Hip Replacement Patient Notebook - Christiana Care Health System
Hip Replacement Patient Notebook - Christiana Care Health System
Hip Replacement Patient Notebook - Christiana Care Health System
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Notebook</strong> for <strong>Hip</strong>s
<strong>Notebook</strong> for <strong>Hip</strong>s<br />
<strong>Christiana</strong> <strong>Care</strong><br />
Center for Advanced Joint<br />
<strong>Replacement</strong><br />
Your surgery date: __________________________________________________________________<br />
Return to your orthopedic physician for your final pre-operative check up on:<br />
_______________________________________________________________ at ________________ .<br />
Please Bring This Book With You To:<br />
■ Every office visit.<br />
■<br />
■<br />
■<br />
■<br />
Your physical therapy evaluation before surgery.<br />
Your hospital joint replacement information class.<br />
The hospital on admission.<br />
All physical therapy visits after hospital discharge.
Welcome<br />
Thank you for choosing the Center for Advanced Joint <strong>Replacement</strong> to help bring back a<br />
higher quality of living to your life with a new joint. We were recognized as a Magnet<br />
facility in 2010 and the Joint Commission recognized our program in 2011 with the<br />
designation of “Disease Specific Certification”. We are very proud of these awards that<br />
show we are meeting our pledge to you to give the best care possible.<br />
We are patient and family centered, during your stay we work as a team to meet your<br />
needs. We will also include your family or whomever you tell us is important to be there<br />
to support you if you wish.<br />
Every year, more than 700,000 people have total joint replacement surgery in our country.<br />
Total knee replacement patients usually recover quickly. Most patients are out of bed and<br />
walking the same day as their surgery. Generally, you may return to driving in two to<br />
four weeks, dance in four to six weeks and golf in six to twelve weeks. However, your<br />
rate of recovery will depend on what your activity was before surgery, everyone is<br />
different.<br />
We have a planned course for your care. We believe that you play a key role to a<br />
successful recovery. We will involve you through each step. This patient guide will give<br />
you the necessary information needed for a safe and successful recovery.<br />
Your health care team will include:<br />
■ YOU!<br />
■ Your family<br />
■ Doctors<br />
■ Doctor assistants<br />
■ Nurses<br />
■ <strong>Patient</strong> care technician<br />
■ Physical therapists<br />
■ Occupational therapists<br />
Every part, from before surgery (pre-operative) teaching to after surgery (post-operative)<br />
exercises, will be reviewed with you. Together we will plan your treatment program and<br />
guide you through it.<br />
The Purpose of the <strong>Notebook</strong><br />
For the best results preparation, education, and a pre-planning what will happen when<br />
you go home (discharge) is needed. Communication is important; this notebook is a tool<br />
for you to review with your doctors, physical therapists, occupational therapists, and<br />
nurses. It will help you know:<br />
■ What to expect every step of the way.<br />
■ What you need to do.<br />
■ How to care for your new joint for life.<br />
Remember this is just a guide. Your doctor, nurse or therapist may add to or change any<br />
of the recommendations. Always use their recommendations first and ask questions if<br />
you are unsure. Keep your notebook handy for at least the first year after your surgery.<br />
Take your <strong>Notebook</strong> with you to the hospital, rehab/subacute facility, outpatient physical<br />
therapy and all your doctor visits.<br />
Take your <strong>Notebook</strong> with you to the hospital, rehab/subacute facility, outpatient physical<br />
therapy and all physician visits.
Overview of <strong>Christiana</strong><br />
<strong>Care</strong>’s Center for Advanced<br />
Joint <strong>Replacement</strong><br />
The Center for Advanced Joint <strong>Replacement</strong> has dedicated centers located within<br />
<strong>Christiana</strong> and Wilmington Hospitals.<br />
The program includes:<br />
■ A case manager who organizes all preoperative and discharge planning.<br />
■ A pre-operative physical therapy evaluation.<br />
■ A pre-operative education class.<br />
■ Nurses who dedicate themselves to the care of joint replacement patients.<br />
■ Physical therapists who help get you moving again: from getting out of bed to climbing<br />
stairs.<br />
■ Group activities as well as personal care.<br />
■ A special lunch for you and your coach on the second day after your surgery.<br />
■ Occupational therapist to make sure you can care for yourself.<br />
■ Family and friends are encouraged to participate as coaches in your recovery process. We<br />
will teach them how to help you.<br />
■ Organized care when you leave the hospital.
Role of the Center for<br />
Advanced Joint <strong>Replacement</strong><br />
Case Manager<br />
The Center for Advanced Joint <strong>Replacement</strong> case manager will be responsible for your care<br />
needs from the pre-operative course through discharge.<br />
Your case manager will:<br />
■ Take your medical history by phone.<br />
■ Consider your needs at home including someone to help you when you go home and order<br />
any equipment you may need.<br />
■ Help you understand and plan for your special needs: special anesthesia needs or medical<br />
clearance for surgery.<br />
■ Coordinate your hospital care with the other Total Joint Team members.<br />
■ Work with your insurance provider to get answers to insurance questions.<br />
■ Coordinate your plan when you leave : to home with help; to an outpatient physical therapy<br />
facility or to home health services. Consult with a social worker if a rehab/subacute facility is<br />
needed.<br />
■ Act as your contact throughout your treatment.<br />
Shortly after your surgeon’s office has scheduled your surgery you will called by the a case<br />
manager who will:<br />
■<br />
■<br />
■<br />
coordinate your care before surgery between your doctors’ offices, the hospital and any<br />
testing, if needed.<br />
Arrange with you a schedule for both the pre-operative physical therapy evaluation and the<br />
joint replacement class.<br />
Answer questions.<br />
You can reach a case manager :<br />
Monday through Friday between 8 a.m. and 4 p.m.<br />
You may call the case manager at any time to ask questions or concerns about your<br />
surgery. If the case manager is not there, you may leave a message for a return telephone call.<br />
Center for Advanced Joint <strong>Replacement</strong> cas manager<br />
Case manager for Wilmington Hospital patients: 302-428-2460<br />
Case manager for <strong>Christiana</strong> Hospital patients: 302-428-2430<br />
Secretary: 302-428-4377<br />
Fax: 302-428-4644
About Total <strong>Hip</strong> Surgery<br />
and FAQs<br />
We are glad you have chosen the Center for Advanced Joint <strong>Replacement</strong> to care for your<br />
hip problem. Below is a list of the most often asked questions along with their answers. This<br />
notebook gives added information. If your have any other questions, please ask your<br />
surgeon or the Center for Advanced Joint <strong>Replacement</strong> case manager. Our goal is for you to<br />
be fully informed about this procedure.<br />
What is arthritis and why does my hip hurt?<br />
In the hip joint there is a layer of smooth cartilage on the<br />
ball of the upper end of the thigh bone (femur) and<br />
another layer within your hip socket. This cartilage<br />
serves as a cushion and lets smooth motion of your hip.<br />
Arthritis is a wearing away of this cartilage. This wears<br />
down to your bone. Rubbing of bone against bone<br />
causes pain, swelling and stiffness.<br />
What is a total hip replacement?<br />
A total hip replacement is an operation that removes the<br />
ball of the upper thigh bone (femur) as well as harmed<br />
cartilage from your hip socket. The ball is replaced with a<br />
metal ball that is fixed solidly inside the thigh bone.<br />
BEFORE: Raw bone<br />
rubbing on raw bone<br />
AFTER: A new<br />
surface creates a<br />
smooth functioning<br />
joint<br />
The socket is replaced with a plastic liner that is most often fixed inside a metal shell. This<br />
makes a smoothly working joint that does not hurt.<br />
When should I have this type of surgery?<br />
Your orthopedic surgeon will decide if you may have the surgery. This will be based on<br />
your history, exam, X-rays and response to treatment that has been tried to now. Your<br />
surgeon will ask you to decide if your pain, stiffness and inability to do the things you wish<br />
warrant having surgery.<br />
Am I too old for this surgery?<br />
Age is not a problem if you are in reasonable health and have the wish to keep on living a<br />
productive, active life. You will be asked to see your personal doctor for his/her opinion<br />
about your general health before your surgery.
FAQs about<br />
Total <strong>Hip</strong> Surgery<br />
How long will my new hip last and can a second replacement be done?<br />
We expect most hips to last more than 10-15 years. But there is no guarantee and 5-10<br />
percent may not last that long. A second replacement may be needed.<br />
Why do they fail?<br />
The most common reason for failure is loosening of the artificial ball where it is set in the<br />
thigh bone, or loosening of the socket. Wearing of the plastic spacer may also result in the<br />
need for revision.<br />
What are the major r isks?<br />
Most surgeries go well, without any problems. Infection and blood clots are two potential<br />
serious complications. To skirt these problems, we take special precautions in the operating<br />
room to lower the risk of infection and we use antibiotics and blood thinners post<br />
operatively. The chances of these happening in your lifetime are one percent or less. Having<br />
your hip joint fall out of place after surgery is also a potential problem. Your orthopedist<br />
and<br />
PT will talk ways to lower that risk.<br />
Should I exercise before the sur gery?<br />
Yes. You should talk about physical therapy/exercise choices with your surgeon. Exercises<br />
should begin as soon as possible.<br />
Will I need blood?<br />
You may need blood after the surgery. You may:<br />
(1) Donate your own blood, if you can, (ask your doctor his/her choice)<br />
(2) Use the community blood bank supply.<br />
When will I be able to get out of bed?<br />
Your surgeon will ask that you get out of bed the day of your surgery. The next morning<br />
you will get up, sit in a chair or recliner and walk with a walker with help from our staff.<br />
Most patients will get out of bed the day of surgery.<br />
How long will I be in the hospital?<br />
Most patients will be in the hospital for 2-3 days after their surgery. Before your surgery set<br />
up to have someone stay with you for a minimum of 3 days when you go home from the<br />
hospital.<br />
How do I make ar rangements for surgery?<br />
After your surgeon has scheduled your surgery, the Center for Advanced Joint <strong>Replacement</strong><br />
case manager will call and guide you through the program. The role of the case manager is<br />
described in this notebook. The case manager’s phone number is 302-428-2460.
How long does the surgery take?<br />
We say roughly two to two and a-half hours for surgery.<br />
What are my anesthesia options?<br />
You may have a general anesthetic which most people call "being put to sleep." Some patients<br />
have a spinal anesthetic. The choice is between you and the anesthesiologist. For more<br />
information read “Anesthesia” in the FYI section of your notebook.<br />
Will I have pain after surgery?<br />
Yes, but we will keep you comfortable. Generally most patients are able to stop strong<br />
medication within one day. The day of surgery, most patients control their own medicine with<br />
a special pump that delivers medication directly into their IV. Your surgeon will talk with you<br />
what pain control option is best for you. For more information read about <strong>Patient</strong> Controlled<br />
Analgesia (PCA) in the FYI section of your notebook.<br />
Who will be doing the surgery?<br />
Your orthopedic surgeon will do the surgery. A physician's assistant often helps during the<br />
procedure.<br />
How long and where will my scar be?<br />
The scar will be six to eight inches long and found along the side of your hip.<br />
Will I need a walker, crutches or cane?<br />
Yes. Until your muscle strength returns after surgery, you will need a walker, a cane or<br />
crutches. Your needs will be decided by the PT and ordered for you by the Center for<br />
Advanced Joint <strong>Replacement</strong> case manager and delivered to you before you leave the<br />
hospital.<br />
Will I need other supplies?<br />
After hip replacement surgery, you may need a high toilet seat for three months.<br />
You might also think about installing grab bars in your tub or shower and buying a bath seat<br />
for safety. If needed, an OT will teach you how to use adaptive tools to help you with lower<br />
body dressing and bathing.<br />
Where will I go after go home from the hospital from the hospital?<br />
Most patients are sent home and carry on with their PT in an outpatient office. Some will<br />
need in home therapy three times a week for two weeks which will be arranged by the case<br />
manager. Others need a short inpatient stay at an extended care facility. This stay is most often<br />
from three to ten days. Check with your insurance company to understand your rehabilitation<br />
benefits. For more information about the Rehabilitation Services available through <strong>Christiana</strong><br />
<strong>Care</strong>, see the FYI section of your notebook.<br />
Will I need help at home?<br />
Yes. The first several days or weeks you will need someone to help you with making meal,<br />
housekeeping, etc. If you live alone, please set up to have someone in your home around the<br />
clock for at least the first three days when you go home.
