Dr Ho Kerr Asia Ceramics 2012 ( PDF )
Dr Ho Kerr Asia Ceramics 2012 ( PDF )
Dr Ho Kerr Asia Ceramics 2012 ( PDF )
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
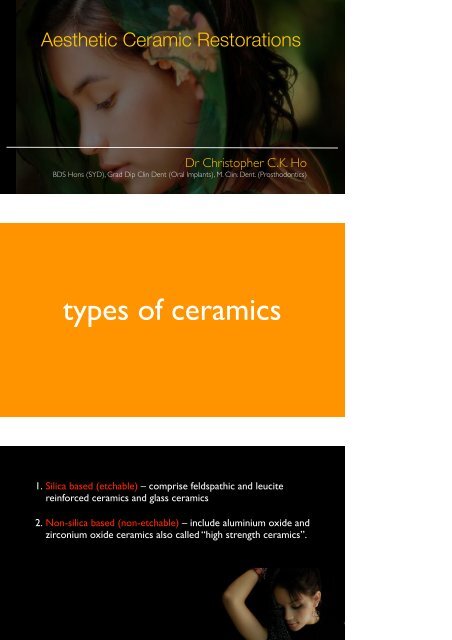
Aesthetic Ceramic Restorations<br />
<strong>Dr</strong> Christopher C.K. <strong>Ho</strong><br />
BDS <strong>Ho</strong>ns (SYD), Grad Dip Clin Dent (Oral Implants), M. Clin. Dent. (Prosthodontics)<br />
types of ceramics<br />
1. Silica based (etchable) – comprise feldspathic and leucite<br />
reinforced ceramics and glass ceramics<br />
2. Non-silica based (non-etchable) – include aluminium oxide and<br />
zirconium oxide ceramics also called “high strength ceramics”.
SILICA BASED!<br />
•Feldspathic<br />
•Leucite containing. E.g. Empress Esthetic<br />
•Lithium Disilicate containing. E.g. E.max<br />
ceramics<br />
NON-SILICA BASED, HIGH STRENGTH<br />
CERAMICS<br />
•Glass infiltrated alumina (InCeram)<br />
• Procera alumina (densely sintered alumina)<br />
•Zirconia (Y-TZP)<br />
Physical Properties (Strength)<br />
• Flexural strength (bending strength) (MPa): maximum<br />
vertical load that material can support without<br />
fracture<br />
Three point.<br />
• Fracture toughness (Kic): ability of a material<br />
containing a crack to resist enlargement (MPa m1/2)<br />
Flexural strengths<br />
Fracture toughness<br />
MPa m1/2<br />
SILICA BASED CERAMICS<br />
Feldspathic 200 MPa 1.77<br />
Emax 400 MPa 3.0<br />
HIGH STRENGTH CERAMICS<br />
Alumina >600 MPa 5.0<br />
Zirconia >1100 MPa 10.0
Optical translucency/Aesthetics<br />
Strength<br />
7<br />
Silica based <strong>Ceramics</strong><br />
• Higher the glass content - better optical properties,<br />
but weaker mechanical properties<br />
• Need to be bonded for strength<br />
• Etch: hydrofluoric acid<br />
• Silanisation<br />
• Adhesive bonding<br />
• Examples: feldspathic porcelain, leucite, lithium<br />
disilicate<br />
Lithium Disilicate<br />
Press<br />
• 15+ years. Lost wax process, wax up, sprue, invest and<br />
press ceramic.<br />
CAD<br />
• Computer aided design and milling, blue phase then<br />
sintered.
