Final Program - Canadian Society of Hospital Pharmacists
Final Program - Canadian Society of Hospital Pharmacists
Final Program - Canadian Society of Hospital Pharmacists
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
ANNUAL PROFESSIONAL PRACTICE CONFERENCE<br />
THE LARGEST PHARMACY CONFERENCE IN CANADA<br />
FEBRUARY 4-8, 2012<br />
CONFÉRENCE ANNUELLE SUR LA PRATIQUE PROFESSIONNELLE<br />
LE PLUS GRAND CONGRÈS EN PHARMACIE AU CANADA<br />
4-8 FÉVRIER 2012<br />
<strong>Final</strong> <strong>Program</strong><br />
<strong>Program</strong>me final<br />
The Sheraton Centre Toronto Hotel<br />
123 Queen Street West<br />
Toronto, ON
What is CSHP 2015?<br />
● Vision <strong>of</strong> pharmacy practice excellence in the year 2015<br />
● Strategic objective <strong>of</strong> CSHP’s Vision 2014 which aims to improve<br />
patient medication outcomes and safety by advancing practice<br />
excellence<br />
● A quality care initiative<br />
● A project aiming to answer the questions… “What would make the<br />
most difference to our patients?” and “What will convey the positive<br />
contributions <strong>of</strong> the pharmacist?”<br />
● Six specific goals that will guide practitioners towards the CSHP vision<br />
● Sub-objectives that include measurable targets with established<br />
baselines used to monitor progress, which can be reviewed and<br />
revised as practice goals change<br />
Qu’est-ce que le projet SCPH 2015?<br />
● Une vision de l’excellence en pratique pharmaceutique en l’an 2015<br />
● Un objectif stratégique de la Vision 2014 de la SCPH, lequel s’applique<br />
à améliorer les résultats et la sécurité de la pharmacothérapie des<br />
patients en faisant avancer l’excellence en pratique.<br />
● Un projet axé sur la qualité des soins<br />
● Un projet qui vise à répondre aux questions suivantes : « Qu’est-ce qui<br />
serait le plus pr<strong>of</strong>itable pour nos patients? Qu'est ce qui permettrait de<br />
communiquer les contributions positives du pharmacien? »<br />
● Six buts précis qui aideront les pharmaciens à concrétiser la vision de la<br />
SCPH<br />
● Des objectifs sous-jacents qui sont assortis de cibles mesurables nous<br />
permettant d'établir un point de référence et de suivre les progrès, et<br />
qui pourront être réexaminés et modifiés à mesure que les objectifs et<br />
les lignes directrices de la pratique changent<br />
CSHP<br />
Targeting Excellence in Pharmacy Practice<br />
Goals<br />
1Increase 2Increase 3Increase 4<br />
Increase<br />
5Increase 6Increase the extent to which pharmacists help individual hospital<br />
inpatients achieve the best use <strong>of</strong> medications<br />
the extent to which pharmacists help individual<br />
non-hospitalized patients achieve the best use <strong>of</strong> medications<br />
the extent to which hospital and related healthcare setting<br />
pharmacists actively apply evidence-based methods to the<br />
improvement <strong>of</strong> medication therapy<br />
the extent to which pharmacy departments in hospitals and<br />
related healthcare settings have a significant role in improving the<br />
safety <strong>of</strong> medication use<br />
the extent to which hospitals and related healthcare settings<br />
apply technology effectively to improve the safety <strong>of</strong> medication use<br />
the extent to which pharmacy departments in hospitals and<br />
related healthcare settings engage in public health initiatives on<br />
behalf <strong>of</strong> their communities<br />
To get started on CSHP 2015 now, go to CSHP’s website at www.cshp.ca.<br />
There you will find the complete list <strong>of</strong> goals and objectives, a<br />
self-assessment tool, PowerPoint presentations and more.<br />
*CSHP 2015 was adapted with permission from the ASHP 2015 Initiative.<br />
SCPH<br />
Point de mire sur l’excellence en pratique pharmaceutique<br />
Buts<br />
1<br />
Accroître<br />
le degré d'intervention des pharmaciens auprès de<br />
chaque patient hospitalisé afin d'assurer l'utilisation optimale des<br />
médicaments.<br />
2Accroître le degré d'intervention des pharmaciens auprès de la<br />
clientèle non hospitalisée afin d'assurer une utilisation optimale des<br />
médicaments.<br />
3Étendre l'application du principe des décisions fondées sur les<br />
preuves à la pratique clinique quotidienne des pharmaciens des<br />
établissements de santé dans le but d'améliorer la pharmacothérapie<br />
4Accroître le rôle joué par les départements de pharmacie des<br />
établissements de santé dans l'amélioration de l'utilisation sécuritaire<br />
des médicaments.<br />
5Étendre l'application efficace des technologies dans les<br />
départements de pharmacie des établissements de santé pour<br />
améliorer l'utilisation sécuritaire des médicaments.<br />
6Accroître le degré d'intervention des départements de pharmacie<br />
des établissements de santé dans la mise en oeuvre d'initiatives de<br />
santé publique.<br />
Pour vous engager dès maintenant dans le projet SCPH 2015, visitez le<br />
site Web de la SCPH au www.cshp.ca. Vous y trouverez une liste<br />
complète des buts et des objectifs du projet, un outil d’autoévaluation,<br />
des présentations PowerPoint et d'autres renseignements.<br />
*Le projet SCPH 2015 est une adaptation approuvée de l’ASHP 2015 Initiative.<br />
www.cshp.ca
4<br />
Dear Colleague,<br />
On behalf <strong>of</strong> the Officers, Council and staff <strong>of</strong> the <strong>Canadian</strong> <strong>Society</strong> <strong>of</strong><br />
<strong>Hospital</strong> <strong>Pharmacists</strong> (CSHP), it is our pleasure to welcome you to CSHP’s<br />
43rd Annual Pr<strong>of</strong>essional Practice Conference.<br />
Over the last 10 months, CSHP’s Educational Services Committee has worked<br />
hard to assemble an impressive faculty <strong>of</strong> pharmacy specialists and develop a<br />
program <strong>of</strong> exceptional educational value with topics covering a wide range<br />
<strong>of</strong> specialties, management issues and pharmacy practice-related challenges.<br />
This conference is designed to maximize your opportunities for pr<strong>of</strong>essional<br />
development, networking and socializing with practitioners from across the<br />
country. It is our hope that you are able to take full advantage <strong>of</strong> the 2012<br />
<strong>of</strong>ferings – and enjoy yourself in the process.<br />
At anytime throughout the conference, the Officers and staff <strong>of</strong> CSHP are<br />
available to you. Please let us know if we can answer any <strong>of</strong> your questions,<br />
address any <strong>of</strong> your concerns or be <strong>of</strong> assistance in any way. Be sure to take<br />
a few minutes and stop by the CSHP booth during the exhibits program and<br />
say hello.<br />
We look forward to welcoming each <strong>of</strong> you to another spectacular<br />
conference.<br />
Thank you for your ongoing support <strong>of</strong> CSHP!<br />
Janice Munroe<br />
BScPhm<br />
CSHP President<br />
Myrella Roy<br />
BScPhm, PharmD, FCCP<br />
Executive Director
5<br />
Chères (Chers) collègues,<br />
Au nom de la Direction, du Conseil et du personnel de la Société canadienne<br />
des pharmaciens d’hôpitaux (SCPH), nous avons le plaisir de vous souhaiter la<br />
bienvenue à la 43e Conférence annuelle sur la pratique pr<strong>of</strong>essionnelle de la<br />
SCPH.<br />
Au cours des dix derniers mois, le Comité des services éducatifs de la SCPH<br />
s’est affairé à rassembler un groupe impressionnant de conférenciers<br />
spécialisés en pharmacie et à vous préparer un programme d’une valeur<br />
éducative exceptionnelle avec des sujets touchant un large éventail de<br />
spécialités, de questions relatives à la gestion et de défis posés à la pratique<br />
pharmaceutique. Ce congrès est destiné à maximiser les possibilités de<br />
perfectionnement pr<strong>of</strong>essionnel, de réseautage et de rencontre avec d’autres<br />
praticiens de toutes les régions du pays. Nous espérons que vous pourrez tirer<br />
pleinement pr<strong>of</strong>it de ce que nous vous <strong>of</strong>frons en 2012 – tout en vous<br />
divertissant.<br />
Nous vous rappelons qu’au cours du congrès, la Direction et le personnel de<br />
la SCPH seront à votre entière disposition. Nous ferons tout en notre pouvoir<br />
pour répondre à vos questions, discuter des sujets qui vous préoccupent et<br />
vous aider au besoin de quelques manières que ce soit. Pendant le salon des<br />
exposants, assurez-vous d’effectuer un arrêt au stand de la SCPH afin de<br />
nous saluer!<br />
Nous sommes impatients de vous accueillir à cet autre congrès exceptionnel<br />
et vous remercions de votre appui soutenu à la SCPH.<br />
Janice Munroe<br />
Myrella Roy<br />
B. Sc. Phm. B. Sc. Phm., Pharm. D., FCCP<br />
Présidente de la SCPH<br />
Directrice générale
6<br />
Table <strong>of</strong> Contents<br />
Table des matières<br />
Executive, Council and Staff<br />
Bureau de direction, Conseil et Personnel<br />
Executive Committee Bureau de direction 7<br />
Council Conseil 7<br />
CSHP Staff Personnel de la SCPH 7<br />
With Thanks<br />
Remerciements<br />
CSHP Industry Corporate Members Entreprises membres du secteur de l’industrie 8<br />
CSHP <strong>Hospital</strong> Corporate Members Entreprises membres du secteur hospitalier 8<br />
CSHP Sponsors 2011 Commanditaires de la SCPH en 2011 9<br />
Awards <strong>Program</strong><br />
<strong>Program</strong>me des prix<br />
Distinguished Service Award Prix pour service distingué 10<br />
Isabel E. Stauffer Meritorious Service Award Prix Isabel E. Stauffer pour service méritoire 10<br />
New <strong>Hospital</strong> Pharmacy Practitioner Award Prix du nouveau praticien en pharmacie hospitalière 10<br />
<strong>Hospital</strong> Pharmacy Student Award Prix de l’étudiant en pharmacie hospitalière 10<br />
2011/2012 Awards Committee Comité des prix 2011-2012 11<br />
2011/2012 Awards <strong>Program</strong> <strong>Program</strong>me des prix 2011-2012 11<br />
Tribute to Appraisers Hommage aux évaluateurs 11<br />
Conference Information<br />
Information sur la conférence<br />
Upcoming Events Événements à venir 12<br />
Satellite Symposiums Symposiums satellites 12<br />
CSHP Educational Services Committee Comité des services éducatifs 13<br />
<strong>Program</strong><br />
<strong>Program</strong>me<br />
<strong>Program</strong> <strong>of</strong> Events <strong>Program</strong>me des événements 14<br />
Speakers Abstracts Résumés des conférenciers 22<br />
SES 2012 Call for Abstracts Demande de résumés pour les SÉÉ 2012 41<br />
Oral Presentations Présentations orales 44<br />
Poster Abstracts Résumés des affiches 46<br />
Poster Abstract Reviewers Réviseurs des présentations par affiches 68<br />
CSHP Fellows Associés de la SCPH 69<br />
Faculty Conférenciers 72<br />
Exhibitor List Liste des exposants 73
7<br />
Executive Committee • Bureau de direction<br />
President<br />
Présidente<br />
Janice Munroe<br />
Fraser Health<br />
Langley, BC<br />
President Elect<br />
Président designé<br />
Doug Sellinger<br />
Regina Qu’Appelle Health Region<br />
Pasqua <strong>Hospital</strong> Site<br />
Regina, SK<br />
Past President<br />
Président sortant<br />
Neil MacKinnon<br />
University <strong>of</strong> Arizona<br />
Tucson, AZ<br />
Director <strong>of</strong> Finance<br />
Directeur des finances<br />
Patrick Fitch<br />
Victoria General <strong>Hospital</strong><br />
Winnipeg, MB<br />
Executive Director<br />
Directrice générale<br />
Myrella Roy<br />
<strong>Canadian</strong> <strong>Society</strong> <strong>of</strong> <strong>Hospital</strong><br />
<strong>Pharmacists</strong><br />
Société canadienne des<br />
pharmaciens d’hôpitaux<br />
Ottawa, ON<br />
Council • Conseil<br />
British Columbia<br />
Colombie-Britannique<br />
Bruce Millin<br />
Fraser Health Authority<br />
Langley, BC<br />
Manitoba<br />
Albert Eros<br />
Winnipeg Regional Health<br />
Authority<br />
Winnipeg, MB<br />
Quebec<br />
Québec<br />
Diem Vo<br />
Hôpital Pierre-Boucher<br />
Longueuil, QC<br />
Prince Edward Island<br />
Île-du-Prince-Édouard<br />
Amy Cheverie<br />
Kings County Memorial <strong>Hospital</strong><br />
Montague, PE<br />
Alberta<br />
Sheri Koshman<br />
University <strong>of</strong> Alberta<br />
Calgary, AB<br />
Saskatchewan<br />
Donald Kuntz<br />
Regina Qu’Appelle Health Region<br />
Regina, SK<br />
Ontario – Senior/Principale<br />
Rita Dhami<br />
London Health Sciences Centre<br />
London, ON<br />
Ontario – Junior/Débutant<br />
Olavo Fernandes<br />
University Health Network<br />
Toronto, ON<br />
New Brunswick<br />
Nouveau-Brunswick<br />
Faith Louis<br />
Horizon Health Network<br />
Fredericton, NB<br />
Nova Scotia<br />
Nouvelle-Écosse<br />
Theresa Hurley<br />
QEII Health Sciences Centre<br />
Halifax, NS<br />
Newfoundland and Labrador<br />
Terre-Neuve-et-Labrador<br />
Tiffany Lee<br />
General <strong>Hospital</strong>,<br />
Health Sciences Centre<br />
St. John’s, NL<br />
Student Delegate<br />
Déléguée des étudiants<br />
Megan Riordon<br />
Dalhousie University<br />
Halifax, NS<br />
CSHP Staff • Personnel de la SCPH<br />
Executive Director<br />
Directrice générale<br />
Myrella Roy<br />
Operations Manager<br />
Gérante des opérations<br />
Laurie Frid<br />
Coordinator, Pr<strong>of</strong>essional &<br />
Membership Affairs<br />
Coordonnatrice, Affaires<br />
pr<strong>of</strong>essionnelles et service<br />
aux membres<br />
Cathy Lyder<br />
Executive Assistant<br />
Adjointe de direction<br />
Rosemary Pantalone<br />
Conference & PSN<br />
Administrator<br />
Agente des congrès et des RSP<br />
Desarae Davidson<br />
Membership & Awards<br />
Administrator (on leave)<br />
Agente du service aux<br />
membres et des prix<br />
(en congé)<br />
Robyn Rockwell<br />
Interim Membership & Awards<br />
Administrator<br />
Agente par intérim du service<br />
aux membres et des prix<br />
Amanda Cuirrier<br />
CHPRB & Advocacy<br />
Administrator<br />
Agente du CCRPH et de la<br />
valorisation<br />
Gloria Day<br />
Finance Administrator<br />
Agente des finances<br />
Anna Dudek<br />
Publications Administrator<br />
Agente des publications<br />
Colleen Drake<br />
Web Administrator<br />
Agente du Web<br />
Olga Chrzanowska<br />
Ontario Branch & Board <strong>of</strong><br />
Fellows Administrator<br />
Agente de la section de<br />
l’Ontario et du Conseil des<br />
associés<br />
Susan Korporal<br />
CSHP 2015 Project Coordinator<br />
Coordonnatrice du projet<br />
SCPH 2015<br />
Carolyn Bornstein<br />
CSHP Research and Education<br />
Foundation Administrator<br />
Agente de la Fondation pour<br />
la recherche et l’éducation de<br />
la SCPH<br />
Janet Lett
8<br />
2011-2012 CSHP<br />
Industry Corporate Members<br />
(At time <strong>of</strong> printing)<br />
2011-2012 Entreprises membres du<br />
secteur de l’industrie<br />
(au moment de l’impression)<br />
2010-2011 CSHP<br />
<strong>Hospital</strong> Corporate Members<br />
(At time <strong>of</strong> printing)<br />
2010-2011 Entreprises membres du<br />
secteur hospitalier<br />
(au moment de l’impression)<br />
Amgen Canada Inc.<br />
AstraZeneca Canada Inc.<br />
Bayer Inc.<br />
<strong>Canadian</strong> Pharmaceutical Distribution Network<br />
Eli Lilly Canada Inc.<br />
Fresenius Kabi Canada<br />
Galenova Inc.<br />
Healthmark Ltd.<br />
Hospira Healthcare Corporation<br />
LIfeScan Canada<br />
Alberta Health Services<br />
Horizon Health Network<br />
Lakeridge Health Network<br />
London Health Sciences Centre<br />
Medbuy Corporation<br />
Northern Health<br />
St. Michael’s <strong>Hospital</strong><br />
The Royal Victoria <strong>Hospital</strong> <strong>of</strong> Barrie<br />
University Health Network<br />
McKesson Canada Corporation<br />
Merck Canada Inc.<br />
Omega Laboratories Ltd.<br />
Pendopharm, a Division <strong>of</strong> Pharmascience Inc.<br />
Pfizer Canada Inc.<br />
Pharmaceutical Partners <strong>of</strong> Canada<br />
A Company <strong>of</strong> the Fresenius Kabi Group<br />
San<strong>of</strong>i-aventis Canada Inc.<br />
Teva Canada
9<br />
CSHP Sponsors 2011<br />
The following list reflects all CSHP<br />
Sponsorship received from January 1 to<br />
December 31, 2011.<br />
Commanditaires de la<br />
SCPH en 2011<br />
La liste suivante reflète toutes les<br />
commandites reçues du premier janvier au<br />
31 décembre 2011.<br />
Diamond Sponsor<br />
Commanditaires diamant<br />
$80,000 or greater<br />
80 000 $ et plus<br />
CSHP<br />
Targeting Excellence in Pharmacy Practice<br />
Platinum Sponsor<br />
Commanditaires platine<br />
$60,000 - $79,999<br />
• Hospira Healthcare Corporation<br />
Gold Sponsor<br />
Commanditaires or<br />
$40,000 - $59,999<br />
• Boehringer-Ingelheim Canada Ltd.<br />
• Eli Lilly Canada Inc.<br />
• TEVA Canada<br />
Silver Sponsor<br />
Commanditaires argent<br />
$20,000 - $39,999<br />
• Apotex Inc.<br />
• AstraZeneca<br />
• Bayer Inc.<br />
• Johnson & Johnson Family <strong>of</strong> Companies<br />
• Merck Canada Inc.<br />
Bronze Sponsor<br />
Commanditaires bronze<br />
$10,000 - $19,999<br />
• Abbott Laboratories Inc.<br />
• Mylan Pharmaceuticals<br />
• Pendopharm,<br />
a division <strong>of</strong> Pharmascience Inc.<br />
• San<strong>of</strong>i-aventis Canada Inc.<br />
CSHP would like to acknowledge and thank the following CSHP Sponsors for their<br />
contributions to CSHP 2015 initiatives:<br />
• Pfizer Canada Inc.<br />
• Sandoz Canada Inc.<br />
• Pharmaceutical Partners <strong>of</strong> Canada<br />
A Company <strong>of</strong> the Fresenius Kabi Group<br />
SCPH<br />
Point de mire sur l’excellence en pratique pharmaceutique<br />
Donor Sponsor<br />
Commanditaires donateurs<br />
$1000 - $9,999<br />
• Alveda Pharma<br />
• AmeriscourceBergen Canada<br />
• Amgen Canada Inc.<br />
• Astellas Canada<br />
• ATP a TCP Company<br />
• B Braun Medical Inc.<br />
• Baxa Corporation<br />
• Baxter Corporation<br />
• British Columbia Ministry <strong>of</strong> Health<br />
• Bristol-Meyers Squibb Canada<br />
• <strong>Canadian</strong> Agency for Drugs and<br />
Technologies in Health (CADTH)<br />
• Caverly Consulting Group<br />
• <strong>Canadian</strong> Pharmaceutical Distribution<br />
Network (CPDN)<br />
• <strong>Canadian</strong> Patient Safety Institute (CPSI)<br />
• Fraser Health Authority<br />
• Galenova Inc.<br />
• Healthmark Ltd.<br />
• HealthPRO<br />
• H<strong>of</strong>fman La Roche Limited<br />
• HSBC<br />
• LEO Pharma Inc.<br />
• Lexi-comp Inc.<br />
• Lundbeck Canada Inc.<br />
• Manrex Ltd.<br />
• McKesson Canada<br />
• Medbuy<br />
• Department <strong>of</strong> National Defence (DND)<br />
• Northwest Telepharmacy<br />
• Novartis Pharma Canada<br />
• Omega Laboratories Limited<br />
• Omnicell<br />
• Ontario College <strong>of</strong> <strong>Pharmacists</strong> (OCP)<br />
• PCCA Canada<br />
• Pharmacy Examining Board <strong>of</strong> Canada<br />
(PEBC)<br />
• RxFiles - Academic Detailing <strong>Program</strong><br />
• Servier Canada Inc.<br />
• Shoppers Drug Mart Specialty Health<br />
• St. Paul’s <strong>Hospital</strong><br />
• SteriMax Inc.<br />
• Swisslog Healthcare Solutions
10<br />
Distinguished Service<br />
Award<br />
Prix pour service<br />
distingué<br />
Sponsored by Johnson & Johnson Family<br />
<strong>of</strong> Companies • $10,000<br />
This award recognizes outstanding<br />
achievement in hospital pharmacy<br />
practice.<br />
Individuals are nominated by their peers.<br />
2012 Winner<br />
Carolyn Bornstein<br />
Past Winners<br />
2011 Myrella Roy<br />
2010 Emily Musing<br />
2009 Robin Ensom<br />
2008 Nancy Roberts<br />
2007 Thomas W. Paton<br />
2006 Linda Poloway<br />
2005 Bill Bartle<br />
2004 Garry King<br />
2003 Bob Nakagawa<br />
2002 Glen R. Brown<br />
2001 Charlie Bayliff<br />
2000 James Blackburn<br />
1999 Bonnie Salsman<br />
1998 Scott Walker<br />
1997 Rosemary Bacovsky<br />
1996 Kevin Hall<br />
1995 James L. Mann<br />
1994 William McLean<br />
1993 Pauline Beaulac<br />
1992 William Wilson<br />
1991 C. Brian Tuttle<br />
1990 Reta Fowler<br />
1989 Alan Samuelson<br />
1988 Bruce R. Schnell<br />
1987 Jack Dancey<br />
1986 William R. Foltas*<br />
1985 Donna M. Shaw*<br />
1984 Sister Grace Sauvé<br />
1983 Mary T. Gannon*<br />
1982 J. Glen Moir*<br />
1981 Brian A. Dinel<br />
1980 Betty C. Riddell<br />
1979 Jack L. Summers*<br />
1978 Douglas J. Stewart*<br />
1977 Phyllis Yagi*<br />
1976 Orest Buchko<br />
1975 Muriel Hale<br />
1974 Anne O’Toole<br />
1973 Leonard Gibson*<br />
1972 J. Edwin Smith*<br />
1971 Paule Benfante<br />
1970 Gordon Brown*<br />
1969 Isabel E. Stauffer*<br />
1968 Jacqueline McCarthy<br />
1967 Michael J.V. Naylor<br />
*Deceased<br />
Isabel E. Stauffer<br />
Meritorious Service<br />
Award<br />
Prix Isabel E. Stauffer<br />
pour service méritoire<br />
Sponsored by Pharmaceutical Partners <strong>of</strong><br />
Canada A Company <strong>of</strong> the Fresenius Kabi<br />
Group • $3,750<br />
This award recognizes prolonged service<br />
and involvement in CSHP, primarily at the<br />
branch or chapter level.<br />
Individuals are nominated by their peers.<br />
2012 Winner<br />
Judy Chong<br />
Past Winners<br />
2011 John McBride<br />
2010 Victoria Sills<br />
2009 Lynda Chilibeck<br />
2008 Catherine Doherty<br />
2007 Harry S. Hopkins<br />
2006 Susan Poulin<br />
2005 Donna Wheeler-Usher<br />
2004 Nancy Roberts<br />
2003 Margaret Gray<br />
2002 Margaret Colquhoun<br />
2001 No candidates this year<br />
2000 Kelly Babcock<br />
1999 Linda Poloway<br />
1999 Kenneth McGregor<br />
1998 Larry Legare<br />
1998 Emily Somers<br />
1997 No candidates this year<br />
1996 Dennis Leith<br />
1996 Robert S. Nakagawa<br />
1995 Donna Pipa<br />
1995 Kristina Wichman<br />
1994 Rosemary Bacovsky<br />
1994 Roy A. Steeves<br />
1993 No candidate this year<br />
1992 John Iazzetta<br />
1992 Cecilia Laskoski<br />
1991 Louanne Twaites<br />
1991 David Windross<br />
1990 Doris A. Thompson<br />
1989 Fred Rumpel<br />
1988 D. Bryce Thompson<br />
1987 Alan Samuelson<br />
1986 Herbert A. Dixon<br />
1986 A.W. Stanley Garvin<br />
New <strong>Hospital</strong> Pharmacy<br />
Practitioner Award<br />
Prix du nouveau<br />
praticien en pharmacie<br />
hospitalière<br />
Sponsored by<br />
Sandoz Canada Inc. • $3,750 x 2<br />
This award acknowledges new hospital<br />
pharmacy practitioners, who through their<br />
service to patient care, to education or<br />
research, to the pr<strong>of</strong>ession and to the<br />
society, are worthy <strong>of</strong> recognition. The<br />
individuals exhibit promising leadership,<br />
dedication and commitment to practice<br />
excellence and pr<strong>of</strong>essional growth.<br />
2012 Winners<br />
Christina Adams & Erin Marie Yakiwchuk<br />
Past Winners<br />
2011 Zack Dumont & Shanna Trenaman<br />
2010 Erin Cashin & Rochelle Gellatly<br />
2009 Eva Cho & Lynette Kolodziejak<br />
2008 Yvonne Kwan & Adrienne Lindblad<br />
2007 Tracy Cheung & Jennifer Dyck<br />
2006 Dawn Dalen & Gloria Tsang<br />
2005 Stephanie Ong & Kerry Wilbur<br />
<strong>Hospital</strong> Pharmacy<br />
Student Award<br />
Prix de l’étudiant en<br />
pharmacie hospitalière<br />
Sponsored by CSHP and the <strong>Canadian</strong><br />
Association <strong>of</strong> Pharmacy Students and<br />
Interns (CAPSI) • $500<br />
This award recognizes pharmacy students<br />
who show promise as future hospital<br />
pharmacy practitioners through their<br />
student activities or their experiential<br />
training in direct patient care, research or<br />
education. The winners exhibit eagerness,<br />
dedication and a positive attitude toward<br />
the academic learning, the practice, and<br />
the pr<strong>of</strong>ession <strong>of</strong> hospital pharmacy.<br />
2012 Winner<br />
Sarah Hasenbank<br />
Past Winners<br />
2011 Jessica Gagatek & Timothy Leung<br />
2010 Christine Leong<br />
2009 Amy Grossberndt<br />
2008 Omolayo O. Famuyide<br />
2007 Cathryn Sibbald<br />
2006 Justin Lee
11<br />
2011-2012 Awards Committee<br />
Comité des prix 2011-2012<br />
Sincere appreciation is extended to the CSHP National Awards<br />
Committee.<br />
Chairperson<br />
Présidente<br />
Kathryn Hollis<br />
Management and Leadership<br />
Best Practices Award<br />
Sponsored by:<br />
Apotex Inc. ...................$3,750<br />
Hospira Healthcare<br />
Corporation ..................$3,750<br />
Patient Care Enhancement<br />
Award<br />
Sponsored by:<br />
AstraZeneca<br />
Canada Inc. ..................$3,750<br />
TEVA Canada................$3,750<br />
Pharmacotherapy Best<br />
Practices Award<br />
Sponsored by:<br />
Merck Canada Inc.........$3,750<br />
Pfizer Canada Inc. .........$3,750<br />
Members<br />
Membres<br />
Candra Cotton<br />
Janice Ma<br />
My-Linh Nguyen<br />
Pooja Patel<br />
Rosemary Zvonar<br />
2011-2012 Awards <strong>Program</strong><br />
<strong>Program</strong>me des prix 2011-2012<br />
The CSHP general awards program will be presented in six<br />
categories with nine sponsors, as listed below. The redesign was<br />
implemented several years ago. This was a recommendation by the<br />
Members Rewards and Recognition Task Force in order to update<br />
the program, increase accessibility and foster innovative pharmacy<br />
practice.<br />
Safe Medication Practices<br />
Award<br />
Sponsored by:<br />
Baxter Corporation .......$3,750<br />
Hospira Healthcare<br />
Corporation ..................$3,750<br />
Specialties in Pharmacy<br />
Practice Award<br />
Sponsored by:<br />
Pharmascience Inc. .......$3,750<br />
Hospira Healthcare<br />
Corporation ..................$3,750<br />
Teaching, Learning and<br />
Education Award<br />
Sponsored by:<br />
Eli Lilly Canada Inc. ......$3,750<br />
2011-2012 Tribute to CSHP National<br />
Award Appraisers<br />
Hommage aux évaluateurs<br />
Award appraisers are an integral part <strong>of</strong> the CSHP National Awards<br />
program. We would like to extend our sincere thanks to the<br />
individuals listed below who volunteered their time to review this<br />
year’s award submissions. We are very grateful to you for sharing<br />
your time and expertise in support <strong>of</strong> the CSHP Awards <strong>Program</strong>.<br />
Without your dedicated efforts on the <strong>Society</strong>’s behalf, the program<br />
would not exist.<br />
Shirin Abadi<br />
Alison Alleyne<br />
Mayce Al-Sukhni<br />
Trudy Arbo<br />
Tejinder Bains<br />
Swasti Bhajan-Mathur<br />
Judy Chong<br />
Celine Corman<br />
Anne Dar Santos<br />
Mario De Lemos<br />
Anar Dossa<br />
Douglas Doucette<br />
Liz Edwards<br />
Dinie Engels<br />
Barb Evans<br />
Olavo Fernandes<br />
Michelle Foisy<br />
Susan Halasi<br />
Nicholas Honcharik<br />
Sherilyn Houle<br />
Christine Hughes<br />
Cynthia Jackevicius<br />
Derek Jorgenson<br />
Christopher Judd<br />
Jean-Yves Julien<br />
Zahra Kanji<br />
Heather Kertland<br />
Jaclyn LeBlanc<br />
Larry Legare<br />
Adrienne Lindblad<br />
Anita Lo<br />
Peter Loewen<br />
Barry Lyons<br />
Janice Ma<br />
Greta Mah<br />
Mark Makowsky<br />
Anne Massicotte<br />
Karen McDermaid<br />
Tania Mysak<br />
Carmine Nieuwstraten<br />
Glen Pearson<br />
Patricia Pracsovics<br />
Irina Rajakumar<br />
Cheryl Sadowski<br />
Brenda Schuster<br />
Roy Steeves<br />
Daniel Thirion<br />
Joyce Totton<br />
Régis Vaillancourt<br />
Lori Wazny<br />
Bertha (Mary) Whyte<br />
Sharon Yamashita<br />
Peter Zed<br />
If you are interested in acting as an appraiser for the 2012-2013<br />
Awards <strong>Program</strong>, please contact Amanda Cuirrier:<br />
Tel.: 613-736-9733, ext. 222<br />
Fax: (613) 736-5660or<br />
Email at acuirrier@cshp.ca.
12<br />
Upcoming Events<br />
Événements à venir<br />
Pr<strong>of</strong>essional Practice<br />
Conference (PPC):<br />
February 2-6, 2013<br />
Sheraton Centre Toronto Hotel<br />
February 1-5, 2014<br />
Sheraton Centre Toronto Hotel<br />
January 31-February 4, 2015<br />
Sheraton Centre Toronto Hotel<br />
January 30-February 3, 2016<br />
Sheraton Centre Toronto Hotel<br />
Summer Educational<br />
Sessions (SES):<br />
August 11-14, 2012<br />
Delta Prince Edward Hotel<br />
Charlottetown, Prince Edward Island<br />
August 10-13, 2013<br />
Hyatt Regency Calgary<br />
Calgary, Alberta<br />
August 9-12, 2014<br />
Delta Newfoundland Hotel<br />
St. John’s, Newfoundland & Labrador<br />
August 8-11, 2015<br />
Hilton London Ontario<br />
London, Ontario<br />
Attendance at CSHP conferences, PPC and<br />
SES, are approximately 550 and 250<br />
respectively, excluding exhibitors. Please<br />
note we <strong>of</strong>fer an exhibit program at both<br />
events.<br />
For further information, please contact<br />
Desarae Davidson, Conference & PSN<br />
Administrator.<br />
Tel.: (613) 736-9733, ext. 229<br />
Fax: (613) 736-5660<br />
Email: ddavidson@cshp.ca<br />
Satellite Symposiums<br />
Symposiums satellites<br />
CSHP would like to thank the following<br />
sponsors <strong>of</strong> Satellite Symposiums for their<br />
participation in conjunction with the<br />
PPC 2012.<br />
Sunday, February 5<br />
12:15-13:45 • AstraZeneca Canada<br />
• Boehringer-Ingelheim<br />
Canada Inc.<br />
• Eli Lilly Canada Inc.<br />
Monday, February 6<br />
17:30-19:30 • Janssen Inc. Canada<br />
• Hospira Healthcare<br />
Corporation<br />
Tuesday, February 7<br />
17:30-19:30 • Hospira Healthcare<br />
Corporation<br />
• Otsuka Pharmaceutical Inc.<br />
Wednesday, February 8<br />
12:40-14:10 • Bayer Inc.<br />
• Purdue Pharma<br />
See the program section for more details.<br />
Satellite<br />
Symposium<br />
SPONSORSHIP<br />
OPPORTUNITY<br />
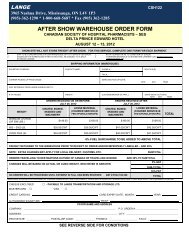
65th Summer Educational Sessions<br />
Delta Prince Edward Hotel<br />
Charlottetown, PEI<br />
August 11 to 14, 2012<br />
Breakfast and<br />
Luncheon Availability<br />
For more information please contact<br />
Desarae Davidson<br />
Conference & PSN Administrator<br />
(613) 736-9733, ext. 229 or<br />
ddavidson@cshp.ca
13<br />
The Educational Services Committee<br />
Le Comité des services éducatifs<br />
EP C.C.E.P.<br />
<strong>Canadian</strong> Council on<br />
Continuing Education in Pharmacy<br />
Chairperson • Présidente<br />
Margaret Ackman, PharmD, FCSHP<br />
Alberta Health Services<br />
Edmonton, AB<br />
Members • Membres<br />
Toni Bailie, BScPhm<br />
Mount Sinai <strong>Hospital</strong><br />
Toronto, ON<br />
Claudia Bucci, PharmD<br />
Sunnybrook Health Sciences Centre<br />
Toronto, ON<br />
Allison Callaghan, BScPhm<br />
QEII Health Sciences Centre<br />
Halifax, NS<br />
Roxane Carr, PharmD, BCPS, FCSHP<br />
BC Children’s and Women’s Health Centre<br />
Vancouver, BC<br />
Clarence Chant, PharmD, FCSHP<br />
St. Michael’s <strong>Hospital</strong><br />
Toronto, ON<br />
Elaine Chong, PharmD, BCPS<br />
BC Ministry <strong>of</strong> Health Services<br />
New Westminster, BC<br />
Judy Chong, BScPhm<br />
Royal Victoria <strong>Hospital</strong> <strong>of</strong> Barrie<br />
Barrie, ON<br />
Olavo Fernandes, PharmD, FCSHP<br />
University Health Network<br />
Toronto, ON<br />
Alfred Gin, PharmD, FCSHP<br />
Health Sciences Centre<br />
Winnipeg, MB<br />
Colette Raymond, PharmD<br />
Winnipeg Regional Health Authority<br />
Winnipeg, MB<br />
Kat Timberlake, PharmD<br />
The <strong>Hospital</strong> for Sick Children<br />
Toronto, ON<br />
Erica Wang, BScPhm<br />
PharmD Candidate<br />
University <strong>of</strong> British Columbia<br />
Vancouver, BC<br />
The Educational Services Committee (ESC) <strong>of</strong><br />
CSHP has been working for approximately<br />
10 months on the content and format <strong>of</strong><br />
PPC 2012. The committee also works on the<br />
Summer Educational Sessions, in<br />
conjunction with the local host task force<br />
and the national <strong>of</strong>fice. The ESC is<br />
comprised <strong>of</strong> a core committee <strong>of</strong> 15 CSHP<br />
members as well as corresponding members<br />
from the CSHP branches.<br />
Goal and Objectives for the<br />
2012 PPC <strong>Program</strong><br />
Goal:<br />
• To provide registrants with quality<br />
educational sessions.<br />
Objectives:<br />
• To provide educational sessions which<br />
inform, educate and motivate clinical<br />
practitioners and managers.<br />
• To provide leadership in hospital<br />
pharmacy practice by presenting sessions<br />
on innovative pharmacists’ roles,<br />
pharmacy practice and pharmacy<br />
programs.<br />
• To promote life-long learning skills<br />
through active participation in<br />
problem-based workshops.<br />
• To provide registrants with networking<br />
and sharing opportunities through the<br />
exhibits program and poster sessions.<br />
• To promote excellence in pharmacy<br />
practice through oral and poster<br />
presentations <strong>of</strong> original work and<br />
award winning projects.<br />
• To provide an opportunity for Pharmacy<br />
Specialty Networks to share their<br />
expertise with others and meet as<br />
Networks.<br />
Le Comité des services éducatifs travaille<br />
depuis près de 10 mois à l’élaboration du<br />
contenu et de la forme de la CPP 2012.<br />
Le Comité prépare aussi les Séances<br />
éducatives d’été de la SCPH en<br />
collaboration avec le Groupe de travail<br />
hôte local et le personnel de la SCPH. Le<br />
Comité comprend 15 membres principaux<br />
et membres correspondants des sections<br />
de la SCPH.<br />
But et objectifs du<br />
programme de la CPP 2012<br />
But :<br />
• Présenter des conférences éducatives de<br />
qualité aux participants.<br />
Objectifs :<br />
• Présenter aux personnes inscrites des<br />
conférences éducatives susceptibles<br />
d’informer, d’instruire et de motiver les<br />
cliniciens et les gestionnaires.<br />
• Orienter la pratique de la pharmacie<br />
hospitalière en présentant des<br />
conférences sur les nouveautés touchant<br />
le rôle du pharmacien, la pratique de la<br />
pharmacie et les programmes de<br />
pharmacie.<br />
• Développer des habiletés pour un<br />
apprentissage continu par une<br />
participation active à des ateliers de<br />
formation axés sur la résolution de<br />
problèmes.<br />
• Donner aux participants des occasions<br />
de réseautage et d’échanges grâce au<br />
salon des exposants, aux séances<br />
d’affichage et aux discussions<br />
interactives structurées.<br />
• Promouvoir l’excellence dans la pratique<br />
de la pharmacie par des présentations<br />
orales et des séances d’affichage sur des<br />
travaux originaux et des projets primés.<br />
• Donner l’occasion aux réseaux de<br />
spécialistes en pharmacie de se réunir et<br />
de partager leur savoir-faire.
14<br />
<strong>Program</strong><br />
<strong>Program</strong>me<br />
Saturday, February 4 • Samedi 4 février<br />
15:00-17:00 Registration<br />
Inscription<br />
CONCOURSE COAT CHECK<br />
17:30-19:30 CHPRB 50th Anniversary Reception<br />
Everyone welcome<br />
Réception pour le 50 e anniversaire du CCRPH<br />
Bienvenue à tous<br />
CHURCHILL ROOM<br />
Sponsored by Pendopharm,<br />
a division <strong>of</strong> Pharmascience Inc.<br />
Sunday, February 5 • Dimanche 5 février<br />
Research Focus Day<br />
Journée consacrée à la recherche<br />
07:30-17:00 Registration<br />
Inscription<br />
CONCOURSE COAT CHECK<br />
08:00-08:15 Opening Remarks<br />
Remarques préliminaires<br />
DOMINION BALLROOM<br />
08:15-09:15 Motivational Plenary<br />
Assemblée plénière de motivation<br />
DOMINION BALLROOM<br />
Dr. Roberta Bondar, OCO Ont, MD, PhD, FRCP, FRSC<br />
Consultant, Physician, Scientist, Author,<br />
Photographer, Educator<br />
Canada’s first female astronaut. Dr. Roberta Bondar<br />
is an advocate for our unique planet after the rare<br />
opportunity to view Earth from space. As science<br />
and photography have always been linked in Dr.<br />
Bondar’s life, it was natural that one <strong>of</strong> Bondar’s<br />
assignments aboard the space shuttle Discovery in<br />
January 1992 was to take photographs <strong>of</strong> Earth.<br />
Sponsored by Sandoz Canada Inc. through an<br />
unrestricted educational grant<br />
9:30-11:00 Facilitated Poster Session<br />
Discussions <strong>of</strong> original research, award-winning<br />
projects and pharmacy practice projects<br />
Séance animée de présentations par<br />
affiches<br />
Discussions sur des projets de recherche originale,<br />
des projets primés et des projets dans le domaine<br />
de la pratique pharmaceutique<br />
ESSEX BALLROOM<br />
11:15-12:00 Concurrent Sessions<br />
Séances concomitantes<br />
1. Managing Acute Stroke: What You Need<br />
To Know<br />
WINDSOR<br />
Tania Mysak, BSP, PharmD<br />
Alberta Health Services<br />
Edmonton, AB<br />
2. Extended Infusion <strong>of</strong> Beta Lactams: A<br />
Primer on Why, When, and Mainly How<br />
SIMCOE/DUFFERIN<br />
Sandra Walker, BSc, BScPhm, ACPR, PharmD,<br />
FCSHP<br />
Sunnybrook Health Sciences Centre<br />
Toronto, ON<br />
3. Smartphones: A Novel “App”roach to<br />
Patient Care<br />
CONFERENCE B/C<br />
Sean Spina, BScPhm, ACPR, PharmD<br />
Vancouver Island Health Authority<br />
Victoria, BC<br />
4. Understanding Observational Studies and<br />
Implications for Patient Care<br />
CONFERENCE D/E<br />
David Juurlink, BScPhm, MD, PhD, FRCPC<br />
Sunnybrook Health Sciences Centre<br />
Institute for Clinical Evaluative Sciences<br />
Toronto, ON<br />
12:15-13:45 Satellite Symposiums<br />
Luncheon included<br />
Symposiums satellites<br />
Dîner inclus<br />
1. Pharmacy C.A.R.E. in ACS (Clinical<br />
Advances for the Reduction <strong>of</strong> Events)<br />
CITY HALL<br />
Patrick Robertson, PharmD – Moderator<br />
Saskatoon Health Region<br />
Saskatoon, SK<br />
Jennifer Pickering, BScPhm, ACPR<br />
Hamilton Health Sciences<br />
Hamilton, ON<br />
Hosted by AstraZeneca Canada<br />
2. From Sliding Scale to Basal Bolus:<br />
Optimizing the Management <strong>of</strong><br />
Hyperglycemia in Non-Critically Ill<br />
<strong>Hospital</strong>ized Patients<br />
DOMINION BALLROOM NORTH<br />
Anar Dossa, BScPhm, PharmD, CDE<br />
Vancouver General <strong>Hospital</strong><br />
Vancouver, BC<br />
Maureen Clement, MD, CCFP<br />
University <strong>of</strong> British Columbia<br />
Vancouver, BC<br />
Hosted by Eli Lilly Canada Inc.
