Dr - LRS Institute of Tuberculosis & Respiratory Diseases
Dr - LRS Institute of Tuberculosis & Respiratory Diseases Dr - LRS Institute of Tuberculosis & Respiratory Diseases
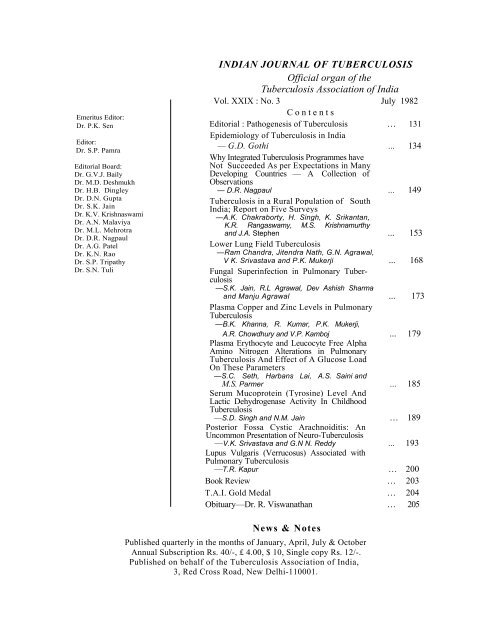
Emeritus Editor: Dr. P.K. Sen Editor: Dr. S.P. Pamra Editorial Board: Dr. G.V.J. Baily Dr. M.D. Deshmukh Dr. H.B. Dingley Dr. D.N. Gupta Dr. S.K. Jain Dr. K.V. Krishnaswami Dr. A.N. Malaviya Dr. M.L. Mehrotra Dr. D.R. Nagpaul Dr. A.G. Patel Dr. K.N. Rao Dr. S.P. Tripathy Dr. S.N. Tuli INDIAN JOURNAL OF TUBERCULOSIS Official organ of the Tuberculosis Association of India Vol. XXIX : No. 3 July 1982 Contents Editorial : Pathogenesis of Tuberculosis … 131 Epidemiology of Tuberculosis in India — G.D. Gothi ... 134 Why Integrated Tuberculosis Programmes have Not Succeeded As per Expectations in Many Developing Countries — A Collection of Observations — D.R. Nagpaul ... 149 Tuberculosis in a Rural Population of South India; Report on Five Surveys —A.K. Chakraborty, H. Singh, K. Srikantan, K.R. Rangaswamy, M.S. Krishnamurthy and J.A. Stephen ... 153 Lower Lung Field Tuberculosis —Ram Chandra, Jitendra Nath, G.N. Agrawal, V K. Srivastava and P.K. Mukerji ... 168 Fungal Superinfection in Pulmonary Tuberculosis —S.K. Jain, R.L Agrawal, Dev Ashish Sharma and Manju Agrawal ... 173 Plasma Copper and Zinc Levels in Pulmonary Tuberculosis —B.K. Khanna, R. Kumar, P.K. Mukerji, A.R. Chowdhury and V.P. Kamboj ... 179 Plasma Erythocyte and Leucocyte Free Alpha Amino Nitrogen Alterations in Pulmonary Tuberculosis And Effect of A Glucose Load On These Parameters —S.C. Seth, Harbans Lai, A.S. Saini and M.S. Parmer ... 185 Serum Mucoprotein (Tyrosine) Level And Lactic Dehydrogenase Activity In Childhood Tuberculosis —S.D. Singh and N.M. Jain … 189 Posterior Fossa Cystic Arachnoiditis: An Uncommon Presentation of Neuro-Tuberculosis —V.K. Srivastava and G.N N. Reddy ... 193 Lupus Vulgaris (Verrucosus) Associated with Pulmonary Tuberculosis —T.R. Kapur … 200 Book Review … 203 T.A.I. Gold Medal … 204 Obituary—Dr. R. Viswanathan … 205 News & Notes Published quarterly in the months of January, April, July & October Annual Subscription Rs. 40/-, £ 4.00, $ 10, Single copy Rs. 12/-. Published on behalf of the Tuberculosis Association of India, 3, Red Cross Road, New Delhi-110001.
- Page 2 and 3: The Indian Journal of Tuberculosis
- Page 4 and 5: The unsolved problems in pathogenes
- Page 6 and 7: EPIDEMIOLOGY OF TUBERCULOSIS IN IND
- Page 8 and 9: EPIDEMIOLOGY OF TUBERCULOSIS IN IND
- Page 10 and 11: EPIDEMIOLOGY OF TUBERCULOSIS IN IND
- Page 12 and 13: EPIDEMIOLOGY OF TUBERCULOSIS IN IND
- Page 14 and 15: EPIDEMIOLOGY OF TUBERCULOSIS IN IND
- Page 16 and 17: EPIDEMIOLOGY OF TUBERCULOSIS IN IND
- Page 18 and 19: EPIDEMIOLOGY OF TUBERCULOSIS IN IND
- Page 20 and 21: WHY INTEGRATED TUBERCULOSIS PROGRAM
- Page 22 and 23: WHY INTEGRATED TUBERCULOSIS PROGRAM
- Page 24 and 25: TUBERCULOSIS IN A RURAL POPULATION
- Page 26 and 27: TUBERCULOSIS IN A RURAL POPULATION
- Page 28: TUBERCULOSIS IN A RURAL POPULATION
- Page 32 and 33: TUBERCULOSIS IN A RURAL POPULATION
- Page 34 and 35: TUBERCULOSIS IN A RURAL POPULATION
- Page 36 and 37: TUBERCULOSIS IN A RURAL POPULATION
- Page 38 and 39: TUBERCULOSIS IN A RURAL POPULATION
- Page 40 and 41: LOWER LUNG FIELD TUBERCULOSIS 169 T
- Page 42 and 43: TABIF IV Radiological nature of les
- Page 44 and 45: FUNGAL SUPERINFECTION IN PULMONARY
- Page 46 and 47: FUNGAL SUPERINFECTION IN PULMONARY
- Page 48 and 49: FUNGAL SUPERINFECTION IN PULMONARY
- Page 50 and 51: PLASMA COPPER AND ZINC LEVELS IN PU
Emeritus Editor:<br />
<strong>Dr</strong>. P.K. Sen<br />
Editor:<br />
<strong>Dr</strong>. S.P. Pamra<br />
Editorial Board:<br />
<strong>Dr</strong>. G.V.J. Baily<br />
<strong>Dr</strong>. M.D. Deshmukh<br />
<strong>Dr</strong>. H.B. Dingley<br />
<strong>Dr</strong>. D.N. Gupta<br />
<strong>Dr</strong>. S.K. Jain<br />
<strong>Dr</strong>. K.V. Krishnaswami<br />
<strong>Dr</strong>. A.N. Malaviya<br />
<strong>Dr</strong>. M.L. Mehrotra<br />
<strong>Dr</strong>. D.R. Nagpaul<br />
<strong>Dr</strong>. A.G. Patel<br />
<strong>Dr</strong>. K.N. Rao<br />
<strong>Dr</strong>. S.P. Tripathy<br />
<strong>Dr</strong>. S.N. Tuli<br />
INDIAN JOURNAL OF TUBERCULOSIS<br />
Official organ <strong>of</strong> the<br />
<strong>Tuberculosis</strong> Association <strong>of</strong> India<br />
Vol. XXIX : No. 3 July 1982<br />
Contents<br />
Editorial : Pathogenesis <strong>of</strong> <strong>Tuberculosis</strong> … 131<br />
Epidemiology <strong>of</strong> <strong>Tuberculosis</strong> in India<br />
— G.D. Gothi ... 134<br />
Why Integrated <strong>Tuberculosis</strong> Programmes have<br />
Not Succeeded As per Expectations in Many<br />
Developing Countries — A Collection <strong>of</strong><br />
Observations<br />
— D.R. Nagpaul ... 149<br />
<strong>Tuberculosis</strong> in a Rural Population <strong>of</strong> South<br />
India; Report on Five Surveys<br />
—A.K. Chakraborty, H. Singh, K. Srikantan,<br />
K.R. Rangaswamy, M.S. Krishnamurthy<br />
and J.A. Stephen ... 153<br />
Lower Lung Field <strong>Tuberculosis</strong><br />
—Ram Chandra, Jitendra Nath, G.N. Agrawal,<br />
V K. Srivastava and P.K. Mukerji ... 168<br />
Fungal Superinfection in Pulmonary <strong>Tuberculosis</strong><br />
—S.K. Jain, R.L Agrawal, Dev Ashish Sharma<br />
and Manju Agrawal ... 173<br />
Plasma Copper and Zinc Levels in Pulmonary<br />
<strong>Tuberculosis</strong><br />
—B.K. Khanna, R. Kumar, P.K. Mukerji,<br />
A.R. Chowdhury and V.P. Kamboj ... 179<br />
Plasma Erythocyte and Leucocyte Free Alpha<br />
Amino Nitrogen Alterations in Pulmonary<br />
<strong>Tuberculosis</strong> And Effect <strong>of</strong> A Glucose Load<br />
On These Parameters<br />
—S.C. Seth, Harbans Lai, A.S. Saini and<br />
M.S. Parmer ... 185<br />
Serum Mucoprotein (Tyrosine) Level And<br />
Lactic Dehydrogenase Activity In Childhood<br />
<strong>Tuberculosis</strong><br />
—S.D. Singh and N.M. Jain … 189<br />
Posterior Fossa Cystic Arachnoiditis: An<br />
Uncommon Presentation <strong>of</strong> Neuro-<strong>Tuberculosis</strong><br />
—V.K. Srivastava and G.N N. Reddy ... 193<br />
Lupus Vulgaris (Verrucosus) Associated with<br />
Pulmonary <strong>Tuberculosis</strong><br />
—T.R. Kapur … 200<br />
Book Review … 203<br />
T.A.I. Gold Medal … 204<br />
Obituary—<strong>Dr</strong>. R. Viswanathan … 205<br />
News & Notes<br />
Published quarterly in the months <strong>of</strong> January, April, July & October<br />
Annual Subscription Rs. 40/-, £ 4.00, $ 10, Single copy Rs. 12/-.<br />
Published on behalf <strong>of</strong> the <strong>Tuberculosis</strong> Association <strong>of</strong> India,<br />
3, Red Cross Road, New Delhi-110001.
The<br />
Indian Journal <strong>of</strong> <strong>Tuberculosis</strong><br />
Vol. XXIX New Delhi, July 1982 No. 3<br />
PATHOGENESIS OF TUBERCULOSIS<br />
Robert Koch, in his famous dissertation announcing the discovery <strong>of</strong><br />
Tubercle Bacillus, said : “<strong>Tuberculosis</strong> has so far been habitually considered<br />
to be a manifestation <strong>of</strong> social misery, and it has been hoped that an improvement<br />
in the latter would reduce the disease. Measures specifically directed<br />
against tuberculosis are not known to preventive medicine. But in the future<br />
the fight against this terrible plague <strong>of</strong> mankind will deal no longer with an<br />
undetermined something, but with a tangible parasite, whose living conditions<br />
are, for the most part, known and can be investigated further”. Robert Koch’s<br />
pronouncement presaged a complete break from the past thinking and suggested<br />
an entirely new direction towards the control <strong>of</strong> tuberculosis. However,<br />
subsequent observations showed that even Robert Koch was not completely<br />
correct and his prophesy was the result <strong>of</strong> dogmatism and over-enthusiasm.<br />
Nageli and, subsequently, Opie and Ghon showed the presence <strong>of</strong> obsolete<br />
tuberculous lesions at autopsy in persons who had never suffered from tuberculosis<br />
in their life time. What is more important, many <strong>of</strong> these<br />
lesions contained viable tubercle bacilli. In other words, infection and<br />
mere presence <strong>of</strong> the aetiological agent in the tissues <strong>of</strong> the host is not<br />
sufficient per se to determine the development <strong>of</strong> manifest disease. A<br />
question naturally arises - why do only some <strong>of</strong> the enormous number<br />
<strong>of</strong> infected individuals develop the disease ? What are the factors which influence<br />
the development <strong>of</strong> disease, once infection has taken place ? Could it be<br />
that the very factors which Robert Koch decried are the factors which decide<br />
whether infection will go on to disease or not?<br />
The association <strong>of</strong> heredity and tuberculosis has been the subject <strong>of</strong> discussion<br />
for ages. We may not believe that one inherits tuberculosis but one<br />
also cannot deny that heredity can and does influence resistance against disease.<br />
Hill’s hypothesis <strong>of</strong> the speed <strong>of</strong> reaction is merely old wine served in a<br />
new bottle. It does not elucidate at all as to what makes the body react and<br />
what determines the speed <strong>of</strong> reaction.<br />
Knowledge regarding the mechanism through which the natural resistance<br />
operates and factors which augment or depress this is crucial but unfortunately<br />
still lacking. It has been hypothesised that the degree <strong>of</strong> natural resistance<br />
is dependent in part on ability to develop acquired resistance. But then,<br />
why does primary infection itself heal and the subsequent re-infection some<br />
times progress to disease inspite <strong>of</strong> the natural resistance being further<br />
augmented by acquired resistance ?<br />
Ind. J. Tub., Vol. XXIX, No, 3
132<br />
The increased susceptibility <strong>of</strong> household contacts <strong>of</strong> an open case <strong>of</strong><br />
tuberculosis is well-known and attributed to one or other <strong>of</strong> the three factors<br />
viz. intensity <strong>of</strong> exposure, heredity, adverse environmental factors. Seemingly<br />
valid arguments can be adduced for and against each <strong>of</strong> these factors.<br />
Inherent ability <strong>of</strong> an individual to maintain resistance at a high level may<br />
be, and very probably is, governed in part by heredity but the maintenance <strong>of</strong><br />
a satisfactory degree <strong>of</strong> resistance is also influenced by many environmental<br />
factors. The influence <strong>of</strong> ‘psyche’ is being increasingly incriminated in the<br />
problems <strong>of</strong> ‘soma’. But, whether a given unfavourable factor actually depresses<br />
the mechanism <strong>of</strong> natural resistance or whether the mechanism remains unaltered<br />
but conditions are introduced which thwart it or prevent it from functioning<br />
effectively is, <strong>of</strong> course, not known. Since many <strong>of</strong> these factors which influence<br />
the outcome <strong>of</strong> infection are intangible, the fate <strong>of</strong> the individual remains<br />
unpredictable.<br />
Mode <strong>of</strong> reinfection is another moot point in pathogenesis. It is common<br />
knowledge that most <strong>of</strong> the progressive pulmonary disease is not the<br />
direct result <strong>of</strong> primary infection but follows re-infection, sometimes many<br />
years after the primary infection. Is reinfection endogenous or exogenous ?<br />
Arguments for and against both have been many and fascinating. Consensus<br />
appears to be in favour <strong>of</strong> endogenous reinfection being more likely<br />
and more plausible though it cannot be proved that exogenous reinfection<br />
is not possible. This controversy is not merely an exercise in intellectual<br />
polemics without any practical implication. Prevention <strong>of</strong> tuberculosis does<br />
seem to be linked with this problem. If endogenous reinfection was the only<br />
mode, isolation <strong>of</strong> an open case from individuals already infected is meaningless.<br />
If on the other hand, exogenous reinfection is possible, then isolation<br />
from both infected and uninfected is imperative.<br />
Endogenous reinfection is also linked with the problem <strong>of</strong> dormant bacilli.<br />
What makes the bacilli dormant ? Our knowledge in respect <strong>of</strong> growth requirements<br />
<strong>of</strong> the bacillus and its metabolism is still limited. Is dormancy governed<br />
by some inherent and intrinsic character <strong>of</strong> the bacillus or is it in response<br />
to some altered state <strong>of</strong> the tissues in which the bacilli are lodged ? We are<br />
still ignorant about the mechanism which triggers dormancy and subsequent reanimation.<br />
A substance called “Hibernation Induction Trigger” has been<br />
isolated from the blood <strong>of</strong> hibernating animals. Could it that some such<br />
substance is involved in dormancy <strong>of</strong> the tubercle bacillus also ?<br />
The importance <strong>of</strong> the dormant bacillus is not merely because <strong>of</strong> its role<br />
in reinfection and relapse but also because <strong>of</strong> its influence on epidemiology.<br />
When tuberculosis started declining rapidly in the western countries, the high<br />
priests <strong>of</strong> epidemiology prophesied that eradication <strong>of</strong> tuberculosis was imminent.<br />
Their optimism was more wishful than rational. As long as there is but<br />
one human being in the world who has but one dormant bacillus inside his<br />
body, he can generate, at least theoretically, a new epidemic <strong>of</strong> tuberculosis<br />
even if the previous one had completely died out. This has been corroborated<br />
by a number <strong>of</strong> small localised epidemics that have occurred recently in developed<br />
countries where tuberculosis has declined tremendously.<br />
Ind. J. Tub., Vol. XXIX, No. 3
The unsolved problems in pathogenesis <strong>of</strong> tuberculosis are many and<br />
varied. Rich summarised the position admirably in 1951. What passed for<br />
knowledge about pathogenesis was more a matter <strong>of</strong> belief based on reasoning<br />
from analogy rather than a conviction based on valid statistical and scientific<br />
pro<strong>of</strong>. And there the matter rests even today!<br />
133<br />
Ind. J. Tub., Vol. XXIX, No. 3
REVIEW ARTICLE<br />
EPIDEMIOLOGY OF TUBERCULOSIS IN INDIA<br />
<strong>Tuberculosis</strong> is known to have existed in<br />
India since ancient times and has been mentioned<br />
in classical literature including Ayurvedic<br />
Samhitas. However, quantitative information<br />
about its epidemiology has become available<br />
only in the last half century. Unlike western<br />
countries, where a more or less efficient notification<br />
system has existed for a long time,<br />
India has been lacking in even approximate<br />
data about the prevalence and incidence <strong>of</strong><br />
tuberculous infection and disease as well as<br />
mortality rates. One <strong>of</strong> the earliest <strong>of</strong>ficial<br />
documents in which data regarding tuberculosis<br />
have been given is the Bhore Commission<br />
Report, 1946. The general impression at that<br />
time was that tuberculosis was mainly an urban<br />
problem and that younger persons, specially<br />
females, were more prone to it than others.<br />
Although the relevant facts regarding the<br />
present day epidemiology <strong>of</strong> tuberculosis in<br />
India have not yet been fully elucidated, a<br />
considerable amount <strong>of</strong> information, <strong>of</strong> varying<br />
degrees <strong>of</strong> reliability and accuracy, has accumulated<br />
during the course <strong>of</strong> the last 30 or 40<br />
years enabling us to see at least the outlines <strong>of</strong><br />
the problem and furnishing the basis for future<br />
action.<br />
As is well known, infection and disease are<br />
not synonymous in tuberculosis. We have, thus,<br />
two parameters to consider, both interdependent,<br />
even though the extent <strong>of</strong> interdependence<br />
is itself an enigma.<br />
Prevalence <strong>of</strong> tuberculous infection<br />
Prevalence <strong>of</strong> infection is measured by the<br />
proportion <strong>of</strong> tuberculin reactors in the total<br />
population at any point <strong>of</strong> time and is usually<br />
expressed as a percentage. However, in the<br />
absence <strong>of</strong> a well defined test, available information<br />
on this point is highly variable. Because<br />
<strong>of</strong> the use <strong>of</strong> different types <strong>of</strong> tuberculins,<br />
different dosages and methods <strong>of</strong> testing,<br />
considerable variations in the reading <strong>of</strong> reactions<br />
by different workers, imprecise knowledge<br />
about the exact size <strong>of</strong> tuberculin induration<br />
that should be regarded as evidence <strong>of</strong><br />
tubercular infection, the possibility <strong>of</strong> a boosting<br />
effect due to earlier tuberculin testing and the<br />
prevalence <strong>of</strong> non-specific tuberculin sensitivity<br />
in some areas, the interpretation <strong>of</strong> tuberculin<br />
G.D. GOTHI*<br />
test reactions is a highly complex job. In view<br />
<strong>of</strong> these limitations, it is not possible to compare<br />
infection rates reported from time to time by<br />
different workers from different areas. A review<br />
<strong>of</strong> literature reveals that, unaware <strong>of</strong> the limitations<br />
<strong>of</strong> the test, different workers have used<br />
different strengths and types <strong>of</strong> tuberculin and<br />
arbitrarily set critical values for separating<br />
tuberculin reactors and non-reactors.<br />
The earliest report on prevalence <strong>of</strong> infection<br />
in India is by Ukil (1930) who found 11%<br />
tuberculin reactors in the 0 to 4 age group and<br />
75% among persons aged 10 years or more in<br />
a survey carried out in areas <strong>of</strong> Bengal, Bihar,<br />
Assam and Madras. The observed rates were<br />
much higher -in the urban areas. Benjamin<br />
(1938-39), surveying a sample population in<br />
the rural and urban areas <strong>of</strong> Chittoor district<br />
and in Saidapet (in the suburbs <strong>of</strong> Madras),<br />
made similar observations although, contrary<br />
to the then current general impression, he<br />
concluded that villages were not free from tuberculous<br />
infection. Rist and Rose (1938) carried<br />
out a survey among Muslim girls in Ludhiana,<br />
Ilahi Baksh (1939) in the rural population <strong>of</strong><br />
Jullunder and Rao and Cochran (1943) repeated<br />
a tuberculin survey in Saidapet. All<br />
these reported a high prevalence <strong>of</strong> infection<br />
in towns, semi-urban areas and villages. High<br />
infection rates were also reported by Frimodt-<br />
Moller (1949) in Madanapalle town and surrounding<br />
rural areas.<br />
More extensive data regarding infection<br />
rates became available as a by-product <strong>of</strong> the<br />
mass BCG vaccination campaign undertaken<br />
by the Government <strong>of</strong> India. Analysis <strong>of</strong> data<br />
showed a high prevalence <strong>of</strong> infection even at<br />
the young age <strong>of</strong> 5 years in West Bengal,<br />
Bombay and Uttar Pradesh. The tuberculin<br />
reactor rates at this age in the three states were<br />
23.0%, 32.2% and 27.4% respectively for<br />
males and 21.5%, 32.2%’ and 22.8% for<br />
females. It was found that by the age <strong>of</strong> 10,<br />
more than half the males and over 45 % <strong>of</strong> the<br />
females had already been infected. In the hilly<br />
regions, half the population was infected by the<br />
age <strong>of</strong> 15 years as against the age <strong>of</strong> 10 years<br />
in the plains. Infection rates in the industrial<br />
towns were higher than elsewhere, 50% level<br />
<strong>of</strong> infection having been reached before the<br />
age <strong>of</strong> 10 years.<br />
*Director, New Delhi <strong>Tuberculosis</strong> Centre, Jawahar Lai Nehru Marg, New Delhi-110002.<br />
Ind. J. Tub., Vol. XXIX, No. 3
EPIDEMIOLOGY OF TUBERCULOSIS IN INDIA 135<br />
Several other studies carried out at the same<br />
time (Sikand and Raj Narain, 1952 in Faridabad<br />
township, Hertzberg, 1952 in Trivandrum city<br />
and Frimodt-Moller in Madanapalle town and<br />
surrounding villages) also revealed a very high<br />
rate <strong>of</strong> tuberculintzation. Frimodt-Moller (I960)<br />
carried out a large scale tuberculin survey<br />
among a population living within 10 miles<br />
radius <strong>of</strong> Madanapalle. Using 5 TU PPD<br />
(XIX, XX and XXI with a reaction <strong>of</strong> 10 mm<br />
or more taken as an evidence <strong>of</strong> infection),<br />
he found that at the ages <strong>of</strong> 10 years, 20 years<br />
and 30 years, the infection rates were 10%,<br />
21% and 31% respectively. Using 1 TU and<br />
considering an induration <strong>of</strong> 6 mm or more as<br />
an evidence <strong>of</strong> infection the rates at the same<br />
ages were slightly lower.<br />
Considering a reaction <strong>of</strong> 10 mm or more<br />
to 1 TU PPD RT 23 with tween 80 as positive,<br />
Raj Narain et al (1963) found an overall infection<br />
rate <strong>of</strong> 38.3% in a sample population<br />
<strong>of</strong> Tumkur district (42.8% among males and<br />
33.9% among females). Infection rates in the<br />
rural and semi-rural areas were 37.9% and<br />
43.9% respectively. The overall prevalence <strong>of</strong><br />
infection in 119 villages <strong>of</strong> Bangalore district<br />
(based on the same tuberculin and reaction<br />
as above) was found to be 30% (35% among<br />
males and 25% among females) (National<br />
<strong>Tuberculosis</strong> <strong>Institute</strong> (NTI), 1974). The infection<br />
rates for both sexes increased with<br />
age upto ‘45 to 54 years’ (66% to 72% for<br />
males, 47% to 50% for females). The rate <strong>of</strong><br />
increase in females, unlike males, slowed down<br />
after the age <strong>of</strong> 15 years. Repeated tuberculin<br />
testing <strong>of</strong> the same population at intervals <strong>of</strong><br />
1-1/2 years to 2 years did not show any change<br />
over a period <strong>of</strong> 5 years. In a recently conducted<br />
study in Chingleput district <strong>of</strong> Tamil Nadu,<br />
<strong>Tuberculosis</strong> Prevention Trial (TPT, 1980),<br />
using 3 TU <strong>of</strong> PPD-S and considering an<br />
induration <strong>of</strong> 12 mm or more as evidence <strong>of</strong><br />
infection, reported an overall prevalence rate<br />
<strong>of</strong> infection <strong>of</strong> 50% (males 54%; females 46%).<br />
Among males, the infection rate rose rapidly<br />
upto the age <strong>of</strong> 25 years (reaching 80 %) whereas<br />
in females the rise continued upto 35 years<br />
(reaching 70%). In both sexes the rate levelled<br />
<strong>of</strong>f after the peak had been reached. In the<br />
Kashmir valley, infection rates were found to<br />
be considerably lower than, say, in the south<br />
Indian states <strong>of</strong> Karnataka and Tamil Nadu.<br />
(Unpublished material 1980).<br />
In Tumkur survey, the prevalence rates <strong>of</strong><br />
infection in the age groups 0 to 4 years, 5 to 9<br />
years and 10 to 14 years were 2.7%, 5.5% &<br />
25.4% respectively (Raj Narain, 1963). Gothi<br />
et al (1979) found nearly the same rates among<br />
children and adolescents in the same population<br />
after 12 years.<br />
Udani (1968) reported a prevalence rate <strong>of</strong><br />
4.7% in the age group 0 to 6 years on the west<br />
coast. In the semi-urban areas <strong>of</strong> Delhi the<br />
rate was 4.6% (Dingley, 1979) in the age group<br />
0 to 4 years but among school children (5 to<br />
14 years) in the city, the figure was 40.7%<br />
(Singh, 1960). Figures for school children<br />
<strong>of</strong> Nagpur were reported as 24.4% by Majumdar<br />
(1960). At the age <strong>of</strong> 15 years, Benjamin<br />
(1951) found the lowest infection rates in<br />
Assam (51% among males and 36% among<br />
females) and the highest in U.P. (males 75%,<br />
females 74%). In the <strong>Tuberculosis</strong> Prevention<br />
Trial (1980), the rates for age groups 1 to 4<br />
years, 5 to 9 years and 10 to 14 years were<br />
4.9%, 7.9% and 16.5% respectively, males in<br />
general showing a higher prevalence than<br />
females. Krishnaswami (1978) reporting on the<br />
urban slums <strong>of</strong> Madras found a very high<br />
rate <strong>of</strong> infection for children below 5 years.<br />
In another congested urban areas <strong>of</strong> Madras,<br />
Narmada et al (1973) reported rate <strong>of</strong> 7.3%<br />
in the 0 to 4 years age group.<br />
Although data available from various<br />
sources are not strictly comparable, nevertheless,<br />
there are some common features viz. (i) infection<br />
rates increase with age and are higher in males<br />
than in females (ii) the difference can probably<br />
be explained by the fact that males in general<br />
lead a more active life and mix with people in<br />
a much wider circle, thus coming across more<br />
chances <strong>of</strong> acquiring infection, (iii) infection<br />
rates, in general, are more or less the same in<br />
urban and rural areas, although they are somewhat<br />
higher in congested urban areas and<br />
industrial towns.<br />
Incidence <strong>of</strong> infection<br />
The conventional method <strong>of</strong> estimating the<br />
incidence <strong>of</strong> infection is by repeated tuberculin<br />
testing <strong>of</strong> the population. Persons classified as<br />
non-reactors at an earlier tuberculin testing who<br />
become reactors at a subsequent testing can be<br />
considered to have acquired tuberculous infection<br />
in the intervening period and incidence<br />
<strong>of</strong> infection is calculated per annum by expressing<br />
the latter as a percentage <strong>of</strong> the former.<br />
Several attempts have been made, mostly in<br />
south Indian states, to estimate the incidence<br />
<strong>of</strong> infection.<br />
Bogen (1957) used age specific prevalence<br />
rates <strong>of</strong> infection for his estimate <strong>of</strong> 5.3 % per<br />
year for all ages. Using similar data, Frimodt-<br />
Moller (1960) estimated the annual incidence<br />
<strong>of</strong> infection as lying between 4.7% and 6.2%<br />
for different ages and Raj Narain et al (1963)<br />
between 0.9% to 2.4%. Partly these differences<br />
may be accounted for by different standards<br />
Ind. J. Tub., Vol. XXIX, No. 3
136 G.D. GOTHI<br />
adopted for judging tuberculin positivity.<br />
Frimodt-Moller (1960), however, also gave a<br />
different estimate <strong>of</strong> the incidence <strong>of</strong> infection<br />
(2%) per year by direct observation i.e. after<br />
repeated tuberculin testing at intervals <strong>of</strong> 2-1/2<br />
years. Narmada et al (1977) reported 3%<br />
annual incidence <strong>of</strong> infection in 0-12 years age<br />
group.<br />
Serious doubts about the validity <strong>of</strong> the<br />
studies mentioned above arose as a result <strong>of</strong><br />
the findings <strong>of</strong> Raj Narain et al (1965) wherein<br />
they proved that a previous tuberculin test<br />
boosts the induration <strong>of</strong> any subsequent tuberculin<br />
test reaction. Also, it was found that the<br />
prevalence <strong>of</strong> non-specific sensitivity (Frimodt-<br />
Moller 1960; Raj Narain et al 1965-72; Chakraborty<br />
et al 1976) may interfere with the<br />
estimation <strong>of</strong> the incidence <strong>of</strong> infection. Raj<br />
Narain (1966) found a method for overcoming<br />
this difficulty and suggested a new approach for<br />
identifying the newly infected persons. By<br />
this method Raj Narain (1965) and Gothi et al<br />
(1972) estimated the incidence in the age group<br />
‘0 to 4’ years at 0.9 % per year and for the age<br />
groups ‘5-9’ years and ‘10-14’ years, 1.4% and<br />
2.1% respectively. National <strong>Tuberculosis</strong> <strong>Institute</strong><br />
(NT1-1974), using the same method reported<br />
that the average annual incidence <strong>of</strong><br />
infection for all ages was 1 %, that for the age<br />
group ‘0 to 4’ years being 0.8%. The incidence<br />
rates increased with age. For the age group<br />
‘35 years and above’ the figure varied from<br />
1.3% to 3.16% during three periods. Adopting<br />
the same method <strong>of</strong> calculation, TPT (1980)<br />
found a much higher annual incidence <strong>of</strong> infection,<br />
3%, 4% and 6% per year for the age<br />
groups ‘1 to 4’ years, ‘5 to 9’ years and ‘10<br />
to 14’ years, respectively. A plausible reason<br />
for such differences could be the considerable<br />
difference in the prevalence <strong>of</strong> bacillary disease<br />
in the two areas (4 per 1000 in the NTI study<br />
area and 11 per 1000 in the TPT area).<br />
<strong>Tuberculosis</strong> Morbidity<br />
Two principal indices are generally used<br />
to measure tuberculosis morbidity in any<br />
community, the prevalence <strong>of</strong> active disease and<br />
fresh incidence <strong>of</strong> disease among previously<br />
healthy persons. As in the case <strong>of</strong> studies<br />
relating to infection, there is a considerable<br />
paucity <strong>of</strong> data in respect <strong>of</strong> tuberculosis morbidity<br />
in India and in practically all developing<br />
countries. In western countries, tuberculosis<br />
has been a notifiable disease for a long time<br />
and the system works fairly efficiently. As such,<br />
some data (more or less precise, depending on<br />
the efficiency <strong>of</strong> the notification system in any<br />
particular country) relating to the prevalence<br />
and incidence <strong>of</strong> disease have been available<br />
Ind. J. Tub., Vol. XXIX, No. 3<br />
for a long time, even though these statistics are<br />
based only on ‘known’ cases. Although these<br />
data do not take into account the undetected,<br />
asymptomatic cases <strong>of</strong> tuberculosis, nevertheless<br />
they provide very valuable information<br />
about TB morbidity and trends in the community.<br />
For several decades, these were the<br />
only statistics available even in the western<br />
countries for evaluating the tuberculosis problem.<br />
In India, on the other hand, practically no<br />
reliable data, were available till the early fifties<br />
about the prevalence or incidence <strong>of</strong> tuberculosis.<br />
One <strong>of</strong> the earliest estimates made by<br />
Benjamin (1945), based on findings <strong>of</strong> a small<br />
scale survey in the suburbs <strong>of</strong> Madras city,<br />
and certain other observations, placed the total<br />
number <strong>of</strong> active TB cases in the country at<br />
about 25 lakhs, the estimated total TB mortality<br />
in a year being <strong>of</strong> the order <strong>of</strong> 5 lakhs (Bhore<br />
Commission Report, 1946).<br />
It was only in the early 1950s that, with the<br />
availability <strong>of</strong> mobile mass miniature radiographic<br />
facilities, one acquired the means for<br />
evaluating the tuberculosis problem by carrying<br />
out surveys in various groups. In the last 30<br />
years, a number <strong>of</strong> surveys (some in representative<br />
community groups and others in selected<br />
groups) have been carried out and although<br />
data available are still not sufficient, considering<br />
the size <strong>of</strong> the country, they provide a<br />
useful basis for planning tuberculosis control<br />
strategies.<br />
It must not be presumed, however, that<br />
with the availability <strong>of</strong> mass radiography and<br />
sputum examination (the main tools employed<br />
for tuberculosis morbidity surveys) all problems<br />
relating to estimation <strong>of</strong> TB morbidity have<br />
been solved. Both chest radiography and<br />
bacteriological examination have their limitations.<br />
In addition, the diagnostic problems <strong>of</strong><br />
tuberculosis are so complicated that no two<br />
studies are, strictly speaking, comparable and<br />
for that reason it is not possible to make any<br />
general statement about the country as a whole<br />
by taking into account the various studies<br />
carried out in different regions. It would be<br />
useful at the outset to consider all these limitations<br />
to serve as caveat before drawing any<br />
rash and possibly unjustified conclusions from<br />
the various studies carried out at different<br />
centres.<br />
The first difficulty arises from limitations <strong>of</strong><br />
the two principal diagnostic tools viz. radiography<br />
and bacteriological examination. Radiological<br />
assessment <strong>of</strong> chest shadows, as is well<br />
known, is highly subjective and is influenced
EPIDEMIOLOGY OF TUBERCULOSIS IN INDIA 137<br />
by the competence <strong>of</strong> the x-ray reader and his<br />
impression about the prevalence <strong>of</strong> other<br />
pulmonary diseases in the region concerned.<br />
A number <strong>of</strong> studies have brought out the<br />
extent <strong>of</strong> ‘reader variations’, both intra-individual<br />
and inter-individual, in intrepretation<br />
<strong>of</strong> chest x-rays (Yerushalmy et al 1950, Sikand<br />
et al 1962, Raj Narain et al 1962, Karan 1962,<br />
Gothi et al 1974). An additional difficulty in<br />
large scale surveys is that usually it is not<br />
possible to have anything more than a single<br />
miniature film to decide the aetiology and<br />
activity <strong>of</strong> abnormal shadows. This is <strong>of</strong>ten<br />
not an adequate basis on which to arrive at a<br />
conclusive diagnosis. A number <strong>of</strong> procedures<br />
for radiological assessment <strong>of</strong> miniature films<br />
have been evaluated empirically and the system<br />
commonly followed in the better planned<br />
studies, nowadays, is to have two independent<br />
assessments by two readers with a third ‘umpire’<br />
reading by another reader to settle the<br />
differences between the first two. It has been<br />
found after experimentation that this procedure<br />
is fairly adequate for minimizing errors <strong>of</strong><br />
both under-reading and over-reading.<br />
In well planned surveys, all persons with<br />
abnormal chest x-rays are subjected to a set <strong>of</strong><br />
bacteriological examinations. The fact that<br />
intensity <strong>of</strong> such bacteriological examinations<br />
varies from place to place and from time to<br />
time is an additional factor which makes it<br />
difficult to compare or combine results <strong>of</strong><br />
studies carried out at different centres. Many<br />
centres lacking culture facilities have perforce no<br />
option but to depend entirely on direct<br />
microscopy <strong>of</strong> sputum. Some carry out both<br />
direct smear and culture examination <strong>of</strong> a<br />
single specimen. Some others are in the fortunate<br />
position <strong>of</strong> being able to examine more than one<br />
specimen at different intervals <strong>of</strong> time and<br />
sometimes even repeat the chest x-ray, if<br />
