PVL-associated Staphylococcus aureus infections
PVL-associated Staphylococcus aureus infections
PVL-associated Staphylococcus aureus infections
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>PVL</strong>-<strong>associated</strong> <strong>Staphylococcus</strong><br />
<strong>aureus</strong> <strong>infections</strong><br />
Infection Control Nurses<br />
December 2009
Introduction<br />
• What is <strong>PVL</strong>-Staph?<br />
• Why is it important?<br />
• How do we spot it?<br />
• What do we do about it?
History of <strong>PVL</strong><br />
• Discovered by Van de Velde in 1894 - ability to<br />
destroy leucocytes<br />
• Named after Sir Philip Noel Panton and Francis<br />
Valentine when they <strong>associated</strong> this with soft<br />
tissue <strong>infections</strong> in 1932<br />
• <strong>PVL</strong> has been seen in the UK since the 1950s<br />
and 60s
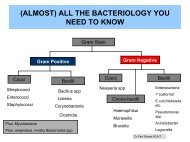
What is <strong>PVL</strong>-Staph?<br />
• Strains of <strong>Staphylococcus</strong> <strong>aureus</strong><br />
producing the toxin Panton Valentine<br />
Leukocidin.<br />
• <strong>PVL</strong> is a toxin which destroys WBCs<br />
• Can be MSSA or MRSA, but to date,<br />
most <strong>PVL</strong>-SA in UK have been MSSA<br />
• Less than 2% of S. <strong>aureus</strong> in England<br />
carry the genetic encoding for <strong>PVL</strong><br />
• Usually community-acquired, although<br />
has spread in hospital setting
Clinical significance<br />
• <strong>PVL</strong> Infections remain uncommon in the UK<br />
• To date, MOST are sensitive to a range of<br />
antibiotics.<br />
• The risk to the UK general public is small,<br />
but the HPA agency is actively raising<br />
awareness of this infection and monitoring<br />
trends - Why?<br />
-Horizon Scanning-
Epidemiology<br />
• Patients often young, previously well<br />
• Majority of <strong>PVL</strong>-SA cause mild skin and<br />
soft tissue <strong>infections</strong><br />
• Rarely, it causes pneumonia, septic<br />
arthritis or bacteraemia in otherwise<br />
healthy young people<br />
• 224 cases of <strong>PVL</strong>- S. <strong>aureus</strong> identified in<br />
England in 2005 (117 MRSA), 496 in 2006<br />
(159 MRSA). 62% were MSSA.<br />
• two recent outbreaks in healthcare settings<br />
• 7 deaths in England & Wales in past 2<br />
years
Internationally<br />
• A major problem has emerged with<br />
CA <strong>PVL</strong> producing MRSA in North<br />
America, the USA300 clone, which is<br />
now spreading within their healthcare<br />
system
HA-MRSA<br />
VS<br />
CA-<strong>PVL</strong> Staph<br />
1. Elderly, debilitated,<br />
critically/chronically ill patients<br />
2. Infections - wounds, devices,<br />
bacteraemia<br />
3. Transmission - within hosp<br />
setting, less in household<br />
contacts<br />
4. Diagnosis - in-patient setting<br />
5. PMH - Prev colonisation,<br />
recent surgery, adm to<br />
hosp/NH, antibiotics, renal<br />
dialysis, indwelling catheter,<br />
skin ulcers, DM<br />
6. Virulence - <strong>PVL</strong> neg,<br />
community spread minimal<br />
7. Limited antibiotic agents<br />
1. Patient often young, healthy,<br />
students, athletes, children,<br />
military personnel<br />
2. Infection - skin, cellulitis,<br />
abscesses, necrotising fasciitis,<br />
Pneumonia<br />
3. Community aquired, spreads in<br />
close contacts in family, sports,<br />
via pets too!!!<br />
4. Diagnosis - minor ssti opd,<br />
serious inf in- patient<br />
5. No PMH<br />
6. Virulence - <strong>PVL</strong> positive, ready<br />
spread in community,<br />
7. More antibiotic susceptibilities
Risk Factors<br />
• Compromised skin integrity<br />
• Skin to skin contact<br />
• Sharing of contaminated items like towels<br />
• CDC - 5 Cs - Contaminated items<br />
Close contact<br />
Crowding<br />
Cleanliness<br />
Cuts<br />
High risk settings - households, gym, military training<br />
camps, prisons, close contact sports
Disease associations<br />
Local<br />
• Skin/soft tissue infection (cellulitis,<br />
abscesses, boils, carbuncles)<br />
Invasive<br />
• Necrotising pneumonia preceded by a<br />