How can I get my home ready before my surgery?<br />
Getting ready ahead of time can lessen help needed when you go home for example: having<br />
the laundry done, house cleaned, yard work completed, clean linens on bed, and meals ready.<br />
Evaluate your environment for safety. Consider taking up throw rugs, clearing walkways to<br />
make room for using a walker, and make sure you have enough lighting ready. Check for the<br />
need to add handrails on stairways.<br />
Will I need physical therapy when I go home?<br />
Yes. Physical therapy will continue after you go home with a therapist at an outpatient<br />
physical therapy office or in your home. The length of time needed varies with each patient.<br />
We will help you set this up before you go home. ( A map with the <strong>Christiana</strong> <strong>Care</strong> outpatient<br />
physical therapy facilities is in the FYI section of this notebook.)<br />
How long until I can dr ive and get back to nor mal?<br />
Being able to drive depends on whether surgery was on your right leg or your left leg and the<br />
kind of car you have. If surgery was on your left leg and you have an automatic car, you<br />
could be driving in two weeks. If the surgery was on your right leg, your driving could be<br />
limited as long as six weeks. Getting “back to normal” will depend on your progress. Talk<br />
with your surgeon for their advice, you should not drive if you are taking narcotic pain<br />
medication.<br />
When will I be able to get back to work?<br />
We recommend that most people take at least one month off from work, even if your job<br />
allows you to sit often. More strenuous jobs will need a longer absence from work.<br />
When can I have sexual intercourse?<br />
The time to resume sexual intercourse should be discussed with your surgeon. We have a<br />
guide on restarting sexual intercourse and a copy will be given to you when you leave the<br />
hospital.<br />
How often will I need to be seen by my doctor following my sur gery?<br />
Two to four weeks after leaving, you will be seen for your first post-surgery office visit. The<br />
frequency of follow-up visits will depend on your progress.<br />
Do you recommend any limits following this sur gery?<br />
Yes. High-impact activities such as contact sports, running, singles tennis and basketball are<br />
not recommended. Injury-prone sports such as downhill skiing are also dangerous for a new<br />
joint. Ask your surgeon for more information.<br />
What physical/ recreational activities may I participate in after my recovery?<br />
You are encouraged to take part in low impact activities such as walking, dancing, golfing,<br />
hiking, swimming, bowling and gardening.<br />
Will I notice anything different about my hip?<br />
In many cases, patients with hip replacements think that the new joint feels natural. But, we<br />
recommend avoiding extreme positions or high impact activities. Your leg with the new hip<br />
may be longer than it was before, either because of it became shorter with your hip disease, or<br />
to avoid risk of dislocation. Most patients get used to this feeling in time or can use a small lift<br />
in their other shoe. Some patients have aching in their thigh for a few months after surgery.
Before Surgery Check List<br />
What to do 4-6 weeks prior to surgery<br />
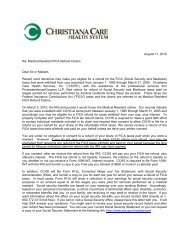
Contact Your Insurance Company<br />
Before surgery, you will need to call your insurance company. you will need to ask them if<br />
pre-authorization, pre-certification, second opinion or a referral form is needed before your<br />
surgery. It is important to make this call if things are missed they may not pay for some<br />
portions or delay your surgery. Complete the “Center for Advanced Joint <strong>Replacement</strong><br />
Insurance Checklist” form found on the next page and have this information ready when<br />
you talk to your case manager.<br />
If you do not have insurance, please tell the registration staff that you will need help in<br />
making payment arrangements.<br />
Pre-Register<br />
After your surgery has been scheduled, the admitting department will call you to gather<br />
your “pre-registration information” by phone. You will need to have the following<br />
information ready:<br />
■<br />
■<br />
■<br />
■<br />
■<br />
■<br />
■<br />
■<br />
■<br />
■<br />
Your full legal name and address, including county<br />
Home phone number<br />
Religion<br />
Marital status<br />
Social Security Number<br />
Name of insurance holder, his or her address and phone number<br />
Name of insurance company, mailing address, policy and group number<br />
Your employer, address, phone number and occupation<br />
Your retirement date, if applicable<br />
Name, address and phone number of someone to notify in case of emergency (this can be<br />
the same as the nearest relative)<br />
Get Medical And Anesthesia Clearance<br />
When you are scheduled for surgery, your surgeon will tell you whether you need to see<br />
your primary care doctor and/or a specialist before your surgery. Your case manager will<br />
call you to get medical information for the anesthesiologist 1-2 weeks before your operation.<br />
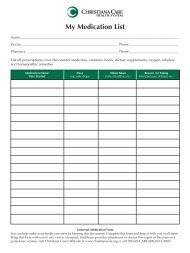
You will need to have a list of all your medications and the doses. The case manager may<br />
ask you to see your primary care doctor and/or a specialist after going over your history<br />
with the anesthesiologist. Call 302-428-2460 if you have any questions.
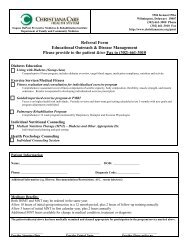
FYI: Joint <strong>Replacement</strong><br />
Insurance Checklist<br />
Member’s Name ____________________________ID#______________Date of Birth__________<br />
Address _____________________________________________________________<br />
City __________________________________________________State __________Zip __________<br />
Group Name/Group# ______________________________________________________________<br />
Lifetime Maximum _________________________________________________________________<br />
Other insurance ____________________________________________________________________<br />
__________________________________________________________________________________<br />
Deduction/Out of Pocket____________________________________________________________<br />
Co-Pays ___________________________________________________________________________<br />
Benefits<br />
Ask your insurance company what benefits you have for the following items:<br />
Where can you have your pre-admission testing done?__________________________________<br />
__________________________________________________________________________________<br />
Rehabilitation: (Skilled Nursing Facility, Subacute, Acute Rehabilitation) __________________<br />
__________________________________________________________________________________<br />
Home <strong>Care</strong> ________________________________________________________________________<br />
Outpatient Physical Therapy_________________________________________________________<br />
__________________________________________________________________________________<br />
Durable Medical Equipment _________________________________________________________<br />
__________________________________________________________________________________<br />
If I need to be on the medication Lovenox, when I go home would I be covered? ___________<br />
__________________________________________________________________________________
Obtain Laboratory Tests<br />
When you are scheduled for surgery you will get a laboratory-testing order sheet from your<br />
surgeon. Your case manager may also ask for some testing.<br />
Have your testing done at a lab approved by your insurance company 7-10 days before your<br />
surgery or within 30 days of your surgery. Have the results faxed to the Center for Advanced<br />
Joint <strong>Replacement</strong> at 302-428-4644. Call 302-428-2460, if you have any questions.<br />
Pre-Admission testing is available at <strong>Christiana</strong> <strong>Care</strong>. Testing areas are located at both<br />
Wilmington and <strong>Christiana</strong> Hospitals and are open 7 a.m. – 4:30 p.m. Monday through Friday<br />
and 8 – 11:30 a.m. on Saturdays. No appointment is needed.<br />
Lab Services at Wilmington Hospital Lab Services at <strong>Christiana</strong> Hospital Campus<br />
501 West 14th Street, <strong>Christiana</strong> <strong>Care</strong> Medical Arts Pavilion 1, Suite 100<br />
Wilmington, DE 19801 4745 Ogletown-Stanton Road, Newark, DE 19713<br />
302-428-6801 302-733-6244<br />
Decide Whether to Donate Your Blood (FYI section)<br />
You may wish to donate your own blood, please discuss your options with the surgeon.<br />
Review “About Blood Transfusions” in the FYI section of your notebook.<br />
Choose Your Coach<br />
Your Coach is someone (family or friend) who will be able to share in some of your physical<br />
therapy sessions, help you plan what happens when you go home and be a companion in<br />
your home when you go home to help with your needs. The Center for Advanced Joint<br />
<strong>Replacement</strong> welcomes coaches’ participation in all of your recovery to make sure you move<br />
smoothly home after your surgery.<br />
Review “What is an Advance Directive” (FYI section)<br />
The law requires that everyone being admitted to a medical facility have the chance to tell us<br />
how future decisions about their medical care should be decided (advance directives). Please<br />
refer to the FYI section of notebook for further information. Although you are not required to<br />
make an advance directive, you may if you wish. If you have advance directives, e.g. living<br />
will, please bring copies with you to the hospital on the day of your surgery.<br />
Schedule Physical Therapy Evaluation<br />
Many patients with arthritis favor their painful joint and become weaker. This delays your<br />
recovery. To help, it is important that you begin an exercise program before your surgery.<br />
We will contact you to schedule a pre-operative evaluation with one of our physical<br />
therapists. Please bring this notebook to your evaluation.<br />
A section in this notebook has some of exercises that your surgeon or physical therapist may<br />
recommend.<br />
Register For Joint <strong>Replacement</strong> Infor mation Class<br />
A special class is held weekly for patients scheduled for joint surgery. We will schedule this<br />
class with you before your surgery. You only need to attend one class. Members of our team<br />
will be there to answer your questions. It is strongly suggested that you bring your coach<br />
with you to class.
The outline of the class is as follows:<br />
■ Getting ready for surgery<br />
■<br />
■<br />
■<br />
■<br />
■<br />
■<br />
What to expect the day of surgery<br />
What to expect during your hospital stay<br />
Physical and Occupational therapy plan<br />
Role of the coach<br />
Planning for your release home after your surgery a review with the Case Manager<br />
Questions and answers<br />
What to do 4 weeks before Surgery<br />
Read “Anesthesia and You” (FYI Section)<br />
Total joint surgery does require the use of either general anesthesia or spinal anesthesia.<br />
Please review “Anesthesia and You”. If you have questions please contact your case manager<br />
or your surgeon’s office.<br />
What to do 5-10 Days before Surgery<br />
Stop medications that increase bleeding<br />
Seven days before surgery stop taking aspirin or products with aspirin in them. Five days<br />
before surgery stop all anti-inflammatory medications like Motrin, Naproxen, etc. These<br />
medications may cause bleeding. Talk to your doctor about other medications you can take<br />
for pain before surgery that do not cause bleeding. If you are on Coumadin, Plavix or<br />
Pradaxa, you will need special instructions for stopping these medication. Do not stop taking<br />
these medications without medical direction. Your case manager will tell you what to do with<br />
your other medications.<br />
Find Out Your Arrival Time<br />
Your surgeon asks you come to the hospital two to three hours before your surgery to give the<br />
staff plenty time to get you ready for surgery and answer any questions. It is important that<br />
you arrive come in on time because the surgical time can be moved up. If you are late, it may<br />
cause a significant problem with starting your surgery on time. Sometimes lateness could<br />
result in your surgery being moved to a much later time. If you are unsure when to arrive at<br />
the hospital, call your surgeon’s office.<br />
Prepare Your Home<br />
Have your house ready for your to come home. Clean. Do the laundry and put it away. Put<br />
clean linens on the bed. Make meals and freeze them in single serving containers. Cut the<br />
grass, tend to the garden and other yard work. Pick up throw rugs and tack down loose<br />
carpets. Remove electrical cords and other barriers from walkways. Put nightlights in<br />
bathrooms, bedrooms, and hallways. Stop the newspaper. Arrange to have someone collect<br />
your mail and take care of loved-ones or pets, if needed.<br />
Review “Fall Prevention in Your Home” in FYI section.
