titanium<br />
shell – self threading screw<br />
• Long-term Objective outcomes<br />
data?
Helica<br />
• Hach (2009):<br />
• Implant loosening 12.5% - 0 luxations<br />
• Short procedure<br />
• Viefhues (2010):<br />
• Aseptic loosening 8.1% - 0 luxations<br />
• Andreoni (2010):<br />
• Revision of aseptically loosened stem and cup<br />
with kyon<br />
• Kim (2011):<br />
• Sig alterations in strain - decreases in medial<br />
longitudinal compression<br />
• Correlates with loosening seen clinically
Complications - Luxation<br />
• Early complication (< 9 weeks) (Cross 2000)<br />
• Trigonometric assessment of acetabular<br />
position in 3 axes (Cross 2000) –<br />
• Acetabular version and inclination poor<br />
indicators of luxation.<br />
• Tolerance of malposition<br />
• Associated with Acetabular cup position (Dyce<br />
2000):<br />
• ALO > 60 degrees - *x increased risk<br />
• Pelvic Limb amputees increased risk (44%)<br />
(Preston 1999)
Complications – Ventral Luxation<br />
• Ventral Luxation 4 th most<br />
common complication (Nelson<br />
2007)<br />
• Risk factors:<br />
• St Bernard Breed – risk recurrent VL<br />
• Short Neck Extension<br />
• High ALO ???<br />
• Recommended ALO protective <strong>vs</strong><br />
ventral luxation
Luxation – Dual Mobility Prosthesis<br />
• Recent development: (Guillaumot 2012)<br />
• Metal backed outer acetabular component<br />
• Inner mobile UHMWPE component<br />
• Metallic head<br />
• <strong>Cemented</strong> stem prosthesis<br />
• Prospective trial of 50 dogs – no<br />
luxation (Guillaumot 2012)
Complications – Septic Loosening<br />
• Reports of incidence vary from 1-3.7%<br />
• Lee (2002)<br />
• 40% positive culture rate<br />
• Closing culture results not assoc with success<br />
• Increased risk positive culture with increased<br />
surgical duration
Complications – Aseptic Loosening<br />
• Activation of macrophages by submicron<br />
wear products in effective joint<br />
space results in: (Iwata 2008, Gristina<br />
1994, Holt 2007**)<br />
• Wear products result from biomechanical<br />
forces and host physiologic processes<br />
• Macrophages attempt to ingest and eliminate<br />
wear products – chronic inflammatory reaction<br />
• Direct enzymatic osteolysis via production of<br />
reactive oxygen species<br />
• Osteoclastic activation
Complications – Aseptic Loosening<br />
• Constant remodelling mediated by both<br />
osteoclastic and osteoblastic activity<br />
• Imbalances in blastic <strong>vs</strong> clastic activity result<br />
from altered cytokine expression<br />
• Many pro-inflammatory cytokines expressed :<br />
• TNF-a<br />
Osteoclastogenesis<br />
• IL-1
Aseptic Loosening – Osteoclastogenesis<br />
RANKL-RANK-OPG-NF-κβ<br />
• Initially termed cement disease<br />
• PMMA wear products increase<br />
expression of RANKL<br />
• RANKL binding with cell surface<br />
receptor RANK results in initiation of<br />
NF-kb pathways resulting in<br />
osteoclastogenesis and Activation of<br />
mature osteoclasts<br />
• RANKL-RANK inhibited by OPG
RANKL-RANK-NF-κβ
Complications Aseptic Loosening<br />
• Chronic inflammation also results in a<br />
fibro-inflammatory zone populated by<br />
exhausted macrophages resulting in<br />
immuno-incompetance<br />
• Low virulence bacteria can survive and<br />
populate in biofilms<br />
• Advanced cementing techniques<br />
improve mantle grade but did not affect<br />
incidence of aseptic loosening (Ota<br />
2005)
Aseptic Loosening Diagnosis<br />
• Animals present with progressive<br />
lameness<br />
• Radiographs poorly specific<br />
(52%) (Frankel 2004)<br />
• Findings indicative of loosening<br />
• Cement mantle cracks<br />
• Cement-metal interface leucency<br />
• Implant retroversion<br />
• Endosteal pedestal formation
Complications - Aseptic loosening Prevention?<br />
• Wise 2005 :<br />
• Dose dependant effect of ZLN<br />
• Improved amt endosteal bone @ 26 weeks<br />
• Reduced loss of bone assoc with implant stress<br />
shielding but not aseptic loosening<br />
• Inconclusive and short term assessment<br />
• Wood (2003)<br />
• Future:<br />
• Avoid use of uncoated <strong>hip</strong>s skids<br />
• RANK blockade (RANK;Fc Ab)<br />
• OPG?
