View PDF Edition - U.S. Pharmacist
View PDF Edition - U.S. Pharmacist
View PDF Edition - U.S. Pharmacist
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
BRIEF SUMMARY OF FULL PRESCRIBING INFORMATION for<br />
ULORIC ® (febuxostat) tablets<br />
INDICATIONS AND USAGE<br />
ULORIC ® is a xanthine oxidase (XO) inhibitor indicated for the chronic management<br />
of hyperuricemia in patients with gout.<br />
ULORIC is not recommended for the treatment of asymptomatic hyperuricemia.<br />
CONTRAINDICATIONS<br />
ULORIC is contraindicated in patients being treated with azathioprine, mercaptopurine,<br />
or theophylline [see Drug Interactions].<br />
WARNINGS AND PRECAUTIONS<br />
Gout Flare<br />
After initiation of ULORIC, an increase in gout flares is frequently observed. This<br />
increase is due to reduction in serum uric acid levels resulting in mobilization of<br />
urate from tissue deposits.<br />
In order to prevent gout flares when ULORIC is initiated, concurrent prophylactic<br />
treatment with an NSAID or colchicine is recommended.<br />
Cardiovascular Events<br />
In the randomized controlled studies, there was a higher rate of cardiovascular<br />
thrombo embolic events (cardiovascular deaths, non-fatal myocardial infarctions,<br />
and non-fatal strokes) in patients treated with ULORIC [0.74 per 100 P-Y<br />
(95% CI 0.36-1.37)] than allopurinol [0.60 per 100 P-Y (95% CI 0.16-1.53)] [see<br />
Adverse Reactions]. A causal relationship with ULORIC has not been established.<br />
Monitor for signs and symptoms of myocardial infarction (MI) and stroke.<br />
Liver Enzyme Elevations<br />
During randomized controlled studies, transaminase elevations greater than 3 times<br />
the upper limit of normal (ULN) were observed (AST: 2%, 2%, and ALT: 3%, 2%<br />
in ULORIC and allopurinol-treated patients, respectively). No dose-effect<br />
relationship for these transaminase elevations was noted. Laboratory<br />
assessment of liver function is recommended at, for example, 2 and 4 months<br />
following initiation of ULORIC and periodically thereafter.<br />
ADVERSE REACTIONS<br />
Clinical Trials Experience<br />
Because clinical trials are conducted under widely varying conditions, adverse<br />
reaction rates observed in the clinical trials of a drug cannot be directly compared<br />
to rates in the clinical trials of another drug and may not reflect the rates observed<br />
in practice.<br />
A total of 2757 subjects with hyperuricemia and gout were treated with ULORIC<br />
40 mg or 80 mg daily in clinical studies. For ULORIC 40 mg, 559 patients<br />
were treated for 6 months. For ULORIC 80 mg, 1377 subjects were treated for<br />
6 months, 674 patients were treated for 1 year and 515 patients were treated<br />
for 2 years.<br />
Most Common Adverse Reactions<br />
In three randomized, controlled clinical studies (Studies 1, 2 and 3), which were<br />
6 to 12 months in duration, the following adverse reactions were reported by<br />
the treating physician as related to study drug. Table 1 summarizes adverse<br />
reactions reported at a rate of at least 1% in ULORIC treatment groups and at<br />
least 0.5% greater than placebo.<br />
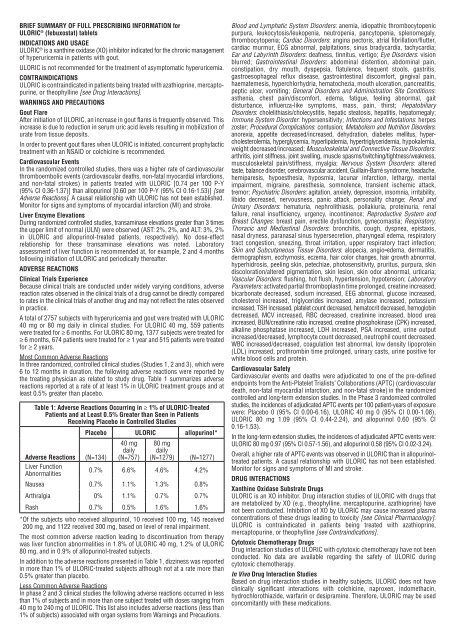
Table 1: Adverse Reactions Occurring in 1% of ULORIC-Treated<br />
Patients and at Least 0.5% Greater than Seen in Patients<br />
Receiving Placebo in Controlled Studies<br />
Placebo ULORIC allopurinol*<br />
40 mg 80 mg<br />
daily daily<br />
Adverse Reactions (N=134) (N=757) (N=1279) (N=1277)<br />
Liver Function<br />