15<br />
3. Preventing Stroke in Atrial Fibrillation:<br />
From Clinical Trials to the Bedside<br />
DOMINION BALLROOM SOUTH<br />
William Semchuk, MSc, PharmD, FCSHP (Chair)<br />
Regina Qu’Appelle Health Region<br />
Regina, SK<br />
Claudia Bucci, PharmD<br />
Sunnybrook Health Sciences Centre<br />
Toronto, ON<br />
Hosted by Boehringer-Ingelheim Canada Inc.<br />
14:00-16:00 Workshops & PSN Sessions<br />
Ateliers et séances des RSP<br />
1. Research Design for Dummies:<br />
Chart Review Studies<br />
SIMCOE/DUFFERIN<br />
Ross Tsuyuki, BScPhm, PharmD, MSc, FCSHP,<br />
FACC<br />
Faculty <strong>of</strong> Medicine and Dentistry<br />
University <strong>of</strong> Alberta<br />
Edmonton, AB<br />
2. Geriatrics PSN<br />
RSP en gériatrie<br />
CONFERENCE B/C<br />
Antipsychotic Use Circa 2012: What Have<br />
We Learned Regarding Their Efficacy and<br />
Safety for Behavioural Psychological<br />
Symptoms <strong>of</strong> Dementia (BSPD)?<br />
Carlos Rojas-Fernandez, BScPhm, PharmD<br />
Schlegel-UW Research Institute on Aging &<br />
School <strong>of</strong> Pharmacy, University <strong>of</strong> Waterloo<br />
Kitchener, ON<br />
Blood Pressure and Diabetes in the<br />
Elderly: Moving Targets<br />
Naomi Dore, BScH, MSc, BScPhm<br />
Hamilton Health Sciences Centre<br />
Hamilton, ON<br />
3. Global Health PSN<br />
RSP en santé mondiale<br />
WINDSOR<br />
Is an Ounce <strong>of</strong> Palivizumab Worth a<br />
Pound <strong>of</strong> Cure? The Intersection <strong>of</strong><br />
Research Advocacy and Politics in the<br />
Arctic<br />
Anna Banerji, MD, MPH, FRCPC, DTM&H<br />
St. Michael’s <strong>Hospital</strong><br />
Toronto, ON<br />
Student Insights from Bottom-Up and<br />
Top-Down: Approaches in Global Health<br />
Matt Koehler, BScPhm, RPh<br />
Shoppers Drug Mart<br />
Thunder Bay, ON<br />
Ryan McGuire, BScPhm<br />
Toronto General <strong>Hospital</strong><br />
Toronto, ON<br />
4. Anticoagulation PSN<br />
RSP en anticoagulation<br />
CONFERENCE D/E<br />
Anticoagulation Risk Assessment:<br />
Practical Implications for <strong>Pharmacists</strong><br />
Cynthia Brocklebank, BScPhm, PharmD, ACPR<br />
Alberta Health Services<br />
Calgary, AB<br />
New Anticoagulants for Stroke<br />
Prevention in Atrial Fibrillation<br />
Jennifer Pickering, BScPhm, ACPR<br />
Hamilton Health Sciences Centre<br />
Hamilton, ON<br />
16:10-17:50 Awards Ceremony<br />
Everyone welcome<br />
Cérémonie de remise des prix<br />
Bienvenue à tous<br />
ESSEX BALLROOM<br />
18:00-19:30 Career Opportunities Evening<br />
Soirée de perspectives d’emploi<br />
Research and Education Silent Auction<br />
Vente aux enchères par écrit de la Fondation<br />
pour la recherche et l’éducation de la SCPH<br />
OSGOODE HALL<br />
Monday, February 6 • Lundi 6 février<br />
Primary Care Day<br />
Journée des soins primaires<br />
07:30-17:00 Registration<br />
Inscription<br />
CONCOURSE COAT CHECK<br />
08:00-08:15 Announcements<br />
Annonces<br />
DOMINION BALLROOM<br />
08:15-09:45 Immigrant Health Issues: Implications for<br />
<strong>Hospital</strong> <strong>Pharmacists</strong><br />
DOMINION BALLROOM<br />
Kevin Pottie, MD, MCIS<br />
Department <strong>of</strong> Family Medicine and Clinical<br />
Epidemiology and Community Medicine<br />
University <strong>of</strong> Ottawa<br />
Ottawa, ON
16<br />
New Fellows Presentation<br />
Présentation des nouveaux membres associés<br />
Acknowledgement <strong>of</strong> the recipient <strong>of</strong> the<br />
Distinguished Service Award<br />
Reconnaissance de la lauréate du prix pour<br />
service distingué<br />
Acknowledgement <strong>of</strong> the Research and<br />
Education Foundation Grant Recipients<br />
Reconnaissance des boursiers de la Fondation<br />
pour la recherche et l’éducation<br />
DOMINION BALLROOM<br />
09:45-10:15 Break, Exhibits<br />
Pause, Kiosques<br />
SHERATON/OSGOODE HALLS<br />
10:30-11:15 Concurrent Sessions<br />
Séances concomitantes<br />
1. Total Parenteral Nutrition for Pediatrics:<br />
A Pharmacy Perspective<br />
SIMCOE/DUFFERIN<br />
Vijay Rasaiah, RPh, BScPhm, MSc, BSc(Hon)<br />
The <strong>Hospital</strong> for Sick Chidlren<br />
Toronto, ON<br />
2. Highlights in Pharmacy Excellence:<br />
Oral Abstract Session<br />
Intriguing Papers from Original Research,<br />
Award Winners and Research and<br />
Education Grants<br />
For details on the specific projects, please see<br />
page 44.<br />
Plein feu sur l'excellence en pharmacie :<br />
Séance d’exposés oraux<br />
Communications fascinantes tirées de<br />
travaux de recherche inédits.<br />
Récipiendaires de prix, de bourses de<br />
recherche et de perfectionnement<br />
Pour plus de détails, s'il vous plaît voir la page 44.<br />
CONFERENCE D/E<br />
3. Controversies in Diabetes Management:<br />
Are we ADVANCE-ing our Knowledge<br />
and Treatment ACCORD-ingly?<br />
CITY HALL<br />
Anar Dossa, BScPhm, PharmD, CDE<br />
Vancouver General <strong>Hospital</strong><br />
Vancouver, BC<br />
4. Transition with Success! Increasing the<br />
Awareness <strong>of</strong> Medication Misadventures<br />
after Discharge from <strong>Hospital</strong><br />
CONFERENCE B/C<br />
Lisa Sever, BScPhm, ACPR, CGP<br />
York Central <strong>Hospital</strong><br />
Richmond Hill, ON<br />
11:25-12:10 Concurrent Sessions<br />
Séances concomitantes<br />
1. To TREAT or not to TREAT: Making Sense<br />
<strong>of</strong> ESAs and Targets in CKD<br />
SIMCOE/DUFFERIN<br />
Amy Sood, BScPhm, PharmD<br />
Manitoba Renal <strong>Program</strong>, St. Boniface <strong>Hospital</strong><br />
Winnipeg, MB<br />
2. Beyond Statins: Treating Dyslipidemia<br />
and Residual Cardiovascular Risk with<br />
Other Lipid-Lowering Agents<br />
CITY HALL<br />
Glen Pearson, BSc, BScPhm, PharmD, FCSHP<br />
Division <strong>of</strong> Cardiology, University <strong>of</strong> Alberta<br />
Manzankowski Alberta Institute<br />
Edmonton, AB<br />
3. Highlights in Pharmacy Excellence:<br />
Oral Abstract Session<br />
Intriguing Papers from Original Research,<br />
Award Winners and Research and<br />
Education Grants<br />
For details on the specific projects, please see<br />
page 44.<br />
Plein feu sur l’excellence en pharmacie :<br />
Séance d'exposés oraux<br />
Documents fascinants tirés de travaux de<br />
recherche inédits. Récipiendaires de prix,<br />
de bourses de recherche et d’étude<br />
Pour plus de détails, s'il vous plais voir la page 44.<br />
CONFERENCE D/E<br />
4. Smartphones: A Novel “App”roach to<br />
Patient Care (encore)<br />
CONFERENCE B/C<br />
Sean Spina, BScPhm, ACPR, PharmD<br />
Vancouver Island Health Authority<br />
Royal Jubilee <strong>Hospital</strong><br />
Victoria, BC<br />
12:15-13:50 Lunch, Exhibits, Posters, Silent Auction<br />
Dîner, Kiosques, Affiches, Vente aux<br />
enchères par écrit<br />
SHERATON/OSGOODE HALLS<br />
13:55-14:55 A Practical Approach to Drug Interactions<br />
DOMINION BALLROOM<br />
David Juurlink, BScPhm, MD, PhD, FRCPC<br />
Sunnybrook Health Sciences Centre<br />
Institute for Clinical Evaluative Sciences<br />
Toronto, ON<br />
15:00-17:00 Workshops & PSN Sessions<br />
Ateliers et séances des RSP<br />
1. What are the Appropriate National<br />
Clinical Pharmacy Key Performance<br />
Indicators (KPI) for <strong>Canadian</strong> <strong>Hospital</strong><br />
<strong>Pharmacists</strong>?<br />
SIMCOE/DUFFERIN
17<br />
Olavo Fernandes, PharmD, FCSHP<br />
University Health Network<br />
Leslie Dan Faculty <strong>of</strong> Pharmacy<br />
University <strong>of</strong> Toronto<br />
Toronto, ON<br />
Richard Slavik, PharmD, FCSHP<br />
Pr<strong>of</strong>essional Practice Interior Health<br />
University <strong>of</strong> British Columbia<br />
Kelowna, BC<br />
2. Paediatric PSN<br />
RSP en pédiatrie<br />
CONFERENCE D/E<br />
Chemotherapy-Induced Nausea and<br />
Vomiting in Children: An Evidence-Based<br />
Approach<br />
Lee Dupuis, RPh, ACPR, MScPhm, FCSHP<br />
The <strong>Hospital</strong> for Sick Children<br />
Toronto, ON<br />
Pain, Pain, Go Away. Don’t Come Back<br />
Another Day! Exploring Treatment<br />
Options and Strategies for the<br />
Management <strong>of</strong> Pediatric Chronic Pain<br />
Régis Vaillancourt, OMM, OD, CD, BPhm,<br />
PharmD, FCSHP<br />
Children’s <strong>Hospital</strong> <strong>of</strong> Eastern Ontario<br />
Ottawa, ON<br />
3. Primary Care PSN<br />
RSP en soins de santé primaires<br />
CONFERENCE B/C<br />
Practical Approaches to Reducing<br />
Polypharmacy in the Elderly: An<br />
Interactive Workshop<br />
Debbie Kwan, BScPhm, MSc, FCSHP<br />
Toronto Western <strong>Hospital</strong><br />
Family Health Team<br />
Toronto, ON<br />
Barbara Farrell, BScPhm, PharmD, FCSHP<br />
Bruyère Continuing Care<br />
Ottawa, ON<br />
4. Infectious Disease PSN<br />
RSP en infectiologie<br />
CITY HALL<br />
MRSA Guidelines and Clinical<br />
Controversies: A Practical Overview<br />
Tim Lau, PharmD, FCSHP<br />
Vancouver General <strong>Hospital</strong><br />
Vancouver Coastal Health<br />
Vancouver, BC<br />
Update on Urinary Tract Infections<br />
Monique Pitre, BScPhm, FCSHP<br />
University Health Network<br />
Toronto, ON<br />
17:30-19:30 Satellite Symposiums<br />
Dinner included<br />
Symposiums satellites<br />
Souper inclus<br />
1. The Value <strong>of</strong> Biologics and Follow-On<br />
Biologics: What the Future Holds for<br />
Personalized Medicine, Co-Diagnostics<br />
and Subsequent Entry Biologics<br />
DOMINION BALLROOM NORTH<br />
George Dranitsaris, MPharm, FCSHP, DPH<br />
<strong>Canadian</strong> Association <strong>of</strong> <strong>Pharmacists</strong> in Oncology<br />
Toronto, ON<br />
Vandana Ahluwalia, MD, FRCPC<br />
Ontario Rheumatology Association<br />
Toronto, ON<br />
Hosted by Janssen Inc. Canada<br />
2. Implementation <strong>of</strong> Smart Pump<br />
Technology: How We Did It<br />
ESSEX BALLROOM<br />
Karen Smith, RN, MHSPCM<br />
Ross Tilley Burn Centre<br />
Sunnybrook Health Sciences<br />
Toronto, ON<br />
Hosted by Hospira Healthcare Corporation<br />
Tuesday, February 7 • Mardi 7 février<br />
07:30-17:00 Registration<br />
Inscription<br />
CONCOURSE COAT CHECK<br />
08:00-08:15 Announcements<br />
Annonces<br />
DOMINION BALLROOM<br />
08:15-9:30 Pharmacy Issues and Controversies Forum –<br />
Panel Discussion<br />
Forum sur des questions et controverses en<br />
pharmacie – Panel<br />
Issues and Controversies: Pr<strong>of</strong>essional<br />
Integrity and Conflict <strong>of</strong> Interest<br />
DOMINION BALLROOM<br />
Judy Chong, BScPhm, RPh - Moderator<br />
Royal Victoria <strong>Hospital</strong> <strong>of</strong> Barrie<br />
Barrie, ON<br />
Peter Loewen, BScPhm, ACPR, PharmD, RPh, FCSHP<br />
Provincial Health Services Authority<br />
University <strong>of</strong> British Columbia<br />
Vancouver, BC<br />
James E. Tisdale, BScPhm, PharmD, BCPS, FCCP,<br />
FAPhA, FAHA<br />
College <strong>of</strong> Pharmacy, Purdue University<br />
Indianapolis IN
18<br />
Anne Hiltz, BScPhm, ACPR, RPh<br />
Capital District Health Authority<br />
Halifax, NS<br />
09:45-10:15 Break, Exhibits<br />
Pause, Kiosques<br />
SHERATON/OSGOODE HALLS<br />
10:25-11:10 Concurrent Sessions<br />
Séances concomitantes<br />
1. Top Clinical Papers in General Medicine<br />
CITY HALL<br />
Derek Jorgenson, BSP, PharmD, FCSHP<br />
University <strong>of</strong> Saskatchewan<br />
Saskatoon, SK<br />
2. Probiotics for C. difficile Infections, Yes...<br />
No... Maybe? A Review <strong>of</strong> Evidence<br />
SIMCOE/DUFFERIN<br />
Miranda So, BScPhm, PharmD<br />
University Health Network<br />
Toronto, ON<br />
3. COPE Implementation: Prescription for<br />
Success<br />
CONFERENCE B/C<br />
Janice Wells, PharmD<br />
St. Michael’s <strong>Hospital</strong><br />
Toronto, ON<br />
Pegi Rappaport, BSc, MSc<br />
Toronto East General <strong>Hospital</strong><br />
Toronto, ON<br />
11:20-12:05 Concurrent Sessions<br />
Séances concomitantes<br />
1. Management <strong>of</strong> Street Drug Toxicities<br />
SIMCOE/DUFFERIN<br />
Debra Kent, PharmD, DABAT, CSPI<br />
BC Drug and Poison Information Centre,<br />
BC Centre for Disease Control, Provincial Health<br />
Services Authority<br />
Vancouver, BC<br />
2. Controversies in Diabetes Management:<br />
Are we ADVANCE-ing our Knowledge<br />
and Treatment ACCORD-ingly? (encore)<br />
CITY HALL<br />
Anar Dossa, BScPhm, PharmD, CDE<br />
Vancouver General <strong>Hospital</strong><br />
Vancouver, BC<br />
3. Best Papers in Pharmacy Practice<br />
CONFERENCE B/C<br />
Jean-François Bussières, BPharm, MSc, MBA, FCSHP<br />
CHU Sainte-Justine<br />
Montréal, QC<br />
12:15-13:50 Lunch, Exhibits, Posters, Silent Auction<br />
Dîner, Kiosques, Affiches, Vente aux<br />
enchères par écrit<br />
SHERATON/OSGOODE HALLS<br />
14:00-15:00 What is the Optimal Prioritization <strong>of</strong><br />
Pr<strong>of</strong>essional Activities in a<br />
Collaboratively-Developed <strong>Hospital</strong><br />
<strong>Pharmacists</strong> Best Practice Model?<br />
DOMINION BALLROOM<br />
Olavo Fernandes, PharmD, FCSHP<br />
University Health Network<br />
Leslie Dan Faculty <strong>of</strong> Pharmacy<br />
University <strong>of</strong> Toronto<br />
Toronto, ON<br />
15:10-17:10 Workshops & PSN Sessions<br />
Ateliers et séances des RSP<br />
1. Simulation Game: Building Pharmacy<br />
Services from Scratch<br />
SIMCOE/DUFFERIN<br />
Jean-François Bussières, BPharm, MSc, MBA,<br />
FCSHP<br />
CHU Sainte-Justine<br />
Montréal, QC<br />
2. Cardiology PSN<br />
RSP en cardiologie<br />
CONFERENCE B/C<br />
Antiplatelet in 2012 and Beyond<br />
Heather Kertland, BScPhm, PharmD<br />
St. Michael’s <strong>Hospital</strong><br />
Toronto, ON<br />
Antiarrhythmic Drug Safety: Illusion,<br />
Fantasy, and Wishful Thinking?<br />
Dronedarone and Other Disappointments<br />
James E. Tisdale, BScPhm, PharmD, BCPS, FCCP,<br />
FAPhA, FAHA<br />
College <strong>of</strong> Pharmacy, Purdue University<br />
Indianapolis, IN<br />
3. Medication Safety PSN<br />
RSP en sécurité des médicaments<br />
CITY HALL<br />
Current Accreditation Challenges:<br />
Panel Discussion with Representatives <strong>of</strong><br />
Key National Organizations<br />
Janice Munroe, BScPhm - Moderator<br />
Fraser Health Pharmacy Services<br />
Regional Pharmacy Administration<br />
Lanlgey, BC<br />
Joanne Garrah<br />
Health Canada<br />
Ottawa, ON
19<br />
Julie Greenall, RPh, BScPhm, MHSc<br />
ISMP Canada<br />
Toronto, ON<br />
Diana Sarakbi<br />
Accreditation Canada<br />
Ottawa, ON<br />
17:30-19:30 Satellite Symposiums<br />
Dinner included<br />
Symposiums satellites<br />
Dîner inclus<br />
1. Addressing Drug Supply Issues in Canada<br />
and from a Global Perspective<br />
ESSEX BALLROOM<br />
Grace Breen<br />
Hospira Healthcare Corporation<br />
Lake Forest, IL<br />
Beryl Chan<br />
Tina Dematos<br />
Hospira Healthcare Corporation<br />
Montréal, QC<br />
Hosted by Hospira Healthcare Corporation<br />
2. Recognition and Treatment <strong>of</strong><br />
Hyponatremia in the <strong>Hospital</strong> Setting<br />
DOMINION BALLROOM NORTH<br />
Hosted by Otsuka Pharmaceutical Inc.<br />
Wednesday, February 8 • Mercredi 8 février<br />
07:30-15:00 Registration<br />
Inscription<br />
CONCOURSE COAT CHECK<br />
08:00-08:15 Announcements<br />
Annonces<br />
DOMINION BALLROOM<br />
08:15-09:15 CPSI-ISMP Canada Patient Safety Lecture<br />
Conférence sur la sécurité des patients de<br />
l’ICSP et de l’IUSM du Canada<br />
DOMINION BALLROOM<br />
Improving Medication Safety at Transitions<br />
in Care<br />
Chaim Bell, MD, PhD, FRCPC<br />
Li Ka Shing Knowledge Institute<br />
St. Michael’s <strong>Hospital</strong><br />
Toronto, ON<br />
Sponsored by the <strong>Canadian</strong> Patient Safety Institute<br />
and the Institute for Safe Medication Practices<br />
Canada through an unrestricted grant<br />
Commandité par l’Institut canadien sur la sécurité<br />
des patients et l’Institut pour l’utilisation sécuritaire<br />
des médicaments du Canada grâce à une<br />
subvention sans restriction<br />
09:15-10:15 Learning from High Reliability<br />
Organizations to Improve Reliability and<br />
Safety in Health Care<br />
DOMINION BALLROOM<br />
Marlys Christianson, MD, PhD<br />
Rotman School <strong>of</strong> Management<br />
University <strong>of</strong> Toronto<br />
Toronto, ON<br />
10:15-10:45 Break, Posters<br />
Pause, Affiches<br />
DOMINION FOYER<br />
10:55-11:40 Concurrent Sessions<br />
Séances concomitantes<br />
1. New Advances in the Management <strong>of</strong><br />
Metastatic Renal Cell Carcinoma<br />
SIMCOE/DUFFERIN<br />
Shirin Abadi, BScPhm, ACPR, PharmD<br />
BC Cancer Agency<br />
Vancouver, BC<br />
2. Combination Therapy for Problem Gram<br />
Negative Pathogens<br />
CITY HALL<br />
Linda Dresser, PharmD, FCSHP<br />
University Health Network<br />
Toronto, ON<br />
3. The State <strong>of</strong> <strong>Hospital</strong> Pharmacy Practice<br />
in Canada: The Good, The Bad, and the<br />
Perhaps a Bit Ugly (Courtesy <strong>of</strong> the<br />
<strong>Hospital</strong> Pharmacy in Canada 2009/10<br />
Report)<br />
CONFERENCE B/C<br />
Kevin Hall, BScPhm, PharmD, FCSHP<br />
Faculty <strong>of</strong> Pharmacy and Pharmaceutical<br />
Sciences, University <strong>of</strong> Alberta<br />
Edmonton, AB<br />
11:50-12:35 Concurrent Sessions<br />
Séances concomitantes<br />
1. VTE in the ICU<br />
SIMCOE/DUFFERIN<br />
David Williamson, MSc, BCPS<br />
Hôpital du Sacré-Cœur de Montréal<br />
Montréal, QC<br />
2. How will Pharmacogenomics Practically<br />
Impact Patient Care & Practicing<br />
<strong>Pharmacists</strong>: Now and In the Future?<br />
CITY HALL<br />
Anke-Hilse Maitland-van der Zee, PharmD, PhD<br />
Utrecht Institute for Pharmaceutical Services,<br />
Utrecht University<br />
Utrecht, The Netherlands
20<br />
3. What Should a System for the<br />
Recognition <strong>of</strong> Special Areas <strong>of</strong> Practice<br />
Look Like?<br />
CONFERENCE B/C<br />
Arthur Whetstone, EdD, MA, BEd, BA(Hon), RPN<br />
<strong>Canadian</strong> Council on Continuing Education in<br />
Pharmacy<br />
Saskatoon, SK<br />
12:40-14:10 Satellite Symposiums<br />
Luncheon included<br />
Symposiums satellites<br />
Dînr inclus<br />
1. Management <strong>of</strong> New Oral Anticoagulant<br />
Therapy for Stroke Prevention in Atrial<br />
Fibrillation<br />
ESSEX BALLROOM<br />
Kori Leblanc, BScPhm, ACPR, PharmD<br />
Peter Munk Cardiac Centre<br />
Toronto, ON<br />
Claudia Bucci, BScPhm, PharmD, ACPR<br />
Sunnybrook Health Sciences Centre<br />
Toronto, ON<br />
Shaun Goodman, MD, MSc, FRCPC<br />
St. Michael's <strong>Hospital</strong><br />
Toronto, ON<br />
Hosted by Bayer Inc.<br />
2. Prescription Opioid Misuse: What<br />
<strong>Pharmacists</strong> Really Need to Know<br />
CIVIC BALLROOM<br />
Donnie Edwards, RPh, BScPhm<br />
Boggio Pharmacy Ltd.<br />
Port Colborne, ON<br />
Hosted by Purdue Pharma<br />
14:15-15:15 CSHP 2015 Town Hall: Are We on Target for<br />
Pharmacy Practice Excellence?<br />
2 CSHP<br />
Targeting Excellence<br />
in Pharmacy Practice<br />
DOMINION BALLROOM<br />
Carolyn Bornstein, BScPhm, ACPR, FCSHP -<br />
Moderator/Speaker<br />
CSHP 2015 Project Coordinator<br />
Newmarket,ON<br />
Stephen Shalansky, BScPhm, PharmD, ACPR, FCSHP<br />
Providence Healthcare<br />
Vancouver, BC<br />
Emily Muir, BScPhm, ACPR<br />
Horizon Health Network<br />
Saint John, NB<br />
15:25-17:30 Workshops & PSN Sessions<br />
Ateliers et séances des RSP<br />
1. Critical Care PSN<br />
RSP en soins intensifs<br />
SIMCOE/DUFFERIN<br />
Dexmedetomidine: A New Sedative in<br />
the ICU: Balancing Responsibility and<br />
Real Life<br />
Salmaan Kanji, BScPhm, PharmD, ACPR<br />
The Ottawa <strong>Hospital</strong><br />
Ottawa <strong>Hospital</strong> Research Institute<br />
Ottawa, ON<br />
What's New, What's Next? 1 Year<br />
Experience for an Antimicrobial<br />
Stewardship <strong>Program</strong> in a Community<br />
<strong>Hospital</strong> Intensive Care Unit (ICU)<br />
Kelly Walker, BSP<br />
Toronto East General <strong>Hospital</strong><br />
Toronto, ON<br />
Jaclyn Litynsky, BCPS, PharmD<br />
Toronto East General <strong>Hospital</strong><br />
Toronto, ON<br />
2. Pharmacist-in-Training PSN<br />
RSP des pharmaciens en apprentissage<br />
CONFERENCE B/C<br />
Antibiotic Pharmacokinetics and<br />
Pharmacodynamics: Putting the Practical<br />
into Practice<br />
Rosemary Zvonar, BScPhm, ACPR, FCSHP<br />
The Ottawa <strong>Hospital</strong><br />
Ottawa, ON<br />
Miranda So, BSc, BScPhm, PharmD<br />
University Health Network<br />
Toronto, ON<br />
3. What are the Appropriate National<br />
Clinical Pharmacy Key Performance<br />
Indicators (KPI) For <strong>Canadian</strong><br />
<strong>Pharmacists</strong>? (encore)<br />
CONFERENCE D/E<br />
Olavo Fernandes, PharmD, FCSHP<br />
University Health Network<br />
Leslie Dan Faculty <strong>of</strong> Pharmacy<br />
University <strong>of</strong> Toronto<br />
Toronto, ON<br />
Richard Slavik, PharmD, FCSHP<br />
Pr<strong>of</strong>essional Practice Interior Health<br />
University <strong>of</strong> British Columbia<br />
Kelowna, BC<br />
17:30 Close <strong>of</strong> the 43rd Annual Pr<strong>of</strong>essional<br />
Practice Conference<br />
Clôture de la 43 e Conférence annuelle sur la<br />
pratique pr<strong>of</strong>essionnelle
R&E Foundation<br />
Silent Auction<br />
This year’s Research & Education Foundation<br />
Fundraiser at the PPC 2012 will once again be<br />
the popular silent auction. Items will be on<br />
display Sunday, February 5, 2012 inside the Career<br />
Opportunities Evening (Osgoode Hall, Lower<br />
Concourse) and on Monday and Tuesday during the<br />
exhibitor lunches (12:15-13:50) in the Exhibit Hall.<br />
<strong>Final</strong> bids will be tallied at 13:00 on Tuesday. Winners<br />
will be announced at the end <strong>of</strong> the exhibits program.<br />
We request your presence in order to pick up your<br />
item(s). All payments must be made on-site.<br />
Money raised on behalf <strong>of</strong> the R&E Foundation means<br />
you are helping to support the development <strong>of</strong><br />
research skills among practicing hospital pharmacists<br />
as well as research projects and targeted pharmacy<br />
education programs undertaken by CSHP members.<br />
Awards Ceremony<br />
Please join us for our CSHP’s National Awards<br />
Ceremony and Cocktail Reception! It is an<br />
opportunity to congratulate your colleagues,<br />
network, and socialize with members.<br />
This event is open to the public (you do not have to be<br />
registered for the PPC to attend).<br />
Sunday, February 5, 2012 • 16:10-17:50<br />
Essex Ballroom<br />
Cocktails to follow<br />
Career Opportunities<br />
Evening<br />
This annual networking and recruitment event will<br />
take place after the Awards Ceremony on Sunday,<br />
February 5, 2012. Join us in the Osgoode Hall<br />
(new location!) from 18:00-19:30 and chat with hospitals<br />
and other organizations from across the country.<br />
This event is open to the public (you do not have to be<br />
registered for the PPC to attend). Refreshments will be<br />
provided.
22<br />
Speaker Abstracts<br />
Résumés des conférenciers<br />
Sunday, February 5<br />
Dimanche 5 février<br />
Managing Acute Stroke: What You Need To Know<br />
Tania Mysak, BSP, PharmD, Alberta Health Services, Edmonton, AB<br />
The goal <strong>of</strong> this session is to provide pharmacists with a strategy to<br />
manage the top clinical issues patients face in the first days<br />
following an acute stroke.<br />
Stroke is the fourth leading cause <strong>of</strong> death and the leading cause<br />
<strong>of</strong> long term adult disability in Canada. It burdens our health care<br />
system with annual costs <strong>of</strong> at least $6 billion due to<br />
hospitalization, long term care, rehabilitation, drug use and lost<br />
productivity. Over half <strong>of</strong> those costs occur within the first 6<br />
months <strong>of</strong> care and 80% <strong>of</strong> those early costs can be attributed to<br />
the acute hospitalization period. To help manage those costs and<br />
optimize patient care, clinical efforts are focussed on reducing<br />
stroke size, prevention <strong>of</strong> acute complications as well as prevention<br />
<strong>of</strong> early recurrent stroke.<br />
In the hyperacute stage, the goal is to minimize infarct size and<br />
prevent mortality and morbidity. In the acute stage (i.e. the first<br />
days to weeks following acute stroke) patients are exposed to risks<br />
such as venous thromboembolism, infection, depression and<br />
recurrent stroke. While clinical guidelines exist to aid clinicians<br />
navigate these early stages <strong>of</strong> a patient’s recovery, gaps in evidence<br />
require care providers to exercise clinical judgement in areas such<br />
as hypertension management. <strong>Final</strong>ly, clinicians must consider<br />
optimal timing <strong>of</strong> initiation <strong>of</strong> pharmacotherapy for secondary<br />
stroke prevention.<br />
Goals and Objectives<br />
1. To provide pharmacists with an overview <strong>of</strong> management <strong>of</strong><br />
hyperacute and acute stroke, including optimal timing for<br />
initiation <strong>of</strong> secondary stroke prevention strategies.<br />
2. To provide pharmacists context in which guideline<br />
recommendations are made, to enable them to make<br />
patient-specific choices in their practice.<br />
Self-Assessment Questions<br />
1. How would you approach management <strong>of</strong> hypertension in<br />
patients with acute stroke?<br />
2. What is the optimal strategy for prevention <strong>of</strong> venous<br />
thromboembolism in a patient with intracerebral hemorrhage?<br />
Extended Infusion Beta Lactams: A Primer on<br />
Why, When, and Mainly How<br />
Sandra A.N. Walker, BSc, BScPhm, ACPR, PharmD, FCSHP,<br />
Sunnybrook Health Sciences Centre, Toronto, ON<br />
The purpose <strong>of</strong> this concurrent session is to provide a brief<br />
overview about the use <strong>of</strong> extended infusion (EI) β-lactams.<br />
There is accumulating interest and support for the use <strong>of</strong> EI<br />
β-lactams. β-lactams have time dependent bacterial killing, where<br />
the rate and extent <strong>of</strong> killing is independent <strong>of</strong> increases in<br />
concentration <strong>of</strong> the antibiotic; but rather, is determined by the<br />
length <strong>of</strong> time that unbound drug remains above the minimum<br />
inhibitory concentration <strong>of</strong> the bacteria. The bactericidal activity is<br />
optimal when the time that the β-lactam concentration remains<br />
above the MIC (T>MIC) for at least 40-70% <strong>of</strong> the dosing interval.<br />
However, the short half-life <strong>of</strong> most β-lactams necessitates frequent<br />
intermittent dosing to achieve this pharmacokinetic /<br />
pharmacodynamic target. The use <strong>of</strong> EI β-lactams provides a<br />
feasible method <strong>of</strong> optimizing T>MIC compared to intermittent<br />
infusion.<br />
Goals and Objectives<br />
1. To review the rationale for EI β-lactams, with a summary <strong>of</strong><br />
existing evidence (The Why).<br />
2. To identify when EI β-lactams may be beneficial.<br />
3. To provide practical information on how to use EI β-lactams in<br />
patient care.<br />
Self-Assessment Questions<br />
1. Why is there an interest in using EI β-lactams?<br />
2. Under what circumstances may EI β-lactams be most beneficial<br />
for patients?<br />
3. How would you determine appropriate dosing for a specific<br />
β-lactam using published pharmacokinetic data, in the absence<br />
<strong>of</strong> published recommendations for EI?<br />
Smartphones: A Novel ‘App’roach to Patient Care<br />
Sean P. Spina, BScPhm, ACPR, PharmD, Vancouver Island Health<br />
Authority, Victoria, BC<br />
The goal <strong>of</strong> this session is to provide the pharmacist with an<br />
overview <strong>of</strong> how smartphone technology can be incorporated into<br />
patient care.<br />
Over the past decade, the use <strong>of</strong> technology in healthcare has<br />
grown exponentially. The days <strong>of</strong> pharmacists having a desktop<br />
computer in an <strong>of</strong>fice and then carrying a drug information<br />
reference in their labcoat pocket have been transformed into<br />
pharmacists carrying powerful multifunctional mobile devices in<br />
their pockets to the bedside. The smartphone has become the 21st
23<br />
century workhorse for timely communication, obtaining efficient<br />
drug information, organizing schedules and providing bedside<br />
decision support tools to the pharmacist. The smartphone has<br />
become an integral part <strong>of</strong> many pharmacist’s personal and<br />
pr<strong>of</strong>essional life.<br />
Incorporating technology into clinical practice can be<br />
overwhelming at times. This session will outline how smartphones<br />
can be effectively incorporated into clinical practice including a<br />
review <strong>of</strong> common clinically useful applications.<br />
Goals and Objectives<br />
1. To provide pharmacists with an overview <strong>of</strong> how smartphone<br />
technology can be incorporated into patient care.<br />
2. To provide pharmacists with practical suggestions <strong>of</strong> ways that<br />
smartphones can improve their daily workflow.<br />
3. To provide pharmacists with a glimpse <strong>of</strong> the technology which<br />
will be available in the near future.<br />
Self-Assessment Questions<br />
1. List 5 smartphone applications which will improve your worklife.<br />
2. Describe how smartphone technology can keep pharmacists up<br />
to date with the literature.<br />
3. Outline how smartphone technology can allow pharmacists to<br />
work more efficiently.<br />
Research Design for Dummies: Chart Review<br />
Studies<br />
Ross T. Tsuyuki, BScPhm, PharmD, MSc, FCSHP, FACC. Faculty <strong>of</strong><br />
Medicine and Dentistry, University <strong>of</strong> Alberta, Edmonton, AB<br />
Retrospective chart review studies are popular in pharmacy<br />
research and are an excellent choice for many (but not all) research<br />
questions.<br />
The purpose <strong>of</strong> this presentation is to discuss the methodologic<br />
principles necessary to conduct high quality chart review studies,<br />
including sampling, case definition, sample size, blinding,<br />
abstractor training, standardized data collection forms, abstractor<br />
monitoring, and testing for agreement.<br />
This workshop is for residents, those who supervise residents, and<br />
pharmacists who see clinical problems and would like to be able to<br />
address them by conducting their own studies.<br />
I also hope you will bring along your ideas for chart review studies<br />
or studies you are working on or have completed yourself. Or,<br />
bring along a published chart review study and we can review and<br />
critique it together.<br />
Goals and Objectives<br />
1. To understand the strength and weaknesses <strong>of</strong> chart review<br />
studies<br />
2. To review the methodologic features necessary to design and<br />
conduct high quality chart review studies.<br />
Self-Assessment Questions<br />
1. What kind <strong>of</strong> research questions are best addressed using a<br />
chart review study design?<br />
2. What are the limitations <strong>of</strong> using convenience sampling <strong>of</strong> cases<br />
for chart review studies?<br />
Antipsychotic Use Circa 2012: What have we<br />
Learned Regarding their Efficacy and Safety for<br />
Behavioural and Psychological Symptoms <strong>of</strong><br />
Dementia (BSPD)?<br />
Carlos Rojas-Fernandez, PharmD, University <strong>of</strong> Waterloo School <strong>of</strong><br />
Pharmacy, RBJ-UW Schlegel Research Institute for Ageing,<br />
McMaster University School <strong>of</strong> Medicine and The Centre for Family<br />
Medicine, Kitchener, ON<br />
The purpose <strong>of</strong> this presentation is to provide a historical<br />
perspective on the safety and efficacy <strong>of</strong> antipsychotic drugs for<br />
management <strong>of</strong> BPSD, and put these findings into an appropriate<br />
contemporary clinical context.<br />
Antipsychotic medications have been used for over 25 years for<br />
treatment <strong>of</strong> behavioural and psychological symptoms <strong>of</strong> dementia<br />
(BSPD). In the 1990s, atypical antipsychotic drugs (AAPs) largely<br />
supplanted older antipsychotics due to their perceived safety<br />
advantage. In the early 21st century it became evident that AAPs<br />
were associated with a different set <strong>of</strong> adverse outcomes, namely<br />
metabolic side effects. Additionally, it was revealed that they were<br />
associated with a higher risk <strong>of</strong> cerebrovascular adverse events<br />
(CVAEs) and mortality in patients with BPSD (compared to<br />
placebo). These findings led regulatory agencies to issue safety<br />
warnings regarding their use in this population in 2005.<br />
Subsequently, a plethora <strong>of</strong> pharmacoepidemiologic studies were<br />
published which continued to clarify these risks, as well as identify<br />
additional risks associated with use <strong>of</strong> these drugs in patients with<br />
BPSD. These risks include increased risk <strong>of</strong> pneumonia, diabetes,<br />
venous thromboembolic events, and cognitive impairment.<br />
Nevertheless, evidence to support use <strong>of</strong> other pharmacological<br />
strategies for moderate to severe psychosis or aggression in this<br />
population are lacking. Of equal, if not greater interest, are studies<br />
that have documented successful withdrawal <strong>of</strong> antipsychotic<br />
drugs in patients with BPSD after an adequate treatment duration,<br />
which is consistent with the natural course <strong>of</strong> dementia. While a<br />
matter <strong>of</strong> debate, the manner in which antipsychotics are used in<br />
contemporary (and judicious) practice in essence, has not changed,<br />
and, until improved alternatives are brought forth, likely should not<br />
change. Thus, appropriate use <strong>of</strong> antipsychotics, in safe and<br />
effective doses, and for time-limited periods should not be viewed<br />
upon in a pejorative manner.<br />
Goals and Objectives<br />
1. To provide pharmacists a historical perspective regarding the<br />
associations between antipsychotics, mortality and<br />
cerebrovascular events in patients with dementia.<br />
2. To discuss, in summary form, evidence for the efficacy <strong>of</strong><br />
antipsychotics for BPSD.
24<br />
3. To put recent safety data regarding antipsychotics in context <strong>of</strong><br />
contemporary practice.<br />
Self-Assessment Questions<br />
1. What are two potential key safety concerns for using<br />
antipsychotics in patients with BPSD?<br />
2. Which atypical antipsychotics have the most evidence for<br />
efficacy for BPSD?<br />
3. Describe data that support discontinuation <strong>of</strong> psychotropic drugs<br />
in stable patients with BPSD.<br />
Blood Pressure and Diabetes in the Elderly: Moving<br />
Targets<br />
Naomi Dore, BScH, MSc, BScPhm, Hamilton Health Sciences,<br />
Hamilton ON<br />
The purpose <strong>of</strong> this session is to discuss blood pressure and<br />
diabetes targets in very elderly patients. Though the very elderly are<br />
<strong>of</strong>ten treated to the same targets as identified for younger<br />
patients, no trials have been designed to examine treatment<br />
targets in this population.<br />
In younger patients (aged 60-79), treating hypertension to a SBP<br />
80 years treated to achieve a target <strong>of</strong> 150/80 mmHg<br />
showed benefit in stroke reduction, but this evidence cannot be<br />
applied to the sick or frail elderly population. In the general<br />
>80-year population the same degree <strong>of</strong> anti-hypertensive<br />
treatment may be associated with an increase in mortality, and<br />
lower SBP (
25<br />
Student Insights from Bottom-up and Top-down<br />
Approaches in Global Health<br />
Matt Koehler, BScPhm, RPh, Shoppers Drug Mart, Thunder Bay, ON<br />
The purpose <strong>of</strong> this session is to explore the experience <strong>of</strong> a<br />
pharmacy student in global health initiatives. The initiatives <strong>of</strong><br />
focus include projects with a “bottom-up” approach working at a<br />
hospital in Gambia, West Africa, and a “top-down” approach<br />
working at the WHO headquarters in Geneva, Switzerland.<br />
In The Gambia, the speaker participated in a project under the<br />
direction <strong>of</strong> <strong>Canadian</strong> hospital pharmacist Jennifer Dyck, focused<br />
on inventory management and education. There, they worked with<br />
staff and students <strong>of</strong> the regional hospital, and the national drug<br />
and medical supply procurement and distribution center.<br />
Following this experience, the speaker completed an internship<br />
with the Good Governance for Medicines program in the WHO’s<br />
department <strong>of</strong> Essential Medicines and Pharmaceutical Policy. The<br />
goal <strong>of</strong> the program is to contribute to health system<br />
strengthening and prevent corruption by promoting good<br />
governance in the pharmaceutical sector. This is achieved largely<br />
through partnering with state ministries <strong>of</strong> health in improving<br />
transparency and accountability in medicine regulatory and supply<br />
management systems.<br />
Student initiatives, specifically related to global health will also be<br />
discussed in broad terms, paying particular interest in aspects <strong>of</strong><br />
meaningful and lasting impact.<br />
Goals and Objectives<br />
1. To teach pharmacists and students about various types <strong>of</strong><br />
student initiatives in global health, including successes and<br />
challenges.<br />
2. To demonstrate the impact a student can have on a project, as<br />
well as the impact such projects can have on the student and<br />
mentor themselves.<br />
3. To describe ways pharmacists and students can get involved in<br />
global health initiatives.<br />
Self-Assessment Questions<br />
1. Name an important initial consideration in developing a<br />
successful global health initiative.<br />
2. Describe what is mean by a top-down and bottom-up approach<br />
in global health initiatives.<br />
Anticoagulation Risk Management: Practical<br />
Implications for <strong>Pharmacists</strong><br />
Cynthia Brocklebank, BScPhm, PharmD, ACPR, Alberta Health<br />
Services, Calgary, AB<br />
Optimizing pharmacist management <strong>of</strong> high-risk medication<br />
regimens, which include anticoagulants, in ambulatory and<br />
specialty clinics is a goal <strong>of</strong> CSHP 2015. Patient assessment for risk<br />
<strong>of</strong> thrombosis and bleeding is a cornerstone <strong>of</strong> good<br />
anticoagulation practice regardless <strong>of</strong> the indication. Patient<br />
assessment for bleeding risk in an ambulatory setting can be<br />
challenging, particularly as risk factors change, and depending on<br />
the clinic service delivery model.<br />
Factors contributing to increased bleeding in anticoagulated<br />
patients have been well documented. Variations <strong>of</strong> the Outpatient<br />
Bleeding Risk Score have been used by ambulatory programs for<br />
years to categorize bleeding risk. More recently, the<br />
HEMORR2HAGES and HASBLED scoring tools have been used in<br />
atrial fibrillation populations. Recent published <strong>Canadian</strong> guidelines<br />
in atrial fibrillation have also incorporated thrombosis risk<br />
assessment tools for clinicians to assist with anticoagulation<br />
decision making. CHADS2 and CHADS2VaSc scores have been<br />
validated for estimating the annual stroke risk, <strong>of</strong>f anticoagulants,<br />
for patients with non-valvular atrial fibrillation. Estimating<br />
thrombosis risk for other anticoagulation indications is much less<br />
formalized but equally important.<br />
The purpose <strong>of</strong> this presentation is to provide an overview <strong>of</strong><br />
thrombosis and bleeding risks using a case based approach, and<br />
outline strategies for integrating risk assessment into ambulatory<br />
care pharmacist anticoagulation practice.<br />
Goals and Objectives<br />
1. Define factors that increase bleeding risk in an anticoagulated<br />
patient.<br />
2. Apply thrombosis and bleeding risk scores to an atrial fibrillation<br />
case example.<br />
3. Consider strategies for incorporating bleeding and thrombosis<br />
risk assessment and reassessment into an ambulatory care<br />
pharmacy practice.<br />
Self-Assessment Questions<br />
1. Patient C.D. is a 90 year old female with a past medical history<br />
that includes: hypertension, CHF, and atrial fibrillation. She has<br />
fallen twice at home, and with one <strong>of</strong> those events her physician<br />
queried whether or not she also had a TIA. What<br />
anticoagulation strategy is best for this patient?<br />
2. What other risk factors, that are not included in the HASBLED<br />
scoring system, should be considered when assessing a patient’s<br />
bleeding risk with anticoagulation.<br />
New Anticoagulants for Stroke Prevention in Atrial<br />
Fibrillation<br />
Jennifer Pickering, BScPhm, ACPR, Hamilton Health Sciences<br />
Centre, Hamilton, ON<br />
Atrial fibrillation (AF) affects approximately 200,000 to 250,000<br />
<strong>Canadian</strong>s and is responsible for approximately 1 in 5 <strong>of</strong> all strokes.<br />
Of these 20% will result in death and 60% will result in disability.<br />
Registries show us that only 50-60% <strong>of</strong> eligible patients receive<br />
warfarin therapy. Those patients who are receiving warfarin<br />
therapy it is important that the time in therapeutic range is greater<br />
than 60% which can be difficult to obtain given the variability in<br />
response to warfarin. In the past few years, new antithrombotic<br />
agents (dabigatran, rivaroxaban and apixaban) have published data<br />
<strong>of</strong>fering AF patients improved options for care. The purpose <strong>of</strong> this<br />
talk is to discuss the clinical evidence for, and pharmacological
26<br />
differences <strong>of</strong>, these new agents and also the challenges they bring<br />
to practice.<br />
Goals and Objectives<br />
1. Be familiar with current knowledge regarding new anticoagulant<br />
treatment options for patients with AF<br />
2 Discuss some <strong>of</strong> the challenges and opportunities these agents<br />
(dabigatran, rivaroxaban, apixaban) bring in management <strong>of</strong> AF<br />
patients.<br />
Self-Assessment Questions<br />
1. List at least 3 pharmacological differences between dabigatran,<br />
rivaroxaban and apixaban<br />
2. Mr. A.S. is currently taking dabigatran 150mg po bid. His<br />
CHADS2 is 2. He is booked for cardiac bypass surgery this<br />
admission. He has normal renal function. What is the<br />
recommendation for stopping dabigatran prior to surgery?<br />
Monday, February 6<br />
Lundi 6 février<br />
New recommendations from <strong>Canadian</strong> Task Force<br />
and <strong>Canadian</strong> Collaboration for Immigrant and<br />
Refugee Health<br />
Kevin Pottie, MD, MClSc, Departments <strong>of</strong> Family Medicine and<br />
Clinical Epidemiology and Community Medicine, University <strong>of</strong><br />
Ottawa, Ottawa, ON<br />
Immigrant and refugee health needs may differ significantly from<br />
those <strong>of</strong> native-born populations. Proactive interventions for<br />
preventable and treatable disease <strong>of</strong>fer an opportunity to reduce<br />
emerging health inequities that are <strong>of</strong>ten aggravated by limited<br />
local access to health care. But which migrants are most at risk for<br />
decline in health and which require special attention? Which<br />
conditions require tailored clinical recommendations?<br />
The <strong>Canadian</strong> Collaboration for Immigrant and Refugee Health<br />
(CCIRH) combined the AGREE best practice framework for<br />
guidelines, Cochrane Evidence Review Methods and the GRADE<br />
approach to devise evidence based clinical guidelines for<br />
immigrants and refugees. CCIRH guidelines differ from other<br />
guidelines because <strong>of</strong> their insistence on finding evidence for clear<br />
benefits before recommending routine interventions and in their<br />
explicit detailing <strong>of</strong> values and preference that influence<br />
recommendation statements.<br />
For example, in the context <strong>of</strong> possible asymptomatic intestinal<br />
parasites, the CCIRH guidelines recommend serology testing for<br />
parasites with associated morbidity and mortality (for example,<br />
strongyloides and schistosoma) rather than the traditional series <strong>of</strong><br />
stool tests given the finding that most tropical worms and parasites<br />
will resolve once the person has left the endemic region and this<br />
marks a significant shift in current clinical practice. Content focuses<br />
on four areas: infectious diseases; mental health and maltreatment;<br />
chronic and noncommunicable diseases; and women’s health.<br />
Detailed evidence reviews on specific illnesses and conditions<br />
including diabetes, PTSD, malaria, hepatitis, vision and dental<br />
disorders, provide an opportunity to advocate for effective<br />
interventions for all migrants and the evidence-base toward<br />
international migrant health guidelines.<br />
Goals and Objectives<br />
1. To provide pharmacists with an introduction to the “GRADE”<br />
approach for developing clinical guidelines<br />
2. To introduce pharmacists to new evidence based<br />
recommendations for immigrants and refugees<br />
Self-Assessment Questions<br />
1. What are the factors that increase the risk for poor health<br />
outcomes for migrants?<br />
2. Which conditions require interventions for which pharmacists<br />
should be aware?<br />
Total Parenteral Nutrition for Pediatrics: A<br />
Pharmacy Perspective<br />
Vijay P.A. Rasaiah, RPh, BScPhm, MSc, BSc (Hon), Staff Pharmacist,<br />
Department <strong>of</strong> Pharmacy, The <strong>Hospital</strong> for Sick Children, Toronto,<br />
ON<br />
This session will review some <strong>of</strong> the challenges facing pharmacists<br />
who compound Total Parenteral Nutrition (TPN) for pediatric<br />
patients.<br />
Pediatric patients have high nutritional requirements for growth<br />
and development. TPN is a life-saving therapy for many patients<br />
who are unable to meet these requirements through traditional<br />
enteral routes. TPN is compounded using macronutrients (protein,<br />
carbohydrate, fat, and water) and micronutrients (calcium,<br />
phosphorus, magnesium, etc). <strong>Pharmacists</strong> can play an important<br />
role in prescribing, compounding, and administering TPN by<br />
working collaboratively with nurses, dieticians, and physicians.<br />
Many pediatric patients also have complex therapeutic needs<br />
requiring long-term treatment with TPN. Although TPN is an<br />
essential part <strong>of</strong> the therapeutic plan <strong>of</strong> care for these patients, it<br />
may contribute to various adverse complications (such as infection<br />
and parenteral nutrition-associated cholestasis). <strong>Pharmacists</strong> may<br />
play an important role in customizing TPN compounds for these<br />
patients in order to optimize nutritional support and minimize the<br />
risk <strong>of</strong> adverse complications.<br />
Goals and Objectives<br />
1. To describe the pharmacist’s role in compounding TPN in a large<br />
pediatric hospital.
