JCMC Nursing Annual Report - Mountain States Health Alliance
JCMC Nursing Annual Report - Mountain States Health Alliance
JCMC Nursing Annual Report - Mountain States Health Alliance
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
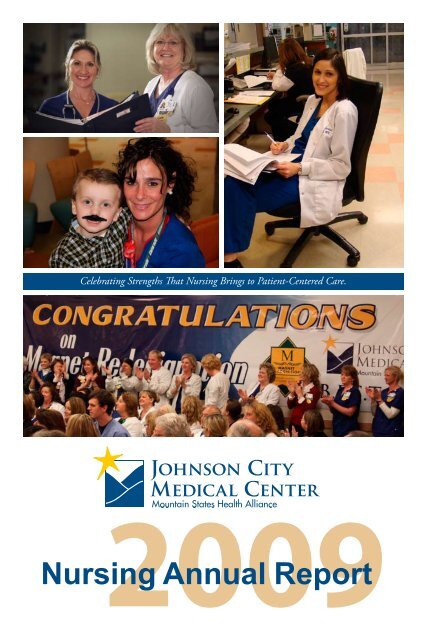
Celebrating Strengths That <strong>Nursing</strong> Brings to Patient-Centered Care.<br />
Johnson City<br />
Medical Center<br />
2009<br />
<strong>Nursing</strong> <strong>Annual</strong> <strong>Report</strong>
From the Chief <strong>Nursing</strong> Officer<br />
It is with great<br />
pleasure that I am<br />
writing to you as the<br />
chief nursing officer<br />
to acknowledge the<br />
nursing excellence<br />
evidenced at Johnson<br />
City Medical Center.<br />
Being the first hospital<br />
in Tennessee to<br />
achieve Magnet status<br />
and redesignation<br />
has provided us with an opportunity to focus on our<br />
success as a Magnet organization by “Celebrating the<br />
Strengths That <strong>Nursing</strong> Brings to Patient-Centered<br />
Care.” These strengths are the key to excellence and<br />
our overall success at Johnson City Medical Center<br />
( <strong>JCMC</strong>). The strengths cross all Magnet forces and<br />
provided the basis for our redesignation success and<br />
the evidence that our nursing staff is continuously<br />
identifying new ways to improve how patient care is<br />
delivered.<br />
The exemplars identified by the Magnet Site<br />
appraisers included our strategic plan to eliminate<br />
travel nurses with the onboarding of 120 new grads<br />
and the hiring of 10.6 FTEs of support in clinical<br />
resource nurses and educational roles to support<br />
the transition of the new grads. The projected cost<br />
savings for elimination of contract labor, an 84-hour<br />
cardiovascular option, an Emergency Department<br />
weekend staffing option, the use of i-choice<br />
scheduling options and nursing role definitions have<br />
been estimated at $7.2 million. We also exceeded<br />
Magnet expectations in disseminating quality<br />
data throughout the organization. Our personal<br />
Blueprint cards, based on our four pillars of quality,<br />
Magnet cited as an exemplar for communicating<br />
quality data to all team members. We exceeded<br />
Magnet expectations in providing adequate resources<br />
for consultation and access to nursing expertise to<br />
nurses at all levels in the organization and fiscal<br />
allocations for affiliated schools and colleges of<br />
nursing based on the identification of needs within<br />
the nursing program to meet the goals for health care<br />
in the region. They commended the examples offered<br />
that demonstrate how nurses are used in promotional<br />
materials, brochures, advertisements, newspaper<br />
articles, television and radio advertisements, direct<br />
mailings, educational booklets, pamphlets and<br />
community activities. <strong>JCMC</strong> was congratulated on<br />
providing resources that include tuition support,<br />
scholarships and flex time to attend school, and<br />
demonstrating support to nurses, financially, to<br />
attend different conferences or symposiums.<br />
With our Magnet redesignation, it will truly be<br />
a year to celebrate our excellence. ANCC honors<br />
all the newly designated and redesignated Magnet<br />
organizations at the National Magnet Conference<br />
each year. We look forward to receiving this honor<br />
at the 2010 ANCC National Magnet Conference<br />
in Phoenix, Oct. 13-15, 2010, at the Phoenix<br />
Convention Center.<br />
We also realized a successful Joint Commission<br />
survey and achieved, for a second time, the TNCPE<br />
Governor’s Award for Excellence.<br />
Over the past five years, our organization<br />
has made significant investments in improving<br />
recruitment and retention. RN recruitment, turnover<br />
and retention are now blueprint measures for the<br />
CNO and her nursing leaders. We now have 150<br />
students enrolled in our scholarship program who<br />
will be employed at the completion of their RN<br />
program. We are developing LPN to RN and LPN<br />
to BSN programs. We have also implemented a<br />
<strong>JCMC</strong> Nurse Retention Committee. With these new<br />
initiatives and dedicated resources, our recruitment<br />
numbers have shown an increase for this year.<br />
In addition, to recognize and financially reward<br />
excellence at the bedside, the “BEST” Nurse (Bedside<br />
Excellence Shining Through) Clinical Advancement<br />
Program at Johnson City Medical Center is the spirit<br />
and practice of caring for patients, families and the<br />
community through leadership, knowledge and<br />
compassion. We believe that nursing is both an art<br />
and a science incorporating multiple realms of care<br />
including the physical, developmental, emotional,<br />
social, psychological, cultural and spiritual. <strong>Nursing</strong><br />
2
exemplifies the highest degrees of accountability,<br />
integrity and honesty in all relationships with<br />
patients, families, colleagues and community. The<br />
nurse is a patient advocate committed to upholding<br />
the American Nurses Association’s Code of Ethics<br />
for Nurses and other professional and regulatory<br />
standards of nursing practice and patient care. The<br />
program supports nursing practice by assisting<br />
the retention of experienced, motivated bedside<br />
nurses in direct patient care by acknowledging their<br />
professional development. We now have 250 BEST<br />
nurses at <strong>JCMC</strong>.<br />
Many accomplishments, advances, contributions<br />
and innovations have been mentioned in the<br />
preceding paragraphs and will be expanded upon<br />
throughout the <strong>Annual</strong> <strong>Report</strong>. I applaud the efforts<br />
that have been undertaken that substantiate the<br />
achievement of Magnet redesignation.<br />
I am very proud of our nursing staff for<br />
their professional contributions, as well as their<br />
commitment to our patients, Johnson City Medical<br />
Center and our community.<br />
Congratulations on a year of excellence. This<br />
certainly is a time to celebrate our strengths.<br />
Inside<br />
Contents<br />
Congratulations from Senior Leadership............4<br />
New Magnet Model.................................................5<br />
Magnet Redesignation.............................................6<br />
Transformational Leadership.................................8<br />
Structural Empowerment.................................... 10<br />
Exemplary Professional Practice......................... 14<br />
New Knowledge, Innovation<br />
and Improvement.................................................. 18<br />
Imperical Quality Outcomes.............................. 21<br />
Niswonger Children’s Hospital.......................... 23<br />
Years of Service....................................................... 24<br />
Pressure Ulcers....................................................... 26<br />
Turnover.................................................................. 26<br />
Rapid Response...................................................... 27<br />