What to Do the Night Before Surgery<br />
Do not eat or drink anything after midnight unless otherwise instructed to do so.<br />
If you are told to take any medications by mouth the day of surgery, you may take these with<br />
a sip of water.<br />
What to Bring to the Hospital<br />
■ Picture ID.<br />
■ Copy of your Advance Directive, living will.<br />
■ Your <strong>Notebook</strong>.<br />
■ CPAP OR BiPap Equipment.<br />
■ Personal hygiene items (toothbrush, deodorant, etc.).<br />
■ Loose fitting clothing — drawstring or elastic waist shorts, loose fitting short sleeved t-shirts<br />
(golf shirts, button down short sleeved shirts — avoid long sleeved shirts) Please bring 3<br />
days’ worth of clothing.<br />
■ Button down or zip up fleece or cardigan sweater.<br />
■ Consider nylon underwear for women.<br />
■ Boxers and T-shirts for gentlemen.<br />
■ Night clothes if wished for sleeping (you can wear hospital gown at bedtime).<br />
■ Sneakers or flat soled rubber shoes and socks — avoid shoes without backs<br />
(flip flops and clogs).<br />
■ Technology items can be brought in but <strong>Christiana</strong> <strong>Care</strong> is not responsible for lost, damaged<br />
or stolen items. A Wireless network is offered and the Get Well Network is in each patient’s<br />
room allowing internet access from your bedside.<br />
Please Do Not Bring<br />
■ Medications not asked by the case manager.<br />
■<br />
Valuables such as wallets, pocketbooks, jewelry, large sums of money.<br />
Visiting Guidelines<br />
Our visitor guidelines are flexible to meet everyone’s needs. Visits from family members,<br />
friends and clergy are an important part of the healing. Our guidelines were made for safe<br />
and healthy healing for our patients. Children under the age of twelve may visit but must be<br />
with an adult, other than the patient, at all times. If family will be staying overnight with the<br />
patient, please set up this with the case manager or charge nurse before you come to the<br />
hospital.
Day of Surgery<br />
Wilmington Hospital<br />
Parking at Wilmington Hospital<br />
Garage parking is available; follow the signs to self parking. Valet parking is also available<br />
at the main entrance for a fee. Handicapped vehicles may use valet for free. Driving<br />
directions are available in the FYI section of your notebook for reference.<br />
Where to go once at Wilmington Hospital<br />
On the day of surgery, enter Wilmington Hospital at the main entrance. Take the South<br />
elevators to the 3rd floor, exit to your right and check in at the surgical waiting room on<br />
the left.<br />
What to expect at Wilmington Hospital<br />
Following check in, our surgical staff will get you ready for surgery. Family members will<br />
be directed to the waiting room. The surgeon will call them into the waiting room area once<br />
surgery is over. If family is not present and you would like your sugeon to call them, please<br />
have a contact number/cell phone number available at the time of check in.<br />
While in the operating room holding area, an IV will be started and your joint site will be<br />
scrubbed. Your operating room nurse as well as your anesthesiologist, will talk with you.<br />
They will take you to the operating room.<br />
<strong>Christiana</strong> Hospital<br />
Parking at <strong>Christiana</strong> Hospital<br />
Parking at <strong>Christiana</strong> Hospital is free in the visitor parking areas. Valet parking is available<br />
at the main entrance for a fee. Handicapped vehicles may use valet for free. Driving<br />
directions are available in the FYI section of your notebook for reference.<br />
Where to go once at <strong>Christiana</strong> Hospital<br />
On the day of surgery enter <strong>Christiana</strong> Hospital at the main entrance. Stop at the<br />
information desk in the main lobby for directions to the Surgery and Procedure Unit.<br />
What to expect at <strong>Christiana</strong> Hospital<br />
In the Surgery and Procedure Unit, you will get ready for surgery. You will then be taken to<br />
the operating room holding area.<br />
Family members will be directed to the surgical waiting room area. If your family is not<br />
present and you would like the surgeon to call them, please have the contact number.<br />
While in the operating room holding area, an IV will be started and your joint site will be<br />
scrubbed. Your operating room nurse as well as your anesthesiologist, will talk with you.<br />
They will take you to the operating room.
After Surgery Hospital <strong>Care</strong><br />
After Surgery<br />
Following surgery, you will go to a recovery area where you will stay for 1-2 hours. We will<br />
work with you to control your pain and your vital signs will be checked. You will then go to<br />
the Center for Advanced Joint <strong>Replacement</strong> floor where a nurse will care for you.<br />
Pain medication is available for you throughout your stay. You will be asked to rate your pain<br />
on a scale of 0-10, with “0” being no discomfort and “10” being the worst pain possible. Refer<br />
to the “Pain Control” in the FYI section of the notebook.<br />
Your surgeon may ask that you get out of bed, sit up and walk within hours after your<br />
surgery. It is important that you help with blood clot prevention as soon as possible after<br />
surgery by doing the ankle pumps, quad sets and glute set exercises in this notebook. Along<br />
with walking, these help prevent blood clots from forming in your legs.<br />
To help prevent any congestion, you will be taught and encouraged to use the incentive<br />
spirometer. Refer to the FYI pages in this notebook.<br />
Post-Operative Day 1<br />
The morning after surgery, you will be helped in bathing and dressed in clothing that you<br />
have brought from home. A physical therapy evaluation or your first group physical therapy<br />
session will take place. The physical therapist will check your progress and help you walk<br />
with a walker. Nurses will be help you move from IV pain medication to pain medicine by<br />
mouth. After lunch, you will have your second physical therapy session as a group setting.<br />
Coaches are encouraged to take part in physical therapy sessions as much as possible. Other<br />
visitors are welcome before and after therapy sessions.<br />
Post-Operative Day 2<br />
On day two after surgery, occupational therapy will visit you at your bedside and help you<br />
with your bathing and dressing, giving you adaptive equipment as needed. Following<br />
breakfast, you will take part in your first group physical therapy session of the day. A<br />
complimentary lunch for you and your coach is given this day. After lunch, you will have<br />
your second therapy session and may begin practicing stair climbing and car transfers. Your<br />
coach is encouraged to go to at least one physical therapy session this day.<br />
Post-Operative Day 3 or Discharge Day<br />
On day three after surgery, you will have breakfast and then attend an early morning physical<br />
therapy session. You will usually get to leave the hospital after this therapy session. Your<br />
nurse and physical therapist will give you detailed instructions before your leave. A family<br />
member or friend (or coach) is always encouraged to take part.<br />
The decision to go home or to a rehab/subacute facility will be made together by you, your<br />
surgeon, other members of the health care team, and your insurance company. Every attempt<br />
will be made to have this decision wrapped up in advance, but may be delayed until the day<br />
you are ready to leave depending on your progress.
Heading Home<br />
Someone will need to drive you home. Please make these arrangements before your surgery.<br />
Most patients will leave after morning therapy, after they get their discharge instructions<br />
about medications, physical therapy, activity, etc.. Any equipment, such as a walker, will be<br />
delivered to your room before you leave. Out-patient physical therapy or in home therapy<br />
arrangements will be done. Take your notebook to all physical therapy visits.<br />
If you are going to a Rehab/ Subacute Facility<br />
Someone needs to drive you to the rehab/subacute facility or we can help you arrange for<br />
transportation. There may be a charge if a van or ambulance is used. Transfer papers will be<br />
completed by the nursing staff. Either your primary care doctor or a doctor from<br />
rehab/subacute facility will be caring for you in discussion with your surgeon. Expect to stay<br />
three to 10 days based on your progress. On discharge home, instructions will be given to you<br />
by the rehab/subacute staff. Take this notebook with you.
Center for Advanced Joint<br />
<strong>Replacement</strong> Exercise<br />
Program – <strong>Hip</strong>
Exercising Before Surgery<br />
It is vital to be as fit as you can be before having a total joint replacement. This will make<br />
your healing go faster. Your surgeon will decide if pre-operative physical therapy (PT) is<br />
right for you.<br />
You will be taught in the hospital which exercises you should do after surgery. These may be<br />
unalike the exercises in this section. Be sure to check with your surgeon or PT about which<br />
exercises are best for you.
Seated Push-up<br />
1. Sit in chair with arms as shown.<br />
2. Push yourself up from the chair, using your arms as much<br />
as you can.<br />
3. It is OK to use your legs to help if necessary.<br />
4. Hold 1-2 seconds, slowly lower.<br />
5 30 repetitions, 2 times per day.
Ankle Pumps<br />
1. Bend your ankles up and down as if you are pumping<br />
the gas pedal.<br />
2. 30 repetitions, 2 times per day.
Quad Sets<br />
1. Sit or lie on your back with both legs straight.<br />
2. Press the back of your knee down.<br />
3. This will tighten the muscle on top of your thigh and move<br />
your kneecap towards your head.<br />
4. Hold 5 seconds.<br />
5. 30 repetitions, 2 times per day.
Gluteal Sets<br />
X X X<br />
1. Squeeze your buttocks together as tightly as possible.<br />
2. Hold for 5 seconds.<br />
3. Repeat this exercise 30 times.<br />
4. Do 2 times a day.
Exercising After Surgery<br />
Exercise is of great value to get the best results from your joint replacement surgery. You will<br />
need to keep doing your exercise program at an outpatient health site or at home as ordered<br />
by your surgeon when you leave the hospital.<br />
We offer choices for you to keep your PT going once you leave the hospital.<br />
Outpatient PT care can be set up at many places including <strong>Christiana</strong> <strong>Care</strong>’s PT PLUS or if<br />
you are not able to travel from your home preparations can be made through <strong>Christiana</strong><br />
<strong>Care</strong>’s Visiting Nurse Association or any other provider. (For a list of outpatient PT clinics,<br />
see “Outpatient PT Facilities” found in the FYI section of your notebook. )Your case manager<br />
will firm up these plans before you go home from the hospital.<br />
No matter what you choose, exercise is of great value to your care. It will support rapid healing<br />
and help you return to a more normal lifestyle.<br />
Please bring your notebook to all PT visits . After each session, ask your therapist to mark in<br />
your <strong>Notebook</strong> the right exercises for you. The goals and steps to take are listed on the next<br />
few pages.
Heel Slides<br />
1. Lie on back.<br />
2. Bend _____ knee and slide heel up toward body as shown.<br />
3. Hold 1 second, slowly relax.<br />
4. 30 repetitions, 2 times per day.
Windshield Wipers<br />
1. Lie on back.<br />
2. Side your leg out to the side, keeping your kneecap pointing<br />
towards the ceiling and your toes pointing up.<br />
3. Bring your leg back to the starting position.<br />
4. Do NOT cross the center of your body.<br />
5. Hold 1 second, slowly relax.<br />
6. 30 repetitions, 2 times per day.
Seated Knee Extension<br />
1. Sit on edge of table or bed.<br />
2. Straighten knee fully.<br />
3. Hold 1 second, and slowly lower.<br />
4. 30 repetitions, 2 times per day.
Seated <strong>Hip</strong> Flexion<br />
1. Sit on the edge of the chair or bed.<br />
2. Lift ________ knee ________ your hip level.<br />
3. Hold 1 second.<br />
4. 30 repetitions, 2 times per day.
Short Arc Quads<br />
1. Lie on your back with ________ inch roll under ________ knee.<br />
2. Raise heel off floor until knee is straight.<br />
3. Hold 1 second and slowly lower.<br />
4. 30 repetitions, 2 times per day.
Standing <strong>Hip</strong> Flexion<br />
1. Stand with legs straight.<br />
2. While holding onto a solid surface, bend ________ knee and<br />
hip upward as shown.<br />
3. Hold 1 second, slowly relax.<br />
4. 30 repetitions, 2 times per day.
Standing <strong>Hip</strong> Abduction<br />
1. Stand, holding onto solid surface for balance.<br />
2. Raise ________ leg out to side, without letting it come<br />
forward.<br />
3. Hold 1 second, slowly relax.<br />
4. 30 repetitions, 2 times per day.
Standing <strong>Hip</strong> Extension<br />
1. Stand with feet slightly apart.<br />
2. While holding onto a solid surface, lift ________leg backward<br />
as shown.<br />
3. Keep your body upright.<br />
4. Hold 1 second, slowly relax.<br />
5. 30 repetitions, 2 times per day.
