Association of Ontario Midwives Summer 2012
Association of Ontario Midwives Summer 2012
Association of Ontario Midwives Summer 2012
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Association</strong> <strong>of</strong> <strong>Ontario</strong> <strong>Midwives</strong> <strong>Summer</strong> <strong>2012</strong><br />
03<br />
Protesting federal<br />
cuts to refugee<br />
health<br />
04<br />
<strong>Midwives</strong> advocate<br />
for pay equity<br />
06<br />
Conference focuses<br />
on growth<br />
08<br />
Meet three future<br />
midwives<br />
11<br />
New hypertensive<br />
guidelines<br />
<strong>Association</strong> <strong>of</strong> <strong>Ontario</strong> <strong>Midwives</strong><br />
Minister <strong>of</strong> Health and Long-Term Care Deb Matthews<br />
makes a surprise visit to the closing ceremonies <strong>of</strong> the<br />
<strong>Association</strong>’s 28 th Annual Conference.
AOM News & Updates<br />
New practice in Attawapiskat will<br />
return birth to the community<br />
There’s only one word to describe midwife Christine Roy’s reaction when provincial<br />
Minister <strong>of</strong> Health and Long-Term Care Deb Matthews called her personally to let her<br />
know <strong>Ontario</strong> would be funding a midwifery practice in Attawapiskat: “Stunned,” Roy<br />
says with a laugh. “I was very thrilled.”<br />
Roy says the minister<br />
thanked her for the<br />
work she was doing.<br />
“She was happy to<br />
know we were going<br />
to do great things<br />
for women and<br />
their families in this<br />
community.”<br />
The road Roy and<br />
fellow midwife Carol<br />
Couchie traveled to<br />
get to this moment<br />
was a long one. The<br />
two have known each<br />
other for more than 20<br />
years and got the idea<br />
to build a midwifery<br />
practice in Attawapiskat<br />
several years<br />
Attawapiskat<br />
Fort Albany<br />
Moosonee/<br />
Moose Factory<br />
Communities in WAHA<br />
catchment area<br />
Former routine<br />
evacuation sites<br />
Timmins<br />
Returning Birth<br />
to the North<br />
Kingston<br />
ago when they were working on the Quebec side <strong>of</strong> James Bay planning midwifery<br />
services for a Cree community in the region.<br />
The new practice, Neepeeshowan <strong>Midwives</strong>, will provide care and services in the<br />
Weeneebayko Area Health Authority (WAHA), which includes the communities <strong>of</strong><br />
Moose Factory, Moosonee, Fort Albany and Attawapiskat. The midwives will provide<br />
midwifery care to women in the catchment area, aiming to return birth to the<br />
community while improving health outcomes.<br />
As part <strong>of</strong> midwifery care services, Roy and Couchie will also provide breastfeeding<br />
education and support and liaise with existing local health programs to reduce<br />
smoking rates, improve nutrition and provide sexual health education.<br />
Recent media reports have shone a light on how underserved the WAHA area<br />
is, particularly with regard to housing, sewage and waste disposal. The need<br />
for maternal care in the area is essential: the closest midwifery practices are in<br />
Hearst and Timmins, both more than 350 km away and the nearest physicians<br />
in the area are located in Moose Factory, more than 200 km away. Women are<br />
typically evacuated from Attawapiskat around 37 weeks to either Moose Factory<br />
(low-risk women), or Timmins or Kingston (high-risk women). Neepeeshowan<br />
<strong>Midwives</strong> wants to reduce evacuations by allowing low-risk women to remain in<br />
the community to birth because, according to Roy, “women should not have to hide<br />
their pregnancy because they are afraid <strong>of</strong> being sent out.”<br />
Roy says she and Couchie are planning on going to Moose Factory this fall for several<br />
months to work with health pr<strong>of</strong>essionals in the local hospital and to look at what<br />
changes need to be made to policies and guidelines for processes such as emergency<br />
medical transfers prior to starting to practice in Attawapiskat.<br />
The new practice marks an important step in expanding midwifery services to remote<br />
areas as well as Aboriginal communities.<br />
AOM welcomes new<br />
registrants into the<br />
pr<strong>of</strong>ession<br />
This list includes new registrant<br />
members from December 10, 2011<br />
to May 31, <strong>2012</strong>:<br />
Erin Bleasdale<br />
Cambridge <strong>Midwives</strong><br />
Khadija Boulaftali<br />
Midwifery Collective <strong>of</strong> Ottawa<br />
Courtney Dini<br />
<strong>Midwives</strong> <strong>of</strong> Sudbury / Sagesfemmes<br />
de Sudbury<br />
Suzan Lorenz<br />
Midwife Alliance<br />
Susannah Merritt<br />
Diversity <strong>Midwives</strong><br />
Jyothy Nair<br />
Talbot Creek <strong>Midwives</strong><br />
Karen Ross<br />
Thames Valley <strong>Midwives</strong><br />
Shezeen Suleman<br />
The <strong>Midwives</strong>’ Clinic <strong>of</strong> East<br />
York-Don Mills<br />
<strong>Ontario</strong> Midwife is published three<br />
times a year by the <strong>Association</strong> <strong>of</strong><br />
<strong>Ontario</strong> <strong>Midwives</strong>. This publication is<br />
available online at www.aom.on.ca,<br />
or you may request a printed copy. All<br />
websites listed are “hotlinked” in the<br />
digital copy. Scroll over the website<br />
address and click to launch the site.<br />
We welcome all feedback. Please<br />
contact commsmanager@aom.on.ca,<br />
or by phone: 416-425-9974 x2261 or<br />
866-418-3773 x2261.<br />
<strong>Association</strong> <strong>of</strong> <strong>Ontario</strong> <strong>Midwives</strong><br />
365 Bloor St. E., Suite 301<br />
Toronto, ON M4W 3L4<br />
www.<strong>Ontario</strong><strong>Midwives</strong>.ca<br />
2<br />