27<br />
2. To explain some <strong>of</strong> the complications <strong>of</strong> TPN in pediatric<br />
patients.<br />
Self-Assessment Questions<br />
1. What is the importance <strong>of</strong> typical components <strong>of</strong> TPN for<br />
pediatric patients?<br />
2. What are some <strong>of</strong> the ingredients in TPN that are associated<br />
with adverse complications?<br />
Controversies in Diabetes Management: Are we<br />
ADVANCE-ing our Knowledge and Treatment<br />
ACCORD-ingly?<br />
Anar Dossa, BScPhm, PharmD, CDE, Vancouver General <strong>Hospital</strong>,<br />
Vancouver, BC<br />
The purpose <strong>of</strong> this session is to address current clinical<br />
controversies in diabetes management.<br />
In the last 2-3 years several landmark trials have been published<br />
increasing our knowledge base in the area <strong>of</strong> diabetes<br />
management. The United Kingdom Prospective Diabetes Study<br />
(UKPDS) and the Diabetes Control and Complications (DCCT) trials<br />
demonstrated that microvascular, not macrovascular complications<br />
can be reduced with intensive control. The A1c targets achieved in<br />
these trials was 7% in the UKPDS study and 7.4% in the DCCT<br />
study.<br />
Most diabetes patients, however, die <strong>of</strong> macrovascular causes. The<br />
Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial<br />
was designed to investigate if ‘normalizing’ the A1c, that is, aiming<br />
for an A1c <strong>of</strong> under 6%, would reduce macrovascular<br />
complications. This trial was stopped early due to the increased<br />
mortality risk.<br />
The Action in Diabetes and Vascular Disease:Preterax and<br />
Diamicron MR Controlled Evaluation (ADVANCE) trial was also<br />
looking to see if achieving a lower A1c (< 6.5%) would reduce<br />
microvascular and/or macrovascular complications. Aiming for the<br />
lower A1c did reduce nephropathy but not macrovascular<br />
outcomes. Mortality was not increased in this trial.<br />
The ACCORD blood pressure trial demonstrated that a systolic<br />
target <strong>of</strong>
28<br />
To TREAT or not to TREAT: Making Sense <strong>of</strong> ESAs<br />
and Targets in CKD<br />
Amy Sood, BScPhm, PharmD, Manitoba Renal <strong>Program</strong>, St.<br />
Boniface <strong>Hospital</strong>, Winnipeg, MB<br />
Erythropoiesis-stimulating agents (ESAs) have been essential for the<br />
treatment <strong>of</strong> anemia <strong>of</strong> chronic kidney disease (CKD). Treating to<br />
maintain a hemoglobin target <strong>of</strong> 110 to 120 g/L has been widely<br />
practiced and supported by guidelines. The results <strong>of</strong> previous<br />
studies have shown either no benefit or increased risk <strong>of</strong><br />
cardiovascular events with higher hemoglobin targets. With the<br />
recent publication <strong>of</strong> the TREAT study, the debate on hemoglobin<br />
targets has been stirred up again.<br />
On June 24, 2011, the U.S. Food and Drug Administration (FDA)<br />
released a Safety Communication with modified recommendations<br />
for more conservative dosing <strong>of</strong> ESAs in CKD. Among their<br />
recommendations, they state that the lowest dose <strong>of</strong> ESA to avoid<br />
red blood cell transfusions should be used. In addition, they<br />
recommend reducing or interrupting the ESA dose when the<br />
hemoglobin level exceeds 100 g/L in CKD patients not on dialysis<br />
or 110 g/L in CKD patients on dialysis. In the U.S., the<br />
manufacturers have also changed their labeling <strong>of</strong> ESAs to reflect<br />
the FDA’s recommendations. The previous target range for<br />
hemoglobin levels in CKD patients has been removed.<br />
The purpose <strong>of</strong> this session is to critically analyze the evidence to<br />
determine whether these FDA recommendations make sense and<br />
to help you determine whether these recommendations should be<br />
adopted in your practice.<br />
Goals and Objectives<br />
1. To re-examine the evidence for ESAs in CKD in light <strong>of</strong> the new<br />
FDA recommendations.<br />
2. To assist pharmacists in determining whether they should adopt<br />
these new FDA recommendations in their practice.<br />
Self-Assessment Questions<br />
1. Does the evidence support the FDA’s new recommendations on<br />
dosing <strong>of</strong> ESAs in CKD?<br />
2. What risks and benefits should I discuss with patients with CKD<br />
before initiating ESA therapy?<br />
Beyond Statins: Treating Dyslipidemia and Residual<br />
Cardiovascular Risk with Other Lipid-Lowering<br />
Agents<br />
Glen J. Pearson, BSc, BScPhm, PharmD, FCSHP; Division <strong>of</strong><br />
Cardiology, University <strong>of</strong> Alberta, Manzankowski Alberta Heart<br />
Institute, Edmonton, AB<br />
Cholesterol treatment targets levels recommended in current<br />
guidelines have been defined from randomized control trials. The<br />
2009 CCS Dyslipidemia Guidelines suggest as a primary target,<br />
lowering the low-density lipoprotein (LDL) cholesterol to
29<br />
may guide the selection process <strong>of</strong> appropriate clinical KPI not<br />
possible before. A national working group has recently been<br />
formed with representatives from across Canada with the aim to<br />
develop national clinical pharmacy KPI for hospital pharmacists via<br />
a systematic evidence-informed consensus process. It is envisioned<br />
that these consensus KPI will be generalizable and adoptable in all<br />
hospital settings (small, large, urban, rural, community and<br />
academic centres). In this workshop, feedback will be pro-actively<br />
gathered on: the process and criteria to select KPI, candidate KPI as<br />
well as practical advantages and limitations for each.<br />
One health region’s experience with the development and<br />
implementation <strong>of</strong> a clinical KPI monitoring system will be<br />
presented to generate ideas and discussion. Embedding quality<br />
improvement (balancing, process, or outcome) measures to<br />
prioritize clinical services and track clinical performance has<br />
important rationale but also challenging barriers. Resolution <strong>of</strong><br />
DTPs (process measure) with pharmaceutical care is essential to a<br />
pharmacist’s role, and is a standardized, accepted surrogate <strong>of</strong><br />
clinical outcomes proven to affect important dimensions <strong>of</strong> quality.<br />
These can serve as the foundation for development <strong>of</strong> clinical KPIs<br />
that are collected using handheld personal data assistant (PDA)<br />
device. Standardized analyses can benchmark the value and<br />
productivity <strong>of</strong> clinical services.<br />
Goals and Objectives<br />
1. To provide pharmacists with an overview <strong>of</strong> the rationale,<br />
development, and implementation <strong>of</strong> a clinical KPI monitoring<br />
system from one health region along with the PDA tool used to<br />
collect the information.<br />
2. To facilitate an interactive discussion to gather feedback on the<br />
national process and criteria to select KPI, potential candidate<br />
KPI and practical definitions, advantages and limitations for each<br />
measure.<br />
Self-Assessment Questions<br />
1. Outline the background and rationale for why it is important to<br />
implement clinical pharmacy KPI measures<br />
2. List 3 potential clinical pharmacy KPI metrics and practical<br />
advantages and limitations for each.<br />
3. List some ideal attributes and anticipated barriers to the<br />
implementation <strong>of</strong> a KPI system.<br />
Chemotherapy-Induced Nausea and Vomiting in<br />
Children: An Evidence-Based Approach<br />
L.L. Dupuis, RPh, ACPR, MScPhm, FCSHP, The <strong>Hospital</strong> for Sick<br />
Children, Toronto, ON<br />
Chemotherapy-induced nausea and vomiting (CINV) continue to be<br />
negative influences on the lives <strong>of</strong> children with cancer. Although<br />
acute antineoplastic-induced vomiting may improve over the<br />
course <strong>of</strong> treatment, antineoplastic-induced nausea may actually<br />
become more problematic. The use <strong>of</strong> evidence-based or<br />
consensus-based guidelines for antiemetic selection has been<br />
shown to improve control <strong>of</strong> acute CINV in adults. Evidence-based<br />
guidelines for the classification <strong>of</strong> antineoplastic emetogenicity and<br />
the selection <strong>of</strong> antiemetic agents for children have now been<br />
developed under the auspices <strong>of</strong> the Pediatric Oncology Group <strong>of</strong><br />
Ontario (POGO).<br />
The methods used to develop the POGO CINV guidelines will be<br />
presented. Recommendations regarding the emetic risk <strong>of</strong><br />
antineoplastic regimens in children will be reviewed as will<br />
recommendations regarding antiemetic selection to optimize CINV<br />
control in children. The use <strong>of</strong> aprepitant in children and antiemetic<br />
options for children who cannot receive corticosteroids will be<br />
discussed. Research gaps in the available evidence base informing<br />
the POGO CINV guidelines will be highlighted.<br />
Goals and Objectives<br />
1. To inform pharmacists regarding the importance <strong>of</strong> CINV control<br />
in children<br />
2. To provide pharmacists with an evidence-based approach to the<br />
prevention <strong>of</strong> acute CINV in children<br />
Self-Assessment Questions<br />
1. How does the classification <strong>of</strong> the emetogenicity <strong>of</strong><br />
antineoplastic agents differ between adults and children?<br />
2. What antiemetic strategies are recommended to children who<br />
are receiving antineoplastic agents <strong>of</strong> high, moderate, low and<br />
minimal emetogenic risk?<br />
3. What is the role <strong>of</strong> aprepitant in controlling CINV in children?<br />
Pain, Pain, Go Away. Don’t Come Back Another<br />
Day! Exploring Treatment Options and Strategies<br />
for the Management <strong>of</strong> Pediatric Chronic Pain<br />
Regis Vaillancourt, OMM, OD, CD, BPhm, PharmD, FCSHP,<br />
Children’s <strong>Hospital</strong> <strong>of</strong> Eastern Ontario, Ottawa, ON<br />
The goal <strong>of</strong> this session is to provide pharmacists with an<br />
understanding <strong>of</strong> current practices and treatment strategies when<br />
managing chronic pediatric pain conditions.<br />
During this module the emerging and increasing practice <strong>of</strong><br />
multidisciplinary care will be discussed. Specifically, the topic <strong>of</strong>:<br />
The Three P’s <strong>of</strong> Pediatric Pain Management: Pharmacology,<br />
Physical therapy and Psychotherapy will be explored and how<br />
integrating these three elements have affected our practice, patient<br />
outcomes and relationships with other care providers.<br />
This presentation will also provide pharmacists with an overview <strong>of</strong><br />
pharmacological approaches to pain management with a focus on<br />
Chronic Regional Pain Syndrome (CRPS). Additionally, the role <strong>of</strong><br />
natural health products used to manage pain and its secondary<br />
symptoms such as insomnia will also be addressed. Evidence for<br />
each <strong>of</strong> these therapies will be presented for review and discussion.<br />
Goals and Objectives<br />
1. To provide pharmacists with an overview <strong>of</strong> the three P approach<br />
to pediatric chronic pain management<br />
2. To describe the role <strong>of</strong> natural health products in the treatment<br />
<strong>of</strong> pediatric chronic pain
30<br />
3. To outline the pharmacological approaches to managing chronic<br />
pain in children<br />
Self-Assessment Questions<br />
1. What is the role <strong>of</strong> magnesium in the management <strong>of</strong> chronic<br />
pain?<br />
2. What is the benefit <strong>of</strong> using pregabaline in chronic pain?<br />
3. What is the relationship between vitamin D anc chronic pain?<br />
Practical Approaches to Reducing Polypharmacy in<br />
the Elderly: An Interactive Workshop<br />
Debbie Kwan, BScPhm, MSc, FCSHP, Toronto Western <strong>Hospital</strong>,<br />
Family Health Team, Toronto, ON; Barbara Farrell, BScPhm,<br />
PharmD, FCSHP, Bruyère Continuing Care, Ottawa, ON<br />
The <strong>Canadian</strong> National Population Health Survey showed that ≥ 5<br />
medications are used by 53% <strong>of</strong> seniors residing in health care<br />
institutions and 13% <strong>of</strong> community dwelling seniors.(1) Multiple<br />
medication use is associated with increased non-adherence,<br />
adverse reactions, fall risk, medication errors, and inappropriate<br />
prescribing.(2,3,4) Several approaches to screening for and<br />
managing polypharmacy have been studied but are not routinely<br />
implemented in practice.(5)<br />
Polypharmacy in the elderly is a major public health issue.<br />
<strong>Pharmacists</strong> must take responsibility for identifying prescribing<br />
cascades, reducing un-necessary medications, managing<br />
medication adverse effects and reducing pill burden. We are best<br />
suited to work with prescribers and their elderly patients to<br />
minimize polypharmacy.<br />
This interactive workshop will discuss practical approaches to<br />
addressing polypharmacy in the frail elderly.<br />
Participants will work through several cases designed to highlight<br />
common prescribing cascades and opportunities for interventions<br />
to minimize medication use. Steps to avoid or detect prescribing<br />
cascades, and the use <strong>of</strong> explicit and implicit criteria to ensure<br />
appropriate medication use will be discussed. Adapting guidelines<br />
and targets for the frail elderly population will be highlighted.<br />
Non-pharmacological and interpr<strong>of</strong>essional approaches to<br />
managing symptoms will be presented as alternatives to<br />
medication use. Strategies to safely manage the withdrawal <strong>of</strong><br />
medication will be described. The importance <strong>of</strong> communicating<br />
reasons for medication reduction or simplification, and practical<br />
mechanisms for doing so, will be covered. Participants will leave<br />
the workshop with a toolkit <strong>of</strong> practical tips and suggestions that<br />
will enable them to help their patients prevent or reduce the risks<br />
associated with polypharmacy.<br />
Goals and Objectives<br />
Participants will be able to:<br />
1. Describe the impact <strong>of</strong> polypharmacy on patient health, quality<br />
<strong>of</strong> life and health services utilization<br />
3. Structure an approach to manage patient symptoms and risk,<br />
while minimizing medication use<br />
4. Consider the impact <strong>of</strong> psychosocial issues on managing<br />
polypharmacy<br />
Self Assessment Questions<br />
1. Review a patient’s history to determine whether a prescribing<br />
cascade may have occurred.<br />
2. Summarize the advantages and disadvantages <strong>of</strong> various<br />
screening and prescribing guidelines for the elderly<br />
MRSA Guidelines and Clinical Controversies: A<br />
Practical Overview<br />
Tim T.Y. Lau, PharmD, FCSHP, Vancouver General <strong>Hospital</strong>,<br />
Vancouver Coastal Health, Vancouver, BC<br />
Methicillin-resistant Staphylococcus aureus (MRSA) is a significant<br />
pathogen that causes a range <strong>of</strong> infections in the hospital and the<br />
community setting worldwide. MRSA resistance is encoded by the<br />
mecA gene that changes the conformation <strong>of</strong> the penicillin-binding<br />
protein 2a, conferring resistance to beta-lactam anti-infectives. Two<br />
general types <strong>of</strong> MRSA exist: hospital-associated MRSA (HA-MRSA)<br />
and community-associated MRSA (CA-MRSA). HA-MRSA is<br />
associated with multi-drug resistance, while CA-MRSA appears to<br />
be more susceptible to anti-infectives such as co-trimoxazole,<br />
tetracyclines, and clindamycin. The newer anti-MRSA agents will be<br />
reviewed and other anti-infectives will be highlighted. Common<br />
infections caused by MRSA include skin and s<strong>of</strong>t tissue infections,<br />
bactermia and endocarditis, pneumonia, bone and joint infections,<br />
and central nervous system infections. In 2011, the Infectious<br />
Diseases <strong>Society</strong> <strong>of</strong> America published clinical practice guidelines<br />
for the treatment <strong>of</strong> MRSA. Recommendations on the<br />
management <strong>of</strong> common infections associated with MRSA in<br />
adults will be summarized. Clinical controversies exist with the<br />
treatment <strong>of</strong> MRSA. These include the effectiveness <strong>of</strong> incision and<br />
drainage alone for s<strong>of</strong>t tissue abscesses, the addition <strong>of</strong> rifampin in<br />
skin and s<strong>of</strong>t tissue infections, the use <strong>of</strong> combination therapy for<br />
endocarditis, the superiority <strong>of</strong> linezolid over vancomycin for<br />
pneumonia, and the general effectiveness <strong>of</strong> vancomycin for MRSA<br />
infections.<br />
Goals and Objectives<br />
1. To describe the epidemiology <strong>of</strong> MRSA<br />
2. To understand the differences between HA-MRSA and CA-MRSA<br />
3. To become familiar with the antibiotics used in MRSA treatment<br />
4. To recognize the common infections associated with MRSA<br />
infections<br />
5. To be acquainted with the guidelines on the treatment <strong>of</strong> MRSA<br />
infections<br />
6. To review the clinical controversies with MRSA treatment<br />
2. Identify common prescribing cascades
31<br />
Self-Assessment Questions<br />
1. What is the difference between the treatment <strong>of</strong> HA-MRSA and<br />
CA-MRSA?<br />
2. Is vancomycin still a good drug for treating MRSA infections?<br />
Update on Urinary Tract Infections<br />
Monique Pitre, BScPhm, FCSHP, University Health Network,<br />
Toronto, ON<br />
The purpose <strong>of</strong> this session is to review the diagnostic criteria and<br />
the treatment options for complicated health-care associated<br />
urinary tract infections and highlight the challenges.<br />
The diagnosis and treatment <strong>of</strong> uncomplicated cystitis and<br />
pyelonephritis is well defined and does not pose many challenges.<br />
However, the increasing resistance <strong>of</strong> urinary pathogens to<br />
commonly prescribed antimicrobials does pose treatment<br />
challenges.<br />
The diagnosis and treatment <strong>of</strong> hospitalized patients with<br />
complicated urinary tract infections is less well defined.<br />
Catheter-associated bacteriuria is one <strong>of</strong> the most common<br />
health-care associated infections and results in considerable<br />
antimicrobial use. Urinary tract infections causing bacteremia have<br />
also been associated with increased mortality. Antimicrobial<br />
Stewardship <strong>Program</strong>s can play a major role in determining<br />
appropriateness <strong>of</strong> diagnostic criteria and treatment options. This is<br />
very important for the appropriate treatment <strong>of</strong> the patient and the<br />
ecological impact to the health-care facility. Inappropriate<br />
antimicrobial use in the treatment <strong>of</strong> urinary tract infections can<br />
lead to increased resistance and can become a reservoir for<br />
multi-drug resistant organisms.<br />
Goals and Objectives<br />
1. To review the challenges in diagnosis and treatment <strong>of</strong><br />
complicated urinary tract infections.<br />
2. To identify the role <strong>of</strong> antimicrobial stewardship programs in<br />
developing guidelines for the diagnosis and treatment <strong>of</strong><br />
health-care associated urinary tract infections.<br />
3. To provide data on current resistance patterns in urinary tract<br />
pathogens in Canada and Ontario.<br />
4. To discuss treatment options for multidrug-resistant pathogens.<br />
Self-Assessment Questions<br />
1. Do all positive urine cultures in hospitalized patients require<br />
treatment?<br />
2. How can antimicrobial stewardship programs play a role in<br />
appropriate treatment <strong>of</strong> health-care associated urinary tract<br />
infections?<br />
3. What are the current treatment options for resistant urinary<br />
pathogens?<br />
Top Clinical Papers in General Medicine<br />
Derek Jorgenson, BSP, PharmD, FCSHP, University <strong>of</strong> Saskatchewan,<br />
Saskatoon, SK<br />
Every year dozens <strong>of</strong> new clinical trials are published that have<br />
significant relevance to pharmacists who practice in generalist acute<br />
or ambulatory care settings. To be effective clinicians it is important<br />
be aware <strong>of</strong> these new papers and the impact that they should have<br />
on patient care. This session will provide a detailed critical appraisal<br />
and summary <strong>of</strong> 3-4 <strong>of</strong> the most influential clinical papers published<br />
in the general medicine literature within the last year.<br />
Goals and Objectives<br />
1. Summarize and critically appraise 3-4 <strong>of</strong> the most influential<br />
papers published in the general medicine literature within the<br />
last year.<br />
2. Make specific recommendations regarding how these 3-4 new<br />
papers should change practice.<br />
Self-Assessment Questions<br />
1. Describe one key take-home message from each <strong>of</strong> the papers<br />
summarized during this session?<br />
2. Describe two aspects <strong>of</strong> your practice that you will change<br />
starting tomorrow as a result <strong>of</strong> attending this session?<br />
Tuesday, February 7<br />
Mardi 7 février<br />
Issues and Controversies: Pr<strong>of</strong>essional Integrity &<br />
Conflicts <strong>of</strong> Interest<br />
Judy Chong, BScPhm, The Royal Victoria <strong>Hospital</strong> <strong>of</strong> Barrie, Barrie,<br />
ON – Moderator. Panelists: Peter Loewen, PharmD, Lower<br />
Mainland Pharmacy Services, Vancouver General <strong>Hospital</strong>,<br />
University <strong>of</strong> British Columbia, Vancouver, BC; James E. Tisdale,<br />
PharmD, College <strong>of</strong> Pharmacy, Purdue University School <strong>of</strong><br />
Medicine, Indiana University, Indianapolis, IN; Anne Hiltz, BScPhm,<br />
ACPR, Capital District Health Authority, QEII Health Sciences<br />
Centre, Halifax, NS<br />
By virtue <strong>of</strong> their specialized knowledge and skills, pharmacists are<br />
in a privileged position to make decisions which affect the health<br />
<strong>of</strong> other people. Patients, therefore, expect that pharmacists’<br />
decisions are based primarily on what is in their best interests. In<br />
our complex healthcare environment, pharmacists have the<br />
opportunity to form many different kinds <strong>of</strong> pr<strong>of</strong>essional and<br />
personal relationships with a wide variety <strong>of</strong> people. Each <strong>of</strong> these<br />
relationships has the potential to positively or negatively affect the<br />
pr<strong>of</strong>essional integrity <strong>of</strong> the pharmacist involved. As such,<br />
pharmacists who are interested in maintaining a high degree <strong>of</strong><br />
pr<strong>of</strong>essional integrity are well served by a appreciating the<br />
implications <strong>of</strong> each relationship from this viewpoint.<br />
In this interactive case-based panel discussion, several case<br />
vignettes involving different kinds <strong>of</strong> relationships which may have<br />
positive, neutral, or detrimental effects on the pr<strong>of</strong>essional integrity
32<br />
<strong>of</strong> the pharmacists involved will be explored. These scenarios will<br />
involve inter-pr<strong>of</strong>essional relationships, relationships with industry,<br />
patients, and others. Participants’ views and perspectives will be<br />
invited and debated.<br />
Goals and Objectives<br />
After the session and upon personal reflection, participants should<br />
be able to:<br />
1. Articulate a personal vision for what pr<strong>of</strong>essional integrity means<br />
to them<br />
2. Weigh the benefits and risks <strong>of</strong> entering relationships which may<br />
have implications for their pr<strong>of</strong>essional integrity.<br />
Probiotics for C. difficile Infection: Yes… No…<br />
Maybe? A Review <strong>of</strong> Evidence<br />
Miranda So, BScPhm, PharmD, University Health Network, Toronto,<br />
ON<br />
Clostridium difficile infection (CDI) is a distinct and severe form <strong>of</strong><br />
antibiotic-associated diarrhea (AAD), implicated in 20-30% <strong>of</strong><br />
cases. The association between C. difficile and<br />
pseudomembraneous colitis was first described decades ago,<br />
though CDI remains a major cause <strong>of</strong> nosocomial infections today.<br />
Risk factors include antibiotic use, hospitalization or residence in<br />
long-term care facilities; advanced age and proton pump inhibitor<br />
therapy. Since CDI carries significant mortality, morbidity and<br />
economic burden to society, outbreaks in Canada in recent years<br />
have prompted the calls for multi-modal strategies to tackle this<br />
problem. These include diligent infection control practices; new<br />
antibiotics against C. difficile; antimicrobial stewardship programs<br />
to guide the appropriate use <strong>of</strong> antibiotics; and probiotics, the<br />
“good bugs”, in an attempt to affect the gut flora composition in<br />
the host.<br />
Several probiotics <strong>of</strong> interests include Saccharomyces boulardii;<br />
Lactobacillus spp.; Bifidobacterium bifidum, and their combination.<br />
Although probiotics have long been studied for AAD, their roles in<br />
the prevention and/or treatment <strong>of</strong> CDI remain controversial for<br />
several reasons. First, regimens and formulations have not been<br />
standardized. Second, evidence from clinical trials has been<br />
conflicting, and is <strong>of</strong>ten limited by small sample size, highly<br />
selective study patients, or methodology flaws. Third, the safety <strong>of</strong><br />
probiotics, especially in those with severe comorbidities, has been<br />
called into question following reports <strong>of</strong> fungemia or bacteremia<br />
from probiotic therapy.<br />
This session will provide the clinical context regarding probiotics in<br />
CDI by critically reviewing existing evidence on this subject, as well<br />
as new information from ongoing trial(s).<br />
Goals and Objectives<br />
1. Explain the possible mechanisms <strong>of</strong> action <strong>of</strong> probiotics in CDI.<br />
2. Interpret the evidence supporting and refuting the use <strong>of</strong><br />
probiotics in preventing and treating CDI.<br />
Self-Assessment Questions<br />
1. What are the risk factors <strong>of</strong> developing CDI, its recurrence and<br />
complications?<br />
2. What are probiotics?<br />
CPOE Implementation: Prescription for Success<br />
Pegi Rappaport, BSc, MSc, Toronto East General <strong>Hospital</strong>, Janice<br />
Wells, PharmD, Pharmacy, St. Michael’s <strong>Hospital</strong>, Toronto, ON<br />
Your organization has committed to implementing Computer<br />
Provider Order Entry (CPOE), including medications. This session<br />
will outline important roles that pharmacists should lead, areas<br />
requiring collaboration, and suggestions for measuring impact and<br />
benefits from medication system and patient care perspectives.<br />
<strong>Pharmacists</strong> should contribute actively or lead development <strong>of</strong><br />
evidenced based order sets, and ensure a robust Pharmacy and<br />
Therapeutics process is in place to expedite their review and<br />
approval. <strong>Pharmacists</strong> must collaborate to redesign<br />
inter-pr<strong>of</strong>essional accountabilities and workflows in the new<br />
environment for issues such as medication administration times,<br />
re-assessment <strong>of</strong> medications approaching expiry, integration <strong>of</strong><br />
pharmacy information systems and databases with the hospital<br />
information system, as well as new workflows for validation <strong>of</strong><br />
orders, therapeutic interchange and managing new types or more<br />
complex orders. <strong>Pharmacists</strong> can also contribute to measuring<br />
CPOE impact through metrics such as turn around time, near<br />
misses, proportion <strong>of</strong> telephone orders and compliance with<br />
initiatives such as VTE prophylaxis.<br />
Goals and Objectives<br />
1. To describe leadership and collaborative roles for pharmacists to<br />
support the development, implementation and evaluation <strong>of</strong><br />
CPOE in healthcare organizations.<br />
2. To facilitate sharing and comparing approaches to CPOE in<br />
academic, community and paediatric hospitals.<br />
Self-Assessment Questions<br />
1. The recommended approach to implementing CPOE for<br />
medications is to transition all paper based orders, policies and<br />
processes to electronic. True/ False<br />
2. The practice <strong>of</strong> physicians, nurses and pharmacists is largely<br />
unchanged after CPOE is introduced. True/ False<br />
Management <strong>of</strong> Street Drug Toxicities<br />
Debra A. Kent, PharmD, DABAT, CSPI, B.C. Drug and Poison<br />
Information Centre, B.C. Centre for Disease Control, Provincial<br />
Health Services Authority, Vancouver, BC<br />
The purpose this session is to discuss current street drug use in<br />
Canada, their acute clinical effects and approach to treatment.<br />
Clinical pharmacists should be knowledgeable about current street<br />
drug use and understand the toxicology <strong>of</strong> these substances in<br />
order to enhance patient care in the emergency and critical care
33<br />
setting. Street drug patterns vary by region, and information<br />
volunteered by patients may be unreliable, incomplete or<br />
unobtainable. Literature and media reports from other countries<br />
may not reflect local street drug use patterns in Canada.<br />
The most commonly abused substances in many <strong>Canadian</strong> regions<br />
include ethanol, benzodiazepines, prescription opioids, and<br />
marijuana. These will not be the primary focus <strong>of</strong> this talk.<br />
Discussion in this session will highlight toxicity and management <strong>of</strong><br />
exposures to ecstasy, methamphetamine, cocaine, GHB and<br />
ketamine. While use varies across Canada, toxicity and<br />
management required are similar. Newer synthetic designer drugs<br />
will also be discussed including the piperazines (e.g., BZP), the<br />
tryptamines (e.g., 5-MeO-DiPT, “foxy methoxy”), the<br />
phenethylamines (e.g., cathinone, mephedrone, “bath salts”), and<br />
the synthetic cannabinoids (“spice”).<br />
Life-threatening toxicities <strong>of</strong> these agents range from extreme<br />
hyperthermia, acute kidney injury, coagulopathy, metabolic<br />
acidosis, hypertension and dysrhythmias to CNS and respiratory<br />
depression, hyponatremia and cerebral edema. Mechanisms <strong>of</strong><br />
acute toxicity and approach to management will be discussed.<br />
Goals and Objectives<br />
1. To discuss current and emerging street drugs and their toxicity.<br />
2. To discuss the current approach to managing toxicity <strong>of</strong> street<br />
drug overdose.<br />
Self-Assessment Questions<br />
1. What are the primary acute toxicities associated with street<br />
drugs in Canada?<br />
2. What treatment strategies should be considered in the<br />
management <strong>of</strong> these patients?<br />
3. What information sources can clinical pharmacists use to find<br />
local trends/patterns <strong>of</strong> street drug use in their region?<br />
Best Papers in Pharmacy Practice<br />
Jean-François Bussières, BPharm, MSc, MBA, FCSHP, CHU<br />
Saint-Justine, Montréal, QC<br />
In this age <strong>of</strong> constantly changing information and new<br />
developments in healthcare and the medical literature, the<br />
publication <strong>of</strong> influential papers and investigations can have an<br />
immediate impact on contemporary pharmacy practice. Keeping<br />
pace with the rapid pace <strong>of</strong> change can be a challenge for<br />
pharmacy practitioners, administrators and educators. The goal <strong>of</strong><br />
this session is to provide a practical overview and summary <strong>of</strong> key<br />
findings <strong>of</strong> the significant publications in pharmacy practice over<br />
the last 18 months (2010-2012). Selected key papers (3-5) will be<br />
highlighted and selected from a broad range <strong>of</strong> pharmacy practice<br />
settings and topics including clinical pharmacy practice,<br />
pharmaceutical care, medication safety and pharmacy education.<br />
For published papers that are controlled investigations, trial<br />
objectives, patient populations, study endpoints will be reviewed<br />
with an emphasis on practical practice implications, strengths and<br />
limitations. This session is aimed to broaden awareness <strong>of</strong><br />
developments in pharmacy practice.<br />
Goals and Objectives<br />
1. To highlight and summarize key findings <strong>of</strong> influential pharmacy<br />
practice publications in 2010-2012<br />
2. To provide an overview <strong>of</strong> selected controlled trial evidence in<br />
pharmacy practice in terms <strong>of</strong> highlighting major objectives,<br />
results and conclusions as well as strengths, limitations and<br />
practical implications.<br />
3. To provide participants with an open forum for sharing<br />
interactive discussion and questions on current published<br />
developments in pharmacy practice.<br />
Self-Assessment Questions<br />
1. What two practical strategies based on recent findings can I<br />
consider to incorporate into my everyday pharmacy practice or<br />
into my departmental initiatives for the next year?<br />
2. What three novel developments in pharmacy practice can I<br />
summarize for my pharmacy team?<br />
What is the Optimal Prioritization <strong>of</strong> Pr<strong>of</strong>essional<br />
Activities in a Collaboratively Developed <strong>Hospital</strong><br />
Pharmacist Best Practice Model?<br />
Olavo Fernandes, PharmD, FCSHP, University Health Network, Leslie<br />
Dan Faculty <strong>of</strong> Pharmacy, University <strong>of</strong> Toronto, Toronto, On<br />
This session focuses on addressing the fundamental need for clarity<br />
and direction for pharmacists amidst a time <strong>of</strong> unprecedented<br />
challenges and opportunities within our pr<strong>of</strong>ession. <strong>Hospital</strong><br />
pharmacists today are challenged with many competing and<br />
overlapping pr<strong>of</strong>essional priorities for the scope <strong>of</strong> pharmacy<br />
practice including: pharmaceutical care, patient safety, expanded<br />
experiential teaching responsibilities, competency –based residency<br />
training, enhanced expectations for scholarly activity,<br />
evidence-informed medicine, computerized prescriber order entry,<br />
medication reconciliation, hospital accreditation requirements, as<br />
well as expanded scope <strong>of</strong> practice legislation. Consequently, there<br />
is an authentic need for pharmacists to objectively assess, reflect<br />
and realign our current practice patterns to effectively address<br />
these priorities with the resource challenges <strong>of</strong> our current<br />
healthcare environment. This session will outline a multi-faceted<br />
generalizable framework for collaboratively discerning a practical,<br />
relevant and robust hospital pharmacist best practice model with a<br />
focus on an optimal prioritization <strong>of</strong> pr<strong>of</strong>essional activities (clinical<br />
and operational). This evolving model takes into practical<br />
consideration feedback from front-line pharmacists, pharmacy<br />
leaders, pharmacy practice published evidence, peer hospitals,<br />
CSHP 2012/ ASHP PPMI and local hospital priorities. This adaptable<br />
process is intended to position hospital pharmacists to best meet<br />
the needs <strong>of</strong> patients, healthcare pr<strong>of</strong>essionals, students, staff,<br />
government funders, and academia. It is envisioned that this<br />
hospital pharmacist practice model can be personalized for<br />
individual hospitals, as it should appropriately account for local<br />
priorities, influences, resources and perspectives.
34<br />
Goals and Objectives<br />
1. Outline a multi-faceted generalizable framework for discerning<br />
an optimal prioritization <strong>of</strong> pr<strong>of</strong>essional activities in a<br />
collaboratively developed hospital pharmacist best practice<br />
model.<br />
2. Highlight key bottom-lines <strong>of</strong> published evidence to inform this<br />
prioritization process: What specific pharmacist interventions/<br />
clinical services have demonstrated impact on meaningful<br />
patient outcomes?<br />
3. Illustrate various stakeholder perspectives with imagery for<br />
prioritized activities and practice models<br />
Self-Assessment Questions<br />
1. What specific clinical pharmacy activities have linked to<br />
improved patient outcomes?<br />
2. What specific meaningful patient outcomes have been improved<br />
by specific hospital pharmacy interventions?<br />
3. List and define four generalized hospital pharmacist practice<br />
models.<br />
4. Outline specific practical pr<strong>of</strong>essional responsibility domains that<br />
can be used to categorize and prioritize pr<strong>of</strong>essional<br />
responsibilities for hospital pharmacists.<br />
Simulation Game: Building Pharmacy Services from<br />
Scratch<br />
Jean-François Bussières, BPharm, MSc, MBA, FCSHP, CHU<br />
Sint-Justine, Montréal, QC<br />
<strong>Hospital</strong> pharmacy practice has undergone many changes over the<br />
course <strong>of</strong> the last three decades. New technologies such as<br />
automated repackaging technologies, robotic unit dose cart-fill<br />
systems, and automated dispensing cabinets have improved the<br />
efficiency, effectiveness and quality <strong>of</strong> drug distribution systems.<br />
New pharmacy practice models have been introduced in which<br />
pharmacists accept responsibility and accountability for drug<br />
therapy management. While there is an abundance <strong>of</strong> evidence<br />
related to the positive impact that many pharmacy services can<br />
have on the quality and effectiveness <strong>of</strong> health care, the uptake <strong>of</strong><br />
many evidence-based services has been slow and incomplete.<br />
There is a relative paucity <strong>of</strong> literature regarding the<br />
decision-making processes that are used by pharmacy managers<br />
and practitioners to prioritize the pharmaceutical services that they<br />
provide. Given the limited human and financial resources that are<br />
available, it is important for pharmacy managers and others in the<br />
pr<strong>of</strong>ession to identify and understand the basis on which their<br />
prioritization decisions are being made. We need to understand if<br />
the portfolio <strong>of</strong> services provided by pharmacy departments is<br />
evidence-based, preference-based, or a result <strong>of</strong> random<br />
opportunities that have arisen in a given hospital. We developed a<br />
simulation game to examine how prioritization decisions are made<br />
by hospital pharmacy managers<br />
Goals and Objectives<br />
1. To examine the consistency <strong>of</strong> prioritization decisions made by<br />
pharmacists in a simulated environment where the available<br />
resources are constrained.<br />
2. To rank the factors that influenced prioritization decisions and to<br />
compare individual and teams’ rankings <strong>of</strong> these factors.<br />
Self-Assessment Questions<br />
1. Do pharmacists agree on a core set <strong>of</strong> pharmaceutical activities<br />
that should be prioritized ?<br />
2. What are the factors that influence prioritization decisions in<br />
pharmacy practice ?<br />
3. What should the pharmacy pr<strong>of</strong>ession do to better prioritize<br />
pharmaceutical activities ?<br />
Antiplatelets in 2012 and Beyond<br />
Heather Kertland, BScPhm, PharmD, St. Michael’s <strong>Hospital</strong>,<br />
Toronto, ON<br />
Antiplatelet therapy is recommended in the guidelines for a variety<br />
<strong>of</strong> cardiac conditions ranging from acute coronary syndrome,<br />
post-PCI, primary prevention, and post-CABG. In the last year, the<br />
choice <strong>of</strong> agents has increased to include ticagrelor. The question is<br />
which agent or what combination <strong>of</strong> agents, at which dose and for<br />
how long. The goal <strong>of</strong> this session is to provide pharmacists with<br />
the knowledge to be able to determine what agent(s) are the<br />
optimal agents for their patients.<br />
Goals and Objectives<br />
1. Compare and contrast the risks and benefits <strong>of</strong> the various<br />
antiplatelet agents available on the <strong>Canadian</strong> market<br />
2. Identify which patient groups will benefit from which agent<br />
3. Defend your recommendation for antiplatelet agents for a given<br />
clinical scenario with reference to primary literature.<br />
Self-Assessment Questions<br />
1. On average, what is the rate <strong>of</strong> non-CABG major bleeding for a<br />
patient receiving dual antiplatelet therapy?<br />
2. What if any, is the benefit <strong>of</strong> using ticagrelor and ASA compared<br />
to clopidogrel and ASA in a patient with non-ST segment ACS?<br />
3. What is the optimal dose <strong>of</strong> ASA in a patient receiving<br />
prasugrel?<br />
Antiarrhythmic Drug Safety: Illusion, Fantasy and<br />
Wishful Thinking? Dronedarone and Other<br />
Disappointments<br />
James E. Tisdale, BScPhm, PharmD, BCPS, FCCP, FAPhA, FAHA,<br />
College <strong>of</strong> Pharmacy, Purdue University, Indianapolis, IN<br />
Antiarrhythmic drug safety has been an issue for many years.<br />
Quinidine-induced syncope was reported in the 1950s, and has<br />
been known to be due to the ventricular arrhythmia torsades de
35<br />
pointes (TdP) since the 1970s. TdP is associated with many<br />
antiarrhythmic drugs, including procainamide, sotalol, d<strong>of</strong>etilide,<br />
ibutilide, and, to a lesser extent, amiodarone and dronedarone. In<br />
the late 1980s and early 1990s, flecainide, encainide and<br />
moricizine were found to be associated with increased mortality in<br />
patients with a history <strong>of</strong> myocardial infarction, likely by inducing<br />
ventricular tachycardia in the presence <strong>of</strong> structural heart disease.<br />
Similar findings were subsequently reported associated with other<br />
antiarrhythmic agents including quinidine and procainamide.<br />
Perhaps the most effective antiarrhythmic agent available,<br />
amiodarone, is associated with many adverse effects, including<br />
life-threatening pulmonary fibrosis, hypothyroidism or<br />
hyperthyroidism, neurologic issues, bradycardia, hepatic toxicity,<br />
and dermatologic effects including blue-grey skin discoloration and<br />
photosensitivity. The newest available antiarrhythmic drug,<br />
dronedarone, was developed in an effort to create a drug with<br />
similar efficacy to amiodarone, but with a more favorable adverse<br />
effect pr<strong>of</strong>ile. However, dronedarone has been shown to be less<br />
effective for atrial fibrillation management than amiodarone. In<br />
addition, while dronedarone is free <strong>of</strong> adverse thyroid adverse<br />
effects and, possibly, pulmonary fibrosis, the drug is associated<br />
with increased mortality in patients with heart failure and in<br />
patients with permanent atrial fibrillation, severely limiting the use<br />
<strong>of</strong> this agent. Despite continued efforts to develop antiarrhythmic<br />
drugs with favorable adverse effect pr<strong>of</strong>iles, antiarrhythmic drug<br />
safety may simply be illusion, fantasy, and wishful thinking.<br />
Goals and Objectives<br />
1. Describe adverse effects associated with commonly used<br />
antiarrhythmic drugs<br />
2. Describe the advantages and disadvantages <strong>of</strong> the<br />
antiarrhythmic drug dronedarone, particularly its safety pr<strong>of</strong>ile in<br />
patients with heart failure or permanent atrial fibrillation<br />
Self-Assessment Questions<br />
1. Which <strong>of</strong> the following antiarrhythmic agents is safe to use<br />
(does not increase mortality) in patients with a history <strong>of</strong><br />
myocardial infarction?<br />
a. Amiodarone<br />
b. Flecainide<br />
c. Procainamide<br />
d. Quinidine<br />
2. Which <strong>of</strong> the following antiarrhythmic agents is safe to use<br />
(does not increase mortality or worsen the disease) in patients<br />
with heart failure?<br />
a. D<strong>of</strong>etilide<br />
b. Dronedarone<br />
c. Flecainide<br />
d. Propafenone<br />
3. Which <strong>of</strong> the following adverse effects or drug interactions<br />
associated with amiodarone is not associated with dronedarone?<br />
a. Bradycardia<br />
b. Hypothyroidism<br />
c. QT interval prolongation<br />
d. Interaction with digoxin<br />
Wednesday, February 8<br />
Mercredi 8 février<br />
Learning from High Reliability Organizations to<br />
Improve Reliability and Safety in Health Care<br />
Marlys Christianson, MD, PhD, Rotman School <strong>of</strong> Management,<br />
University <strong>of</strong> Toronto, Toronto, ON<br />
The purpose <strong>of</strong> this session is to introduce the concept <strong>of</strong> high<br />
reliability organizing as a way <strong>of</strong> thinking about consistent and<br />
excellent performance and to provide some examples <strong>of</strong> how high<br />
reliability organizing is being used in health care.<br />
Aircraft carriers, electrical power grids, and wildland firefighting,<br />
although seemingly different, are exemplars <strong>of</strong> high reliability<br />
organizations (HROs) – organizations that have the potential for<br />
catastrophic failure, yet engage in nearly error-free performance.<br />
HROs commit to safety at the highest level and adopt a special<br />
approach to its pursuit. High reliability organizing has been studied<br />
and discussed for some time in other industries and is receiving<br />
increasing attention in healthcare. The essence <strong>of</strong> high reliability<br />
organizing is a set <strong>of</strong> practices that enable organizations to focus<br />
attention on emergent problems and to deploy the right set <strong>of</strong><br />
resources to address those problems. HROs behave in ways that<br />
sometimes seem counterintuitive – they don’t try and hide failures<br />
but rather celebrate them as windows into the health <strong>of</strong> the<br />
system, they seek out problems, they avoid focusing on just one<br />
aspect <strong>of</strong> work and are able to see how all the parts <strong>of</strong> work fit<br />
together, they expect unexpected events and develop the capability<br />
to manage them, and they defer decision making down to local<br />
front-line experts who are empowered to solve problems. Given<br />
that health care is also a setting where error has potentially<br />
catastrophic consequences, high reliability organizing practices<br />
hold promise for improving reliability and safety in health care.<br />
Goals and Objectives<br />
1. To introduce the concept <strong>of</strong> high reliability organizing as a way<br />
<strong>of</strong> thinking about consistent and excellent performance.<br />
2. To provide some examples <strong>of</strong> how high reliability organizing is<br />
being used in health care<br />
Self-Assessment Questions<br />
1. What practices enable high reliability organizing?<br />
2. What are some ways to build the capability for high reliability<br />
organizing in health care?
36<br />
New Advances in the Management <strong>of</strong> Metastatic<br />
Renal Cell Carcinoma<br />
Shirin Abadi, BScPhm, ACPR, PharmD, BC Cancer Agency,<br />
Vancouver, BC<br />
In 2011, kidney cancer was the 6th most common cancer diagnosis<br />
affecting <strong>Canadian</strong> men and the 11th most common cancer<br />
diagnosis affecting <strong>Canadian</strong> women. Based on the 2004-2006<br />
<strong>Canadian</strong> Cancer Statistics, the estimated 5-year relative survival<br />
rate for kidney cancer is about 67%, and is significantly worse in<br />
cases <strong>of</strong> advanced disease. Drug therapy options are currently<br />
restricted to patients with advanced disease and have historically<br />
included cytokine-based therapies with high dose interleukin 2, or<br />
interferon-alpha. In recent years, a number <strong>of</strong> new treatment<br />
options have been introduced into the market for the management<br />
<strong>of</strong> metastatic renal cell carcinoma, including tyrosine kinase<br />
inhibitors such as sunitinib, sorafenib, and pazopanib, monoclonal<br />
antibodies such as bevacizumab, and mTOR inhibitors such as<br />
temsirolimus and everolimus. This presentation will provide an<br />
overview <strong>of</strong> the efficacy and safety <strong>of</strong> the new treatment options<br />
for the management <strong>of</strong> metastatic renal cell carcinoma.<br />
Goals and Objectives<br />
1. To review the clinical evidence behind the use <strong>of</strong> the new<br />
pharmacotherapeutic options for the management <strong>of</strong> metastatic<br />
renal cell carcinoma.<br />
2. To discuss the toxicity parameters and potential drug interactions<br />
associated with the use <strong>of</strong> the new pharmacotherapeutic<br />
options for the management <strong>of</strong> metastatic renal cell carcinoma.<br />
Self-Assessment Questions<br />
1. What are the roles <strong>of</strong> tyrosine kinase inhibitors, monoclonal<br />
antibodies, and mTOR inhibitors in the management <strong>of</strong><br />
metastatic renal cell carcinoma?<br />
2. What are the most common side effects and drug interactions<br />
associated with the use <strong>of</strong> sunitinib, sorafenib, pazopanib,<br />
bevacizumab, temsirolimus, and everolimus?<br />
Combination Therapy for Problem Gram Negative<br />
Pathogens<br />
Linda Dresser PharmD, FCSHP, University Health Network, Toronto,<br />
ON<br />
The goal <strong>of</strong> this presentation is to provide pharmacists involved in<br />
the care <strong>of</strong> patients with infectious diseases a familiarity with the<br />
literature and evidence concerning the use <strong>of</strong> combination<br />
antimicrobial therapy to manage problem gram negative infections.<br />
The role <strong>of</strong> combination therapy for the treatment <strong>of</strong> infections<br />
due to gram negative organisms, particularly those associated with<br />
resistance issues, is an ongoing topic <strong>of</strong> debate. The rationale for<br />
initiating combination therapy is usually justified by one fo the<br />
following: the potential for synergistic activity between two or<br />
more classes <strong>of</strong> antimicrobials; initial provision <strong>of</strong> broad spectrum<br />
activity from antimicrobial agents with differing spectra <strong>of</strong> activity<br />
and resistance patterns; or the prevention <strong>of</strong> resistance<br />
development while on therapy. The disadvantages <strong>of</strong> ongoing<br />
combination therapy include increased risk <strong>of</strong> toxicity, increased<br />
costs, increased risk <strong>of</strong> superinfection with more-resistant<br />
organisms. This common practice <strong>of</strong> prescribing double coverage<br />
for the treatment <strong>of</strong> gram negative pathogens is not congruent<br />
with current evidence.<br />
In this presentation the literature comparing monotherapy and<br />
combination therapy for gram negative infections will be reviewed<br />
and guidance for the pharmacotherapy practitioner provided.<br />
Goals and Objectives<br />
1. To review the evidence for monotherapy versus combination<br />
therapy for infections due to gram negative pathogens.<br />
2. To discuss the pharmacists role in translating the evidence into<br />
practice.<br />
Self-Assessment Questions<br />
1. For what indications is the empiric use <strong>of</strong> combination therapy<br />
to manage gram negative infections supported by the literature?<br />
2. For what patient populations is the empiric use <strong>of</strong> combination<br />
therapy to manage gram negative infections supported by the<br />
literature?<br />
The State <strong>of</strong> <strong>Hospital</strong> Pharmacy Practice in Canada:<br />
The Good, The Bad, and Perhaps a Bit <strong>of</strong> Ugly<br />
(Courtesy <strong>of</strong> the <strong>Hospital</strong> Pharmacy in Canada<br />
2009/10 Report)<br />
Kevin W. Hall, BScPhm, PharmD, Faculty <strong>of</strong> Pharmacy and<br />
Pharmacutical Sciences, University <strong>of</strong> Alberta; <strong>Hospital</strong> Pharmacy in<br />
Canada Report, Edmonton, AB<br />
The goals <strong>of</strong> this presentation are to review the 2009/10 results <strong>of</strong><br />
the biannual, national survey <strong>of</strong> hospital pharmacy departments in<br />
Canada, and to highlight a few areas that warrant discussion and<br />
action by hospital pharmacy practitioners.<br />
All <strong>Canadian</strong> hospitals with a minimum <strong>of</strong> 50 acute care beds are<br />
invited to participate in the biannual survey. The response rate in<br />
2009/10 was 72% (160/222), which was similar to the 2007/08<br />
response rate <strong>of</strong> 74% (166/223). Seventy-three percent <strong>of</strong><br />
respondents were from non-teaching organizations and 27% were<br />
from teaching facilities, compared to 76% and 24% respectively in<br />
the 2007/08 report. The data provided by respondents was<br />
reviewed and analyzed by members <strong>of</strong> the editorial board, who<br />
subsequently wrote the 12 chapters that appear in the <strong>Hospital</strong><br />
Pharmacy in Canada 2009/10 Report.<br />
Goals and Objectives<br />
1. To provide conference participants with a summary <strong>of</strong> the<br />
national survey data that appears in the <strong>Hospital</strong> Pharmacy in<br />
Canada 2009/10 Report.<br />
2. To highlight certain findings in the Report which warrant<br />
discussion and action by hospital pharmacy practitioners.
