Journal_1_2014_final_WEB
Journal_1_2014_final_WEB
Journal_1_2014_final_WEB
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Science, Practice and Education<br />
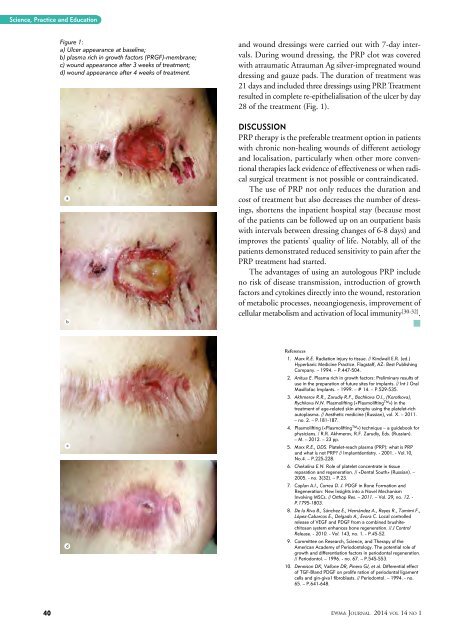
Figure 1:<br />
a) Ulcer appearance at baseline;<br />
b) plasma rich in growth factors (PRGF)-membrane;<br />
c) wound appearance after 3 weeks of treatment;<br />
d) wound appearance after 4 weeks of treatment.<br />
a<br />
b<br />
and wound dressings were carried out with 7-day intervals.<br />
During wound dressing, the PRP clot was covered<br />
with atraumatic Atrauman Ag silver-impregnated wound<br />
dressing and gauze pads. The duration of treatment was<br />
21 days and included three dressings using PRP. Treatment<br />
resulted in complete re-epithelialisation of the ulcer by day<br />
28 of the treatment (Fig. 1).<br />
Discussion<br />
PRP therapy is the preferable treatment option in patients<br />
with chronic non-healing wounds of different aetiology<br />
and localisation, particularly when other more conventional<br />
therapies lack evidence of effectiveness or when radical<br />
surgical treatment is not possible or contraindicated.<br />
The use of PRP not only reduces the duration and<br />
cost of treatment but also decreases the number of dressings,<br />
shortens the inpatient hospital stay (because most<br />
of the patients can be followed up on an outpatient basis<br />
with intervals between dressing changes of 6-8 days) and<br />
improves the patients’ quality of life. Notably, all of the<br />
patients demonstrated reduced sensitivity to pain after the<br />
PRP treatment had started.<br />
The advantages of using an autologous PRP include<br />
no risk of disease transmission, introduction of growth<br />
factors and cytokines directly into the wound, restoration<br />
of metabolic processes, neoangiogenesis, improvement of<br />
cellular metabolism and activation of local immunity [30-32] .<br />
<br />
m<br />
c<br />
d<br />
References<br />
1. Marx R.E. Radiation injury to tissue. // Kindwall E.R. (ed.)<br />
Hyperbaric Medicine Practice. Flagstaff, AZ: Best Publishing<br />
Company. – 1994. – P.447-504.<br />
2. Anitua E. Plasma rich in growth factors: Preliminary results of<br />
use in the preparation of future sites for implants. // Int J Oral<br />
Maxillofac Implants. – 1999. – # 14. – P.529-535.<br />
3. Akhmerov R.R., Zarudiy R.F., Bochkova O.I., (Korotkova),<br />
Rychkova N.N. Plasmolifting («Plasmolifting TM ») in the<br />
treatment of age-related skin atrophy using the platelet-rich<br />
autoplasma. // Aesthetic medicine (Russian), vol. X. – 2011.<br />
– no. 2. – P.181-187.<br />
4. Plasmolifting («Plasmolifting TM ») technique – a guidebook for<br />
physicians. / R.R. Akhmerov, R.F. Zarudiy, Eds. (Russian).<br />
– M. – 2012. – 23 pp.<br />
5. Marx R.E., DDS. Platelet-reach plasma (PRP): what is PRP<br />
and what is not PRP? // Implantdentistry. - 2001. - Vol.10,<br />
No.4. – P.225-228.<br />
6. Chekalina E.N. Role of platelet concentrate in tissue<br />
reparation and regeneration. // «Dental South» (Russian). –<br />
2005. - no. 3(32). – P.23.<br />
7. Caplan A.I., Correa D. J. PDGF in Bone Formation and<br />
Regeneration: New Insights into a Novel Mechanism<br />
Involving MSCs. // Orthop Res. – 2011. – Vol. 29, no. 12. -<br />
P.1795-1803.<br />
8. De la Riva B., Sánchez E., Hernández A., Reyes R., Tamimi F.,<br />
López-Cabarcos E., Delgado A., Evora C. Local controlled<br />
release of VEGF and PDGF from a combined brushitechitosan<br />
system enhances bone regeneration. // J Control<br />
Release. - 2010. - Vol. 143, no. 1. - P.45-52.<br />
9. Committee on Research, Science, and Therapy of the<br />
American Academy of Periodontology. The potential role of<br />
growth and differentiation factors in periodontal regeneration.<br />
// Periodontol. – 1996. - no. 67. – P.545-553.<br />
10. Dennison DK, Vallone DR, Pinero GJ, et al. Differential effect<br />
of TGF-Bland PDGF on prolife ration of periodontal ligament<br />
cells and gin-giva l fibroblasts. // Periodontol. – 1994. - no.<br />
65. – P.641-648.<br />
40<br />
EWMA <strong>Journal</strong> <strong>2014</strong> vol 14 no 1