ontario midwife • <strong>Summer</strong> <strong>2012</strong>
Advocacy<br />
<strong>Midwives</strong> protest planned cuts<br />
to refugee health care<br />
<strong>Midwives</strong> across <strong>Ontario</strong> joined other care providers and<br />
concerned citizens on June 18 to protest cuts to the Interim<br />
Federal Health Program, which provides temporary health<br />
coverage to refugees and refugee claimants.<br />
Rallies across Canada including Hamilton, Ottawa and Toronto<br />
drew thousands who oppose the cuts that will come into<br />
effect June 30 and leave already vulnerable populations<br />
without access to medications to treat conditions such as<br />
gestational diabetes, hypertension and nausea and vomiting.<br />
A group <strong>of</strong> approximately 40 midwives attended the Toronto<br />
rally, where midwife Manavi Handa<br />
addressed the crowd to highlight how the<br />
cuts will affect pregnant women.<br />
“The proposed IFHP cuts will result in a<br />
drastic number <strong>of</strong> women with no access to<br />
prenatal care. Prenatal care is well-known to<br />
be one <strong>of</strong> the most cost-effective interventions<br />
in health care and inadequate prenatal<br />
care will result in much sicker mothers and<br />
babies,” Handa said.<br />
Take action now<br />
<strong>Midwives</strong> and supporters who wish to speak<br />
out against the cuts can send Prime Minister<br />
Stephen Harper and Minister <strong>of</strong> Citizenship<br />
and Immigration Jason Kenney an e-postcard<br />
from the <strong>Ontario</strong><strong>Midwives</strong>.ca website.<br />
National campaign<br />
calls for equal access to<br />
midwifery care<br />
On May 5, the Canadian <strong>Association</strong><br />
<strong>of</strong> <strong>Midwives</strong> (CAM) kicked <strong>of</strong>f their<br />
national campaign “Choice. Access.<br />
<strong>Midwives</strong>.” seeking midwifery care for<br />
all Canadian women and babies.<br />
Despite the fact that midwives<br />
are primary care providers in<br />
many provincial health systems,<br />
regulated midwifery care is<br />
currently unavailable to women<br />
living in the Yukon, New Brunswick,<br />
Newfoundland and Labrador and<br />
Prince Edward Island.<br />
Many women living in rural and<br />
remote areas are being sent away<br />
from their families, their support<br />
systems and their communities weeks<br />
before giving birth because they lack<br />
access to obstetrical care.<br />
And, although midwifery care has<br />
been shown to greatly improve health<br />
outcomes in Aboriginal communities,<br />
the federal government is currently<br />
unable to employ midwives on<br />
reserves because the Treasury Board<br />
lacks a job description for midwives.<br />
CAM is urging all midwives and<br />
midwifery supporters to sign an e-letter<br />
addressed to Prime Minister Stephen<br />
Harper, the Federal Minister <strong>of</strong> Health<br />
and other government <strong>of</strong>ficials pushing<br />
for equal access to safe, quality care for<br />
all Canadian women.<br />
CAM is pushing the federal<br />
government to:<br />
• work with and require all<br />
provinces and territories to<br />
legislate and fund midwifery as<br />
part <strong>of</strong> their health care systems;<br />
• support midwives in rural and<br />
remote regions <strong>of</strong> Canada, to<br />
ensure that women can stay in<br />
their communities during the<br />
normal and healthy process <strong>of</strong><br />
pregnancy and birth;<br />
• include a job description for<br />
midwife in the federal Treasury<br />
Board, thereby allowing<br />
midwifery care to become part<br />
<strong>of</strong> direct services <strong>of</strong>fered to<br />
Aboriginal communities under<br />
federal jurisdiction.<br />
Though regulated in <strong>Ontario</strong>, midwifery<br />
care is still out <strong>of</strong> reach for nearly 40% <strong>of</strong><br />
women who seek it here. <strong>Midwives</strong> know<br />
the value <strong>of</strong> keeping birth close to home<br />
and keeping birth within the community.<br />
As the largest group <strong>of</strong> regulated<br />
midwives in Canada, <strong>Ontario</strong> midwives<br />
can prove valuable in voicing the need for<br />
access to midwifery care for all.<br />
<strong>Midwives</strong> can access the letter<br />
campaign on the main page <strong>of</strong> the<br />
CAM website, www.canadianmidwives.org.<br />
Supporters are also urged to<br />
copy the letter and send it to their MP.<br />
www.aom.on.ca 3
AOM News and Updates<br />
<strong>Midwives</strong> bring pay equity message to Queen’s Park<br />
The AOM’s second annual lobby day at<br />
Queen’s Park on May 2,held just three<br />
days before the International Day<br />
<strong>of</strong> the Midwife, was an opportunity<br />
for midwives and clients to educate<br />
MPPs about the key issues facing<br />
the pr<strong>of</strong>ession. It was also a time to<br />
discuss strategies for giving Ontarians<br />
even greater access to midwifery<br />
care. During formal presentations and<br />
casual conversations, politicians from<br />
all three parties learned more about<br />
hospital integration challenges, infrastructure<br />
deficits and the wage parity<br />
gap between midwives and comparable<br />
pr<strong>of</strong>essions. MPPs also shared<br />
their perspectives on maternal and<br />
newborn care in their communities.<br />
Highlights <strong>of</strong> the day included:<br />
• A press conference with Katrina<br />
Kilroy, then president <strong>of</strong> the AOM,<br />
and midwife Vicki Van Wagner,<br />
member <strong>of</strong> the Provincial Council<br />
for Maternal and Child Health,<br />
that focused on issues including<br />