37<br />
Self-Assessment Questions<br />
1. What type <strong>of</strong> pharmacy practice model should we be aiming for<br />
as the future standard for hospital pharmacy practice in<br />
Canada? Is the integrated drug distribution/clinical practice<br />
model where we want to be in the future?<br />
3. Will the health care system/the public demand consistency and<br />
accountability for the clinical services provided by pharmacists?<br />
Is hospital pharmacy practice evidence-based or<br />
preference-based?<br />
3. Are hospital pharmacists providers <strong>of</strong> care or providers <strong>of</strong><br />
information?<br />
4. Are today’s competency requirements for pharmacists different<br />
than in the past? Do existing pharmacists and/or new pharmacy<br />
graduates possess these competencies?<br />
VTE in the ICU<br />
David Williamson, BPharm, MSc, BCPS, Hôpital du Sacré-Cœur de<br />
Montréal and Faculté de pharmacie, Université de Montréal,<br />
Montréal, QC<br />
The purpose <strong>of</strong> this session is to review the causes, prophylaxis and<br />
treatment <strong>of</strong> venous thromboembolism in the setting <strong>of</strong> the<br />
intensive care unit.<br />
The practice <strong>of</strong> venous thromboembolism (VTE) prevention critically<br />
ill patients is in constant evolution as new clinical trials are being<br />
published. In addition, intensive care unit (ICU) patients <strong>of</strong>ten have<br />
comorbidities or complications that increase the risk <strong>of</strong> bleeding or<br />
alter the pharmacokinetics <strong>of</strong> anticoagulants. Thromboprophylaxis<br />
regimens may require different dosing and monitoring strategies.<br />
The use <strong>of</strong> heparins in the ICU is not without risks and<br />
heparin-induced thrombocytopenia (HIT) is <strong>of</strong>ten suspected in<br />
patients with thrombocytopenia. However, this complication<br />
remains relatively rare and strategies enabling proper identification<br />
are key. Advances in laboratory diagnostic and new scoring systems<br />
may help clinicians tackle this conundrum. Unfortunately, deep vein<br />
thrombosis and pulmonary embolism still occur in the critically ill<br />
and prompt treatment <strong>of</strong> these complications is key. Massive and<br />
selected cases <strong>of</strong> submassive pulmonary embolism can potentially<br />
be treated with intravenous thrombolytics.<br />
Goals and Objectives<br />
1. Evaluate interventions for VTE prevention with respect to<br />
efficacy, safety, and cost in critically ill patients.<br />
2. Design optimal dosing strategies for low molecular weight<br />
heparin in renal failure and obesity.<br />
3. Design interventions for preventing, identifying and optimally<br />
treating patients with heparin induced thrombocytopenia<br />
4. Evaluate the role <strong>of</strong> thrombolysis in the treatment <strong>of</strong> submassive<br />
and massive pulmonary embolism<br />
Self-Assessment Questions<br />
1. What is the role for low molecular weight heparins in VTE<br />
prevention <strong>of</strong> medical-surgical ICU patients?<br />
2. What is the optimal dosing strategy for anticoagulants in the<br />
VTE prevention <strong>of</strong> renally impaired ICU patients?<br />
3. How can HIT be optimally identified in ICU patients?<br />
4. What is the role for thrombolytics in submassive pulmonary<br />
embolism?<br />
How will Pharmacogenomics Practically Impact<br />
Patient Care & Practicing <strong>Pharmacists</strong>: Now and In<br />
the Future?<br />
Anke-Hilse Maitland-van der Zee, PharmD, PhD, Utrecht Institute<br />
for Pharmaceutical Sciences, Utrecht University, Utrecht,<br />
The Netherlands<br />
Pharmacogenomics uses genetic information to individualize drug<br />
therapy. Even though it did not fulfill the expectations that we had<br />
10-15 years ago, there are gene-drug interactions known that can<br />
and should be used in clinical practice. However implementing<br />
these interactions in challenging. How much evidence is needed?<br />
Who should perform and who should pay for genotyping. Is It<br />
cost-effective? <strong>Pharmacists</strong> might be able to play an important role<br />
in bringing this into practice.<br />
Goals and Objectives<br />
1. Give an introduction in pharmacogenetics/genomics<br />
2. Give an overview <strong>of</strong> clinical relevant gene-drug interactions<br />
3. Discuss challenges in implementation<br />
4. Talk about future opportunities in research and implementation<br />
Self-Assessment Questions<br />
1. Which gene-drug interactions are ready for practice?<br />
2. How can pharmacists play a role in implementation <strong>of</strong><br />
pharmacogenomics in everyday practice?<br />
What Should a System for the Recognition <strong>of</strong><br />
Special Areas <strong>of</strong> Practice in Pharmacy Look Like?<br />
Arthur Whetstone, EdD, MA, Bed, BA(Hon), RPN, <strong>Canadian</strong> Council<br />
on Continuing Education in Pharmacy, Saskatoon, SK<br />
The CPD/CE Policy Summit, which brought together pharmacy<br />
pr<strong>of</strong>essionals from all sectors <strong>of</strong> the pharmacy community,<br />
advocated that action needed to be taken now on the<br />
establishment <strong>of</strong> a system <strong>of</strong> recognition <strong>of</strong> specialization and<br />
special areas <strong>of</strong> practice in pharmacy. While a number <strong>of</strong> models<br />
were discussed, there was agreement the system needed to be a<br />
Condominium <strong>of</strong> specialities in which a core administrative system<br />
and framework enabled a number <strong>of</strong> individual specialities.<br />
Specialization in pharmacy has been discussed for over two<br />
decades. It has never gotten beyond the discussion stage. The<br />
Summit participants stated that there has been enough talk, it is<br />
now time to walk the talk.<br />
In the session we will discuss: (i) What do we mean by<br />
specialization, special areas <strong>of</strong> practice, and are they the same
38<br />
thing? (ii) What are different models for the recognition or<br />
certification <strong>of</strong> specialities and special areas <strong>of</strong> practice in<br />
pharmacy? (iii) What are the issues that need to be addressed to<br />
develop a system <strong>of</strong> recognition? (iv) Is there really a need and<br />
interest in becoming a specialist among <strong>Canadian</strong> pharmacists? (v)<br />
And, what is the preferred approach to a system <strong>of</strong> recognition <strong>of</strong><br />
specialization in pharmacy practice?<br />
Goals and Objectives<br />
At the end <strong>of</strong> the session, the participant will be able to:<br />
1. State the differences between area <strong>of</strong> specialization and special<br />
area <strong>of</strong> practice.<br />
2. Describe four basic models <strong>of</strong> certification <strong>of</strong> pr<strong>of</strong>essional<br />
practice.<br />
3. Describe the issues with recognition <strong>of</strong> special areas <strong>of</strong> practice<br />
and specialization in Canada.<br />
4. Identify a preferred approach to a system <strong>of</strong> recognition <strong>of</strong><br />
specialization and special areas <strong>of</strong> practice.<br />
Self-Assessment Questions<br />
1. What are the options for the development <strong>of</strong> a system <strong>of</strong><br />
recognition for special areas <strong>of</strong> practice in pharmacy in Canada?<br />
2. What are the issues that must be addressed to establish a system<br />
<strong>of</strong> recognition <strong>of</strong> special areas <strong>of</strong> practice in pharmacy in<br />
Canada?<br />
3. What is a feasible option for a system <strong>of</strong> recognition <strong>of</strong> special<br />
areas <strong>of</strong> practice in pharmacy?<br />
CSHP 2015 Town Hall: Are we on Target for<br />
Pharmacy Practice Excellence?<br />
Carolyn Bornstein, BScPhm, ACPR, FCSHP, CSHP 2015 Project<br />
Coordinator, Newmarket, ON, Stephen Shalansky, BScPhm, PharmD,<br />
ACPR, FCSHP, Providence Healthcare, Vancouver, BC, Emily Muir,<br />
BScPhm, ACPR, Horizon Health Network, Saint John, NB<br />
CSHP 2015 is a vision <strong>of</strong> Pharmacy Practice Excellence. Its 6 goals<br />
aim to ensure that the use <strong>of</strong> medications is effective,<br />
evidence-based and safer, and to contribute meaningfully to public<br />
health. Thirty-six pharmacy practice-related objectives support the<br />
goals. Highlights <strong>of</strong> the progress <strong>of</strong> hospital pharmacy departments<br />
in Canada towards the CSHP 2015 objective targets will be<br />
presented. Although some targets have been reached, progress in<br />
many areas falls short <strong>of</strong> the targets. Some say they are “too busy”<br />
for the CSHP 2015 initiative, without realizing that as they strive to<br />
comply with Accreditation Canada’s Medication Management<br />
Standards and the Safer Healthcare Now! initiatives they are<br />
already “committed” to CSHP 2015. The supports and resources<br />
provided for CSHP 2015 will be highlighted.<br />
CSHP 2015’s success depends on the commitment <strong>of</strong> pharmacy<br />
departments and their implementation <strong>of</strong> the CSHP 2015<br />
objectives. Incorporating CSHP 2015 into your pharmacy<br />
departments’ strategic plan is critical. Strategies for strategic<br />
planning will be presented, including the experience <strong>of</strong> a CSHP<br />
2015 branch champion and interim pharmacy director.<br />
In one organization the pharmacists identified evidence-based<br />
medicine and critical appraisal skills as a learning need. The third<br />
speaker will share her experience <strong>of</strong> using the CSHP toolkit, FROM<br />
PAPER TO PRACTICE: Incorporating Evidence into Pharmacy<br />
Practice in the development <strong>of</strong> an evidence based medicine<br />
curriculum for her organization. Their goal was to increase the<br />
pharmacist’s confidence and ability to seek the best possible clinical<br />
evidence and apply it to patient care.<br />
The town hall will conclude by welcoming CSHP member feedback<br />
on the value <strong>of</strong> the information, supports, resources and tools that<br />
CSHP has provided to help incorporate CSHP 2015 into their<br />
practice.<br />
Goals and Objectives<br />
1. To provide highlights <strong>of</strong> the CSHP 2015 progress to date and<br />
some <strong>of</strong> the many supports, resources and tools that CSHP has<br />
provided for its members.<br />
2. To provide an example <strong>of</strong> a strategic planning process that<br />
considers and aligns as much as possible: a) previous pharmacy<br />
department strategic goals, b) institutional strategic goals, and c)<br />
CSHP 2015 goals and objectives.<br />
3. To provide insight and an opportunity for discussion regarding<br />
how CSHP 2015 objectives can be implemented in a manner<br />
that maximizes the chance <strong>of</strong> success and sustainment.<br />
Self-Assessment Questions<br />
1. When planning a pharmacy department strategic planning<br />
session, why is it important to consider previous departmental<br />
objectives, as well as the institutions strategic priorities?<br />
2. Name two documents available on the CSHP National website<br />
that you will use during your next departmental strategic<br />
planning session.<br />
3. What CSHP 2015 toolkits are available on the CSHP website and<br />
how can you use them in your pharmacy department to reach<br />
CSHP 2015 goals and objectives?<br />
Dexmedetomidine: A New Sedative in the ICU:<br />
Balancing Responsibility and Real Life<br />
Salmaan Kanji, BScPhm, PharmD, ACPR, The Ottawa <strong>Hospital</strong> and<br />
Ottawa <strong>Hospital</strong> Research Institute, Ottawa, ON<br />
The purpose <strong>of</strong> this session is to discuss the role <strong>of</strong> a new sedative<br />
agent, dexmedetomidine, in the context <strong>of</strong> ICU sedation and<br />
analgesia during a time where current strategies are being<br />
re-evaluated in light <strong>of</strong> new information and new tools.<br />
Sedation practices in the ICU are in a current state <strong>of</strong> flux. The<br />
consequences <strong>of</strong> over-sedation <strong>of</strong> ICU patients are increasingly<br />
being recognized and associated with negative outcomes such as<br />
increased length <strong>of</strong> stay, increased duration <strong>of</strong> mechanical<br />
ventilation, complications associated with critical illness and even<br />
mortality. Furthermore, long term evaluations have established a
39<br />
correlation between ICU sedation and complications during the<br />
rehabilitative phase <strong>of</strong> survivors <strong>of</strong> critical illness including mood<br />
disturbances, post traumatic stress disorders and prolonged<br />
myopathic rehabilitation.<br />
In the last 10 years many strategies to minimize the consequences<br />
<strong>of</strong> oversedation have been investigated and challenge our<br />
traditional paradigms as they relate to sedation in the critically ill<br />
patient. These consist <strong>of</strong> new procedural strategies and<br />
interventions (i.e., nurse driven sedation protocols, spontaneous<br />
breathing trials, goal directed sedation, daily sedation interruption)<br />
and new drugs (i.e., dexmedetomidine, ketamine, clonidine).<br />
Dexmedetomidine has entered the <strong>Canadian</strong> market amidst much<br />
anticipation and controversy. It is expensive relative to alternative<br />
drug therapy and approved for only niche indications. It is also a<br />
new novel therapy that has attractive qualities particularly from a<br />
pharmacokinetic/pharmacodynamic point <strong>of</strong> view and from a<br />
pharmacologic perspective. This combination <strong>of</strong> attributes lends<br />
new therapies to the potential for misuse.<br />
Goals and Objectives<br />
1. To review the evidence for dexmedetomidine in the ICU with<br />
respect to comparative efficacy and safety.<br />
2. To propose the “place in therapy” for dexmedetomidine as it<br />
pertains to clinicians caring for patients in <strong>Canadian</strong> ICUs.<br />
3. To propose strategies to use dexmedetomidine responsibly while<br />
maximizing its niche potential for benefit within the scope <strong>of</strong><br />
approval.<br />
Self-Assessment Questions<br />
1. For what indication is dexmedetomidine approved in Canada?<br />
2. What type <strong>of</strong> ICU patient is most likely to benefit from<br />
dexmedetomidine within the approved <strong>Canadian</strong> indication?<br />
3. What strategies can be employed to minimize cost and adverse<br />
events related to dexmedetomidine while maximizing the<br />
potential benefits in ICU patients.<br />
What’s New, What’s Next… 1 Year Experience for<br />
an Antimicrobial Stewardship <strong>Program</strong> in a<br />
Community <strong>Hospital</strong> Intensive Care Unit (ICU)<br />
Kelly Walker, BSP, Toronto East General <strong>Hospital</strong>, Toronto, ON,<br />
Jaclyn Litynsky, PharmD, BCPS, Toronto East General <strong>Hospital</strong>,<br />
Toronto, ON<br />
Antimicrobial stewardship promotes appropriate antimicrobial use<br />
with the overall goal <strong>of</strong> optimizing patient outcomes while<br />
minimizing negative consequences <strong>of</strong> antimicrobial use such as<br />
nosocomial Clostridium difficile infection. In 2007, the Infectious<br />
Disease <strong>Society</strong> <strong>of</strong> America (IDSA) and the <strong>Society</strong> for Healthcare<br />
Epidemiology <strong>of</strong> America (SHEA) published evidence-based<br />
guidelines on how to develop an institutional program to enhance<br />
antimicrobial stewardship.<br />
Our antimicrobial stewardship program (ASP) goal is to reduce the<br />
use and expenditure <strong>of</strong> antimicrobials using a prospective audit and<br />
feedback approach (a core strategy in the IDSA/SHEA guidelines).<br />
This is carried out by an Infectious Disease (ID)<br />
physician-pharmacist team. The critical care/stewardship<br />
pharmacist independently reviews all ICU patients on antimicrobials<br />
and meets with the ID physician to discuss the cases. Afterwards,<br />
the ASP team meet with the ICU team and provides feedback on<br />
antimicrobial optimization.<br />
1 year following implementation <strong>of</strong> an ASP, a substantial reduction<br />
in both antimicrobial use and overall cost savings has been<br />
achieved. No adverse impact on patient outcomes, such as length<br />
<strong>of</strong> stay or mortality has been observed.<br />
Community hospitals can successfully implement ASP. We<br />
identified knowledge exchange, peer-to-peer communication and<br />
decision support as key to the ongoing success factors in our<br />
community-hospital based program.<br />
Goals and Objectives<br />
1. To describe the day to day activities <strong>of</strong> an antimicrobial<br />
stewardship program in a community hospital ICU.<br />
2. To review the key successes <strong>of</strong> the TEGH antimicrobial<br />
stewardship program.<br />
3. To explore innovative ways to improve upon and ensure<br />
sustainability <strong>of</strong> the antimicrobial stewardship program at TEGH.<br />
Self-Assessment Questions<br />
1. What is my institution’s readiness to implement a formal<br />
antimicrobial stewardship program?<br />
2. What is my own readiness and/or ability as a clinician to be part<br />
<strong>of</strong> an ASP?<br />
3. Are there any other antimicrobial stewardship strategies that are<br />
already in place at my institution? If so, how can these be<br />
optimized?<br />
Antibiotic Pharmacokinetics and<br />
Pharmacodynamics: Putting the Practical into<br />
Practice<br />
Rosemary Zvonar, BScPhm, ACPR, FCSHP, The Ottawa <strong>Hospital</strong>,<br />
Ottawa, ON, Miranda So, BScPhm, PharmD, University Health<br />
Network, Toronto, ON<br />
As part <strong>of</strong> the healthcare team, pharmacists are <strong>of</strong>ten relied upon<br />
to choose and adjust drug doses. Selecting an appropriate<br />
antibiotic dosing regimen improves the chances <strong>of</strong> a positive<br />
outcome in patients with infection, and is an essential component<br />
<strong>of</strong> antimicrobial stewardship.<br />
Several factors should be considered in order to optimize a<br />
patient’s antibiotic dose. These include characteristics <strong>of</strong> the host<br />
such as organ function and immune status, the pharmacokinetics<br />
<strong>of</strong> the drug, the pharmacodynamic action <strong>of</strong> the antibiotic, the<br />
severity <strong>of</strong> infection, and infecting organism.<br />
Pharmacodynamic considerations include whether the antibiotic is<br />
concentration dependant or time dependant and the associated<br />
pharmacodynamic target. Patient specific pharmacokinetic<br />
variables are <strong>of</strong>ten calculated using serum drug levels for the
40<br />
aminoglycoside antibiotics and vancomycin. This allows for<br />
individualized dosing regimens to maximize therapeutic efficacy<br />
while minimizing toxicity.<br />
Critical illness, obesity, and organ dysfunction may alter volume <strong>of</strong><br />
distribution and/or elimination. These pharmacokinetic parameters<br />
should also be taken into account when selecting drug doses.<br />
This session will review important aspects <strong>of</strong> pharmacokinetics and<br />
pharmacodynamics which influence the dosing <strong>of</strong> antibacterial<br />
agents. It will also include a review <strong>of</strong> aminoglycoside<br />
pharmacokinetic calculations. Participants will be given the<br />
opportunity to apply the information to sample cases. The target<br />
audience <strong>of</strong> this session is pharmacists-in-training; however, any<br />
pharmacist wishing a review <strong>of</strong> these concepts will benefit from<br />
this session. A scientific calculator will facilitate aminoglycoside<br />
sample calculations.<br />
Goals and Objectives<br />
1. Interpret a set (peak, trough) <strong>of</strong> aminoglycoside levels, and<br />
calculate patient specific pharmacokinetic parameters.<br />
2. Understand the difference between pharmacokinetics and<br />
pharmacodynamics and how these may influence antibiotic<br />
dosing.<br />
Self-Assessment Questions<br />
1. What factors should be considered when selecting an empiric<br />
aminoglycoside dosing regimen?<br />
2. What is the role <strong>of</strong> ‘Monte Carlo Simulation’ in the assessment<br />
<strong>of</strong> the adequacy <strong>of</strong> antibiotic dosages?
41<br />
Call for Abstracts<br />
2012 Summer Educational Sessions (SES)<br />
Delta Prince Edward, Charlottetown, Prince Edward Island<br />
August 11 to 14, 2012<br />
Demande de résumés<br />
Séances éducatives d’été (SÉÉ) 2012<br />
Delta Prince Edward, Charlottetown, Île-du-Prince-Édouard<br />
11 au 14 août 2012<br />
GENERAL INFORMATION<br />
Category<br />
Author must specify the category that best suits the particular<br />
abstract.<br />
1. Original Research (includes Pharmaceutical/Basic Science, Clinical<br />
Research, Drug Use Evaluations, Systematic Reviews and<br />
Meta-Analysis, Pharmacoeconomics Analysis, etc.)<br />
2. Case Reports<br />
3. Pharmacy Practice (includes Administration Projects, Health<br />
Pr<strong>of</strong>essional Education, Medication Safety Initiatives, etc.)<br />
CSHP 2015<br />
CSHP 2015 related abstracts will be designated as such at SES. If<br />
your abstract is linked to CSHP 2015 initiatives, please clearly<br />
indicate this on the online abstract submission form.<br />
Abstract Submissions<br />
All abstract submissions must be submitted no later than 18:00<br />
(Eastern Daylight Time) on May 6, 2012.<br />
Abstracts MUST be submitted electronically. Please complete the<br />
abstract submission form online at CSHP’s Web site<br />
(http://www.cshp.ca) prior to submitting the abstract. If you are<br />
submitting more than one abstract, an abstract submission form<br />
must be completed for each abstract. Abstracts are then submitted<br />
by e-mail to ddavidson@cshp.ca. Please provide 2 copies <strong>of</strong> your<br />
abstract. One copy must be blinded (remove authors’ affiliations<br />
and identifying features in body <strong>of</strong> abstract). Please indicate in the<br />
filename which copy is blinded. Please submit your file in MS Word<br />
Format.<br />
Abstract review and grading is conducted by 2 randomly assigned,<br />
blinded, and independent reviewers. Abstracts are selected on the<br />
basis <strong>of</strong> scientific merit, originality, level <strong>of</strong> interest to pharmacists,<br />
and compliance with style rules. Guidance for authors and sample<br />
abstracts will be available on the CSHP website shortly at<br />
www.cshp.ca/event/SES2012.<br />
Failure to comply with requirements for submission, including<br />
submission <strong>of</strong> blinded abstract or any other style rules, will result in<br />
automatic rejection <strong>of</strong> the submission.<br />
Research in progress will not be accepted.<br />
Abstracts previously presented at non-CSHP meetings or at local or<br />
provincial CSHP meetings will be reviewed for potential inclusion as<br />
INFORMATION GÉNÉRALE<br />
Catégorie<br />
L’auteur doit indiquer la catégorie qui sied le mieux au résumé<br />
soumis.<br />
1. Recherche originale (inclut la recherche pharmaceutique ou<br />
fondamentale, scientifique ou clinique, les évaluations de<br />
l’utilisation des médicaments, les examens systématiques et les<br />
méta-analyses, les analyses pharmacoéconomiques, etc.)<br />
2. Observations cliniques<br />
3. Pratique pharmaceutique (inclut les projets administratifs, la<br />
formation des pr<strong>of</strong>essionnels de la santé, les projets liés à la<br />
sécurité des médicaments, etc.)<br />
SCPH 2015<br />
Les résumés liés au projet SCPH 2015 seront désignés comme tels<br />
sur les lieux des SÉÉ. Si votre résumé est relié au projet SCPH 2015,<br />
assurez-vous de le mentionner clairement sur le formulaire de<br />
soumission en ligne des résumés.<br />
Soumission des résumés<br />
Tous les résumés doivent être soumis au plus tard à 18 h (heure<br />
avancée de l’est) le 6 mai 2012.<br />
Les résumés DOIVENT être présentés électroniquement. Veuillez<br />
remplir le formulaire de soumission en ligne des résumés affiché<br />
sur le site Web de la SCPH à http://www.cshp.ca avant de<br />
soumettre votre résumé. Si vous présentez plus d’un résumé, vous<br />
devez remplir un formulaire pour chaque résumé soumis. Les<br />
résumés sont ensuite expédiés par courriel à ddavidson@cshp.ca.<br />
Veuillez fournir deux exemplaires de votre résumé. Un de ces<br />
exemplaires doit être anonyme. (Il faut supprimer du corps du texte<br />
l’affiliation des auteurs et les éléments qui révèlent leur identité.) Le<br />
nom du fichier doit préciser quel exemplaire est anonyme. Le<br />
fichier doit être présenté en format MS Word.<br />
Les résumés sont examinés et évalués par deux réviseurs<br />
indépendants assignés au hasard et en aveugle. Les résumés seront<br />
choisis en tenant compte de leur valeur scientifique, leur<br />
originalité, leur intérêt pour les pharmaciens et le respect des règles<br />
de présentation. Des directives à l’intention des auteurs et des<br />
exemples de résumés seront affichés d’ici peu sur le site Web de la<br />
SCPH à www.cshp.ca/event/SES2012.<br />
Si la demande ne respecte pas les exigences pour la soumission de<br />
résumés, y compris la soumission d’un résumé anonyme ou toute<br />
autre règle de présentation, cette soumission sera<br />
automatiquement rejetée.
42<br />
encore presentations. These encore presentations will be marked as<br />
such. These submissions must include the original conference/date<br />
citation on the abstract submission form. Abstracts presented<br />
previously at national CSHP events (PPC or SES) will not be eligible<br />
to be presented again as an encore.<br />
Accepted abstracts will be published in the final SES 2012 program<br />
and also in the <strong>Canadian</strong> Journal <strong>of</strong> <strong>Hospital</strong> Pharmacy.<br />
Authors <strong>of</strong> accepted abstracts will be notified within 3 to 4 weeks.<br />
Authors are responsible for their own transportation and<br />
accommodations at SES. Early registration fees will apply to all<br />
accepted poster applications. Guidelines for posters will be<br />
provided to authors <strong>of</strong> accepted abstracts.<br />
Abstract Style Rules<br />
Title should be brief and should clearly indicate the nature <strong>of</strong> the<br />
presentation. Capitalize only the first letter <strong>of</strong> each word <strong>of</strong> the<br />
title. Do not use abbreviations in the title. List the authors,<br />
institutional affiliation, city, and province. Omit degrees, titles, and<br />
appointments. The recommended font is Times New Roman, 12<br />
point.<br />
Organize the body <strong>of</strong> the abstract according to the selected<br />
category as follows:<br />
Original Research:<br />
a. rationale,<br />
b. objectives,<br />
c. study design and methods,<br />
d. results <strong>of</strong> study including statistical analysis used,<br />
e. conclusion <strong>of</strong> study (which should be supported by results<br />
presented).<br />
Case Reports:<br />
a. rationale for case report,<br />
b. description <strong>of</strong> case,<br />
c. assessment <strong>of</strong> causality if appropriate,<br />
d. evaluation <strong>of</strong> the literature,<br />
e. importance <strong>of</strong> case to pharmacy practitioners.<br />
Pharmacy Practice:<br />
a. rationale for report;<br />
b. description <strong>of</strong> concept, service, role, or situation;<br />
c. steps taken to identify and resolve problem, implement change,<br />
or develop and implement new program;<br />
d. evaluation <strong>of</strong> project,<br />
e. the concept’s importance and usefulness to current and/or<br />
future practice.<br />
Abstract Text<br />
• Abstract body (not including title and authors) is limited to 300<br />
words.<br />
• A table is equivalent to 30 words.<br />
• A graphic is equivalent to 60 words.<br />
Les recherches en cours ne seront pas acceptées.<br />
Les résumés qui ont déjà fait l’objet d’une présentation lors de<br />
réunions autres que celles de la SCPH ou dans des assemblées<br />
locales ou provinciales de la SCPH seront évalués et possiblement<br />
acceptés comme des reprises. Ces présentations seront clairement<br />
identifiées comme des reprises. Le formulaire de soumission doit<br />
faire mention de la date et du nom du congrès où le résumé a été<br />
présenté précédemment. Les résumés qui ont déjà été présentés à<br />
un événement national de la SCPH (CPP ou SÉÉ) ne sont pas<br />
admissibles.<br />
Les résumés qui auront été acceptés seront publiés dans le<br />
programme final des SÉÉ 2012 et dans le Journal canadien de la<br />
pharmacie hospitalière.<br />
Les auteurs des résumés acceptés seront avisés dans un délai de<br />
trois à quatre semaines. Les auteurs doivent assumer leurs propres<br />
frais de transport et de logement pour les SÉÉ. Tous les auteurs des<br />
résumés acceptés auront droit aux frais d’inscription anticipée. Des<br />
directives concernant l’affichage seront fournies aux auteurs dont<br />
les résumés auront été acceptés.<br />
Règles de présentation<br />
Le titre devrait être bref et indiquer clairement la nature de la<br />
présentation. Seule la première lettre du premier mot du titre doit<br />
être en majuscule. Le titre ne doit pas contenir d’abréviations. Le<br />
nom des auteurs, l’établissement auquel ceux-ci sont affiliés ainsi<br />
que la ville et la province où est situé l’établissement doivent être<br />
précisés, tandis que les diplômes, les titres et les affectations ne<br />
doivent pas être mentionnés. Il est recommandé d’utiliser la police<br />
Times New Roman 12.<br />
Le texte du résumé doit être organisé conformément aux règles<br />
propres à la catégorie à laquelle il appartient, de la manière<br />
suivante :<br />
Recherche originale :<br />
a. justification,<br />
b. objectifs,<br />
c. méthodologie et démarche de l’étude,<br />
d. résultats de l’étude, y compris les analyses statistiques utilisées,<br />
e. conclusion de l’étude (la conclusion devrait être appuyée par les<br />
résultats présentés).<br />
Observations cliniques:<br />
a. justification de l’observation clinique,<br />
b. description du cas,<br />
c. analyse de la causalité s’il y a lieu,<br />
d. évaluation de la documentation,<br />
e. importance du cas pour les praticiens en pharmacie.<br />
Pratique pharmaceutique:<br />
a. justification du rapport;<br />
b. description du concept, du service, du rôle ou de la situation;<br />
c. mesures prises en vue de cerner et de résoudre le problème,<br />
d’apporter des changements, ou de créer et de mettre en œuvre<br />
un nouveau programme;<br />
d. évaluation du projet;<br />
e. importance et utilité du concept par rapport à la pratique<br />
actuelle et future.
43<br />
• Results or evaluation must be included in the abstract. It is not<br />
acceptable to state that results will be discussed.<br />
• Do not indent the start <strong>of</strong> a paragraph.<br />
• Place abbreviations in parentheses after the full word the first<br />
time it appears. Please keep abbreviated terms to a minimum.<br />
• Use numerals to indicate numbers, except to begin sentences.<br />
• Use only generic names <strong>of</strong> drugs, material, devices, and<br />
equipment.<br />
Abstracts should not include citations or reference numbers.<br />
For original research or pharmacy practice projects, ensure that the<br />
objectives, methods, analysis, results, and conclusions are internally<br />
consistent<br />
Email Confirmation <strong>of</strong> Abstract Submissions<br />
You should receive an email confirmation <strong>of</strong> your abstract<br />
submission. If you have not received an email confirmation by the<br />
deadline, please contact Desarae Davidson:<br />
Tel.: (613) 736-9733, ext. 229<br />
Fax: (613) 736-5660<br />
Email: ddavidson@cshp.ca<br />
Texte du résumé<br />
• Le corps du résumé (excluant le titre et les auteurs) ne doit pas<br />
dépasser 300 mots.<br />
• Un tableau compte pour 30 mots.<br />
• Un graphique compte pour 60 mots.<br />
• Les résultats ou l’évaluation doivent être inclus dans le résumé. Il<br />
est inacceptable de mentionner que les résultats seront discutés.<br />
• Le début des paragraphes ne doit pas être précédé d’un alinéa.<br />
• Placer les abréviations entre parenthèses après le terme qu’elles<br />
remplaceront, la première fois que le terme est utilisé. Veuillez<br />
limiter au minimum l’utilisation d’abréviations.<br />
• Les nombres doivent être écrits en chiffres, sauf lorsqu’ils<br />
représentent le premier mot d’une phrase.<br />
• Seuls les noms génériques des médicaments, du matériel, des<br />
instruments et de l’équipement doivent être employés.<br />
• Les résumés ne devraient pas comprendre de citations ni de<br />
numéros de référence.<br />
Dans le cas d’une recherche originale ou de projets liés à la<br />
pratique pharmaceutique, il faut s’assurer que les objectifs, la<br />
méthodologie, les analyses, les résultats et les conclusions sont<br />
intrinsèquement logiques.<br />
Confirmation par courriel de la réception<br />
du résumé<br />
La réception de votre résumé devrait être confirmée par courriel.<br />
Si vous n’avez pas reçu de confirmation par courriel avant la date<br />
limite, veuillez téléphoner à madame Desarae Davidson:<br />
Téléphone : (613) 736-9733, ext. 229<br />
Fax : (613) 736-5660<br />
Courriel : ddavidson@cshp.ca
44<br />
Oral Presentations <strong>of</strong> Award-Winning<br />
Projects and Original Research<br />
Présentations orales de projets primés<br />
et de recherche originale<br />
Monday February 6, 2011<br />
10:35-11:15<br />
Simcoe/Dufferin<br />
1. National Survey <strong>of</strong> Critical Care <strong>Pharmacists</strong>’ Views and Involvement in<br />
Clinical Research<br />
2. <strong>Hospital</strong> Wide Roll-Out <strong>of</strong> Antimicrobial Stewardship: A Stepped Wedge<br />
Randomized Controlled Trial<br />
3. Evaluation <strong>of</strong> Concordance to Ventilator-Associated Pneumonia<br />
Guidelines in the Intensive Care Unit Before and During Antimicrobial<br />
Stewardship<br />
11:25-12:10<br />
1. Identifying Barriers to Pharmacist Medication Discharge Counselling<br />
2. Lack <strong>of</strong> Effectiveness <strong>of</strong> a Pharmacist Intervention Towards Improving<br />
Medication Adherence in Patients Attending Cardiac Rehabilitation: A<br />
Randomized Controlled Trial<br />
3. Prioritizing Pharmaceutical Activities – A Simulation<br />
National Survey <strong>of</strong> Critical Care <strong>Pharmacists</strong>’ Views and<br />
Involvement in Clinical Research<br />
Marc Perreault, Zoé Thiboutot, Lisa Burry, Louise Rose, Salmaan Kanji,<br />
Jaclyn LeBlanc, Roxane Carr, David Williamson<br />
Rationale: <strong>Canadian</strong> critical care pharmacists are increasingly involved in<br />
clinical research. Over the last four years, two multicenter studies evaluating<br />
use <strong>of</strong> pharmacotherapy in <strong>Canadian</strong> intensive care units were successfully<br />
performed by pharmacists. However, the current state <strong>of</strong> clinical research<br />
conducted by these clinicians is not known.<br />
Objectives: The objectives were to describe the clinical research experience<br />
as well as beliefs and views about clinical research <strong>of</strong> <strong>Canadian</strong> critical care<br />
pharmacists.<br />
Study Design and Methods: A nation-wide survey <strong>of</strong> critical care<br />
pharmacists was conducted. The questionnaire was pre-tested and then<br />
submitted to a validation process that included pilot-testing and clinical<br />
sensibility testing. Once completed, the survey was distributed to an<br />
identified sample <strong>of</strong> critical care pharmacists. Pharmacy associations and<br />
individual hospital pharmacy departments across Canada were contacted to<br />
establish a list <strong>of</strong> Critical Care <strong>Pharmacists</strong>. The survey was self-administered<br />
and a mixed-mode format was used. Only surveys completed >70% were<br />
analysed.<br />
Results: 325 Critical Care pharmacists were identified and invited to<br />
participate. A total <strong>of</strong> 215 from all regions <strong>of</strong> Canada completed the survey.<br />
In regards to research experience in the last 5 years, 32,7% <strong>of</strong> respondents<br />
had participated at least once in the development <strong>of</strong> a research protocol,<br />
24,3% more than 3 times and 43,7% had presented results at least one or<br />
twice. In regards to publications, 15,9% <strong>of</strong> respondents had published as<br />
first authors and 23,8% as coauthors. When asked about their interest and<br />
opportunities, 64,5% had a strong interest in research and 61,9%<br />
responded they had opportunities to be involved in research. However,<br />
80,8% felt they did not have enough time to carry out research and only<br />
50,2% felt pharmacy administration support.<br />
Conclusion: Critical care pharmacists across Canada are interested and<br />
involved in clinical research. Opportunities are present but adequate time<br />
and support seem to be barriers.<br />
<strong>Hospital</strong> Wide Roll-Out <strong>of</strong> Antimicrobial Stewardship:<br />
A Stepped Wedge Randomized Controlled Trial<br />
Nick Daneman, Marion Elligsen, Sandra Walker, Lesley Palmay, Andrew<br />
Simor, Samira Mubareka, Anita Rachlis, Vanessa Allen, Ruxandra Pinto<br />
Sunnybrook Health Sciences Centre, Toronto, ON<br />
Rationale: Inappropriate antimicrobial use, increasing antibiotic resistance,<br />
and lack <strong>of</strong> development <strong>of</strong> new antimicrobial agents, has provided the<br />
impetus for worldwide initiatives in antimicrobial stewardship. However,<br />
there is paucity <strong>of</strong> good quality evidence to evaluate the impact <strong>of</strong> such<br />
initiatives. As a result <strong>of</strong> the positive impact our institution’s Antimicrobial<br />
Stewardship <strong>Program</strong> (ASP) had in the critical care unit, we rolled out our<br />
stewardship intervention to seven patient care services across the hospital<br />
using a stepped-wedge design to provide a more rigorous evaluation <strong>of</strong> the<br />
efficacy <strong>of</strong> our interventions.<br />
Objective: To determine the impact <strong>of</strong> antimicrobial stewardship on<br />
antimicrobial use and C. difficile infection rates in seven non-intensive care<br />
medical and surgical services.<br />
Study Design and Methods: A formal review <strong>of</strong> all patients on their 3rd<br />
or 10th day <strong>of</strong> broad-spectrum antibiotic therapy in seven patient care<br />
services was conducted at Sunnybrook Health Sciences Centre using a<br />
stepped–wedge randomized design. The primary outcome for the<br />
preliminary 11 month analysis was a comparison <strong>of</strong> days <strong>of</strong> therapy (DOTs)<br />
<strong>of</strong> targeted antibiotics/1000 patient bed days/month during the<br />
intervention period compared to the control period. Secondary outcomes<br />
included overall and non-targeted antibiotic use and rates <strong>of</strong> nosocomial<br />
C.difficile infections.<br />
Results: From November, 1, 2010 to July 31, 2011, the ASP reviewed a<br />
total <strong>of</strong> 1,042 orders with an overall suggestion and acceptance rate <strong>of</strong><br />
48% and 84%, respectively. Across all services, our program reduced<br />
broad-spectrum antimicrobial use by 12% (256 to 225 DOT/1000 patient<br />
days) and the number C. difficile infection by 59% (44 to 18 cases).<br />
Conclusion: Sunnybrook’s ASP hospital-wide roll-out <strong>of</strong> its case-by-case<br />
audit-and-feedback intervention was successful in reducing broad-spectrum<br />
antimicrobial use and C. difficile infection rates.<br />
Evaluation <strong>of</strong> Concordance to Ventilator-Associated<br />
Pneumonia Guidelines in the Intensive Care Unit Before and<br />
During Antimicrobial Stewardship<br />
Eileen Hill 1 , Matthew Muller 1,2 , Clarence Chant 1 , Reem Haj 1<br />
1 St Michael’s, Toronto, ON<br />
2 University <strong>of</strong> Toronto, Toronto, ON<br />
Rationale: Ventilator-associated pneumonia (VAP) guideline concordance<br />
may improve patient outcomes. Concordance measures the appropriate<br />
physician application <strong>of</strong> guidelines at a patient-specific level. When<br />
guideline concordance is suboptimal, an antimicrobial stewardship program<br />
(ASP) has the potential to improve it.<br />
Objectives: To measure guideline concordance and outcomes for patients<br />
in the intensive care unit (ICU) with VAP before and during implementation<br />
<strong>of</strong> an ASP-pilot.<br />
Methods: This was a retrospective review <strong>of</strong> patients in the<br />
Medical/Surgical and Trauma/Neurosurgery (MS/TN) ICUs with suspected<br />
VAP on ≥3 days <strong>of</strong> targeted antimicrobials. Data was collected<br />
pre-implementation (January to June 2010), and during implementation <strong>of</strong><br />
the ASP-pilot (October 2010 to February 2011). The primary outcome was<br />
overall guideline concordance, which consisted <strong>of</strong> concordance with<br />
empiric drug choice, duration, de-escalation, and route. Concordance was<br />
assessed, using standard case-report forms, by an investigator and a<br />
blinded 3rd party observer. Secondary outcomes were ICU mortality, ICU<br />
length <strong>of</strong> stay (LOS) and duration <strong>of</strong> therapy. Data was summarized using
45<br />
descriptive statistics and compared using Student’s t-test, Mann-Whitney<br />
test and Fischer’s-exact test where appropriate.<br />
Results: Nineteen patients with VAP were enrolled into each group, with<br />
similar baseline demographics and clinical parameters. There were no<br />
differences between the pre-ASP group and the ASP-pilot group in overall<br />
concordance and in concordance to the individual components (overall:<br />
5.3% vs. 10.5%, p=1.0; empiric drug choice: 33.3% vs. 50%, p=0.68;<br />
de-escalation: 76.5% vs. 93.8%, p=0.34; duration: 27.8% vs. 29.4%,<br />
p=1.0; route: 47.4% vs. 47.4%, p=1.0). There were also no differences<br />
between the groups for ICU mortality (2 vs. 6, p=0.2), mean ICU LOS (21<br />
vs. 26 days, p=0.99), or mean duration <strong>of</strong> therapy (10 vs. 9.4 days, p=0.3).<br />
Conclusion: VAP guideline concordance is poor overall, but concordance to<br />
individual components is highly variable. The ASP-pilot did not significantly<br />
improve concordance or change patient outcomes.<br />
2 CSHP<br />
Targeting Excellence<br />
Identifying Barriers to Pharmacist Medication<br />
Discharge Counselling<br />
in Pharmacy Practice<br />
Sandra AN Walker, Jennifer Lo, General Medicine <strong>Pharmacists</strong>,<br />
Sunnybrook Health Sciences Centre, Toronto, ON<br />
Rationale: Medication errors may occur more frequently at discharge,<br />
making discharge counselling a vital facet <strong>of</strong> medication reconciliation.<br />
Data identifying barriers to discharge counselling by pharmacists in adult<br />
hospitalized patients is lacking.<br />
Objective: The objective was to identify barriers to pharmacists performing<br />
medication discharge counselling and to determine their relative frequency<br />
<strong>of</strong> occurrence and time expenditure.<br />
Study Design and Methods: A prospective study <strong>of</strong> all general medicine,<br />
nephrology or medical oncology acute care hospital pharmacists (N=8) was<br />
conducted. <strong>Pharmacists</strong> completed a survey on each <strong>of</strong> the first 50 patients<br />
eligible for discharge counselling on their wards (n = 400). Patients were<br />
considered ineligible for counselling if they were to be discharged to<br />
another facility, had
46<br />
Poster Sessions<br />
There are two different types <strong>of</strong> poster presentations at PPC 2012. A<br />
Facilitated Poster session on Sunday and traditional Poster sessions on<br />
Monday, Tuesday and Wednesday.<br />
Facilitated Poster Session<br />
Posters in the facilitated poster session consist <strong>of</strong> a mixture <strong>of</strong> award<br />
winners and those abstracts submitted in the categories <strong>of</strong> original research<br />
and pharmacy practice. They are grouped as 5 or 6 posters with similar<br />
themes outlined below. The author <strong>of</strong> each poster will do a 6 minute<br />
presentation in front <strong>of</strong> their poster highlighting the key points <strong>of</strong> their<br />
work. This will be followed by questions and group discussion. The<br />
presentations within each group will occur in sequence as the participants<br />
move from one poster to the next. The session is scheduled from 09:30 to<br />
11:30, but posters will be displayed throughout the day.<br />
Traditional Poster Session<br />
Posters in the traditional sessions were selected from those submitted in the<br />
categories <strong>of</strong> original research and pharmacy practice. Although no formal<br />
presentations will occur, the author <strong>of</strong> each poster will be available during<br />
the presentation timeslot for discussion and questions. Posters will be<br />
available for viewing throughout the day.<br />
CSHP 2015<br />
CSHP 2015 is a quality program that sets out a vision <strong>of</strong> pharmacy practice<br />
excellence in the year 2015. Through this project, CSHP challenges hospital<br />
pharmacists to reach measurable targets for 36 objectives grouped under 6<br />
goals, all aimed toward the effective, scientific, and safe use <strong>of</strong> medications<br />
and meaningful contributions to public health. CSHP 2015 applies to<br />
inpatients and outpatients, community and hospital pharmacists, and all<br />
practice settings. Posters identified with a “CSHP 2015” logo are those<br />
judged by the CSHP 2015 Steering Committee to be particularly relevant to<br />
one or more <strong>of</strong> the 36 objectives.<br />
Séances d’affichage<br />
Deux types de présentation par affiches seront <strong>of</strong>ferts dans le cadre de la<br />
CPP 2012. Une séance animée de présentations par affiches qui se tiendra<br />
le dimanche et des séances traditionnelles d’affichage qui auront lieu lundi,<br />
mardi et mercredi.<br />
Séance animée d’affichage<br />
Les affiches de la séance animée d’affichage sont formées d’un mélange de<br />
résumés primés et de résumés soumis dans les catégories recherche<br />
originale et pratique de la pharmacie. Elles sont combinées en groupes de<br />
cinq ou six affiches ayant des thèmes similaires comme il est fait mention<br />
ci-dessous. L’auteur de chaque affiche fera une présentation de six minutes<br />
devant son affiche, faisant ressortir les principaux points de son travail.<br />
Cette présentation sera suivie d’une période de questions et d’une<br />
discussion de groupe. Les présentations à l’intérieur de chaque groupe<br />
auront lieu les unes à la suite des autres au fur et à mesure que les<br />
participants se déplaceront d’une affiche à la suivante. Cette séance se<br />
déroulera de 9 h 30 à 11 h 30.<br />
Séance traditionnelle d’affichage<br />
Les affiches pour les séances traditionnelles ont été choisies parmi celles<br />
soumises dans les catégories recherche originale et pratique de la<br />
pharmacie. Bien qu’aucune présentation <strong>of</strong>ficielle n’ait été prévue, les<br />
auteurs de chaque affiche seront sur place pendant les heures d’affichage<br />
et pourront répondre aux questions et s’entretenir avec vous. Les affiches<br />
pourront être examinées tout au long de la journée.<br />
SCPH 2015<br />
Le projet SCPH 2015 est un programme axé sur la qualité qui propose une<br />
vision de l’excellence en pratique pharmaceutique en l’an 2015. Au moyen<br />
de ce projet, la SCPH met les pharmaciens d’établissements au défi<br />
d’atteindre les cibles mesurables de 36 objectifs répartis entre 6 buts, visant<br />
tous l’utilisation efficace, scientifique et sûre des médicaments ainsi que des<br />
contributions significatives à la santé publique. Le projet SCPH 2015<br />
s’applique aux patients hospitalisés et externes, aux pharmaciens<br />
d’hôpitaux et communautaires, et à tous les milieux de pratique. Les<br />
affiches marquées du logo « SCPH 2015 » sont celles que le comité<br />
directeur du projet SCPH 2015 a jugé particulièrement appropriées à l’un<br />
ou l’autre des 36 objectifs.<br />
Sunday February 5, 2012<br />
09:30-11:30 (presentations)<br />
Essex Ballroom<br />
Facilitated Poster Session: Discussion <strong>of</strong> Original Research, Award<br />
Winning Projects and Pharmacy Practice Projects<br />
Séance animée de présentations par affiches: Discussions sur des projets<br />
de recherche originale, des projets primés et des projets dans le domaine de<br />
la pratique pharmaceutique<br />
Antimicrobials and Pediatrics<br />
1. An Outpatient Parenteral Antimicrobial Therapy <strong>Program</strong> Experience at<br />
the University Health Network<br />
2. Evaluation <strong>of</strong> a Prospective Audit and Feedback <strong>Program</strong> in Critical Care:<br />
A Controlled Interrupted Time Series Analysis (Award)<br />
3. Antimicrobial Prescribing Practices for Catheter Urine Cultures<br />
4. Oseltamivir Pharmacocinketics in Morbid Obesity (OPTIMO Trial) (Award)<br />
5. Description <strong>of</strong> Prop<strong>of</strong>ol Use in a Pediatric Intensive Care Unit<br />
6. Development and Implementation <strong>of</strong> a Pediatric Emergency Department<br />
Asthma Action Plan and Prescription (AAPP) (Award)<br />
Clinical Pharmacy<br />
1. Providing Comprehensive Assessment and Pharmaceutical Care at the<br />
Geriatric Clinic for Parkinson’s<br />
2. Performance <strong>of</strong> Clinical Prediction Tools Used to Predict Major Bleeding<br />
in Patients Receiving Anticoagulation Therapy<br />
3. Development <strong>of</strong> a Clinical Institute Withdawl Assessment (CIWA) Scale<br />
and Treatment Regimen for the Management <strong>of</strong> Alcohol Withdrawl<br />
4. Implementation <strong>of</strong> an Insulin Pen Piolet in an In-Patient <strong>Hospital</strong> Setting<br />
5. Organizational Restructuring <strong>of</strong> Regional Pharmacy Services and<br />
Pharmacy Practice Model (Award)<br />
6. Drug Evaluation <strong>of</strong> Intravenous Tranexamic Acid: Adherence to <strong>Hospital</strong><br />
Guidelines and Adverse Events in an Off-Label Use in Orthopedic<br />
Patients<br />
Patient Safety<br />
1. Extending <strong>Hospital</strong>-Based Medication Incident Reporting to Enhance<br />
Medication Safety and Continuous Quality Assurance in Pharmacy<br />
Practice (Award)<br />
2. Implementation and Evaluation <strong>of</strong> Medication Reconciliation Tool on<br />
Internal <strong>Hospital</strong> Transfer (Award)<br />
3. Improving Continuity <strong>of</strong> Care Post-<strong>Hospital</strong> Discharge: A Needs<br />
Assessment <strong>of</strong> Community <strong>Pharmacists</strong><br />
4. Patient Recall <strong>of</strong> Interaction with a Pharmacist During <strong>Hospital</strong><br />
Admission<br />
5. How Well Do Pharmacy Clinicians Perform in a Patient<br />
Simpultion-Based Admission Medication Reconciliation Validation<br />
<strong>Program</strong>?