Monolithic Block<br />
Mouth motion-simulator NYU<br />
• None of lithium disilicate crowns failed below 1,000N<br />
and 1 million cycles.<br />
• Veneered zirconia crowns 50% crowns failed - veneer<br />
chip-off fractures by 100 K cycles at 200N.<br />
• 90% veneered zirconia crowns tested failed by 100 K<br />
cycles at 350 N.<br />
Stick bite<br />
Photographs<br />
Bite records<br />
Stump shade<br />
12
1.Shade of restoration<br />
2.Stump shade<br />
3.Cement colour<br />
All-ceramics Restoration Colour<br />
Matching shades<br />
14<br />
Light Reflection<br />
Angle of camera relative to labial surface influences reflectance<br />
To record colour and internal character camera should be placed at<br />
15-30 degree angle for reduced light reflectance.<br />
15
Stump Shades<br />
16<br />
Communication with lab<br />
Stump shade<br />
This enables excellent control of the shade and<br />
brightness during the individual production steps.<br />
17
E.max Restorations<br />
• HT ingots (High Translucency)<br />
• LT ingots (Low Translucency)<br />
• MO ingots (Medium Opacity)<br />
• HO ingots (High Opacity)<br />
• Impulse ingots (Value, Opal)<br />
Tetracycline Discolouration
SILICA BASED!<br />
CERAMIC MATERIALS<br />
•Feldspathic<br />
•Leucite containing. E.g. Empress Esthetic<br />
•Lithium Disilicate containing. E.g. E.max<br />
NON-SILICA BASED, HIGH STRENGTH<br />
CERAMICS<br />
•Glass infiltrated alumina (InCeram)<br />
• Procera alumina (densely sintered alumina)<br />
•Zirconia (Y-TZP)
High Strength (Non-etchable) <strong>Ceramics</strong><br />
• Aesthetic characteristics, mechanical properties and<br />
biocompatability<br />
• Glass infilitrated ceramics – Inceram<br />
• Densely sintered high purity aluminium oxide ceramic –<br />
Procera alunmina.<br />
• Zirconium oxide ceramics - LAVA, Procera Zi, Cercon, Everest<br />
Zirconia !<br />
• LAVA (3M)<br />
• Everest (Kavo),<br />
• Procera Zircon (NobelBiocare)<br />
• Cercon (Denstply),<br />
• Zfx (zfx)<br />
Flexural strengths<br />
Fracture toughness<br />
SILICA BASED CERAMICS<br />
HIGH STRENGTH CERAMICS<br />
Feldspathic 200 MPa 1.77<br />
Emax Press 400 MPa 3.0<br />
Alumina >600 MPa 5.0<br />
Zirconia >1100 MPa 10.0
Empress Procera Alumina Zirconia<br />
Grain size impacts translucency and strength<br />
Zirconia Indications<br />
Anterior crowns<br />
Posterior crowns<br />
Bridgework frameworks<br />
Abutments<br />
Zirconia - YTZP<br />
• Superior flexural strength and fracture toughness - transformation<br />
toughening<br />
• Three different crystal structures - cubic, tetragonal, monoclinic<br />
• Tetragonal to monoclinc transformation around 1000 C - large vol<br />
increase and shear strains. Addition of ytria - stabilises Zr<br />
tetragonal phase at room temp. Y-TZP = yttria tetragonal zirconia<br />
polycrystals
37<br />
• Crack propagation - Tetragonal crystal to monoclinic.<br />
• 4% increase in crystal size which resists crack propagation.<br />
• Zirconia not self-healing - crack can only be resisted once.<br />
•<br />
Placing in the furnace cannot change the crystal and heal the crack.<br />
38
Limitations of Zirconia<br />
• Poorer light transmission, due to reduced glass content.<br />
• Higher value, optical opacity.<br />
• Supragingival margins may be visible<br />
• Concern with delamination, chipping<br />
Veneering <strong>Ceramics</strong><br />
• Coefficients of thermal expansion (CTE) of both ceramics<br />
have to be checked against each other, especially for zirconia<br />
which shows a relatively low CTE (approx. 10 ppm).<br />
• Special veneer ceramics with the same or lower CTE have<br />