indicated. It is natural in this situation that the<br />
final assessments would lack comparability. An<br />
idea <strong>of</strong> how much difference this would make<br />
can be had from the study <strong>of</strong> Chandra-sekhar et<br />
al (1970) wherein it was shown that if 4<br />
bacteriological specimens were examined in a<br />
survey, nearly 25% <strong>of</strong> the bacillary cases were<br />
added by the third and fourth specimens. Nair et al<br />
(19761 have also shown that the rate <strong>of</strong> bacillary<br />
disease increased by an additional , 39 % if eight<br />
specimens were examined instead <strong>of</strong> two. It is<br />
thus obvious that unless suitable ‘corrections’<br />
are made, data obtained from one study would<br />
not be directly comparable with any other study<br />
with a different intensity <strong>of</strong> bacteriological<br />
examination.<br />
Further problems arise because <strong>of</strong> the fact<br />
that there is no commonly agreed definition <strong>of</strong><br />
pulmonary tuberculosis (Raj Narain, 1968).<br />
Except for bacteriologically proved cases, there<br />
is always an element <strong>of</strong> doubt about cases<br />
adjudged tuberculous merely on radiological<br />
basis. To overcome this difficulty and to provide<br />
a sort <strong>of</strong> lowest common denominator, the<br />
WHO Expert Committee in its VIIIth Report<br />
(1964) recommended that only sputum positive<br />
patients should be considered as ‘cases’ <strong>of</strong> tuberculosis<br />
and all others labelled as ‘suspects’.<br />
This definition too is not, however, free from<br />
faults. Bacteriological diagnosis, although highly<br />
specific, is not sensitive enough and it is well<br />
known that a large proportion <strong>of</strong> tuberculosis<br />
patients with minimal disease are bacteriologically<br />
negative to start with. This, besides the<br />
difficulties enumerated earlier, detracts somewhat<br />
from evaluation <strong>of</strong> tuberculosis problem<br />
based only on bacteriological confirmation <strong>of</strong><br />
diagnosis.<br />
So far as the prevalence rates are concerned, a<br />
certain comparability can be achieved between<br />
various studies by comparing the rate <strong>of</strong> bacillary<br />
disease. Where estimation <strong>of</strong> incidence<br />
rates among previously healthy persons is<br />
concerned, a further difficulty arises. Since<br />
there is no agreed definition <strong>of</strong> a tuberculosis<br />
case, it follows that there is no agreed definition<br />
<strong>of</strong> a non-case. In a longitudinal study, in which<br />
prevalence <strong>of</strong> only bacteriologically confirmed<br />
disease at the first survey has been calculated,<br />
the remaining population including bacteriologically<br />
unproved but radiologically active<br />
patients, persons with inactive disease and<br />
those with clear chest x-ray would form the<br />
denominator (population at risk) for calculation<br />
to further incidence. In another study in which<br />
prevalence is calculated on the basis <strong>of</strong> radiological<br />
and/or bacteriological evidence, the<br />
people at risk which would form the denominator<br />
for calculation <strong>of</strong> incidence would be<br />
only persons with a clear chest x-ray. Since the<br />
attack rate in the two types <strong>of</strong> ‘non-cases’ in<br />
the two studies is likely to be different, it is<br />
obvious that incidence rates would also not be<br />
comparable.<br />
Inspite <strong>of</strong> the difficulties and handicaps<br />
mentioned above, surveys based on examination<br />
by various procedures and techniques<br />
have contributed valuable fundamental knowledge<br />
about tuberculosis morbidity in the<br />
country.<br />
Prevalence <strong>of</strong> disease<br />
Prevalence is defined as the number <strong>of</strong><br />
patients at a given point <strong>of</strong> time and is expressed<br />
either in absolute numbers or as a<br />
rate per 1,000 or per 100,000 <strong>of</strong> population.<br />
Ind. J. Tub., Vol. XXIX, No. 3
138 G.D. GOTHI<br />
Prior to 1950 only a few small scale surveys<br />
were carried out in some parts <strong>of</strong> the country<br />
to ascertain prevalence <strong>of</strong> tuberculosis. Benjamin<br />
et al (1939) surveyed a population <strong>of</strong> 3,309 in<br />
Saidapet, a suburb <strong>of</strong> Madras. Persons having<br />
a strongly positive tuberculin test reaction or<br />
having suspicious symptoms were physically<br />
examined and 241 out <strong>of</strong> these were picked up<br />
for x-ray. The disease prevalence thus estimated<br />
was 2.3%. Another survey (Lai et al, 1943)<br />
carried out in an urban population at Serampore<br />
in Bengal showed a morbidity prevalence <strong>of</strong><br />
7% <strong>of</strong> which sputum positive disease accounted<br />
for 3%. In both these surveys, because <strong>of</strong><br />
meagre x-ray facilities, only a small adult<br />
population was examined. It is easy to see that<br />
the figures do not reflect the correct tuberculosis<br />
prevalence even for the limited areas covered.<br />
Mobile miniature radiography was first<br />
used by Aspin in 1945 to survey Gurkha recruits<br />
for the Army and labour units. All those<br />
examined were aged 18 years or more. In<br />
Gurkha recruits the prevalence <strong>of</strong> tuberculosis<br />
was found to be 1 % and among labour recruits<br />
3.4%. Obviously, these figures cannot be considered<br />
representative. Besides the fact that<br />
they were all adults, recruits presenting themselves<br />
for appointment in the Army were<br />
expected to be healthier than the community<br />
to which they belonged. In 1947, Frimodt-<br />
Moller surveyed a population <strong>of</strong> 10,000 in<br />
Madanapalle town and reported a prevalence<br />
<strong>of</strong> 0.7% bacillary disease. This figure was<br />
confirmed by a series <strong>of</strong> 5 longitudinal surveys<br />
carried out by Frimodt-Moller in the same area<br />
between 1950 and 1955 in which the population<br />
studied was about 60,000. In 1951. the New<br />
Delhi TB Centre surveyed Faridabad township<br />
(housing displaced population) and found<br />
active disease prevalence rate <strong>of</strong> 13.6 per 1000<br />
among persons aged 5 years or more (Sikand<br />
and Raj Narain, 1952). Other surveys carried<br />
out about the same time in selected groups at<br />
Madras and Trivandrum were reported by<br />
Phillips (1952) and Hertzberg (1952). These<br />
were the best available data on the subject till<br />
about 1954-55. On the basis <strong>of</strong> personal impressions<br />
and limited data obtained from<br />
surveys, the general belief about this .time was<br />
that tuberculosis was commoner among younger<br />
people rather than the aged, females rather than<br />
males, and cities and towns rather than villages.<br />
Studies carried out during last 30 years have<br />
disproved these beliefs. The first doubt about<br />
these hypotheses arose from the data obtained<br />
as a by-product <strong>of</strong> the mass BCG programme<br />
carried out throughout the country starting in<br />
1951. Tuberculin testing <strong>of</strong> the rural population<br />
revealed an unexpectedly high prevalence <strong>of</strong><br />
tuberculous infection in the villages (Benjamin,<br />
1951) suggesting the probability <strong>of</strong> a substantially<br />
high prevalence <strong>of</strong> tuberculosis in the<br />
rural areas as well.<br />
To verify this impression, the Indian Council<br />
<strong>of</strong> Medical Research (1959) organized a large<br />
scale Sample Survey to assess the tuberculosis<br />
situation in urban, semi-urban and rural areas<br />
in various parts <strong>of</strong> the country during 1955-57.<br />
The survey was carried out in 6 zones <strong>of</strong> the<br />
country and covered a sample <strong>of</strong> nearly 300,000<br />
persons aged 5 years or more. All persons<br />
included in the sample were <strong>of</strong>fered mass miniature<br />
radiography. Sputa <strong>of</strong> persons with<br />
abnormal chest shadows were examined by<br />
direct microscopy and by culture. The main<br />
findings <strong>of</strong> the survey were (i) the rate <strong>of</strong><br />
radiologically active pulmonary tuberculosis<br />
varied from 13.5 to 26.6 per 1,000 population<br />
in different zones and within each zone from<br />
cities to small towns and rural areas, (ii) the<br />
prevalence <strong>of</strong> bacillary disease varied from<br />
2.4 to 8.2 per 1,000 (iii) prevalence <strong>of</strong> disease<br />
in rural areas did not differ significantly from<br />
the urban areas, (iv) prevalence <strong>of</strong> disease<br />
showed a continuous rise with age in both<br />
sexes but for females there was a decline from<br />
the age <strong>of</strong> 45 years onwards. Nearly 2/3rd <strong>of</strong><br />
the total disease was in males. Villages accounted<br />
for nearly 80 % <strong>of</strong> the total cases (the same<br />
proportion as the rural population bore to the<br />
total population).<br />
Further information about prevalence rates<br />
is available from longitudinal studies carried<br />
out in Delhi, Bangalore, Madanapalle and<br />
Chingleput. The surveys in Delhi and Madanapalle<br />
(the former in an urban and the latter in<br />
a rural areas) confirmed the findings regarding<br />
prevalence rates obtained from the earlier ICMR<br />
survey. In the Delhi study, carried out in a<br />
congested old city area and covering a population<br />
<strong>of</strong> about 30,000, the prevalence was<br />
found to be 13.2 per 1,000 (bacillary : 4 per<br />
1.000). It is interesting to note that in the Delhi<br />
survey the rate <strong>of</strong> bacillary disease in the 6<br />
surveys carried out from 1962 to 1977 varied<br />
from 2.1 to 4 per 1,000. Tumkur survey (Raj<br />
Narain et al 1963) carried out in a rural population<br />
<strong>of</strong> 36,000 showed an overall prevalence<br />
<strong>of</strong> 19 active cases per 1,000, <strong>of</strong> which 4 per<br />
1,000 were bacillary. The NTI (1974) found<br />
practically uniform rate <strong>of</strong> bacillary disease<br />
(3 to 4 per 1,000) in rural population <strong>of</strong><br />
Bangalore district during the 4 surveys carried<br />
out between 1962 and 1968.<br />
In the Chingleput study (TPT 1980) where a<br />
rural population <strong>of</strong> about 300,000 was under<br />
surveillance in connection with a BCG trial,<br />
the prevalence <strong>of</strong> bacillary disease was<br />
Ind. J. Tub., Vol. XXIX, No. 3
EPIDEMIOLOGY OF TUBERCULOSIS IN INDIA 139<br />
extremely high (17 per 1,000 for males, 4 per<br />
1,000 for females and 11 per 1,000 for both<br />
sexes).<br />
A number <strong>of</strong> studies carried out in special<br />
groups have also brought forth interesting data.<br />
These include a survey <strong>of</strong> Delhi Police (Sikand<br />
et al, 1954-1959), Civil Servants in Delhi<br />
(Pamra et al, 1968), Textile Workers (Sikand<br />
and Raj Narain, 1953). Also <strong>of</strong> interest is a<br />
study carried out in a rural population in<br />
Bangalore in which 22,957 persons were examined;<br />
the prevalence <strong>of</strong> bacillary disease was<br />
3.0 per 1,000 (Gothi et al, 1976). In Bangalore<br />
city in a small slum population a low prevalence<br />
<strong>of</strong> bacillary disease (2.6 per 1,000) was reported<br />
(Chakarborty et al, 1979). The low prevalence<br />
in the city slums is probably a reflection <strong>of</strong> the<br />
better epidemiological situation in Bangalore,<br />
a fact which was also marked in the ICMR<br />
(1959) survey.<br />
Since radiological and bacteriological examination<br />
<strong>of</strong> children below 5 years is impracticable,<br />
no authentic information on prevalence<br />
<strong>of</strong> respiratory disease in this age group is<br />
available. However, judging from the infection<br />
rates it can be safely presumed that prevalence<br />
<strong>of</strong> disease too must be low. Prevalence <strong>of</strong> disease<br />
(including primary disease) in the age group<br />
5 to 14 years in the rural population <strong>of</strong><br />
Bangalore was reported as 0.3% (bacillary<br />
disease 0.1%) by Gothi et al (1972). Similar<br />
figures for Chingleput rural area (TPT, 1980)<br />
in the 10 to 14 years age group were 0.36%<br />
(bacillary, 0.04%). Prevalence, in general, was<br />
somewhat higher among male children. The<br />
surprising finding was that although the prevalence<br />
<strong>of</strong> infection in the 10 to 14 years age<br />
group in Chingleput was almost twice that<br />
in Balgalore rural area, the morbidity rates were<br />
not different.<br />
It was also found that children with large<br />
tuberculin test reactions (greater than 20 mm,<br />
1 TU PPD-S with RT 23) had more disease<br />
than those with small induration. As expected,<br />
the prevalence <strong>of</strong> respiratory TB in children<br />
was much less than among adults.<br />
Although extra-pulmonary tuberculosis is<br />
believed to be more common in children than<br />
adults, no authentic information about its<br />
prevalence is available from any large scale<br />
community survey. A study carried out in the<br />
slum population <strong>of</strong> Bangalore (Gothi et al,<br />
1974), in which all systems <strong>of</strong> the total child<br />
population were examined, showed a very low<br />
prevalence <strong>of</strong> all manifestations <strong>of</strong> tuberculosis<br />
(0.35%) in the age group 0 to 14 years.<br />
Incidence <strong>of</strong> disease<br />
Incidence <strong>of</strong> bacillary disease is defined as<br />
the number <strong>of</strong> new bacillary cases occurring<br />
annually at subsequent re-examination among<br />
1,000 persons either with normal chest x-ray<br />
or healed x-ray abnormality but bacteriologically<br />
negative at the previous examination (NTI,<br />
1974). The incidence <strong>of</strong> abacillary disease is<br />
the number <strong>of</strong> new radiologically active but<br />
bacteriologically negative cases arising annually<br />
among 1,000 persons with a normal chest x-ray<br />
at an earlier examination.<br />
Information regarding incidence <strong>of</strong> tuberculosis<br />
is available from four areas <strong>of</strong> the<br />
country, Madanapalle, Delhi, Bangalore and<br />
Chingleput. In the congested areas <strong>of</strong> Delhi,<br />
the overall annual incidence <strong>of</strong> bacteriologically<br />
confirmed tuberculosis was found to be 1.3 %<br />
per year (Pamra et al, 1973, Goyal et al, 1978).<br />
In rural area <strong>of</strong> Bangalore (NTI, 1974) the<br />
rate varied from 0.9 to 1.3 per 1,000 per year.<br />
Frimodt-Moller reported an incidence <strong>of</strong> 1.3<br />
per 1,000 per year in the rural population <strong>of</strong><br />
Madanapalle. On the other hand, <strong>Tuberculosis</strong><br />
Prevention Trial (1980) has shown a very<br />
high annual incidence <strong>of</strong> 2.5 per 1,000 between<br />
the first two surveys carried out in Chingleput.<br />
In all areas, incidence <strong>of</strong> bacillary disease<br />
was higher among males than in females. All<br />
four studies had shown a rising incidence with<br />
age for both sexes. Of the total ‘incidence’<br />
cases arising more than half were contributed<br />
by persons more than 35 years <strong>of</strong> age among<br />
males and less than 35 years <strong>of</strong> age among<br />
females.<br />
In the Delhi study (Goyal et al, 1978) the<br />
incidence <strong>of</strong> abacillary disease among previously<br />
healthy persons was found to vary from 1.5 to<br />
3.8 per 1,000 per year at different periods,<br />
whereas in Madanapalle it was <strong>of</strong> the order <strong>of</strong><br />
4 per 1,000 per year. The follow up <strong>of</strong> persons<br />
with healed inactive disease in Delhi showed<br />
that their breakdown rates varied considerably<br />
from One period to another, the rate <strong>of</strong> fresh<br />
bacillary disease ranging from 4 per 1,000 to<br />
14 per 1,000 per year and <strong>of</strong> active abacillary<br />
disease from 7 per 1,000 to 21 per 1,000 per<br />
year between 1962 and 1967.<br />
Also worth reporting is a study carried<br />
out by New Delhi TB Centre in Delhi Police<br />
(Sikand et al, 1959). It was found that in this<br />
group an average <strong>of</strong> 7.8 per 1,000 previously<br />
healthy persons (obviously all adults) broke<br />
down every year with tuberculosis, either<br />
bacillary or abacillary.<br />
Ind. J. Tub., Vol. XXIX, No. 3
140 G.D. GOTHI<br />
Gothi et al (1978) analysed the breakdown<br />
rate among previously healthy persons according<br />
to size <strong>of</strong> tuberculin reaction. They found<br />
that among non-reactors (0 to 9 mm), 0.41 per<br />
1,000 per year developed bacillary disease<br />
whereas among reactors (10 mm or more), the<br />
rate was 1.73 per 1,000 per year. The annual<br />
incidence rate among persons with normal<br />
x-ray chest and a tuberculin reaction between<br />
10 and 19 mm was lowest (0.27 per 1,000).<br />
It was highest (1.9 per 1,000) among those<br />
with a tuberculin reaction <strong>of</strong> 20 mm or more<br />
(NTI, 1974).<br />
The follow up <strong>of</strong> persons with inactive<br />
tuberculous or non-tuberculous lesions in the<br />
same population (Gothi et al, 1978) showed<br />
that 3.73 per 1,000 developed bacillary disease<br />
every year. It was also found that among untreated<br />
persons with radiologically active or<br />
probably active tuberculous lesions the annual<br />
breakdown to bacillary disease was 26 per<br />
1,000. An analysis <strong>of</strong> the total bacillary<br />
‘incidence cases, showed that 76% arose from<br />
the group <strong>of</strong> previous tuberculin positives. The<br />
population with normal chest x-ray at an<br />
earlier examination contributed 48% <strong>of</strong> the<br />
total new bacillary cases.<br />
Krishnamurthy et al (1976) found that<br />
the attack rate <strong>of</strong> disease among recently infected<br />
persons was 7 times higher than among<br />
those infected for more than 9 months.<br />
However, <strong>of</strong> the total new cases, 72% arose<br />
from the previously infected population, a<br />
finding which corroborates the results obtained<br />
by Frimodt-Moller (1960) and several other<br />
workers in other countries.<br />
Raj Narain et al (1972) & Gothi et al (1976)<br />
calculated the annual incidence <strong>of</strong> bacillary<br />
disease among persons with low grade tuberculin<br />
sensitivity (reaction O to 9 mm to 1 TU<br />
PPD RT 23 but more than 10 mm in the former<br />
and 8 mm in the latter study to 20 TU) which<br />
is presumed to be due to infection with Mycobacteria<br />
other than tuberculosis. The five<br />
year incidence in this group was found to be<br />
1.4 per 1,000 which was significantly lower<br />
than among reactors to 1 TU PPD RT 23<br />
(10.8 per 1,000 per year). Among non-reactors<br />
to 20 TU PPD RT 23 it was 2.6 per 1,000<br />
(Gothi et al. 1976).<br />
A point <strong>of</strong> some importance is the length<br />
<strong>of</strong> interval between two consecutive surveys<br />
in longitudinal studies. In the studies reported<br />
above the intervals varied from one to 2½<br />
years. While calculating incidence rates between<br />
any two surveys one always takes into account<br />
symptomatic breakdowns occurring during the<br />
Ind. J, Tub., Vol. XXIX, No. 3<br />
interval. However, it is not inconceivable that,<br />
if the interval is long, some cases may develop<br />
the disease and die or get cured without treatment<br />
and thus miss being counted in the calculation<br />
<strong>of</strong> incidence rates. To that extent,<br />
calculation <strong>of</strong> incidence rates from longitudinal<br />
surveys could be regarded, theoretically, as an<br />
under-estimate. To assess the extent <strong>of</strong> this<br />
possible under-estimate, Gothi et al (1978)<br />
carried out a study in Bangalore rural population<br />
in which a group <strong>of</strong> 30,576 was examined<br />
after a short interval <strong>of</strong> 3 months. The incidence<br />
during the 3-month period was .99 per 1,000<br />
as against the reported annual incidence rates<br />
<strong>of</strong> 1.3 per 1,000 in some other studies (Frimodt-<br />
Moller, 1976; Pamra et al, 1978; NTI, 1974).<br />
From this, it would appear that there is probably<br />
a significant imprecision in the estimates <strong>of</strong><br />
annual incidence as calculated in the studies<br />
referred to above, in which re-examination <strong>of</strong><br />
population was carried out after long intervals.<br />
Another possible source <strong>of</strong> error is the fact<br />
that the second survey may bring to light healed<br />
lesions among persons who had a clear x-ray<br />
at the first survey. Such persons must have had<br />
active disease sometime between the surveys<br />
and must not be ignored while calculating<br />
incidence rates.<br />
Incidence <strong>of</strong> disease among children is a<br />
parameter <strong>of</strong> special interest. Gothi et al (1972)<br />
reported the incidence in 5 to 9 year and 10 to<br />
14 year age groups as 0.5 and 1.0 per 1.000<br />
respectively. Children with a large tuberculin<br />
reaction (>20 mm) were found to have a higher<br />
incidence as also those who had been newly<br />
infected between the two surveys. It is possible<br />
that the newly infected lack resistance with the<br />
result that containment <strong>of</strong> infection takes a<br />
long time and disease manifests itself within<br />
a short period after infection leading to high<br />
morbidity and mortality. New disease was<br />
also seen among children who continued to<br />
remain non-reactors to tuberculin. A plausible<br />
reason for such findings could be (i) tuberculin<br />
test being given in pre-allergic phase or (ii)<br />
overwhelming infection which suppressed the<br />
hypersensitivity.<br />
Narmada et al (1977) reported an incidence<br />
<strong>of</strong> 2.8 per 1,000 per year in the age group 0-12<br />
years in a congested area <strong>of</strong> Madras and 1.2<br />
per 1,000 per year among the non-infected and<br />
8.8 per 1,000 per year among the infected.<br />
The high rates in this population reflect the<br />
unhygienic conditions as well as the chances<br />
<strong>of</strong> acquiring massive and repeated super-infection<br />
among children <strong>of</strong> poor nutritional status.<br />
The low rates prevalence and incidence<br />
<strong>of</strong> infection and disease suggest that respiratory
EPIDEMIOLOGY OF TUBERCULOSIS IN INDIA 141<br />
‘<br />
tuberculosis is not a major problem <strong>of</strong> childhood.<br />
However, it appears that recently infected<br />
children and those with a strong tuberculin<br />
reaction have higher risk <strong>of</strong> developing disease<br />
and dying <strong>of</strong> it.<br />
<strong>Tuberculosis</strong> mortality<br />
In the absence <strong>of</strong> notification regarding<br />
cause <strong>of</strong> death, very little is known about<br />
tuberculosis mortality rates in India. One <strong>of</strong><br />
the earliest reports on the subject is by Sir<br />
Leonard Roger (quoted by Lankaster, 1920)<br />
who, on the basis <strong>of</strong> 22 years’ post-mortem<br />
records <strong>of</strong> Calcutta, concluded that 17% <strong>of</strong><br />
the total deaths were due to tuberculosis and<br />
estimated the annual tuberculosis mortality<br />
as 800 per 100,000 <strong>of</strong> population. Lankaster<br />
(1920) on the basis <strong>of</strong> Roger’s data and some<br />
other available information reported that<br />
Ahmedabad had an annual tuberculosis mortality<br />
<strong>of</strong> 591 per 100,000 and put forward a speculative<br />
estimate <strong>of</strong> at least 400 per 100,000 per year<br />
for most Indian cities. Benjamin et al<br />
(1949) on the basis <strong>of</strong> the Saidapet study put<br />
the estimate at 462 per 100,000. McDougal<br />
(1949) estimated the annual mortality in India<br />
at about 200 per 100,000 and in the same year,<br />
Frimodt-Moller arrived at a rate <strong>of</strong> 253 per<br />
100,000 on the basis <strong>of</strong> Madanapalle study.<br />
Frimodt-Moller (1960) reported that tuberculosis<br />
mortality in the area declined from 64<br />
per 100,000 in 1953-54 to 21 per 100,000 in<br />
1954-55. The marked reduction was probably<br />
due to incomplete recording <strong>of</strong> deaths as natural<br />
decline and intensive treatment could not have<br />
achieved it in so short a time.<br />
Chakarborty et al (1978), from data collected in<br />
Bangalore area estimated the mortality rate at<br />
84 per 100,000 and further found that the rate<br />
was higher in males and in the older age groups,<br />
(a finding which corroborates earlier results <strong>of</strong><br />
Frimodt-Moller, 1960). Among females the<br />
highest mortality was in the age group 30 to 39<br />
years. It may be mentioned that data collected<br />
in the Bangalore area represented the natural<br />
trend since anti-TB services could not be<br />
provided in the area concerned. Goyal et al<br />
(1978) reported an annual mortality rate <strong>of</strong><br />
about 40 per 100,000 in a congested area <strong>of</strong><br />
Delhi where good domiciliary treatment service<br />
was provided. It must, however, be pointed out<br />
that in this calculation no correction was made<br />
for any possible deaths due to non-tuberculous<br />
conditions among tuberculous patients who<br />
died.<br />
Even taking into account the varying reliability<br />
<strong>of</strong> the data collected at different periods<br />
<strong>of</strong> time by different workers, there is little doubt<br />
that tuberculosis mortality is much less to day<br />
than it was in the forties. It is however not<br />
possible to comment on the factors responsible<br />
for the decline which could be due to one or<br />
more factors such as (i) natural decline as a<br />
result <strong>of</strong> increased resistance and socio-economic<br />
betterment, (ii) availability <strong>of</strong> more effective<br />
specific anti-TB measures or (iii) increase in<br />
the number <strong>of</strong> patients coming forward for<br />
treatment in the wake <strong>of</strong> efficient chemotherapy.<br />
Little is known about tuberculosis mortality<br />
in children. Raj Narain (1975) compared the<br />
crude mortality rates among infected and noninfected<br />
children on the assumption that the<br />
differences in the two could be ascribed to tuberculosis.<br />
<strong>Tuberculosis</strong> mortality among children<br />
aged 1 to 4 years on this assumption was found<br />
to be 5.5, 5.2 and 23.9 per 10,000 children in<br />
rural Bangalore, Chingleput and Choolai<br />
city area <strong>of</strong> Madras respectively. The mortality<br />
rate was significantly higher among children<br />
with a tuberculin reaction <strong>of</strong> 20 mm or more,<br />
specially in the O to 4 years age group. Raju<br />
et al (1971) reported a higher mortality rate<br />
among infected compared to non-infected<br />
children below 5 years. Gothi et al (1972)<br />
reported that <strong>of</strong> the total deaths from any<br />
cause in the age group O to 14 years, 19%<br />
could be ascribed to TB.<br />
INH resistance<br />
In recent years, a new index has been added<br />
to the usual indices employed for assessing the<br />
tuberculosis situation in any community. This<br />
is the prevalence <strong>of</strong> primary drug resistance<br />
(specially to INH) in any community. Although<br />
a number <strong>of</strong> antimicrobial drugs have been<br />
in use during the last 30 years, INH is, for<br />
several reasons, the most important and widely<br />
used <strong>of</strong> all the drugs and forms part <strong>of</strong> all regimens<br />
being prescribed anywhere. Primary<br />
resistance to INH may be regarded mainly as<br />
a consequence <strong>of</strong> unsatisfactory therapy <strong>of</strong><br />
infectors (the only other reason being mutation<br />
<strong>of</strong> bacilli) and is a reflection on the quality <strong>of</strong><br />
anti-TB services provided to the community<br />
and availed <strong>of</strong> by the patients. Although the<br />
significance <strong>of</strong> INH resistance is still a moot<br />
point, yet the prevalence <strong>of</strong> primary resistance<br />
in the community is now considered a factor<br />
<strong>of</strong> considerable epidemiological importance.<br />
As in the case <strong>of</strong> other indices there is<br />
considerable lack <strong>of</strong> uniformity in the data<br />
available. This arises due to a number <strong>of</strong> factors<br />
such as (i) differences in the techniques used<br />
and standards adopted for defining drug resistance<br />
and (ii) difference in the care taken to<br />
elicit history <strong>of</strong> previous treatment.<br />
Ind. J. Tub., Vol. XXIX, No. 3
142 G.D. GOTHI<br />
Findings on the subject have been reported<br />
by different workers. Frimodt-Moller (1962)<br />
found INH resistant strains in 6% <strong>of</strong> the untreated<br />
sputum positive patients in Madanapalle<br />
area. Parthasarthy et al (1967) estimated the<br />
prevalence <strong>of</strong> disease with primary INH resistant<br />
strains as 0.9 and 0.8 per 10,000 in the rural<br />
population <strong>of</strong> Rayachoty and Madanapalle<br />
respectively and in Madanapalle town, 6 per<br />
10,000. In the rural areas <strong>of</strong> Bangalore, Raj<br />
Narain et al (1967) reported prevalence <strong>of</strong><br />
INH resistance among bacteriologically confirmed<br />
cases as 12%, 15.4% and 25.4% during 3<br />
surveys carried out between 1961 and 1966.<br />
One fourth <strong>of</strong> these were considered as primary<br />
resistance. However due to unreliable history<br />
<strong>of</strong> previous treatment this finding can be<br />
considered questionable.<br />
A number <strong>of</strong> reports are available regarding<br />
prevalence <strong>of</strong> INH resistant strains among<br />
persons reporting for treatment. Menon (1963)<br />
reported a figure <strong>of</strong> 15% from Hyderabad<br />
which in the subsequent year rose to 21 %<br />
(Menon, 1964); Pamra (1967) reported a figure<br />
<strong>of</strong> 14.1 % from Delhi. Rao et al (1967) reported<br />
that among sanatorium patients, 53.7% were<br />
INH resistant, the corresponding figure in<br />
patients attending a clinic being 27.5% in<br />
rural primary health centre, 32.5%, in selective<br />
house to house case finding programme in rural<br />
areas, 15.5%, and in general population surveys,<br />
11.2%. The history <strong>of</strong> their previous treatment<br />
was not reported.<br />
In 1967, Gangadharam reported the results<br />
<strong>of</strong> a co-operative investigation sponsored by<br />
the ICMR among previously untreated patients<br />
attending 9 urban clinics in the country situated<br />
in Delhi, Bombay, Calcutta, Madras, Bangalore,<br />
Patna, Nagpur, Hyderabad and Amritsar.<br />
Among untreated patients the overall figure<br />
for INH resistant strains was 16%. Among<br />
treated patients the corresponding figure was<br />
46%, nearly three times as high as in untreated.<br />
It may be worth pointing out that history<br />
<strong>of</strong> previous treatment was probably not uniformly<br />
reliable in this investigation.<br />
In the longitudinal surveys carried out by<br />
NTI in rural areas, the proportion <strong>of</strong> sputum<br />
positive patients with INH resistant strains<br />
rose from 11.2% at the first survey to 21.6%<br />
at the 4th survey. The increase was ascribed<br />
to longer survival <strong>of</strong> the resistant cases <strong>of</strong> earlier<br />
surveys and the emergence <strong>of</strong> resistant strains<br />
due to insufficient treatment among those who<br />
had earlier shown sensitive strains. Among the<br />
newly discovered (‘incidence’) cases the percentage<br />
with INH resistant strains during three<br />
successive inter-survey periods was 11.4 %,<br />
Ind. J. Tub., Vol. XXIX, No. 3<br />
10.0% and 6.4% whereas in the Delhi study<br />
there was no significant change in the primary<br />
resistance pattern over a 15 years’ period.<br />
Fate <strong>of</strong> TB patients in the community<br />
The rural population <strong>of</strong> Bangalore was<br />
surveyed 4 times during a period <strong>of</strong> 5 years<br />
at an -interval <strong>of</strong> 1J and 2 years. The patients<br />
discovered in this study could not be <strong>of</strong>fered<br />
treatment for want <strong>of</strong> resources and facilities.<br />
Pamra (1966) and Goyal et al (1978) have also<br />
reported on the fate <strong>of</strong> cases from their longitudinal<br />
study conducted in a congested city<br />
area <strong>of</strong> Delhi. In this study all patients discovered<br />
were <strong>of</strong>fered good intensive ambulatory<br />
domiciliary treatment. Another study by<br />
Frimodt-Moller (1961) gave similar data about<br />
the rural area <strong>of</strong> Madanapalle distinct where<br />
too the patients were provided satisfactory<br />
service. Raj Narain reported a tuberculosis<br />
case fatality <strong>of</strong> 34% and sputum conversion <strong>of</strong><br />
11 % in patients 1½ years after the first survey;<br />
24% continued to remain positive. The fate<br />
<strong>of</strong> direct smear positive culture negative patients<br />
was somewhat better, death rate being 18.4%.<br />
A 5 year study reported by NTI (1974)<br />
shows that <strong>of</strong> the 178 sputum positive patients,<br />
126 could be followed up. Of these 49.2%<br />
died, 18.3% continued to remain bacillary and<br />
sputa <strong>of</strong> 32.5% became negative. Death rates<br />
were reported to be highest during the initial<br />
1½ years period <strong>of</strong> observation; subsequent<br />
survivors continued to live longer and remained<br />
bacillary. Of the new sputum positive cases<br />
discovered during subsequent surveys amongst<br />
the abacillary population <strong>of</strong> the first survey,<br />
sputum conversion rate during the 1½ years<br />
was 52%, mortality 14.3%; 33.3% remained<br />
sputum positive. The fate <strong>of</strong> old cases <strong>of</strong><br />
previous surveys which were considered as<br />
‘prevalence cases’ was poorer than that <strong>of</strong> new<br />
cases discovered in the subsequent surveys.<br />
Frimodt-Moller, on the basis <strong>of</strong> the longitudinal<br />
survey, reported a high mortality<br />
(31.1%) amongst advanced cases in a year;<br />
18% improved. It was further seen that the<br />
mortality in the other category <strong>of</strong> cases was less.<br />
As for the fate <strong>of</strong> patients <strong>of</strong> doubtful activity<br />
judged to be not requiring treatment, 7 to 8 %<br />
developed active disease and 13% showed<br />
clearing <strong>of</strong> the lesion whereas <strong>of</strong> the persons<br />
with inactive disease, 1 % developed active or<br />
probably active disease. The overall intensive<br />
treatment given to the patients for a period<br />
<strong>of</strong> about 1 year in the rural areas by Frimodt-<br />
Moller did not show any change in the tuberculosis<br />
prevalence over a period <strong>of</strong> 5 years.