Pat Niday, VP, CNO<br />
bringing loving care to health care | www.msha.com 3
A Message from the CEO<br />
This was a year of<br />
accolades for nurses at<br />
<strong>JCMC</strong> and Quillen<br />
Rehabilitation Hospital.<br />
The achievement of<br />
redesignation as a<br />
Magnet Hospital for<br />
<strong>Nursing</strong> in 2009 was<br />
confirmation of the<br />
excellence of nursing and<br />
nurses at these hospitals. Many people worked long,<br />
hard hours to write the application that told our<br />
story about nursing and its accomplishments. We<br />
continued to make significant strides in improving<br />
the quality of patient care, including the aspects<br />
of patient care that are so dependent on nursing<br />
expertise, such as preventing falls and pressure ulcers,<br />
decreasing the rate of infections and preventing<br />
ventilator-associated pneumonia. This excellence<br />
was recognized by the Magnet examiners and in the<br />
granting of redesignation.<br />
We also received an excellent report from our<br />
Joint Commission survey, with no requirements<br />
for improvement in nursing cited. What a truly<br />
outstanding accomplishment! And if those<br />
accomplishments weren’t enough, nurses contributed<br />
significantly to the winning of the prestigious<br />
Tennessee Center for Performance Excellence Award<br />
after a site visit to our facilities in November 2009.<br />
Many other accomplishments are presented in this<br />
<strong>Annual</strong> <strong>Report</strong> for <strong>Nursing</strong>. Nurses are making major<br />
contributions to the improvement of patient care<br />
and safety in our hospitals, and their efforts are being<br />
recognized. As we navigate the uncertain future of<br />
healthcare reform, it is very clear to me that nurses are<br />
ready to take a significant leadership role in designing<br />
a system that works for our patients and communities<br />
and actually improves health and wellness and the<br />
ability of people to have better lives.<br />
I am very proud of every nurse who has contributed<br />
to the successes of the past year. Congratulations<br />
on this wonderful year of achievement, and I am<br />
privileged to work with you and support you in your<br />
efforts.<br />
Candace Jennings, senior VP, CEO<br />
4
New Magnet Model<br />
Global Issues in <strong>Nursing</strong> and <strong>Health</strong> Care<br />
Structural<br />
Empowerment<br />
Transformational<br />
Leadership<br />
Empirical<br />
Outcomes<br />
New Knowledge,<br />
Innovations &<br />
Improvements<br />
Exemplary<br />
Professional<br />
Practice<br />
Transformational Leadership:<br />
The CNO in a Magnet organization is a knowledgeable transformational leader who develops a strong vision<br />
and well-articulated philosophy, professional practice model and strategic and quality plans in leading nursing<br />
services.<br />
Structural Empowerment:<br />
Magnet structural environments are generally flat, flexible and decentralized. Nurses throughout the<br />
organization are involved in self-governance and decision-making structure and processes that establish<br />
practice and address issues of concern.<br />
Exemplary Professional Practice:<br />
A professional practice model is the overreaching conceptual framework for nurses, nursing care and<br />
interdisciplinary patient care. It depicts how nurses practice, collaborate, communicate and develop<br />
professionally to provide the highest quality of care for those served by the organization.<br />
New Knowledge, Innovations and Improvements:<br />
Magnet organizations integrate evidence-based practice and research into clinical and operational processes.<br />
Nurses are educated about evidence-based practice and research, which enables them to explore the safest and<br />
best practices and to generate new knowledge.<br />
Empirical Outcomes:<br />
<strong>Nursing</strong> makes an essential contribution to patient, nursing workforce and community outcomes. The<br />
measurement of quality outcomes is imperative and directly related to nursing leadership and clinical practice<br />
in Magnet organizations.<br />
American Nurses Credentialing Center. (2008). Application Manual Magnet Recognition Program.<br />
Silver Springs, MD: Author.<br />
bringing loving care to health care | www.msha.com 5
Magnet Redesignation<br />
When Johnson City Medical Center was named<br />
a Magnet Hospital by the American Nurses<br />
Credentialing Center in 2005, it was the first<br />
hospital in the state to receive that prized distinction.<br />
Since that time, only Vanderbilt Medical Center<br />
in Nashville has also received the honor of being<br />
recognized as one of the state’s top places for a nurse<br />
to work.<br />
On Wednesday, Nov. 18, 2009, <strong>JCMC</strong> achieved<br />
Magnet designation for a second time.<br />
“The commission on Magnet was very impressed<br />
with the great work done at Johnson City Medical<br />
Center and Quillen Rehabilitation Hospital, and as<br />
a result of some outstanding work, the Commission<br />
voted unanimously to redesignate Johnson City<br />
Medical Center as a Magnet organization,”<br />
said Karen Drenkard, director of the Magnet<br />
Recognition Program. “When you reach the level<br />
that redesignation demonstrates, it shows such<br />
commitment, and it’s very, very difficult to have<br />
sustained effort toward quality. The excellence in<br />
patient care that was demonstrated at Johnson City<br />
Medical Center makes the community very fortunate<br />
to have such a team.”<br />
The ANCC is the arm of the American Nurses<br />
Association, and Magnet status is the ANCC’s<br />
highest honor. It is also considered one of the<br />
highest possible levels of achievement for a medical<br />
facility on any level. The award is bestowed only<br />
after criteria from a book of standards are in place,<br />
evidence is gathered to support the claim, review of<br />
written responses is complete and an on-site, threeday<br />
visit by a team of Magnet appraisers has taken<br />
place. A Magnet hospital is the gold standard in<br />
patient care and the highest honor of excellence, and<br />
only around 2 percent of the 6,000 hospitals in the<br />
United <strong>States</strong> have earned the title.<br />
As the news was delivered to more than 100 nurses<br />
and administrators gathered together inside<br />
Niswonger Children’s Hospital, President and CEO<br />
Dennis Vonderfecht said he was again filled with<br />
pride for the work of the nurses inside the hospital.<br />
“We are very honored. This is truly exciting knowing<br />
we were the first hospital in the state to receive the<br />
designation in 2005, and to know we are now the<br />
only hospital in Tennessee to earn the redesignation.<br />
The nursing staff at Johnson City Medical Center<br />
truly is bringing loving care to each and every one of<br />
its patients,” Vonderfecht said.<br />
Candace Jennings, MSHA senior vice president of<br />
Tennessee operations and a registered nurse, said,<br />
“This is a reflection of something we already know,<br />
and that is our nurses are wonderful and make The<br />
MSHA Difference.”<br />
6
