WOM N WOM N - Mount Sinai Hospital
WOM N WOM N - Mount Sinai Hospital WOM N WOM N - Mount Sinai Hospital
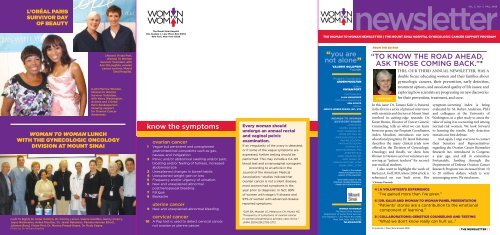
L’ORÉAL PARIS SURVIVOR DAY OF BEAUTY WOM N WOM TO N The Mount Sinai Hospital One Gustave L. Levy Place, Box #1252 New York, New York 10029 newsletter THE WOMAN TO WOMAN NEWSLETTER | THE MOUNT SINAI HOSPITAL GYNECOLOGIC CANCER SUPPORT PROGRAM WOM N WOM TO N VOL. 3, NO. 1 | FALL 2008 (Above) Vivian Port, Woman To Woman Survivor Volunteer, with Ann McLaughlin, ovarian cancer survivor, Mount Sinai Hospital. (Left) Myrtice Wooten, Woman to Woman Survivor Volunteer, with Kerry Washington, Actress and L’Oréal Paris Spokesperson showing support for Ovarian Cancer Awareness. WOMAN TO WOMAN LUNCH WITH THE GYNECOLOGIC ONCOLOGY DIVISION AT MOUNT SINAI (Left To Right) Dr. Peter Dottino, Dr. Dimitry Lerner, Valerie Goldfein, Nancy Irizarry, Joyce Manheimer, Arden Moulton, Dr. Jamal Rahaman, Pamela Herman Elliott, Julianne Bond, Vivian Port, Dr. Monica Prasad Hayes, Dr. Rudy Segna. Photo by Dr. William Bradley know the symptoms ovarian cancer 1 . Vague but persistent and unexplained gastrointestinal complaints such as gas, nausea, and indigestion 2 Pelvic and/or abdominal swelling and/or pain; bloating and/or feeling of fullness, increased abdominal size 3 Unexplained changes in bowel habits 4 Unexplained weight gain or loss 5 Frequency and/or urgency of urination 6 New and unexplained abnormal postmenopausal bleeding 7 Fatigue 8 Backache uterine cancer 9 New and unexplained abnormal bleeding 10 cervical cancer A Pap test is used to detect cervical cancer, not ovarian or uterine cancer. Every woman should undergo an annual rectal and vaginal pelvic examination. If an irregularity of the ovary is detected, or if some of the vague symptoms are expressed, further testing should be performed. This may include a CA-125 blood test and a transvaginal sonogram. According to an article in the Journal of the American Medical Association,* studies indicate that ovarian cancer is not a silent disease; most women had symptoms in the year prior to diagnosis. In fact, 89% of women with stage I/II disease and 97% of women with advanced disease reported symptoms. *Goff BA, Mandel LS, Melancon CH, Muntz HG. “Frequency of symptoms of ovarian cancer in women presenting to primary care clinics.” JAMA 2004;291:2705-2712 “you are not alone” VALERIE GOLDFEIN Founder Program Coordinator ARDEN MOULTON Editor VIVIAN PORT PHOTOGRAPHY ALAN MANHEIMER EDITORIAL ASSISTANCE KEN ATKATZ DESIGN JESSICA WEBER DESIGN, INC., NYC WOMAN TO WOMAN ADVISORY BOARD JAMIE BORIS CARMEL COHEN, MD MARY COSGROVE, MD PETER DOTTINO, MD ANNE BUSH FEELEY, RN VALERIE GOLDFEIN FAITH KATES KOGAN CYNTHIA LEVY SARA PASTERNAK, PHD JENNIFER PECK JAMAL RAHAMAN, MD RUDY SEGNA, MD VIRGINIA WALTHER, LCSW ROBIN ZAREL, LCSW Thanks to the Holland Family Foundation for its support of the newsletter. WITH GRATITUDE TO THE OVARIAN CANCER RESEARCH FUND FOR THEIR SUPPORT. WOMAN TO WOMAN The Mount Sinai Hospital Department of Social Work Services One Gustave L. Levy Place, Box #1252 New York, New York 10029 Tel: 212.241.3793 FROM THE EDITOR “TO KNOW THE ROAD AHEAD, ASK THOSE COMING BACK.”* THIS, OUR THIRD ANNUAL NEWSLETTER, HAS A double focus: educating women and their families about gynecologic cancers, their prevention, early detection, treatment options, and associated quality of life issues; and exploring how scientists are progressing on new discoveries VIVIAN PORT *Chinese Proverb All materials © Mount Sinai Hospital 2008 for their prevention, treatment, and cure. In this issue: Dr. Tamara Kalir is featured in the first in a series of planned interviews with scientists and doctors at Mount Sinai involved in cutting-edge research; Dr. Karen Brown, Director of Cancer Genetic Counseling, tells us what we can learn from our genes; our Program Coordinator, Arden Moulton, introduces our new educational programs; Dr. Jamal Rahaman describes the many clinical trials now offered in the Division of Gynecologic Oncology; and finally, we show how Woman to Woman survivor volunteers are serving as “patient teachers” for secondyear medical students. I also want to highlight the work of Barbara A. Goff, MD, whose 2004 article is referenced on our back cover. Her 4 | A VOLUNTEER’S EXPERIENCE “I’ve gained more than I’ve given.” symptom-screening index is being evaluated by M. Robyn Andersen, PhD, and colleagues at the University of Washington, in a pilot study to assess the value of using it as a screening tool among normal-risk women. We look forward to learning the results. Early detection remains our best defense. And, again, I urge everyone to contact their Senators and Representatives regarding the Ovarian Cancer Biomarker Research Act, introduced in Congress a year ago, and still in committee. Fortunately, funding through the Department of Defense Ovarian Cancer Research Program was increased from 10 to 20 million dollars, which is very encouraging news. We need more. 6 | DR. KALIR AND WOMAN TO WOMAN PANEL PRESENTATION “Patients’ stories are a contribution to the emotional component of learning.” 8 | COLLABORATIONS: GENETICS COUNSELING AND TESTING “What we don’t know really can hurt us...” | THE NEWSLETTER | 1
- Page 2 and 3: interview with JAMAL RAHAMAN, MD Th
- Page 4 and 5: WOMAN TO WOMAN VOLUNTEERS TELL THEI
- Page 6: frequent screenings or screenings t
L’ORÉAL PARIS<br />
SURVIVOR DAY<br />
OF BEAUTY<br />
<strong>WOM</strong> N<br />
<strong>WOM</strong> TO<br />
N<br />
The <strong>Mount</strong> <strong>Sinai</strong> <strong>Hospital</strong><br />
One Gustave L. Levy Place, Box #1252<br />
New York, New York 10029<br />
newsletter<br />
THE <strong>WOM</strong>AN TO <strong>WOM</strong>AN NEWSLETTER | THE MOUNT SINAI HOSPITAL GYNECOLOGIC CANCER SUPPORT PROGRAM<br />
<strong>WOM</strong> N<br />
<strong>WOM</strong> TO<br />
N<br />
VOL. 3, NO. 1 | FALL 2008<br />
(Above) Vivian Port,<br />
Woman To Woman<br />
Survivor Volunteer, with<br />
Ann McLaughlin, ovarian<br />
cancer survivor, <strong>Mount</strong><br />
<strong>Sinai</strong> <strong>Hospital</strong>.<br />
(Left) Myrtice Wooten,<br />
Woman to Woman<br />
Survivor Volunteer,<br />
with Kerry Washington,<br />