pay equity. Kilroy explained<br />
that due to a long history <strong>of</strong><br />
poor, inconsistent negotiations<br />
between the pr<strong>of</strong>ession and the<br />
government, midwives’ salaries<br />
have not only fallen behind<br />
comparable health care providers,<br />
but they have fallen behind both<br />
the average public sector worker<br />
and the rate <strong>of</strong> inflation.<br />
• Statements on the floor <strong>of</strong><br />
the legislature by Minister <strong>of</strong><br />
Health and Long-Term Care Deb<br />
Matthews, Progressive Conservative<br />
MPP Bill Walker, and NDP<br />
critic for Health and Long-Term<br />
Care France Gélinas honouring<br />
the work that <strong>Ontario</strong> midwives<br />
perform and celebrating International<br />
Day <strong>of</strong> the Midwife (May<br />
5). MPP Gélinas also specifically<br />
mentioned pay equity.<br />
• A luncheon that was attended<br />
by more than 60 MPPs and their<br />
staff. At the event, Minister<br />
Matthews, MPP Bill Walker (PC),<br />
and Deputy House Leader Cindy<br />
Forster (NDP) expressed their<br />
support for midwifery. Katrina<br />
Kilroy and Vicki Van Wagner gave<br />
a presentation on growing and<br />
MPP Bill Walker, Minister <strong>of</strong> Health and Long-Term Care Deb Matthews, MPP Michael Gravelle and MPP Cindy<br />
Forster pose with midwifery client babies at the lobby day lunch reception<br />
strengthening<br />
midwifery care<br />
including pay equity.<br />
For midwife and<br />
former AOM board<br />
member Kelly<br />
Gascoigne, the lobby<br />
day was an “opportunity<br />
to catch the ear<br />
<strong>of</strong> elected <strong>of</strong>ficials.”<br />
At lunch she had an<br />
opportunity to speak<br />
with a number <strong>of</strong><br />
MPPs about issues<br />
such as pay equity.<br />
“It’s so important for<br />
politicians to hear<br />
from frontline workers<br />
and their clients,”<br />
says Gascoigne. “It’s<br />
more meaningful in that<br />
context.”<br />
Gascoigne attended the AOM’s first<br />
lobby day last year, which kicked<br />
<strong>of</strong>f the <strong>Ontario</strong> Needs Birth Centres<br />
provincial election campaign. The<br />
successful campaign culminated in<br />
a March 20, <strong>2012</strong> announcement<br />
by Premier McGuinty and Minister<br />
Matthews to develop two<br />
freestanding, midwifery-led birth<br />
centres.<br />
Midwifery client Kat Tannock and her baby Madi travelled from Peterborough<br />
to be part <strong>of</strong> the day. Photo with MPP Christine Elliott.<br />
“It’s astonishing the impact that you<br />
can have when you make yourself<br />
heard,” says Gascoigne.<br />
Kelly Gascoigne attended this year’s<br />
lobby day with a client, Michelle<br />
Cruz. Cruz said she wanted to attend<br />
because she feels strongly about<br />
midwifery, having been in care with<br />
both her children. She says she found<br />
the lobby day informative and was<br />
surprised to learn how many women<br />
are unable to access midwifery care<br />
4<br />
ontario midwife • <strong>Summer</strong> <strong>2012</strong>
Above: Attorney General John Gerretsen speaks with AOM President Lisa Weston, AOM Executive Director<br />
Kelly Stadelbauer and then-President Katrina Kilroy<br />
Right top to bottom: The AOM produced an information booklet for MPPs regarding the challenges and<br />
opportunities apparent with the growth <strong>of</strong> midwifery; Over 60 MPPs and political staff attended the lunch<br />
and learn session; A client finds a quiet moment during the busy day.<br />
and how much midwifery is growing<br />
in the province. She hopes politicians<br />
came away from the event with<br />
an increased<br />
understanding<br />
<strong>of</strong> the value <strong>of</strong><br />
midwifery care.<br />
“I hope they see<br />
how important<br />
midwifery<br />
Michelle Cruz<br />
is,” says Cruz.<br />
“Women need Midwifery client<br />
the care and<br />
they believe in<br />
it. It’s so important and it needs to be<br />
supported.”<br />
Cruz and Gascoigne plan to schedule a<br />
personal meeting with their local MPP<br />
in the fall to discuss midwifery issues.<br />
A statement made by Minister<br />
Matthews in the legislature on May 2<br />
underlined government support for the<br />
midwifery model.<br />
“Our government recognizes the<br />
enormous<br />
contribution<br />
that midwives<br />
make to our<br />
health care<br />
system and to<br />
the well-being<br />
<strong>of</strong> thousands<br />
<strong>of</strong> women and<br />
their newborn<br />
babies,”<br />
Matthews said. “The number <strong>of</strong><br />
midwives practising is expected<br />
to grow at about 15 per cent per<br />
year. I want to assure them that our<br />
government is fully committed to<br />
supporting this growth in midwives.”<br />
“I hope they see how important midwifery is.<br />
Women need the care and they believe in it.<br />
It’s so important and it needs to be supported.”<br />
To learn more about the lobby day, visit www.<strong>Ontario</strong><strong>Midwives</strong>.ca<br />
www.aom.on.ca 5
AOM Conference and Annual General Meeting<br />
Strength in numbers: supporting the growth <strong>of</strong> midwifery<br />
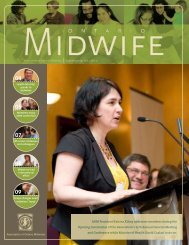
When Minister <strong>of</strong> Health and Long-Term<br />
Care Deb Matthews stopped by<br />
the Annual General Meeting and<br />
Conference closing ceremonies to<br />
announce funding for a practice in<br />
Attawapiskat, the crowd responded<br />
with a standing ovation. Funding<br />
a practice for a remote Aboriginal<br />
community in great need garnered an<br />
emotional reaction from members.<br />
This continued<br />
support for the<br />
growth <strong>of</strong> midwifery<br />
is key as the<br />