47<br />
6. Who's Looking at the BPMH? Prescription and Utilization <strong>of</strong> the Best<br />
Possible Medication History in a Tertiary Care <strong>Hospital</strong><br />
Education and Research<br />
1. The Evaluation <strong>of</strong> a New Hierarchical Teaching Model for Pharmacy<br />
Students in Experiential Education<br />
2. Evaluation <strong>of</strong> Effectiveness <strong>of</strong> Online versus Face to Face Interactions in<br />
Interpr<strong>of</strong>essional Education<br />
3. An Online E-Learning Patient Education Tool for SOT Recipients (Award)<br />
4. Diabetes Education in Pharmacy Residencies Across Canada<br />
5. Evaluating the Role <strong>of</strong> Pharmacist Teachers in <strong>Canadian</strong> Family<br />
Medicine Residency <strong>Program</strong>s: A Qualitative Analysis (Award)<br />
6. A Survey <strong>of</strong> Institutional <strong>Pharmacists</strong> Involvement in and Attitudes<br />
Towards Research (Award)<br />
Oncology<br />
1. Interactions Between Antiretroviral Agents and Chemotherapy<br />
Regimens for the Treatment <strong>of</strong> Lymphoma: A Quick Reference Guide<br />
(Award)<br />
2. Impact <strong>of</strong> Drug Access Facilitator in an Outpatient Chemotherapy Clinic<br />
3. High Dose Methotrexate in Adult Oncology Patients: A Case-Control<br />
Study Assessing the Risk Association Between Drug Interactions and<br />
Methotrexate Toxicity<br />
4. Stability <strong>of</strong> Azacitidine Solutions in Sterile Water for Injection<br />
5. Pharmacist-Directed Toxicity Management <strong>Program</strong> for Patients<br />
Receiving Capecitabine: Implementation and Evaluation (Award)<br />
Monday February 6, 2012<br />
09:45-10:15 (viewing)<br />
13:15-13:50 (presentations)<br />
Sheraton/Osgoode Halls<br />
1. In For a Penny, in for a Pound: Evaluation <strong>of</strong> Factors Affecting Learner<br />
Participation in the Pilot ADAPT E-Learning Primary Health Care<br />
<strong>Program</strong><br />
2. Moving Practice Forward with Early Exposure Students<br />
3. Provincial Implementation <strong>of</strong> Accreditation Canada Required<br />
Organizational Practices: The Alberta Experience<br />
4. Drugs Obtained by Quebec University Health Centers through Health<br />
Canada’s Special AccessPprogramme – Descriptive Analysis by the<br />
programme de gestion therapeutique des Medicament<br />
5. Safety and Efficacy <strong>of</strong> CHOP or R-chop for Treatment <strong>of</strong> Diffuse Large<br />
B-cell Lymphoma with Protease Inhibitor or Non-Protease Inhibitor<br />
Based Antiretroviral Regimens in HIV–infected patients: SCULPT Study<br />
6. Drug Access Navigator Database: Improving the Management <strong>of</strong> Drug<br />
Access Cases through the Development and Implementation <strong>of</strong> a<br />
Computerized Database<br />
7. Residents as Preceptors: Development, Implementation and Evaluation<br />
<strong>of</strong> a Pharmacy Summer Student Clinical Experience<br />
8. Imatinib Plasma Through Concentrations and the Ability to Assess<br />
Patient Adherence<br />
9. Evolution de la thromboprophylaxie chez les usagers medicaux dans un<br />
institute universitaire<br />
10. 2010-2011 Perspectives on Drug Shortages in <strong>Hospital</strong>s in Quebec<br />
11. Multicenter Study on Environmental Contamination by Hazardous<br />
Drugs in Quebec Healthcare Centres<br />
12. Temps associe a la purge des tublures lors de la preparation d’une dose<br />
de medicament dangereux et contamination visuelle<br />
13. Is Vasopressin (>0.03 units/minute) Associated with the Adverse Events<br />
in Cardiac Surgery Patients?<br />
14. Assessing the Extent <strong>of</strong> Fluoroquinolone-Cation Interactions at a<br />
Teaching <strong>Hospital</strong><br />
Tuesday February 7, 2012<br />
09:45-10:15 (viewing)<br />
13:15-13:50 (presentation)<br />
Sheraton/Osgoode Halls<br />
1. A Systematic Analysis <strong>of</strong> Pharmacist Referrals Originating from the<br />
Order Desk<br />
2. Audit <strong>of</strong> Antibiotic Duration <strong>of</strong> Therapy, Appropriateness and Outcome<br />
in Patients with Nosocomial Pneumonia Following the Removal <strong>of</strong> an<br />
Automatic Stop-date Policy<br />
3. Identification <strong>of</strong> Predictors <strong>of</strong> Infection in Acute Burn Injury<br />
4. Impact <strong>of</strong> a Multi-Layered Initiative to Improve Venous<br />
Thromboembolism Prophylaxis Rates in Medicine Patients in a<br />
Community <strong>Hospital</strong> Setting<br />
5. A Pilot Study to Evaluate Methodology for Assessing the Treatment <strong>of</strong><br />
Low Back Pain<br />
6. Classifications <strong>of</strong> Drug Related Problems Discovered During Senior<br />
Brown Bag Medication Reviews<br />
7. Evaluation <strong>of</strong> Education on Preventative Care and Poison Control<br />
Center Awareness During Brown Bag Medication Reviews for Older<br />
Adults<br />
8. Self-Perceived Knowledge Gained and Satisfaction from Brown Bag<br />
Medication Reviews for Older Adults<br />
9. Cost Analysis <strong>of</strong> an Insulin Pen Pilot Project in an In-Patient <strong>Hospital</strong><br />
Setting<br />
10. Venous Thromboembolism Prophylaxis Electronic Physician Risk<br />
Assessment Tool<br />
11. Fingertip Sampling is a More Sensitive Evaluation <strong>of</strong> Aseptic Technique<br />
Competency<br />
12. Potential Cross-Reactivity between Prasugrel and Clopidogrel<br />
13. Total Parenteral Nutrition: Supporting Practice Through Standardizing<br />
Solutions<br />
14. Determination <strong>of</strong> Tobramycin Pharmacokinetics in Burn Patients to<br />
Evaluate the Potential Utility <strong>of</strong> Once Daily Dosing in this Population<br />
Wednesday February 8, 2012<br />
10:15-10:45 (presentations)<br />
Churchill Room<br />
1. Diagnostic Reasoning by <strong>Hospital</strong> <strong>Pharmacists</strong>: An Assessment <strong>of</strong><br />
Attitudes, Knowledge, Skills, and Learning Needs<br />
2. A Pilot Study on the Use <strong>of</strong> Warfarin Sliding Scales in Hemodialysis<br />
Patients<br />
3. Potentially Inappropriate Medication Use in Elderly Patients Presenting<br />
to the Emergency Department<br />
4. Intentional Overdose <strong>of</strong> Enoxaparin<br />
5. Implementation <strong>of</strong> a Pharmacy Residency <strong>Program</strong> in Primary Care<br />
6. Differences in Nova Scotian <strong>Pharmacists</strong>’ Experiences and Barriers to<br />
Providing the Emergency Contraceptive Pill Based on Primary Practice<br />
Site<br />
7. Chemotherapy-Induced Nausea and Vomiting in Children Receiving<br />
Ifosfamide Plus Etoposide: Preliminary Results<br />
8. Improving a Complex Pharmacist Scheduling Model at a Tertiary Care<br />
<strong>Hospital</strong><br />
9. Statin Treatment Use in Diabetics with Breast Cancer: A Potential<br />
C-Reactive Protein Mediated Benefit
48<br />
Sunday, February 5<br />
Dimanche 5 février<br />
An Outpatient Parenteral Antimicrobial Therapy <strong>Program</strong><br />
Experience at the University Health Network<br />
Anjie Yang 1 , Ron Fung 1 , James Brunton 2 , Linda Dresser 1,3<br />
1 Department <strong>of</strong> Pharmacy, University Health Network, Toronto, ON<br />
2 Department <strong>of</strong> Medicine - Division <strong>of</strong> Infectious Diseases, University Health<br />
Network, Toronto, ON<br />
3 Leslie Dan Faculty <strong>of</strong> Pharmacy, University <strong>of</strong> Toronto, Toronto, ON<br />
Rationale for Report: Current literature shows that Outpatient Parenteral<br />
Antimicrobial Therapy (OPAT) programs improve treatment efficacy and<br />
safety for patients discharged on intravenous (IV) antimicrobials. However,<br />
such programs are still relatively new in Ontario. In response to cases <strong>of</strong><br />
treatment related adverse events with the present standard <strong>of</strong> care, an<br />
OPAT program was developed, implemented and evaluated.<br />
Description <strong>of</strong> Situation: Adverse events involving nephrotoxicity among<br />
outpatients receiving IV vancomycin identified a gap in antimicrobial<br />
management. The OPAT program was developed to address this gap.<br />
Development <strong>of</strong> Service: This interpr<strong>of</strong>essional antimicrobial stewardship<br />
effort was fully implemented in February 2010 and included all eligible<br />
patients discharged on IV antimicrobials. The OPAT pharmacist role is<br />
integral in selecting the choice <strong>of</strong> therapy and vascular access device, as<br />
well as providing patient education and monitoring throughout the<br />
treatment course.<br />
Evaluation: A retrospective matched cohort study was conducted involving<br />
108 surgery patients enrolled in the OPAT program between Feb 1 and Nov<br />
30, 2010, with cure rates, 30-day rehospitalization within our hospital and<br />
length <strong>of</strong> stay as primary endpoints. The OPAT patients were matched 1:1<br />
to historical controls discharged between Jan 1, 2001 and Jan 1, 2010<br />
based on age, gender, type <strong>of</strong> surgery, infection, and co-morbidities<br />
(Charlson Co-morbidity Index). Due to the rigor <strong>of</strong> the matching criteria,<br />
twenty-one OPAT patients were matched. For this cohort, the OPAT<br />
program was trending towards improved cure rates (61.9% vs 57.1%),<br />
reductions in rehospitalization (14.3% vs 28.6%) and mean length <strong>of</strong> stay<br />
(10.7 vs 13.9 days) compared to the control group.<br />
Importance to Practice: The OPAT program is an innovative expansion <strong>of</strong> the<br />
antimicrobial stewardship program, with the pharmacist role being crucial<br />
in optimizing antimicrobial therapy in the outpatient setting. A further<br />
evaluation <strong>of</strong> the impact <strong>of</strong> this project on rehospitalizations province-wide<br />
is in progress.<br />
Evaluation <strong>of</strong> a Prospective Audit and Feedback <strong>Program</strong> in<br />
Critical Care: A Controlled Interrupted Time Series Analysis<br />
Marion Elligsen 1 , Sandra A.N. Walker 1,2,4 , Ruxandra Pinto 3 , Andrew Simor 4,5 ,<br />
Samira Mubareka 3,4,5 , Anita Rachlis 4,5 , Vanessa Allen 4,5,6 , Nick Daneman 3,4,5,7<br />
1 Sunnybrook Health Sciences Centre, Department <strong>of</strong> Pharmacy; Toronto, ON<br />
2 University <strong>of</strong> Toronto, Leslie L. Dan Faculty <strong>of</strong> Pharmacy; Toronto, ON<br />
3 Sunnybrook Research Institute; Toronto, ON<br />
4 Sunnybrook Health Sciences Centre, Department <strong>of</strong> Microbiology and<br />
Division <strong>of</strong> Infectious Diseases; Toronto, ON<br />
5 University <strong>of</strong> Toronto, Faculty <strong>of</strong> Medicine; Toronto, ON<br />
6 Public Health Ontario; Toronto, ON<br />
7 Institute for Clinical Evaluative Sciences, Toronto, ON<br />
Rationale: While there is support for antibiotic stewardship programs in<br />
critical care, most data comes from uncontrolled before-and-after studies<br />
that are prone to bias and temporal confounding.<br />
Objective: We aimed to rigorously evaluate the impact <strong>of</strong> a prospective<br />
audit-and-feedback program in critical care patients, using a controlled,<br />
interrupted time series analysis.<br />
Methods: The antimicrobial stewardship team provided prospective<br />
audit-and-feedback for all patients in level III ICUs on their 3rd or 10th day<br />
<strong>of</strong> targeted broad-spectrum antibiotic therapy. Antibiotic use during the<br />
one year pilot was compared to the year prior using a controlled<br />
interrupted time series analysis. Secondary outcomes included overall<br />
antibiotic use, gram negative bacterial susceptibility, rates <strong>of</strong> nosocomial<br />
C.difficile infection, length <strong>of</strong> stay and mortality.<br />
Results: Broad-spectrum antibiotic use significantly decreased (119<br />
DOTs/1000 PDs; SE=37.9; p=0.0054) with the implementation <strong>of</strong> the<br />
program, with no change in either control wards or use <strong>of</strong> control<br />
medications (stress ulcer prophylaxis). The incidence <strong>of</strong> C. difficile infections<br />
decreased from 11 to 6 cases, while increasing in the control wards from 87<br />
to 116 cases (p=0.04). Overall gram negative susceptibility to meropenem<br />
increased. Length <strong>of</strong> stay and mortality did not change.<br />
Conclusions: Through collaboration with critical care, a successful<br />
prospective audit-and-feedback program was implemented in the level III<br />
ICUs.<br />
Key Words: Antimicrobial Stewardship, Critical Care, Intensive Care<br />
Antimicrobial Prescribing Practices for Catheter Urine<br />
Cultures<br />
Jonathan Chiu, William G. Thompson, Thomas W. Austin, Michael John,<br />
Zafar Hussain, Anne Marie Bombassaro, Sarah Connelly, Sameer Elsayed,<br />
London Health Sciences Centre, London, ON<br />
Rationale: To investigate the literature suggestion that positive catheter<br />
urine cultures frequently result in unnecessary antimicrobial prescribing.<br />
Objectives: The study objective was to determine the need for<br />
antimicrobial stewardship directed to catheter urine cultures by evaluating<br />
concordance <strong>of</strong> treatment decisions between an expert panel and<br />
prescribers.<br />
Methods: This was a retrospective case-control study <strong>of</strong> adults at a tertiary<br />
care centre. Cases and controls were defined as having positive and<br />
negative catheter urine cultures, respectively, and were identified through a<br />
microbiology laboratory report. Medical records were consecutively<br />
screened to select a convenience sample <strong>of</strong> 80 inpatients (40 per group).<br />
Abstracted patient histories were independently evaluated by an expert<br />
panel (3 Infectious Diseases consultants) blinded to decisions <strong>of</strong> prescribers<br />
and fellow panelists. The primary endpoint <strong>of</strong> concordance was defined as<br />
agreement between experts and prescribers (majority response) with<br />
respect to the indication for therapy. Secondary endpoints including<br />
unnecessary days <strong>of</strong> therapy and predefined patient outcomes were<br />
assessed over a 7-day period.<br />
Results: Target enrolment required screening 591 charts. Intensive care<br />
stay, immunosuppression and emergency/outpatient status were the main<br />
reasons for exclusion. Baseline demographics between groups were<br />
comparable. Concordance was 40% (16/40) and 85% (34/40) in cases and<br />
controls, respectively (OR 0.118, 95% CI 0.04-0.344; p
49<br />
4 Department <strong>of</strong> Medicine, Dalhousie University, Halifax, NS<br />
5 Capital District Health Authority Halifax Infirmary, Pharmacy Department,<br />
Halifax, NS<br />
6 WK Health Centre, Halifax, NS<br />
7<br />
<strong>Canadian</strong> Centre for Vaccinology, Halifax, NS<br />
Synopsis<br />
Background: Detailed pharmacokinetics to guide oseltamivir (Tamiflu ®)<br />
dosing in morbidly obese patients is lacking.<br />
Objectives: Characterize the single dose and steady state<br />
pharmacokinetics <strong>of</strong> oseltamivir and its active carboxylate metabolite in this<br />
population.<br />
Methods: The OPTIMO trial was a single center non-randomized open<br />
label pharmacokinetic study <strong>of</strong> single dose and steady state oral oseltamivir<br />
phosphate and active metabolite in healthy morbidly obese and healthy,<br />
non-obese subjects.<br />
Results: In the morbidly obese v.s. control subjects, respectively, the<br />
single-dose median oseltamivir: oral clearance, CL/F [840 v.s. 580 L h-1] was<br />
higher; the area under the curve (AUC0-¥) [89 v.s. 132 ng mL-1 h] was<br />
lower and, the volume <strong>of</strong> distribution Vd/F [2320 v.s. 1670 L] was<br />
unchanged. In the morbidly obese v.s. control subjects, respectively, the<br />
single-dose median oseltamivir carboxylate CL/F, AUC0-12h and Vd/F did<br />
not differ significantly. Similar results for oseltamivir and oseltamivir<br />
carboxylate CL/F, AUC0-12h and Vd/F values were observed in the multiple<br />
dose study.<br />
Conclusions: Systemic exposure to oseltamivir is decreased but that <strong>of</strong><br />
oseltamivir carboxylate is largely unchanged. Based on these<br />
pharmacokinetic data, an oseltamivir dose adjustment for body weight<br />
would not be needed in morbid obese individuals.<br />
Key Words: Oseltamivir, obesity, body mass index, obese,<br />
pharmacokinetics<br />
Description <strong>of</strong> Prop<strong>of</strong>ol Use in a Pediatric Intensive Care Unit<br />
Hiromi Koriyama 1 , Margaret L. Ackman 2 , Jonathan P. Duff 3 , Alice W. Chan 2<br />
1 Pharmacy Services, Covenant Health, Edmonton, AB<br />
2 Pharmacy Services, Alberta Health Services, Edmonton, AB<br />
3 Department <strong>of</strong> Pediatrics, University <strong>of</strong> Alberta, Edmonton, AB<br />
Rationale: Prop<strong>of</strong>ol infusions continue to be used in pediatric intensive<br />
care units (PICUs), despite being contraindicated in this population due to<br />
concerns <strong>of</strong> prop<strong>of</strong>ol related infusion syndrome (PRIS). However, some<br />
studies have not identified harm with prop<strong>of</strong>ol use in PICUs. The <strong>Canadian</strong><br />
Pediatric Critical Care Network (CPCCN) prepared a consensus statement<br />
on prop<strong>of</strong>ol use in PICUs, suggesting a 4 mg/kg/h maximum mean rate and<br />
24 hour maximum duration. Since this statement was developed, no<br />
studies have evaluated prop<strong>of</strong>ol use in the Stollery Children’s <strong>Hospital</strong> PICU.<br />
Objectives: To describe the practice patterns <strong>of</strong> prop<strong>of</strong>ol use in a<br />
single-center PICU, the rate <strong>of</strong> concordance <strong>of</strong> prop<strong>of</strong>ol use with CPCCN<br />
guidelines, and assess for the presence <strong>of</strong> signs and symptoms <strong>of</strong> PRIS.<br />
Methods: A retrospective chart review <strong>of</strong> initial prop<strong>of</strong>ol infusions used in<br />
PICU patients admitted during January 1 – December 31, 2009 was<br />
conducted. Charts were reviewed for prop<strong>of</strong>ol infusion characteristics, and<br />
presence <strong>of</strong> signs and symptoms <strong>of</strong> PRIS.<br />
Results: Data were collected from 223 patients. The mean <strong>of</strong> the average<br />
hourly prop<strong>of</strong>ol dose (including boluses) was 2.8±1.2 mg/kg/h and the<br />
average infusion duration was 10.3±6.7 hours. 86.5% and 97.8% <strong>of</strong><br />
infusions were concordant with CPCCN guideline maximum mean rate and<br />
duration, respectively. No cases <strong>of</strong> PRIS or deaths associated with prop<strong>of</strong>ol<br />
infusions were identified.<br />
Conclusions: Initial prop<strong>of</strong>ol infusions are being used in the Stollery<br />
Children’s <strong>Hospital</strong> PICU with a mean average hourly dose <strong>of</strong> 2.8 mg/kg/h<br />
and average duration <strong>of</strong> 10.3 hours. The majority <strong>of</strong> use was in<br />
concordance with CPCCN guidelines, but the need for consideration <strong>of</strong> the<br />
use and contribution <strong>of</strong> bolus doses to hourly prop<strong>of</strong>ol dose was identified.<br />
The use <strong>of</strong> initial prop<strong>of</strong>ol infusions in PICU patients appears to be safe, as<br />
an association with presence <strong>of</strong> signs and symptoms <strong>of</strong> PRIS, cases <strong>of</strong> PRIS,<br />
or death were not found.<br />
Development and Implementation <strong>of</strong> a Pediatric Emergency<br />
Department (ED) Asthma Action Plan And Prescription<br />
(AAPP)<br />
Danica Irwin, Régis Vaillancourt, Roger Zemek, Elena Pascuet, Children’s<br />
<strong>Hospital</strong> <strong>of</strong> Eastern Ontario (CHEO), Ottawa, ON<br />
Background: National and international asthma guidelines endorse asthma<br />
action plan (AP) use. Preprinted prescription incorporation into the AP<br />
should enhance physician use. Provision <strong>of</strong> information in visual and text<br />
format addresses varied health literacy levels.<br />
Objectives: To develop and implement a pediatric AP combined with a<br />
prescription based on validated pictograms accessible to the patient,<br />
pharmacist and physician.<br />
Methods: The Asthma Action Plan and Prescription (AAPP) was developed<br />
by a working group from ED, Respirology and Pharmacy, with additional<br />
input from the Ontario College <strong>of</strong> <strong>Pharmacists</strong> and the Institute for Safe<br />
Medication Practices. Evidence-based content was enhanced with<br />
pictograms <strong>of</strong> asthma control/triggers, with prescriptions embedded.<br />
Education was sent to ED staff via emails, posters and educational sessions.<br />
The ED pharmacist, via the region’s pharmacy email system/website and<br />
telephone, instructed retail pharmacies how to incorporate the AAPP into<br />
practice.<br />
Results: Since implementation in March 2011, more than 750 AAPPs have<br />
been used. Response is positive based on physician, pharmacist and patient<br />
feedback. An analysis <strong>of</strong> effectiveness is planned.<br />
Conclusions: An AAPP has been developed and implemented to enhance<br />
patient, pharmacist and physician asthma management. The AAPP<br />
facilitates physician use <strong>of</strong> the document and subsequent enhanced rational<br />
medication prescribing.<br />
Key Words: asthma action plan, emergency department, health literacy<br />
2 CSHP<br />
Targeting Excellence<br />
in Pharmacy Practice<br />
Providing Comprehensive Assessment and<br />
Pharmaceutical Care at the Geriatric Clinic for<br />
Parkinson’s<br />
Greta Mah, Joyce Lee, North York General <strong>Hospital</strong>, Toronto, ON<br />
Rationale: Parkinson’s disease (PD) is a common neurodegenerative disease<br />
with majority <strong>of</strong> patients being over the age <strong>of</strong> 60. Traditionally, PD<br />
management focuses on only motor features which are more apparent.<br />
However, recent studies showed up to 60% <strong>of</strong> patients also suffer from<br />
non-motor symptoms (NMS) leading to cognitive, autonomic and<br />
neuropsychiatric dysfunction which result in greater disability and hospital<br />
admission. Unfortunately, NMS are <strong>of</strong>ten under-diagnosed. In addition,<br />
elderly patients with PD are at high risk <strong>of</strong> experiencing drug therapeutic<br />
problems (DTPs) from their complex medication regimen. Therefore, a<br />
Geriatric Clinic with a physician-pharmacist team was established to provide<br />
comprehensive assessment and pharmaceutical care.<br />
Objectives & Descriptions: A prospective observational study was<br />
designed to determine whether comprehensive assessment could identify<br />
previously unrecognized NMS and to describe the nature <strong>of</strong> DTPs. Patients<br />
were seen by pharmacist followed by physician during each clinic<br />
appointment. Patients also have easy access to the pharmacist for<br />
telephone consultation or urgent assistance. All patients seen from Jan<br />
2008 to Nov 2009 were included in the study which was approved by the<br />
ethic review board.<br />
Results: One hundred and forty patients with an average age <strong>of</strong> 76 were<br />
assessed. About 4 DTPs per patient were identified. Most common DTP was<br />
NMS required treatment such as dementia, depression, anxiety,<br />
constipation, psychosis, orthostatic hypotension and sleep disorders. Other<br />
common DTPs were adverse drug reactions (ADRs), sub-therapeutic dosing<br />
and medication non-adherence. Over 120 ADRs were identified. Most<br />
common presentations were hallucination, confusion, dizziness, sedation
50<br />
and impulsive behaviours (i.e. gambling, hyper-sexuality) which <strong>of</strong>ten lead<br />
to caregiver stress and E.R. visits if not identified early.<br />
Conclusion: Patients and families appreciated the comprehensive<br />
assessment and pharmaceutical care provided by the clinic. Many NMS and<br />
DTPs were managed to maintain patient’s function, quality <strong>of</strong> life and to<br />
prevent unnecessary hospital admission.<br />
2 CSHP<br />
Targeting Excellence<br />
in Pharmacy Practice<br />
Performance <strong>of</strong> Clinical Prediction Tools Used to<br />
Predict Major Bleeding in Patients Receiving<br />
Anticoagulation Therapy<br />
Sarah Burgess, Alejandro Lazo-Langner, George Dresser, Richard Kim,<br />
Natalie Crown, London Health Sciences Centre, London, ON<br />
Rationale: Fear <strong>of</strong> bleeding is a major determinant <strong>of</strong> the underuse <strong>of</strong><br />
anticoagulation therapy. Studies suggest clinical tools developed to predict<br />
major bleeding have poor agreement and predictive ability; however,<br />
guidelines recommend the HAS-BLED score to assess bleeding risk in<br />
patients with atrial fibrillation. The purpose <strong>of</strong> this study is to evaluate the<br />
performance and utility <strong>of</strong> these tools in a real-world clinical setting.<br />
Methods: A retrospective cohort study was performed at the<br />
anticoagulation clinic at University <strong>Hospital</strong>, London Health Sciences Centre.<br />
Clinic charts <strong>of</strong> patients receiving warfarin therapy between September<br />
2008 and February 2011, were reviewed. Bleeding risk factors identified at<br />
first clinic visit were used to apply bleeding risk tools (Outpatient Bleeding<br />
Risk Index, Contemporary Bleeding Risk Model, HEMORR2HAGES,<br />
HAS-BLED) which stratified major bleeding risk as low, moderate or high.<br />
The primary endpoint <strong>of</strong> agreement in risk stratification between the tools<br />
was assessed using Kendall’s tau-b coefficient. All predefined major and<br />
clinically relevant non-major bleeding events were identified from hospital<br />
charts and emergency department encounters. The predictive ability <strong>of</strong> each<br />
tool was evaluated using the C-statistic as a secondary endpoint.<br />
Results: The study included chart-abstracted data for 321 patients on<br />
warfarin therapy with a follow-up <strong>of</strong> 319 patient-years to assess for<br />
bleeding events. The stratification <strong>of</strong> bleeding risk was inconsistent<br />
between the tools, evidenced by Kendall’s tau-b coefficients for agreement<br />
(0.30 to 0.54). There were 3.8 major bleeds and 8.1 clinically relevant<br />
non-major bleeds per 100 patient-years <strong>of</strong> observation. C-statistics for<br />
predicting major bleeding were 0.61, 0.67, 0.71, 0.74 for Outpatient<br />
Bleeding Risk Index, HAS-BLED, Contemporary Bleeding Risk Model, and<br />
HEMORR2HAGES, respectively, demonstrating limited predictive ability.<br />
Conclusion: Bleeding risk prediction tools demonstrated poor agreement<br />
and limited predictive ability for major bleeding events. Further study should<br />
focus on how to incorporate such tools into clinical decision making.<br />
Development <strong>of</strong> a Clinical Institute Withdrawal Assessment<br />
(CIWA) Scale and Treatment Regimen for the Management <strong>of</strong><br />
Alcohol Withdrawal<br />
Rajini Retnasothie, Jason Volling. University Health Network, Toronto, ON,<br />
University <strong>of</strong> Toronto, Toronto, ON<br />
Rationale: The Clinical Institute Withdrawal Assessment Scale – Alcohol<br />
revised (CIWA-Ar) with symptom-triggered benzodiazepine therapy is the<br />
management <strong>of</strong> choice for alcohol withdrawal. Preliminary exploration<br />
revealed that practice at the University Health Network (UHN) was not<br />
completely aligned with these recommendations.<br />
Description: The objective <strong>of</strong> this project was to determine which factors<br />
UHN clinicians felt impeded the current alcohol withdrawal management<br />
process. The goal was to use this information to modify the CIWA-Ar tool<br />
and develop management regimens which integrate the best evidence and<br />
promote consistent, standardized use across our sites.<br />
Implementation: A focus group and survey were conducted to gather<br />
clinicians’ opinions on barriers they faced when managing patients<br />
experiencing acute alcohol withdrawal. A working group was then formed<br />
to review survey results and current evidence, revise the CIWA scoring tool<br />
and develop management regimens.<br />
Evaluation: Survey respondents identified inconsistencies in the prescribing<br />
process as well as variation in benzodiazepine choice, dose, route, and<br />
frequency as major impediments to optimal workflow.<br />
The previous CIWA scoring tool was deemed user-unfriendly, leading many<br />
assessors to use tools from other centers. Respondents also indicated that<br />
most benzodiazepine orders were not linked to CIWA scores. Based on<br />
this information and the evidence, the CIWA scoring tool was revised<br />
and standard orders were developed in paper and electronic form, for<br />
outpatients and inpatients, respectively. These orders feature<br />
three unique benzodiazepine regimens, selected based on patient<br />
factors, which correlate directly to CIWA scores.<br />
Importance: By creating a more user-friendly CIWA-Ar tool with correlating<br />
benzodiazepine orders, we are promoting symptom-triggered therapy,<br />
which is proven to reduce the risk <strong>of</strong> mortality associated with alcohol<br />
withdrawal (when compared to fixed dosing therapy). The modified scoring<br />
tool and order sets can be used by other centers that are also facing<br />
challenges with their alcohol withdrawal management process.<br />
2 CSHP<br />
Targeting Excellence<br />
in Pharmacy Practice<br />
Implementation <strong>of</strong> an Insulin Pen Pilot Project in an<br />
In-Patient <strong>Hospital</strong> Setting<br />
Sara Kynicos 1 , Jin Hyeun Huh 1,2<br />
1 University Health Network, Toronto, ON<br />
2 Leslie Dan Faculty <strong>of</strong> Pharmacy, University <strong>of</strong> Toronto, ON<br />
Rationale: Insulin is considered a high-risk medication due to its potential<br />
to cause severe patient harm when implicated in adverse drug events.<br />
Following insulin medication incidents in our institution, the Safe<br />
Medication Practice committee recommended trialling a novel approach;<br />
in-patient administration by nurses using insulin pens.<br />
Objective: To implement an insulin pen pilot in general internal medicine<br />
(98 beds across 3 floors) at one hospital site over 3 months, then measure<br />
safety outcomes related to medication incidents and satisfaction outcomes<br />
using nurse and patient feedback.<br />
Method: In order to ensure that nursing staff would be able to use the pen<br />
devices and that new types <strong>of</strong> errors would not be introduced, a human<br />
factors usability study was conducted. This simulated various scenarios to<br />
test all steps in the process; including loading cartridges, labelling, priming,<br />
using safety needles and administration <strong>of</strong> dose. The results <strong>of</strong> this testing<br />
were used to design the pilot workflow processes and education for staff.<br />
All existing formulary insulins were made available in pen devices as<br />
floor-stock and each patient was allocated their own pen for each insulin<br />
type.<br />
Results: A review <strong>of</strong> all reported incidents showed that no medication<br />
incidents involving insulin were reported on the pilot floors.<br />
A survey <strong>of</strong> nursing staff showed they preferred to use the insulin pens with<br />
75% wanting to continue. The staff felt that the pens decreased the risk <strong>of</strong><br />
administration <strong>of</strong> incorrect doses, were easy and efficient to use and<br />
allowed for increased patient teaching opportunities. A patient survey<br />
showed that the majority <strong>of</strong> insulin users (87%) preferred for nurses to<br />
administer their insulin with pen devices.<br />
Conclusion: This project demonstrates that insulin pen devices can be<br />
successfully implemented in an in-patient hospital setting, and should be<br />
considered as an option to potentially reduce errors with this high-risk<br />
medication.<br />
Organizational Restructuring <strong>of</strong> Regional Pharmacy Services<br />
to Facilitate Pharmacy Practice Model Change<br />
Kevin W Hall 1 , Colette B Raymond 2 , Donna MM Woloschuk 2 , and Nicholas<br />
Honcharik 2<br />
1 Faculty <strong>of</strong> Pharmacy, University <strong>of</strong> Alberta<br />
2 Winnipeg Regional Health Authority<br />
Background: Prior to restructuring, the Winnipeg Regional Health<br />
Authority’s Pharmacy <strong>Program</strong> (WRHAPP) coordinated the delivery <strong>of</strong><br />
pharmacy services at eight facilities with different drug distribution systems
51<br />
and pharmacy practice models. Pharmacy Managers had matrix<br />
accountability to their site and the WRHAPP.<br />
Objectives: A three year pharmacy change initiative was approved, with<br />
the objectives <strong>of</strong>: i) creating a single line <strong>of</strong> staff accountability to the<br />
WRHAPP, ii) expanding, and standardizing the use <strong>of</strong><br />
information/automation technologies, iii) focusing pharmacists on direct<br />
patient care activities, iv) expanding the role <strong>of</strong> pharmacy technicians to<br />
encompass responsibility for most drug distribution activities, v) creating<br />
management positions for pharmacy technicians, and vi) developing<br />
regional teams <strong>of</strong> specialized pharmacists, aligned with the WRHA’s clinical<br />
program model.<br />
Methods: Changes in the roles <strong>of</strong> pharmacists, technicians, and<br />
automation technology were facilitated by: i) the use <strong>of</strong> a structured project<br />
management approach, ii) the development and delivery <strong>of</strong> targeted<br />
educational/training programs, and iii) a consistent, repetitive<br />
communication strategy<br />
Conclusions: The new model optimizes the use <strong>of</strong> pharmacy staff and<br />
automation technologies and positions the WRHAPP to efficiently deliver<br />
high quality, patient-focused pharmacy services.<br />
Keywords: Pharmacy Practice Model, Automation, Project Management<br />
Drug Use Evaluation <strong>of</strong> Intravenous Tranexamic Acid:<br />
Adherence to <strong>Hospital</strong> Guidelines and Adverse Events in an<br />
Off-Label Use in Orthopedic Patients<br />
C. Dara, North York General <strong>Hospital</strong>, Toronto, ON<br />
Rationale: Routine administration <strong>of</strong> intravenous tranexamic acid (IVTA) for<br />
<strong>of</strong>f-label use during total knee replacement in patients without history <strong>of</strong><br />
thromboembolic disease is associated with a 67% reduction in red blood<br />
cell (RBC) transfusions and, in those transfused, with a reduction in the<br />
number <strong>of</strong> units administered. In the literature, IVTA treatment was not<br />
associated with an increase in thromboembolic complications.<br />
Objectives: The primary objective was to evaluate utilization <strong>of</strong> IVTA based<br />
on Pharmacy and Therapeutics (P&T) approved criteria in both knee and hip<br />
orthopedic patients. The secondary objective was to describe safety<br />
outcomes in patients treated with IVTA, after 6 months <strong>of</strong> usage<br />
Study Design and Methods: The agent was approved for addition to<br />
North York General <strong>Hospital</strong> (NYGH) formulary in January 2011 at a dose <strong>of</strong><br />
10-15mg/kg/dose given intra-operatively and repeated 3 hours<br />
post-operative. A retrospective drug use evaluation was completed on all<br />
patients identified through the pharmacy electronic database receiving IVTA<br />
between January - June 2011. Electronic charts were reviewed by a<br />
pharmacist using an audit tool. Criteria evaluated included compliance with<br />
prescribing criteria in orthopedic patients, incidence <strong>of</strong> hemoarthrosis,<br />
venous thromboembolism (VTE) and transfusion rates, and any hospital<br />
readmission.<br />
Results <strong>of</strong> Study: From January 2011 to June 2011, 31 orthopedic<br />
patients received IVTA<br />
NYGH approved<br />
indications for<br />
IVTA<br />
RBC<br />
n Transfused Hemoarthrosis VTE<br />
Hip/Knee revision 1 1 unit 0 0 0<br />
1 1 unit 0 0 0<br />
Major long bone<br />
fractures<br />
Bilateral total knee 26 No 0 0 0<br />
replacement<br />
Single knee<br />
replacement in an<br />
anemic patient Hgb<br />
< 125 g/L<br />
3 No 0 0 0<br />
Readmit/<br />
ER visits<br />
Conclusion: Use <strong>of</strong> tranexamic acid for the <strong>of</strong>f-label indication to decrease<br />
need for blood transfusions in orthopedic surgery has been within the<br />
NYGH approved indications with no adverse events (hemoarthosis or VTE)<br />
complicating hospital stay, discharge or follow-up.<br />
Extending <strong>Hospital</strong>-Based Medication Incident Reporting to<br />
Enhance Medication Safety and Continuous Quality<br />
Assurance in Pharmacy Practice<br />
Certina Ho 1,2 , Roger Cheng 1 , Calvin Poon 1,2 , Patricia Hung 1,2 , Gary Lee 1 , Joe<br />
O’Leary 1 , Kristian Duwyn 1 , Medina Kadija 1 , Carol Lee 1 , Sanaz Riahi 1,2<br />
1 Institute for Safe Medication Practices Canada, Toronto, ON<br />
2 School <strong>of</strong> Pharmacy, University <strong>of</strong> Waterloo, Waterloo, ON<br />
Background: Medication safety / risk management is a relatively foreign<br />
terminology in community pharmacy practice when compared to other<br />
health care settings in Canada. This stems from the lack <strong>of</strong> a medication<br />
incident reporting tool tailored for community pharmacies, thereby<br />
discouraging community pharmacies from learning past mistakes.<br />
Objective: Based on learning and experience acquired from hospital-based<br />
incident reporting, the ISMP Canada Community Pharmacy Incident<br />
Reporting (CPhIR) program was created specifically for community /<br />
ambulatory pharmacies.<br />
Methods: After multiple iterations <strong>of</strong> feedback, pilot-testing, and<br />
consultation with community pharmacy practitioners, CPhIR is now<br />
available to community / ambulatory pharmacies. Reported incidents are<br />
analyzed anonymously using a qualitative aggregate analysis approach with<br />
key findings disseminated back to frontline users by ISMP Canada.<br />
Results: As <strong>of</strong> August 2011, there are over 300 registered CPhIR users. An<br />
accumulative total <strong>of</strong> 17,000 incidents have been anonymously reported.<br />
CPhIR provides users with a secure online interface to document medication<br />
incidents, export data for analysis, and view comparisons <strong>of</strong> individual<br />
pharmacy and aggregate data.<br />
Conclusions: The innovative CPhIR program provides the necessary tools to<br />
empower community pharmacies to enhance safe medication practices.<br />
Through anonymous reporting, community pharmacies can analyze<br />
medication incidents, identify root causes, and consequently implement<br />
system-based strategies for continuous quality assurance.<br />
Key Words: Community Pharmacy, Ambulatory Pharmacy, Incident<br />
Reporting, Medication Incidents, Near Miss, Continuous Quality Assurance<br />
2 CSHP<br />
Targeting Excellence<br />
Implementation and Evaluation <strong>of</strong> a Medication<br />
Reconciliation Tool on Internal <strong>Hospital</strong> Transfer<br />
in Pharmacy Practice<br />
Natalie LeBlanc, Timothy MacLaggan, Leslie Manuel, Julie<br />
Levesque, Rochelle Johnston, Julie Weir, Horizon Health Network, Zone 1,<br />
Moncton, NB<br />
Background: Patients are susceptible to medication errors at the point <strong>of</strong><br />
transfer, particularly in transfer from an intensive care unit to a general<br />
ward. Data to assess the optimal strategy in performing medication<br />
reconciliation at the time <strong>of</strong> transfer is currently limited.<br />
Objectives: To determine if implementation <strong>of</strong> a medication reconciliation<br />
tool comprised <strong>of</strong> a patient-specific computer generated physician order<br />
form would result in a decrease in the number, type and severity <strong>of</strong><br />
medication discrepancies that occur on internal hospital transfer.<br />
Methods: Two groups <strong>of</strong> patients transferred from the intensive care unit<br />
to the surgery step-down unit were compared. Current practices with<br />
regard to transfer orders were provided to the control group and a<br />
patient-specific medication reconciliation tool (completed by the<br />
transferring physician) was utilized for the intervention group. Medication<br />
discrepancies at the time <strong>of</strong> transfer were identified by two independent<br />
reviewers.<br />
Results: Fifty-two patients were included in the analysis. Mean number <strong>of</strong><br />
discrepancies per-patient were significantly decreased in the intervention<br />
group compared to the control group (0.96 ± 1.5 vs. 2.37 ± 1.8; p =<br />
0.003). There was a significant reduction in the number <strong>of</strong> policy violation<br />
discrepancies (0% vs. 45%; p
52<br />
Key Words: medication reconciliation, internal hospital transfer,<br />
medication discrepancy, intensive care unit, patient safety<br />
2 CSHP<br />
Targeting Excellence<br />
in Pharmacy Practice<br />
Improving Continuity <strong>of</strong> Care Post-<strong>Hospital</strong><br />
Discharge: A Needs Assessment <strong>of</strong> Community<br />
<strong>Pharmacists</strong><br />
Minh-Hien Le, Vincent Teo , Sunnybrook Health Sciences Centre, Toronto, ON<br />
Rationale: Increasing information exchange between community and<br />
hospital pharmacists has been shown to increase the number <strong>of</strong><br />
interventions by both. Sunnybrook Health Sciences Centre (SHSC) currently<br />
provides patients with a discharge summary (DS), generated by SHSC’s<br />
e-discharge program, which outlines details <strong>of</strong> their hospital admission.<br />
Such information may be useful to community pharmacists to ensure<br />
continuity <strong>of</strong> care.<br />
Description: To determine the importance <strong>of</strong> various hospital admission<br />
details to community pharmacists and to identify common barriers that are<br />
encountered when ensuring continuity <strong>of</strong> care.<br />
Steps: A feedback survey was developed from findings <strong>of</strong> previous studies<br />
and information currently provided in the DS. Surveys were distributed to<br />
over 600 community pharmacists working within a 10 km radius <strong>of</strong> SHSC.<br />
The survey asked pharmacists to rank the importance <strong>of</strong> patient hospital<br />
admission details using a five-point scale. It also asked a series <strong>of</strong><br />
open-ended questions relating to barriers in providing continuity <strong>of</strong> care,<br />
feedback on other discharge tools seen in practice, and other information<br />
that would be helpful in improving post-discharge care.<br />
Evaluation: Sixty pharmacists responded and 90% or more ranked the<br />
following as being “very important”: current medication list on discharge;<br />
list <strong>of</strong> discontinued medications; list <strong>of</strong> medications which have been<br />
adjusted. Details such as procedures performed while in hospital, results <strong>of</strong><br />
procedures and tests performed in hospital, list <strong>of</strong> complications occuring<br />
while in hospital and course in hospital were ranked from “neutral” to “not<br />
important” by the majority <strong>of</strong> pharmacists. Common barriers included<br />
prescription processing issues, lack <strong>of</strong> contact information and medication<br />
reconciliation issues. <strong>Pharmacists</strong> commented that lab results might be<br />
helpful to facilitate patient monitoring, particularly if the scope <strong>of</strong> practice<br />
<strong>of</strong> pharmacists was to expand.<br />
Relevance: Having identified the needs <strong>of</strong> community pharmacists, we can<br />
improve communication tools that will enhance the continuity <strong>of</strong> care for<br />
patients.<br />
2 CSHP<br />
Targeting Excellence<br />
Patient Recall <strong>of</strong> Interaction with a Pharmacist<br />
During <strong>Hospital</strong> Admission<br />
in Pharmacy Practice<br />
Douglas Doucette, Regional Pharmacy Services; Carole<br />
Goodine, Zone 3 Fredericton; Jodi Symes, Zone 2 Saint John; Erin Clarke,<br />
Zone 1 Moncton; Scott Simpson, Zone 7 Miramichi. All authors affiliated<br />
with Pharmacy Services, Horizon Health Network, NB<br />
Purpose: CSHP 2015 Objective 1.5 proposes that at least 50% <strong>of</strong> recently<br />
hospitalized patients or their caregivers will recall speaking with a<br />
pharmacist while in the hospital. Following a major reorganization <strong>of</strong> health<br />
authorities in New Brunswick, we sought to determine the baseline<br />
prevalence <strong>of</strong> patients who recall interacting with the pharmacist during<br />
their hospital admission, and their level <strong>of</strong> satisfaction with these<br />
encounters.<br />
Methods: Former inpatients from 27 units in 9 hospitals in Horizon Health<br />
Network were randomly selected to complete a telephone questionnaire<br />
within 5 to 7 months <strong>of</strong> discharge from hospital. Patient responses were<br />
validated against pharmacist documentation in the patient health record.<br />
Approval was granted by Horizon’s Research Ethics Board. Funding was<br />
provided by Medbuy Incorporated.<br />
Results: From August 2010 to July 2011, 1055 former inpatients were<br />
screened and 399 completed the telephone survey. Respondents were<br />
mainly female (56%) with mean age 67 years. During their recent<br />
admission 46% (n=184) <strong>of</strong> patients recalled speaking with a pharmacist.<br />
Eighty-nine percent responded they were “satisfied” or “very satisfied” in<br />
their interaction with the pharmacist. If the hospital <strong>of</strong>fered the opportunity<br />
to talk with a pharmacist who could help answer their questions about<br />
medications, 83% <strong>of</strong> respondents indicated they would want this service.<br />
For patients who recalled speaking with a pharmacist, a sample <strong>of</strong> 181<br />
patients was explored for evidence <strong>of</strong> pharmacist intervention or encounter<br />
with subject (medication history, consultation, etc.). Pharmacist<br />
documentation was found in health records <strong>of</strong> 65% <strong>of</strong> patients who<br />
recalled an interaction and in 88% <strong>of</strong> all patients.<br />
Conclusions: During a recent hospital admission, 46% <strong>of</strong> former inpatients<br />
recalled speaking with a pharmacist. The vast majority <strong>of</strong> patients were<br />
satisfied with this interaction and would welcome future services from<br />
hospital pharmacists.<br />
2 CSHP<br />
Targeting Excellence<br />
in Pharmacy Practice<br />
How Well Do Pharmacy Clinicians Perform in a<br />
Patient Simulation-Based Admission Medication<br />
Reconciliation Validation <strong>Program</strong>?<br />
Karen Cameron 1,2 , Natalia Persad 1,2 , Cindy Natsheh 1,2 , Kristie Small 1,2 , Sara<br />
Ingram 1,2 , Shiwani Chhibbar 1,3 , Olavo Fernandes 1,2<br />
1 University Health Network, Toronto, ON<br />
2 Leslie Dan Faculty <strong>of</strong> Pharmacy, University <strong>of</strong> Toronto, Toronto, ON<br />
3 University <strong>of</strong> Waterloo School <strong>of</strong> Pharmacy, Kitchener, ON<br />
Rationale: <strong>Hospital</strong>s are looking for effective strategies to implement<br />
medication reconciliation, train clinicians, and meet accreditation standards.<br />
The purpose <strong>of</strong> this study was to assess performance <strong>of</strong> pharmacy clinicians<br />
participating in a standardized formal medication reconciliation training<br />
program and compare the results among participant groups.<br />
Description: Pharmacy clinicians participated in an educational program<br />
designed to teach and evaluate key competencies linked to medication<br />
reconciliation. In the education phase, participants completed a pre-reading<br />
package and attended a group learning session that introduced medication<br />
reconciliation, best possible medication history (BPMH) taking, and<br />
identification and coding <strong>of</strong> discrepancies. In the validation phase,<br />
participants interviewed a standardized patient and were evaluated on: 1)<br />
time to complete BPMH; 2) BPMH process accuracy; 3) identification and<br />
coding <strong>of</strong> discrepancies. Data was grouped by participant type and<br />
analyzed.<br />
Evaluation: During a 5 year period, 135 pharmacy clinicians including<br />
pharmacists (n=87), pharmacy students (n=36) and pharmacy<br />
residents/interns (n=12) participated in the program. In the validation<br />
phase, the overall mean BPMH score was 88.9% [range 64.0-100.0%]. The<br />
mean BPMH scores for pharmacists, students and new graduates were<br />
88.4% [56.0-100.0%], 88.8% [64.0-100.0%] and 93.0% [88.0-100.0%]<br />
respectively. The overall mean BPMH completion time was 17 minutes<br />
[5-60] The average BPMH time (in minutes) by group was: pharmacists 20<br />
[5-60], students15 [10-30] and residents/interns 17 [12-23]. The overall<br />
discrepancy identification and coding accuracy scores were 94.4%<br />
[50.0-100.0%] and 99.5% [90.0-100.0%] respectively. The participants<br />
who used the BPMH interview guide (102/135) had a higher average score<br />
than those that did not (91.3% vs. 81.6%).<br />
Importance: A standardized medication reconciliation validation process<br />
enables consistent teaching and promotes competence in BPMH taking and<br />
medication reconciliation. This process can be widely applied to other<br />
institutions and clinician groups. Notably, the evaluation scores are high and<br />
similar across pharmacy clinician groups.<br />
2 CSHP<br />
Targeting Excellence<br />
in Pharmacy Practice<br />
Who’s Looking at the BPMH? Perception and<br />
Utilization <strong>of</strong> the Best Possible Medication History<br />
in a Tertiary Care <strong>Hospital</strong><br />
Sara Ingram 1,2 , Julia Streminsky 1,2 , Rosalyn Fleites 1,3 , Olavo Fernandes 1,2<br />
1 University Health Network, Toronto, ON<br />
2 Leslie Dan Faculty <strong>of</strong> Pharmacy, University <strong>of</strong> Toronto, Toronto, ON<br />
3 University <strong>of</strong> Waterloo School <strong>of</strong> Pharmacy, Waterloo, ON<br />
Rationale: The Best Possible Medication History (BPMH) is a comprehensive<br />
medication history completed by clinicians, using several sources <strong>of</strong>
53<br />
information. The BPMH is used in medication reconciliation, where a<br />
systematic comparison with current orders helps ensure safe, accurate<br />
medication information transfer. The study hospitals had admission<br />
medication reconciliation completed for >75% <strong>of</strong> inpatients, but it was<br />
unclear to what extent the BPMH was being used by healthcare providers.<br />
The primary objective <strong>of</strong> this study was to assess the utilization and<br />
integration into practice <strong>of</strong> the BPMH across healthcare pr<strong>of</strong>essionals<br />
providing direct patient care at a tertiary hospital in order to better direct<br />
education and quality improvement measures.<br />
Description: The study was conducted via a survey over a 10-week period.<br />
Specific groups targeted included: Medicine, Nursing, Pharmacy and Allied<br />
Health. Participants were contacted by email via hospital mailing lists, or<br />
were provided a paper copy <strong>of</strong> the survey by study coordinators.<br />
Evaluation: This study (N=330) revealed the majority <strong>of</strong> respondents used<br />
the BPMH (64%), <strong>of</strong> which 40% reported regular use (>10 times/week). An<br />
analysis <strong>of</strong> BPMH utilization by listed pr<strong>of</strong>ession revealed that 50% <strong>of</strong><br />
physicians, 63% <strong>of</strong> nurses, 70% <strong>of</strong> nursing leadership/nurse practitioners,<br />
71% <strong>of</strong> dieticians and 93% <strong>of</strong> pharmacists use the BPMH. Participants who<br />
did not use the BPMH (36%) cited being unaware <strong>of</strong> the resource as the<br />
most frequent reason for not using it. Further education on the BPMH,<br />
including its content and location is warranted to increase its clinical impact<br />
in patient care.<br />
Importance: Findings suggest that the majority <strong>of</strong> clinicians were familiar<br />
with the BPMH and actively used it as part <strong>of</strong> routine patient care. However,<br />
results also highlight that more education about the purpose and<br />
availability <strong>of</strong> the BPMH is still required, in order for all clinicians to<br />
integrate it more commonly into their practice.<br />
The Evaluation <strong>of</strong> a New Hierarchical Teaching Model for<br />
Pharmacy Students in Experiential Education<br />
Laura Tsang, Minh-Hien Le, Vincent Teo, Sunnybrook Health Sciences<br />
Centre, Toronto, ON<br />
Rationale: Pharmacy students undergoing experiential education are<br />
traditionally mentored by pharmacist preceptors. The changing curriculum<br />
at the University <strong>of</strong> Toronto (UT) and increased number <strong>of</strong> pharmacy<br />
students have created stress on this system and other teaching models<br />
should be explored.<br />
Description: To evaluate a new teaching model involving UT fourth-year<br />
pharmacy Structured Practical Experience <strong>Program</strong> (SPEP) students and<br />
residents mentoring junior pharmacy students under pharmacist<br />
supervision. The impact on learning, overall experience and pharmacist<br />
workload were examined.<br />
Steps: Surveys were distributed to 13 second year UT pharmacy students<br />
completing their Early <strong>Hospital</strong> Experience (EHE) rotation and their mentors.<br />
Seven EHE students were matched with SPEP students, two with residents<br />
and four with pharmacists concurrently preceptoring SPEP students.<br />
Evaluation: Of the nine EHE students with an SPEP/resident mentor, 89%<br />
found the experience worthwhile and 100% agreed this hierarchical<br />
teaching model should be repeated. All students agreed that a SPEP<br />
student/resident mentor enriched learning and those EHE students with<br />
pharmacist mentors wished they had this opportunity. For mentors, none<br />
“strongly agreed” to a significantly increased workload or impaired learning<br />
experience and described improved teaching skills and a worthwhile<br />
experience. <strong>Pharmacists</strong> agreed the program did not significantly increase<br />
workload, space constraints or disrupt SPEP learning and would coordinate<br />
this model again.<br />
Relevance: This new hierarchical teaching model was well received. EHE<br />
students preferred SPEP/resident mentors as they were more accessible,<br />
familiar with the curriculum and could advise on course selection and career<br />
options. Traditionally, preceptoring students requires a large time<br />
commitment and many pharmacists feel they cannot grant the increasing<br />
requests for rotations. However, this study shows the successful<br />
implementation and feasibility <strong>of</strong> a student structured teaching model with<br />
supervision by pharmacists with both clinical and dispensing responsibilities.<br />
Furthermore, this model helps to maximize the number <strong>of</strong> students exposed<br />
to hospital pharmacy practice.<br />
Evaluation <strong>of</strong> the Effectiveness <strong>of</strong> Online versus Face to Face<br />
Interactions in Interpr<strong>of</strong>essional Education<br />
Vincent Ho, Joan Lee, Justin Lee. Hamilton Health Sciences, Hamilton, ON<br />
Rationale for Report: The focus <strong>of</strong> interpr<strong>of</strong>essional education (IPE) is the<br />
development <strong>of</strong> skills to facilitate collaboration but achieving this goal can<br />
be difficult due to logistical challenges. Utilizing online services may provide<br />
an effective and familiar way for students to interact.<br />
Description <strong>of</strong> Concept: Undergraduate students from nursing,<br />
occupational therapy, pharmacy, physiotherapy and social work completed<br />
2 clinical scenarios, one as an online interaction utilizing Google Docs,<br />
Gmail and Skype, then was compared to a face to face (F2F) interaction.<br />
Development and Implement <strong>of</strong> Project: Seven students were recruited<br />
and took part in the study. Two observers assessed the students on the<br />
number <strong>of</strong> pre-defined learning objectives achieved and the demonstration<br />
<strong>of</strong> interpr<strong>of</strong>essional competencies in each interaction. Participants’<br />
experiences and attitudes toward IPE were assessed using pre- and<br />
post-interaction surveys and the Readiness for Interpr<strong>of</strong>essional Learning<br />
Survey (RIPLS).<br />
Evaluation <strong>of</strong> Project: The online and F2F interactions achieved 71% and<br />
86% <strong>of</strong> the learning objectives respectively. The F2F interaction resulted in a<br />
higher team score in the demonstration <strong>of</strong> interpr<strong>of</strong>essional competencies<br />
and 57% <strong>of</strong> students also received higher individual scores. The F2F<br />
interaction was preferred overall by 71% <strong>of</strong> students and both observers.<br />
The F2F interaction was preferred by 71% <strong>of</strong> students in terms <strong>of</strong> logistics<br />
and 100% <strong>of</strong> students in terms <strong>of</strong> IPE experience and learning experience.<br />
RIPLS scores improved after completing the interactions. Participants<br />
highlighted components <strong>of</strong> each interaction that could be combined to<br />
improve future interactions.<br />
Concept’s Importance and Usefulness to Current and or Future<br />
Practice: The online interaction may not be as effective as the F2F<br />
interaction in IPE. Students felt that the online interaction was less effective<br />
for discussion but may help address some logistical challenges. Educators<br />
should implement a combination <strong>of</strong> components highlighted by<br />
participants to help improve the online collaborative experience.<br />
An Online e-Learning Patient Education Tool for Solid Organ<br />
Transplant Recipients<br />
Jennifer Harrison 1,2 , Julia Cervenko 1 , Penny Demas-Clarke 1 , Bassem<br />
Hamandi 1,2 , Dipika Munyal 1 , June Wang 1 , Teresa Yi 1<br />
1 Department <strong>of</strong> Pharmacy, Toronto General <strong>Hospital</strong>, University Health<br />
Network, Toronto, ON<br />
2 Leslie Dan Faculty <strong>of</strong> Pharmacy, University <strong>of</strong> Toronto, Toronto, ON<br />
Background: Medication regimens for solid organ transplant recipients<br />
(SOTR) are complex and non-adherence can lead to rejection and graft loss.<br />
Educational tools are needed to reinforce patient knowledge <strong>of</strong> transplant<br />
medications.<br />
Objective: To develop a tool to support ongoing medication education<br />
needs <strong>of</strong> SOTR.<br />
Methods: <strong>Program</strong> content was developed by pharmacists and reviewed by<br />
an interpr<strong>of</strong>essional clinician group. Micros<strong>of</strong>t Power Point®, Adobe®<br />
Captivate® and Dreamweaver® were used to create an e-learning<br />
internet-based format. A Virtual Patient Focus Group (VPFG) assessed<br />
usability and utility <strong>of</strong> the tool.<br />
Results: The Transplant Medication Information Teaching Tool (TMITTã,<br />
www.TMITT.ca) launched in September 2010. Content is structured as<br />
medication courses and lessons, and includes interactive quizzes and<br />
medication summaries. ‘Learning Prescriptions’ direct patients to<br />
appropriate content to meet their learning objectives. The majority <strong>of</strong> VPFG<br />
members (n=27) agreed or strongly agreed that the program was an<br />
effective way to learn, language and difficulty level were appropriate, and<br />
that they had the necessary computer skills to use the tool.
