AND PLUS - University College London Hospitals
AND PLUS - University College London Hospitals
AND PLUS - University College London Hospitals
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
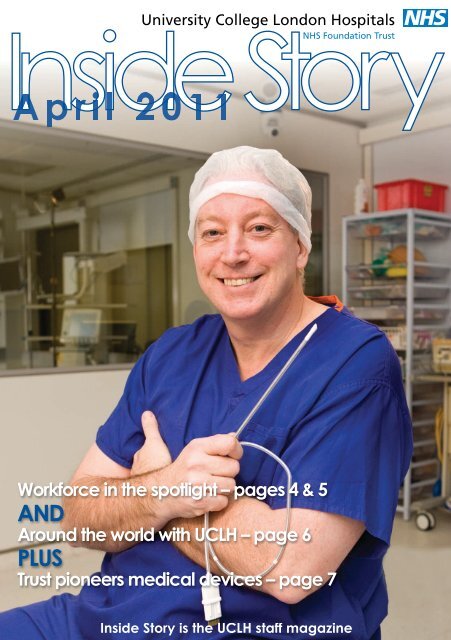
Inside Story<br />
Workforce in the spotlight – pages 4 & 5<br />
<strong>AND</strong><br />
Around the world with UCLH – page 6<br />
<strong>PLUS</strong><br />
Trust pioneers medical devices – page 7<br />
Inside Story is the UCLH staff magazine
news<br />
Evergreen tree marks cancer centre milestone<br />
An evergreen tree has been hung at<br />
the top of what will be the most<br />
advanced cancer centre in the UK to<br />
bless the building and all those who<br />
are treated there.<br />
The traditional 'topping out' ceremony<br />
at the <strong>University</strong> <strong>College</strong> Hospital<br />
Macmillan Cancer Centre marked the<br />
completion of the structure of the<br />
building which is set to open in 2012.<br />
Representatives from Skanska, the<br />
construction company, were joined by<br />
charity partners and donors as well as<br />
staff.<br />
Speaking at the ceremony Richard<br />
Murley, UCLH chairman said: “Cancer<br />
is one of the greatest challenges of<br />
our generation – it will affect one in<br />
three of us at some stage in our lives.<br />
Its state-of-the-art facilities and<br />
leading edge research and<br />
development will make all the<br />
difference in treating and surviving<br />
this disease."<br />
Cancer charity Macmillan Cancer<br />
Support is contributing £10 million to<br />
help build the centre. The Trust is also<br />
working with other charity partners<br />
including Teenage Cancer Trust and<br />
the UCLH Charitable Foundation, to<br />
help fund it.<br />
The £100 million centre will redefine<br />
the way patients are treated and there<br />
will be increased focus on the best<br />
treatments, wellbeing, rehabilitation<br />
and cancer survivorship.<br />
Phone number changes<br />
The next big milestones in the<br />
Trust-wide phone and fax number<br />
changes are:<br />
The Heart Hospital (8 May)<br />
The new number for The Heart<br />
Hospital will be 020 3456 7898<br />
All existing four digit<br />
extensions will become five<br />
digits by adding the number ‘6’<br />
(ext 6098 will become 66098)<br />
Staff must add 020 345 to the<br />
start of any Heart Hospital<br />
extension to create the full<br />
telephone number (eg 020<br />
3456 6098)<br />
NHNN (22 May) and RLHIM (5<br />
June)<br />
These sites will change over<br />
two weekends: 22 May, when<br />
the majority of<br />
the NHNN will<br />
be affected and<br />
5 June, when 33 Queen Square<br />
and the RLHIM will change<br />
All existing four digit extensions<br />
will become five digits. Most will<br />
change by adding the number ‘8’<br />
(ext 3491 will become 83491).<br />
There are some exceptions to the<br />
rule, including current 4 digit<br />
extensions begin with 87<br />
Staff must add 020 344 to the<br />
start of any NHNN extension to<br />
create the full telephone number<br />
(eg 020 3448 3491)<br />
For more information please see the<br />
project page on Insight or contact<br />
John McGhee, project manager on<br />
ext 5135.<br />
Are you a top trainer?<br />
Nominations are now open for The<br />
Chairman’s Medal for Excellence and<br />
Chairman’s Awards for Ideas and<br />
Innovation. The awards recognise those<br />
who have made an exceptional<br />
contribution to education throughout the<br />
Trust. The competition is open to all staff<br />
involved in teaching or training, including<br />
those on UCLH/UCL honorary contracts.<br />
Contact stephanie.eborall@uclh.nhs.uk<br />
for an application form. The deadline is 29<br />
April.<br />
You can now follow us at<br />
twitter.com/UCLH. Content for the channel<br />
will include a mix of news, information<br />
about events we are running and links to<br />
new content on our external website.<br />
Contact Us<br />
If you have any information you would like included in Inside Story, or on the Trust<br />
intranet site Insight, contact: Communications Unit, 2nd Floor Central, 250 Euston Road,<br />