inging loving care to health care | www.msha.com 7
Transformational Leadership<br />
(Forces of Magnetism: Quality of <strong>Nursing</strong> Leadership, Management Style)<br />
Global Issues in <strong>Nursing</strong> and <strong>Health</strong> Care<br />
Structural<br />
Empowerment<br />
Transformational<br />
Leadership<br />
Empirical<br />
Outcomes<br />
New Knowledge,<br />
Innovations &<br />
Improvements<br />
Exemplary<br />
Professional<br />
Practice<br />
Transformational leadership describes nurses who are<br />
knowledgeable, strong risk-takers who follow a wellarticulated,<br />
strategic philosophy in the day-to-day<br />
operations of nursing services. Nurses, at all levels of<br />
the organization, convey a strong sense of advocacy,<br />
vision and support for the nursing staff and for the<br />
patient.<br />
Pat Niday, VP and CNO, conveys a strong and<br />
supportive role as our chief nursing officer at Johnson<br />
City Medical Center. Under the CNO’s scope of<br />
practice, Pat has direct-line authority responsibilities<br />
and matrix responsibilities where nursing is practiced<br />
at <strong>JCMC</strong>. Pat is the leader with the development<br />
of our MSHA <strong>Nursing</strong> Strategic Plan that outlines<br />
strategies for optimizing outcomes through improved<br />
clinical processes, enhancing financial performance<br />
and creating a safe environment for patients and<br />
caregivers. Promoting patient safety, quality nursing<br />
care, and patient and nursing satisfaction are major<br />
components in ensuring Patient-Centered Care,<br />
positive patient outcomes and integrity in everything<br />
we do.<br />
8
Results from the 2009 NDNQI RN Satisfaction Survey demonstrate an increase in <strong>Nursing</strong> Management<br />
T-Scores over this past year. Our nursing leaders, Pat Niday and Candace Jennings, RN, senior vice president/<br />
CEO of Washington County Operations, serve as strong and visible leaders for the front-line team members<br />
of <strong>JCMC</strong>. Pat and Candace attend the newly restructured <strong>Nursing</strong> Retention Committee, which is<br />
co-chaired by front-line nurses and the manager of Human Resources.<br />
Johnson City Medical Center<br />
<strong>Nursing</strong> Management T-Scores<br />
bringing loving care to health care | www.msha.com 9
Structural Empowerment<br />
(Forces of Magnetism: Organizational Structure, Personnel Policies and Programs, Community and the<br />
<strong>Health</strong>care Organization, Image of <strong>Nursing</strong>, Professional Development)<br />
Structural<br />
Empowerment<br />
Global Issues in <strong>Nursing</strong> and <strong>Health</strong> Care<br />
Transformational<br />
Leadership<br />
Empirical<br />
Outcomes<br />
New Knowledge,<br />
Innovations &<br />
Improvements<br />
Exemplary<br />
Professional<br />
Practice<br />
Magnet nurses throughout Johnson City Medical<br />
Center and Quillen Rehab Hospital are involved<br />
in self-governance, decision-making structures,<br />
processes that establish standards of practice, address<br />
issues of concern and information dissemination.<br />
The front-line team member is the central core to<br />
our Shared Governance structure. Nurses and other<br />
care providers contribute through multidisciplinary<br />
partnerships throughout the organization to improve<br />
patient outcomes and the health of the communities<br />
they serve.<br />
Unit-based councils are the functioning units or<br />
the “worker bees” that give and receive information.<br />
The flow of information is bidirectional and<br />
horizontal between and among professional nurses<br />
at the bedside, the leadership team and the CNO.<br />
Nurses extend their support and commitment to the<br />
professional growth of nursing through these shared<br />
governance councils, professional organizations and<br />
community service.<br />
BEST Nurse Program<br />
The BEST Nurse Clinical Advancement Program is based on the Synergy Model and Jean Watson’s Theory<br />
of Human Caring. The BEST (Bedside Excellence Shining Through) Nurse Clinical Advancement Program<br />
was developed by and for bedside nurses at MSHA. The BEST Nurse program recognizes the value of the<br />
clinical bedside nurse by evaluating the following eight characteristics: clinical judgment, advocacy and moral<br />
agency, caring practices, collaboration, systems thinking, response to diversity, clinical inquiry, and facilitator<br />
of learning. The BEST nurse exhibits knowledge-seeking behaviors and takes advantage of educational<br />
opportunities that enhance optimal evidence-based care.<br />
The BEST program supports nursing practice by facilitating the retention of experienced, motivated bedside<br />
nurses by supporting their professional development, diversity in field of practice and clinical excellence at<br />
the bedside. Nurses achieve points in the BEST program that translate into a higher level in the program<br />
and an increase in wages. Points are earned for professional education, teaching, volunteering and preceptor<br />
achievements. For each level achieved, the nurse receives a percentage increase in base pay. After a successful<br />
6-month introductory period, nurses can apply to the program, where the applications are peer reviewed<br />
by a panel of BEST nurses. Since August 2008, 33% of 750 eligible RNs have participated in the program,<br />
compared to 3-5% participation in the previous program.<br />
10
NDNQI Scores<br />
The NDNQI RN Satisfaction Survey measures different aspects of the nurse’s satisfaction with his/her work.<br />
Included here are graphs depicting RN-RN Interactions, Decision Making and Professional Development.<br />
All of these characteristics showed an improvement from 2008 to 2009.<br />
RN-RN Interactions<br />
RN-RN Interactions is the combination of scores related to the following comments: <strong>Nursing</strong> personnel pitch<br />
in and help each other when things get in a rush, it is hard for new nurses to feel “at home” on the unit, there is<br />
a good deal of teamwork among nursing personnel, the nurses on our unit support each other.<br />
Johnson City Medical Center<br />
Rn-Rn Interactions T-Scores<br />
Decision Making<br />
Decision Making is the combination of scores related to the following comments: There is ample opportunity<br />
for nursing staff to participate in administrative decision-making processes, they can count on nursing<br />
administrators to back them up, nursing administrators generally consult with the staff on daily problems.<br />
Johnson City Medical Center<br />
Decision Making T-Scores<br />
11<br />
bringing loving care to health care | www.msha.com
Professional Development<br />
Professional Development is the combination of scores related to the following comments: They have career<br />
development opportunities, they have access to regional and national conferences, they have opportunities for<br />
advancement, they have clinical nurse specialists who provide patient care consultations.<br />
Johnson City Medical Center<br />
Professional Development T-Scores<br />
Volunteering Enhances Image of <strong>Nursing</strong> in the Community<br />