Using the Clinical Diary<br />
A note for Professionals using this book<br />
This <strong>Notebook</strong> will help passing on information between all the health professionals who<br />
will be caring for our patient. The use of the Clinical Diary will let all important information<br />
be shared. Many patients see many professionals during the first three months.<br />
Upon discharge from the Center for Advanced Joint <strong>Replacement</strong> please record the following<br />
in the Clinical Diary:<br />
■<br />
■<br />
■<br />
■<br />
■<br />
<strong>Patient</strong> name, surgeon’s name, date of surgery and diagnosis.<br />
Center for Advanced Joint <strong>Replacement</strong> therapist’s name and discharge date.<br />
Knowledge of knee precautions.<br />
Discharge functional status for bed mobility, transfers, gait, and stairs.<br />
If the patient is going home, please insert appropriate home exercises in “Exercising After<br />
Surgery” section.<br />
Rehab/ Subacute/ Home <strong>Health</strong>/ Outpatient PT<br />
■ Please look at the whole notebook so that you are familiar with it and the goals that we<br />
expect the patient to meet.<br />
■ Check all information in the Clinical Diary and document the progress at least<br />
once a week.<br />
■ Include your name, agency or facility, and phone number.<br />
■ Choose the proper exercises and place them in the Exercising After Surgery<br />
section of the notebook.
Caring for Yourself at Home<br />
When you go home there are a many things you need to know for safety, speedy healing and<br />
your comfort.<br />
Caring for Yourself at Home<br />
■ Control your pain.<br />
■ Take your pain meds at least 30 minutes before PT.<br />
■ Do not drive or run machinery while taking narcotics.<br />
■ Use cold for pain control. Putting ice onto your joint will lower your pain and swelling.<br />
You can use ice before and after your exercise sessions. Do not put ice straight onto your<br />
skin. Your nurse will teach you on the use of cold treatment before you are sent home.<br />
■ Change your position every 45 minutes throughout the day to ease after surgery stiffness.<br />
Body Changes<br />
■ A well-nourished body will react better to healing and therapy. You may not feel hungry,<br />
but it is of great value to drink plenty of fluids to keep from being dehydrated. Your want<br />
for solid food will come back.<br />
■ You may have trouble sleeping. This is normal. Don’t sleep or nap too much during<br />
the day.<br />
■ Your drive level will be low for the first month.<br />
■ You may feel like you can not have a bowel movement or constipation. Use stool softeners<br />
or laxatives if needed. For more facts, read about "constipation" in the FYI section of your<br />
notebook.<br />
Blood Thinners<br />
You will need to take a blood thinner for one to six weeks after surgery, based on your condition.<br />
Be sure to take the drug exactly as set by your surgeon. Lovenox is one type of blood<br />
thinner that your surgeon may order for you. If so, you will be taught to give yourself an<br />
shot. Your surgeon may order aspirin as a blood thinner when you go home from the hospital.<br />
(coated aspirin in preferred.)<br />
Coumadin is a blood thinner that may be ordered by your doctor. If you are sent home on<br />
Coumadin, facts will be given to you.
Post-operative Swelling<br />
■ You may have swelling in your legs. To help it is best to lie down and raise your legs above<br />
your heart level a few times a day.<br />
■ Your surgeon may order stockings to help lower limb swelling. If in use, take off the<br />
stockings at least daily and check your skin. Talk over with your surgeon how long stockings<br />
will be needed.<br />
Caring for Your Incision<br />
■ Keep your incision dry.<br />
■ If your incision is without drainage, you may keep it open to air.<br />
■ Your incision will be closed with steri strips (small pieces of white tape) or staples.<br />
■ Most patients are free to shower 24 hours after all drainage has stopped.<br />
■ Tell your surgeon or home health professional if there is added drainage, redness, pain, odor<br />
or heat around your incision.<br />
■ Take your temperature if you feel warm or sick. Call your surgeon if it is over 101° F.<br />
■<br />
Your nurse will teach you on the care of your incision upon go home from the hospital.
Stopping and Recognizing<br />
Potential Complications<br />
Pleae read the FYI Sheets “DVT” and “Bleeding Precautions”.<br />
Signs of Infection<br />
■ Added swelling, redness at incision site.<br />
■<br />
■<br />
Change in color, amount, odor of drainage.<br />
Added pain in knee.<br />
■ Fever greater than 101 degrees F.<br />
Stop Infection<br />
■ Wash your hands before and after you take care of your incision.<br />
■ Take proper care of your incision as explained by your nurse and surgeon.<br />
■ You will need to take antibiotics before having dental work or other treatments from now<br />
on.<br />
■ Tell your doctor and dentist that you have a total joint replacement.<br />
Blood Clots in Legs<br />
Surgery may cause your blood flow to slow and clot in the veins of your legs, forming a<br />
blood clot. This is why you take blood thinners after surgery. If a clot does happen you may<br />
need to be admitted to the hospital for care. Prompt care most often stops the more serious<br />
problem of pulmonary embolus (A blood clot in a vein in the leg and moves to the lung<br />
where it can block blood flow).<br />
Signs of Blood Clots in Legs<br />
■ Swelling in your thigh, calf or ankle that does not go down when you raise your legs above<br />
the level of your heart..<br />
■ Pain, tenderness in your calf.<br />
NOTE: blood clots can form in either leg.<br />
Prevention of Blood Clots<br />
■ Do Post-operative exercises — ankle pumps, quad and gluteal sets.<br />
■<br />
■<br />
Walking.<br />
Blood thinners such as Lovenox, aspirin, or Coumadin. (as ordered by your surgeon)
Blood Clot (Pulmonary Embolus)<br />
An unrecognized blood clot could break off the vein and go to the lungs.<br />
If you suspect that you have a pulmonary embolus, call 911 immediately.<br />
Signs of an Embolus<br />
■ Sudden chest pain.<br />
■<br />
■<br />
■<br />
■<br />
■<br />
■<br />
Find it hard to breathe and/or rapid breathing.<br />
Shortness of breath.<br />
Sweating.<br />
Confusion.<br />
Rapid heart rate.<br />
Fainting.<br />
Stopping a lung Clot<br />
■ Stop blood clots in legs.<br />
■<br />
Know the signs of a blood clot in your leg and call doctor right away if you see any of these.<br />
Signs of <strong>Hip</strong> Dislocation<br />
■ Severe pain.<br />
■<br />
■<br />
Your leg is shorter than your other leg and rotated in the wrong direction.<br />
Unable to walk/move leg.<br />
Prevention of Dislocation<br />
■ Your PT will tell you about your activity limits.
When Standing Up<br />
from a Chair<br />
Proper Method<br />
Improper Method<br />
Do NOT pull up on the walker to stand!<br />
Sit in a chair with armrests when possible.<br />
1. Scoot to the front edge of the chair.<br />
2. Slide your operated leg out in front of you.<br />
3. Push up with both hands on the armrests. If sitting in a chair<br />
without armrests, place one hand in the center of the walker<br />
while pushing off the side of the chair with the other hand.<br />
4. Balance yourself before putting your hands on the walker.
Walking with Walker<br />
1. Move the walker forward to a comfortable arms length.<br />
2. Ensure all four walker legs are firmly on the ground. Step<br />
forward with the operated leg. Place the foot in the middle<br />
of the walker area.<br />
3. Take your weight on your hands and step forward with the<br />
unoperated leg.<br />
NOTE: Take small steps. Do NOT take a step until all four<br />
walker legs are flat on the floor. Stand tall.
Using a “Reacher” or<br />
“Dressing Stick”<br />
Putting on pants<br />
and underwear:<br />
1. Sit down.<br />
2. Using a reacher<br />
or dressing stick<br />
to guide the waist<br />
band over your<br />
foot, put your<br />
operated leg into<br />
the pants first,<br />
then your<br />
unoperated leg.<br />
3. Pull your pants up over your knees to within easy reach.<br />
4. Stand with the walker in front of you to pull your pants up the<br />
rest of the way.<br />
Taking off pants and underwear:<br />
1. Back up to the chair or bed where you will be undressing.<br />
2. Unfasten your pants and let them drop to the floor. Push your<br />
underwear down to your knees.<br />
3. Lower yourself down. Take your unoperated leg out first and<br />
then the operated leg.<br />
4. A reacher or dressing stick can help you remove your pants<br />
from your foot and off the floor.
Using a “Sock Aid”<br />
How to use a sock aid:<br />
1. Slide the sock onto the sock aid with the toe completely tight<br />
at the end.<br />
2. Hold the cord and drop the sock aid in front of your foot. It is<br />
easier to do this if your knee is bent as much as possible.<br />
3. Slip your foot into the sock aid.<br />
4. Straighten your knee, point your toe, and pull the sock on.<br />
5. Keep pulling until the sock aid pulls out.<br />
6. Do not cross your legs when putting on your socks.
Using a Long-Handled<br />
Shoehorn<br />
1. Use your reacher, dressing<br />
stick, or long-handled shoehorn<br />
to slide your shoe in<br />
front of your foot. Bend your<br />
knee as much as possible<br />
when doing this.<br />
2. Place the shoehorn inside<br />
the shoe against the back of<br />
the heel. Have the curve of the shoe horn match the curve of<br />
the shoe.<br />
3. Lean back, if necessary, as you lift your leg and place your toes<br />
in your shoe.<br />
4. Step down into your shoe, sliding your heel down the shoehorn.<br />
NOTE: Wear sturdy rubber-soled slip-on shoes or shoes<br />
with Velcro closures or elastic shoe laces. DO NOT wear<br />
high-heeled shoes or shoes without backs.
Moving into Tub<br />
Getting into the tub using a bath seat:<br />
1. Place the bath seat in the tub facing the faucets.<br />
2. Back up until you feel the tub with the back of your legs. Be<br />
sure you are in front of the tub bench.<br />
3. Reach back with one hand for the tub bench. Keep the other<br />
hand in the center of the walker.<br />
4. Slowly lower yourself onto the tub bench.<br />
5. Move the walker out of the way, but keep it within reach.<br />
6. Lift your legs over the edge of the tub, one at a time.<br />
Getting out of the tub using a bath seat:<br />
1. Keeping your body and legs in line, lift your legs one at a<br />
time, over the outside of the tub.<br />
2. Scoot to the edge of the bath seat.<br />
3. Push up withboth hands on the tub seat.<br />
4. Balance yourself before putting your hands on the walker.<br />
Tub Seat<br />
Tub Bench
NOTE: To keep soap within easy reach, make a<br />
soap-on-a-rope by placing a bar of soap in the toe<br />
of an old pair of pantyhose and attach it to the<br />
bath seat.<br />
NOTE: ALWAYS use a rubber mat or non-skid<br />
adhesive on the bottom of the tub or shower.<br />
NOTE: While using a tub seat, grab bars, longhandled<br />
bath brushes, and hand-held showers<br />
make bathing easier and safer, they are typically<br />
not covered by insurance.<br />
Getting in and out of the tub using the tub<br />
transfer bench:<br />
■ Follow the steps for getting in/out of the tub using<br />
a tub seat.<br />
■ The advantage of using a tub transfer bench is that<br />
it extends over the edge of the tub giving a larger<br />
area to sit.
Moving to Toilet<br />
When sitting down on<br />
the toilet:<br />
1. Take small steps and turn<br />
until your back is to the<br />
toilet. Never pivot!<br />
2. Back up until you feel the<br />
toilet touch the back of your<br />
leg. If using a commode with<br />
armrests, reach back for<br />
both armrests and lower<br />
yourself onto the toilet.<br />
If using a toilet without armrests,<br />
keep one hand in the<br />
center of the walker while<br />
reaching back for the toilet<br />
seat with the other hand.<br />
When getting up from the toilet:<br />
1. If using a commode with armrests, use the armrests to push<br />
up. If using a raised toilet seat without armrests, place one<br />
hand in the center of the walker and push off the toilet seat<br />
with the other.<br />
2. Balance yourself before putting your hands on the walker.
Moving Into Bed<br />
When getting into bed:<br />
1. Back up to the bed until you feel the bed against the back of<br />
your legs (Position yourself so your head will be on the pillow<br />
when you lie down).<br />
2. Reaching back with both hands, sit down on the edge of the<br />
bed. Scoot back toward the center of the mattress. (Silk<br />
pajama bottoms or satin sheets, may make it easier)<br />
3. Move your walker out of the way, but keep it within reach.<br />
4. Keeping your body and legs in line, move around until you<br />
are facing the foot of the bed.<br />
5. Lift your leg into the bed (if this is your operated leg, you may<br />
use a cane, a rolled bed sheet, a belt, or your leg lifter to assist<br />
with lifting that leg into bed).<br />
6. Keep moving around and lift your other leg into the bed.<br />
NOTE: DO NOT CROSS YOUR LEGS to help the operated<br />
leg into bed.