Actress and L’Oréal<br />
Paris Spokesperson<br />
showing support<br />
for Ovarian Cancer<br />
Awareness.<br />
<strong>WOM</strong>AN TO <strong>WOM</strong>AN LUNCH<br />
WITH THE GYNECOLOGIC ONCOLOGY<br />
DIVISION AT MOUNT SINAI<br />
(Left To Right) Dr. Peter Dottino, Dr. Dimitry Lerner, Valerie Goldfein, Nancy Irizarry,<br />
Joyce Manheimer, Arden Moulton, Dr. Jamal Rahaman, Pamela Herman Elliott,<br />
Julianne Bond, Vivian Port, Dr. Monica Prasad Hayes, Dr. Rudy Segna.<br />
Photo by Dr. William Bradley<br />
know the symptoms<br />
ovarian cancer<br />
1 . Vague but persistent and unexplained<br />
gastrointestinal complaints such as gas,<br />
nausea, and indigestion<br />
2 Pelvic and/or abdominal swelling and/or pain;<br />
bloating and/or feeling of fullness, increased<br />
abdominal size<br />
3 Unexplained changes in bowel habits<br />
4 Unexplained weight gain or loss<br />
5 Frequency and/or urgency of urination<br />
6 New and unexplained abnormal<br />
postmenopausal bleeding<br />
7 Fatigue<br />
8 Backache<br />
uterine cancer<br />
9 New and unexplained abnormal bleeding<br />
10<br />
cervical cancer<br />
A Pap test is used to detect cervical cancer,<br />
not ovarian or uterine cancer.<br />
Every woman should<br />
undergo an annual rectal<br />
and vaginal pelvic<br />
examination.<br />
If an irregularity of the ovary is detected,<br />
or if some of the vague symptoms are<br />
expressed, further testing should be<br />
performed. This may include a CA-125<br />
blood test and a transvaginal sonogram.<br />
According to an article in the<br />
Journal of the American Medical<br />
Association,* studies indicate that<br />
ovarian cancer is not a silent disease;<br />
most women had symptoms in the<br />
year prior to diagnosis. In fact, 89%<br />
of women with stage I/II disease and<br />
97% of women with advanced disease<br />
reported symptoms.<br />
*Goff BA, Mandel LS, Melancon CH, Muntz HG.<br />
“Frequency of symptoms of ovarian cancer<br />
in women presenting to primary care clinics.”<br />
JAMA 2004;291:2705-2712<br />
“you are<br />
not alone”<br />
VALERIE GOLDFEIN<br />
Founder<br />
Program Coordinator<br />
ARDEN MOULTON<br />
Editor<br />
VIVIAN PORT<br />
PHOTOGRAPHY<br />
ALAN MANHEIMER<br />
EDITORIAL ASSISTANCE<br />
KEN ATKATZ<br />
DESIGN<br />
JESSICA WEBER DESIGN, INC., NYC<br />
<strong>WOM</strong>AN TO <strong>WOM</strong>AN<br />
ADVISORY BOARD<br />
JAMIE BORIS<br />
CARMEL COHEN, MD<br />
MARY COSGROVE, MD<br />
PETER DOTTINO, MD<br />
ANNE BUSH FEELEY, RN<br />
VALERIE GOLDFEIN<br />
FAITH KATES KOGAN<br />
CYNTHIA LEVY<br />
SARA PASTERNAK, PHD<br />
JENNIFER PECK<br />
JAMAL RAHAMAN, MD<br />
RUDY SEGNA, MD<br />
VIRGINIA WALTHER, LCSW<br />
ROBIN ZAREL, LCSW<br />
Thanks to the Holland<br />
Family Foundation for its<br />
support of the newsletter.<br />
WITH GRATITUDE TO THE<br />
OVARIAN CANCER RESEARCH<br />
FUND FOR THEIR SUPPORT.<br />
<strong>WOM</strong>AN TO <strong>WOM</strong>AN<br />
The <strong>Mount</strong> <strong>Sinai</strong> <strong>Hospital</strong><br />
Department of Social Work Services<br />
One Gustave L. Levy Place, Box #1252<br />
New York, New York 10029<br />
Tel: 212.241.3793<br />
FROM THE EDITOR<br />
“TO KNOW THE ROAD AHEAD,<br />
ASK THOSE COMING BACK.”*<br />
THIS, OUR THIRD ANNUAL NEWSLETTER, HAS A<br />
double focus: educating women and their families about<br />
gynecologic cancers, their prevention, early detection,<br />
treatment options, and associated quality of life issues; and<br />
exploring how scientists are progressing on new discoveries<br />
VIVIAN PORT<br />
*Chinese Proverb<br />
All materials © <strong>Mount</strong> <strong>Sinai</strong> <strong>Hospital</strong> 2008<br />
for their prevention, treatment, and cure.<br />
In this issue: Dr. Tamara Kalir is featured<br />
in the first in a series of planned interviews<br />
with scientists and doctors at <strong>Mount</strong> <strong>Sinai</strong><br />
involved in cutting-edge research; Dr.<br />
Karen Brown, Director of Cancer Genetic<br />
Counseling, tells us what we can learn<br />
from our genes; our Program Coordinator,<br />
Arden Moulton, introduces our new<br />
educational programs; Dr. Jamal Rahaman<br />
describes the many clinical trials now<br />
offered in the Division of Gynecologic<br />
Oncology; and finally, we show how<br />
Woman to Woman survivor volunteers are<br />
serving as “patient teachers” for secondyear<br />
medical students.<br />
I also want to highlight the work of<br />
Barbara A. Goff, MD, whose 2004 article is<br />
referenced on our back cover. Her<br />
4 | A VOLUNTEER’S EXPERIENCE<br />
“I’ve gained more than I’ve given.”<br />
symptom-screening index is being<br />
evaluated by M. Robyn Andersen, PhD,<br />
and colleagues at the University of<br />
Washington, in a pilot study to assess the<br />
value of using it as a screening tool among<br />
normal-risk women. We look forward<br />
to learning the results. Early detection<br />
remains our best defense.<br />
And, again, I urge everyone to contact<br />
their Senators and Representatives<br />
regarding the Ovarian Cancer Biomarker<br />
Research Act, introduced in Congress<br />
a year ago, and still in committee.<br />
Fortunately, funding through the<br />
Department of Defense Ovarian Cancer<br />
Research Program was increased from 10<br />
to 20 million dollars, which is very<br />
encouraging news. We need more.<br />
6 | DR. KALIR AND <strong>WOM</strong>AN TO <strong>WOM</strong>AN PANEL PRESENTATION<br />
“Patients’ stories are a contribution to the emotional<br />
component of learning.”<br />
8 | COLLABORATIONS: GENETICS COUNSELING AND TESTING<br />
“What we don’t know really can hurt us...”<br />
| THE NEWSLETTER | 1
interview with<br />
JAMAL RAHAMAN, MD<br />
The Division is a major training center for Fellows in<br />
the field of gynecologic oncology and Dr. Rahaman has<br />
been Director of the Gynecologic Oncology Fellowship<br />
Program since 2006.<br />
“In New York, with eleven gynecologic oncologists,<br />
we have the biggest complement of faculty and the largest<br />
volume of patients treated for benign and gynecologic<br />