been developed during the last few years
Proper Support<br />
Powder-condenstation<br />
Slip Casting<br />
All-ceramic Manufacturing<br />
<strong>Ho</strong>t Pressing<br />
CAD CAM<br />
CAD CAM
CAD CAM<br />
• Precision<br />
• Material <strong>Ho</strong>mogeneity<br />
• Material Quality<br />
• Economic<br />
• Guarantee<br />
Materials Available<br />
• Titanium<br />
• Zirconia<br />
• Glass ceramic - Lithium disilicate<br />
• Alumina<br />
• Co-Cr<br />
• PMMA<br />
• Nano-composite<br />
Ceramic choices: <strong>Ho</strong>’s opinion<br />
Translucency Masking ability Strength<br />
Feldspathic High Low Low<br />
Leucite and<br />
lithium disilicate<br />
Variable Variable Medium<br />
Alumina Medium Good<br />
Zirconia Low Good<br />
Medium-high<br />
High
Ceramic choices: <strong>Ho</strong>’s opinion<br />
Veneers Onlays/Inlays Crowns Bridgework<br />
Feldspathic<br />
porcelain<br />
Leucite<br />
containing<br />
Lithium<br />
Disilicate<br />
++++ + - -<br />
++++ +++ - -<br />
+++ ++++ +++ ++ anteriors<br />
Alumina + - +++ ++ anteriors<br />
Zirconia --- --- +++<br />
+++ ant. and<br />
49<br />
post.<br />
provisionalisation<br />
temporary cementation<br />
Purpose:<br />
“To restore, protect and maintain the position of prepared teeth between<br />
appointments and until the placement of the permanent crown or bridge”<br />
Provisionalisation<br />
“Test run for Esthetics”
Provisionalisation
Crowns<br />
Tempbond NE or Tempbond Clear<br />
Eugenol containing provisional cements<br />
inhibits the set of resin<br />
Temporary Try-in
cementation
Cement Requirements<br />
Non irritant to pulp and gingiva (gums)<br />
Cariostatic or anticariogenicity<br />
Strong bond with enamel and dentin<br />
Provide good marginal sealing<br />
Insoluble<br />
Aesthetics<br />
Radio-opaque<br />
Translucency<br />
cementation<br />
adhesive<br />
Chemical and micro-mechanical<br />
non-adhesive<br />
Micro-mechanical<br />
1. Zinc phosphate<br />
CEMENT<br />
TYPES<br />
2. Polycarboxylate<br />
3. Glass Ionomer Cements<br />
4. Resin-modified GIC<br />
5. Resin Cements
Cementation<br />
What type of ceramic??<br />
....Silica based or high strength<br />
Cementation<br />
Silica based Resin Cement<br />
E.max Self adhesive RC or Resin cement<br />
Zr Conventional, Self adhesive RC or Resin cement<br />
E.max<br />
Crowns: adhesive or non-adhesive cementation - no difference clincial studies<br />
Partial coverage restorations (inlays, onlays, veneers): adhesive cementation<br />
increase retention and fracture resistance
GIC<br />
RMGIC<br />
SELF-ADHESIVE<br />
RESIN<br />
TRADITIONAL<br />
RESIN<br />
Compressive<br />
Strength<br />
Weak Moderate Strong Strongest<br />
Flexural strength Weak Moderate Strong Strongest<br />
Fluoride content High High Minimal No Fluoride<br />
Aesthetics Average Good Best Best<br />
Sensitivity Risk Low Low Minimal Moderate<br />
Adhesive strength Low/Moderate Moderate Moderate/high High<br />
3<br />
TYPES of RESIN CEMENTS<br />
1<br />
Adhesive<br />
System<br />
Resin Cement<br />
(Light, Chemical or Dual Cure)<br />
11<br />
Self-adhesive Cement<br />
E.g. Maxcem Elite,<br />
Unicem, G-Cem,<br />
Speedcem,<br />
111<br />
Self-etching Primer<br />
with cement<br />
E.g. Panavia F2.0,<br />
Multilink automix<br />
Self-adhesive resin cement<br />
Easy conventional technique<br />
Low solubility and high<br />
strength<br />
High level radiopacity<br />
Light Cure<br />
High-strength restorations only<br />
! •! Lithium disilicate (e.g. IPS e.max)<br />
! •! Metal & Metal-Ceramic<br />
! •! Oxide Ceramic (Zirconia, Alumina)<br />
Adequate retention in prep design<br />