Moving Out of Bed<br />
When getting out of bed:<br />
1. Sit up on your elbows.<br />
2. Move to the edge of the bed.<br />
3. Move around keeping your body and legs in line.<br />
4. Lower your legs to the floor and sit up.<br />
5. Check to make sure you are not dizzy.<br />
6. Slide your operated leg out in front of you.<br />
7. Use both hands to push off the bed.<br />
8. Balance yourself before putting your hands on the walker.
Lying In Bed<br />
Keep a pillow between your legs when lying on your back.<br />
Try to keep the operated leg positioned in bed so the kneecap<br />
and toes are pointing toward the ceiling. Try not to let your<br />
kneecaps roll inward or outward. A blanket or towel-roll on<br />
the outside of your leg may help you maintain this position.
Lying in Bed –<br />
Four Weeks Post-op<br />
When rolling from your back to your side, first bend your<br />
knees toward you until your feet are flat on the bed.<br />
Then place at least two pillows (bound together) between<br />
your legs. With knees slightly bent, and pillows between your<br />
knees, roll over on to your side.
Moving into or out of the Car<br />
1. Push the car seat all the<br />
way back and recline the<br />
back.<br />
2. Back up until you feel the<br />
back of your legs against<br />
the car.<br />
3. Reach back for the car seat<br />
with your right hand and<br />
the dashboard with your left,<br />
or the middle of the walker.<br />
4. Place your operated leg in<br />
front of you.<br />
5. Lower yourself down.<br />
6. Watch your head!!!<br />
7. Scoot your bottom<br />
back into the car.<br />
8. Lean back as you lift<br />
your legs into the<br />
car one at a time.<br />
Remember to bend<br />
your hip and ankle<br />
to clear the door.<br />
9. TIP: Place a plastic<br />
trash bag on the seat<br />
of the car to help<br />
you slide and turn<br />
toward the front.
Household Chores:<br />
Saving Energy and<br />
Protecting Your Joints<br />
Kitchen<br />
■ Do NOT get down on your knees to scrub floors. Use a mop and long-handled brushes.<br />
■ Plan ahead! Gather all your cooking goods at one time. Then sit to get ready your meal.<br />
■ Place commonly used cooking goods and tools where they can be reached without too<br />
much bending or stretching.<br />
■ To give a better working height, use a high stool, or put cushions on your chair when<br />
making meals.<br />
Bathroom<br />
■ Do NOT get down on your knees to scrub bathtub. Use a mop or other long-handled<br />
brushes.<br />
Safety and Avoiding Falls<br />
■ Pick up throw rugs and tack down loose carpeting. Cover slick surfaces with carpets that<br />
are firmly anchored to the floor or that have non-skid backs.<br />
■ Be aware of all floor hazards such as pets, small objects or not flat surfaces.<br />
■ Provide good lighting throughout. Install nightlights in the bathrooms, bedrooms,<br />
and hallways.<br />
■ Keep extension cords and phone cords out of pathways. Do NOT run wires under<br />
rugs, this is a fire hazard.<br />
■ Do NOT wear open-toe slippers or shoes without backs. They do not give enough<br />
support and can lead to slips and falls.<br />
■ Sit in chairs with arms. It makes it simpler to get up and down.<br />
■ Rise slowly from either a sitting or lying position so as not to get light-headed.<br />
■ Do NOT lift heavy objects for the first three months, and then only with your<br />
surgeon's okay.<br />
■ Stop and think. Use good wisdom.
Do’s and Don’ts<br />
For the Rest of Your Life<br />
Whether you have reached all your goals in three months or not, you need to have a normal<br />
exercise program to keep up your fitness and the health of the muscles around your joints.<br />
With your doctors okay you should be on a exercise program three to four times per week<br />
lasting 20 - 30 minutes. Impact activities such as running and singles tennis may put too<br />
much stress on your joint and are not advised. High-risk activities such as downhill skiing<br />
are discouraged because of the risk of broken bones around the artificial joint. Infections are<br />
could always be a problem and you will need antibiotics for help stop this, mainly with<br />
dental treatments. Please talk with your surgeon and dentist.<br />
What to Do in General<br />
■ Even If the risks are very low for post-op infections, it is of great value to realize that the<br />
risk stays. A prosthetic joint could likely draw the germs from an infection found in some<br />
other part of your body. If you should get a fever of more than 101 degrees, or have an<br />
injury such as a deep cut or puncture wound, you should clean the wound as best you can,<br />
put a sterile dressing or Band-Aid on it and tell your doctor. The closer the damage is to<br />
your joint, the bigger the fear. Now and then, antibiotics may be needed. On the surface<br />
scratches may be treated with an antibiotic ointment. Tell your doctor if the area becomes<br />
painful or red.<br />
■ When traveling, stop and change position hourly to stop your joint from getting stiff.<br />
■ See your surgeon yearly unless otherwise suggested.<br />
■ Exercise regularly.<br />
■ Start a weight reduction/management program if you are heavy.<br />
What to Do for Exercise<br />
Choose a Low Impact Activity<br />
Suggested exercise classes<br />
■ Home program as outlined in <strong>Notebook</strong><br />
■ Regular one to three mile walks<br />
■ Home treadmill<br />
■ Stationary bike<br />
■ Regular exercise at a fitness center<br />
■ Arthritis aquatic classes<br />
■ Low impact sports-golf, bowling, walking, gardening, dancing, etc.<br />
What Not to Do<br />
■ Skip running or engaging in high-impact activities.<br />
■ Skip high-risk activities such as contact sports or downhill skiing.
FYI: Advance Directive<br />
Advance directive are steps you leave for others when you cannot make your own health<br />
choices. These choices are written down while you are feeling well and thinking clearly.<br />
They make clear to your family and your doctors the amount of care you wish to get, or not<br />
to get, should you become not awake or aware or too ill to make a choice at a later point in<br />
your life.<br />
There are two ways to make an advance directive:<br />
■ Individual Instructions (at one time called living will)<br />
A living will is a written record of the care you would choose for yourself during “terminal<br />
injury or illness”. A terminal illness or injury is one that will cause you to die within the<br />
near future. It is called a "living will" because it is used while you are still alive, but your<br />
death is very near. Your living will usually tell your doctors what kind of care you do or do<br />
not want. Your decision maker (agent) and caregivers must follow your instructions in a living<br />
will. <strong>Christiana</strong> <strong>Care</strong> offers the 5 Wishes advance directive form.<br />
■<br />
Power of Attorney <strong>Health</strong> <strong>Care</strong> Choices<br />
This is a paper where you name some other person(s) as your agent to make health care<br />
choices for you when you are not able to do so yourself.<br />
Federal law calls for hospitals to ask all patients whether they have Advance<br />
Directive for health care. It our policy to honor your wishes for your health care<br />
through your Advance Directive, as long as they follow Delaware law and the rules<br />
of the <strong>Christiana</strong> <strong>Care</strong> <strong>Health</strong> <strong>System</strong>.<br />
For more information<br />
You can get more information through:<br />
<strong>Christiana</strong> <strong>Care</strong>'s <strong>Patient</strong> Relations Department<br />
<strong>Christiana</strong> Hospital, 302-733-1340<br />
Wilmington Hospital, 302-428-4608<br />
Pastoral Services<br />
<strong>Christiana</strong> Hospital, 302-733-1280<br />
Wilmington Hospital, 302-428-2780<br />
Delaware's Division of Services for Aging and Adults with Physical Disabilities<br />
Statewide, 800-223-9074<br />
New Castle County, 302-453-3820,<br />
Kent and Sussex Counties, 302-422-1386.<br />
Although it is not required, you may also contact an attorney.
FYI: Anesthesia<br />
Anesthesia is given by a member of the Department of Anesthesiology. Your care will be<br />
given by a team of caregivers, this team is made up of anesthesia doctors (anesthesiologists)<br />
as well as nurses (nurse anesthetists) who are specially trained in this area.<br />
On the day of your surgery, a member of the team will talk to you about your anesthesia,<br />
will put an IV (intravenous catheter) into a vein so that they can give you medicine<br />
and fluids.<br />
Types of Anesthesia<br />
Listed below are some ways that anesthesia can be given. How you will get treated will be<br />
explained in detail to you before your surgery. No matter what type of anesthesia is given,<br />
we will watch over you, check your blood pressure, heart rate, temperature and oxygen<br />
level the whole time.<br />
■ General Anesthesia: You will not be awake. Most major surgery’s need you to be totally<br />
asleep. A breathing tube is most often used; this tube is put in while you are asleep and in<br />
most cases comes out before you wake up, so you will not know it was there at all.<br />
■ Spinal or Epidural: This is given by putting numbing medicine around the nerves in your<br />
back. This keeps the lower half of your body numb. Other drugs will be given to make you<br />
sleepy and relaxed during surgery.<br />
■ Regional: This causes brief numbness and lack of strength to an exact part of your body.<br />
This is done by placing numbing medicine into that part of your body. Other drugs may be<br />
given to make you sleepy and relaxed during surgery.<br />
■ Monitored Anesthesia <strong>Care</strong>(MAC): the anesthesia team and your surgeon will work<br />
together to keep you relaxed. Medicine to briefly numb the part of you having surgery will<br />
be given by your surgeon. Your heart rate, blood pressure, temperature and oxygen level<br />
will be watched by the anesthesiology team who will give you other drugs to make you<br />
sleepy and relaxed during the operation.<br />
Side effects and risks can happen with all types of anesthesia. You may have a brief loss of<br />
clear thinking and be clumsy after your surgery. Your team will talk to you about this on<br />
the day of your operation.<br />
Special Monitoring<br />
For some surgeries you may need extra monitoring, the types of extra monitoring that may<br />
be used are below:<br />
■ Arterial Catheter: A thin, plastic tube (like an IV) is put into an artery in your wrist. This<br />
tube checks your blood pressure all the time.<br />
■ Central Venous Catheter or Pulmonary Artery Catheter: A small plastic tube (like an IV) is<br />
put into a large vein in your neck or upper chest. This tube keeps a close eye on your vital<br />
signs and heart.<br />
If your team thinks they may need to use any type of special monitoring, they will tell this<br />
to you when you meet. Sometimes the need for these things happens during your surgery.<br />
If so, the team may start this while you are asleep, even though you did not talk about it<br />
before operation. When you sign the Surgical/Procedure Consent, you give consent for the<br />
anesthesia team to be part of your care.
FYI: Bleeding Precautions<br />
Sometimes there are drugs, illness, diseases, and/or surgeries that can put you at a higher<br />
risk for bleeding. Follow the safety tips below to lower your risk for bleeding:<br />
Safe grooming tips<br />
■ Shave with an electric razor.<br />
■ Use a soft bristled toothbrush to clean your teeth.<br />
■ Keep dry skin moisturized. Do not scratch your skin.<br />
■ Skip manicures and pedicures.<br />
■ Wear shoes to protect your feet..<br />
Safety tips for activity<br />
■ Skip activities or sports that could cause injury or bleeding.<br />
■ Wear gloves when gardening.<br />
■ Protect yourself from cutting or bruising your skin.<br />
■ Always wear a seat belt.<br />
Personal habits<br />
■ Skip drinking large amounts of alcohol.<br />
■ Avoid constipation (not able to have a bowel movement).<br />
■ Blow your nose gently.<br />
Medical care<br />
■ Check with your doctor before taking any new medicines, take care with over-the-counter<br />
medicines and herbal medicines too.<br />
■ Do not use suppositories unless your doctor asks you to use.<br />
■ Skip aspirin or any medicine with aspirin in them<br />
■ Check with your doctor before having any operation, dental work, or tests.<br />
■ Hold pressure on a cut or area from which blood is taken until bleeding stops.