EPIDEMIOLOGY OF TUBERCULOSIS IN INDIA 143<br />
He reported the same prevalence rates in the<br />
‘treated towns’ as in the ‘untreated<br />
towns’.<br />
Patients discovered in Delhi longitudinal<br />
surveys were <strong>of</strong>fered treatment under a good<br />
domiciliary chemotherapy service. Of these<br />
74 % became sputum negative, 15 % continued<br />
to remain positive and 11 % died during a 2½<br />
year follow up. The outlook for patients who<br />
were regular in treatment improved but the<br />
prevalence rates, even after good chemotherapy,<br />
did not vary significantly over a period <strong>of</strong><br />
15 years.<br />
The Delhi and Madanapalle studies have<br />
shown the course <strong>of</strong> disease under good chemotherapy<br />
in the community whereas the Bangalore<br />
survey provides information on the natural<br />
course <strong>of</strong> the disease among tuberculosis<br />
patients without treatment. No change in the<br />
prevalence <strong>of</strong> the disease in any <strong>of</strong> the three<br />
areas suggests that probably there is something<br />
other than treatment which is necessary for<br />
making an impact on the problem <strong>of</strong> tuberculosis.<br />
However, a good treatment service<br />
brings down the mortality amongst sputum<br />
positive cases considerably and also leads to<br />
sputum conversion in a fairly large proportion<br />
<strong>of</strong> patients even though 15 to 17 % continue<br />
to remain bacillary.<br />
Of the x-ray negative abacillary cases discovered<br />
in the longitudinal survey at Bangalore<br />
(Raj Narain 1966) 6% became sputum positive,<br />
42% got well without any treatment, 26%<br />
remained active abacillary and 5.2% died over<br />
a period <strong>of</strong> 1 j years. For some patients followed<br />
for a period <strong>of</strong> over 5 years, the fate was studied<br />
by the NTI (unpublished data). It was observed<br />
that over a period <strong>of</strong> 5 years, there was a mortality<br />
rate <strong>of</strong> 26%, breakdown rate to sputum<br />
positivity <strong>of</strong> 5% and cure rate <strong>of</strong> 29%. The<br />
remaining 20% continued to have active abacillary<br />
disease.<br />
The fate <strong>of</strong> active abacillary cases reported<br />
by Pamra and Goyal was found to be much<br />
better under chemotherapy (cure rate <strong>of</strong> about<br />
65% and death rate <strong>of</strong> about 5%). Sputum<br />
positivity was not different in this material<br />
as compared with that <strong>of</strong> the NTI material<br />
where no treatment could be <strong>of</strong>fered. Frimodt-<br />
Moller (1960) found mortality rate <strong>of</strong> 13.1 %<br />
in a year among x-ray cases with advanced<br />
disease; improvement was recorded in 18%.<br />
In other categories, namely, those with minimal<br />
or moderately advanced disease, the mortality<br />
was less. The comparison <strong>of</strong> Pamra’s findings<br />
with the NTI observations points to the<br />
achievements that are possible under Indian<br />
conditions with and without good treatment<br />
ment service. Somewhat poor outcome even<br />
under good treatment service could be attributed<br />
to low literacy, poverty etc. leading to incomplete<br />
and irregular treatment.<br />
<strong>Tuberculosis</strong> in Industry<br />
The beginning <strong>of</strong> industrialization influences<br />
the epidemiological curve <strong>of</strong> tuberculosis in<br />
any country. <strong>Tuberculosis</strong> morbidity, at this<br />
point, gets a sudden spurt due to urban influx,<br />
over-crowding, insanitary living conditions,<br />
hard work, poor nutrition and lack <strong>of</strong> rest and<br />
recreation. The virgin population moving from<br />
villages to cities gets infected and succumbs<br />
quickly on account <strong>of</strong> poor resistance and<br />
stresses and strains <strong>of</strong> urban life. Many <strong>of</strong><br />
these break down and contract tuberculosis,<br />
migrate back to their villages carrying with<br />
them infection and disease. With the passage<br />
<strong>of</strong> time the immunologically deficient and<br />
highly susceptible population is weeded out<br />
further. As industrialization progresses, the<br />
economic and environmental conditions <strong>of</strong> the<br />
workers improve, helping them to build up<br />
their health and acquire resistance against<br />
infection, leading in course <strong>of</strong> time, to reduction<br />
in morbidity. India during the last 3 decades<br />
has been passing through this phase which may<br />
account for any apparent decrease.<br />
Apart from the usual hazards <strong>of</strong> urbanisation<br />
and industrialization there are certain<br />
industries, specially those involving risk <strong>of</strong><br />
inhalation <strong>of</strong> dust, fumes, gas and other respiratory<br />
irritants etc. in which tuberculosis morbidity<br />
is generally much higher than among nonindustrial<br />
workers. Silica is known to alter<br />
susceptibility to tuberculosis. Clinical studies,<br />
animal experiments and surveys have shown<br />
that silicosis lowers the resistance to tuberculosis.<br />
Reports No. 3, 11 and 20 from the <strong>of</strong>fice<br />
<strong>of</strong> the Chief Adviser <strong>of</strong> Factories indicate that<br />
tuberculosis is a major cause <strong>of</strong> death and<br />
disability among pottery and ceramic workers.<br />
This is also corroborated by the Bihar Factory<br />
Inspectorate, Labour Department, Government<br />
<strong>of</strong> Bihar. A survey among coal mine workers<br />
<strong>of</strong> Raniganj and Jharia also revealed a high<br />
prevalence <strong>of</strong> tuberculosis among workers<br />
who had pneumoconiosis. Deshmukh et al<br />
(1967) reported a prevalence <strong>of</strong> 1.32% in coal<br />
mines in Chanda district, no significant difference<br />
being found between surface workers and<br />
underground miners. These rates are not higher<br />
than those in the general population. Several<br />
surveys in coal mining industry have shown<br />
a high prevalence <strong>of</strong> particles in the working<br />
environment which have an adverse effect on<br />
the lungs. Steel workers (Billimoria, 1967)<br />
Ind. J. Tub., Vol. XXIX, No. 3
144 G.D. GOTHI<br />
although working under unfavourable environmental<br />
conditions did not have a particularly<br />
high prevalence <strong>of</strong> pulmonary disease (2.57%)<br />
which was not significantly different from<br />
comparable economic and ethnic groups working<br />
in other pr<strong>of</strong>essions. According to Billimoria,<br />
the environment, as far as steel industry is<br />
concernad, has very little to do with the<br />
incidence <strong>of</strong> tuberculosis.<br />
Sikand and Raj Narain (1953) carried out<br />
a survey among textile workers <strong>of</strong> Delhi and<br />
found that the percentage varied between 2%<br />
and 3%. This was higher than in the printing<br />
industry (Government <strong>of</strong> India Press, Delhi)<br />
which was also surveyed about the same time.<br />
The rates were also higher than the overall<br />
rate for Faridabad township but since the latter<br />
contains all age-groups, a direct comparison<br />
may be misleading and only age-specific morbidity<br />
rate would be comparable. Patel (1967)<br />
reported a high prevalence (160 per 1,000)<br />
<strong>of</strong> tuberculosis among textile workers <strong>of</strong><br />
Ahmedabad. However, the authenticity <strong>of</strong> this<br />
finding is questionable since the diagnosis<br />
was based only on radiology and very few<br />
bacteriological specimens were examined.<br />
On the other hand, Gupta and Kulkarni (1963)<br />
in a small scale survey <strong>of</strong> textile workers in<br />
Ahmedabad found a prevalence <strong>of</strong> 186 per<br />
1,000 in the spinning department and 147<br />
per 1,000 in weaving and other departments.<br />
These findings are unexpectedly high. Sikand<br />
and Raj Narain (1953) and Gupta and Kulkarni<br />
(1963) reported a higher prevalence among persons<br />
who had worked in the industry for longer<br />
periods. This could <strong>of</strong> course be a reflection <strong>of</strong><br />
the higher morbidity rate among older persons<br />
who would, naturally, have a longer duration<br />
<strong>of</strong> service.<br />
The prevalence <strong>of</strong> tuberculosis among bidi<br />
workers as reported by Deshmukh (1967)<br />
was fairly high i.e. 3.9% (5.6% among females<br />
and 3.1% among males). The high morbidity<br />
in this group may be attributed to poor socioeconomic<br />
conditions, lack <strong>of</strong> facilities for<br />
employment, medical examination and subsequent<br />
medical care, and insanitary working<br />
environment besides the fact that being sedentary<br />
and not requiring any particular skill,<br />
the job attracts the already physically weak<br />
persons.<br />
<strong>Tuberculosis</strong> trends<br />
As in the case <strong>of</strong> other infectious diseases,<br />
the epidemic curve <strong>of</strong> tuberculosis follows<br />
a definite course over a period <strong>of</strong> time. The<br />
morbidity and mortality curves are composed<br />
<strong>of</strong> two unequal segments, one a short steep<br />
Ind. J. Tub., Vol. XXIX, No. 3<br />
ascending and the other a long slow descending<br />
limb interposed with a plateau. Unlike acute<br />
diseases which have a short time span, the<br />
epidemic curve <strong>of</strong> tuberculosis is spread over<br />
several centuries with the result that changes<br />
over a short period, say 10 or 20 years, cannot<br />
be perceived.<br />
Information on tuberculosis trends is<br />
obviously <strong>of</strong> vital importance for planning a<br />
control programme. In the absence <strong>of</strong> notification<br />
data, reliance has to be placed once more<br />
on repeated tuberculosis surveys or epidemetric<br />
models for providing data regarding tuberculosis<br />
trends.<br />
The decline <strong>of</strong> tuberculosis in almost all<br />
developed countries had started even before<br />
the application <strong>of</strong> specific control measures;<br />
the morbidity and mortality had reached a<br />
low level on the descending limb <strong>of</strong> the tuberculosis<br />
epidemic curve (Grigg, 1958). The<br />
factors that influence the trend <strong>of</strong> tuberculosis<br />
in any country are (i) changes in the socioeconomic<br />
conditions (ii) the rate and extent<br />
<strong>of</strong> tuberculinization <strong>of</strong> the population (iii)<br />
immigration and emigration (iv) war and pestilence<br />
(v) industrialization (vi) prevalence level<br />
<strong>of</strong> disease and infection (vii) specific anti-TB<br />
measures.<br />
Some limited data are available from repeat<br />
surveys carried out in general population groups<br />
as well as selected groups by several workers<br />
in various regions <strong>of</strong> the country. Some <strong>of</strong><br />
these are summarised below.<br />
In a selected group in Delhi comprising<br />
Delhi Police, Government Press employees<br />
etc., Sikand and Raj Narain (1954 & 1959)<br />
did not find any change in the prevalence <strong>of</strong><br />
bacillary disease over a 15 months period.<br />
The overall abacillary disease at two surveys<br />
was 1.5% & 2.0% respectively. It may be pointed<br />
out that the group survey consisted entirely<br />
<strong>of</strong> adults.<br />
In a 5 year study <strong>of</strong> 15 villages (population:<br />
9,537) in Karnataka, Raj Narain (1962) did<br />
not find any change in the prevalence <strong>of</strong> bacillary<br />
disease (4.3% in 1956, 4.5% in 1961). The<br />
prevalence <strong>of</strong> abacillary active disease at the<br />
two points was 1.7% and 1.8% respectively.<br />
Reviewing the various studies carried out<br />
in differents parts <strong>of</strong> the country, specially<br />
the 3 longitudinal studies in Madanapalle,<br />
Delhi and Bangalore, there does not appear<br />
to be any discernible change in the overall<br />
prevalence <strong>of</strong> disease. The prevalence <strong>of</strong><br />
bacillary disease which was around 4 per 1,000
EPIDEMIOLOGY OF TUBERCULOSIS IN INDIA 145<br />
in the middle fifties continued to remain at<br />
almost the same level till about 1974. Frimodt-<br />
Moller (1960) observed a lower prevalence<br />
<strong>of</strong> active disease in younger age in the 1955<br />
survey as compared to the 1950 survey. Similar<br />
reduction in the disease prevalence and incidence<br />
were reported by Pamra (1973) and NTI (1974)<br />
for age group “5 to 34” years although the<br />
differences were not very marked. The longitudinal<br />
survey conducted by NTI showed a<br />
significant decline in the prevalence <strong>of</strong> infection<br />
in the O to 24 years age group and incidence<br />
<strong>of</strong> infection for all ages over a period <strong>of</strong> 5<br />
years. In almost all surveys very little tuberculous<br />
infection was reported in younger children<br />
below 5 years <strong>of</strong> age. This observation was<br />
corroborated by Gothi et al (1978) who surveyed<br />
a slum population <strong>of</strong> Bangalore city.<br />
The slight fall in the prevalence and incidence<br />
<strong>of</strong> infection and morbidity in the younger age<br />
group mentioned earlier is <strong>of</strong>fset by the higher<br />
incidence in older age group and their longer<br />
survival than before. Probably due to chemotherapy,<br />
there are a considerable number <strong>of</strong><br />
patients who are neither cured nor converted<br />
but continue to survive, thus helping to maintain<br />
the status quo in regard to tuberculosis prevalence.<br />
From the Bangalore longitudinal study,<br />
where treatment facilities were non-existent,<br />
it was found that nearly 20 % <strong>of</strong> bacillary cases<br />
die every year, which may be a social failure<br />
but could be considered as an epidemiological<br />
gain. Another 14% <strong>of</strong> the cases become<br />
abacillary during the course <strong>of</strong> the year either<br />
without any treatment or with sufficient treatment—an<br />
epidemiological benefit. The depletion<br />
<strong>of</strong> these 34% cases from the existing pool is<br />
however made up by the fresh incidence <strong>of</strong><br />
disease from the healthy population. The<br />
prevalence rate <strong>of</strong> tuberculosis is thus maintained<br />
from year to year at more or less the same<br />
level. It is thus that inspite <strong>of</strong> various anti-TB<br />
measures taken during the last 30 years, no<br />
appreciable dent seems to have been made on<br />
the problem.<br />
Gradual problem reduction is possible<br />
if a large scale war is waged against tuberculosis<br />
by finding and treating a considerable proportion,<br />
say at least 40% <strong>of</strong> the total cases every<br />
year. However, no control measures can be<br />
expected to give quick results (as, for example,<br />
in the case <strong>of</strong> small pox) since almost half the<br />
population is already infected and new cases<br />
shall continue to arise from amongst these.<br />
Improvement in environmental conditions,<br />
nutrition, etc. will ultimately play a major role<br />
in reducing the tuberculosis problem as was<br />
the case in most western countries where rapid<br />
decline started in late 19th century even before<br />
effective specific control measures were applied.<br />
It would thus appear that although there is<br />
no consensus about the trend <strong>of</strong> tuberculosis<br />
in our country, there is some indirect evidence<br />
suggesting that the disease is entering the<br />
endemic phase and is possibly on the decline.<br />
This may be deduced from the following:<br />
(i) fall in the prevalence <strong>of</strong> infection and disease<br />
in the younger age groups in the longitudinal<br />
surveys (ii) change in the clinical picture <strong>of</strong><br />
tuberculosis from the acute fulminating exudative<br />
type <strong>of</strong> yester-year to a more chronic type<br />
with milder symptoms and almost complete<br />
absence <strong>of</strong> complications like TB meningitis,<br />
enteritis, tumorous suppurative glands in the<br />
neck (Sikand, 1958), (iii) less disease among<br />
young people and in women, (iv) primary<br />
infection and primary disease occurring with<br />
equal frequency among adolescents and adults<br />
and in early childhood. From the history <strong>of</strong><br />
tuberculosis in western countries it can be seen<br />
that such changes in the pattern <strong>of</strong> disease<br />
occur when disease is in the endemic phase and<br />
on the decline. These surmises are also supported<br />
by the fact that prevalence and incidence is<br />
higher in the older age groups, specially males,<br />
that prevalence in towns and villages is nearly<br />
the same and that there is a wide gap between<br />
infection and disease rates (40% and 0.4%<br />
respectively). On the basis <strong>of</strong> these observations,<br />
Nagpaul (1978) and Aneja (1979) have expressed<br />
the opinion that the tuberculosis epidemic<br />
in India is on the decline, probably slowly,<br />
in view <strong>of</strong> the prevailing poverty, malnutrition<br />
and over-crowding.<br />
Epidemetric Models<br />
One <strong>of</strong> the main purposes <strong>of</strong> epidemiological<br />
studies is to make predictions about tuberculosis<br />
trends in future from past trends. This<br />
cannot be done by considering prevalence,<br />
incidence or mortality rates etc. piecemeal.<br />
An overall view can best be had by the use <strong>of</strong><br />
suitable epidemetric models. This, however,<br />
requires accurate or near-accurate calculation<br />
<strong>of</strong> a large number <strong>of</strong> ‘transfer rates’ from<br />
one epidemiological group to another. It is not<br />
<strong>of</strong>ten that reliable data for such studies are<br />
available from the same study and for this<br />
reason not many reports on this subject are<br />
available for India. Waaler et al (1974) have,<br />
however, prepared a model based on the longitudinal<br />
studies carried out by NTI (1974) and<br />
Raj Narain et al (1963), The model indicates<br />
that with case finding coverage <strong>of</strong> 30%, completion<br />
<strong>of</strong> treatment by cases discovered and<br />
with BCG vaccination coverage <strong>of</strong> 30% the<br />
Ind. J. Tub., Vol. XXIX, No. 3
146 G.D. GOTHI<br />
incidence <strong>of</strong> disease can be reduced by 26%<br />
after 25 years whereas if measures to combat<br />
the disease are not taken, the tuberculosis<br />
problem is not likely to be reduced even after<br />
100 years. On the other hand, with case finding<br />
coverage <strong>of</strong> 66 % and treatment completion <strong>of</strong><br />
discovered cases the tuberculosis morbidity<br />
could be brought down from 4 per 1,000 to<br />
1 per 1,000 in 60 years.<br />
REFERENCES<br />
1. Aneja, K.S. & Chakraborty, A.K.; Newsletter.<br />
National <strong>Tuberculosis</strong> <strong>Institute</strong>; 1980, 15, 9.<br />
2. Aspin, J.; Tubercle 1946, 27, 25.<br />
3. Baksh, I.; Ind. Med. Gazt.; 1939, 73, 551.<br />
4. Benjamin, P.V.; Ind. Med. Gazt.; 1938,73, 540.<br />
5. Benjamin, P.V.; Ind. Med. Gazt.; 1939, 74,<br />
516.<br />
6. Benjamin, P.V.: Proc. II TB Workers Conf. New-<br />
Delhi ; 1940, 16.<br />
7. Benjamin, P.V.; Proc. VIII TB Workers Conf.<br />
Hyderabad; 1951, 41.<br />
8. Billimoria, F.J.; Proc. XX11 TB Workers Conf.<br />
Hyderabad; 1967, 142.<br />
9. Banerji, D.P. et al; Proc. XXII TB Workers Conf.<br />
Hyderabad; 1967, 137.<br />
10. Bhore Committee Report; Health Survey & Development<br />
Committee; 1946, 1, 97.<br />
11. Bogen, E.; Ind. J. Tuberc. 1957: 4, 3, 80.<br />
12. Bordia, N.L. et al; Ind. J. Tuberc. I960, 8, 25.<br />
13. Chakraborty, A.K., et al; Ind. J. Tuberc. 1978, 4,<br />
188.<br />
14. Chakraborty, A.K. et al; Ind. J. Pub. Hlth.; 1979,<br />
2, 88.<br />
15. Chakraborty, A.K., et al; Ind. J. Med. Res. 1980,<br />
72, 7.<br />
16. Chandrasekhar, P. et al; Tubercle; 1970, 51, 255.<br />
17. Deshmukh, P.A. et al; Proc. XXII T.B. Workers<br />
Conf. Hyderabad; 1967, 181.<br />
18. Dingley, H.B.; Bull. Int. Un. Tub.; 1979, 54, 2,<br />
154.<br />
19. Frimodt-Moller, J.; Proc. VII TB Workers Conf.<br />
Bombay; 1949, 88.<br />
20. Frimodt-Moller, J.; Proc. IX TB Workers Conf.<br />
Lucknow; 1952, 8.<br />
21. Frimodt-Moller, J.; Bull. Wrld. Hlth. Org. 1960,<br />
22. 61.<br />
22. Frimodt Moller, J.; Tubercle; 1962, 43, 88.<br />
23. Gothi, G.D. et al; Ind. Pediatrics; 1972, 8, 1, 186.<br />
24. Gothi, G.D. et al; Ind. J. Tuberc.; 1976, 2, 58.<br />
25. Gothi, G.D. et al; Ind. J. Tuberc.; 1974, 2, 90.<br />
26. Gothi, G.D. el al; Ind. J. Med. Res.; 1976, 64, 8,<br />
1150.<br />
27. Gothi, G.D. et al; Ind. J. Med. Res.; 1977, 66, 3,<br />
389.<br />
28. Gothi, G.D. et al; Ind. J. Tuberc.; 1978, 3, 122.<br />
29. Gothi, G.D. et al; Ind. J. Tuberc.; 1979, 3, 121.<br />
30. Gothi, G.D. et al; Ind. J. Tuberc.; 1978, 2, 83.<br />
31. Gothi, G.D. et al; Ind. J. Med. Res.; 1978,68,<br />
564.<br />
32. Gangadharam, P.R.J.; Proc. XXM TB Workers<br />
Conf. Hyderabad; 1967, 78.<br />
33. Gangadharam, P.J.R.; Proc. XXII TB Workers<br />
Conf. Hyderabad; 1967, 215.<br />
34. Goyal, S.S. et al; Ind. J. Tuberc. 1978, 2, 77.<br />
35. Grigg, F..R.N.; Am. Rev. Res. Dis.; 1958, 78, 426.<br />
36. Gupta, K. & Kulkarni, P.S.; Ind. J. Chest Dis.;<br />
1963, 5, 136.<br />
37. Hertzberg, G. et al; Proc. IX TB Workers Conf.<br />
Lucknow; 1952, 101.<br />
38. Indian Council <strong>of</strong> Medical Research; A Tuber<br />
culosis Sample Survey; 1959, Special Report, 34.<br />
39. Karen, J.P.; Proc. XVIII TB Workers Conf.<br />
Bangalore; 1962, 57.<br />
40. Krishnamurthy, V.V. et al; Ind. J. Tuberc.; 1976,<br />
XXIII, 1, 3.<br />
41. Krishnaswamy, K.V. et al; Ind. J. Tuberc.; 1978,<br />
XXV, 2, 93.<br />
Ind. J. Tub., Vol. XXIX, No. 3
EPIDEMIOLOGY OF TUBERCULOSIS IN INDIA 147<br />
42. Lai, R.B. et al; A report on tuberculosis survey in<br />
urban & rural areas <strong>of</strong> Bengal; 1944. Quoted from<br />
symp. on TB by Heaf, F.R.G. 618 Cassels & Co.<br />
London, 1957.<br />
43. Lankaster, A.; <strong>Tuberculosis</strong> in India; 1920, Butterworths,<br />
Calcutta.<br />
44. McDougal, J.B.; <strong>Tuberculosis</strong> : A Global Study<br />
in Social Pathology; 1949, Williams & Wilkins,<br />
Baltimore.<br />
45. Menon, N.K.; Tubercle; 1963, 44, 34.<br />
46. Menon, N.K.; BMJ 1964, 1313.<br />
47. Nagpaul, D.R.;J. Ind. Med. Asso.; 1978, 71,2,<br />
44.<br />
48. Nair, S.S. et al; Ind. J. Tuberco; 1976, 4,152.<br />
49. Narmada, R. et al; Ind. J. Med. Res.; 1977, 65, 2,<br />
171.<br />
50. National <strong>Tuberculosis</strong> <strong>Institute</strong> (NTI); Bull. Wrld.<br />
Hlth. Org. 1974, 51, 473.<br />
51. National <strong>Tuberculosis</strong> <strong>Institute</strong> (NTI); Ind. J.<br />
Tuberc.; 1979.<br />
52. National <strong>Tuberculosis</strong> <strong>Institute</strong> (NTI); (Un<br />
published data).<br />
53. Pamra, S.P. & Mathur, G.P.; Ind. J. Tuberc.<br />
1968, XV, 3, 81.<br />
54. Pamra, S.P. et al; Proc. XXIV TB Workers Conf.,<br />
Trivandrum; 1969, 366.<br />
55. Pamra, S.P. et al; Proc. XXII TB Workers Conf.<br />
1967, 82.<br />
56. Pamra, S.P.; Proc. XXI TB Workers Conf.<br />
Calcutta; 1966.<br />
57. Pamra, S.P. et al; Proc. XXIII TB^ Workers<br />
Conf. Bombay; 1968, 61.<br />
58. Pamra, S.P. et al; Ind. J. Tuberc.; 1973, 2, 57.<br />
59. Pamra, S.P. et al; Ind. J. Tuberc.; 1976, 2, 75.<br />
60. Parthasarthy, R. et al; Proc. XXII TB Workers<br />
Conf. Hyderabad; 1967, 63.<br />
61. Patel, R.B. & Ambwani, G.J.; Proc. XXII TB<br />
Workers Conf. Hyderabad, 1967, 161.<br />
62. Philip, S. et al; Proc. IX TB Workers Conf.<br />
Lucknow; 1952,125.<br />
63. Raj Narain et al; Proc. XVIII TB Workers Conf.<br />
Bangalore; 1962, 34.<br />
64. Raj Narain & Subramanian, M.; Proc. XVIII TB<br />
Workers Conf. Bangalore; 1962, 64.<br />
65. Raj Narain et al; Ind. J. Tuberc.; 1965, XIII, 1, 5.<br />
66. Raj Narain et al; Ind. J. Tuberc.; 1966, XIII, 43.<br />
67. Raj Narain et al; Ind. J. Tuberc.; 1963, X, 3; 85.<br />
68. Raj Narain et al; Bull. Wrld. Hlth. Org.; 1966,<br />
34, 623.<br />
69. Raj Narain et al; Proc. XXII TB Workers Conf.<br />
Hyderabad; 1967, 37.<br />
70. Raj Narain et al; Bull. Wrld. Hlth. Org.; 1968,<br />
39, 681.<br />
71. Raj Narain & Diwakar, A.M.; Ind. Fed. 1975,<br />
XII, 528.<br />
72. Raj Narain et al; Am. Rev. Resp. Dis.; 1972;<br />
105, 578.<br />
73. Raj Narain; Proc. XXI TB Workers Conf. Calcutta,<br />
1966, 72.<br />
74. Raju, V.B. et a!; Ind. Pediatrics; 1971, 8, 2, 11.<br />
75. Rao, K.P.; Proc. XXII TB Workers Conf. Hyderabad;<br />
1967, 52.<br />
76. Rao, S., & Cochmani, R.G.; Ind. Med. Gazt.;<br />
1943, 78, 191.<br />
78. Rist, A. & Rose, E.; Ind. Med. Gazt.; 1933, 73,<br />
551.<br />
79. Sikand, B.K. & Raj Narain; Proc. XX TB Workers<br />
Conf., Lucknow, 1952, 106.<br />
80. Sikand, B.K. & Raj Narain; Proc. X TB Workers<br />
Conf. Mysore, 1953, 307.<br />
81. Sikand, B.K. & Pamra, S.P.; Proc. XVIII TB<br />
Workers Conf. Bangalore, 1962, 48.<br />
82. Sikand, B.K.; Proc. XIV TB Workers Conf.<br />
Madras 1958, 184.<br />
83. Sikand, B.K. et al; Ind. J. Tuberc.; 1959, 3, 73.<br />
84. Sikand, B.K. et al; Proc. XI TB Workers Conf.<br />
Nagpur; 1954, 42.<br />
Ind. J. Tub., Vol. XXIX, No. 3
148 G.D.GOTHI<br />
85. Singh, M.M.; Proc. XVI TB Workers Conf.<br />
Poona; 1960, 257 .<br />
86. <strong>Tuberculosis</strong> Prevention Trial (TPT) Madras,<br />
I.C.M.R. Supplement 72, 1980.<br />
87. <strong>Tuberculosis</strong> Prevention Trial, 1980, Unpublished<br />
data.<br />
88. Ukil, A.C.; Ind. J.; Ind. J. Med. Res.; 1930, 17,<br />
2066<br />
88. WHO Expert Committe on <strong>Tuberculosis</strong>, Ninth<br />
Report, 1964. Wrld. Hlth. Org.; Proc. <strong>of</strong> Tech.<br />
Report Series 290.<br />
89. Yerushalmy, J. et al; Am. Rev. Tub. 1950, 61,<br />
443.<br />
Ind. J. Tub., Vol. XXIX, No. 3
WHY INTEGRATED TUBERCULOSIS PROGRAMMES HAVE NOT SUCCEEDED<br />
AS PER EXPECTATIONS IN MANY DEVELOPING COUNTRIES—A<br />
COLLECTION OF OBSERVATIONS 1<br />
D.R. NAGPAUL 2<br />
Summary : Hard work is still needed to make integrated tuberculosis services, and integration<br />
in general, acceptable to health workers and to improve all the support systems for integrated<br />
tuberculosis services to the extent that the envisioned fruits are borne simultaneously with the<br />
introduction <strong>of</strong> these services through primary health care.<br />
Now that case-finding and treatment for<br />
tuberculosis are being considered for introduction<br />
into primary health care, it is relevant<br />
that the experience gained from integration <strong>of</strong><br />
vertical tuberculosis programmes into the<br />
general health service be reviewed critically.<br />
It would be unwise to let the problems and<br />
weaknesses <strong>of</strong> integrated national tuberculosis<br />
programmes (NTP) flow into the new emerging<br />
primary health care system without batting an<br />
eyelash.<br />
It could be stated at the outset, and with due<br />
emphasis, that there really is no alternative<br />
to an integrated tuberculosis service, all its<br />
drawbacks notwithstanding. The point at issue<br />
is that the present form <strong>of</strong> integrated TNPs<br />
need not necessarily be the basis <strong>of</strong> application<br />
<strong>of</strong> tuberculosis control technology through<br />
primary health care.<br />
Success with integration has been patchy so far<br />
In the 1960s, when WHO started recommending<br />
NTPs, especially for developing countries,<br />
the epidemiological, socio-economic and operational<br />
reasons in its favour were indeed compelling<br />
(W.H.O. 1964, 1976). After over two<br />
decades, it cannot be truthfully said that NTPs<br />
have succeeded; nor that they have failed. The<br />
old justifications have not changed since, but<br />
the manner in which integration was brought<br />
about has provided a fresh perspective.<br />
It is true that a tuberculosis patient out in a<br />
village has a much greater chance today than<br />
before <strong>of</strong> being diagnosed and treated, but the<br />
proportion being missed, misdiagnosed and<br />
improperly treated is uncomfortably large.<br />
And, it appears, nothing much is being done by<br />
the integrated health services to correct the<br />
situation. True again, that a newborn baby,<br />
infant, or school entrant has a far greater<br />
probability <strong>of</strong> getting BCG vaccinated under<br />
the integrated health services, compared with<br />
the BCG mass campaign days. But, vital aspects<br />
like maintaining the potency <strong>of</strong> the vaccine<br />
and proper vaccination technique were neglected<br />
by general health workers to the extent<br />
that some special programme aspects had to<br />
be reintroduced under the Expanded Programme<br />
on Immunization to make BCG meaningful.<br />
In some countries even voluntary/private<br />
agencies have joined hands with the government’s<br />
integrated NTP but specialized institutions,<br />
both under public and private sectors,<br />
still maintain that they purvey a much superior<br />
kind <strong>of</strong> tuberculosis service compared with what<br />
general health institutions have to <strong>of</strong>fer. A<br />
degree <strong>of</strong> competition exists between general<br />
and specialized health institutions in securing<br />
preferential attention <strong>of</strong> the public, despite freeflowing<br />
bilateral referral provided under the<br />
NTP. This should be enough to confuse the<br />
health workers and the public alike.<br />
Integration is great to talk about<br />
Health <strong>of</strong>ficials and workers <strong>of</strong>ten talk<br />
about integration knowingly and with enthusiasm<br />
but, like the talk about weather,<br />
nobody does anything about it. The number<br />
who “know” what is wrong with integration is<br />
legion. But it is not for them to find out the<br />
reason there<strong>of</strong> and do something, albeit at<br />
their own levels.<br />
Compartmentalized thinking, attitudes, and<br />
functioning abound at all the levels <strong>of</strong> the health<br />
infrastructure. Strangely enough, those presently<br />
charged with primary health care do not<br />
appear to be above all this. To many, it is the<br />
newest health technology and those not directly<br />
involved could be kept at arm’s length. Is<br />
primary health care gradually and unconsciously<br />
being regarded as a new speciality?<br />
Philosophy <strong>of</strong> integration is understood but not<br />
really accepted<br />
Integration is most visible in the grassroots<br />
level rural health institutions because that<br />
is where in the estimation <strong>of</strong> most health<br />
1 Also issued as WHO/IUAT/JSG/BP/81’4 document.<br />
2 WHO Medical Officer, WPRO, and formerly Director, National <strong>Tuberculosis</strong> <strong>Institute</strong>, Bangalore, India.<br />
N.B. Views expressed in this article are the author’s own views--Editor.<br />
Ind. J. Tub., Vol. XXIX, No. 3
150 D.R. NAGPAUL<br />
<strong>of</strong>ficials, integration is most suited and needed.<br />
In cities and higher levels <strong>of</strong> the health organization,<br />
integration is either missing or cosmetic,<br />
because it is regarded as unnecessary there.<br />
Despite the welcome success <strong>of</strong> integration in<br />
rural health institutions the attitudes and<br />
practices <strong>of</strong> rural health staff are not always<br />
helpful. Poor attitudes could be the reason for<br />
the sizeable misdiagnosis and mistreatment in<br />
respect <strong>of</strong> tuberculosis under the integrated<br />
health service. By training and the examples <strong>of</strong><br />
peers, health workers face serious problems in<br />
forming the needed attitude towards “integration.<br />
Besides, integration conceptually is not<br />
meant for rural areas alone. Attitudinal and<br />
functional changes have to take place at all<br />
levels <strong>of</strong> the health infrastructure, for success<br />
even for the most peripheral level (W.H.O.<br />
1965 and D.G.H.S. 1967).<br />
The widespread covert non-acceptance <strong>of</strong><br />
integration at all levels is there, perhaps, because<br />
integration cuts across the present-day medical<br />
sociology and health services politics. The<br />
apprehensions, insecurity, and confusion generated<br />
by integration among health workers are<br />
just too many. The absence <strong>of</strong> a strong logical<br />
support to the fears is what is making the nonacceptance<br />
covert and non-vocal.<br />
Highly placed <strong>of</strong>ficials, who <strong>of</strong>ten exercise<br />
disproportionately large influence on account<br />
<strong>of</strong> expert clinical services rendered by them to<br />
those in political power, are the ones espousing<br />
the idea that integration needs to be confined<br />
only to the rural health institutions; that people<br />
need and are demanding the establishment <strong>of</strong><br />
many more specialized and prestigious centres<br />
and that no country can afford to lower its<br />
medical expertise and not have at least a few<br />
centres equal to the best in the world. In this<br />
way they try to meet the “threat” posed by<br />
integration to their positions/prestige acquired<br />
through a different system. The element <strong>of</strong><br />
truth in their statements conveniently is not put<br />
in the perspective that could <strong>of</strong>ten be achieved<br />
only by denying the simplest health services or<br />
rendering second-class services to the millions<br />
to provide what is first-class to a few. It is done<br />
perhaps because it is a question <strong>of</strong> survival for<br />
them.<br />
The purpose <strong>of</strong> the above suggestion is not<br />
to denigrate but to ascribe the <strong>of</strong>ten noted<br />
“weak” political will behind many a public<br />
health programme, the re-separation after the<br />
passage <strong>of</strong> some years <strong>of</strong> departments, bureaux,<br />
posts and functions that had been integrated<br />
earlier, the continued opening <strong>of</strong> new tuberculosis<br />
hospitals and centres when their nonessentiality<br />
has been amply demonstrated, etc.<br />
Ind. J. Tub., Vol. XXIX, No. 3<br />
to just one causation, namely, non-acceptance<br />
<strong>of</strong> integration. None can afford to be overly<br />
critical or cynical. It is those, who are either<br />
pushing forward integrated health services,<br />
primary health care, etc. or have to sit in judgment<br />
over their success, that must search their<br />
minds. Must planning for the better health <strong>of</strong><br />
the people brush aside the felt-needs <strong>of</strong> the<br />
pr<strong>of</strong>essional staff who have to carry out the<br />
plans?<br />
Need for acceptability studies<br />
At the time when integration <strong>of</strong> health<br />
services was being recommended, a pilot project<br />
or two in every country helped to demonstrate<br />
to the local workers that the strategy is feasible<br />
and works well. The mental walls appeared<br />
much later. One after another even promising<br />
NTPs got bogged down with difficulties. The<br />
pilot project approach is also being used to<br />
promote primary health care, to attain the goal<br />
<strong>of</strong> “Health for All by Year 2000”. This is good,<br />
but when will we learn that what is feasible is<br />
not necessarily acceptable?<br />
Time and effort must be spared now for<br />
acceptability studies regarding integration. No<br />
sooner had difficulties arisen with integration<br />
in respect <strong>of</strong> NTP than health services research<br />
should have examined its pragmatic basis.<br />
Pragmatically planned programmes are essentially<br />
short-term expedients, but for one reason<br />
or another they succeed in eluding scientific<br />
scrutiny for varying periods. If this note is<br />
regarded as overly critical or unrealistic, pragmatism<br />
will win once again.<br />
This is not to suggest that nothing should<br />
be done until the studies are completed. There<br />
is also no denying that a long time is needed to<br />
bring about a major change from specialization/high<br />
technology <strong>of</strong> the vertical programmes<br />
involving concentration <strong>of</strong> “line” and “staff”<br />
functions in the hands <strong>of</strong> the same persons, to<br />
the people-oriented integrated services with<br />
stress on decentralization, prevention and costbenefit.<br />
The points being made are that a<br />
quarter <strong>of</strong> a century has elapsed and we do<br />
not have unlimited time at our disposal since<br />
primary health care services have to be pushed<br />
forward now and that we are in a stalemate<br />
with regard to integration and do not have<br />
sufficient awareness as well as knowledge about<br />
what to do.<br />
There was inadequate preparation<br />
A part <strong>of</strong> the blame for the poor attitudes<br />
and practices among general health workers
WHY INTEGRATED TUBERCULOSIS PROGRAMMES 151<br />
must be borne by those who had the responsibility<br />
for bringing about integration. Compared<br />
with what was demonstrated to them in pilot<br />
projects, the preparations they made for the<br />
extension phase were either deficient or grossly<br />
inadequate, in order perhaps to attain the set”<br />
extension targets. Some programme extensions<br />
comprised merely an administrative order and<br />
despatch <strong>of</strong> supplies. Training quite <strong>of</strong>ten was<br />
improperly organized with the result that untrained<br />
staff rendering the services, some trained<br />
staff awaiting equipment and supplies long<br />
enough to forget their training, and microscopes<br />
lying around in packing cases for years,<br />
were observed quite frequently. The seminars/<br />
workshops that were organized for training<br />
laid far more stress on technology and too<br />
little on the change <strong>of</strong> attitudes. The people in<br />
general were hardly prepared for the integrated<br />
services and its enshrined referral system. It is<br />
not clear how during the pilot phase the comparative<br />
inadequacy <strong>of</strong> organizational/training<br />
capabilities, available generally to tackle the<br />
enormous task <strong>of</strong> extension, was not foreseen<br />
and something done about it. It is hoped that<br />
history will not repeat itself when it comes to<br />
extension in respect <strong>of</strong> primary health care.<br />
Other observations<br />
Besides poor acceptability <strong>of</strong> integration,<br />
and inadequate preparation for its implementation,<br />
there is :<br />
(a) unexplained, almost paralyzing, lack<br />
<strong>of</strong> sustained interest/enthusiasm among<br />
general health workers in respect <strong>of</strong><br />
tuberculosis services; perhaps some<br />
other programmes as well. Compared<br />
with acute diseases and physical injuries,<br />
the beneficial results from tuberculosis<br />
services do not become visible quickly,<br />
which may lead to a general state <strong>of</strong><br />
disinterest. But, in some cultural milieu,<br />
the apathy tends to disappear when a<br />
family member, friend, or a person with<br />
a “letter <strong>of</strong> reference” approaches for<br />
the service, suggesting that a part <strong>of</strong><br />
the explanation is insufficient social<br />
consciousness among health workers.<br />
Therefore, the apathy needs looking<br />
into and not merely explained away.<br />
(b) Health workers are prone to regard the<br />
functions connected with their “category<br />
training” for entry into service as<br />
“legitimate duty” and other duties<br />
given to them as multipurpose workers<br />
merely as “extra work”. This psycho<br />
logy <strong>of</strong> extra work perhaps is behind<br />