! •! Less than 8 degree taper<br />
! •! Minimum 4mm height<br />
Adequate thickness of restoration
Self-adhesive Cements Adhesion<br />
ENAMEL<br />
• Shear bond strength 14.5 MPa lower than resin cements 17-32 MPa<br />
• Lower after thermocycling, c.f. Resin cements<br />
• Still higher than GIC cements<br />
DENTINE<br />
Similar results to resin<br />
cements for SBS, tensile<br />
bond strength<br />
Abo-Hamar SE et al, Clin Oral Investig 2005<br />
Al-Assaf et al, Dentl Mater 2007<br />
De Munck et al 2004<br />
Self-adhesive Cements Adhesion<br />
• Adhesion comparable to multi-step resin cements<br />
• LC higher bond strengths<br />
• Adhesion to enamel appears to be weaker<br />
• Etching detrimental to dentinal adhesion - extreme precision if<br />
applying to enamel<br />
Maxcem Elite<br />
• Tack cure or Self Cure (2-3<br />
minutes)<br />
• 5 colours (clear, white, white<br />
opaque, yellow, brown)
Self-adhesive Cement<br />
Contraindication<br />
Lacking retention either taper or min axial height<br />
Or<br />
Minimal ceramic thickness<br />
Adhesive Resin Cement<br />
All types of restorations<br />
! •! Including Feldspathic, Leucite,<br />
Any preparation design<br />
! •! Retentive and non-retentive<br />
Any thickness<br />
! •! Including “thin” veneer restorations<br />
NX3<br />
• Automix syringe - dual-cure<br />
• Single syringe light-cure cement<br />
• Proprietary amine-free initiator system and optimized resin matrix,<br />
• Overcomes known incompatibilities between resin cements and<br />
newer acidic adhesives<br />
Clear White Yellow Bleach White Opaque
• amine-free redox initiator system and well-balanced resin matrix,<br />
the NX3 dual-cure formula is the first truly color stable adhesive<br />
resin cement<br />
Prior to Cementation<br />
Assess from Lab<br />
• Check fit<br />
• Assess if any cracks/crazing
Remove temporary restorations<br />
• Use a flat plastic, haemastat<br />
• If cannot remove, can slice through carefully and torque apart<br />
• Any staining - hydrogen peroxide<br />
• Clean preps - pumice slurry
Tryin<br />
• <strong>Dr</strong>y and individually<br />
• Not apply excessive pressure while trialling<br />
veneers, as they are brittle prior to bonding.<br />
Incomplete seating<br />
Occlusion<br />
• Remaining provisional material,<br />
• Luting resin that has not been removed<br />
• Tight contact points<br />
• High strength ceramics check<br />
• Veneers do not check<br />
Veneer Cementation<br />
Try in - assess fit and contact<br />
points<br />
• articulating paper<br />
• lipstick<br />
• black marker
TRY IN CEMENTS (use for veneers)<br />
(IPS e.max Press,etched with 5<br />
percent hydrofluoric acid for 20<br />
seconds.<br />
1.Try-in paste to verify shade<br />
2.Start with clear try-in paste<br />
3.Veneer not bright enough, try white cement<br />
4.Still too dark - recommend adding opaque to the clear try-in<br />
paste in 5% increments until the desired value is obtained.<br />
Minimal influence on final colour 10-15%<br />
>25% opaque white will tend to make the veneer look artificial<br />
Let patient see them – try in paste (different try in<br />
pastes to modify colour<br />
Use of water soluble try-in paste<br />
Patient should not be asked to<br />
check occlusion as this may cause<br />
fracture of an unbonded veneer<br />
Hydrofluoric Acid Etch<br />
• Increase surface area<br />
• Micro-mechanical retention<br />
• Clean surface
Etch – 37% phosphoric if lab<br />
has etched ceramic already<br />
Silanisation<br />
• Chemical bond between resin matrix and hydroxylated porcelain surface<br />
• Increase wettability of surface<br />