Magnet nurses contribute to the organization and<br />
community and are recognized for their positive<br />
effect on patients and families. Nurses who volunteer<br />
enhance the image of nursing in the community. The<br />
exemplar written by Candy Mink, RN, expresses in<br />
her own words her volunteering experience during<br />
the RAM (Remote Area Medical) event held in<br />
Wise, Va. Candy is a registered nurse at Quillen<br />
Rehabilitation Hospital.<br />
“Volunteering to work the RAM event was<br />
something I had wanted to do for several years.<br />
When I registered for the event, I was not sure what<br />
I would be assigned to do because I registered as a<br />
volunteer after all the nursing positions had been<br />
filled.<br />
“Driving to the location (Wise County Fairgrounds)<br />
at 5:30 a.m. was the beginning of the day’s adventure.<br />
Soon after turning onto the small, two-lane road<br />
leading into the site, the traffic stopped. There was<br />
bumper-to-bumper traffic heading to the fairground.<br />
“After arriving and registering in, I was given a name<br />
badge that read ‘support staff.’ In other words, do<br />
whatever needed to be done.<br />
“The number of volunteers was amazing, and<br />
they were from all walks of life. Volunteers were<br />
needed for everything from emptying trash cans to<br />
performing surgery. I met people who had traveled<br />
from Oregon and Michigan just to volunteer at this<br />
event.<br />
“The services provided were huge. There were<br />
medical services, mammograms, bone density tests,<br />
pap tests, vision care with eyeglasses, and dental care<br />
from cleaning, fillings, X-rays and extractions to<br />
oral surgery. There were pharmacy services, social<br />
services, and a tent with free clothes and toys. There<br />
were many teaching activities, and free samples with<br />
educational literature.<br />
“The patients were the primary concern for the event,<br />
and all were very grateful for the care they received.<br />
They were either uninsured or under-insured and<br />
continued<br />
12
unable to afford health care. It seemed the biggest<br />
need for the majority of the patients was for dental<br />
care. Patients waited in long, hot lines for hours for<br />
dental services. The tents for the dental services were<br />
full of rows and rows of dental chairs and they were<br />
all filled with patients. As soon as one person got up,<br />
another was waiting to take their place.<br />
“One of my duties as support staff was to escort<br />
patients from one area to another area. Another task<br />
was to take a patient’s place in line while they either<br />
had to have a restroom break or go to a different area<br />
for a different service. I didn’t do any actual nursing<br />
duties, but I worked side by side with students,<br />
secretaries, housewives, nurses and even a hospital<br />
CEO in assisting the patients to obtain the care they<br />
needed.<br />
“What I learned from this experience is that there are<br />
people in our own back yards in dire need of health<br />
care. These people each have their own stories to tell.<br />
Often the look on their faces is a glimpse into their<br />
life struggles.<br />
“Another thing I learned is that the world is still full<br />
of good people. People are willing to give days at a<br />
time out of their schedule to volunteer and in some<br />
way be a help to another person.<br />
“At the end of the day, I was hot, tired and dirty, but<br />
grateful for the experience. The things I learned that<br />
day were things that could not be learned from a<br />
classroom or a book.”<br />
13<br />
bringing loving care to health care | www.msha.com
Exemplary Professional Practice<br />
(Forces of Magnetism: Professional Models of Care, Consultation and Resources, Autonomy, Nurses as<br />
Teachers, Interdisciplinary Relations, Quality of Care: Ethics, Patient Safety and<br />
Quality Infrastructure, Quality Improvement)<br />
Transformational<br />
Leadership<br />
Global Issues in <strong>Nursing</strong> and <strong>Health</strong> Care<br />
Structural<br />
Empowerment<br />
Empirical<br />
Outcomes<br />
New Knowledge,<br />
Innovations &<br />
Improvements<br />
Exemplary<br />
Professional<br />
Practice<br />
A professional practice model is the overarching<br />
conceptual framework for nurses, nursing care and<br />
interdisciplinary relationships. It is a schematic<br />
description of a system or theory that depicts how<br />
nurses practice, collaborate, communicate and<br />
develop professionally to provide the highest quality<br />
of care for those served by the organization.<br />
Candace Jennings, senior VP, CEO, and Pat Niday,<br />
VP, CNO, as part of their roles and responsibilities,<br />
are to ensure that adequate resources for consultation<br />
and access to nursing experts are available to all levels<br />
of nurses in the organization. Whenever the need<br />
for this resource arises, filling that need is discussed<br />
at various council meetings with the stakeholders<br />
involved. The discussion also includes identification<br />
and availability of the individual who is best suited<br />
for the task required. The clinical resource nurses<br />
and clinical educators are an asset to Johnson City<br />
Medical Center. Nurses in this capacity work various<br />
shifts, helping with classroom instruction as well<br />
as bedside demonstration, providing guidance and<br />
support to the front-line nursing team.<br />
National <strong>Nursing</strong> Conference Involvement<br />
Poster abstracts and podium presentations at national<br />
nursing conferences are rewarding both to the nurse<br />
presenting and the conference attendees. Applying<br />
to present a poster or podium presentation is very<br />
competitive. Some national conferences receive up<br />
to 1,600 poster abstract or podium presentation<br />
submissions from nurses all over the country. It<br />
is believed and supported by our nursing leaders<br />
that nurses at all levels grow professionally through<br />
attending local and national conferences. National<br />
conferences serve as meeting places for nurses all<br />
over the country to network, provide support and<br />
guidance, and to experience “like” opportunities for<br />
improvements or celebrations. The following list<br />
includes our nurses who have presented at national<br />
conferences:<br />
14
Lisa Anderson, RN, MSN, CCRN, CCNS, APN<br />
Physical Violence Against Nurses<br />
National Association of Clinical Nurse Specialists<br />
(NACNS)<br />
Portland, Ore.<br />
Beverly Gugliotta, RN, <strong>Nursing</strong> Quality Facilitator<br />
Jeannette Clark, RN, Nurse Manager<br />
Quillen Rehab Hospital<br />
Falls Reduction at Quillen Rehabilitation Hospital<br />
National Database of <strong>Nursing</strong> Quality Indicators<br />
(NDNQI) Conference<br />
New Orleans<br />
Millie Wykoff, RN, Apache Coordinator<br />
Lisa Boghozian, RN, MSN, ICU Clinical Educator<br />
<strong>JCMC</strong> ICU Outcomes<br />
Society for Critical Care Medicine Conference<br />
Miami<br />
Millie Wykoff, RN, Apache Coordinator<br />
<strong>JCMC</strong> ICU Outcomes Data<br />