cancer surgeries,” he explained.<br />
When Dr. Rahaman gave me a demonstration of<br />
the dynamic and interactive electronic platform he<br />
developed for the Division, it became clear that he is<br />
the Division’s “techie” extraordinaire. He explained how<br />
the platform allows anyone in the Division to prescribe<br />
or track a patient’s treatment, onsite or offsite, allowing<br />
for efficiency and continuity of care. Appointments and<br />
schedules can be accessed as well.<br />
“This past year, there has been an increase from<br />
900 cycles of chemotherapy to 1,300-1,500 cycles, an<br />
increase in volume as well as access to clinical trials,”<br />
he said. A system such as this is designed to make it<br />
all run smoothly. Dr. Rahaman is the Director of the<br />
Chemotherapy Infusion Service.<br />
All Attending Physicians are co-investigators of<br />
trials, so any doctor can enroll patients. Supervisory<br />
responsibility for each trial is divided among the<br />
Attendings. Since 2006, when the Division joined the<br />
2 | THE NEWSLETTER |<br />
Dr. Jamal Rahaman, who is an Associate Professor, <strong>Mount</strong><br />
<strong>Sinai</strong> School of Medicine, and an Attending Physician in the<br />
Department of Obstetrics, Gynecology, and Reproductive<br />
Science since 1998, has been instrumental in helping to expand the<br />
Division of Gynecologic Oncology. In his own words, “The Division has<br />
moved from its reputation for top-notch surgeons to a comprehensive<br />
Division that is also a major research center with investigator-initiated<br />
clinical trials [those initiated at <strong>Mount</strong> <strong>Sinai</strong>], national trials through<br />
the Gynecologic Oncology Group [the collaborative national research<br />
organization], and basic science and translational research [scientific<br />
research with possible clinical applications].”<br />
GOG, 15 national clinical trials have opened up at<br />
<strong>Mount</strong> <strong>Sinai</strong>. There are clinical trials for ovarian,<br />
endometrial, and cervical cancers. Studies comparing<br />
different chemotherapy agents in various stages of<br />
disease are being conducted in endometrial and ovarian<br />
cancer. There is a study of pre-operative imaging for<br />
cervical cancer. There is a prospective (before disease)<br />
study of women at increased genetic risk for ovarian<br />
cancer, and another study of the effect of zoledronic acid<br />
to build up bone mineral density for the lumbar spine<br />
in women who have elected risk-reducing surgery to<br />
remove both ovaries. In addition, a tissue biorepository<br />
has been developed to freeze and store human<br />
gynecologic tissue to use in studying causes, diagnosis,<br />
prevention, and treatment of cancer—some to go into<br />
a national bank and some into our own. Dr. Rahaman<br />
is very excited to be the principal investigator of two<br />
GOG trials currently open, which allow women with<br />
ovarian cancer free access to Avastin (Bevacizumab)<br />
in combination with standard chemotherapy for firstline<br />
(GOG 218) and second-line therapy (GOG 213).<br />
<strong>Mount</strong> <strong>Sinai</strong> participated in international clinical<br />
trials that led to development of the HPV vaccine<br />
Gardasil by Merck, which was approved two years ago.<br />
At this time, <strong>Mount</strong> <strong>Sinai</strong> has two investigational studies<br />
about vaccines. Dr. Rahaman, who is co-investigator<br />
of these trials with Dr. Rhoda Sperling—Professor<br />
and Vice Chair of Research for the Department of<br />
Obstetrics, Gynecology, and Reproductive Science, and<br />
Professor of Medicine, Infectious Diseases—explained:<br />
“We are working with both Merck and Glaxo-Smith<br />
Kline. Glaxo-Smith Kline has another vaccine that’s not<br />
approved in the US yet, but will be, hopefully, within the<br />
next two years. Merck is now looking at a new vaccine<br />
with nine strains versus the current four strains. That<br />
trial is open right now.”<br />
There is a tremendous breadth of clinical trials<br />
taking place now, because of the Division’s membership<br />
in the Gynecologic Oncology Group, established<br />
by the efforts of Drs. Dottino and Segna in 2006.<br />
The Division holds a monthly translational research<br />
meeting with scientists and doctors from different<br />
departments, including Breast and<br />
Oncological Sciences, to brainstorm<br />
new projects. The Fellows work in<br />
different labs within Oncological<br />
Sciences. Dr. Rahaman expects that<br />
this exciting research will translate<br />
into cutting-edge trials offered<br />
only here at <strong>Mount</strong> <strong>Sinai</strong>, resulting<br />
in the development of improved<br />
treatments and potential cures.<br />
Many may not know that<br />
Dr. Rahaman had completed a<br />
fellowship in Cardiothoracic and Vascular Surgery at<br />
the Texas Heart Institute in Houston, Texas, with Dr.<br />
Denton Cooley as his mentor, before completing his<br />
Obstetrics and Gynecology Residency and Gynecologic<br />
Oncology Fellowship at <strong>Mount</strong> <strong>Sinai</strong>. Following his<br />
training, Dr. Rahaman left <strong>Mount</strong> <strong>Sinai</strong> to be an<br />
Attending Physician at Williamson ARH <strong>Hospital</strong><br />
in South Williamston, Kentucky, where he became<br />
Chairman of the Department of Obstetrics and<br />
Gynecology. Three years after leaving <strong>Mount</strong> <strong>Sinai</strong>,<br />
he returned to become Director of the Gynecologic<br />
Oncology Service at <strong>Mount</strong> <strong>Sinai</strong> affiliate Elmhurst<br />
There is a tremendous<br />
breadth of clinical trials<br />
taking place now, because<br />
of the Division’s membership<br />
in the Gynecologic Oncology<br />
Group, established by the<br />
efforts of Drs. Dottino and<br />
Segna in 2006.<br />
Medical Center, where he reorganized and developed<br />
an expanded comprehensive department. In 2005, the<br />
service was transferred to one of the Junior Faculty who<br />