FYI: Blood Transfusions<br />
Transfusion is the word that we use when we talk about giving blood to a you in your IV.<br />
<strong>Christiana</strong> <strong>Care</strong> gets most of the blood we need from the Blood Bank of Delmarva, which<br />
runs many blood bank centers (where you go to give blood) in Delaware and Maryland.<br />
Blood is donated by a volunteer who meets all the rules that make sure their blood is safe to<br />
use.<br />
All blood is tested to see the type (A, B, O), antibodies (things that could make you sick), and<br />
certain illnesses, like syphilis and viruses like AIDS and hepatitis. Once the blood gets to the<br />
hospital, it is tested to make sure the blood type ( A, B, O) matches your blood type.<br />
Risks<br />
Your doctor is aware of all the risks of giving blood to you and will make sure the you get<br />
only what is needed for your care. With all the testing done when the blood is given at the<br />
blood bank, the risks of getting blood is less than the risks to you if you do not get blood<br />
when you need it.<br />
Here is what we know of risk for getting blood in the United States:<br />
Viral Risks<br />
■ HIV ...................................................................................1 in 2,300,000<br />
■ Hepatitis B.......................................................................1 in 220,000<br />
■ Hepatitis C ......................................................................1 in 1,800,00<br />
■ HTLV (can cause leukemia) .........................................1 in 2,900,000<br />
Getting a virus can happen even with all the strict rules of donor testing that are used.<br />
The largest risks when you get blood are written below::<br />
■ Acute Hemolytic Reaction............................................1 in 50,000<br />
■ Bacterial contamination in red cells (infection).........1 in 30,000<br />
■ Anaphylaxis (serious allergic reaction) .....................1 in 30,000<br />
■ Bacterial contamination in platelets (infection).........1 in 3,000<br />
■ Delayed Hemolytic Reaction........................................1 in 2,000<br />
■ Transfusion Related Acute Lung Injury (TRALI) .....1 in 1,500 - 1 in 190,000<br />
■ Allergic reaction or hives ..............................................1 in 100<br />
■ Fever .................................................................................1 in 500<br />
Blood is given as red cells (PRBC), platelets, frozen plasma or cryoprecipitate<br />
(this helps your blood clot).<br />
Other Choices<br />
Other Choices to the standard transfusion are:<br />
■ Autologous (Your own blood): Giving your own blood before you come for surgery.<br />
Your blood is kept cold and can be used for 42 days. Your doctor can set<br />
this up with the Blood Bank of Delmarva.<br />
■ Blood Salvage (Cell Saver): Blood that you lose during your operation is gathered,<br />
cleaned and given back to you.<br />
■ Directed Donation: You can ask a friend or family member to give blood for<br />
you. This blood is tested like all other blood; your doctor can set this up with<br />
the Blood Bank of Delmarva.<br />
Your doctor can give you more facts about blood transfusion risks, benefits, or other choices.
FYI: Constipation<br />
Constipation, when you are not able to have a bowel movement, happens when waste is<br />
slow to move through your gut. The result is less than three stools (BMs) a week. Surgery,<br />
not exercising, a change in your eating/drinking habits, and certain drugs can cause constipation.<br />
Constipation may cause cramping, bloating/gas, loss of hunger, stomach or back pain, and<br />
upset belly. Many people use this term when they feel they haven't emptied their gut, or<br />
when they feel they should have BMs more often.<br />
Recommendations<br />
■ Keep a written record of your BMs.<br />
■ Drink 6 to 8 (soda can size) glasses of liquid each day. The best liquids to drink are water<br />
and fruit juice.<br />
■ Limit the amount of caffeine you drink such as coffee, tea and soda.<br />
■ Eat a well-balanced high fiber diet; it makes BMs softer and simpler to pass. Good choices<br />
are fresh fruits and vegetables, whole-grain breads, oatmeal and bran cereal and brown rice.<br />
■ Skip milk and dairy products and foods high in sugar because they can make it worse.<br />
■ Plan time for BMs, when you don't have to hurry.<br />
■ Exercise will help, walking, swimming and biking are good choices.<br />
(Note: Be sure to talk with your doctor before starting any exercise program.)<br />
■ Your doctor may order medicine to put off constipation. Take these meds as ordered.<br />
■ Talk with your doctor or nurse before using laxatives, enemas, or suppositories for constipation.<br />
Call your doctor or nurse if you have:<br />
■ Constipation that lasts longer than two weeks<br />
■ Fever and belly pain with the constipation<br />
■ Bright red blood in your BMs<br />
■ Loose Bowel Movements
FYI: Deep Vein Thrombosis<br />
(DVT) Prevention<br />
What is a DVT?<br />
Deep vein thrombosis (DVT) is a blood clot inside a vein. It usually happens in the veins of<br />
your thighs or calves.<br />
What are some of the risk factors for A DVT?<br />
■ Major surgery which limit mobility ■ Cancer<br />
■ 40 years of age or older ■ History of heart and lung disease<br />
■ Activity level less than normal ■ History of DVT<br />
■ Sitting still for too long ■ Pregnancy<br />
■ Birth control medication ■ Blood clotting diseases<br />
■ Hormone replacement medication ■ Smoking<br />
■ Chronic breathing problems ■ Traumatic injuries<br />
What are some of the signs that I could have a DVT?<br />
■ Redness and warmth in a leg or arm<br />
■ Pain or tenderness in a leg or arm<br />
■ Increased swelling in a leg or arm not better with elevation<br />
■ May have no signs at all<br />
What are the risks of DVT?<br />
Clots that form in your veins can break in bits and travel to other parts of the body,<br />
including your lungs. A blood clot in the lungs is called a pulmonary embolism (PE).<br />
These types of clots can be life threatening and must be treated right away.<br />
Signs of PE<br />
■ Trouble breathing ■ Sharp chest pain<br />
■ Rapid heart beat ■ Anxiety or nervousness<br />
■ Fever ■ Cough that may make bloody discharge<br />
■ Fainting<br />
If you have any of these, call your doctor or nurse right away or dial 911 if you are at home.
How do I prvent DVT?<br />
DVT precautions<br />
■ Start walking as soon as possible after surgery/injury with your doctors say-so.<br />
■ Do your post-operative exercises:<br />
Ankle pumps: Pump your ankles like you would on a car gas pedal.<br />
Gluteal sets: Squeeze your thighs and buttocks and hold them tight for 3 seconds.<br />
■ Wear compression<br />
■ Wear compression boots at all times unless you are walking, until you go home from the<br />
hospital.<br />
■ Drink plenty of fluids; skip caffeine and alcohol.<br />
■ Skip tight socks, shoes and clothing, which could cut off blood flow to your legs.<br />
■ Do not cross your legs or ankles.<br />
■ Stop smoking.<br />
■ Do not sit for long periods of time.<br />
■ When you watch TV, stand up and stretch and walk around the room<br />
during commercials<br />
■ When you are driving long distances, stop and get out of the car and walk around for 10-<br />
15 minutes every hour.<br />
■ Your doctor may order medicine to help avoid clotting; these come in pills, shots or IV<br />
infusions; your doctor will decide what is best for you.<br />
■ For more information on DVT prevention, complication, and treatment watch these<br />
patient education videos:<br />
■ Lovenox<br />
■ Coumadin<br />
■ Smoking Cessation<br />
■ Pulmonary Embolism<br />
■ Anticoagulants<br />
Ready in the “Get Well Network” or by calling 7620 on your phone. Ask your nurse for<br />
help to play the videos.
FYI: Disposal of Needles,<br />
Syringes & Lancets<br />
in the Home<br />
Don’t get stuck<br />
■ Every time you need to throw away a needle/syringe or lancet, drop it into a plastic container<br />
(such as a bleach or laundry detergent bottle) as soon as you have used it.<br />
■ When the bottle is filled to the bottom of the handle, screw on the cap and throw it away<br />
in your trash.<br />
■ Store in a safe place away from children.<br />
Safety tips<br />
■ Have the throwaway container open and next to you when using a needle/syringe<br />
■ Never hand a needle/syringe to some other person. Never walk with an open<br />
needle/syringe in your hand.<br />
■ Never set a needle/syringe down after using it; always place it inside the bottle.
FYI: Fall Prevention<br />
in the Home<br />
Falls occur in all age groups. The chance of falling grows with age. Each year three out of<br />
every ten people over the age of 65 will fall. Often these falls happen at home and can lead<br />
to serious injury. The good news is that many of these falls can be avoided. We want to<br />
help make your home a safer place. Please use these tips to help avoid falls in your home:<br />
General<br />
■ Be sure hallways, stairs and other areas are brightly lit.<br />
■ Remove all clutter (boxes, stacks of magazines, toys, extra furniture).<br />
■ Get rid of throw rugs. Tack down loose or torn carpet.<br />
■ Use non-slip wax on floors.<br />
■ Put safety tape where there is a change in level so that they are simpler to see.<br />
■ Put in night-lights or motion-detector lights in most often used areas (hallways, bathrooms<br />
and bedrooms).<br />
■ Keep electrical and phone cords out of your walkway.<br />
■ Tape down or hide extension cords.<br />
■ Be aware of pets that can get under your feet.<br />
■ Think about a personal emergency response set-up or cell phone if you live alone or spend<br />
most of the day alone.<br />
■ Keep important phone numbers close to the phone your doctor, family, etc.<br />
■ Keep the phone close to your bed.<br />
Medications<br />
■ Some drugs may place you at a higher risk for falls (such as, some heart pills, blood pressure<br />
pills, sleeping pills, nerve pills, water pills, allergy and cold drugs). Check with your<br />
doctor if you feel dizzy or lightheaded.<br />
■ Share a list of all medicines you are taking with your doctor. Be sure to list all the things<br />
you take prescribed drugs, herbs and natural products that you take.<br />
■ Keep your drug list with you at all times. Also place this list close to the phone in case of an<br />
emergency.<br />
Clothing<br />
■ Be sure to wear your glasses or hearing aid if you need them.<br />
■ Wear shoes that fit and have no heels. Or, wear sturdy slippers with non-skid soles. Do not<br />
wear shoes with thick heavy soles. Try using shoes with stretchy laces or Velcro closures.<br />
■ Do not wear clothes that are too long.<br />
Kitchen and other rooms<br />
■ Make an open pathway throughout the house.<br />
■ Arrange furniture to keep from tripping or bumping into it.<br />
■ Use a normal height bed or lower bed if likely to fall from bed.<br />
■ Handrails can be used for balance when walking.