54<br />
Conclusions: While further study is needed, use <strong>of</strong> an internet-based<br />
e-learning program to control content, sequence, pace and timing <strong>of</strong><br />
education to achieve personal learning objectives appears to be an<br />
attractive and effective teaching modality in SOTR.<br />
Keywords: patient education, e-learning, internet, solid organ<br />
transplantation<br />
Diabetes Education in Pharmacy Residencies Across Canada<br />
Henry Halapy, St. Michael’s <strong>Hospital</strong>, Toronto, ON, Gary Wong, University<br />
Health Network, Toronto, ON<br />
Rationale: Diabetes is a growing chronic health problem in Canada,<br />
requiring complex management. As a result teaching, pharmacy students<br />
about diabetes has become increasingly important. However, little is known<br />
about the amount and type <strong>of</strong> education regarding diabetes given to<br />
post-graduate pharmacy residents in Canada.<br />
Objective: To evaluate the extent and type <strong>of</strong> training currently conducted<br />
around diabetes management in <strong>Canadian</strong> pharmacy residencies.<br />
Study design and methods: A web-based survey tool asking about<br />
exposure to diabetes topics (such as diabetes medication pharmacology,<br />
insulin dosing) in pharmacy residency training was distributed to pharmacy<br />
residency coordinators/ directors and residents across Canada via email.<br />
Most answers were recorded using a 5 point Likhert scale (no exposure, a<br />
little, some, a lot, resident becomes pr<strong>of</strong>icient). The survey was reviewed for<br />
face and content validity prior to distribution. Congestive heart failure, a<br />
frequently occurring chronic health problem in Canada, was used as a<br />
comparator therapeutic topic.<br />
Results: A total <strong>of</strong> 41 responses were received (19 coordinators, 5<br />
directors, 17 residents). Diabetes rotations were uncommon in <strong>Canadian</strong><br />
pharmacy residencies (2.4% <strong>of</strong> responses), while cardiology rotations were<br />
common (81% <strong>of</strong> responses). Residents were exposed predominantly to no<br />
(4/15 topics, e.g., carbohydrate counting), a little (5/15 topics, e.g., blood<br />
glucose meters), or some (6/15 topics, e.g., sliding scales) with regard to<br />
diabetes topics while residents were exposed predominantly to some (8/15<br />
topics, e.g., amiodarone use) or a lot (4/15 topics, e.g., blood pressure<br />
monitoring) to heart failure topics. Between 4-9% <strong>of</strong> residents became<br />
pr<strong>of</strong>icient in some heart failure topics (warfarin counseling) while very few<br />
residents became pr<strong>of</strong>icient in diabetes topics.<br />
Conclusions: This survey would suggest that pharmacy residents are<br />
exposed to diabetes topics relatively less than congestive heart failure.<br />
Greater exposure to diabetes topics may be beneficial in pharmacy<br />
residency training.<br />
Evaluating the Role <strong>of</strong> Pharmacist Teachers in <strong>Canadian</strong><br />
Family Medicine Residency <strong>Program</strong>s: A Qualitative Analysis<br />
Derek Jorgenson 1 , Andries Muller 1 , Anne Marie Whelan 2<br />
1 University <strong>of</strong> Saskatchewan<br />
2 Dalhousie University<br />
Background: A 2009 survey found >25% <strong>of</strong> <strong>Canadian</strong> family medicine<br />
residency programs have a pharmacist teaching residents; however, little is<br />
known about the impact <strong>of</strong> these pharmacists.<br />
Objective: Evaluate the role <strong>of</strong> pharmacist teachers within <strong>Canadian</strong> family<br />
medicine residency programs.<br />
Methods: One-on-one interviews with residents, physicians and<br />
pharmacists from the 40 <strong>Canadian</strong> family medicine residency programs that<br />
employ a pharmacist teacher. Interviews continued until data saturation<br />
was observed. Transcripts were analyzed using grounded theory analysis<br />
(inductive and deductive) to identify themes. Codes were entered into<br />
NVivo s<strong>of</strong>tware. Themes were sent to participants to confirm validity.<br />
Results: 11 residents, 6 physicians and 17 pharmacists participated. Four<br />
themes emerged from deductive analyses regarding the impact <strong>of</strong><br />
pharmacists on residents: (1) Improved drug knowledge (2) Improved<br />
confidence (3) Improved patient care (4) Appreciation for pharmacist<br />
expertise. Five additional themes emerged from inductive analyses: (1)<br />
Desire to expand pharmacist teaching (2) Impact on collaboration (3) Impact<br />
on faculty (4) Lack <strong>of</strong> criticism <strong>of</strong> the role (5) No formal curriculum utilized.<br />
Conclusions: The role <strong>of</strong> pharmacist teachers is valued in <strong>Canadian</strong> family<br />
medicine residency programs and consideration could be made to expand<br />
the role. Developing a formal curriculum is recommended.<br />
Key words: family medicine residency, pharmacist teacher, qualitative<br />
A Survey <strong>of</strong> Institutional <strong>Pharmacists</strong>’ Involvement In and<br />
Attitudes Towards Research<br />
Joseph E. Blais 1 , Sheila L. Walter 1 , Dean T. Eurich 2 , Ross T. Tsuyuki 3 , Sheri L.<br />
Koshman 3<br />
1 Pharmacy Services, Alberta Health Services, Edmonton, AB<br />
2 School <strong>of</strong> Public Health, University <strong>of</strong> Alberta, Edmonton, AB<br />
3 Division <strong>of</strong> Cardiology, University <strong>of</strong> Alberta, Edmonton, AB<br />
Background: Research is critical for the future <strong>of</strong> pharmacy yet institutional<br />
pharmacists’ current research activities and perceptions towards research<br />
are largely unknown.<br />
Objectives: To describe institutional pharmacists’ involvement in research<br />
activities and to assess the attitudes <strong>of</strong> pharmacists towards research.<br />
Methods: We conducted a cross-sectional survey <strong>of</strong> all institutional<br />
pharmacists within Alberta Health Services, Alberta, Canada, in March<br />
2011. The survey explored involvement in research, current research<br />
activities, and attitudes towards research.<br />
Results: Overall response rate was 45% (286/636). Respondents were<br />
predominantly female (80%), practiced in urban institutions (76%) and<br />
reported a primary clinical role (61%). Over half <strong>of</strong> pharmacists indicated<br />
having involvement in research (168/286 [60%]) with 43% <strong>of</strong> pharmacists<br />
(119/280) currently participating in research activities but only 26%<br />
(72/280) leading research projects. <strong>Pharmacists</strong> tended to agree (94%) that<br />
research was important to the pr<strong>of</strong>ession <strong>of</strong> pharmacy. Almost all<br />
respondents (99%) felt that pharmacists should be involved in research, but<br />
indicated additional time and training were barriers to their personal<br />
involvement.<br />
Conclusion: While the majority <strong>of</strong> institutional pharmacists in Alberta have<br />
had involvement in research projects, few were involved in leading research.<br />
There is strong support from pharmacists to be involved in research.<br />
Key Words: research, institutional pharmacist, attitudes, involvement,<br />
activities<br />
Interactions between Antiretroviral Agents and<br />
Chemotherapy Regimens for the Treatment <strong>of</strong> Lymphoma: A<br />
Quick Reference Guide<br />
Alison YJ Wong 1,2,3 , Alice Tseng 1,2 , Jack Seki 1,2 , Pam Ng 1 , Vishal Kukreti 1<br />
1 University Health Network, Toronto, ON<br />
2 University <strong>of</strong> Toronto, Toronto, ON<br />
3 McGill University Health Centre, Montréal, QC<br />
Background: Despite the success <strong>of</strong> antiretroviral therapy, HIV-infected<br />
individuals remain at higher risk <strong>of</strong> developing malignancies. Clinically<br />
important interactions between cART and chemotherapy agents have been<br />
described in the literature, but practical, comprehensive guidelines for<br />
clinical practice do not exist.<br />
Objective: To provide a comprehensive summary <strong>of</strong> documented and<br />
potential interactions between antiretroviral agents (ARVs), common<br />
chemotherapy regimens used in the treatment <strong>of</strong> lymphoma, and<br />
supportive therapy.<br />
Methods: A literature review was conducted through Ovid Medline 1948 –<br />
March 2011 using MeSH terms for individual antineoplastics, keywords for<br />
chemotherapy regimens, and available and emerging ARVs. Pertinent<br />
conference abstracts were identified through the International AIDS <strong>Society</strong>
55<br />
USA abstract search engine. Quality <strong>of</strong> evidence was evaluated according to<br />
an adapted GRADE system.<br />
Results: Thirteen documents were developed, summarizing potential<br />
interactions between ARVs and the following chemotherapy regimens:<br />
ABVD, BEACOPP, CHOP, CNS LYMPHOMA, CODOX-M, CVP, DHAP, ESHAP,<br />
GDP, ICE, IVAC, MINIBEAM, and supportive therapy. A summary <strong>of</strong> current<br />
principles <strong>of</strong> HIV treatment was also developed for non-HIV specialists.<br />
Conclusion: This guide provides clinicians with a user-friendly tool which<br />
allows quick identification <strong>of</strong> possible ARV-chemotherapy interactions;<br />
clinical implications and practical management guidelines are included to<br />
facilitate optimal treatment <strong>of</strong> both disease states with minimal toxicity.<br />
Key words: HIV infection, lymphoma, antiretrovirals, chemotherapy,<br />
interactions<br />
Impact <strong>of</strong> a Drug Access Facilitator in an Outpatient<br />
Chemotherapy Clinic<br />
Mei Shi, Daniela Gallo-Hershberg, Nicole Harvey, North York General<br />
<strong>Hospital</strong>, Toronto, ON<br />
Rationale: Obtaining reimbursement and access for treatment and<br />
supportive therapies for outpatient chemotherapy clinics has been<br />
fragmented where multiple stakeholders, including patients, are involved in<br />
the process. The role <strong>of</strong> a drug access facilitator (DAF) was investigated to<br />
reduce wait time to treatments, clinician administrative workload, and<br />
clinician and patient frustration.<br />
Description and Steps Taken: Through interviewing key stakeholders, a<br />
needs assessment <strong>of</strong> the existing reimbursement process was conducted.<br />
This resulted in the development <strong>of</strong> a new streamlined workflow as well as<br />
drug specific access protocols, and led to the creation <strong>of</strong> the centralized<br />
DAF role. Because the DAF would require extensive knowledge in<br />
medications and experience in dealing with third-party payers, a pharmacy<br />
technician was selected to fulfill this role. A pharmacist was available for<br />
consultation for clinically challenging cases.<br />
Evaluation: Over a 6-month period, the DAF managed a total <strong>of</strong> 140<br />
reimbursement cases. The average time to approval for Exceptional Access<br />
<strong>Program</strong> applications was decreased from 35 days to less than 10 days with<br />
the DAF intervention. A similar pattern was observed with applications for<br />
the Special Access <strong>Program</strong> and Trillium <strong>Program</strong>. Also, centralization <strong>of</strong> the<br />
drug access workflow to a single individual reduced administrative<br />
workload for members <strong>of</strong> the interpr<strong>of</strong>essional team. A follow-up written<br />
survey <strong>of</strong> clinic staff and patients reported high levels <strong>of</strong> satisfaction with<br />
the DAF with average scores <strong>of</strong> 90.8% and 88.3%, respectively.<br />
Importance: The DAF has demonstrated a positive impact for the<br />
chemotherapy clinic. This role can be applied to various medical specialities<br />
outside <strong>of</strong> oncology for any medication with outpatient reimbursement and<br />
access barriers. This concept also aligns with the future <strong>of</strong> pharmacy<br />
practice as it empowers pharmacy technicians to expand their scope <strong>of</strong><br />
practice to promote seamless care.<br />
2 CSHP<br />
Targeting Excellence<br />
in Pharmacy Practice<br />
High Dose Methotrexate in Adult Oncology<br />
Patients: A Case-Control Study Assessing the Risk<br />
Association Between Drug Interactions and<br />
Methotrexate Toxicity<br />
April Chan, Irina Rajakumar, London Health Sciences Centre, London, ON<br />
Background: High-dose methotrexate, defined as dose ≥ 1g/m2, is<br />
commonly used in chemotherapy protocols. Certain drugs such as acyclovir,<br />
allopurinol, proton pump inhibitors (PPIs) and some antibiotics have been<br />
associated with delayed renal clearance <strong>of</strong> methotrexate and may<br />
predispose patients to toxicities. Currently, no specific recommendations<br />
exist on adjusting high-dose methotrexate regimen in the presence <strong>of</strong><br />
potential interacting drugs. This study aims to determine whether presence<br />
<strong>of</strong> interacting drugs is associated with delayed methotrexate clearance.<br />
Methods: This was a case-control study <strong>of</strong> adult oncology patients who<br />
received their first cycle <strong>of</strong> high-dose methotrexate. Cases were defined as<br />
patients who experienced delayed methotrexate clearance, as indicated by<br />
serum methotrexate level ≥ 0.1 umol/L at 72 hours. The primary endpoint<br />
was the frequency <strong>of</strong> interacting drugs between cases and controls. These<br />
were compared using Fisher’s exact test. Where possible, adjustment for<br />
significant baseline differences was made using logistic regression. The<br />
secondary endpoint was frequency <strong>of</strong> methotrexate-related clinical toxicities<br />
between groups and included myelosuppression, nephrotoxicity,<br />
hepatotoxicity and mucositis.<br />
Results: From January 2004 to March 2011, 73 patients met study criteria,<br />
<strong>of</strong> which 23 were defined as cases. Significant baseline differences were<br />
high-dose methotrexate dose received and renal impairment. The presence<br />
<strong>of</strong> interacting drugs was not associated with delayed methotrexate<br />
clearance (OR 0.91, 95% CI 0.24-3.38, p>0.999). After adjusting for<br />
high-dose methotrexate dose, drugs observed with the most frequency<br />
(allopurinol, PPIs and sulfamethoxazole/ trimethoprim) were not associated<br />
with delayed methotrexate clearance (p-values <strong>of</strong> 0.948, 0.592 and 0.204<br />
respectively). Cases experienced more severe anemia (grade 2.52 versus<br />
1.68, p=0.007) and higher rates <strong>of</strong> mucositis (65.2% versus 20.0%,<br />
p
56<br />
Background: Capecitabine is an oral pro-drug <strong>of</strong> the cytotoxic agent<br />
5-fluorouracil used in the treatment <strong>of</strong> several types <strong>of</strong> cancer. As more oral<br />
chemotherapy agents come to market, there is interest in how pharmacists<br />
in oncology can adapt their practices to best provide patient care.<br />
Objective: To establish and evaluate the impact <strong>of</strong> a pharmacist-led toxicity<br />
management program for patients being treated with capecitabine.<br />
Methods: Implementation and prospective evaluation <strong>of</strong> the program was<br />
conducted using a matched historical cohort. <strong>Pharmacists</strong> performed<br />
weekly toxicity assessments. Interventions were made using developed<br />
algorithms and evidence-informed guidelines. Patient quality <strong>of</strong> life and<br />
satisfaction with the program were also evaluated.<br />
Results: Seventeen patients were enrolled with 17 retrospective matches<br />
subsequently identified. There was a trend towards a decreased<br />
requirement for dose modifications and a significant decrease in the<br />
number <strong>of</strong> days <strong>of</strong> treatment delay in the intervention group (94 vs. 14<br />
days, p=0.03). The mean number <strong>of</strong> toxicities identified per patient was 5.3<br />
in the prospective group compared to 1.6 in the retrospective group<br />
(p15hrs over three<br />
weeks.<br />
Conclusion: While average weekly time spent on the ADAPT program was<br />
consistent with outlined requirements, participants struggled with technical<br />
aspects <strong>of</strong> online learning, as well as, committing time learning and<br />
practicing skills. Feedback will assist revisions to program marketing,<br />
‘readiness to participate’ self-assessment and learner orientation.<br />
Moving Practice Forward with Early Exposure Students<br />
Thomas ER Brown 1,2 , Farida Meghji 1 , Jane Mosley 1 , Lisa McCarthy 1,2<br />
1 Women’s College <strong>Hospital</strong>, Toronto, ON<br />
2 Leslie Dan Faculty <strong>of</strong> Pharmacy, University <strong>of</strong> Toronto, Toronto, ON<br />
Acknowledgements: Michaela Hogan, Adam Lam, Mitsumi Louis-Foster,<br />
Lauren Sule<br />
Rationale: Early practice experience rotations help students apply and build<br />
confidence with skills they are learning in the classroom while enhancing<br />
their appreciation for the aims <strong>of</strong> their education. Preceptors may feel<br />
challenged to identify project activities for these students given the limited<br />
amount <strong>of</strong> formal therapeutics education they have received.<br />
Description: Our aim was to demonstrate that early learners can make<br />
vital contributions to pharmacy department initiatives. Second-year<br />
undergraduate pharmacy students were assigned projects around optimal<br />
medication use and safety during 4-week rotations. Topics were<br />
strategically selected to lay the foundation for important safety initiatives at<br />
our institution, including: an audit <strong>of</strong> medication sampling practices; review<br />
<strong>of</strong> institutional practices around dangerous abbreviations; an audit <strong>of</strong><br />
non-formulary medication requests; and a review <strong>of</strong> medication<br />
reconciliation initiatives in ambulatory care settings.<br />
Evaluation: Four students participated in the program between May and<br />
August 2011. The audit <strong>of</strong> medication sampling found that 80% <strong>of</strong><br />
samples in the audited areas were expired and has led to creation <strong>of</strong> a safer<br />
medication sampling pilot program in partnership with the Department <strong>of</strong><br />
Psychiatry. Dangerous abbreviations have been removed from all<br />
pre-printed order sets and an online learning module has been created for<br />
staff. An assessment <strong>of</strong> non-formulary items in floor stock found that 20%<br />
<strong>of</strong> products in the hospital are non-formulary and raised questions about<br />
the concept <strong>of</strong> a formulary in an ambulatory institution. Lastly, the<br />
medication reconciliation review led to striking <strong>of</strong> a working group to<br />
develop a strategy for identifying patient populations to target in<br />
ambulatory care thereby satisfying a test <strong>of</strong> compliance for a required<br />
organizational practice for Accreditation Canada.<br />
Importance: This program demonstrates that learners early in their<br />
pharmacy careers can lay the groundwork for pharmacy initiatives around<br />
optimal medication use and safety.<br />
2 CSHP<br />
Targeting Excellence<br />
in Pharmacy Practice<br />
Provincial Implementation <strong>of</strong> Accreditation Canada<br />
Required Organizational Practices: The Alberta<br />
Experience<br />
Dawn McDonald 1 , Gwen Erdmann 2 , Kefah Hayek 2 , Nancy Louis 1 , Jim<br />
Manley 1 , Shaheen Nenshi Nathoo 1 , Laurine Sanderson 2 , Medication Quality<br />
and Safety Team, Pharmacy Services, Alberta Health Services
57<br />
1 Alberta Children’s <strong>Hospital</strong>, Calgary, AB<br />
2 Seventh Street Plaza, Edmonton, AB<br />
Rationale: Alberta Health Services (AHS) was created in 2008 through the<br />
amalgamation <strong>of</strong> nine former health regions and oversees 107 hospitals.<br />
The first AHS Accreditation Canada (AC) on-site survey was conducted in<br />
October 2010. Within the AC Managing Medications standards, seven<br />
Required Organizational Practices (ROPs) were identified as essential<br />
practices to be implemented. Four <strong>of</strong> these ROPs were within the purview<br />
<strong>of</strong> AHS Provincial Pharmacy Services: concentrated electrolytes, heparin<br />
safety, narcotics safety, and standardized concentrations. The challenge for<br />
the Provincial Pharmacy Services Medication Quality and Safety Team<br />
(MQST) was how to assess the current level <strong>of</strong> compliance at each site and<br />
fully implement the 4 ROPs across the province.<br />
Description: Online assessments were created and used to quantify<br />
compliance with each ROP. The results <strong>of</strong> the assessments were used to<br />
develop a provincial implementation plan for each <strong>of</strong> the ROPs.<br />
Steps Taken: The first online assessment, ROP Compliance Assessment –<br />
Current State, was completed in January 2011 by all 107 AHS acute care<br />
sites. This provided a provincial baseline. Alternatives were suggested to<br />
assist with product removal where required. When product removal was<br />
not possible, rationale was requested. A repeat assessment, Verification <strong>of</strong><br />
Compliance, was completed in February 2011 to assess each site’s progress<br />
in the actual implementation <strong>of</strong> the ROPs.<br />
Evaluation: As <strong>of</strong> April 2011, the 4 ROPs within the Managing Medication<br />
standard were fully implemented throughout all 107 AHS sites. In<br />
September 2011, two pharmacy policies (High Potency Narcotics and<br />
Concentrated Electrolytes) were implemented provincially. A<br />
post-implementation audit will be conducted to evaluate safety<br />
mechanisms and processes in place, and determine the effectiveness <strong>of</strong> the<br />
Policies and Procedures.<br />
Importance: Similar efforts to address AC ROP requirements provincially<br />
across 107 sites are unprecedented in Canada. Local engagement with<br />
provincial oversight was key to the success <strong>of</strong> this work.<br />
Drugs Obtained by Quebec University Health Centers<br />
through Health Canada’s Special Access <strong>Program</strong>me –<br />
Descriptive Analysis by the programme de gestion<br />
thérapeutique des Medicaments<br />
Élaine Pelletier 1 , Benoît Cossette 2 , Céline Dupont 3 , Nathalie Marcotte 4 ,<br />
Marie-Claude Michel 4 , France Varin 5 , Louise Deschênes 4 , Paul Farand 2 ,<br />
Daniel Froment 5 , Pierre Gaudreault 1 , Raghu Rajan 3<br />
1 Centre hospitalier universitaire Sainte-Justine (CHU Sainte-Justine), Québec<br />
2 Centre hospitalier universitaire de Sherbrooke (CHUS), Québec<br />
3 Centre hospitalier universitaire de Santé McGill (CUSM), Québec<br />
4 Centre hospitalier universitaire de Québec (CHUQ), Québec<br />
5 Centre hospitalier universitaire de Montréal (CHUM), Québec, 1 à 5 :<br />
<strong>Program</strong>me de gestion thérapeutique des médicaments (PGTM), Québec<br />
Rationale: University health centres (CHU) in the Province <strong>of</strong> Quebec<br />
commonly have to use medications authorized by Health Canada’s Special<br />
Access <strong>Program</strong>me (“SAP-drugs”). Indeed many <strong>of</strong> their patients have<br />
diseases that are rare, complex or refractory to conventional drugs available<br />
on the <strong>Canadian</strong> market. In January 2008, Health Canada issued a new<br />
version <strong>of</strong> its guidance document defining principles and practices<br />
pertaining to SAP-drugs.<br />
Objectives: To describe the overall utilization pr<strong>of</strong>ile <strong>of</strong> SAP-drugs and the<br />
CHU’s compliance with the administrative and therapeutic management<br />
guidelines proposed by Health Canada.<br />
Design and methods: Retrospective identification <strong>of</strong> SAP-drugs used<br />
between 1 April 2008 and 31 March 2009. Sampling procedure allowing to<br />
describe the main usage characteristics, including prescription frequency<br />
and costs, and measure compliance with five criteria for management and<br />
monitoring <strong>of</strong> use <strong>of</strong> SAP-drugs.<br />
Results: The utilization pr<strong>of</strong>ile brings to light the diversity, distribution, and<br />
impact <strong>of</strong> SAP-drugs use. For the reference one-year period, approximately<br />
12,000 prescriptions were written, corresponding to more than 140<br />
nonproprietary names. This represents 10.4 M CAN$ or 7.5% <strong>of</strong> the CHU’s<br />
overall annual budget. Compliance with the criteria was very variable.<br />
Interesting qualitative observations and gaps have been identified at several<br />
stages <strong>of</strong> the drug distribution circuit.<br />
Conclusion: Quebec’s university health centres must improve their<br />
management <strong>of</strong> SAP-drugs, namely documentation and archiving, clinical<br />
monitoring, and funding.<br />
Safety and Efficacy <strong>of</strong> Chop or R-chop for Treatment <strong>of</strong><br />
Diffuse Large b-cell Lymphoma with Protease Inhibitor or<br />
Non-Protease Inhibitor Based Antiretroviral Regimens in<br />
HIV-Infected Patients: SCULPT Study<br />
Alison Y.J. Wong 1,2,3 , Suzanne Marcotte 4 , Mathieu Laroche 4 , Nancy L.<br />
Sheehan 3 , Vishal Kukreti 1 , Jean-Pierre Routy 3 , Bernard Lemieux 4 , Jack Seki 1 ,<br />
Danielle Rouleau 4,5 , Alice Tseng 1,2<br />
1 University Health Network, Toronto, ON<br />
2 University <strong>of</strong> Toronto, Toronto, ON<br />
3 McGill University Health Centre, Montréal, QC<br />
4 Centre hospitalier de l’Université de Montréal, Montréal, QC<br />
5 Université de Montréal, Montréal, QC<br />
Rationale: Use <strong>of</strong> combination antiretroviral therapy (cART) and<br />
cyclophosphamide, doxorubicin, vincristine, prednisone with or without<br />
rituximab (CHOP+/-R) for treatment <strong>of</strong> diffuse large B-cell lymphoma<br />
(DLBCL) substantially increases response rates but may also increase toxicity,<br />
possibly due to antiretroviral-antineoplastic drug interactions.<br />
Objectives: We evaluated the frequency <strong>of</strong> confirmed or unconfirmed<br />
complete remission (CR/CRu) <strong>of</strong> DLBCL in HIV-positive patients treated with<br />
CHOP+/-R while receiving protease inhibitor (PI) versus non-PI based cART.<br />
Design and Methods: A retrospective multi-centered observational pilot<br />
study was conducted in patients on cART, treated for DLBCL with CHOP+/-R<br />
between 2002-2010. Percentage <strong>of</strong> CR/CRu, 2-year overall survival (OS)<br />
and frequency <strong>of</strong> severe adverse events were evaluated. Possible predictors<br />
<strong>of</strong> CR/CRu between groups were evaluated by univariate logistic<br />
regressions.<br />
Results: Thirty-four patients were included, 65% and 35% <strong>of</strong> patients<br />
received a PI and non-PI based cART, respectively. Baseline characteristics<br />
were similar between both groups; 85% <strong>of</strong> patients were male, median age<br />
43 years, 50% with International Prognostic Index (IPI) score 2-3, median 7<br />
years since HIV diagnosis and CD4+ <strong>of</strong> 225 cells/mm3. CR/CRu was<br />
achieved in 77% and 58% <strong>of</strong> patients in the PI and non-PI group,<br />
respectively (p=0.21), with 65% and 63% <strong>of</strong> patients achieving 2-year<br />
overall survival (p=1.00). Univariate analyses showed that a lower IPI score<br />
and a higher total number <strong>of</strong> received chemotherapy cycles were<br />
significantly associated with higher CR/CRu rates (p=0.02 and 0.03,<br />
respectively). Tolerability was similar between both groups except decreased<br />
frequency <strong>of</strong> anemia in the PI group (23% versus 37%, p=0.04).<br />
Conclusion: Similar efficacy and tolerability <strong>of</strong> CHOP+/-R was observed<br />
with PI based and non-PI based cART, though less anemia was observed in<br />
the PI group. Response rates appear to be higher in patients receiving a PI<br />
based cART but requires confirmation with larger studies.<br />
Drug Access Navigator Database: Improving the<br />
Management <strong>of</strong> Drug Access Cases through the<br />
Development and Implementation <strong>of</strong> a Computerized<br />
Database<br />
Allison Jocko, Janet Lui, The Scarborough <strong>Hospital</strong>, Toronto, ON<br />
Most oral chemotherapy and related support medications prescribed for<br />
oncology patients in Ontario are not routinely funded by the provincial drug<br />
programs. Navigating patient access is challenging and requires special<br />
request letters, private insurance investigations, or enrolment in assistance<br />
programs. Tracking case status and associated workload is equally difficult.<br />
As referrals and complexities increase, the need for a tool to facilitate
58<br />
processes was identified. Consequently, a Drug Access Navigator Database<br />
(DAND) was created using Micros<strong>of</strong>t Access s<strong>of</strong>tware to support the<br />
process <strong>of</strong> tracking cases and generating reports on workload and<br />
outcomes.<br />
The DAND links to forms, websites, costs, and contact information. Reports<br />
capture number <strong>of</strong> referrals, time spent, time for case resolution by drug,<br />
monthly or per cycle patient cost savings for new cases, approval expiry list,<br />
and pending case list. In the month <strong>of</strong> August 2011, there were 49<br />
referrals, and 33 hours spent with an estimated patient cost diverted <strong>of</strong><br />
$130,000.<br />
After implementing DAND, tracking and managing drug access cases was<br />
found to be simpler and faster. It was also found to be an easy tool for<br />
workload tracking and solidifying the need for the role <strong>of</strong> a drug access<br />
navigator for Oncology drugs in Ontario.<br />
Residents as Preceptors: Development, Implementation and<br />
Evaluation <strong>of</strong> a Pharmacy Summer Student Clinical<br />
Experience<br />
Natalie Crown, Sarah Burgess, April Chan, Jonathan Chiu, Janice Lee, Kelly<br />
MacLean, Anne Marie Bombassaro, London Health Sciences Centre,<br />
London, ON<br />
Rationale: <strong>Hospital</strong> pharmacy residency programs seek to ensure graduates<br />
exhibit competencies in patient care and teaching. Opportunities for<br />
residents to precept students may be limited in the current program<br />
structure. Conversely, undergraduate pharmacy students are frequently<br />
employed in technical roles with limited opportunities to participate in<br />
patient care.<br />
Description: A 1 week rotation was developed to provide residents with an<br />
opportunity to provide practice based teaching to pharmacy students in a<br />
patient care setting, and practice direct instruction, modeling and coaching<br />
skills. The rotation provided students the opportunity to practice curriculum<br />
based skills, enhance understanding <strong>of</strong> patient care roles for hospital<br />
pharmacists and the benefits <strong>of</strong> a residency.<br />
Steps: The rotation took place during the clinical practice rotation in the<br />
final month <strong>of</strong> the residency program. Students were matched to clinical<br />
rotations based on interest, complexity and academic year completed.<br />
Resident and student specific objectives were developed. Participants<br />
completed a daily self-reflection guide and submitted an end <strong>of</strong> rotation<br />
evaluation in a blinded format.<br />
Evaluation: Five residents and 5 students participated in rotations<br />
including critical care, cardiac care, general surgery, internal medicine and<br />
nephrology. All residents strongly agreed that the experience increased<br />
“readiness” to function as a preceptor in the future, with 4 <strong>of</strong> 5 strongly<br />
feeling that the experience provided the opportunity to develop teaching<br />
and precepting skills. All pharmacy students strongly agreed that the<br />
rotation enhanced understanding <strong>of</strong> clinical practice in a hospital setting<br />
and were influenced positively about a career in hospital pharmacy, with 4<br />
<strong>of</strong> 5 being motivated to pursue a post-graduate residency.<br />
Importance: There was unanimous agreement amongst participants that a<br />
clinical rotation conducted by pharmacy residents for undergraduate<br />
pharmacy students should be incorporated into the residency program. The<br />
opportunity was subjectively evaluated as benefiting both residents and<br />
students from teaching and learning perspectives, respectively.<br />
2 CSHP<br />
Targeting Excellence<br />
in Pharmacy Practice<br />
Imatinib Plasma Through Concentrations and the<br />
Ability to Assess Patient Adherence<br />
Narducci 1 , S.E. Walker 1,2 , C. DeAngelis 1,2<br />
1 Leslie Dan Faculty <strong>of</strong> Pharmacy, University <strong>of</strong> Toronto<br />
2 Sunnybrook Health Sciences Centre, Toronto, ON<br />
Rationale: Imatinib mesylate is an oral tyrosine kinase inhibitor used for the<br />
treatment <strong>of</strong> chronic myeloid leukemia (CML) and gastrointestinal stromal<br />
tumours (GIST). Therapeutic drug monitoring has been recommended due<br />
to recent studies demonstrating improved clinical outcomes.<br />
Objectives: To determine the proportion <strong>of</strong> patients with imatinib plasma<br />
trough concentrations (Cmin) below the therapeutic range and the<br />
probability that a sub-therapeutic Cmin level is due to patient<br />
non-adherence.<br />
Methods: A literature search was conducted to identify adult<br />
pharmacokinetic (PK) studies that determined any <strong>of</strong> the following: imatinib<br />
clearance, volume <strong>of</strong> distribution or half-life. Data was pooled to calculate a<br />
weighted mean ± SD for each PK parameter and these values were used to<br />
create a concentration-time pr<strong>of</strong>ile based on a 1 compartment model. A<br />
Monte Carlo Simulation (MCS; Crystal Ball v.11.1.1.3) was then completed<br />
to generate a distribution <strong>of</strong> steady state Cmin values for 1 million patients.<br />
This distribution was based solely on kinetic data; however, patient<br />
adherence would also affect Cmin. The MCS was used to demonstrate the<br />
probability <strong>of</strong> patient nonadherence (NA) according to the equation: NA =<br />
100% - [The probability <strong>of</strong> a specific Cmin according to the distribution].<br />
Results: The MCS demonstrated that at a standard dose <strong>of</strong> 400mg once<br />
daily, 63% <strong>of</strong> patients do not achieve the Cmin threshold (> 1000 ng/mL)<br />
recommended for CML patients, and 68% <strong>of</strong> patients are below 1100<br />
ng/mL, the target suggested for GIST patients. At Cmin levels between 0<br />
and 300 ng/ml, the probability <strong>of</strong> nonadherence is 90-100%; whereas at<br />
Cmin levels greater than 800 ng/ml, the probability <strong>of</strong> nonadherence is less<br />
than 50%.<br />
Conclusions: The majority <strong>of</strong> patients do not achieve the imatinib trough<br />
levels proposed for clinical efficacy with the standard dose <strong>of</strong> 400mg daily.<br />
Also, it is difficult to determine patient adherence based solely on Cmin<br />
levels.<br />
2 CSHP<br />
Targeting Excellence<br />
Évolution de la thromboprophylaxie chez les<br />
usagers médicaux dans un institut universitaire<br />
in Pharmacy Practice<br />
Julie Méthot, Marie-Noëlle Bartholoméi, Karine Lejeune, Institut<br />
universitaire de cardiologie et de pneumologie de Québec, QC<br />
La thromboprophylaxie s’inscrit dans une politique de sécurisation et<br />
d’amélioration de la prise en charge des patients. Cette dernière se place au<br />
cœur même de la prévention du risque thromboembolique chez les patients<br />
nécessitant des soins médicaux entraînant une immobilisation prolongée ou<br />
subissant une chirurgie. Des actions stratégiques ont été mises en œuvre au<br />
sein de l’Institut universitaire de cardiologie et de pneumologie du Québec<br />
afin de promouvoir et évaluer la thromboprophylaxie chez les patients<br />
médicaux admis. En 2008 la création et la mise en place d’un aide-mémoire<br />
sur la thromboprophylaxie fut placé avec les documents d’admission à<br />
l’urgence. L’aide-mémoire comprenait les indications, les contre–indications<br />
et les posologies des médicaments utilisés en thromboprophylaxie. L’impact<br />
de la création de cet outil a été évalué suite à la révision de 263 dossiers. Le<br />
taux de thromboprophylaxie est demeuré stable (36,5% avant la mise en<br />
place de l’aide-mémoire à 38,7% après l’implantation de l’aide-mémoire).<br />
Cette première étude nous a amené à reconsidérer et remanier notre<br />
approche de la prévention des complications thromboemboliques chez les<br />
patients médicaux admis. L’étape suivante consista en la réalisation d’une<br />
ordonnance pré-imprimée de thromboprophylaxie. Elle fut annexée aux<br />
feuilles d’admission de l’urgence de l’établissement pour favoriser son<br />
utilisation et fut implantée en février 2010. Une révision de 241 dossiers a<br />
été faite. Nos données suggèrent un taux de thromboprophylaxie d’environ<br />
72% chez les patients médicaux admis après l’implantation de cette<br />
prescription. Les actions posées et les évaluations effectuées ont permis de<br />
promouvoir et améliorer la prescription adéquate de thromboprophylaxie.<br />
2010-2011 Perspectives on Drug Shortages in <strong>Hospital</strong>s in<br />
Quebec<br />
Ottino G. 1 , Lebel D. 1 , Bussières J.F. 1,2<br />
1 Pharmacy practice research unit, Pharmacy department, CHU<br />
Sainte-Justine, Montréal, QC<br />
2 Faculty <strong>of</strong> Pharmacy, Université de Montréal, Montréal, QC<br />
Rationale: Many stakeholders underscore the importance <strong>of</strong> the drug<br />
shortage problem and its risks, but few quantitative data have been<br />
published on the subject.