first class <strong>of</strong> the<br />
expanded Midwifery<br />
Education Program<br />
(MEP) graduates<br />
this spring. The<br />
MEP now enrolls 90 Elizabeth Brandeis, RM<br />
new students each<br />
AOM vice-president<br />
year at the three<br />
sites combined,<br />
compared with 60<br />
prior to 2008. There are more than 600<br />
midwives currently practicing in <strong>Ontario</strong><br />
and by 2015 it is anticipated there will<br />
be more than 1,000.<br />
This year’s conference theme, Strength<br />
in Numbers, Supporting the Growth<br />
<strong>of</strong> Midwifery, addressed the need<br />
for careful thought about shaping a<br />
growing pr<strong>of</strong>ession and addressing the<br />
challenges inherent to that growth.<br />
Conference presenter and assistant<br />
dean <strong>of</strong> midwifery at McMaster<br />
University Eileen Hutton says the<br />
larger number <strong>of</strong> students has created<br />
a challenge with regard to physical<br />
space for clinical placements.<br />
“When we were starting out, practices<br />
were new, underutilized, there was lots <strong>of</strong><br />
space,” Hutton says. “Now practices have<br />
more midwives but they haven’t changed<br />
space . . . so even if the birth capacity is<br />
there, the space availability isn’t.”<br />
Finding non-midwifery clinical placements<br />
is also proving to be difficult as<br />
other health education programs are<br />
also looking to grow their pr<strong>of</strong>essions.<br />
“We have more students, but the<br />
medical programs have also grown<br />
quite a lot . . . so there is direct competition<br />
for spots,” Hutton says.<br />
Fundamental changes both within<br />
the pr<strong>of</strong>ession and beyond will<br />
have to be explored to help address<br />
the changing needs <strong>of</strong> a growing<br />
pr<strong>of</strong>ession, Hutton says.<br />
“Having our own standards allow us to<br />
advocate on behalf <strong>of</strong> our clients who<br />
may choose care that may not be reflected<br />
in other pr<strong>of</strong>essional guidelines yet is<br />
evidence-based, reasonable and safe.”<br />
Universities may need to work with<br />
hospitals to change how placements<br />
work; Hutton suggested a “package<br />
deal” where hospitals who want<br />
medical residents<br />
also get midwifery<br />
students, nursing<br />
students and<br />
physiotherapy<br />
students, among<br />
others.<br />
As the pr<strong>of</strong>ession<br />
grows, some<br />
hospitals are<br />
capping the<br />
number <strong>of</strong><br />
midwives<br />
practicing there.<br />
Hospitals and<br />
health care providers need to work<br />
together to find solutions to support<br />
the growth <strong>of</strong> midwifery. For example,<br />
having OBs on salary would enable<br />
midwives to attend increasing<br />
numbers <strong>of</strong> low-risk births, Hutton<br />
suggested.<br />
<strong>Association</strong> <strong>of</strong> <strong>Ontario</strong> <strong>Midwives</strong><br />
vice-president Elizabeth Brandeis’s<br />
conference panel presentation focused<br />
on how a greater understanding is<br />
needed <strong>of</strong> both the similarities and<br />
differences between the midwifery<br />
model and care provided by obstetricians<br />
and other providers.<br />
“It’s important to establish where<br />
common ground exists,” she says.<br />
“Working in interpr<strong>of</strong>essional groups<br />
like MoreOB and labour and delivery<br />
committees allows midwives to<br />
interact on a more personal level<br />
with leaders in the hospital and<br />
set the tone for understanding the<br />
foundation on which differences may<br />
exist and when common standards<br />
are appropriate.”<br />
She noted that advocating for midwifery<br />
community standards is an essential<br />
part <strong>of</strong> growing a strong pr<strong>of</strong>ession.<br />
“If we don’t have our own midwifery<br />
community standards, we are forced<br />
to conform to other established<br />
standards,” she says. “Having our own<br />
standards allows us to advocate on<br />
behalf <strong>of</strong> our clients who may choose<br />
care that may not be reflected in other<br />
pr<strong>of</strong>essional guidelines yet is evidencebased,<br />
reasonable and safe.”<br />
Advocating for midwifery standards<br />
in a hospital setting and educating<br />
other pr<strong>of</strong>essionals about midwifery is<br />
critical. Brandeis says midwives should<br />
initiate conversation via planning a<br />
rounds or presenting to a committee.<br />
Using tools such as clinical practice<br />
guidelines (CPG) can depersonalize<br />
conflict and show hospital colleagues<br />
that midwives are part <strong>of</strong> a wellinformed<br />
pr<strong>of</strong>essional community.<br />
“Our clients come to us with the<br />
expectation that their choices will be<br />
respected and supported. CPGs provide<br />
a framework for us to inform and<br />
support our clients in a range <strong>of</strong> diverse<br />
choices,” she says. “When the conversation<br />
is about the client and supporting<br />
her autonomy and choice, the issues can<br />
move away from ‘us vs. them’ and focus<br />
on client-centred, evidence-based care<br />
that supports normal birth.”<br />
Providing support toward the kind <strong>of</strong><br />
research that informs tools such as the<br />
CPGs is an important next step in moving<br />
midwifery forward, Hutton says. Though<br />
other pr<strong>of</strong>essions can tap into dedicated<br />
pockets <strong>of</strong> funding, such as hospital<br />
competitions, midwives have few<br />
funding streams to support research.<br />
“In the last 20 years we’ve focused<br />
on building a very strong education<br />