was trained in the Division’s fellowship program.<br />
In his many years of service at <strong>Mount</strong> <strong>Sinai</strong>, Dr.<br />
Rahaman has filled leadership, training, and research<br />
roles. However, he has always engaged in a vast amount<br />
of direct clinical work, making him one of the most<br />
experienced gynecologic oncology surgeons in the<br />
country. Dr. Rahaman has also been a member of many<br />
administrative committees within the hospital and<br />
medical school.<br />
He has written numerous publications in national<br />
and international journals, several book chapters in<br />
the field of gynecologic oncology with Dr. Carmel<br />
Cohen, and most recently, a chapter with Dr. William<br />
Bradley, “Pediatric Gynecologic<br />
Cancers,” in Pediatric, Adolescent<br />
and Young Adult Gynecology.<br />
His lectures and oral conference<br />
presentations include many on the<br />
use of laparoscopy. Recently, he<br />
has been credentialed to teach and<br />
perform da Vinci Robotic Surgery<br />
for gynecologic cancers.<br />
In the last six to eight months,<br />
the Division has started to do more<br />
robotic surgery. All surgeons in the<br />
Division are now trained to perform it. Laparoscopic<br />
robotic surgeries are done with endometrial, cervical,<br />
and selected cases of ovarian cancers.<br />
Dr. Rahaman received awards in college, the<br />
University of Cambridge, and medical school,<br />
University of the West Indies, as well as teaching and<br />
peer recognition awards throughout his career.<br />
With all that Dr. Rahaman does, I hope he has<br />
enough time to enjoy his beautiful family: his wife,<br />
Kathleen—a pharmacist—and two children, a daughter<br />
age 11, and a son, age 8. They live in Bergen County<br />
with their two Bichon Frises. —VIVIAN PORT<br />
| THE NEWSLETTER | 3
a volunteer’s<br />
EXPERIENCE<br />
survivors &<br />
VOLUNTEERS<br />
In the spring of 2001 I was the picture of wellness.<br />
I was engaged to be married. I had recently lost<br />
45 pounds and felt better at 40 than I had at 25... but I<br />
had ovarian cancer and didn’t know it.<br />
After experiencing pelvic pain during menstruation<br />
for three months, I was diagnosed with a benign ovarian<br />
cyst. My gynecologist was scheduled to remove it with a<br />
minimally invasive device called a laparoscope, and a<br />
gynecologic oncologist would be available “just in case.”<br />
And then my world came crashing down. When<br />
I went into surgery, I noticed a big clock in the presurgery<br />
suite that said 8:30am. When I awoke, the first<br />
thing I noticed was another big clock in the recovery<br />
room that said 5:30pm. So, I knew I had cancer.<br />
It was ovarian cancer stage one. Since it was caught<br />
early, I didn’t have a complete hysterectomy, but I would<br />
need chemotherapy.<br />
There are no words to describe how it feels to be told<br />
that you have cancer. Shocked and devastated are too<br />
mild. It was as if someone had hit me between the<br />
eyes with a brick, made me get back up, and then<br />
hit me again.<br />
So, my wedding was postponed and I began chemo.<br />
During chemo, I worked pretty much full time.<br />
I surprised my friends and family by not being upset<br />
when my hair started falling out. As a matter of fact, I<br />
had my fiancé Chris shave it off and then we celebrated<br />
with a fun night out at my favorite restaurant. I never<br />
got a wig and pretty much did everything I wanted to<br />
do that summer.<br />
Chemo ended in September, and in November Chris<br />
and I were married. I had a second-look surgery in July<br />
2002, and stage one uterine cancer was found, so I had a<br />
complete hysterectomy.<br />
Well that’s that, I thought. Two stage-one cancers.<br />
Twice blessed. But I couldn’t shake the nagging question<br />
“is that all there is?” I wondered how I could go through<br />
this life-changing incident and just have life go on<br />
normally when it wasn’t normal at all.<br />
One day, I discovered an online ovarian cancer<br />
support group, and the more I connected with those<br />
women in cyberspace, the more at ease I felt about<br />
my cancer diagnosis. It was as if I was being healed from<br />
the inside out.<br />
Then in 2003 I got a call from Arden Moulton about<br />
joining a new program at <strong>Mount</strong> <strong>Sinai</strong> called Woman to<br />
Woman. The very first time I met with a patient, I walked<br />
out of her room and cried. I cried because I felt that this<br />
was what I was meant to gain from my cancer experience.<br />
I took the worst thing that ever happened to me and<br />
began helping other people. I’ve met the most incredible<br />
families over these past five years and I’ve gained more<br />
than I’ve given. Many of the patients have become<br />
friends. Many have died. But in the end, I know I’ve<br />
made a difference in people’s lives and what could be<br />
better than that? —PAMELA HERMAN ELLIOTT<br />
<strong>WOM</strong>AN TO <strong>WOM</strong>AN UPDATE<br />
FROM ARDEN MOULTON,<br />
PROGRAM COORDINATOR<br />
On behalf of the survivor volunteers,<br />
I want to thank all of you who<br />
have generously welcomed us<br />
into your lives. Our mission is<br />
to provide support and information to women<br />
in treatment for gynecologic cancer and their<br />
families. We hope our remarkable volunteers<br />
have helped make your difficult journey easier<br />
to manage.<br />
Allow me to update you on our very<br />
busy year. After undergoing training in<br />
June, Marilyn Aronson, Andrea Licari,<br />
Marie Sanford, and Myrtice Wooten were<br />
welcomed into the program. There are<br />
now 15 Woman to Woman volunteers,<br />
representing a wide demographic, cultural,<br />
and medical cross-section of women, all<br />
ARDEN MOULTON ready and able to provide one-to-one<br />
support to our diverse patient population.<br />
Woman to Woman volunteers, who range in age from<br />
30–65, are all survivors of gynecologic cancer. Eight<br />
volunteers are currently employed: a real estate agent,<br />