persistent demand for “incentive pay”<br />
when other duties are entrusted to<br />
them in the wake <strong>of</strong> integration, on the<br />
grounds that they are overworked. A<br />
number <strong>of</strong> studies has demonstrated<br />
that all categories <strong>of</strong> health staff in<br />
rural health centres, including medical<br />
<strong>of</strong>ficers, are in fact under-utilized. Yet<br />
the myth <strong>of</strong> overwork continues to<br />
thrive, and is generally accepted. No<br />
sooner are more hands provided to<br />
help reduce the overwork, than the<br />
staff tend to revert to the unipurpose<br />
system <strong>of</strong> work, sometimes by private<br />
arrangements among themselves. If<br />
supervisors would not allow it openly,<br />
they are ready to turn a blind eye<br />
towards it.<br />
Under some health programmes the<br />
grant <strong>of</strong> incentive pay is permitted on<br />
the grounds that health workers in<br />
most developing countries get poor<br />
salaries. There is no reason why health<br />
workers should get less salary than<br />
comparable other categories, but linking<br />
this up with the aim <strong>of</strong> achieving<br />
higher targets in respect <strong>of</strong> a high<br />
priority health programme, which indisputably<br />
leads to neglect <strong>of</strong> other<br />
activities and duties in health institutions,<br />
borders on the undesirable.<br />
Ironically, in spite <strong>of</strong> the incentive pay<br />
the achievements may turn out to be<br />
fictitious if supervision is lax or cannot<br />
be . exercised for a period. Primary<br />
category training as “multipurpose<br />
health worker”, to cover all the integrated<br />
health duties as the terms <strong>of</strong><br />
service at entry, better salary, and good<br />
supervision may resolve the problem.<br />
(c) One <strong>of</strong> the reasons for NTPs not<br />
succeedings as per expectations could<br />
be that the expectations are unrealistic.<br />
After all, these expectations are those<br />
<strong>of</strong> the overseeing specialized workers<br />
who are not really familiar with the<br />
structure and dynamics <strong>of</strong> a general<br />
health service. Replacement <strong>of</strong> population/prevalence-based<br />
targets with<br />
operational ones within the reach <strong>of</strong><br />
multipurpose health workers might<br />
provide the answer.<br />
(d) The “oil crisis” facing the world,<br />
especially the developing countries, may<br />
yet prove a blessing in disguise for the<br />
integrated services. Parenthetically,<br />
transport is an essential prerequisite<br />
for implemtntors/supervisors <strong>of</strong> a public<br />
health programme. The role <strong>of</strong> transport<br />
Ind. J. Tub., Vol. XXIX, No. 3
152 D.R. NAGPAUL<br />
as an image builder <strong>of</strong> health workers,<br />
however, became apparent when attempts<br />
were made to apply management<br />
principles leading to the optimal use<br />
<strong>of</strong> all roadworthy vehicles belonging<br />
to any health programme in an area.<br />
Marked reluctance was observed for<br />
programme functionaries to travel by<br />
public transport when necessary,<br />
share the vehicle with others from<br />
sister health programmes, and agree<br />
to the allocation <strong>of</strong> roadworthy transport<br />
according to optimal utilization<br />
and not merely status <strong>of</strong> those using<br />
them. The most frequent reaction to<br />
“pooling <strong>of</strong> vehicles” practice was for<br />
the supervisors to forego supervision<br />
duty on one plea or another. Now,<br />
with increasing problems <strong>of</strong> maintenance<br />
<strong>of</strong> vehicles and rising price <strong>of</strong><br />
gasoline, coupled with insufficient<br />
budgets for supervisory travel, a pattern<br />
<strong>of</strong> small radius supervision exercised<br />
from each successive level in a<br />
step-ladder fashion might help resolve<br />
the problem.<br />
(e) The supervision <strong>of</strong> NTPs by general<br />
health workers has been decidedly<br />
infrequent, and at times even incorrect,<br />
making it altogether grossly insufficient.<br />
Quite <strong>of</strong>ten, there is great enthusiasm<br />
at the time <strong>of</strong> introduction <strong>of</strong> integrated<br />
tuberculosis services in a health centre,<br />
but very soon hardly any case-finding<br />
or treatment are left to be seen, as if<br />
the service had never been introduced<br />
at all. The specialized “staff” <strong>of</strong>ficers<br />
in the higher levels <strong>of</strong>ten try to correct<br />
the situation by exercising supervision<br />
at all levels, which is obviously an<br />
impracticable proposition. Tf proper<br />
supervision <strong>of</strong> integrated tuberculosis<br />
services by the general health service<br />
“line” <strong>of</strong>ficers cannot be expected at<br />
present, it would take a long time to<br />
make tuberculosis services meaningful<br />
under primary health care.<br />
Not by studies alone<br />
An impression might have been given that<br />
nothing could be done to correct the present<br />
not so satisfactory position <strong>of</strong> NTPs until the<br />
operational studies have been completed. That<br />
technology <strong>of</strong> tuberculosis control has reached<br />
the peripheral level is a gain which should not<br />
be thrown to the winds while awaiting scientific<br />
studies. Until then, the status quo should<br />
continue with whatever could be done to<br />
improve poor attitudes, weak programme support<br />
systems, inadequate training and super-<br />
vision, and the general climate <strong>of</strong> confusion and<br />
apathy. No cut-and-dried solutions for the<br />
interregnum are <strong>of</strong>fered on purpose, not because<br />
it is not possible to <strong>of</strong>fer some suggestions. The<br />
temptation has been resisted. If the earlier<br />
pragmatism and successful pilot projects did<br />
not quite succeed, more time should not be<br />
lost in trying some new pragmatic solutions,<br />
thus tinkering with the problems instead <strong>of</strong><br />
tackling them systematically.<br />
<strong>Tuberculosis</strong> control technology and philosophy<br />
<strong>of</strong> primary health care<br />
However, there is one basic point between<br />
NTPs and the primary health care systems that<br />
needs a pragmatic rationalization now. Under<br />
the philosophy <strong>of</strong> primary health care, people<br />
have the right and duty individually and collectively<br />
to participate in the planning and<br />
implementation <strong>of</strong> their health care activities.<br />
It has to be remembered, however, that at<br />
times people’s perception <strong>of</strong> the health “threats”<br />
facing them and their participation in meeting<br />
the hazards has to be moulded through health<br />
education. <strong>Tuberculosis</strong> and leprosy have a<br />
long history <strong>of</strong> “stigma” which even today<br />
makes individuals and families deny that the<br />
hazard exists for them. They may agree to<br />
these diseases being a community problem, to<br />
which they may accord a low priority. True,<br />
comparatively fewer persons in the community<br />
are afflicted with tuberculosis, but those few<br />
suffer a lot more than others having most other<br />
diseases (Nagpaul et al, 1966). And, before<br />
dying, they infect healthy contacts—about ten<br />
in the case <strong>of</strong> tuberculosis—who may develop<br />
the disease much later. There has to be a kind<br />
<strong>of</strong> understanding, at this stage, on the point <strong>of</strong><br />
educating the public suitably, because faced<br />
with the enormous and difficult task <strong>of</strong> ushering<br />
primary health care in the context <strong>of</strong> a low<br />
perception <strong>of</strong> tuberculosis as a health hazard,<br />
whatever gains NTPs have already registered,<br />
may be allowed to wither away. That would<br />
mean a real failure <strong>of</strong> integration.<br />
REFERENCES<br />
1. Directorate General <strong>of</strong> Health Services, Govern<br />
ment <strong>of</strong> India, New Delhi; Committee on Integra<br />
tion <strong>of</strong> Health Services. Report; 1967.<br />
2. Nagpaul, D.R. et al; Suffering in tuberculosis :<br />
Proceedings <strong>of</strong> <strong>Tuberculosis</strong> and Chest <strong>Diseases</strong><br />
Workers Conference, Hyderabad, India; 1966.<br />
3. WHO Expert Committee on <strong>Tuberculosis</strong>. Eighth<br />
Report; Tech. Rep. Ser. 290, 1964;<br />
4. WHO Study Group on Integration <strong>of</strong> Mass<br />
Campaigns against Specific <strong>Diseases</strong> into General<br />
Health Services. Report; Tech. Rep. Ser. 294; 1965.<br />
5. WHO Expert Committee on <strong>Tuberculosis</strong>. Ninth<br />
Report; Tech. Rep. Ser. 552; 1976.<br />
Ind. J. Tub., Vol. XXIX, No. 3
TUBERCULOSIS IN A RURAL POPULATION OF SOUTH INDIA:<br />
REPORT ON FIVE SURVEYS<br />
A.K. CHAKRABORTY 1 H. SLNGH 2 K. SRIKANTAN 3 K.R. RANGASWAMY 4 M.S.<br />
KR1SHNAMURTHY 8 AND J.A. STEPHEN 6<br />
Summary : The trend <strong>of</strong> tuberculosis in a sample <strong>of</strong> 22 villages observed over a period <strong>of</strong> about 16<br />
years (1961-77). is reported. Distributions <strong>of</strong> tuberculin indurations did not show a clear cut demarcation<br />
between infected and non-infected. The choice <strong>of</strong> demarcation level, therefore, is somewhat<br />
arbitrarily made on the basis <strong>of</strong> the distributions and these varied from survey to survey; between 10<br />
mm at survey I and 16 mm at survey V. The method adopted to demarcate the cut <strong>of</strong>f point has been<br />
described in detail. The actual and standardised infection rates showed more or less declining trend<br />
in 0-4 years, 5-9 years and 10-14 years age groups, The prevalence <strong>of</strong> cases was not significantly different<br />
from survey to survey (varying from 3.96 to 4.92 per thousand from first to fifth survey). However,<br />
there was a shift in the mean age <strong>of</strong> cases, and better survival rate <strong>of</strong> cases diagnosed at later<br />
surveys.<br />
Introduction<br />
For the study <strong>of</strong> epidemiology <strong>of</strong> tuberculosis,<br />
it is necessary to obtain information<br />
on its long-term trend, either natural or following<br />
the control programme. In the absence <strong>of</strong> a<br />
well distributed, adequate and reliable diagnostic<br />
service and reporting system for pulmonary<br />
tuberculosis in India, data on the disease<br />
compiled from the records and reports available<br />
with the health services cannot be considered<br />
representative <strong>of</strong> the community situation. The<br />
house to house surveys, repeated at intervals<br />
in the population <strong>of</strong> the same geographical<br />
area, therefore, form the principal means to<br />
study the trend <strong>of</strong> the disease. However, repeated<br />
surveys in a systematically selected<br />
countrywide sample <strong>of</strong> population, required<br />
to study the trend <strong>of</strong> infection and disease, can<br />
be considered a virtual impossibility under the<br />
existing conditions in India; even the one time<br />
prevalence survey has not yet been carried out<br />
for the entire population till todate. The information<br />
on the trend <strong>of</strong> the tuberculosis<br />
situation in India is therefore usually obtained<br />
from the few isolated repeat surveys conducted<br />
in some areas (Frimodt Moller 1960, NT!<br />
1974, Goyal et al 1978, Gothi et al 1979),<br />
problems <strong>of</strong> extrapolation <strong>of</strong> the findings to the<br />
country as a whole notwithstanding.<br />
One such epidemiological study conducted<br />
four times in a period <strong>of</strong> 5 years among a rural<br />
population <strong>of</strong> Bangalore district, South India<br />
from 1961-68 (NTI, 1974) has indicated a dec-<br />
line in prevalence rates <strong>of</strong> infection in the age<br />
groups 0-14 and 15-24 years and in its incidence<br />
in overall as well as in 0-34 years. The prevalence<br />
and incidence <strong>of</strong> bacteriologically proven<br />
disease also showed a decline among population<br />
aged 5-14 and 5-34 years, during first<br />
three surveys. This trend appeared to be arrested<br />
during the last survey, presumed to have been<br />
caused by conditions <strong>of</strong> deprivation in the<br />
population consequent upon a severe drought<br />
in the study area.<br />
The data on prevalence and incidence <strong>of</strong><br />
infection and disease obtained from the above<br />
study have since been purposefully utilised in<br />
order to project and study the long-term disease<br />
trend in the population by constructing epidemetric<br />
models (Waaler et al 1974, Nair 1977).<br />
Nevertheless, the rather brief period <strong>of</strong> the<br />
study coupled with the uncertainty about the<br />
observation caused by drought before the last<br />
survey, may not permit firm conclusions to be<br />
drawn regarding a secular trend <strong>of</strong> the disease<br />
from the study material itself. Moreover, the<br />
projections and conclusions drawn from the<br />
model may require revision on the basis <strong>of</strong><br />
further actual observations obtained through<br />
surveys <strong>of</strong> the population <strong>of</strong> the same geographical<br />
area from time to time.<br />
Objective<br />
In view <strong>of</strong> the above, the present study was<br />
designed to repeat the survey in the same geo-<br />
1 Senior Medical Officer<br />
2 Statistician<br />
3 Sr Statistical Officer<br />
4 Team Leader<br />
5 Team Leader<br />
6 Statistical Section<br />
National <strong>Tuberculosis</strong> <strong>Institute</strong>. Bangalore<br />
Ind. J. Tub., Vol. XXIX, No. 3
154 A.K. CHAKRABORTY et. al.,<br />
graphical area as for the four surveys between<br />
1961 and 68 (NTI, 1974) to:<br />
(A) obtain information on:<br />
(i) prevalence <strong>of</strong> infection & bacillary<br />
case<br />
(ii) fate <strong>of</strong> the bacillary cases<br />
(B) study changes in tuberculosis situation<br />
over a period <strong>of</strong> about 16 years, in terms <strong>of</strong><br />
changes in prevalence rates <strong>of</strong> infection and<br />
cases.<br />
Study Area & Population<br />
In 1961 the selection <strong>of</strong> the villages for the<br />
study <strong>of</strong> dynamics <strong>of</strong> tuberculosis was made in<br />
such a manner that independent samples were<br />
drawn, consisting <strong>of</strong> 22 and 119 villages, the<br />
former also forming part <strong>of</strong> the succeeding<br />
sample. The population in the bigger sample <strong>of</strong><br />
119 villages was surveyed four times between<br />
1961-68. While planning survey V, it was intended<br />
to cover 119 villages, material from<br />
which has been reported already (NTI, 1974).<br />
However, owing to paucity <strong>of</strong> resources, it was<br />
decided to stop the survey after completing<br />
work in the sample <strong>of</strong> 22 villages only.<br />
The material reported here is thus obtained<br />
from a survey carried out in 1977-78 among the<br />
population in a random sample <strong>of</strong> 22 villages<br />
<strong>of</strong> the 3 taluks (sub-divisions) <strong>of</strong> Magadi,<br />
Channapatna and Nelamanagala in Bangalore<br />
district <strong>of</strong> South India. The data pertaining to<br />
the V survey have been compared with those<br />
from earlier four surveys in respect <strong>of</strong> the<br />
22 villages only. The population registered for<br />
the 22 villages was 3% <strong>of</strong> the total population<br />
in 3 taluks in 1961 and 2.6% in 1977. Till 1975,<br />
no organized anti-tuberculosis services were<br />
available in the area in the form <strong>of</strong> diagnosis<br />
and treatment <strong>of</strong> tuberculosis cases and BCG<br />
vaccination <strong>of</strong> susceptible population. Such<br />
services were also not <strong>of</strong>fered to the population<br />
by the survey teams. The District <strong>Tuberculosis</strong><br />
Programme was implemented in the area only<br />
in 1973, following which antituberculosis<br />
services were generally available through dispensaries<br />
in the area and direct mass BCG<br />
vaccination was started for the first time.<br />
Time Table for the Surveys<br />
The data collection for the survey V was<br />
completed in a year and half starting from<br />
February 1977. The interval between the IV<br />
and V surveys was 11 years and that between<br />
I and V surveys was nearly 16 years. The order<br />
in which the villages were surveyed earlier was<br />
unchanged at survey V.<br />
Method<br />
The entire population in each <strong>of</strong> the 22<br />
villages was registered on individual cards by<br />
visiting them in their houses. Each registered<br />
person was invited 1o attend the examination<br />
centre set up for the day at a convenient place<br />
in the village for tuberculin test and X-ray.<br />
On attending the centre, he was identified with<br />
the help <strong>of</strong> the card prepared and both his<br />
shoulders were examined for BCG scar. Persons<br />
for whom the minimum examinations for BCG<br />
scar were carried out, formed the ‘response<br />
group’, as distinct from the ‘non-response<br />
group’, who did not present themselves for the<br />
scar reading. Each person was given a tuberculin<br />
test with 1 TU RT 23 with Tween 80 on<br />
the upper third <strong>of</strong> the dorsal aspect <strong>of</strong> the<br />
right forearm, a site previously not used for<br />
testing. After the test he was subjected to a<br />
70 mm miniature X-ray <strong>of</strong> chest.<br />
The induration to tuberculin test was read<br />
by a trained reader between 72-96 hours <strong>of</strong><br />
testing, by visiting the persons in their homes.<br />
Longitudinal diameter was measured and the<br />
measurement entered on the respective card.<br />
The tuberculin tester and readers were the same<br />
only for last two surveys. However, the testers<br />
and readers for all the surveys had similar<br />
training and assessment at the NTI before they<br />
undertook testing/reading in the surveys.<br />
The X-rays were interpreted, as in the<br />
previous surveys (NTI, 1974) by two readers<br />
and an umpire. Persons with any chest X-ray<br />
abnormalities were eligible for sputum collection.<br />
Sputum was also collected from persons<br />
who were diagnosed as cases in any <strong>of</strong> the<br />
previous surveys.<br />
Sputum samples were processed, cultured<br />
and examined at the NTI, following techniques<br />
identical to those adopted at the earlier four<br />
surveys (NTI, 1974). These were examined by<br />
fluorescence microscopy and Ziehl Neelsen<br />
techniques, homogenised with 4% NaOH and<br />
cultured on LJ medium slopes. A person with<br />
positive culture and satisfying identification<br />
test criteria <strong>of</strong> Mycobacterium tuberculosis was<br />
diagnosed as a case, provided he also had a<br />
chest X-ray abnormality at the current survey<br />
(‘cases’).<br />
Material<br />
Registered population<br />
Age sex distribution <strong>of</strong> the registered popu-<br />
Ind. J. Tub., Vol. XXIX, No. 3
TUBERCULOSIS IN A RURAL POPULATION OF SOUTH INDIA 155<br />
lation in the five surveys reveals significant<br />
differences here and there between age composition<br />
from survey to survey, which did not<br />
indicate an overall pattern and were generally<br />
small in magnitude (Table not presented). There<br />
was an overall increase in the population in<br />
about 11 years after the survey IV at the growth<br />
rate <strong>of</strong> 1.82 % per year. It was 1.23 per year for<br />
the entire period <strong>of</strong> 16 years, lack <strong>of</strong> population<br />
increase between II and IV surveys being the<br />
reason for the observed lower values for the<br />
entire period.<br />
The permanent residents (de jure population)<br />
in the villages constituted between 95 and 98 %<br />
<strong>of</strong> the total population (Table 1). Their age and<br />
sex composition was different from survey to<br />
survey and children aged 0-9 years were significantly<br />
less in proportion at survey V (P <<br />
0.05) compared to any other survey (Table not<br />
presented).<br />
Coverages<br />
Whereas all registered persons in the villages<br />
were eligible for tuberculin testing and reading,<br />
only those aged 5 years and over were eligible<br />
for X-ray examination. Only the persons with<br />
chest X-ray abnormality were eligible for sputum<br />
collection and such eligibles were found to<br />
be the lowest (6.6%) during survey V. The<br />
proportions <strong>of</strong> X-rayed persons who were found<br />
eligible for sputum collection were 9.6 %, 15.3 %,<br />
17.9% and 10.7% at survey I, II, III and IV<br />
respectively.<br />
Coverages for tuberculin test reading, X-ray<br />
and sputum examination <strong>of</strong> eligibles were<br />
uniformly high in all the surveys. Coverages for<br />
tuberculin testing and reading (86.4%) and for<br />
X-ray examination (89.0%) were highest in I<br />
survey and coverage <strong>of</strong> sputum collection among<br />
the eligibles were the highest (97.5%) in V<br />
survey.<br />
Population with BCG scars<br />
As mentioned earlier, persons for whom the<br />
minimum investigation <strong>of</strong> reading <strong>of</strong> the BCG<br />
scar was carried out were taken as the response<br />
group. Overall size <strong>of</strong> response groups ranged<br />
in five surveys from 91 % (I survey) to 84.8%<br />
(III survey) <strong>of</strong> the de jure population.<br />
De jure population without BCG scars<br />
have been taken up for detailed analysis in this<br />
report for calculation <strong>of</strong> prevalence rates.<br />
Their sexwise distribution is presented in Table<br />
2. Between 0.6% and 4.3% <strong>of</strong> the population<br />
in response group among the de jure population<br />
TABLE 1<br />
Registered Population According to Sex & Residential Status During Five Surveys<br />
Residential<br />
status<br />
Sex<br />
I Survey II Survey III Survey IV Survey V Survey<br />
No. % No. % No. % No.<br />
%<br />
No. %<br />
Permanent<br />
resident<br />
Both sexes 12088 95.6 12370 96.6 12418 96.6 12078 95.9 14382 95.1<br />
Male 6172 97.2 6271 98.1 6293 97.9 6100 97.0 7277 96.5<br />
Female 5916 94.0 6099 95.1 6125 95.3 5978 94.7 7105 93.6<br />
Temporary<br />
resident<br />
Total<br />
Both sexes<br />
Male<br />
Female<br />
Both sexes<br />
Male<br />
Female<br />
556<br />
181<br />
4.4<br />
2.8<br />
438<br />
124<br />
3.4<br />
1.9<br />
437<br />
136<br />
3.4<br />
2.1<br />
521<br />
189<br />
4.1<br />
3.0<br />
744<br />
262<br />
4.9<br />
3.5<br />
375 6.0 312 4.9 301 4.7 332 5.3 482 6.4<br />
12644 100.0 12806 100.0 12855 100.0 12599 100.0 15126 100.0<br />
6353 100.0 6395 100.0 6429 100.0 6289 100.0 7539 100.0<br />
6291 100.0 6411 100.0 6426 100.0 6310 100.0 7587 100.0<br />
Ind. J. Tub., Vol. XXIX, No. 3
156 A.K. CHAKRABORTY et. al.,<br />
TABLE 2<br />
Distribution <strong>of</strong> the ‘Response’* Population by BCG-Scar status in 5 Surveys<br />
Survey<br />
No BCG Scar BCG Scar Total<br />
Male Female Total Male Female Total Male Female Total<br />
I 5574<br />
(99.4)<br />
5369<br />
(99.4)<br />
10943<br />
(99.4)<br />
31<br />
(0.6)<br />
32<br />
(0.6)<br />
63<br />
(0.6)<br />
5605 5401 11006<br />
II 5204<br />
(95.3)<br />
5209<br />
(96.9)<br />
10413<br />
(96.1)<br />
255<br />
(4.7)<br />
165<br />
(3.1)<br />
420<br />
(3.9)<br />
5459 5374 10833<br />
III 5052<br />
(94.6)<br />
5005<br />
(96.5)<br />
10057<br />
(95.5)<br />
290<br />
(5.4)<br />
184<br />
(3.5)<br />
474<br />
(4.5)<br />
5342 5189 10531<br />
IV 4867<br />
(94.7)<br />
4961<br />
(96.7)<br />
9828<br />
(95.7)<br />
271<br />
(6.2)<br />
167<br />
(3.3)<br />
438<br />
(4.3)<br />
5138 5128 10268<br />
V 4235<br />
(69.4)<br />
4600<br />
(74.2)<br />
8835<br />
(71.8)<br />
1865<br />
(30.6)<br />
1599<br />
(25.8)<br />
3464<br />
(28.2)<br />
6100 6199 12299<br />
Note : Figures in bracket show the percentages<br />
*Response—those in whom reading <strong>of</strong> scar status was done<br />
had BCG scars between survey I & IV, but for<br />
survey V such proportion was 28.2%. Age sex<br />
structure <strong>of</strong> the de jure population without scar<br />
was significantly different from survey to survey<br />
(Table not presented.)<br />
Results<br />
Choice <strong>of</strong> level <strong>of</strong> demarcation to classify<br />
infected:<br />
the<br />
Distribution <strong>of</strong> tuberculin indurations: As<br />
expected and in line with the earlier observation<br />
already reported (NTI, 1974), distribution <strong>of</strong><br />
tuberculin induration size for all ages both<br />
sexes in any <strong>of</strong> the surveys did not show a<br />
clear bimodal pattern. To decide on any level<br />
<strong>of</strong> demarcation to classify the infected and noninfected<br />
among the tuberculin tested population<br />
aged 15 years and over on the basis <strong>of</strong><br />
histograms <strong>of</strong> tuberculin indurations was not<br />
feasible, due to the fact that almost the entire<br />
population in this age group are already infected<br />
with some mycobacteria or other<br />
(Chakraborty et al 1978). In view <strong>of</strong> this,<br />
demarcation into negative and positive reactors<br />
on the basis <strong>of</strong> distributions <strong>of</strong> indurations<br />
could only be attempted in children aged 0-14<br />
years. The demarcation level so arrived at, was<br />
extrapolated to higher age groups, though such<br />
extrapolation may be regarded as hypothetical.<br />
Distribution <strong>of</strong> indurations in population<br />
aged 0-4, 5-9 and 10-14 years for surveys I-V<br />
are presented in figures I-III. Even in these<br />
curves <strong>of</strong> distributions pertaining to younger<br />
age groups, the antimodes are not clearly<br />
defined. However, by fitting normal curves<br />
depicting either <strong>of</strong> the two likely modes, the<br />
anti-mode could be more or less reasonably<br />
hypothesised to lie at around 10 mm for I<br />
survey (Fig. I, II, III : A). The distributions for<br />
surveys II to V (Fig. I, II & III : B, C & D)<br />
were such that it was even more difficult than<br />
in I survey to define two separate modes in<br />
them. Dips in curves <strong>of</strong> distributions <strong>of</strong> indurations<br />
which could be taken as antimodes,<br />
could probably be expected to lie around 11 or<br />
12 mm at II survey, 11 or 12 mm at III survey,<br />
10 to 12 mm at IV survey and 14 to 15 mm at V<br />
survey. Based on the above observations, the<br />
demarcation level to classify infected persons<br />
could be < 10 mm,
TUBERCULOSIS IN A RURAL POPULATION OF SOUTH INDIA 157<br />
indurations among the sputum positive tuberculosis<br />
cases diagnosed at each <strong>of</strong> the I to the<br />
V surveys are presented in Table 4. On the basis<br />
<strong>of</strong> mean minus one SD, if 17 mm is chosen as<br />
the minimum induration <strong>of</strong> I survey cases, the<br />
chances <strong>of</strong> misclassification <strong>of</strong> tuberculosis cases<br />
as tuberculin negative would be about 15%<br />
(P < 0.3); but if 10 to 13 mm (mean minus<br />
2 x SD) is chosen, such chances would be almost<br />
eliminated (P < 0.05). This would justify<br />
selection <strong>of</strong> the demarcation line to be anywhere<br />
between 10-13 mm. However, the level <strong>of</strong><br />
TUBERCULOSIS IN A RURAL POPULATION OF SOUTH INDIA 159<br />
tion levels were also separately worked out<br />
(Method b : to be reported in a separate paper)<br />
on similar lines as followed in the earlier report<br />
on four surveys (NTI, 1974), by making allowances<br />
for the differences <strong>of</strong> mean indurations <strong>of</strong><br />
subsequent surveys over the first. The computed<br />
levels are presented in Table 3: row b. These<br />
are, additionally, in line with distribution <strong>of</strong><br />
indurations in cases.<br />
Prevalence <strong>of</strong> infection<br />
Table 3 also presents the prevalence <strong>of</strong><br />
infection by age and sex from surveys I to V,<br />
worked out on the basis <strong>of</strong> the two sets <strong>of</strong><br />
demarcation levels, one on distribution and the<br />
other computed. Estimates on prevalence rates<br />
with the population <strong>of</strong> first survey as standard,<br />
are presented in table 5 for the sake <strong>of</strong> comparison<br />
from survey to survey after making<br />
due allowance for age sex differences in population.<br />
Prevalence rates <strong>of</strong> infection, as in the<br />
previous surveys, were higher in males than in<br />
Ind. J. Tub., Vol. XXIX, No. I
TUBERCULOSIS IN A RURAL POPULATION OF SOUTH INDIA 161<br />
females except in children in age group 0-14<br />
years (not presented on table). The prevalence<br />
rates were found to rise continuously with age<br />
in all the surveys.<br />
There was a decline in the observed prevalence<br />
<strong>of</strong> infection between I-V surveys in<br />
0-4 years old children (Table 3). The trend was<br />
significant when the demarcation level to classify<br />
the infected was decided by method ‘a’ (0.05 ><br />
P>0.02); but it just missed being significant<br />
by method ‘b’ (0.10 > P > 0.05).<br />
In 5-9 years age group there was declining<br />
trend in prevalence after II survey by method<br />
‘b’ (0.05 > P > 0.02); in 10-14 years also there<br />
was decline in trend after the II survey both by<br />
method ‘a’ (P < 0.001) and ‘b’ (P < 0.001).<br />
The standardised infection rates were compared<br />
in 0-14 years and all age groups (Table<br />
5). It will be seen that for 0-14 years age group,<br />
there was declining trend after the II survey<br />
both by method ‘a’ or ‘b’. However, the overall<br />
standardised rates showed a rise between I-II<br />
Ind. J. Tub., Vol. XXIX, No. 3
162 A.K. CHAKRABORTY et. al.,<br />
TABLE 5<br />
Agewise Prevalence Rate <strong>of</strong> Infection (Standardised) l-V Surveys<br />
Age<br />
Survey<br />
Standardised prevalence rate <strong>of</strong> infection<br />
Population* I II III IV V<br />
1 2 3 4 5 6 7<br />
0-14<br />
years<br />
a 4679<br />
b 4679<br />
6.48 7.84<br />
6.48 8.06<br />
7.84<br />
7.48<br />
6.48<br />
6.06<br />
8.43<br />
4.72<br />
All Ages<br />
A 10369<br />
b 10369<br />
23.35 27.49<br />
23.85 27.58<br />
30.16<br />
27.52<br />
27.76<br />
25.79<br />
27.95<br />
27.18<br />
* Standard population <strong>of</strong> I Survey<br />
a On the basis <strong>of</strong> frequency curve by induration size<br />
b By adding, at each survey, mean difference over I Survey<br />
surveys, but were more or less stationary<br />
thereafter with small fluctuations in between<br />
(rates at II, III & V surveys being similar by<br />
‘b’ method, and at II, IV and V surveys by<br />
‘a’ method). This is due to the influence <strong>of</strong> the<br />
highly significant rising trend in infection rates<br />
observed between I and V surveys in population<br />
aged 15 years and over.<br />
Prevalence <strong>of</strong> cases<br />
Unfortunately the number <strong>of</strong> cases found in<br />
each <strong>of</strong> the surveys was small, the highest being<br />
37 at II survey and lowest 25 at III survey<br />
(Table 6). This did not permit a detailed study<br />
<strong>of</strong> prevalence rates in various ages and sex<br />
groups. Only a few broad patterns are therefore<br />
pointed out below:<br />
There were fewer cases detected among<br />
population in younger age groups than in the<br />
older, in any survey. Of the total cases, the<br />
proportion detected in population aged upto<br />
20 years was consistently falling with time,<br />
from the highest level <strong>of</strong> 13.5% at the II survey<br />
to 2.9 % at V survey (Fig. IV). Partly this could<br />
be explained by the difference in population<br />
sizes in different age groups at V survey as<br />
compared to earlier surveys.<br />
At survey I, half the total prevalence cases<br />
were in persons aged 5 to 39 years and the other<br />
half in 40 years and over age group (1 : 1).<br />
At survey IV, the proportion was 1 : 1.4 and<br />
at the survey V it was 1 : 4. This shows increasing<br />
concentration <strong>of</strong> cases in higher age group<br />
with time.<br />
Of the total cases detected, the proportion<br />
<strong>of</strong> cases in the females showed a rising pattern<br />
with time, especially in those aged 40 years and<br />
over. Of the total cases in this age group,<br />
females were one out <strong>of</strong> 18 or 20 at surveys I &<br />
II; and one out <strong>of</strong> 6 or 4 at surveys IV & V<br />
(Not presented in table).<br />
Owing to small numbers, the prevalence<br />
rates are presented for all ages both sexes and<br />
in two broad age groups, i.e., 5 to 39 years,<br />
and 40 years and over (Table 6). In none <strong>of</strong> the<br />
age groups or in overall, the difference in rates<br />
between surveys were significant.<br />
The all ages both sexes case prevalence<br />
rates were 3.96 per thousand at survey I and<br />
4.92 per thousand at survey V, the last being<br />
the highest overall rate observed at any survey.<br />
The rates in 5 to 39 years age group for both<br />
sexes were 2.68 at survey II as the highest, and<br />
1.57 per thousand at survey V as the lowest.<br />
In 40 years and over age group the rates for<br />
both sexes ranged from 6.7 at III survey to<br />
10.5 at survey V.<br />
The standardised prevalence rates, on the<br />
basis <strong>of</strong> standard population <strong>of</strong> survey I, as<br />
presented in Table 6 were similar to the observed<br />
Ind. J. Tub., Vol. XXIX, No. 3
TUBERCULOSIS IN A RURAL POPULATION OF SOUTH INDIA 163<br />
Ind. J. Tub., Vol. XXIX, No. 3
164 A.K. CHAKRABORTY Ct. al.,<br />
rates. The prevalence rates showed a continued<br />
reduction through the surveys, from<br />
2.62 per thousand at I survey to 1.18 at survey<br />
V, in 5 to 39 years age group. On the other<br />
hand continued rise in the rates was observed<br />
after the III survey (6.59 per thousand) to V<br />
survey (10.98) among population, 40 years and<br />
over in age. Whether with larger number <strong>of</strong><br />
cases, the differences in rates from survey to<br />
survey would have been significant or not cannot<br />
be commented upon.<br />
Fate <strong>of</strong> Cases<br />
Out <strong>of</strong> 36 cases found at the I survey, 31<br />
have been followed up (Fig. V) for a minimum<br />
period <strong>of</strong> 1-1/2 years (I-II survey) and also<br />
for 5 years (I-TV survey). Among 29 cases<br />
diagnosed at IV survey, 26 were followed up<br />
after 11 years at survey V. The number <strong>of</strong><br />
deaths observed were 4, 12 and 17 respectively<br />
in the three periods mentioned above. The<br />
proportion <strong>of</strong> cases dead were 387 per thousand<br />
in 5 years as compared to 654 per thousand in<br />
11 years. Annual case specific mortality* rate<br />
is calculated to be 77 per thousand and 59<br />
*Deaths due to all causes among cases <strong>of</strong> tuberculosis.<br />
Ind, J, Tub., Vol. XXIX, No. 3<br />
per thousand, estimated from the observations<br />
made in the first five and subsequent 11 year<br />
periods respectively. The outcome in terms <strong>of</strong><br />
survival was better for cases diagnosed at IV<br />
survey than that in the I survey.<br />
Discussion<br />
In the epidemiological survey carried out in<br />
119 villages forming a sample <strong>of</strong> the 3 taluks<br />
<strong>of</strong> Bangalore district South India (NTI, 1974),<br />
it was observed that the natural trend <strong>of</strong> the<br />
disease showed a decline in 5 years, as revealed<br />
from a downward trend <strong>of</strong> prevalence and incidence<br />
<strong>of</strong> infection in younger age groups and a<br />
slight decline in prevalence and incidence <strong>of</strong><br />
cases in the younger age groups. The trend<br />
as studied from prevalence rates from survey<br />
to survey, tended to be arrested at the time <strong>of</strong><br />
the last survey owing to unfavourable economic<br />
situation obtaining at that time in the area.<br />
The observations, made on the basis <strong>of</strong> data<br />
collected in a relatively short span <strong>of</strong> 5 years,<br />
gave rise to speculations as to whether these<br />
represented a long-term epidemiological trend<br />
<strong>of</strong> tuberculosis for the area.
TUBERCULOSIS IN A RURAL POPULATION OF SOUTH INDIA 165<br />
The present study extending over nearly a<br />
period <strong>of</strong> 16 years, appears to confirm the<br />
earlier observation <strong>of</strong> the declining trend <strong>of</strong> the<br />
disease though in a smaller sample <strong>of</strong> population.<br />
The points in favour <strong>of</strong> a declining<br />
trend <strong>of</strong> the disease can be summarised as (a)<br />
descending prevalence <strong>of</strong> infection rate in<br />
paediatric age group (b) very few cases in<br />
younger age group upto 19 years <strong>of</strong> age, relative<br />
concentration <strong>of</strong> cases in higher age groups<br />
and higher mean age <strong>of</strong> the prevalence cases<br />
diagnosed in the later surveys (indirect<br />
evidence); (c) even the unchanged prevalence<br />
rates <strong>of</strong> the cases from survey to survey may<br />
indirectly indicate decline.<br />
The entire situation probably represents a<br />
natural trend <strong>of</strong> tuberculosis, though organized<br />
anti-tuberculosis diagnostic and treatment<br />
services were made available in the area in<br />
1973 and direct mass BCG vaccination to the<br />
eligibles was carried out after that. This is<br />
because an implemented programme may not<br />
be expected to influence the natural epidemiological<br />
course in the population in a short time<br />
(Gothi et al 1979).<br />
An important problem concerning the choice<br />
<strong>of</strong> demarcation level merits discussion here,<br />
since it has considerable influence on the interpretation<br />
<strong>of</strong> the trend <strong>of</strong> tuberculous infection.<br />
The mean induration sizes from survey I<br />
through survey V are found to be progressively<br />
rising in 0-14 years population (Table not<br />
presented). It may also be pointed out that<br />
children aged 0-9 yrs. <strong>of</strong> survey V were never<br />
tested with tuberculin previously. Such progressive<br />
rise in mean induration sizes <strong>of</strong> tuberculin<br />
reaction has been observed by other workers<br />
also (Edward et al 1965). Further, it should be<br />
appreciated that there is a significant increase<br />
in the proportion <strong>of</strong> individuals with the indurations<br />
size <strong>of</strong> 10-14 mm in 1977, as compared<br />
to those in 1962. For example, among<br />
children aged 5-9 years with > 10 mm tuberculin<br />
induration size, about 7.7% and 92.3%<br />
were having 10-14 and 15+ mm sizes respectively<br />
in 1962. At the V survey in 1977, these proportions<br />
were 56.7% and 43.3% respectively.<br />
Considerable increase was observed among<br />
children aged 0-4 and 10-14 years also, though<br />
comparatively less pronounced in the former<br />
(Table not presented). Thus the increase in the<br />
proportion <strong>of</strong> reactors beyond 10 mm at V,<br />
survey over that in I survey was mainly due to<br />
the substantial increase in the proportion <strong>of</strong><br />
Ind. J. Tub., Vol. XXIX, No. 3
166 A.K. CHAKRABORTY, et al.,<br />
the intermediate reactors only, i.e. those lying<br />
between 10-14 mm induration sizes. This could<br />
be interpreted as due to factors other than<br />
specific tuberculous infection; otherwise it was<br />