program and strong practices . . . and<br />
we are getting to a size where we can<br />
put money into (research),” Hutton<br />
says. “Practice didn’t evolve without<br />
lots <strong>of</strong> support, and I think research is<br />
no different.”<br />
One <strong>of</strong> the benefits <strong>of</strong> expanding<br />
the MEP and growing the number<br />
<strong>of</strong> midwives is that strength really<br />
does come in numbers. Now more<br />
than ever, midwives can capitalize<br />
on opportunities for creating new<br />
practices, improving hospital<br />
relations, and advocating for<br />
dedicated research funds.<br />
6<br />
ontario midwife • <strong>Summer</strong> <strong>2012</strong>
Top left to right: National Aboriginal Council <strong>of</strong> <strong>Midwives</strong> (NACM) Vice-President Kerry Bebee with Aboriginal midwife<br />
Dorothy Green; AOM members Natalie Kirby and Melissa Bevan check out the exhibitor booths<br />
Centre left to right: Suzanne McGurn, Assistant Deputy Minister, Ministry <strong>of</strong> Health and Long-Term Care and AOM board<br />
member Esther Willms; Members Mary Sharpe and Elana Johnson visit with Opening Ceremonies speaker and Toronto Star<br />
columnist Catherine Porter; Members Jasmine Chatelain and Aimée Carbonneau share a conference hug<br />
Bottom left to right: Canadian <strong>Association</strong> <strong>of</strong> <strong>Midwives</strong> (CAM) President Anne Wilson and AOM President Lisa Weston;<br />
HIROC CEO Peter Flattery, AOM Director <strong>of</strong> Insurance and Risk Management Bobbi Soderstrom and Rogers Partners LLB<br />
Sr. Partner Don Rogers ; Registered Nurses <strong>Association</strong> <strong>of</strong> <strong>Ontario</strong> (RNAO) President Rhonda Seidman-Carlson, RNAO CEO<br />
Doris Grinspun and AOM Executive Director Kelly Stadelbauer
Student Pr<strong>of</strong>iles<br />
Recent graduates bring new energy<br />
and perspectives to midwifery<br />
In an attempt to address a shortage <strong>of</strong> obstetrical care in <strong>Ontario</strong>, the provincial<br />
government announced an expansion in 2007 <strong>of</strong> the Midwifery Education<br />
Program (MEP) that would eventually see an additional 30 students per year<br />
enrolling in the MEP, bringing each class to 90.<br />
This spring, the first class <strong>of</strong> the expanded MEP graduated, helping to bump the<br />
number <strong>of</strong> practicing midwives in <strong>Ontario</strong> to more than 600.<br />
Meet three newly graduated midwives who are coming into the pr<strong>of</strong>ession as part <strong>of</strong><br />
this first expanded class.<br />
Stephanie Biswell<br />
(McMaster)<br />
Witnessing the prevailing racism in<br />
her community while growing up,<br />
Stephanie Biswell didn’t identify closely<br />
with her Aboriginal heritage.<br />
“It’s hard in Winnipeg to be outwardly<br />
Aboriginal, so I ‘whited’ myself as much<br />
as possible,” Biswell says.<br />
All <strong>of</strong> that changed over the course<br />
<strong>of</strong> completing the MEP at McMaster<br />
University, which Biswell graduated<br />
from in May.<br />
“A large part <strong>of</strong> my growing and selfawareness<br />
came from my classmates,”<br />
she says. “I realized that being Aboriginal<br />
is a key part <strong>of</strong> who I am and I really<br />
embrace it.”<br />
Thanks to her husband’s work in<br />
Mozambique, Biswell had visions <strong>of</strong><br />
traveling to remote communities in<br />
Africa to provide maternity care when<br />
she first joined the program. But over<br />
time and thanks to a placement at a<br />
clinic in downtown Winnipeg, Biswell<br />
shifted her view <strong>of</strong> how she’d like to practice midwifery.<br />
“I still have visions <strong>of</strong> doing oversees work and seeing<br />
midwifery from a global perspective, but I’ve also seen how I<br />
have a lot <strong>of</strong> work to do here, in part with Aboriginal women.<br />
These are my people who need help, and I am in this position<br />
and I should help.”<br />
Biswell is this year’s winner <strong>of</strong> the Murray and Eleanor<br />
Enkin Midwifery Award at McMaster – which is awarded<br />
to a graduating student who exemplifies superior<br />
achievement in the humanitarian, pr<strong>of</strong>essional and<br />
academic domains <strong>of</strong> midwifery practice.<br />
Biswell says that beyond her clinical learning, midwifery<br />
education has also helped expand her perspective and develop<br />
a broader sense <strong>of</strong> cultural understanding.<br />
“I was young when I joined the program . . . and I felt maybe<br />
I had come into it with all <strong>of</strong> these ideas <strong>of</strong> what people were<br />
like or the world was like. (But) you realize the world isn’t so<br />
narrow and you can’t make decisions about how people are.<br />
It’s a life-long journey to never really close <strong>of</strong>f how I think<br />
about something or put people in a box.”<br />
Biswell has accepted a position with Burlington and Area<br />
<strong>Midwives</strong> and expects to start providing clinical care this<br />
summer.<br />
8<br />
ontario midwife • <strong>Summer</strong> <strong>2012</strong>
Heather Heinrichs (Laurentian)<br />
Though Heather Heinrichs faced many <strong>of</strong> the common challenges<br />
inherent to the MEP – such as juggling class work while being on<br />
call – the toughest by far was having her apartment burn down<br />
during her Normal Childbearing placement.<br />
“I had to take a week <strong>of</strong>f and sort out my life . . . it was definitely<br />
a struggle trying to adapt to not having any <strong>of</strong> my notes or text<br />
books,” she says. “But I persevered and got through it.”<br />