Cerner Presentation<br />
Kansas City, Mo<br />
Cathy Ivory, RN, MSN, Corporate Director of<br />
Women’s <strong>Health</strong><br />
Presentation: <strong>Health</strong>care IT and Perinatal Safety:<br />
Friends or Foes?<br />
Cerner <strong>Health</strong> Conference Women’s <strong>Health</strong> Track<br />
Kansas City, Mo<br />
Cathy Ivory, RN, MSN, Corporate Director of<br />
Women’s <strong>Health</strong><br />
Presentation: CPOE: Challenges and Opportunities<br />
AWHONN Informatics Breakfast<br />
San Diego<br />
Cathy Ivory, RN, MSN, Corporate Director of<br />
Women’s <strong>Health</strong><br />
Presentation: <strong>Health</strong>care IT and Perinatal Safety:<br />
Friends or Foes?<br />
AWHONN<br />
San Diego<br />
Cathy Ivory, RN, MSN, Corporate Director of<br />
Women’s <strong>Health</strong><br />
Presentation: Technology and Evidence-Based<br />
Practice<br />
FL/GA/AL/TN AWHONN Conference<br />
Atlanta<br />
Patricia Niday, RN, Ed.D.<br />
Presentation: Achieving Clinical Excellence:<br />
Putting Evidence into Practice<br />
Tennessee Hospital Association 2009 <strong>Nursing</strong> and<br />
Quality Leadership Summit<br />
Nashville, Tenn.<br />
Lisa Carter, RN, MSN<br />
Presentation: Retinopathy of Prematurity<br />
Tennessee Hospital Association 2009 <strong>Nursing</strong> and<br />
Quality Leadership Summit<br />
Nashville, Tenn.<br />
15<br />
bringing loving care to health care | www.msha.com
RN-MD Interactions<br />
RN-MD Interactions have been tracked for the past five years through NDNQI. Results continue to<br />
demonstrate high satisfaction with our nurses and physicians. <strong>JCMC</strong> is a teaching hospital for many colleges<br />
that train nurses, physicians, allied healthcare team members and pharmacy students. Students at all levels<br />
of learning form relationships with team members and develop communication skills and interactions that<br />
provide them with positive learning experiences. Nurses have a direct line to the physician during rounds,<br />
communicating and reciprocating needs and concerns regarding patient care. Physicians and nurses need<br />
reliable processes, transparency and effective communication in order to provide the best care to our patients.<br />
Johnson City Medical Center<br />
RN-MD Interactions T-Scores<br />
Autonomy<br />
Autonomy t-scores demonstrated an increase from 2008 to 2009. <strong>Nursing</strong> leadership believes the changes<br />
to the practice, quality and research councils in addition to the stabilization of nursing leadership has had<br />
a positive impact on the autonomy of our nurses. The Shared Governance councils facilitate autonomy by<br />
offering opportunities for direct care, advanced practice, nurse leaders, nurses in non-traditional roles and<br />
other clinical disciplines, to bring forward practice issues into a forum that helps them identify opportunities<br />
and assists in implementation of action plans. The councils also function to facilitate team member education<br />
regarding the importance of small tests of change, Plan-Do-Check-Act Model of Performance Improvement,<br />
use of evidence-based clinical practice and literature search.<br />
Johnson City Medical Center<br />
Autonomy T-Scores<br />
16
Exemplary Professional Practice in Action<br />
Exemplary Professional Practice is the manner<br />
in which our nurses provide Patient-Centered<br />
Care every day (Professional Model of Care). It<br />
embodies the relationships among nursing and other<br />
disciplines. Follow a nurse as she displays Exemplary<br />
Professional Practice:<br />
Katie, Mr. Richards’ nurse for the day, enters his room<br />
with a knock on the door and a smile on her face.<br />
“Hello Mr. Richards, my name is Katie, and I will<br />
be your nurse today.” Katie examines Mr. Richards<br />
and explains what the plan for the day will be. She<br />
tells him that she will be coming in to check on him<br />
approximately every hour, and to ring his call light if<br />
he needs anything before she returns. Before exiting<br />
his room, she asks “How well is your pain managed?”<br />
Mr. Richards does admit that his pain level is a 5.<br />
Katie explains that he has medication available that<br />
will manage his pain and that she will return shortly<br />
with his medication (Autonomy).<br />
Later in the morning, Katie sees Mr. Richards’<br />
physician in the alcove. She approaches to round with<br />
the physician (Interdisciplinary Relationship). When<br />
they enter the room, the physician explains test<br />
results and some new medications that he will order<br />
for Mr. Richards. Katie mentions to the physician<br />
that Mr. Richards is not eating well, and requests<br />
a consult for the dietitian to assist Mr. Richards in<br />
finding a more palatable diet. The physician agrees<br />
and writes the consult (Consultation and Resources).<br />
As midday approaches, the physical therapy assistant<br />
presents on the unit. He has worked with Mr.<br />
Richards to increase the distance Mr. Richards can<br />
ambulate. The physical therapy assistant sees Katie<br />
in the alcove charting and he asks how Mr. Richards<br />
is doing. She tells him that Mr. Richards is up in<br />
the chair and ready to ambulate (Interdisciplinary<br />
Relationship). Katie assists the PTA with ambulating<br />
Mr. Richards in the hallway, and as they return and<br />
assist him into bed, Katie notices some redness to<br />
Mr. Richards’ backside. Katie calls the wound care<br />
nurse to evaluate Mr. Richards’ skin and bed surface<br />
and give input on other interventions that could be<br />
used to prevent further pressure to Mr. Richards’ skin<br />
(Autonomy and Consultation and Resources).<br />
Now that Mr. Richards is settled in his bed, it is<br />
time for Katie to administer his new medications.<br />
She reviews each medication with Mr. Richards as<br />
she scans the barcode in MAK. She explains what<br />
the medications are for and how they will help him<br />
(Nurses as Teachers).<br />
As Katie is finishing her shift, Mr. Richards thanks<br />
her for the care she has provided him today. He tells<br />
her how her care has made a difference and that he<br />
feels he is one step closer to returning to wellness.<br />
As Katie steps back and watches Mr. Richards<br />
enjoy his dinner meal (after some adjustments by<br />
the dietitian), with a manageable pain level (after<br />
administration of his PRN medications during the<br />
day), and with a pressure-relieving bed surface (after<br />
discussion with the wound care nurse), she feels<br />
proud to know the impact her exemplary professional<br />
practice has made on her patient.<br />
The true essence of a Magnet organization stems<br />
from exemplary professional practice within nursing.<br />
This entails a comprehensive understanding of<br />
the role of nursing; the application of that role<br />
with patients, families, communities and the<br />
interdisciplinary team; and the application of new<br />
knowledge and evidence. The goal of this component<br />
is more than the establishment of strong professional<br />
practice; it is what that professional practice can<br />