an accountant, the head of marketing for a large<br />
fashion conglomerate, a pediatrician, and two mental<br />
health professionals. Two volunteers are Spanishspeaking,<br />
and one of them speaks French as well.<br />
The other seven are retired, with very busy volunteer<br />
and family lives.<br />
In addition to our one-to-one mentoring,<br />
Woman to Woman has added programs to<br />
address our mission to educate and inform.<br />
On November 15th, we partnered with Cancer<br />
Care to host a one-day conference for couples<br />
impacted by gynecologic cancer (of course, there<br />
was information for single women, too). This<br />
unique conference allowed partners to address<br />
issues common to both patient and caregiver.<br />
In the morning session, women interacted with<br />
an expert on self-esteem and body image, while<br />
their partners met with Floyd Allen, a Cancer<br />
Care social worker who specializes in sexuality<br />
and intimacy. Afterwards, couples came together<br />
to learn about nutrition and get some cooking<br />
tips from Esther Trepole, Director of Nutrition<br />
at God’s Love We Deliver. The afternoon session<br />
included information on workplace issues and<br />
caregiving. We hope this conference was an<br />
enjoyable as well as informative experience for<br />
individuals and couples.<br />
Woman to Woman is producing an interactive<br />
Web-based education system for women<br />
in treatment for gynecologic cancer and their<br />
families. Our first program will address the<br />
needs of women with ovarian cancer, followed<br />
by programs on uterine and cervical cancers.<br />
There’s a great need for reliable, accessible information<br />
on gynecologic cancer, its treatment,<br />
and the emotional and practical issues associated<br />
with diagnosis. This user-friendly system will be<br />
a groundbreaking new way to provide accurate,<br />
helpful information to families. Our consultants<br />
on the site are experts in health literacy, Internet<br />
technology, and research. We hope to have it on<br />
the Web within the next six months.<br />
Please contact us with any personal questions<br />
and concerns, or other programming ideas that<br />
you may have. We are here for you.<br />
4 | THE NEWSLETTER |<br />
| THE NEWSLETTER | 5
<strong>WOM</strong>AN TO <strong>WOM</strong>AN VOLUNTEERS<br />
TELL THEIR DIAGNOSIS STORIES TO<br />
SECOND-YEAR MEDICAL STUDENTS<br />
DR. KALIR’S<br />
EXCITING RESEARCH<br />
Dr. Tamara Kalir, Associate Professor of<br />
Pathology and Course Director of “Sexual<br />
and Reproductive Health and Disease,”<br />
had wanted to include a patient panel in her course<br />
to heighten awareness of, and sensitivity to, the<br />
patient’s point of view. As<br />
soon as Woman to Woman<br />
began, Dr. Kalir worked<br />
closely with Arden Moulton,<br />
the Woman to Woman<br />
Program Coordinator, to<br />
organize the details.<br />
In my interview with<br />
Dr. Kalir, she expressed<br />
deep appreciation for all<br />
the survivor volunteers<br />
who participated in the<br />
past five years, including<br />
Valerie Goldfein, the late<br />
Silvana Keegan, Vivian<br />
Port, Joyce Manheimer,<br />
Jane Lury, Joan Brown,<br />
Pamela Herman Elliott,<br />
Nancy Irizarry, and Linda<br />
Newson.<br />
“The student response<br />
has been very positive,” she<br />
said. “Conventional teaching<br />
is intellectual; patients’<br />
stories are a contribution to<br />
the emotional component<br />
of learning. Everybody has<br />
a different story. Each one<br />
is so individual. In the classroom, we present<br />
standard medical teaching and the Woman to<br />
Woman panel follows. This allows us to drive the<br />
intellectual points home emotionally.”<br />
Survivor volunteers tell their stories so that<br />
students can hear firsthand not only how difficult<br />
6 | THE NEWSLETTER |<br />
(Left To Right) Nancy Irizarry, Pamela Herman Elliott,<br />
Joyce Manheimer, and Dr. Tamara Kalir.<br />
Nancy Irizarry, Survivor Volunteer, speaking with<br />
a medical student after panel presentation.<br />
it is to confront a cancer diagnosis, but also, in<br />
the case of ovarian cancer, how difficult it can be to<br />
diagnose it correctly and quickly.<br />
“Because ovarian cancer is such a difficult<br />
clinical diagnosis, it is important to consider it in<br />
the differential diagnosis,”<br />
Dr. Kalir said. “A delayed<br />
diagnosis may negatively<br />
impact prognosis.”<br />
Many in the class will<br />
become primary care physicians,<br />
and we hope that<br />
our personal stories will<br />
remain with the students.<br />
The students were told<br />
about the survivor volunteers’<br />
symptoms and their<br />
experiences with missed<br />
diagnoses and insensitive<br />
doctors. Medical students<br />
heard about our feelings<br />
of confusion and fear,<br />
sadness and anger. One of<br />
the women related how<br />
she was engaged to be<br />
married when diagnosed<br />
at age 36. Another<br />
described how she had<br />
just finished chemotherapy<br />
for breast cancer<br />
when she was diagnosed<br />
with both uterine and<br />
early-stage ovarian cancer.<br />
Another volunteer told of gastrointestinal problems<br />
that her doctors did not recognize as symptoms of<br />
ovarian cancer. Yet another told how she was given<br />
her diagnosis abruptly and without compassion. Dr.<br />
Kalir sums it up perfectly when she says, “We want<br />
them to be humanitarians as well as good scientists.”<br />
Dr. Kalir herself is an excellent role model for the<br />
students. She’s also an excellent teacher. I know that<br />
because she explained so clearly to me the exciting and<br />
original ovarian cancer research she’s working on with<br />
Drs. Peter Dottino, Stave Kohtz, and Yayoi Kinoshita.<br />
Funded by the Gynecologic Cancer Research Fund in<br />
the Division of Gynecologic Oncology, the research<br />
is designed to help doctors better understand what<br />
causes ovarian cancer at the molecular biology level<br />
and to discover new therapies to offer patients. What is<br />