<strong>London</strong> NW1 2PG. Email: communications@uclh.nhs.uk, Tel: ext 9897, Fax: ext 9401.<br />
Front cover: Professor Monty Mythen with<br />
the Oesophageal Doppler Monitor probe.<br />
(Story on page 7)<br />
2
news<br />
One infection is too many<br />
As part of a new zero tolerance<br />
campaign for infection prevention and<br />
control, the Trust this month<br />
announced its top ten actions for<br />
preventing healthcare associated<br />
infections.<br />
Drawing on best practice from across<br />
the NHS, the actions are designed to<br />
help the Trust achieve its goal of<br />
having no MRSA infections in<br />
2011/12. The top ten actions will also<br />
help reduce C difficile and other<br />
significant infections.<br />
A section has been developed on<br />
Insight with details of who is<br />
responsible for each action, how to<br />
comply with them and how<br />
performance will be measured<br />
The actions include: screening<br />
patients; effective risk assessment<br />
and management; inserting safe<br />
intravenous lines; hand hygiene;<br />
prescribing antibiotics properly;<br />
providing a clean safe environment;<br />
taking blood cultures the right way<br />
and excellent education and training.<br />
Sir Robert Naylor, UCLH chief<br />
executive, said: “Patients depend on<br />
us to protect them. Infection control<br />
begins with every single member of<br />
staff and individuals need to take<br />
ownership of this issue.<br />
“One infection is too many and failure<br />
is not an option. These top ten<br />
actions, which have been laid out in<br />
an easy-to-read format on Insight,<br />
give staff all the tools they need to<br />
ensure we achieve our goal. UCLH<br />
staff will be expected to comply with<br />
infection control guidance and<br />
policies and will be held to account for<br />
not doing so.” The actions will be<br />
launched on Insight soon.<br />
New QEP campaign - time is of the essence!<br />
From management meetings and<br />
surgical sessions to outpatient<br />
appointments – starting and finishing<br />
on time can have a radical knock-on<br />
effect for both staff and patients.<br />
The On Time campaign launched by<br />
Trust medical directors Dr Gill Gaskin,<br />
Dr Paul Glynne and Dr Geoff<br />
Bellingan is part of the Trust’s quality<br />
efficiency and productivity (QEP)<br />
programme.<br />
The campaign highlights the<br />
importance of starting clinic, theatre<br />
and meetings on time with no delays<br />
for patients, no overruns and no early<br />
finishes.<br />
It is already improving the service<br />
UCH surgical teams provide for<br />
patients.<br />
At the beginning of 2010, theatres lost<br />
an average of 142 hours of operating<br />
time per month due to starting lists<br />
later than planned. In the first two<br />
months of 2011 main theatres<br />
reduced this to 98 hours - a 30 per<br />
cent improvement.<br />
If it continues over the coming year<br />
this will help theatre teams to:<br />
Reduce overrunning theatre<br />
sessions, which is costly<br />
Minimise the chance of patients<br />
being cancelled on the day<br />
Help with smooth running of lists.<br />
Katie Rawlings, theatre service<br />
manager, said: “One of our theatre<br />
efficiency initiatives is a policy of zero<br />
tolerance towards late starts.<br />
“Everyone understands we are in a<br />
culture of efficiency and our systems<br />
have been refined so that patients are<br />
ready, prepped and brought down to<br />
the receiving bay as soon as a<br />
theatre is ready. The theatre coordinator<br />
for the day ensures the lists<br />
are running smoothly and slickly, with<br />
minimal lags.”<br />
3
focus on workforce<br />
Rising to the challenge ahead<br />
Staff issues are high on the agenda<br />
in the current climate; Elke Tullett<br />
looks at the burning issues facing<br />
the Trust’s workforce team.<br />
The Trust workforce team is faced with<br />
a tricky balancing act.<br />
With UCLH committed to making £45<br />
million savings over the coming<br />
financial year, it is hardly surprising<br />
that workforce costs and efficiencies<br />
will be in the spotlight more than ever.<br />
