Diabetes in pregnancy: are we providing the best care ... - HQIP
Diabetes in pregnancy: are we providing the best care ... - HQIP
Diabetes in pregnancy: are we providing the best care ... - HQIP
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
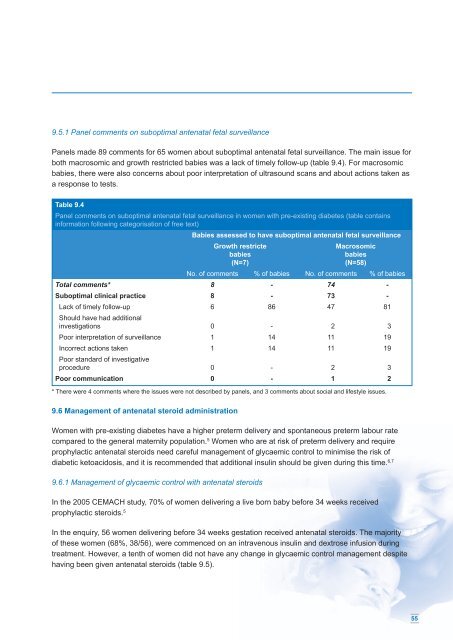
9.5.1 Panel comments on suboptimal antenatal fetal surveillance<br />
Panels made 89 comments for 65 women about suboptimal antenatal fetal surveillance. The ma<strong>in</strong> issue for<br />
both macrosomic and growth restricted babies was a lack of timely follow-up (table 9.4). For macrosomic<br />
babies, <strong>the</strong>re <strong>we</strong>re also concerns about poor <strong>in</strong>terpretation of ultrasound scans and about actions taken as<br />
a response to tests.<br />
Table 9.4<br />
Panel comments on suboptimal antenatal fetal surveillance <strong>in</strong> women with pre-exist<strong>in</strong>g diabetes (table conta<strong>in</strong>s<br />
<strong>in</strong>formation follow<strong>in</strong>g categorisation of free text)<br />
Babies assessed to have suboptimal antenatal fetal surveillance<br />
Growth restricte<br />
babies<br />
(N=7)<br />
Macrosomic<br />
babies<br />
(N=58)<br />
No. of comments % of babies No. of comments % of babies<br />
Total comments* 8 - 74 -<br />
Suboptimal cl<strong>in</strong>ical practice 8 - 73 -<br />
Lack of timely follow-up 6 86 47 81<br />
Should have had additional<br />
<strong>in</strong>vestigations 0 - 2 3<br />
Poor <strong>in</strong>terpretation of surveillance 1 14 11 19<br />
Incorrect actions taken 1 14 11 19<br />
Poor standard of <strong>in</strong>vestigative<br />
procedure 0 - 2 3<br />
Poor communication 0 - 1 2<br />
* There <strong>we</strong>re 4 comments where <strong>the</strong> issues <strong>we</strong>re not described by panels, and 3 comments about social and lifestyle issues.<br />
9.6 Management of antenatal steroid adm<strong>in</strong>istration<br />
Women with pre-exist<strong>in</strong>g diabetes have a higher preterm delivery and spontaneous preterm labour rate<br />
comp<strong>are</strong>d to <strong>the</strong> general maternity population. 5 Women who <strong>are</strong> at risk of preterm delivery and require<br />
prophylactic antenatal steroids need c<strong>are</strong>ful management of glycaemic control to m<strong>in</strong>imise <strong>the</strong> risk of<br />
diabetic ketoacidosis, and it is recommended that additional <strong>in</strong>sul<strong>in</strong> should be given dur<strong>in</strong>g this time. 6,7<br />
9.6.1 Management of glycaemic control with antenatal steroids<br />
In <strong>the</strong> 2005 CEMACH study, 70% of women deliver<strong>in</strong>g a live born baby before 34 <strong>we</strong>eks received<br />
prophylactic steroids. 5<br />
In <strong>the</strong> enquiry, 56 women deliver<strong>in</strong>g before 34 <strong>we</strong>eks gestation received antenatal steroids. The majority<br />
of <strong>the</strong>se women (68%, 38/56), <strong>we</strong>re commenced on an <strong>in</strong>travenous <strong>in</strong>sul<strong>in</strong> and dextrose <strong>in</strong>fusion dur<strong>in</strong>g<br />
treatment. Ho<strong>we</strong>ver, a tenth of women did not have any change <strong>in</strong> glycaemic control management despite<br />
hav<strong>in</strong>g been given antenatal steroids (table 9.5).<br />
55