Abnormalities<br />
0.7% 6.6% 4.6% 4.2%<br />
Nausea 0.7% 1.1% 1.3% 0.8%<br />
Arthralgia 0% 1.1% 0.7% 0.7%<br />
Rash 0.7% 0.5% 1.6% 1.6%<br />
* Of the subjects who received allopurinol, 10 received 100 mg, 145 received<br />
200 mg, and 1122 received 300 mg, based on level of renal impairment.<br />
The most common adverse reaction leading to discontinuation from therapy<br />
was liver function abnormalities in 1.8% of ULORIC 40 mg, 1.2% of ULORIC<br />
80 mg, and in 0.9% of allopurinol-treated subjects.<br />
In addition to the adverse reactions presented in Table 1, dizziness was reported<br />
in more than 1% of ULORIC-treated subjects although not at a rate more than<br />
0.5% greater than placebo.<br />
Less Common Adverse Reactions<br />
In phase 2 and 3 clinical studies the following adverse reactions occurred in less<br />
than 1% of subjects and in more than one subject treated with doses ranging from<br />
40 mg to 240 mg of ULORIC. This list also includes adverse reactions (less than<br />
1% of subjects) associated with organ systems from Warnings and Precautions.<br />
Blood and Lymphatic System Disorders: anemia, idiopathic thrombocytopenic<br />
purpura, leukocytosis/leukopenia, neutropenia, pancytopenia, splenomegaly,<br />
throm bo cytopenia; Cardiac Disorders: angina pectoris, atrial fibrillation/flutter,<br />
cardiac murmur, ECG abnormal, palpitations, sinus bradycardia, tachycardia;<br />
Ear and Labyrinth Disorders: deafness, tinnitus, vertigo; Eye Disorders: vision<br />
blurred; Gastrointestinal Disorders: abdominal distention, abdominal pain,<br />
constipation, dry mouth, dyspepsia, flatulence, frequent stools, gastritis,<br />
gastro esophageal reflux disease, gastrointestinal discomfort, gingival pain,<br />
haematemesis, hyperchlorhydria, hematochezia, mouth ulceration, pancreatitis,<br />
peptic ulcer, vomiting; General Disorders and Administration Site Conditions:<br />
asthenia, chest pain/discomfort, edema, fatigue, feeling abnormal, gait<br />
disturbance, influenza-like symptoms, mass, pain, thirst; Hepatobiliary<br />
Disorders: cholelithiasis/cholecystitis, hepatic steatosis, hepatitis, hepatomegaly;<br />
Immune System Disorder: hypersensitivity; Infections and Infestations: herpes<br />
zoster; Procedural Complications: contusion; Metabolism and Nutrition Disorders:<br />
anorexia, appetite decreased/increased, dehydration, diabetes mellitus, hypercholesterolemia,<br />
hyperglycemia, hyperlipidemia, hypertriglyceridemia, hypokalemia,<br />
weight decreased/increased; Musculoskeletal and Connective Tissue Disorders:<br />
arthritis, joint stiffness, joint swelling, muscle spasms/twitching/tightness/weakness,<br />
musculoskeletal pain/stiffness, myalgia; Nervous System Disorders: altered<br />
taste, balance disorder, cerebrovascular accident, Guillain-Barré syndrome, headache,<br />
hemiparesis, hypoesthesia, hyposmia, lacunar infarction, lethargy, mental<br />
impairment, migraine, paresthesia, somnolence, transient ischemic attack,<br />
tremor; Psychiatric Disorders: agitation, anxiety, depression, insomnia, irritability,<br />
libido decreased, nervousness, panic attack, personality change; Renal and<br />
Urinary Disorders: hematuria, nephrolithiasis, pollakiuria, proteinuria, renal<br />
failure, renal insufficiency, urgency, incontinence; Reproductive System and<br />
Breast Changes: breast pain, erectile dysfunction, gynecomastia; Respiratory,<br />
Thoracic and Mediastinal Disorders: bronchitis, cough, dyspnea, epistaxis,<br />