Bathroom(s)<br />
■ Put In grab bars to help get in and out of the bathtub, shower, or on and off the toilet.<br />
■ Use non-skid bath mats or rubber strips on the bottom of the bathtub or shower.<br />
■ Use a shower chair, tub bench or raised toilet seat.*<br />
■ Leave the bathroom door unlocked, so it can be opened from both sides.<br />
Assistive devices<br />
■ Use walkers, canes, and wheelchairs as recommended.*<br />
* Medicare, Medicaid or other insurance may cover some of these items.<br />
Check with your insurance provider.<br />
Activity<br />
■ If you have lightheadedness due to low blood sugar or low blood pressure, eat soon after<br />
waking up. Keep a drink or snack at your bedside.<br />
■ Change position slowly. Dangle your legs at the side of your bed, sofa, etc. for a few minutes<br />
before standing.<br />
■ Place things that you use often within easy reach.<br />
■ Avoid climbing and reaching to high shelves. Use a reacher or stable step-stool with<br />
handrails. Do not stand on a chair reach high shelves.<br />
Stairs<br />
■ Cover stairs with tightly woven carpet or non-slip treads.<br />
■ Put In sturdy handrails on both sides of the stairway and outside steps.<br />
■ Tighten loose handrails.<br />
Community Resources - Local:<br />
■ Agility, Balance & Coordination Program -<br />
(Eugene du Pont Preventive Medicine & Rehabilitation Institute)<br />
■<br />
■<br />
■<br />
■<br />
■<br />
A six-week exercise program to improve stability. 302-661-3300.<br />
Balance & Mobility Center<br />
Check with your doctor if you have problems with balance and need a special evaluation.<br />
302-428-6780<br />
Home Safety Evaluation<br />
You may qualify for a home safety evaluation. Please check with your doctor or <strong>Christiana</strong><br />
<strong>Care</strong> <strong>Health</strong> <strong>System</strong>’s referral service, 302-428-4100, for more information<br />
Are You OK? (Dover City Police Program)<br />
Daily telephone reassurance for seniors or the disabled living in Kent County.<br />
302-734-1200, ext. 128.<br />
Delaware State <strong>Health</strong> and Social Services<br />
Division of Services for Aging and Adults With Physical Disabilities<br />
256 Chapman Road, Newark, DE Phone – 302-453-3820<br />
1901 N. DuPont Highway, New Castle, DE Phone – 302-577-4791<br />
Booklet available: Guide to Services for Older Delawareans. Home care agencies and home<br />
medical equipment agencies are listed in this book.<br />
Delaware Safety Council, Inc.<br />
3 Old Barley Mill Road, Wilmington, DE 19807<br />
302-654-7786 - Fax 302-654-4617<br />
800-342-2287 (outside of New Castle County)<br />
Email: desafe@mail.del.net
■<br />
■<br />
■<br />
■<br />
■<br />
Delaware Stroke Initiative<br />
Newark, DE<br />
302-633-9313<br />
Email: destrokeinitiative@yahoo.com<br />
Offer names and addresses for resources and supplies for patient with CVA<br />
Home Medical Equipment Agencies<br />
For walkers, raised toilet seats, and other assistive devices. Check with your physician.<br />
Medicare, Medicaid or other insurance may pay for equipment and devices. Agencies are<br />
listed in the Yellow Pages of the phone book or in the Guide to Services for Older<br />
Delawareans.<br />
Home <strong>Care</strong> Agencies<br />
Check with your physician. Some offer a home safety evaluation. Medicare, Medicaid or<br />
other Insurance may pay for services. Agencies are listed in the Yellow Pages of the phone<br />
book or the Guide to Services for Older Delawareans.<br />
Visiting Nurse Association<br />
One Reads Way<br />
New Castle, DE 19720<br />
302-327-5200<br />
Out-patient Providers<br />
Community Resources - National:<br />
■<br />
■<br />
■<br />
National Stroke Association<br />
9707 E Easter Lane, Building B<br />
Centennial, CO 80112<br />
303-649-9299 - Fax 303-649-1328<br />
Web site: www.stroke.org Email: info@stroke.org<br />
American Academy of Orthopaedic Surgeons<br />
6300 North River Road Rosemont, Illinois 60018-4262<br />
800-824-BONES (2663) Web site: ww.aaos.org<br />
National Institute Of Aging<br />
A clearinghouse for health information. For information on preventing falls and fractures,<br />
call 800-222-2225. Web site: www.nih.gov/nia<br />
Personal Emergency Response <strong>System</strong>s:<br />
■<br />
■<br />
■<br />
American Red Cross - Life Line<br />
215-299-4000<br />
800-959-6989<br />
Web Site: www.redcross-philly.org<br />
BERS Corporation<br />
Med Alert<br />
215-699-5766<br />
800-985-4357<br />
PERSYS<br />
800-631-7370<br />
Web Site: www.amcest.com<br />
Exit Alarm Resources:<br />
■<br />
Col Com, Inc.<br />
800-864-7778
FYI: Guided Imagery<br />
for Relaxation<br />
Guided imagery is a simple way to use the power of your own imagination to help you<br />
relax, help your body to heal, or simply relax! By listening to a guided imagery story, you<br />
will be helped to think positive, pleasant thoughts while you picture a pleasant image<br />
such as a tropical beach, mountain meadow.<br />
These pleasant images can feel real. This is often called the “mind-body connection.” You<br />
may have felt this when you read a recipe or just think about a certain food that you really<br />
like makes your mouth start to water! It is of great value to understand that guided<br />
imagery is used as well as common nursing and medical care, not as an alternative.<br />
Some good result of guided imagery are:<br />
■ Lower stress and worry<br />
■ Lower stress, anxiety and pain<br />
■ Help with sleep<br />
■ Get ready for surgical or procedures<br />
■ Help with stopping smoking<br />
■ Lower upset belly/vomiting<br />
■ Help you sleep<br />
Guided imagery can be felt by listening to an audiotape/CD, being guided by a coach or<br />
teacher, or alone.<br />
Getting Started<br />
■ You may listen to a guided imagery story or music.<br />
■ Two guided imagery stories are on hand. One story takes you to a tropical beach and the<br />
other walks you through a mountain meadow. Each story lasts 20 minutes.<br />
■ When you are ready, you will be given a headset and we will help you get started.<br />
■ Get cozy. You may want to use the bathroom first.
Guided Imagery Programs<br />
To select the program you would like to listen to, follow the directions below for either the<br />
<strong>Patient</strong> Education Television or the Get Well Network.<br />
<strong>Patient</strong> Education Television<br />
1. Dial 7620 on your telephone.<br />
2. Listen to the instructions and enter the<br />
3 digit code of the audiotape that you<br />
would like to listen to:<br />
• Tropical beach story: 0 6 9<br />
• Mountain meadow story: 0 7 0<br />
• Music only selection: 0 9 8<br />
3. Change the TV channel as instructed.<br />
4. Plug the headset/ear plug into the TV.<br />
5. Close your eyes and listen to the story<br />
or music.<br />
Get Well Network<br />
1. From the Welcome Screen, select “My<br />
<strong>Health</strong>”<br />
2. Select “My <strong>Health</strong> Videos”<br />
3. Select “<strong>Health</strong> Video Library”<br />
4. Select “Guided Imagery Relaxation”<br />
from the main menu.<br />
5. Choose the audiotape that you would<br />
like to listen to:<br />
• Tropical beach story<br />
• Mountain meadow story<br />
• Music only selection<br />
6. Plug the headset/ear plug into the TV<br />
or listen via the pillow speaker<br />
7. Close your eyes and listen to the story<br />
or music.<br />
When you are done listening to the program, stretch slowly and enjoy how you feel!<br />
Listen to a story or music as often as you would like. The benefits of guided imagery often<br />
grow when used more than once.<br />
If you would like to buy any of the guided imagery audiotapes, they are on hand in the<br />
hospital gift shop.<br />
Note: DO NOT use guided imagery while operating machinery or driving a motor vehicle.
FYI: Incentive Spirometer<br />
An incentive spirometer is a tool that<br />
helps deep breathing and measures the<br />
size of each breath. Incentive spirometry<br />
also helps you cough and get rid of<br />
extra mucous in your lungs.<br />
How to use your incentive spirometer<br />
1. Sit in a good position to take<br />
a deep breath.<br />
2. Make a tight seal around the<br />
mouth- piece with your lips.<br />
3. Slowly breathe in deeply through<br />
the mouthpiece.<br />
4. Take the mouthpiece out of your<br />
mouth and breathe out.<br />
5. Repeat this 10-20 times.<br />
6. When you have done this,<br />
cough several times.<br />
7. Repeat the 10-20 deep breaths and<br />
coughing as ordered by your doctor.<br />
8. If you have had belly or chest surgery,<br />
placing a pillow or your hand over<br />
your incision for support will make<br />
taking deep breaths.<br />
➳<br />
Mouth<br />
Piece
FYI: Pain Control<br />
■<br />
■<br />
We believe the treatment of your pain is a vital part of your care. Pain is your body's way<br />
of reacting to injury or illness. There are two types of pain:<br />
Acute pain follows an injury to the body and most often goes away when the injury heals.<br />
Chronic pain lasts for six months or longer and can get in the way of normal movements.<br />
Your nurse will ask you to use a number scale to rate your level of pain:<br />
No pain Moderate pain Worst pain possible<br />
Or, you may choose the face below that best fit the pain you are feeling. Each face is for a<br />
person who feels happy because he has no pain (hurt) or sad because he has some pain.<br />
Face 0 is very happy because he doesn’t hurt at all. Face 2 hurts just a little bit. Face 4 hurts<br />
just a little bit more. Face 6 hurts even more. Face 8 hurts a whole lot. Face 10 hurts as much<br />
as you can imagine, though you don’t have to be crying to feel this bad.<br />
It is vital to tell your nurse when you are having pain. By knowing what your pain feels<br />
like to you, we can better handle your pain.<br />
Some things that may be used to control your pain are:<br />
■ Medications<br />
■ <strong>Patient</strong> controlled analgesia (PCA)<br />
■ Epidural analgesia<br />
■ Relaxation techniques<br />
■ Changing your position<br />
■ Heat or cold treatment<br />
■ Physical therapy (PT)<br />
■ Direct you to a pain center<br />
You and your doctor will work together to find what pain control care are best for you.<br />
The goal is to control your pain, keeping you as comfortable as possible.
FYI: <strong>Patient</strong> Controlled<br />
Analgesia (PCA) Pump<br />
PCA lets you run your pain medication. Instead of calling for a nurse when you need pain<br />
medicine, you can simply push the PCA pump button. This gives you the right dose of pain<br />
drug your doctor has ordered - no more, no less.<br />
Your doctor will order the amount of pain medicine that you can get. The pump is set to<br />
give you medicine in one of three ways:<br />
■<br />
■<br />
■<br />
■<br />
■<br />
■<br />
■<br />
Only when you push the button.<br />
All of the time.<br />
All of the time, with an extra dose of drug when you push<br />
the button. (Your nurse will let you know how your doctor has<br />
ordered your pain medication).<br />
If your pump has been set to give drug when you push the<br />
button, push the button with your thumb and let go, a beep<br />
will sound, letting you know that the drug has been given.<br />
You cannot by accident make the machine work by rolling<br />
over onto the button.<br />
You cannot give yourself more drug than your doctor has<br />
ordered because there are safety checks built into the<br />
pump. The pump will alarm to alert your nurse when the<br />
drug supply is low or if it is not running the right way.<br />
Do not wait until you are in bad pain before pushing the<br />
button. Push the button when you first have pain so that<br />
you can better curb your pain. It is also a good idea to take<br />
pain medicine before activities such as coughing and deep breathing, therapy or walking to<br />
the bathroom.<br />
You should let your nurse know if your pain is not being controlled. Also let the nurse<br />
know if you are having dizziness, constipation, upset belly, vomiting, itching or pain at the<br />
place where the needle goes into your skin.<br />
Important visitor information<br />
It is expected that family members and guests are worried for their loved one’s pain. A<br />
patient can have serious harmful reactions, such as becoming too sleepy, and may stop<br />
breathing if a well-intentioned family member or friend were to push the button for them.<br />
The pain button is to be used by the patient only. If you feel your family member is having<br />
trouble pressing the button or have other concerns, please talk to the nurse right away.