achieve.<br />
17<br />
bringing loving care to health care | www.msha.com
New Knowledge, Innovation and Improvement<br />
(Forces of Magnetism: Quality of Care: Research and Evidence-Based Practice, Quality Improvement)<br />
Global Issues in <strong>Nursing</strong> and <strong>Health</strong> Care<br />
Structural<br />
Empowerment<br />
Transformational<br />
Leadership<br />
Empirical<br />
Outcomes<br />
Exemplary<br />
Professional<br />
Practice<br />
New Knowledge,<br />
Innovations &<br />
Improvements<br />
Research Conference<br />
In June 2009, the <strong>Nursing</strong> Research Council held its<br />
4th annual research conference. As an annual event,<br />
we have the opportunity to invite researchers from<br />
all disciplines to participate and share their original<br />
research in podium presentations or as posters. Our<br />
presenters come from our own organization, and<br />
as far away as Lexington, Ky. We have also had the<br />
good fortune of hearing Dr. Mona Baharestani,<br />
Ph.D., APN, CWOCN, CWS, noted expert in the<br />
prevention and care of wounds and pressure ulcers,<br />
as our keynote speaker at the 3rd annual conference.<br />
Most of our presentations and posters come from<br />
local nurse researchers from <strong>Mountain</strong> <strong>States</strong> <strong>Health</strong><br />
<strong>Alliance</strong> and other organizations in our region.<br />
Our goal is to not only showcase the research being<br />
conducted in our area, but to also give our local<br />
nursing community the opportunity to network<br />
with nurse researchers. This networking opportunity<br />
encourages collaboration and partnerships to help<br />
generate and use evidence to improve practice and<br />
the quality of care delivered. As we currently plan our<br />
5th annual nursing research conference, we hope to<br />
continue to see the interest and enthusiasm that has<br />
been evident in increasing attendance.<br />
Chest Pain Center/ Emergency Department Nurse Liaison Position<br />
One of the entries for the Quality Awards Banquet<br />
was the submission by Rebecca Pullon, RN, and<br />
Lori Kelley, RN, to improve proper utilization of the<br />
Chest Pain Center while decreasing ED wait times<br />
and limiting unnecessary inpatient admissions for<br />
low-risk cardiac patients. The plan was to implement<br />
a Chest Pain Center/Emergency Department<br />
Nurse Liaison. This nurse would assess, educate and<br />
assist with the evaluation of criteria for inpatient or<br />
observed care.<br />
A 90-day pilot study was implemented with the<br />
CPC/ED Nurse Liaison based in the ED. Improved<br />
ED wait times and reduced inpatient admissions<br />
for low-risk cardiac patients were identified. This<br />
has led to greater patient satisfaction and decreased<br />
healthcare costs to the patient.<br />
18
Falls Prevention Program:<br />
Decision Making by Front-Line Nurses<br />
FALL RISK<br />
Direct-care nurses were asked to use the Hendrich<br />
and Morse fall risk tools on each of their patients for<br />
a two-week period trial in 2008. From their input,<br />
the Morse risk assessment tool was determined to<br />
be most appropriate for our nursing practice. The<br />
Hendrich fall risk assessment tool received a mean<br />
rating of 2.66 out of 4.00 on a Likert scale, while the<br />
Morse tool received a mean score of 3.27.<br />
On July 27, 2009, the new Fall Prevention Program<br />
using the Morse fall risk tool was implemented. This<br />
was a very comprehensive undertaking regarding<br />
the change of policy, forms and practice throughout<br />
MSHA. Using the yellow armband with “Fall<br />
Risk” inscribed on the band was adopted by our<br />
organization as the method of identifying patients at<br />
high risk for falls.<br />
Nationally recognized as the color for high fall<br />
risk patients, the yellow armband is just one of<br />
the colored armbands that identify patients with<br />
special needs. The adoption of a uniform colorcoded<br />
armband system by MSHA in July 2009<br />
presents a clearly defined practice for identifying and<br />
communicating patient risk factors, or special needs,<br />
by standardizing the use of color-coded armbands<br />
to support safe patient care based upon the patient’s<br />
assessed needs and wishes.<br />
JOHNSON CITY MEDICAL CENTER<br />
PATIENT FALL RATES<br />
Rate = falls per patient days x 1000<br />
4.00<br />
3.50<br />
3.00<br />
2.50<br />
2.00<br />
2010<br />
1.50<br />
2009<br />
1.00<br />
2008<br />
0.50<br />
0.00<br />
JAN FEB MAR APR MAY JUN JUL<br />
AUG SEP<br />
OCT<br />
NOV<br />
DEC<br />
New Fall Program<br />
started July 27, 2009<br />
2008<br />
2009<br />
2010<br />
JAN FEB MAR APR MAY JUN JUL AUG SEP OCT NOV DEC<br />
2010 3.59 3.16<br />
2009 3.37 3.00 2.48 3.04 3.29 2.85 3.55 1.98 3.79 2.89 3.75 2.74<br />
2008 3.30 2.44 2.02 1.59 2.23 2.46 3.39 1.89 2.57 2.60 2.31 3.27<br />
Aquapheresis<br />
A new treatment for congestive heart failure<br />
was made available to our patient population in<br />
2009. Aquapheresis, a pump that filters blood and<br />
removes only water and sodium, was purchased in<br />
2009 with the first utilization starting in August<br />
2009. Congestive heart failure patients are able to<br />
get out of bed during this therapy, which is much<br />
more comfortable for them. Most patients receive<br />
the treatment for 3 days, with most seeing a drastic<br />
weight loss between 15 and 30 pounds in 3 days.<br />
Patients have been able remove their bipap apparatus<br />
or oxygen therapy after the aquapheresis treatment.<br />
Swelling is dramatically decreased in all areas so<br />
patients who have had severe pain secondary to<br />
swelling are able to mobilize more freely.<br />
19<br />
bringing loving care to health care | www.msha.com
Quality Awards 2009<br />
Individual Award Winner: Katie Rice, RNC<br />
Holding the Gains: Operational Effectiveness<br />
After implementation of Centricity Perinatal (CPN),<br />
missed charges were dramatically reduced and charges<br />
generated by CPN were found to be consistently<br />
correct when nursing documentation was correct and<br />
complete. Nurses in the Center for Women’s <strong>Health</strong><br />
continually monitored for correct capture of patient<br />
charges. The nurse caring for the patient must verify<br />
and sign the electronically generated charge form prior<br />
to submitting it, and as a double-check the clerical<br />
associate who entered charges notified the CPN<br />
system administrator if anything seemed unusual. In<br />
addition, a review of all available charts for a 5-week<br />
period was conducted 2.5 years after implementation<br />
of CPN charge capture to verify that gains were indeed<br />
being held as well as we perceived. Over the past two<br />
years, CPN has correctly captured 100% of patient<br />
charges when nursing documentation is correct and<br />
complete, and nursing staff is consistently reviewing<br />
charges and ensuring accuracy before submission of<br />
charges. This method of charge capture, which started<br />
with the Obstetrics unit at <strong>JCMC</strong>, has been expanded<br />
to the OB units at JCSH, SSH and IPMC.<br />