nasal dryness, paranasal sinus hypersecretion, pharyngeal edema, respiratory<br />
tract congestion, sneezing, throat irritation, upper respiratory tract infection;<br />
Skin and Subcutaneous Tissue Disorders: alopecia, angio edema, dermatitis,<br />
dermographism, ecchymosis, eczema, hair color changes, hair growth abnormal,<br />
hyperhidrosis, peeling skin, petechiae, photosensitivity, pruritus, purpura, skin<br />
discoloration/altered pigmentation, skin lesion, skin odor abnormal, urticaria;<br />
Vascular Disorders: flushing, hot flush, hypertension, hypotension; Laboratory<br />
Parameters: activated partial thromboplastin time prolonged, creatine increased,<br />
bicarbonate decreased, sodium increased, EEG abnormal, glucose increased,<br />
cholesterol increased, triglycerides increased, amylase increased, potassium<br />
increased, TSH increased, platelet count decreased, hematocrit decreased, hemoglobin<br />
decreased, MCV increased, RBC decreased, creatinine increased, blood urea<br />
increased, BUN/creatinine ratio increased, creatine phosphokinase (CPK) increased,<br />
alkaline phosphatase increased, LDH increased, PSA increased, urine output<br />
increased/decreased, lymphocyte count decreased, neutrophil count decreased,<br />
WBC increased/decreased, coagulation test abnormal, low density lipoprotein<br />
(LDL) increased, prothrombin time prolonged, urinary casts, urine positive for<br />
white blood cells and protein.<br />
Cardiovascular Safety<br />
Cardiovascular events and deaths were adjudicated to one of the pre-defined<br />
endpoints from the Anti-Platelet Trialists’ Collaborations (APTC) (cardiovascular<br />
death, non-fatal myocardial infarction, and non-fatal stroke) in the randomized<br />
controlled and long-term extension studies. In the Phase 3 randomized controlled<br />
studies, the incidences of adjudicated APTC events per 100 patient-years of exposure<br />
were: Placebo 0 (95% CI 0.00-6.16), ULORIC 40 mg 0 (95% CI 0.00-1.08),<br />
ULORIC 80 mg 1.09 (95% CI 0.44-2.24), and allopurinol 0.60 (95% CI<br />
0.16-1.53).<br />
In the long-term extension studies, the incidences of adjudicated APTC events were:<br />
ULORIC 80 mg 0.97 (95% CI 0.57-1.56), and allopurinol 0.58 (95% CI 0.02-3.24).<br />
Overall, a higher rate of APTC events was observed in ULORIC than in allopurinoltreated<br />
patients. A causal relationship with ULORIC has not been established.<br />
Monitor for signs and symptoms of MI and stroke.<br />
DRUG INTERACTIONS<br />
Xanthine Oxidase Substrate Drugs<br />
ULORIC is an XO inhibitor. Drug interaction studies of ULORIC with drugs that<br />
are metabolized by XO (e.g., theophylline, mercaptopurine, azathioprine) have<br />
not been conducted. Inhibition of XO by ULORIC may cause increased plasma<br />
concentrations of these drugs leading to toxicity [see Clinical Pharmacology].<br />
ULORIC is contraindicated in patients being treated with azathioprine,<br />
mercaptopurine, or theophylline [see Contraindications].<br />
Cytotoxic Chemotherapy Drugs<br />
Drug interaction studies of ULORIC with cytotoxic chemotherapy have not been<br />
conducted. No data are available regarding the safety of ULORIC during<br />
cytotoxic chemotherapy.<br />
In Vivo Drug Interaction Studies<br />
Based on drug interaction studies in healthy subjects, ULORIC does not have<br />
clinically significant interactions with colchicine, naproxen, indomethacin,<br />
hydrochlorothiazide, warfarin or desipramine. Therefore, ULORIC may be used<br />
concomitantly with these medications.