Complications - Fracture<br />
• CFX:<br />
• BFX<br />
• 2.9% (Liska 2004)<br />
• Intra or post operative (up to 2196 days)<br />
• Excessive reaming, osteopathy, aseptic<br />
loosening, altered modulus<br />
• Plate, screw, wire ORIF<br />
• 13% (Ganz 2004)<br />
• Earlier complication resulting from press-fit<br />
preparation/ undetected fissures<br />
• ↓Canal Flare Index (Stovepipe conformation)<br />
• Increasing age
Canal Flare Index<br />
• Ratio of intracortical width<br />
at level of lesser<br />
trochanter to the<br />
intracortical width at<br />
isthmus A/B
Complications – Implant Failure<br />
• Loss of stem support and cyclic cantilever<br />
loading results in fatigue failure (Yates 2010)<br />
• Aseptic Loosening<br />
• Stress shielding<br />
• Cement mantle quality<br />
• Human literature:<br />
• Femoral stem fracture 0.23-0.67%<br />
• Cantilever bending assoc with 62%<br />
• Implant design<br />
• Metallurgical composition<br />
• Cement mantle quality
Complications – Sciatic Neuropraxia<br />
• Incidence 1.2-2%<br />
• 1000 same surgeon THR (BFX/CFX/Hybrid)<br />
• Risk Factors:<br />
– Age at sx<br />
– Difficulty of sx<br />
– Traumatic pre-sx luxation<br />
– Revision sx<br />
• Complete recovery expected (Time<br />
variable)<br />
• Mean 35 days (10-120days)
Complications – Pulmonary Embolism<br />
• Incidence: (Liska 2003) - CFX<br />
• Perfusion defects in 82% of 44 dogs<br />
• Assessed via:<br />
– Scintigraphic perfusion studies<br />
– Transoesophageal u/s<br />
• During stem implantation – intramedullary<br />
pressure<br />
• Embolic sources:<br />
• Air, PMMA, Fat, Clots<br />
• Consequences:<br />
• Clinically silent/spontaneous recovery<br />
• Fatal (Terrell 2004)
Complications Tabular Summary<br />
Author Outcome Luxation<br />
Aseptic<br />
Loosening Septic Fracture<br />
Implant<br />
Failure<br />
Pulmonary<br />
Embolism<br />
Sciatic<br />
Neuropraxia<br />
Acetabular<br />
Displacement<br />
Comments<br />
Skurla 2000<br />
84.1% excellent or good.<br />
Cross 2000 12% CFX<br />
Warnock 2003 83% good to excellent 11% 5% Mini CFX<br />
Liska 2010 91% 18% 2% 2% 2% Micro CFX in dogs and cats<br />
Marino 2012 92% 10% 2% Micro CFX in dogs and cats<br />
Jankovits<br />
Micro CFX in dogs for avascular necrosis and cats<br />
Gemmil 2012 92% good to excellent 6% Hybrid THR for slipped capital physis<br />
Ireifej 2012 100% 25% 8% Nano CFX in dogs<br />
Ganz 2010 13.10% BFX<br />
Liska 2004 2.90% CFX<br />
Hummel 2010 3.70% 3.70% 11% 2.50% 1.20% Kyon<br />
Guererro 2009 97% 11.00% 1.50% 3% 1.5% 3% Kyon<br />
Ota 2005 7% 2.10% 1.10% CFX examining effect of cement technique<br />
Preston 1999 44% CFX - pelvic limb amputees<br />
Dyce 2000 4.70% 0.50% 1% 1% CFX<br />
Bergh 2006 6.50% 1.50% 6.40% 1.30% 4.80% CFX<br />
Forster 2012<br />
94% good to very good<br />
Andrews 2008 1.90%<br />
Liska 2003 82%<br />
Hach 2009 0 12.50% 2% 2% Helica<br />
Viefhues 2010 0 8.10% 2.70% Helica
Complications by System<br />
Complication CFx BFx Zurich/Kyon Helica<br />
Luxation 4.7-12%<br />
18% (Nano)<br />
44% (Amputees)<br />
Septic 1-1.5% 1.5-3.7%<br />
3.7-11% 0%<br />
Aseptic Loosening 0.5-5% 8.1-12.5%<br />
Fracture 1-6.4%<br />
25% (Nano)<br />
13% 3-11% 2%<br />
Implant Failure 1.1% 1.5-2.5%<br />
Sciatic<br />
Neuropraxia<br />
1.3-2% 1.3-2% 2%
Removal / Revision<br />
• Indications:<br />
• Aseptic Loosening of Stem / cup components<br />
• Septic Implants<br />
• Luxation<br />
• Femoral Window Technique (Dyce 2002)<br />
• Removal of infected CFX implants<br />
• Complete cement removal in 83%<br />
• 50% Staph aureus – 3-10 weeks Abx<br />
• Outcome sim to FHNE<br />
• Human Classification Systems
Removal Revision<br />
• Torres ( 2009):<br />
• BFX revision of 3 failed CFX<br />
• Autogenous cancellous bone graft<br />
• Successful in all cases despite +ve culture in 1<br />
• Massat (1998)<br />
• Single stage revision ( 1 x septic, 1 x aseptic)<br />
• Revision common in humans – explantation<br />
more common in dogs<br />
• Single stage revision successful in both
Future Developments<br />
• Hybrid fixation stems<br />
(Baleani 2000)<br />
• Combination press-fit and<br />
cement<br />
• Less micromotion in ex-vivo<br />
biomech studies<br />
• Dual Mobility Implants<br />
• Targeted therapy <strong>vs</strong><br />
mechanisms of Aseptic<br />
Loosening
Questions?