Team Award Winner: Lisa Carter, MSN, RN, Nurse<br />
Manager of PICU<br />
Renee’ Lowe, RN, Nurse Manager of NICU<br />
Jill Naylor, RN, Assistant Clinical Leader of NICU<br />
Dr. William Devoe, MD, Neonatologist<br />
Retinopathy of prematurity is a condition affecting<br />
premature infants in which blood vessels in the eye<br />
begin to grow abnormally. In 2006, the overall NICU<br />
rate was found to be 75%. We have since decreased<br />
this rate to 24%, and the rate for severe ROP dropped<br />
from 14.3% to 2%. To ensure continued success with<br />
the ROP protocol, specific elements are monitored<br />
monthly by nursing and respiratory staff. The<br />
results from these monitors show that the staff have<br />
consistently maintained compliance rates at 94% or<br />
greater with following the ROP protocol. We have<br />
continued to see drastic reductions in the number of<br />
infants diagnosed with severe ROP (stage 3 or greater),<br />
and have continued to see fewer infants requiring<br />
surgical interventions. Only two infants have needed<br />
treatment in the last 12 months. The rate for severe<br />
ROP has dropped from our initial rate of 14.3% to 2%,<br />
which is well below the national average. The rates for<br />
any stage of ROP have dropped from 75% to 24%.<br />
20
Empirical Quality Outcomes<br />
(Forces of Magnetism: Quality of Care)<br />
Global Issues in <strong>Nursing</strong> and <strong>Health</strong> Care<br />
Structural<br />
Empowerment<br />
Transformational<br />
Leadership<br />
Empirical<br />
Outcomes<br />
New Knowledge,<br />
Innovations &<br />
Improvements<br />
Exemplary<br />
Professional<br />
Practice<br />
<strong>Nursing</strong> Excellence: Empirical Outcomes<br />
During our celebration of nursing excellence<br />
and Magnet redesignation, we discussed the<br />
components of the new Magnet nursing excellence<br />
model. Empirical outcomes are a common thread<br />
throughout the Magnet model for nursing excellence.<br />
These outcomes are the identified endpoints for each<br />
aspect of the model using measurable quantitative<br />
data, as well as qualitative data. They are based on<br />
using existing evidence as well as generating that<br />
evidence. We discussed two models for using the<br />
evidence and one model for generating the evidence.<br />
We were reminded that research occurs in all practice<br />
arenas including administration, clinical, education<br />
and research. We must evaluate the evidence<br />
and its impact on healthcare resources, patient/<br />
participant preferences and actions, level of evidence,<br />
and settings and circumstances. Clinical or area<br />
expertise is needed to integrate all the information to<br />
determine if the evidence fits our environment.<br />
When evidence is generated, practice, theory and<br />
education are part of a continuous cycle to support<br />
our practice and contribute to nursing’s body of<br />
knowledge. There are internal and external factors<br />
that affect how evidence is used, and both research<br />
and non-research evidence should be included. Using<br />
the evidence or generating the evidence both will<br />
lead to quality outcomes in all areas of practice. This<br />
will result in improved quality and a continuation of<br />
nursing excellence at Johnson City Medical Center.<br />
21<br />
bringing loving care to health care | www.msha.com
MSHA receives TNCPE Excellence Award for second time<br />
<strong>Mountain</strong> <strong>States</strong> <strong>Health</strong> <strong>Alliance</strong> was formally<br />
recognized as the recipient of the 2009 Excellence<br />
Award at the <strong>Annual</strong> Conference of the Tennessee<br />
Center for Performance Excellence (TNCPE) in<br />
Nashville, Tenn. MSHA previously received this<br />
recognition in 2005, thus making MSHA the only<br />
healthcare organization in Tennessee to receive this<br />
recognition twice.<br />
“A large number of our leadership attended the<br />
events of the conference, which featured past<br />
Baldrige National Quality Award recipient speakers,<br />
as well as several of our team who have been involved<br />
in helping lead MSHA’s quality journey,” said MSHA<br />
President and CEO Dennis Vonderfecht.<br />
Vonderfecht and MSHA Vice President of Quality<br />
Tamera Fields both presented at the conference,<br />
sharing the healthcare system’s model for quality<br />
delivery of health care and its performance<br />
improvement process.<br />
2009<br />
Excellence Award<br />
22
Niswonger Children’s Hospital Opening<br />
The dream has finally become a reality. After<br />
nearly five years of fundraising, community support<br />
and steady construction, Niswonger Children’s<br />
Hospital opened March 3, 2009. The $36 million,<br />
69-bed hospital for children admitted patients<br />
approximately one year ago.<br />
“This is truly a great and momentous day for our<br />
region,” said Dennis Vonderfecht, president and<br />
CEO of MSHA. “With the opening of Niswonger<br />
Children’s Hospital and its associated Children’s<br />
Emergency Department, the Tri-Cities joins the<br />
other four metropolitan areas of Tennessee in<br />
having a full-service children’s hospital.” Niswonger<br />
Children’s Hospital is named after lead donors Scott<br />
and Nikki Niswonger of Greeneville, Tenn., who<br />
gave $10 million toward the construction.<br />
Using natural light to provide feelings of comfort<br />
and healing, the main entrance lobby and threestory<br />
glass atrium-lined hallways provide bountiful<br />
light. The stained glass kite gallery suspended from<br />
the ceiling provides a calming environment to the<br />
patients and families. Direct care nurses’ feedback<br />
was crucial to the design and work flow of the patient<br />
care provision areas in the new Niswonger Children’s<br />
Hospital for efficient delivery of patient care. Directcare<br />
nursing team members were involved in all of<br />
the renovation and refurbishment projects for the<br />
patient care units. Women’s and Children’s nursing<br />
team members participated on multiple teams in the<br />
design of the new Niswonger Children’s Hospital.<br />
23<br />
bringing loving care to health care | www.msha.com
Years of Service<br />
Donna Ledbetter<br />
Donna Ledbetter, RN, ONC,<br />
director of the Ortho/Neuro/<br />
Trauma SSU, is very dedicated<br />
to the development and<br />
advancement of the nursing<br />
profession. As a team member<br />
of MSHA for 40 years,<br />
Donna’s devotion to Patient-<br />
Centered Care is well-known by all team members at<br />
<strong>JCMC</strong>. She is a nurse with high integrity, regarded<br />
by her peers as kind and accessible, and a strong<br />
patient and nursing advocate. She exudes grace and<br />
a soft-spoken manner in which her experienced<br />
voice is heard and respected. Donna is a member of<br />
the American Association of Critical Care Nurses<br />
and the Advisory Council for the Surgical Tech and<br />
Cardiovascular Technician Program at Northeast<br />
State Technical Community College. She is a<br />
member of the American College of <strong>Health</strong>care<br />