expected to be distributed in all 10 mm and<br />
over reaction ranges. These observations further<br />
necessitated choice <strong>of</strong> a separate and higher<br />
demarcation level as compared to that at 1<br />
survey, to compensate the increase <strong>of</strong> intermediate<br />
reactors at V survey. Such compensation<br />
has, in fact, been made for each survey<br />
to the next varying the demarcation level from<br />
survey to survey, based on the distribution <strong>of</strong><br />
indurations. The possible explanations for this<br />
phenomenon would be: different readers<br />
employed at different surveys, intra-reader<br />
variation for the same reader performing test<br />
readings at different times—resulting from<br />
constant practice and experience gained from<br />
survey to survey; a possibility <strong>of</strong> rising incidence<br />
<strong>of</strong> infection with other mycobacteria and to<br />
varying potency <strong>of</strong> tuberculin supplied at different<br />
times. Boosting, thought to be an important<br />
factor in the earlier studies (Raj Narain et al<br />
1966), is no longer considered contributory to<br />
the increase (Raj Narain *et al 1979), especially<br />
since the surveys are conducted at more than<br />
3 months interval from each other. In any case,<br />
the question <strong>of</strong> boosting is irrelevant to 0-4 &<br />
5-9 year old children <strong>of</strong> V survey, who were<br />
not even born at the earlier survey.<br />
It is, no doubt, interesting to compare the<br />
infection rates at 1962 and 1977 surveys, in<br />
case the demarcation levels are kept constant<br />
at both the points. In Appendix Table such an<br />
exercise has been carried out, with 10 mm and<br />
14 mm levels. There is no change in the prevalence<br />
rate <strong>of</strong> infection for 0-4 as well as 0-14<br />
year age group, with 14 mm demarcation<br />
level at both surveys. This prevalence <strong>of</strong> infection<br />
corresponds to the annual risk <strong>of</strong> infection<br />
<strong>of</strong> about 0.8 % (ITS, 1981). On the other<br />
hand, enormous increase in the prevalence<br />
rate for the 1977 survey for 5-9 and 10-14 year<br />
age groups will be estimated, if 10 mm is selected<br />
as the demarcation level for both 1962 and 1977<br />
surveys. In any case, for the reasons mentioned<br />
earlier, especially keeping in view the distribution<br />
<strong>of</strong> tuberculin induration, it appears<br />
logical to select varying demarcation levels from<br />
survey to survey as suggested in the paper,<br />
rather than select the same demarcation level<br />
for all surveys,<br />
Prevalence rate <strong>of</strong> cases was found unchanged<br />
at all the surveys, which, however, is<br />
not <strong>of</strong> much significance owing to the small<br />
number <strong>of</strong> cases involved. The prevalence rate<br />
<strong>of</strong> bacillary cases being small, a large population<br />
size is required for the study <strong>of</strong> its trend<br />
(Chakraborty, 1973). By itself, therefore, the<br />
study <strong>of</strong> prevalence <strong>of</strong> cases did not yield<br />
sufficient data to enable one to comment on the<br />
trend <strong>of</strong> the disease. However, the age wise<br />
proportional distribution showing relative concentration<br />
<strong>of</strong> cases in higher ages (Figure IV),<br />
may be interpreted as supportive <strong>of</strong> the hypothesis<br />
<strong>of</strong> a declining course <strong>of</strong> tuberculosis in<br />
the community.<br />
Acknowledgement<br />
The authors are grateful to the International<br />
<strong>Tuberculosis</strong> Surveillance Centre, The<br />
Hague, Netherlands and particularly to<br />
its Research Director <strong>Dr</strong>. M.A. Bleiker, for<br />
the courtesy in <strong>of</strong>fering valuable assistance and<br />
suggestions after an independent review <strong>of</strong> the<br />
material. The authors express their indebtedness<br />
to <strong>Dr</strong>. Raj Narain & <strong>Dr</strong>. G.D. Gothi,<br />
former Epidemiologists NT1, who were associated<br />
with survey I-IV; <strong>Dr</strong>. Gothi was additionally<br />
associated with survey V also in its<br />
initial phases. The hard work in the field put<br />
in by Epidemiological teams deserves special<br />
acknowledgement. The authors are thankful<br />
to Mrs. Anuradha & other statistical staff, to<br />
Messrs Narayana Prasad & Nagraj for the<br />
drawings and Mr. P. Perumal for Secretarial<br />
assistance.<br />
REFERENCES<br />
1. Chakraborty A.K.; NTI Newsletter; 1973, 10,<br />
57.<br />
2. Chakraborty A.K., Ganapathy K.T., Nair S.S.,<br />
Kul Bhushan; Indian J. Med. Res., 1976, 64, 639.<br />
3. Edwards L.B. & Smith D.T., Amer. Rev. Resp.<br />
Dis., 1965, 92(1), 43.<br />
4. Frimodt-Moller J; Bull. Wld. Hlth. Org., I960,<br />
22, 61.<br />
5. Gothi G.D., Chakraborty A.K., Nair S.S., Ganapathy<br />
K.T. & Banerjee G.C., Ind. Jour. Tub.,<br />
1979, 26, 121.<br />
6. Goyal S.S., Mathur G.P., Pamra S.P., Ind. Jour.<br />
Tub., 1978, 25, 77.<br />
7. International <strong>Tuberculosis</strong> Surveillance Centre,<br />
The Hague; Personal Communication, 1981.<br />
8. Nair S.S., Indian I. Tub. Hlth., 1977,21, 111.<br />
9. National <strong>Tuberculosis</strong> <strong>Institute</strong>; Bull. Wld. Hlth.<br />
Org., 1974, 51, 473.<br />
Ind. J. Tub., Vol. XXIX, No. 3
TUBERCULOSIS IN A RURAL POPULATION OF SOUTH INDIA 167<br />
10. Raj Narain, Nair S.S., Ramanatha Rao G., 12. <strong>Tuberculosis</strong> Prevention Trial, Madras, Indian J.<br />
Chandrasekhar P. & Pyare Lai : Bull. Wld. Hlth. Med. Res.- 1979, 70, 349.<br />
Org., 1966, 34, 622.<br />
11. Raj Narain, Gothi G.D., Ganapathy K.T. &<br />
Shyamasundra C.V., Indian J. Med. Res., 1979, 13. Waaler H.T., Gothi G.D., Baily G.V.J. & Nair<br />
69, 886. S.S.; Bull Wld. Hlth. Org., 1974, 51, 263.<br />
APPENDIX TABLE<br />
Agewise Infection Rates in Children At I & V Surveys. Selecting the Same Demarcation Levels at Both Surveys<br />
at 10 mm<br />
at 14 mm<br />
Demarcation level<br />
Age Group<br />
Survey I* Survey V* Survey I* Survey v*<br />
With Infected With Infected With Infected With Infected<br />
Induration (No.) Induration (No.) Induration (No.) Induration<br />
( %)<br />
(%)<br />
(%)<br />
(No.)<br />
0-4 33 2.1 36 2.4 31 1.9 24 1.6<br />
5-9 91 5.7 127 15.4 87 5.5 60 7.3<br />
10-14 179 12.0 159 32.1 159 10.7 75 15.2<br />
*For number <strong>of</strong> test read children see Table 3.<br />
Ind. J. Tub., Vol. XXIX, No. 3
LOWER LUNG FIELD TUBERCULOSIS<br />
RAM CHANDRA, JITENDRA NATH, G.N. AGARWAL, V.K. SRIVASTAVA AND P.K. MUKERJI<br />
Summary : Prevalence <strong>of</strong> lower lung field tuberculosis was found to be 1.3% among patients<br />
<strong>of</strong> pulmonary tuberculosis, nearly three times more in females (2.3%) than in males (0.9%). Onset<br />
was mostly insiduous and duration less than 6 months. Right lung was involved more <strong>of</strong>ten. Consolidation<br />
with cavity was seen in 28.2%, productive infiltration, exudative infiltration and consolidation<br />
in 14.1 % each. Microscopic sputum smear was positive in 57.7% <strong>of</strong> the cases and 92.0%<br />
<strong>of</strong> them showed sputum conversion at the end <strong>of</strong> four months treatment.<br />
Introduction<br />
It is a well known fact that post primary<br />
tuberculosis originates in the apices <strong>of</strong> the lungs.<br />
Only in a few patients it starts in the bases <strong>of</strong> the<br />
lungs and produces lot <strong>of</strong> confusion in the<br />
diagnosis <strong>of</strong> the disease, specially in the absence<br />
<strong>of</strong> positive sputum.<br />
Most <strong>of</strong> the reports on basal tuberculosis<br />
became available only after 1920 (Feber, 1931;<br />
Dufault, 1932; Anspatch, 1934; Hamilton and<br />
Freed, 1935; Reisner, 1935; Gorden, 1936;<br />
Viswanathan, 1936; Busley, 1939; Sokol<strong>of</strong>f,<br />
1940; Andosca and Foley. 1943; Ossen, 1944;<br />
Romendic et al., 1944; Dock, 1946; Ostrum<br />
and Saber, 1949; Fries, 1955; Johnson, 1959;<br />
Segarra et al., 1963; Tripathv and Nanda,<br />
1970; Mathur et al., 1974). Only a limited<br />
number <strong>of</strong> studies have been conducted in our<br />
country (Viswanathan, 1936; Parmar, 1967;<br />
Tripathy and Nanda, 1970 and Mathur et al.,<br />
1974). In the present report an attempt has<br />
been made to study the problem <strong>of</strong> lower lung<br />
field tuberculosis and its clinical features,<br />
bacteriological status, radiological presentation<br />
and response to therapy.<br />
Material and Methods<br />
The material for the present study was<br />
selected from patients <strong>of</strong> pulmonary tuberculosis<br />
admitted to Kasturba T.B. Hospital,<br />
K.G.’s Medical College, Lucknow, during<br />
the period January 1969 to December, 1978.<br />
Of the total patients <strong>of</strong> pulmonary tuberculosis,<br />
only those patients who had radiological<br />
shadows confined to lower lung field, either<br />
with history <strong>of</strong> contact and clinical features<br />
suggestive <strong>of</strong> tuberculosis and/or a positive<br />
sputum smear for A.F.B. were considered as<br />
patients <strong>of</strong> lower lung field <strong>Tuberculosis</strong>(LLFT).<br />
Since sputum culture for mycobacterium tuberculosis<br />
was done only in a few cases, its results<br />
were not considered in the present study.<br />
The lower lung field has been defined as<br />
that area on P A view <strong>of</strong> the chest which extends<br />
below the imaginary horizontal line<br />
traced across the centre <strong>of</strong> hilar or parahilar<br />
region (Segarra et al 1963). This area includes<br />
middle lobe or lingula in addition to lower<br />
lobe (Parmar, 1967).<br />
The following types <strong>of</strong> patients were excluded<br />
from the present study:<br />
i) Those with either ipsilateral or contralateral<br />
involvement <strong>of</strong> both upper and<br />
lower lung fields.<br />
ii) Pleural effusion and thickening, unless<br />
associated with parenchymal lesion in<br />
the area described.<br />
iii) Possibility <strong>of</strong> non-tuberculous lesion<br />
occuring in the lower lung fields.<br />
iv) Those below 14 years <strong>of</strong> age.<br />
The clinical and radiological features <strong>of</strong><br />
the cases were studied and the response to<br />
therapy was assessed in terms <strong>of</strong> sputum status<br />
and radiological changes at the end <strong>of</strong> four<br />
months’ treatment.<br />
Discussion<br />
It is a well-known fact that post-primary<br />
tuberculosis is located in the apices <strong>of</strong> the<br />
lungs, but in certain proportion <strong>of</strong> patients,<br />
the disease may start from lower lung field<br />
(Segarra et al., 1963; Parmar, 1967; Tripathy<br />
and Nanda, 1970). In the present study the<br />
prevalence <strong>of</strong> lower lung field tuberculosis<br />
was 1.3% <strong>of</strong> the total cases (Table I). A review<br />
<strong>of</strong> literature shows a great variation in the<br />
reported frequency. It varies from 0.003%<br />
(Colton, 1923) to 18.3% (Ross, 1930). Reports<br />
from our country indicate that prevalence<br />
* Department <strong>of</strong> <strong>Tuberculosis</strong> & <strong>Respiratory</strong> <strong>Diseases</strong>,<br />
** Department <strong>of</strong> Radiology,<br />
*** Department <strong>of</strong> Social & Preventive Medicine, King George’s Medical College, Lucknow-226003.<br />
Ind. J. Tub., Vol. XXIX, No. 3
LOWER LUNG FIELD TUBERCULOSIS 169<br />
TABLE 1<br />
Prevalence <strong>of</strong> Lower Lung Field <strong>Tuberculosis</strong> (LLFT) according to age and sex<br />
Age group<br />
(years)<br />
Total patients <strong>of</strong> pulmonary<br />
tuberculosis<br />
Prevalence <strong>of</strong> LLFT<br />
Male Female Total Male Female Total<br />
No. % No. % No. %<br />
Below 20 591 406 997 2 0.3 12 2.9 14 1.4<br />
21-29 371 699 2070 12 0.9 15 2.1 27 1.3<br />
30-39 1081 400 1481 10 0.9 10 2.5 20 1.3<br />
40 & above 1108 258 1366 13 1.2 4 1.5 17 1.2<br />
Total 4151 1763 5914 37 0.9 41 2.3 78 1.3<br />
varies from 0.63% to 6.4% (6.4% Viswanathan,<br />
1936; 3.4% Parmar, 1967; 5.1%<br />
Tripathy and Nanda, 1970 and 0.63% Mathur<br />
et al., 1974). The discrepancy in these figures<br />
may be due to confusion in the terms used<br />
viz. basal, lower lobe, parahilar, lower lung<br />
field tuberculosis and variation in the type <strong>of</strong><br />
material (hospitalized or ambulatory patients<br />
and sputum positive or negative cases). The<br />
prevalence <strong>of</strong> 1.3% observed in the present<br />
series seems to be quite low as compared to<br />
other studies. This is probably because <strong>of</strong> the<br />
fact that Kasturba T.B. Hospital, from where<br />
the study material has been taken is a Centre<br />
which receives patients, from the neighbouring<br />
places usually in advanced stages.<br />
Parmar (1967) observed that most <strong>of</strong> his<br />
patients were generally young, especially below<br />
the age <strong>of</strong> 20 years (46% well below the age <strong>of</strong><br />
20 years). In our series lower lung field tuberculosis<br />
was seen <strong>of</strong>tener in younger age groups but<br />
not statistically different from other age groups<br />
(P>0.05). On the other hand the frequency <strong>of</strong><br />
lower lung field tuberculosis was 2.3 % in females<br />
in comparison to 0.9 % in males, the difference<br />
being statistically significant (P
170 RAM CHANDRA, ET AL.,<br />
TABLE II<br />
Clinical features <strong>of</strong> 78 cases <strong>of</strong> lower lung field tuberculosis<br />
the other hand Viswanathan (1936) reported<br />
chest pain only in 0.95 % <strong>of</strong> cases. Our findings<br />
are much lower than those <strong>of</strong> Lathrop and Lyman<br />
(1924), who reported chest pain in as many<br />
as 50% <strong>of</strong> their cases. In the present study,<br />
only a small percentage (7.7%) <strong>of</strong> patients<br />
<strong>of</strong> lower lung field tuberculosis had dyspnoea<br />
and that too exertional.<br />
Fever was seen in 91.0% <strong>of</strong> the patients<br />
in our series. Viswanathan (1936) noted fever<br />
in 100% <strong>of</strong> his patients. On the other hand only<br />
half <strong>of</strong> the cases <strong>of</strong> Mathur et al. (1974) had<br />
fever. Other toxaemic manifestations such as<br />
loss <strong>of</strong> weight and appetite were observed in<br />
23.1 % <strong>of</strong> our patients. Middlestone and Taylor<br />
(1954) observed these symptoms in 21% <strong>of</strong><br />
their patients. Parmar (1967) was also <strong>of</strong> the<br />
view that toxaemic manifestations are common<br />
features in the patients <strong>of</strong> lower lung field<br />
tuberculosis.<br />
Radiological study revealed many interesting<br />
features (Table III). In half <strong>of</strong> the cases (51.3%)<br />
<strong>of</strong> lower lung field tuberculosis, the right lung<br />
above was involved. In 26.9% cases, only<br />
the left lung was involved and in the remaining<br />
(21.8%) both lungs were involved. Similar<br />
observations were made by Parmar (1967)<br />
and by Mathur et al (1974). Many other workers<br />
failed to observe any marked predominance <strong>of</strong><br />
any side (Reisner, 1935 ;Sokol<strong>of</strong>f, 1940; Weidman<br />
and Campbell, 1937; Romendick et al, Segarra<br />
et al, 1963 and Tripathi and Nanda, 1970).<br />
In our study 32. 0% <strong>of</strong> the cases had far<br />
advanced lesion and in 46.1% <strong>of</strong> cases lesion<br />
was moderately advanced (Table III). The<br />
figures are more or less comparable to those<br />
reported by Tripathi and Nanda (1970) and<br />
Mathur et al (1974).<br />
As shown in Table IV, most <strong>of</strong> the patients<br />
had consolidation with cavity (28.2%) followed<br />
by productive infiltration, consolidation and<br />
exudative infiltration with cavity (14.1% each).<br />
Lower lung field tuberculosis is probably due<br />
TABLE III Radiological (PA view) Features<br />
Ind. J. Tub., Vol. XXIX, No. 3
TABIF IV<br />
Radiological nature <strong>of</strong> lesion<br />
to the ulceration <strong>of</strong> a bronchus by tuberculous<br />
caseous lymph node with spillage <strong>of</strong> tuberculous<br />
material into terminal bronchioles<br />
and alveoli, or progression <strong>of</strong> primary focus<br />
situated in lower lung field, this may commonly<br />
lead to consolidation and cavity formation.<br />
LOWER LUNG FIELD TUBERCULOSIS<br />
71<br />
Evidence <strong>of</strong> cavity was seen in 62.8% <strong>of</strong><br />
cases and its size was less than 4 cm in 43.6%<br />
cases (Table V). Nine patients (11.5%) had<br />
features suggestive <strong>of</strong> tension cavity. Cohen<br />
(1935) noticed cavities in 70% <strong>of</strong> his cases,<br />
while Hawkins (1946) noticed cavitation in<br />
as many as 90%. Most <strong>of</strong> the workers have<br />
reported cavitation in more than 60 % <strong>of</strong> their<br />
patients (Rothstein, 1949; Johnson, 1959;<br />
Segarra et al., 1963; Parmar, 1967 and Tripathy<br />
and Nanda, 1970). Segarra et al. (1963)<br />
obsered that majority <strong>of</strong> cavities were larger<br />
than 3 cm in diameter and were <strong>of</strong> tension<br />
type. In the study <strong>of</strong> Mathur et al. (1974) the<br />
size <strong>of</strong> the cavity was 4 cm or more in 31.2% <strong>of</strong><br />
the cases as compared to only 19.2% <strong>of</strong> the<br />
patients in the present study.<br />
Out <strong>of</strong> the total 78 patients, 45 (57.7 %)<br />
were sputum positive (smear only) and the<br />
remaining (42.3%) were negative for acid fast<br />
bacilli. Patients <strong>of</strong> lower lung field tuberculosis<br />
showed a favourable response to antitubercular<br />
treatment. Only 25 sputum smear<br />
positive cases could be followed for four<br />
months and sputum conversion was seen in 92<br />
% <strong>of</strong> these (Table VI). Almost all the patients<br />
showed radiological improvement. 28%<br />
patients showed cavity closure while others<br />
showed appreciable decrease in the size <strong>of</strong><br />
the cavities. Parmar (1967) advised that such<br />
cases should be put initially under intensive<br />
chemotherapy for eight to nine months and if<br />
the cavity persists, sputum remains positive and<br />
residual bronchi-actasis is left behind,<br />
patients should be considered for resection.<br />
Poor results <strong>of</strong> the treatment observed by<br />
earlier workers were due to mechanical<br />
factors and non-availability <strong>of</strong> chemotherapy<br />
(Mathur et al., 1974).<br />
TABLE V<br />
Cavitary Status in 78 Cases <strong>of</strong> Lower Lung Field <strong>Tuberculosis</strong><br />
Ind. J. Tub., Vol. XXIX, No. 3
172 RAM CHANDRA, ET AL.,<br />
T<br />
TABLE VI<br />
Sputum A Status for A.F.B. in cases <strong>of</strong> LLFT at the end <strong>of</strong> four months therapy<br />
REFERENCES<br />
1. Andosca, J.B. and Foley, .T.A., Jour. Thor. Surg.;<br />
1943, 12, 258.<br />
2. Anspatch, W.E., Am. Jour. Dis. Child.; 1934, 47,<br />
1011.<br />
3. Busley, J.F., Amer. Rev. Tub.; 1939, 40, 692.<br />
4. Cohen, R.C., Brit. Med. Jour.; 1945, 1, 662.<br />
5. Dock, W.M., Amer. Rev. Tub.; 1946, 58, 297.<br />
6. Dutault, P.. Amer. Rev. Tub.; 1932,25, 17.<br />
7. Feber, K., Acta. Med. Scandinav.; 1931, 75, 403.<br />
8. Fries, J.W., Jour. Meil. Med.; 1955, 54, 1310.<br />
9. Gorden, B., Internal Clin.; 1936, 1, 67.<br />
10. Hamilton, C.E. and Fredd, H., Jour. Am. Med.<br />
Ass.; 1935,105, 427.<br />
11. Hawkins, F.S. and Thomas, G.O., Tubercle;<br />
1946, 27, 82.<br />
12. Johnson, J.H.P., Brit. Jour. Dis. Chest.; 1950,<br />
52, 385.<br />
13. Lathrop and Lyman, Quoted by Hamilton and<br />
Fredd, J. Am. Med. Ass.; 1935, 105, 427.<br />
14. Mathur, K.C., Tanwar, K.L. and Razdan, J.N.,<br />
Ind. Jour. Chest Dis.; 1974, 16, 31.<br />
15. Middlestone, H.J.H. and Taylor, A.J., Thorax,;<br />
1954, 9, 344.<br />
16. Ostrum, H.M. and Saber, W., Radiology; 1949,<br />
. 53, 42.<br />
17. Ossen, E.Z., New Eng. J. Med.; 1944, 230, 693.<br />
18. Parmar, M.S., Amer. Rev. Resp. Dis.; 1967, 95,<br />
310.<br />
19. Reisner, D., Arch, Int. Med,; 1935,56, 258.<br />
20. Romendic, S.S., Friedman, B. and Schwartz,<br />
H.F. (1944) Quoted by Tripathi and Nanda (1970).<br />
21. Rothstein, E., Amer. Rev. Tub.; 1949, 59, 39.<br />
22. Segarra, F., Shetman, D.S. and Rodriguiz-Agnero,<br />
J., Amer. Rev. Resp. Dis.; 1963, 87, 37.<br />
23. Sokol<strong>of</strong>f, M.J., Radiology; 1940, 34, 589.<br />
24. Tripathy, S. and Nanda, C.N., Jour. Ass. Phys.<br />
Ind.; 1970,18, 999.<br />
25. Viswanathan, R., Brit. Med. Jour.; 1936, 2, 1300.<br />
26. Weidman, W.H. and Campbell, H.B. (1937)<br />
Quoted by Tripathy and Nanda, J. Ass. Phys. Ind;<br />
1970, 18, 999.<br />
Ind. J. Tub., Vol. XXIX, No. 3
FUNGAL SUPERINFECTION IN PULMONARY TUBERCULOSIS<br />
S.K. JAIN, 1 R.L. AGRAWAL, 2 DEV ASHISH SHARMA 3 AND MANJU AGRAWAL 4<br />
Summary : One hundred forty patients <strong>of</strong> pulmonary tuberculosis were studied to find out (he<br />
prevalence <strong>of</strong> fungal superinfection. Fungus positivity was found in 53 % <strong>of</strong> cases. It was higher in<br />
the treated (chronic) group that in the fresh untreated cases <strong>of</strong> tuberculosis. Fungal growth was found<br />
to be independent <strong>of</strong> extent <strong>of</strong> lesion. Positivity was influenced mainly by the duration <strong>of</strong> previous<br />
antitubercular treatment, duration <strong>of</strong> disease, chronicity <strong>of</strong> lesion and associated illness such as<br />
diabetes mellitus.<br />
Introduction<br />
The prevalence <strong>of</strong> mycotic involvement in<br />
pulmonary tuberculosis is well documented<br />
(Beatty & Saliba, 1963; Shome et a], 1969,<br />
1976; Sandhu et al, 1964, 1966; Chakravarty<br />
et al, 1964, 1967), but there is no comprehensive<br />
study to find out the correlation <strong>of</strong> fungus<br />
superinfection with that <strong>of</strong> duration <strong>of</strong> previous<br />
antitubercular treatment, duration, extent and<br />
severity <strong>of</strong> pulmonary tuberculosis. An attempt<br />
was made to investigate the above problems.<br />
Material and Methods<br />
One hundred and forty patients (age range<br />
10-64 years) were randomly selected for the<br />
present study amongst the diagnosed pulmonary<br />
tuberculosis cases admitted in Government<br />
<strong>Tuberculosis</strong> Hospital, Allahabad from January<br />
1979 to February 1980. They were divided into<br />
two groups: (1) Fresh or untreated group,<br />
comprising cases who had taken none or less<br />
than one month’s antitubercular treatment,<br />
and (2) chronic or treated group—cases who<br />
had antitubercular treatment for more than a<br />
month.<br />
Early morning sputum was collected from<br />
each case after a proper mouth wash with hot<br />
saline water and with proper aseptic precautions.<br />
It was homogenized with the help <strong>of</strong> sterile<br />
glass beads for smear and culture for fungus.<br />
Direct smear examination for fungal elements<br />
was carried out with 10% KOH or lactopHenol<br />
cotton blue and/or grams staining. For culture<br />
<strong>of</strong> fungus, a sterile platinum loopful <strong>of</strong> sputum<br />
was inoculated on three different slopes <strong>of</strong><br />
Sabouraud’s dextrose agar medium prepared<br />
by Emmons’ modification (1977) vi/. (1)<br />
Sabouraud’s dextrose agar (SDA) plain, (2)<br />
SDA with antibiotic (Chloramphenicol 0.04<br />
mg/ml), and (3) SDA with antibiotic and<br />
actidion (Chloramphenicol 0.04 mg/ml and<br />
cycloheximide 0.5 mg/ml). To exclude air contaminants,<br />
a plain Sabouraud’s dextrose agar<br />
culture tube was kept as a control along with<br />
slants <strong>of</strong> each case. Evaluation <strong>of</strong> the amount<br />
<strong>of</strong> growth was done according to Kahanpaa<br />
(1972). Criteria for diagnosis <strong>of</strong> secondary<br />
mycoses in the present study were as follows:<br />
(1) heavy growth <strong>of</strong> fungus in culture repeatedly<br />
for at least three times, and (2) fungus positivity<br />
by direct smear examination.<br />
Identification <strong>of</strong> fungal species was made in<br />
accordance with criteria laid down by Mackenzie<br />
(1966), Ajello et al (1966), Conant et al (1971),<br />
and Emmons et al (1977). Candida albicans<br />
was recognised on the basis <strong>of</strong> pseudomycelia,<br />
blastopore and chlamydospore formation on<br />
cornmeal agar with tween 80 media, and formation<br />
<strong>of</strong> germ tube (R.B. effect)—serum tube<br />
method (Taschdjian et al, 1960) Candida albicans<br />
along with other species <strong>of</strong> Candida<br />
were distinguished by biochemical reactions.<br />
Detailed morphology <strong>of</strong> filamentous fungi<br />
CAspergillus. Rhi/opus, Penicillium) was studied<br />
by slide culture method and/or by Czapeck<br />
media in petri dish. Cryptococcus was identified<br />
by demonstration <strong>of</strong> thick walled yeast cells<br />
in sputum and sensitivity to actidion. Capsule<br />
<strong>of</strong> yeast is better seen in India ink preparation.<br />
Results<br />
The fungus positivity by direct smear and<br />
culture was found in equal number <strong>of</strong> cases<br />
(Table 1). In treated group, the fungus was<br />
found in higher percentage (59 %) than in the<br />
fresh group (37.51%).<br />
Out <strong>of</strong> 140 cases. 6 were suffering from<br />
diabetes mellitus. Fungus was isolated in all<br />
the 6 (100%) diabetic cases, while in the remaining<br />
134 fungus was isolated in 68 (about 50%).<br />
Aspergillus was the commonest fungus<br />
Pr<strong>of</strong>essor and Head <strong>of</strong> Department <strong>of</strong> <strong>Tuberculosis</strong> & <strong>Respiratory</strong> <strong>Diseases</strong>.<br />
2 Ex-Registrar<br />
3 Lecturer in Statistics and Demography, Post-partum Programme<br />
*Lecturer in Anaesthesia From : Moti Lai Nehru Medical College,<br />
Allahabad-211001.<br />
Ind. J. Tub., Vol. XXIX, No. 3
174 S.K. JAIN, R.L. AGRAWAL, DEV ASHISH SHARMA AND MANJU AGRAWAL<br />
TABLE l<br />
found in both fresh and treated groups, followed<br />
Results <strong>of</strong> direct smear and culture examinations for by Candida, Penicillium, Cryptococcus and<br />
fungus in pulmonary tuberculosis<br />
Rhizopus (Table 2). Double growth <strong>of</strong> fungus<br />
was seen in 8 cases <strong>of</strong> chronic (treated) group.<br />
Table 3 shows the correlation <strong>of</strong> fungus<br />
positivity with the duration <strong>of</strong> previous antitubercular<br />
treatment. The positivity was in<br />
39% (35/90) <strong>of</strong> cases who gave a history <strong>of</strong><br />
previous antitubercular treatment for less than<br />
one year, while it was in 78 % (39/50) in those<br />
who had taken more than one year treatment.<br />
The difference was statistically significant.<br />
X 2 = 5.30, df = 1, P < 0.05, S. 3<br />
Correlation between duration <strong>of</strong> illness and<br />
fungal positivity was also worked out. The<br />
difference in fungus positivity among patients<br />
with duration <strong>of</strong> illness below 3 years and above<br />
3 years was statistically significant (Table 4).<br />
TABLE 2<br />
Fungal Isolation<br />
Ind. J. Tub., Vol. XXIX, No. 3
FUNGAL SUPERINFECTION IN PULMONARY TUBERCULOSIS<br />
TABLE 3 TABLE 4<br />
175<br />
Isolation <strong>of</strong> fungus in relation to duration <strong>of</strong> antitubercular<br />
Isolation <strong>of</strong> fungus in relation to duration <strong>of</strong> illness<br />
Comparison was made between upto 1 year and above<br />
one year duration <strong>of</strong> treatment.<br />
Duration <strong>of</strong> illness upto 3 years and above 3 years were<br />
compared.<br />
TABLE 5<br />
Fungal Isolation in Relation to the Extent <strong>of</strong> the Lesions<br />
Extent <strong>of</strong> lesion Fresh group Treated group Total<br />
No. +ve % No. +ve % No. +ve %<br />
1. Minimal 8 50 9 67 17 59<br />
2. Moderate 10 30 11 45 21 38<br />
3. Far advanced 22 36 80 60 102 55<br />
Total 40 37.5 100 59 140 53<br />
Table 5 shows correlation <strong>of</strong> growth <strong>of</strong> fun- in the fresh and the treated group (Table 6),<br />
gus with the extent <strong>of</strong> lesions. Statistically, the but difference was not statistically significant,<br />
chance <strong>of</strong> isolating fungus was irrespective <strong>of</strong><br />
the extent <strong>of</strong> the lesions.<br />
Discussion<br />
Fungus was found in a higher proportion<br />
<strong>of</strong> cavitary cases than non-cavitary cases, both<br />
Superinfection with fungus was significantly<br />
higher in treated (chronic) group than in the<br />
Ind. J. Tub., Vol. XXIX, No. 3
176 S.K. JAIN, R.L. AGRAWAL, DEV ASHISH SHARMA AND MANJU AGRAWAL<br />
TABLE 6<br />
Fungal Isolation in relation to Cavitary Status <strong>of</strong> the lesion<br />
Type <strong>of</strong> lesion Fresh group Treated group Total<br />
No. — ve % No. — ve % No. — ve %<br />
1. Cavitary 13 54 60 60 73 59<br />
2. Non-cavitary 27 30 40 57.5 67 46<br />
Total 40 37.5 100 59 140 53<br />
X 2 =2.19, clf-1,<br />
P>0.05, NS.<br />
fresh group. A comparison <strong>of</strong> results <strong>of</strong><br />
secondary fungal infection in the sputum <strong>of</strong><br />
pulmonary tuberculosis cases reported by<br />
various authors is given below in a tabulated<br />
form:<br />
Author with year<br />
No. <strong>of</strong> Fungus positivity in<br />
cases %<br />
Smear<br />
Culture<br />
Grower & Junnarkar<br />
(1965) 100 30.0 58.0<br />
Shome et al (1976) 860 28.3 18.0<br />
Khanna et al (1977) 110 34.3 36.4<br />
Present study 140 52.9 52.9<br />
— Fresh cases 40 37.5 37.5<br />
— Treated cases 100 59.0 59.0<br />
Percentage <strong>of</strong> Candida species in sputa<br />
<strong>of</strong> patients with pulmonary tuberculosis has<br />
been reported in the literature to vary from<br />
8 to 80 per cent (Norris, 1933, 8.5% Shome<br />
et al, 1976, 9.19%; Schwarting & Skinner,<br />
1949, 20%; Gonzalez Mendoza, 1958, 23%;<br />
Burt & Ketchum, 1941, 42%; Grower &<br />
Junnarkar, 1965, 42%; Chakravarty et al,<br />
1960, 80%), Aspergillus species, however, has<br />
been found less frequently (Shome et al, 1976,<br />
0.69%; Grower & Junnarkar, 1965, 6%;<br />
Ind. J. Tub., Vol. XXIX, No. 3<br />
Khanna et al, 1977,<br />
10%). In contrast, we found Aspergillus more<br />
frequently (29.28%; 41/140) than Candida<br />
(23.57%; 33/140).<br />
Antibiotics, corticosteroids, antimetabolites<br />
and radiation therapy, etc. influence the<br />
incidence <strong>of</strong> both primary and secondary<br />
fungal infection (Wood, 1951; Jha et al, 1974;<br />
Shome et al, 1976). Relationship with the<br />
duration <strong>of</strong> previous antitubercular therapy<br />
has also been mentioned in the literature.<br />
Khanna et al (1977) found higher incidence<br />
<strong>of</strong> fungus positivity in the treated group cases<br />
than the fresh group. Gonzalez Mendoza<br />
(1958) did not find any difference in the prevalence<br />
<strong>of</strong> Candida species in pulmonary tuberculosis<br />
cases before and after the availability<br />
<strong>of</strong> streptomycin. In the present study the<br />
incidence <strong>of</strong> positivity was significantly higher<br />
(78%) in cases who had had antitubercular<br />
treatment for more than one year than those<br />
who had it for less than one year (39%).<br />
A correlation <strong>of</strong> the duration <strong>of</strong> illness<br />
with the fungus positivity was also seen in this<br />
study, the percentage increasing with the<br />
duration <strong>of</strong> illness (P0.05).<br />
Schwarting & Skinner (1949) also reported that<br />
the degree <strong>of</strong> tuberculosis had no influence on<br />
the incidence <strong>of</strong> Candida.<br />
Fungus positivity was higher (59%) in
FUNGAL SUPERINFECTION IN PULMONARY TUBERCULOSIS 177<br />
cavitary group than in the noncavitary group<br />
(46 %). but the difference was not statistically<br />
significant (P>0.05). An interesting finding <strong>of</strong><br />
our study was that the percentage <strong>of</strong> positivity<br />
was high even in the noncavitary cases <strong>of</strong> the<br />
chronic (treated) group (58 %) than the cavitary<br />
cases (54%) <strong>of</strong> the fresh group. It is concluded<br />
that chronicity <strong>of</strong> illness plays a more important<br />
role in superinfection with fungi rather<br />
than the cavitary status <strong>of</strong> the lesions. Khanna<br />
et al (1977) were also <strong>of</strong> the opinion that yield<br />
<strong>of</strong> fungi in pulmonary tuberculosis is related<br />
to chronicity <strong>of</strong> lesion.<br />
The predominance <strong>of</strong> fungal infection in<br />
diabetic patients has been reported by Jha et<br />
al (1974) and Khanna et al (1977). Fungus<br />
superinfection was found in cent percent diabetic<br />
cases in our study.<br />
The authors are <strong>of</strong> the view that factors<br />
mainly responsible for prevalence <strong>of</strong> fungal<br />
superinfection in pulmonary tuberculosis are:<br />
1) duration <strong>of</strong> previous antitubercular treatment,<br />
2) duration <strong>of</strong> illness, 3) chronicity <strong>of</strong><br />
diseases, and 4) associated disease such as<br />
diabetes mellitus.<br />
Acknowledgements<br />
The authors are grateful to the Director,<br />
V.P. Chest <strong>Institute</strong>, Delhi for the kind permission<br />
and <strong>Dr</strong>. H.S. Randhawa, Ph.D., Head<br />
<strong>of</strong> Medical Mycology Department for his<br />
valuable guidance and training given to one<br />
<strong>of</strong> the authors.<br />
REFERENCES<br />
1. Ajello, L., Georg, L.K., Kaplan, W., Kaufman,<br />
L.; CDC Lab Manual for Medical Mycology,<br />
U.S. Department <strong>of</strong> Health, Education and Welfare<br />
Public Health Service Communicable disease<br />
centre; 1966.<br />
2. Beatty, O.A., Saliba, A.; Coexisting Pulmonary<br />
Fungus Infection and <strong>Tuberculosis</strong> at District two<br />
State Hospital; Kentucky Med. J.; 1963, 61, 502.<br />
3. Burt, K.L., Ketchum, H.M.; Classification <strong>of</strong><br />
Strain <strong>of</strong> Candida isolated from Sputum; Am.<br />
J. Trop. Med.; 1941, 21, 427.<br />
4. Chakravarty, S.C.; Incidence and significance <strong>of</strong><br />
Fungi in Sputum in bronchopulmonary diseases;<br />
Acta Tuberc. Scand.; 1964, 45, 295.<br />
5. Chakravarty, S.C.; Clinical aspect <strong>of</strong> Bronchopulmonary<br />
Candidiasis; Proceedings <strong>of</strong> the 22nd<br />
<strong>Tuberculosis</strong> and Chest <strong>Diseases</strong> Workers’ con<br />
ference, Hyderabad, 1967, p. 262.<br />
6. Chakravarty, S.C., Randhawa, H.S., Roy, B.K.,<br />
Viswanathan, R.; Candida species in Throat swab<br />
culture <strong>of</strong> Normal people and in the Sputum <strong>of</strong><br />
Patients with Bronchopulmonary <strong>Diseases</strong>; Calcutta<br />
Med. J.; 1960, 57, 127.<br />
7. Conant, N.F., Smith, D.T., Baker, R.G., Callway,<br />
J.L.; Manual <strong>of</strong> Clinical Mycology, III Ed.<br />
Saunders, W.B. Company Philadelphia; 1971.<br />
8. Emmons, C.W., Binford, C.H., Utz, J.P., Kwon-<br />
Chung, K.J.; Medical Mycology, Ed. III. Lea &<br />
Febiger, Philadelphia; 1977.<br />
9. Gonzalez-Mendoza, A., Bojalil, L.F.; Incidence <strong>of</strong><br />
C. albicans in the sputum <strong>of</strong> Tuberculous Patients;<br />
Am. Rev. <strong>of</strong> Tuberc. & Pulm. Dis.; 1958, 77, 543.<br />
10. Grower, S., Junnarkar, R.V.; Mycological flora in<br />
Patients suffering from Bronchopulmonary <strong>Diseases</strong>;<br />
Ind. J. Med. Sc.; 1965, 19, 823.<br />
11. Hill, A.B.; Principle <strong>of</strong> Medical Statistics 7th ed.<br />
The Lancet Ltd., London; 1961. p. 139.<br />
12. Jha, V.K., Joshi, M., Sen, P.C.; Significance <strong>of</strong><br />
Isolation <strong>of</strong> Fungi from Sputum in Broncho<br />
pulmonary <strong>Diseases</strong>; Presented at 9lh Eastern<br />
Region <strong>Tuberculosis</strong> Conference and 29th National<br />
Conference on <strong>Tuberculosis</strong> and Chest <strong>Diseases</strong>,<br />
Delhi; 1974.<br />
13. Kahanpaa, A.; Bronchopulmonary occurrence <strong>of</strong><br />
Fungi in Adults; Acta Path, et Microbiol. Scand.;<br />
1972, SOB, 1.<br />
14. Khanna, B.K., Nath, P., Ansari, A.H.; A Study<br />
<strong>of</strong> Mycotic flora <strong>of</strong> <strong>Respiratory</strong> tract in Pulmonary<br />
<strong>Tuberculosis</strong>; Ind. J. Tub.; 1977, 24, 159.<br />
15. Mackenzie, D.W.R.; Lab. investigation <strong>of</strong> Candida<br />
infections; In : Symposium on Candida infections.<br />
Ed. H.I. Winner and R. Hurley, Livingstone,<br />
Edinburgh; 1966.<br />
16. Norris, J.C.; Further observations on pathological<br />
yeasts; J. Med. Ass. Georgia; 1933, 22, 250.<br />
17. Sandhu, R.S., Jaggi, O.P., Randhawa, H.S.,<br />
Sandhu, D.K., Gupta, I.M.; Isolation <strong>of</strong> cryptococcus<br />
ne<strong>of</strong>ormans from a patients without clinical<br />
sings <strong>of</strong> Infection; Ind. J. Chest Dis.; 1964, 6, 93.<br />
18. Sandhu, D.K., Sharma, N.V., Sandhu, R.S.,<br />
Damodaran, V.N., Randhawa, H.S.; Broncho<br />
pulmonary Aspergilloma; Indian J. Chest Dis.;<br />
1966, 7, 198.<br />
19. Schwarting, V.M., Skinner, C.E.; Candida in<br />
Sputum <strong>of</strong> Patient with <strong>Tuberculosis</strong>, Mycopathologia;<br />
1949, 4, 349.<br />
Ind. J. Tub., Vol. XXIX, No. 3
178 S.K. JAIN, R.L. AGRAWAL, DEV ASHISH SHARMA AND MANJU AGRAWAL<br />
20. Shome, S.K., Gugnani, H.C., Sirkar, D.K., Murty,<br />
D.K., Raghavan, N.G.S., Rao, P.U.; Cryptococcosis<br />
associated with Pulmonary <strong>Tuberculosis</strong>;<br />
Indian J. Chest Dis.; 1969, 11, 45.<br />
21. Shome, S.K., Upreti, H.B., Singh, M.M., Pamra,<br />
S.P.; Mycoses associated with Pulmonary Tuber<br />
culosis; Ind. J. Tub.; 1976, 23, 64.<br />
22. Taschdjian, C.L., Burchall, J.J., Kozinn, P.P.;<br />
Rapid identification <strong>of</strong> Candida albicans by Filamentation<br />
on Serum and Serum substitute, J.<br />
Dis. Child; 1960, 99, 212.<br />
23. Wood, J.W., Manning, I.H., Patterson, C.N.,<br />
Durham, N.C.; Moniltal infections complicating<br />
therapeutic use <strong>of</strong> antibiotics; JAMA; 1951, 145,<br />
207.<br />
Ind. J. Tub., Vol. XXIX, No. 3
PLASMA COPPER AND ZINC LEVELS IN PULMONARY TUBERCULOSIS<br />
B.K. KHANNA, R. KUMAR, P.K. MUKERJI,* A.R. CHOWDHURY AND V,P. KAMBOJ**<br />
Summary : A study <strong>of</strong> plasma copper and zinc level was conducted in 46 normal subjects and 94<br />
patients <strong>of</strong> pulmonary tuberculosis. 64 patients had received specific anti-tuberculosis therapy for over<br />
one month and 30 were previously untreated. Plasma copper and zinc levels were recorded initially in<br />
all patients and subsequently after 1, 2 & 3 months chemotherapy in the latter group ouly. Itwas found<br />
that pulmonary tuberculosis is characterised by rise in level <strong>of</strong> plasma copper and decline in plasma<br />
zinc level. Only 14 patients did not register any alteration in their levels Highly significant correlation<br />
was established between the level <strong>of</strong> these trace elements and the presence <strong>of</strong> acid-fast bacilli in the<br />
sputum, extent <strong>of</strong> pulmonary involvement, and the nature <strong>of</strong> lesions seen on chest X-ray. Clinical,<br />
bacteriological and radiological improvement following effective therapy led to partial reversal <strong>of</strong><br />
these changes. The depression <strong>of</strong> plasma zinc level was found to be more pronounced and a highly<br />
sensitive index <strong>of</strong> tuberculous activity compared to elevation <strong>of</strong> plasma copper level.<br />
Introduction<br />