59<br />
Objectives: To report all the drug shortages experienced in Quebec<br />
hospitals.<br />
Study design and methods: This is a retrospective study based on all drug<br />
shortages reported by the wholesaler and individuals members <strong>of</strong> the<br />
Group Purchasing Organization (SigmaSanté) for Montreal, Laval and<br />
Eastern township regions for 12 months (e.g. August 30, 2010 to August<br />
23, 2011).<br />
Results: A total <strong>of</strong> 429 drug shortages were reported in 2010-2011 vs.<br />
similar 12-month period; 493 in 2006, 400 in 2007, 442 in 2008, 680 in<br />
2009 and 385 in 2010 (only the 8 first months). The average duration <strong>of</strong><br />
the drug shortages remained similar, with 103 ± 85 days [8-363] in 2010 vs<br />
108 ± 130 days [5-1623] in 2006-2010. A smaller number <strong>of</strong><br />
manufacturers involved in drug shortages was also noted (41 in 2010-2011<br />
vs. 70 in 2006-2010), a decrease that was undoubtedly related to mergers<br />
and the integration or closing <strong>of</strong> certain drug manufacturers. Most <strong>of</strong> the<br />
reported shortages in 2010-2011 came from generic drug manufacturers<br />
and their relative ranking remained similar (i.e., in decreasing order, in<br />
2006-2010, Apotex (19% <strong>of</strong> total drug shortages), Pharmascience (14%),<br />
Novopharm (now TEVA) (12%), Sandoz (10%), Hospira (6%), TEVA (4%),<br />
Baxter (3%), Ratiopharm (taken over by Teva) (3%), Omega (2%), Taro<br />
(2%) vs. in 2010-2011, TEVA (23%), Apotex (16%), Pharmascience (12%),<br />
Hospira (7%), Sandoz (7%), Baxter (5%), AA Pharma (created from the<br />
resale <strong>of</strong> certain licenses held by Apotex) (3%), Schering (3%), Abbott<br />
(3%), Merck Canada (2%). Most therapeutic classes were involved in drug<br />
shortages in 2006-2010 as in 2010-2011,<br />
Conclusion: There are an important amount <strong>of</strong> drug shortages in Quebec<br />
hospital since 2006 and there are no sign <strong>of</strong> reduction <strong>of</strong> their occurrence.<br />
2 CSHP<br />
Targeting Excellence<br />
in Pharmacy Practice<br />
Multicenter Study on Environmental<br />
Contamination by Hazardous Drugs in Quebec<br />
Healthcare Centers<br />
Bussières J.F. 1,2 , Touzin K. 1 , Tanguay C. 1 , Langlois E. 3 , Métra A. 4 , Lefebvre M. 3<br />
1 Pharmacy department and Pharmacy practice research unit<br />
2 Faculty <strong>of</strong> pharmacy, University <strong>of</strong> Montreal<br />
3 Centre de toxicologie du Québec, Institut national de santé publique du<br />
Québec<br />
4 Association paritaire de santé et sécuritaire au travail – secteur affaires<br />
sociales<br />
Rationale: Many occupational exposure studies have revealed the presence<br />
<strong>of</strong> hazardous drugs contamination on work surfaces used for the<br />
preparation, storing and administration <strong>of</strong> hazardous drugs in healthcare<br />
centers. Most studies were conducted in the United States, Europe and<br />
Japan. This multicenter study is the first to be conducted in Quebec<br />
healthcare centers.<br />
Objectives: To describe environmental contamination by hazardous drugs<br />
in Quebec healthcare centers.<br />
Study design and methods: Descriptive, prospective, comparative study.<br />
Six standardized sites in the pharmacy and six sites on wards were sampled<br />
in each participating center. Samples were analysed for the presence <strong>of</strong><br />
cyclophosphamide, ifosfamide and methotrexate by UPLC-MS-MS. A<br />
sample was considered positive if these drugs were detected and a sample<br />
was considered contaminated if the detected concentration was above<br />
1ng/cm 2 .<br />
Results: Twenty-five <strong>of</strong> 68 (37%) Quebec healthcare centers were included<br />
in the study. A total <strong>of</strong> 259 samples were collected between April 2008 and<br />
January 2010. Each center had at least one positive sample for one <strong>of</strong> the<br />
three drugs tested (median [min-max] 5[1-12] positive samples per center<br />
and 0[0-3] contaminated samples per center). Overall, 135 (52%) samples<br />
were positive for cyclophosphamide, 45 (17%) were positive for ifosfamide<br />
and 3 (1%) were positive for methotrexate. The pharmacy hood front grille<br />
was the sample site with the higher proportion <strong>of</strong> positive samples, with 23<br />
out <strong>of</strong> 25 (92%) samples positive for cyclophosphamide. The median<br />
[min-max] concentration <strong>of</strong> hazardous drug was <strong>of</strong> 0.004[0-28.0] ng/cm 2<br />
for cyclophosphamide, ND[0-8.6] ng/cm2 for ifosfamide and ND[0-0.58]<br />
ng/cm2 for methotrexate.<br />
Conclusion: Although hazardous drug traces are frequently found, a<br />
median <strong>of</strong> less than one sampling site per center was actually<br />
contaminated. Periodic surface contamination measurements are necessary<br />
to ensure that current practices limit occupational exposure to hazardous<br />
drugs.<br />
Temps associé à la purge des tubulures lors de la préparation<br />
d’une dose de médicament dangereux et contamination<br />
visuelle<br />
Voisine M.1, Touzin K. 1 , Therrien R., Bussières J.F. 1,2<br />
1 Unité de recherche en pratique pharmaceutique, Département de<br />
pharmacie, CHU Sainte-Justine, Montréal, QC<br />
2 Faculté de pharmacie, Université de Montréal, Montréal, QC<br />
Justification : L’amorçage des sacs de médicaments dangereux ainsi que la<br />
purge centralisée à la pharmacie de la tubulure peuvent contribuer à<br />
minimiser l’exposition pr<strong>of</strong>essionnelle aux médicaments dangereux.<br />
L’impact de cette centralisation sur la charge de travail est méconnu.<br />
Objectifs : Évaluer l’impact de la purge centralisée des tubulures sur le<br />
temps associé à la préparation d’une dose de médicament dangereux et sur<br />
la présence de contamination visuelle à la pharmacie et à l’unité de soins<br />
d’hématologie-oncologie.<br />
Méthodologie : Il s’agit d’une étude observationnelle comparative en deux<br />
phases. La première consistait à comparer le temps médian pour la<br />
préparation d’une dose de médicament dangereux par un<br />
assistant-technique en pharmacie sans purge et avec purge des tubulures à<br />
la pharmacie. La seconde visait à évaluer le temps médian nécessaire à la<br />
préparation d’une dose de médicament dangereux par le personnel<br />
infirmier à l’étage, suite à la purge des tubulures par le personnel de la<br />
pharmacie. Pour l’étude, le médicament dangereux était remplacé par une<br />
solution d’eau stérile colorée (essence de cerise). La contamination visuelle<br />
était évaluée dans les deux phases.<br />
Résultats : Dans la première phase, le temps médian [intervalle] de<br />
préparation d’un sac de médicament non purgé (n=30) était de 98[80-167]<br />
secondes et le temps médian de préparation d’un sac purgé par la<br />
pharmacie (n=30) s’élevait à 295[207-520] secondes (Kruskal-Wallis<br />
p 0.03 units/minute) Associated with Adverse<br />
Events in Cardiac Surgery Patients?<br />
Hina Ahmed, Marcin Wasowicz, Lior Flor, Vivek Rao, Toronto General<br />
<strong>Hospital</strong>, Toronto, ON<br />
Rationale: Vasopressin is used in the setting <strong>of</strong> vasopressor resistant<br />
vasodilatory shock. The Surviving Sepsis guidelines recommend maximum<br />
vasopressin infusion <strong>of</strong> 0.03units/minute as an adjunct to norepinephrine.<br />
Vasopressin has been used to help reduce norepinephrine dose and to<br />
prevent adverse events related to high dose norepinephrine. In higher doses<br />
vasopressin has been associated with adverse events including reduced<br />
cardiac output, decreased oxygen delivery, decrease in mixed-venous<br />
oxygen saturation leading to impaired tissue perfusion, reduction in platelet<br />
count, hyponatremia, and injury to splanchnic organs. The safety <strong>of</strong><br />
vasopressin use in cardiac surgery patients has not been studied as a<br />
primary endpoint.<br />
Objectives: Use <strong>of</strong> high dose vasopressin (> 0.03 units/minute) is<br />
associated with adverse events in cardiac surgery patients.<br />
Study Design and Methods: Upon REB approval, retrospective chart<br />
review was conduced to identify patients scheduled for cardiac surgery
60<br />
receiving vasopressin (> 0.03units/minute). Data was collected through<br />
retrospective chart review. Primary outcome: adverse events potentially<br />
related to high dose vasopressin. Secondary objective: review vasopressin<br />
infusion use in relation to other vaopressor support.<br />
Results: Over a 60-day period, 280 patients underwent cardiac surgery and<br />
34 (12.5%) received vasopressin. Major perioperative bleeding was seen in<br />
8 patients (26%) receiving vasopressin. Vasopressin was infused at doses<br />
higher than recommended, ranging from 0.03 units/min – 0.13 units/min<br />
with an average duration <strong>of</strong> 34 hours. Ischemic complications were seen in<br />
less than 10% <strong>of</strong> patients and only one patient developed bowel ischemia.<br />
Among all patients, 85% received norepinephrine concurrently.<br />
Norepinephrine was used first line in over 50% <strong>of</strong> cases. In majority (87%)<br />
vasopressin was used an adjunct to other vasopressors. Average hospital<br />
LOS was 16 days as opposed to 6 days.<br />
Conclusion: Adverse events were seen infrequently with high dose<br />
vasopressin. Due to limitations <strong>of</strong> this study, a prospective study will help<br />
capture the true incidence <strong>of</strong> adverse events.<br />
Assessing the Extent <strong>of</strong> Fluoroquinolone-Cation Interactions<br />
at a Teaching <strong>Hospital</strong><br />
Wenya Miao, Pharmacy Student, University <strong>of</strong> Toronto, Toronto ON,<br />
Rosemary Zvonar, The Ottawa <strong>Hospital</strong>, Ottawa, ON<br />
Rationale: Both fluoroquinolone antibiotics (FQ) and divalent or trivalent<br />
cationic drugs (DTC), such as aluminum, magnesium, iron, calcium and<br />
zinc, are frequently prescribed in hospitalized patients. The interaction<br />
between oral FQs and DTCs is well recognized, and therapeutic failures due<br />
to impaired FQ absorption have been reported when these agents are taken<br />
concomitantly.<br />
Objective: To determine the prevalence <strong>of</strong> the interaction between FQs<br />
and DTCs at our institution.<br />
Methods: On a single day in July 2010, patients prescribed formulary oral<br />
FQs (lev<strong>of</strong>loxacin and cipr<strong>of</strong>loxacin) and DTCs were identified by the<br />
Pharmacy computer system. The Medication Administration Records <strong>of</strong><br />
these patients were examined and scheduled drug administration times<br />
recorded. An interaction was defined as follows: for lev<strong>of</strong>loxacin, an<br />
administration time for the DTC within 2 hours before or after that <strong>of</strong><br />
lev<strong>of</strong>loxacin; for cipr<strong>of</strong>loxacin, an administration time for the DTC within 4<br />
hours before or 2 hours after any cipr<strong>of</strong>loxacin dose. Based on the results <strong>of</strong><br />
the initial review, additional interventions to those already in place to<br />
minimize the chance <strong>of</strong> interaction were implemented. A similar assessment<br />
was repeated in June 2011.<br />
Review performed<br />
Results:<br />
July 26, 2010<br />
Number <strong>of</strong> patients on oral 61 68<br />
FQ<br />
Number <strong>of</strong> patients on an oral 27 38<br />
FQ and DTC<br />
Number <strong>of</strong> interactions 16 18<br />
59.2% 47.4%<br />
Percentage <strong>of</strong> patients on<br />
both oral FQ and DTC with<br />
interaction<br />
Review performed<br />
June 15, 2011<br />
Conclusion: We identified a significant proportion <strong>of</strong> patients receiving oral<br />
FQs and DTCs either concomitantly or with inappropriate spacing, despite<br />
education and additional computer warnings following the initial review.<br />
Healthcare workers must remain vigilant for this frequent interaction.<br />
Continual review and intervention may be required to limit its occurrence.<br />
Tuesday, February 7<br />
Mardi 7 février<br />
2 CSHP<br />
Targeting Excellence<br />
A Systematic Analysis <strong>of</strong> Pharmacist Referrals<br />
Originating from the Order Desk<br />
in Pharmacy Practice<br />
Danette Beechinor, Credit valley <strong>Hospital</strong>, Mississauga, ON and<br />
University <strong>of</strong> Waterloo, Kitchener, ON<br />
Rationale for Report: Significant clinical pharmacist time is spent resolving<br />
problems which originate on the order desk, which is typical for many<br />
hospitals. There is no published or local data which describes the problems<br />
returned to the clinical pharmacist.<br />
Description <strong>of</strong> Concept, Service, Role or Situation: A study <strong>of</strong> the types<br />
<strong>of</strong> problems which are returned to the floor pharmacist was undertaken to<br />
determine potential time saving policies and procedures which could be<br />
developed while ensuring patient safety and minimizing distribution related<br />
delays.<br />
Steps Taken to Identify and Resolve Problem: Two hundred forty<br />
documents (convenience sample) which were identified by the order desk<br />
pharmacist as needing follow up by the floor pharmacist were analyzed<br />
using content analysis methodology. The documents were categorized<br />
according to problem type and analyzed to determine if improved policies<br />
or programs could facilitate problem resolution by the order desk and serve<br />
patients more efficiently and safely. All categories were considered for<br />
potential time savings and safety enhancement. Examples <strong>of</strong> categories<br />
which emerged included: identifying patients’ own non-formulary<br />
medication, inappropriate dosage form ordered crushed, confirm date <strong>of</strong><br />
weekly and monthly medications and dosage adjustment for renal<br />
dysfunction.<br />
Evaluation <strong>of</strong> Project: <strong>Hospital</strong> and departmental policies are under<br />
development as a result <strong>of</strong> this study to save time and enhance patient<br />
safety. Examples <strong>of</strong> policies include: pharmacist adjustment <strong>of</strong> antibiotics for<br />
poor renal function, non-formulary medication identification and<br />
documentation by technician during Best Possible Medication History, and<br />
standardized administration dates for weekly or monthly medications such<br />
as bisphosphonates.<br />
Importance and Usefulness: A systematic exploration <strong>of</strong> the<br />
departmental needs and typical problems which arise on order entry was<br />
used to propose policy changes to improve efficiency in order entry.<br />
Systematic problem review by hospital pharmacies can identify time- and<br />
cost-saving measures which enhance patient safety and delivery <strong>of</strong> care.<br />
Audit <strong>of</strong> Antibiotic Duration <strong>of</strong> Therapy, Appropriateness<br />
and Outcome in Patients with Nosocomial Pneumonia<br />
Following the Removal <strong>of</strong> an Automatic Stop-date Policy<br />
Jennifer Do, Sandra A. N. Walker, Scott E. Walker, William Cornish, Andrew<br />
E. Simor, Sunnybrook Health Sciences Centre. Toronto, ON<br />
Rationale: Although automatic stop-orders (ASOs) may discourage<br />
inappropriately prolonged antibiotic therapy, risks to patient safety<br />
associated with premature antibiotic discontinuation resulting from ASO<br />
policies have been reported. An ASO policy necessitating reordering <strong>of</strong><br />
antibiotics after day seven <strong>of</strong> therapy had been in place at our institution<br />
prior to 2002; but was revoked after instances <strong>of</strong> compromised patient care<br />
associated with inadvertent and inappropriate interruption <strong>of</strong> antimicrobial<br />
treatment. Comparative data <strong>of</strong> patient outcomes with and without<br />
institutional ASO policies is lacking.<br />
Objectives: The study objective was to evaluate the impact <strong>of</strong> revoking the<br />
ASO policy on duration <strong>of</strong> antibiotic therapy, infection-related outcome,<br />
relapsing infection, occurrence <strong>of</strong> resistant bacteria and superinfection in<br />
patients with nosocomial pneumonia.<br />
Study Design and Methods: A retrospective chart review <strong>of</strong> hospitalized<br />
adults (> 18 years) who developed nosocomial pneumonia requiring<br />
antibiotic therapy was conducted. Duration <strong>of</strong> antibiotic therapy,
61<br />
infection-related outcome (cure vs. failure), rate <strong>of</strong> relapsing infection,<br />
resistance and superinfection were compared for the pre and post-ASO<br />
policy revocation cohorts. An unpaired t-test or Fisher’s exact test was used<br />
for interval and nominal data comparisons, respectively. Multiple regression<br />
analysis and propensity score adjustment were completed to adjust for<br />
imbalances between groups. A p-value 0.5).<br />
Conclusion: Revocation <strong>of</strong> the ASO policy for antibiotics at our institution<br />
was not associated with a longer duration <strong>of</strong> antibiotic therapy, or an<br />
increased incidence <strong>of</strong> infection-related mortality, relapsing infection,<br />
resistant bacteria or superinfection for patients with nosocomial<br />
pneumonia.<br />
Identification <strong>of</strong> Predictors <strong>of</strong> Infection in Acute Burn Injury<br />
Patients<br />
Laura Schultz, Sandra A.N. Walker, Marion Elligsen, Scott E. Walker,<br />
Andrew Simor, Samira Mubareka, Nick Daneman, Toronto, ON<br />
Rationale: Burn patients are at high risk for infections; however, common<br />
indicators <strong>of</strong> infection are unreliable in this population and can lead to<br />
unnecessary use <strong>of</strong> antibiotics.<br />
Objectives: The objective <strong>of</strong> this study was to determine if predictors <strong>of</strong><br />
infection in adult acute burn injury patients could be identified in order to<br />
provide clinicians with a practical tool to aid in the diagnosis <strong>of</strong> infection in<br />
acute burn injury, thereby minimizing unnecessary antimicrobial exposure.<br />
Study Design and Methods: A retrospective chart review was conducted on<br />
all adult acute burn injury patients admitted to the burn centre at SHSC<br />
over a 1 year period. If a patient was started on the antibiotics during the<br />
first 10 days <strong>of</strong> admission, they were assessed for infection using the<br />
American Burn Association guidelines. Patient demographic data and<br />
clinical parameters were collected from admission to day 10 <strong>of</strong><br />
hospitalization. If the patient was started on antibiotics, information was<br />
gathered inclusively from 3 days before to 7 days after antibiotic initiation.<br />
Patients without infection were compared to patients with sepsis and those<br />
with infection using unpaired t-test, Fisher’s exact, regression analysis and<br />
CART analysis.<br />
Results: Of the 111 patients studied, 50% had infection and 16% had<br />
sepsis within the first 10 days <strong>of</strong> admission. Using regression analysis and<br />
CART identified breakpoints, it was determined that heart rate ≥110 bpm,<br />
systolic blood pressure ≤100 mmHg and intubation were the best predictors<br />
<strong>of</strong> sepsis; and fraction <strong>of</strong> inhaled oxygen >25% and maximum temperature<br />
≥39˚C were the best predictors <strong>of</strong> infection (p
62<br />
A Pilot Study to Evaluate Methodology for Assessing the<br />
Treatment <strong>of</strong> Low Back Pain<br />
Jerrold Petr<strong>of</strong>sky 1 , Lee Berk 1,2 , Gurinder Bains 1 , Geraldine Doyle 3 , Shijie<br />
Chen 3 , Lisa Baird 3 , Paul Desjardins 3 , and Jill Stark 3<br />
1 Department <strong>of</strong> Physical Therapy<br />
2 Department <strong>of</strong> Pathology & Human Anatomy, Loma Linda University,<br />
Loma Linda, CA<br />
3 Pfizer Consumer Healthcare, Madison, NJ<br />
Rationale: Low back pain (LBP) is a common and costly medical problem.<br />
Using a stopwatch to measure the time <strong>of</strong> the onset <strong>of</strong> the analgesic effect<br />
has not been evaluated in a LBP model.<br />
Objective: This pilot study was to evaluate the sensitivity <strong>of</strong> using the<br />
methodology for assessing LBP relief with ThermaCare LowBack/Hip<br />
Heatwraps.<br />
Study Design and Methods: Subjects with baseline primary muscle acute<br />
LBP were randomized to ThermaCare, oral placebo, unheated “sham”<br />
wrap, or oral ibupr<strong>of</strong>en. The last 2 treatments were included for blinding<br />
purposes only.<br />
Subjects stopped the first stopwatch upon feeling the “first perceptible”<br />
pain relief, and the second stopwatch upon feeling “meaningful” pain<br />
relief. Subjects also assessed pain relief hourly.<br />
Results: Sixty-one subjects participated in this single-center, single-dose<br />
(single wrap wear occasion), randomized, single-blind, placebo-controlled<br />
trial.<br />
The TOTPAR 0-8 was significantly higher for ThermaCare Heatwrap than<br />
placebo group (22.0 vs. 11.5; p240 and 215.7 vs. >240,<br />
respectively; p
63<br />
Self-Perceived Knowledge Gained and Satisfaction from<br />
Brown Bag Medication Reviews for Older Adults<br />
Nishi S. Gupta 1 , Feng Chang 1 , Megan E. Kleinow 2 , Jamie M. Hwang 3 ,<br />
Candice L. Garwood 4 , Hanan S. Khreizat 2 , Mary Beth O’Connell 4<br />
1 University <strong>of</strong> Waterloo, School <strong>of</strong> Pharmacy, Waterloo, ON<br />
2 Henry Ford Health System, Detroit, MI<br />
3 Henry Ford Piersen Clinic, Grosse Pointe Farms, MI<br />
4 Wayne State University, Eugene Applebaum College <strong>of</strong> Pharmacy and<br />
Health Sciences, Detroit, MI<br />
Rationale: Community based brown bag medication reviews are used in<br />
settings without access to primary care providers or the medical chart.<br />
Objectives: To examine self-perceived knowledge gained and participant<br />
satisfaction during community based brown bag medication reviews.<br />
Methods: Reviews were conducted in 9 senior centers for adults over the<br />
age <strong>of</strong> 60 and on 5 or more medications. Each appointment was scheduled<br />
for 45-60 minutes. A medication calendar and a list <strong>of</strong> recommendations<br />
were given. Seniors were asked to complete a 13-items satisfaction<br />
questionnaire following the session and rate the program’s helpfulness in a<br />
follow-up survey at 3 months. Each item was ranked 1-5 (strongly disagree<br />
– strongly agree). Self-perceived learning was reported using an 8-items<br />
survey. Each item was ranked 1-5 (very little – lots). Unreturned surveys<br />
were followed-up over the phone. Descriptive statistics were used.<br />
Results: Sixty-four participants completed follow-up. All items on the<br />
satisfaction questionnaire were ranked between 4.44– 4.90. The highest<br />
ranked items were: having enough time to ask questions (4.90); time and<br />
place <strong>of</strong> the review were convenient (4.83); trust in the pharmacist’s<br />
answers (4.83); and better understanding <strong>of</strong> their medications (4.83). The<br />
lowest ranked item was perceived resolution <strong>of</strong> their health problems<br />
(4.44). At 3-months, 98% ranked the brown bag program as helpful.<br />
Self-perceived knowledge gained was rated between 4.40-4.71. The<br />
highest ranked items were: learning how to use their medications (4.71);<br />
when to correctly take the medications (4.66); and learning the purpose <strong>of</strong><br />
their medications (4.64). Perceived knowledge gained in understanding<br />
medication side effects was rated the lowest (4.40). Over 95% would like<br />
to attend the program again.<br />
Conclusion: Seniors were highly satisfied with the brown bag medication<br />
reviews. They felt a high degree <strong>of</strong> learning and found the program<br />
convenient. Individual items ranked demonstrated unique advantages and<br />
limitations <strong>of</strong> such programs.<br />
Cost Analysis <strong>of</strong> an Insulin Pen Pilot Project in an In-Patient<br />
<strong>Hospital</strong> Setting<br />
Sara Kynicos 1 , Jin Hyeun Huh 1,2<br />
1 University Health Network, Toronto, ON<br />
2 Leslie Dan Faculty <strong>of</strong> Pharmacy, University <strong>of</strong> Toronto, ON<br />
Rationale: Following medication incidents involving insulin, a known<br />
high-risk medication, a 3 month pilot project using insulin pens for<br />
in-patients was implemented in general internal medicine (98 beds across 3<br />
floors) at one hospital site.<br />
Objective: To review costs and wastage associated with implementing<br />
insulin pens, together with nursing and safety benefits using staff surveys<br />
and a review <strong>of</strong> medication incidents.<br />
Method: All existing formulary insulins were made available in pen devices<br />
as floor-stock and each patient was allocated their own pen for each insulin<br />
to be administered by nurses. A review <strong>of</strong> data compared the usage and<br />
costs <strong>of</strong> insulin dispensed during the 3-month pilot period to the 3 previous<br />
months <strong>of</strong> traditional 10mL insulin vial dispensing.<br />
Results: The results showed that there was a 12% decrease in total volume<br />
(mLs) <strong>of</strong> insulin dispensed during the pen pilot, however less favourable<br />
contract prices resulted in increased total cost for pre-filled pens /<br />
cartridges, equivalent to a 24% increase ($115 per month per floor). During<br />
the pilot 20% more safety needles were used compared to traditional<br />
safety syringes.<br />
A review <strong>of</strong> insulin pen wastage over one month showed that 64% <strong>of</strong><br />
insulin not used in the pen devices was short or rapid insulin types.<br />
No medication incidents involving insulin were identified during the pilot<br />
and nursing staff surveys indicated that they felt nursing time was saved<br />
due to pens being readily available for individual patient-use. Staff also<br />
suggested that less time was spent on discharge patient education,<br />
resulting in an improved patient discharge process.<br />
Conclusion: This project demonstrates that insulin pen devices can be<br />
successfully implemented in an in-patient hospital setting, with medication<br />
safety, nursing time and patient discharge benefits, despite increased<br />
medication costs.<br />
2 CSHP<br />
Targeting Excellence<br />
in Pharmacy Practice<br />
Venous Thromboembolism Prophylaxis Electronic<br />
Physician Risk Assessment Tool<br />
Pauline Santora and Cristina Scherf, Baycrest, Toronto, ON<br />
Rationale: VTE prophylaxis is the number 1 strategy to improve patient<br />
safety in hospitals and is recognized by Accreditation Canada as an<br />
‘organizational required practice’. Universally starting prophylaxis on<br />
admission did not seem justifiable at Baycrest, a geriatric acute, complex<br />
continuing care and long-term care facility where the situation is <strong>of</strong>ten<br />
more long term and risks <strong>of</strong> harm from the prophylaxis elevated.<br />
Description <strong>of</strong> Concept: To develop an electronic tool that would provide<br />
a physician assessment <strong>of</strong> VTE prophylaxis for each geriatric hospitalized<br />
patient and that could electronically generate preselected quality indicators.<br />
Steps Taken: Based on a literature review and manual chart audits, a<br />
multi-disciplinary group developed an algorithm with input from experts.<br />
Background information specific to geriatrics is available for each question<br />
at the click <strong>of</strong> a button. Information Technology built the algorithm into<br />
Meditech for easy access by the admitting physician who completes it<br />
within 24 hours <strong>of</strong> admission, transfer or new acute medical illness in the<br />
hospitalized patient. The policies, procedures, and algorithm were approved<br />
prior to training and implementation.<br />
Evaluation: Physician’s evaluation indicated that this electronic point and<br />
click tool is straight forward and can be completed in 15-60 seconds.<br />
The tool provides the electronic means to audit VTE prophylaxis assessment<br />
rates, the timeline <strong>of</strong> assessment completion, which VTE protection was<br />
ordered and if not, the reason(s), for any period, on any day, within<br />
minutes.<br />
Previously documented VTE Risk Assessments were hard to find. The<br />
electronic tool has increased this to 68 % <strong>of</strong> admissions in May, 80 % in<br />
June and 92 % in July.<br />
Importance to Practice: The use <strong>of</strong> technology to provide a practical<br />
standardized approach for VTE prophylaxis, supported by educational<br />
information and up-to-date audit results is extremely useful in our efforts to<br />
improve the safety <strong>of</strong> hospitalized elderly patients.<br />
2 CSHP<br />
Targeting Excellence<br />
Fingertip Sampling is a More Sensitive Evaluation<br />
<strong>of</strong> Aseptic Technique Competency<br />
in Pharmacy Practice<br />
Mari Culotta-Mascioli, John Iazzetta, Scott Walker, Fausto Noce,<br />
Sunnybrook Health Sciences Centre, Odette Cancer Centre, Department <strong>of</strong><br />
Pharmacy, Toronto, ON<br />
Rationale: A system <strong>of</strong> random gloved finger tip testing in tandem with a<br />
media fill test allows auditors to visually inspect aseptic technique in<br />
addition to producing evidence <strong>of</strong> positive or negative growth <strong>of</strong> microbes<br />
through finger tip imprinting on agar plates filled with test media.<br />
Objectives: To determine microbial contamination rate during sterile<br />
preparation with the best <strong>of</strong> controls being in place. Compare these results<br />
with those from planned media fill tests done as part <strong>of</strong> an annual<br />
recertification.
64<br />
Study design: We conducted gloved finger tip sampling in 32 sterile<br />
compounders. Raised test plates containing trypticase soy agar with<br />
polysorbate and lecithin were used as the test media. Samples <strong>of</strong> gloved<br />
finger tips were taken under three scenarios. A group <strong>of</strong> 18 volunteers gave<br />
finger tip samples without having performed a scrub or hand hygiene. A<br />
second group <strong>of</strong> 16 after thorough hand scrubbing and a third group <strong>of</strong> 16<br />
under random conditions while performing regular aseptic compounding<br />
duties. The samples collected were incubated for 48 hours at 33-37°C.<br />
After 48 hours the plates were visually inspected for colony forming units.<br />
The Media fill testing was conducted during annual recertification.<br />
Results: After the incubation period it was noted that while some plates<br />
resulted in no growth, 62% <strong>of</strong> plates from all three groups were positive<br />
with CFU’s. However, all the volunteers were able to produce test media<br />
bags with no growth at time <strong>of</strong> planned testing in previous tests.<br />
Conclusion: Our results indicate a need for an additional evaluation to<br />
ensure a high standard <strong>of</strong> aseptic technique is maintained. Perhaps an<br />
evaluating system that allows for more frequent random auditing.<br />
Potential Cross-Reactivity between Prasugrel and Clopidogrel<br />
Joyce Chan 1 , Yvonne Kwan 1 , Sonia Mota 1 and Kori Leblanc 1,2<br />
1 University Health Network, Toronto, ON<br />
2 Faculty <strong>of</strong> Pharmacy, University <strong>of</strong> Toronto, Toronto, ON<br />
Rationale: Prasugrel is a third-generation thienopyridine antiplatelet agent<br />
effective for the management <strong>of</strong> acute coronary syndrome in planned<br />
percutaneous coronary intervention (PCI). It became available to <strong>Canadian</strong><br />
patients in June 2010 and is attractive as an alternative in patients who<br />
have experienced adverse reactions to clopidogrel. Cross-reactivity between<br />
clopidogrel and other thienopyridine antiplatelet agents has been reported.<br />
Although cross-reactivity with prasugrel on allergy testing has been seen,<br />
reports <strong>of</strong> patient experience are extremely limited.<br />
Objective: To document the experience <strong>of</strong> patients with a history <strong>of</strong><br />
adverse skin reactions to clopidogrel who received prasugrel.<br />
Methods: Patients with a documented skin reaction to clopidogrel who<br />
were prescribed prasugrel were followed at 24h and post-discharge. Data<br />
was collected regarding tolerance as well as adherence to therapy.<br />
Results: Eight patients received prasugrel. All reported good medication<br />
adherence. One patient developed an itchy macular rash over the body and<br />
upper thighs within 24 hours <strong>of</strong> prasugrel exposure, requiring<br />
discontinuation and replacement with ticlopidine. A Naranjo Adverse Drug<br />
Reaction (ADR) probability score <strong>of</strong> 4 defined this as a “possible” ADR<br />
association. No other patients experienced skin reactions. Seven out <strong>of</strong> 8<br />
patients required financial assistance to afford prasugrel which was<br />
facilitated by the pharmacist pre-discharge. In all cases, the patients’<br />
community pharmacy did not have prasugrel readily available.<br />
See table on page 65.<br />
Conclusion: Our experience with 8 patients with previous skin reactions to<br />
clopidogrel suggests that there is at least a small risk <strong>of</strong> cross-reactivity with<br />
prasugrel. Further experience is needed to clearly define that risk.<br />
Determining patients’ financial coverage for prasugrel and facilitating its<br />
availability in community pharmacies post-discharge is essential to ensure<br />
that doses are not unintentionally missed.<br />
2 CSHP<br />
Targeting Excellence<br />
Total Parenteral Nutrition: Supporting Practice<br />
Through Standardized Solutions<br />
in Pharmacy Practice<br />
Rosemary Tanzini and Jill Garland, St. Michael’s <strong>Hospital</strong>,<br />
Toronto, ON<br />
Rationale: Commercial options for TPN base solutions no longer met<br />
evolving practice. Over the years, in order to meet protein requirements, the<br />
administration <strong>of</strong> TPN had become more complex, due to the additional<br />
administration <strong>of</strong> amino acids (Y-connected in a separate bag to the 2-in-1<br />
(dextrose/amino acid) bsolutions. This “modular” approach to supplying<br />
TPN complicates the prescribing process and increases the risk <strong>of</strong> pump<br />
programming errors and workload for the RN. Lack <strong>of</strong> standardization and<br />
a manual system <strong>of</strong> generating patient specific worksheets and labels for<br />
compounding purposes was also labor intensive for Pharmacy and<br />
increased the risk <strong>of</strong> errors. It also became apparent that to enable<br />
electronic compounding worksheets automated for calculations, it was<br />
necessary to provide the daily dextrose/amino acid requirement into 1 bag.<br />
Developing a “menu” <strong>of</strong> TPN base solutions which would meet the needs<br />
<strong>of</strong> the majority <strong>of</strong> patients and a comprehensive TPN order form has the<br />
potential to facilitate prescribing, production and administration.<br />
Description/Implementation: Project began with audit <strong>of</strong> current state to<br />
determine different permutations <strong>of</strong> amino acids/dextrose/lipids being<br />
prescribed, as well as wastage. Empiric calculations, for the purpose <strong>of</strong> dose<br />
banding, was done for patients ranging in weight, taking into account<br />
target calories and step-wise approach to advancing caloric intake in<br />
patients at risk <strong>of</strong> refeeding syndrome. Next, there was a review <strong>of</strong><br />
commercial and compounding options (with stability data), including a<br />
time-motion study. Input from Nutrition team was critical to coming up<br />
with a final list <strong>of</strong> solutions. Accordingly, an order set was developed which<br />
clearly outlined options and provide decision support. Electronic<br />
compounding worksheets and computer-generated labels were to follow.<br />
Evaluation: Over first 5 months post implementation, <strong>of</strong> 53 patients,<br />
standard solutions met the needs <strong>of</strong> all but 2 patients.<br />
Importance to Practice: Improved safety, quality, transparency, efficiency<br />
and communication.<br />
Determination <strong>of</strong> Tobramycin Pharmacokinetics in Burn<br />
Patients to Evaluate the Potential Utility <strong>of</strong> Once Daily<br />
Dosing in this Population<br />
Diane Vella, Sandra A.N. Walker, Scott E. Walker, Andrew Simor,<br />
Sunnybrook Health Sciences Centre, Toronto, ON<br />
Rationale: Once-daily aminoglycosides (ODAs) have been avoided in burn<br />
injury patients, due to their complicated pharmacokinetics. Theoretically,<br />
ODAs may have the same advantages in burn patients as in other<br />
populations.<br />
Objectives: The objectives were to determine the pharmacokinetics <strong>of</strong><br />
tobramycin in adult critically ill burn patients and evaluate a variety <strong>of</strong><br />
mg/kg dosing regimens to determine if ODA therapy was feasible.<br />
Methods: A retrospective study <strong>of</strong> 58 adult critically ill burn injury patients<br />
who received tobramycin and had at least one set <strong>of</strong> tobramycin<br />
steady-state levels was conducted. Pharmacokinetic parameters were<br />
calculated using first-order pharmacokinetic equations. CART analysis to<br />
identify whether a breakpoint for days post burn injury existed for<br />
tobramycin clearance (Cl) and Monte Carlo Simulations (MCS) <strong>of</strong> a range <strong>of</strong><br />
mg/kg dosing regimens, using mean pharmacokinetic parameters with<br />
respective standard deviations targeting a peak <strong>of</strong> ≥ 20mg/L and trough <<br />
2mg/L with at least 70% probability were run.<br />
Results: A CART identified breakpoint <strong>of</strong> days post burn for Cl <strong>of</strong> ≤45 days<br />
versus >45 days was determined. The geometric mean (95% CI)<br />
pharmacokinetic parameters in patients receiving tobramycin: ≤45 days<br />
post-burn were: ke 0.167h-1 (0.15-0.18), t1/2 4.1h (3.8-4.6), Vd 0.40L/kg<br />
(0.37-0.43), Cl 5.3L/h (4.9-5.8); and >45 days post-burn were: ke 0.13h-1<br />
(0.11-0.14), t1/2 5.4h (4.8-6.1), Vd 0.37L/kg (0.32-0.41), Cl 3.7L/h<br />
(3.2-4.1). MCS identified ODA regimens that attained the desired targets<br />
using higher mg/kg dosing known to be safe in other populations (≤45<br />
days post-burn: 10 to 13mg/kg; >45 days post burn: 8 to 10mg/kg).<br />
Conclusion: This study identified initial ODA tobramycin dosing<br />
recommendations that could attain desired targets in burn patients.