Although the Trust has made huge<br />
savings by reducing the use of agency<br />
and bank staff, overall pay still<br />
accounts for 49% of Trust expenditure.<br />
Encouraging staff survey results show<br />
most staff feel high levels of<br />
engagement and would recommend<br />
UCLH to patients and as a place to<br />
work. So how does the Trust maintain<br />
that level of morale, retain top quality<br />
staff and patient care, whilst making<br />
tough and sometimes unpopular<br />
decisions?<br />
David Wherrett, workforce director,<br />
said: “We have no option but to reduce<br />
overall workforce costs and some<br />
decisions will be easier than<br />
others.<br />
“It will be a challenge for us all,<br />
especially as UCLH has grown so<br />
significantly over recent years. To<br />
be successful we must work together,<br />
with openness and honesty, with staff<br />
and their representatives. Change,<br />
whilst unsettling, can bring new<br />
opportunities, the chance to develop<br />
new skills and work in different ways –<br />
but that is not to underestimate the<br />
challenges we face.”<br />
Although reducing the overall<br />
workforce is unavoidable, the Trust<br />
hopes to minimise any redundancies.<br />
David, who leads the Trust’s workforce<br />
team supporting managers achieve<br />
change, said his team will have to be<br />
extremely creative. Sometimes<br />
necessity is the mother of invention.<br />
A Workforce Efficiency and<br />
Productivity strategy is currently being<br />
drafted and the Mutually Agreed<br />
Resignation Scheme (MARS) is an<br />
example of one of the workstreams.<br />
Others include offering staff the the<br />
opportunity to buy additional leave, tax<br />
efficient schemes and further<br />
reductions in agency spend. Details<br />
will be posted on Insight.<br />
One of the priorities for the workforce<br />
team, and key to supporting staff<br />
during change, is reforming the Trust’s<br />
appraisals process: there is evidence a<br />
robust process improves staff morale<br />
which, in turn, improves the quality of<br />
care patients receive. Training and<br />
development programmes which help<br />
staff maximise their potential and<br />
simplifying procedures to make it<br />
easier for managers to manage are<br />
also linked to staff engagement.<br />
David added: “It is not necessarily<br />
what is happening that can negatively<br />
affect morale. It’s the sense of control<br />
and understanding that staff have of<br />
the situation. Staff need to know why<br />
something needs to be done, to share<br />
it, be part of it.<br />
“In difficult times of change and<br />
uncertainty we have to keep talking,<br />
listening and communicating with each<br />
other. Communicate, communicate,<br />
communicate – that must be our<br />
mantra.”<br />
Helping staff fulfil their potential<br />
The Trust is stepping up its<br />
commitment to achieve full take up<br />
of appraisals by launching new tools,<br />
training and simplified material.<br />
An annual appraisal provides staff<br />
with the support they need to give<br />
their best and develop and deliver<br />
against challenging goals.<br />
A new policy, launched this month,<br />
means a change in the way we<br />
approach the appraisal procedure.<br />
The workforce compliance team will<br />
support line managers with any<br />
queries they have.<br />
The policy applies to all Trust<br />
employees except medical and<br />
dental staff who are covered by<br />
other specific appraisal processes.<br />
For more information contact the<br />
workforce compliance team on ext<br />
3145 or see the workforce pages on<br />
Insight.<br />
4
focus on workforce<br />
Staff survey results<br />
The 2010 staff survey results show a marked improvement on the previous year and have identified areas where staff<br />
believe the Trust needs to perform better.<br />
The survey results have been published against 38 key findings: overall staff feedback shows the Trust is better or has<br />
stayed the same in all 38 key categories. The full results for all trusts are published on the Care Quality Commission<br />