Elevation <strong>of</strong> plasma copper and/or depression<br />
<strong>of</strong> plasma zinc level (Tani 1965, Halsted<br />
and Smith 1970, Underwood 1971, Beisel,<br />
Pekarek and Wannemacher 1974, Bogden et<br />
al 1977) has been reported in pulmonary tuberculosis<br />
and in many other chronic diseases.<br />
Most <strong>of</strong> the studies on these two biochemical<br />
parameters relate only to one <strong>of</strong> them. For<br />
example, whereas Tani (1965) has emphasised<br />
the importance <strong>of</strong> measuring serum copper<br />
as a useful biochemical modality in pulmonary<br />
tuberculosis, Halsted and Smith (1970) have<br />
demonstrated reduced plasma zinc level. Bogden<br />
et al (1977) have drawn attention to the importance<br />
<strong>of</strong> measuring both the parameters simultaneously<br />
in these cases, although in most <strong>of</strong><br />
their cases, high copper concentration and<br />
low zinc level was not encountered simultaneously.<br />
Pulmonary tuberculosis has a wide spectrum<br />
<strong>of</strong> presentation. The lesions, radiographically,<br />
may range from acute pneumonic form to that<br />
<strong>of</strong> chronic fibroid lesion. Likewise, the symptoms<br />
may also vary from severe to none. It<br />
is well recognised that many patients, especially<br />
those following chemotherapeutic treatment,<br />
may not excrete tubercle bacilli in their sputum,<br />
though they continue to suffer from active<br />
pulmonary tuberculosis. Consequently, it is<br />
expected that the basic metabolic alteration,<br />
encountered in this disease, will vary according<br />
to the mode <strong>of</strong> presentation, severity <strong>of</strong> the<br />
disease and presence or absence <strong>of</strong> tubercle<br />
bacilli in the sputum. Adaptation <strong>of</strong> a single<br />
criterion for the diagnosis <strong>of</strong> pulmonary tuberculosis<br />
e.g. isolation <strong>of</strong> T.B. from the sputum,<br />
will necessarily restrict the spectrum <strong>of</strong> case<br />
studies (Bogden et al 1977). Furthermore, the<br />
authors felt that correlation <strong>of</strong> these biochemical<br />
parameters, with the clinical, radiographic and<br />
bacteriological status <strong>of</strong> the patient may be<br />
essential. Further, an effort has been made in<br />
this study, to record the effect <strong>of</strong> anti-tuberculosis<br />
chemotherapy, administered for 3<br />
months, on plasma copper and zinc concentration.<br />
Material and Methods<br />
The material for the study was selected<br />
from human volunteers (controls) and from<br />
proved patients <strong>of</strong> pulmonary tuberculosis<br />
admitted to the indoor wards <strong>of</strong> the department<br />
<strong>of</strong> tuberculosis and respiratory diseases.<br />
The control group included doctors, nurses<br />
and other staff members working in the department.<br />
They were thoroughly examined and<br />
had a negative medical history. They were not<br />
receiving any medication (46 subjects).<br />
94 patients <strong>of</strong> pulmonary tuberculosis were<br />
included in the study. 46 patients were sputum<br />
positive (by smear examination) at the time <strong>of</strong><br />
admission to the study, while 48 patients were<br />
reported to have been sputum positive in the<br />
past, though negative at the time <strong>of</strong> the study.<br />
Patients who had hepatic or renal disorders,<br />
diabetes mellitus, hypertension, rheumatoid<br />
disease, lymphoma, myocardial infarction,<br />
pernicious anaemia, hyperthyroidism and<br />
chronic alcoholics were excluded. Women who<br />
were pregnant or were taking oral contraceptives<br />
were also not included.<br />
Detailed history, particularly relating to<br />
previous therapy, was taken. On the basis <strong>of</strong><br />
history <strong>of</strong> previous anti-tuberculosis treatment<br />
the patients were divided in two groups:—<br />
(a) The random group: Patients who had<br />
*Department <strong>of</strong> <strong>Tuberculosis</strong>, K.G’s Medical College, Lucknow-226 003 (India).<br />
**Division <strong>of</strong> Endocrinology, Central <strong>Dr</strong>ug Research <strong>Institute</strong>, Lucknow-226 003.<br />
Ind. J. Tub., Vol. XXIX, No. 3
180 B.K. KHANNA, et al.,<br />
had anti-tuberculosis therapy for more<br />
than a month prior to their induction<br />
in the study (64 cases).<br />
(b) The follow up group: Patients who had<br />
not been treated previously, or who had<br />
taken less than one month <strong>of</strong> antituberculosis<br />
chemotherapy. After initial<br />
observations, these patients were put<br />
on specific anti-tuberculosis therapy;<br />
comprising <strong>of</strong> either streptomycin 1<br />
gm. I.M.I, once a day. I.N.H. 300 mg.<br />
orally once a day and PAS 10 gms.<br />
orally (S-f P+H in 6 patients) or streptomycin<br />
and I.N.H. in the same dose as<br />
above and thioacetazone 150 mg./day<br />
orally in place <strong>of</strong> PAS (S+T+H in<br />
21 patients) or streptomycin + I.N.H.<br />
in the same dose as above and Ethambutol<br />
1000 mg. by month/day (S4- H+E<br />
in 2 patients) or streptomycin + I.N.H.<br />
in the same dosage as given above<br />
(S+H in 1 patient).for a period <strong>of</strong><br />
3 months. All the clinical and biochemical<br />
observations were recorded in<br />
these patients at the end <strong>of</strong> 1, 2 and<br />
3 months <strong>of</strong> therapy (30 patients).<br />
Observations recorded in these patients<br />
included detailed clinical examination, routine<br />
laboratory investigations including sputum<br />
smear examination for A.F.B. and special<br />
investigations such as plasma copper and zinc<br />
estimation.<br />
The method for assessment <strong>of</strong> plasma copper<br />
and zinc was the same as that employed by<br />
Bogden et al (1977). The blood samples were<br />
withdrawn between the hours <strong>of</strong> 10 A.M. and<br />
4 P.M. which coincided with the working<br />
hours <strong>of</strong> the department.<br />
Observations<br />
A. Correlation between plasma copper and<br />
plasma zinc levels in tuberculosis patients<br />
and control subjects:—<br />
Correlation between plasma (Cu) and Zinc<br />
(Zn) in relation to normal values at the time<br />
<strong>of</strong> admission to the study.<br />
A significant rise <strong>of</strong> 22% in plasma copper<br />
level (154.5 ug% ± 33.6) took place in the<br />
patients in contrast to controls (t = 6.04,<br />
df = 138, P < 0.001), while the decline in the<br />
plasma zinc level (63.6 ug% ±17.8) was 28.8%.<br />
The difference was highly significant (t = 10.22,<br />
df = 138, P < 0.001). The reduction in zinc<br />
level was more pronounced. However, no<br />
significant difference was observed in plasma<br />
copper and plasma zinc level between treated<br />
and untreated patients (t = 1.24, df = 42,<br />
P > 0.05).<br />
Out <strong>of</strong> 94 patients, there were 69 males and<br />
25 females. Their age varied from 10 years to<br />
50 years. No statistical correlation could be<br />
obtained between plasma copper and plasma<br />
zinc values with relation to age and sex <strong>of</strong> the<br />
patients.<br />
The dietary level <strong>of</strong> copper and zinc in this<br />
study was not estimated, though all the patients<br />
continued to receive the standard hospital diet.<br />
B. Copper/Zinc ration in tuberculosis patients<br />
and control subjects:<br />
Copper/Zinc ratio was estimated in 46<br />
controls and 94 tuberculosis patients. The ratio<br />
was 2.61 ± 0.85 in tuberculosis cases, while it<br />
was 1.44 ± 0.27 in controls. The difference was<br />
highly significant (t= 12.14, df= 138, P < 0.001).<br />
80 out <strong>of</strong> 94 patients showed abnormalities<br />
<strong>of</strong> either plasma copper level or <strong>of</strong> plasma zinc<br />
level or both. 14 patients had normal plasma<br />
copper as well as zinc level. 20 patients had<br />
normal plasma copper and low plasma zinc<br />
level (value less than 70 ug%). There were 6<br />
patients who had high plasma copper level<br />
(value exceeding 145 ug%) and normal zinc<br />
TABLE 1<br />
Correlation Between Plasma (Cu) and Zine, (Zn) in Relation to Normal Values at the time <strong>of</strong> admission to the study<br />
Ind. J, Tub., Vol. XXIX, No. 3
PLASMA COPPER AND ZINC LEVELS IN PULMONARY TUBERCULOSIS 181<br />
level, while 54 patients had high plasma copper As there was no statistical difference in<br />
level and as well as low plasma zinc level, plasma copper and zinc concentration between<br />
treated and untreated groups (vide table 1),<br />
C. Correlation between plasma copper con a11 the Patients (94) were clubbed together for<br />
centration and zinc concentration with sputum analysis.<br />
status <strong>of</strong> tuberculosis patients:<br />
TABLE 2<br />
Correlation between Plasma Copper and Zinc Levels with Sputum Status<br />
Sputum for A.F.B. No. <strong>of</strong> Ps. Plasma Copper Plasma Zinc<br />
Meam (ug%) ± S.D. % rise Meantug%) ± S.D. % fall<br />
Positive 46. 175.4 ± 19.3 38.5 54.6 ± 16.5 38.8<br />
Negative 48 139.8 ± 39.4 10.4 71.7 ± 22.5 19.7<br />
Normal Value: 126.6ug% ±20.6 89.3 ug% ± 9. 5<br />
It is apparent from table 2 that plasma<br />
copper concentration was significantly higher<br />
in sputum positive cases (t=5.61 df=92,<br />
P
182 B.K. KHANNA, et at.,<br />
tically significant (between I & II—1 = 1.77, patients who had improved with the therapy,<br />
df=75, P > 0.05; II & III—1=3.52, df=64, irrespective <strong>of</strong> the therapy administered. Con-<br />
P < 0.001; and I & III—t==3.86, df=43, P < sequently, the values obtained in these patients<br />
0.001). Plasma zinc changes were manifest even are being presented below as a single group,<br />
in patients with one or two zones involvement<br />
as compared to serum copper level which In the patients, who showed improvement<br />
showed no change from normal in these patients due to chemotherapy, plasma copper level<br />
(i.e. those with less than 3 zones involvement). declined from mean value <strong>of</strong> 152.4 ug% to<br />
TABLE 4<br />
Table showing the levels <strong>of</strong> Plasma Copper and Zinc in Relation to Predominant Nature <strong>of</strong> the Lesion<br />
Nature <strong>of</strong> predominant lesion No. <strong>of</strong> patients Plasma Copper Plasma Zinc<br />
Mean (ug%) ± S.D. % rise Mean (ug%) ± S.D. % fall<br />
Exudative 26 149.6 ± 30.4 18 68.9 ± 16.6 21.7<br />
Productive 10 141.9 ± 15.8 12 73.9 ±14.5 17<br />
Cavitary 44 171.9 ± 30 35.8 56.5 ±13.1 37<br />
Fibrotic 12 131 3.5 79.5 ±17.6 11<br />
Miliary 2 192 51.6 61 31<br />
Normal Value : 126.6 ug% ±20.6 89.3 ug% ±9.8<br />
Plasma copper concentration was highest in<br />
cases suffering from miliary tuberculosis. It<br />
showed a rise <strong>of</strong> 51.6% from normal value.<br />
Plasma zinc level was lowest in cavitary cases<br />
and registered a fall <strong>of</strong> 37 % from the normal.<br />
We were unable to find any correlation <strong>of</strong><br />
plasma copper and zinc level with duration <strong>of</strong><br />
disease as reported by the patient (which, no<br />
doubt, was highly subjective), mean temperature<br />
<strong>of</strong> the patients, and the average size <strong>of</strong> the<br />
cavities seen in our cases.<br />
E. Follow up group:<br />
Out <strong>of</strong> a total 94 patients, only 30 patients<br />
stayed in the wards for a period <strong>of</strong> 3 months to<br />
permit us a follow up <strong>of</strong> these patients. They<br />
were administered (S+P+H in 6 cases, S+Tf-H<br />
in 21 cases, S+H+E in 2 cases and S-j-H<br />
in 1 case) four different regimen. 25 <strong>of</strong> them<br />
improved clinically, radiographically and<br />
bacteriologically. On the other hand, 5 <strong>of</strong> them<br />
had remained stationary.<br />
There was no different in plasma copper and<br />
zinc levels between the various sub-groups <strong>of</strong><br />
149.2 ug%, but the difference was not statistically<br />
significant (t=0.43, df=48, P > 0.05).<br />
The level <strong>of</strong> plasma zinc rose with effective<br />
chemotherapy. The rise was found to be significant<br />
(t== 3.10, df=48, P < 0.01). On the other<br />
hand, cases showing no improvement did not<br />
have any significant effect on the plasma zinc<br />
level.<br />
Discussion<br />
Pulmonary tuberculosis affects metabolism<br />
<strong>of</strong> trace elements like any other infectious<br />
disease. High plasma copper and low plasma<br />
zinc concentrations obtained in our cases reflect<br />
only one aspect <strong>of</strong> these disturbances. Similar<br />
observations have been recorded by other<br />
workers too (Tani 1965, Halsted and Smith<br />
1970, Underwood 1971, Beisel, Pekarek,<br />
Wannemacher 1974, Bogden et al 1977), though<br />
some <strong>of</strong> them have highlighted the alterations<br />
in plasma copper level (Tani 1965) while others<br />
have focused attention on the plasma zinc level<br />
(Halsted and Smith 1970). Bogden et al (1977)<br />
have attempted to study both the trace metals<br />
at the same time in proved cases <strong>of</strong> pulmonary<br />
tuberculosis and have come to similar con-<br />
Ind. J. Tub., Vol. XXIX, No. 3
PLASMA COPPER AND ZINC LEVELS IN PULMONARY TUBERCULOSIS<br />
183<br />
TABLE 5<br />
Correlation <strong>of</strong> Plasma Copper ami Zinc Level with Response to Therapy in Follow-up group<br />
(30 Patients)<br />
No. <strong>of</strong> Patients Before treatment Alter 3 months’ treatment<br />
Plasma Cu Plasma Zn Plasma Cu Plasma Zn<br />
Mean<br />
(ug%) ±<br />
S.D.<br />
% Mean rise<br />
(ug %)<br />
± S.D.<br />
% Mean %<br />
fall (ug%) change<br />
±S.D.<br />
Mean<br />
(ug%) ±<br />
S.D.<br />
%<br />
change<br />
Improvement<br />
25 152.4<br />
±25<br />
No Improvement<br />
5 172.4<br />
±8.7<br />
20.3 65.6<br />
±15.7<br />
24 64.6<br />
±36.8<br />
26.5 149.2 2.3<br />
±23 (fall)<br />
27.6 176.5 5.5<br />
±8.8 (rise)<br />
78<br />
±12.3<br />
62<br />
±34<br />
13<br />
(rise)<br />
2.9<br />
(fain<br />
elusions. However, they have raised and left<br />
many questions unanswered, which no doubt,<br />
will have serious bearing on the trace element<br />
metabolism in pulmonary tuberculosis. In this<br />
study we have attempted to answer some <strong>of</strong><br />
these.<br />
Plasma Copper and Zinc<br />
<strong>Tuberculosis</strong><br />
levels in Pulmonary<br />
Rise in plasma copper and fall in plasma<br />
zinc level was recorded in our cases. Both <strong>of</strong><br />
these alterations were found to be statistically<br />
significant. Fall in plasma zinc level was more<br />
pronounced compared to rise in plasma copper<br />
level. Lowering <strong>of</strong> plasma zinc has been considered<br />
to be a more sensitive index <strong>of</strong> tuberculous<br />
infection compared to rise in plasma<br />
copper level (Beisel, Pekarek and Wannemacher<br />
1974). Consequently, Bogden et al<br />
(1977) concluded that low plasma zinc level<br />
with normal plasma copper may mean that<br />
infection is in early stages.<br />
Patients <strong>of</strong> pulmonary tuberculosis, who had<br />
demonstrable acid fast bacilli (A.F.B.) in<br />
sputum smear examination had higher plasma<br />
copper level and lower plasma zinc level compared<br />
to those who did not have A.F.B. in<br />
their sputum smear. This again shows that the<br />
activity <strong>of</strong> the lesion has a direct bearing on<br />
the plasma level <strong>of</strong> these trace elements. The<br />
same was found to be true for patients who had<br />
lesions extending beyond two zones <strong>of</strong> the<br />
lung. Lesionwise, patients with miliary tuberculosis<br />
had highest rise in plasma copper level<br />
and maximum depression <strong>of</strong> plasma zinc level.<br />
These cases were closely followed by patients<br />
having cavities in the lungs. The patients having<br />
predominantly productive lesions had minimal<br />
alterations in plasma level <strong>of</strong> these trace<br />
elements. Those having predominantly<br />
fibrotic lesion did not have any alteration in<br />
their plasma copper level, though slight depression<br />
in their zinc level was seen.<br />
It might, therefore, seem that alterations<br />
in the plasma level <strong>of</strong> these trace elements can<br />
be directly associated with evidence <strong>of</strong> activity<br />
<strong>of</strong> tuberculous lesions which may be direct, for<br />
example, sputum containing acid fast bacilli<br />
or indirect such as nature and extent <strong>of</strong> pulmonary<br />
radiographic lesion. Understandably,<br />
because <strong>of</strong> the highly subjective and variable<br />
factors, no clear cut correlation could be<br />
obtained between plasma level <strong>of</strong> these trace<br />
elements and age and sex <strong>of</strong> patients, duration<br />
<strong>of</strong> illness, temperature <strong>of</strong> patients and size <strong>of</strong><br />
the cavities as observed radiographically.<br />
Alterations noted after 3 months <strong>of</strong> effective<br />
chemotherapy<br />
The patients who had improved following<br />
therapy revealed elevation <strong>of</strong> plasma zinc level<br />
which was more pronounced and more rapid<br />
Ind. J. Tub., Vol. XXIX, No. 3
184 B.K. KHANNA, et al.,<br />
compared to depression in plasma copper level.<br />
Rise in plasma zinc level was found to be<br />
significant though decline in plasma copper<br />
level was not statistically significant. Plasma<br />
zinc level, therefore, appears to be a more<br />
sensitive indicator <strong>of</strong> activity <strong>of</strong> the tuberculous<br />
lesion as compared to plasma copper level.<br />
In patients who did not improve with<br />
chemotherapy, the process <strong>of</strong> rise in the plasma<br />
copper and decline in plasma zinc continued<br />
unabated.<br />
Four schedules <strong>of</strong> chemotherapy were administered<br />
in our patients. Alterations in the<br />
level <strong>of</strong> these trace elements did not appear to<br />
be influenced by the chemotherapy employed.<br />
Indeed it was the improvement in clinical<br />
condition <strong>of</strong> the patients which appeared to be<br />
the only influencing factor.<br />
The more gradual change in the plasma<br />
copper level is consistent with the concept that<br />
a period <strong>of</strong> time is required to allow the liver<br />
to synthesize and release the copper binding<br />
protein, ceruloplasmin (Beisel, Pekarek and<br />
Wannemacker 1974). The persistence <strong>of</strong> high<br />
copper concentrations in contrast to more<br />
rapid return <strong>of</strong> zinc concentration to base line<br />
value could be because <strong>of</strong> relatively long half<br />
life <strong>of</strong> ceruloplasmin (Beisel, Pekarek and<br />
Wannemacker 1974). Tani (1965) has demonstrated<br />
that serial measurements <strong>of</strong> both serum<br />
iron and copper concentrations could not only<br />
serve as an indicator <strong>of</strong> a favourable host<br />
response to chemotherapy but also as an early<br />
sign <strong>of</strong> relapse. Our study has confirmed that<br />
serial measurements <strong>of</strong> plasma copper and,<br />
more importantly, plasma zinc level may serve<br />
as an indirect pointer to the diagnosis <strong>of</strong> tuberculosis,<br />
to the degree <strong>of</strong> tuberculo-toxaemia,<br />
to the extent and nature <strong>of</strong> the pulmonary<br />
involvement and to the favourable response <strong>of</strong><br />
the host to the specific anti tuberculosis therapy.<br />
The role <strong>of</strong> kidneys in retention <strong>of</strong> copper<br />
and increased excretion <strong>of</strong> zinc leading to<br />
alterations in the serum level <strong>of</strong> those trace<br />
elements has not yet been defined.<br />
REFERENCES<br />
1. Beisel W.R., Pekarek R.S., Wannemacker R.W., :<br />
The impact <strong>of</strong> infections disease on trace element<br />
metabolism <strong>of</strong> the host. Trace element metabolism<br />
in animals. Volume 2. Edited by Hoekstra W.G.,<br />
Suttie, J.W., Ganther, H.E. et al. Baltimore,<br />
University Park Press, 1974, pp. 217-240.<br />
2. Bogden, J.D., Lintz, D.I., Joselow, M.M., Charles,<br />
J., and Salaki, J.S. Effect <strong>of</strong> pulmonary tuber<br />
culosis on blood concentrations <strong>of</strong> copper and<br />
zinc, Am. J. Clin. Path.; 1977, 67, 251-256.<br />
3. Halsted, J.A., and Smith J.C. Plasma zinc in health<br />
and diseases, Lancet; 1970, 322-324.<br />
4. Tani P. Serum iron, copper, iron-binding capacity<br />
and marrow hemosiderin in pulmonary tuberculosis,<br />
Ann. Med. Intern. Fenn.; 1965, 54 Suppl. 44, 1.<br />
5. Underwood, F.J. (1971) Trace elements in human<br />
and animal nutrition, New York Academic Press,<br />
1971, pp. 68-73, pp. 214-216.<br />
Ind. J. Tub., Vol. XXIX, No. 3
PLASMA ERYTHOCYTE AND LEUCOCYTE FREE ALPHA AMINO NITROGEN<br />
ALTERATIONS IN PULMONARY TUBERCULOSIS AND EFFECT OF A<br />
GLUCOSE LOAD ON THESE PARAMETERS<br />
S.C. SETH, HARBANS LAL, A.S. SAINI AND M.S. PARMAR<br />
Summary : Plasma, erythrocyte and leucocyte free amino nitrogen (FαAN) levels were estimated<br />
in bacteriologically proved active cases <strong>of</strong> pulmonary tuberculosis, arrested cases and controls<br />
(15 subjects in each ,group). The effect <strong>of</strong> a glucose load on these parameters was also studied. In<br />
active pulmonary tuberculosis, plasma and leucocyte FαAN levels were decreased while erythrocyte<br />
FαAN concentration remained unaltered when compared with the controls and with the group <strong>of</strong><br />
arrested cases. The glucose load led to fall in the levels <strong>of</strong> plasma FαAN in all the three groups. The<br />
possible mechanism (s) for the low levels <strong>of</strong> plasma and leucocyte FαAN in patients with pulmonary<br />
tuberculosis is discussed.<br />
Introduction<br />
In protein calorie malnutrition which is a<br />
condition associated with reduced protein<br />
anabolism, both plasma and leucocyte free a-<br />
amino nitrogen (FαAN) levels are reduced as<br />
compared to normals (Gupta and Agarwal,<br />
1973; Lai ct al 1975). Further, a variety <strong>of</strong><br />
infections are known to alter free amino acid<br />
levels in plasma, the pattern <strong>of</strong> change may<br />
depend upon the type <strong>of</strong> microorganism responsible<br />
for infection (George et al, 1974;<br />
Wannemacher et al, 1975). Serum amino acid<br />
concentration has been shown to be decreased<br />
in pulmonary tuberculosis (Kibrik and Khautina,<br />
1973X However, leucocyte free amino acid<br />
concentration in pulmonary tuberculosis has<br />
not been studied, as yet. It will therefore be<br />
interesting to study both plasma and leucocyte<br />
FαAN concentrations in pulmonary tuberculosis.<br />
It is further planned to see the effect<br />
<strong>of</strong> a glucose load on these parameters since<br />
Jaya Rao and Raghuramulu (1972) found that<br />
after a glucose load, plasma FαAN concentration<br />
is reduced in normal children and that the<br />
reduction is delayed in malnourished subjects.<br />
Material and Methods<br />
Fifteen patients (13 males and 2 females)<br />
in the age group <strong>of</strong> 23 to 40 years except 3 who<br />
were between 50-65 years, having active<br />
pulmonary tuberculosis were selected for the<br />
study. The activity <strong>of</strong> the disease was proved by<br />
positive sputum for acid fast bacilli (AFB) and<br />
by the presence <strong>of</strong> pulmonary lesion radiologically.<br />
All the patients had cough expectoration,<br />
mild to moderate evening rise <strong>of</strong> fever, complaint<br />
<strong>of</strong> generalised weakness and malaise.<br />
The mean hemoglobin concentration <strong>of</strong> the<br />
patients was 10.5il.87g/dl. These patients<br />
also had 15-20% weight loss when compared<br />
with the normal weight for their age and height.<br />
They were not receiving any therapy for at<br />
least 2 weeks prior to study. Another group<br />
included 15 subjects who had earlier taken<br />
antitubercular treatment for at least 18 months<br />
and were not getting medication for two weeks<br />
prior to study. Disease was considered quiescent<br />
after clinical, radiological and repeated<br />
sputum examination which did not reveal any<br />
activity. The mean hemoglobin concentration<br />
<strong>of</strong> this group was 12.4±1.23g/dl which was<br />
comparable with the controls (12.8rtO.95g/dl).<br />
Fifteen apparently normal persons within the<br />
same age group not having any illness or infection<br />
for at least two weeks prior to the study<br />
served as controls.<br />
Fasting venous blood (3-5 ml) was collected<br />
for the estimation <strong>of</strong> free L-amino nitrogen<br />
(FαAN) in plasma, erythrocyte and leucocyte,<br />
in tubes containing heparin as anticoagulant.<br />
Each subject was then orally administered 100 g<br />
<strong>of</strong> D-glucose in 2-3 dl <strong>of</strong> water. Thereafter three<br />
blood samples were collected at 45, 90 and 135<br />
min, respectively. Blood was allowed to sediment<br />
at 4° for 30 min for the seperation <strong>of</strong><br />
plasma, erythrocytes and leucocytes. The<br />
blood was centrifuged at 500g for 5 minutes and<br />
plasma was removed. From the remaining<br />
aliquot erythrocytes and leucocytes were separated<br />
as reported by Gupta and Agarwal (1973).<br />
Plasma, erythrocyte and leucocyte FαAN<br />
concentrations were estimated according to the<br />
principle <strong>of</strong> Goodwin (1968), as reported by<br />
Lai and Agarwal (1974).<br />
Results<br />
Plasma erythrocyte and leucocyte free a-amino<br />
nitrogen (FαAN) concentrations in different<br />
groups :<br />
Fasting plasma FαAN concentration was<br />
49.3±12.38mg/l in normal controls and 50.4±<br />
Departments <strong>of</strong> <strong>Tuberculosis</strong> & Chest <strong>Diseases</strong> and Biochemistry, Medical College, Rohtak-124 001.<br />
Ind. J. Tub., Vol. XXIX, No 3
186 S.C. SETH, HARBANS LAL, A.S. SAINI AND M.S. PARMAR<br />
TABLE 1<br />
Fasting plasma, erythrocyte and leucocyte free α.-amino nitrogen concentrations in normal subjects, patients and arrested<br />
cases <strong>of</strong> pulmonary tuberculosis<br />
(Values are means ± S.D. for 15 subjects in each group.)<br />
Subjects<br />
Free a-amino nitrogen<br />
Plasma (mg/1)<br />
(mg/l)<br />
Erythrocyle<br />
Leucocyte<br />
(µ.g/10 8 colls)<br />
Controls 49.3 ± 12.38 105.2 ± 38.33 4.40 ± 1.10<br />
Patients 37.6 ± 4.48* 97.3 ± 28.84 2.93 ± 0.56**<br />
Arrested 50.4 ± 7.18 109.7 ± 32.14 3.70 ± 0.82<br />
* P < 0.001 when patients compared with the controls and treated cases. ** P < 0.001 when patients compared<br />
with the controls and < 0.01 when compared with the group <strong>of</strong> treated<br />
subjects.<br />
The erythrocyte FαAN concentrations at<br />
7.18 mg/1 in a group <strong>of</strong> treated cases.-The<br />
various times remained unaltered in the different<br />
levels in the two groups were comparable with each groups studied (P>0.05; fig 2).<br />
other. In patients with pulmonary tuberculosis the<br />
value was lowered to 37.6±4.48 mg/1, the decrease<br />
being statistically significant when compared with<br />
the other two groups (P
PLASMA ERYTHROCYTE ALTERATIONS 187<br />
reduced when compared with the controls<br />
(P
188 S.C. SETH, HARBANS LAL, A.S. SAINI AND M.S. PARMAR<br />
condition with enhanced protein catabolism<br />
and neoglucogensesis. The findings <strong>of</strong> low<br />
FαAN in leucocyte in a protein catabolic<br />
process like tuberculosis would mean that<br />
leucocyte like muscle may also participate in<br />
transferring amino acids to liver for neoglucjjenesis.<br />
Similar observations have been made<br />
in protein calorie malnutrition where again<br />
low FαAN levels in leucoyte have been explained<br />
because <strong>of</strong> the protein catabolic state<br />
resulting in transfer <strong>of</strong> amino acids from<br />
leucocyte to liver (Lai et al, 1979). Beisal (1972<br />
and 1975) reported that infection is associated<br />
with low insulin/glucagon ratio which is likely<br />
to promote neoglucogenesis and it may also<br />
be a reason for increased neoglucogenesis<br />
observed in tuberculosis. The erythrocyte did<br />
not show any change in FαAN levels meaning<br />
thereby that unlike leucocytes, erythrocytes<br />
do not participate in protein catabolic response,<br />
since erythrocyte is insulin insensitive cell.<br />
Erythrocyte amino acid levels were not found<br />
to be significantly altered with the food intake<br />
whereas plasma amino acid levels were reduced<br />
(Elwyn, 1966).<br />
As shown in Table II, glucose load in different<br />
groups led to reduction in the levels <strong>of</strong><br />
plasma FαAN. However, FαAN levels in<br />
erythrocytes and leucocytes were not affected<br />
(figs 2 and 3). It was also interesting that the<br />
response was slightly delayed in patients. Reduction<br />
in plasma amino acid levels in healthy<br />
individual after a glucose load has been reported<br />
by several workers (Munro and Thompson,<br />
1953; Swendseid et al, 1967; Adibi et al, 1975).<br />
Potter et al (1972) suggested that glucose depletes<br />
plasma free amino acids by promoting the<br />
cellular uptake <strong>of</strong> amino acids with or without<br />
protein synthesis. The delayed response in<br />
plasma FαAN in patients with tuberculosis<br />
may be a result <strong>of</strong> delayed insulin response in<br />
these patients.<br />
REFERENCES<br />
1. Adibi, S.A., Morse, E.L. and Amin. P.M. : Role <strong>of</strong><br />
insulin and glucose in the induction <strong>of</strong> hypoaminoacidemia<br />
in man: Studies in normal juvenile diabetic<br />
and insuloma patients. J. Lab, Clin. Med. 1975,<br />
85, 395.<br />
2. Beisel, W.R. : Interrelated changes in host metabolism<br />
during generalised infectious illness. Am. J.<br />
Clin. Nutr. 1972, 25, 1254.<br />
3. Beisel, W.R. : Metabolic response to infection.<br />
Am. Rev. Med. 1975, 26, 9.<br />
4. Elwyn, D.H. : Distribution <strong>of</strong> amino acids between<br />
plasma and red blood cells in the dog. Fe.i. Prar.<br />
1965, 25, 854.<br />
Ind, J. Tub., Vol. XXIX, No. 3<br />
5. George, D.T., Rayfield, R.J. and Wannamacher,<br />
R.W.. Jr. : Altered glucoregulatory hormones<br />
during acute pneumococcal sepsis in Rhesus<br />
monkey. Diabetes 1974, 15, 544.<br />
6. Goodwin, J.F. : The calorimetric estimation <strong>of</strong><br />
plasma amino nitrogen with DNFB. Clit,. Chem.<br />
1968, 14. 1080.<br />
7. Gupta, M. and Agarwal, K.N. : Free amino acid<br />
patterns <strong>of</strong> plasma erythrocyte and leucocyte<br />
in hypoproteinemia. Br. J. Nutr. 1973, 29, 151.<br />
8. Java Rao, K.S. and Raghuramulu, N.: Insulin<br />
secretion in Kwashiorkor. ,7. Clin. Entiocrinol.<br />
Met’,b. 1972, 35, 62.<br />
9. Kibrik, D.S. and Khautina, F.S. : Fiee amino acid<br />
contents in blood during pulmonary tuberculosis.<br />
Sov. Med. Rnssian (Eng. Tranf.) 1973, 36, 146.<br />
10. Lai, H. and Agarwal, K.N. : Influence <strong>of</strong> hormones<br />
on free alpha amino nitrogen alterations in plasma<br />
erythrocyte and leucocyte in rats. Nutr. Metab.<br />
1974, 17, 148.<br />
11. Lai, H., Agarwal, K.N. And Shanker, R. : Changes<br />
in free alpha amino nitrogen and nucleic acid<br />
patterns in protein deficient rats. Indian J. Expt.<br />
Biol 1975, 13, 19.<br />
12. Lai, H., Saini, A.S., Yadav, N.S. and Dhatt, P.S. :<br />
Free alpha amino nitrogen levels in protein calorie<br />
malnutrition Proc. Nutr. So.. India 1979, 23, 39.<br />
13. Munro, H.N. and Thompson, W.S.T. : Influence<br />
<strong>of</strong> glucose on amino acid metabolism. Metabolism<br />
1953, 2, J54.<br />
14. Potter, E.L., Purser, D.B. and Bergen. G.W.: Plasma<br />
reference index for predicting limiting amino<br />
acids <strong>of</strong> sheep and rats. J. Anim. Sci. 1972, 34, 650.<br />
15. Swendseid, M.E., Juttle, S.G., <strong>Dr</strong>enick, G.J., Joven,<br />
C.B. and Massay, F.J. : Plasma amino acid response<br />
to glucose administration in various nutritive<br />
states. Am. J. Cliv. Nutr. 1967, 20, 243.<br />
16. Wannemacher, R.W., Jr., Pekerck, R.S., Bertalloni,<br />
P.J., Vollmer, R.J. and Beisel, R.W. . Changes<br />
in plasma amino acids following experimentally<br />
induced sandfly fever virus infection. Metabolism<br />
1972, 21,67.<br />
17. Wannemachsr, R.W., Jr., Dinterman, R.E., Perkerck,<br />
R.S., Bertalloni, P.J. and Beisel, W.R. :<br />
Urinary amino acid excretion during experimentally<br />
induced sandfly fever in map. Am. J. Clw.<br />
Nutr. 1975, 28, 110.<br />
-
SERUM MUCOPROTEIN (TYROSINE) LEVEL AND LACTIC DEHYDROGENASE<br />
ACTIVITY IN CHILDHOOD TUBERCULOSIS*<br />
S.D. SINGH** AND N.M. JAIN***<br />
Summary : Mucoprotein (tyrosine) levels and lactic dehydrogenase activity were estimated in the<br />
serum <strong>of</strong> fifty children suffering from tuberculosis and 10 healthy controls. It was observed that various<br />
types <strong>of</strong> childhood tuberculosis showed raised values <strong>of</strong> serum mucoprotein ranging from 9.5 to<br />
139 mgm% with maximum rise incases <strong>of</strong> tuberculous pleural effusion. Lactic dehydrogenase<br />
activity was also increased ranging from 132 to 560 I.U., with maximum rise in cases <strong>of</strong> tuberculous<br />
meningitis.<br />
Introduction and Review<br />
The prevalence <strong>of</strong> childhood tuberculosis is<br />
still high in India. Various authors have reported<br />
14 to 17 % <strong>of</strong> total admissions in hospital<br />
being due to tuberculosis. However, the prevalance<br />
<strong>of</strong> the disease is much more than can<br />
be presumed from hospital admissions. Early<br />
detection <strong>of</strong> cases and their proper management<br />
is necessary to prevent serious complications <strong>of</strong><br />
the disease which otherwise may endanger<br />
life <strong>of</strong> these children. The authors in their<br />
study <strong>of</strong> measles cases found that those cases<br />
<strong>of</strong> measles which were associated with tuberculosis<br />
had significantly higher levels <strong>of</strong> serum<br />
mucoprotein (tyrosine). It was therefore planned<br />
to study the changes in serum mucoprotein<br />
(Tyrosine) in childhood tuberculosis, since<br />
authentic information about it is lacking so<br />
far.<br />
Mucoproteins are polypeptides <strong>of</strong> high<br />
molecular weight and are an important constituent<br />
<strong>of</strong> the ground substance <strong>of</strong> connective<br />
tissue. Tyrosine constitutes 4-2% fraction <strong>of</strong><br />
mucoproteins. The exact physiological significance<br />
<strong>of</strong> this fraction is not known. Variations<br />
in serum mucoprotein level have been reported<br />
in various disorders. According to Greenspan<br />
(1965) total mucoprotein levels are lowered in<br />
impaired hepatic function and endocrine functions,<br />
while inflammatory, neoplasic and traumatic<br />
changes tend to increase the mucoprotein<br />
levels. The number <strong>of</strong> cases studied were Malnutrition<br />
19, Diabetes 18, Rheumatism 13, renal<br />
disorders 16, Indian childhood Cirrhosis 14 and<br />
Measles 17. Elevated levels <strong>of</strong> total serum<br />
mucoprotein in tuberculosis in adults have<br />
been reported by Pilheu et al (1962). They<br />
have also described changes in various types<br />
<strong>of</strong> tuberculosis which revert to normal<br />
with regression <strong>of</strong> disease, in these cases. However,<br />
studies in childhood are lacking.<br />
Lactic dehydrogenase (LDH) was first discovered<br />
by Meyerh <strong>of</strong> in 1979. Lactic dehydrogenase<br />
is an intracellular glycolytic enzyme<br />
which catalyses the reversible reduction <strong>of</strong><br />
alpha keto and alpha and gamma di keto acids<br />
to their corresponding hydroxy acids in the<br />
presence <strong>of</strong> reduced nicotinamide adenine<br />
dinucleotide. Normal value <strong>of</strong> serum lactic<br />
dehydrogenase varies from 50-150 L.U. in older<br />
children and 300 to 1500 in newborn (Nelson,<br />
1975 and Pohowala, 1973) L.D.H. is very<br />
widely distributed in body tissues like brain,<br />
liver, lymph nodes, kidney, heart, lung, erythrocytes,<br />
leucocytes and is also present in cerebrospinal<br />
fluid and serum (Abderhalden, 1961).<br />
Lactic dehydrogenase activity in serum is<br />
markedly elevated in patients with megaloblastic<br />
anaemia, acute leukemia, urinary tract<br />
infection, pulmonary embolism, pulmonary<br />
tuberculosis in adults, tubercular meningitis<br />
(Amader and Pochen, 1966; Agrawal, 1968;<br />
Zimmermann and Henry, 1969: Brijkishore and<br />
Nagrath, 1970).<br />
Material and Methods<br />
* Paper presented at 3rd Asian Congress <strong>of</strong> Paediatrics at Bangkok.; 1979.<br />
** Pr<strong>of</strong>. & Head, Department <strong>of</strong> Paediatrics<br />
*** Asstt. Surgeon, Distt. Narsinghpur, M.P.<br />
(From the Department <strong>of</strong> Paediatrics, M.G.M. Medical College, Indore).<br />
50 children suffering from childhood tuberculosis<br />
were taken up for this study. 15 cases<br />
had uncomplicated primary tuberculosis, 10<br />
cases had bronchogenic tuberculosis, 5 cases<br />
were <strong>of</strong> plural effusion, 10 cases <strong>of</strong> collapse<br />
with consolidation and 10 were <strong>of</strong> tuberculous<br />
meningitis. 10 healthy controls in the same age<br />
groups were concurrently taken.<br />
Routine investigations like total and differential<br />
count, blood E.S.R. tuberculin test and<br />
X-ray chest were done. Total serum proteins<br />
and its fractions were also analysed. Serum<br />
mucoprotein (tyrosine) was estimated by modified<br />
Winzler method (Winzler et al 1948). Estimation<br />
<strong>of</strong> serum lactic dehydrogenase activity<br />
Ind. J. Tub., Vol. XXIX, No. 3
190 S.D. SINGH AND N.M. JAIN<br />
was made by calorimetric method <strong>of</strong> Cabaud<br />
and Wroblewski (King, 1959).<br />
There was no case below the age <strong>of</strong> one year,<br />
(Table 1).<br />
Observations<br />
The total proteins in controls ranged between<br />
TABLE 1<br />
Showing Age & Sex Distribution <strong>of</strong> Cases in Various Types <strong>of</strong> Childhood <strong>Tuberculosis</strong><br />
*<br />
No. Types <strong>of</strong> tuberculosis Total No. Sex Distribution Age-Wise Distribution <strong>of</strong><br />
cases Male Female 0-1 yr. 1-5 yrs. about 5<br />
1. Primary tuberculosis 15 8 7 1 14<br />
2. <strong>Tuberculosis</strong> Broncho-Phenomena 10 7 3 1 6 3<br />
3. Tuberculous pleural effusion 5 3 2 2 3<br />
4. Tuberculous collapse consolidation 10 5 5 2 5 3<br />
5. Tuberculous meningitis 10 6 4 8 2<br />
Total 50 29 21 4 35 11<br />
TABLE 2<br />
Showing Mean Levels <strong>of</strong> Serum Proteins in Various Types <strong>of</strong> Childhood <strong>Tuberculosis</strong><br />
SI.<br />
No.<br />
Types <strong>of</strong> cases<br />
Total proteins<br />
(In gms%)<br />
Albumin<br />
(In gms%)<br />
Globulin<br />
(In gms%)<br />
A/G Ratio<br />
1. Controls 6.12 3.05 2.80 1.04<br />
2. Primary tuberculosis 5.80 2.71 3.27 0.77<br />
3. Tubercular Broncho pneumonia 6.10 2.40 3.60 0.73<br />
4. Tubercular Pleural effusion 6.90 2.30 4.60 0.53<br />
5. Tubercular collapse consolidation 5.80 2.20 3.50 0.64<br />
6. Tuberculous meningitis 5.70 2.10 3.60 0.59<br />
Discussion 6-6.5 gms. %, with an average <strong>of</strong> 6.12 gms %.<br />
In tuberculosis cases it ranged between 4-7.8<br />
Out <strong>of</strong> the 50 children included in this study, gms%. The albumin fraction had lower values<br />
35 were in the age group <strong>of</strong> 1 to 5 years and in all types <strong>of</strong> cases. The globulin fraction<br />
only four were, below the age <strong>of</strong> one year, showed elevated levels as compared to controls.<br />
29 <strong>of</strong> these children were males and 21 were This type <strong>of</strong> change in total proteins and its<br />