That kind <strong>of</strong> determination will serve her well as she moves<br />
forward with the career she long dreamed about. Growing up,<br />
Heinrichs gained an interest in midwifery when she read The<br />
Midwife’s Apprentice, a book geared toward young women.<br />
“I thought being a midwife was really cool, but the book takes<br />
place in the Middle Ages and I thought, doctors deliver babies<br />
now, I can’t do that.”<br />
Heinrichs not only learned that she could in fact be a midwife,<br />
but now also has long-term aspirations <strong>of</strong> eventually returning to<br />
her hometown <strong>of</strong> Winnipeg and setting up an Aboriginal-focused<br />
midwifery practice.<br />
Herself Métis, Heinrichs says she has found a great fit with<br />
Seventh Generation <strong>Midwives</strong> Toronto, where she completed<br />
her senior-year placement and will also be completing her new<br />
registrant year.<br />
“I feel really well supported by Seventh Generation <strong>Midwives</strong>,<br />
in learning to be a midwife and in setting up my own<br />
midwifery practice.”<br />
Rachel Dennis (Ryerson)<br />
Long before she even thought <strong>of</strong> entering<br />
the pr<strong>of</strong>ession, Rachel Dennis was having<br />
an effect on midwifery clients.<br />
In an effort to spend more time<br />
together, Dennis’s<br />
mom, midwife<br />
Carol Couchie,<br />
would bring<br />
Dennis along to<br />
postpartum visits.<br />
One such visit was<br />
to a new mom<br />
having trouble<br />
breastfeeding.<br />
Rachel Dennis, RM<br />
“My mom said,<br />
‘Rachel was such a<br />
good breastfeeder,<br />
I brought her along as a good luck<br />
charm,’” Dennis recalls. And her luck<br />
proved true – the baby latched that day.<br />
Years later at a goodbye party for<br />
Couchie, who was moving out <strong>of</strong><br />
Toronto, a woman and her daughter<br />
approached Dennis. It was the mother<br />
from that day.<br />
“She said, ‘this is the girl who helped<br />
you breastfeed.’ It shocked me that she<br />
remembered me and linked me to that<br />
amazing moment,” Dennis says. “Even<br />
though I didn’t think <strong>of</strong> it as a career,<br />
midwifery was having an impact on<br />
me for a very<br />
long time.”<br />
Despite<br />
growing<br />
up around<br />
midwifery and<br />
attending her<br />
first birth at<br />
age 12, Dennis<br />
says she<br />
never really<br />
considered<br />
it as a viable<br />
career for herself until she was in her<br />
twenties.<br />
“It just kind <strong>of</strong> dawned on me one<br />
day in terms <strong>of</strong> thinking what I could<br />
do as a career where I could benefit<br />
other people and work with babies<br />
and women,” Dennis says. “I thought<br />
about all the times I came across my<br />
“I thought about all the times I came across<br />
my mom with clients and all the things they<br />
said about how she made their experience so<br />
wonderful and life changing and I thought,<br />
okay, maybe I can do that.”<br />
Recent midwifery graduate<br />
mom with clients and all the things<br />
they said about how she made their<br />
experience so wonderful and life<br />
changing and I thought, okay, maybe I<br />
can do that.”<br />
Without previous experience in a<br />
university setting, Dennis credits<br />
Ryerson’s Aboriginal Student Services<br />
for providing a support system that<br />
helped her succeed.<br />
“Without them, I would have felt<br />
isolated,” Dennis says, noting she<br />
valued the academic counselling<br />
services the centre provided, as well<br />
as socialization opportunities and<br />
the ability for her to give back while<br />
working as a peer support worker .<br />
Dennis graduated in June as part<br />
<strong>of</strong> Ryerson’s MEP and plans to start<br />
working at Seventh Generation<br />
<strong>Midwives</strong> Toronto later this year, after<br />
taking some time <strong>of</strong>f following the<br />
birth <strong>of</strong> her second child this summer.<br />
www.aom.on.ca 9
Rural and Remote Practice<br />
Locum Program fosters sustainability and growth <strong>of</strong> rural and remote practice<br />
In many rural, remote and northern<br />
communities, midwifery care is<br />
provided by a solo midwife or by<br />
a small practice. Rural and remote<br />
midwives accept the challenges <strong>of</strong><br />
working in smaller and sometimes<br />
isolated communities, and the<br />
additional strain <strong>of</strong> being completely<br />
tied to their work. Unlike midwives in<br />
larger midwifery practice groups, they<br />
can’t rely on their colleagues to access<br />
time <strong>of</strong>f-call. The Locum Program<br />
provides much needed vacation and<br />
emergency relief for rural and remote<br />
midwives, allowing them to recharge<br />
and relax or to tend to pressing<br />
personal matters. This in turn helps<br />
midwifery to remain strong in small<br />
communities.<br />
In 2009, the AOM introduced a<br />
program to respond to the needs<br />
<strong>of</strong> rural and remote midwives with<br />
funding from the Ministry <strong>of</strong> Health<br />
and Long-Term Care. The AOM Rural<br />
and Remote Locum Program provides<br />
relief for midwives for holidays,<br />
illness, emergencies, continuing<br />
education or parental leave. It<br />
enables midwives to turn <strong>of</strong>f their<br />
pagers with the confidence that their<br />
clients are in the experienced hands<br />
<strong>of</strong> another midwife.<br />
For Natalie Kirby, who usually<br />
works at <strong>Midwives</strong> Nottawasaga in<br />
Collingwood, a locum placement<br />
allowed her to support a solo midwife<br />
in Powassan, near Kirby’s hometown<br />
<strong>of</strong> North Bay. While on locum, Kirby<br />