65<br />
Patient Age<br />
Gender<br />
Antiplatelet<br />
Therapy Indication ADR To Other Antiplatelets Follow up Tolerability<br />
1 60 Male PCI- DES Clopidogrel (urticaria) At 24 hours Prasugrel discontinued due<br />
to pruritic macular rash<br />
2 58 Female PCI- DES and BMS Clopidogrel (total body rash)<br />
Ticlopidine (rash and diarrhea)<br />
At 24 hours, then at 6 months and 7<br />
months post discharge<br />
3 63 Male PCI- DES Clopidogrel (localized rash)<br />
Ticlopidine (severe diarrhea<br />
resulting in weight loss)<br />
At 24 hours, then at 5 months post<br />
discharge<br />
4 63 Male PCI- BMS Clopidogrel (pruritic rash) At 24 hours, then at 1 week, 6 weeks<br />
and 4 months post discharge<br />
5 52 Female PCI- DES Acetylsalicylic acid (urticaria)<br />
Clopidogrel (pruritic maculopapular<br />
rash with positive rechallenge)<br />
6 59 Male PCI- DES Clopidogrel (pruritic rash - first to<br />
arms then to entire body)<br />
At 24 hours, then at 3 weeks and 4<br />
months post discharge<br />
At 24 hours, then at 3 weeks and 3<br />
months post discharge<br />
7 42 Male PCI- BMS Clopidogrel (total body rash) At 24 hours, then at 24 days post<br />
discharge<br />
8 73 Male PCI- DES Clopidogrel (non-itchy rash to arms,<br />
chest, abdomen, and upper back)<br />
DES: Drug Eluting Stent<br />
BMS: Bare Metal Stent<br />
At 1 week, 6 weeks, and 4 months<br />
post discharge (prasugrel was started<br />
the day after discharge)<br />
Well tolerated<br />
Well tolerated<br />
Well tolerated<br />
Well tolerated<br />
Well tolerated<br />
Well tolerated<br />
Wednesday, February 8<br />
Mercredi 8 février<br />
Diagnostic Reasoning by <strong>Hospital</strong> <strong>Pharmacists</strong>: An<br />
Assessment <strong>of</strong> Attitudes, Knowledge, Skills, and Learning<br />
Needs<br />
Kseniya Chernushkin, Peter Loewen, Joanne Jung, Amneet Aulakh, Jane de<br />
Lemos, Karen Dahri<br />
Background: Currently, hospital pharmacists participate in activities that<br />
can be seen as diagnostic in nature. Two reasoning approaches to making<br />
diagnoses have been previously described: non-analytic and analytic. Of the<br />
six analytic traditions “probabilistic” has been shown to improve diagnostic<br />
accuracy and reduce unnecessary testing. <strong>Pharmacists</strong>’ attitudes toward<br />
having a diagnostic role and their diagnostic knowledge and skills have<br />
never been studied.<br />
Objectives: To describe pharmacists’ attitudes toward the role <strong>of</strong> diagnosis<br />
in pharmacotherapeutic problem-solving; to characterize the extent <strong>of</strong><br />
pharmacists’ knowledge and skills related to diagnostic literacy; to identify<br />
knowledge/skill gaps and propose means <strong>of</strong> closing them.<br />
Method: <strong>Pharmacists</strong> <strong>of</strong> Lower Mainland Pharmacy Services with at least<br />
33% in direct patient care were studies in a prospective observational<br />
survey.<br />
Results: A sample <strong>of</strong> 260 pharmacists was identified. Results showed that<br />
89% <strong>of</strong> participants agreed with the proposed definition <strong>of</strong> diagnosis and<br />
92% agreed that it is important for pharmacists to have skills related to<br />
diagnosis. Respondents preferred analytic to non-analytic approach to<br />
diagnostic decision-making. Probabilistic tradition was not the preferred<br />
method in any <strong>of</strong> the three cases. In the evaluation <strong>of</strong> clinical scenarios that<br />
may require diagnostic skills 84% <strong>of</strong> respondents agreed that they should<br />
be involved in assessing such problems and 84% agreed that the case<br />
problems were diagnostic in nature. Participants’ knowledge <strong>of</strong> and ability<br />
to apply probabilistic diagnostic tools were highest with test sensitivity<br />
(61% <strong>of</strong> correct answers) and lower with test specificity (48% <strong>of</strong> correct<br />
answers) and likelihood ratios (39% <strong>of</strong> correct answers).<br />
Conclusions: The pharmacists studied strongly believe that diagnostic skills<br />
are important for them to solve drug-related problems, but demonstrated<br />
low levels <strong>of</strong> knowledge and ability to apply concepts <strong>of</strong> probabilistic<br />
diagnostic reasoning. Opportunities to expand pharmacists’ knowledge <strong>of</strong><br />
diagnostic reasoning exist, and our findings indicate that they would<br />
consider such development valuable.<br />
2 CSHP<br />
Targeting Excellence<br />
A Pilot Study on the Use <strong>of</strong> Warfarin Sliding Scales<br />
in Hemodialysis Patients<br />
in Pharmacy Practice<br />
Grace Leung, Emmelia Lau, and Henry Chen, York Region<br />
Chronic Kidney Disease <strong>Program</strong>, York Central <strong>Hospital</strong>, Richmond Hill, ON<br />
Background: Inter-prescriber variation is one <strong>of</strong> the causes <strong>of</strong> INR<br />
fluctuations in patients on warfarin. The use <strong>of</strong> a pharmacist-driven<br />
warfarin sliding scale (WSS) has the potential to decrease inter-prescriber<br />
variation to achieve more stable INRs within the therapeutic range. This<br />
pilot study investigates the use <strong>of</strong> WSS in hemodialysis patients at a<br />
multi-site dialysis program with weekly nephrologist rotations.<br />
Methods: In this self-controlled study, 27 hemodialysis patients stable on<br />
warfarin with a target INR <strong>of</strong> 2-3 were selected to have warfarin dosed by<br />
WSS. <strong>Pharmacists</strong> designed and adjusted the WSS based on previous INR<br />
results and warfarin doses with nephrologist approval. INR results 6 weeks<br />
before and 6 weeks after the implementation <strong>of</strong> WSS were compared. The<br />
primary outcome was percentage <strong>of</strong> time with a therapeutic, sub- (INR<br />
4) INR. Secondary outcomes include<br />
bleeding or clotting events. Statistical analysis was performed with<br />
Wilcoxon Paired Signed Rank Test. A p-value <strong>of</strong>
66<br />
The use <strong>of</strong> WSS resulted in significantly more therapeutic INRs versus<br />
traditional dosing. Supra-therapeutic INRs were also reduced significantly<br />
and sub-therapeutic INRs were trending lower.<br />
Discussion: <strong>Pharmacists</strong> provided consistency in warfarin dosing via WSS<br />
by avoiding drastic changes in warfarin doses as a result <strong>of</strong> over-reaction to<br />
sub- or supra-therapeutic INRs. Nursing and physician time was saved as<br />
nurses no longer need to call physicians about patients’ INRs.<br />
Conclusions: More therapeutic INRs are achieved by pharmacists’<br />
involvement in warfarin dosing via the WSS, which has positive impact for<br />
patients, nurses and nephrologists. WSS use can be considered for other<br />
hemodialysis patients stable on warfarin.<br />
Potentially Inappropriate Medication Use In Elderly Patients<br />
Presenting to the Emergency Department<br />
Vincent Teo 1 , Patrick Edwards 2 , Minh-Hien Le 1<br />
1 Sunnybrook Health Sciences Centre, Toronto, ON<br />
2 Leslie Dan Faculty <strong>of</strong> Pharmacy, University <strong>of</strong> Toronto, ON<br />
Rationale: The Beers criteria is a list <strong>of</strong> medications considered<br />
inappropriate in elderly patients and it has been widely used to assess the<br />
safety <strong>of</strong> medications in ambulatory and nursing facilities. Currently, few<br />
studies have examined the prevalence <strong>of</strong> potential inappropriate medication<br />
use in elderly patients presenting to the emergency department (ED).<br />
Objective: To determine the incidence <strong>of</strong> potentially inappropriate<br />
medication use in elderly patients presenting to the ED at Sunnybrook<br />
Health Sciences Centre.<br />
Methods: Patients 65 years <strong>of</strong> age or older who were eligible for coverage<br />
by Ontario Drug Benefit (ODB) were included in the study. Patients were<br />
excluded if they had removed consent from the ODB drug pr<strong>of</strong>ile viewer<br />
(DPV). A current medication list for each patient was obtained from the<br />
DPV and demographic information for each patient was collected from the<br />
ED chart. Using the Beers criteria, medication lists were assessed for<br />
potentially inappropriate medications independent <strong>of</strong> a diagnosis or<br />
condition.<br />
Results: Data were collected for 60 consecutive days resulting in a total <strong>of</strong><br />
2940 patients who met the inclusion criteria. A total <strong>of</strong> 252 patients (8.6%<br />
<strong>of</strong> eligible ED visits) were found to be taking at least one potentially<br />
inappropriate medication when they presented to the ED. Nineteen patients<br />
were taking two potentially inappropriate medications and one patient was<br />
taking three. The three most frequently occurring potentially inappropriate<br />
medications were amiodarone (50 instances), followed by amitriptyline and<br />
nitr<strong>of</strong>urantoin (44 and 39 instances, respectively).<br />
Conclusion: Although this study did not determine whether the potentially<br />
inappropriate medications were the cause for a patient’s presentation to the<br />
ED, it highlights the need for increased awareness concerning safe<br />
medication prescribing practices in the elderly.<br />
Intentional Overdose <strong>of</strong> Enoxaparin<br />
Koren Lui 1,2 , Vincent Teo 3<br />
1 <strong>Canadian</strong> Forces Health Services Group<br />
2 Leslie Dan Faculty <strong>of</strong> Pharmacy, University <strong>of</strong> Toronto, Toronto, ON<br />
3 Sunnybrook Health Sciences Centre, Toronto, ON<br />
Rationale: Minimum toxic doses <strong>of</strong> low molecular weight heparins<br />
(LMWH) are not well established. Published cases <strong>of</strong> LMWH overdose have<br />
reported consumption <strong>of</strong> up to 30-times the therapeutic dose. Overdoses <strong>of</strong><br />
LMWH are rarely fatal and there are no clear guidelines pertaining to the<br />
management <strong>of</strong> acute LMWH overdoses. A case <strong>of</strong> acute intentional<br />
enoxaparin overdose is reported.<br />
Description <strong>of</strong> case: A 42 year-old male presented to the emergency room<br />
claiming he had injected himself with a 10-day supply <strong>of</strong> enoxaparin. He<br />
exhibited signs <strong>of</strong> intoxication and also complained <strong>of</strong> leg pain. The<br />
patient’s medical history included bilateral deep vein thrombosis, pulmonary<br />
embolism, hepatitis B, cholecystitis, ethanol abuse, and suspected<br />
tetrahydrocannabinol (THC) use. His medications prior to admission<br />
consisted <strong>of</strong> enoxaparin 100mg subcutaneous injection daily. On<br />
examination, it was noted that the patient lacked motor coordination.<br />
There were no signs <strong>of</strong> bleeding. His INR (1.23) and aPTT (97.1 s) were<br />
elevated. Poison control was contacted and suggested hourly monitoring <strong>of</strong><br />
aPTT, INR, and vital signs until the patient’s INR and aPTT normalized.<br />
Assessment <strong>of</strong> Causality: Temporal relationship suggests that the<br />
elevated INR and aPTT were the result <strong>of</strong> acute LMWH overdose.<br />
Evaluation <strong>of</strong> Literature: At time <strong>of</strong> writing, three published case reports<br />
<strong>of</strong> acute intentional LMWH overdose were found. In all cases, the patients<br />
did not experience bleeding. The aPTT’s were monitored until normalized. A<br />
published analysis <strong>of</strong> available case reports suggested that management by<br />
observation is appropriate.<br />
Importance <strong>of</strong> Case to Pharmacy Practitioners: There are available<br />
antidotes for the anticoagulant activity <strong>of</strong> LMWH. However, a more<br />
appropriate course <strong>of</strong> action may be to observe and monitor for signs <strong>of</strong><br />
bleeding until the aPTT is normalized. It is not necessary to treat with<br />
protamine or factor VIIa unless there is an active bleed in the setting <strong>of</strong><br />
LMWH overdose.<br />
2 CSHP<br />
Targeting Excellence<br />
Implementation <strong>of</strong> a Pharmacy Residency <strong>Program</strong><br />
in Primary Care<br />
in Pharmacy Practice<br />
Kwan, Debbie 1,2 ; Cameron, Karen 1,2 ; Marr, Patricia 1,2 ;<br />
Papoushek, Christine 1,2 ; Siu, Victoria 1,2<br />
1 University Health Network, Department <strong>of</strong> Pharmacy, Toronto, ON<br />
2 Leslie Dan Faculty <strong>of</strong> Pharmacy, University <strong>of</strong> Toronto, ON<br />
Rationale: Integration <strong>of</strong> pharmacists into primary care has been identified<br />
as a priority for primary health care reform in Canada. However, little exists<br />
by way <strong>of</strong> formal training to prepare pharmacists for this role.<br />
Description: The Toronto Western <strong>Hospital</strong> Academic Family Health Team<br />
(FHT) serves approximately 14,000 patients in downtown west Toronto. In<br />
2008, the FHT launched Canada’s first Pharmacy Residency <strong>Program</strong> in<br />
Primary Care. The goal <strong>of</strong> the program is to provide practice-based,<br />
experiential learning to prepare residents to develop expertise and<br />
successful careers as pharmacists in primary care. The resident works with<br />
patients and in collaboration with members <strong>of</strong> the inter-pr<strong>of</strong>essional team.<br />
Required and ambulatory-based elective rotations are completed<br />
longitudinally. The resident is also required to complete a primary care<br />
focused research project, teach health pr<strong>of</strong>essional students and give<br />
academic presentations.<br />
Implementation: The application process for this residency program was<br />
linked to the same application process for hospital pharmacy residency<br />
programs in Ontario and was open to graduates <strong>of</strong> post-baccalaureate<br />
pharmacy programs. As such, the application and interview process<br />
commenced in the fall <strong>of</strong> 2007 and the first resident was accepted into the<br />
program starting July 2008.<br />
Evaluation: Two candidates have successfully completed the program. One<br />
graduate continues to work in the Toronto Western FHT. The number <strong>of</strong><br />
applications to the program has risen yearly indicating an ongoing demand<br />
for such a program.<br />
Importance: As the pharmacist’s role in primary care continues to grow,<br />
training for practitioners in this unique practice area will continue to be<br />
required. In addition, the implementation <strong>of</strong> new residency programs helps<br />
to fill the increasing demand for pharmacy residency training in Canada.<br />
Differences in Nova Scotian <strong>Pharmacists</strong>’ Experiences and<br />
Barriers to Providing the Emergency Contraceptive Pill Based<br />
on Primary Practice Site<br />
Anne Marie Whelan 1 , Donald Langille 2 , Eileen Hurst 1,2<br />
1 College <strong>of</strong> Pharmacy Dalhousie University, Halifax, Nova Scotia<br />
2 Department <strong>of</strong> Community Health & Epidemiology, Dalhousie University,<br />
Halifax, NS
67<br />
Rationale: There is little in the literature about differences between<br />
pharmacists whose primary place <strong>of</strong> practice is hospital versus community,<br />
pertaining to their experiences and barriers to providing the emergency<br />
contraceptive pill (ECP).<br />
Objectives: In 2005 ECP became more accessible to women in Canada<br />
when the regulatory status <strong>of</strong> levonorgestrel changed from Schedule I to<br />
Schedule II (available without a prescription in pharmacies following a<br />
consultation with a pharmacist). The objective <strong>of</strong> this study was to examine<br />
if there is a difference between primarily hospital based versus community<br />
based pharmacists’ experiences providing ECPs.<br />
Study Design and Methods: All pharmacists licensed to practice in Nova<br />
Scotia were invited to anonymously complete a 25 item paper<br />
questionnaire sent in the mail. The research was approved by Dalhousie<br />
University Health Sciences Ethics Board. Descriptive statistics were<br />
generated using SPSS.<br />
Results: The response rate was 53% (595/1123) with 415 pharmacists<br />
indicating that they had previously provided nonprescription ECP in<br />
community pharmacy and their primary place <strong>of</strong> practice was either<br />
hospital or community (13 hospital, 402 community). In comparing their<br />
experiences providing ECP, 38.7% <strong>of</strong> hospital pharmacists indicated they<br />
spent 11minutes or longer providing consults while only17.4% <strong>of</strong><br />
community pharmacists spent this much time. With regard to barriers to<br />
ECP provision, more hospital pharmacists than community pharmacists<br />
reported the following as barriers: 1) lack <strong>of</strong> privacy (61.6% vs. 46.0%), 2)<br />
lack <strong>of</strong> staffing (76.9% vs. 49.6%), and 3) length <strong>of</strong> consultation (46.2%<br />
vs. 28.0%).<br />
Conclusion: Results from this survey suggest that there may be some<br />
differences in the experiences between hospital and community based<br />
pharmacists providing ECP which should be explored further. Regardless <strong>of</strong><br />
primary practice site, results indicate that there are some barriers to ECP<br />
provision that should be addressed when considering providing this type <strong>of</strong><br />
consultation in a community pharmacy.<br />
Chemotherapy-Induced Nausea and Vomiting in Children<br />
Receiving Ifosfamide Plus Etoposide: Preliminary Results<br />
S.R. Lavoratore, C. Lui, M. Linseman, A.M. Maloney, P.C. Nathan, T. Taylor,<br />
E. Zelunka, L.L. Dupuis, The <strong>Hospital</strong> for Sick Children, Toronto, Ontario;<br />
Leslie Dan Faculty <strong>of</strong> Pharmacy, University <strong>of</strong> Toronto, Toronto, ON<br />
Rationale: Adult evidence is commonly used to determine the<br />
emetogenicity <strong>of</strong> chemotherapeutic agents in children and informs the<br />
selection <strong>of</strong> nausea and vomiting prophylaxis. This approach may be<br />
inaccurate in children. Pediatric information regarding the emetogenic<br />
potential <strong>of</strong> ifosfamide plus etoposide, a combination which in adults is<br />
deemed to be moderately emetogenic, is lacking.<br />
Objective: To describe chemotherapy-induced nausea and vomiting (CINV)<br />
in the acute and delayed phases in children receiving ifosfamide<br />
1800mg/m2/day plus etoposide 100mg/m2/day for 5 days.<br />
Study Design and Methods: A diary was used by children to record<br />
episodes <strong>of</strong> vomiting and retching, nausea severity and antiemetic agents<br />
administered during acute and delayed phases. Patients themselves<br />
reported nausea severity a minimum <strong>of</strong> twice daily using a validated<br />
pediatric nausea assessment instrument. During the phase <strong>of</strong> interest,<br />
complete CINV control was defined as no emetic episodes (no vomiting or<br />
retching) and a maximum nausea score <strong>of</strong> 1 (none) out <strong>of</strong> 4. Patients<br />
received antiemetic agents as prescribed by the clinical team.<br />
Results: 10 patients (median age: 10.1yrs; range: 5-17yrs) participated. No<br />
patient was chemotherapy-naïve. Three had a history <strong>of</strong> motion sickness<br />
and 2 experienced anticipatory CINV. All patients received ondansetron<br />
during the acute phase; 9 also received dexamethasone. Four patients<br />
experienced complete acute phase CINV control. Six patients received<br />
ondansetron during the delayed phase while 2 also received<br />
dexamethasone. Six patients experienced complete CINV control during the<br />
delayed phase.<br />
Conclusions: Preliminary findings suggest that ifosfamide plus etoposide is<br />
highly emetogenic in children. Interventions aimed at improving CINV<br />
control in both the acute and delayed phases should be investigated. Study<br />
findings are limited by small sample size.<br />
Improving a Complex Pharmacist Scheduling Model at a<br />
Tertiary Care <strong>Hospital</strong><br />
Daniel Cortes, Kevin Curley, Jodie Leung, Jenny Lieu, St. Michael’s <strong>Hospital</strong>,<br />
Toronto, ON<br />
Rationale: Pharmacist scheduling has undergone increased strain and<br />
demand amidst recent medication system changes such as a computerized<br />
physician order entry system and expansion to 24-hour pharmacy<br />
operations. In this new environment, the complexities <strong>of</strong> scheduling for 25<br />
pharmacists necessitated the development <strong>of</strong> a new scheduling model that<br />
would decrease workload for schedulers, while meeting the needs <strong>of</strong><br />
individual pharmacists.<br />
Description: A literature review on MEDLINE and CINHAL provided<br />
guidance based on nursing scheduling models. A hybrid model <strong>of</strong><br />
self-scheduling and set-scheduling was identified, that allows for autonomy,<br />
flexibility, fairness and transparency for pharmacists and decreased<br />
workload for schedulers.<br />
An Excel-based scheduling tool was developed that allows pharmacists’<br />
availability based on cross-coverage responsibilities, vacations, teaching and<br />
pr<strong>of</strong>essional development responsibilities to be entered. This data can then<br />
be used to ensure all assigned shifts are covered, shifts are equally<br />
distributed and that each pharmacist meets their quota <strong>of</strong> required shifts.<br />
Evaluation: Post-implementation, pharmacists were surveyed to assess if<br />
the new model met their needs based on customizability, flexibility, fairness,<br />
transparency and effort required. A total <strong>of</strong> 23 pharmacists responded and<br />
the ratings for the new model met or exceeded ratings for the prior model<br />
in all categories. Overall, 21 <strong>of</strong> the pharmacists (92% <strong>of</strong> respondents)<br />
reported being somewhat or very satisfied with the new model. In contrast,<br />
70% <strong>of</strong> eligible respondents were dissatisfied with the previous scheduling<br />
model. Schedulers found a reduced administrative burden for filling vacant<br />
shifts and decreased time needed to create the schedule.<br />
Importance: The new scheduling model provides decreased workload for<br />
schedulers while meeting individual clinical pharmacists’ needs.<br />
Statin Treatment use in Diabetics with Breast Cancer: A<br />
Potential C-Reactive Protein Mediated Benefit<br />
A.C. Ceacareanu, C. C. Hong, J.J. Brennan III, M. Epstein, E. Koss<strong>of</strong>f, G.K.<br />
Nimako, K. Patel, A. Forrest; School <strong>of</strong> Pharmacy and Pharmaceutical<br />
Sciences, State University <strong>of</strong> New York, Buffalo, NY, NYS Center <strong>of</strong><br />
Excellence, Buffalo, NY, Roswell Park Cancer Institute, Buffalo, NY<br />
Background: Statin treatment has not yet been evaluated in relation to<br />
breast cancer (BC) prognosis in diabetes mellitus (DM) patients. Reported<br />
decreased survival following BC in women with metabolic syndrome, led us<br />
to investigate whether specific statin therapy may lead to improved BC<br />
survival. Reported associations between elevated C-reactive protein (CRP)<br />
levels at the time <strong>of</strong> diagnosis with worse cancer prognosis, and<br />
CRP-lowering properties <strong>of</strong> statin treatment in non-cancer patients, led us<br />
to investigate whether statin use is associated with lower CRP levels at the<br />
time <strong>of</strong> BC diagnosis and with improved BC outcomes.<br />
Methods: All DM patients newly diagnosed with BC between 2003 and<br />
2007 (Roswell Park Cancer Institute) were retrospectively reviewed (n =<br />
225). BC pathology, outcomes, existing comorbidities and drug therapy<br />
were documented. Follow up began at BC diagnosis and ended with first<br />
confirmed recurrence and/or death, or last date <strong>of</strong> follow-up. Hazard ratios<br />
(HR) and 95% confidence intervals (CI)s representing the association<br />
between statins, BC and a defined event were computed with Cox<br />
proportional hazards model. CRP plasma levels were determined by<br />
enzyme-linked immunosorbent assay in specimens donated at the time <strong>of</strong><br />
BC diagnosis. A total <strong>of</strong> 98 study patients, DM+BC, and their matched<br />
controls, BC only (n = 196) were analyzed.
68<br />
Results: After a median follow up <strong>of</strong> 30 months, patients receiving statins<br />
for cholesterol management were found to have better disease-free survival<br />
(HR 0.27, 95% CI: 0.10, 0.71, X2 = 7.31, p = 0.06), and lower overall<br />
mortality (HR 0.23, 95% CI: 0.08, 0.66, X2 = 7.80, p = 0.05) compared to<br />
patients not receiving any cholesterol management medication. CRP levels<br />
have ranged between 0.2 and 21 mg/L and clinically relevant levels (><br />
3mg/L) were noted in the study group.<br />
Conclusions: This study explored for the first time the association between<br />
statin therapy and BC prognosis in DM. We observed improved outcomes in<br />
statin-treated patients. While we currently analyze statin therapy in<br />
relationship with baseline CRP levels and BC prognosis, our existing findings<br />
suggest that statins have the potential to improve BC outcomes potentially<br />
through lowering overall inflammation.<br />
Poster Abstract Reviewers<br />
Réviseurs des présentations par affiches<br />
Sincere appreciation is extended to the abstract reviewers for PPC 2012.<br />
Educational Services Committee<br />
Roxane Carr<br />
Allison Callaghan<br />
Olavo Fernandes<br />
Alfred Gin<br />
Colette Raymond<br />
Kat Timberlake<br />
Erica Wang<br />
Research Committee<br />
David Blackburn<br />
Roxane Carr<br />
Dawn Dalen<br />
Scott Edwards<br />
Janice Irvine-Meek<br />
Salmaan Kanji<br />
Sheri Koshman<br />
Marc Perreault<br />
Kerry Wilbur<br />
Adjudicators<br />
Margaret Ackman<br />
Clarence Chant<br />
Peter Zed
69<br />
CSHP New Fellows<br />
Nouveaux associés de la SCPH<br />
CSHP Fellow status is conferred by the Board <strong>of</strong> Fellows upon CSHP<br />
members who have demonstrated noteworthy, sustained service<br />
and excellence in the practice <strong>of</strong> pharmacy in an organized<br />
healthcare setting.<br />
Board <strong>of</strong> Fellows 2011-2012<br />
Conseil des associés 2011-2012<br />
Chairperson<br />
Président:<br />
Jim Mann, FCSHP<br />
Chair-Elect:<br />
Président désigné<br />
Peter Loewen, FCSHP<br />
Past Chair<br />
Président sortant:<br />
Peter Zed, FCSHP<br />
Board Members<br />
Membres du Conseil:<br />
Shallen Letwin, FCSHP<br />
Glen Pearson, FCSHP<br />
Kris Wickman, FCSHP<br />
Rita Dhami (ex-<strong>of</strong>ficio<br />
member)<br />
Carole Chambers, BScPhm, MBA, FCSHP<br />
Carole Chambers holds both a Bachelor <strong>of</strong><br />
Science in Pharmacy and a Masters in Business<br />
Administration, and is the Director <strong>of</strong><br />
Pharmacy, Cancer Services with the Alberta<br />
Health Services in Alberta Canada.<br />
Carole has cross appointments in the two<br />
Universities in Alberta. Practicing for over 30<br />
years she has many peer reviewed<br />
publications. She is the immediate Past President <strong>of</strong> the<br />
International <strong>Society</strong> <strong>of</strong> Oncology Pharmacy and has recently<br />
served on an international advisory panel for the creation <strong>of</strong> a<br />
Medication Safety Self-Assessment tool in Oncology.<br />
Kevin W. Hall, BScPhm, PharmD, FCSHP<br />
Kevin obtained his B. Sc. Pharm. From<br />
Dalhousie University in 1976 and his Pharm.<br />
D. from the State University <strong>of</strong> New York at<br />
Buffalo in 1978. He subsequently joined the<br />
staff <strong>of</strong> the Winnipeg Health Sciences Centre<br />
as a critical care clinical pharmacist<br />
(1978-1986), and later held positions as<br />
Coordinator <strong>of</strong> Critical Care Pharmacy Services<br />
(1981 to 1986), Assistant Director <strong>of</strong> Pharmacy (1986-1991) and<br />
Director <strong>of</strong> Pharmacy (1991 to 1998). In 1998 he became the<br />
Director <strong>of</strong> Pharmacy for the Winnipeg Regional Health Authority<br />
(WRHA), with responsibility for managing pharmacy services at 8<br />
Winnipeg hospitals. In 2010, Kevin accepted a position as a Clinical<br />
Associate Pr<strong>of</strong>essor in the Faculty <strong>of</strong> Pharmacy and Pharmaceutical<br />
Sciences at the University <strong>of</strong> Alberta, where he teaches courses on<br />
pharmacy management and the <strong>Canadian</strong> health care system. He is<br />
currently involved in a research initiative that is studying the impact<br />
that the “mindset” <strong>of</strong> pharmacy practitioners and the “culture” <strong>of</strong><br />
the pharmacy pr<strong>of</strong>ession has on the adoption <strong>of</strong> new pharmacy<br />
practice models, such as those being pursued through the<br />
Blueprint for Pharmacy initiative.<br />
Kevin has been active in a number <strong>of</strong> pharmacy organizations and<br />
has served as President <strong>of</strong> both the <strong>Canadian</strong> <strong>Society</strong> <strong>of</strong> <strong>Hospital</strong><br />
<strong>Pharmacists</strong> and the <strong>Canadian</strong> <strong>Pharmacists</strong> Association. Other<br />
appointments that he has held include serving as Co-chair <strong>of</strong> the<br />
Steering Committee for “Moving Forward: Pharmacy Human<br />
Resources for the Future”, a $1.5 million national study <strong>of</strong><br />
pharmacy manpower issues; serving as a member <strong>of</strong> the Human<br />
Resources Sub-group for the development <strong>of</strong> the Blueprint for<br />
Pharmacy’s implementation plan; serving as a member <strong>of</strong> the<br />
National Advisory Committee for the development <strong>of</strong> the <strong>Canadian</strong><br />
Medication Incident Reporting System (CMIRPS); and serving two<br />
terms as Chair <strong>of</strong> the CSHP Research and Education Foundation.<br />
Since the early 1990s Kevin has been an Editor, and currently<br />
serves as one <strong>of</strong> the two Managing Editors, for the <strong>Hospital</strong><br />
Pharmacy in Canada Survey and Report, which biannually collects<br />
and publishes comprehensive data on the state <strong>of</strong> hospital<br />
pharmacy practice in Canada. He also currently serves as an<br />
Associate Editor for the <strong>Canadian</strong> Journal <strong>of</strong> <strong>Hospital</strong> Pharmacy.<br />
During his career to date Kevin has authored or co-authored 34<br />
peer-reviewed papers and has given over 60 invited presentations<br />
at national, regional and provincial conferences across Canada.<br />
Derek Jorgenson, BSP, PharmD, FCSHP<br />
Derek Jorgenson received his Bachelor <strong>of</strong><br />
Pharmacy Degree from the University <strong>of</strong><br />
Saskatchewan and his Doctor <strong>of</strong> Pharmacy<br />
Degree from the University <strong>of</strong> Toronto.<br />
His practice experience includes positions in<br />
Manitoba, Ontario and Saskatchewan where<br />
he has worked as a community pharmacist, a<br />
researcher for the Saskatchewan Health<br />
Quality Council and as a clinical pharmacist / practice leader in a<br />
large variety <strong>of</strong> hospital based ambulatory clinics.<br />
Derek was recently honoured for his service to the pr<strong>of</strong>ession by<br />
being awarded the <strong>Canadian</strong> Pharmacist <strong>of</strong> the Year in 2010 by the<br />
<strong>Canadian</strong> <strong>Pharmacists</strong> Association.<br />
Derek is currently an Assistant Pr<strong>of</strong>essor <strong>of</strong> Pharmacy at the<br />
University <strong>of</strong> Saskatchewan and a clinical pharmacist in an<br />
interpr<strong>of</strong>essional primary care clinic in Saskatoon.<br />
Zahra Kanji, BScPhm, ACPR, PharmD, FCSHP<br />
Zahra Kanji received her Bachelor <strong>of</strong> Science in<br />
Pharmacy degree at the University <strong>of</strong> British<br />
Columbia (UBC) in 1995, completed a hospital<br />
pharmacy residency at the Children’s and<br />
Women’s Health Centre <strong>of</strong> British Columbia in<br />
1996 and graduated with a Doctor <strong>of</strong><br />
Pharmacy (PharmD) degree from UBC in 1998.
70<br />
Since completing her PharmD, Zahra has been working as a Clinical<br />
Pharmacy Specialist in Critical Care at Lions Gate <strong>Hospital</strong> and has<br />
held the positions <strong>of</strong> Residency Coordinator and Education<br />
Coordinator. Zahra is also a Clinical Pr<strong>of</strong>essor with the Faculty <strong>of</strong><br />
Pharmaceutical Sciences at UBC.<br />
She has led and participated in numerous initiatives within the<br />
Intensive Care Unit (ICU) to improve patient care and patient safety<br />
<strong>of</strong> the critically ill population and has been involved in similar<br />
initiatives hospital wide. Zahra has also served on a number <strong>of</strong><br />
institutional and regional committees, most recently including the<br />
Antimicrobial Stewardship Working Group for Lower Mainland<br />
Pharmacy Services.<br />
Zahra has been actively involved in teaching, precepting, and<br />
mentoring undergraduate pharmacy students, pharmacy residents,<br />
PharmD students and clinical pharmacists. She has precepted over<br />
30 Pharmacy residents and PharmD students for clinical critical care<br />
rotations. Zahra has also been serving as a member the Regional<br />
Residency Advisory Council for a number <strong>of</strong> years.<br />
Zahra has been extensively involved in clinical research and<br />
published numerous articles in a variety <strong>of</strong> different areas. She<br />
received the National CSHP/Glaxo Smith Kline Award in<br />
Pharmaceutical Care in 2004. She has served on research review<br />
committees both institutionally and within the community.<br />
Zahra has been involved with CSHP in a number <strong>of</strong> roles, including<br />
leadership positions. She has just completed her term as President<br />
<strong>of</strong> CSHP BC Branch and is now serving as Past President. She held<br />
the position <strong>of</strong> Communications Officer with CSHP BC Branch for<br />
two years prior to this and was instrumental in making the Branch’s<br />
website an effective communication tool for members. She served<br />
on the <strong>Canadian</strong> <strong>Hospital</strong> Pharmacy Residency Board (CHPRB) for<br />
six years from 2005-2010 during which a major revision <strong>of</strong> the<br />
Accreditation Standards, by which pharmacy practice residency<br />
programs are accredited, were developed and implemented. In<br />
addition, Zahra has served as an appraiser <strong>of</strong> the CSHP awards<br />
programs both nationally and provincially for many years and is<br />
also a reviewer with <strong>Canadian</strong> Journal <strong>of</strong> <strong>Hospital</strong> Pharmacy.<br />
Zahra is honored to receive Fellow status and would like to thank<br />
her family, friends, and colleagues for their continued support. She<br />
would like to especially acknowledge her husband, Anil, for his<br />
support and their children, Noah and Jenna, for the immense joy<br />
that they bring to her life.<br />
Brenda G. Schuster, BSP, ACPR, PharmD, FCSHP<br />
Brenda Schuster received her Bachelor <strong>of</strong><br />
Science in Pharmacy degree at the University<br />
<strong>of</strong> Saskatchewan in 1986 and completed a<br />
hospital pharmacy residency at the Regina<br />
General <strong>Hospital</strong> in 1987. Following her<br />
residency she worked at St. Paul’s <strong>Hospital</strong> in<br />
Vancouver as a Clinical Pharmacist on the<br />
internal medicine ward until 1993. From<br />
1994-1996 she had a leadership position as Pharmaceutical Care<br />
Coordinator with the Saskatchewan College <strong>of</strong> <strong>Pharmacists</strong><br />
assisting pharmacists to implement pharmaceutical care into their<br />
practice. This included assisting with the several implementation <strong>of</strong><br />
several pilot projects, and the development and implementation <strong>of</strong><br />
the Trial Prescription <strong>Program</strong>.<br />
In 1996-98 she attended the University <strong>of</strong> Toronto where she<br />
completed her Doctor <strong>of</strong> Pharmacy Degree. From1998-2010 she<br />
provided pharmacy services on internal medicine and family<br />
practice with the Regina Qu’Appelle Health Region Pharmacy<br />
Department. During this time she worked as the Pharmacy<br />
Educator/Pharmacist Development Specialist mentoring many<br />
pharmacists, residents and students. She developed the Pharmacist<br />
Orientation <strong>Program</strong>, Pharmacist Educational Development<br />
<strong>Program</strong> and the Preceptor Development <strong>Program</strong>. She was also<br />
involved in the development <strong>of</strong> the Anemia Management<br />
Certification program and with updates/reviews <strong>of</strong> the residency<br />
program.<br />
Over the last 12 years her passion for promoting excellence in drug<br />
therapy is demonstrated with her with the RxFiles Academic<br />
Detailing <strong>Program</strong>. This work complements her most recent clinical<br />
practice in the Academic Family Medicine Unit which includes<br />
patient care responsibilities, teaching medical residents and<br />
students in the College <strong>of</strong> Medicine. Brenda has demonstrated<br />
leadership in her commitment to evidence based educational<br />
programming through her numerous provincial and national<br />
presentations to both pharmacists and physicians. She teaches with<br />
the College <strong>of</strong> Pharmacy and Nutrition, University <strong>of</strong> Saskatchewan<br />
in her specialty interest <strong>of</strong> gastroenterology.<br />
Throughout her career, Brenda has demonstrated significant<br />
involvement and leadership in CSHP and many other organizations.<br />
She has held presidential roles with both Saskatchewan College <strong>of</strong><br />
<strong>Pharmacists</strong> and the Saskatchewan branch <strong>of</strong> CSHP. Other activities<br />
include work for the CSHP National Educational Services<br />
Committee, Pharmacy Examining Board <strong>of</strong> Canada, advisory<br />
committees <strong>of</strong> NAPRA, CADTH, <strong>Canadian</strong> Patient Safety and the<br />
Pharmacy Human Resources Study. Local involvement included the<br />
RQHR Antimicrobial Utilization Committee and Saskatchewan<br />
Continuing Medication Education conference planning<br />
committees.<br />
Brenda strives for innovation in teaching and clinical practice. This<br />
has been recognized by the Saskatchewan Branch CSHP<br />
<strong>Pharmacists</strong> <strong>of</strong> the Year Award, & JL Summers Achievement Award.<br />
Her contribution as a teacher was acknowledged through the work<br />
<strong>of</strong> the RxFiles Academic Detailing <strong>Program</strong> being awarded the<br />
2010 Dr. Michael Krochak Award in recognition <strong>of</strong> significant<br />
contributions to Family Medicine in Saskatchewan and the program<br />
receiving Teacher <strong>of</strong> the Year Award from the College <strong>of</strong> Medicine<br />
Continuing Pr<strong>of</strong>essional Learning. She has received presentation<br />
awards from CCCP and the University <strong>of</strong> Toronto Doctor <strong>of</strong><br />
Pharmacy program. She has published on several topics, and was<br />
awarded a CSHP national award for her coauthoring <strong>of</strong> a “Critical<br />
Analysis <strong>of</strong> the Pharmaceutical Care Research Literature”.<br />
Brenda and her husband Rob enjoy travelling, biking, cooking and<br />
time at their cabin.
71<br />
Rosemary Zvonar, BScPhm, FCSHP<br />
Rosemary obtained her Bachelor <strong>of</strong> Science in<br />
Pharmacy degree from the University <strong>of</strong><br />
Toronto, and the following year completed the<br />
<strong>Hospital</strong> Pharmacy Residency <strong>Program</strong> at the<br />
Ottawa Civic <strong>Hospital</strong>. Rosemary remained on<br />
staff at The Ottawa <strong>Hospital</strong>, working in a<br />
number <strong>of</strong> different areas including Drug<br />
Information, and Internal Medicine. Prior to<br />
her current position, Rosemary was a clinical pharmacist in the<br />
Intensive Care Unit at the Civic Campus.<br />
In 2002, Rosemary was the successful candidate for the new<br />
corporate position <strong>of</strong> Antimicrobial Pharmacy Specialist at The<br />
Ottawa <strong>Hospital</strong>.<br />
She developed this new role, and was responsible for creating<br />
institutional guidelines, protocols, and tools in conjunction with the<br />
Division <strong>of</strong> Infectious Diseases to improve anti-infective use within<br />
the hospital. Rosemary implemented antibiotic use monitoring<br />
strategies, established two new institutional policies and<br />
procedures, and has been involved in various research projects. She<br />
also played a key role in launching a formal Antimicrobial<br />
Stewardship program at the hospital in 2011.<br />
Rosemary has devoted substantial effort in providing education in<br />
antimicrobial use and infectious disease. Within the hospital,<br />
Rosemary precepts all five pharmacy residents each year for their<br />
Infectious Diseases rotation and is a frequent preceptor for<br />
residents’ research projects. She regularly presents to the<br />
pharmacists and teaches medical and surgical housestaff. In<br />
addition, Rosemary lectures for the School <strong>of</strong> Nursing and Faculty<br />
<strong>of</strong> Medicine at the University <strong>of</strong> Ottawa. Over the years, Rosemary<br />
has been invited to speak at various conferences and courses, with<br />
over 30 oral presentations given locally and nationally.<br />
Rosemary has been actively involved in CSHP, including as a<br />
longstanding member <strong>of</strong> the National Awards Committee, and<br />
previous Education Coordinator for the ID-PSN. Additional activities<br />
include being a regular reviewer in the area <strong>of</strong> Infectious Disease<br />
for a number <strong>of</strong> pharmacy journals, and participating in various<br />
hospital committees.
72<br />
Faculty<br />
Conférenciers<br />
CSHP would like to recognize the<br />
generous contributions <strong>of</strong> the<br />
following speakers:<br />
La SCPH désire souligner les<br />
généreuses contributions des<br />
conférenciers suivants:<br />
Shirin Abadi<br />
BScPhm, ACPR, PharmD<br />
BC Cancer Agency<br />
Vancouver, BC<br />
Anna Banerji<br />
MD, MPH, FRCPC, DTM&H<br />
St. Michael’s <strong>Hospital</strong><br />
Toronto, ON<br />
Chaim Bell<br />
MD, PhD, FRCPC<br />
Li Ka Shing Knowledge Institute<br />
St. Michael’s <strong>Hospital</strong><br />
Toronto, ON<br />
Roberta Bondar<br />
OCO Ont, MD, PhD, FRCP, FRSC<br />
Consultant, Physician, Scientist,<br />
Author, Photographer, Educator<br />
Carolyn Bornstein<br />
BScPhm, FCSHP<br />
CSHP 2015<br />
Newmarket, ON<br />
Cynthia Brocklebank<br />
BScPhm, PharmD, ACPR<br />
Alberta Health Services<br />
Calgary, AB<br />
Jean-François Bussières<br />
BPharm, MSc, MBA, FCSHP<br />
CHU Sainte-Justine<br />
Montréal, QC<br />
Judy Chong - Moderator<br />
BScPhm, RPh<br />
Royal Victoria <strong>Hospital</strong> <strong>of</strong> Barrie<br />
Barrie, ON<br />
Marlys Christianson<br />
MD, PhD<br />
Rotman School <strong>of</strong> Management<br />
University <strong>of</strong> Toronto<br />
Toronto, ON<br />
Naomi Dore<br />
BScH, MSc, BScPhm<br />
Hamilton Health Sciences Centre<br />
Hamilton, ON<br />
Anar Dossa<br />
BScPhm, PharmD, CDE<br />
Vancouver General <strong>Hospital</strong><br />
Vancouver, BC<br />
Linda Dresser<br />
BScPhm, PharmD, FCSHP<br />
University Health Network<br />
Toronto General <strong>Hospital</strong><br />
Toronto, ON<br />
Lee Dupuis<br />
RPh, ACPR, MScPhm, FCSHP<br />
The <strong>Hospital</strong> for Sick Children<br />
Toronto, ON<br />
Barbara Farrell<br />
BScPhm, PharmD, FCSHP<br />
Bruyère Continuing Care<br />
Ottawa, ON<br />
Olavo Fernandes<br />
BScPhm, PharmD, FCSHP<br />
Leslie Dan Faculty <strong>of</strong> Pharmacy<br />
University <strong>of</strong> Toronto<br />
Toronto, ON<br />
Joanne Garrah<br />
Health Canada<br />
Ottawa, ON<br />
Julie Greenall<br />
RPh, BScPhm, MHSc<br />
ISMP Canada<br />
Toronto, ON<br />
Kevin Hall<br />
BScPhm, PharmD, FCSHP<br />
Faculty <strong>of</strong> Pharmacy Pharmaceutical<br />
Sciences, University <strong>of</strong> Alberta<br />
Edmonton, AB<br />
Anne Hiltz<br />
BScPhm, ACPR, RPh<br />
Capital District Health Authority<br />
Halifax, NS<br />
Derek Jorgenson<br />
BSP, PharmD<br />
University <strong>of</strong> Saskatchewan<br />
Saskatoon, SK<br />
David Juurlink<br />
BScPhm, MD, PhD, FRCPC<br />
Sunnybrook Health Sciences Centre<br />
Institute for Clinical Evaluative<br />
Sciences<br />
Toronto, ON<br />
Salmaan Kanji<br />
BScPhm, PharmD<br />
The Ottawa <strong>Hospital</strong><br />
General Campus<br />
Ottawa, ON<br />
Debra Kent<br />
PharmD, DABAT<br />
CSPI andBC Centre for Disease<br />
Control, Provincial Health Services<br />
Authority<br />
BC Drug & Poison Information<br />
Centre<br />
Vancouver, BC<br />
Heather Kertland<br />
BScPhm, PharmD<br />
St. Michael’s <strong>Hospital</strong><br />
Toronto, ON<br />
Matt Koehler<br />
BScPhm<br />
Shoppers Drug Mart<br />
Thunder Bay, ON<br />
Debbie Kwan<br />
BScPhm, MSc, FCSHP<br />
Toronto Western <strong>Hospital</strong><br />
Family Health Team<br />
Toronto, ON<br />
Tim Lau<br />
PharmD, FCSHP<br />
Vancouver General <strong>Hospital</strong><br />
Vancouver Coastal Health<br />
Vancouver, BC<br />
Jaclyn Litynsky<br />
BCPS, PharmD<br />
Toronto East General <strong>Hospital</strong><br />
Toronto, ON<br />
Peter Loewen<br />
BScPhm, ACPR, PharmD, RPh,<br />
FCSHP<br />
Provincial Health Services Authority<br />
University <strong>of</strong> British Columbia<br />
Vancouver, BC<br />
Anke-Hilse Maitland-van der Zee<br />
PharmD, PhD<br />
Utrecht University<br />
Utrecht, The Netherlands<br />
Ryan McGuire<br />
BScPhm<br />
University <strong>of</strong> Toronto<br />
Toronto, ON<br />
Emily Muir<br />
BScPhm, ACPR<br />
Horizon Health Network<br />
Saint John, NB<br />
Janice Munroe - Moderator<br />
BScPhm<br />
Fraser Health Pharmacy Services<br />
Regional Pharmacy Administration<br />
Langley, BC<br />
Tania Mysak<br />
BSP, PharmD<br />
Alberta Health Services<br />
Edmonton, AB<br />
Glen Pearson<br />
BScPhm, PharmD, FCSHP<br />
Division <strong>of</strong> Cardiology, University <strong>of</strong><br />
Alberta<br />
Manzankowski Alberta Heart<br />
Institute<br />
Edmonton, AB<br />
Jennifer Pickering<br />
BScPhm, ACPR<br />
Hamilton Health Sciences Centre<br />
Hamilton, ON<br />
Monique Pitre<br />
BScPhm, FCSHP<br />
University Health Network<br />
Toronto, ON<br />
Kevin Pottie<br />
MD, CCFP, MCISc, FCFP<br />
University <strong>of</strong> Ottawa<br />
Elisabeth Bruyère Research Institute<br />
Pegi Rappaport<br />
BSc, MSc<br />
Toronto East General <strong>Hospital</strong><br />
Toronto, ON<br />
Vijay Rasaiah<br />
RPh, BScPhm, MSc, BSc (Hon)<br />
The <strong>Hospital</strong> for Sick Children<br />
Toronto, ON<br />
Carlos Rojas-Fernandez<br />
BScPhm, PharmD<br />
Schlegel-UW Research Institute on<br />
Ageing & School <strong>of</strong> Pharmacy,<br />
University <strong>of</strong> Waterloo<br />
Kitchener, ON<br />
Diana Sarakbi<br />
Accreditation Canada<br />
Ottawa, ON<br />
Lisa Sever<br />
BScPhm<br />
York Central <strong>Hospital</strong><br />
Richmond Hill, ON<br />
Stephen Shalansky<br />
BScPhm, PharmD, ACPR, FCSHP<br />
Providence Healthcare<br />
Vancouver, BC<br />
Richard Slavik<br />
PharmD, FCSHP<br />
Pr<strong>of</strong>essional Practice Interior<br />
Health, University <strong>of</strong> British<br />
Columbia<br />
Kelowna, BC<br />
Miranda So<br />
BSc, BScPhm, PharmD<br />
University Health Network<br />
Toronto, ON<br />
Amy Sood<br />
BScPhm, PharmD<br />
Manitoba Renal <strong>Program</strong>/St.<br />
Boniface <strong>Hospital</strong><br />
Winnipeg, MB<br />
Sean Spina<br />
BScPhm, ACPR, PharmD<br />
Vancouver Island Health Authority<br />
Victoria, BC<br />
James E. Tisdale<br />
BScPhm, PharmD, BCPS, FCCP,<br />
FAPhA, FAHA<br />
College <strong>of</strong> Pharmacy, Purdue<br />
University<br />
Indiana University<br />
Indianapolis, IN<br />
Ross Tsuyuki<br />
PharmD, MSc, FCSHP, FACC<br />
University <strong>of</strong> Alberta<br />
Faculty <strong>of</strong> Medicine and Dentistry<br />
Edmonton, AB<br />
Régis Vaillancourt<br />
OMM, OD, CD, BPharm, PharmD,<br />
FCSHP<br />
Children’s <strong>Hospital</strong> <strong>of</strong> Eastern<br />
Ontario<br />
Ottawa, ON<br />
Kelly Walker<br />
BSP, ACPR<br />
Toronto East General <strong>Hospital</strong><br />
Toronto, ON<br />
Sandra Walker<br />
BSc, BScPhm, PharmD, ACPR, FCSHP<br />
Sunnybrook Health Sciences Centre<br />
Toronto, ON<br />
Janice Wells<br />
PharmD<br />
St. Michael’s <strong>Hospital</strong><br />
Toronto, ON<br />
Arthur Whetstone<br />
EdD, MA, BEd, BA (Hon), RPN<br />
<strong>Canadian</strong> Council on Continuing<br />
Education in Pharmacy<br />
Saskatoon, SK<br />
David Williamson<br />
MSc, BCPS<br />
Hôpital du Sacré-Coeur du<br />
Montréal<br />
Montréal, QC<br />
Rosemary Zvonar<br />
BScPhm, FCSHP, ACPR<br />
The Ottawa <strong>Hospital</strong><br />
Ottawa, ON
73<br />
The Sheraton Centre Toronto Hotel<br />
All booths are 8’ x 10’, except where noted.<br />
Floor plan subject to facility approval.<br />
79 equivalent 8’ x 10’ booths.<br />
■ RESERVED<br />
Exhibitor List (at time <strong>of</strong> printing)<br />
Liste des exposants (au moment de l’impression)<br />
Company Booth #<br />
Compagnie Kiosque #<br />
Abbott Labs ..............................................................................200<br />
Alveda Pharma..........................................................................411<br />
Apotex Inc. ...............................................................................209<br />
Amerisourcebergen Canada ......................................................402<br />
AstraZeneca Canada Inc. ..........................................................406<br />
B Braun Medical........................................................................107<br />
Baxa Corporation ......................................................................409<br />
Bayer Inc. ..........................................................................103/105<br />
Bio-K International ...................................................................500<br />
Blueprint for Pharmacy..............................................................708<br />
Boehringer-Ingelheim Canada Ltd. ....................................106/108<br />
<strong>Canadian</strong> Institute for Health Information .................................505<br />
<strong>Canadian</strong> Patient Safety Institute...............................................700<br />
<strong>Canadian</strong> Pharmaceutical Distribution Network .........................207<br />
<strong>Canadian</strong> <strong>Pharmacists</strong> Association......................................508/510<br />
Cardinal Health Canada .....................................................501/503<br />
Caverly Consulting Group .........................................................206<br />
Department <strong>of</strong> National Defence...............................................400<br />
Eli Lilly Canada Inc. ...................................................................102<br />
Fresenius Kabi ....................................................................208/210<br />
Galenova...................................................................................311<br />
Health Canada - Canada Vigilance ............................................506<br />
Healthmark Ltd. .................................................................308/310<br />
Company Booth #<br />
Compagnie Kiosque #<br />
Hospira Healthcare ......................................................305/307/309<br />
Lexicomp...................................................................................202<br />
McKesson Canada ....................................................................407<br />
Merck Canada Inc. ...................................................................203<br />
Mylan Pharmaceuticals Inc. .......................................................100<br />
North West Telepharmacy..........................................................104<br />
Northern Health ........................................................................504<br />
Omega Laboratories Limited......................................................306<br />
PCCA Canada Corp. .................................................................410<br />
Pendopharm a Division <strong>of</strong> Pharmascience Inc. ...........................111<br />
PEPID LLC..................................................................................511<br />
Pharmacy Examining Board .......................................................408<br />
Pfizer Canada Inc. ........................................112/114/213/215/509<br />
Pharmascience ..........................................................................109<br />
Pharmaceutical Partners <strong>of</strong> Canada<br />
A Company <strong>of</strong> the Fresenius Kabi Group ............................301/303<br />
Purdue Pharma..........................................................................502<br />
RxFiles .......................................................................................101<br />
Sandoz Canada Inc. ............................................300/302/401/403<br />
San<strong>of</strong>i-Aventis Canada ..............................................................204<br />
SDM Specialty Health Network..................................................205<br />
SteriMax Inc. .............................................................................404<br />
Teva Canada..............................................................................201
SES 2012<br />
A U G U S T 11 - 1 4<br />
on the<br />
la<br />
SES Sbeach<br />
SÉÉ plage<br />
à<br />
o<br />
August ust 11-14 Charlottetown 11-14 août<br />
ÉÉ<br />
h 2012
Connecting pharmacists across Canada<br />
PHARMACY SPECIALTY NETWORKS<br />
NETWORK<br />
communicate<br />
CSHP has more<br />
than 20 PSNs to<br />
join! Check out<br />
www.cshp.ca for<br />
a complete list.<br />
Join the Pharmacy Specialty Network! CSHP membership will connect<br />
you with what’s important – people and information.<br />
PSNs:<br />
• connect members with others who share a passion for a particular facet<br />
<strong>of</strong> pharmacy practice<br />
• facilitate the quick exchange <strong>of</strong> ideas, developments, methods,<br />
experiences, knowledge to improve practice<br />
• support collaboration on projects, research, and educational programs to<br />
address the needs <strong>of</strong> the members <strong>of</strong> a PSN<br />
• provide additional opportunities for members to serve as both opinion<br />
leaders and key resources for CSHP Council on pr<strong>of</strong>essional specialty<br />
issues, including development <strong>of</strong> relevant position statements, guidelines,<br />
and information papers<br />
Participation in PSNs is free <strong>of</strong> charge to CSHP members<br />
Visit MY.CSHP.ca and sign up today!
Join Us!<br />
CSHP M EMBERSHIP HAS M ANY ADVANTAGES<br />
MEMBER BENEFITS<br />
As a member <strong>of</strong> CSHP, you connect<br />
not only to a strong pr<strong>of</strong>essional<br />
organization, but also to a dynamic<br />
network <strong>of</strong> over 3,100 hospital<br />
pharmacy colleagues. When you join CSHP,<br />
you instill fresh energy into a 65-year-strong<br />
association for expanding and improving<br />
programs and services.<br />
● Advocacy<br />
● Awards <strong>Program</strong><br />
● <strong>Canadian</strong> <strong>Hospital</strong> Pharmacy Residency Board<br />
● Continuing Education<br />
● CSHP 2015<br />
● Partner Discount <strong>Program</strong>s<br />
● Fellows <strong>Program</strong><br />
● Pharmacy Specialty Networks (PSNs)<br />
● Products and Services<br />
● Pr<strong>of</strong>essional Liability/Malpractice Insurance<br />
● CSHP Research and Education Foundation<br />
For more information about CSHP member benefits, please contact:<br />
Membership services<br />
T: 613-736-9733, ext. 222 | F: 613-736-5660 | E: membershipservices@cshp.ca | www.cshp.ca