so innovative is that they are focusing on “the nuclear<br />
membrane pore complex.”<br />
The pore is a multiprotein structure that forms<br />
a hole in the double-layer membrane of the nucleus<br />
of a cell (all body tissue is made up of hundreds<br />
of thousands of cells, and the nucleus is like the<br />
command center for the cell). The pore is important<br />
in information exchange between the nucleus and<br />
the rest of the cell (the cytoplasm). The pore can be<br />
considered a gateway of information exchange.<br />
Because of the role it plays, it seems that it should be<br />
Schematic diagram of a nuclear pore, showing the<br />
doughnut shape with pore (opening) in the center.<br />
Nuclear pore seen with an electron<br />
microscope, magnified 200,000 times.<br />
critical in regulating cell growth in the development of<br />
cancer, since cancer is a dysregulation of growth. The<br />
hypothesis is that in cancer, the pore might not be<br />
bringing correct information to the cell.<br />
“Recently, we discovered that the pore appears to<br />
be a critical regulator of cell growth in the G1 phase<br />
of the cell cycle,” Dr. Kalir explained. “We are looking<br />
at one of the proteins within the pore complex<br />
called NUP 62 that sits in the center. It holds the pore<br />
intact.” Dr. Kinoshita has developed ovarian cancer<br />
cell lines that are deficient in this protein and their<br />
pores are larger. These cells grow differently than<br />
other cancer cells.<br />
“This type of research holds promise for developing<br />
new drug therapies for ovarian cancer,” explained<br />
Dr. Kalir. “For example, if one protein in the pore<br />
complex is either abnormal or missing, we might be<br />
able to replace that protein.”<br />
Since there are over 200 proteins in the pore, there<br />
are many possible approaches to try.<br />
Let’s hope that the initial discovery involving<br />
NUP 62 will provide the key to unlocking very<br />
important information for everyone awaiting a<br />
breakthrough in ovarian cancer research. Dr. Kalir<br />
and her team may have made a promising start<br />
toward that goal. —VIVIAN PORT<br />
| THE NEWSLETTER | 7
collaborations<br />
GENETICS COUNSELING<br />
AND TESTING<br />
INTERVIEW WITH<br />
KAREN BROWN, MS, CGC<br />
One of the goals of our newsletter and Woman<br />
to Woman is to educate women about their<br />
health and ways to reduce the risk of disease.<br />
One option for women to educate themselves<br />
is to see a genetic counselor. But I have met many women<br />
who express reluctance to do that. I understand because<br />
I was apprehensive myself. What would I learn that would<br />
affect my future or my children’s future? However, I put my<br />
fears aside in order to learn as much as I could that might<br />
help our family. What we don’t know really can hurt us,<br />
especially when it comes to hereditary cancers.<br />
Most cancers are not hereditary. In fact, only 10% of<br />
ovarian cancer cases and 5–10% of breast cancer cases<br />
are linked to an inherited predisposition. In some<br />
families, the tendency to develop these cancers is due<br />
to an inherited change, or genetic mutation, in what<br />
are called the BRCA1 or BRCA2 genes (BRCA stands<br />
for Breast Cancer). The genetic test for mutations in<br />
these genes requires drawing a small sample of blood<br />
from the arm. But before any testing is done, a certified<br />
genetic counselor discusses the pattern of cancer in the<br />
family and whether testing is appropriate to consider.<br />
I met with Karen Brown, MS, CGC, Director<br />
of Cancer Genetic Counseling in the Department<br />
of Genetics and Genomic Sciences at <strong>Mount</strong> <strong>Sinai</strong>,<br />
who was generous with her time and very helpful in<br />
explaining a complex subject. “People need a certain<br />
comfort level to do genetic counseling and testing,” she<br />
said. “Genetic counseling is an educational resource. It<br />
is a process to assist people in deciding whether genetic<br />
testing is important for them.”<br />
8 | THE NEWSLETTER |<br />
KAREN BROWN, MS, CGC<br />
Director of Cancer Genetic Counseling<br />
I asked Ms. Brown who should<br />
consider BRCA testing.<br />
Anyone who has had ovarian<br />
cancer, regardless of family<br />
history<br />
Any Ashkenazi Jewish woman (Jews of<br />
Eastern European or German origin) who has<br />
had breast cancer<br />
Any woman, regardless of ethnicity, diagnosed<br />
at age 50 or younger with breast cancer or with<br />
two breast cancers at any age<br />
Anyone who has a strong family history of breast<br />
and/or ovarian cancer<br />
Any man with breast cancer<br />
Ms. Brown further explained that it is good to<br />
start testing with the person in the family who has<br />
had the cancer.<br />
She told me that the lifetime risk of developing<br />
ovarian cancer for the general population is 1–2% or<br />
1 in 70. Among Ashkenazi Jews, 30–40% of ovarian<br />
cancer is attributed to inherited mutations in the<br />
BRCA1 and BRCA2 genes. In non-Ashkenazi women,<br />
10% of ovarian cancer is due to a BRCA mutation. It<br />
is estimated that in the US general population, 1 in<br />
800 individuals has a BRCA mutation compared to<br />
approximately 1 in 40 Ashkenazi Jewish individuals.<br />
The likelihood that a mutation is present in a family is<br />
increased by the occurrence of breast and /or ovarian<br />
cancer in that family.<br />
Risks associated with BRCA1 or BRCA2 are<br />
somewhat different from each other, although both<br />
predispose to breast and ovarian cancer. It is important<br />
to understand that not all women who inherit an<br />
altered gene will develop breast or<br />
ovarian cancer. Testing only provides<br />
information about risk; it does not<br />
indicate whether or when cancer will<br />
actually develop.<br />
BRCA1 and BRCA2 mutations<br />
confer up to an 85% lifetime risk of<br />
developing breast cancer, compared<br />
to the general population risk of<br />
12%. The lifetime risk of developing<br />
ovarian cancer for BRCA1 carriers is<br />