"flu-like” illness<br />
• Bacteraemia<br />
• Necrotising fasciitis<br />
• Osteomyelitis & septic arthritis
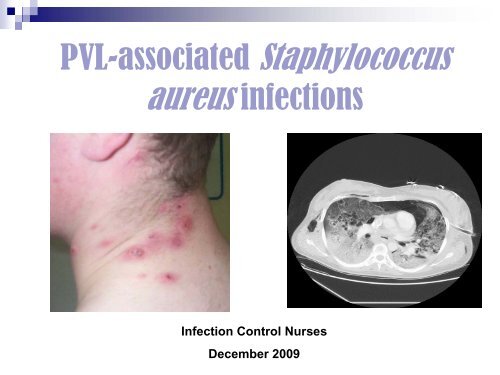
Cavitation<br />
Surgical emphysema<br />
Consolidation
Skin and Soft Tissue<br />
Infections
What do we do about it?<br />
• Clinical management<br />
• Infection control
Clinical Management<br />
Skin and soft tissue <strong>infections</strong><br />
•Minor SSTIs do not need antibiotic treatment unless<br />
immunocompromised,<br />
Incision and drainage is the optimal management for abscesses.<br />
•Moderate SSTIs including cellulitis and larger abscesses should be<br />
treated with oral anti-staphylococcal antibiotics, and drainage.<br />
•If there is systemic involvement suggestive of toxic shock or<br />
pyomyositis, use empirical parenteral antibiotics for MRSA with<br />
immunoglobulin<br />
General care<br />
Lesions should be covered, personal hygiene emphasised (avoid sharing towels,<br />
bath water etc.), and patients advised to return if the lesions do not resolve or<br />
there is clinical deterioration.
Clinical Management of patient with<br />
suspected <strong>PVL</strong>-related pneumonia<br />
CAP hospitalised<br />
– treat with local hospital<br />
severe CAP regimen – cefotaxime/<br />
co-amoxiclav and clarithromycin<br />
Clinical suspicion of<br />
<strong>PVL</strong>–S. <strong>aureus</strong> pneumonia<br />
Admit to ICU<br />
Obtain cultures:<br />
(isolation and masks to be worn<br />
if exposed to respiratory secretions)<br />
- Bronchoalveolar lavage<br />
Protected specimen brush<br />
Tracheal aspirate or sputum<br />
Start empiric antibiotics covering MRSA<br />
- linezolid , clindamycin ,- if<br />
deteriorating , rifampicin
Infection Control
Decolonisation- Community<br />
•Topical decolonisation should be offered to primary<br />
cases. Repeated screening is not recommended unless<br />
the patient is particularly vulnerable to infection, poses<br />
a special risk to others (e.g. a healthcare worker) or<br />
spread of infection is continuing in close contacts.<br />
• Close household contacts of a patient diagnosed with<br />
necrotising pneumonia likely to be caused by <strong>PVL</strong>-SA<br />
should be offered a five-day topical decolonization<br />
regimen
Infection Prevention and Control<br />
in Hospital<br />
“Hospitals should have policies and<br />
procedures which deal with MRSA and these<br />
are generally appropriate for the control of<br />
<strong>PVL</strong>-SA.”<br />
SSTIs - These precautions include:<br />
•isolation in a single room<br />
•use of PPE (plastic apron and gloves)<br />
• meticulous hand hygiene,<br />
•environmental cleaning with Actichlor plus.
Infection Prevention and Control<br />
in Hospital<br />
Necrotising pneumonia<br />
Transmission of <strong>PVL</strong>-SA to staff has occurred following<br />
contact with respiratory secretions (intubation where PPE<br />
was not worn)<br />
Healthcare workers (HCWs) should:<br />
• wear PPE, (face and eye protection) during intubation and<br />
respiratory care<br />
•be screened by occupational health, three to seven days<br />
after any respiratory exposure when not protected by PPE<br />
•report to a physician if symptoms of infection present after<br />
contact with confirmed case
Screening other Patients and Staff<br />
•Should be performed on a risk assessment<br />
basis<br />
•Positive individuals should receive<br />
decolonisation
On a more positive note:<br />
The outcome of a similar case at Wythenshaw<br />
Hospital in Dec 2007<br />
• ECMO in Leicester for 5 days<br />
• Transferred back to Wythenshawe Hospital 28 th Jan 08<br />
• Weaned off ventilator after 32 days<br />
• Discharged to ward 12 th Feb<br />
• Discharged home with baby 22 nd Feb (baby repeatedly<br />
negative on screening)<br />
• Reviewed in clinic 14 th April – well, CXR clear!
Success depended upon:<br />
• Awareness / clinical suspicion<br />
• Early laboratory detection<br />
Microscopy<br />
Culture<br />
Typing<br />
• Appropriate clinical management<br />
• Screening, decolonisation and infection control
Any<br />
Questions?