website. Because the Trust had such a high survey response rate, professional groups and divisions/boards have been<br />
able to provide detailed information. This will be used to inform local action planning on areas needing improvement.<br />
UCLH is in the top 20% of all acute<br />
trusts for:<br />
staff recommending UCLH as a place to work or receive<br />
treatment<br />
staff who believe their role makes a difference to patients<br />
fair and effective incident reporting procedures<br />
good opportunities to develop staff potential at work<br />
good communications between senior management and staff<br />
fewer staff reporting work pressure than national average<br />
fewer staff feeling pressure to attend work when feeling<br />
unwell<br />
number of staff experiencing physical abuse from patients,<br />
relatives and the public is lower than the average<br />
The Trust also scored in the top 20% of all acute trusts for overall<br />
staff engagement – significantly better than the previous year.<br />
UCLH is in the bottom 20%<br />
of all acute trusts for:<br />
staff feeling valued by their work<br />
colleagues<br />
staff working extra hours<br />
staff receiving health and safety<br />
training<br />
staff believing the Trust provides equal<br />
opportunities for career progression or<br />
development<br />
staff using flexible working options<br />
staff experiencing harassment, bullying<br />
and abuse from staff in last 12 months<br />
impact of health and well-being on<br />
ability to perform work or daily activities<br />
staff experiencing discrimination at<br />
work in the last 12 months<br />
Mutually Agreed Resignation Scheme<br />
As part of the Trust’s plans to reduce<br />
workforce costs, staff are being<br />
offered the opportunity to apply to<br />
resign voluntarily in return for a<br />
severance payment by mutual<br />
agreement.<br />
The newly launched Mutually Agreed<br />
Resignation Scheme (or MARS) is<br />
open for a fixed period until Friday 20<br />
May, as part of our overall efficiency<br />
programme. MARS is not a<br />
redundancy, and is completely<br />
voluntary.<br />
It aims to create job vacancies which<br />
can be filled by redeployment of staff<br />
from other jobs or as an alternative<br />
employment including for those facing<br />
redundancy.<br />
David Wherrett, the Trust’s workforce<br />
director, said: “The time limited<br />
scheme is entirely voluntary for<br />
employees with individual applications<br />
considered for approval on their<br />
merits. It is intended to prompt new<br />
ways of working or thinking.”<br />
Key points on MARS:<br />
A minimum of three months and a<br />
maximum of one year’s severance<br />
pay are available, depending on<br />
length of service.<br />
It is subject to eligibility criteria and<br />
is unlikely to be agreed for any<br />
member of staff providing vital<br />
clinical or operational services.<br />
If your request for severance<br />
payment is agreed a number of<br />
conditions apply. These impact on<br />
your ability to be employed<br />
elsewhere in the NHS for the<br />
period covered by the payment and<br />
any future redundancy payments.<br />
There is no right of appeal if an<br />
application is not supported<br />
If you are interested in applying:<br />
Refer to full details on Insight and then<br />
discuss it with your line manager who<br />
will decide whether to support the<br />
application. He/she will consider<br />
whether it is in the financial and<br />
organisational interests of the<br />
department. The application also<br />
needs to be signed off by the medical<br />
director and other members of the<br />
edical director’s team. Supported<br />
applications will then be considered<br />
for approval by the finance director<br />
and workforce director.<br />
For more information contact Wendy<br />
Murphy, junior HR business partner,<br />
via email or on ext 3385.<br />
5
our trust<br />
Flying the flag for UCLH<br />
From cleaners to consultants, from midwives to managers –<br />
the UCLH workforce bring their expertise from all corners of<br />
the globe.<br />
Some have left behind families to seek a better quality of life<br />