FYI: Preventing Infection<br />
We are committed to your safety. We want your hospital stay to be safe. Please tell us if you<br />
have questions or concerns. By regularly talking to the people caring for you, a mix-up may<br />
be skirted. If you are not sure why something is being done, just ask.<br />
Everyone has a part in making health care safe. We want you to ask questions. If something<br />
does not seem right, it is okay to speak up. We want you to get the safest care.<br />
Everyone in a health care setting, whether in a hospital or doctor's office, is at risk for infection.<br />
Hands can carry and spread germs. Many germs can live a long time on objects, mostly<br />
items that are handled often, such as pens, countertops, faucets and side-rails. Hands can<br />
pick up and carry millions of germs without even looking dirty.<br />
Washing your hands is the best way to stop infection. Alcohol hand gel may also be used to<br />
clean hands unless they look dirty. Alcohol hand gel cleans hands by killing germs. A dimesized<br />
amount of gel is rubbed over the hands and let dry. Ask our staff if they have washed<br />
their hands before starting your care. We will not be offended.<br />
All hands can spread germs, not just those of health care staff. It is just as important for you<br />
and your visitors to keep your hands clean.<br />
Handwashing<br />
■ If your hands are dirty, place your hands under warm water, lathering with soap for at least<br />
15 seconds.<br />
■ Rinse your hands well with plenty of warm water and dry them with a paper towel. Wash<br />
or clean your hands often:<br />
■ Before eating or drinking and after using the bathroom.<br />
■ After wiping or blowing your nose, sneezing or coughing.<br />
■ After touching anything that is known to be dirty or has germs (pets, plants, floor/ground,<br />
mouth, etc.)<br />
■ If you cannot get to a sink to wash your hands, ask your nurse for help. Washing your<br />
hands at the bedside can be done.<br />
Please remind your guests to clean their hands before and after they visit you. Bottles of<br />
alcohol hand gel are on the walls inside patient rooms. All staff and guests can use these.<br />
Also, ask friends and family members not to visit you if they are sick, because they can also<br />
spread germs, putting you and other patients at risk for infection.<br />
For More Information<br />
Ask questions and stay involved. If something does not seem right, speak up! While in the<br />
hospital, you can learn more about safety by watching our <strong>Patient</strong> Education TV <strong>System</strong>.<br />
Turn your TV to channel 32 to see a list of available videos.<br />
We suggest watching:<br />
■ Medication safety ■ Infection control<br />
■ <strong>Patient</strong> rights ■ Fall prevention
FYI: Preventing Falls<br />
We are committed to your safety. We want your hospital stay to be safe. Please tell us if you<br />
have questions or concerns. By regularly talking to the people caring for you, a mix-up may<br />
be skirted. If you are not sure why something is being done, just ask.<br />
Everybody has a part in making health care safe. We want you to ask questions. If something<br />
does not seem right, it is okay to speak up. We want you to get the safest care.<br />
Most falls in the hospital will take place if you try to get out of bed or a chair on your own.<br />
While in the hospital, remember:<br />
■ Drugs that you get may make you feel drowsy, dizzy or light-headed.<br />
■ Having surgery or other procedures may make it hard for you to get out of bed.<br />
■ You may have equipment attached to your body that may raise your risk of falling.<br />
■ Being in a different place might make you feel a little disoriented, mostly at night.<br />
■ Having pain can make it hard to move around.<br />
If you want to get out of bed:<br />
■ Keep your call button nearby so you can easily call your nurse. Call the nurse before getting<br />
out of bed.<br />
■ Do not ask your family members to help you get out of bed without speaking to the nurse<br />
first. We want you to get up and move , but also want to protect you from falling.<br />
■ Wait for your nurse to help you get up if you have equipment attached to you. Some equipment<br />
on your body may need to be taken off such as a blood pressure cuff or leg boots.<br />
Other equipment may need to be handled with care like an IV or urine drainage bag. We<br />
may, at times, use equipment to help you sit up, such as a patient lift.<br />
■ Seek help from your nurse if you are using oxygen. Moveable equipment will be brought<br />
into your room so you can use oxygen while you are up walking in the halls.<br />
■ Wear slippers or socks with a non-slip sole.<br />
■ Do not lean on your IV pole for support when you are trying to walk. The wheels could<br />
roll, making you lose your balance and fall.<br />
While in the bathroom:<br />
■ If you should feel lightheaded, dizzy or drowsy while in the bathroom, sit down and pull<br />
the call-light string. This will let your nurse know that you need help.<br />
■ We may not leave you alone in the bathroom , we respect your privacy but we want to<br />
make sure you are safe.<br />
For More Information<br />
We are committed to your safety. We need your help to do this. Ask questions and stay<br />
involved. If some- thing does not seem right, speak up! While in the hospital, you can learn<br />
more about safety by watching our <strong>Patient</strong> Education TV <strong>System</strong>. Turn your TV to channel<br />
32 to see a list of available videos.<br />
We suggest watching:<br />
■ Medication safety ■ Infection control<br />
■ Fall prevention ■ <strong>Patient</strong> rights
FYI: Rehabilitation Services<br />
After surgery, your surgeon will order rehabilitation services (<strong>Health</strong> care services that help<br />
a you keep, learn or improve skills for daily living. These services may include physical and<br />
occupational therapy, speech-language pathology and other services for people with disabilities).<br />
Based on how well you do and the help you have at home, your doctor may order<br />
more treatment to help you return home safely and pick up your daily activities. You<br />
should plan to have someone to help you for a short time after you go home.<br />
Our team will work with you to set up care when you go home if needed. We will check<br />
with your insurance company to make the right choices for you.<br />
Rehabilitation services provided by <strong>Christiana</strong> <strong>Care</strong> <strong>Health</strong> <strong>System</strong>:<br />
■ Acute inpatient rehabilitation unit at Wilmington Hospital.<br />
■ Outpatient rehabilitation services at Wilmington Hospital, <strong>Christiana</strong> Hospital, and at a<br />
number of local sites including Physical Therapy PLUS.<br />
■ Home care therapy with Visiting Nurse Association.+<br />
We invite you to call us for more information and/or a tour of our facilities. Please talk to<br />
your doctor about your rehabilitation choices.<br />
Center for Rehabilitation at<br />
Wilmington Hospital<br />
302-428-6667<br />
Outpatient Rehabilitation<br />
Wilmington or <strong>Christiana</strong> hospitals<br />
302-428-6600 or 302-733-1950<br />
Visiting Nurse Association<br />
302-327-5200 or 888-VNA-0001<br />
Our main focus is to help you reach your goals, we are always more than happy to help, so<br />
please give us a call.<br />
* There are many providers in the area, not associated with <strong>Christiana</strong> <strong>Care</strong>, who can treat<br />
you after you leave the hospital. <strong>Christiana</strong> <strong>Care</strong> has a non-exclusive list of people who supply<br />
care in the area. This list is on hand to you upon request. Your doctor may know of<br />
other providers in the area who can meet your needs. Also, your insurance may have preferred<br />
providers for you to use after leaving the hospital. Please talk with your doctor and<br />
insurer to learn about services that are on hand to you once you leave the hospital.<br />
+ The Visiting Nurse Association and <strong>Christiana</strong> <strong>Care</strong> <strong>Health</strong> Services are affiliated entities.
FYI: Outpatient Physical<br />
Therapy Facilities<br />
<strong>Christiana</strong> <strong>Care</strong> Physical Therapy PLUS sites<br />
New Castle<br />
One Read's Way<br />
Suite 300<br />
New Castle, DE 19720<br />
302-327-5755<br />
Newark<br />
<strong>Health</strong>care Center at <strong>Christiana</strong><br />
200 Hygeia Drive<br />
Newark, DE 19713<br />
302-623-0390<br />
Middletown<br />
Middletown <strong>Care</strong>Center<br />
124 Sleepy Hollow Drive<br />
Middletown, DE 19709<br />
302-449-3050<br />
Glasgow<br />
Springside Plaza<br />
Conner Building<br />
300 Biddle Avenue<br />
Newark, DE 19702<br />
302-838-4700<br />
Brandywine<br />
Foulkstone Plaza<br />
1401 Foulk Road<br />
Wilmington, DE 19803<br />
302-477-4305<br />
Wilmington<br />
Wilmington Hospital<br />
6th Floor<br />
501 West 14th Street,<br />
Wilmington, DE 19899<br />
302-428-6662<br />
Pike Creek<br />
Pike Creek Fitness Club<br />
4905 Mermaid Boulevard<br />
Wilmington, DE 19808<br />
302-235-0456<br />
Greenville<br />
Preventive Medicine &<br />
Rehabilitation Institute<br />
3506 Kennett Pike<br />
Wilmington, DE 19807<br />
Phone: 302-661-3350<br />
Fax: 302-661-3310<br />
Dover<br />
230 Beiser Boulevard<br />
Dover, DE 19904<br />
302-736-0994<br />
Convenient evening and Saturday hours and<br />
transportation available.
FYI: Directions to Hospitals<br />
Wilmington Hospital and Roxana Cannon Arsht Surgicenter<br />
From I-95, southbound<br />
Take exit 7 B (Delaware Avenue). Turn left onto Delaware Avenue. At the second traffic<br />
light, turn left onto Jefferson Street and go one block onto the Wilmington Hospital<br />
Campus.<br />
From I-95, northbound<br />
Take exit 7 (Delaware Avenue). Pass through four traffic lights then turn right onto<br />
Delaware Avenue and move into the left lane. At the first light, turn left onto Jefferson Street<br />
and go one block onto the Wilmington Hospital campus.<br />
From I-495, southbound<br />
Take exit 3 (12th Street) north to U.S. 13. Turn left at traffic light on U.S. 13, crossing over<br />
bridge, bearing right and passing through one traffic light. Turn right on E. 10 th Street.<br />
Turn right on Walnut Street. Go two blocks and turn left on 12 th Street. Follow 12th Street<br />
to Jefferson Street and turn right onto the Wilmington Hospital campus.<br />
When you arrive on the Wilmington Hospital campus, follow signs to the appropriate<br />
location.<br />
<strong>Christiana</strong> Hospital<br />
From I-95, southbound<br />
Take Exit 4B onto Route 58 west (Churchmans Rd.). Follow Route 58 one mile.<br />
Turn left at the light to enter <strong>Christiana</strong> Hospital campus.<br />
From I-95, northbound<br />
Take Exit 4B onto Route 7/Route 1 north. Take Exit 166 onto Route 58 west (Churchmans<br />
Rd.). Follow Route 58 for six-tenths of a mile.<br />
Turn left at the light to enter <strong>Christiana</strong> Hospital campus.
Wilmington Area<br />
Directions to Wilmington Hospital Campus<br />
From I-95, southbound<br />
Take exit 7B (Delaware Avenue). Turn left onto Delaware Avenue. At<br />
the second traffic light, turn left onto Jefferson Street and go one block<br />
onto the Wilmington Hospital campus. For the Roxana Cannon Arsht<br />
Surgicenter, turn left into parking lot from Jefferson Street. For<br />
Wilmington Hospital, park in the parking garage.<br />
From I-95, northbound<br />
Take exit 7 (Delaware Avenue). Turn right onto<br />
Delaware Avenue and move into the left lane.<br />
At the first light, turn left onto Jefferson<br />
Street and go one block onto the Wilmington<br />
Hospital campus. For the Roxana Cannon<br />
Arsht Surgicenter, turn left into<br />
parking lot from Jefferson Street.<br />
For Wilmington Hospital, park<br />
in the parking garage.<br />
Pennsylvania Ave.<br />
52<br />
Delaware Ave.<br />
Exits<br />
7 & 7B<br />
Brandywine Park<br />
95<br />
Brandywine Creek<br />
Wilmington<br />
Hospital<br />
Jefferson<br />
Baynard Blvd.<br />
14th Street<br />
202<br />
Concord Pike<br />
Washington Street<br />
North Market Street<br />
13<br />
Fourth Street<br />
95<br />
MLK Blvd.<br />
Washington Street<br />
Orange Street<br />
Market Street Mall<br />
Train<br />
Station<br />
King Street<br />
12th Street<br />
11th Street<br />
Walnut Street<br />
10th Street<br />
Church Street<br />
Northeast Blvd.<br />
13<br />
Gov. Printz<br />
Market Street<br />
13<br />
Christina River
<strong>Christiana</strong> Hospital Campus<br />
From I-95, southbound<br />
Take Exit 4B onto Route 58 west<br />
(Churchman’s Road).<br />
Follow Route 58 for one mile.<br />
Turn left at the light to enter <strong>Christiana</strong><br />
Hospital campus.<br />
Follow signs for Parking at the Main<br />
Entrance.<br />
From I-95, northbound<br />
Take Exit 4 onto Route 7/Route 1 north.<br />
Take Exit 166 onto Route 58 west<br />
(Churchman’s Road).<br />
Follow Route 58 for 6/10 of a mile.<br />
Turn left at the light to enter <strong>Christiana</strong><br />
Hospital campus.<br />
Follow signs for the Parking at the<br />
Main Entrance.<br />
Lot F<br />
Lot G<br />
Lot F<br />
Lot E<br />
Textile<br />
Services<br />
Service Building<br />
Lot J Lot K Lot L<br />
To Rt.7<br />
To I-95<br />
Lot D<br />
MD Lot<br />
E<br />
Education<br />
Building<br />
Emergency<br />
Department<br />
<strong>Christiana</strong> Hospital<br />
D C B A<br />
Lot B<br />
Women’s<br />
<strong>Health</strong><br />
Services<br />
MRI<br />
Medical Arts<br />
Pavilion 1<br />
Lot P<br />
<strong>Christiana</strong><br />
Surgicenter<br />
Lot N<br />
Medical Arts<br />
Pavilion 2<br />
Lot M<br />
Churchmans Road (Rt. 58)<br />
Lot C<br />
Lot B<br />
Lot A<br />
Lot R<br />
10<br />
Helen F. Graham<br />
Cancer Center<br />
To Rt.7<br />
Hygeia Drive<br />
Blood Bank<br />
of Delaware<br />
Ogletown-Stanton Road (Rt. 4)<br />
Entrance to buildings<br />
<strong>Health</strong><strong>Care</strong> Center<br />
at <strong>Christiana</strong><br />
Handicapped Parking