females. There were 8 cases <strong>of</strong> tuberculous fractions was also described by Seibett and<br />
meningitis between the age <strong>of</strong> one to five years. Nelson (1947).<br />
Ind. J. Tub., Vol. XXIX, No. 3
SERUM MUCOPROTEIN (TYROSINE) LEVEL AND LACTIC -DEHYDROGENASE<br />
TABLE 3<br />
Showing Mean Levels <strong>of</strong> Serum Mucoprotein (Tyrosine) and Lactic Dehydrogenase Activity in various types<br />
<strong>of</strong> Childhood <strong>Tuberculosis</strong>.<br />
SI.<br />
No.<br />
Types <strong>of</strong> cases<br />
Serum Mucoprotein (Tyrosine)<br />
(in mgm %)<br />
Serum lactic Dehydrogenase<br />
(in I.U.)<br />
1. Control 5.02 130.8<br />
2. Primary <strong>Tuberculosis</strong> 17.52 170.0<br />
3. Tubercular Broncho-pneumonia 83.20 359.0<br />
4. Tubercular pleural effusion 126.00 297.5<br />
5. Tubercular collapse consolidation 46.70 260.6<br />
6. Tubercular meningitis 55.70 367.4<br />
Mucoprotein (tyrosine) values in normal<br />
cases ranged between 2.4-7.6 mgms. % with an<br />
average <strong>of</strong> 5.02 rag. % and lactic dehydrogenase<br />
activity in serum in normal persons ranged<br />
between 102 to 216 I.U., with a mean level <strong>of</strong><br />
130.8 I.U.<br />
Mucoprotein (tyrosine) fraction was increased<br />
in all clinical types <strong>of</strong> childhood tuberculosis,<br />
but the increase was not uniform in<br />
all types. In cases <strong>of</strong> uncomplicated primary<br />
tuberculosis values ranged between 9.5-26.5<br />
mgms. % with an average <strong>of</strong> 17.52 mgms. % ±<br />
5.5. In the other forms <strong>of</strong> tuberculosis, Mucoprotein<br />
values were substantially raised as<br />
follows:<br />
Tuberculous<br />
Broncho-pneumonia —71-96mgm%, average<br />
83, 20mgm% ± 9.(<br />
Pleural Effusion<br />
Collapse<br />
consolidation<br />
— lll-139mgms%, averagel26%mgm<br />
; ± 12.:<br />
—31-58 mgm%, average<br />
46.70mgm% ± 10.95<br />
TB Meningitis —42-69mgm%, average<br />
55.70 mgm% ± 9.40<br />
It would be seen that the values were highest<br />
in cases <strong>of</strong> pleural effusion. Table 2 will show<br />
that the serum globlin level was also highest<br />
(4.60 gm%) in pleural effusion. In other words,<br />
mucoprotein level follows the level <strong>of</strong> serum<br />
globlin since mucoprotein (tyrosine) goes with<br />
a 2 globlin fraction <strong>of</strong> the serum. Mucoprotein<br />
levels are increased usually following infection,<br />
destruction <strong>of</strong> collagen tissue and involvement<br />
<strong>of</strong> the liver. Factors which may be responsible<br />
for the maximum increase in cases <strong>of</strong> pleural<br />
effusion are not known.<br />
There is also a suggestion <strong>of</strong> a possible<br />
correlation between mucoprotein level and<br />
severity <strong>of</strong> tuberculous disease, since the mucoprotein<br />
level is lowest in uncomplicated primary<br />
tuberculosis as compared to the other more<br />
severe forms <strong>of</strong> tuberculosis.<br />
Serum lactic dehydrogenase levels were also<br />
increased in tuberculous cases. The values in<br />
different manifestations were as follows (Table 3):<br />
Primary <strong>Tuberculosis</strong><br />
(uncomplicated)<br />
—132-236 IU, average<br />
170 ± 32.6<br />
Tuberculous<br />
Broncho-pneumonia —280-492 IU, average<br />
359 IU ± 74.3<br />
Pleural Effusion<br />
Collapse<br />
Consolidation<br />
TB Meningitis<br />
—272-336 IU. average<br />
297.5 IU ± 27.7.<br />
—148-396 IU, average<br />
260.6 IU ± 66.4<br />
—272-460 IU. average<br />
367.4 IU ± 56<br />
Lactic dehydrogenase values depend on its<br />
Ind. J. Tub., Vol. XXIX, No.3
192 S.D. SINGH AND N.M. JAIN<br />
release from damaged tissue because <strong>of</strong> changes<br />
in cellular permeability. In 63 to 100% cases<br />
<strong>of</strong> post-primary tuberculosis, liver is involved.<br />
This being a source <strong>of</strong> LDH activity, increased<br />
values are seen in pulmonary disease. Since<br />
brain is the richest source <strong>of</strong> LDH, maximum<br />
LDH activity in cases <strong>of</strong> TB Meningitis may<br />
be due to its increase in the CSF. This view is<br />
supported by Aronson (1966) and Jain (1976).<br />
REFERENCES<br />
1. Abderhalden, R. : Clinical Enzymalogy, B.K.<br />
Onmort and Company, INC, 1961.<br />
2. Agrawal, R.K. : Observations on pleural effusion<br />
with special reference to enzyme study and pleural<br />
biopsy. Thesis for M.D. (Medicine) University<br />
<strong>of</strong> Indore, 1968.<br />
3. Amader, E., Pochen, E.J. Serum Lactic dehydrogenase<br />
activity and radio active scanning in diagnosis<br />
<strong>of</strong> pulmonary embolism. Ann. Intern. Med.<br />
1966, 65, 1247.<br />
4. Aronson, M.B. : Enzyme determination in neurological<br />
and neuromuscular disorders <strong>of</strong> infancy<br />
and childhood. Paed. Clin. North. America. 1966,<br />
7:527.<br />
5. Brijidshore, Nagrath, S.P.: Serum and pleural fluid<br />
lactic dehydrogenase activity in tuberculous pleural<br />
effusion. The J. <strong>of</strong> Ase. Phy. Ind. 1970, 18:15.<br />
6. Greenspan, E.M. ; Clinical significance <strong>of</strong> serum<br />
mucoprotein. Adv. Int. Med., 19o5, 7:101.<br />
7. Jain, N.N. : Serum L.D.H. activity in childhood<br />
tuberculosis thesis for M.D. (Paed.) University<br />
<strong>of</strong> Indore, 1976.<br />
8. King, E.L. : Routine methods for estimation <strong>of</strong><br />
L.D.H. Activity. J.M. Lab. Tach. 1959, 16:26.<br />
9. Nelson : Text book <strong>of</strong> Paediatrics, 1975. W.B.<br />
Saunders and Co.<br />
10. Pilheu, K.A. Lannello, J.A. Wilson, J. : Serum<br />
proteins in Pulmonary tuberculosis. Dis. <strong>of</strong> Chest<br />
1962, 41:173.<br />
11. Pohowalax, P. : Serum L.D.H. activity in newborn,<br />
Thesis for M.D. (Paed.) University <strong>of</strong> Indore,<br />
1973.<br />
12. Seibett, F.B. Nelson, J.M. : Serum proteins in<br />
tuberculosis. Am. Rev. Tub. 1974, 47:66.<br />
13. Singh, S.D. Chhaparwal, B.C. Deshpande, J. : Serum<br />
Mucoprotein (Tyrosine) in rheumatism, Ind. Jour,<br />
<strong>of</strong> Paed., 1971, 38:32.3.<br />
14. Sineh, S.D. Khan, M.A. Dabke, A.T. Chhaparwal,<br />
B.C. : Serum Mucoprotein (tyrosine) in Indian<br />
Childhood Cirrhosis, Paed. Clin. Ind., 1973. Jan, 51.<br />
15. Singh, S.D. Bhagwat, C. Kutumbale, A, : Serum<br />
Mucoprotein (tyrosine) in protein calories<br />
Malnutrition. Paed. Clin. Ind., 1975, 10:117<br />
16. Singh, S.D. Mehta, S. Chhaparwal, B.C. Khan.<br />
M.A. : Serum mucoprotein levels in acute<br />
glomerulonephritis and nephrotic syndromes in<br />
children. The Indian Practitioner, 1975, Sept., 564.<br />
17. Singh, S.D. Parekh, P. Jain N.N. : Serum Mucoprotein<br />
(tyrosine) in meagles. Paed. Clin. India,<br />
1976, Oct. 205.<br />
18. Singh, S.D. Pathak, R. Kutumbale, A. Ramnani,<br />
R.O. : Serum mucoprotein (tyrosine) in diabetes<br />
mellitus. Jour. Diab. Asso. Ind., 1977, 17:27.<br />
19. Winzler, R.J. Devom, A.N. Mehli, J.W. Smythe,<br />
I.M. : Studies in mucoprotein in human plasma,<br />
its determination and isolation. Clin. Invast, 1948,<br />
27:609.<br />
20. Zimmermann, M.G. Henry, J.B. : Serum enzyme<br />
estimation as an aid to diagnosis. Clinical Diagnosis,<br />
W.B. Saunders Co. Philadelphia. P.p. 558,<br />
1969.<br />
Ind. J. Tub., Vol. XXIX, No. 3
Introduction<br />
POSTERIOR FOSSA CYSTIC ARACHNOIDITIS : AN UNCOMMON<br />
PRESENTATION OF NEURO-TUBERCULOSIS<br />
V.K. SRIVASTAVA and G.N.N. REDDY<br />
Summary : Thirty cases <strong>of</strong> posterior fossa cystic arachnoiditis were studied over a period <strong>of</strong> three<br />
years. Out <strong>of</strong> these, nine cases showed evidence <strong>of</strong> tuberculous pathology. It is these nine cases, where<br />
neurotuberculosis presented in form <strong>of</strong> a pseudocyst, which form the basis <strong>of</strong> this presentation. Their<br />
clinical pr<strong>of</strong>ile and clinico-radio-pathological correlation is being presented.<br />
In literature, various presentations <strong>of</strong> neurotuberculosis<br />
have been described. We are presenting<br />
nine cases, where the patients presented<br />
with symptoms and signs <strong>of</strong> raised intracranial<br />
pressure with localisation to posterior fossa.<br />
At surgery, arachnoid at cisterna magna was<br />
found to be thickened and ballooned. For the<br />
present communication, posterior fossa cystic<br />
arachnoiditis is defined as a pseudocyst, formed<br />
by adhesions around cisterna magna. In literature,<br />
various terms like posterior fossa meningitis<br />
and arachnoiditis with cerebellar syndrome, have<br />
been used. In earlier part <strong>of</strong> the century, Horrax<br />
(1924) and Craig (1932) described similar cases.<br />
In recent literature, there has been a dearth <strong>of</strong><br />
such reports.<br />
female patients (Table IV). Six patients presented<br />
with less than six months’ duration,<br />
whereas the rest presented with a history <strong>of</strong><br />
one year or more. Most <strong>of</strong> the patients presented<br />
with symptoms <strong>of</strong> headache, vomiting<br />
and seizures. Of the six patients who presented<br />
with seizures, three had focal and three had<br />
generalised seizures. Four patients had history<br />
<strong>of</strong> fever in the present illness (Table 1). Only<br />
one patient gave a past history, suggestive <strong>of</strong><br />
pulmonary tuberculosis.<br />
Symptom<br />
TABIH 1<br />
Symptomatology<br />
Number <strong>of</strong><br />
Cases<br />
Material and Method<br />
Arachnoid was studied from thirty cases <strong>of</strong><br />
posterior fossa cystic arachnoiditis. Tissue<br />
culture or staining <strong>of</strong> tissue section for demonstration<br />
<strong>of</strong> acid fast bacilli was not done in<br />
any <strong>of</strong> the cases. The diagnosis <strong>of</strong> tuberculous<br />
arachnoid was made on presence <strong>of</strong> all or any<br />
<strong>of</strong> the following histological criteria.<br />
(a) Presence <strong>of</strong> caseation necrosis.<br />
(b) Presence <strong>of</strong> typical Langhans giant cells.<br />
(c) Presence <strong>of</strong> follicles made up <strong>of</strong> epitheloid<br />
cells and mononuclear cellular<br />
aggregation.<br />
On histological grounds, nine cases were<br />
found to be tuberculous. These nine cases<br />
were analysed in retrospect. A clinicoradiopathological<br />
correlation was attempted.<br />
Findings<br />
Clinical features<br />
Headache 8<br />
Vomiting 7<br />
Seizures f.<br />
Fever 4<br />
Unsteadiness <strong>of</strong> gait 4<br />
Giddiness 3<br />
Double vision 2<br />
Blurring <strong>of</strong> vision 1<br />
Diminished vision 2<br />
Deafness 1<br />
Excessive sleep 1<br />
Altered sensorium 5<br />
Four out <strong>of</strong> nine cases were in the paediatric<br />
age group. Seven were males and two were<br />
General Physical Examination did not reveal<br />
any significant findings. Objectively, five cases<br />
*Department <strong>of</strong> Neurosurgery, National <strong>Institute</strong> <strong>of</strong> Mental Health and Neuro Sciences (NIMHANS)<br />
Bangalore-560 029.<br />
Ind. J. Tub., Vol. XXIX, No. 3
194 V.K. SRIVASTAVA AND G.N.N. REDDY<br />
presented with altered sensorium, out <strong>of</strong> which<br />
one was unconscious and decerebrating at the<br />
time <strong>of</strong> admission. Of the seven patients with<br />
fundal changes, six had bilateral florid papilloedema,<br />
whereas one presented with Foster-<br />
Kennedy syndrome. Three patients out <strong>of</strong> nine<br />
were nearly blind. Gait disorders in five patients<br />
were in form <strong>of</strong> a broad-based gait with difficulty<br />
in tandem walking (Table II). All the<br />
nine cases had symptoms and signs <strong>of</strong> raised<br />
intracranial pressure. Five out <strong>of</strong> these nine<br />
cases presented with symptoms and signs <strong>of</strong><br />
raised intracranial pressure alone without any<br />
localisation. Two cases had a definite localisation<br />
to posterior fossa. One case suggested a<br />
diffuse lesion and one had a false localisation to<br />
supratentorial compartment (Table IV).<br />
Erythrocytic sedimentation rate was high<br />
in five cases. Other blood investigations were<br />
well within normal limits. Ventricular CSF<br />
obtained at the time <strong>of</strong> ventriculography was<br />
subjected to biochemical analysis (Table 111).<br />
Cellular reaction was found in seven cases,<br />
which was predominantly lymphocytic. C.S.F.<br />
was not examined for acid fast bacilli as there<br />
was no clue to tuberculous etiology before<br />
operation.<br />
Physical signs<br />
TABLE II<br />
Physical Signs<br />
Number <strong>of</strong> Cases<br />
Altered sensorium at the time <strong>of</strong> admission 5<br />
Neck* stiffness 4<br />
Fundal changes 7<br />
Changes in visual acuity 3<br />
Other cranial nerve deficits 3<br />
Pyramidal involvement 1<br />
Nystagmus<br />
Truncal ataxia 3<br />
Hypotonia 2<br />
Inco ordination 3<br />
Gait disorders 5<br />
C<br />
TABLE III<br />
Analysis <strong>of</strong> Ventricular C.S.F.<br />
SI. No. Cell Count Types <strong>of</strong> cells Protein mg% Chloride mg% Glucose ing% Globulin<br />
1 16<br />
*100<br />
°L<br />
L<br />
40<br />
190<br />
720<br />
QNS<br />
40<br />
QNS<br />
+<br />
2 18 L 7 680 42 Absent<br />
3 41<br />
*333<br />
L L 20<br />
350<br />
760<br />
QNS<br />
44<br />
QNS<br />
Absent<br />
4 0 — 20 760 46 Absent<br />
5 45 L 8 720 40 +<br />
6 45 L 7 700 20 +<br />
7 0 — 20 700 43 Absent<br />
8 12 L 38 QNS 32 Absent<br />
9 2 *8 L L 9<br />
250<br />
720<br />
700<br />
40<br />
34<br />
Absent<br />
Ind. J. Tub., Vol. XXIX, No. 3
POSTERIOR FOSSA CYSTIC ARACHNOIDITIS 195
196 V.K. SRIVASTAVA AND G.N.N. REDDY<br />
Fig. 1 (a and b)<br />
Conray Ventriculogram showing symmetrical dilatation <strong>of</strong> whole ventricular system, including the fourth ventricle.<br />
Radiological features<br />
X-ray skull showed evidence <strong>of</strong> raised<br />
intracranial pressure in only one case. X-ray<br />
chest showed evidence <strong>of</strong> primary complex in<br />
only one case. Carotid angiography showed<br />
ventricular dilatation in seven cases.<br />
Ventriculography showed aqueductal block<br />
in two cases. Total fourth ventricular exit<br />
block was found in six cases. In one case, the<br />
block was partial (Table IV). Symmetrical<br />
dilatation <strong>of</strong> whole ventricular system including<br />
fourth ventricle was found in six cases (Fig. 1).<br />
In three cases, an irregular filling defect was<br />
found (Fig. 2). In one case, no pattern seemed<br />
to emerge.<br />
Operative findings<br />
Posterior fossa craniectomy was done in all<br />
cases. At surgery, the dura was found to be<br />
tense. After opening dura, cisterna magna area<br />
was found to be ballooned. The pseudocyst<br />
was found to be indenting the inferior vermis<br />
and in some cases, adjacent cerebellar hemi-<br />
Ind. J. Tub., Vol. XXIX, No. 3<br />
spheres. Arachnoid in the region <strong>of</strong> cisterna<br />
magna was found to be thickened and opaque.<br />
It was adherent to the underlying cerebellum.<br />
After excising arachnoid, cerebellum became<br />
lax and pulsatile. C.S.F. flow could be established<br />
in all the cases.<br />
Histopathology<br />
Histopathology showed thickened arachnoid<br />
with varying degree <strong>of</strong> cellular reaction (Fig. 3).<br />
Frank caseation necrosis was found in three<br />
cases (Fig. 4) (Table IV).<br />
Prognosis<br />
Four out <strong>of</strong> nine patients died. Of five<br />
surviving patients, three are normal after a<br />
follow up <strong>of</strong> ten, eleven and nineteen months<br />
respectively. One patient looked sick one month<br />
after discharge and was found to have jaundice.<br />
One patient, two months later, was found to<br />
have residual deficits, in the form <strong>of</strong> ataxia.<br />
left facial (L.M.N) palsy and left conjugate<br />
gaze palsy.
POSTERIOR FOSSA CYSTIC ARACHNOIDITIS 197<br />
\<br />
>*•<br />
Fig 2 (a and b)<br />
Conray ventriculogram showing irregular filling defect in fourth ventricle.<br />
Fig. 3<br />
Photomicrograph showing presence <strong>of</strong> follicles<br />
tuberculous arachnoid (H and E x 25).<br />
Autopsy findings<br />
Out <strong>of</strong> four deaths, autopsy was available<br />
in two cases (cases 8 and 9). Brain in both the<br />
cases showed evidence <strong>of</strong> basal exudates.<br />
in<br />
Photomicrograph showing evidence <strong>of</strong> caseation necrosis<br />
in tuberculous arachnoid (H x B x 25).<br />
Adhesions were found at the foremen magendie<br />
area, blocking the fourth ventricular exit.<br />
Both the cases showed evidence <strong>of</strong> ventricular<br />
dilatation. In one case basilar artery showed<br />
Ind. J. Tub., Vol. XXIX, No. 3
198 V.K. SRIVASTAVA AND G.N.N. REDDY<br />
Since lumbar puncture could not be done<br />
in any <strong>of</strong> these cases in view <strong>of</strong> raised intracranial<br />
pressure, it is interesting to note the<br />
ventricular C.S.F. findings. Predominently<br />
lymphocytic reaction suggests a chronic inflammatory<br />
pathology. C.S.F. analysis from the<br />
pseudocyst, though available only in three<br />
cases, suggests that the pathology is more<br />
active in that area. It is clearly evidenced by<br />
higher cellular count and protein values as<br />
compared to their corresponding ventricular<br />
C.S.F. analysis (Table III).<br />
Ventriculographic rinding <strong>of</strong> obstructive<br />
hydrocephalus due to tuberculous etiology has<br />
been well-documented. Sifontes, Sabeti and<br />
Sorvidillo (1957) showed pneumoencephalographic<br />
evidence <strong>of</strong> 4th ventricular exit block<br />
in one <strong>of</strong> their cases. Dastur and Pandya<br />
(1972) while describing cases <strong>of</strong> tuberculous<br />
meningitis, showed 22 cases with 4th ventricular<br />
exit block and 10 cases with aqueductal<br />
block. Tandon, P.N. (1978) has also described<br />
cases <strong>of</strong> obstructive hydrocephalus in tuberculous<br />
meningitis.<br />
Fig. 5<br />
Autopsy specimen to demonstrate basal exudative<br />
reaction.<br />
an almost total occlusion <strong>of</strong> lumen due to<br />
endarteritis. Some <strong>of</strong> the cranial nerves were<br />
found to be trapped in the mesh <strong>of</strong> exudate<br />
(Fig. 5). Microscopy confirmed the tuberculous<br />
pathology in both cases.<br />
Discussion<br />
In earlier part <strong>of</strong> the century, Horrax (1924)<br />
and Craig (1932) described cases <strong>of</strong> cystic<br />
arachnoiditis. They considered an infective<br />
aetiology for their cases. The exact nature <strong>of</strong><br />
infection was not specified in their cases. Udani,<br />
Parekh and Dastur (1972) while describing<br />
various manifestations <strong>of</strong> neuro-tuberculosis,<br />
mentioned two cases <strong>of</strong> posterior fossa meningitis.<br />
Our cases appear to similate these cases.<br />
All nine cases clinically and radiologically<br />
presented like a posterior fossa tumour. Only<br />
in one case, where there were meningeal signs<br />
with diffuse involvement associated with fever,<br />
tuberculous etiology was suspected preoperatively.<br />
None <strong>of</strong> the other cases gave a preoperative<br />
clue to tuberculous etiology.<br />
We fail to understand at the moment as to<br />
why these cases differ from cases <strong>of</strong> typical<br />
tuberculous meningitis. We feel inclined to<br />
attribute the difference to immunological<br />
reasons.<br />
It is suggested that these cases represent<br />
rarer cases <strong>of</strong> obstructive hydrocephalus <strong>of</strong><br />
tuberculous etiology and it is the conversion<br />
<strong>of</strong> cisterna magna into a pseudocyst due to<br />
arachnoiditis (slightly different for immunological<br />
reasons) in the posterior fossa, that<br />
forms the basis <strong>of</strong> this anatomo-clinical syndrome.<br />
REFERENCE<br />
1. Craig, W.M., Chronic cystic arachnoiditis, Amer.<br />
J. Surg.; 1932, 17, ?84.<br />
2. Dastur, H.M., Pandya, and Rao, V.C. Aetiology<br />
<strong>of</strong> hydrocephalus in tuberculous meningitis, Neurol<br />
(Bombay) Suppl. 1972, 1, 73.<br />
3. Horrax, G., Generalised cisternal arachnoiditis<br />
simulating brain tumour: its surgical treatment<br />
and results. Arch. Surg.; 1924, 9, 95.<br />
4. Reddy, G.N.N., Srivastava, V.K., Sagar, C.V.<br />
and Murthy V.S., Infratentorial arachnoid cyst,<br />
an enigma, Paper presented at 27th Annual Conference<br />
<strong>of</strong> Neurological Society <strong>of</strong> India held at<br />
Poona; 1977.<br />
Ind. J. Tub., Vol. XXIX, No. 3
POSTERIOR FOSSA CYSTIC ARACHNOIDITIS 199<br />
5. Sifoutes, J.E., Sordillo, S.V.R. and Lincoln, E.M.<br />
P.E.G. in tuberculous meningitis, J. Paediatr.;<br />
1957, 50, 695.<br />
6. Tandon, P.N., Tuberculous meningitis. In Infections<br />
<strong>of</strong> the Nervous System, part 1 Edited by<br />
Vinken, P.J. and Bruyn G.W.; 1978, 195.<br />
7. Udani, P.M., Parekh, Usha, Bhat, C. and Dastur,<br />
D.K.. Neurological tuberculosis in children with<br />
further observations: <strong>Tuberculosis</strong> <strong>of</strong> the Nervous<br />
system: Monograph on the proceedings <strong>of</strong><br />
the symposium, held in Bombay on 2nd to 5th<br />
February, 1972: 1972, 37.<br />
8. Udani, P.M., Parekh, Usha, C. and Dastur, D.K.:<br />
Neurological and related syndromes in CNS<br />
tuberculosis—Clinical features and pathogenesis,<br />
J. Neurol. Sci.; 1971, 14, 341.<br />
Ind. J. Tub., Vol. XXIX, No.3
LUPUS VULGARIS (VERRUCOSUS) ASSOCIATED WITH PULMONARY<br />
TUBERCULOSIS<br />
T.R. KAPUR*<br />
Summary : An unusual case <strong>of</strong> Lupus Vulgaris ^Verrucosus) associated with Pulmonary <strong>Tuberculosis</strong><br />
in a young man is presented. He had asymptomatic pulmonary tuberculosis and developed<br />
a cold abscess in the perineum, leading to two bilateral, symmetrical Verrucosus plaques in the Ischiorectal<br />
areas. Chemotherapy gave excellent results.<br />
Introduction<br />
That the human skin may react in many<br />
different ways to a single infective organism<br />
is nowhere better illustrated then in <strong>Tuberculosis</strong>.<br />
It can produce nodules, papillomatous<br />
tumours, vegetative verrucosus and cicatricial<br />
lesions. A classification based on morphology<br />
is not possible because Lupus Vulgaris may<br />
produce all the above types <strong>of</strong> lesions; hence a<br />
classification based on immunologic pattern is<br />
made (Augustine, 1973). In <strong>Tuberculosis</strong> Lupus<br />
Vulgaris (LV) and <strong>Tuberculosis</strong> Verrucosa<br />
Cutis (TVC) immunity is good. On the other<br />
hand immunity is variable i.e. moderate in<br />
Scr<strong>of</strong>uloderma and Gumma but poor in tuberculosis<br />
cutis orificials. Tuberculoids are allergic<br />
in nature with high degree <strong>of</strong> immunity.<br />
Clinical data from different geographic<br />
regions suggest a marked variation in the<br />
incidence <strong>of</strong> various forms <strong>of</strong> cutaneous tuberculosis.<br />
While skin tuberculosis appears to<br />
be rare in the U.S.A., incidence in Europe is<br />
reported to be around 1 % <strong>of</strong> all skin diseases<br />
(Wolff, 1971). Kagoj (1949) observed in 0.2%<br />
cases in Yugoslavia. Some investigators (Fasal<br />
and Rhodes, 1952 and Zoon, 1957) report<br />
that cutaneous tuberculosis is rare in tropics<br />
but studies from East, South and North <strong>of</strong><br />
India do not suggest this to be <strong>of</strong> such an uncommon<br />
occurrence. Incidence was 0.5%<br />
(Banerjee, 1956), 0.24% (Satyanarayan. 1962)<br />
and 0.11 % (Mammen, 1973) and 0.59% (Singh,<br />
1974) and 0.28% (Pandhi, Bedi, Kanwar and<br />
Bhutani, 1977) respectively.<br />
pain in abdomen, diminished appetite or fever.<br />
General examination did not reveal anaemia<br />
or lymphadenitis. Weight was 72 kgs.<br />
Lungs were clear clinically. Abdomen was<br />
not doughy. No lump was felt. Liver and<br />
spleen were not palpable. No Ischio-rectal sinus<br />
could be demonstrated. Cutaneous examination<br />
revealed two erythematous verrucosus, well<br />
demarcated plaques starting 1 cm from the<br />
anal margin and extending over Ischio-rectal<br />
region. Both the plaques were almost symmetrical<br />
and equal in size (5 cm x 6 cm). The<br />
surfaces were slightly wet with pus discharge<br />
from adjoining abscess (Fig. 1). There was one<br />
indurated abscess with discharging pus in the<br />
left perineum 2 cms away at 7 O’clock <strong>of</strong> the<br />
anal margin. There was hypoaesthesia over the<br />
plaques without any thickened cutaneous nerve<br />
twigs to the plaques. The clinical features<br />
were not suggestive <strong>of</strong> L.V. (Verrucosus).<br />
Presenting Features<br />
A twenty-six years old, well-built man<br />
reported without any history <strong>of</strong> fever, cough,<br />
pain in the chest or haemoptysis. He developed<br />
an abscess in the left perineum in July 1977<br />
which burst in due course. The pus discharge<br />
was contaminating the perianal area and he<br />
felt small plaques on either side <strong>of</strong> the perianal<br />
areas in September 1977. The plaques enlarged<br />
gradually and he got admitted on 1st December<br />
1977. He denied history <strong>of</strong> recurrent diarrhoea,<br />
Fig. 1<br />
Two erythematous, verrucosus, well-demarcated<br />
Plaques, seen between anal and Ischiorectal regions.<br />
Both are almost symmetrical and equal in size.<br />
Investigations<br />
DGI for treponema pallidum was negative.<br />
Scrappings for fungus in 10% KOH were also<br />
negative. Skin clippings were stained for mycobacteria<br />
tuberculosis and leprae and were<br />
*Lt.-Colonel; Classified Specialist (Derm & Yen), Military Hospital, Bareilly-243 001.<br />
Ind. J. Tub,, Vol. XXIX, No. 3
LUPUS VULGARIS (VERRUCOSUS) ASSOCIATED WITH PULMONARY TUBERCULOSIS 201<br />
negative for both. Sputum was negative for<br />
tubercle bacilli repeatedly. Pus from discharging<br />
abscess was negative for tubercle bacilli by<br />
direct smear and culture. Saprophytic staphylococci<br />
were grown from pus on blood agar<br />
media. Blood counts & ESR were within normal<br />
limits. Tuberculin reaction was 11 mm. X-ray<br />
chest revealed streaky-cum mottled opacities<br />
in the left apex and slight pulling up <strong>of</strong> the left<br />
hilum. Plain X-ray abdomen did not reveal<br />
any abnormal calcificarion or radio-opaque<br />
calculi. Skin biopsy showed hyperkeratosis and<br />
acanthosis <strong>of</strong> epidermis which in areas was<br />
appearing as pseudoepitheliomatous hyperplasia.<br />
There was also scattered atrophy <strong>of</strong><br />
epidermis. The dermis showing granulomatous<br />
infiltration by lymphocytes, histiocytes, a few<br />
epithelioid cells and Langhans type <strong>of</strong> gaint<br />
cells. Caseation was absent. Tubercles were<br />
seen in the upper corium. Tubercle bacilli<br />
could not be demonstrated on staining the<br />
specimen. Guinea pig inoculation <strong>of</strong> pus or<br />
biopsy material was not done due to lack <strong>of</strong><br />
facilities.<br />
Treatment<br />
The lesions were diagnosed as L.V. (Verrucosus)<br />
on histopathological evidence, associated<br />
with cold abscess and pulmonary tuberculosis<br />
in the left upper zone. He was placed on antitubercular<br />
treatment consisting <strong>of</strong> Streptomycin.<br />
Isoniazid and Ethionamide daily in the 2nd<br />
week <strong>of</strong> December 1977. The surface <strong>of</strong> the<br />
plaques started drying up along with regression<br />
<strong>of</strong> the borders by the end <strong>of</strong> 2nd week <strong>of</strong> the<br />
therapy. The plaques almost subsided with nonindurated<br />
residual erythema with a slight<br />
indurated lower border on the right side and the<br />
abscess healed after 90 days <strong>of</strong> therapy. He was<br />
put on Streptomycin with Isoniazid biweekly<br />
for another 15 months (total treatment 18<br />
months). X-ray chest revealed healed foci with<br />
a light scaring in Ischio-rectal areas on the<br />
completion <strong>of</strong> 18 months’ therapy.<br />
Discussion<br />
A well built individual with asymptomatic<br />
pulmonary tuberculosis <strong>of</strong> the left lung <strong>of</strong> unknown<br />
duration, developed a cold abscess in<br />
the perineum which is one <strong>of</strong> the possibilities<br />
in Lupus Vulgaris (Mammen, 1973 and Singh<br />
1974). Acute tuberculous ulcers (Orificial tuberculosis)<br />
also occur around anus but only in<br />
individuals suffering from advanced pulmonary<br />
or intestinal tuberculosis (Wilkinson, 1969).<br />
There was nothing to suggest abdominal tuberculosis.<br />
In lupus vulgaris, face is reported to be the<br />
commonest site in the European countries<br />
(Wolff, 1971 and Horwitz 1959). In India,<br />
lower extremities especially the buttocks seem<br />
to be affected most <strong>of</strong>ten, most probably due<br />
to accidental inoculation <strong>of</strong> the crawling children<br />
on the ground where Mycobacterium tuberculosis<br />
may have been deposited in the sputum<br />
(Singh, 1974 and Pandhi et al, 1977). The<br />
patient developed two identical verrucosus<br />
lesions in the Ischio-rectal areas due to exogenons<br />
inoculation with the pus discharge from the<br />
cold abscess. As the suppurative material,<br />
rich in bacilli, comes to the surface <strong>of</strong> the skin<br />
through sinuses, it reinfects skin and produces<br />
lupus vulgaris lesions (Singh, 1974). There is<br />
usually a single lesion but dissemination may<br />
occur through endogeous spread if the cellular<br />
immunity is depressed (Pandhi et al, 1977 and<br />
Wilkinson 1969).<br />
Lesion <strong>of</strong> the L.V. appear to be more<br />
common as compared to T.V.C. in Indian<br />
studies (Mammen, 1973 and Pandhi et al,<br />
1977). Both the lesions developed in an individual<br />
with good immunity (Augustine,<br />
1973; Mammen, 1973; Wilkinson, 1969 and<br />
Moschella 1975). Singh (1974) observed cases<br />
with histological evidence <strong>of</strong> L.V. at sites where<br />
T.V.C. is commonly found i.e. exposed<br />
areas. He postulated the interplay <strong>of</strong> several<br />
factors like immunity <strong>of</strong> the host, dose <strong>of</strong><br />
inoculum and virulence <strong>of</strong> bacilli, being responsible<br />
for the difference. On the other hand<br />
Pandhi et al (1977) and Kumar and Bhutani<br />
(1959) are <strong>of</strong> the opinion that L.V. and T.V.C.<br />
should be categorized together because they<br />
feel there are no immunological or bacteriological<br />
differences between the two conditions.<br />
Clinico-pathological differences are only quantitative<br />
and morphological differences are not<br />
adequate to justify two different terms. Epidermal<br />
changes are helpful in differentiating<br />
between L.V. and T.V.C. (Mammen 1973).<br />
In L.V. a combination <strong>of</strong> achanthosis and<br />
atrophy <strong>of</strong> the epidermis is very common<br />
whereas in T.V.C. acanthosis and hyperkaratosis<br />
are constant features. The granuloma<br />
appears in upper corium in L.V. but it is in middermis<br />
in T.V.C. (Wilkinson, 1969 and<br />
Moschella, 1975). The author feels that L.V.<br />
and T.V.C. are two separate entities morphologically<br />
as well as histopathologically. appearing<br />
in an individual having good cellular immunity.<br />
The clinico-histopathology in the case reported<br />
here was suggestive <strong>of</strong> Lupus Vulgaris<br />
(Verrucosus).<br />
Tubercle bacilli could not be demonstrated in<br />
this case. Pandhi et al (1977) failed to demonstrate<br />
bacilli in all the 23 cases <strong>of</strong> L.V. and 11<br />
cases <strong>of</strong> T.V.C. on staining the smear as well<br />
Ind. J. Tub., Vol. XXIX, No. 3
202 T.R. KAPUR<br />
as by culture and guinea pig inoculation in<br />
all the four cases where it was carried out.<br />
Bacilli were cultured in 6% out <strong>of</strong> 4000 cases<br />
in L.V. (Wilkinson, 1969). It is postulated that<br />
the bacilli are destroyed or walled <strong>of</strong>f by local<br />
tissue reaction.<br />
<strong>Tuberculosis</strong> <strong>of</strong> the other organs may be<br />
associated with the Lupus Vulgaris. Glandular<br />
involvement is the most frequent but pulmonary<br />
tuberculosis is also common (Mammen, 1973;<br />
Singh 1974 and Wilkinson 1969).<br />
There are different schedules <strong>of</strong> antitubercular<br />
therapy for pulmonary and cutaneous<br />
tuberculosis (Mammen, 1973; Pandhi et al<br />
1977; Wilkinson, 1969 and Citron, 1973). As<br />
a routine three drugs are prescribed for the<br />
first 90 days. Later, the therapy is continued<br />
with two drugs for another 15 months as<br />
per schedule <strong>of</strong> the <strong>Tuberculosis</strong> Chemotherapy<br />
Centre, Madras (<strong>Tuberculosis</strong> Chemotherapy<br />
Centre, 1964 and Ramakrishna, et al 1969).<br />
Pandhi et al (1977) treated cases with streptomycin<br />
and isoniazid daily for one year.<br />
There was complete recovery in 12, good<br />
response in another 12 but no response in<br />
one case. In Lupus Vulgaris, scars may break<br />
down and active lumps may frequently reappear<br />
in scar tissue. Therefore it is suggested<br />
that a full course <strong>of</strong> anti-tubercular therapy<br />
for 18 months should be given instead <strong>of</strong> 6 to<br />
12 months (Augustine, 1973: Mammen, 1973;<br />
Pandhi et al, 1977 and Wilkinson, 1969), even<br />
in the absence <strong>of</strong> associated tuberculosis <strong>of</strong> the<br />
other organs to prevent a relapse in the scars.<br />
Use <strong>of</strong> calciferol (Vitamin D2) is discouraged<br />
these days due to its toxicity.<br />
REFERENCES<br />
1. Augustine S.M. : <strong>Tuberculosis</strong> <strong>of</strong> the skin; Antiseptic;<br />
1973, 70, 791.<br />
2 Banerjee, B.M. : Common clinical manifestations<br />
<strong>of</strong> <strong>Tuberculosis</strong> <strong>of</strong> skin in the tropics; Indian<br />
J. Derm., 1956; 1,11.<br />
3. Citron, K.M. : <strong>Tuberculosis</strong>; Brit. Med. ].; 1973,<br />
2, 296.<br />
4. Fasal P. and Rhodes B. : Cutaneous tuberculosis<br />
and Sarcoidosis in the American Negro and Inhabitants<br />
<strong>of</strong> Tropical Countries, In hand book <strong>of</strong><br />
Tropical Dermatology and Medical Mycology,<br />
Ed., Simons R.G., Vol. 1, Elsevier Pub. Co.,<br />
Amsterdam, 1952.<br />
5. Horwitz O. : The localization <strong>of</strong> lupus vulgaris<br />
<strong>of</strong> the skin, Acta Tuber Scand, supp; 1959, 47,<br />
175.<br />
6. Kagoj, F. : The Luposa Tuberculose, 1: 292, 1949<br />
(quoted by Singh, 1974).<br />
7. Kumar A.S., Bhutani L.K. : Self Assessment<br />
programme, Ind. J. Derm. Vener Leprol; 1979,<br />
45, 67.<br />
8. Lahiri, K.D. : Etiology and patholoey <strong>of</strong> skin<br />
tuberculosis in the tropics, Ind. J. Derm.; 1956,<br />
2, 3.<br />
9. Mammen, A., Thambiah, A.S. : <strong>Tuberculosis</strong> <strong>of</strong><br />
the skin, Ind. .1. Derm. Vener; 1973, 39, 15’.<br />
10. Moschella, S.L. : Benign Reticulo-endothelial<br />
diseases, Dermatology, Vol. 1, 1st Ed. Edited by<br />
Moschella, S.L., Pillsbury D.M. and Burley H.J.,<br />
W.B. Saunders Coy, Philadelphia, 1975; Paee<br />
795.<br />
11. Pandhi, R.K., Bedi, T.R., Kanwar AJ. & Bhutani,<br />
I.K., Cutaneous tuberculosis—A clinical and<br />
investigative study, Ind. J. Derm.; 1977, 22,99.<br />
12. Ramakrishna C.V., Devadatta, S., Evans C,<br />
Fox W., Menon N.K., Nazarath O. and Velu<br />
S., et al : A four year follow up <strong>of</strong> patients with<br />
quiescent pulmonary tuberculosis at the end <strong>of</strong><br />
a year <strong>of</strong> chemotherapy with twice weekly isoniazid<br />
plus streptomycin or daily isoniazid plus PAS;<br />
Tubercle; 1969, 50, 115.<br />
13. Satyanarayan B.V. : Tuberculoma—A brief review<br />
together with statistical analysis and observations,<br />
Ind. J. Derm. Vener.; 1962, 28, 25.<br />
14. Singh, C. : Lupus Vulgaris in India, Ind. J. Derm.<br />
Vener.; 1974, 40, 257.<br />
15. <strong>Tuberculosis</strong> Chemotherapy Centre, <strong>of</strong><br />
the WHO; 1964, 31, 247.<br />
Bulletin<br />
16. Wilkinson, D.S. : <strong>Tuberculosis</strong> <strong>of</strong> the skin, Text<br />
Book <strong>of</strong> Dermatology, 1st Ed., Editors Rook A,<br />
Wilkinson D.S. and Ebling F.I.D., Blackwell<br />
Scientific Publications, Oxford 1969; Page 655.<br />
17. Wolff, K. : <strong>Tuberculosis</strong> in Dermatology in general<br />
medicine, Mycobacterial diseases, 1st Ed., Edited<br />
by Thomas B. Fitzpatrick et al, McGraw Hill<br />
Book Co. New York, 1971; Page 1743.<br />
18. Zoon J.J. : <strong>Tuberculosis</strong> <strong>of</strong> the skin in consideration<br />
about Pathogenesis; Arch Derm.; 1957; 75,<br />
161.<br />
Ind. J. Tub., Vol. XXIX, No. 3
BOOK REVIEW<br />
Clinical Investigation <strong>of</strong> <strong>Respiratory</strong> Disease:<br />
Edited by T.J.H. Clark; Chapman & Hall<br />
Ltd., London. 1981, pp. 526. Price £22.50.<br />
There have been tremendous advances in the<br />
science and art <strong>of</strong> medicine in recent years.<br />
As a result <strong>of</strong> these, there is better understanding<br />
<strong>of</strong> the structure and functioning <strong>of</strong><br />
the various systems <strong>of</strong> the human body. New<br />
investigative procedures based on this knowledge<br />
are being evolved for assessment as well<br />
as diagnosis <strong>of</strong> various conditions some <strong>of</strong><br />
which used to be obscure. This comprehensive<br />
book deals with procedures pertaining to the<br />
respiratory system.<br />
Non-respiratory functions <strong>of</strong> the lung have<br />
not attracted sufficient attention till recently.<br />
There is better understanding <strong>of</strong> the metabolic<br />
and biochemical functions <strong>of</strong> the lung as well<br />
as mechanism <strong>of</strong> host defence. Similarly,<br />
advances in the field <strong>of</strong> immunology have helped<br />
to devise some sophisticated diagnostic pro<br />
cedures, which are being increasingly deployed<br />
in routine clinical practice. Chapters dealing<br />
with these aspects are a »very welcome and<br />
important feature <strong>of</strong> this book.<br />
The Editor has presented in one volume<br />
all that is worth knowing and applying in the<br />
investigation <strong>of</strong> chest diseases. The timehonoured<br />
diagnostic procedures like history<br />
taking, physical signs, symptoms and pulmonary<br />
function tests have not been neglected.<br />
New knowledge about radiological procedures<br />
such as radio-isotope imaging and computerised<br />
tomographic scanning have also been included.<br />
Screening procedures for asymptomatic diseases<br />
and their cost-effectiveness have been dealt<br />
with in a proper perspective. References have<br />
also been made to tumour markers and ectopic<br />
hormones. New light has been thrown on<br />
susceptibility to smoking-induced lung cancer<br />
in relation to the subjects’ capacity to metabolise<br />
the carcinogens in cigarettes and accumulation<br />
<strong>of</strong> drugs in the lungs as an important<br />
factor in causing local drug toxicity leading to<br />
pulmonary fibrosis following prolonged administration<br />
<strong>of</strong> drugs like Busulphan and Bleomycin.<br />
The Editor is conscious <strong>of</strong> the investigations<br />
tending to become more and more complex.<br />
The object <strong>of</strong> the book appears to be to make<br />
the clinician conversant with all possible investigations<br />
and yet to be selective and critical in<br />
the choice <strong>of</strong> investigations based on their corelation<br />
with signs and symptoms etc.<br />