gained insight into the life <strong>of</strong> a solo<br />
midwife when she was on call for 28<br />
days in a row. During her second week<br />
she attended four births, three in<br />
hospital and one at home.<br />
“Being a solo midwife is an incredible<br />
responsibility,” says Kirby. She says<br />
being able to provide relief to the<br />
local midwife and provide care to her<br />
clients was very rewarding. “Balance<br />
is essential in our career. You need<br />
time to be pager-free so you can sleep,<br />
travel or do whatever you need to do.”<br />
She was also happy to ensure that<br />
clients had the birth experiences<br />
they were seeking. “If a locum didn’t<br />
come, the women might have been<br />
transferred out <strong>of</strong> midwifery care<br />
and wouldn’t have<br />
had home visits,”<br />
says Kirby.<br />
Susan Wilts, a<br />
solo midwife at<br />
Huron Community<br />
Midwifery Services<br />
in Auburn, uses her<br />
time <strong>of</strong>f to volunteer<br />
with a medical team<br />
in Haiti. For the past<br />
four years, the Locum<br />
Program has enabled<br />
midwife Maggie<br />
Fioravanti to care<br />
for Susan’s clients<br />
while she is away.<br />
Wilts says Fioravanti<br />
(who retired from St.<br />
Jacobs <strong>Midwives</strong> in 2008) is the ideal<br />
person to relieve her because she has<br />
extensive experience with Old Order<br />
Amish and Mennonite women, who<br />
make up 80 percent <strong>of</strong> Wilts’s practice.<br />
According to Wilts, Fioravanti also<br />
has the sense <strong>of</strong> adventure needed to<br />
navigate southwest Bruce County in<br />
the middle <strong>of</strong> winter. Many <strong>of</strong> Wilts’s<br />
clients live on rural roads that don’t<br />
appear on maps and aren’t plowed<br />
between 9:30 p.m. and 4:30 a.m. –<br />
even if there’s been a snowstorm. Her<br />
clients don’t have telephones and<br />
Top and above: Collingwood midwife Natalie Kirby provided <strong>of</strong>f-call relief for<br />
a solo midwife in northern <strong>Ontario</strong> during a locum placement in Powassan,<br />
near Kirby’s hometown <strong>of</strong> North Bay. She was on call for 28 days straight and<br />
attended four births in one week.<br />
there is limited cell phone service in<br />
the area. Babies are <strong>of</strong>ten delivered by<br />
lantern light and using the bathroom<br />
means a cold walk to the outhouse.<br />
“A midwife (working in this area)<br />
definitely has to have a good vehicle,<br />
warm clothes and boots, and a GPS,”<br />
says Wilts.<br />
As midwifery in <strong>Ontario</strong> grows with<br />
more practices in rural and remote<br />
areas <strong>of</strong> the province, the AOM Locum<br />
Program will continue to support<br />
midwives and sustain midwifery care<br />
in these communities.<br />
To find out more about the Rural and Remote Locum Program,<br />
please contact the AOM at 416-425-9974 or 1-866-418-3773 x2257.<br />
10<br />
ontario midwife • <strong>Summer</strong> <strong>2012</strong>
Clinical Practice Guidelines Update<br />
New CPG will facilitate evidence-based midwifery care<br />
related to hypertensive disorders<br />
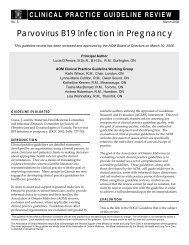
The AOM’s newest Clinical Practice Guideline (CPG), Hypertensive<br />
Disorders <strong>of</strong> Pregnancy, provides a critical review<br />
<strong>of</strong> research questions relating to midwifery care and the<br />
screening, diagnosis, assessment and monitoring <strong>of</strong> hypertensive<br />
disorders <strong>of</strong> pregnancy (HDP).<br />
The new HDP CPG replaces AOM<br />
CPG No. 4: Guideline for Monitoring<br />
Blood Pressure in Pregnancy. It is now<br />
available at www.aom.on.ca under the<br />
health care pr<strong>of</strong>essionals tab.<br />
For the first time ever, the AOM has<br />
produced a summary document to<br />
accompany the new CPG. Designed<br />
for busy clinicians, the summary<br />
contains key highlights as well as a<br />
complete list <strong>of</strong> recommendations for<br />
practice from the full HDP CPG. The<br />
six-page summary provides midwives<br />
Pictured to the right: the AOM’s latest CPG on<br />
hypertensive disorder and the first ever CPG<br />
summary on HDP.<br />
with easy access to some <strong>of</strong> the most essential content <strong>of</strong><br />
the CPG. The document is intended to be used in conjunction<br />
with the full HDP CPG, not instead <strong>of</strong> it. For a complete<br />
analysis <strong>of</strong> the research relevant to HDP and midwifery<br />
practice, along with all citations, midwives are strongly<br />
encouraged to read the full CPG.<br />
An AOM Clinical Practice Guideline Summary<br />
Hypertensive DisorDers <strong>of</strong> pregnancy<br />
Hypertensive disorders <strong>of</strong> pregnancy (HDP) are a major<br />
cause <strong>of</strong> poor pregnancy outcome in Canada and internationally.<br />
HDP encompasses a spectrum <strong>of</strong> conditions,<br />
including pre-existing hypertension, gestational hypertension<br />
and preeclampsia. These conditions range in severity<br />
from a mild increase in blood pressure at term to multisystem<br />
conditions with the potential for significant harm. For<br />
many <strong>of</strong> the clinical manifestations <strong>of</strong> HDP, optimal strategies<br />
for prevention and management have yet to be determined,<br />
with delivery <strong>of</strong> the fetus being the only definitive<br />
treatment. Despite extensive research, the onset <strong>of</strong> hypertension<br />
during pregnancy has proven difficult to predict.<br />
Definition and Classification <strong>of</strong> HDP<br />
See Society <strong>of</strong> Obsetricians and Gynaecologists <strong>of</strong> Canada<br />