or to escape unstable regimes. Others were lured by love<br />
…or better career prospects.<br />
The Evening Standard newspaper featured six of our staff<br />
from multi-ethnic backgrounds, dubbing them the “rainbow<br />
warriors”. It said an international workforce is vital for<br />
hospitals such as ours, to reflect the diversity of the local<br />
population. Here are some of their personal stories…<br />
France<br />
The midwife<br />
Celine Delanoue<br />
Elizabeth Garrett Anderson Wing<br />
“ I came to <strong>London</strong> from Paris in 2008 to follow my<br />
husband Hugues, who is an engineer. I was quite scared!<br />
I intended to keep working as a midwife and didn’t know<br />
if I’d enjoy working here. It’s true that in France the care<br />
has a good reputation but it’s a lot more medicalised, so<br />
a very different experience for women having babies.<br />
“Now I’m proud to work for the NHS. People give you a<br />
chance and they employ you for who you are. ”<br />
Outreach charge nurse<br />
Francis Cruz<br />
The Heart Hospital<br />
Philippines<br />
“Nurses are very well respected in the Philippines as<br />
professionals but they are very poorly paid compared to<br />
the UK. So, in 2002, I left behind my family who I love<br />
very much. But it made it easier knowing I would be able<br />
to support them – making life a little easier for all of us.<br />
"People at work are very friendly and I have been given<br />
the same opportunity as any other candidates who have<br />
applied for the same job. <strong>London</strong> is a very expensive<br />
place to live, but I find the people friendly and the NHS is<br />
an open and diverse place to work.”<br />
The business manager<br />
Bozena Corbett<br />
Eastman Dental Hospital<br />
Poland<br />
“ When I was a student I stayed with a Polish family in<br />
Ealing in 1972. I loved the atmosphere, the culture,<br />
double-decker buses, the Royal family, red phone boxes<br />
– every little bit of <strong>London</strong>. I only stayed for a few months<br />
but I dreamed of coming back to live.<br />
“I met my English husband in a ski resort where I was<br />
working as a receptionist and it was love at first sight. We<br />
married in 1976. British people in the 70s were very<br />
reserved and less accepting of foreigners.<br />
“These days we see a very different <strong>London</strong>, an<br />
integrated multicultural society. It is my privilege to work<br />
at UCLH Eastman dental hospital and assist patients with<br />
different needs including interpreting."<br />
From left: Francis Cruz, Mary Rose Falzon, Ogechi Anodu, Celine<br />
Delanoue, Nacho Ponce Rosas, Bozena Corbett<br />
Nigeria<br />
Outpatients manager<br />
Ogechi Anodu<br />
Elizabeth Garrett Anderson Wing<br />
“I came to <strong>London</strong> in 1992 from Nigeria. We moved here<br />
for a better education and economic stability. Back home<br />
we were a middle-class family with a good lifestyle. Here<br />
we went to a comprehensive school, where education<br />
and superiors were not respected.<br />
“The biggest challenge was getting used to UK culture,<br />
the way people speak, and trying to adjust my behaviour<br />
to fit in without losing who I am and where I came from.<br />
“The healthcare provided in the UK is first-class."<br />
Malta<br />
The consultant<br />
Dr Mary Rose Falzon<br />
UCH, Pathology<br />
“Coming to <strong>London</strong> from a small island was daunting and<br />
lonely but I was made very welcome by the Middlesex<br />
Hospital Medical School. It was 1978 and I came as a<br />
student to do my clinical studies.<br />
“I worked very hard as I felt I had to be better than good,<br />
being a woman and foreign. But it paid off – I’m now the<br />
only female divisional clinical director on the Medicine<br />
Board."<br />
Spain<br />
The midwife<br />
Ignacio “Nacho” Ponce Rosas<br />
Elizabeth Garrett Anderson Wing<br />
“I first came to the UK in 2006 as a nurse in A&E in<br />
Bridgend, South Wales. As a newly qualified nurse, it<br />
was difficult finding work in Spain. Over there, you only<br />
get short contracts, like holiday cover. Spain’s a bit oldfashioned<br />
and you’re seen as a freak if you leave to<br />