up to 60%, compared to the general<br />
population risk of 1–2%. A BRCA2<br />
mutation confers up to a 27% lifetime<br />
risk for ovarian cancer.<br />
BRCA mutations are associated<br />
with a somewhat increased risk for<br />
certain other cancers as well, including<br />
pancreatic cancer in men and<br />
women as well as prostate and breast<br />
cancer in men.<br />
For women with a BRCA<br />
mutation, current recommendations<br />
include frequent screening for<br />
breast cancer with self and clinical<br />
examinations, mammograms, and<br />
breast MRI. For ovarian cancer,<br />
screening with transvaginal ultra<br />
sound and CA-125 measurement is available, but not<br />
highly successful in detecting it at an early stage when<br />
it is most curable. Therefore, to significantly reduce the<br />
risk of ovarian cancer, women with a BRCA mutation<br />
are advised to have their ovaries removed by age 35–40,<br />
or once childbearing is complete. Because of the high<br />
risk of breast cancer with BRCA mutations, some<br />
women choose prophylactic mastectomy to reduce this<br />
risk.<br />
For individuals with a strong family history<br />
of cancer, without detection of a BRCA mutation,<br />
preventive guidelines need to be discussed with one’s<br />
doctor. Recommendations may also include more<br />
ANDREA LICARI<br />
SURVIVOR VOLUNTEER<br />
Woman to Woman BRCA Stories<br />
“It was a no-brainer,” is how Andi described her decision<br />
to have a prophylactic mastectomy, after learning she was<br />
BRCA positive. Her mother’s family was Jewish, originally<br />
from Russia. Andrea had been treated for ovarian cancer,<br />
her mother and grandmother had breast cancer, and<br />
so she was not surprised at her test results. However,<br />
her husband was.<br />
She said “You only have a problem when you have<br />
choices. I had no choice, so there wasn’t a problem.” She<br />
thought, “I have to take the chance of being aggressive<br />
against cancer because it’s the only way to secure the<br />
future of my young children and my husband.”<br />
Andrea’s husband lost his first wife young to cancer.<br />
She did not want to take a chance that this might<br />
happen again.<br />
Her husband became very supportive of her decision<br />
and she feels that having a very positive husband is critical.<br />
Her reconstructive surgery was so good, she said, that<br />
you cannot detect any difference. She feels lucky about<br />
the cosmetic results, and most of all, for having peace<br />
of mind.<br />
| THE NEWSLETTER | 9
frequent screenings or screenings to begin at an earlier<br />
age than for the general population.<br />
Ms. Brown indicated that women do not have to<br />
be patients at <strong>Mount</strong> <strong>Sinai</strong> to utilize the services of the<br />
Genetics Department. Physicians may refer patients<br />
for genetic counseling, but many come on their own<br />
initiative. This confirms what I have learned talking to<br />
many women during the years since my diagnosis.<br />
In addition to genetic testing for BRCA mutations,<br />
some women with endometrial (uterine) or<br />
ovarian cancer are offered genetic testing for Lynch<br />
Syndrome, usually referred to as HNPCC (Hereditary<br />
Nonpolyposis Colorectal Cancer). HNPCC is a<br />
condition in which a tendency to develop colorectal<br />
and certain other cancers is inherited (Nonpolyposis<br />
means that the colorectal cancer can occur when<br />
only a small number of polyps are present in the<br />
colorectal region or when polyps are not present<br />
at all). HNPCC accounts for 2–3% of all colorectal<br />
cancer; however, polyps in these individuals can<br />
ROBIN ZAREL<br />
ADVISORY BOARD MEMBER<br />
Woman to Woman BRCA Stories<br />
Robin was 36 when she had her first breast cancer in<br />
1991, and 39 when diagnosed with ovarian cancer.<br />
A few years after her treatment for ovarian cancer,<br />
she happened to receive a brochure in the mail from<br />
the Strang Cancer Center about genetic testing. She<br />
decided to look into it. Robin had no family history of<br />
either cancer. “I wanted to know why all this happened<br />
to me,” she explained.<br />
Robin tested positive but did not elect to have a<br />
prophylactic mastectomy at that time. However, when<br />
she developed a second primary cancer in the same<br />
breast in 2004, she elected to have a double mastectomy.<br />
It has given her peace of mind. And she’s quite confident<br />
about her ovarian cancer. Although she was diagnosed<br />
in Stage III, she has survived 15 years.<br />
become cancerous more quickly than in the general<br />
population. There is up to an 80% chance that a<br />
man or woman with HNPCC will develop colorectal<br />
cancer over his or her lifetime and up to a 60%<br />
chance that a woman with HNPCC will develop<br />
uterine cancer. Additionally, the lifetime risk of<br />
ovarian cancer is approximately 10% for women<br />
with HNPCC. Other cancers linked to HNPCC<br />
are those of the stomach, small intestine, bile duct<br />
and gallbladder, urinary tract, and pancreas.<br />
Three of the genes that account for the majority of<br />
HNPCC (MLH1, MSH2, and MSH6) can be analyzed<br />
through a blood test. Testing is considered according<br />
to the pattern of cancer in a family. Families with<br />
three or more cases of HNPCC-related cancers<br />
in two or more generations, with at least one<br />
affected family member diagnosed under the<br />
age of 50, are considered to have HNPCC. Testing<br />
is also appropriate for individuals diagnosed with<br />
two HNPCC-associated cancers or colorectal or<br />
uterine cancer under the age of 50.<br />
Unlike the BRCA mutations, HNPCC<br />
is not more common among people of<br />
Jewish descent.<br />
Knowledge of this condition can<br />
help determine a need for frequent<br />
cancer screenings, preferably starting at<br />
an early age. Genetic testing, however,<br />
is not available for all HNPCC-causing<br />
genes. In addition, in some high-risk<br />
families, genes other than those associated<br />
with HNPCC may account for the<br />