(SOGC) Clinical Practice Guideline No. 206: Diagnosis,<br />
Evaluation and Management <strong>of</strong> the Hypertensive Disorders<br />
<strong>of</strong> Pregnancy.<br />
• Hypertension in pregnancy is defined as a dBP ≥ 90<br />
mmHg, based on the average <strong>of</strong> at least two measurements<br />
taken using the same arm.<br />
• Severe hypertension is defined as a sBP ≥ 160<br />
mmHg or a dBP ≥ 110 mmHg.<br />
• Proteinuria is defined as a urinary protein measurement<br />
equal to or greater than 0.3g/day in a 24-hour<br />
urine collection or ≥ 30 mg/mmol urinary creatinine<br />
in a spot urine sample.<br />
Hypertensive disorders <strong>of</strong> pregnancy should be classified<br />
as pre-existing or gestational hypertension based on<br />
gestational age (GA) at diagnosis.<br />
• Pre-existing hypertension: diagnosis before pregnancy<br />
or prior to 20 weeks’ GA. In women with<br />
pre-existing hypertension, preeclampsia is defined<br />
by the presence <strong>of</strong> one or more <strong>of</strong> the following at<br />
or after 20 weeks’ GA:<br />
» resistant hypertension<br />
» new or worsening proteinuria<br />
» one or more other adverse conditions*<br />
• Gestational hypertension: Diagnosis at or after 20 weeks’<br />
GA. In women with gestational hypertension, preeclampsia<br />
is defined by the presence <strong>of</strong> one or both <strong>of</strong>:<br />
» new-onset proteinuria<br />
» one or more <strong>of</strong> the other adverse conditions*<br />
For a full description <strong>of</strong> research questions<br />
relating to midwifery and hypertensive disorders<br />
<strong>of</strong> pregnancy (HDP), please refer to the<br />
full HDP CPG at http://bit.ly/aomcpgs<br />
• Severe preeclampsia is defined as preeclampsia<br />
with onset before 34 weeks’ GA, with heavy proteinuria<br />
or one or more other adverse conditions.*<br />
• HELLP syndrome is charactherized by hemolysis, elevated<br />
liver enzymes and low platelet count. It can<br />
occur either with or without other typical symptoms<br />
<strong>of</strong> preeclampsia.<br />
*Adverse conditions associated with preeclampsia<br />
• Maternal symptoms: persistent or new/unusual<br />
headache, visual disturbances, persistent abdominal<br />
or right upper quadrant pain, severe nausea or<br />
vomiting, chest pain or shortness <strong>of</strong> breath.<br />
• Maternal signs <strong>of</strong> end-organ dysfunction: seizures,<br />
severe hypertension, pulmonary edema, or suspected<br />
placental abruption.<br />
• Fetal morbidity: oligohydramnios, intrauterine<br />
growth restriction, absent or reversed end-diastolic<br />
flow in the umbilical artery by Doppler velocimetry,<br />
or intrauterine fetal death.<br />
• Abnormal maternal laboratory testing:<br />
» elevated serum creatinine (see below)<br />
» elevated AST, ALT or LDH with symptoms<br />
(see below)<br />
» platelet count < 100 x 10 9 /L<br />
» serum albumen < 20 g/L<br />
NORMAL VALUES IN PREGNANCY<br />
First<br />
trimester<br />
Second<br />
trimester<br />
Third<br />
trimester<br />
Creatinine (µmol/L) 35-62 35-71 35-80<br />
AST (SGOT) (U/L) 3-23 3-33 4-32<br />
A LT (SGPT) (U/L) 3-30 2-33 2-25<br />
LDH (U/L) 78-433 80-447 82-524<br />
Source: James D, Steer P, Weiner C et al. Pregnancy and laboratory<br />
studies: a reference table for clinicians. Obstet Gynecol.<br />
2010 Apr;115(4):868<br />
Emergency Skills Workshops<br />
The <strong>Association</strong> <strong>of</strong> <strong>Ontario</strong> <strong>Midwives</strong><br />
reminds members that all registered<br />
midwives in <strong>Ontario</strong> are required to<br />
recertify in emergency skills every two<br />
years in order to maintain their registration<br />
with the College <strong>of</strong> <strong>Midwives</strong><br />
<strong>of</strong> <strong>Ontario</strong>.<br />
Register early because space is limited<br />
and sessions sell out.<br />
The AOM is pleased to <strong>of</strong>fer the<br />
following courses.<br />
August 24, <strong>2012</strong> - Hamilton<br />
Crowne Plaza Hamilton<br />
Pavillion BC<br />
150 King St. East<br />
September 7, <strong>2012</strong> - Markham<br />
Holiday Inn & Suites Markham<br />
Ellesmere Room<br />
7095 Woodbine Ave.<br />
September 14, <strong>2012</strong> - Ottawa<br />
Travelodge Ottawa Hotel &<br />
Conference Centre<br />
Greenery Room<br />
1376 Carling Ave.<br />
November 16, <strong>2012</strong> - Toronto<br />
<strong>Association</strong> <strong>of</strong> <strong>Ontario</strong> <strong>Midwives</strong><br />
365 Bloor St. E. Suite 301<br />
Fees:<br />
AOM Member - $325.00<br />
ESW Workbook (2009 version) -<br />
$45.00<br />
Session times:<br />
AM: 08:30 - 12:30 or<br />
PM: 13:30 - 17:00<br />
To register for any <strong>of</strong> these sessions<br />
visit the AOM member site to register<br />
online, or print the registration form<br />
on the website and mail or fax it back<br />
to the address provided.<br />
If you require any additional information<br />
please do not hesitate to<br />
contact ESW Co-ordinator Kristina<br />
Mullen at events@aom.on.ca or by<br />
calling (416) 425-9974 x 2255.<br />
www.aom.on.ca 11
Choice.<br />
Access.<br />
<strong>Midwives</strong>.<br />
Registration Now Open!<br />
Accès.<br />
Choix.<br />
Sages-<br />
Femmes.<br />
Register before September 7, <strong>2012</strong> and save up to $75!<br />
For more information including travel discounts and booking accommodations, visit:<br />
www.canadianmidwives.org/conference<br />
CAM’s 12 th AGM, Conference & Exhibit<br />
October 17 to 19, <strong>2012</strong><br />
Sheraton Hotel<br />
St. John’s, Newfoundland & Labrador<br />
12 ième AGA, congrès et exposition ACSF<br />
du 17 au 19 octobre, <strong>2012</strong><br />
Hôtel Sheraton<br />
Saint-Jean de Terre-Neuve & Labrador