develop your career.<br />
“A year in Bridgend was enough! It was the same pub,<br />
the same karaoke every night. So I came to <strong>London</strong>!<br />
“Midwifery gives you a lot of satisfaction. I’ve delivered<br />
about 130 babies and participating in that special<br />
moment is great. The NHS is awesome – we’re 20 years<br />
behind in Spain. Here, women have so much more<br />
choice over childbirth.”<br />
6
Device pioneered at UCLH could save NHS millions<br />
our trust<br />
A medical device developed at UCLH<br />
has won support from the NHS<br />
Standards Authority.<br />
The minimally-invasive technology<br />
could save the NHS £850 million a<br />
year: patients recover from their<br />
surgery more quickly, are mobile, have<br />
fewer complications and can be<br />
discharged sooner. There is also<br />
evidence that it saves lives.<br />
Oesophageal Doppler Monitoring<br />
(ODM), used in major surgery and in<br />
acutely ill patients, involves a thin<br />
ultrasound probe being placed down a<br />
patient's throat.<br />
ODM accurately measures the<br />
patient's blood flow, which affects the<br />
delivery of oxygen. If the flow drops,<br />
the clinician can then accurately<br />
measure how much fluid and drugs<br />
need to be given to ensure adequate<br />
oxygen supplies to vital tissues and<br />
organs are maintained or quickly<br />
restored.<br />
Healing on the move<br />
Two consultants have been crucial to<br />
its development. Professor Mervyn<br />
Singer, Professor of Intensive Care<br />
Medicine at UCL/UCLH, invented the<br />
device. Professor Monty Mythen<br />
(pictured right), consultant in<br />
anaesthesia and critical care and<br />
director of research and development<br />
at UCLH, carried out the first clinical<br />
trial in heart surgery patients.<br />
Professor Mythen’s ongoing research<br />
into outcomes from surgery is funded<br />
by our National Institute for Health<br />
Research Comprehensive Biomedical<br />
Research Centre.<br />
Professor Mythen said: “UCLH can be<br />
rightly proud of its role in developing<br />
ODM which has culminated in the<br />
guidance published today. I have<br />
worked with ODM for over 20 years<br />
and my patients have enjoyed the<br />
benefits from better management of<br />
their fluid levels during surgery.”<br />
Recent guidance published by the<br />
National Institute for Health and<br />
Clinical Excellence (NICE) supports<br />
the use of ODM during surgery.<br />
A new ‘mobile healing’ device which<br />
could reduce length of stay, save NHS<br />
money and improve patient outcomes<br />
is being pioneered at UCH.<br />
The recyclable portable device –<br />
known as the VAC® VIA – helps<br />
speed up the healing process for<br />
From left: Patient Tawfik Shahin with Rosemary Fosah and<br />
Toby Richards<br />
patients with surgical wounds and<br />
means they can return home from<br />
hospital more quickly.<br />
The new device just launched in the<br />
UK is smaller, quieter and costs a<br />
fraction of the price compared to<br />
existing equipment which is expensive<br />
and bulky.<br />
UCH has developed a<br />
dedicated clinic where<br />
complex wounds and ulcers<br />
can be assessed and cared<br />
for by a team including<br />
surgeons, specialist nurse<br />
and podiatrists.<br />
Toby Richards, vascular<br />
surgeon, said: “Because it<br />
is a portable and<br />
disposable system, it<br />
reduces NHS costs and<br />
frees up hospital beds<br />
relieving pressure on the<br />
system. Ultimately it is<br />
better for patients to be at<br />
home recovering with their<br />
families.”<br />
A special foam dressing is<br />
placed over the wound and<br />
then connected to a<br />
lightweight disposable vacuum pump.<br />
Vacuum therapy is then applied which<br />
enhances the cleaning of the wound<br />
and helps it close.<br />
Patient Tawfik Shahin, who had a<br />
gangrenous foot infection, was one of<br />
the first in the world to benefit: he was<br />
back at home within two weeks. A golf<br />
ball sized wound was quickly reduced<br />
in size and has now completely<br />
healed.<br />