• Hydrolysed - one bottle system - shorter shelf life and can be<br />
detrimental if expired<br />
Silanate – air dry<br />
1. Apply 2-3 coats of fresh silane<br />
2. Air dry for more than 1 minute
Veneer Cementation<br />
•All at once or a few at the time<br />
•Light cured resin cement only<br />
Dual/Self cure Colour change<br />
• Catalyst and base: tertiary amines undergo a colour change.<br />
• Clinical darkening – known as “amine discolouration”
Use of opaque cements<br />
•Opaque resin cements - metal oxide particle e.g. TiO2.<br />
•Unpredictable slight variations in film thickness, alter<br />
the value<br />
•Optically distinct does not blend at margins visible<br />
margin - poorer longevity<br />
Veneer Cementation<br />
1. “Wave” technique<br />
2. “Tack” technique<br />
Wave technique<br />
• Seating the veneer waving the curing light few seconds.<br />
• Partially polymerises - gel state<br />
•<br />
Excess cement removed with a brush or a gum stimulator
Pull floss through lingually<br />
TACK TECHNIQUE<br />
2-4 mm tack tip<br />
Spot tacks the veneer stabilising the veneer at the correct position
Tack Technique Cleanup – Use Butler<br />
Gum Stimulator or Bendabrush
Bleeding when bonding<br />
aaaaaaaaaaahhhhhhhh!!!!!! $#%@!!!!!<br />
• Bleeding happens after you etch, and before bond – need to<br />
control bleeding and re-etch<br />
• Bleeding after bond placed and cured– wash, rebond and cure<br />
• While placing veneer. Don’t panic, cure your veneer straight<br />
away.<br />
High Strength <strong>Ceramics</strong>
High Strength <strong>Ceramics</strong> Cementation:<br />
Conventional or Adhesive?<br />
Zinc Phosphate GIC Resin Cement<br />
109<br />
Bonding to High Strength <strong>Ceramics</strong><br />
• High strength alumina or zirconia ceramics do not have a silicon oxide phase.<br />
• Cannot be roughened by etching with hydrofluoric acid<br />
• Activation: Sanblast intaglio Al2O3 or use COJET (3M)<br />
Conventional Cementation<br />
• Conventional cements e.g. RMGIC, ZnPo4,<br />
Adhesive Luting<br />
• Panavia<br />
• Self-adhesive: Maxcem Elite/Unicem<br />
• COJET and conventional resin cementation<br />
Zr primers<br />
Silane coupling agents alone do not<br />
promote chemical bonding<br />
Use a ceramic primer containing an<br />
acidic adhesive monomer, such as<br />
MDP for the priming of zirconia-based<br />
ceramics.<br />
Dent Mater. 2010 Apr;26(4):345-52. Epub 2010 Jan 4.<br />
New zirconia primer improves bond strength of resin-based cements.<br />
Magne P, Paranhos MP, Burnett LH Jr.<br />
111
MDP based Zirconia Primer<br />
• Bisco Z Prime Plus single-component priming agent<br />
• Enhance adhesion between indirect restorative materials and resin<br />
cements. It is used as a surface treatment for zirconia, alumina,<br />
metal/alloy, composite, endodontic posts, and intraoral repairs.<br />
Cementation<br />
The use of the MDP-containing composite resin Panavia F on air abraded<br />
zirconia ceramic can be recommended as promising bonding method.<br />
Wolfart M, et al. Durability of the resin bond strength to zirconia ceramic after using different surface<br />
conditioning methods. Dent Mater. 2007;23:45-50.<br />
Blatz MB, et al. In vitro evaluation of shear bond strengths of resin to densely-sintered high-purity<br />
zirconium-oxide ceramic after long-term storage and thermal cycling. J Prosthet Dent.<br />
2004;91:356-362.<br />
Kern M, Wegner SM. Bonding to zirconia ceramic: adhesion methods and their durability. Dent<br />
Mater. 1998;14:64-71.<br />
Cementation to Zirconia<br />
• GIC minimal bond strength 4MPa, susceptible to water degradation<br />