increased colorectal cancer risk. Therefore,<br />
in high-risk families, where no<br />
mutation has been detected, individuals<br />
need to consult with their doctors<br />
to determine the best screening practices<br />
to follow. For women with a personal<br />
and/or family history suggestive of HN-<br />
PCC, besides an annual gynecological<br />
exam and early, frequent colonoscopies,<br />
doctors may recommend pelvic ultrasounds<br />
and/or uterine biopsies to screen<br />
for cancer of the uterus or ovaries.<br />
Both HNPCC and BRCA mutations<br />
are inherited in an autosomal<br />
dominant pattern. That means that each<br />
time a person has a child, there is a 50%<br />
(or 1 in 2) chance that the child will inherit<br />
the mutation or condition. Children<br />
who do not inherit it cannot pass it on<br />
to their own children; it does not “skip<br />
generations.” Again, not everyone who<br />
inherits the BRCA mutation or HNPCC<br />
will develop cancer. Siblings of a person<br />
with HNPCC or a BRCA mutation have a<br />
50% chance of having inherited it.<br />
Many insurance companies cover<br />
the cost of testing and most people<br />
use their insurance, Ms. Brown said. Some people<br />
prefer to pay out-of-pocket for genetic testing<br />
because they worry that the information might be<br />
used against them if it is included in their medical<br />
records. However, federal and state laws are in<br />
place to help protect individuals from genetic<br />
discrimination. Genetic test results may not be used<br />
by a health insurance company or employer when<br />
making decisions about coverage or employment.<br />
Now, to summarize the reasons for considering<br />
undergoing any type of genetic testing: Many<br />
women ask, why be tested if they already have<br />
developed cancer? Ms. Brown explains that it helps<br />
people make better and more informed medical<br />
management decisions. Gaining knowledge about<br />
genetic risk allows one to increase surveillance<br />
(medical observation) and take preventive measures.<br />
JOYCE MANHEIMER<br />
SURVIVOR VOLUNTEER<br />
Woman to Woman BRCA Stories<br />
“I wanted more information because I had three cancers:<br />
breast, uterine, and early-stage ovarian, within two years.<br />
I wasn’t reluctant to have the tests. If they are available<br />
to me, I would be foolish not to take advantage of them,”<br />
Joyce told me.<br />
She had the BRCA and HNPCC testing. Joyce learned<br />
that she tested negative but no longer thinks about how<br />
all this happened to her. Her mother had three different<br />
cancers and did not dwell on it after she was treated. Joyce<br />
adopted her mother’s attitude; that is, “I am a healthy<br />
individual, I was treated, and I move forward.”<br />
In addition, pinpointing an inherited cause of cancer<br />
can allow informative testing for other relatives.<br />
Testing has the potential to reduce uncertainty and<br />
anxiety about who in the family is at increased<br />
risk for cancer.<br />
One purpose of Woman to Woman is to inform and<br />
educate in order to empower women.<br />
It has been my experience that discussion of<br />
genetic counseling and/or testing is feared and<br />
avoided when it should be understood and utilized to<br />
save our lives and those of our family members. Just as<br />
we need to know symptoms, we need to understand<br />
newly discovered information. Genetic counselors,<br />
along with our doctors, can teach us and help us<br />
to appreciate whatever knowledge does exist about<br />
our illnesses. —VIVIAN PORT<br />
| THE NEWSLETTER | 11<br />
(Left to Right) Arden Moulton, LMSW, and Alison Snow, LCSW, Recipients of the<br />
Susan Blumenfield Award for Clinical Excellence; Maura Surnamer, President of<br />
the Auxiliary Board; and Dr. Susan Bernstein, Director of Social Work Services.<br />
ARDEN MOULTON, LMSW, <strong>WOM</strong>AN TO <strong>WOM</strong>AN<br />
PROGRAM COORDINATOR, RECEIVES ONE OF THE<br />
TWO DR. SUSAN BLUMENFIELD AWARDS FOR<br />
CLINICAL EXCELLENCE<br />
At the Department of Social Work Services Grand Rounds on March 11 of this year,<br />
our dear Arden received a very special award. Maura Surnamer, President of the<br />
Auxiliary Board, honored her with one of two Dr. Susan Blumenfield Awards, while<br />
Alison Snow, LCSW, an inpatient oncology social worker, received the other.<br />
Ms. Surnamer read comments written by those who nominated both Arden and<br />
Alison. She noted that Alison, who has been at <strong>Mount</strong> <strong>Sinai</strong> since 2004, has established<br />
herself as “an exceptional patient advocate” who is dedicated to oncology services and<br />
works to insure their prominence at <strong>Mount</strong> <strong>Sinai</strong>. “Alison is the real thing,” she said,<br />
“caring, compassionate and self-motivated.” Woman to Woman survivor volunteers<br />
know personally how important a caring, compassionate, and effective social worker is<br />
at this difficult time. Congratulations from all of the survivor volunteers, Alison.<br />
Arden was described as the creative force behind Woman to Woman. As one<br />
colleague noted, “Arden took the vision of a peer-to-peer support initiative and made<br />
it flourish.” Another said that Arden has built Woman to Woman into a prototype for<br />
peer-to-peer support programs nationwide.<br />
We volunteers feel so strongly that she makes the work we do possible, on a very<br />
personal level. One volunteer said that “Arden literally helped save my soul, enabling me<br />
to craft a meaningful life after cancer…She has guided me with a firm but gentle hand<br />
toward the realization that by helping other women, I am helping myself.”<br />
When I meet with patients, their faces light up when Arden’s name is mentioned,<br />
even after surgery or during chemotherapy. It is no wonder that the Auxiliary Board<br />
selected our very own Arden to receive the award in its inaugural year. All the Woman<br />
to Woman survivor volunteers are very thankful for her exceptional personality and<br />
professional leadership. Congratulations, Arden! —VIVIAN PORT