Tawfik said: “This device is beautiful. It<br />
means I don’t have to stay in hospital<br />
and can go home. My independence is<br />
really important to me and because of<br />
this device I still feel alive.”<br />
The device has benefits for community<br />
health funds too – 75 per cent of all<br />
district nursing time is spent on wound<br />
care.<br />
Rosemary Fosah, clinical nurse<br />
specialist, said: “It’s much more<br />
convenient for patients and people<br />
who need walking aids can use it with<br />
ease as it leaves their shoulders free<br />
of any strappings. It is also far less<br />
noisy which encourages patients to<br />
use it more, improving compliance ,<br />
speeding up their recovery.”<br />
7
the back page<br />
Secret lives<br />
Silver-haired Derek Mason is a<br />
walking, talking encyclopaedia of facts<br />
and figures. Want to know about Lead<br />
Belly, Woody Guthrie, or the history of<br />
skiffle and its influence on the rock ‘n<br />
roll greats down the decades? Well,<br />
Derek is the man to ask.<br />
Booted-and-suited in his office just off<br />
Queen Square, the softly spoken<br />
project architect is far removed from<br />
the world described by Fifties blues<br />
singer Lead Belly: a world of chain<br />
gangs, racial segregation in the Deep<br />
South, murder, poverty and the<br />
penitentiary. Yet the Louisiana legend<br />
has inspired not only Derek but The<br />
Beatles, Van Morrison and Bruce<br />
Springsteen, among many.<br />
Derek and his semi-professional<br />
Lonnigans Skiffle Group have just<br />
released their fifth album – a jolly,<br />
upbeat tribute to Lead Belly – which<br />
features Ralph ‘Streets of <strong>London</strong>’<br />
McTell and American folk Legend Pete<br />
Seeger. They’ve<br />
been booked to<br />
play in the Town<br />
Hall Theatre New<br />
York this autumn<br />
with other Lead<br />
Belly fans<br />
including Neil<br />
Young, Paul<br />
Simon & Suzanne<br />
Vega.<br />
When playing<br />
skiffle, Derek will<br />
grab a set of<br />
bongos, congas or<br />
a washboard –<br />
harking back to its<br />
musical roots when street-corner<br />
groups would spring up, making music<br />
with whatever everyday objects they<br />
could lay their hands on.<br />
“It started with Skiff parties in America.<br />
Poor people would try to raise money<br />
to pay the rent by playing on tea<br />
chests, cardboard boxes,<br />
anything really. It became a<br />
craze in Britain for a while<br />
… and then Bill Hayley and<br />
the Comets and rock ‘n roll<br />
swept in,” he said ruefully.<br />
Derek has been playing in<br />
bands since he was a<br />
teenager and he's appeared<br />
at the 100 Club, Royal<br />
Albert Hall, The Festival<br />
Hall,as well as on Breakfast<br />
TV and the Gloria Hunniford<br />
show.<br />
“You see someone at work<br />
in their hospital ‘uniform’ -<br />
but there’s another side you<br />
rarely find out about. That’s why I like<br />
Secret Lives,” he said.<br />
Derek has worked as project architect<br />
for 18 years at UCLH. Currently based<br />
just off Queen Square, he designed the<br />
new Molly Lane Fox brain tumour unit<br />
at the NHNN.<br />
Archives<br />
Picture entitled, Two Old Friends, 1908.<br />
Sir John Bland Sutton (1855 - 1936) and friend! He used<br />
this photograph as a Christmas card in 1908. Sir John<br />
Bland Sutton was a surgeon to the Middlesex Hospital<br />
from 1886 - 1920 and a lecturer in Anatomy. A student of<br />
the day wrote:<br />
'When other men were in the fields,<br />
At pastimes not a few,<br />
John would be found dissecting seals<br />
Or Monkeys at the Zoo.'<br />
UCLH is a winning team!<br />
The Trust’s first netball team has shot to the top of the<br />
Euston first division league table– just one year after<br />
launching.<br />
Tahlita Mabuza, a specialist in neurophysiology at UCH,<br />
formed the “All Blues” after posting a message on the<br />
Insight staff room . Nurses, physiologists and<br />
administrative staff signed up.<br />
She said: “It’s been hard work – blood sweat and tears. I<br />
dislocated a thumb, another team member twisted her<br />
ankle – but we have been determined to win!”<br />
8