• Self adhesive cements - phosphate monomers effective bond to<br />
methacrylate
Summary of Cementation<br />
All-ceramic crowns/bridgework (High Strength - Zirconia/alumina):<br />
• Sandblast with Al2O3 and conventional cementation e.g. Maxcem Elite,, GIC, Zinc<br />
Phosphate, etc.<br />
• Sandblast with Al2O3 and Panavia<br />
• Cojet, silane and dual cure resin cement<br />
• Zirconia primer and resin cement<br />
RECOMMENDATION<br />
All-ceramic crowns/bridgework (High Strength - Zirconia/alumina):<br />
Sandblast with Al2O3, and self-adhesive cement<br />
When Should Zirconia-Based<br />
Ceramic Restorations be Bonded?<br />
Cementation with Self-adhesive Resin Cement<br />
Tooth preparation with adequate cervical-occlusal height: h ><br />
4mm<br />
Tooth preparation with adequate taper: a = 2 - 5 degree<br />
Bonding with Adhesive Resin Cement<br />
Tooth with short clinical crown: h < 4mm<br />
Tooth with over-tapered preparation: a > 5 degree
Feldspathic<br />
porcelain<br />
Leucite<br />
containing<br />
Lithium<br />
disilicate<br />
Alumina<br />
Zirconia<br />
Resin Cement<br />
Resin Cement<br />
Resin cement or self-adhesive cement<br />
1.Conventional cement<br />
2. Surface activation and Panavia resin cement or phosphate monomer<br />
containing cement<br />
3. COJET or Zr primer and resin cement<br />
1.Conventional cement<br />
2. Surface activation and Panavia resin cement or phosphate monomer<br />
containing cement<br />
3. COJET or Zr primer and resin cement<br />
118<br />
OUTLINE<br />
• Adhesive dentistry and isolation<br />
• Ceramic types and preparation for bonding<br />
• Cementation<br />
• Finishing and Polishing<br />
• Maintenance and complications<br />
finishing and polishing
Finishing and Polishing<br />
AIMS<br />
• Anatomical form and contour<br />
• Marginal integrity and adaptation<br />
• Smooth surface - resist stain and plaque accumulation<br />
• High lustre and aesthetics<br />
Customising Cases<br />
Rough porcelain surfaces<br />
• Abrasion of opposing and adjacent teeth<br />
• Plaque accumulation and retention<br />
• Reduction in strength of porcelain
Intra-oral polishing can equal or surpass smoothness of glazed porcelain<br />
Fracture toughness of polished porcelain > glazed porcelain and<br />
that both types of finish were equally resistant to staining by<br />
coffee<br />
Rosenstiel SF et al, Int J Prosthodont1989; 2:524-9<br />
before cementation......<br />
Polishing rubbers<br />
Red band football and flame<br />
Shofu Ceramaster KN7<br />
after cementation......<br />
• Minimal cement to clean up<br />
• #12 blade<br />
•<br />
•<br />
<strong>Ho</strong>rico saws, Cerisaw, Finishing strips<br />
Margins: rotary instrument to finish the<br />
margins - may remove the glaze layer<br />
increasing the roughness of the porcelain<br />
and cause increased plaque retention
after cementation......<br />
Optishine (<strong>Kerr</strong>)<br />
Optrafine (Ivoclar)<br />
without water
#12 Blade – removing excess<br />
Finishing strips<br />
Checking Occlusion multiple units, veneers<br />
• Only when bonded<br />
• Begin with centric occlusion<br />
• Adjust with diamonds and silicone points<br />
• Bilateral synchronous contacts on posteriors, with light contact<br />
on anteriors<br />
• Canine guidance<br />
• Preventive occlusal splint?
case examples
Tx plan<br />
• Hygiene - perio<br />
• Diagnostic models and waxup<br />
• Mock up with increase in length prior to preparation<br />
• Gingival recontouring<br />
• Porcelain veneer/crowns<br />
• Occlusal splint/implant tx for posterior missing teeth
Anna
T H A N K Y O U