Tendency to resort to every conceivable investigation<br />
in every situation as a substitute for<br />
history and orderly physical examination has<br />
been rightly deprecated.<br />
All the contributors are specialists in their<br />
own field. The book is well-written, wellproduced<br />
and amply illustrated. It would be<br />
extremely useful for the post-graduate students<br />
as well as a reference book for the clinician.<br />
Ind. J. Tub., Vol. XXIX, No. 3
Citation read on the occasion <strong>of</strong> the presentation <strong>of</strong> the TAI Gold Medal<br />
to <strong>Dr</strong>. R.N. Tandon, former Pr<strong>of</strong>essor and Head <strong>of</strong> the Department <strong>of</strong> TB<br />
and Chest <strong>Diseases</strong>, Lucknow University, on 2.11.1981<br />
The <strong>Tuberculosis</strong><br />
Association <strong>of</strong> India<br />
awards a “Gold<br />
Medal” every year to a<br />
person who has rendered<br />
outstanding<br />
service to promote the<br />
cause <strong>of</strong> <strong>Tuberculosis</strong><br />
in India. For the year<br />
1981, the Association<br />
has selected Pr<strong>of</strong>. R.N.<br />
Tandon, former Pr<strong>of</strong>essor<br />
and Head <strong>of</strong> the<br />
Department <strong>of</strong> <strong>Tuberculosis</strong><br />
and Chest <strong>Diseases</strong>,<br />
Lucknow University,<br />
for this Award.<br />
Born in November 1899 at Agra (Uttar<br />
Pradesh) <strong>Dr</strong>. R.N. Tandon graduated from<br />
St. John’s College, Agra in 1921, took his<br />
M.B.B.S degree from the King George Medical<br />
College. Lucknow in 1926 and joined the K.G.<br />
Hospital (now known as the Gandhi Memorial<br />
Hospital) as Senior House Surgeon. During<br />
the years 1927 to 1929, he visited U.K. and<br />
Europe for further studies and obtained<br />
D.M.R.E. (Cambridge) and TDD (Wales). He<br />
joined the Bhowali Sanatorium in 1930 as its<br />
Assistant Superintendent and in 1934 he was<br />
awarded an International Scholarship at the<br />
Carlo Forlanini <strong>Institute</strong> for six months. Later,<br />
he undertook a study tour abroad for two<br />
years during which period he passed the<br />
Membership Examination <strong>of</strong> the Royal College<br />
<strong>of</strong> Physicians at Edinburg with <strong>Tuberculosis</strong><br />
as his special subject and also worked in several<br />
institutions in Paris, Switzerland and Berlin.<br />
On his return to India in 1936 he was deputed<br />
by the Uttar Pradesh Government to establish<br />
a TB Clinic at Allahabad, in 1945 he was<br />
appointed as the Head <strong>of</strong> the newly started<br />
<strong>Tuberculosis</strong> Department <strong>of</strong> the Lucknow University,<br />
with clinic and nearly 100 beds in the<br />
Kasturba TB Hospital, and subsequently as<br />
Pr<strong>of</strong>essor and Head <strong>of</strong> the Department <strong>of</strong><br />
<strong>Tuberculosis</strong> and Chest Disease?. <strong>Dr</strong>. Tandon<br />
is a renowned teacher and his students are now<br />
manning <strong>Tuberculosis</strong> services throughout the<br />
country.<br />
Apart from his pr<strong>of</strong>essional distinction and<br />
fame as a renowned teacher and an eminent<br />
clinician, <strong>Dr</strong>. Tandon was closely associated<br />
with the Uttar Pradesh <strong>Tuberculosis</strong> Association<br />
for several years as its founder-member, Vice-<br />
President and Organising Secretary for TB<br />
Seal Sale. He has also been the Vice-President<br />
<strong>of</strong> the Anti-TB League, Lucknow. for a long<br />
time.<br />
<strong>Dr</strong>. Tandon was a member <strong>of</strong> the Technical<br />
Committee <strong>of</strong> the <strong>Tuberculosis</strong> Association <strong>of</strong><br />
India from 1958-65, its Chairman in 1961-62<br />
and President <strong>of</strong> the 18th National Conference<br />
on TB & Chest <strong>Diseases</strong> held in Bangalore in<br />
1962. He attended practically all the National<br />
Conferences held from its inception till his<br />
retirement. He was also a member <strong>of</strong> the Central<br />
Committee <strong>of</strong> the <strong>Tuberculosis</strong> Association <strong>of</strong><br />
India during the years 1966-75. He was the<br />
recipient <strong>of</strong> the first Wander-TAT Oration in<br />
1973 which he delivered at the 28th National<br />
Conference on <strong>Tuberculosis</strong> and Chest <strong>Diseases</strong><br />
held in Madras in January 1974.<br />
In recognition <strong>of</strong> the meritorious services<br />
rendered in the field <strong>of</strong> tuberculosis, the <strong>Tuberculosis</strong><br />
Association <strong>of</strong> India decided to award<br />
its Gold Medal to him.<br />
Ind. J. Tub., Vol. XXIX, No. 3
Obituary<br />
DR. R. VISWANATHAN<br />
The grand old man <strong>of</strong> tuberculosis and chest diseases discipline is no more. <strong>Dr</strong>. R. Viswanathan,<br />
doyen <strong>of</strong> the discipline, and a renowned scientist died, literally, in harness on 14th July, 1982. In the<br />
83rd year <strong>of</strong> life, he was exceptionally agile both physically and mentally. Even on the last day preceding<br />
his fatal illness <strong>of</strong> about a month, he fulfilled the daily routine <strong>of</strong> his work.<br />
<strong>Dr</strong>. Viswanathan was a muifi-splendoured personality.<br />
Few have achieved such excellence in so many spheres. He<br />
was brilliant academician, a talented clinician, a gifted teacher, a<br />
prolific writer and a research worker <strong>of</strong> the highest calibre.<br />
Having obtained M.D. in general medicine from Madras<br />
and M.R.C.P. from London, he joined the Madras Medical<br />
College as an Assistant Pr<strong>of</strong>essor <strong>of</strong> Medicine and later<br />
joined the Visakhapatnam Medical College as Pr<strong>of</strong>essor.<br />
During the second World War, he served as a medical<br />
specialist to the Indian Army from 1942 to 1946. After release<br />
from the Army, he Joined the Directorate-Genera! <strong>of</strong> Health<br />
Services as first Tube! culosis Adviser to the Government <strong>of</strong><br />
India and Deputy Director-General. He took over as founder<br />
Director <strong>of</strong> the Vallabhbhai Pate! Chest <strong>Institute</strong> and after<br />
retirement from this post in 1969, he had been working as<br />
Emeritus Scientist CS1R and Honorary Pr<strong>of</strong>essor, V.P.<br />
Chest <strong>Institute</strong>, Delhi University. He was the Dean <strong>of</strong> the<br />
Faculty <strong>of</strong> Medical Sciences <strong>of</strong> Delhi University from 1946 to 1964.<br />
Apart from guiding hundreds <strong>of</strong> students in their research<br />
studies during his long pr<strong>of</strong>essorial career, he had to his credit original and outstanding research in<br />
several fields, especially pulmonary eosinophilia, pulmonary oedema <strong>of</strong> high altitude, acute massive<br />
collapse <strong>of</strong> the lung, bronchiectasis, etc. He contributed to the discovery <strong>of</strong> a new species <strong>of</strong> candide<br />
which, in recognition <strong>of</strong> his contribution, was named after him.<br />
He was closely associated with the <strong>Tuberculosis</strong> Association <strong>of</strong> India for several years and was<br />
a member <strong>of</strong> all its important committees, viz. Central Committee, Executive Committee, Technical<br />
Committee, Research Committee and the Local Advisory Committee. He was also a founder fellow <strong>of</strong><br />
the National Academy <strong>of</strong> Medical Sciences. He was the President <strong>of</strong> the Indian Association for Chest<br />
Physicians from its inception till last year when it transformed itself into the National College <strong>of</strong> Chest<br />
Physicians. He was Founder President <strong>of</strong> the Asthma and Chronic Bronchitis Foundation <strong>of</strong> India.<br />
He presided at the 8th National Congress <strong>of</strong> <strong>Diseases</strong> <strong>of</strong> Chest in 1963; Conference <strong>of</strong> Association <strong>of</strong><br />
Physicians <strong>of</strong> India in 1968: National <strong>Tuberculosis</strong> Conference in 1968 and World Congress on Asthma,<br />
Bronchitis and Allied Conditions in 1974.<br />
He published over 150 scientific papers in reputed National and International Journals, apart<br />
from numerous Orations and Guest Lectures in Conferences in India and abroad. He was the author<br />
<strong>of</strong> seven books, one <strong>of</strong> which dealt with his personal reminiscences, and contributed chapters in text<br />
and reference books. He was probably the best known medical scientist <strong>of</strong> this country in the International<br />
circles.<br />
Honours and awards came to him galore. He was a Padtna Bhushan and Honorary Physician to<br />
the President <strong>of</strong> India. The <strong>Tuberculosis</strong> Association <strong>of</strong> India awarded its Gold Medal for outstanding<br />
achievements to him in 1972. He was also the recipient <strong>of</strong> Dhanwantri Prize <strong>of</strong> the National Science<br />
Academy, Eugino Morelli Prize and Forlanini Medal from Italy.<br />
His demise is a great loss to the country, its medical pr<strong>of</strong>ession, the <strong>Tuberculosis</strong> Association <strong>of</strong><br />
India and many other organisations. The void left by him will be extremely difficult, if not impossible,<br />
to fill. May God grant eternal peace to the departed soul and may his achievements continue to inspire<br />
the coming generations!<br />
Ind. J. Tub., Vol. XXIX, No. 3
NEWS AND NOTES<br />
KOCH CENTENARY CELEBRATIONS<br />
The <strong>Tuberculosis</strong> Association <strong>of</strong> India<br />
celebrated the Centenary <strong>of</strong> the Discovery <strong>of</strong><br />
Tubercle Bacillus by Robert Koch by organising<br />
a special function in Delhi on 24th March,<br />
1982. Brief details about this function appeared<br />
in the “News & Notes” section <strong>of</strong> the April<br />
1982 issue <strong>of</strong> this Journal. The following are<br />
brief details <strong>of</strong> the various functions held in<br />
the States to celebrate the Centenary:<br />
Andhra Pradesh: In Andhra Pradesh the<br />
State TB Association designated its Xth State<br />
TB Workers’ Conference held in Hyderabad<br />
from the 12th to 15th March, 1982 as “Robert<br />
Koch’s Discovery <strong>of</strong> TB Centenary Conference”.<br />
Details <strong>of</strong> this Conference were given<br />
in the previous issue <strong>of</strong> the Journal. The<br />
Prakasam District TB Association conducted<br />
an intensive BCG Vaccination programme in<br />
the slum areas <strong>of</strong> Ongole, Addanki, Giddalur,<br />
Markapur Chirala. Kandukur and Kanigiri<br />
covering 3207 children. The Association also<br />
conducted two anti-TB Shibirs in Rajupalem<br />
and Gundayapalem and intensified its health<br />
education and case-finding activities. The District<br />
Association <strong>of</strong> Nizamabad organised a few<br />
health camps in some villages and slum areas.<br />
In cooperation with the Public Relations Office,<br />
lectures were arranged in the Beedi Factories<br />
with the help <strong>of</strong> Flip Charts, slides, cinema<br />
shows, display <strong>of</strong> posters, etc. The Adilabad<br />
District TB Association also carried out an<br />
intensive health education programme and<br />
<strong>of</strong>fered incentives to indigent patients for regularity<br />
in taking drugs. The West Godavari<br />
District Association organised an anti-TB<br />
Shibir in Prathikollanka which was attended<br />
by about 400 people. An intensive BCG vaccination<br />
programme in the slum areas <strong>of</strong> Eluru,<br />
Narsapur, Kovvur, Bhimavaram, T.P. Gudem<br />
and Nidadavolu Municipalities was undertaken<br />
and a total <strong>of</strong> 3027 BCG vaccinations were<br />
given. A valedictory function was held in the<br />
Red Cross Hall at Government Headquarters<br />
Hospital, Eluru. The Visakhapatnam District<br />
Association arranged a <strong>Tuberculosis</strong> and Chest<br />
<strong>Diseases</strong> Camp at Peda Gantyada, which was<br />
attended by 769 patients.<br />
Assam: The Assam TB Association, which<br />
had become inactive after bifurcation <strong>of</strong> the<br />
State into Assam and Meghalaya, has now<br />
revived its activities with headquarters at<br />
Gauhati. The Executive and other Committees<br />
<strong>of</strong> the Association are being reconstituted and<br />
the newly constituted General Body is expected<br />
Ind. J. Tub., Vol. XXIX, No. 3<br />
to meet towards the end <strong>of</strong> July 1982. As part<br />
<strong>of</strong> the Centenary Celebrations <strong>of</strong> the Discovery<br />
<strong>of</strong> the Tubercle Bacillus the Association organised<br />
public meetings at different places to educate<br />
the people about the various aspects <strong>of</strong> tuberculosis<br />
and pamphlets and leaflets were also<br />
widely distributed throughout the State. The<br />
Association has also taken steps to intensify<br />
the case-finding and health education activities.<br />
An article on ‘Fight TB’ in English by <strong>Dr</strong>. J.N.<br />
Bhuyan, Honorary Secretary, State TB Association<br />
and another article on <strong>Tuberculosis</strong> in<br />
Assamese by <strong>Dr</strong>. A.K. Adhikary, were published<br />
in the local dailies. A radio talk on <strong>Tuberculosis</strong><br />
was broadcast from the AIR Station at Gauhati<br />
on 19.7.1982. The State Association proposes<br />
to organise a refresher course in tuberculosis for<br />
private medical practitioners. The first State<br />
<strong>Tuberculosis</strong> Workers Conference is also proposed<br />
to be held towards the end <strong>of</strong> the current<br />
year after revitalisation <strong>of</strong> the District TB<br />
Association.<br />
Bengal: The Bengal TB Association organised<br />
a special function to celebrate the hundredth<br />
anniversary <strong>of</strong> the discovery <strong>of</strong> Tubercle Bacillus<br />
by Robert Koch and also the 5th State TB &<br />
Chest <strong>Diseases</strong> Workers Conference in Calcutta<br />
on the 22nd and 23rd May, 1982. Shri B.D.<br />
Pande. Governor <strong>of</strong> West Bengal and President<br />
<strong>of</strong> the Bengal TB Association inaugurated the<br />
centenary function by unveiling the Portrait <strong>of</strong><br />
Robert Koch and by switching on 100 Coloured<br />
bulbs. <strong>Dr</strong>. Werner Handke, Consul-General<br />
<strong>of</strong> the Federal German Republic was the Guestin-Chief.<br />
<strong>Dr</strong>. P.K. Sen, Chairman <strong>of</strong> the Association,<br />
proposed the Vote <strong>of</strong> thanks <strong>Dr</strong>. P.K-<br />
Chatterjee presided over the Conference while<br />
<strong>Dr</strong>. B.B. Manna delivered the Guest Lecture.<br />
The subjects discussed at the conference included<br />
Pathology, Control <strong>of</strong> <strong>Tuberculosis</strong>, Air<br />
Pollution, Pediatric <strong>Tuberculosis</strong> and Bronchial<br />
Asthma. About 300 delegates attended the<br />
Conference. A souvenir was also brought out<br />
on this occasion.<br />
Bihar: The Bihar <strong>Tuberculosis</strong> Association<br />
celebrated the Centenary by organising a special<br />
function on the 18th April, 1982 at the I.M.A.<br />
Hall, Patna. The First State Conference <strong>of</strong><br />
TB & Chest <strong>Diseases</strong> workers was also combined<br />
with this function. <strong>Dr</strong>. Umeshwar Prasad<br />
Verma, Minister for Health & Family Welfare,<br />
Bihar, inaugurated the celebrations while Shri<br />
Shamaele Bani, State Minister for P.R.D. and<br />
Higher Education, Bihar was the Chief Guest.<br />
<strong>Dr</strong>. M. Pathak, Chairman <strong>of</strong> the Association<br />
welcomed the guests and Pr<strong>of</strong>. R. Viswanathan,
NEWS & NOTES 207<br />
Pr<strong>of</strong>essor Emeritus, V.P. Chest <strong>Institute</strong>, University<br />
<strong>of</strong> Delhi and Pr<strong>of</strong>. U.N. Shahi, Retd.<br />
Head <strong>of</strong> the Department <strong>of</strong> Surgery. Patna<br />
Medical College were the Guest Speakers. The<br />
function was attended by a large number <strong>of</strong><br />
TB Workers from all over the State including<br />
District TB Officers, teachers <strong>of</strong> Patna and<br />
Nalanda Medical Colleges, general practitioners,<br />
High Court Judges and a cross-section <strong>of</strong> the<br />
population.<br />
In the afternoon the Scientific Session was<br />
inaugurated by <strong>Dr</strong>. A.K.N. Sinha, Presidentelect,<br />
World Medical Association. The subjects<br />
discussed included all aspects <strong>of</strong> tuberculosis.<br />
<strong>Dr</strong>. R. Viswanathan delivered a Guest Lecture<br />
on “Chronic Bronchitis”. The function concluded<br />
with a Vote <strong>of</strong> Thanks by <strong>Dr</strong>. B.K. Prasad,<br />
Organising Secretary. A Souvenir was released<br />
on the occasion by Shri Shamaele Bani, State<br />
Minister for P.R.D. and Higher Education and<br />
the film ‘Your Enemy—TB’ was shown to the<br />
audience which was very much appreciated.<br />
Goa: The Government and the State TB<br />
Association <strong>of</strong> Goa, Daman & Diu jointly<br />
arranged a function to celebrate the Centenary<br />
<strong>of</strong> the Discovery <strong>of</strong> Tubercle Bacillus by Robert<br />
Koch in the Auditorium <strong>of</strong> Hotel Mandovi in<br />
Panjim on 15th May, 1982. The function was<br />
inaugurated by the Lt.-Governor <strong>of</strong> Goa and<br />
it was presided over by the Chief Minister <strong>of</strong><br />
the State. <strong>Dr</strong>. Jacinto Estibeiro, Director <strong>of</strong><br />
Health Services and Chairman, TB Association<br />
<strong>of</strong> Goa, Daman & Diu gave the welcome address<br />
and <strong>Dr</strong>. Ananda Helecar, Deputy Director<br />
<strong>of</strong> Health Services, introduced the Chief Guests.<br />
<strong>Dr</strong>. S.P. Pamra, Honorary Technical Adviser,<br />
<strong>Tuberculosis</strong> Association <strong>of</strong> India, delivered<br />
the Key Note Address. The function came to<br />
a close with a Vote <strong>of</strong> Thanks by <strong>Dr</strong>. Damodar<br />
Bhounsule, Honorary Secretary <strong>of</strong> the State<br />
TB Association.<br />
The Centenary function was followed by a<br />
Symposium on <strong>Tuberculosis</strong> on 16.5.1982 which<br />
was attended by over 100 General Practitioners.<br />
<strong>Dr</strong>. Pamra delivered three lectures at the<br />
Symposium on the various aspects <strong>of</strong> tuberculosis<br />
and its management. The other lecturers<br />
were <strong>Dr</strong>. K.C. Mohanty. Hony. Pr<strong>of</strong>essor and<br />
Head <strong>of</strong> the Dept. <strong>of</strong> TB, Grant Medical<br />
College and J.J. Group <strong>of</strong> Hospitals, Bombay<br />
and <strong>Dr</strong>. A.S. Bagga, Pr<strong>of</strong>, <strong>of</strong> <strong>Tuberculosis</strong>,<br />
Medical College, Goa. The subjects discussed<br />
included Epidemiology, Pathology and Differential<br />
Diagnosis <strong>of</strong> <strong>Tuberculosis</strong>, Chemotherapy<br />
<strong>of</strong> <strong>Tuberculosis</strong> and Role <strong>of</strong> General<br />
Practitioners in <strong>Tuberculosis</strong> Control Programme.<br />
There was also a Panel Discussion with<br />
<strong>Dr</strong>. S.P. Pamra as the Moderator.<br />
Gujarat: The Gujarat TB Association celebrated<br />
the Centenary along with their Xth<br />
State TB & Chest <strong>Diseases</strong> Workers Conference<br />
held at Ahmedabad on the 14th March,<br />
1982. The Conference was inaugurated by<br />
Shri N. Vittal, Health Secretary to the Government<br />
<strong>of</strong> Gujarat and it was presided over by<br />
<strong>Dr</strong>. A.G. Patel, Vice-Chairman, State TB<br />
Association and Medical Superintendent, S.P.<br />
Sanatorium, Baroda. <strong>Dr</strong>. S.H. Patel, Honorary<br />
Secretary <strong>of</strong> the State Association presented a<br />
brief report on the working <strong>of</strong> the State Association<br />
while <strong>Dr</strong>. A.S. Shah, the Treasurer<br />
read out the messages. A booklet on <strong>Tuberculosis</strong>,<br />
brought out in cooperation with the<br />
local branch <strong>of</strong> the I.M.A., was presented by<br />
<strong>Dr</strong>. P.K. Pandya, Honorary Secretary, Scientific<br />
Committee <strong>of</strong> the Gujarat State IMA Branch<br />
and it was formally released by <strong>Dr</strong>. O.P. Gupta,<br />
Director, Medical & Health, Gujarat State.<br />
The Scientific sessions included two panel<br />
discussions, one on “Recent Trends and<br />
Advances in the management <strong>of</strong> <strong>Tuberculosis</strong>”<br />
chaired by <strong>Dr</strong>. S.B. Trivedi and the other on<br />
“Present Status <strong>of</strong> <strong>Tuberculosis</strong> situation in<br />
Gujarat” chaired by Shri Bhogibhai Lalani.<br />
The Conference came to a close with a Vote <strong>of</strong><br />
Thanks proposed by <strong>Dr</strong>. I.G. Bhatt, Honorary<br />
Secretary. TB Relief Organisation, Ahmedabad.<br />
The State Association, in cooperation with<br />
its District and Taluk Associations, arranged<br />
for special radio talks, T.V. programmes,<br />
screening <strong>of</strong> film on T.B., etc. with a view to<br />
educate the public on various aspects <strong>of</strong> tuberculosis.<br />
The Association also organised a press<br />
conference and distributed a hand-out on<br />
Robert Koch and other literature on tuberculosis<br />
for publication in the lay press. They<br />
also put up banners and posters at public<br />
places and organised public meetings in cooperation<br />
with the local branches <strong>of</strong> the I.M.A.,<br />
Lions and Rotary Clubs, etc.<br />
Jammu & Kashmir: The Centenary was<br />
celebrated in Jammu & Kashmir State on the<br />
24th March, 1982, by organising public<br />
meetings in all the Districts under the Chairmanship<br />
<strong>of</strong> the Divisional Commissioner.<br />
Special efforts were made to create better<br />
awareness among the public about tuberculosis<br />
and the facilities available for its diagnosis and<br />
treatment and also to motivate patients to<br />
take treatment regularly and as long as advised.<br />
A special function was organised at the TB<br />
Demonstration Centre, Srinagar, and it was<br />
addressed by the District <strong>Tuberculosis</strong> Officer,<br />
and the Director <strong>of</strong> the Centre. The function<br />
was covered by Radio Kashmir. The feature<br />
film “Fight against TB” in Kashmiri language<br />
was also screened.<br />
Ind. J. Tub., Vol. XXIX, No. 3
208 NEWS & NOTES<br />
Karnataka: The Karnataka Government<br />
constituted a special Committee, with <strong>Dr</strong>. K.<br />
Nagappa Alva as Chairman, to celebrate the<br />
Centenary <strong>of</strong> the Discovery <strong>of</strong> Tubercle Bacillus<br />
and also the Silver Jubilee <strong>of</strong> the S.D.S. TB<br />
Hospital, Bangalore in a befitting manner.<br />
The Centenary celebration, presided over by<br />
Shri A.K.A. Samad, Minister for Health &<br />
Family Welfare, Government <strong>of</strong> Karnataka,<br />
was inaugurated by Shri Govind Narain, the<br />
State Governor and the Silver Jubilee Celebrations<br />
<strong>of</strong> the S.D.S. TB Hospital by Shri R.<br />
Gundu Rao, Chief Minister <strong>of</strong> Karnataka, at<br />
a special function held on the 28th May, 1982<br />
at the Auditorium <strong>of</strong> the Bangalore Medical<br />
College, Bangalore. The Health Exhibition on<br />
<strong>Tuberculosis</strong>, arranged in connection with the<br />
Centenary Celebrations, was inaugurated by<br />
Smt. Chandra Govind Narain while the Special<br />
Souvenir brought out on the occasion was<br />
released by Shri Dharam Singh, Minister for<br />
Housing & Urban Development, Government<br />
<strong>of</strong> Karnataka. The function came to a close<br />
with a Vote <strong>of</strong> Thanks proposed by <strong>Dr</strong>. B.<br />
Krishnacharya, Joint Director (TB), Government<br />
<strong>of</strong> Karnataka. The Scientific Sessions<br />
were held on the 29th and 30th <strong>of</strong> May at the<br />
National <strong>Tuberculosis</strong> <strong>Institute</strong> and the S.D.S.<br />
TB Hospital, Bangalore, and these were chaired<br />
by <strong>Dr</strong>. V. Parameswara, President, I.M.A.,<br />
Karnataka and <strong>Dr</strong>. Y. Rajasekhara, ex-<br />
Superintendent, S.D.S. TB Hospital, respectively.<br />
The subjects discussed included <strong>Tuberculosis</strong><br />
in Children, Recent Developments in<br />
the Studies <strong>of</strong> Mycobacteria, case-finding in<br />
<strong>Tuberculosis</strong>, Chemotherapy, <strong>of</strong> <strong>Tuberculosis</strong>,<br />
Review <strong>of</strong> National <strong>Tuberculosis</strong> Programme,<br />
Role <strong>of</strong> Survey in <strong>Tuberculosis</strong>, <strong>Respiratory</strong><br />
Allergy, Tubercular Meningitis, Role <strong>of</strong> Voluntary<br />
Organisation, etc. The celebrations concluded<br />
with a Valedictory function presided<br />
over by Shri K. Nagappa Alva and with Shri<br />
A.K.A. Samad, Minister for Health & Family<br />
Welfare, Government <strong>of</strong> India, as the Chief<br />
Guest.<br />
Kerala: The Kerala TB Association inaugurated<br />
the Centenary Celebrations by organising a public<br />
meeting at the Primary Health Centre, Kesavapuram,<br />
Trivandrum on 24.3.1982. The meeting<br />
was attended by prominent public leaders and<br />
members <strong>of</strong> the pr<strong>of</strong>ession. <strong>Dr</strong>. A. Ananthaswamy,<br />
Supervising Medical Officer, BCG<br />
Campaign, gave a talk on infection and preventive<br />
measures <strong>of</strong> tuberculosis and the District<br />
Medical Officer <strong>of</strong> Health, Trivandrum, inaugurated<br />
a BCG Camp where about 2000<br />
children were vaccinated. An exhibition highlighting<br />
the magnitude <strong>of</strong> the tuberculosis<br />
problem, mode <strong>of</strong> infection, symptoms treatment,<br />
prevention, etc. was inaugurated in the<br />
Conference Hall <strong>of</strong> the Association by <strong>Dr</strong>. P.U.<br />
Abubacker, Additional Director <strong>of</strong> Health<br />
Services, Kerala. The exhibition is being moved<br />
from place to place and shown throughout the<br />
State with a view to educate the people and<br />
create better awareness among them about<br />
tuberculosis. Another public meeting was held<br />
in the IMA Hall, Trivandrum, on the same day<br />
under the joint auspices <strong>of</strong> the State TB Association<br />
and IMA branch, Trivandrum with<br />
Pr<strong>of</strong>. R. Ananthanarayan in the Chair. <strong>Dr</strong>. B.N.<br />
Kudubi, Superintendent, Sanatorium for Chest<br />
<strong>Diseases</strong>, Pulayanarcottah and <strong>Dr</strong>. M. Habeeb,<br />
District TB Officer, Trivandrum, spoke on<br />
“The life <strong>of</strong> <strong>Dr</strong>. Robert Koch” and “Recent<br />
trends in the Management <strong>of</strong> <strong>Tuberculosis</strong>”<br />
respectively. The District TB Association,<br />
Ernakulam, organised tuberculosis detection<br />
medical camps and BCG vaccination camps<br />
while seminars and panel discussions were held<br />
under the joint auspices <strong>of</strong> the district TB<br />
Associations and I.M.A. Branches <strong>of</strong> Kottayam,<br />
Trichur, Shornur. Palghat and Manjeri. Special<br />
articles on <strong>Dr</strong>. Robert Koch and on the various<br />
aspects <strong>of</strong> tuberculosis were published both in<br />
the English and Malayalam dailies and magazines<br />
and talks by leading TB Specialists over the<br />
All India Radio, Trivandrum, Trichur and<br />
Calicut, in the form <strong>of</strong> questions and answers,<br />
group discussions, etc., were also arranged.<br />
Essay competitions among Arts and Science<br />
students and Medical College Students were<br />
held and prizes were awarded for the best<br />
essay from each category. The Anti-TB Week<br />
was celebrated in all the districts and the film<br />
on tuberculosis was shown on these occasions.<br />
Madhya Pradesh: The Madhya Pradesh<br />
Association celebrated the Centenary by<br />
organising its First Madhya Pradesh TB and<br />
Chest <strong>Diseases</strong> Workers’ Conference in Bhopal<br />
on the 8th and 9th <strong>of</strong> May, 1982. <strong>Dr</strong>. M.N.<br />
Nagu, Director, Medical and Health Services,<br />
Madhya Pradesh, presided over the Scientific<br />
Sessions. H.E. the Governor <strong>of</strong> Madhya<br />
Pradesh addressed the afternoon session and<br />
distributed the various medals, prizes, etc. to<br />
distinguished TB workers and for highest<br />
collections by sale <strong>of</strong> TB Seals. <strong>Dr</strong>. S.P. Pamra,<br />
Honorary Technical Adviser, T.A.T. delivered<br />
the <strong>Dr</strong>. N.L. Bordia Memorial Oration on<br />
“<strong>Tuberculosis</strong> an Enigma”. About 50 delegates<br />
attended the Scientific Sessions.<br />
The Anti-TB Association <strong>of</strong> Indore in collaboration<br />
with the Indore Chest Society and the<br />
Indian Medical Association organised a function<br />
to celebrate the Centenary <strong>of</strong> the Discovery<br />
<strong>of</strong> Tubercle Bacillus by Robert Koch at the<br />
Maharaja Yeshwant Rao Hospital. <strong>Dr</strong>. S.M.<br />
Jain spoke on the achievements <strong>of</strong> Robert Koch,<br />
Ind. J. Tub., Vol. XXIX, No. 3
NEWS & NOTES 209<br />
<strong>Dr</strong>. S. Mandovra about the treatment <strong>of</strong> tuberculosis<br />
and <strong>Dr</strong>. K.C. Sharma about the control<br />
<strong>of</strong> Intestinal <strong>Tuberculosis</strong>. The function was<br />
followed by organising special health education<br />
programmes in the Maharaja Yeshwant Rao<br />
Hospital, TB Clinic. Malharganj, Cloth Market<br />
Hospital, Manorama Raje TB Hospital and<br />
E.S.I. Hospital.<br />
Maharashtra: The Maharashtra State Anti-<br />
TB Association advised its District Associations<br />
and I.M.A. branches all over the State to celebrate<br />
the Centenary in a befitting manner by<br />
organising reorientation courses for general<br />
practitioners intensifying their health education<br />
activities and carry out mass immunisation and<br />
case-finding programmes in urban and rural<br />
areas. The State TB Association and the<br />
Bombay branch <strong>of</strong> the I.M.A jointly organised<br />
a Conference on the 26th, 27th and 28th March,<br />
1982 <strong>of</strong> which one morning and an afternoon<br />
were devoted for discussing the various aspects<br />
<strong>of</strong> tuberculosis and its management. The Association<br />
also organised jointly with the Lions<br />
Club <strong>of</strong> Mazgaon, a special meeting presided<br />
over by His Excellency Shri Homi J.H. Taleyarkhan,<br />
Governor <strong>of</strong> Sikkim, whe.re workers in<br />
tuberculosis in the State were honoured. Special<br />
functions were also held at Pune, Nasik and<br />
Nanded where a symposium, a panel discussion<br />
and some Guest Lectures on tuberculosis were<br />
arranged. The Association arranged publication<br />
<strong>of</strong> special articles on different aspects <strong>of</strong> tuberculosis<br />
in English and Marathi dailies. Mass<br />
immunisation and case-finding programmes<br />
were held at Sudhagad, Pali Taluka in Raigad<br />
district and Dindori Taluka in Nasik District.<br />
The main aspects <strong>of</strong> the project were multiple<br />
vaccination for all the children <strong>of</strong> eligible group<br />
in the Taluka, door-to-door enumeration <strong>of</strong> TB<br />
symptomatics and their sputum examination<br />
and a series <strong>of</strong> diagnostic shibirs following<br />
BCG vaccination programme. The Bombay<br />
City programme for enumeration <strong>of</strong> the symptomatics<br />
with the help <strong>of</strong> N.S.S. students will<br />
commence shortly. The Bombay Municipal<br />
Corporation has released Rifamycin for all<br />
cases which would be discovered in the intensive<br />
drive.<br />
Meghalaya: The State TB Association celebrated<br />
the Centenary <strong>of</strong> the Discovery <strong>of</strong><br />
Tubercle Bacillus by organising’a Special function<br />
at Shillong on 17th July, 1982. The function<br />
presided over by Shri D.D. Lapang, Minister<br />
for Health & Family Welfare and President,<br />
Meghalaya TB Association, was inaugurated<br />
by Shri Prakash Mehrotra, Governor <strong>of</strong> Assam<br />
and Meghalaya by unveiling the portrait <strong>of</strong><br />
Robert Koch. <strong>Dr</strong>. L.N. Chintey, Honorary<br />
Secretary <strong>of</strong> the State Association welcomed the<br />
distinguished invitees and <strong>Dr</strong>. (Mrs.) F.N.<br />
Kharkongor, Deputy Director, Pasteur <strong>Institute</strong>,<br />
proposed the Vote <strong>of</strong> Thanks. This was<br />
followed by a Scientific Session which was<br />
chaired by <strong>Dr</strong>. O. Lyngdoh and a panel<br />
discussion with <strong>Dr</strong>s. E. Lyngdoh and C.M.<br />
Brahma as moderators. The session was well<br />
attended and the subjects discussed covered<br />
all aspects <strong>of</strong> tuberculosis. The function<br />
came to a close with the screening <strong>of</strong> the film<br />
‘Your Enemy—TB’.<br />
Orissa: The Orissa State TB Association<br />
organised its 3rd State TB & Chest <strong>Diseases</strong><br />
Workers’ Conference and also a special function<br />
to celebrate the Centenary <strong>of</strong> the Discovery <strong>of</strong><br />
the Tubercle Bacillus by Robert Koch at the<br />
Medical College, Burla on the 13th and 14th<br />
March, 1982. The Minister <strong>of</strong> State for Health<br />
and Family Welfare, Orissa, inaugurated the<br />
function. On the 14th a Seminar on TB Control<br />
Programme was organised which was chaired<br />
by the Director <strong>of</strong> Health Services. The Scientific<br />
Sessions were presided over by the Director<br />
<strong>of</strong> Medical Education and Training.<br />
The State Association also organised a<br />
Symposium on <strong>Tuberculosis</strong> at the S.C.B.<br />
Medical College, Cuttack on 26.4.1982 which<br />
was attended by a large number <strong>of</strong> students<br />
from the Medical Colleges <strong>of</strong> Cuttack, Berhampur<br />
and Burla.<br />
Sikkim: The Sikkim Anti-TB Association,<br />
organised a special function to celebrate the<br />
Centenary on 25th May, 1982, in the Secretariat<br />
Hall at Raj Bhavan, Gangtok. The function<br />
was inaugurated by the Hon’ble Shri S.<br />
Shankaranand, Union Minister for Health and<br />
Family Welfare in the presence <strong>of</strong> Shri Homi<br />
J.H. Taleyarkhan, Governor <strong>of</strong> Sikkim, Kumari<br />
Kumud Ben Joshi, Union Deputy Minister for<br />
Health, Shri N.B. Bhandari, Chief Minister <strong>of</strong><br />
Sikkim, Shri S.M. Limboo, State Health Minister<br />
and delegates from Sikkim and North-Eastern<br />
States. In his inaugural address Shri Shankaranand<br />
urged the need for community involvement<br />
in the fight against tuberculosis and<br />
assured the State Government <strong>of</strong> adequate<br />
Central assistance in their efforts to control<br />
tuberculosis in the State. Shri Homi J.H.<br />
Taleyarkhan stressed the need for expansion<br />
<strong>of</strong> the domiciliary treatment services coupled<br />
with an army <strong>of</strong> devoted health visitors to<br />
monitor the health <strong>of</strong> the patients and to see<br />
that they take medicines regularly at home and<br />
visit the treatment centres at regular intervals<br />
for check-up. The Chief Minister, Shri N.B.<br />
Bhandari and the State Health Minister Shri S.<br />
M. Limboo paid rich tributes to Robert Koch<br />
for his epoch-making discovery which brought<br />
Ind. J. Tub., Vol. XXIX, No. 3
210 NEWS & NOTES<br />
tuberculosis control within the realm <strong>of</strong> possibility.<br />
The function came to a close with a<br />
Vote <strong>of</strong> Thanks by <strong>Dr</strong>. A. Pazo, Joint Secretary<br />
<strong>of</strong> the State Association.<br />
Tamil Nadu: The Tamil Nadu <strong>Tuberculosis</strong><br />
Association organised an Anti-TB Week in<br />
Madras from 15.4.1982. His Excellency the<br />
Governor <strong>of</strong> Tamil Nadu, Thiru Sadiq Ali,<br />
unveiled the Portrait <strong>of</strong> Robert Koch and delivered<br />
the valedictory address. TheHon’ble <strong>Dr</strong>. H.V.<br />
Hande, Minister for Health presided and Smt.<br />
Tara Cherian, M.L.C. Chairman, State Social<br />
Welfare Board distributed prizes to the winners<br />
in the Essay Competition conducted by the<br />
Association both in English and Tamil for the<br />
students <strong>of</strong> City Colleges and Higher Secondary<br />
Schools. The Health Education activities were<br />
also intensified during the week. A series <strong>of</strong><br />
lectures and film shows were arranged with the<br />
help <strong>of</strong> the Lions Club and certain Primary<br />
Health Centres. Articles <strong>of</strong> topical interest on<br />
<strong>Tuberculosis</strong>, its prevention and control were<br />
published in “The Hindu” in English and<br />
“Dinamani” in Tamil. Radio and Television<br />
authorities arranged suitable programmes on<br />
<strong>Tuberculosis</strong> in which <strong>Dr</strong>. K.V. Krishnaswami,<br />
<strong>Dr</strong>. Santosham and others participated. As<br />
part <strong>of</strong> effective delivery <strong>of</strong> Primary Health<br />
Care at the peripheral level, some <strong>of</strong> the District<br />
Associations organised case-finding programmes<br />
in selected villages and intensified their health<br />
education activities by holding public meetings,<br />
organising cultural programmes, film shows,<br />
etc. The Medical Colleges at Coimbatore,<br />
Tirunelveli. Madurai and Chingleput conducted<br />
symposia on the History <strong>of</strong> TB and at Tirupathur<br />
in North Arcot District, the local Indian<br />
Medical Association Branch organised a<br />
Refresher Course for General Medical Practitioners<br />
and also a training programme rfo paramedical<br />
personnel.<br />
Tripura: The TB Association <strong>of</strong> Tripura<br />
proposes to celebrate the Koch Centenary Year<br />
by launching a special case-finding drive in certain<br />
groups <strong>of</strong> workers, viz. tea garden, jute mill,<br />
beedi sramik etc. phase by phase. It has chosen<br />
the Kalashara Tea Garden workers to start<br />
with, and the programme will be carried out in<br />
cooperation with the Department <strong>of</strong> TB,<br />
Government <strong>of</strong> Tripura. The Tripura Jute Mill<br />
has agreed for a similar check up drive among<br />
its workers which will be taken up shortly.<br />
Beedi workers <strong>of</strong> Bishalgarh Block area will<br />
be taken up later.<br />
Uttar Pradesh: The Uttar Pradesh TB Association<br />
organised its 5th State TB and Chest<br />
<strong>Diseases</strong> Workers’ Conference in Dehra Dun<br />
from 8th to 10th January, 1982. The Conference<br />
was inaugurated by the State Finance<br />
Minister and the Scientific Sessions were<br />
presided over by <strong>Dr</strong>. O.P. Mital. <strong>Dr</strong>. S.P.<br />
Pamra Honorary Technical Adviser <strong>of</strong> the<br />
<strong>Tuberculosis</strong> Association <strong>of</strong> India delivered the<br />
Key Note Address on “Case-finding”. The<br />
subjects discussed at the Scientific Sessions<br />
included National TB Programme, Chemotherapy<br />
and recent advances, Extra-pulmonary<br />
<strong>Tuberculosis</strong>, Childhood <strong>Tuberculosis</strong>, Allergic<br />
and other <strong>Respiratory</strong> <strong>Diseases</strong>, etc.<br />
Ind. J. Tub,, Vol. XXIX, No. 3