Executives and an American Heart Association<br />
Board Member. She was certified as an orthopedic<br />
nurse in 2007, and is a member of the National<br />
Association of Orthopaedic Nurses (NAON). Other<br />
memberships include the North East Tennessee<br />
Organization of Nurse Executives (NETONE),<br />
TONE, Tennessee Hospital Association (THA)<br />
and Tennessee Nurses Association. She received the<br />
Nurse of Distinction Clinical Award from TNA<br />
in 2005. Donna’s knowledge, devotion to Patient-<br />
Centered Care and advocacy to the profession of<br />
nursing truly exemplify The MSHA Difference.<br />
30 Plus Years of Service<br />
Linda Allen<br />
Lana Renfro<br />
Brenda Campbell<br />
Delores “Ann” Wilson<br />
Mitchell Hathaway<br />
Martha K. Smith<br />
Pat Looney<br />
Mary Farrington<br />
Karen Adkins<br />
Connie Hatcher<br />
Vickie Torbett<br />
Pamela Kubisiak<br />
Uta Lewey<br />
Richard Blevins<br />
Carolyn “Charlie” Wishon<br />
Harriet Fitzgerald<br />
40 years<br />
38 years<br />
38 years<br />
38 years<br />
37 years<br />
36 years<br />
36 years<br />
35 years<br />
35 years<br />
35 years<br />
34 years<br />
34 years<br />
34 years<br />
34 years<br />
34 years<br />
34 years<br />
Cassandra Moore<br />
Mary “Peep” Adams<br />
Teresa Bailey<br />
Connie Jessee<br />
Ernestine Hatcher<br />
Patrick Kiernan<br />
Treva Williams<br />
Sharon Johnson<br />
Donna Rice<br />
Wilmetta Collie<br />
Sharon Jarrett<br />
Amy Belcher<br />
Victoria Privette<br />
Loreta “Sue” Clark<br />
Beverly Gugliotta<br />
33 years<br />
33 years<br />
33 years<br />
32 years<br />
32 years<br />
32 years<br />
32 years<br />
32 years<br />
32 years<br />
31 years<br />
31 years<br />
30 years<br />
30 years<br />
30 years<br />
30 years<br />
24
Georgita Washington<br />
On Dec. 19, 2009, Georgita<br />
Tolbert Washington, Ph.D.,<br />
RN-BC, MSN, CCRN,<br />
received her doctor of<br />
philosophy in nursing<br />
from East Tennessee State<br />
University in Johnson City,<br />
Tenn. A native of Charleston,<br />
S.C., she received her bachelor of science in nursing<br />
from Clemson University and her master of science<br />
in nursing from the Medical University of South<br />
Carolina.<br />
Dr. Washington’s dissertation research, titled,<br />
“Effects of Anxiety-Reducing Interventions on<br />
Performance Anxiety in Graduate Nurses,” was<br />
conducted to determine the best methods of<br />
reducing anxiety in those newly graduated from<br />
nursing school. This would hopefully facilitate<br />
their transition from student to professional nurse,<br />
helping to contribute to strategies to ease the nursing<br />
shortage. She plans on further research in this<br />
area to facilitate the retention of new nurses to the<br />
profession and to <strong>Mountain</strong> <strong>States</strong> <strong>Health</strong> <strong>Alliance</strong>.<br />
Georgita is a 10-year team member at <strong>Mountain</strong><br />
<strong>States</strong> <strong>Health</strong> <strong>Alliance</strong> and is currently the director of<br />
nursing education for Johnson City Medical Center.<br />
She has a clinical background of 26 years in critical<br />
care nursing, with 18 as a critical care clinical nurse<br />
specialist. Her role at MSHA also includes chair of<br />
the nursing research council, which is very active in<br />
mentoring new researchers.<br />
25<br />
bringing loving care to health care | www.msha.com
N u m b e r o f H o s p ita l A c q u ire d P re s s u re U lc e rs<br />
30<br />
20<br />
10<br />
0<br />
3Q<br />
08<br />
4Q<br />
08<br />
1Q<br />
09<br />
2Q<br />
09<br />
3Q<br />
09<br />
4Q<br />
09<br />
1Q<br />
10<br />
Stage I 7 21 13 6 6 12 3<br />
Stage II 20 18 16 18 11 5 14<br />
Stage III 10 2 0 3 0 1 0<br />
Stage IV 1 0 0 0 0 0 0<br />
2Q<br />
10<br />
3Q<br />
10<br />
Stage I<br />
Stage II<br />
Stage III<br />
Stage IV<br />
DTI<br />
Unstageable<br />
Indeterminate<br />
The prevention of hospital-acquired pressure ulcers<br />
is a constant priority at <strong>JCMC</strong>. The skin care team<br />
and wound care nurses are available to assist bedside<br />
nurses with treatments, education and appropriate<br />
selection of wound care dressings and specialty<br />
beds. Quarterly pressure ulcer prevalence surveys are<br />
Pressure Ulcers<br />
conducted by a group of nurses educated in pressure<br />
ulcer assessment with validation from the wound<br />
care experts. Tracking of in-house specialty beds has<br />
been enhanced over the past year to determine the<br />
right bed for the right patient at the right time for<br />
prevention and treatment of pressure ulcers.<br />
Turnover<br />
26
Percentage of Non-ICU Code Blue Occurence 2009<br />
45<br />
40<br />
35<br />
30<br />
25<br />
Percentage<br />
20<br />
Actual<br />
Target<br />
15<br />
10<br />
5<br />
0<br />
Jan Feb March April May June July Aug Sept Oct Nov Dec<br />
January - December<br />
Rapid Response Team<br />
One of our quality care initiatives, started in 2005<br />
and continuing today, was the development of the<br />
Rapid Response Team. Opportunities were identified<br />
to bring critical care expertise, RNs and respiratory<br />
therapists to the bedside of patients whose condition<br />
was deteriorating or uncertain. There is a large<br />
amount of variability in both quality of care and the<br />
safety of patients in health care today. This variability<br />
is evident in hospital mortality rates. There are<br />
three main systemic issues that contribute to the<br />
problem such as failures in planning (assessment,<br />
treatments, goals), failure to communicate (patient<br />
to staff, staff to staff, staff to physician), and failure<br />
to recognize deteriorating patient condition. These<br />
fundamental problems can often lead to a failure<br />
to rescue. Establishing rapid response teams stands<br />
to impact this problem by identifying unstable<br />
patients and those patients likely to suffer cardiac or<br />
respiratory arrest. If identified in a timely fashion,<br />
their unnecessary deaths can often be prevented.<br />
Successful<br />
Joint Commission Survey at<br />
<strong>JCMC</strong>/QRH/Woodridge !!!<br />
27<br />
bringing loving care to health care | www.msha.com
Patient -Centered Care<br />
10 Guiding Principles<br />
Care is based on continuous healing relationships.<br />
The patient is the source of control for their care.<br />
Care is customized and reflects patient needs, values and choices.<br />
Families and friends of the patient are considered an essential part of the care team.<br />
All Team Members are considered as caregivers.<br />
Care is provided in a healing environment of comfort, peace and support.<br />
Knowledge and information are shared freely between and among patients, care<br />
partners, physicians and other caregivers.<br />
Transparency is the rule in the care of the patient.<br />
Patient safety is a visible priority.<br />
All caregivers cooperate with one another through a common focus on the best interest<br />
and personal goals of the patient.<br />
400 N. State of Franklin Road<br />
Johnson City, TN 37604<br />
bringing loving care to health care | www.msha.com